Chapter 46The Stifle
Anatomy
Developmental Anatomy
The seven centers of ossification in the stifle of the foal are the metaphyses of the femur and tibia, the distal femoral epiphysis, the proximal tibial epiphysis, the patella, the tibial tuberosity (the apophysis), and the fibula. The proximal tibial physis closes at about  years of age. The tibial apophyseal-epiphyseal physis closes by 1 year of age. The apophysis does not fuse with the metaphysis until 3 years of age. This apophysis is an important radiological feature in a young horse and can be mistaken for a fracture. The distal femoral physis closes by about
years of age. The tibial apophyseal-epiphyseal physis closes by 1 year of age. The apophysis does not fuse with the metaphysis until 3 years of age. This apophysis is an important radiological feature in a young horse and can be mistaken for a fracture. The distal femoral physis closes by about  years of age. In young foals, the margins of the femoral trochleas and the patella are irregular for the first 3 months of life because of incomplete ossification. The fibula is not evident radiologically until about 2 months of age, and a high percentage of adult horses have one and occasionally up to three horizontal radiolucent lines in the fibula distal to its head. These should not be confused with fracture lines.1
years of age. In young foals, the margins of the femoral trochleas and the patella are irregular for the first 3 months of life because of incomplete ossification. The fibula is not evident radiologically until about 2 months of age, and a high percentage of adult horses have one and occasionally up to three horizontal radiolucent lines in the fibula distal to its head. These should not be confused with fracture lines.1
Reciprocal Apparatus
The reciprocal apparatus has an important influence on the action of the stifle. Extension of the joint exerts a pull on the superficial digital flexor tendon, which originates in the supracondyloid fossa of the femur and is mostly tendonous. Because this flexor tendon has an insertion on the calcaneus, the hock must extend simultaneously with the stifle. On the cranial aspect of the stifle, the fibularis (peroneus) tertius, also a tendonous structure, originates in common with the long digital extensor tendon between the lateral trochlea and the lateral condyle of the femur.2 The fibularis tertius passes through the extensor sulcus in the lateral part of the tibial head, associates closely with the deeper tibialis cranialis muscle, and inserts on the third tarsal and third metatarsal bones and the fourth tarsal bone and calcaneus. Flexion of the stifle necessitates flexion of the hock because of the action of the fibularis tertius.2 Weight bearing is achieved without much muscular effort by the parapatellar fibrocartilage of the medial patellar ligament hooking over the medial femoral trochlea by contraction of the quadriceps femoris. The patella is released by contraction of the quadriceps femoris, combined with the lateral pull of the tensor fascia latae and biceps femoris.
Femoropatellar Joint
The articulation between the patella and the trochleas of the femur forms the femoropatellar articulation. The patella has three straight ligaments. The medial patellar ligament attaches to the medial border and the distal aspect (apex) of the patella through the parapatellar fibrocartilage. Arthroscopically the ligament can be viewed beneath the joint capsule. Distally the medial patellar ligament attaches medial to the groove on the cranial aspect of the tibial tuberosity. The middle patellar ligament originates on the cranial part of the patella just proximal to the apex and inserts in the distal part of the groove of the tibial tuberosity. The lateral patellar ligament extends from the lateral aspect of the patella to the lateral part of the tibial crest. The biceps femoris has a tendon of insertion on this ligament.3 Femoropatellar ligaments also reinforce the joint capsule medially and laterally, the lateral ligament being the more distinct.
The medial trochlear ridge of the femur is larger and more rounded than the lateral trochlear ridge and articulates with the medial part of the patella and the fibrocartilage of the medial patellar ligament. The joint capsule has a large suprapatellar pouch and inserts abaxially on the trochlear ridges forming lateral and medial recesses, the lateral being the smaller. A large fat pad is cranial to the joint capsule, proximal and distal to the patella. In my experience, most horses have a slitlike opening into the respective femorotibial joints at the distal end of the medial trochlear ridge and frequently the lateral trochlear ridge as well. Latex passed from the femoropatellar to the medial femorotibial joint in 60% to 65% of horses and in the reverse direction in 80% of horses.3 Diffusion of mepivacaine between all the compartments may occur in about 75% of horses.4
Femorotibial Joints
The medial and lateral femorotibial joints are separate compartments, which are divided by an intact median septum in a healthy joint. However, they may communicate after trauma.5 The crescent-shaped, fibrocartilaginous medial and lateral menisci lie between the respective femoral and tibial condyles to form a congruent articulation.2 Both are attached to the tibia, cranial to the intercondylar eminences, by cranial ligaments. The medial ligament wraps around the cranial aspect of the medial intercondylar eminence before inserting on the tibia. The medial meniscus is also attached caudally to the medial intercondylar eminence by the caudal ligament, which can be seen arthroscopically in the caudal part of the medial femorotibial joint. The lateral meniscus attaches caudally to the popliteal notch of the tibia and through the strong meniscofemoral ligament to the caudal part of the intercondylar notch of the femur. Only the cranial and caudal poles of the menisci can be viewed arthroscopically because of the close apposition of the tibia and femur, but the respective cranial ligaments are clearly visible. During flexion the menisci slide caudally, and during extension they slide cranially.
The cranial cruciate ligament has its tibial attachment cranial to the medial intercondylar eminence and its femoral attachment in the lateral part of the intercondylar notch. The cranial cruciate ligament lies beneath the median septum and usually cannot be directly viewed arthroscopically without removing the septum. A better view is often gained from the lateral compartment. The caudal cruciate ligament originates in the popliteal notch of the caudal aspect of the tibia and runs proximally, medial to the cranial cruciate ligament, to insert cranially in the intercondylar notch of the femur.6 The ligament can be viewed beneath the septum in the cranial and caudal medial compartment of the femorotibial joint. In the dog, the cranial cruciate ligament is under tension during extension of the femorotibial joint,7 and this may be so in the horse.
The collateral ligaments both originate proximally on the respective epicondyles of the femur. The medial collateral ligament inserts distally on the tibia distal to the medial condyle and has attachments to the medial meniscus. The lateral collateral ligament lies over the popliteal tendon and inserts distally on the head of the fibula. The popliteal tendon originates close to the lateral collateral ligament on the femur and courses distally and caudally, in close apposition to the femoral condyle, to a triangular area of insertion on the proximal caudal aspect of the tibia. The tendon is viewed arthroscopically in the cranial aspect of the lateral femorotibial joint and also in the caudal part, which it effectively divides, limiting the arthroscopic accessibility. The tendon of origin of the long digital extensor muscle can be followed arthroscopically in the cranial compartment of the lateral femorotibial joint from its origin on the extensor notch of the femur and is usually invested within the joint capsule, although in some traumatized joints, the tendon appears separate.5
Diagnosis
General Considerations
The history may give an important lead to diagnosing the cause of lameness. For example, a young horse is a candidate for osteochondrosis or subchondral cystic lesions. Acute-onset stifle lameness in a horse at pasture or during work is more likely to be a traumatic injury involving ligaments or bone. Sudden reduction of work or poor condition may predispose to upward fixation of the patella. Palpation of the patellar ligaments and the outline of the patella, collateral ligaments, long digital extensor tendon, tibial crest, and medial and lateral tibial condyles should be possible. Many horses with stifle injuries manifest no abnormalities on physical examination of the joint. If severe trauma has occurred, the whole region may be swollen, making palpation of the individual structures difficult. The horse may guard the limb so strongly that instability may not be obvious. Because of the ligamentous structures around the joint, distention is only readily palpable over the cranial aspect of the femoropatellar joint and over the medial femorotibial joint cranial to the medial collateral ligament.
Gait and Manipulative Tests
Differentiating stifle lameness in the horse by studying the gait is difficult because the reciprocal apparatus coordinates the movement of the whole limb. In my view, attributing the cause of certain gait changes to stifle pain is not possible. Some horses with stifle pain may carry the stifle slightly abducted, but this is not specific![]() . A careful analysis of the whole limb is required to establish the site of pain causing lameness. Other gait changes that may be seen with stifle lameness, but which are also not specific, are a reduced cranial phase of the stride and a reduced flexion of the limb in flight. Many horses with stifle pain dislike going downhill. Horses with delayed release or upward fixation of the patella tend to avoid fully extending the limb and appear to have a crouching gait. Flexion of the upper limb exacerbates lameness in horses with stifle pain, and abduction of the limb may be resented. When performing proximal limb flexion tests, holding the limb at midmetatarsal level, rather than by the foot, helps to differentiate between upper and lower limb pain.
. A careful analysis of the whole limb is required to establish the site of pain causing lameness. Other gait changes that may be seen with stifle lameness, but which are also not specific, are a reduced cranial phase of the stride and a reduced flexion of the limb in flight. Many horses with stifle pain dislike going downhill. Horses with delayed release or upward fixation of the patella tend to avoid fully extending the limb and appear to have a crouching gait. Flexion of the upper limb exacerbates lameness in horses with stifle pain, and abduction of the limb may be resented. When performing proximal limb flexion tests, holding the limb at midmetatarsal level, rather than by the foot, helps to differentiate between upper and lower limb pain.
Three specific manipulative tests have been described for the stifle. These are the cruciate test, collateral ligament test,8 and patellar displacement test. Most horses with clinically significant stifle pain resent these tests, which makes the tests difficult to perform and to interpret. All manipulation or flexion tests should be done on the contralateral limb first. For the cruciate test, the affected limb should be weight bearing. The head of the tibia is pushed caudally and then released 5 to 10 times before trotting the horse. Laxity is supposed to be appreciated and lameness exacerbated if severe cruciate injury exists. I have never found this test effective. Pain in the affected joint provokes strong guarding by the horse so that the procedure is impossible to perform. The medial collateral ligament test involves abducting the distal limb against shoulder pressure exerted on the femorotibial joint 5 to 10 times before trotting the horse. Horses with ruptured medial collateral ligaments are so painful and instability is so great that this test is inappropriate, but it can be useful for a sprain of the ligament. The lateral collateral ligament is less often affected, but it can be tested by pulling the distal aspect of the limb medially. Lameness associated with problems with patella release may be worsened by pushing the patella proximally several times with the horse weight bearing before trotting, but again this is often an unrewarding test.
Diagnostic Analgesia
In many horses with low-grade stifle lameness, positive diagnostic analgesia is the only way to localize the site of pain, so it is an important test. Because diffusion of local anesthetic solution between the three joint compartments is so variable,4 all three must be blocked to ensure a valid test. Alleviation of lameness after analgesia of one compartment does not necessarily infer that that compartment is definitely the source of pain.
I use a 5-cm, 19-gauge needle for each joint compartment and up to 30 mL of local anesthetic solution because experience has shown that 20 mL in each compartment might be incompletely effective in a 600-kg horse. Strict aseptic procedure should be followed. Arthrocentesis of the femoropatellar joint is well tolerated and performed first. An intradermal bleb is usually unnecessary. However, an inexperienced veterinarian may find one helpful for the medial femorotibial compartment because some horses are sensitive to injection at this site. My preferred approach for the femoropatellar joint is between the middle and medial patellar ligaments. Synovial fluid is infrequently retrieved from this site unless the joint capsule is distended. If a synovial fluid sample is required, it may be retrieved more easily through a lateral approach.9 The lateral cul-de-sac is entered caudal to the caudal edge of the lateral patellar ligament and 5 cm proximal to the tibial condyle. The medial femorotibial compartment is entered over the medial tibial condyle between the medial patellar ligament and the medial collateral ligament. A small outpouching of the joint capsule may be palpated. The lateral femorotibial compartment is best approached just cranial or caudal to the long digital extensor tendon and close to the tibial plateau. Less space is available between the meniscus and the joint capsule in the latter approach, so the former is preferred. An improvement in lameness can be expected in 30 minutes, but the clinician is wise to allow at least 1 hour for the final assessment.
Horses with a number of conditions causing lameness in the stifle respond incompletely or not at all to intraarticular analgesia. Horses with medial or lateral collateral ligament or patellar ligament injuries may be unaffected. Horses with subchondral bone cysts in the medial femoral condyle show a variable response, ranging from resolution of lameness to little change, and analgesia can take a long time to take effect. Horses with conditions that cause severe lameness are often only partially improved by analgesia; these conditions include infections; fractures, particularly patellar and tibial crest fractures; advanced osteoarthritis (OA); and severe cruciate and meniscal tears.
Imaging Considerations
Radiography
Although many stifle injuries are not associated with detectable radiological changes, radiography is usually the first imaging mode to be used once the site of pain causing lameness has been established as the stifle, or if the distal aspect of the limb has been excluded as a potential source of pain. An x-ray machine capable of producing at least 90 kV and 20 mAs is required. In larger horses, adequate definition will only be achieved with even higher-powered x-ray generators. Fast-screen film combinations can be used particularly for caudocranial images. Using as slow a combination as possible is always worthwhile, commensurate with safe practice, to achieve the best definition on the radiograph. Large cassettes are necessary and should be held in a cassette holder with a long handle. Because of the difficulty of aligning the cassette perfectly in the standing horse, using a grid is impractical, although one can be used if the horse is under general anesthesia. Many horses dislike having cassettes placed close to the stifles, so great care must be taken with this procedure. If any doubt exists about the horse’s temperament, the horse should be sedated.
Five standard images are most commonly used: lateromedial, flexed lateromedial, caudocranial, caudolateral-craniomedial oblique, and cranioproximal-craniodistal oblique (skyline). The radiographic anatomy of the soft tissue attachments of the stifle is well described.10
Lateromedial Image
The horse should be standing naturally for this image. The x-ray beam is directed perpendicular to the stifle. The stifle is naturally rotated slightly laterally in most horses, which predisposes to the beam being directed from too far cranially. The x-ray beam should pass just proximal to and parallel to the tibial plateau. The landmark on which to target the x-ray beam is the lateral condyle of the tibia. The cassette has to be pushed as far proximal as possible, which can be difficult in a well-muscled horse or a stallion. In a well-positioned radiographic image, the femoral condyles are superimposed on each other.
Flexed Lateromedial Image
The limb is held in the farrier’s position with the tibia parallel to the ground. If the stifle is held with its axial plane vertical, directing the x-ray beam perpendicular to the joint is easier. The same landmarks are used as for the standing lateromedial image. When the x-ray beam is correctly positioned, the femoral condyles are superimposed. When compared with the standing lateromedial radiographic image, the flexed image reveals a greater area of the medial intercondylar eminence of the tibia and the cranial part of the femoral condyles and also allows more complete imaging of the patella.
Caudocranial Image
The caudocranial image requires relatively high exposure factors. A key feature for correct positioning is the angle of the tibia because the x-ray beam should be perpendicular to the tibia. Placing the horse in its natural stance or with the limb slightly caudal to the contralateral limb facilitates correct alignment. The x-ray beam should divide the limb in the caudocranial plane and pass just proximal to the level of the lateral tibial condyle. The natural lateral rotation of the stifle should also be taken into account. Thus the x-ray beam is usually aimed craniodistally and craniolaterally and meets the caudal musculature of the thigh surprisingly proximally. The correct image defines the femorotibial joint spaces and clearly images the intercondylar eminence of the tibia within the supracondylar fossa of the femur.
Caudal 30° Lateral-Craniomedial Oblique Image
For the caudal 30° lateral-craniomedial oblique image, the x-ray beam is directed 30 degrees from the caudocranial plane and slightly from proximal to distal, so that it crosses parallel to the tibial plateau, which it should bisect. The main value of this image is imaging the lateral femoral trochlea, with the advantage of highlighting the medial femoral condyle, and it can be used to screen for osteochondrosis lesions and subchondral cystic lesions.
Cranioproximal-Craniodistal Oblique Image
The cranioproximal-craniodistal oblique image is a skyline image of the patella and femoral trochlear ridges and may be the only view on which a patellar fracture may be seen. In a standing horse, the limb is held in the farrier’s position with the tibia horizontal. The x-ray beam is aimed along the articular surface of the patella, but it may be impeded by the horse’s flank. Twisting the metatarsal region medially, which rotates the stifle laterally, sometimes allows better access to the patella. The cassette is held along the cranial proximal aspect of the tibia, and the x-ray beam is directed almost vertically. Checking the position of the patella on a previous flexed lateromedial image helps to decide on the correct beam angle. In an anesthetized horse, the leg is flexed with the horse in dorsal recumbency, and the x-ray beam is directed from distal to proximal.
The contours of the femoral trochlear ridges and the patella are irregular in young foals. In most foals this irregularity is present up to 11 weeks of age, and in 45% of foals, up to 25 weeks.11 In foals older than 5 months of age, irregularity of the femoral trochleas is abnormal. Irregularity of the femoral or tibial condyles is abnormal at any age.
Ultrasonography
A substantial proportion of stifle lameness is caused by soft tissue damage; therefore ultrasonography has a potential diagnostic role in defining the injury and has several advantages over other imaging diagnostic techniques. At present, ultrasonography is the only method of assessing soft tissue injury in the stifle in a standing horse. The disadvantages are that ultrasonography requires experience to be used effectively and a good-quality ultrasound scanner with a sector and a linear array transducer is necessary. Transducer frequencies of 7.5 and 5 MHz are needed to image the cranial aspect of the stifle, but a 3-MHz transducer is required to image the caudal part of the stifle.12-15 When it becomes available, magnetic resonance imaging (MRI) is likely to be a superior imaging technique for soft tissues of the equine stifle.16 Computed tomography (CT) has already proven useful for evaluation of meniscal tears and for detection of cartilage and subchondral and trabecular bone injury.17
Ultrasonography can be valuable for differentiating joint capsule distention from extraarticular swelling. Soft tissue structures that can be imaged include the patellar ligaments, the menisci and the respective cranial ligaments, the collateral ligaments, the cranial and caudal cruciate ligaments, the meniscofemoral ligaments, the origin of the long digital extensor tendon, and the popliteal tendon. The articular cartilage and bony outline of the femoral trochlear ridges and the cranial and caudal third of the femoral condyles may also be imaged.12-15
The patellar ligaments and the collateral ligaments can be imaged longitudinally and transversely with a 7.5- to 10-MHz linear array transducer with the horse weight bearing. The middle patellar ligament is the most obvious of the three and is a useful landmark. The femorotibial collateral ligaments can be imaged from the attachments on the distal lateral or medial femoral epicondyles to the attachments on the proximal medial or lateral aspects of the tibia, and they lie over the respective menisci.18 The menisci can also be imaged with this transducer from caudal to the medial and the lateral patellar ligaments. They appear as wedge-shaped structures of moderate echogenicity with the base of the wedge closer to the transducer. The cranial ligaments of the menisci are more easily imaged with a small convex array or sector transducer, which can be aimed more perpendicular to the meniscal ligaments and which can be more easily positioned between the patellar ligaments. The cruciate ligaments are difficult to image because aligning the transducer perpendicular to the fibers of the ligament is difficult. Only a small length of ligament can be imaged at a time, which can make interpretation equivocal. Cruciate ligaments can only be viewed with the stifle in a flexed position using a convex array or sector scanner. Useful information on the surfaces of the femoral trochlear ridges and condyles can be obtained. The condyles are imaged with the stifle in a flexed position, and this can be helpful in diagnosing subchondral bone cysts.19 From caudal, a sector transducer is preferable for imaging the caudal cruciate ligament and the meniscofemoral ligaments, and a 3-MHz transducer is necessary in large horses.13
Scintigraphy
Scintigraphy has been used on horses for more than 30 years, but little published evidence assesses its specificity and sensitivity for conditions of the stifle. A recent study of 16 horses indicated moderate to high sensitivity of scintigraphy for detection of meniscal damage, cruciate ligament injury, or articular cartilage pathology in the stifle using arthroscopy as the gold standard, but specificity was low, indicating a high risk of false-negative results.20 For most stifle conditions, scintigraphic findings are variable, and although positive findings are obviously helpful, negative findings can also add useful information. The clinical significance of any scintigraphic result should be confirmed as exhaustively as possible by other tests, particularly diagnostic analgesia because false-positive results also occur. In the normal adult stifle, the caudal aspect of the tibial epiphysis often has highest uptake of radiopharmaceutical.21
Nuclear scintigraphy is most consistently valuable in diagnosing incomplete avulsion fractures associated with the stifle.22,23 However, although positive results may be obtained within 24 hours of injury, in some horses at least 3 days must elapse before clinically significant increased radiopharmaceutical uptake (IRU) occurs. Subchondral cystic lesions that cause lameness may be scintigraphically positive or negative (Figure 46-1). The lesions are more likely to be detected in older horses, using a caudal image, than in an immature horse with high background activity. Absence of radiopharmaceutical uptake was thought to be the result of osteoclasts being the dominant cells in certain stages of the condition.24,25 However, in the Editors’ experience the majority of subchondral cystic lesions do have focal IRU. Although scintigraphy has been used to assess osteochondrosis in people,26 bone scan findings are not well documented in horses. I have seen positive and negative scintigraphic results associated with clinically significant osteochondrosis of the lateral femoral trochlea. Soft tissue injuries of the stifle are often scintigraphically negative, but in my experience IRU can occasionally be encountered in these horses, especially in association with enthesopathy.
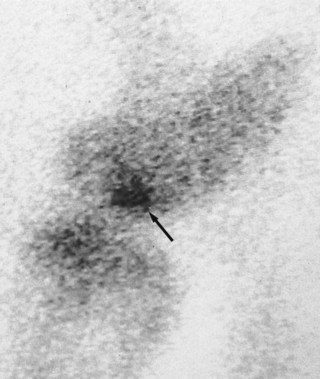
Fig. 46-1 Lateral delayed (bone) phase scintigraphic image of the right stifle of a 9-year-old Thoroughbred cross gelding. There is focal increased radiopharmaceutical uptake in the distal femoral condyle (arrow). A subchondral bone cyst in the medial femoral condyle thought to be causing lameness was seen radiologically.
Scintigraphy is certainly a useful tool as a diagnostic aid for lameness in the stifle and can be useful for evaluating the bone activity of lesions. Occasionally horses may respond positively to intraarticular analgesia, but no clinically significant abnormalities are found on radiography, ultrasonography, and arthroscopy. IRU in the stifle may be the only finding. Making a definitive diagnosis in these horses is difficult, although conceivably subchondral bone pain may be a possible cause of the lameness. One should bear in mind that many stifle conditions are negative scintigraphically. Conversely, the joint may be scintigraphically positive when the cause of lameness is elsewhere in the limb.
Articular Diseases
Femoropatellar Joint
Osteochondrosis
Osteochondrosis has been recognized in horses for more than 50 years and is an important cause of stifle lameness in young horses. The exact cause of the disease is still not well defined, but several factors are known to influence its development. Adequate dietary copper is important. Mare’s milk is relatively low in copper, and because the foal relies on copper stored in its liver during late pregnancy, it will be deficient if the mare’s diet contains insufficient copper. The zinc/copper ratio is also important because zinc inhibits the absorption of copper.27 Foals on high-energy diets are more prone to the disease.28 Insufficient or excessive exercise and trauma may be factors that influence the development of the disease. Genetic factors may predispose to osteochondrosis in the hock of Swedish Standardbreds (STBs).29 Large, fast-growing males are more susceptible. Osteochondrosis is most frequently seen in Thoroughbreds (TBs) and Warmbloods. The lesions probably develop in the first 7 months of life,30 but sometimes clinical signs may not be manifest until the horse is brought into work. In the sports horse this may be as late as 5 years of age or even older when a mild to moderate lameness may develop as the horse begins more serious work. In my experience, surprisingly severe lesions can remain undetected until this time. Lesions are most commonly seen on the lateral trochlear ridge of the femur31 but do occur on the medial trochlea, intertrochlear groove, and patella and are often bilateral.
Signs and Diagnosis
Osteochondrosis may be present asymptomatically. Lameness is often acute in onset and varies from a subtle gait deficit to marked lameness. Lameness is often more acute in onset and more severe in foals and young yearlings than in older horses. Distention of the femoropatellar joint capsule is often present and can be severe, especially in foals and yearlings. Gluteal muscle atrophy is seen in horses with severe lesions. Flexion tests are mostly positive. Synovial fluid may be hemorrhagic, but it is often normal. Intraarticular analgesia of the femoropatellar joint should improve lameness. However, in mature horses lameness may be mild, with no effusion and a poor response to intraarticular analgesia. In such horses arthroscopic evaluation often reveals an extensive area of cobblestone-like cartilage, with extensive fibrillation over a large portion of the lateral trochlea of the femur. This cartilage is often well adherent to the subchondral bone and little clinical benefit is derived from surgery.
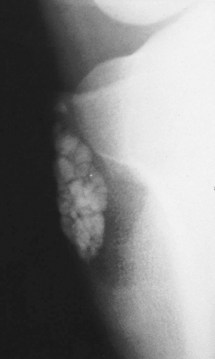
Radiological changes include the following: no detectable signs, slight loss of contour or loss of outline of the lateral trochlear ridge, irregular defects in the trochlear ridge, radiodense fragments within the defect (Figure 46-2), round radiopaque bodies loose in the joint, and more rarely, irregularities on the patellar apex or the medial trochlear ridge.1,32,33 Lateromedial and caudolateral-craniomedial oblique images are the most useful projections. Horses with radiological lesions do not always show lameness.25,27 Some horses have no detectable radiological abnormalities, but osteochondrosis lesions are diagnosed on arthroscopic examination. Lesions without fragmentation in young foals may resolve with time,32,33 but many progress.34
Treatment
Conservative management, with confinement and correction of dietary imbalances, and arthroscopic debridement of the lesions are the main treatment options. Conservative management is appropriate for horses with mild lesions. Because of the insensitivity of radiological evaluation of osteochondrosis lesions, an argument can be made for arthroscopic examination of most horses with lesions seen radiologically or persistent femoropatellar effusion and lameness that fails to respond to conservative treatment.35 Arthroscopic examination would ensure that horses with radiologically silent cartilage lesions are treated effectively. OA can also be evaluated. For horses with fragmentation and clinically significant radiolucent defects of subchondral bone, arthroscopic surgery is probably the treatment of choice.31 In my opinion, more caution is required when treating foals arthroscopically because some foals with large lesions seen radiologically are found to have intact cartilage at arthroscopy. Debridement of such lesions can leave unacceptably large deficits in the lateral trochlear ridge. Reattaching these cartilage flaps with polydioxanone pins may be a more appropriate treatment and has shown good results with seven of nine foals achieving athletic use.36
A variety of lesions are seen arthroscopically. The articular cartilage may appear intact, but if probed, large flaps may lift from the subchondral bone. Large defects on the lateral trochlear ridge may contain nodules of mineralized cartilage, which are readily removed, and often large tufts of fibrillated cartilage are associated with the lesion. The exposed subchondral bone is frequently soft and crumbly. Extensive areas of fibrillated cartilage over the adjacent lateral trochlear ridge and the opposing patella are often present in older horses.5 Loose cartilage should be removed, and the lesion should be curetted to healthy subchondral bone, which is a source of pluripotential cells. The cartilage perimeter should be vertical to allow better attachment of tissue regrowth.37 Thorough lavage to remove all debris, particularly of the suprapatellar pouch, at the completion of surgery is essential. Six weeks of stable rest with daily handwalking after 2 weeks is recommended postoperatively. The horse should then be left for another 4 to 5 months at pasture before returning to work.
Prognosis
Mild lesions in foals were shown to heal with conservative management.32,33 For foals with more severe lesions, better results were reported with arthroscopic debridement.31 Sixty-four percent of 161 horses were able to perform athletically. In this series, treatment of older horses and those with mild to moderate lesions was most successful, which has also been the experience in my practice. The presence of extensive secondary articular cartilage fibrillation did not have a significant effect on the outcome in horses more than 2 years of age.5
Upward Fixation of the Patella and Delayed Patellar Release
Upward fixation of the patella occurs when the stifle subtends an angle of approximately 145 degrees and the medial patellar ligament hooks over the medial trochlea of the femur, thus locking the reciprocal apparatus with the limb in extension. The condition is more common in horses with a straight hindlimb conformation with a stifle angle nearer 140 degrees (in the normal horse the angle is about 135 degrees), so that only a small degree of extension is required for upward fixation to occur.38 Upward fixation is not a luxation of the patella, despite being commonly described as such. Predisposing straight hindlimb conformation or the condition itself may be hereditary.39 Upward fixation of the patella is more commonly seen in young horses and ponies, especially if they are in poor condition, when weak thigh musculature fails to release the patella. Upward fixation can occur in older horses after trauma to the stifle region, is most frequently manifest when the affected horse is stabled, and sometimes occurs in fit horses that are suddenly given box rest. Lameness may develop in horses with more severe or long-standing lesions. I recognize delayed patellar release as a condition in which delayed release of the patella occurs, without complete upward fixation, and which presumably is a less severe form of the disease.
Signs and Diagnosis
A horse with upward fixation of the patella stands with the hindlimb locked in extension with the fetlock flexed (Figure 46-3)![]() . The leg releases with a snap, usually unaided, but occasionally the horse needs assistance. Some horses merely show intermittent delayed release of the patella, especially when turned toward the affected limb. This can be mistaken for stringhalt. Delayed patellar release is manifested by a catching of the patella as the limb is protracted, usually as the horse moves off. Delayed release of the patella may be evident as a rather jerky movement of the patella when the horse moves over in the stable or as it decelerates from canter to trot or trot to walk. Horses in which the condition is chronic develop stifle soreness and may be resistant to work, especially in deep going. If the condition is more serious, horses try to avoid extending the hindlimbs while walking uphill or downhill. Femoropatellar effusion may be present. Diagnosis may depend on the history and the owner’s description if the horse does not lock the patella during the examination. Locking the patella manually may be possible by pushing it proximally, although this can be difficult and is resented by many horses. A careful search should be made for concurrent stifle disease such as osteochondrosis or soft tissue injury, and the site of any lameness should be confirmed by diagnostic analgesia. Radiographic examination of both stifles is prudent because any pathological condition caused by upward fixation or concurrent with it affects treatment and prognosis.
. The leg releases with a snap, usually unaided, but occasionally the horse needs assistance. Some horses merely show intermittent delayed release of the patella, especially when turned toward the affected limb. This can be mistaken for stringhalt. Delayed patellar release is manifested by a catching of the patella as the limb is protracted, usually as the horse moves off. Delayed release of the patella may be evident as a rather jerky movement of the patella when the horse moves over in the stable or as it decelerates from canter to trot or trot to walk. Horses in which the condition is chronic develop stifle soreness and may be resistant to work, especially in deep going. If the condition is more serious, horses try to avoid extending the hindlimbs while walking uphill or downhill. Femoropatellar effusion may be present. Diagnosis may depend on the history and the owner’s description if the horse does not lock the patella during the examination. Locking the patella manually may be possible by pushing it proximally, although this can be difficult and is resented by many horses. A careful search should be made for concurrent stifle disease such as osteochondrosis or soft tissue injury, and the site of any lameness should be confirmed by diagnostic analgesia. Radiographic examination of both stifles is prudent because any pathological condition caused by upward fixation or concurrent with it affects treatment and prognosis.
Treatment
For a horse that has the patella locked, pushing the patella medially and distally and backing the horse is recommended but difficult to do. Pulling the limb forward with a side line may provide relief. If the upward fixation of the patella is intermittent and not causing lameness, a conditioning program should be undertaken. This includes an exercise regimen, the administration of anthelmintics, an increased plane of nutrition, and dentistry as appropriate for each horse. The exercise regimen depends on the specific circumstances for each horse. Daily lunging should be instituted to a level that is appropriate for the age and type of horse. Stable rest is usually contraindicated, and turning the horse out to pasture as much as possible is preferable. Immature horses should be allowed time to outgrow the problem. Injection of counterirritants containing iodine into the medial and middle patellar ligaments has been used at this stage of the disease.40 Horses with delayed patellar release require the same management.
Because of potential complications, which include fragmentation of the patella and lameness, surgery is only indicated when the following criteria have been fulfilled:
The surgery can be performed under local anesthesia in the standing horse.41 A small incision is made over the distal part of the medial patellar ligament. I find that minimizing the incision length seems to reduce the incidence of postoperative swelling. A curved Kelly forceps is then advanced caudally under the ligament, developing a path for a blunt-ended bistoury. The bistoury is passed until its end can be palpated caudal to the medial patellar ligament, before the ligament is severed close to its tibial insertion. Stringent asepsis should be observed. Once the ligament is severed, the border of the tendon of the sartorius muscle is palpable caudally. Some surgeons prefer to perform this surgery with the horse under general anesthesia, which allows for complete asepsis: the ligament can be exteriorized before severing, and the fascia overlying the ligament can be sutured before skin closure.
An alternative treatment involving numerous splitting incisions in the medial patellar ligament was described and was successful in four horses and three Shetland ponies, but only two horses were followed beyond 5 months.42
Postoperatively I prefer to confine the horse for 2 months to allow the patella to settle in its new position in the intertrochlear groove. Handwalking can be introduced during the second month.
Prognosis
A substantial number of horses respond to conservative treatment. Occasional recurrences happen if the horse has enforced stable rest, but many grow out of the condition. After surgery and in the absence of degenerative changes in the joint, the horse should return to normal use, although some appear to have a slightly restricted gait. Recurrence of the condition is unusual. Some fibrous thickening is palpable at the surgical site for many years in most horses and indefinitely in some horses. Clinically significant complications including lameness, local swelling, fragmentation of the patella, and fracture of the patella were reported.43-48 Fragmentation of the patella was produced after experimental medial patellar desmotomy.46 If fragmentation causes lameness, horses can be managed arthroscopically with good results.33 In my experience, up to 30% of horses have minor fragmentation of the patella, without clinical signs, after medial patellar desmotomy. Injury of the middle patellar ligament can also occur secondary to medial patellar desmotomy.49,50
Fragmentation of the Patella
Fragmentation of the patella is generally considered to be a sequela to medial patellar desmotomy or to be associated with upward fixation of the patella, and it is manifested by fragmentation of cartilage and bone off the apex of the patella.43,46,48,50 This condition is not chondromalacia of the patella, which could be a form of osteochondrosis, and has not been specifically reported in horses. If the condition follows desmotomy, clinical signs can appear from 3 weeks to more than 12 months postoperatively. Horses can develop fragmentation within a few weeks of surgery without clinical signs.5 Medial patellar desmotomy was performed experimentally in 12 horses, and of these eight developed fragmentation.46 The lesions may be caused by instability of the patella after medial patellar desmotomy.
Signs and Diagnosis
Lameness varies from a stiff hindlimb action to an obvious lameness. Flexion is resented and worsens the lameness. Synovial effusion is common, and excessive fibrous tissue reaction may be present at the surgical site. Radiologically, small bone fragments are present close to the apex of the patella (Figure 46-4), often combined with radiolucent defects of subchondral bone and roughening or spurring of the distal cranial aspect of the patella.
Treatment
Arthroscopic debridement is indicated. The lesions are most commonly on the lateral surface of the apex of the patella and may be partly obscured by synovial villi; therefore a careful arthroscopic examination should be performed before deciding on the site of the instrument portal. Debridement of the lesion to healthy subchondral bone is required.
Prognosis
The prognosis for athletic function is reasonable, although some horses appear to have a slightly stiff hindlimb action because of the original medial patellar desmotomy. Ten of 15 horses returned to athletic use.43 In my experience, the incidence of the condition has decreased in the past 8 years, which may be because fewer patellar desmotomies are performed or because more care is taken during convalescence.5 However, the condition still occurs despite appropriate rest after medial patellar desmotomy.50
Luxation of the Patella
Lateral luxation of the patella in the foal is considered to be an inherited condition caused by a recessive gene.51 Luxation in an adult horse is likely to be traumatic in origin.38 Because the medial trochlear ridge of the femur is largest, only severe trauma induces medial displacement of the patella. Hypoplasia of the lateral trochlea of the femur is often present in association with lateral luxation of the patella,39 but the condition also occurs in foals with apparently normal conformation.51 Luxation is most common in miniature breeds but has been reported in STBs, TBs, and an Arabian foal,52-54 and I have seen it in a Welsh Cob.5
Signs and Diagnosis
The condition may be unilateral or bilateral and has been graded as follows:
Severely affected foals are unable to extend the stifle and stand in a characteristic crouching position. If less severe, the condition may not be obvious clinically, but horses are usually reluctant to flex the stifle and have a stiff gait in the affected limb. Some horses show little evidence of the disease until degenerative changes provoke lameness. I have seen a TB yearling with severe osteochondrosis of the lateral trochlear ridge, which led to a diminution of the ridge and allowed the patella to luxate laterally. One of the Editors (MWR) has seen numerous STB foals with severe osteochondrosis of the lateral trochlear ridge of the femur and patellar luxation. Lateromedial, cranioproximal-craniodistal oblique, and caudocranial radiographic images are the most useful to ascertain the position of the patella and to evaluate the trochlear ridges.
Treatment
Lateral release and medial imbrication of the femoropatellar compartment are necessary to maintain the patella in the intertrochlear groove.52-54 Both lateral release and medial imbrication appear to be important. Recession sulcoplasty is valuable in the presence of hypoplasia of the lateral trochlear ridge of the femur.54
Prognosis
Poor success can be expected with surgery in the presence of OA, large osteochondrosis lesions, and in larger horses. In foals there is a moderate prospect of achieving athletic function. Aggregating the results from the three reported case series, the patella maintained its position postoperatively in eight of 11 foals.52-54 Breeding from affected horses should be discouraged.
Osteoarthritis
Any injury to the femoropatellar joint can potentially cause OA. The injury could be simple trauma or result from any of the previously mentioned conditions if they have caused irreversible changes.
Signs and Diagnosis
The clinical signs depend on the cause and severity of the condition. Lameness is usually persistent, and chronic joint distention may be present. If osteochondrosis is responsible for OA, radiological changes typical of chronic osteochondrosis are likely to be present (see page 536). Cartilage fibrillation, ranging from focal tufting to widespread involvement of the femoral trochlear or patellar articular cartilage, may be seen arthroscopically, and full-thickness defects of the articular cartilage may be present in more severely affected horses.
Treatment
Initially treatment depends on the inciting condition and is described in the appropriate sections. However, once chronic osteoarthritic changes have developed, realistically therapy is likely only to be palliative. Intraarticular medication with small doses of corticosteroids, such as 10 mg of triamcinolone acetonide combined with hyaluronan, may give temporary relief. A controlled exercise regimen may help, and an arthroscopic debridement prolongs working life in some horses.
Distal Luxation of the Patella
One report of distal luxation of the patella has been made.55 The horse held the affected limb flexed and non–weight bearing. The patella was relocated with the horse under general anesthesia, and when the horse was reexamined 3 months later, no lameness was seen.
Patellar Ligament Injuries
Patellar ligament injuries are rare. Sprain of the middle patellar ligament is the most common, although lateral patellar ligament injuries also occur.49 There may be an association between middle patellar desmitis and previous medial patellar desmotomy. Jumping horses are most commonly affected. Lesions may occur unilaterally, or less commonly bilaterally.
Signs and Diagnosis
Lameness can be moderate to severe in the acute phase but varies. The severity of lameness is usually commensurate with the degree of ligamentous damage and is most severe in horses with partial ruptures. Sometimes no localizing signs are apparent, but femoropatellar effusion, periarticular thickening, or edema may be seen in some horses. Intraarticular analgesia of the femoropatellar joint may slightly improve lameness in some horses, but in others there is no effect on the lameness. The diagnosis is confirmed by ultrasonography. Proximal, midbody, and distal lesions have been identified. Differentiation should be made between core lesions and partial-thickness tears. Radiological changes are unusual, and one should bear in mind that entheseous change on the cranial distal aspect of the patella may be seen as an incidental radiological finding. However, extensive entheseous new bone may be of clinical significance. Scintigraphy may show focal IRU in the patella or more commonly the cranioproximal aspect of the tibia in association with proximal or distal lesions of the middle patellar ligament.
Treatment
Horses with severe injuries may require rest for up to 6 months. In one Editor’s experience (SJD) conservative management has yielded poor results in horses with extensive core lesions, and treatment by injection of porcine urinary bladder matrix or mesenchymal stem cells has improved the prognosis. The presence of periligamentous fibrosis is a poor prognostic finding. Horses with partial-thickness tears have also responded poorly to any form of management, including surgical debridement.
Femorotibial Joint
Subchondral Cystic Lesions
The cause of subchondral bone cysts and other osseous cystlike lesions is still unknown. The distal weight-bearing aspect of the medial femoral condyle is the most frequent site for subchondral bone cysts.56 Osseous cystlike lesions were identified in the caudal aspect of the femoral condyles in foals.57 Osseous cystlike lesions also occur in the proximal aspect of the tibia. Lesions thought to result from osteochondrosis were in the lateral aspect of the tibia, and those associated with OA were more common medially in a report of 12 horses.58 Subchondral bone cysts and osseous cystlike lesions may be a form of osteochondrosis,59 but trauma is also probably an important factor. Subchondral bone cysts in the medial femoral condyle have been produced experimentally after development of full-thickness defects in cartilage and subchondral bone.24 Lesions did not form if the defects were made only in cartilage. The lining of these lesions has been shown to contain active inflammatory enzymes that cause bone resorption.60 In the literature the syndrome in the young horse is emphasized, but in my experience subchondral bone cysts and osseous cystlike lesions occur in any age group, mostly apparent as a primary lesion but sometimes as a sequel to OA.
Signs and Diagnosis
The condition is reported to be more common in horses less than 4 years old,56 but in my practice it is encountered in horses of all ages.5 Lameness is mild to moderate but can be severe at first and acute in onset. Lameness may be intermittent, especially in older horses. Affected horses seem to be lamer when turning. Occasionally mild medial femorotibial effusion occurs, but often no signs are obvious on physical examination. Intraarticular analgesia of the medial femorotibial joint may be required to diagnose the site of pain causing lameness. Because the subchondral bone is probably the site of pain, local anesthetic solution must diffuse into the lesion and may not be completely effective. A 50% improvement in lameness justifies radiographic examination.
The caudocranial, caudolateral-craniomedial oblique, and flexed lateromedial radiographic images are the most useful for demonstrating the lesion. Subchondral bone cysts in the medial femoral condyle are relatively round or oval, with a variably sized base and communication with the joint (Figure 46-5). Increased radiopacity of the rim is usually seen only in horses with older lesions. Radiological signs of OA may also be apparent in some horses. The osseous cystlike lesions in the tibia have a similar morphology. Subchondral bone cysts can also occur as incidental radiological findings in sound horses. Lesions in the caudal aspect of the femoral condyles in foals may appear radiologically as localized or extensive osseous defects. Scintigraphic findings in horses with subchondral bone cysts are inconsistent,24 but most have IRU. Flattening or indentation of the distal medial femoral condyle is sometimes seen radiologically and may be a precursor of a subchondral bone cyst. These lesions are relatively common and frequently do not cause lameness. Occasionally IRU is seen associated with these defects.5 In my experience, positive scintigraphic findings, together with a positive response to diagnostic analgesia, are good indications that the defect is a cause of lameness, but some scintigraphically positive lesions do not result in clinical signs; the Editors consider this unusual. Arthroscopic evaluation of horses with subtle osteochondral defects of the medial femoral condyle detected radiologically revealed that flattening of the medial condyle or a subchondral lucent area was associated with a focal or more generalized cartilage defect in 18 of 20 and four of four limbs, respectively. Treatment by abrasion arthroplasty and microfracture resulted in seven of nine horses with focal cartilage lesions returning to full athletic function, and two of six with generalized cartilage pathology.61
Treatment
Conservative treatment involves stable or pasture rest, with or without nonsteroidal antiinflammatory medication or intraarticular corticosteroids.62,63 Horses with nonarticular osseous cystlike lesions or small articular defects are probably best managed conservatively. For articular lesions and horses that do not respond to conservative management, arthroscopic debridement has been advocated.56,59,64 Debridement of the cyst lining and removal of all debris from the joint are the goals. Experimentally the use of cancellous bone grafts did not improve the outcome.65 Postoperative intralesional corticosteroid has been advocated to suppress the inflammatory mediators.60 Subchondral bone forage is contraindicated because reports indicate that it may worsen the lesion.56 Debridement of small medial condylar defects should be approached with caution because this may provoke a worsening of the lesion. Tibial osseous cystlike lesions can be debrided arthroscopically, but many of them lie beneath the cranial meniscal ligament, which must be divided to gain access. It was reported that the success rate for horses more than 3 years of age was poor (35% of 46 horses sound at follow-up evaluation),66 and many surgeons now lean toward intralesional corticosteroid treatment. There is evidence that numerous injections of corticosteroids into the fibrous lining of the cyst under arthroscopic guidance is the most effective method of management in older horses, and early reported success appears to be superior to that achieved using debridement in older horses (13/18 horses sound at follow-up evaluation).67
Prognosis
A 50% success rate was reported with conservative treatment of horses with medial femoral condylar subchondral cysts, but remodeling of bone may be more prolonged than with surgical treatment.62 Arthroscopic debridement carries a 70% to 75% success rate in horses less than 3 years old.56,64 Preexisting OA results in a more guarded prognosis. Improvement of clinical signs after surgery frequently occurs without radiological resolution. Limited reports of surgical treatment of tibial osseous cystlike lesions58 suggest that horses with lateral proximal tibial osteochondrosis-associated lesions may respond best, and this is also my experience.
Meniscal and Meniscal Ligament Injuries
The cause of meniscal injuries in horses is not well documented, but in dogs meniscal injuries are considered to be caused by crushing forces combined with tibial rotation and flexion or extension of the stifle.7 Meniscal injuries have also been reported in horses.68-71 I have diagnosed 126 meniscal injuries arthroscopically as the primary cause of lameness. The medial meniscus was affected in 80% of horses. The cranial ligaments of the menisci were involved in nearly all horses.72 Concurrent injury to other structures in the stifle was frequently diagnosed, including articular cartilage damage on the femoral condyles in 96 horses and cruciate injury in 18 horses. Secondary medial collateral ligament injury was not diagnosed. Primary medial collateral ligament rupture with secondary meniscal injury was not included in the series. Twenty-seven of 79 other horses that were examined arthroscopically and that had other stifle injuries, but no evidence of meniscal damage, did have fibrillation of the axial borders of the cranial ligaments of the menisci.68 The clinical significance of this is uncertain.
Signs and Diagnosis
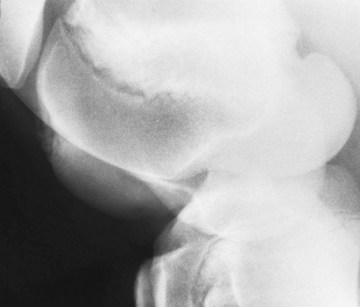
Lameness is often acute and severe in onset after trauma but mostly becomes low grade and persistent. Distention of the femoropatellar or medial femorotibial joints can be expected in horses with more severe injury.71 Lameness is exacerbated by flexion of the limb in about 90% of horses.55 Diagnostic analgesia is usually necessary to confirm the site of pain causing lameness but may not render the horse completely sound. Radiological signs occured in 52% of horses that I have diagnosed with meniscal injury. New bone formation on the cranial aspect of the medial intercondylar eminence of the tibia was the most frequent finding (25%)72 and appears to be more common with meniscal than cruciate ligament disease, in which it occurred in five of 71 (7%) cases treated at my hospital72 (Figure 46-6). Dystrophic mineralization and osteoarthritic radiological changes may be seen in horses with severe lesions. Ultrasonography can be a valuable aid in diagnosis, although some lesions will not be visible ultrasonographically, and artifactual changes can be difficult to differentiate.73,74

Fig. 46-6 Lateromedial radiographic image of the left stifle of a 7-year-old Thoroughbred cross gelding. There is new bone on the cranial aspect of the intercondylar eminences of the tibia (arrow). Note also the large radiolucent zone in the proximal aspect of the tibia. There is an old osteochondrosis lesion involving the lateral trochlear ridge of the femur. Arthroscopic examination revealed a tear of the medial meniscus.
Arthroscopy offers the best chance of a definitive diagnosis and an assessment of concurrent damage. Because only the cranial and caudal poles of the menisci can be seen, assessment of meniscal injury is limited. Owing to these limitations, I graded changes visible from cranially as follows:
Treatment
Horses with acute stifle injuries that have no definitive diagnosis should be managed with rest and antiinflammatory medication, followed by controlled exercise. Arthroscopy is indicated if conservative therapy is unsuccessful or for severely lame horses. Grade 1 meniscal tears can only be superficially debrided. Intraarticular suturing for some horses may be a way forward. Grade 2 and 3 tears are debrided as effectively as possible by removing all loose tissue. A careful assessment of visible concurrent damage should be made. Postoperatively controlled exercise begins at 2 to 3 weeks and can gradually be increased over 3 months, depending on progress and the extent of the injury. Free exercise at pasture should be avoided for 6 months.
Prognosis
Return to full athletic use can be expected in about 50% of horses overall, although improvement may be seen in another 10%.71,72 Full function was regained in 60% of 67 horses with grade 1 tears, 65% of 35 horses with grade 2 tears, 10% of 24 horses with grade 3 tears, and neither of 2 horses with two menisci affected. In the Editors’ experience the prognosis for return to full athletic function in upper level sports horses is guarded. Concurrent articular cartilage damage significantly worsened the prognosis,71 and nine of 18 horses with concurrent cruciate ligament injury became sound. Horses treated arthroscopically within 2 months of injury fared 25% better than those treated later than 2 months.72 If radiological signs of OA were present, the prognosis was also significantly worsened.71
Cranial and Caudal Cruciate Ligament Injuries
In the dog the cranial cruciate ligament can be injured when the stifle is in hyperextension or after sudden rotation with the stifle in flexion,7 and this is likely to pertain to the horse. Direct trauma to the joint or degenerative change in the ligament can also lead to cruciate injury in the horse.5,75 Experimentally76 and in my clinical experience5 the cranial cruciate ligament fails most frequently at midbody level, but avulsions of its tibial and less often of its femoral attachments have been reported.75,77 Caudal cruciate ligament injuries occur less frequently.78 Concurrent injuries, including damage to the medial collateral ligament, the menisci, and articular cartilage, are often associated with cruciate tears.75,79
Signs and Diagnosis
Lameness is often associated with a history of trauma and is usually acute in onset and severe at first. Distention of the femoropatellar or the femorotibial joints is sometimes present. In horses with severe injuries, crepitus may be detectable. The cruciate draw test appears to be valueless in the conscious horse, but a proximal limb flexion test is usually positive, especially with severe injury. In horses with mild injuries, diagnostic analgesia is required to confirm the site of pain causing lameness. In my series of 75 horses with cranial and caudal cruciate ligament injuries diagnosed at arthroscopy, radiological signs included the following5:
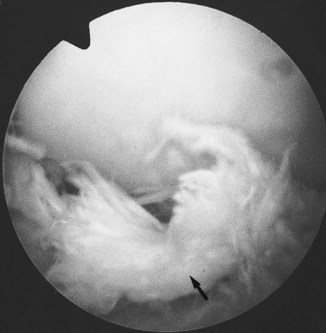
Ultrasonographic evaluation of the cruciate ligaments is difficult. Arthroscopy offers the best evaluation of the cruciate ligaments. The cranial cruciate ligament is covered by the median septum, which may make the ligament difficult to assess, but the septum is often disrupted in cranial cruciate ligament injury. Motorized debridement of the septum may be required to see the ligament. The caudal cruciate ligament is viewed from the cranial and caudal aspects of the medial femorotibial joint. The caudal medial aspect of the femorotibial joint can be approached cranially80 or caudally.81 Mild cranial cruciate ligament changes are difficult to quantify because of inflammatory changes in the median septum, but fiber disruption is seen in moderate injuries (Figure 46-8). With acute, severe injuries of the cranial cruciate ligament, inflammatory debris must be removed before the torn ends of the ligament can be seen. Concurrent articular cartilage or meniscal damage within the joint is common.
Treatment
With acute injuries the same treatment criteria apply as for meniscal injuries. The indications for arthroscopy and postoperative management are also similar. Arthroscopic debridement is best performed with a motorized synovial resector. Repair in horses with complete cruciate ligament rupture has not been reported, and the best treatment that can be offered is good debridement of loose tissue to allow less severe injuries the best chance to heal.
Prognosis
Prognosis is poor in horses with moderate to severe injuries. In one report, two of 10 horses were pasture sound and one raced,75 and in another report two of six were pasture sound.79 In my series, lameness persisted in four of six horses with severe injuries; 10 of 17 horses with moderate injuries became sound; and 18 of 29 horses with minor superficial changes became sound.5
Collateral Ligament Injuries
Injury of the medial collateral ligament is more frequently diagnosed than injury of the lateral collateral ligament. Such injury is associated with acute trauma, which, as in the dog, probably involves a medial or lateral force on the joint or distal aspect of the limb.79 Concurrent injury of the menisci or cruciate ligaments commonly occurs in horses with severe injuries,79,82 but not necessarily in those with more moderate injuries.
Signs and Diagnosis
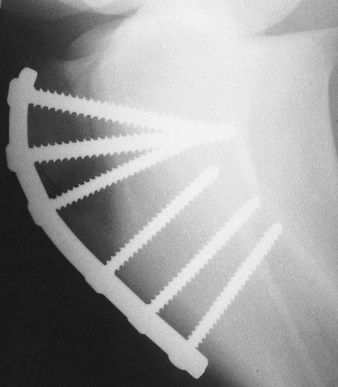
The most easily diagnosed collateral ligament injuries are complete ruptures of the medial collateral ligament, which manifest as acute, severe lameness after trauma. Instability of the stifle occurs with swelling and pain over the ligament. Sprains of the collateral ligaments are less obvious. Heat and pain may be palpable, and chronic thickening develops in some horses. The collateral ligament test can be useful but is not specific. Flexion of the limb is usually painful, but intraarticular analgesia of the medial femorotibial joint may be negative. If complete rupture of the ligament has occurred, stressed caudocranial radiographs are diagnostic. Widening of the joint space occurs on the affected side (Figure 46-9). Enthesophyte formation at the origin and insertion may be seen in horses with chronic injuries. Ultrasonography can be helpful in diagnosing and assessing the injury.18

Fig. 46-9 Stressed caudocranial radiographic image of the left stifle of a 10-year-old riding horse with rupture of the medial collateral ligament of the femorotibial joint. Medial is to the right. There is widening of the medial joint space. Note also the osseous opacity proximal to the intercondylar eminences (arrows).
Treatment
Horses with mild sprains, in which no instability occurs, are treated with stall rest for 6 weeks and antiinflammatory medication until the inflammation subsides, followed by controlled exercise for another 6 weeks. One report describes the repair of a complete rupture of the medial collateral ligament using braided polyester material attached to two 6.5-mm cancellous screws in the femur and tibia to stabilize the joint.83 Orthopedic wire was originally used, but it dislodged postoperatively. The surgery is a salvage procedure and is not well documented, and concurrent injury and horse compliance should be carefully assessed before undertaking surgery.
Prognosis
Horses with mild sprains have a moderate chance of returning to athletic use, depending on the extent of any concurrent injury. Results are not well documented, and in my view the prognosis is probably poor if entheseous change develops at the medial collateral ligament attachments. The prognosis for horses with complete ruptures is grave. The horse described above that was treated surgically was comfortable at pasture until it became lame after falling 9 months postoperatively. Because associated meniscal or cruciate injury is common, a high chance exists of OA in the long term, even if the medial collateral ligament heals.
Articular Cartilage Trauma
Articular cartilage defects on the medial or lateral femoral condyles or on the axial part of the tibial plateau are frequently encountered during arthroscopic examination. Usually they accompany other femorotibial injuries, but occasionally they are the only finding, in which case they may be considered the primary cause of lameness.84 Cartilage lesions were diagnosed as the primary cause of lameness in 150 of 632 horses undergoing diagnostic arthroscopy of the stifle in my series.5 Primary lesions may be seen on both the medial and lateral femoral condyles.
Signs and Diagnosis
Horses in which articular cartilage lesions are a primary cause of lameness usually have mild to moderate lameness. Diagnostic analgesia is required to define the site of pain causing lameness. Abnormalities are rarely seen radiologically. At arthroscopy, a variety of lesions may be present. These include thickening, softening, and creasing of the cartilage, widespread fibrillation, focal tufts of fibrillated cartilage, circumscribed nodules of cartilage, apparent tears of the articular surface, and areas of exposed subchondral bone.72,84,85
Treatment
Doubt about the long-term effect of debridement of cartilage lesions still exists.86 Small, full-thickness lesions are probably best debrided to subchondral bone; micropicking the bone appears to improve healing to a degree.87 The effect of smoothing partial-thickness defects is still controversial and may provoke the development of an osseous cystlike lesion.56,86 Debris should be thoroughly lavaged from the joint. Postoperative intraarticular medication with disease-modifying OA drugs could be helpful.
Prognosis
The prognosis for return to soundness for horses with cartilage defects is generally considered guarded. Six of seven horses with focal defects returned to racing, but five horses with larger lesions remained lame.84 In my practice, a full-thickness articular cartilage defect was diagnosed arthroscopically in 38 horses as being the primary cause of lameness. Sixteen of 24 horses (67%) for which follow-up information was available became sound.5 Of the horses with less severe lesions, 30 of 38 (79%) of those with mild changes (mild fibrillation, mild soft creased cartilage, mild focal fibrillation, n = 77) and 17 of 22 (77%) of those with moderate changes (generalized fibrillation, shear lesions, severe thickening and creasing, partial-thickness linear defect, n = 37) returned to full use. In the Editors’ experience prognosis for upper level sports horses to return to full athletic function is guarded.
Osteoarthritis
OA of the femorotibial joint can be a sequel to any injury described in this chapter that has the potential to damage the articular cartilage. OA is likely to develop when the initial tissue damage is severe, is not treated, or is treated ineffectively. OA of the medial femorotibial joint is much more common than in the lateral femorotibial joint.
Signs and Diagnosis
Many horses have a history of lameness that has already been treated or chronic lameness of varying intensity. Diagnostic analgesia may be required to identify the site of pain causing lameness, but joint effusion and thickening are palpable on the medial aspect of the joint in many horses. Flexion of the limb is painful, and some horses resent holding up the limb for shoeing. Radiological examination reveals typical changes associated with OA, including osteophytosis, flattening of the articular surfaces of the femoral condyles, increased radiopacity and radiolucent zones in the subchondral bone, narrowing of the joint space, and dystrophic mineralization of soft tissues.
Treatment
Management of OA is at best palliative. If possible, the inciting lesion should be treated appropriately in an attempt to prevent worsening of the changes. Intraarticular corticosteroids, glycosaminoglycans, or any medication designed to slow the progress of the disease, as well as arthroscopy in some horses, may give temporary relief.
Subchondral Bone Trauma and “Bone Bruising”
Early experience with CT17 and MRI is providing some explanation for horses with lameness that is improved by intraarticular analgesia of the stifle joints, but in which radiography, ultrasonography, scintigraphy, and, in some horses, exploratory arthroscopy fail to explain the cause of pain. Primary osseous lesions have been identified reflecting bone trauma.
Fractures Involving the Stifle
Fractures of the Patella
External trauma is the commonest cause of patellar fracture in the horse.88 Contraction of the quadriceps muscles may be the cause of some avulsion fractures. The majority of horses have a history of direct trauma, such as a kick, or an impact on the stifle by hitting a fixed fence while jumping. If the trauma occurs while the stifle is in flexion, the patella is fixed against the trochlear ridge of the femur, which is thought to render it more vulnerable to fracture.89
A variety of fracture morphology is seen.89,90 Sagittal fractures of the medial aspect of the patella are probably the most frequent. These are usually articular, and the fragment often involves a substantial area of the attachment of the parapatellar fibrocartilage of the medial patellar ligament. Fragmentation of the base of the patella sometimes accompanies these fractures88 or may be seen separately. Nonarticular fractures are mostly seen as mildly displaced fragments on the cranial aspect. Complete horizontal fractures are severe injuries, and the massive forces exerted by the extensor muscles have an important bearing on their management. Complete sagittal fractures are less catastrophic because the distracting forces are not as strong. Comminuted fractures of the whole body of the patella occasionally occur after severe trauma.
Signs and Diagnosis
The history and clinical signs often strongly suggest the possibility of patellar fracture. Initially lameness may be severe and remains so in horses with midsagittal and horizontal fractures. In horses with many of the smaller avulsion fractures or fractures of the medial aspect, lameness becomes moderate to mild after a few days. Often evidence of trauma and local swelling are apparent in the stifle region. Crepitus is occasionally present, and pain may be elicited on palpation of the patella. The femoropatellar joint is usually distended. Horses with chronic, less severe fractures often have surprisingly little direct evidence of the injury. Flexion of the limb is usually painful.
Radiography is essential to confirm the diagnosis and to evaluate the fracture. Lateromedial images may give no indication of the fracture, so a cranioproximal-craniodistal image is essential (Figure 46-10). Severely injured horses greatly resent positioning for this radiographic image and may require analgesia. Occasionally general anesthesia is required, but it should not be attempted without treatment options being in place.
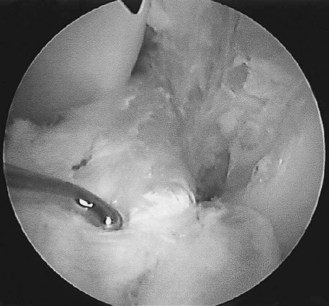
Treatment
Horses with open wounds must be treated with debridement and antibiotics, and it is vital to establish if joint infection exists and treat it appropriately. Horses with small nondisplaced, nonarticular fractures may be managed conservatively with stable rest. Most heal by fibrous union only. Horses may return to work in 8 weeks. Horses with fragments originating from the base of the patella need arthroscopic debridement if debris is loose in the joint. Small fragments at the base of the patella, which are embedded in the soft tissue attachments, may not require removal.91 Articular fractures of the medial aspect are best removed.88 This can be done by arthrotomy or arthroscopy (Figure 46-11) and requires careful dissection of the fragment from the medial patellar ligament. The distal end of the fracture is clearly seen arthroscopically. Concurrent joint damage should be evaluated and can have an important bearing on the outcome. Horses with complete horizontal fractures must be treated by internal fixation.89,92,93 Lag screw fixation with 5.5-mm cortex screws or partially threaded 6-mm cancellous screws, possibly with reinforcement with tension band wiring, is necessary to combat the huge distraction forces of the extensor muscles. Recovery from general anesthesia has to be carefully controlled by delaying attempts of the horse to stand by use of sedation to avoid breakdown of the repair. Sagittal fractures can also be repaired using the lag screw principle.94
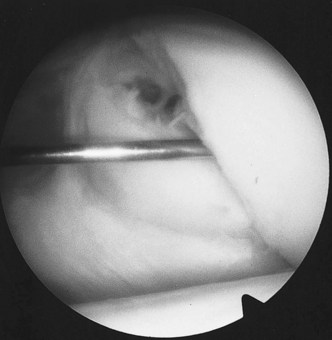
Fig. 46-11 Arthroscopic photograph of the left patella of the horse in Figure 46-10 showing the fracture line (with probe inserted) in the medial aspect of the patella.
Prognosis
Horses with small, nonarticular fractures usually have a good prognosis with conservative management.91 Ten of 12 horses with medial fractures without concurrent joint disease treated by partial patellectomy returned to athletic use.88 My experience has been similar. Internal fixation of horizontal and midbody vertical fractures can be rewarding, but the risk of breakdown during recovery from general anesthesia is substantial, especially in horses with horizontal fractures. Horses with severely comminuted fractures have a poor prognosis.
Fracture of the Intercondylar Eminence of the Tibia
These fractures have been described as avulsion fractures of the insertion of the cranial cruciate ligament.75,95,96 However, because the insertion of the cranial cruciate ligament is cranial to the eminence, they are not avulsions but are likely caused by trauma from a lateral force from the medial femoral condyle on the intercondylar eminence.97
Signs and Diagnosis
The history and clinical signs are similar to those seen with other acute, severe stifle injuries, and confirmation of the fracture is made radiologically. The caudocranial and flexed lateromedial images are the most useful. Once the acute inflammation has subsided, lameness can be mild to moderate in horses that do not have clinically significant injuries to vital soft tissue structures.
Treatment
An arthroscopic assessment is essential for evaluating the fracture and concurrent soft tissue damage in the joint, which is extensive in some horses. If accompanying soft tissue injuries are not severe, treatment can be rewarding. Small fragments should be removed. Horses with large fragments can be treated by internal fixation.97 Alternatively, large fragments can be removed, but this depends on fragment configuration and the involvement of soft tissue structures, such as the cranial cruciate ligament or the cranial ligament of the medial meniscus that wraps around the cranial surface of the eminence.95,96
Fracture Fragments Originating from the Femoral Trochlear Ridges or Femoral Condyles in Adult Horses
Fractures of the distal aspect of the femur usually result from direct external trauma, such as hitting a fence while jumping, a penetrating wound, or a kick.91,98
Signs and Diagnosis
Characteristically there is a sudden-onset, moderate to severe lameness, with a history of acute trauma. Effusion of the femoropatellar joint is usually present. With condylar fractures there is also effusion of the medial femorotibial joint. Crepitus may be present, and flexion of the joint causes pain. In the femoropatellar joint, fragments arise most commonly from the distal aspect of the lateral trochlear ridge and are best seen on flexed and standing lateromedial radiographic images. Caudocranial images are also important for identifying the position of fragments in the cranial or caudal femorotibial joints, and cranioproximal-craniodistal oblique images are necessary to rule out concurrent patellar fractures. The fracture site may not be obvious. Because these fractures are commonly caused by direct trauma, often the stifle region has a wound, and in these circumstances a strong chance of infection in the joint exists. Infection should be ruled out by arthrocentesis. Infection can also occur by extension into the joint, hours or even days after the injury. If a sudden increase in lameness occurs, arthrocentesis must be repeated.
Treatment
Fragments should be removed to prevent the development of OA. Most can be removed arthroscopically,91,98 but arthrotomy may be necessary for excision of large fragments.99 In many horses I prefer to wait a few days before examining the joints arthroscopically because the initial intraarticular hemorrhage hinders surgery. Many horses have a severely inflamed synovium in which fragments may be embedded and difficult to find. Fragments in the femoropatellar joints are often loose, whereas in the femorotibial joints they more often have soft tissue attachments, but conditions vary greatly, and intraoperative radiography to ensure removal of all fragments can be useful. Evaluation of the remainder of the stifle joint for concurrent injuries is important.
Prognosis
Horses with trochlear ridge fractures have a good prognosis after fragment removal.91,98 If no clinically significant soft tissue damage occurred, the prognosis is also favorable after removal of fracture fragments in the femorotibial joint. One should bear in mind on the initial assessment that some of these injuries are not as catastrophic as the radiological changes suggest.
Salter-Harris Fractures of the Femur, Types III and IV
Type III and IV Salter-Harris fractures of the femur tend to occur in older foals and usually result from a fall with the limb in adduction or from an external trauma. From limited reports, type II fractures, which are not discussed in this section, are the most common physeal fracture; however, of the articular fractures, type IV fractures appear to be more common.100-102 Type IV fractures often have a characteristic configuration in which the fracture begins in the trochlear ridges in the horizontal plane and exits through the caudal lateral diaphyseal cortex.100
Signs and Diagnosis
Foals with minimally displaced fractures may be weight bearing, but the others usually have acute, severe lameness, swelling, pain, and often crepitus in the affected joint. Radiology confirms the fracture and should include enough views to establish its configuration.
Treatment
Conservative treatment may be appropriate for horses with stable, minimally displaced fractures.100 Internal fixation is indicated for horses with displaced or unstable fractures. Repairs using lag screw fixation, cobra head bone plates, and angle blade plates have been reported.100-103 Implanting screws through the articular cartilage of the femoral trochlea is sometimes necessary, and crossing the physis with an implant does not seem to have affected growth in the distal femoral physis in older foals.100 The dynamic condylar screw plate may be of value.
Fractures of the Tibial Tuberosity
The tibial tuberosity is a relatively exposed structure and is susceptible to fracture after direct trauma, such as a kick, or a collision with a fence. These fractures are not associated with the physis of the tibial tuberosity and may not be authentic avulsion fractures, although the lateral patellar ligament is often involved. If patellar ligaments are involved, fractures may displace proximally.104 If proximal displacement is observed radiologically, a tension band technique should be used for surgical repair, although conservative management can be successful (see below). Traction apophysitis similar to Osgood-Schlatter disease in people has been reported in horses105 but is rare. In the horse reported, lameness was mild, and small fragments detached from the cranial aspect of the tibial tuberosity were visible radiologically. A variety of fracture configurations occur, from small fragments on the cranial proximal aspect to large fractures extending from distal to the tibial crest to proximally into the femorotibial joint.
Signs and Diagnosis
Most horses are acutely, severely lame immediately after sustaining the fracture, but in some this may settle into a milder lameness if left untreated. Swelling and crepitus are common. Occasionally with minimally displaced fractures there is only mild lameness and no history suggestive of a fracture. A wound on the lateral aspect of the tibia may be present, and intraarticular fractures may be associated with joint effusion. Care should be taken to rule out other injuries in the stifle, such as fracture of the patella, or joint infection if an open wound exists. Infection can even develop by extension into the joint through a skin graze. Because of the lateral curvature of the tibial tuberosity, several radiographic images are often required to identify the contour of the fracture, the caudolateral-craniomedial oblique image being the most useful. The tibial tuberosity does not fuse until at least 3 years of age,106 and its physis should not be confused with a fracture.
Treatment
Nonarticular fractures may heal with conservative treatment. Horses with large intraarticular fractures can also be treated by internal fixation. Lag screw fixation does not provide a secure enough repair, so tension band wiring,107 a lateral narrow dynamic compression plate,108 and a cranial narrow dynamic compression plate85 have been used. I believe that the most secure repair is achieved with the latter (Figure 46-12). The plate should extend well distal to the distal extremity of the fracture to withstand the distraction forces of the quadriceps muscles. Because of the shape of the cranial proximal aspect of the tibia, contouring of the plate demands considerable twisting and bending, but this does not seem to affect its efficacy. A technique for preoperative plate bending was reported as a way of saving surgery time,109 but in my experience plate contouring is not especially time consuming. Most horses are substantially more comfortable postoperatively, but they should be prevented from lying down for 2 weeks.
Prognosis
Conservative treatment of horses with nondisplaced, small fragments results in a good prognosis. Horses with larger fractures may also respond to conservative treatment with complete return to soundness. Fifteen horses with nonarticular fractures were treated conservatively, and 12 returned to full use. Neither size nor displacement of the fragment affected outcome, and the horses returned to work in a mean of 6.3 months.110 Those that remained lame had concurrent soft tissue injury in the stifle.110 Good results for return to full athletic function have been reported after repair with a cranially applied plate,104 and in my view this is the treatment of choice for articular fractures. A potential risk exists for failure of the repair during recovery from general anesthesia or the early postoperative period108 or for catastrophic tibial fracture. This emphasizes the importance of adequate fixation and restriction of the horse during early convalescence.
Fractures of the Fibula
Fracture of the fibula is usually caused by direct trauma and is a rare injury (see Chapter 45). Lameness is often moderate to severe at first. Palpation of the region may not elicit obvious pain, but radiography should be diagnostic. The caudocranial image is the most useful, but great care must be taken to differentiate a fracture from persistent radiolucent lines that result from separate ossification centers in the fibula. As many as three of these lines can be present, and they may be irregular. Scintigraphy is a useful aid to diagnosis in the absence of localizing clinical signs or if one has difficulty in radiological interpretation. From limited experience, confinement of the horse for 2 to 4 months is usually long enough for reasonable healing to take place, and the prognosis is good.
Other Diseases
Avulsion of the Origin of the Fibularis (Peroneus) Tertius and Long Digital Extensor Tendon
Avulsion of the origin of the fibularis tertius and long digital extensor tendon is a relatively rare condition in horses and is usually caused by sudden, forceful hyperextension of the hindlimb. Midsubstance tears are probably more common than avulsions of the common tendon of origin of the fibularis tertius and long digital extensor muscles, but the latter have been reported in foals.111-113 Avulsions of the origin of the fibularis tertius and long digital extensor muscle occasionally occur in adult horses,5 although more distal injuries are commoner. Foals may be more likely to suffer avulsions because of weaker bone.112 Minor disruption of the common tendon of origin may be seen arthroscopically.5
Signs and Diagnosis
The classical sign of rupture of fibularis tertius and avulsion of its origin is the ability to extend the hock while the stifle is flexed, resulting in a dimpling of the common calcaneal (“Achilles”) tendon. Synchronous flexion of the hock and stifle was reported with avulsions of the origin, presumably because the avulsed bone is held by the joint capsule.112 Horses may bear weight normally, but during the protraction phase of a stride, the distal limb appears flaccid. Lameness can be severe at first, and distention of the femorotibial and femoropatellar joints may be present. Radiological examination is necessary for diagnosing avulsion fractures. Minor disruptions of the tendon of origin manifest as nonspecific lameness associated with pain in the stifle and can be diagnosed by arthroscopic examination; they may accompany other stifle injuries.5
Treatment
Horses with injuries to the tendon of origin are usually best evaluated arthroscopically, which also offers the opportunity to check for concurrent injury. Small bone fragments can be removed, but large fragments embedded in the joint capsule may be better left.112 Six weeks of stable rest followed by controlled exercise for 3 months is recommended after surgery.
Calcinosis Circumscripta
Calcinosis circumscripta lesions are described as calcified, granular, amorphous deposits that induce fibrous reaction.114 They usually lie in the subcutaneous tissue close to joints or tendon sheaths. The lateral aspect of the stifle adjacent to the fibula is the predilection site for these lesions,114-116 but they have been reported on the dorsolateral surface of the hock,114 the neck, and the shoulder.114,115 Calcinosis circumscripta is an uncommon condition, more often seen in young horses. The cause is unknown.
Signs and Diagnosis
The usual reason for examination is an unsightly lesion that has been slowly increasing in size. Occasionally the lesion appears to affect the horse’s gait. Lesions are usually hard, well circumscribed, and firmly attached to underlying tissue. The overlying skin is not involved. Caudocranial radiographs show a circumscribed, roughly oval lesion of mineralized tissue (Figure 46-13) lying close to the lateral aspect of the femorotibial joint, with the bulk of the lesion distal to this. These lesions may be seen incidentally on scintigraphic examination as focal areas of intense IRU on the lateral proximal aspect of the crus. The lesion is clearly visible in a caudal image in a subcutaneous location, superficial to the tibial cortex, but in a lateral image IRU could be confused with a proximal tibial stress fracture.
Treatment
Treatment is only indicated if the lesion causes clinical complications or for cosmetic reasons. Surgical excision is necessary to remove the mass. Care should be taken when embarking on excision because some lesions are attached to the femorotibial joint capsule, which may be entered inadvertently. Steps should be taken to prevent postoperative seroma formation by closing dead space, suturing a stent bandage over the wound, and preventing the horse from lying down for several days postoperatively. The mass usually has a thick fibrous capsule and contains deposits of gritty material.
Hematoma in the Stifle Region
The stifle region is vulnerable to external trauma, particularly when horses jump. Profound injuries to vital structures may result, but frequently external trauma causes only superficial bruising or a subcutaneous hematoma. The clinician’s task is to differentiate between a swollen stifle that has a potentially career-threatening injury and one that has a superficial lesion such as a hematoma.
Signs and Diagnosis
A hematoma is manifested as a variably sized swelling, usually on the cranial aspect of the stifle, and may take several hours to reach maximum size. Smaller swellings may be difficult to differentiate from femoropatellar joint effusion. A hematoma is only painful on palpation until the initial bruising and swelling have settled. An uncomplicated hematoma does not usually cause lameness once the discomfort associated with the initial bleeding has passed. Other concurrent injury should be suspected if the horse is substantially lame, especially if lameness persists for several days. A hematoma may occasionally involve only the stifle initially but appears to spread to the inguinal and ventral abdominal areas. Huge swellings can cause oozing from the skin and skin loss. A careful search should be made for open wounds, which could lead to infection in the hematoma or cellulitis. Cellulitis usually takes at least 24 hours to form, and the swelling is firmer than a hematoma, hot, and painful. Lameness worsens as infection progresses.
Ultrasonography is a helpful tool for diagnosing hematoma, which can be confirmed by centesis of the swelling using aseptic technique. In the early stages, frank blood is retrieved, but as the blood clots, the fluid collected will be serum. Radiographic examination is indicated if lameness is severe or persists.
Treatment
In the initial phase, when hemorrhage is likely, the horse should be confined and cold applied to help to slow hemorrhage. Phenylbutazone can be given for its antiinflammatory effect. Antibiotics should be administered if the horse has an open wound. Although some clinicians believe that draining these hematomas is contraindicated, in my experience hematomas resolve better after effective drainage. Drainage should not be attempted until the hemorrhage has stopped and the free blood has clotted, usually 3 to 4 days after the injury. A 2- to 4-cm scalpel incision at the most dependent point of the hematoma ensures that drainage continues until the cavity has filled in.