Chapter 109The European and Australasian Standardbreds
 The European Standardbred
The European Standardbred
Dimensions and Characteristics
The European Standardbred (STB) is historically the result of different crosses between the classic American bloodlines and European families. The French STB is known for its stamina and aptitude for long distances. The American-derived families, however, have been selected for speed and racing at a fixed distance of 1 mile and are represented more widely in Italy and Sweden. Several countries (especially France, Italy, Germany, and the Scandinavian countries) have developed individual bloodlines and today are able to produce good-quality STB trotters. In Europe no races are available for pacers. In Table 109-1 the STB population and racing activity of different European countries are listed.
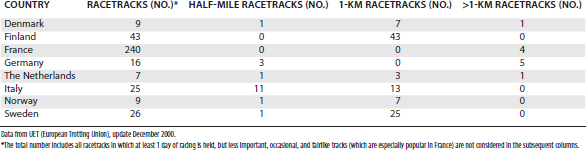
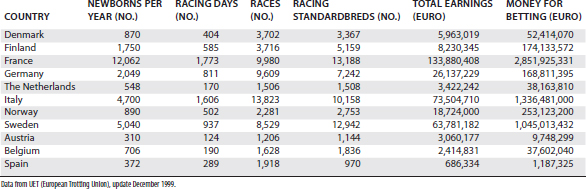
TABLE 109-1 Distribution of Standardbreds Born in Different European Countries, Summary of the Racing Activity, Earnings, and Betting
Europe has a large number of racetracks for STBs, and they are characterized by different circuit lengths, surfaces, and designs. Half-mile tracks have been replaced progressively by 1-km ( -mile) tracks, and no 1-mile racetracks (with the exception of training centers) are present in Europe. The most characteristic and popular racetrack is the Plateau de Gravelle in Vincennes, Paris, where the Prix d’Amerique is held. The track surface is made of pressed charcoal powder; slopes and descents are present; and the circuit is egg-shaped, which is unique in Europe, where other racetracks have a regular design. Another famous French racetrack, Cagnes-sur-Mer in Nice, is well known for being 1200 m in length and for hosting the Criterium de Vitesse, one of the main European free-for-all races. In Sweden, Solvalla racetrack in Stockholm represents the heart of the Swedish STB racing, and in late May the multiple-heat race Elitlopp is held. In Norway, in addition to well-developed STB racing (the main racetrack being Bjerke near Oslo), races for Warmblood horses (a breed historically devoted to hard work but now genetically selected for speed) are still popular and meet the special interest of the local public.
-mile) tracks, and no 1-mile racetracks (with the exception of training centers) are present in Europe. The most characteristic and popular racetrack is the Plateau de Gravelle in Vincennes, Paris, where the Prix d’Amerique is held. The track surface is made of pressed charcoal powder; slopes and descents are present; and the circuit is egg-shaped, which is unique in Europe, where other racetracks have a regular design. Another famous French racetrack, Cagnes-sur-Mer in Nice, is well known for being 1200 m in length and for hosting the Criterium de Vitesse, one of the main European free-for-all races. In Sweden, Solvalla racetrack in Stockholm represents the heart of the Swedish STB racing, and in late May the multiple-heat race Elitlopp is held. In Norway, in addition to well-developed STB racing (the main racetrack being Bjerke near Oslo), races for Warmblood horses (a breed historically devoted to hard work but now genetically selected for speed) are still popular and meet the special interest of the local public.
A variety of track designs and purposes are present in Europe. For example, a large number of small country tracks are found in France, and local races are organized in a fairlike fashion, whereas the main racing activity is concentrated in Paris. In Italy, however, important races have a more even distribution among racetracks, Milan and Rome being the main places. In Table 109-2 the distribution of racing tracks in the main European countries is summarized.
Differences exist in availability of prize money among different countries, and this makes France and Italy the most attractive countries for trainers and owners. A number of well-known trainers started to move in the early 1980s toward France and Italy, especially from northern Europe, and this has enhanced the exchange of experiences between trainers and veterinarians.
Prize money distribution among horses of different ages has strongly influenced racing, especially in Italy, where 2- and 3-year-olds have the richest races. Higher purses for younger horses have also affected breeding programs and have stimulated an interest in many of the orthopedic problems affecting young horses, especially osteochondrosis, which has been studied widely in northern Europe.
Approaching Lameness Problems
Only STB trotters are allowed to race in Europe, and this makes the trainer’s work more challenging. Any possibility to switch gaits or to move an unnaturally fast gaited trotter to a potentially good pacer is precluded. When the fast gait is compromised by biomechanical problems and substantial interference between limbs (unlike in the pacer), corrections aimed at avoiding interference are attempted. Finding a solution for mechanical problems is not always possible, and corrective shoeing that alters the natural gait may cause compensatory lameness in different locations.
A series of mechanical limitations may be present at the beginning of training, and relatively soon they are followed by pain-related problems, usually affecting joints and less frequently digital flexor tendons and the suspensory ligament (SL). A less than 100% natural trotting athlete is more likely than a natural trotter to have its gait totally compromised, even by a mild subclinical lameness problem, and consequently gait limitations increase. However, anything that is attempted by the trainer to improve gait (corrective shoeing, special equipment that prevents turning the head and neck toward one side, or shifting the hindlimbs toward one shaft) forces the horse to a nonnatural fast gait and often results in lameness. In fact, when a nonnatural gait is forced, the end result is usually that a single limb (or a biped) is overloaded, and the uneven loading is exacerbated by the progression of training.
When young horses start training, they frequently have been subjected to basic lameness and radiological evaluations. This allows trainers the opportunity to treat conditions such as osteochondrosis or to be aware of other abnormalities. Prepurchase radiographic examinations and, when needed, preventative arthroscopic surgery (mostly for osteochondrosis of the tarsocrural joint and osteochondral fragments in the fetlock joints) are now practices that have received general acceptance. The reason to operate early is to have the horse rested before any training program is started. In yearlings eligible for autumn sales, it is important to perform surgery early to have presale radiographs without evidence of osteochondral fragments and to decrease effusion before the sale.
When moderate gait anomalies are present, experienced trainers usually give the horse time and keep going with a light exercise program instead of making radical changes. This allows, in many horses, a complete maturation of the equine athlete, and when the growth is complete and the muscular function well conditioned, the gait in many horses automatically improves without injuring the immature skeleton. Shoeing is also central in early training. Light plastic shoes are ideal to allow foot growth and expansion and to minimize trauma in the early phases of fast training.
Lameness Examination
Horses with acute, severe lameness should be allowed to rest. Radiographs are frequently diagnostic, revealing the most common severe musculoskeletal injuries affecting trained STBs, such as incomplete sagittal fractures of the proximal phalanx, fractures of the proximal sesamoid bones (PSBs), splint bone fractures, fractures of the third or radial carpal bones, fractures of a palmar process of the distal phalanx, fractures of the lateral condyle of the third metacarpal bone (McIII), slab fractures of the third tarsal bone, and stress fractures of the palmar aspect of the McIII or the plantar aspect of the third metatarsal bone (MtIII). Apical fractures of the PSBs are a common injury in young STBs, and the lateral PSB in the hindlimbs is the most common location.1
The conditions mentioned previously represent injuries of the racing STB requiring rest or surgical repair. More commonly the veterinarian is consulted for mild or obscure lameness, gait disturbances, or poor performance. In any case, a thorough history is mandatory before the lameness examination is initiated.
A basic lameness history must include the following:
Concerning conformation, the clinician should check the following:
Palpation
Many clinicians spend little time palpating a lame horse, a practice that I believe is a mistake. Areas of warmth (heat), especially in the hoof wall, must be detected, and regions of special interest include the fetlock joints, the metacarpal and metatarsal regions, carpus, hock, stifle, and back.
In the forelimb, the DIP joint capsule just above the coronary band is palpated to detect effusion. The character of the digital pulse is evaluated and compared between limbs.
Hoof tester examination can be considered part of palpation. When possible, feet are first tested without removing the shoes, and ideally the horse should be kept shod until any examination in movement is completed. When diagnostic analgesia is needed, hoof testing must precede palmar digital analgesia, and shoes may be removed temporarily if bar shoes or pads prevent accurate testing. These six points are tested in each horse: lateral and medial quarters, lateral and medial middle sole, and lateral and medial toe. Testing the frog rarely produces useful information, and squeezing the quarters from lateral to medial with hoof testers may cause pain unrelated to the primary lameness.2 Pain arising from the quarters, especially mild pain medially, should not be overrated because this region is frequently sensitive to hoof testers in normal horses. The contralateral foot may serve as a reference. In my experience the right medial quarter is the most common region to find pain elicited by hoof tester examination in STBs, and this is probably secondary to the counterclockwise direction of racing. This may be a clinically significant finding, but generally a painful response is considered more important when it arises from the toe or from the lateral side of the sole. When shoes are removed, a further evaluation of the lateral-to-medial balance is performed. The sole itself is observed, and when it appears flat and painful, this may correlate with type of shoes and padding that are used. Overzealous padding may add to, rather than relieve, pressure on the sole. A leather or rubber layer may allow sand to pack quickly under the pad and create pressure and secondary bruises. These horses are better managed with shoes in which the contact is limited to the hoof wall and no contact is made with the sole.
In the forelimb the fetlock joint is examined for effusion, alteration of the dorsal outline, and enlargement of the suspensory branches. The latter are palpated carefully with the joint flexed. Each branch is pressed gently axially, and alterations in consistency and pain response are noted. Range of motion of the fetlock joint is assessed. In a normal STB, the fetlock joint can be flexed up to 90 degrees (angle between the McIII and the proximal phalanx) without eliciting a painful response. With one hand holding the dorsal pastern region, the dorsal aspect of the fetlock joint can be palpated further by using the other hand to compress the dorsal joint capsule against the bony prominences of the sagittal ridge and condyles of the McIII. Horses with osteochondritis dissecans (OCD) or a hypertrophic synovial pad exhibit a painful response. The bony profile of the McIII must be followed with fingers to detect painful areas in the dorsal, lateral, and medial aspects. Palmar soft tissues are evaluated with the limb in a weight-bearing position and while being held off the ground. Each structure is palpated accurately to detect heat, pain, and edema in horses with acute lesions or fibrotic consistency and adhesions in those with chronic conditions. Fingers must be pressed firmly, deep in the proximal palmar metacarpal region, where pain originating from the proximal aspect of the SL is hard to detect. The carpus is better evaluated by holding the limb in a moderate degree of flexion. Careful digital palpation along the dorsal aspect should be performed. Of particular importance is the dorsomedial aspect where a thickened joint capsule and painful response correspond to the common finding of OA of the middle carpal joint. Palpation of the forelimb proximal to the carpus is rarely helpful. Elbow and shoulder lameness are rare, and bicipital bursitis has seldom been reported.
In the distal aspect of the hindlimb, palpation is similar to that described for the forelimb with the exception that foot lameness is less important. The metatarsophalangeal joint region is best evaluated while holding the limb in a semiflexed position. When the proximal metatarsal and distal tarsus regions are palpated, some false-positive painful reactions frequently are elicited, especially on the medial aspect. This pain frequently is overemphasized in horses with back pain, especially when the trainer thinks the horse has primary lameness in the tarsus. Effusion of the tarsocrural joint often indicates the likely presence of osteochondrosis (OC). The stifle must be palpated deeply and carefully because the joint is complex, but the structures that can be assessed are limited. The femorotibial joints seldom appear distended, but effusion of the medial femorotibial joint is an important abnormal clinical sign. More frequently, joint effusion is limited to the femoropatellar joint, but because the femoropatellar and medial femorotibial joints communicate, inflammation in one may result in effusion of both. With the exception of acute trauma, painful responses to palpation are rare in this area, even from the patellar ligaments that are identified easily. On the medial side, scar tissue and irregularities or enlargement of the medial patellar ligament may suggest previous desmotomy. When associated with femoropatellar effusion, the latter sign may suggest apical patellar fragmentation, and radiographic examination is indicated. The stifle can be flexed only in unison with most other hindlimb joints, so a painful response is not specific. With moderate flexion the medial collateral ligament can be stressed by the veterinarian pulling the tibia in a lateral direction with both hands and pressing the shoulder against the femur.
Palpation of the back is aimed at evaluating pain arising from joints (intervertebral, lumbosacral, sacroiliac, and sacrococcygeal), nerve roots, and muscles. The latter are the most likely origin of pain elicited by palpation, but other problems must be ruled out if associated clinical signs (atrophy, asymmetry) are present. Pain in the gluteal area may be secondary to many problems, including straight hindlimb conformation, hock or stifle pain, sore feet, gait imbalance, and stiff corrective harness equipment. Therefore pain in this area should not be treated as a primary problem unless a thorough clinical examination has ruled out other sources of pain.
Movement
After palpation, the horse is examined during movement. I commonly tranquilize each horse I examine for lameness. Tranquilization (10 mg of acetylpromazine maleate intravenously) improves the possibilities of handling the horse and lowers the risk of injuries to the veterinarian. Furthermore, the horse appears less stiff; mild lameness becomes somewhat more obvious; and the horse stands better for radiographic or ultrasonographic examination. The trainer must be consulted before injecting a tranquilizer because this practice may preclude racing because of doping regulations (the term used in Europe for a blood or urine drug test for a prohibited substance). Lameness is rarely detectable at the walk, but it is important to observe the way the horse lands with each foot to identify lateral-to-medial hoof imbalance. The horse is then trotted in a straight line on a firm surface, and the character of movements is observed. Abduction or circumduction of forelimbs is considered characteristic of carpal lameness because the horse appears to attempt to avoid flexion. In the hindlimb, stiffness has been related anecdotally to distal hock joint pain but in fact is not a specific sign. In horses with pain arising from the distal part of a hindlimb (frequently the metatarsophalangeal joint), the horse tends to moderately overflex the hock and stifle to shorten the weight-bearing phase of the stride.3 In horses with more severe lameness, drifting forward of the sound limb is observed, and a drop of the fetlock joint is easily seen. Abduction of the hindlimb is thought to be related to stifle lameness.
Flexion tests are used to supplement findings during movement and are similar to those used in other sports horses. Flexion of the carpus is accomplished by pulling the metacarpal region laterally, and the clinician’s elbow may act as a lever against the horse’s radius to stress the medial aspect. In young horses affected by carpitis, this maneuver frequently elicits pain.
Diagnostic Analgesia
Diagnostic analgesia can be performed in sequence from distal to proximal, or, to save time, selective analgesic techniques can be used. For example, European trotters with a positive response to forelimb lower limb flexion inconsistently respond to palmar digital analgesia; therefore analgesia of the metacarpophalangeal or DIP joints may be the first option. Perineural analgesia is preferred, however, to avoid minor risks of joint infections or to save the opportunity to provide intraarticular therapy immediately (when working in stables, trainers frequently are interested more in treatment than in diagnosis). I frequently start with low plantar analgesia in the hindlimbs because lameness of the digit is rare. In young STBs with forelimb lameness and a positive response to carpal flexion, I block the middle carpal joint first.
In horses with obscure lameness or when lameness is only apparent during fast exercise, examining the horse on the track may be useful. The horse is rigged in full harness and first examined trotting in a clockwise direction. Speed then is increased, and the horse is turned to train in a counterclockwise direction, the same as racing. Clinicians can drive the horse themselves, sit in a two-seat wagon, or observe the horse from a car or from a distance. In my opinion, watching the horse during exercise is important, especially when routine training and racing can be simulated, and I prefer the horse to be driven by its usual trainer. Having the horse fully equipped, mimicking the stress of racing, and observing the horse in turns are important advantages to this form of lameness examination.
Diagnostic analgesia is useful, but the clinician must be aware of related risks and make the trainer and owner aware as well. Diagnostic blocks should be avoided in horses suspected of having incomplete fractures. Radiographic examination should precede diagnostic analgesia in these horses. When examining a horse on the track after local analgesia, the trainer should be told to limit the speed as much as possible, avoiding any sudden stop or sharp turn. An experienced trainer normally is able to appreciate the benefits of a block quickly and without stressing the horse. Examination at speed is needed to make a diagnosis in horses with plantar process osteochondrosis fragmentation of the proximal phalanx and fragmentation of the distal border of the distal phalanx.
Diagnostic Imaging
Sophisticated equipment for diagnostic imaging is now available in most European equine clinics. Scintigraphy is available in Europe but is limited to large referral hospitals. Radiography remains the mainstay of equine diagnostic imaging, and the availability of excellent portable units has improved the radiographic examination under field conditions. Digital radiography offers advantages in terms of imaging processing, time saving, radiation protection, and easier image storage. Ultrasonographic examination is commonly performed.
Common pathological findings in the distal limb of European trotters include osteophyte formation on the distal aspect of the middle phalanx, sometimes associated with modeling of the extensor process of the distal phalanx, as seen on a lateromedial image of the foot (Figure 109-1). This radiological pattern often is associated with heel growth proceeding faster than toe growth (club foot). When associated with a positive lower limb flexion test and lameness abolished using analgesia of the DIP joint, this radiological finding is important and indicates the presence of OA. Fragmentation of the extensor process of the distal phalanx has controversial clinical significance, but in my experience these fragments cause synovitis of the DIP joint and should be removed using arthroscopy.

Fig. 109-1 Lateromedial radiographic image of the distal interphalangeal joint of a Standardbred trotter. Osteophyte formation on the distal border of the middle phalanx associated with moderate remodeling of the extensor process of the distal phalanx (arrows) is a common pathological finding in European trotters.
The dorsoproximal-palmarodistal oblique radiographic image of the distal phalanx, unlike scintigraphy, rarely helps in diagnosing pain arising from stress remodeling of the distal phalanx; thus the diagnosis of pedal osteitis is limited to horses with chronic lameness characterized by substantial radiolucency.4 Fragmentation of the lateral and medial palmar processes of the distal phalanx, although controversial as a cause of acute lameness, may be an important source of pain best managed by shoeing.
The flexed lateromedial image of the metacarpophalangeal or metatarsophalangeal joints is useful in evaluating lesions of the distal aspect of the McIII or the MtIII. In the hindlimb, the oblique images must be acquired in a proximal to distal direction (down-angled) to see better the area between the proximal phalanx and the base of the PSBs. Fragmentation of the proximal plantar aspect of the proximal phalanx represents a major cause of subtle hindlimb lameness (Figure 109-2).

Fig. 109-2 Dorsoproximal 45-degrees medial-plantarodistolateral oblique radiographic image of a hind fetlock of a 2-year-old Standardbred. There is plantar fragmentation (arrow) of the proximal medial aspect of the proximal phalanx.
A dorsopalmar image of the carpus helps to evaluate the proximal suspensory origin from the McIII, and focal or diffuse increased radiopacity of the McIII may be found (Figure 109-3). In yearlings and young horses, this image allows examination of the distal radius, and pathological modifications of the growth plate on the medial side (physitis) are a frequent cause of early lameness. The most common lesions of the carpus are seen with the dorsolateral-palmaromedial oblique image and the dorsal 35° proximal-dorsal distal oblique (skyline) image of the flexed carpus to highlight the distal row of carpal bones. The radiographs must be of excellent quality, and the appropriate projection must be obtained because false-negative radiographic images are frequent. Abnormal findings include areas of radiolucency in the dorsoproximal articular border of the radial fossa of the third carpal bone, radiolucent lines suggestive of fractures, and increased radiopacity of the third carpal bone.5 A moderate degree of increased radiopacity in the radial fossa of the third carpal bone is considered normal in racing horses, but more severe increased radiopacity associated with radiolucent areas represents a pathological finding.6,7

Fig. 109-3 Dorsopalmar radiographic image of the proximal metacarpal region of a Standardbred trotter (lateral is to the left). Increased radiopacity of the palmar cortex of the proximal aspect of the third metacarpal bone (arrows) is a common finding in trotters with chronic proximal suspensory desmitis.
In the hindlimb the centrodistal and tarsometatarsal joints frequently appear normal radiologically even when distal hock joint pain is diagnosed clinically as the source of pain. Scintigraphy is an excellent tool for diagnosing OA of these joints.8 The tarsocrural joint is a predilection site for OC in STBs, and the presence of fragments associated with effusion may represent an indication for arthroscopic surgery. Lesions affecting the lateral trochlear ridge of the talus and medial malleolus of the tibia more frequently cause lameness and effusion than do those of the cranial aspect of the intermediate ridge of the tibia. In horses with effusion but without obvious fragmentation, a specific dorsal 10° to 15° lateral-plantaromedial oblique image is required to evaluate the axial aspect of the medial malleolus. Subtle osteochondral fragmentation or radiolucency easily can be overlooked (Figure 109-4).
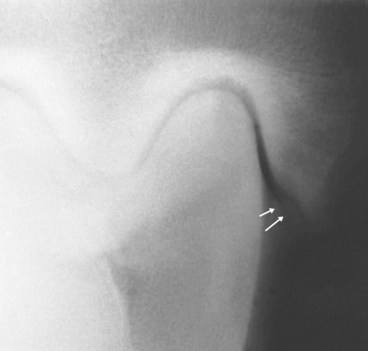
Fig. 109-4 Dorsal 15° lateral-plantaromedial oblique radiographic image of the hock of a 2-year-old Standardbred colt. There is axial fragmentation of the medial malleolus of the tibia (arrows), which is difficult to detect unless oblique images are obtained. The condition can cause effusion of the tarsocrural joint and lameness.
Curb is not seen frequently but can develop in the early stages of training in young horses. Curbs represent thickening of the plantar aspect of the hock and must be differentiated from the soft swelling caused by distention of a tarsal sheath. Abnormal stress to the plantar soft tissue structures can be predisposed by sickle-hocked or cow-hocked conformation. Accurate palpation differentiates curb from tarsal tenosynovitis. Ultrasonographic evaluation helps characterize the soft tissue structures involved in curb and assess severity (see Chapter 78). In the European STB, curb nearly invariably represents inflammation and thickening of the long plantar ligament, but ultrasonographic evaluation is necessary to differentiate long plantar desmitis from other soft tissue injury.
Trainers frequently ask for radiography or ultrasonography of the stifle because they seem to incriminate this joint as the source of pain causing lameness in horses with obscure hindlimb lameness. Radiography of the stifle is important in foals and yearlings with femoropatellar effusion. Lateromedial and caudocranial images must be obtained. OCD of the lateral trochlear ridge and, less frequently, subchondral bone cysts of the medial femoral condyle can cause effusion and lameness in young STBs. Ultrasonographic evaluation of the stifle is useful in detecting soft tissue injuries, but these lesions are rare in STBs. Mild dimples or cartilaginous defects on the articular surface of the medial femoral condyle can be detected using ultrasonographic examination by holding the stifle in a semiflexed (90 degrees) position.
Final Diagnosis, Prognosis, and Treatment Options
A final diagnosis is made easily when the horse has obvious severe lameness, as is the case in horses with the more common fractures and tendon or ligament injuries (incomplete sagittal fracture of the proximal phalanx, PSB fracture, carpal chip or slab fractures, SDF tendonitis, and acute suspensory desmitis). Surgery or rest most often is recommended for these horses. In some horses, rest is the best option, and accurate monitoring of the healing process must follow (fracture of the distal phalanx, stress fractures of the proximal aspect of the McIII, and proximal suspensory desmitis [PSD]).
OA of the DIP joint, the metacarpophalangeal or metatarsophalangeal joints, or the middle carpal joint (particularly in young horses) can cause chronic lameness. Racetrack clinicians frequently inject the tarsometatarsal (TMT), centrodistal, and tarsocrural joints, but the true prevalence of problems arising from these joints has not been substantiated using diagnostic analgesia. Problems affecting the proximal aspect of the hindlimb, in the absence of visible lameness, frequently are diagnosed, but definitive diagnosis is difficult to substantiate.
Intraarticular therapy includes corticosteroids or nonsteroidal antiinflammatory drugs (NSAIDs) and, more recently, interleukin-1 receptor antagonist protein (IRAP). A series of four intraarticular injections of polysulfated glycosaminoglycans (PSGAGs), 250 mg every fourth day and then at weekly intervals, is helpful to treat juvenile OA, especially in the carpus. PSGAGs also have been useful parenterally (500 mg every 4 days for seven treatments).9 High-molecular-weight hyaluronan (20 to 40 mg) may be used alone or with corticosteroids. Hyaluronan (20 to 40 mg) may be used intravenously.10 The most popular corticosteroids for intraarticular therapy in horses include methylprednisolone acetate (40 to 60 mg), betamethasone disodium phosphate or betamethasone acetate (3 to 9 mg), and triamcinolone acetonide (6 mg). A basic treatment includes three intraarticular injections using 60 mg of methylprednisolone acetate for the first injection, followed by two injections of 40 mg at 2-week intervals. A similar protocol may be applied to betamethasone disodium phosphate and betamethasone acetate (6 to 9 mg the first time followed by two injections of 6 mg each). This treatment is usually helpful in horses with chronic OA of the DIP joint, the metacarpophalangeal or metatarsophalangeal joints, and the distal tarsal joints and sometimes resolves acute synovitis in young horses. When using triamcinolone acetonide (6 mg), clinicians must be aware of systemic effects and problems (laminitis and rhabdomyolysis) if several joints are injected at the same time. Although the cause is unsubstantiated, these complications may develop because of iatrogenic hyperadrenocorticism. Corticosteroids must be used in compliance with doping regulations.
Liniments, paints, and blisters are still popular, and despite lack of scientific support, they appear strongly tested by time. Iodide-based light paints diluted in dimethyl sulfoxide may be helpful in improving circulation to the distal aspect of the limbs and help to remove edema. Stronger blisters (with iodide mercury, cantharis, cedar oil, or turpentine) may play a role in improving circulation in some areas, but trainers must be made aware of possible secondary effects of the chemical-induced inflammation (scars, adhesions, cellulitis, and excessive joint inflammation) and that using most irritant blisters is no longer justified. Thermocautery (pin firing) is now less popular in Europe but is still used to treat STBs with curbs and proximal splint exostoses. Paints and blisters are used more frequently in France and Italy than in northern Europe.
Corrective Shoeing
Corrective shoeing is important for many STBs with forelimb lameness conditions. Generally speaking, a good lateral-to-medial balance and an ideal dorsal hoof wall angle must be provided before any shoe is applied. Then a large-based (wide-web) shoe is ideal but not always possible because of gait characteristics. Many trainers prefer thinner and lighter shoes because they are associated with increased speed. In horses with a flat sole the shoe must be in contact only with the wall border, and any rubber, leather, or silicon pad must be avoided. In these horses a rigid (aluminum) sole may prove helpful, but frequent cleaning is required to avoid sand accumulation under the sole. In horses with OA of the metacarpophalangeal or metatarsophalangeal joints, bar shoes must be avoided because the bar prevents the natural slipping of the foot when landing and increases stress on these joints. A bar shoe may prove helpful in horses with SDF tendonitis, but I prefer to leave this shoe on only during the recovery phase and during light training, whereas an open shoe is preferred for fast training and racing.
Training Programs
Alternative training programs can be a valuable adjunct therapy, especially when dealing with unnatural fast-gaited trotters. Clockwise jogging and training, training on straight tracks (using interval training schedules), and swimming are preferred. Training programs aimed at reducing speed and stress on the large upper limb muscles, such as fast trotting in a circle in deep sand and use of heavy wagons or wagons with preselected brake sets (power carts), have been used, but scientific studies and objective data to support use of these alternatives are lacking.
Proceeding without A Diagnosis
Progress in diagnostic imaging has made the situation rare in which a clinician cannot determine a diagnosis. When available, whole body scintigraphic examination in horses with occult lameness is useful. Results of scintigraphy must not be overinterpreted, and clinicians must be aware that conditions may be subtle or difficult to detect. Bone remodeling around OCD or osseous cystlike lesions may be subtle. When detailed clinical examination has failed to reveal a diagnosis, I suggest the following options:
Lameness in the European Trotter
Hoof Pain
This nonspecific definition refers to a number of conditions, including what most clinicians and trainers call foot pain. Lameness varies, and the response to flexion may be equivocal. Negative flexion tests in a lame horse may suggest nonarticular hoof pain, and the same applies to horses in which the trainer’s complaint is pain (with compromised gait) at the end of the race. Horses may break stride on the last turn or may get on a line in the straightaway.
A thorough examination of the feet, including hoof tester examination, is performed as previously described. A series of selective diagnostic analgesic procedures follows. Palmar digital analgesia commonly improves lameness by 75% to 90%. If a less than 50% response is obtained, palmar blocks at the base of the PSBs are performed. I avoid analgesia of the DIP joint because I may choose to medicate the joint. Recent evidence suggests analgesia of the DIP joint is not specific, and pain originating from the sole may be abolished.11
Diagnostic imaging includes radiography and scintigraphy. Stress remodeling of the distal phalanx is a common finding in trained STBs. Radiographs are usually negative, although occasionally marginal changes of the distal phalanx are seen.
Management includes corrective shoeing, controlled exercise, DIP joint injections, and local application of iodide ointments or blisters. Temporary pain relief has been reported anecdotally after perineural injection of cobratoxin, alcohol, or other preparations and after percutaneous cryotherapy. There can be complications such as substantial local inflammation and abscess formation with perineural injections. Horses with mild lameness respond to corrective shoeing: rubber or leather soles may be added to wide-web shoes, or different types of rubber flaps may be used temporarily. Light training for 2 to 3 weeks is suggested, and the horse is best trained on a soft track or on a straight track if available. Swimming is a good alternative method of training.
Osteoarthritis of the Distal Interphalangeal Joint
History, character of the lameness, response to flexion tests, and shape of the hoof are points to consider when OA of the DIP joint is suspected. Horses can be lame or reported to be intermittently lame. The tendency is for horses to develop OA of the DIP joint and club foot because the hoof growth in the heel region is faster than in the toe region. Evaluation and trimming of the hoof wall to lower the dorsal angle may help prevent this conformational change. Palpation of the area over the coronary band may elicit pain, especially medially where the condition must be distinguished from chronic collateral ligament strain of the DIP joint. Mild pain also may be detected by palpation of the proximal aspect of the SL in the forelimb and muscles of the back, two common compensatory lameness conditions. Diagnosis can be frustrating because horses are not always improved with DIP analgesia (this may suggest pain originating in the subchondral bone), and the gait may be abnormal because of other problems frequently secondary to pain originating from the DIP joint. An 80% to 90% positive response to perineural analgesia must be considered clinically relevant.
Lateromedial radiographs of the distal aspect of the limb frequently show a prominent osteophyte on the distal aspect of the middle phalanx, sometimes associated with secondary remodeling of the proximal aspect of the distal phalanx (see Figure 109-1). Fragmentation of the extensor process of the distal phalanx may also be observed, in which case the hoof wall frequently has a grossly triangular shape. OA of the DIP joint may be bilateral but is most commonly unilateral.
Suggested therapy includes intraarticular therapy with corticosteroids, PSGAGs, high-molecular-weight hyaluronan, or a combination of these drugs three times at 7-day intervals (14 days when using corticosteroids); IRAP therapy represents a new promising alternative. Corrective trimming to decrease excessive heel growth and maintaining the hoof angle at about 50 degrees appear important. Wide-web shoes distribute load on a large surface area, and when possible, a rubber or leather pad is needed. The shoe should have a rolled toe to ease breakover. A thick rubber pad (flap or flip-flop) is used sometimes to replace the classic shoe (Figure 109-5).
Osteoarthritis of the Metacarpophalangeal Joint
OA of the metacarpophalangeal joint may be acute or chronic. Acute synovitis is seen in young horses when training is intensified or when the track surface changes. Clinical signs include mild to moderate lameness, pain on palpation, and lameness after flexion. Radiographs are usually negative in young horses, but flattening or more severe changes of the sagittal ridge of the McIII in older horses with chronic OA often are seen. Contrast radiology reveals a filling defect corresponding to a hypertrophic synovial pad of the distal, dorsal aspect of the McIII. Ultrasonographic examination reveals various degrees of dorsal joint capsule thickening and increase in echogenicity of the synovial pad. Intraarticular analgesia abolishes the lameness in most horses.
In horses with acute synovitis, training program modulation (2 to 3 weeks of light jogging), corrective shoeing (wide-based shoes and pads), and intraarticular corticosteroids (a series of three injections at 2-week intervals) may resolve the problem. In these horses, concurrent pathological conditions of the articular cartilage, subchondral bone, and the synovial pad usually are lacking or mild. Horses with hypertrophic synovial pads benefit from arthroscopic surgery to remove the thickened tissues because response to medical management is poor. This is frequently the case in older horses, in which advanced OA is often present. Prognosis after surgery is only fair to guarded, however.
Middle Carpal Joint
The middle carpal joint is the most common site of lameness in young STBs. Typically, affected horses tend to trot with a wide gait, abducting the affected limb or limbs in an attempt to minimize carpal flexion.12 Visual inspection from a dorsolateral perspective reveals abnormal contour of the dorsomedial aspect of the carpus. Palpation often elicits a painful response over the dorsal aspect of the radial and third carpal bones. Usually the response to carpal flexion is positive, and intraarticular analgesia abolishes lameness in most horses. A negative result from intraarticular analgesia does not rule out the middle carpal joint as the source of pain causing lameness because subchondral bone damage under a relatively normal cartilage layer may cause pain that may not be desensitized completely. Radiographs are usually diagnostic, especially the skyline image of the distal row of carpal bones. Abnormal radiological findings range from complete slab fracture of the third carpal bone to more subtle signs of radiolucency of the radial fossa of the third carpal bone. Scintigraphy is a sensitive and excellent tool in the early diagnosis of middle carpal joint injury.8
Training program modulation and intraarticular injections of PSGAGs, hyaluronan, or small amounts of corticosteroids are the first steps in the treatment program. Arthroscopy is suggested when evidence of more severe bone damage exists. Chip fractures in STBs most frequently involve the third and radial carpal bones. Counterclockwise racing, especially in the turns, concentrates forces along the medial aspect of the right forelimb, and this makes the right middle carpal joint more predisposed to injuries.13-15 The proximal border of the third carpal bone is involved more frequently than the distal border of the radial carpal bone in the STB trotter, unlike in the Thoroughbred (TB) and in the pacer.13,15,16 Arthroscopic surgery and rest generally yield a fair to good prognosis.15 STBs with incomplete slab fractures of the third carpal bone may heal with rest, possibly preceded by diagnostic arthroscopy and curettage of the lesion. Horses with complete slab fractures are best treated by internal fixation. Thin fragments are removed. When arthroscopy shows substantial loss of articular cartilage, the micropick technique may increase the possibilities of cartilage repair.17 Arthroscopic findings in young STBs have been shown to correlate poorly with radiological findings, and lesions appear frequently more severe than expected.16 In horses without radiological changes, I frequently find depressions and discoloration of articular cartilage (especially in the radial fossa of the third carpal bone), loss of articular cartilage in focal areas of the third and radial carpal bones, and partial or complete tearing of the medial palmar intercarpal ligament. Ligament injuries, especially affecting the medial palmar intercarpal ligament, must be suspected in the absence of radiological abnormalities.18 However, medial palmar intercarpal ligament injuries are rare. These horses are treated using arthroscopic trimming and are given 4 to 6 weeks of stall rest followed by 4 weeks of stall rest with handwalking exercise, and joints are injected with short-acting corticosteroids.
Proximal Palmar Metacarpal Pain Including Proximal Suspensory Desmitis
Proximal palmar metacarpal pain affects many more horses than we once thought. Mild pain in the proximal palmar aspect of the metacarpal region may be secondary to other gait disturbances and may reflect attempts to maintain balance when trotting fast. In these horses the lesion rarely is substantiated by ultrasonography, but pain may be detected with accurate palpation (racetrack clinicians used to diagnose and treat “blind splints” in this area).
PSD is usually acute in onset, and direct palpation of the SL elicits pain. A carpal flexion test is often positive. Intraarticular analgesia of the middle carpal joint produces a variable amount of improvement, but some degree of lameness still is elicited by flexion. Subcarpal analgesia (4 mg of local anesthetic solution placed axial to each of the second and fourth metacarpal bones or direct infiltration of 2% mepivacaine over the proximal aspect of the SL) usually abolishes lameness.
Diagnostic imaging includes radiography, scintigraphy, and ultrasonography. Scintigraphy is useful in identifying horses with bony injury, including horses with an avulsion fracture of the McIII at the origin of the SL, those with enthesopathy, or those with a longitudinal fracture of the McIII. Horses with PSD without bony involvement may have positive pool phase images, but delayed images are usually negative. Radiography (dorsopalmar and flexed lateromedial images) may reveal associated longitudinal or avulsion fractures of the proximal, palmar aspect of the McIII or, in horses with chronic lameness, increased radiopacity of the McIII at the SL origin (see Figure 109-3). Ultrasonography is useful in identifying patterns of ligamentous injury, palmar cortical bone damage, and monitoring the healing process.
The prognosis is fair to good, provided the affected horse is subjected to walking exercise and controlled training with concurrent monitoring of the healing process. STBs may tolerate an acceptable level of training with chronic injuries of the SL compared with TBs, possibly because of the increased percentage of muscle fibers present in the SL.19 The prognosis in horses with PSD is better than those affected with lesions in the suspensory body.
Therapy includes 6 to 8 weeks of rest followed by 4 to 6 weeks of 20 to 60 minutes of walking exercise or swimming. Local application of blisters and injections of corticosteroids or PSGAGs may help but rarely shorten the healing period. Cryotherapy has gained some popularity in treating STBs with PSD in racetrack practice, but its usefulness has not been substantiated scientifically. Several biological therapies have gained recent acceptance: intralesional injection of bone marrow,20 isolated or cultured stem cells, and platelet-rich plasma (PRP). However, more research and clinical work are required to substantiate their value. Shock wave therapy also has been used to treat horses with PSD in recent years (see Chapter 96).
Sesamoiditis
Sesamoiditis may be defined as enthesopathy at the insertion of the branches of the SL to the abaxial surface of the PSBs. The condition also may affect the base of PSBs, but this form is rare and is best defined as distal sesamoidean desmitis. Two types of sesamoiditis are recognized. Type 1, or juvenile sesamoiditis, is characterized by radiolucent lines (vascular channels) in the proximal third of a PSB, radially oriented as seen in lateromedial or oblique radiographic images, and is a frequent feature in young (2- and 3-year-old) STBs (Figure 109-6). This radiological pattern is not always associated with lameness, and no link has been observed between the presence of these lines and PSB fractures.21 Affected horses tend to be lame after training, but pain subsides with rest. Intraarticular analgesia does not abolish lameness. Lameness disappears after perineural analgesia of the medial and lateral plantar (palmar) nerves. The condition usually involves one or both hindlimbs, and the lateral PSB is affected more frequently. Scintigraphic examination reveals increased radiopharmaceutical uptake (IRU), but radiological changes are seen in only 50% of STBs with scintigraphic abnormalities.8 The lateral PSB represents one of the most frequent locations for IRU in racing STBs.8,22

Fig. 109-6 Dorsolateral-plantaromedial oblique radiographic image of a metatarsophalangeal joint of a lame 2-year-old Standardbred colt with juvenile sesamoiditis. Note the radiolucent lines in the lateral proximal sesamoid bone.
Type 2 sesamoiditis is chronic, frequently affects a single PSB, and is found more commonly in the forelimbs of older horses. Radiological signs of type 2 sesamoiditis (evidence of radiolucent lines in the proximal half of the bone, irregular palmar/plantar and abaxial outline of the bone, enthesophytes, and mineralization of the adjacent intersesamoidean ligament) are associated with ultrasonographic evidence of suspensory insertion desmitis. One or both suspensory branches often are involved. Focal loss of echogenicity in horses with acute disease and increased echogenicity in horses with chronic lameness are common abnormal ultrasonographic findings. The insertion on the PSB (enthesis) becomes grossly irregular.
In horses with type 1 sesamoiditis, treatment involves rest, slow training, or turnout for 30 to 90 days, depending on the degree of lameness present. Radiological monitoring of the lesion is probably not helpful because lameness may improve substantially despite the persistence of radiolucent lines. More information is provided by scintigraphy initially and during follow-up examination. Medical treatment includes local application of paints or mild blisters and corrective shoeing (bars must be avoided; the quarters must be lowered moderately; and shoes must provide a wide base in the hindlimbs). Medical treatment is aimed at improving local blood flow, and isoxsuprine hydrochloride (0.6 to 1.2 mg/kg PO twice daily) and sodium acetylsalicylate (10 mg/kg PO twice daily) are recommended for 45 to 60 days. The efficacy of this therapy, however, is questionable. The prognosis is fair if lameness is not severe and if the horse tends to warm out of lameness. If severe lameness is observed and associated radiological changes are pronounced, the prognosis is guarded. These horses are best given long periods of rest and paddock turnout (6 to 8 months). Treatment of horses with type 2 sesamoiditis includes rest, corrective shoeing (wide-web aluminum shoes, leather pad, with particular attention to lateral-to-medial hoof balance), local application of dimethyl sulfoxide, and paints and blisters. Pin firing is no longer justified. Cryotherapy has become popular in recent years, but in my opinion its clinical efficacy is poor. The prognosis is fair, but hoof balance must be monitored to prevent recurrence. Low-level or alternative (swimming) training is indicated.
Suspensory Branch Desmitis
Suspensory branch desmitis can be acute or chronic and is caused by lateral-to-medial hoof imbalance, exercise over uneven track surfaces, strains, and chronic fractures of the second and fourth metacarpal/metatarsal (splint) bones. Acute desmitis can be associated with metacarpophalangeal/metatarsophalangeal joint effusion. Shoeing changes, particularly when the hoof angle is modified (usually increased), frequently precede the condition, and when treating the condition, hoof imbalances must be identified and corrected. Ideally the dorsal hoof angle in the forelimb should be kept between 48 and 52 degrees, with a shoe providing good support to the heel. The routine training regimen, track conditions, and the counterclockwise direction of racing may affect the distribution of suspensory branch desmitis. In my experience the right forelimb and right hindlimb are most commonly affected, and lesions of the medial branch are twice as common as those of the lateral branch. Radiography and ultrasonography are performed to assess ligament damage and bone involvement. Enlargement and loss of definition of the margins of the branch, focal hypoechogenic areas, or diffuse loss of echogenicity and hyperechogenic foci in horses with chronic desmitis are the most frequent ultrasonographic findings.23 Radiologically the ipsilateral splint bone may appear deviated abaxially, and in horses with chronic lameness, adhesions may develop between the splint bone and suspensory branch, causing fracture during fast exercise. For the latter reason, radiological monitoring of the splint bones is suggested in horses with chronic desmitis. The insertion of the branch on the PSB must be assessed by ultrasonography for the presence of insertional desmitis.
The treatment in horses with acute desmitis includes rest, antiinflammatory drugs (phenylbutazone 2.2 mg/kg), or local application of dimethyl sulfoxide and poultices. Intraarticular injection of corticosteroids may be beneficial when the condition is associated with metacarpophalangeal/metatarsophalangeal joint effusion. In horses with chronic or severe desmitis, rest and local application of mild blisters may help. Fast training must be avoided when possible, and corrective shoeing must be provided. Alternative training programs, especially swimming physiotherapy, are indicated and can allow an acceptable level of exercise without worsening the lesion.
Metatarsophalangeal Joint
The metatarsophalangeal joint represents a major source of hindlimb lameness in STBs.24 Lameness of the metatarsophalangeal joint and specifically the plantar aspect is frequently subtle, and diagnosis can be challenging. Mal- or nonadaptive modeling of the plantar aspect of the metatarsophalangeal joint, proximal plantar fragmentation of the proximal phalanx, and nonunion of the lateral eminence of the proximal phalanx represent the most common conditions. Traumatic OC of the distal plantar aspect of the condyles of the MtIII and mineralization of the distal sesamoidean ligaments are observed rarely.
Subchondral nonadaptive remodeling of the MtIII has been described and represents a scintigraphic finding, with a corresponding radiological pattern not easily identifiable (Figure 109-7).22 Proximal plantar fragmentation of the proximal phalanx has been reported by several authors in radiological surveys of young STBs and is commonly seen (see Figure 109-2).25,26 Plantar fragments from the proximal phalanx rarely are associated with lameness at a trot in hand. Trainers’ complaints include gait disturbances during fast exercise, especially in turns, and the tendency for the horse to be on one shaft. Intraarticular analgesia of the metatarsophalangeal joint can alleviate lameness, but a fast exercise test is required, and owners must be aware of the potential consequences of this procedure. For this reason, when the clinical pattern indicates pain arising from the metatarsophalangeal joint, a radiographic examination including the oblique images (dorsoproximolateral-plantarodistomedial oblique and dorsoproximomedial-plantarodistolateral oblique) is required. In horses with plantar process OC fragments, arthroscopic surgical removal of fragments is indicated. The prognosis after surgical treatment is good. In horses with nonadaptive remodeling of the distal aspect of the MtIII, rest or reduced training, intraarticular injections of PSGAGs, or low doses of corticosteroids and hyaluronan are recommended.
Superficial Digital Flexor Tendonitis
The incidence and morbidity of STBs with SDF tendonitis are lower compared with TBs, but tendonitis of the superficial digital flexor tendon (SDFT) and suspensory desmitis represent the main indications for ultrasonographic examination of the distal aspect of the forelimbs in STB racehorses in Europe.
In my experience, most of the lesions are located in the middle and distal thirds of the SDFT. A core lesion located in the palmarolateral border of the tendon characterizes more than 30% of the lesions identified using ultrasonography. More rarely central core lesions are seen. Horses with chronic lesions have the typical pattern of diffuse tendonitis. Therapy includes rest; corrective shoeing; local application of antiinflammatory ointments, poultices, dimethyl sulfoxide, paints, or blisters; tendon splitting; desmotomy of the accessory ligament of the SDFT; and desmotomy of the palmar annular ligament. Intralesional injections of hyaluronan or PSGAGs have been reported. Promising results after bone marrow, cultured stem cell, and PRP therapy have been reported anecdotally. My treatment of choice in horses with acute lameness includes corrective shoeing (moderate lowering of the heels, correcting lateral-to-medial balance, and using wide-based shoes without pads, especially rubber pads), local application of dimethyl sulfoxide, cold water therapy twice a day, poultice application, and walking exercise for 2 to 4 weeks. The initial treatment is followed by the local application of an iodide blister, and the horse is given an additional 4 to 8 weeks of walking exercise. The horse usually is able then to resume jogging unless lameness is present. Ultrasonographic examination is performed 12 weeks later.
In horses with recurrent tendonitis, my treatment of choice includes desmotomy of the accessory ligament of the SDFT (superior check desmotomy). Desmotomy of the palmar annular ligament also is performed when substantial tendonitis involving the distal aspect of the tendon or digital flexor tendon sheath effusion is present. After surgery, horses are given 2 weeks of box stall rest, followed by 8 weeks of walking exercise.
Tendonitis of the SDFT within the pastern region is less common but more difficult to manage than tendonitis in the metacarpal region. Lameness is more pronounced, and recurrence of clinical signs is common. With ultrasonography, lesions can be detected at the tendon insertion over the lateral or medial aspect of the middle phalanx. Treatment includes rest, local and systemic antiinflammatory drugs, blisters, corrective shoeing, and alternative training, particularly swimming. Monitoring of the healing process is important to prevent recurrence.
Osteochondrosis of the Tarsocrural Joint
Joint effusion represents the most common feature of tarsocrural OC, a condition with a reported prevalence ranging between 4% and 20%.25-33 Tarsocrural OC frequently is diagnosed in yearlings, and breeders are particularly concerned because the condition may lower the yearling’s price at the autumn sales. For this reason, tarsocrural effusion in yearlings now represents a frequent indication for radiographic examination and preventative arthroscopy.
Lameness associated with OC is rare, but selected lesions may cause gait disturbances. In horses with effusion and osteochondral fragmentation, it is important to rule out other causes of lameness. Lesions affecting the lateral trochlear ridge of the talus and medial malleolus of the tibia are more likely to cause lameness and synovial effusion than are lesions of the cranial aspect of the intermediate ridge of the tibia. Focal areas of radiolucency or loss of radiopacity on the medial malleolus may be associated with osteochondral fragmentation and may represent an indication for diagnostic arthroscopy.34 In young horses with effusion, arthroscopic removal of fragment(s) represents the best option. Prognosis after arthroscopic treatment of tarsocrural OC is good, but synovial effusion may persist especially when OC involves the lateral trochlear ridge of the talus and the medial malleolus.35,36 Studies performed in Europe found no significant differences in the racing performance and longevity of STB trotters with or without tarsocrural OC.1,32,37
 The Australasian Standardbred
The Australasian Standardbred
Description of the Sport
Standardbred (STB) horses have been racing in Australia and New Zealand for more than 140 years. In both countries the sport does not enjoy the same high profile as Thoroughbred (TB) racing, and prize money is generally lower, which attracts fewer professional trainers than TB racing. Owner/trainers are common, with many stables having fewer than 10 horses. Horses can begin racing at 2 years of age and generally race until 8 or 9 years of age.
Most races are for pacers, with trotting races being much less common. In Australia, races range in distance from 1600 to 2600 m, and most pacing races are from a mobile start, with an occasional standing start. All trotting races are from a standing start. In New Zealand, races tend to be longer, up to 3200 m, and standing starts are more common.
Regional meetings carry prize money of $A2000 (Australian dollars) to $A5000 per race, whereas metropolitan meetings offer $A15,000 per race. The 15 most valuable pacing races in Australia and New Zealand make up what is called the Grand Circuit. Prize money for Grand Circuit races ranges from $A125,000 to $A1,000,000 for the Interdominion Pacing Championship Final and the New Zealand Cup. Prize money for trotting races is substantially less than that for pacers. The Interdominion trotter’s Championship Final carries a $A250,000 prize, and New Zealand’s Row Cup has a prize of $NZ300,000.
An increased number of stakes programs for young horses have become available in recent years. The Australasian Breeders Crown is held over all states of Australia and both islands of New Zealand for 2-, 3-, and 4-year-old pacers and trotters. Australian Pacing Gold is a program for yearlings sold at the sales of the same name and also has feature races for 2-, 3-, and 4-year-olds. The value of these programs puts great pressure on trainers and clinicians to persist with young horses that may benefit from rest.
Race speeds generally are expressed as mile rates, which is the time taken to travel 1 mile averaged over the whole race. Tight tracks result in slightly slower rates than large tracks. Typical mile rates for pacers in 1600-m races are 1 : 56 to 1 : 58. For 2400-m races, mile rates of 2 minutes are typical.
Track Surface or Training Surface and Lameness
Most of the racetracks are 700 to 1000 m in circumference, and races are run in a counterclockwise direction, except for the north island of New Zealand, where races are run clockwise. Track surfaces vary but usually consist of sand or fine gravel. Banking of turns tends to be modest, although a trend to greater degrees of banking and resulting reduced injury rates has been demonstrated. Many trainers have their own homemade training track that is often just graded dirt or sand and not always well maintained, and recurrent subsolar bruising can be a major problem. Banking on these tracks tends to be minimal. In coastal areas, training on the beach is popular and considered beneficial for horses with injuries.
Training Methods
A typical training program involves a period of jogging exercise, generally of about 6 weeks, and these sessions generally last 35 to 40 minutes. Higher-speed work in hobbles (pace work) is introduced two to three times a week. A typical workout is two intervals of half to three-quarter pace over  miles. The speed of these workouts is steadily increased over 4 to 6 weeks until speeds approaching those of race speed are achieved. A horse that is racing generally is hobbled twice a week and jogged on the other days. Training in New Zealand is similar, with the major difference being the tendency to house horses in paddocks rather than in stables.
miles. The speed of these workouts is steadily increased over 4 to 6 weeks until speeds approaching those of race speed are achieved. A horse that is racing generally is hobbled twice a week and jogged on the other days. Training in New Zealand is similar, with the major difference being the tendency to house horses in paddocks rather than in stables.
Lameness Examination
Experience in examining STBs for lameness is essential because of their awkward gait, even when trotting. A high incidence of lameness occurs in horses in full work, and numerous sites of pain are common.
Examination at Rest (Preferably in a Stable)
The clinician should observe the horse standing for any obvious swelling, abnormal weight bearing, and areas of hair loss on the proximal limbs associated with the position of the hobbles. The clinician should palpate the neck and back to detect any areas of pain; palpate the supraspinous ligament, dorsal spinous processes, and dorsal sacroiliac ligament, along with the longissimus dorsi muscles; and then examine each limb in turn. Palpation is performed with the limb bearing weight and not bearing weight. The veterinarian should palpate the digital pulse amplitude in the distal aspect of the pastern or over the abaxial surface of the proximal sesamoid bones (PSBs). Observe each joint and palpate for swelling or effusion. Palpate the tendons and ligaments for heat, pain, and swelling. Particular attention should be paid to all levels of the suspensory ligaments (SLs) of the forelimbs and hindlimbs. The clinician should take time to examine the hind fetlock joints for effusion. Flex the joints firmly to detect pain, and apply hoof testers to each foot.
Trotting in a Straight Line
The horse should be trotted on a firm flat surface. Many horses pace initially, which makes the diagnosis of subtle lameness difficult. Persistence is important because most horses will trot after two or three runs up and down. The horse should be observed trotting away from and toward the observer and should be observed from the side.
Diagnostic Analgesia
Nerve blocks generally are required where no cause of lameness is obvious or the importance of a clinical finding is not clear. Where no localizing clinical signs are apparent, I use a standard approach: in the forelimb a pastern ring block is performed. The veterinarian should avoid nerve blocks at the level of the PSBs because distinguishing between PSB pain and foot pain is difficult. This is followed by a low four-point block and then a subcarpal block and intraarticular blocks of the middle carpal joint and then the antebrachiocarpal joint. Should the horse fail to respond to these blocks, median and ulnar nerve blocks are performed to rule out the lower limb as a source of pain. Rarely are blocks of the elbow joint, intertubercular (bicipital) bursa, or shoulder joint required.
A similar sequence of blocks is used in the hindlimb. A single lateral plantar metatarsal nerve block may be performed if plantar condylar subchondral bone pain is suspected. A subtarsal block is followed by an intraarticular block of the tarsometatarsal joint and then the centrodistal joint. The tarsocrural joint is seldom blocked because there is generally swelling associated with intraarticular pathological conditions. Tibial and fibular blocks are performed to rule out the lower limb as the source of pain. Occasionally an intraarticular stifle block is required, in which case all compartments should be blocked at one time.
Imaging Considerations
Radiography remains an important imaging technique. Oblique images of the distal phalanx are important when a fracture is suspected because some may be missed on dorsopalmar images. A flexed lateromedial image of the metacarpophalangeal joint should be obtained to highlight the sagittal ridge of the distal aspect of the third metacarpal bone (McIII) and the dorsal surfaces of the PSBs. Proximodistal oblique images of the hind fetlocks are obtained to demonstrate fragments of the proximal plantar aspect of the proximal phalanx and the lateral condyle of the third metatarsal bone (MtIII). Carpal images should always include a skyline image of the third carpal bone.
Ultrasonographic examination of the digital flexor tendons and SLs commonly is required. Superficial digital flexor tendon (SDFT) lesions are often peripheral rather than core lesions. Lesions also may involve the distal third of the metacarpal region or the proximal metatarsal region, areas that are examined less commonly by ultrasonography and may be more difficult to assess. Cross-sectional area measurements comparing affected and nonaffected limbs are essential when assessing subtle lesions. When examining the SLs, it is important to assess the full length because lesions can affect the origin, body, and branches.
Scintigraphy is useful for assessing STBs with complex lameness, STBs that fail to improve with diagnostic analgesia, and when pain is localized but no abnormalities are detected with radiography or ultrasonography. Stress fractures are common and can be insidious in onset. Typical sites include the third tarsal bone, lateral cortex of the tibial shaft, and the distal phalanges. Subchondral bone injuries may not be observed on radiographs yet are well documented with bone phase scintigraphic images.
Proceeding without a Diagnosis
Intraarticular corticosteroids often are used to assist in diagnosing subtle hindlimb lameness. Bilateral intraarticular injection of the tarsometatarsal and centrodistal joints may be used in horses in which hindlimb lameness is too subtle for accurate assessment by nerve blocks. Triamcinolone acetonide is the most commonly used intraarticular corticosteroid because of its relatively short and predictable detection time. Treatment of metatarsophalangeal joints also is often performed because lameness can be subtle. The clinical relevance of fragments of the plantar aspect of the proximal phalanx is often questionable, and intraarticular therapy may be the only method of confirming that metatarsophalangeal joint pain exists.
Shoeing Considerations
Most horses are shod and trimmed by the trainer or owner. Therefore the quality varies extremely. Steel rim shoes generally are used, with trailers on the hind feet being universal. These shoes are thin and provide little protection for the sole. An occasional horse is trained and raced barefoot. Wider web aluminum shoes, similar to those used on TB racehorses, are available, but the use of these shoes is less common. These shoes generally have steel inserts to improve grip. Glue-on shoes rarely are used. In an attempt to promote increased length of stride, toes are often left overlong but there is no evidence to support this traditional approach. The combination of overlong toes and the lack of sole protection predisposes horses to subsolar bruising. Manipulation of shoeing methods is used for horses that hit the carpi during the swing phase. Generally this is trial and error. Heavier shoes tend to exaggerate any abnormal movement in the swing phase and result in higher hoof flight.
Diagnosis and Management of Lameness
Subsolar Bruising and Abscessation
The diagnosis of subsolar bruising is based on pain with the application of hoof testers over the sole, either localized or generalized, and increased lameness after concussion of the foot. Lameness is localized to the foot with a pastern ring block, and radiography is performed to rule out a fracture of the distal phalanx. Chronic bruising may result in radiolucency and modeling of the margins of the distal phalanx, but these changes do not necessarily mean that the bruising is active. Scintigraphy will allow assessment of active inflammation and bone metabolism. Hemorrhage within the horn of the sole may or may not be evident. Horses with acute lameness are treated with rest and nonsteroidal antiinflammatory drugs. Careful attention should be paid to foot balance, and wide-web aluminum shoes should be fitted.
Osteoarthritis of the Fetlock Joint
Osteoarthritis (OA) of the metacarpophalangeal or metatarsophalangeal (fetlock) joint may or may not be associated with joint effusion and swelling. Usually the horse shows pain on passive flexion and a positive response to a fetlock flexion test. Lameness should be improved with a low four-point block or intraarticular analgesia. If lameness is recent, no radiological abnormalities will be apparent, but more chronic lameness is associated with modeling changes on the dorsal aspects of the proximal phalanx and the McIII or the MtIII. Modeling also may be observed on the articular margins of the PSBs and the palmar or plantar aspect of the proximal phalanx. In advanced OA, subchondral radiolucent or cystic lesions may be observed in the palmar or plantar aspect of the condyles of the McIII or the MtIII. This is most common in the lateral condyle of the MtIII and is best observed on a proximodistal oblique radiographic image. Scintigraphy may be required for horses with few radiological changes and demonstrates increased radiopharmaceutical uptake in the subchondral bone.
Proliferative Synovitis
Proliferative synovitis occasionally causes lameness in STBs. Lameness generally is localized to the metacarpophalangeal joint by either perineural or intraarticular analgesia. Abnormal concavity proximal to the dorsal and occasionally the palmar aspects of the sagittal ridge of the McIII is observed on lateromedial radiographic images. Ultrasonography demonstrates enlargement of the synovial pad medial or lateral to the sagittal ridge of the McIII on the dorsal aspect, which must be differentiated from the joint capsule. Intraarticular corticosteroids may be used, but the results often are disappointing. Surgical excision of the synovial pad using arthroscopy is usually effective in resolving the lameness. The prognosis is poorer in horses with modeling of the palmar aspect of the McIII because this usually reflects the presence of more advanced chronic OA.
Axial, Articular (Type 1) Osteochondral Fragments of the Proximal Plantar Aspect of the Proximal Phalanx
Fragments of the proximal plantar aspect of the proximal phalanx are best observed on proximodistal oblique radiographic images of the metatarsophalangeal joints. These views should be included in the workup of horses with low-grade hindlimb lameness or a history of not running straight. Lameness is generally mild or not present at low speeds. Most horses have a positive flexion test of the affected fetlock, and about half have joint effusion.3 Osteochondral fragments of the proximal plantar aspect of the proximal phalanx are most commonly found medially but can occur laterally or biaxially. These fragments are present by 1 year of age and are thought by some to be traumatic in origin. Treatment involves arthroscopic removal, and treated horses can be returned to training within 6 weeks. Intraarticularly administered corticosteroids are sometimes used to determine the relevance of these lesions because not all are associated with poor performance.
Carpal Joint Disease
Lameness caused by carpal pain is common in Australasian STBs, affecting up to 30% of horses in training. In the absence of intraarticular fractures, lameness is often bilateral, and effusion is mild or absent. Because of the lack of localizing signs, intraarticular analgesia must be used to localize the pain causing lameness to the carpus. Radiographs should always include a skyline image of the third carpal bone. Often only increased radiopacity with or without focal radiolucent defects of the third carpal bone is observed.
Intraarticular fractures of the carpal bones generally involve the middle carpal joint. Fractures involving the antebrachiocarpal joint are less common and lameness is generally mild. More severe lameness is seen in horses with slab fractures or severe joint injury. Joint swelling and pain on flexion are common. Treatment options include arthroscopic surgery to remove diseased bone and cartilage, intraarticularly administered corticosteroids, and rest.
Suspensory Desmitis
In most horses with suspensory desmitis, swelling and pain on palpation of the affected area of the SL are obvious, but lesions confined to the origin may be more difficult to diagnose, and subcarpal or subtarsal nerve blocks are required for diagnosis. Ultrasonographic examination confirms desmitis based on increased cross-sectional area and areas of decreased echogenicity. Radiological examination is used to assess the palmar or plantar aspect of the McIII or the MtIII and the PSBs at the proximal and distal attachments of the SL. The ideal treatment involves an initial period of rest and antiinflammatory treatment to allow the inflammation to resolve, followed by a period of controlled exercise. Horses should not return to full work for 12 months. In practice this is not always possible, and many horses can be managed by reducing the workload for shorter periods, treating with antiinflammatory drugs, and monitoring the response with ultrasonography.
Superficial Digital Flexor Tendonitis
Tendon injuries are easy to diagnose when the midmetacarpal or midmetatarsal area is involved. Swelling and pain on palpation are indications for ultrasonographic examination to confirm the diagnosis and differentiate from peritendonous inflammation. Horses with moderate to severe injuries are treated with rest and antiinflammatory therapy until the swelling is reduced, followed by a controlled exercise program. Intralesional injection of bone marrow or bone marrow–derived stem cells has been used, but long-term follow-up data on efficacy are currently lacking. Full work should not be reintroduced until 12 months after injury. Less severely injured horses may be kept in work, provided the exercise level is reduced and the tendon is monitored by ultrasonography. Such management is more successful in horses with hindlimb injuries. Tendon injuries at the level of the digital flexor tendon sheath (DFTS) may result in secondary palmar annular ligament (PAL) constriction and tenosynovitis. Lameness and effusion of the DFTS are observed when the horse is returned to training. Provided healing of the tendon injury is adequate, the PAL can be sectioned tenoscopically and the horse rapidly returned to training to prevent the formation of adhesions.
Osteoarthritis of the Distal Tarsal Joints
Confirmation of the distal tarsal joints as the source of pain causing lameness involves using intraarticular analgesia or intraarticular medication in horses with more subtle lameness. Although radiographs are useful for determining the extent of bony changes, they are not always diagnostic. Scintigraphy is more sensitive and may also reveal stress fractures of the third tarsal bone or the proximal dorsal aspect of the MtIII. Treatment involves intraarticular injection of long-acting corticosteroids. Triamcinolone acetonide is the most commonly used because of its reliable excretion times and reliable duration of action.
Fracture of the Distal Phalanx
STBs with a sudden onset of forelimb lameness after racing or fast work but with no localizing signs should be suspected of having a fracture of the distal phalanx. Application of hoof testers usually elicits pain, but this is not always consistent. Oblique radiographic images of the foot often are required to assess the fracture properly. It is important to determine whether the fracture enters the DIP joint. Most fractures are intraarticular. In horses that race counterclockwise, left forelimb fractures are generally of the lateral palmar process, and right forelimb fractures are generally of the medial palmar process. Occult fractures are occasionally identified with scintigraphy. Horses with nonarticular fractures are treated with a bar shoe with quarter clips or a rim shoe, and 12 months of rest. Horses with articular fractures may be treated in the same manner or by internal fixation with a single 4.5-mm screw placed in lag fashion along with a bar shoe with quarter clips. Evidence of the relative success of these treatments is limited, with the choice depending on individual preference. Reports indicate that 50% to 75% of Australian STBs with fracture of the distal phalanx are able to race following treatment with a bar shoe.2 It is recommended that a bar shoe be maintained when horses return to racing to reduce the risk of refracture.
Sagittal Fracture of the Proximal Phalanx
The clinical presentation of horses with sagittal fractures of the proximal phalanx depends on fracture configuration. Horses with short, incomplete fractures may have chronic lameness that is localized to the fetlock joint with nerve blocks. Longer fractures often cause acute onset of lameness. Swelling may be present, and the horse often has pain on palpation of the dorsal aspect of the proximal phalanx. Nerve blocks are contraindicated because of the risk of progression of the fracture. Radiological examination confirms the diagnosis. Horses with nondisplaced fractures may be treated with external coaptation. Internal fixation with screws placed in lag fashion is recommended for horses with complete and displaced fractures. Horses with short, incomplete fractures may heal with rest. Internal fixation has been recommended for horses with fractures that fail to heal.
Tarsocrural Osteochondrosis
The most common osteochondrosis lesion affecting the tarsocrural joint of STB horses involves the cranial aspect of the intermediate ridge of the tibia. Most horses have effusion of the tarsocrural joint, and lameness is absent or subtle. Radiographs demonstrate fragmentation of the cranial aspect of the intermediate ridge of the tibia. The fragments are removed arthroscopically.
Stifle Disease
Lameness localized to the stifle is rare in the STB racehorse. These horses appear to be able to race successfully with radiological evidence of OA of the femorotibial joints. Direct trauma to the stifle may result in soft tissue and bony injuries as in other types of horses. Trainers often are concerned that a horse may be locking its stifles, but this generally resolves with increased fitness, and sectioning of the medial patellar ligament is rarely necessary.