Chapter 33 The Distal Phalanx and Distal Interphalangeal Joint
 Primary Pain Associated with the Distal Interphalangeal Joint
Primary Pain Associated with the Distal Interphalangeal Joint
Functional Anatomy
The distal interphalangeal (DIP) joint is a complex structure comprising not only the articulation between the middle and distal phalanges, with supporting collateral ligaments, but also the articulation with the navicular bone. It has a close relationship with the distal sesamoidean impar ligament (DSIL) and the collateral sesamoidean ligaments. The DSIL consists of bundles of longitudinally orientated collagen fibers, interspersed by synovial invaginations from the DIP joint and penetrating blood vessels.
The DIP joint can move in three planes with flexion and extension movements in the sagittal plane, lateromedial movements in the frontal plane, and rotation and sliding in the transverse plane.1,2 During normal load bearing and propulsion on a flat, level surface, DIP joint movement is principally flexion and extension. On an uneven surface and a circle, or if the foot is unbalanced, passive movements result in the distal phalanx sliding and twisting relative to the middle phalanx. Movement is restricted by the collateral ligaments of the DIP joint, the deep digital flexor tendon (DDFT), the distal digital annular ligament, the DSIL, and collateral sesamoidean ligaments. The degree of sliding and axial rotation within the DIP joint3 may predispose the horse to DIP joint injury and may explain why lameness associated with the DIP joint frequently is accentuated on a circle.
History
Lameness associated with the DIP joint may be acute or insidious in onset and unilateral or bilateral. It is more common in forelimbs than in hindlimbs but does occur in both. Lameness in horses with unilateral disease tends to be sudden in onset, but those with bilateral lameness may be evaluated because of poor performance (e.g., shortened stride, unwillingness to jump drop fences, or unwillingness to land with one forelimb leading).
Clinical Signs
The DIP joint capsule often is distended unilaterally or bilaterally. Distention of the joint capsule also can occur in clinically sound horses; therefore this finding is not pathognomonic for DIP joint pain. However, chronic distention does reflect synovitis, and treatment may reduce the risk of future problems. It is possible that chronic distention can predispose to low-grade instability of the joint. The dorsal proximal outpouching of the joint capsule can be palpated on the distal dorsal aspect of the pastern. Distention may result in obvious swelling, but it may be difficult to appreciate unless the horse has a fine hair coat. When distention of the joint capsule is present, ballottement of fluid from medial to lateral of the dorsal midline should be possible. The degree of distention may vary according to the recent work history.
Pain may be present on flexion or rotation of the distal limb joints. However, a marked reaction to distal limb flexion more likely reflects metacarpophalangeal joint pain. Mediolateral, dorsopalmar, or both types of foot imbalance are frequent findings and are considered important predisposing factors for the development of DIP joint pain. The degree of lameness varies depending on the nature of the underlying pathological change, recent work history, and whether lameness is unilateral or bilateral. With bilateral DIP joint pain the horse may move just a bit “flat” with a slightly shorter than normal stride. Severe lameness may reflect trauma to one of the supporting soft tissue structures of the joint. Lameness may be accentuated by distal limb flexion or rotation of the distal limb joints, but the response is variable. Lameness often is worse on a circle, especially on a hard surface, with the lamest limb either on the inside or outside of the circle.
Diagnosis
Local Analgesia
Pain associated with the DIP joint often improves after perineural analgesia of the palmar digital nerves and sometimes is alleviated fully. However, in some horses perineural analgesia of the palmar nerves at the level of the base of the proximal sesamoid bones is required to completely eliminate lameness.
Intraarticular analgesia of the DIP joint is not specific for pain that affects the joint itself. The potential exists for relief of pain from the navicular bone, the DSIL and the DDFT and their insertions on the distal phalanx, the palmar processes of the distal phalanx,4 and the sole, even at the toe.5,6 A standard approach is suggested to aid in interpretation of the response. A maximum volume of 6 mL of local anesthetic solution should be used. After injection through a dorsal midline approach, the horse should stand still until reassessment 5 minutes after injection. The clinician should ascertain whether sensation remains around the coronary band and whether any response to hoof testers has been eliminated to determine the specificity of the block. Lameness caused by primary DIP joint pain usually improves rapidly and substantially after intraarticular analgesia. If the lameness persists, the veterinarian should reassess the horse after an additional 5 minutes. If lameness is still apparent, the DIP joint is not a likely primary source of pain. However, after this time the block still could result in further improvement in lameness as the local anesthetic solution diffuses to adjacent structures, thereby potentially confounding the response to any other block performed at this stage.4,7 Intraarticular analgesia of the DIP joint can substantially improve lameness associated with navicular disease within 5 minutes of injection,8,9 although 20% of horses with navicular bone pain had a negative response to intraarticular analgesia of the DIP joint.8 Therefore the result of intraarticular analgesia of the DIP joint is best interpreted compared with the response to analgesia of the navicular bursa.7,8 Intraarticular analgesia of the DIP joint may not relieve pain associated with a primary injury of one of the collateral ligaments, although improvement may be seen if there is concurrent synovitis or osteoarthritis (OA).
A slight or negative response to intraarticular analgesia of the DIP joint does not eliminate completely a response to treatment of the joint, especially if the joint capsule is distended. For example, medication of the joint with hyaluronan and triamcinolone acetonide (10 mg) sometimes may resolve lameness that was not altered by intraarticular analgesia.
Retrieval of synovial fluid from the DIP joint depends on the synovial fluid pressure and position of the needle. Using a dorsal approach to the joint and a 20-gauge needle, synovial fluid usually appears spontaneously in the needle hub and, if the joint capsule is distended, may flow out under pressure. Relief of this pressure may help to resolve lameness. However, not all horses with considerable pressure within the DIP joint respond to intraarticular analgesia or medication. The pressure within the DIP joint also increases if the contralateral limb is picked up; therefore if the contralateral limb is picked up to aid restraint of the horse for injection of the DIP joint of the ipsilateral limb, a tendency for backflow through the needle puncture site may occur until the contralateral limb is placed on the ground.
Imaging Techniques
Radiography
Comprehensive radiographic examination of the DIP joint should include weight-bearing dorsopalmar, lateromedial, dorsoproximal-palmarodistal oblique, and flexed dorsolateral-palmaromedial and dorsomedial-palmarolateral oblique images of the interphalangeal joints.10 Because intraarticular analgesia may influence pain associated with the palmar processes of the distal phalanx and the navicular bone, these structures also should be evaluated carefully.
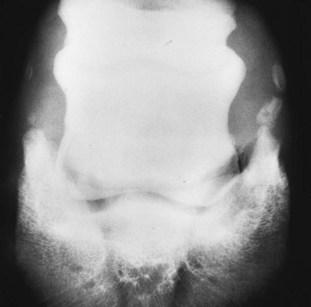
The shape of the extensor process of the distal phalanx varies considerably among horses on lateromedial images (Figure 33-1), but the shape usually is bilaterally symmetrical.10 Modeling changes of the extensor process can be present without associated lameness. Care should be taken in interpretation of the bony prominences on the distal medial and lateral aspects of the middle phalanx, which always appear larger in bigger-boned horses. Entheseous new bone at the origins of the collateral ligaments can be seen as an incidental finding. The DIP joint should be inspected carefully for recognition of small osteophytes on the distal palmar aspect of the middle phalanx and the dorsoproximal aspect of the navicular bone. Joint space congruity and the shape of the proximal articular surface of the distal phalanx should be assessed carefully. A smoothly outlined depression sometimes is seen in the middle of the proximal articular surface of the distal phalanx in clinically normal horses.
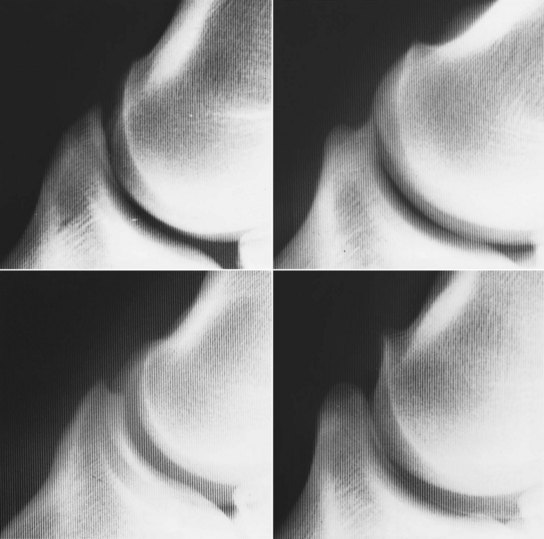
Fig. 33-1 Lateromedial radiographic images of the extensor process of normal distal phalanges. Note the variability in shape.
The flexed oblique radiographic images—dorsal 60° lateral-palmaromedial oblique and dorsal 60° medial-palmarolateral oblique—enhance detection of periarticular new bone (Figure 33-2) modeling of the distal aspect of the middle phalanx and entheseous new bone at the origin of the collateral ligaments of the DIP joint. Care is needed to differentiate between periarticular osteophytes and entheseous new bone at the insertion of the digital extensor tendon. Evaluation of the integrity and thickness of the subchondral bone plate of the middle and distal phalanges is important. Discontinuity of the subchondral bone plate may be the first radiological sign of the development of an osseous cystlike lesion. Increased thickness of the subchondral bone plate may occur with OA.

Fig. 33-2 Flexed dorsal 60° lateral-palmaromedial oblique radiographic image of the distal interphalangeal joint. There are modeling changes of the articular margins of both the distal interphalangeal and proximal interphalangeal joints.
New bone also may develop on the dorsal aspect of the diaphysis of the middle phalanx. Smoothly outlined new bone usually is subsynovial and clinically insignificant, whereas active-appearing, pallisading new bone usually is associated with lameness. Palisading is one of the earliest radiological signs but often is missed. The dorsal cortex of the middle phalanx may develop increased radiopacity (thicker), and early proliferative new bone may be seen.
Small, well-rounded mineralized opacities on the dorsoproximal aspect of the distal phalanx are not uncommon and may be present unassociated with clinical signs. Large mobile pieces are more likely to be associated with lameness.
The distal border of the navicular bone also should be evaluated carefully because the radiolucent zones along the distal border represent synovial invaginations from the DIP joint. An increase in size and number of these lucent zones has been observed with chronic synovitis of the DIP joint.
Ultrasonography
Diagnostic ultrasonography with a 7.5- to 13-MHz transducer and a standoff is invaluable for assessment of the dorsal pouch of the DIP joint, the amount of fluid within the joint, and the presence of synovial proliferation. Assessment of the palmar pouch is much more difficult, and evaluation of the articular cartilage is extremely limited. The structure of the proximal aspect of the collateral ligaments of the DIP joint proximal to the hoof capsule can be assessed,11,12 as well as the chondrocompedal, chondrocoronal, and distal digital annular ligaments. Using a transcuneal approach, the insertion of the DSIL can be assessed.13
Nuclear Scintigraphy
Nuclear scintigraphy has been useful in the identification of horses with DIP joint capsule and subchondral bone trauma. It appears to be rather insensitive to the identification of OA unless the disease is advanced.14 Increased radiopharmaceutical uptake (IRU) is best detected in lateral images.
Diagnostic Arthroscopy
The dorsal and palmar pouches of the DIP joint may be inspected arthroscopically; however, the view of joint surfaces is limited, and complete assessment of the integrity of the articular cartilage is not possible (see Figure 23-5). Access may be enhanced after joint trauma with resultant instability of the joint. Affected horses usually develop long-term lameness problems. Lavage of the joint may be beneficial therapeutically in some horses with chronic DIP joint pain without joint instability. A limited view of the DSIL can be seen from the navicular bursa.
Magnetic Resonance Imaging
Sagittal, frontal, and transverse magnetic resonance (MR) images of the DIP joint permit excellent evaluation of the articular cartilage and subchondral bone of the joint and the dorsal and palmar pouches of the DIP joint capsule (Figure 33-3). The DSIL, DDFT, collateral sesamoidean ligaments, and the navicular bone and bursa also may be assessed. Magnetic resonance imaging (MRI) is the imaging modality of choice for horses with chronic DIP joint pain that does not respond adequately to medical treatment.
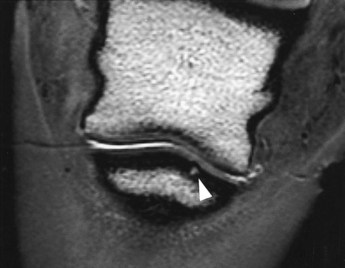
Fig. 33-3 Dorsal three-dimensional T2* gradient-echo magnetic resonance image of the left hind foot of a riding horse with lameness of 3 months’ duration. The lameness was completely resolved by intraarticular analgesia. Radiological examination was negative; scintigraphy revealed focal increased radiopharmaceutical uptake in the proximal aspect of the distal phalanx. A focal lesion is present in the subchondral bone plate of the distal phalanx (arrow).
Differential Diagnosis of Primary Distal Interphalangeal Joint Pain
Synovitis
The most common cause of DIP joint pain is synovitis, which may occur unilaterally or bilaterally. Lameness is mild to moderate in degree, and palpable distention of the DIP joint capsule usually is present. Intraarticular analgesia generally resolves the lameness. Treatment should be directed to identification of any predisposing causes. Corrective trimming to restore correct foot balance and appropriate shoeing are essential for successful management. Horses with a collapsed heel usually benefit substantially from properly fitted egg bar shoes (see Figure 30-18). The timing of trimming and shoeing can be crucial: if the feet are allowed to get too long, soreness may return.
In my experience, systemic administration of hyaluronan is generally of limited benefit in the initial treatment of horses with acute or chronic lameness, but it may have a role in longer-term management. Intraarticular medication using hyaluronan, with or without short-acting corticosteroids (e.g., triamcinolone acetonide) or polysulfated glycosaminoglycans (PSGAG), is the most effective treatment method. In horses with acute synovitis with only mild lameness, a single treatment with hyaluronan alone may be sufficient, but if the lameness is more severe or chronic, better results may be achieved with a combination of triamcinolone acetonide and hyaluronan. Improvement usually is evident within 5 days of treatment. If lameness persists, better results may be achieved by two additional injections using hyaluronan alone at weekly intervals. Intraarticular treatment with PSGAG is contraindicated if acute inflammation is present, but in horses with more chronic lameness, good results have been achieved using serial (up to five) weekly treatments.15,16 PSGAG used systemically may be useful for longer-term management. Treatment is followed by walking for 7 days and then a progressive resumption of work after the final treatment. In some horses, intraarticular therapy results in long-term resolution of the problem. Others require repeated treatments at intervals as needed.
Care is necessary during injection of the DIP joint to avoid puncturing the large vessels on the distodorsal aspect of the pastern. Puncture tends to cause localized fibrosis, and future injections are more difficult. With excellent technique, the DIP joint will tolerate well many injections, and the prognosis for future soundness is good.
Osteoarthritis
Osteoarthritis without Radiological Abnormalities
Scintigraphy may be useful in the diagnosis of early subchondral lesions associated with OA. The definitive diagnosis of OA without radiological abnormalities is possible premortem only by MRI (Figure 33-4). Horses may have signs similar to those of primary synovitis, but the degree of lameness may be more severe, especially if the horse is exerted maximally, and the response to intraarticular medication tends to be shorter and less complete. MRI may show a reduced signal intensity within the articular cartilage of the DIP joint, in addition to irregularity in the cartilage surface, with or without concurrent abnormalities in the subchondral bone. The prognosis for sustained future soundness is guarded.

Fig. 33-4 Sagittal three-dimensional T2* gradient-echo magnetic resonance image of the foot of a Grand Prix show jumper. There is loss of the normal homogeneous signal in the cartilage of the distal interphalangeal joint and irregularities in the subchondral bone in the center of the distal phalanx (arrow). Mild periarticular osteophyte formation was evident on radiographs. Scintigraphic examination was unremarkable.
Osteoarthritis with Radiological Abnormalities
Correlation is lacking between modeling in the region of the extensor process of the distal phalanx and lameness associated with the DIP joint. Enthesophytes at the site of insertion of the common digital extensor tendon should be differentiated from osteophytes. Enthesophytes may not be associated with current lameness, but may reflect chronic instability of the joint. The presence of periarticular osteophytes on the distodorsal and palmar aspects of the middle phalanx and the proximal articular surface of the navicular bone is more likely to be associated with lameness (Figures 33-5 and 33-6). Radiological evidence of OA of the DIP joint can be seen with other causes of lameness, such as navicular disease. Horses with primary OA of the DIP joint may respond better to serial treatments with PSGAG than treatment with hyaluronan and corticosteroids.15,16 However, if concurrent severe synovitis is present, primary treatment with triamcinolone acetonide and hyaluronan, followed by intraarticular PSGAG, may yield the best results. In my experience, better results are achieved in horses that are sound after intraarticular analgesia compared with horses that show partial improvement in lameness. Prognosis usually is inversely related to the severity of the radiological abnormalities.7

Fig. 33-5 Lateromedial radiographic image of the distal interphalangeal joint of a 7-year-old pleasure horse. Marked enthesophyte formation is present on the dorsoproximal aspect of the distal phalanx at the insertion of the common digital extensor tendon (arrow). In addition, there is a well-rounded fragment on the dorsal aspect of the distal interphalangeal joint (arrowhead) and modeling of the extensor process of the distal phalanx.
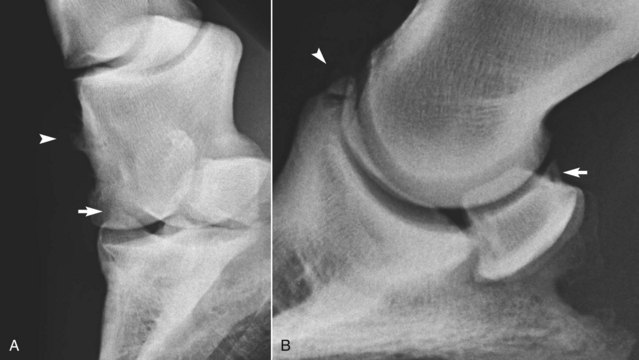
Fig. 33-6 A, Dorsolateral-palmaromedial oblique radiographic image of a flexed distal interphalangeal joint of an 8-year-old show jumper with bilateral forelimb lameness improved by intraarticular analgesia of the distal interphalangeal joints. There is modeling of the proximal articular margin of the distal phalanx (arrow), radiological evidence of osteoarthritis (compare with Figure 33-2). There is also enthesophyte formation on the dorsomedial aspect of the middle phalanx at the origin of the medial collateral ligament of the distal interphalangeal joint. No radiological abnormalities were seen in lateromedial or dorsopalmar radiographic images. B, Lateromedial radiographic image of the left front foot of a riding horse with lameness improved by intraarticular analgesia of the distal interphalangeal joint. An articular osteophyte is seen on the dorsoproximal aspect of the navicular bone (arrow), and there is a fragment on the dorsal aspect of the distal interphalangeal joint (arrowhead).
Traumatic Damage to Articular Cartilage
Sudden onset of unilateral lameness may be related to traumatic damage to the articular cartilage of the DIP joint, with or without other concurrent soft tissue damage. Definitive diagnosis is possible only with MRI. Intraarticular medication may provide temporary relief of clinical signs, but the long-term prognosis is guarded.
Joint Capsule Trauma
Traumatic damage to the joint capsule, with or without subchondral bone trauma, usually results in sudden-onset, severe lameness that persists despite rest. Lameness may be accentuated markedly when the horse turns. In the acute stage, no abnormalities are detected on radiographic examination. However, periarticular new bone may develop after several weeks (Figure 33-7). Nuclear scintigraphic examination may show generalized increased radiopharmaceutical uptake in the region of the DIP joint (Figure 33-8). Arthroscopic evaluation in these horses has been unrewarding. The response to intraarticular medication has been poor, and the prognosis for return to athletic function despite prolonged rest is guarded.

Fig. 33-7 Lateromedial radiographic image of the left front foot of a 3-year-old Thoroughbred filly with severe lameness that improved substantially after intraarticular analgesia of the distal interphalangeal joint. Entheseous new bone is seen on the dorsal aspect of the middle phalanx, in addition to the small fragment at the extensor process of the distal phalanx. Nuclear scintigraphic examination had revealed a similar pattern of uptake of the radiopharmaceutical to that seen in Figure 33-8.
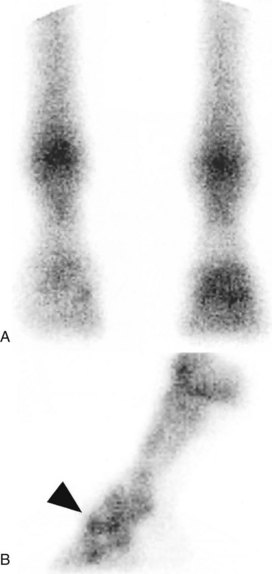
Fig. 33-8 A, Dorsal nuclear scintigraphic image of the front feet of a 6-year-old show jumper with sudden-onset, severe lameness markedly improved by intraarticular analgesia of the distal interphalangeal joint. The left forelimb is on the right. Radiopharmaceutical uptake is increased in the subchondral bone of the distal interphalangeal joint. B, Lateral scintigraphic image of the left front foot shows increased uptake of the radiopharmaceutical centered on the distal interphalangeal joint (arrow). Slight periarticular new bone formation was evident radiologically. Arthroscopic evaluation revealed synovial proliferation. The horse remained lame.
Subchondral Bone Trauma
Subchondral bone trauma may be focal or more generalized and usually is associated with unilateral lameness, which responds poorly to intraarticular medication and short periods of rest. No detectable radiological abnormalities may be apparent in the acute stage, although Ross14 described subtle proliferative changes on the distal aspect of the middle phalanx and the proximal aspect of the distal phalanx and a variable degree of subchondral lucency in the proximal aspect of the distal phalanx. Nuclear scintigraphy may be helpful.14 Several horses have been examined with acute-onset severe and persistent lameness, which was partially improved by intraarticular analgesia of the DIP joint. MRI has revealed a focal lesion in the proximal subchondral bone plate of the distal phalanx, usually axial and toward the palmar or plantar aspect (see Figure 33-3). Response to conservative management, with or without intraarticular medication or systemic treatment with tiludronate, has been poor.
Osseous Cystlike Lesions
Osseous cystlike lesions occur most often in the center of the proximal aspect of the distal phalanx, midway dorsal to palmar and axial.17,18 They vary in size and the presence of visible communication with the DIP joint. Not all are detectable radiologically; some have been identified only either using MRI or at postmortem examination after a poor response to medical treatment of the DIP joint.16 Horses with large osseous cystlike lesions may be asymptomatic but be lame at a later date. Lameness usually is unilateral, sudden in onset, and moderate to severe. Occasionally lameness is sporadic, but when present it is severe. Osseous cystlike lesions may occur in young immature horses and mature athletes. Not all osseous cystlike lesions that cause pain have active bone turnover; therefore nuclear scintigraphy may not be helpful in determining whether a long-standing osseous cystlike lesion is the current cause of lameness. However, currently or recently developing osseous cystlike lesions usually are associated with marked increased bone activity and may be evident on nuclear scintigraphic scans before radiological evidence is evident. Conservative treatment may result in spontaneous resolution of the lameness, with or without resolution of the cyst, but in some horses lameness persists, with or without enlargement of the cyst. Arthroscopic access to a cyst usually may be limited if it is in the central portion of the distal phalanx. Therefore surgical debridement of a well-defined osseous cystlike lesion usually is performed through the hoof wall. Less commonly small osseous cystlike lesions are seen on the dorsoproximal aspect of the distal phalanx, palmar to the extensor process. Such cysts located more dorsally can be debrided arthroscopically. Prognosis depends in part on the integrity of the overlying articular cartilage, and lameness persists in some horses.19,20
Palisading New Bone on Dorsal Aspect of Middle Phalanx
Pain associated with the DIP joint occasionally is associated with new bone formation on the dorsal aspect of the middle phalanx. The origin of this new bone is unknown. Arthroscopic evaluation of the joint may reveal crumbly bone, which is easily debrided, with resolution of lameness in some horses.21
Osseous Fragments on the Dorsal Aspect of the Distal Interphalangeal Joint
Small osseous fragments on the dorsoproximal aspect of the extensor process of the distal phalanx may be seen in clinically normal horses. Some are pointed proximally with a flat base and look like the tip of the extensor process, whereas others are well rounded. These fragments may represent separate centers of ossification or may be a manifestation of osteochondrosis and can be incidental radiological findings. If the fragments are seen in association with DIP joint pain, the clinical significance should be interpreted with care. Arthroscopic removal should be considered only if medical therapy of the joint fails.
Fracture of Extensor Process of Distal Phalanx
Fractures of the extensor process of the distal phalanx are discussed in the next section.
Articular Chip Fracture of the Middle Phalanx
Articular chip fractures of the medial or lateral condyle of the distal aspect of the middle phalanx occasionally cause acute-onset lameness.16 Such fractures can be detected only by flexed oblique radiographic images of the DIP joint. The prognosis after surgical removal is favorable provided joint stability has not been compromised. Surgical repair with arthroscopic guidance also is possible.
Injury of the Distal Sesamoidean Impar Ligament
Focal tears in the DSIL have been seen occasionally in association with sudden-onset, severe lameness that improves after intraarticular analgesia of the DIP joint. In horses with acute lameness, the synovial fluid may be hemorrhagic. Usually no radiological abnormalities are present. Definitive diagnosis is possible with MRI or arthroscopic evaluation of the navicular bursa.4 The prognosis for athletic function is guarded. Rupture of a hindlimb DSIL with proximal displacement of the navicular bone has been described in a French steeplechase horse.22 This horse was managed conservatively and did return to racing but then sustained an identical injury in the contralateral hindlimb.
More commonly, architectural changes of the DSIL reflecting chronic degenerative injury are seen in conjunction with other lesions of the podotrochlear apparatus, the navicular bursa, and sometimes the DDFT.23,24 There may be an axial cluster of abnormally shaped and sized radiolucent zones in the distal border of the navicular bone. Distal border fragments of the navicular bone may also be associated with DSIL pathology.25-28 Definitive diagnosis requires MRI. In low-field MR images the DSIL is difficult to evaluate because of thick slices and inferior resolution compared with high-field images. The presence of a cystic lesion in the distal third of the navicular bone, a distal border fragment, entheseous new bone at the insertion on the distal phalanx, or increased signal intensity at the insertion on the distal phalanx are good indicators of DSIL pathology.26
 Fractures and Fragmentation of the Extensor Process of the Distal Phalanx
Fractures and Fragmentation of the Extensor Process of the Distal Phalanx
History
Osteochondral fragments of the extensor process of the distal phalanx are classified as type IV fractures.1-3 Small fragments may be traumatically induced or represent a separate center of ossification or may be a manifestation of osteochondrosis. Medium-sized fragments are considered as traumatically induced or separate centers of ossification2 or a variation of the traumatically induced, nonunion fracture osseous bodies often observed in other locations on the distal phalanx in foals.4 Very large pieces involving the dorsal quarter to third of the articular surface may be developmental,5 although it has been suggested that such a fragment may be a sequela to an osseous cystlike lesion.6
These fragments involve predominantly the front feet, and lameness may be present. Small fragments can be seen as incidental radiological abnormalities. The fragments almost always are intraarticular, but they usually are nondisplaced to minimally displaced. Large fragments are most commonly seen in young horses, resulting in sudden-onset lameness soon after work commences. However, lameness may be unilateral despite the presence of fragments bilaterally.
Clinical and Imaging Findings
Low-grade lameness may be present in horses with small fragments. Lameness alleviated by intraarticular analgesia of the DIP joint was present in 16 of 21 horses with osteochondral fragments.3 Lameness may not develop until the horse is in full work when the presence of the fragment induces synovitis. The fragment is seen readily on a lateromedial radiographic image. Many fragments are removed prophylactically.3
Lameness associated with large fragments may be sudden in onset, although radiological abnormalities often appear chronic when lameness is first recognized. A strong fibrous union may maintain stability of the fragment until trauma causes minor fragment loosening. There is often marked increased radiopacity of the parent bone and extensive enthesophyte formation at the insertion of the common digital extensor tendon on the distal phalanx, reflecting chronic joint instability. In some horses the hoof shape becomes triangular or pyramidal; this clinical appearance has been described as pyramidal disease or buttress foot.2
Treatment and Prognosis
Removal of small fragments under arthroscopic guidance is a well-accepted treatment with a highly favorable prognosis.3 Lameness resolved in 14 or 16 horses with lameness associated with a small fragment, and 5 of 5 horses remained sound after the fragment was removed prophylactically.3 Horses can return to work within 2 weeks of fragment removal if surgery is prophylactic and at 10 weeks later if preoperative lameness was present.
Guidelines for treatment of horses with medium-sized fragments are less clear. Full recovery after internal fixation of these fragments was reported for two horses in four reports (six horses).1,3-5 At least one horse had an acute fracture.7 Fragment removal by dorsal midline arthrotomy has been reported in 14 horses with a successful outcome in 8 (57%).1 Of the six horses with unfavorable results, preoperative duration of lameness exceeded 2 years in three horses, suggesting more favorable results might be expected if preoperative lameness duration were shorter. Horses usually return to full work by 4 months after surgery. Prognosis for large fragments is guarded.
 Injuries of the Collateral Ligaments of the Distal Interphalangeal Joint
Injuries of the Collateral Ligaments of the Distal Interphalangeal Joint
Desmitis or desmopathy of the medial and/or lateral collateral ligament of the DIP joint results in a variable degree of unilateral or bilateral lameness in forelimbs or, less commonly, hindlimbs.1-6 The injury is believed to be caused by the biomechanical forces of sliding and rotation of the joint (e.g., lateral sliding of the distal phalanx and medial rotation, which causes the medial collateral ligament to undergo great strain), sometimes superimposed on a primary degenerative lesion.7,8 Degenerative changes are more prevalent toward the insertion of the ligament than farther proximally and include chondroid metaplasia and a unique fissuring necrosis, with cleft formation at the bone ligament interface. There may be osseous resorption at the insertion on the distal phalanx.7 Medial injuries are more common than lateral, probably reflecting biomechanical loading. Severe damage to the body of the ligament results in obvious periligamentous soft tissue swelling and pain immediately proximal to the coronary band, but with many injuries there are no palpable abnormalities. Detection of joint instability is occasionally possible with severe injury. There is an association between extensive ossification of one or both cartilages of the foot and collateral ligament injury.9
In horses with severe lameness the caudal phase of the stride is shortened at the walk; at the walk the stance phase is longer than at the trot, resulting in increased extension of the DIP joint and greater stress on the collateral ligaments. At the trot lameness is generally much worse on a circle compared with straight lines, especially on a firm surface. In some horses lameness is improved by palmar digital nerve blocks, but in others palmar (abaxial sesamoid) nerve blocks are required to abolish the lameness. Intraarticular analgesia of the DIP joint may improve lameness if there is associated synovitis or secondary OA. In some horses desmitis of the body of the medial or lateral collateral ligament can be identified ultrasonographically and is characterized by enlargement in the cross-sectional area of the ligament and a diffuse reduction in echogenicity or a hypoechogenic core lesion, with or without thickening of the periligamentar soft tissues (Figure 33-9). Enthesophyte formation at the origin on the middle phalanx may also be seen ultrasonographically or radiologically (see Figure 33-6, A). However, only a limited length of the ligament can be evaluated using ultrasonography, and there are many false-negative results. Placing a wedge under one side of the foot may enable a greater length of the contralateral ligament to be evaluated than if the foot is bearing weight uniformly. In a few horses a well-defined osseous cystlike lesion has been identified in the distal phalanx at the site of insertion of a collateral ligament and rarely an osseous cystlike lesion at the origin in the middle phalanx.
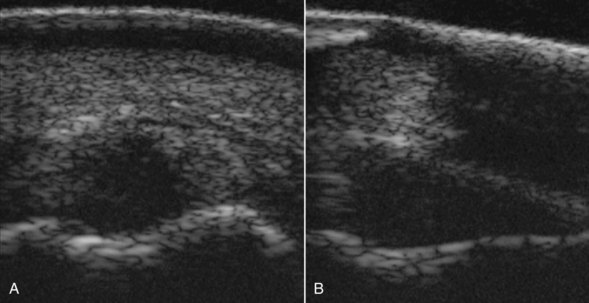
Fig. 33-9 Transverse (A) and longitudinal (B) ultrasonographic images of the lateral collateral ligament of the distal interphalangeal joint of a 10-year-old show jumper with acute-onset, severe lameness, worst on a circle. The ligament is enlarged, and a large proportion of the ligament is anechogenic.
Focal IRU in the distal phalanx in the region of insertion of a collateral ligament is a good indicator of the presence of an injury, although not necessarily involving the insertion.10 However, in many horses MRI is required for definitive diagnosis. Care should be taken when interpreting low-field images obtained in a standing horse because the magic angle effect may result in artifactual increased signal intensity in the lateral collateral ligament.11,12 Magic angle effect may also influence the appearance of high-field MR images in the most proximal aspect of the collateral ligaments.13 Confirmation of genuine injury requires identification of changes in size, shape, and signal intensity in T1- and T2-weighted images, and also in fat-suppressed images in acute injury. There may be entheseous and/or endosteal reaction at the origin and/or insertion. In some horses there is also evidence of bone trauma of the ipsilateral side of the middle or, more commonly, the distal phalanx characterized by diffuse decreased signal intensity in T1-weighted images and increased signal intensity in fat-suppressed images.14,15 Osseous cystlike lesions may develop at the origin, or more commonly the insertion, many of which are not detectable radiologically and are only seen using MRI.
Treatment is box rest for a minimum of 2 months followed by at least 4 months of walking exercise, predominantly in straight lines. Longer convalescence may be preferable.16 In horses with very severe injuries, consideration should be given to application of a foot cast. OA of the DIP joint is a potential sequel if there is instability of the joint. When the medial collateral ligament is damaged, a shoe with a wide medial branch and narrow lateral branch is recommended. For lateral collateral desmopathy, a shoe with a wide lateral branch with a lateral extension and a narrow medial branch is preferred. Medication of the DIP joint is indicated if there is evidence of synovitis or OA. Shock wave or radial pressure wave therapy is popular, although efficacy is questionable.16 A nonsignificant improvement in treatment success was seen in horses treated by either shockwave therapy or radial pressure wave therapy compared with horses managed conservatively.16 Surgical treatment of radiographically evident osseous cystlike lesions has been disappointing.17 Palmar neurectomy has resulted in resolution of lameness in horses that had failed to respond to conservative management, and to date no untoward side effects have been seen.16
The prognosis for return to athletic function is guarded to fair for horses with injuries that affect primarily the body of the ligament. Horses with acute injuries probably have a more favorable prognosis than those with chronic injuries.6,15,16 Overall 47.8% of 69 horses with primary injuries of one or both collateral ligaments returned to full athletic function; 51% of horses with increased signal intensity in fat-suppressed images returned to full function.16 In a different study 60% of 20 horses, all with increased signal intensity in fat-suppressed images in the injured ligament, returned to full athletic function.6 The presence of osseous abnormalities associated with collateral ligament injury did not influence outcome overall, although there was an association between excellent outcome and the presence of entheseous new bone at the insertion on the distal phalanx.16 The coexistence of other injuries within the digit resulted in a much poorer prognosis.16 The prognosis for horses with joint instability, or radiological abnormalities consistent with OA of the DIP joint, is also more guarded. There are anecdotal reports of treatment by stem cell injection, but no reports of clinical efficacy. Although primary traumatically induced injuries unquestionably occur, there is evidence of degenerative pathological change, especially toward the insertion of the ligament in horses that have failed to respond to treatment.7
 Osseous Cystlike Lesions in the Distal Phalanx
Osseous Cystlike Lesions in the Distal Phalanx
History
Osseous cystlike lesions in the distal phalanx usually are unilateral, solitary, and range in location from the extensor process to deep within the weight-bearing surface. Debate continues on whether the lesions have a traumatic or developmental origin. When large bilateral lesions are present in a young horse, a developmental component is strongly suggested.1-3
Clinical and Imaging Findings
Affected horses often are young but mature, and acute-onset, moderate to severe lameness frequently is present. Less commonly the history includes low-grade, intermittent lameness. Occasionally osseous cystlike lesions are identified as incidental radiological findings. Osseous cystlike lesions sometimes are seen in older horses with pain localized to the foot. Such lesions may be clinically significant. Lameness may be exacerbated by distal limb flexion, but results of hoof tester examination usually are negative. Lesions are seen more commonly in the forelimbs, although the hindlimb was affected in 3 of 15 horses in one report.1 Effusion of the DIP joint occasionally is present, and large bilateral lesions sometimes are associated with a buttress foot appearance.
Lameness often is unaltered by perineural analgesia of the palmar digital nerves, but it is resolved by palmar (abaxial sesamoid) nerve blocks. Intraarticular analgesia of the DIP joint improves lameness associated with osseous cystlike lesions that communicate with the joint. Small articular lesions may not be detectable radiologically, but large osseous cystlike lesions usually are readily identifiable on dorsoproximal-palmarodistal (upright pedal) images. Lesions involving the extensor process are seen readily on lateromedial images. Smaller osseous cystlike lesions located in a very medial or lateral location within the more weight-bearing aspect of the joint are best identified in weight-bearing dorsopalmar images. Nuclear scintigraphic examination may identify small osseous cystlike lesions that are not identifiable radiologically. Osseous cystlike lesions may be associated with IRU, depending on the stage of lesion development and activity of the surrounding bone. However, an osseous cystlike lesion that is scintigraphically silent still may be a cause of lameness. Some lesions can only be identified using MRI.
Treatment and Prognosis
Reports documenting results after either conservative or surgical treatment are limited. In one study, conservative treatment resulted in clinical improvement in approximately 30% of horses, but the prognosis for full recovery was guarded.1 One report documented favorable results in a horse with bilateral extensor process fragmentation through what were presumed to be preexisting cystic lesions in the extensor processes.4 Anecdotally, arthroscopic debridement of smaller extensor process lesions can be associated with full return to function.5 Many lesions are not accessible by arthroscopy or arthrotomy through a dorsal approach. Debridement of distal phalanx lesions through the hoof wall has been described,6 but this approach has not gained universal acceptance. However, good results have been achieved in a limited number of horses.7 Arthroscopic debridement of centrally located lesions was successful in 10 of 11 horses (91%) 16 to 33 months of age.8 Intraarticular medication can be useful in the ongoing management of selected horses; occasionally conservative treatment results in a horse suitable for a limited amount of riding activity.
 Osseous Trauma of the Distal and Middle Phalanges
Osseous Trauma of the Distal and Middle Phalanges
Osseous trauma of the middle or distal phalanges usually results in acute-onset, moderate to severe lameness.1,2 There are usually no localizing clinical signs. The response to perineural analgesia depends on the location of injury. Diagnosis usually requires MRI, although there may be IRU at the site of injury. Lesions are characterized by an area of increased signal intensity in the cancellous bone in fat-suppressed images, with a corresponding region of low signal intensity in T1-weighted images and sometimes T2* = weighted images (Figure 33-10). The most common site is the distal dorsal aspect of the middle phalanx.3 However, lesions also occur in the distal phalanx, involving especially the palmar aspect, with or without involvement of the navicular bone. These injuries may occur alone or in association with related soft tissue injuries, such as collateral ligament injury. Extensive ossification of a cartilage of a foot may be a risk factor for osseous trauma of the ipsilateral aspect of the distal phalanx.4-6 Lameness is often very slow to resolve, but in horses with uncomplicated injuries the prognosis is usually favorable, unless there was associated damage of the subchondral bone plate. There are anecdotal reports of beneficial effects of treatment by intravenous infusion of tiludronate.
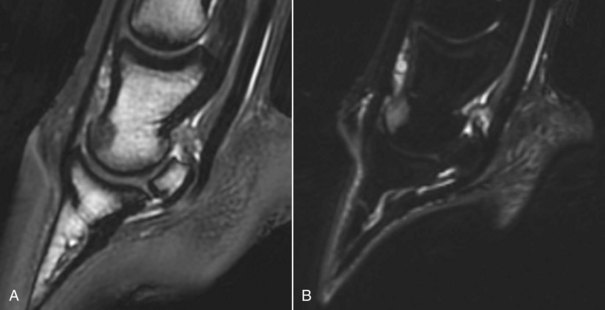
Fig. 33-10 Sagittal T2*-weighted spoiled gradient-echo (A) and short tau inversion recovery (STIR) (B) magnetic resonance images of a 6-year-old show jumper with acute-onset left forelimb lameness abolished by palmar digital analgesia. Radiographic and ultrasonographic examinations revealed no detectable abnormality. There is reduced signal intensity in the dorsal distal aspect of the middle phalanx in the T2*-weighted image and increased signal intensity in the STIR image, consistent with bone trauma.
 Keratomas and Neoplastic and Nonneoplastic Space-Occupying Lesions in the Hoof
Keratomas and Neoplastic and Nonneoplastic Space-Occupying Lesions in the Hoof
Keratomas are classified as aberrant, possibly hyperplastic, keratin masses originating from epidermal horn-producing cells of the coronary band.1 They also have been defined as benign neoplasms originating from the coronary dermis.2 As the abnormal horn tubules grow distally toward the toe, hoof wall deformation may occur with disruption of the white line, which may permit entry of infection. Expansion of the mass results in pressure necrosis of the adjacent distal phalanx. Keratomas occur most often in the dorsal half of the foot.3 A keratoma is the most common space-occupying lesion in the hoof, but other neoplastic conditions occur occasionally and result in similar clinical signs, although they usually can be differentiated radiologically.4-8 Other nonneoplastic space-occupying lesions, such as epidermal inclusion cysts and fibrous dysplasia, have been identified that can be differentiated from a keratoma only by histological examination.9
History
Often mild intermittent forelimb or hindlimb lameness exists, or more severe episodes of lameness associated with recurrent subsolar abscessation may have occurred.2,3,10-12 Neoplastic conditions may be associated with more severe lameness. Distortion of the hoof capsule may have been noted.
Clinical Signs and Diagnosis
The hoof capsule, the white line, or both may be distorted but not invariably. Pressure applied with hoof testers may elicit local pain. A variable degree of lameness is present that is alleviated by desensitization of the foot or unilateral palmar block on the side of the lesion. Radiographic examination may reveal a smoothly demarcated radiolucent defect in the margin of the distal phalanx (Figure 33-11). This characteristic is typical of keratomas or other nonneoplastic space-occupying lesions, whereas neoplastic lesions tend to have more irregular margins and may be associated with new bone formation.8 Infectious osteitis of the distal phalanx may have a similar appearance, although if the osteitis is chronic, marginal sclerosis with or without new bone formation may be present. The crena at the toe of the distal phalanx should not be confused with a space-occupying lesion. Lesions are best detected in dorsoproximal-palmarodistal oblique, dorsolateral-palmaromedial oblique, or dorsomedial-palmarolateral oblique radiographic images. A keratoma also may be present in the absence of radiological change with only distortion of the hoof capsule.3 If the clinical significance of such a radiological lesion is in doubt, nuclear scintigraphy may be helpful because such lesions usually are associated with focal IRU. Diagnostic ultrasonography also has been used to identify a keratoma at the coronary band.13 Small keratomas that were not detected radiologically have also been identified using MRI, although not all are of clinical significance.14 Occasionally other space-occupying lesions in the more palmar aspect of the foot are only identified in a palmaroproximal-palmarodistal oblique radiographic image of the palmar processes of the distal phalanx.
Treatment
Horses with keratomas and other benign space-occupying lesions respond well to surgical excision and have a good prognosis,* but those with neoplastic lesions have a more guarded prognosis. It is best to excise keratomas and other space-occupying lesions through a hoof wall rather than solar approach, if possible. Partial hoof wall resection for keratoma removal was associated with fewer postoperative complications and a more rapid return to athletic function compared with complete hoof wall resection.16
 Fractures of the Distal Phalanx
Fractures of the Distal Phalanx
Fractures of the distal phalanx are a relatively common cause of lameness in horses from all disciplines and often are the result of trauma, through a misstep or high-speed impact, or kicking a fixed object.1-13 Fractures have been classified into six types,1,2 but other configurations also occur. Fractures of the extensor process of the distal phalanx (type IV) are discussed elsewhere (see page 355). Fractures of the solar margin of the distal phalanx (type VI), which may occur in foals or adults, are considered separately from fractures of the body of the bone. The latter may be articular or nonarticular and may comprise sagittal (type III), oblique (extending from the midline to the lateral or medial solar margin) (type II), and comminuted fractures (type V), fracture of a palmar process (type I), and, less commonly, fractures of other configurations.
Fracture of the Solar Margin of the Distal Phalanx
Foals
Fractures of the palmar-most aspect of the palmar process of the distal phalanx occur commonly in foals.3,4 These fractures originate at the incisure (which normally separates the proximal and distal palmar process angles), continue dorsally toward the toe for 1 to 3 cm, and then extend to the solar margin. They are believed to be caused by shear forces generated by tension of the DDFT or by compression of the solar cortical surface and tension on the dorsal cortical surface during weight bearing. One hypothesis is that excessive trimming of the heel, thus increasing tension in the DDFT, or excessive trimming of the sole of the frog, thus increasing concussion on the distal phalanx and forces on the palmar processes, may be predisposing factors to these fractures, but this was not substantiated in a clinical study, perhaps because of the high overall incidence of fractures (34%).5
Clinical Signs and Diagnosis
Lameness usually is mild and extremely transitory, lasting only 1 to 2 days, and may precede radiological identification of a fracture. No consistent response to pressure applied with hoof testers at the heel is present. Diagnosis is based on radiological identification of a discrete osseous body at the palmar process. Fractures may be identified on lateromedial radiographic images, but dorsal 65° proximal-palmarodistal oblique radiographic images are more sensitive. Not all fractures are detectable radiologically.
Adult Horses
Fractures of the solar margin of the distal phalanx in adult horses occur from the quarters toward the more dorsal aspect of the distal phalanx; these fractures also are referred to as cracking off.2,6 These fractures may heal, be resorbed, or persist without signs; therefore radiological identification of solar margin fragmentation is not necessarily synonymous with identification of the source of pain causing lameness. Solar margin fractures occur almost exclusively in forelimbs. A geographical influence on the incidence of solar margin fractures is apparent, which may reflect the footing on which the horses work or other undefined factors. In the Editors’ experience, these fractures are rare, whereas a study in California of distal phalanx fractures in 274 horses identified 132 (48%) horses with solar margin fractures. However, these fractures frequently occurred in association with radiological evidence of laminitis or another potential cause of lameness, such as navicular disease.6 Solar margin fractures as the sole potential cause of lameness were identified only in 25 horses. Irregularity and reduced opacity at the solar margin, with widening of the vascular channels, may be a predisposing factor.
Clinical Signs and Diagnosis
Horses with solar margin fractures often have a history of foot soreness. With an acute solar margin fracture, there may be increased sensitivity to hoof testers at the toe, provided that the sole is not excessively hard. Lameness is removed by perineural analgesia of the palmar nerves in the proximal pastern region or at the level of the proximal sesamoid bones. Diagnosis depends on radiological identification of the fracture or fractures, which may be single or multiple and may affect a variable extent of the solar margin. Primary solar margin fractures usually are single, whereas those that occur in association with laminitis or radiological evidence of demineralization of the solar margin are more likely to be multiple, comminuted, or both. Fractures are identified readily in an appropriately exposed dorsoproximal-palmarodistal oblique radiographic image, but they are overlooked easily if the radiograph is overexposed. The radiographs should be inspected carefully to detect evidence of any other potential cause of lameness that may influence treatment and prognosis.
Treatment
Horses with lameness associated with a solar margin fracture usually require prolonged rest, especially if radiological evidence of preexisting demineralization of the solar margin is present; healing is assessed by periodic radiographic examination. The use of a broad web shoe with a concave solar margin, with or without pads, is recommended. Limited documented long-term follow-up information is available for horses with primary solar margin fractures, but the prognosis generally is favorable.
Fractures of the Body of the Distal Phalanx
Fractures of the body of the distal phalanx occur more commonly in forelimbs than hindlimbs, but they are not uncommon in either limb.1,2,7-13 A fracture of the body of the distal phalanx usually results in acute-onset, severe lameness, but nonarticular fractures of a palmar process of the distal phalanx can occur without severe lameness.13 If the fracture is articular, the DIP capsule may be distended. Pain usually occurs when pressure is applied with hoof testers, but this finding may not be a feature of a nondisplaced fracture of a palmar process, especially if it has been present for more than several days. Articular fractures invariably result in continuous lameness, but a nonarticular fracture of a palmar or plantar process of the distal phalanx may be associated with intermittent lameness, especially in a hindlimb. Clinical signs of an articular fracture usually reflect foot pain, and thus regional analgesia often is not required; however, with nonarticular fractures the clinical signs may be less specific, and perineural analgesia is usually required to determine the source of pain. Some palmar process fractures heal only by fibrous union and not osseous union. The radiological identification of a fracture that has healed by fibrous union, which does not have the appearance of a narrow, clearly defined line, should be interpreted with care. Although such a fracture may be unstable and therefore a potential source of pain, the pain causing lameness may not necessarily be related to the fracture.
Fractures of the distal phalanx are a common racehorse injury in North America. Fractures occur most often in the lateral aspect of the left front foot and the medial aspect of the right front foot in association with the counterclockwise direction of training and racing.12 Fractures of the distal phalanx in the hindlimb in racehorses occur most commonly in the medial aspect of the foot.12 In sports horses and general purpose horses, fracture of the medial palmar process of the distal phalanx occurs most commonly.13
Diagnosis
Diagnosis is based on radiological identification of a fracture (Figures 33-12 and 33-13). A very recent nondisplaced fracture may be difficult to identify radiologically unless the x-ray beam is completely parallel to the fracture line, and many oblique images may be required. The foot should be cleaned thoroughly before radiographic examination to avoid artifacts. The frog clefts may create confusing lucent lines across the distal phalanx; therefore the foot should be packed with a moldable modeling compound (e.g., Play-Doh, Hasbro, Inc., Pawtucket, Rhode Island, United States). Many articular fractures are seen readily on dorsoproximal-palmarodistal oblique radiographic images, but fractures of the palmar processes and other less common configurations of fracture may not be apparent. A fracture of a palmar process may be evident on a lateromedial radiographic image, but oblique radiographic images of the palmar process are required in many horses. Most of these fractures can be detected in dorsal 30- to 45° lateral (or medial)-palmarodistal oblique radiographic images with the foot either bearing weight or in the upright pedal position, but occasionally oblique views are required with the horse standing on the x-ray cassette (e.g., dorsal 45°/proximal 45° lateral-palmarodistal medial oblique radiographic images). Separate centers of ossification at the palmar aspect of the palmar process should not be confused with a fracture.10 Rarely a palmar process fracture is seen only in a palmaroproximal-palmarodistal oblique radiographic image. Occasionally obscure incomplete, nonarticular fractures of the body of the distal phalanx are identified in a palmaroproximal-palmarodistal oblique view.

Fig. 33-12 Dorsoproximal-plantarodistal oblique radiographic image of a left hind foot. The distal phalanx has a complete, articular, parasagittal fracture.

Fig. 33-13 Dorsomedial-plantarolateral oblique radiographic image of a left hind foot. There is an incomplete, nondisplaced, nonarticular fracture of the medial plantar process of the distal phalanx (arrow). This was not seen on standard radiographic images.
Nuclear scintigraphic examination usually is unnecessary for the identification of most acute fractures, except those causing episodic lameness, but can be helpful in confirming the likely clinical significance of older fractures.14 Scintigraphy also is useful for identification of subchondral bone trauma unassociated with detectable radiological abnormalities (see following text).
Although the majority of fractures of the distal phalanx are radiologically detectable, occasionally unusual configurations or locations have only been identified using MRI (e.g., an incomplete nondisplaced fracture on the axial aspect of a palmar process of the distal phalanx).15
Treatment and Prognosis
Conservative treatment of horses with nonarticular palmar process fractures, by box rest and use of a bar shoe with five clips or bar rim shoe, has a good prognosis. Complete healing of the fracture may not be evident radiologically for several months, but most fractures eventually do heal. Horses with fractures extending into the medial or lateral extremity of the DIP joint also have a good prognosis with conservative management. The horse should continue to be shod with a bar shoe when work is resumed to reduce the risks of reinjury. If a bar shoe is replaced by an open shoe, avoidance of maximum work intensity may be preferable until the hoof capsule and distal phalanx have had time to adapt to altered concussive forces. Although sagittal and oblique articular fractures of the distal phalanx often heal well if treated conservatively in horses younger than 3 years of age, the prognosis for adult horses is more guarded, and internal fixation using a lag screw technique is recommended.1,7,9,12 Prognosis depends on whether displacement at the articular margin exists; displacement inevitably results in OA and associated lameness. Potential complications include postoperative infection and screw irritation or rejection. The use of a headless titanium Herbert cannulated screw (Zimmer Corp., Warsaw, Indiana, United States) may result in fewer complications.16 Complete fracture healing requires 6 to 12 months of convalescence with surgical management.
Comminuted Fractures
Comminuted fractures of the distal phalanx are not common1,2,7 but do occur occasionally. Many radiographic images may be required to establish the precise configuration of the fractures and determine possible articular involvement, which results in a more guarded prognosis. The configuration of the fracture determines whether internal fixation is a viable option.7,12
Fractures of the Distal Phalanx Associated with Penetrating Injury
A penetrating injury of the foot (see Chapter 28) may result in a fracture of the distal phalanx of any configuration. Treatment is dictated by the fracture configuration. The primary aim is to control infection. Removal of small bone fragments that otherwise may sequestrate may be preferable.
Subchondral Trauma of the Distal Phalanx
Some horses have forelimb lameness, usually unilateral, associated with pain localized to the foot but no clinically significant detectable radiological abnormality. Nuclear scintigraphic examination reveals a focal round or semicircular area of IRU, seen in a solar image, either medially or laterally, far removed from the DIP joint, or on a lateral image in the center of the bone in a similar location to fractures.17 This lameness is believed to reflect subchondral bone trauma and is an injury that occurs particularly in racehorses in North America but also in other types of horses. Lameness usually is unaffected or, less commonly, only partially affected by intraarticular analgesia of the DIP joint. In some horses, mediolateral foot balance may be a predisposing factor. Less commonly the onset of lameness is associated with trauma. The failure to identify a fracture radiologically may reflect the inherent limitations of radiography. Alternatively, such reactions may indicate that distal phalangeal fractures, especially in racehorses, may not be single-event episodes but rather the result of stress remodeling. Treatment comprises rest and correction of any mediolateral foot imbalance. Floating the heel of the affected side may be helpful. The prognosis is favorable given sufficient time, which is proportional to the duration of lameness before diagnosis and treatment. In horses with acute lesions a period of 6 to 8 weeks of box rest and controlled walking exercise usually is sufficient, with a progressive increase in work intensity thereafter; however, in those with more chronic lesions a longer period may be necessary, and repeated scintigraphic evaluation may be helpful to determine when the lesion is no longer active.
 Pedal Osteitis: Does It Exist?
Pedal Osteitis: Does It Exist?
Pedal osteitis strictly means inflammation of the distal phalanx and has long been suggested as a cause of forelimb lameness. However, it is a poorly defined condition, previously diagnosed radiologically, characterized by focal or general demineralization around the solar margin of the distal phalanx and widening of the vascular channels, with or without abnormal lucent areas in the palmar processes. It is now recognized that considerable variation exists in the radiological appearance of the distal phalanx in normal horses.1-3 No good studies correlate foot conformation and the radiological appearance of the distal phalanx. It is my impression that those horses with a particularly thin sole, especially in association with a horizontal orientation of the solar margin of the distal phalanx, seem prone to foot soreness if worked regularly on hard ground, but the source of pain has been poorly defined. Radiological changes of the distal phalanx, once established, often persist over the long term and therefore are not synonymous with active inflammation. Radiographs represent a historical record of previous activity or injury. Scintigraphic examination of a large number of horses with foot pain occasionally has revealed evidence of abnormal bone turnover around the solar margins of the distal phalanx or confined to the palmar processes (see page 363).4 In those horses with IRU around the solar margin of the distal phalanx in solar views, correlation with other clinical signs and radiological findings frequently is poor unless the condition is localized to the toe, when it often reflects laminitis. The relevance of this finding in the absence of localizing clinical signs remains open to question because it also is seen in clinically normal horses. Pedal osteitis tends to have been used to describe a cause of lameness, when frequently the cause is actually undetermined.5 The cause of pedal osteitis has not been defined, although abnormal concussion has been suggested.
Therefore I suggest that the term pedal osteitis is inappropriate and should not be used to describe a cause of lameness on the basis of radiological findings alone. Nonetheless, a variety of radiological changes of the margins of the distal phalanx can be identified, the causes of which are poorly defined. With our current state of knowledge, attribution of lameness to these radiological changes seems inappropriate unless localizing clinical signs, or concurrent evidence of ongoing inflammation with or without abnormal bone turnover, are documented scintigraphically or using MRI. Abnormalities of one or both palmar processes of the distal phalanx have been identified using MRI (see Osteitis of the palmar processes of the distal phalanx), with irregularity of the cortices and alteration of signal intensity, but only rarely have these been considered to be the primary source of pain causing lameness.6,7 There is an association between extensive ossification of the cartilages of the foot and trauma of the distal phalanx, usually involving the palmar processes.8,9
Chronic laminitis may be associated with modeling of the toe of the distal phalanx and bone resorption with or without new bone on the dorsal aspect at the toe. Mineralization also has been identified on the dorsal aspects of the distal phalanx, midway between the coronary band and the solar margin; mineralization is seen best on lateromedial or slightly oblique radiographic images. This may represent mineralization in the dermal laminae or formation of new bone on the dorsal cortex of the distal phalanx. Extensive mineralization has been associated with lameness, but some roughening of the dorsal cortex in the region of the parietal sulci may be an incidental finding. Some horses with a clubfoot conformation develop focal loss of bone around the solar margin at the toe of the distal phalanx, as well as new bone on the dorsal aspect of the bone, associated with chronic lameness on hard ground. I suggest that in these conditions the radiological changes should be described and attributed to the primary cause rather than labeled as pedal osteitis. Many horses with poor foot conformation suffer chronic lameness, probably associated with abnormal concussion to both the soft tissue and bony elements of the hoof. Identification of the primary cause of the problem and admission that the precise source or sources of pain cannot be defined are preferable to use of the term pedal osteitis, which implies a definitive diagnosis.
 Osteitis of the Palmar Processes of the Distal Phalanx
Osteitis of the Palmar Processes of the Distal Phalanx
Anatomy
The palmar processes or angles of the distal phalanx are prism-shaped masses that project backward on the medial and lateral aspects of the bone. Each is divided into upper and lower parts by a notch or is perforated by a foramen that leads to the dorsal groove of the distal phalanx. The cartilages of the foot attach to the proximal border of each palmar process. In a normal horse, the solar and abaxial surfaces of the palmar processes are relatively smooth.
Osteitis of the palmar processes of the distal phalanx may be part of what has been called the “pedal osteitis complex,” related to the long toe–low heel syndrome. Its origin is poorly understood. It occurs almost exclusively in the forelimbs and may result in irregular roughening of the bone surface (Figure 33-14, A).
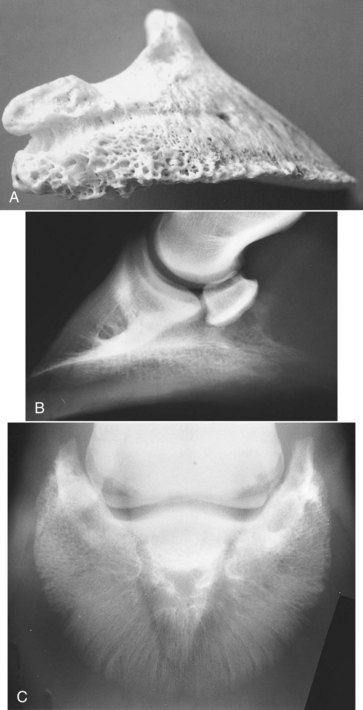
Fig. 33-14 A, The distal phalanx of a horse that had chronic heel pain. The palmar process has a roughened surface, and new bone is evident on the solar surface. B, Lateromedial radiographic image of a foot of an 8-year-old Selle Francais with recurrent heel pain. Note the orientation of the solar surface of the distal phalanx: the palmar process is lower than the toe, and the solar aspect of the palmar processes has an irregular contour. C, Dorsoproximal-palmarodistal oblique radiographic image of the same foot as shown in B. There is a very distinct trabecular pattern in the palmar processes, with many small lucent areas.
History and Clinical Findings
Lameness often is bilateral, insidious in onset, and tends to be worst on hard ground, similar to navicular disease. Affected horses often have poor conformation of the feet, with low, collapsed heels. The sole may be very flat, thin, and readily compressible. If the sole is readily compressible, pressure applied with hoof testers may be resented, but this usually is not a localized response.
Diagnosis
Diagnosis requires a combination of response to nerve blocks, radiography, and, ideally, nuclear scintigraphy and MRI.1-7
Local Analgesia
Lameness is improved by perineural analgesia of the palmar digital nerves but generally is unchanged after intraarticular analgesia of the DIP joint or analgesia of the navicular bursa.
Imaging Techniques
Radiography
The orientation of the distal phalanx should be assessed in a lateromedial image. In a normal horse, the solar margin is smooth in outline and at a 5- to 10-degree angle to the sole, sloping proximally toward its palmar aspect.1 In some affected horses the palmar processes are at the same level or lower than the toe of the distal phalanx (see Figure 33-14, B). The solar aspect of the palmar processes may have a fluffy appearance. The shape may change with elongation of the palmar processes; this change also is seen in dorsal 60-degree lateral-palmaromedial oblique or dorsal 60-degree medial-palmarolateral oblique images (Figure 33-15, A). In a dorsoproximal-palmarodistal oblique image, discrete circular radiolucent areas, 2 to 3 mm in diameter, may be visible in the palmar processes, or the trabecular pattern may be more obvious as a result of generalized demineralization (see Figure 33-14, C).

Fig. 33-15 A, Lateromedial radiographic image of a front foot of a 9-year-old Warmblood. Features include the abnormally elongated shape of the palmar processes, the horizontal orientation of the distal phalanx, and the thin sole. B, Solar scintigraphic image of the same foot in A. There is intense increased radiopharmaceutical uptake in the palmar processes of the distal phalanx.
So-called inversion of the distal phalanx in hindlimbs, with the plantar processes lower than the toe, also has been seen in association with more proximal sites of pain causing hindlimb lameness, such as proximal suspensory desmitis.2,3 I have not recognized this as a primary cause of hind foot pain.
Nuclear Scintigraphy
If the bony changes are active, nuclear scintigraphic evaluation may reveal IRU in the affected palmar processes to substantiate the relavance of the clinical and radiological findings (see Fig. 33-15, B). However, this is sometimes an incidental finding, and its clinical significance should be interpreted in light of other clinical observations. In a comparative radiographic, scintigraphic, and MRI study in 258 lame horses, IRU was more commonly seen in the medial palmar process of the distal phalanx than in the lateral palmar process.4 Focal IRU was overrepresented in palmar processes with MR abnormalities in signal intensity and was more prevalent in lame than nonlame limbs.
Magnetic Resonance Imaging
MRI may reveal increased signal intensity in one or both palmar processes in fat-suppressed images, sometimes with cortical irregularity and disruption of the adjacent laminar architecture. This is evidence of active osteitis and may be a cause of primary pain and lameness. However, it is common to see mild to marked reduced signal intensity in both T1- and T2-weighted images in the medial palmar process consistent with mineralization as either an incidental finding in a nonlame limb or coexistent with one or more other lesions that are more likely to be the primary cause of lameness.4
Treatment and Prognosis
Effective treatment depends on early recognition and corrective trimming and shoeing to try to restore more normal foot conformation. The response to treatment often is slow, and during the convalescent period, work on hard ground should be avoided. Horses with chronic lameness with a markedly distorted hoof capsule have a guarded prognosis. Some horses may benefit from removal of the shoes for 6 months and unrestricted exercise at pasture, provided that the hoof wall quality permits this approach and the ground is not excessively hard.
 Disease of the Cartilages of the Foot
Disease of the Cartilages of the Foot
Anatomy
The cartilages of the foot, also referred to as the collateral cartilages of the distal phalanx, ungular (ungual) cartilages, and lateral cartilages, originate as hyaline-type cartilage and become fibrocartilage in adults.1 They attach to the proximal border of the palmar processes of the distal phalanx. The size and shape vary, as does the degree of ossification. The cartilages have axial extensions, and they seem to provide an internal support structure for the palmar (plantar) aspect of the foot.2 An extensive network of venovenous anastomoses is present within the cartilages. Marked differences in the thickness and tissue composition exist in the front and hind feet. The cartilages of the foot tend to be thicker in forelimbs than in hindlimbs, perhaps reflecting the greater weight-bearing capacity of the forelimbs.2 The digital cushion has more fibrous or cartilaginous tissue in forelimbs than in matched hind feet, which have more adipose and elastic tissues. There may also be breed differences. An extensive and complex relationship exists between the cartilages of the foot and the digital cushion. The combined role is thought to be energy dissipation, which depends on hemodynamic flow.2
The cartilages of the foot are joined to adjacent structures by a variety of ligaments that vary in size and definition. The chondrocompedal ligament attaches the palmaroproximal aspect of the cartilage with the proximal phalanx, with an axial branch to the distal phalanx.1 The chondrocoronal ligament connects the dorsal part of the cartilage with the middle phalanx.1 Ossification of the lateral cartilage of the foot may be more extensive than the medial cartilage.3,5 The term sidebone has been used to describe extensive ossification of one or both cartilages of the foot. Ossification may occur from more than one center of ossification. Radiolucent lines between separate centers of ossification may persist throughout life (Figure 33-16).4,5 The degree of ossification is greater in mature horses than in horses younger than 2 years of age.3 Ossification tends to be more extensive in heavier breeds of horses than in lighter-weight horses. Extensive ossification is unusual in Thoroughbred and Warmblood breeds.5 Among Finnhorses, ossification was more common and extensive in mares compared with male horses,3 but no gender predilection was seen in a British study of mixed breeds.5 There is generally reasonable mediolateral symmetry in the degree of ossification of cartilages of the foot, with the lateral cartilage sometimes slightly more ossified than the medial. Marked asymmetry in ossification is unusual and may be a predisposing factor for lameness.6 There is generally greater radiopharmaceutical uptake at the base of the ossified cartilages than farther proximally, reflecting greater bone modeling, probably because of biomechanical stress.7
Clinical Signs and Diagnosis
The proximal aspect of the cartilages of the foot can be palpated proximal to the coronary band. However, palpation is an unreliable indicator of both the size of the cartilages and the degree of ossification. The degree of ossification can be established only by radiology. Lateromedial and weight-bearing dorsopalmar radiographic images are the most useful (Figure 33-17); however, additional information about modeling of the cartilages of the foot can be obtained from dorsoproximal-palmarodistal oblique and flexed dorsolateral-palmaromedial and dorsomedial-palmarolateral oblique radiographic images.8
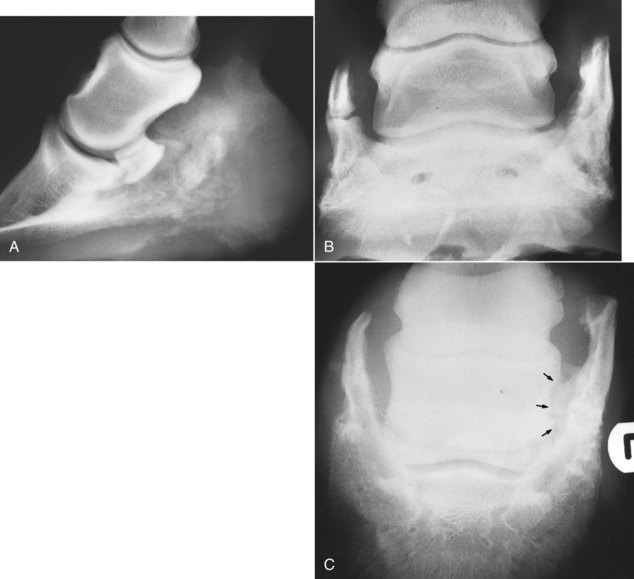
Fig. 33-17 Lateromedial (A), dorsopalmar (B), and dorsoproximal-palmarodistal oblique (C) radiographic images of a foot of a 7-year-old cob gelding. There is extensive ossification of the cartilages of the foot. Medial is to the left. A separate center of ossification of the medial cartilage of the foot is seen in B. The horse had a previous fracture at the base of the lateral cartilage of the foot with smoothly outlined callus axially (arrows, C).
Historically ossification of the cartilages of the foot has rarely been directly associated with lameness, although extensive ossification extending to the level of the proximal interphalangeal joint has been associated with a short-striding gait. However, there is now evidence that moderate to severe ossification of a cartilage of the foot may predispose to a fracture usually at the base of the ossified cartilage8-10 or osseous trauma of the distal phalanx distal to the ossified cartilage.6,8,9 Trauma at the junction between separate centers of ossification can also be associated with lameness.6, 8,9
There are usually no localizing clinical signs. Lameness is generally worse on a circle compared with straight lines, especially on a firm surface. Lameness is abolished by perineural analgesia of the palmar (abaxial sesamoid) nerves but is usually not substantially improved by intraarticular analgesia of the DIP joint.
Care should be taken not to confuse a radiolucent line between separate centers of ossification as a fracture. Nuclear scintigraphy may facilitate a definitive diagnosis of a fracture (Figure 33-18), trauma to the union between separate centers of ossification, and bone trauma of the distal phalanx.6-9 Diagnosis of bone trauma or some fractures at the base of an ossified cartilage is confirmed using MRI.6,8,9 These injuries can occur alone or together with injury of the ipsilateral collateral ligament of the DIP joint6,11,12 and/or the chondrocoronal ligament or the chondrosesamoidean ligament.8,9 There is an association between extensive ossification of the cartilages of the foot and injury of the collateral ligaments of the distal phalanx and distal phalanx trauma.8,9,12
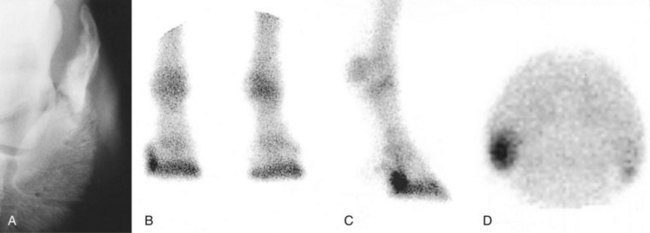
Fig. 33-18 A, Dorsoproximal-palmarodistal oblique radiographic image of the right front foot of a Warmblood mare with severe lameness that partially improved with perineural analgesia of the palmar nerves at the base of the proximal sesamoid bones. The lateral cartilage of the foot is fractured. Dorsal (the right front foot is on the left) (B), lateral (C), and solar (D) scintigraphic images of the same foot in A. There is increased radiopharmaceutical uptake in the lateral cartilage of the right front foot.
Desmitis of the chondrocompedal, chondrosesamoidean, and chondrocoronal ligaments occasionally has been recognized in association with lameness.8,9,13 There are no localizing clinical features and MRI is usually required for diagnosis. Entheseous new bone on the distal diaphyseal region of the proximal phalanx reflects abnormal stress at the origin of the ligament between the apex of the cartilage of the foot and the proximal phalanx and has been seen in association with extensively ossified cartilages.
Occasionally lameness has been associated with marked thickening of an unossified cartilage, hypervascularity, irregularity of the margins (especially abaxially), and increased signal intensity throughout the cartilage in fat-suppressed MR images, extending into the ipsilateral aspect of the distal phalanx.9