Chapter 82Soft Tissue Injuries of the Pastern
Injuries to the digital flexor tendons and ligaments in the pastern are a common cause of lameness in horses.1-6 Injuries to the collateral ligaments or the palmar or plantar ligaments of the proximal interphalangeal joint are a less frequent cause of lameness.1,7-9 Swelling, heat, and sensitivity of the affected tendon or ligament to palpation often accompany lameness. Ultrasonographic evaluation of the pastern is indicated when local swelling, heat, and sensitivity are detected, or when effusion occurs in the digital flexor tendon sheath (DFTS).10 The cause of the swelling can be determined by ultrasonography, and the severity of the injury can be characterized. The clinician should keep in mind that peripheral longitudinal splits in the digital flexor tendons within the DFTS are difficult to detect and can be missed ultrasonographically.10 If injury occurs to the superficial or deep digital flexor tendons (SDFT, DDFT) in the metacarpal or metatarsal region, ultrasonographic examination should include an evaluation of these structures in the pastern. Lameness associated with soft tissue injuries of the pastern also can occur without localized soft tissue swelling, and ultrasonographic examination is indicated if pain is localized to the region using diagnostic analgesia and no radiological abnormality is detected, or entheseous new bone is seen. The clinician should bear in mind that intraarticular analgesia of the metacarpophalangeal or metatarsophalangeal joints, the proximal interphalangeal joint, and the DFTS is not necessarily specific and may influence closely related structures such as the distal sesamoidean ligaments and the palmar ligaments of the proximal interphalangeal joint. It also may be important to use diagnostic analgesia to determine whether the injury causing soft tissue swelling in the pastern region is the source of the lameness. Nuclear scintigraphy may help to determine whether entheseous new bone is active, and magnetic resonance imaging (MRI) has the potential to provide additional information. This chapter focuses on lesions diagnosed using ultrasonography, but the absence of detectable ultrasonographic abnormalities does not preclude soft tissue pathology causing pain.
Anatomy
Most of the soft tissue structures in the pastern are on the palmar or plantar aspects and are similar in the forelimbs and hindlimbs. The following describes the forelimb but applies equally to the hindlimb. The SDFT forms a thin ring around the DDFT at the ergot and in the proximal-most portion of the pastern and then bifurcates into medial and lateral branches. The origin of the branches has a teardrop shape. The cross-sectional area (CSA) of each SDFT branch gradually enlarges as the branch extends distally along the palmarolateral and palmaromedial aspects of the pastern, until the branches insert on the distal aspect of the proximal phalanx and on the proximal aspect of the middle phalanx. The DDFT lies immediately dorsal to the SDFT and extends along the midline to its insertion on the distal phalanx.1-6,11-15 The DDFT has a bilobed shape in the pastern and is surrounded by the DFTS. The oblique (middle) sesamoidean ligaments (OSLs) originate from the base of the lateral and medial proximal sesamoid bones (PSBs) as two large, round to oval branches. These branches become smaller in CSA as they extend distally. The branches join in the proximal to mid aspect of the proximal phalanx and insert as a broad band on the palmar aspect of the middle of the proximal phalanx. The straight sesamoidean ligament (SSL) also has its origin at the base of the PSBs and the palmar ligament and extends distally in the midline, palmar to the OSL, to insert on the scutum medium of the middle phalanx.1-6,11-13,16 The SSL lies dorsal to the DDFT and has an hourglass shape, larger proximally and distally, and narrowest in the middle.
The DFTS surrounds the SDFT and DDFT throughout the proximal aspect of the proximal phalanx to the bifurcation of the SDFT.1-6,11-15,17 The entire length of the DDFT is included in the DFTS, except for a small area in the distal palmar aspect of the pastern, just proximal to the bulbs of the heel. The dorsal aspect of the DFTS extends farther distally than its palmar aspect. The proximal digital annular ligament is adhered closely to the palmar aspect of the SDFT in the proximal aspect of the pastern.1,3-5,18 The distal digital annular ligament forms a sling over the distal part of the DDFT. These two structures are thin in normal horses.
The abaxial and axial palmar ligaments of the proximal interphalangeal joint originate in pairs from the medial and lateral aspects, respectively, of the middle of the proximal phalanx and dorsal to the SDFT branches. They insert on the scutum medium abaxial to the branches of the SDFT (abaxial palmar/plantar ligament) and between the SSL and the branches of the SDFT (axial palmar/plantar ligament). These are large, round to oval ligaments that extend in a diagonal direction from the origin to the insertion. The collateral ligaments of the proximal interphalangeal joint originate from a small eminence on the lateral and medial aspects of the proximal phalanx, distal to the origin of the palmar ligaments, and arc across the joint to insert on a small eminence on the lateral and medial aspects, respectively, of the proximal aspect of the middle phalanx.1,3,7,11 The proximal interphalangeal joint has a closely adhered joint capsule.
The common digital extensor tendon is located on the dorsal aspect of the pastern.1 The extensor branches of the suspensory ligament (SL) join the common digital extensor tendon in the distal part of the proximal phalanx. The main insertion of the common digital extensor tendon is on the extensor process of the distal phalanx, but there are also areas of insertion onto the proximal and middle phalanges. A bursa is present between the tendon and the proximal interphalangeal joint.
Ultrasonographic Anatomy
The pastern has been divided into five zones: three zones for the proximal phalanx and two zones for the shorter middle phalanx1-6,12-15 (see Chapter 16).
Superficial Digital Flexor Tendon
In the proximal aspect of the pastern (zone P1A), the SDFT is imaged from the palmar aspect and is homogeneously echogenic and has a thin, half-moon shape in the transverse plane.1-6,12-14 In longitudinal images the SDFT has a parallel fiber pattern and a triangular shape along the midline in zone P1A because its thickness decreases distally. In normal horses, distinguishing the proximal digital annular ligament from the DFTS and the palmar border of the SDFT is difficult. The proximal digital annular ligament can be identified if thickened by following it medially and laterally to its attachment to the proximal aspect of the proximal phalanx. The body of the SDFT ranges in thickness (palmar to dorsal) from 2 to 6 mm in P1A to 1 to 4 mm over the middle of the proximal phalanx.3 The teardrop-shaped branches in the proximal to mid pastern region (at the junction of zones P1A and P1B) are imaged from the palmaromedial and palmarolateral aspects and are followed individually to triangular-shaped insertions. The SDFT branches are similarly homogeneously echogenic, with a parallel fiber pattern throughout. The branches of the SDFT range in thickness from 4 to 7 mm in the proximal pastern to 7 to 12 mm distally.15 The CSA of the two SDFT branches ranges from 0.3 to 0.4 cm2 in the distal portion of zone P1A where the branch begins, increases to 0.4 to 0.6 cm2 in zone P1B, and further enlarges to 0.6 to 0.8 cm2 near the insertion.
Deep Digital Flexor Tendon
The DDFT has an oval to bilobed appearance in the pastern and is imaged on the palmar midline of the pastern until the DDFT is lost from view distally.1-6,12-15 The two lobes are symmetrical. The fibers of the DDFT extend obliquely from a deeper to a more superficial position in the more distal portion of the pastern and are separated from the SSL by an anechogenic space. The dorsopalmar thickness and lateral to medial width of the DDFT decrease in the mid pastern and increase again in the distal aspect of the pastern. The DDFT measures 5 to 10 mm (palmar to dorsal) in the proximal aspect of the pastern, slightly less in the mid pastern, and 7 to 12 mm in the distal aspect of the pastern. The width of the DDFT in a lateral-to-medial direction ranges from 18 to 33 mm in the proximal aspect of the pastern, decreasing to 15 to 23 mm in the mid pastern, and increasing in the distal aspect of the pastern to 23 to 32 mm.3 Along the dorsal aspect of the DDFT in the mid pastern region is a synovial fold of the DFTS that is imaged readily, surrounded by a small amount of anechogenic synovial fluid. In the distal pastern region, the palmar aspect of the DDFT adheres to the synovial membrane of the DFTS.
Oblique Sesamoidean Ligaments
Injury to the OSLs is often missed ultrasonographically because the origin and proximal to midportion of each OSL (where the majority of the injuries are) are not imaged from the palmaromedial and palmarolateral aspects of the limb. The origin of the medial or lateral OSL is best found by placing the ultrasound transducer over the base of the medial or lateral PSB and scanning distally over the bone to its base, angling the transducer proximally to image the origin of the respective OSL.1-6,12,13 Alternatively, the origin of an OSL can be found by following the SL branches distally over the respective PSBs to the base. Immediately distal to the base of the PSB is the origin of an OSL, best located initially in its transverse section as a large, round to oval structure. The OSLs merge in the distal part of zone P1A into a broad, rectangular band dorsal to the DDFT. The OSLs then insert on the palmar or plantar aspect of the proximal phalanx in zone P1B. An OSL is the most difficult tendon or ligament to follow longitudinally to its insertion because the ligament extends diagonally from its origin to its insertion in two different planes. Following the medial or lateral OSL from its origin to the main body of OSL requires a transducer angle of about 45 degrees from the base of the PSBs to the palmar midline of the proximal phalanx. Properly aligning the transducer and eliminating off-normal incidence artifact is difficult. The OSLs may appear less echogenic because of an oblique orientation. The OSLs are thickest in the medial to lateral direction proximally. Each OSL measures 12 to 20 mm (lateral to medial) in the proximal aspect of P1A, decreasing to 9 to 17 mm just before their convergence, and 0 to 9 mm (one side only) at their insertion. The palmar to dorsal thickness of the OSLs is 5 to 12 mm in P1A, decreasing to 2 to 6 mm just proximal to the convergence, and decreasing again to 0 to 3 mm at the insertion. The mean CSA of an OSL determined with MRI is reported to be 0.86 cm2 in the proximal third, 0.56 cm2 in the middle third, and 0.40 cm2 in the distal third.19 However, there may be size differences between the medial and lateral OSLs.20
Straight Sesamoidean Ligament
The origin of the SSL is found by angling the transducer in a proximal and dorsal direction from the proximal-most aspect of the pastern, just underneath the ergot, to image the ligament and the base of the PSBs. The SSL becomes a more oval-shaped structure and is palmar to the OSLs in zone P1B. The SSL remains dorsal to the DDFT as it inserts on the scutum medium.
The dorsal-to-palmar thickness of the SSL gradually increases as the medial to lateral width decreases. The SSL measures 5 to 9 mm (palmar to dorsal) proximally, increasing slightly over the distal aspect of the proximal phalanx to 6 to 12 mm, and increasing again to 8 to 14 mm at the scutum medium. The medial-to-lateral thickness of the SSL ranges from 17 to 30 mm in zone P1A, decreases to 10 to 15 mm, and then widens over the scutum medium to 45 to 65 mm.3 The SSL is echogenic with normal parallel fiber alignment throughout, except at the insertion. A central symmetric hypoechoic area is commonly imaged in clinically normal horses at the insertion of the SSL.16 Care must be taken to be sure that lesions are not created at the insertion of the SSL because of the difficulty in aligning the transducer perpendicular to the ligamentous fibers owing to the horse’s heel. Comparison of this area with the contralateral normal limb should aid in determining whether a suspected lesion is real.
Cruciate Sesamoidean Ligaments
The cruciate sesamoidean ligaments are imaged only in the proximal-most portion of the pastern and measure 2 to 4 mm in a palmar to dorsal direction.3
Collateral Ligaments
The collateral ligaments of the proximal interphalangeal joint are easiest to examine by imaging in both longitudinal and transverse planes. The collateral ligaments of the proximal interphalangeal joint are homogeneously echogenic structures, with a parallel fiber pattern at the origin on the distal aspect of the proximal phalanx to the insertion on the proximal half of the middle phalanx.1,2
Proximal Interphalangeal Joint
The proximal interphalangeal joint is easiest to image initially in the longitudinal plane by identifying the joint space, and then a transverse evaluation of the joint can be made.7 Fluid normally is not imaged in the proximal interphalangeal joint.
Palmar/Plantar Ligaments of the Proximal Interphalangeal Joint
The palmar ligaments of the proximal interphalangeal joint can be imaged from the origin on the middle of the proximal phalanx to the insertion on the proximal palmar aspect of the middle phalanx. These ligaments are paired on the medial and lateral aspects of the pastern and are located by placing the transducer dorsal to the branch of the SDFT. The more abaxial branch originates first and is easier to follow than the more axial branch. Each branch has a round to oval shape, is homogeneously echogenic with a parallel fiber pattern, and must be followed individually from origin to insertion.
Digital Nerves
The digital nerves are located dorsal to the lateral and medial aspects of the SDFT, adjacent to the lateral or medial palmar digital arteries.1 The nerves are found most easily by identifying the digital vein and artery, looking immediately adjacent (palmar) to the digital vein and the adjacent SDFT. The nerves are tiny, homogeneously echogenic circular structures. The normal thickness of the palmar or plantar digital nerves is 2 to 3 mm, with a CSA of 0.5 to 1 mm2.1
Tendon and Ligament Injuries
In the fore pastern, the SDFT is the most frequently injured tendon or ligament in all performance horses.1-6,21 The OSLs are the second most commonly injured structures in the fore pastern, followed by injuries to the DDFT and SSL.1-6 In the hind pastern, injuries to the DDFT are most common, with a low incidence of injuries to the other tendonous and ligamentous structures.1-5 Injuries to the DDFT are accompanied most often by tenosynovitis of the DFTS.1-6 Injuries to the collateral ligaments of the proximal interphalangeal joint occur infrequently and are more common in the forelimb.1,3,7 Injuries to the palmar/plantar ligaments of the proximal interphalangeal joint are also uncommon and occur in forelimbs (most common) and hindlimbs. The tendonous and ligamentous structures in the pastern have little covering, and thus they are vulnerable to injury with puncture wounds and lacerations. Ultrasonographic evaluation of the pastern region in a horse with an acute laceration or puncture wound to the pastern should be performed aseptically and is an integral part of the evaluation of these soft tissue structures to determine whether injury occurred and the severity of the injury.
Superficial Digital Flexor Tendonitis
Injuries to the branches of the SDFT are more common in the forelimb.1-6,21,22 Injury in the pastern may occur in isolation, without an injury to the SDFT in the metacarpal or metatarsal region, or may be an extension of a more proximal tendon injury. Extension of the SDFT injury into the proximal pastern region, and less frequently into the mid and distal pastern, is more common in the forelimb. Abnormal conformation such as a long pastern, an underrun heel, or an axially displaced heel may predispose to injury of an SDFT branch.
Lameness usually occurs at the onset of injury, is more common with SDFT injuries in the pastern than with those in the metacarpal or metatarsal region, and may persist longer, lasting for 1 to 4 weeks. Longitudinal swelling that extends in a proximal-to-distal direction along the lateral or medial aspect of the pastern throughout its length is often characteristic.1,2,21 Focal heat and sensitivity usually accompany this swelling. However, in horses with acute injuries, no localizing clinical signs may be apparent, but lameness is alleviated by palmar (abaxial sesamoid) nerve blocks. Generally, swelling develops within 3 to 4 days. Ultrasonographic examination in the absence of swelling may result in false-negative results. Subluxation of the proximal interphalangeal joint can occur in horses with severe injury to or complete rupture of the SDFT in the pastern. Dropping of the fetlock joint with weight bearing can occur in horses with severe SDFT injury.
Core injuries are the most common detected by ultrasonography (Figure 82-1), followed by diffuse injury to the affected branch.1,2 Complete ruptures or near complete ruptures of the branches do occur, but they are less frequent. These injuries can be unilateral or bilateral and uniaxial or biaxial, although uniaxial injuries are most common. The frequency of injury to the medial or lateral SDFT branch varies with the type of racing or sporting activity.21,22 Peritendonous soft tissue swelling is common. Avulsion fracture of the insertion of the SDFT branch occurs infrequently. Ultrasonographic evaluation of the more proximal aspect of the SDFT in the metacarpal or metatarsal region is indicated to determine whether the injury is an extension of a more proximal injury (see Chapter 69) (Figure 82-2). Ultrasonographic evaluation of the contralateral fore or hind pastern is recommended because bilateral disease may be present, more frequently in the forelimb. Radiological examination of the pastern is indicated for all horses with subluxation of the proximal interphalangeal joint, avulsion fractures at the insertion of the SDFT branch, or a ruptured SDFT branch.
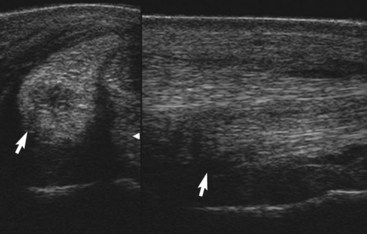
Fig. 82-1 Ultrasonographic images of the right front medial branch of the superficial digital flexor tendon obtained in the proximal part of zone P1C in a horse with a recent injury. The anechoic to hypoechoic core lesion is apparent within the branch (arrows) in the transverse (left) and longitudinal (right) views. Fiber disruption and short linear fibers are imaged within the lesion in the longitudinal view, consistent with a recent injury and early healing. The horse was 1 of 5 degrees lame, with focal swelling, heat, and sensitivity to palpation.

Fig. 82-2 Ultrasonographic images of the left superficial digital flexor tendon (SDFT) in the metacarpal region (A) and pastern (B) obtained from a horse with an acute severe injury to that tendon. This horse was lame at the walk, with substantial swelling of the SDFT in the metacarpal and pastern regions and heat and sensitivity of the tendon on palpation. The metacarpophalangeal joint dropped on weight bearing. A, The SDFT is enlarged (arrows) and contains a large central anechoic lesion completely lacking in tendon fibers. The SDFT was severely injured in the metacarpal region from 7 to 32 cm distal to the accessory carpal bone. The SDFT in zone 3C is surrounded by a thickened hypoechogenic digital flexor tendon sheath (DFTS). The transverse image is on the left, and the longitudinal image is on the right. B, The SDFT in zone P1A is markedly enlarged (arrows) with a central anechoic lesion that extended distally to the insertion of the lateral branch. The surrounding DFTS and peritendonous tissues are greatly thickened and hypoechogenic, and the distinction between the palmar margin of the SDFT and the peritendonous structures is difficult to discern. The lateral branch of the SDFT has nearly complete fiber disruption that extends to its insertion. The lateral side of the proximal pastern is the right image, and the medial side of the pastern is the left image. The SDFT and the DFTS were so enlarged that they could not be imaged in their entirety in a single image. Therefore the two halves of the SDFT were displayed together in these transverse images.
Treatment for horses with acute superficial digital flexor tendonitis in the pastern is similar to that in the metacarpal or metatarsal region.1,2 Horses with SDFT injuries in the pastern may have a poorer prognosis for returning to racing than those with injuries in the metacarpal region, with a more frequent recurrence of injury.1,2,22 Extension of the injury from the pastern to the metacarpal area may also occur, resulting in a shortened racing career.21 However, successful return to performance does occur for horses with SDFT branch injuries. Rare horses are able to continue to compete with SDFT branch injuries, without a period of rest, but these are the exceptions rather than the rule. Healing of the SDFT occurs similarly to that in the metacarpal region, with an increase in the echogenicity of the lesion and the subsequent appearance of short, usually randomly aligned linear echoes. Rehabilitation of horses with injuries to the SDFT branch is similar to that described for proximally located tendonitis and is based on the injury severity (see Chapter 69). A minimum of 6 months in a controlled exercise program is needed for horses with mild SDFT branch injury, whereas 12 months or more are indicated for those with severe injury to the SDFT branch to maximize the horse’s chance of returning to its previous level of competition. Ultrasonographic monitoring of tendon healing is an important part of the rehabilitation program. A central echogenic scar surrounded by a hypoechoic halo may be detected in the SDFT branch with a healed core lesion (Figure 82-3). Peritendonous echogenic tissue representing immature and maturing fibrous tissue often is imaged adjacent to the injured SDFT branch and can result in adhesions between the branch and the surrounding tendonous and peritendonous structures. New areas of fiber disruption often occur adjacent to the previously healed area or are associated with adhesions to the surrounding tendonous or peritendonous structures.
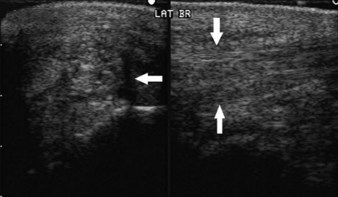
Fig. 82-3 Ultrasonographic images of the left front lateral branch of the superficial digital flexor tendon obtained in zone P1B of a horse with a chronic healed core injury. The horse had sustained the original injury more than 5 years earlier, and after a long, controlled exercise program the horse had raced successfully several times a year, although some small areas of reinjury were detected periodically, necessitating short periods of downtime from race training. The original central core lesion is still visible in this branch as an echogenic central area, with a thin hypoechoic rim (arrow) in the transverse view (left) and longitudinal (right) views. In the longitudinal view, the central area of the tendon has a more random fiber pattern than the periphery (arrows).
Distal Sesamoidean Desmitis
Oblique Sesamoidean Desmitis
Desmitis of an OSL is the most common distal sesamoidean ligament injury and is seen in all types of performance horses.1-6 Horses with a valgus or varus limb conformation or a long sloping pastern may be at increased risk for OSL injuries. Swelling in the pastern region in horses with OSL injuries is characteristic because this ligament runs diagonally across the proximal to mid pastern, and swelling of the pastern usually occurs in this direction. Many horses have a boxy appearance to the fetlock joint from swelling at the origin of an OSL. Most horses have local swelling, heat, and pain detected on palpation of the affected ligament and lameness in the affected leg. However, some lesions restricted to the origin of the ligament occur without palpable abnormalities. Chronic injuries may be associated with dorsal enlargement of the dorsal articular margins of the proximal interphalangeal joint. Subluxation of the proximal interphalangeal joint can also occur in horses with either chronic injuries or complete rupture of the OSLs. This is characterized clinically by a dorsally convex profile of the pastern. Complete biaxial rupture of the OSLs is more common in Thoroughbreds and can have catastrophic implications. Injury to the medial OSL is more common than lateral OSL injury and is more common in the forelimb than in the hindlimb.3 Hindlimb OSL injuries are more common in nonracehorses. Horses with SL injury are also at increased risk of injuring the OSLs. Therefore ultrasonographic evaluation of the SL is recommended for all horses with oblique sesamoidean desmitis.
Discrete core lesions often are seen in both OSLs, although diffuse areas of fiber damage and splits also occur (Figure 82-4). Injuries to the insertion of an OSL are usually diffuse (Figure 82-5). Periligamentous soft tissue thickening is often seen. Comparison of the ultrasonographic findings in the affected limb with the contralateral limb is recommended to be sure that subtle or early injuries are not missed. The origin and insertion of the OSLs should be carefully evaluated for avulsion fractures.1,2 Avulsion fractures usually occur in association with fiber tearing in the distal sesamoidean ligaments and occur from the base of the PSBs (Figure 82-6) and the insertion on the proximal phalanx. Avulsion fractures remain visible for years after the original injury, long after the associated desmitis in the distal sesamoidean ligament has resolved. Radiographs of the fetlock (particularly the PSBs) and the pastern regions should be obtained in all horses with OSL desmitis, paying careful attention to the base of the PSBs. However, it is important to recognize that entheseous new bone on the base of one or both of the PSBs or on the midpalmar aspect of the proximal phalanx can be seen as incidental radiological abnormalities, unassociated with lameness or active desmitis. Homogeneously radiodense mineralized bodies are also sometimes seen distal to the PSBs as incidental findings.

Fig. 82-4 Ultrasonographic images of the origin of the left hind lateral oblique sesamoidean ligament (OSL) obtained in zone P1A. Most of the OSL is hypoechoic (arrow) in the transverse (left) and longitudinal (right) views (proximal is to the right). Substantial fiber disruption is visible in the longitudinal view, beginning at the base of the proximal sesamoid bone (arrow). There is no normal fiber pattern imaged at the origin of the lateral OSL. The more anechoic abaxial region represents a more recent injury, whereas the more echogenic area axially with a random fiber pattern represents a more chronic area of injury that is repairing. Some periligamentous echogenic soft tissue thickening surrounds the branch. The horse had a concurrent distal suspensory desmitis involving both suspensory branches that extended from 37 to 47 cm distal to the point of the hock. The horse was 2 of 5 degrees lame and had local heat, swelling, and mild sensitivity of the lateral OSL.
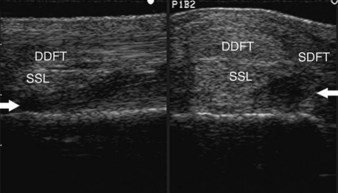
Fig. 82-5 Transverse (right) and longitudinal (left) ultrasonographic images of the right fore lateral oblique sesamoidean ligament (OSL) obtained where the two OSLs join. The lateral aspect of the transverse view is on the right side of the image. This horse had sustained an acute injury to the lateral OSL from the base of the lateral proximal sesamoid bone to its insertion. A large anechoic to hypoechoic core lesion (arrows) is visible. The horse was lame at the walk, with mild subluxation of the proximal interphalangeal joint and local swelling, heat, and sensitivity along the entire lateral OSL. DDFT, Deep digital flexor tendon; SSL, straight sesamoidean ligament; SDFT, superficial digital flexor tendon.
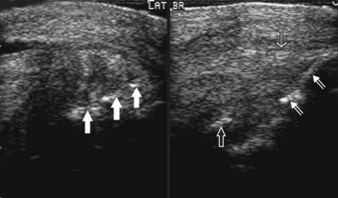
Fig. 82-6 Transverse (left) and longitudinal (right; proximal to the right) ultrasonographic images of the medial oblique sesamoidean ligament (OSL) obtained in zone P1A of the left forelimb in a horse with chronic active desmitis of the OSL and a small basilar sesamoid fracture. The hyperechogenic bony fragment (open arrow) is distracted away from the base of the proximal sesamoid bone (PSB) in the longitudinal view. Hyperechoic areas are visible in the transverse view (large arrows), and areas of amorphous and random fiber pattern are imaged in the longitudinal view, proximal and distal to the fracture fragment. There is cortical irregularity of the base of the PSB (small arrows) in the longitudinal image. The horse was 1 of 5 degrees lame, with thickening of the base of the lateral PSB but no heat or local sensitivity.
Since MRI has become used more frequently in the search for a diagnosis for horses with pain causing lameness localized to the fetlock or pastern region by diagnostic analgesia, the limitations of ultrasonography for injury diagnosis in the pastern have become more apparent.19,20,23 Injuries of the OSLs, SSL, and cruciate ligaments may be overlooked. Moreover, local analgesic techniques may be confusing. Pain associated with proximal lesions of these ligaments can be abolished by intraarticular analgesia of the fetlock or by intrathecal analgesia of the DFTS.23 However, care should be taken in the interpretation of signal intensity alterations on magnetic resonance images of the OSLs because of the magic angle effect,24 and the variable alignment of fibers in the proximal part of the ligaments.25 Lesions characterized by an increase in size of an OSL and increased signal intensity in T1- and T2-weighted images can be seen as incidental findings in association with other primary causes of lameness.20 However, genuine primary lesions can be identified.19,23 Thirty-nine sports horses with pain localized to the fetlock region underwent MRI because conventional imaging techniques failed to yield a diagnosis.23 Injury of one or more of the distal sesamoidean ligaments was identified as the primary cause of lameness in 21 (54%) horses.
Horses with acute injuries to the OSLs should be managed in the same way as those with other tendon and ligament injuries, with initial antiinflammatory therapy and exercise restriction.1,2 A controlled exercise program with incremental increases in the exercise level should be based on ultrasonographic monitoring. As the injury heals, the CSA of the ligament usually decreases, the echogenicity of the lesion increases, and linear echoes are imaged in the area of previous fiber tearing. A long recuperative period usually is indicated for horses with desmitis of an OSL to maximize the chance of return to athletic function.
Prognosis for horses with OSL injury is guarded to grave for returning successfully to racing and other competitive athletic activities and depends on the severity of the injury. Horses with coexisting suspensory desmitis, basilar fractures of the PSBs, or subchondral palmar third metacarpal or plantar third metatarsal bone disease have a poorer prognosis for return to athletic function. The incidence of recurrence of OSL injury is high. Prognosis is grave for athletic horses with subluxation of the proximal interphalangeal joint associated with distal sesamoidean desmitis.
Straight Sesamoidean Desmitis
Injuries to the SSL occur infrequently and may occur alone or with other soft tissue injuries.1-6 These injuries usually are associated with lameness, but focal heat, swelling, and sensitivity are not always detected. Lameness is usually acute in onset and may be severe. Some horses, especially those with proximal lesions, never develop localizing soft tissue swelling, and diagnosis depends on localizing pain to the pastern region by diagnostic analgesia and subsequent ultrasonographic identification of a lesion. The ease with which the most proximal aspect of the ligament can be seen depends on the conformation of the horse and the position of the ergot. Ultrasonographic evaluation of the SSL is most difficult in horses with short pasterns and easiest in those with relatively long, upright pasterns.
Small splits or core lesions may be seen in the SSL.1-6 Large areas of fiber disruption in the SSL are uncommon (Figure 82-7). Areas of periosteal proliferative change or avulsion fractures at the insertion of the SSL on the proximal aspect of the middle phalanx may be seen (Figure 82-8). Avulsion fractures of the origin of the SSL are less common than with OSL desmitis, but the base of the PSBs should be evaluated carefully.
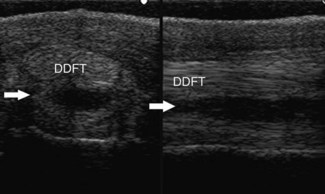
Fig. 82-7 Ultrasonographic images of the right hind pastern obtained in zone P1A from a horse with an acute injury to the straight sesamoidean ligament (SSL). The horse was lame at the walk, with swelling of the proximal palmarolateral aspect of the pastern and local heat and sensitivity. The large anechogenic lesion (arrows) in the plantar aspect of the SSL is visible in the transverse view (left), with complete fiber disruption in this region that is best imaged on the longitudinal view (right). The SSL is mildly enlarged along the midline in the dorsal to palmar direction. Note also the markedly thickened subcutaneous tissues.
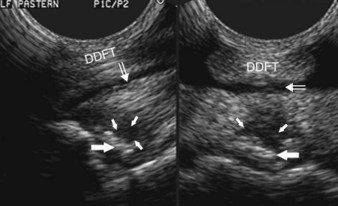
Fig. 82-8 Ultrasonographic images of the left fore straight sesamoidean ligament (SSL) obtained in zone P1C-P2A from a horse with an acute severe injury to the SSL and an avulsion of its insertion onto the scutum medium. The horse was lame at the walk, with subluxation of the proximal interphalangeal joint and substantial soft tissue swelling of the palmar pastern, with local heat and pain on palpation of the oblique sesamoidean ligament (OSL) and SSL. The hypoechoic lesion (small arrows) in the distal-most portion of the SSL and the hyperechogenic fragment distracted away from the middle phalanx (large arrows) are visible in the transverse (right) and longitudinal (left) views. There is anechogenic effusion (open arrows) in the digital flexor tendon sheath. DDFT, Deep digital flexor tendon.
Treatment for horses with SSL desmitis is similar to that recommended for horses with OSL desmitis.1-6 Horses with mild injuries have returned successfully to racing, but the prognosis for horses with more severe lesions is guarded for any form of competitive athletic function because recurrent injury is common. Horses with multiple tendonous or ligamentous injuries in the pastern have a guarded to grave prognosis for returning to full athletic function.
Proximal Digital Annular Desmitis
Desmitis of the proximal digital annular ligament or proximal digital annular ligament constriction occurs infrequently (see Chapter 74).1,3 Affected horses usually have chronic moderate to severe lameness. Distention of the palmar pouch of the DFTS is usually present, in addition to subtle distention proximal to the palmar annular ligament of the fetlock. Thickening of the proximal digital annular ligament and skin usually is substantial, with a combined thickness of 4 to 5 mm (normal thickness is 1 to 2 mm) and distention of the DFTS.21 Ultrasonographic evaluation of horses with proximal digital annular desmitis often reveals thickening of the synovium of the DFTS, in addition to the proximal digital annular ligament, and may reveal tendonitis of the SDFT or DDFT. Adhesions between the SDFT and the proximal digital annular ligament are suspected when restricted movement of the tendon relative to the proximal digital annular ligament is imaged during a dynamic examination.
Soft Tissue Swelling
Soft tissue swelling in the pastern, without tendonous or ligamentous injury, can result from skin irritation caused by liniments, blisters, local therapeutic ultrasound or cold laser treatment, local trauma from a blow, bandaging, or bell (overreach) boots, or from a skin infection. Ultrasonographic findings of thickened anechogenic to echogenic subcutaneous tissues, with normal tendonous and ligamentous structures, are typical for injury or inflammation to the skin and subcutaneous tissues. Thickening of the skin also may be seen in horses with skin irritation or infection. These horses usually respond well to local or systemic antiinflammatory therapy.
Tenosynovitis of the Digital Flexor Tendon Sheath
Tenosynovitis of the DFTS is discussed in Chapter 74.
Abnormalities of the Pastern Joint
Lameness and local swelling are two common findings in horses with injuries of the collateral or palmar ligaments of the proximal interphalangeal joint.1,3-5,7-9 Swelling is usually primarily medial and lateral, although it can be circumferential. Acute desmitis of the collateral ligaments may be confirmed by ultrasonography, with decreased echogenicity and loss of fiber pattern, with or without an associated avulsion fracture (Figure 82-9).1,3-5,7 In horses with more chronic injuries, enthesophyte formation at the origin and the insertion of the collateral ligaments usually is detected. A smoothing of these areas of insertional injury occurs as the desmitis becomes inactive. Similar ultrasonographic findings may be detected in horses with acute (Figure 82-10) and chronic injury (Figure 82-11) to the palmar ligaments of the pastern. These horses have a guarded prognosis for return to full athletic function. Bony proliferative changes associated with “high ringbone” are also easily imaged ultrasonographically.
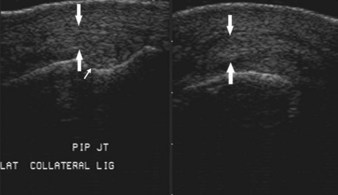
Fig. 82-9 Longitudinal ultrasonographic images of the lateral collateral ligament of the proximal interphalangeal joint of the right hindlimb of horse with moderate lameness and localized swelling. The thickening of the lateral collateral ligament (large arrows), the hypoechoic areas of fiber disruption, and the short random fiber pattern seen in the longitudinal view are consistent with desmitis. The distal portion of the proximal phalanx is on the right side of both longitudinal images, and the proximal portion of the middle phalanx is on the left side of both images. The right image is the proximal portion of the lateral collateral ligament, and the left image is the distal portion of the ligament. The small anechoic slit between the proximal and middle phalanges represents the joint space (small arrow). There is marked bony proliferative change (irregular bone at the joint space), especially on the proximal aspect of the middle phalanx. Some echogenic subcutaneous thickening is present superficial to the collateral ligament.
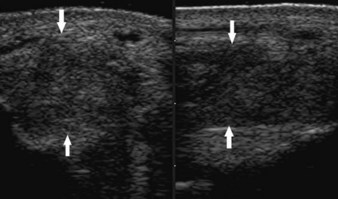
Fig. 82-10 Ultrasonographic images of the left abaxial plantar ligament of the proximal interphalangeal joint in a horse with severe desmitis associated with mild lameness and localized swelling. There is marked enlargement of the ligament. It is hypoechoic and circular to oval in the transverse view (left) and has a random fiber pattern in the longitudinal view (right). The arrows outline the margins of the ligament. A small amount of echogenic peritendonous subcutaneous tissue is visible.
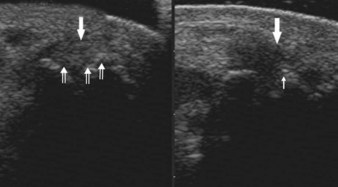
Fig. 82-11 Ultrasonographic images of the lateral palmar ligament of the proximal interphalangeal joint (large arrows) in a horse with chronic severe desmitis and severe enthesopathy. The bony proliferative changes of the proximal phalanx (small arrows) in the transverse (left) and longitudinal views (right) make imaging the ligament in its entirety in either plane impossible at the ligament’s origin. The visible portion of the ligament contains hypoechoic areas adjacent to the bony proliferative change in both views and near the ligament’s origin in the longitudinal view. The gelding was 2 of 5 degrees lame, with thickening over the lateral and medial aspects of the proximal phalanx, but no heat or local sensitivity was detected.
Neuritis/Neuroma
Neuritis of the palmar (plantar) digital nerves results in acute lameness associated with exquisite pain on palpation of the nerves and localized heat and swelling. Ultrasonography shows swelling and decreased echogenicity of the nerve (Figure 82-12). Neuromas following palmar digital neurectomy initially appear as focal painful swellings over the stump of the digital nerve. With ultrasonography, the nerve appears enlarged and hypoechoic, with perineural soft tissue swelling in horses with an acute neuroma. The neuroma becomes more echogenic and heterogeneous with increasing chronicity of injury. A large amount of perineural echogenic tissue may be present in horses with chronic neuromas.
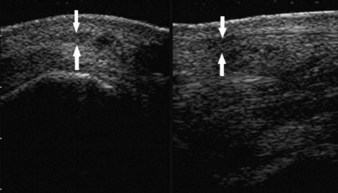
Fig. 82-12 Transverse (left) and longitudinal (right) ultrasonographic images of the right fore medial palmar digital nerve obtained from a horse with a neuroma resulting in acute onset of moderate lameness with local swelling, heat, and exquisite sensitivity to palpation. The enlarged nerve ending (arrows), oval to circular shape, is located palmar to the digital artery in the transverse view and superficial to the medial branch of the superficial digital flexor tendon in both views. The cross-sectional area of the nerve is markedly increased. Anechoic and hypoechoic areas disrupt the nerve ending (arrows). Notice also the perineural soft tissue thickening.