Chapter 119Lameness in the Polo Pony
History of the Sport
Polo was the first equestrian sport in recorded history. With strong ties to military traditions, the game originated in China in ad 272 and was often substituted for war games in preparation for military battle. Polo evolved into an organized sport and spread into Greece, India, and China, where the British colonies adopted the game. During the nineteenth century, the game became more refined in Great Britain and eventually found its way into the northeastern United States in 1876. Today polo continues to be one of the fastest and most dangerous equine sports in the world. Polo is no longer a sport only for the wealthy; an increasing number of small clubs start up each year that attract people of moderate incomes to take lessons, buy horses, and begin to play. The sport has become more complex, with international professional players competing year-round on different teams. Thus professional polo coaches, umpires, trainers, and breeders have emerged, solidifying polo as a genuine equine sport industry. Playing seasons in the northern and southern hemispheres are followed by nomadic players, grooms, horses, and spectators. During the winter months in the United States, thousands of horses enter Florida and California, where the tropical climate is conducive to world-class polo tournaments. During the spring, summer, and fall seasons these horses travel across the Midwest, up the northeast coast and into Canada. The high-goal season begins in the summer in England and Spain, but in the southern hemisphere, the season in Argentina commences in the fall.
Polo as an Industry
Today three types of polo are played: outdoor, indoor (arena), and snow polo. Outdoor polo is by far the most popular and is played on a large, finely manicured grass field measuring 274 m (300 yards) by 137 m (150 yards) (Figure 119-1). Injuries are related to fatigue (because of the distances covered), stopping, turning, speed, and surface consistency, depending whether the soil beneath the grass is compact or soft. Arena polo is played in much smaller arenas and is more common in collegiate settings. Injuries tend to be less frequent and are usually impact related. Snow polo is regarded as a novel exhibition sport played on the surface of a frozen lake and produces surprisingly few injuries. Obviously, footing and surface conditions often can be responsible for the type of lameness seen. Heavy, soft, grass polo fields and deep, sandy, uneven exercise tracks are frequently responsible for proximal suspensory desmitis (PSD), suspensory branch desmitis, and metacarpophalangeal joint sprains. Hard fields, exercise tracks, and polo field sideboards may cause hoof and pastern region injuries, and hard, fast ground predisposes horses to superficial digital flexor (SDF) tendonitis.

Fig. 119-1 Outdoor polo is the most popular format for the game today. Close proximity of horses and riders explains why polo ponies often develop injuries related to direct trauma. Polo is only played right-handed.
In outdoor polo each team is composed of four players, and each member brings an average of seven to eight horses to the field. A game normally runs for six chukkers (a chukker is 7 minutes), and a different horse is used for each chukker. In higher goal polo, numerous mounts are used in single chukkers. Therefore in a single match there may be 50 to 55 horses playing over 1.5 hours. The number of horses that are required to mount a polo team makes each owner’s total investment much larger than that for other equine disciplines.
Polo requires the speed and stamina of a Thoroughbred (TB) or a TB-cross horse, the ability to stop and turn quickly, and the boldness to meet and collide with other horses at high speed. Although called ponies, polo horses stand 15 to 16 hands tall, and mares are preferred to geldings at a ratio of 10 : 1. Most trainers look for a fine neck and throatlatch, a good strong shoulder, powerful hip, quiet disposition, and a responsive, light mouth. Many horses have not raced, so few racetrack-related injuries are found in polo ponies. Argentina, New Zealand, and Australia are the only countries that specifically breed large numbers of horses for polo competition. Horses indigenous to these countries tend to have more bone than those in the United States and Europe, rendering them slightly more durable. Argentina has historically produced the most horses used solely for polo. Since 1970, thousands of Argentine horses have been imported into the United States and Europe, primarily because such a large selection was available at low cost. During the 1970s, inexpensive American former racehorses were sold as polo prospects, but many had numerous orthopedic problems. Today the price of high-goal Argentinian polo ponies continues to increase, and as the cost of importing horses into the United States increases, economic demands necessitate a greater influx of American TBs into polo. Recently, embryo transfer has been used by players from the United States. Embryos are collected from top playing mares during the off-season and from retired superior mares to produce numerous foals each year. Argentina and, to a lesser extent, Australia have led the movement toward embryo transfer.
Most horses are 3 to 4 years old when introduced to the game, and 2 years of training and playing generally are required before a pony becomes seasoned. Exceptionally talented horses are playing high-goal polo at 6 years of age. By the age of 12 to 14 years, speed usually has begun to diminish, and horses are sold to less demanding players. By the age of 15 to 16 years, depending on temperament, polo ponies may be sold to beginners before being retired.
Neck reining is paramount in training a polo prospect because the rider uses only one hand for control. Wide range of movement, the ability to stop and turn quickly, and the ability to exhibit rapid bursts of speed are required. How well and smoothly the horse performs these maneuvers often determines the number of years the horse stays sound and competes successfully. In addition to schooling, fitness training consists of daily galloping (legging up). Ponies often are tied together in sets of four to five. This time-saving practice teaches the horses to travel more calmly together in close contact but can result in traumatic injuries to the lower limbs (Figure 119-2).
Fig. 119-2 Daily legging up is an important part of training polo ponies. Ponies often are tied together in sets of four to five, and although this practice saves time, horses in close contact are at risk of traumatic injury.
Polo ponies are shod with special rim shoes in front that allow for traction and pivoting without applying excessive torque to the lower limb. Medial and lateral heel calks on the hind shoes are helpful for stopping abruptly but often result in coronary band and pastern region lacerations to other horses during competition. For safety reasons, the Great Britain Polo Association only permits a lateral calk on each hind shoe, whereas the United States Polo Association allows medial and lateral heel calks. The size limit for calks is regulated but seldom enforced. Therapeutic corrective shoeing is problematic in playing horses (those actively being used in polo competition) because they may lose traction and maneuverability. Some common shoeing modifications include squared, rolled, and rocker toes; elevated and full-shod heels; and padded soles. The standard support and protection afforded the horse during exercise are leg wraps and coronet boots. All legs are wrapped with double-layer rolled cotton bandages. Impact-resistant European racing boots may be added to cover the metacarpal regions to protect against mallet and hoof trauma. More recently, especially on previously injured limbs, cotton leg bandages have been replaced with neoprene fabric wraps that extend below the fetlock joint and provide additional support. Despite these additional protective barriers, horses may still injure tendons and receive skin lacerations during a game or practice.
Drug testing of polo ponies is not yet compulsory in the United States, and no mention of prohibitive medication is addressed in the United States Polo Association rulebook; however, limited testing is done in Great Britain and France. Attending veterinarians often work for many competing teams within the same tournament, and prompt assessment of injuries is important. Low doses of nonsteroidal antiinflammatory drugs (NSAIDs) are commonly used, especially in horses with wounds and solar bruising. The general aim is to have as many sound horses as possible sharing the workload during a match to avoid the practice of double-chukkering (using the same horse for two chukkers).
Minor conformation abnormalities in polo ponies often can be overlooked, but some faults predispose ponies to specific injuries. Long toes and underrun heels may result in tendonitis of the deep digital flexor tendon (DDFT) and palmar foot pain. Toed-in horses are prone to develop lateral suspensory branch desmitis, whereas toed-out horses are more likely to injure the medial branch. Horses with long pasterns and long third metacarpal bones (McIII) are at increased risk of tendonitis of the superficial digital flexor tendon (SDFT).
The most common sources of lameness in polo ponies are similar to those seen in most other equine sports. Polo ponies are at higher risk for traumatic injury because of the high-impact play and the practice of tethering of horses in close proximity to other horses during shipping, exercise, and polo tournaments. Causes of lameness often seen concurrently include palmar foot pain and PSD and osteoarthritis (OA) of the fetlock joint with chronic suspensory branch desmitis.
Lameness Examination
Horses should be stabled overnight so that they cannot warm out of subtle lameness. The horse is first examined in the stall and then as it walks from the stall. The horse is observed at a trot in a straight line on a hard surface and is circled in both directions. Most polo ponies are reluctant to lunge. If necessary, the horse may be observed under saddle, but Argentine ponies generally resist trotting when ridden.
A systematic examination at rest is begun with the hoof and hoof tester evaluation and then continued proximally in the limb, noting evidence of pain, swelling, or obvious injury. Findings always should be compared with the contralateral limb, especially when palpating the body of the suspensory ligament (SL). Joints are assessed for range of motion and a painful response to flexion. Lower limb flexion is followed by carpal or upper hindlimb flexion. Walking the horse briefly between flexion tests to allow an aggravated response to wear off is wise.
One of us (PJM) attends to many older polo ponies that have effusion of the metacarpophalangeal joints, manifest a positive response to flexion, and even may have visible and radiological evidence of OA, but lameness often is abolished using low palmar digital analgesia. Palpation may reveal one or more fractured splint bones with callus, but the rest of the limb should be examined because the cause of lameness may be elsewhere.
If a definitive diagnosis cannot be made, diagnostic analgesia is performed. Because drug tests are not performed, local anesthetic solutions can be used for diagnostic purposes in actively competing horses. When performing a nerve block, it is important to remember that the block may affect a larger area than intended, primarily related to diffusion of local anesthetic solution to surrounding tissue. High palmar analgesia can mask middle carpal joint pain, and palmar nerve blocks performed at the base of the proximal sesamoid bones (PSBs)can eliminate pain associated with the fetlock joint. For this reason, the horse should be observed at the trot shortly after injection of local anesthetic solution and then again after an appropriate wait.
To reduce time and money spent on lameness diagnosis, one author (PW) prefers to block large areas during the initial examination. Specific blocks then are performed, if necessary, the following day. For example, a horse that shows neither a sensitivity to hoof tester examination nor an increased digital pulse amplitude may go sound after palmar nerve blocks performed at the base of the PSBs. The following day the same horse may show slight improvement after palmar digital analgesia and a 100% improvement with intraarticular analgesia of the distal interphalangeal (DIP) joint. However, two authors (PJM and MWR) prefer to start distally and work proximally in a systematic fashion.
Intraarticular analgesia is used extensively in polo ponies because it is more specific than perineural analgesia. Although intraarticular analgesia requires aseptic preparation and carries a small risk of infection, clients are generally receptive. If lameness is localized to a specific joint on clinical examination, therapeutic agents such as corticosteroids and hyaluronan can be added to local anesthetic solution to confirm diagnosis and initiate treatment simultaneously. One author (PW) uses combination diagnostic and therapeutic arthrocentesis typically in the DIP and proximal interphalangeal (PIP) joints. The horse’s immediate response to local analgesia is noted, and response to therapy is usually evident 2 to 3 days later. Another author (PJM) frequently uses combination diagnostic and therapeutic injections in the DIP and distal hock joints. Combination injections can also be used simultaneously to diagnose and treat back pain. The dorsal aspect of the dorsal spinous process and the interspinous space can be infiltrated with a combination of local anesthetic solution, Sarapin (High Chemical Company, Levittown, Pennsylvania, United States), and a corticosteroid. Response to infiltration is evaluated immediately by riding the horse after injection, and response to medication is evaluated over the next several days.
Because metacarpophalangeal joint disease and splint bone injury are common sources of pain in the polo pony, one author (PJM) prefers specifically to differentiate these sources of pain by first performing intraarticular analgesia of the metacarpophalangeal joint and then later performing a low palmar block. If low palmar analgesia is performed first, both potential sources of pain are eliminated. If pain is detected on palpation of bony exostoses of the splint bones, these areas can be blocked first, before a systematic blocking strategy is followed. One author (PJM) refers to this as the splint block. This block is performed by first blocking the palmar metacarpal nerve distal to the exostoses. If improvement is not seen, the palmar metacarpal nerve just proximal to the exostoses is then blocked (2 mL of local anesthetic solution). A biaxial splint block can be performed if exostoses are found medially and laterally. This block should be done well below the origin of the SL to clearly differentiate PSD from splint bone disease. Splint disease, mainly from direct trauma from mallets and calk trauma, is common in hindlimbs. Diagnostic analgesia is performed as described in the forelimb.
Hindlimb PSD has become a common diagnosis because we are now more aware of it. In the United Kingdom, a variation of the high plantar nerve block, analgesia of the deep branch of the lateral plantar nerve (see Chapter 10), is commonly used to diagnose PSD. Three milliliters of local anesthetic solution is injected deep to the proximal aspect of the lateral splint bone, and 2 mL each is placed over the medial and lateral plantar nerves. If this block is unsuccessful in abolishing pain, each hock joint compartment is blocked subsequently. This procedure then is followed by fibular and tibial nerve blocks. In Argentina, chemical neurolysis (long-term nerve block) of the fibular and tibial nerves frequently is performed for horses with distal hock joint pain or PSD (PJM).
Undiagnosed Lameness
In some horses the lameness is inconsistent and/or subtle, and diagnostic analgesia cannot be performed. Nerve trauma on the abaxial aspect of a PSB may cause episodic, transient severe lameness. An option in a horse with mild inconsistent lameness is to treat with phenylbutazone (2 g orally [PO] twice daily) for 5 days and then reassess the horse. If lameness resolves and does not return after treatment is discontinued, the horse gradually is put back into work. In horses with inconsistent lameness that fail to respond to rest or therapy, we recommend nuclear scintigraphic examination. Exercise intensity can be increased in horses with subtle lameness but is done so with caution. Lameness may become more apparent to the point at which diagnostic analgesia can then be performed. In a horse with recurrent episodes of hindlimb lameness, the veterinarian should be aware of the possibility of an ilial stress fracture (SK).
Occasionally, a polo pony becomes acutely non–weight bearing, with lameness lasting only a few minutes and resolving before examination is possible. If this sort of episode becomes recurrent in the same limb and physical examination reveals no clinically significant findings, we refer the pony for nuclear scintigraphic examination.
Consultation with colleagues and second opinions are always options. It is also important to consider the option of extended turnout. Because the career of a polo pony can last 12 to 15 years, owners are often willing to give the horse 6 to 12 months of turnout to avoid any further injury. If subtle lameness resolves with phenylbutazone therapy, the polo pony can compete because there is no drug testing in polo competition. However, this option must be elected with caution.
Several lameness problems may exist simultaneously in a polo pony, a fact that makes observing the primary or baseline lameness difficult. Subtle signs such as the failure of a horse to stop appropriately, a horse that jumps on after stopping, or a horse that turns one way or the other when stopping (which is probably from outside hindlimb pain; horses turn away from lameness) may reflect low-grade lameness. If these observations have been made, having the horse ridden to witness the problems first hand is useful. In one author’s experience (PJM), the most common source of pain in this type of situation is from the distal hock joints.
Imaging Considerations
Conventional, computed, and digital radiography are the mainstays of imaging, with the front feet and front fetlock joints and hock joints being examined most frequently. The introduction of computed and digital radiography has provided great advantages because, with the exception of faulty positioning or movement, obtaining nondiagnostic radiographs is almost impossible. Exposure can be adjusted at the time of processing, and subtle details that would have been difficult to see on conventional radiographs can now readily be detected and scrutinized easily with computed and digital radiography. Images can be enlarged, and the contrast and brightness can be improved, which are important factors in the diagnosis of incomplete fractures.
Scintigraphic examination is particularly useful in polo ponies with undiagnosed lameness and in those with palmar foot pain, but it is not always helpful in horses with chronic lameness (SK). Motion-correction software has been an important innovation.
Ultrasonography is extremely important in evaluating the damage and healing processes in tendons and the SL in forelimbs and hindlimbs. Transverse images are used more frequently in identifying lesions, whereas longitudinal images aid in assessing healing. Ultrasonographic evaluation of the supraspinous ligament is often useful in horses with obscure hindlimb lameness. We have not found thermography particularly useful in our practices.
Magnetic resonance imaging (MRI) has become available in university settings and in some private equine practices. Despite a long learning curve in the interpretation of magnetic resonance images, many differential diagnoses and prognoses have emerged. Nowhere is this more evident than in obscure foot and pastern lameness with no detectable radiological abnormalities.
Diagnostic arthroscopy in horses with OA of the metacarpophalangeal or carpal joints can be valuable in evaluating the condition of joint surfaces. Palmar intercarpal ligament injury has been diagnosed in ponies with lameness localized to the middle carpal joint but lacking radiological and scintigraphic abnormalities. Tenoscopy and bursoscopy also can be useful diagnostically and therapeutically.
Ten Most Common Lameness Problems in Polo Ponies
Superficial Digital Flexor Tendonitis
SDF tendonitis is the most common soft tissue injury seen in polo ponies and is by far the most common reason for early retirement. SDF tendonitis can be divided into three categories by location on the limb—high (proximal), midmetacarpal, and low (distal)—or by cause: trauma, speed, and fatigue.
We believe that most peripheral injuries of the SDFT result from tendon trauma while the limb is bearing weight. However, the Editors note that peripheral injuries commonly are seen in other sports horses, such as Standardbred racehorses and reining horses, in which direct trauma is usually not a factor. These injuries occur much more frequently at the midmetacarpal region on the lateral aspect and to a lesser extent on the palmar surface of the tendon (Figure 119-3). Proximal SDF tendonitis also can be caused by trauma (PJM). These areas have a high degree of exposure to swinging mallets and flying hooves. Despite new protective boots, the SDFT is still traumatized with surprising frequency. Traumatic tendon injuries are generally noticed 1 to 2 days after the incident and are characterized by a slight widening of the tendon (not a banana-shaped profile). Lameness is usually not present, but the area is warm and tender to palpation. Some horses have recurrent heat and swelling that resolves quickly with topical and systemic antiinflammatory therapy. Peripheral tendon fiber lesions may involve 20% or less of the cross-sectional area (CSA) of the tendon. However, careful ultrasonographic examination of the medial and lateral borders of the SDFT and critical evaluation of longitudinal images are necessary. Recurrent tendonitis leads to typical swelling and later lameness commonly found with moderate or severe SDF tendonitis.
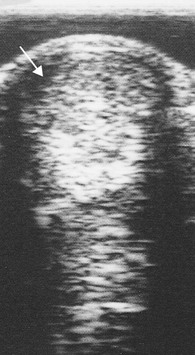
Fig. 119-3 Transverse ultrasonographic image of the palmar metacarpal region of a polo pony with traumatic tendonitis of the lateral aspect of the superficial digital flexor tendon (arrow). Lateral is to the left. After initial diagnosis, the horse continued to play, and the lesion progressed.
Core lesions and lesions of the SDFT adjacent to the DDFT are thought to be injuries related to speed and fatigue. Hard, fast ground may be a predisposing factor. SDF tendonitis may result in a banana-shaped profile of the metacarpal region. Core lesions compromising between 20% and 25% of the CSA of the SDFT are serious, and the risk of recurrence is high (Figure 119-4). Horses with small CSA tears that extend more than 2.5 cm in length or those with distally located tendonitis involving SDFT impingement by the palmar annular ligament (PAL) are at high risk of recurrence. Despite appropriate therapy, these horses often have chronic and recurrent lameness, and ultrasonographic evaluation reveals a lesion that often fails to heal.
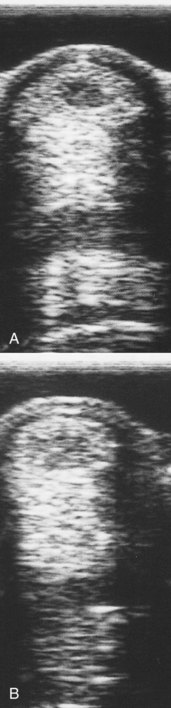
Fig. 119-4 Initial (A) and 40-day follow-up (B) transverse ultrasonographic images of the palmar metacarpal region of a polo pony with a typical core lesion of the superficial digital flexor tendon. Tendon splitting was done immediately after the initial image was obtained. The core lesion is more echogenic in the follow-up image but can still be seen.
Initial therapy for any polo pony with tendonitis regardless of location or cause includes the application of ice boots and cold-water hosing, sweats, and compression wraps, as well as the administration of NSAIDs. A combination of injection and rest or surgical management has been successful (MWR).
Medical Management
Peritendonous injections over lesions and intralesional injections have become the mainstay of today’s preferred therapy for SDF tendonitis. The aim of this therapy is to return the injured segment of tendon to its elastic state and maintain tensile strength. Peritendonous injections of short-acting corticosteroids and hyaluronan may help to reduce inflammation and improve the cosmetic appearance of the tendon profile, but it is important that corticosteroids are not injected directly into a tendon. Peritendonous corticosteroid injection is frowned on in the United Kingdom (PJM). Autologous adult mesenchymal stem cells, platelet-rich plasma (PRP), and porcine bladder matrix (PBM) have emerged as the biological-based therapies of choice and have markedly increased the success of medical management. One author (PW) prefers an ultrasonographic guided injection of PRP directly into lesions and prefers to use only small volumes of the prepared serum into the lesion. Results using adult fat-derived stem cells are equally satisfactory, but this technique requires preinjection surgical collection, as well as transit time, and is substantially more expensive than using in-house processed PRP. PBM is commercially available (ACellVet, ACell Inc., Columbia, Maryland, United States), requires no surgical harvesting or transit time, and is comparable in price to PRP processing, although it occasionally causes postinjection flares. These flares can be reduced by using a small volume of PBM rather than using the entire reconstituted vial. Daily topical icing and rebandaging, along with NSAIDs, are good precautionary therapies to reduce reactions.
Ultrasonographic assessment of tendons 2 months after injection with one of these biologically based products has revealed remarkable filling within hypoechogenic lesions on transverse images. At 6 months after treatment there is good fiber alignment seen on longitudinal images. The real endorsement of success is that approximately 80% of horses with first-time bowed tendons treated with these products have returned to the same level of polo without recurrence of injury within 8 to 12 months.
Surgical Management
Tendon splitting is now seldom used as a standalone therapy to manage polo ponies with SDF tendonitis. If used, tendon splitting within 1 week after injury appears to be beneficial in decompressing the lesion. Tendon splitting must be done early because granulation tissue forms quickly and cannot be decompressed. After appropriate sedation, perineural analgesia, and aseptic preparation, 30 to 40 incisions with a No. 11 scalpel blade in a stabbing manner (a fan-shaped pattern is avoided) are used to decompress only the affected tendon segment. One author prefers using a double-edged tenotome in a fan-shaped pattern (MWR). The procedure can be performed with the limb in a weight-bearing or flexed position, but a weight-bearing position is preferred. With experience, the texture of diseased tendon can be differentiated from surrounding normal tendon structure. Bandages are applied, and horses are confined to a box stall and given controlled, increasing handwalking over the next 8 to 10 weeks. Controlled exercise is recommended for a minimum of 4 to 6 months before any form of turnout exercise is given, but client compliance with this timetable is poor unless a horse walker is available. Unfortunately, most horses are turned out to pasture after blistering within 1 month of injury, a conventional practice we believe is harmful to tendon healing. Total time of turnout exercise (after controlled exercise) is 8 to 12 months. Follow-up ultrasonographic evaluation is important to monitor healing and to determine when exercise level can be stepped up. Desmotomy of the accessory ligament of the SDFT (superior check desmotomy) has been useful in horses with large core lesions (CSA >25%) and in those with small tears (CSA <15%) that are more than 2.5 cm in length. Combining the surgical procedures of desmotomy and tendon splitting early after injury has been successful in returning horses with tendonitis of the SDFT to polo. After surgery, horses are given stall rest and handwalking for 4 to 6 weeks, with a total of 4 to 6 months of controlled exercise, before being turned out or conditioned for polo. Desmotomy of the PAL occasionally is performed when the SDFT is injured and enlarged just above the ligament. This surgery interrupts a self-perpetuating cycle of injury that develops between the enlarged tendon and the thickened PAL. One author (PW) believes that horses with distal tendonitis of the SDFT involving the PAL should initially be treated with peritendonous injection of short-acting corticosteroids followed by compression wraps, not only to reduce the size and improve cosmetic appearance of the SDFT but also to prevent the need for desmotomy of the PAL.
The most common reasons for therapeutic failure in horses with SDF tendonitis are lack of ultrasonographic follow-up evaluation after tendon splitting to determine whether additional therapy is needed, poor owner compliance concerning walking the horse and stretching the injured tendon in the early stages of healing, not allowing for adequate rest before the horse is returned to work, and failure to perform ultrasonographic examination at the time of initial injury, resulting in an inability to evaluate maximal medical improvement before returning the horse to unsupervised work.
Metacarpophalangeal (Fetlock) Osteoarthritis
OA of the fetlock joint is the most common articular problem in polo ponies and the most common articular problem necessitating early retirement. Former racehorses with mild OA, osteochondrosis, chip fractures, and chronic capsulitis may be sold for use as polo ponies and have a high risk of redeveloping lameness. The fetlock region of any polo pony with forelimb lameness should be examined carefully. Lameness apparently originating from the fetlock joint based on the clinical observations of pain on palpation, decreased range of motion, and a positive response to distal limb flexion must be differentiated from suspensory branch desmitis and splint bone disease. Intraarticular analgesia is important for differentiation. A full set of radiographs should be obtained. One author (PJM) recommends using large cassettes to assess the fetlock joint and distal aspect of the splint bones. Common radiological findings include fragmentation of the dorsoproximal aspect of the proximal phalanx (Figure 119-5), radiolucent areas in the distal aspect of the McIII, proliferative new bone formation on the palmar aspect of the PSBs, and mineralization of the proximal and distal fetlock joint capsule attachments (Figure 119-6).

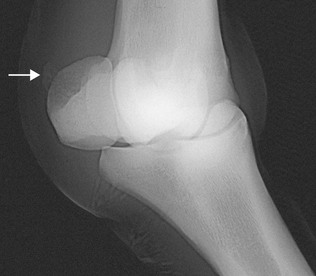
Fig. 119-5 Dorsolateral-palmaromedial oblique radiographic image of a metacarpophalangeal joint of a polo pony with osteoarthritis. Soft tissue swelling is apparent; a rounded osteochondral fragment is on the proximal dorsomedial aspect of the proximal phalanx; and proliferative changes involve the proximal aspect of the proximal phalanx and proximal sesamoid bones.

Fig. 119-6 Slightly oblique lateromedial radiographic image of a metacarpophalangeal joint. Mineralization at the insertion of the lateral digital extensor tendon and metacarpophalangeal joint capsule on the proximal aspect of the proximal phalanx is a common radiological finding in polo ponies with osteoarthritis of the fetlock joint. Although the finding is important, it does not preclude successful playing.
Intraarticular injections are the mainstay of treatment. One author (PW) injects both short-acting corticosteroids and hyaluronan. Another author (PJM) prefers polysulfated glycosaminoglycan (PSGAG; Adequan, Luitpold Animal Health, Shirley, New York, United States) therapy or short-acting corticosteroids and hyaluronan or a combination of atropine, short-acting corticosteroid, and hyaluronan. Intramuscular injections of PSGAGs at biweekly intervals for 1 month and then possibly weekly for the entire season are recommended. Horses that do not respond well to intraarticular injections of corticosteroids may be candidates for serial interleukin-1 receptor antagonist protein (IRAP) injections or arthroscopic evaluation because many of these horses have considerable cartilage damage. IRAP is now commercially available for in-hospital collection, incubation, and administration and is generally administered at bimonthly intervals for a series of three to five doses. IRAP was initially used by one author (PW) in polo ponies that were unresponsive to corticosteroid therapy and was used in conjunction with hyaluronan. Unless the IRAP is prepared with strict asepsis and processed preferably in a sterile hood, it is well advised to use a 2-µm filter to ensure sterility during the injection process. If using hyaluronan in conjunction with the IRAP, be sure to inject the hyaluronan either first or after the filter is removed from the needle hub because the viscosity of the hyaluronan is too thick to pass through the filter. Now many veterinarians, including one auther (PW), are using IRAP as their first line of therapy to treat both acute and chronic joint disease, and its good success tends to appear later rather than earlier in the life of an osteoarthritic joint. Daily icing, poulticing, and NSAID administration can help reduce inflammation in horses with chronic OA. In horses with chronic OA, radiological abnormalities may be extensive, but many horses are serviceably sound (Figure 119-7).

Fig. 119-7 Lateromedial radiographic image of the distal aspect of a forelimb of a serviceably sound polo pony. There is modeling of one of the proximal sesamoid bones (and a mineralized radiopacity distally) and the dorsoproximal aspect of the proximal phalanx, as well as osteoarthritis and osteochondral fragmentation of the proximal and distal interphalangeal joints.
Fetlock joint capsulitis is often a concurrent problem with fetlock OA and can be an additional source of pain and a cause of restricted motion. On rare occasions it can be the only cause of pain and resentment of joint flexion. One author (PW) has seen substantial benefit from mesotherapy applied to the dorsal aspect of the fetlock joint. After aseptic preparation and performing a “ring block” of the fetlock joint, the author uses a 3-tipped mesotherapy injector with 27-gauge × 4-mm needles to inject the area with corticosteroid (triamcinolone acetonide, 9 mg), Sarapin (4 mL), and mepivacaine (4 mL) dorsomedially and dorsolaterally. A compression wrap/sweat is applied for 24 hours after the injection. This treatment usually results in greater range of pain-free motion of the joint and may also be used in conjunction with intraarticular therapy.
Chronic proliferative synovitis (villonodular synovitis) is common in polo ponies with chronic OA of the fetlock joint and may be associated with capsular tearing (SK). The dorsal aspect of the fetlock joint develops an apple-shaped appearance, with only mild or moderate effusion. Chronic proliferative synovitis is most common in horses previously used as racehorses and becomes evident after several years of polo. Radiographs may reveal an abnormal contour of the distal dorsal aspect of the McIII, and positive contrast radiographs may be diagnostic. We prefer ultrasonographic examination because ultrasonography helps differentiate between horses that are surgical and nonsurgical candidates. Chronic proliferative synovitis masses of 1.5 cm or larger should be removed arthroscopically to maximize long-term prognosis, whereas horses with smaller masses respond well to rest and intraarticular corticosteroid injections. Intraarticular atropine sulfate also has been used successfully (SK) to reduce effusion.
Suspensory Desmitis
Suspensory desmitis is seen at three levels: PSD, suspensory body desmitis, and suspensory branch desmitis.
Proximal Suspensory Desmitis
PSD occurs frequently, and diagnosis is confirmed using high palmar or lateral palmar analgesia. PSD results from polo ponies exercising on soft, uneven footing and is not necessarily related directly to playing polo. Lameness is usually only visible at a trot and varies in degree. The cranial phase of the stride is shortened, and lameness is usually most prominent with the affected limb on the outside of a circle. Palpation of the proximal palmar metacarpal region often reveals neither pain nor clinically appreciable enlargement of the SL. Polo ponies with PSD often fail to improve with rest and NSAID administration. Longitudinal ultrasonographic images are most useful in the diagnosis of PSD, but negative ultrasonographic findings do not necessarily eliminate the possibility of injury. MRI is useful to evaluate the bone–ligament interface, particularly in horses in which PSD is difficult to diagnose because there are no detectable changes on radiographs or on ultrasonographic images. CSA measurements on transverse images are occasionally helpful if the same area is measured in the affected and contralateral limbs. One author (PW) has found that variation in CSA measurements leads to misdiagnosis because even in normal polo ponies obtaining reliable repeat measurements is difficult. Hypoechogenic muscle tissue should not be confused as a lesion (SK).
PSD causes more subtle lameness and clinical signs in polo ponies than in other sports horses. Subtle injury and enlargement may cause the ligament to be pinched or compressed by overlying dense fascia, especially in hindlimbs. Horses with long-standing PSD often have increased radiopacity of the proximal aspect of the McIII visible in lateromedial or dorsopalmar radiographic images. Absence of increased radiopacity does not rule out PSD because horses with soft tissue injuries often lack bony involvement. Avulsion fractures of the McIII at the origin of the SL, incomplete longitudinal fractures of the McIII, and stress reaction can occur independently or concomitantly to PSD. Radiological and ultrasonographic examinations may reveal small or large fragments or proliferative changes and radiolucency associated with the palmar cortex of the McIII. Computed and digital radiography, nuclear scintigraphy, and MRI are beneficial in diagnosing bony injury and differentiating it from PSD. Follow-up radiographs may be necessary because avulsion or longitudinal fractures may not show up on initial radiographs.
Even without treatment, almost all polo ponies with PSD and bony causes of proximal palmar metacarpal pain recover within a 3-month rest period. However, horses that are notably lame at a walk, stand somewhat unstably, and occasionally buckle at the carpus of the affected limb may require up to 6 months of rest. In polo ponies with PSD in which a quick return to work is mandated, local injection into and around the origin of the SL with a combination of short-acting corticosteroids and PSGAGs hastens resolution of clinical signs. Ponies are walked for 1 week and then put in light work the second week. By the third week they may be galloped and are able to play shortly thereafter. Owners tend to keep polo ponies with PSD in work if the end of the season is near because ponies are turned out routinely for 3 to 6 months after the season. Owners may gamble successfully by continuing to play the horse through the end of the season without permanently damaging the ligament. Polo ponies rarely get hindlimb PSD, but when they do, prognosis is guarded, and treatment by neurectomy often is required.
In horses with chronic PSD, once bony involvement has been ruled out, local injections of corticosteroids and Sarapin or internal blister may be warranted. In the United Kingdom and Europe, injection of corticosteroids into the proximal aspect of the SL is frowned on because this medication may slow healing and may mask the presence of fractures (SK and PJM). This is especially true in horses with acute injuries. Numerous applications of shock wave therapy are popular and may prove beneficial. Horses with known bony injury should be given rest. One author (PW) prefers the use of concentrated bone marrow–derived stem cells to infiltrate the origin of the SL in combination with fasciotomy.
Body Suspensory Desmitis
Body suspensory desmitis is a serious and often career-ending injury. Diagnosis is straightforward if the SL is thickened and painful. Ultrasonographic examination is crucial in assessing SL damage, but radiology is important to evaluate the medial and lateral splint bones because splint bone disease often is associated with suspensory desmitis in a polo pony. Radiographs should be obtained even if obvious areas of pain or bony and soft tissue swelling associated with the splint bones are absent. Treatment of polo ponies with acute body suspensory desmitis includes immediate application of cold or ice therapy, alternating with topical sweats, and administration of NSAIDs. Periligamentous infiltration of short-acting corticosteroids early after injury improves cosmetic appearance and may minimize adhesion formation between the SL and splint bones. Injections are performed in polo ponies only if the owner agrees the horse is in need of long-term rest. The horse gradually is returned to handwalking in 5 to 7 days and can be turned out after 3 weeks. Intralesional injections of concentrated bone marrow into SL body tears have proven beneficial and successful, and one author (PW) prefers this over PBM and fat-derived adult stem cells. Sclerosing agents (e.g., ethanolamine) injected into the SL may be helpful (SK). Two authors (PW and PJM) believe that long-term box stall rest may increase the chance of adhesion formation. One author (MWR) prefers controlled exercise rather than turnout exercise and believes strongly that turnout exercise is the “antithesis of healing.” Ultrasonographic evaluation of ligament healing is important. One author (PJM) has observed many polo ponies with distal body suspensory desmitis that involves the bifurcation and invariably at least one branch. If desmitis at the suspensory bifurcation is severe, the polo pony may never fully recover. The best results are seen with a combination of periligamentous injections of dimethyl sulfoxide (DMSO) and corticosteroids and long-term rest. Performance level may need to be dropped to junior polo, and even at this level lameness may be persistent or recurrent.
Suspensory Branch Desmitis
Suspensory branch desmitis is common in polo ponies. The lateral branch is injured more frequently than the medial branch, and occasionally both branches are injured simultaneously. Pivoting of the distal limb at high speeds is likely the cause of suspensory branch desmitis. Faulty conformation is another important predisposing factor. Horses that are toed in tend to develop lateral suspensory branch desmitis, whereas those that are toed out tend to develop medial suspensory branch desmitis. Palpation of the branches while the fetlock joint is in partial flexion is a preferred technique of one author (PW). Firm palpation and lower limb flexion followed by trotting exacerbates the degree of lameness. Ultrasonographic examination of the branches is accomplished easily and allows assessment of the degree of suspensory branch desmitis. Radiography should be performed to evaluate the distal aspects of the splint bones because fracture and fracture displacement are common in ponies with suspensory branch desmitis. Mineralization in a branch close to attachment on a PSB may occur in horses with chronic injury (Figure 119-8). Horses with acute injuries are treated identically to those with suspensory body desmitis. The appearance of the branch can be restored cosmetically to near normal over time with periligamentous injection of short-acting corticosteroids. The branch can be split 2 to 3 weeks after injury, although results in the United Kingdom have been disappointing (SK). In the United States, one author (PW) believes that branch splitting in conjunction with shock wave therapy has had superior results compared with adult stem cell or PRP injections. Horses with suspensory branch desmitis need about 6 months of layup time before returning to polo training. One author (PJM) believes that adhesions between the inflamed branch and surrounding tissue or the ipsilateral splint bone negatively influence prognosis, and corticosteroid injections may limit adhesion formation. Surgical adhesiolysis and distal ostectomy of the fractured splint bone may be useful in horses with chronic suspensory branch desmitis and splint bone fracture, but the cosmetic appearance is usually less than desirable. Counterirritants still are used in Europe with variable results. We believe that pin firing (hot firing) is not successful for horses with suspensory body desmitis, but it can be useful for horses with suspensory branch desmitis as a last resort.
Injury to the Hoof and Distal Phalanx
Polo more than other types of equine sporting activity predisposes horses to direct hoof trauma. Direct trauma results from swinging mallets, horses stepping directly on the hard polo balls used during playing, interference or direct impact from hooves of nearby horses, and from horses stepping on wooden sideboards at great speed. Calk or stud injuries to the hoof wall and pastern region are most common. Careful evaluation of wounds for involvement of deeper structures, such as the PIP and DIP joints, is necessary. A common lameness that occurs during polo competition is called getting stung, referring to a sudden crippling lameness, lasting only a few minutes, generally resulting from a blow to the hoof or pastern by a mallet or hoof of another horse. The horse is usually sound within minutes of the incident with no clinical evidence of injury. Occasionally, a fracture occurs that may not be evident radiologically for up to 14 days.
Fractures of the Distal Phalanx
Acute fractures of the palmar processes of the distal phalanx often occur from mallet blows, and because polo is played right-handed, fractures usually are seen in the medial aspect of the left forelimb and lateral aspect of the right forelimb. Oblique fractures are sometimes difficult to see in conventional radiographic images, and several dorsoproximal-palmarodistal oblique images may be necessary. Rarely, fractures of the solar margin or of the extensor process of the distal phalanx are seen. Management of polo ponies with distal phalangeal fractures is similar to that in other sports horses.
Palmar Foot Pain Including Navicular Disease
Palmar foot pain in polo ponies with TB and TB-cross ancestry appears to be decreasing, primarily because of the successful efforts of farriers and owners. The problem may be worse in American TBs than in TBs originating from the United Kingdom, Argentina, Australia, and New Zealand (PJM). The long-toe and underrun heel complex and the tendency to shoe front feet with shoes with short branches that sit tight at the heel (to prevent front plates from being pulled off by hind feet) gradually have been corrected. Squared or rolled toe shoes, with or without an elevated heel (world plates and natural balance plates), have reduced the number of polo ponies with broken pastern foot axes and have reduced DDFT tension caused by prolonged breakover. Owners have allowed farriers to reset polo plates more frequently during the playing season and to perform more frequent four-point trims during the off-season than in previous years. The causes of palmar foot pain are often difficult to differentiate from navicular disease because the horse may show a painful response to hoof testers, and lameness is abolished using palmar digital analgesia. Differentiation may be possible using intraarticular analgesia of the DIP joint, radiography, and scintigraphy. Many polo ponies with palmar foot pain have secondary pain at the origin of the SL, which is thought to be caused by alteration of gait.
A common source of palmar foot pain is laminar tearing at the heel. Sudden stops force the horse to use the heels of the front feet as brakes. Corns or heel bruising can cause poor performance and lameness. Corns are diagnosed easily using hoof testers and by carefully inspecting the seat of the corn for hemorrhage or discoloration. One author (PJM) has seen many polo ponies toward the end of the polo season with bilateral, biaxial horn staining resembling chronic corns that apparently did not result in overt lameness. Management of polo ponies with palmar foot pain resulting from corns is similar to that used for undiagnosed palmar foot pain, including the application of wedge pads to relieve heel pain for a few games, or by using the four-point trimming method with natural balance or straight bar shoes and acrylic rubber frog and heel support. One author (SK) has found that four-point shoeing provides poor grip and traction and considers it unsuitable for polo ponies. However, most feel these shoeing techniques appear to decrease stress on the heel and the DDFT and navicular region. Hoof growth stimulants and NSAID administration may help horses with palmar foot pain.
Osteitis of the Distal Phalanx (Pedal Osteitis)
Although definition and accurate diagnosis of osteitis of the distal phalanx remain obscure, many polo ponies with palmar foot pain have evidence of disease in the margins of the distal phalanx on scintigraphic and radiographic images. There may be new bone projecting distally from the palmar aspect of the distal phalanx seen on a lateromedial radiographic image. This finding should be interpreted carefully on radiographs obtained during purchase examinations.
Navicular Disease
Navicular disease in a polo pony is characterized by chronic forelimb lameness, which is abolished using palmar digital analgesia, intraarticular analgesia of the DIP joint, or analgesia of the navicular bursa, often with little radiological abnormality. Nuclear scintigraphy may be helpful to differentiate navicular disease from other causes of palmar foot pain. Most horses with early navicular disease respond positively to intraarticular administration of hyaluronan and corticosteroids into the DIP joint. The administration of NSAIDs and isoxsuprine and the application of corrective shoeing techniques (see Palmar Foot Pain section) are valuable. Those ponies unresponsive to intraarticular injections of the DIP joint may improve after injection of the navicular bursa, best performed under radiographic guidance. MRI has become extremely valuable in differentiating between navicular bone pathology and soft tissue pathology. Therapy, length of rest, and prognosis differ for horses with deep digital flexor (DDF) tendonitis versus those with acute navicular bone pain. Horses with acute navicular bone injury that fail to respond to treatment of the DIP joint or navicular bursa are rested for 3 to 6 weeks and treated with NSAIDs; work is then resumed for the rest of the season with continued treatment with NSAIDs. Horses with advanced navicular disease or those unresponsive to therapy may be dropped from medium- or high-goal polo. Horses with DDF tendon (DDFT) injury have a much more guarded prognosis and are treated by 6 to 12 months of rest. Initially a frog support is applied and the heel is elevated, combined with stall rest, handwalking for 4 weeks, and NSAIDs. This is followed by 3 months of shoeing with full heel support and then turnout unshod, with monthly trimming for the remainder of the convalescent period. Palmar digital neurectomy is considered undesirable and is not routinely performed. Chemical neurolysis (long-term foot block) is of limited value. Cryoneurectomy can give limited relief, but the palmar digital nerves regrow and lameness recurs. Concomitant or solitary injury of the DDFT does not appear to be as common in polo ponies as in other sports horses (PJM). Shock wave therapy may offer a viable solution for these horses.
Distal Interphalangeal Osteoarthritis
Early (synovitis) and chronic OA of the DIP joint can cause lameness in the polo pony, but diagnosis can be challenging because of the lack of specificity of analgesic techniques in the foot. For example, if more than 6 mL of local anesthetic solution is injected into the DIP joint and lameness is evaluated after 3 to 5 minutes (SK) or 10 minutes (PW), pain from other areas of the foot, including the sole, can be blocked inadvertently. This effect can be avoided by using smaller amounts of local anesthetic solution. Horses with synovitis have DIP joint effusion and manifest only a mildly painful response to lower limb flexion. However, this test may be positive in horses with many sources of pain, including either the navicular bone or the fetlock joint. Management of horses with OA of the DIP joint usually includes intraarticular medication. Short- or long-acting corticosteroids are preferred to injection with hyaluronan. One author (PJM) combines corticosteroids and DMSO because DMSO may improve distribution of corticosteroids to all parts of the joint and the navicular bursa. The DIP joint is the only joint in which one author (PW) uses PSGAGs, combined with short-acting corticosteroids. Another author (PJM) favors using PSGAGs in horses unresponsive to injections with corticosteroids. Most of these horses have clinical and radiological evidence of advanced OA. In some polo ponies, lameness does not improve directly after intraarticular analgesia but inexplicably resolves 24 to 36 hours later, when presumably the effects of the corticosteroid begin. After intraarticular injection, horses are given 3 weeks of limited exercise and a tapered dose of NSAIDs. Weekly intramuscular administration of PSGAGs for a minimum of 30 days and the application of corrective shoes to ease breakover are recommended.
Desmitis of the Accessory Ligament of the Deep Digital Flexor Tendon
Trainers and owners commonly confuse chronic desmitis or acute tears of the accessory ligament of the deep digital flexor tendon (ALDDFT) with bowed tendons. Desmitis of the ALDDFT occurs in polo ponies, especially older ponies (SK), but is less frequent than SDF tendonitis. Mild desmitis is characterized by a meaty, nontender swelling of the proximal palmar metacarpal region between the SL and DDFT. Horses with severe or complete tears can have prominent swelling at or near the junction of the ALDDFT with the DDFT, but neither lameness nor the response to palpation is commensurate with the degree of damage. Diagnosis must be confirmed and healing monitored using ultrasonographic examination. Initially, horses are managed with rest, cold therapy including ice, application of sweats, and administration of NSAIDs. Local infiltration of short-acting corticosteroids around (but not in) the ALDDFT can help cosmetic appearance. Stall rest for 2 weeks is recommended, and thereafter horses can be turned out for 4 to 6 months. Follow-up ultrasonographic examination reveals an enlarged, hyperechogenic ALDDFT. Prognosis for future soundness and return to polo is usually excellent in horses with small (<30% mass) tears, but swelling persists. Chance of recurrence is slim. In horses with large tears (>30% mass) or near ruptures, the chance to return to competitive polo is slim, even with 1 year off work.
Splint Bone Disease
Traumatic exostoses (Figure 119-9) caused by swinging mallets and fractures of the splint bones are common in polo ponies and are sometimes referred to as bamboo fever. Although trauma is usually the inciting cause of exostoses, injury of the SL may play a role (PJM). Horses with splint exostoses resent direct palpation, but many do not manifest overt signs of lameness. If lameness is present but the exostosis is only mildly painful, a splint block (see page 1152) should be performed to confirm the diagnosis. Splint disease can make a veterinarian look foolish because an acute injury may be confused with PSD, but subsequent development of a large golf ball-size swelling reveals the true diagnosis. Oblique radiographic images are most helpful for evaluating the splint bones.

Fig. 119-9 Dorsolateral-plantaromedial oblique radiographic image of the metatarsal region. There is a comminuted fracture of the proximal aspect of the fourth metatarsal bone caused by mallet injury (called bamboo fever). This fracture usually does not require internal fixation, and prognosis for future soundness is good.
Local infiltration of corticosteroids and Sarapin is used to treat polo ponies with acute splint exostoses. Other injections include a combination of corticosteroids, Sarapin, calcitonin, and medroxyprogesterone acetate. Calcitonin (400 IU) and medroxyprogesterone acetate (200 mg) are used commonly in Europe (PJM). Rest, compression wraps, sweats, and the administration of NSAIDs are useful. Polo ponies with chronic exostoses seem to benefit from pin freezing (cryotherapy), and this is the treatment of choice, with a quick return to work in 14 days. Cryotherapy appears to stimulate remodeling of chronic proliferative splint exostoses, and often a cosmetically acceptable limb profile is seen within 6 months. Despite the resulting white spots, clients seem to accept this form of therapy because of a high success rate. Thermocautery (hot firing) has merit, and early results of shock wave therapy appear promising (PJM).
Proximal splint bone fractures may require surgical fixation, and certainly horses need prolonged stall rest and a slow return to work. If fractures are nonarticular and fragments are not displaced or are displaced minimally, prognosis is favorable.
Polo ponies with nondisplaced diaphyseal splint bone fractures respond well to cryotherapy. Cryotherapy not only produces local analgesia but also induces deep fibrous tissue formation that stabilizes fracture fragments. Cryoprobes (No. 17 pointed probes, Veterinary Ophthalmic Specialties, Inc., Moscow, Idaho, United States) are applied two at a time in firm contact with the skin covering the abnormal splint for 1 minute at each site, at sites 1.5 cm apart. Applying two probes at different sites simultaneously decreases treatment time. Preselected aim point patterns for pin freezing are marked by commercially available office white correction fluid. Because each site is to be frozen only once to minimize surface skin necrosis, technicians often draw the pattern on a piece of paper before freezing and check off the appropriate sites once the probes have been applied. A major reason for failure of pin freezing splints is the use of cryospray units to apply nitrogen, rather than using prefrozen probes. Pointed probes pressed firmly into the skin form better ice balls on the surface of the bone, creating a much better bone response, remodeling, and flattening of the exostosis. Maintaining a 1-minute freeze with no movement of the subzero probes is also useful. Failure to pattern the pin freeze outward to slightly beyond the perimeter of the preexisting splint exostosis often results in continued growth of the exostosis above and below the therapy area. After cryotherapy, the limb is kept wrapped for up to 3 weeks, but ponies return to exercise within 4 to 7 days. Ponies with nondisplaced splint bone fractures are given rest for 4 to 6 weeks. Distal splint bone fractures can be diagnosed easily using longitudinal ultrasonographic images or radiography. These fractures usually are associated with chronic suspensory branch desmitis, which is thought to cause bowing of the distal aspect of the splint bone and subsequent displacement and proliferative changes (Figure 119-10). Distal fracture fragments generally are removed surgically, and concomitant splitting of the involved SL branch(s) is often performed.

Fig. 119-10 Dorsolateral-palmaromedial oblique radiographic image of the metacarpal region. A chronic displaced fracture of the fourth metacarpal bone is associated with suspensory branch desmitis. The second metacarpal bone is bowed away from the third metacarpal bone; chronic proliferation has resulted from instability; sesamoiditis is apparent; and the suspensory branch has mineralization.
Distal Hock Joint Pain
Polo ponies can play successfully with moderate to severe radiological changes in the distal hock joints (Figure 119-11). Most of the distal hock joint pain appears to be subclinical, meaning lameness is not the most noticeable clinical sign. Most polo ponies with distal hock joint pain are noticed by owners or riders to lack quick jump-out speed and the ability to stop abruptly and are noticed to be running through the bridle. These ponies generally improve if they are given ample warm-up time before playing. Distal hock joint pain appears to be one source of pain with which a polo pony can live, but such pain is a major cause of poor performance and may induce compensatory lameness such as PSD in the forelimbs as a result of overload. Proximal limb flexion tests may elicit little response, and detecting pain or effusion using careful palpation is difficult in some horses. Because lameness is not necessarily proportional to radiological changes, scintigraphic examination is helpful, especially in polo ponies with subtle hindlimb lameness. Diagnostic analgesia is an important tool if lameness is perceptible, and in horses with bilaterally symmetrical lameness, analgesia of one hindlimb may induce obvious contralateral lameness. Combining diagnostic and therapeutic injections is commonplace because the practice saves time and money. The tarsometatarsal and centrodistal (distal intertarsal) joints are injected most commonly with methylprednisolone acetate, but in some ponies the tarsocrural joint also is injected. Intramuscular administration of PSGAGs and intravenous injection of hyaluronan throughout the playing season appear to be helpful in allowing horses to play up to potential. Horses are kept in work and placed on low doses of NSAIDs throughout the season, and training is limited.
Gluteal Myositis and Back Pain
Gluteal myositis often accompanies subclinical hindlimb lameness and is often a compensatory problem. One or both hindlimbs have a shortened cranial phase of the stride. Deep palpation of the gluteal muscles elicits pain, although the muscles never feel as hard as they do in ponies with rhabdomyolysis. If possible, it is important to determine whether gluteal myositis is a primary or secondary problem. Gluteal myositis can be differentiated easily from rhabdomyolysis because serum creatine kinase and aspartate transaminase levels are invariably normal. Polo ponies with gluteal myositis can be treated with local injections directly into the gluteal muscles and between the biceps femoris and semitendinosus muscles. The horse is allowed light work and is placed on NSAIDs. One author (PW) has had modest success using a 5-day series of rubeola virus immunomodulator. If gluteal myositis is secondary, the primary source of pain must be identified and managed successfully.
Back pain in polo ponies is often secondary to lameness or results from mismanagement, including use of ill-fitting saddles, overweight amateur riders, and mouth problems. Poor dentition from lack of, or inappropriate, tooth floating procedures causes sharp molars to come in contact with gag bits. Horses carry the head and neck high to avoid pain and tend to hollow the back. Back pain can become a permanent or chronic problem if horses are mismanaged continually. Back pain generally is characterized by a painful response to palpation along the lateral edges of the longissimus dorsi muscles. The horse exhibits a crouching gait when mounted and during initial walking under saddle.
Intramuscular injections of corticosteroids combined with Sarapin (2 : 1 ratio) are performed along the length of the longissimus dorsi muscle, from the caudal border of the trapezius muscle to the level of the tuber coxae, 15 cm lateral to the dorsal midline. Injection sites are placed every 15 cm, and 5 mL of the mixture is administered at each site. Mesotherapy is also extremely beneficial and is often used in conjunction with deep muscle injections. After preparation of the lumbar region, mesotherapy is performed using a 5-tipped mesohead with 27-gauge × 4-mm needles. A volume of 35 mL of flumethasone, Sarapin, mepivacaine, and Traumeel is used to inject two passes down each side of the dorsal midline. Generally horses are ponied (led from another horse) for 5 days before being ridden. Relief from pain is quick and predictable with this treatment. Because back pain may be compensatory to primary distal hock joint pain or other lameness, it is important to evaluate the hindlimbs and pelvis carefully. Primary management of the distal hock joint pain and local treatment of acupuncture points in the back are common.
Dorsal spinous process impingement can be a source of back pain, and one author (PJM) believes this is a major cause of back pain in the polo pony. Diagnosis should be confirmed by assessing the effect of local analgesia and/or performing scintigraphy (SK). Treatment involves injection of the spaces between the dorsal spinous processes with corticosteroids and Sarapin. Shock wave therapy may be beneficial (PJM and PW). Horses with back pain are given NSAIDs and are kept fit during a 4- to 6-week period using ponying (being led from another horse) exercise. In Europe, a common management regimen includes paddock exercise as much as possible, lunging exercise with the horse’s head down, and little warm-up before polo games. Internal blisters have been used with some success, but care must be taken when injecting these compounds because deep muscle abscesses can develop. Faradism is useful for longissimus dorsi and gluteal muscle strain (SK).
Other Conditions
Dislocation (Luxation) of the Superficial Digital Flexor Tendon
Although rare, avulsion injury and dislocation of the SDFT from the tuber calcanei is seen nearly once each year in a busy polo pony practice, resulting in extreme panic by the pony, necessitating sedation. The SDFT usually dislocates laterally, but diagnosis may be difficult before swelling develops. In our experience, surgical techniques, including primary repair, mesh augmentation, and laterally located screws combined with full-limb cast application, are neither successful nor necessary. Most horses respond well to confinement in a small pen and subsequent turnout for 6 to 12 months. Turnout exercise is recommended as soon as possible. Despite the fact that the SDFT remains displaced, causing a slight mechanical lameness and enlargement of the calcaneal and gastrocnemius bursae, horses tend to perform well at the canter and gallop, with a fair to good prognosis for medium- and low-goal polo. Some polo ponies with lateral dislocation of the SDFT in one limb develop the same condition in the opposite limb 1 or 2 years later (PJM).
Fractures of the Cranial Thoracic Dorsal Spinous Processes (Fracture of the Withers)
Fracture of the withers is fairly common. Polo ponies are often tied next to each other for long periods, and a frightened horse occasionally rears up and flips over (Figure 119-12), resulting in fractures of the longest dorsal spinous processes at the withers. Often up to four dorsal spinous processes are fractured, with ventral displacement of the fragments resulting in a flattened appearance of the withers. Ponies are usually only mildly painful to palpation but are generally reluctant to lower the head when grazing. The affected horse may travel with a painful, stiff, extended head and neck carriage, and some horses grunt with every stride. The prognosis for return to polo is excellent after rest for 4 to 6 months, as long as secondary infection does not develop. Special consideration should be given to saddle fit; a croup strap may be necessary to keep the saddle from sliding forward.
Proximal Interphalangeal Osteoarthritis and Other Pastern Region Injuries
OA of the PIP joint (high ringbone) occurs occasionally in polo ponies and is seen most frequently in green horses (generally Quarter Horses or Quarter Horse/TB crosses) playing on rough terrain in the western United States and generally results from irregular footing. Pain originating from the PIP joint is difficult to diagnose in horses with acute disease without radiological changes, but it can be identified scintigraphically. OA of the PIP joint is often difficult to manage, and although motion of this joint is limited, lameness can be inappropriately severe. Rest (60 to 90 days), NSAID therapy, and intraarticular long-acting corticosteroid therapy are recommended.
A common finding in oblique radiographic images of the pastern region is periosteal new bone on the medial aspect of the left forelimb and the lateral aspect of the right forelimb proximal phalanges (Figure 119-13). Because polo always is played right-handed, powerful neck shots always hit the right side of each forelimb. Lameness is usually insignificant and short lived. These radiological changes should not be confused with those resulting from enthesitis at the attachment sites of the distal sesamoidean ligaments. To differentiate OA of the PIP joint from these proliferative changes, intraarticular analgesia or pinpoint perineural or local analgesic techniques should be performed.

Fig. 119-13 Dorsomedial-palmarolateral oblique radiographic image of the distal aspect of a left forelimb. Proliferative new bone (arrows) along the palmar medial aspect of the proximal phalanx is typical of a mallet injury. Polo is played right-handed, and trauma usually involves the medial aspect of the left forelimb and the lateral aspect of the right forelimb proximal phalanges.
Sesamoiditis
Inflammation (sesamoiditis) of the PSBs can be caused by direct mallet or hoof trauma and by stress-related injury at the suspensory branch insertions. Traumatic sesamoiditis occurs in the medial PSB in the forelimbs from interference injury and in the lateral PSB in the forelimb and hindlimb from mallet trauma. Diagnosis of sesamoiditis is straightforward using radiography and scintigraphy, but ultrasonographic evaluation provides information about the suspensory attachment as well. One author (PJM) believes that shock wave therapy is a promising treatment modality for sesamoiditis.
Fractures of the PSBs are rare, and response to surgery is similar to that of other sports horses. Ponies with fractures of the base of the PSBs rarely return to athletic soundness with or without surgery. Polo ponies with basilar fractures and desmitis of the oblique sesamoidean ligament often can be helped by using shock wave therapy (PJM). An apical fracture of the PSB may be mistaken for mineralization of the suspensory branch. Polo ponies with apical fractures of the PSBs have a good prognosis, provided that SL injury is not concurrent. Horses with apical fractures associated with sesamoiditis and insertional suspensory branch desmitis often have recurrent lameness. It is important to differentiate true fractures from sesamoiditis or a commonly seen radiological abnormality in older polo ponies, one to three stress lines in the PSBs, which most often are considered incidental changes.
Digital Flexor Tenosynovitis and Desmitis of the Palmar Annular Ligament
Tenosynovitis of the digital flexor tendon sheath (DFTS) is common in polo ponies. Debate exists as to whether this syndrome is caused by desmitis of the PAL or whether the PAL is a passive structure causing only constriction of the inflamed DFTS. The terms tenosynovitis and desmitis of the PAL are sometimes used synonymously, but tenosynovitis with mild thickening of the PAL is more common than primary desmitis. A normal or slightly thickened PAL can restrict SDFT movement in horses with tendonitis, but this is a separate entity (see page 1153). In polo ponies, desmitis of the PAL can be solitary and diagnosed in horses with healthy digital flexor tendons. It can lead to tenosynovitis or can accompany tenosynovitis. Primary desmitis of the PAL occurs most frequently from interference injury, when a hind foot strikes a forelimb PAL, or from direct mallet trauma. Initial trauma may be minor, but continued trauma can lead to substantial injury (Figure 119-14). Whether primary or secondary, tenosynovitis with thickening and compartmentalization of the DFTS can occur proximal and distal to the PAL. Diagnosis can be made by combining the results of clinical examination and intrathecal analgesia. Ultrasonographic evaluation is crucial and should include dynamic studies in which the digital flexor tendons and DFTS are evaluated for possible adhesions between tendons, DFTS, and the PAL. Concomitant conditions, such as OA of the fetlock joint, sesamoiditis, and demineralization of the PSBs at the medial and lateral attachments of the PAL, should be assessed radiologically. Initial management is to apply cold therapy and sweats and to administer NSAIDs. Decompression of the DFTS and injection of hyaluronan and corticosteriods then is followed by 3 weeks of stall rest. Tenoscopy is valuable in identifying horses with tendon tears and to perform adhesiolysis. Palmar annular desmotomy in horses with chronic desmitis or in those with chronic tenosynovitis may be helpful. Definitive therapy should be instituted early and aggressively to minimize adhesion formation.
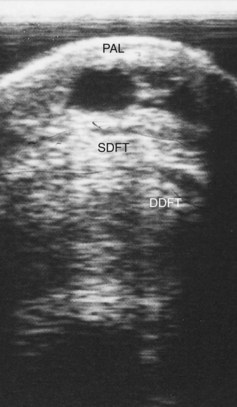
Fig. 119-14 Transverse ultrasonographic image of the distal palmar metacarpal region. An acute injury caused by direct trauma resulted in a chronically thickened palmar annular ligament and huge anechogenic areas within it. PAL, Palmar annular ligament; SDFT, superficial digital flexor tendon; DDFT, deep digital flexor tendon.
Desmitis of the Distal Sesamoidean Ligaments
Desmitis of the distal sesamoidean ligaments (bowed pastern) is seen occasionally in polo ponies and usually involves the straight sesamoidean ligament. Diagnosis is made by detecting pain and swelling, performing perineural analgesia (palmar nerve blocks at the base of the PSBs), and using ultrasonographic examination.
Polo ponies with recurrent injury may not resent palpation, and ultrasonographic examination is necessary to differentiate this from other injuries. Proliferative changes along the base of the PSBs and abaxial surface of the proximal phalanx (at the insertion of the oblique sesamoidean ligaments) are often seen. These injuries may be career ending and at best are performance limiting. Long-term rest for 6 months is often necessary. Numerous applications of shock wave therapy have shown promise, and some owners request pin firing as a last resort.
Carpal Region Lameness
The carpus is an uncommon source of lameness in the polo pony. Preexisting chronic radiological changes are often incidental findings, even in horses with reduced range of carpal flexion and mild effusion. Carpal chip fractures can occur, but they are unusual. Tearing of the medial palmar intercarpal ligaments can cause lameness. Transient traumatic carpitis occasionally is seen after direct trauma from a mallet or ball. Rupture of the carpal sheath is a rare cause of lameness in the polo pony; one author (PJM) has seen two horses with massive swelling in the distal aspect of the antebrachium, and ultrasonographic evaluation revealed rupture of the carpal sheath. Prognosis is not known.
Fractures of the proximal aspect of the splint bones can lead to OA of the carpometacarpal joint. Fracture of the medial splint bone is most serious, but polo ponies usually respond well to conservative management.
Horizontal and vertical fracture of the accessory carpal bone may occur after collapse or a fall. Ponies are occasionally hit on the forehead by a hard-struck polo ball, rendering them unconscious and causing the hind hoof to hit the back of the carpal region. Fracture can also occur if a horse trips inadvertently on a loose polo wrap. Prognosis appears to be indirectly proportional to fracture displacement. Treatment is conservative. Physiotherapy, forcing full carpal flexion, is helpful to restore normal mobility (SK). Tenosynovitis of the carpal sheath can occur primarily or after fracture of the accessory carpal bone and in ponies with tendonitis of the SDFT and DDFT, as well as in horses with desmitis of the accessory ligament of the SDFT, but this condition is rare.
Desmitis of the Accessory Ligament of the Superficial Digital Flexor Tendon
In the United Kingdom, between 10 and 15 polo ponies each year are diagnosed with desmitis of the accessory ligament of the SDFT, which may occur because of the fast and aggressive play of modern polo (PJM). Awareness of the condition and use of ultrasonography may have resulted in increased recognition.
One high-goal player had five horses with this problem in a single year. Diagnosis is made by eliminating the distal aspect of the limb as a source of pain, by palpating pain and swelling in the distal aspect of the antebrachium and in the carpal sheath, and by ultrasonographic assessment. Conservative management is usually successful, including the periligamentous injection of hyaluronan and corticosteroids. Surgical resection of the accessory ligament of the SDFT may be indicated, particularly in polo ponies with considerable fibrosis and bony proliferation on the caudal distal aspect of the radius or in those that stand over at the knee.
Upper Forelimb Lameness
Lameness associated with the antebrachium, elbow, and shoulder regions is uncommon in polo ponies. Occasionally, fractures of the radius or olecranon and wounds with bony sequestration occur from kick trauma. Repair of fractures of the olecranon has been successful. Shoulder region soft tissue trauma, fracture of the supraglenoid tubercle of the scapula, and suprascapular nerve injury occur occasionally from falls, dangerous play, or wrecks.
Other Hindlimb Lameness
The distal aspect of the hindlimb is subject to the same type of bony injuries as seen in the forelimb, with the exception of navicular disease. Fractures of the distal and proximal phalanges and PSBs occur with the same frequency as in the forelimb, but prognosis is better in the hindlimb. In the hindlimb, OA of the fetlock joint, SDF tendonitis, suspensory desmitis, and desmitis of the ALDDFT are not nearly as common as in the forelimb.
Two soft tissue problems occur specifically in the hindlimbs. A form of severe suspensory desmitis occurs in older polo ponies with exceedingly straight hock conformation. The hind fetlock joint drops, and the pastern region is parallel to the ground. However, lameness is often minimal, and despite the abnormal angle of the fetlock joint, these horses can continue to play for years with the help of support wraps. The second specific soft tissue injury of the hindlimb is spontaneous rupture of the common digital extensor tendon above the fetlock joint. This injury results in lameness and hyperflexion of the fetlock joint at the trot. These horses respond well to conservative management, with support wraps and rest, and prognosis is excellent.
Lameness from stifle injuries is uncommon. Osteochondrosis occasionally causes effusion and lameness or poor performance if present bilaterally. Collateral ligament injury may occur from severe bumps. Kick wounds to the tibial crest can cause pronounced lameness and may result in a fracture. Polo ponies with a history of poor stopping or turning ability respond favorably to injection of counterirritants (blisters) around the patellar ligaments and the insertion of the vastus lateralis and rectus femoris muscles. Horses are kept in a working schedule following these injections and typically may be played successfully several days later.
Pelvic injury in polo ponies is infrequent but may result from dangerous play, such as a high-angle ride off behind the saddle (SK), and is best diagnosed using scintigraphy. Stress fractures of the ilium and traumatic fracture of the acetabulum occur but are rare. Disparity in height of the tubera sacrale often is seen, but with no effect on performance.
Rhabdomyolysis
Rhabdomyolysis, or tying up, is fairly common, especially in mares. Two types of horses are predisposed to this syndrome. Unfit horses placed into work too rapidly often develop a stiff gait at the trot and tenderness to palpation over the dorsal musculature. Muscle enzyme levels are only moderately elevated, and horses respond well to rest and NSAIDs. The most common form of rhabdomyolysis is seen in fit polo mares after an extended layup period for illness, unrelated lameness, or foul weather that prevents horses from being played regularly. Rhabdomyolysis can also occur on cold, clear mornings or blustery days during which a decrease in barometric pressure occurs. Horses generally become affected after exercise (when they return to the barn or trailer), are reluctant to move, and have firm, tight gluteal regions. Epaxial muscles rarely are involved. Clinical signs may be confused with colic because horses with rhabdomyolysis often paw, stretch out, and sweat profusely. Muscle enzyme levels are elevated greatly. Management is similar to that described for other sports horses (see Chapter 83). Nutritional management appears to be important in Europe, where bran, which is high in phosphorus (reduces calcium), is fed to reduce recurrence.
Gracilis Muscle Tear
Gracilis muscle tears are seen in several polo ponies each year and are characterized by lameness at the trot and dramatic swelling in the medial thigh region. Abduction of the flexed hindlimb elicits a painful response, and a large hematoma generally develops soon after the injury. The administration of NSAIDs and DMSO intravenously, and the topical application of cold water are beneficial. If necessary, seroma fluid can be drained surgically 5 to 7 days after injury, and exercise is limited for a minimum of 2 weeks.
Equine Protozoal Myelitis
Mild neurological signs typical of equine protozoal myelitis (EPM) or lameness associated with the disease can be confused with other causes of musculoskeletal pain, in particular hindlimb lameness. EPM is prevalent in the United States but is rare in England (PJM). Occasionally, a polo pony in the United Kingdom that was imported from the United States develops clinical signs consistent with EPM under the stress of the latter half of the season.