Chapter 10 Diagnostic Analgesia
Despite the many technological advances in equine sports medicine over the past three decades, diagnostic analgesia arguably remains the most valuable tool in the equine clinician’s arsenal to localize pain causing lameness. Although the technique requires a thorough understanding of anatomy, basic technical skill, and clinical experience, the equipment and expense are minimal. In addition, diagnostic analgesia can be performed on site, with the outcome immediately obvious. Any lingering concern that a suspected “shoulder problem” exists is convincingly erased when the response to perineural analgesia of the digit is observed. This chapter reviews the various perineural, intrasynovial, and local (regional) infiltration techniques for application of local analgesia in the diagnosis of lameness in horses.
Local Anesthetics: Pharmacology and Tissue Interactions
Pain is transmitted specifically in the small, lightly myelinated, A delta and nonmyelinated C nerve fibers.1 All commonly used local anesthetic solutions, regardless of the specific molecular structure, share the same basic mechanism of action—specifically, the ability to block or inhibit nociceptive nerve conduction by preventing the increase in membrane permeability to sodium ions.2 These agents consist of a lipophilic and a hydrophilic group, connected by an intermediate chain containing a carbonyl group of an amide or ester linkage, and have traditionally been categorized as either amide- or ester-type local anesthetics.3 Common local anesthetic solutions used in horses—2% solutions of lidocaine, mepivacaine, and bupivacaine—are of the amide type.
Compared with most local anesthetics, lidocaine and mepivacaine are considered relatively fast-acting and have a reported duration of action of  to 3 hours and 2 to 3 hours, respectively. In contrast, bupivacaine is intermediate in onset but has a much longer duration of action (3 to 6 hours).4 Bupivacaine is most suited for providing therapeutic rather than diagnostic analgesia. The results in clinical practice vary, because in severely lame horses the degree and duration of local analgesia are decreased, regardless of the agent used.
to 3 hours and 2 to 3 hours, respectively. In contrast, bupivacaine is intermediate in onset but has a much longer duration of action (3 to 6 hours).4 Bupivacaine is most suited for providing therapeutic rather than diagnostic analgesia. The results in clinical practice vary, because in severely lame horses the degree and duration of local analgesia are decreased, regardless of the agent used.
When local anesthetic solutions are injected, tissue damage can occur but is extremely rare.3,4 Soft tissue swelling occurs occasionally and is likely caused by needle trauma or hematoma formation and not from a direct drug-tissue interaction. We suggest that alcohol and a clean wrap be applied to the injection sites when the diagnostic evaluation is complete to prevent or minimize swelling at injection sites. Cellulitis or other forms of infection are rare potential complications.
Acute synovitis, or flare, is a rare complication that can occur after intrasynovial (most commonly intraarticular) injection of local anesthetic solutions. Synovitis from intrasynovial injection of local anesthetic solution is much less common than from injection of other medications. Mepivacaine is thought to be less irritating than lidocaine when administered intraarticularly, but we have not recognized this difference.3 However, Dyson reported that lidocaine may be considerably more irritating than mepivacaine, and clinical data documenting differences were used successfully in the licensing of mepivacaine in the United Kingdom.5 Like cellulitis after perineural injections of local anesthetic solutions, infectious synovitis is a rare but possible sequela. To mitigate the possibility of contaminated solution, we use a new vial of local anesthetic solution when performing intrasynovial analgesic procedures.
Systemic side effects from diagnostic analgesic techniques are exceedingly rare. Cardiovascular or central nervous system signs, including muscle fasciculation, ataxia, and collapse, were reported.3 Systemic intoxication would require a dose much higher than is commonly used, even for an extensive diagnostic evaluation. For example, the maximum single infiltration dose of lidocaine that can be safely administered to a 500-kg horse is about 6.0 g, or 300 mL of a 2% solution.6
Strategy, Methodology, and Other Considerations
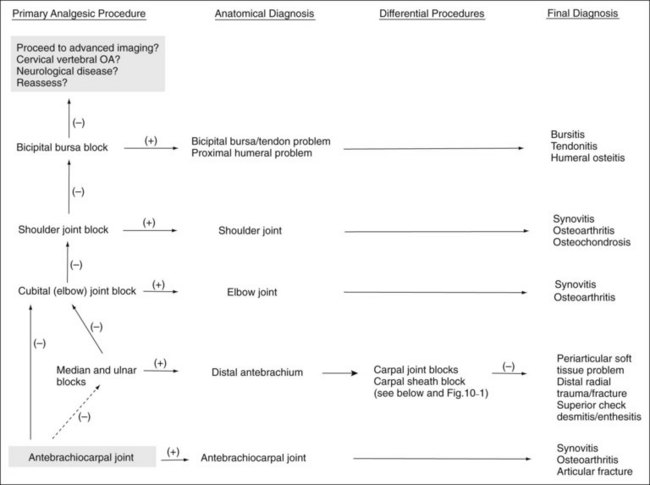
A few basic principles must be followed to ensure success. A thorough working knowledge of regional anatomy is required. Even for seasoned veterans a review of anatomy may be required before less common techniques are performed. A most important principle when performing perineural analgesia is to start distally in the limb and work proximally (Figures 10-1 to 10-4). If possible, sequential blocks from distal to proximal should always be used, but in certain circumstances a different strategy can be successful. Sequential blocking requires a fair amount of time, and in certain horses, selective intraarticular or local blocks can be performed without following this “golden rule.” However, in most situations, blocking a large portion of the distal limb at a proximally located site may preclude accurate determination of the source of pain causing lameness and may require an additional visit to perform additional diagnostic procedures.
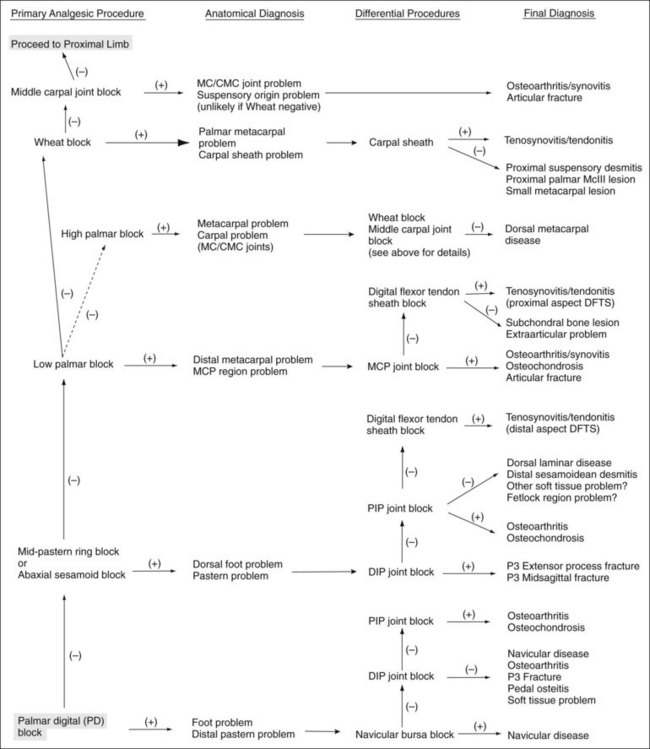
Fig. 10-1 Blocking strategy in the forelimb: foot to carpus. CMC, Carpometacarpal; DFTS, digital flexor tendon sheath; MC, middle carpal; McIII, third metacarpal bone; MCP, metacarpophalangeal; P3, distal phalanx; PIP, proximal interphalangeal.
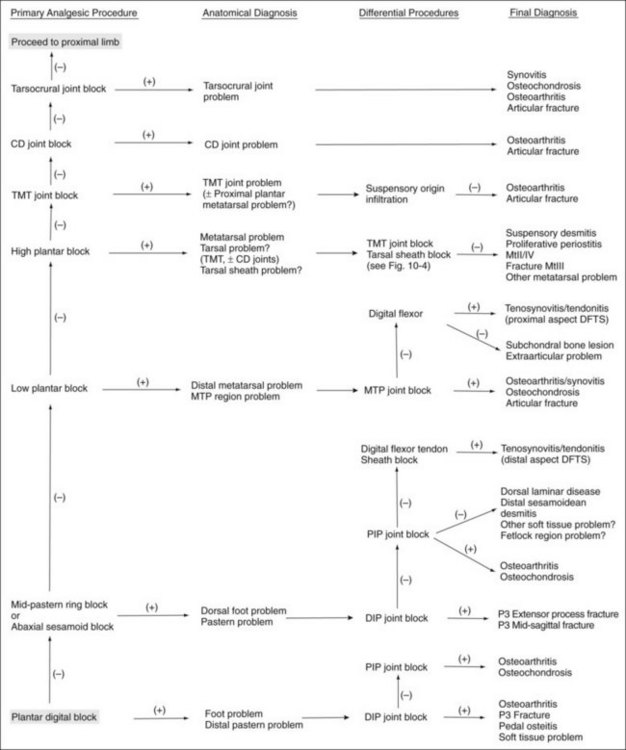
Fig. 10-3 Blocking strategy in the hindlimb: foot to hock joint. CD, Centrodistal; DFTS, digital flexor tendon sheath; DIP, distal interphalangeal; MtII, MtIII, MtIV, second, third, and fourth metatarsal bones, respectively; MTP, metatarsophalangeal; P3, proximal phalanx; PIP, proximal interphalangeal; TMT, tarsometatarsal.
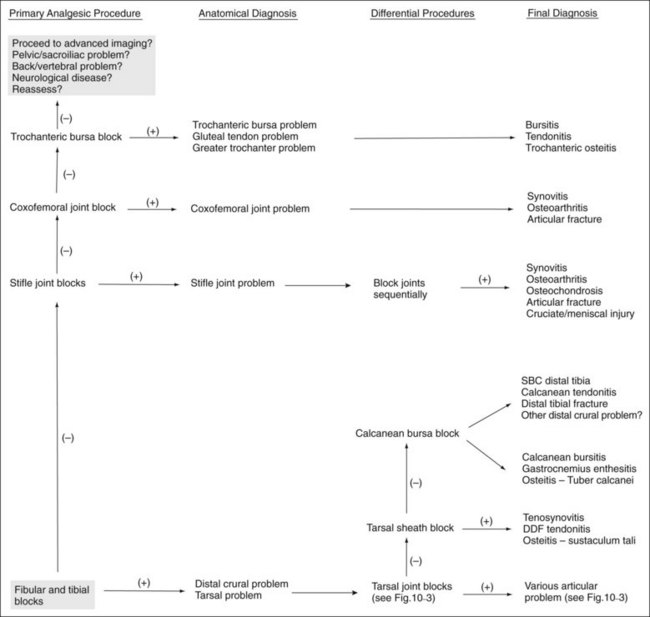
Fig. 10-4 Blocking strategy in the hindlimb: crus to coxofemoral joint. DDF, Deep digital flexor; SBC, subchondral bone cyst.
It is important to test the efficacy of a perineural block before reevaluating the horse’s degree of lameness. If any question exists, the block should be repeated rather than assuming deep pain has been abolished, when skin sensitivity persists. If a horse shows partial improvement only minutes after injection, an additional few minutes should be allowed for complete analgesia to be achieved before proceeding with the next block. Alternatively, the block can be repeated. In so doing, the clinician minimizes the potential for misinterpretation and the tendency to ascribe the residual lameness to a “second problem” that does not exist.
During this portion of the examination, we are attempting to eliminate baseline rather than induced lameness, and care must be taken when adopting the practice of “blocking out a positive flexion test” (see Chapter 8). Once baseline lameness has been eliminated, we rarely perform additional flexion tests or attempt to eliminate all induced lameness.
How is the efficacy of the block assessed? Several methods are available, but the following points should be considered. Individual horses react differently to noxious stimuli applied to the skin. Therefore it is helpful to test the contralateral (unblocked) limb to establish the horse’s baseline response to the test. Similarly, covering a horse’s eye or feigning a few gestures with an instrument (pen tip, hemostatic forceps) without actually contacting the skin can help differentiate between a random or anticipatory response by an apprehensive horse and a true painful response. Positioning oneself on the contralateral side of the horse when testing for sensation also can help in making this determination. The clinician should avoid using sharp instruments that can penetrate the skin and cause hemorrhage, a situation not well understood by a concerned horse owner. Hemostatic forceps, used to pinch the skin, are ideal, because they are blunt and appear to consistently induce an appropriate amount of pain. Forceps are only useful in assessing superficial or skin sensation, however.
Perineural blocks must be assessed for the amelioration of deep and not just superficial pain. To assess whether deep pain in the hoof has been ameliorated after palmar digital analgesia or other techniques, hoof testers can usually be applied with enough force to cause a painful response, even in the most stoic of horses. Physical strength of the operator must be considered. Extreme or hard joint flexion (combined with varus or valgus stress) can be used to assess whether deep pain has been abolished in more proximal locations. In some instances, however, it is impossible to avoid contacting the skin proximal to the site of local anesthetic administration, leading the clinician to assume that the block has not worked. The application of firm digital pressure in the blocked area may be a viable alternative to flexion or manipulation to help avoid these potentially confounding factors.
It is important to understand that the region of the limb that is actually desensitized may, in fact, differ from the region the clinician intended to desensitize.7 Proximal diffusion of local anesthetic solution appears to be the most likely cause, but other, intangible factors may play a role. Using a small volume of local anesthetic solution (1 to 5 mL for most perineural blocks) can minimize but not abolish this phenomenon. To further minimize the potential for diffusion of local anesthetic solution, the horse should be reevaluated no more than 10 minutes after the injection (exceptions apply in certain situations). A recent study using 2 mL of radiopaque contrast medium injected perineurally around the palmar nerves at the level of the proximal sesamoid bones demonstrated proximal diffusion extending 2 to 3 cm within 10 minutes of injection, irrespective of whether horses stood still or walked.8
Complete analgesia, and thus 100% improvement in lameness score, is the goal when performing diagnostic analgesia, but in many horses this level of pain relief is never achieved. Improvement in degree of lameness greater than 70% to 80% after most perineural or intraarticular techniques should be considered a positive response in most horses. The quintessential response is that the horse “switches lameness” to the contralateral limb, indicating that now pain arising from the opposite limb is greater than the pain that caused the baseline lameness. However, complete response may not occur, and the clinician must decide when to stop sequential blocks or when the horse has “blocked out.” The clinician hopes for an obvious difference in lameness score when the horse is blocked, but in some horses, serial improvement occurs with each successive block, a situation that makes assessing the primary source of pain difficult.
Incomplete response to local analgesia in some horses may be explained by the fact that chronic pain, particularly deep bone pain, may remain resistant to complete analgesia when perineural techniques are used. For example, horses with laminitis tend to remain lame despite blocking many times at the appropriate level, probably because of neuropathic pain.9 Mechanical gait deficits do not improve after diagnostic analgesia because pain is minimal. Horses may continue to show lameness even with pain abolition, a situation that appears to be caused by habit. These horses tend to show mild residual lameness initially, only to warm out of it quickly during examination. Other factors affecting response to diagnostic analgesia include individual variation in neuroanatomy, the intermittent nature of certain lameness conditions, and the inherent difficulty in assessing and abolishing pain in horses with subtle lameness.10 Articular and subchondral bone lesions may not be desensitized by intraarticular analgesia, and pain may be more effectively abolished using perineural techniques.
Sensory innervation of joints is complex and involves three classes of neurons that transmit information from four receptor types, each of which has a specific distribution throughout the joint.11-13 Articular pain can arise from several sources, including the synovium (inflammation, effusion), fibrous joint capsule (increased intraarticular pressure), articular and periarticular ligaments, periosteum, and subchondral bone (injury, osseous vascular engorgement).10,12,14,15 Other than small branches in the perichondrium, articular cartilage is devoid of innervation. In osteoarthritic joints, however, erosion channels, formed in the calcified layer of cartilage, are invaded by subchondral vasculature.12 Putative nociceptive neurotransmitters were identified in these areas, and therefore it is plausible that in horses with advanced osteoarthritis, pain could be emanating from the deep cartilage layers.16,17
On occasion, lameness from an articular lesion abates after perineural analgesia but shows minimal or only partial response after intraarticular analgesia. In some horses, this can be explained by the fact that pain is originating from articular and periarticular tissues.8 Subchondral bone pain—caused by maladaptive bone remodeling, cystic or erosive lesions, incomplete fractures, and osteoarthritis—is inconsistently abolished by intraarticular analgesia. In fact, subchondral bone pain is abolished much more consistently by perineural techniques. Subchondral bone receives innervation from endosteal branches of peripheral nerves that enter the medullary cavity through the nutrient foramen.10,11,18,19 Intraarticularly administered local anesthetic solutions may not penetrate subchondral bone sufficiently to completely block these nerves. This shortcoming is presumably even more likely in situations in which the cartilage is intact.
Unfortunately, intraarticular analgesia, although easier to perform, inconsistently abolishes pain from many of the common articular problems. This fact, however, is either overlooked or misunderstood by many practitioners. Whenever possible, perineural analgesia should be performed, particularly in the distal aspect of the limbs, because this type of analgesia more consistently abolishes pain from all aspects of the joint and surrounding soft tissue structures.
Lameness Is Worse after Diagnostic Analgesia
Two uncommon situations arise when performing diagnostic analgesia. The first occurs during a blocking session. After performing palmar digital analgesia in a horse with forelimb lameness, lameness score may worsen by one or two grades. In fact, lameness may occasionally be considerably worse, prompting concern by the lameness diagnostician. Why? This unusual response occurs most commonly in horses with proximal, palmar metacarpal pain caused by proximal suspensory desmitis, avulsion fracture of the proximal palmar aspect of the third metacarpal bone (McIII), or proximally located superficial digital flexor tendonitis. Horses normally shorten the cranial phase of the stride to protect a source of pain, a common response by any lame horse. We reason that after palmar digital analgesia a lack of proprioception in the digit prompts the horse to take a somewhat longer stride, increasing the cranial phase. Compared with before the block an exaggerated load causes the horse to display a higher lameness score. Temporary exacerbation of lameness after palmar digital analgesia can be a useful characteristic to help determine the genuine source of pain.
The second situation is more ominous. A horse will occasionally be very lame, sometimes non–weight bearing, once a block wears off. This unusual, but important and sometimes difficult situation occurs when incomplete fractures become separated, displaced, or comminuted. Horses with fractures of the distal phalanx that are incomplete or have healed partially by a fibrous union or those with incomplete fractures of the proximal phalanx appear most at risk. Horses at risk are candidates for imaging before blocking, but in some this complication is unforeseen (see following discussion).
Perception of Diagnostic Analgesia by Laypersons
One of the intangible factors that can complicate the lameness examination is the layperson’s perception of diagnostic analgesia or nerve blocking. In many instances the opportunity for an owner or trainer to observe the outcome of diagnostic analgesia provides the concrete evidence that finally convinces him or her of the diagnosis. The classic example is the suspected acute shoulder injury that is actually chronic navicular disease. However, for many reasons, misunderstanding about diagnostic analgesia can lead to frustration for everyone involved. Many laypersons are not fully able to recognize the baseline lameness and therefore may not be capable of seeing that the horse’s lameness improves after the block. Another difficulty is trying to explain why lameness in a horse with an articular problem is better after a perineural block but no better when local anesthetic solution is placed directly into a joint. Similarly, many laypersons do not understand why a horse with an articular lameness may “block sound” but does not respond satisfactorily to therapeutic injection. This finding that a horse blocks sound but does not “inject sound” is quite common in young racehorses with subchondral bone pain. Most experienced practitioners have learned to deal with these issues, but the new graduate may need fortitude and ingenuity when explaining the results of diagnostic analgesia.
Role of Chemical Restraint
Whenever possible, use of physical (nose or shoulder twitch) rather than chemical restraint is best when diagnostic analgesia is performed. This is particularly important in horses with low-grade lameness. The analgesic properties of α2-agonists (e.g., xylazine, detomidine) and synthetic opiates (e.g., butorphanol) are well recognized and may lead to false-positive results. Ataxia after sedation can complicate lameness interpretation. However, in some horses mild sedation or tranquilization may be necessary for performance of diagnostic analgesia and may improve the clinician’s ability to evaluate the baseline lameness. Acetylpromazine (0.02 to 0.04 mg/kg intravenously) can calm a highly strung horse and facilitate the lameness examination. Extra care must be taken when performing hindlimb procedures, and the safety of everyone involved and the horse must be considered. In horses with moderate or severe lameness, xylazine (0.15 to 0.30 mg/kg intravenously) may not interfere appreciably with lameness interpretation. Similarly, extremely fractious horses can be sedated with an α2-agonist, which then is reversed with the prescribed α2-antagonist (e.g., yohimbine) before reevaluation. Alternatively, sedation can simply be allowed to wear off before the horse is evaluated, but diffusion of local anesthetic solution may occur or the effect may wear off, both of which may potentially cause misinterpretation of results.
Horse Preparation
Before perineural analgesia is performed, the skin and hair should be cleaned of any gross debris such as mud, bedding, feces, or poultice. Clipping usually is not necessary unless the hair coat is long and prohibits accurate palpation of anatomical landmarks or adequate cleaning of the site. The site should then be scrubbed with an antiseptic, such as povidone-iodine or chlorhexidine, using clean gauze sponges or cotton. If the clinician has any concern about inadvertent penetration of a synovial cavity, a 5-minute aseptic preparation should be performed. This is followed by isopropyl alcohol administration over the site using cotton or gauze sponges.
Aseptic preparation should always be performed before any intrasynovial injection. Considerable debate and variation exists among clinicians regarding the need to clip the hair over the site. Some clinicians always clip the hair, whereas others never do. Still others shave the hair in a small area directly over the injection site. The results of a study indicated no significant difference in the number of postscrub colony-forming units (bacterial flora) between clipped and unclipped skin over the distal interphalangeal (DIP) and carpal joints.20 Nonetheless, we still clip the hair over all proposed intrasynovial injection sites before undertaking a 5-minute aseptic preparation. The only time we deviate from this policy is when we are specifically asked not to clip the hair, a situation that arises in some sports horses actively competing, in claiming horses, or in those being sold.
Similar variation among clinicians exists regarding wearing of sterile latex gloves when performing an intrasynovial injection. However, we recommend wearing sterile gloves during these procedures. Science aside, clipping hair and wearing sterile gloves project a positive impression to all in attendance.
How does, or should, the practitioner attempt perineural or intrasynovial analgesia in a horse with contact or chemical dermatitis (scurf) over the proposed injection site? A superficial wound or abrasion with a localized infection presents a similar quandary. For obvious reasons, these areas are difficult, if not impossible, to clean effectively. If possible, an alternative site, away from the area of dermatitis, should be used. If not, then the procedure should be delayed until the skin condition (or wound) has resolved. In many instances, dermatitis can be treated with topical medications (medicated sweats such as nitrofurazone-dimethylsulfoxide) for a few days to facilitate resolution of the problem.
Injection Techniques
Perineural injections are typically performed using needles ranging in size from 25 gauge, 1.6 cm ( inch) to 20 gauge, 2.5 or 4 cm (1 to
inch) to 20 gauge, 2.5 or 4 cm (1 to  inches). Small needles cause less pain but carry the risk of breaking off within tissues if the horse kicks out or otherwise misbehaves. For this reason, we recommend using 18- or 19-gauge needles for injections or blocks within the proximal metatarsal or plantar tarsal regions. In the distal aspect of the limb the needle is inserted subcutaneously directly over and parallel to the nerve. We generally direct the needle proximally rather than distally, although this portion of the procedure differs among clinicians. One of the Editors (SJD) always inserts the needle distally; if a fractious horse throws the limb to the ground the needle is more likely to stay in situ, and the remainder of the procedure may be completed with the limb on the ground. Directing the needle distally also ensures more distal placement of the local anesthetic solution, which may be important at distal sites. The needle is inserted before the syringe is attached. To avoid excessive manipulation once the needle is inserted, a slip-type syringe hub is preferred. Syringes with screw-on hubs can be difficult to attach, requiring additional manipulation in a sometimes fractious horse, and are not generally used. However, when dense tissue requires that additional force be used for injection, the seal between the hub and the needle can be broken, a complication minimized by using a screw-on hub (see the following discussion of lateral palmar block).
inches). Small needles cause less pain but carry the risk of breaking off within tissues if the horse kicks out or otherwise misbehaves. For this reason, we recommend using 18- or 19-gauge needles for injections or blocks within the proximal metatarsal or plantar tarsal regions. In the distal aspect of the limb the needle is inserted subcutaneously directly over and parallel to the nerve. We generally direct the needle proximally rather than distally, although this portion of the procedure differs among clinicians. One of the Editors (SJD) always inserts the needle distally; if a fractious horse throws the limb to the ground the needle is more likely to stay in situ, and the remainder of the procedure may be completed with the limb on the ground. Directing the needle distally also ensures more distal placement of the local anesthetic solution, which may be important at distal sites. The needle is inserted before the syringe is attached. To avoid excessive manipulation once the needle is inserted, a slip-type syringe hub is preferred. Syringes with screw-on hubs can be difficult to attach, requiring additional manipulation in a sometimes fractious horse, and are not generally used. However, when dense tissue requires that additional force be used for injection, the seal between the hub and the needle can be broken, a complication minimized by using a screw-on hub (see the following discussion of lateral palmar block).
Volume of local anesthetic solution varies, but for a majority of blocks in the distal limb, 1 to 5 mL is injected at each site. Larger volumes are used to perform the median and ulnar or fibular (peroneal) and tibial techniques and when infiltrating the proximal palmar (plantar) metacarpal (metatarsal) region. After injection, we briefly massage the sites with gauze sponges or clean cotton soaked in alcohol. Skin sensation and deep pain are assessed 5 to 10 minutes after injection. More time is allowed under certain circumstances (see specific comments throughout the chapter). At the completion of the examination an alcohol wrap should be applied to minimize swelling, a common sequela resulting from local irritation and bleeding from nearby vessels.
For “ring” blocks, circumferential subcutaneous infiltration of local anesthetic solution, and other local or regional infiltration techniques, we most commonly use 20- to 22-gauge, 4-cm needles. For performance of a ring block, the needle is inserted perpendicular to the long axis of the limb, and local anesthetic solution is injected as the needle is advanced, leaving a clearly visible wheal or subcutaneous bleb in most locations. The needle then is reinserted at the leading edge of this wheal, a practice that minimizes the number of injections and the horse’s discomfort. However, most horses object to needle insertion even when it is performed well within the bleb. The injection is continued around the limb in this manner. For most ring blocks in the distal limb, 10 to 15 mL of local anesthetic solution is used, but larger volumes may be preferred for surgical procedures. Ring blocks can be done as a substitute for or in combination with perineural injections (see the specific blocking techniques discussed in the chapter). However, simply placing local anesthetic solution in a subcutaneous location is not a substitute for the preferred approach, direct perineural injection.
To block a local area such as a splint or curb, the needle is typically inserted in one or two locations, and local anesthetic solution is deposited in a fan-shaped pattern. As with the perineural analgesia, the sites are massaged briefly and the horse is reevaluated in 5 to 10 minutes.
Intrasynovial injections typically are performed using needles ranging in size from 22 gauge, 2.5 cm to 18 gauge, 4 cm. If marked effusion is present, drainage of synovial fluid is advised, either by allowing the fluid to drip from the hub of the needle or by aspirating with a sterile syringe before proceeding with injection. We prefer the former procedure unless fluid analysis is necessary. The manipulation required to attach the syringe may cause the horse discomfort and potentially dislodge the needle but if successful may hasten withdrawal of synovial fluid. Brief evaluation of the color and viscosity of synovial fluid can shed some light on the disease process within and is expected practice among most racehorse trainers. Volume of local anesthetic solution varies considerably between synovial cavities, but the clinician should keep in mind that small volumes might contribute to a false-negative result. False-negative results are common in horses with severe osteoarthritis, and larger volumes of local anesthetic solution should be used. We routinely spray or wipe antiseptic solution over the injection site. After the examination a light bandage is applied over the injection sites from the metacarpophalangeal or metatarsophalangeal joint, distally. Initial reevaluation is done 5 to 10 minutes after injection. Additional evaluations may be necessary depending on the response during the initial time period. General practice is to have the horse walked in hand or with a rider after perineural or intrasynovial analgesia is administered, a procedure thought to hasten distribution of local anesthetic solution and potentially improve success. Excessive diffusion of local anesthetic solution is a potential drawback to this practice, particularly with techniques such as DIP or middle carpal analgesia (see the following discussion), although it would be a complication difficult to quantify.
Another issue to consider when performing diagnostic analgesia is whether riding or driving a horse after blocks have been performed is safe. In general, riding on the flat or driving a horse at slow speed after any of the common blocks have been performed is safe. Stumbling or knuckling can be a concern after upper limb perineural techniques, such as the median and ulnar and fibular (peroneal) and tibial techniques. Common sense should prevail, however, with regard to the horse and rider negotiating fences or performing at high speed. Horses at risk for lameness from stress or incomplete fracture are candidates for imaging before evaluation at speed after diagnostic analgesic techniques have been performed. Moreover, horses suspected of having incomplete fractures but with negative or equivocal radiological findings may best be managed conservatively without use of analgesic techniques and should undergo either follow-up radiographic examination in 10 to 14 days or scintigraphic examination.
Perineural Analgesia in the Forelimb
Palmar Digital Analgesia
Palmar digital analgesia (or palmar digital block) is the most common diagnostic analgesic procedure performed. The medial and lateral digital neurovascular bundles, consisting, in a dorsal to palmar direction, of the digital vein, artery, and nerve, course in an abaxial location to the digital flexor tendons. With the exception of small breeds or draft horses with remarkably long-haired pasterns (feathers), the palmar digital nerve is easily palpable between the proximal sesamoid bones and the cartilages of the foot. The palmar digital block can be performed with the horse in a standing position or with the limb held off the ground. We prefer the latter. If held by an assistant, the limb should be grasped in the midmetacarpal region, with the fetlock and digit hanging in neutral position. The palmar digital nerve is easily palpated in this extended position on the lateral aspect of the deep digital flexor tendon (DDFT). Alternatively, the clinician performing the block can hold the limb, a technique that requires practice. The clinician can stand facing backward with a hand grasping the midpastern region or can stand behind the limb and clutch the hoof between both legs.
A 25-gauge, 1.6-cm needle is inserted subcutaneously, directly over the nerve, just proximal to the cartilages of the foot (Figure 10-5). One of us (LHB) directs the needle in a distal direction, whereas the other (MWR) directs the needle in a proximal direction to avoid deeper penetration or laceration of digital vessels if the horse withdraws the limb. Alternatively, a 22-gauge, 4-cm needle can be inserted on the palmar midline in the midpastern region, and local anesthetic solution is then infiltrated in a V-shaped pattern. This modification of the palmar digital block is quite difficult to perform in the hindlimb but when done in the forelimb provides maximal analgesia to the bulbs of the heel and minimizes the potential for depositing local anesthetic solution dorsal to the nerve. Loss of skin sensation in the midline between the bulbs of the heels should be assessed, because this area seems most recalcitrant to palmar digital analgesia. Deep pain is assessed using hoof testers. However, if skin sensation persists, it is still worth reevaluating lameness, because in some horses deep pain and lameness may be abolished despite the persistence of skin sensation.
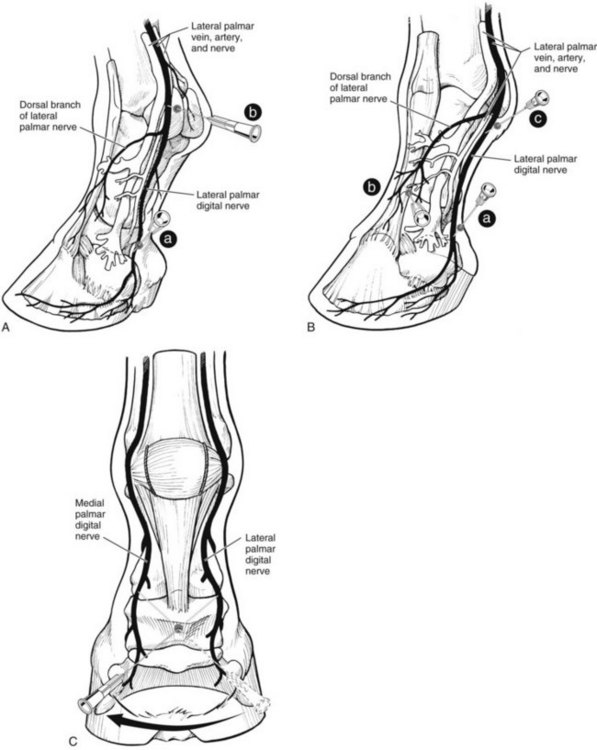
Fig. 10-5 A, Palmarolateral view of the distal aspect of the limb showing site for needle penetration for palmar (plantar) digital analgesia (a). The clinician directs the needle as shown or in a proximal direction. The palmar (plantar) digital nerve is blocked more proximally at the level of the abaxial surface of the proximal sesamoid bone (b). At this level the palmar (plantar) digital nerves and dorsal branches are both blocked. B, Dorsolateral view of the distal aspect of the limb demonstrating needle positions for palmar (plantar) digital analgesia (a) with an additional dorsally directed subcutaneous ring block to desensitize the dorsal aspect of the pastern region and foot (b). A block at the base of the proximal sesamoid bone (c) likely desensitizes the palmar (plantar) digital nerves and dorsal branches of the digital nerve (note close association of both branches to the site of the block) and provides the same region of analgesia as does the palmar digital block with the dorsal ring, or the abaxial sesamoid block. C, Alternative technique used for the palmar digital nerve block. The clinician inserts the needle on the palmar midline and places a line of local anesthetic solution in a proximal dorsal direction to the level of each of the medial and lateral palmar nerves in an approximately V-shaped pattern. This technique confines local anesthetic solution to the palmar aspect of the limb. This blocking technique is difficult to perform in the hindlimb.
Traditionally the palmar digital block was felt consistently to desensitize only the palmar (plantar) one third to one half of the foot.21 However, in clinical practice, this block desensitizes 70% to 80% of the foot. Most of the DIP joint is affected, with the exception of the proximodorsal aspect. Horses with fractures of the extensor process of the distal phalanx or injury of a collateral ligament of the DIP joint may show partial improvement after palmar digital analgesia, however. Our clinical observations have been substantiated in a recent study. Setscrews were placed near the medial and lateral aspects of the toe to simulate pain from the sole. Lameness in these horses was abolished using palmar digital analgesia performed just proximal to the heel bulbs.22
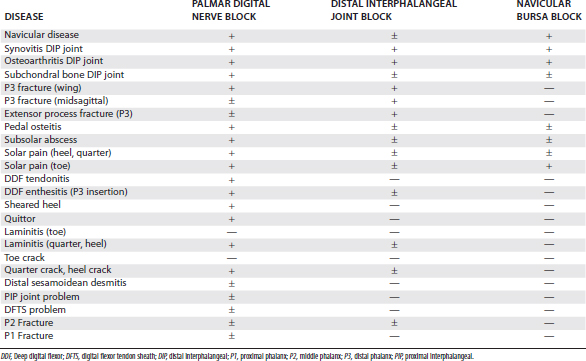
Classically, most horses that responded positively to palmar digital analgesia were thought to have navicular syndrome, but this block desensitizes many lameness conditions within and outside the hoof capsule (Table 10-1). This is an important and common misconception. Lameness in horses with proximal interphalangeal joint pain, midsagittal fracture of the proximal phalanx, or other conditions involving the fetlock joints can be abolished using palmar digital analgesia.7,23 Although using small volumes of local anesthetic solution and performing the block just above the cartilages of the foot may help to minimize the area of analgesia, these procedures do not prevent inadvertent diagnosis in some horses. Diffusion of local anesthetic solution is the most likely explanation, and even a small volume can readily spread in a proximal direction, but the normal anatomy of the digit prevents distal placement of local anesthetic solution (Figure 10-6).

Fig. 10-6 Radiograph showing palmar digital analgesia performed with positive contrast material. The clinician performed palmar digital analgesia as far distal as possible, but the injection site is still at the level of the proximal interphalangeal joint, explaining why palmar digital analgesia desensitizes most of the foot and the pastern region in some horses.
The concept that palmar digital analgesia abolishes lameness in an area considerably more than the palmar (plantar) one third of the foot appears to be difficult for many to accept. Although results of studies are widely published and this finding has been emphasized at international meetings, most veterinary students still graduate today armed with this common misconception. Diffusion of local anesthetic solution easily explains why lameness conditions in the proximal aspect of the pastern or fetlock regions are desensitized by palmar digital analgesia. But what about the innervation of the hoof itself? Skeptics should consider the anatomy of the palmar digital nerve. Most practitioners have severed the palmar digital nerve while performing neurectomy. Can the clinicians recall any instance of having identified a large dorsal branch, or for that matter, any branching of the nerve at all? The lack of nerve branches in the midpastern region is circumstantial evidence that important innervation to the structures located dorsally within the hoof capsule occurs farther proximally (ill-defined dorsal branches) or after the nerve courses deep to the cartilages of the foot. It makes little sense that ill-defined dorsal branches would innervate the dorsal two thirds of the foot, leaving the robust palmar digital nerve to innervate only the palmar one third. When carefully dissected the palmar digital nerves can be seen branching extensively deep to the cartilages of the foot, sending branches dorsally to innervate the dorsal portions of the foot.
Accurately quantifying the contribution of the palmar digital nerve to the innervation of the foot or, for that matter, the exact percentage of structures desensitized by palmar digital analgesia may be impossible. Clinical experience will undoubtedly convince practitioners of the broad nature of palmar digital analgesia. Finally, it is imperative to develop expertise in diagnostic imaging of the entire digit, because the many lameness conditions affected by palmar digital analgesia require detective-like differential diagnostic skills.
Midpastern Ring Block
Traditionally the diagnostic blocks performed after palmar digital analgesia are the basisesamoid or abaxial sesamoid techniques. The basisesamoid block provides little additional information compared with palmar digital analgesia, unless, of course, the dorsal branch, originating from the digital nerve at the level of the proximal sesamoid bones, is blocked. If, however, the dorsal branch is blocked, then the basisesamoid block is in reality an abaxial sesamoid block. For this reason, we rarely perform the basisesamoid block. When performing the abaxial sesamoid technique in racehorses, or, for that matter, in any sport horse with a propensity to develop lameness of the metacarpophalangeal or metatarsophalangeal joints, the veterinarian runs the risk of an additional misdiagnosis. When local anesthetic solution is deposited in a location abaxial to the proximal sesamoid bones, pain from the metacarpophalangeal or metatarsophalangeal joints can be inadvertently blocked, explained most likely because of diffusion of local anesthetic solution, leading the clinician to assume the horse has a problem in the foot or digit, but in reality the pain originated from these joints. For these reasons, we prefer to use a blocking sequence as follows: palmar digital nerve, followed by a dorsally directed subcutaneous ring block, followed by the low palmar or plantar block.
The midpastern ring block affects the dorsal branches of the digital nerves and desensitizes any remaining areas of the foot and pastern region that were not affected by palmar digital analgesia. In most horses this includes the dorsal 20% of the foot (dorsal laminar and extensor process regions of the distal phalanx) and the dorsal pastern region (dorsal aspects of the middle phalanx and proximal interphalangeal joint, and distal portions of the proximal phalanx). Although desirable, performing the dorsal ring block just above the cartilages of the foot usually is not possible. Instead the block is performed at the level of the midpastern region.
A 20- to 22-gauge, 4-cm needle is used to deposit subcutaneously 10 to 12 mL of local anesthetic solution, beginning near the injection site used for palmar digital analgesia over the lateral neurovascular bundle and continuing dorsally and medially, ending over the medial neurovascular bundle (see Figure 10-5). Resistance to needle advancement and injection of local anesthetic solution will invariably be encountered dorsally, if the block is done just proximal to the coronary band, because of the dense tissue (proximal interphalangeal joint capsule, extensor branches of the suspensory ligament, and extensor tendons). Performing the block in the midpastern region minimizes this problem and mitigates the potential for inadvertent penetration of the proximal interphalangeal joint.
Abaxial Sesamoid Block
Desensitizing the medial and lateral palmar nerves at the level of the proximal sesamoid bones is commonly referred to as the abaxial sesamoid block but may provide the same information as the basisesamoid block, if the dorsal branch of the palmar digital nerve is blocked. To avoid redundancy, we rarely perform the basisesamoid technique before progressing to the abaxial sesamoid block (see previous comments). A block done at this level essentially provides analgesia of the entire digit, because the block is performed at the level of or just proximal to the origin of the dorsal branch of the palmar digital nerve. Response to this block may vary, however. Some horses retain skin sensation in the dorsoproximal aspect of the pastern region. In others, pain arising from lesions involving the fetlock joint or periarticular tissues is abolished. In part, these phenomena can be explained by proximal diffusion of local anesthetic solution, affecting the palmar digital nerves proximal to the fetlock joint. Branches of the palmar digital nerves supplying the proximal sesamoid bones, the sesamoidean nerves, could easily be blocked using an analgesic technique in this abaxial position.24 One of the Editors (SJD) regularly performs palmar nerve blocks at the base of the proximal sesamoid bones as a first block if, on the basis of clinical examination, it is considered unlikely that the horse has foot-related pain and there is also no evidence of likely fetlock joint pain.
The abaxial sesamoid block can be performed in the standing horse or with the limb held by the clinician or an assistant. The assistant grasps the foot, facing forward. The assistant should be warned that a fractious horse may kick backwards with the limb, so he or she should stand slightly to one side, outside the plane of the limb. The palmar digital nerve can easily be palpated over the rigid proximal sesamoid bones and in fact is in its most superficial position in this location. A 25-gauge, 1.6-cm needle is directed in a proximal or distal direction and typically 1 to 3 mL of local anesthetic solution are used for each of the medial and lateral injections. Deep pain is assessed by hard flexion of the interphalangeal joints. False-negative or delayed results can arise because of deposition of local anesthetic solution outside the fascia that surrounds the neurovascular bundle.8
Low Palmar Analgesia
Analgesia of the metacarpophalangeal joint region and distal aspect of the limb is induced using the low palmar block or low palmar analgesia (low four-point). This technique blocks the medial and lateral palmar nerves and the medial and lateral palmar metacarpal nerves. In the forelimb a subcutaneous, dorsally directed ring block and block of the dorsal branch of the ulnar nerve completely abolishes skin sensation. Disagreement exists about whether abolishing skin sensation is necessary when performing perineural techniques. Abolition of skin sensation independently from nerves contributing to deep pain sensation, as in the case of the low palmar technique, does not necessarily mean deep pain is abolished, which is particularly relevant when a nerve responsible for skin sensation is blocked. When using these techniques for diagnostic purposes, it may be best to avoid blocking nerves that contribute only skin sensation, thus minimizing the number of needle insertions For therapeutic interventions, however, these nerves need to be blocked.
The low palmar block is performed at the level of the distal end (bell or button) of the second and fourth metacarpal bones (splint bones), with the limb in a standing position or held off the ground (Figure 10-7). A 20- or 22-gauge needle is used to inject 1.5 to 5 mL of local anesthetic solution at each injection site. To block the palmar metacarpal nerves, the needle is inserted perpendicular to the skin, just distal to the end of the splint bones, to a depth of 1 to 2 cm. It is important to deposit local anesthetic solution deep in the injection site, rather than simply in a subcutaneous location. While local anesthetic solution is continuously injected, the needle is slowly withdrawn, leaving a visible bleb in the subcutaneous space. To block the medial and lateral palmar nerves, the needle is inserted subcutaneously, in the palmar aspect of the space between the suspensory ligament and DDFT at the level of or slightly more proximal to the distal end of the splint bone. To improve the accuracy of the injection, using a fan-shaped injection technique is helpful. If the digital flexor tendon sheath (DFTS) is distended, the injections must be performed more proximally. Inadvertent penetration of the DFTS is possible even if it is not distended, so careful skin preparation is mandatory. To complete this block, local anesthetic solution is placed in the subcutaneous tissues from the bleb at the distal end of the splint bone to the dorsal midline. One of the Editors (SJD) does not do this last step.
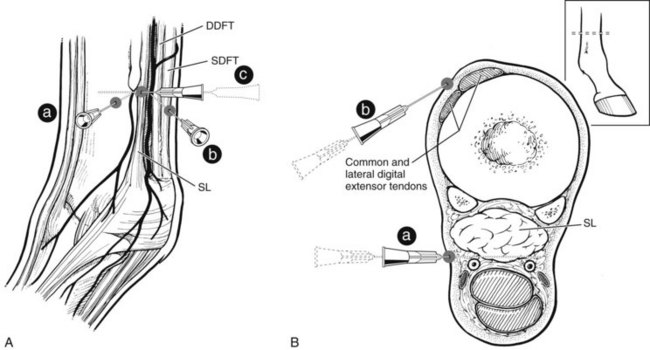
Fig. 10-7 A, This lateral view shows needles positioned for a low palmar (plantar) nerve block. The clinician inserts a needle (a) just distal to the distal aspect of the fourth metacarpal or metatarsal bone and directs it axially to block the lateral palmar (plantar) metacarpal (metatarsal) nerve. The clinician then inserts a needle (b) between the suspensory ligament (SL) and deep digital flexor tendon (DDFT) to block the lateral palmar (plantar) nerve. The clinician repeats the two injections on the medial side. A subcutaneous ring block from the first injection site around to the dorsal midline (c) completely abolishes skin sensation. B, Transverse view of the distal left metacarpal region demonstrating an alternative technique for low palmar (plantar) analgesia. The clinician inserts a needle (a) in a lateral-to-medial direction between the DDFT and the SL to block the lateral and medial palmar (plantar) nerves. The palmar (plantar) metacarpal (metatarsal) nerves are blocked as depicted in A (not shown in this diagram), which also shows the subcutaneous ring block. The clinician inserts a needle (b) in a lateral-to-medial direction dorsal to the digital extensor tendons to block the dorsal metatarsal nerves of the hindlimb.
An alternative technique to abolish pain associated with maladaptive or nonadaptive bone remodeling or other causes of subchondral bone pain of the distal aspect of the McIII is to block the lateral and medial palmar metacarpal nerves separately from the lateral and medial palmar nerves. In some horses suspected of having this injury, use of abbreviated low palmar analgesia will avoid additional injections of local anesthetic solution. With this technique the lateral or medial palmar metacarpal nerve, or both, can be blocked individually or together, and the horse’s gait assessed. In many horses with this cause of lameness, contralateral forelimb lameness will then be seen. If lameness does not abate, the clinician then completes low palmar analgesia using the technique described previously (see the following discussion).
Alternatively, some clinicians prefer to use a longer needle first to deposit local anesthetic solution over the palmar metacarpal (metatarsal) nerves. The needle is then pushed subcutaneously to deposit local anesthetic solution over the palmar nerves (see Figure 10-7). When this modification is performed, incompletely blocking the palmar metacarpal (metatarsal) nerves or lacerating the digital vessels is possible. The lateral and medial palmar nerves can be blocked using only the lateral injection site by advancing the needle in a medial direction, palmar to the DDFT. Although each of these modifications may theoretically decrease the number of injections needed to perform this technique, they have the disadvantages of potential hemorrhage and incomplete analgesia.
High Palmar Block
To provide analgesia to the metacarpal region, the high palmar block (high four-point, subcarpal block) is the most common technique, but a modified block (lateral palmar or Wheat block) can be performed. Inadvertent penetration of the carpometacarpal joint is a potential complication with the high palmar block. A similar complication can occur in the hindlimb but is less frequent (see the following discussion). Inadvertent penetration of the carpometacarpal joint occurred in 17% of specimens, in which a conventional high palmar block was performed, because of extensive distopalmar outpouchings (Figures 10-8 and 10-9). However, when the high palmar block was performed within 2.5 cm of the carpometacarpal joint, inadvertent penetration of this joint occurred in 67% of specimens. The carpometacarpal joint always communicates with the middle carpal joint, and therefore penetration of the carpometacarpal joint during high palmar analgesia would lead the clinician to diagnose a metacarpal problem, when in reality the authentic lameness condition exists in the carpus. Moving the injection site in a distal direction decreases the possibility of entering the carpometacarpal joint but also narrows the scope of the technique and may result in a false-negative response in a horse with proximal suspensory desmitis. Two ways around this likely complication are these: first, the clinician could perform middle carpal analgesia before performing high palmar analgesia; second, the clinician could perform a lateral palmar block in lieu of the conventional high palmar technique. In an experimental study, the carpal joints were unlikely to be entered inadvertently during performance of the lateral palmar block, although in every specimen, local anesthetic solution would have entered the carpal canal.25 Unless the clinician is familiar with the lateral palmar block, the most straightforward approach to reduce the possibility of misdiagnosis in this region is to perform middle carpal analgesia before proceeding to the high palmar block. When local anesthetic solution is placed in the middle carpal joint, not only is the carpometacarpal joint blocked, but also the possibility exists of providing local analgesia to the proximal palmar metacarpal region. With this approach, abolishing pain associated with proximal suspensory attachment avulsion injury (desmitis, fracture), stress remodeling, and longitudinal fracture is possible (see Chapter 37). The palmar metacarpal nerves and suspensory branches from the lateral palmar nerve are closely associated with the distopalmar outpouchings of the carpometacarpal joint, and diffusion of local anesthetic solution from this area could explain in part this clinical finding (Figure 10-10).
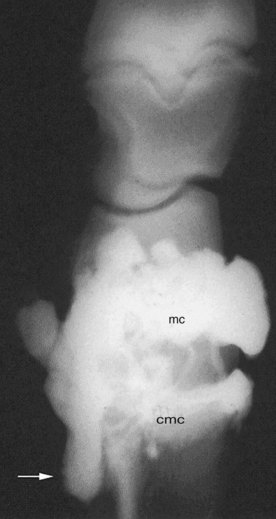
Fig. 10-8 Positive contrast arthrogram of the middle carpal (mc) and carpometacarpal (cmc) joints (dorsal is to the right). Contrast material injected into the middle carpal joint flows freely distally into the carpometacarpal joint and fills the extensive distopalmar outpouchings of the joint (arrow).
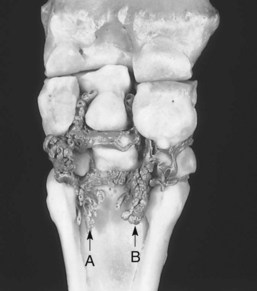
Fig. 10-9 Liquid acrylic injected into the middle carpal joint and allowed to harden created this specimen showing the lateral (A) and medial (B) distopalmar outpouchings of the carpometacarpal joint. Secondary fingerlike outpouchings ramify in the proximal palmar metacarpal region.
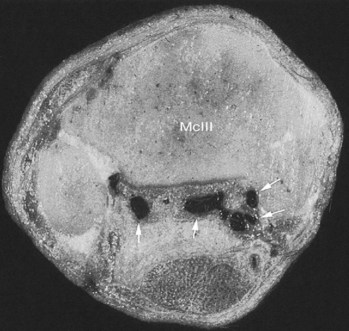
Fig. 10-10 Transverse section of the proximal metacarpal region just distal to the carpometacarpal joint after latex injection into the middle carpal joint showing primary and secondary distopalmar outpouchings of the carpometacarpal joint (dark areas, arrows) interdigitating with the proximal aspect of the suspensory ligament (dorsal is up; lateral is left). This anatomical arrangement explains inadvertent analgesia of the carpus and proximal palmar metacarpal region during high palmar and middle carpal analgesia, respectively. McIII, Third metacarpal bone.
It is important for the clinician to understand that interpretation of analgesic techniques in the proximal palmar metacarpal region or carpus can be somewhat complex. Correct diagnosis is always the key, and comprehensive evaluation using multiple imaging modalities is a must in differentiating lameness in this region. From the clinical perspective, one is more likely to assume incorrectly that one is dealing with a carpal problem when the authentic lameness condition resides in the proximal palmar metacarpal region than vice versa. Numerous techniques are used to perform high palmar analgesia; some provide partial and others provide complete analgesia to the metacarpal region. For complete analgesia, blocking the following nerves is necessary: the medial and lateral palmar nerves, the medial and lateral palmar metacarpal nerves, the suspensory branches, and nerves providing skin sensation along the dorsum (dorsal branch of ulnar nerve and musculocutaneous nerve). To block these nerves effectively, one must use a site close to the carpometacarpal joint, at the level where the splint bones begin to taper (Figure 10-11). If the block is done at a lower level, the region of the suspensory attachment will be missed. A 20- or 22-gauge needle at least 2.5 cm long is necessary to reach the palmar metacarpal nerves in this location. The needle is inserted axial to the splint bones just abaxial to the suspensory ligament and then guided to the palmar cortex of the McIII. Five milliliters of local anesthetic solution are deposited, first deep within the tissues, and continued as the needle is withdrawn, ending with a bleb in the subcutaneous tissues. To block the medial and lateral palmar nerves between the suspensory ligament and DDFT, a smaller-gauge needle can be used to deposit 3 to 5 mL of local anesthetic solution at each of two sites. To complete this block, a circumferential subcutaneous ring block is performed to abolish skin sensation dorsally. Alternatively, the subcutaneous nerves can be blocked on either side of the common digital extensor (CDE) tendon, but small zones of sensation may persist when this technique is used. It is only necessary to complete the dorsal portion of this block to provide complete analgesia when performing procedures in the dorsal metacarpal region, such as laceration repair or standing osteostixis.
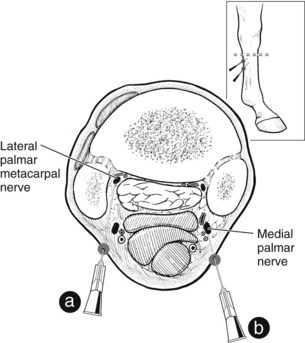
Fig. 10-11 Transverse view of the left metacarpal region showing the technique for high palmar analgesia. The clinician inserts a needle (a) axial to each second and fourth metacarpal bone and uses two separate injections (b) to block the medial and lateral palmar nerves. The location of the high palmar technique appears in the lateral view (inset).
A modification of the high palmar block is performed by locally infiltrating the suspensory origin from a lateral injection site in a fan-shaped pattern. This procedure, along with one specifically to block the medial and lateral palmar metacarpal nerves, improves specificity of this complex block, because pain from only a limited number of structures is eliminated. The medial and lateral palmar nerves can also be blocked from a single lateral injection site. One of the Editors (SJD) regularly blocks just the palmar metacarpal nerves (using only 2 to 3 mL of local anesthetic solution per site) and only adds perineural analgesia of the palmar nerves if the first block is negative, in order to facilitate differentiation of suspensory ligament or McIII pain from pain arising from the more palmar soft tissue structures. A dorsal ring block is never used.
Lateral Palmar Block
An alternative method of providing analgesia to the metacarpal region is to perform what is known as the lateral palmar (high two-point) or Wheat block.26 For complete analgesia, however, combining this block with an independent injection over the medial palmar nerve and with a dorsal subcutaneous ring block is necessary. Originally proposed as an alternative method for analgesia of the suspensory ligament origin, this technique involves blocking the lateral palmar nerve just distal to the accessory carpal bone (Figure 10-12). The lateral palmar nerve is formed as the median and deep ulnar nerves join, proximal to the accessory carpal bone (see Figure 10-12).27 At the level of the block, just distal to the accessory carpal bone, the lateral palmar nerve is blocked before it branches to form the medial and lateral palmar metacarpal nerves and the suspensory branches and continues distally (see Figure 10-12). The high two-point block is completed with the separate but concurrent block of the medial palmar nerve.
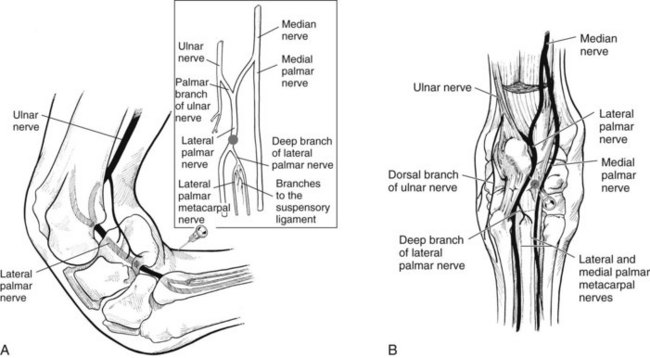
Fig. 10-12 A, This diagram of the left carpus in a flexed position shows the location of the lateral palmar nerve block and parent nerves (inset) contributing to the origin of the lateral palmar and other important nerves. B, Palmar view of the limb showing nerves in situ and the site for needle penetration for lateral palmar nerve block.
This technique has at least three advantages compared with conventional high palmar analgesia. Inadvertently penetrating the distopalmar outpouchings of the carpometacarpal joint is virtually impossible, although local anesthetic solution will likely enter the carpal canal.25 Lateral palmar analgesia requires fewer needle penetrations than does conventional high palmar analgesia. Finally, only a small volume of local anesthetic solution is necessary to desensitize a number of nerves and the origin of the suspensory ligament. Pain associated with the carpal canal is abolished, however, and can be present without palpable effusion.
The lateral palmar block can be performed in the standing position or with the limb held off the ground, with the carpus in 90 degrees of flexion. The nerve cannot be palpated because it courses in the accessorial-metacarpal ligament, dense connective tissue distal to the accessory carpal bone. A 25-gauge, 1.6-cm needle is inserted to the hub, perpendicular to the skin, just distal to the accessory carpal bone, and 5 mL of local anesthetic solution are deposited within this dense tissue. Injection can be difficult to perform, and breaking the seal between the needle and syringe is common, so a screw-type hub should be used. The medial palmar nerve is then blocked as described previously. If desired, a dorsal, circumferential subcutaneous ring block provides complete analgesia to the dorsum. An alternative technique for lateral palmar nerve block has recently been described.28 The primary advantage of this technique is that it mitigates the risk of inadvertent penetration of the carpal synovial sheath (carpal canal). The block is performed with the limb in extension. The primary landmark is a palpable groove in the flexor retinaculum just dorsal to its insertion on the palmaromedial aspect of the accessory carpal bone. A 1.5-cm, 25-gauge needle is inserted in the distal third of the groove in a mediolateral direction, and when contact is made with the medial surface of the accessory carpal bone, local anesthetic solution is injected. However, it is quite easy for the needle to hit the nerve, which results in the horse striking out, and a difficult horse may become even more fractious to block.
Median, Ulnar, and Medial Cutaneous Antebrachial Blocks
Analgesia of the distal aspect of the antebrachium and carpus can be induced by blocking the median, ulnar, and medial cutaneous antebrachial (musculocutaneous) nerves.21 Because the last nerve supplies only skin sensation, for diagnostic purposes it does not need to be included in the technique. In our practices these blocks are most commonly performed to facilitate lavage of the carpal joints or carpal canal or to perform regional limb perfusion of antibiotics in standing horses. We generally default to intrasynovial analgesia in these structures, however. However, one of us (MWR) has recently evaluated several horses with subchondral bone pain in the middle carpal joint in which intraarticular carpal analgesia failed to abolish clinical signs of pain. Lameness was abolished using the median and ulnar blocks. One Editor (SJD) finds these blocks extremely valuable in horses that do not respond to subcarpal or intraarticular carpal analgesia and employs median and ulnar blocks routinely. Although the median and ulnar blocks remain infrequently used in the United States, perhaps they should be considered routine. Median, ulnar, and medial cutaneous antebrachial nerve blocks are useful in diagnosing subchondral carpal bone pain or lameness involving the carpal canal. Although the prevalence of lameness in the distal aspect of the antebrachium is low, these blocks can be used to diagnose distal radial bone cysts or enthesitis at the origin of the accessory ligament of the superficial digital flexor tendon (SDFT) (superior check ligament). These blocks can be used to eliminate the entire distal aspect of the limb as a potential source of pain. Alternatively, these blocks can be used alone to eliminate pain distal to the injection site, or the median and ulnar nerves can be blocked independently to improve specificity of the technique.
The ulnar nerve is blocked about 10 cm proximal to the accessory carpal bone on the caudal aspect of the antebrachium (Figure 10-13). A 20- or 22-gauge, 4-cm needle is inserted to the hub, perpendicular to the skin, in the groove between the flexor carpi ulnaris and the ulnaris lateralis muscles. Needle contact with the ulnar nerve may cause the horse to strike forward.5 Ten milliliters of local anesthetic solution are injected as the needle is slowly withdrawn. Skin sensitivity along the lateral aspect of the limb from the carpus to the metacarpophalangeal joint will be eliminated.21
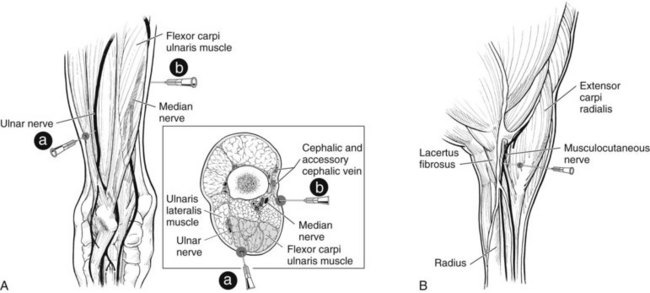
Fig. 10-13 A, This caudal view of the left antebrachium shows the sites of needle insertion for the median and ulnar nerve blocks. A needle placed between the ulnaris lateralis and flexor carpi ulnaris muscles (a), about 10 cm proximal to the accessory carpal bone, blocks the ulnar nerve. A needle inserted along the caudal aspect of the radius about 10 cm distal to the elbow joint (b) blocks the median nerve. The inset shows the orientation between the radius, median artery, vein, and nerve at the site of needle insertion (b) and shows the orientation of the needle for the ulnar nerve block (a), which is performed distally. B, This medial view of the proximal left antebrachium shows the technique for a musculocutaneous nerve block. The nerve is blocked as it crosses the lacertus fibrosus on the cranial aspect of the proximal antebrachium. This block abolishes skin sensation on the medial and dorsal aspects of the antebrachium.
The median nerve is blocked 5 cm distal to the cubital (elbow) joint on the medial aspect of the antebrachium. At this level, the nerve lies along the caudal aspect of the radius, just cranial to the flexor carpi radialis muscle. A 20- or 22-gauge, 4-cm needle is inserted into the hub, in a lateral direction, along the caudal aspect of the radius, just distal to the superficial pectoral muscle, and 10 mL of local anesthetic solution are used (see Figure 10-13). Rarely in large horses, a 9-cm ( -inch) spinal needle may be necessary to reach the median nerve. Often the needle hits the median nerve, a useful indicator that the tip is in the proper location.5 In any event the needle should be kept close to or against the caudal cortex of the radius to avoid inadvertent puncture of the median artery or vein, which lies caudal to the nerve.21,27 However, inadvertent puncture determines that the needle is close to the correct site and is highly unlikely to cause any adverse reaction. To facilitate these deep injections, the skin can be first desensitized by using a small volume of local anesthetic solution. A more distal injection site for the median nerve may eliminate the possibility of inadvertently eliminating elbow joint pain using the suggested approach.5
-inch) spinal needle may be necessary to reach the median nerve. Often the needle hits the median nerve, a useful indicator that the tip is in the proper location.5 In any event the needle should be kept close to or against the caudal cortex of the radius to avoid inadvertent puncture of the median artery or vein, which lies caudal to the nerve.21,27 However, inadvertent puncture determines that the needle is close to the correct site and is highly unlikely to cause any adverse reaction. To facilitate these deep injections, the skin can be first desensitized by using a small volume of local anesthetic solution. A more distal injection site for the median nerve may eliminate the possibility of inadvertently eliminating elbow joint pain using the suggested approach.5
Finally (for therapeutic applications), to block the cranial and caudal branches of the medial cutaneous antebrachial (musculocutaneous) nerve, 3 mL of local anesthetic solution are injected, subcutaneously, on the cranial and caudal aspect of the accessory cephalic and cephalic veins, about halfway between the carpus and elbow (see Figure 10-13).21 Alternatively, this nerve can be blocked before it branches, as it courses across the lacertus fibrosus. At this location, the nerve is easily palpable in most horses. A third method to completely abolish skin sensation is using a circumferential subcutaneous ring block, a technique that can effectively block all four cutaneous antebrachial nerves but requires a large volume of local anesthetic solution.
Intraarticular Analgesia in the Forelimb
Distal Interphalangeal Joint
The assumption is that analgesia of the DIP joint is specific for intraarticular pain, but clinical experience and the results of recent clinical and anatomical investigations have convinced us otherwise (see Figure 10-1). Of great clinical interest is the comparative accuracy of analgesia of the DIP joint and navicular (podotrochlear) bursa in the diagnosis of navicular syndrome. Overall, analgesia of the navicular bursa is likely the most specific technique to diagnose navicular syndrome. However, results of two studies suggest that this block may not be as specific as once thought (see the section on analgesia of the podotrochlear bursa).29,30 Analgesia of the DIP joint lacks specificity for intraarticular pain and in fact can eliminate pain associated with many conditions of the foot.29-32 For instance, when high-performance liquid chromatography was used to study the effects of 8 mL of mepivacaine injected into the DIP joint, there was local anesthetic solution in the synovium of the navicular bursa in all horses and in the medullary cavity of the navicular bones in 40% of horses.33 Similarly, a recent in vitro study showed that 15 minutes after injection of 5 mL of 2% mepivacaine into either the navicular bursa or the DIP joint, mepivacaine was detected in the alternate (uninjected) synovial structure in all specimens. In 48% of navicular bursae after DIP joint injection, and in 44% of DIP joints after navicular bursa injection, mepivacaine was present in clinically effective (analgesic) concentrations (>100 to 300 mg/L).34 Anatomical studies showed that nociceptive neurofibers are present in the dorsal and palmar aspects of the collateral sesamoidean ligaments, within the distal sesamoidean impar ligament, and directly innervating the navicular bone, in the periarticular connective tissues of the DIP joint and proximal intramedullary portions of the distal phalanx.35,36 The close anatomical relationship among all of these structures and the palmar digital neurovascular bundles to the DIP joint capsule makes them susceptible to desensitization by local anesthetic solution injected into the DIP joint.36
In a study using a setscrew model to create solar pain at the toe, DIP intraarticular analgesia abolished lameness, leading to the conclusion that pain in distant sites can be abolished using this technique.22 Therefore a positive response to DIP intraarticular analgesia could mean lameness is caused by an articular problem, navicular syndrome, or, for that matter, solar pain. Close juxtaposition between the palmar synovial extensions of the DIP joint and digital nerves at this level was theorized as the reason that these nerves were blocked, secondary to diffusion of local anesthetic solution from the joint.22 Therefore a protocol to examine a lame horse no longer than 5 minutes after intraarticular analgesia of the DIP joint may theoretically minimize diffusion and improve accuracy. However, in one of the Editor’s (SJD) experience, pain associated with the navicular bone, navicular bursa, or DDFT has frequently been substantially improved within 5 minutes of injection of the DIP joint. Because diffusion of local anesthetic solution may be hastened by moving the horse, some clinicians prefer the horse to stand until the results of the block are evaluated.5
Traditionally, arthrocentesis of the DIP joint has been performed in the dorsal pouch, either medial or lateral to the CDE tendon. A 20-gauge, 2.5- to 4-cm needle is inserted about 1.5 cm proximal to the coronary band, abaxial to the CDE tendon, and directed in a distal and axial direction (Figure 10-14). An easier approach, however, is to insert the needle, angled just slightly distal from horizontal, on the dorsal midline, through the CDE. Synovial fluid is consistently obtained using this approach. One of the Editors (SJD) angles the needle more vertically, inserting it in the palpable dip in the distal dorsal aspect of the pastern. For the dorsal aspect of the DIP joint to be opened up, the limb should be positioned slightly ahead of the contralateral limb, and the horse should be in a standing position. Five to 10 mL of local anesthetic solution have been used traditionally, but a maximum of 6 mL may prevent leakage from the joint. Use of a lower volume of local anesthetic solution may also improve the specificity of the block, as was shown in a similar study using setscrews to create solar pain. Decreasing the volume of local anesthetic solution in the DIP joint from 10 mL to 6 mL resulted in a significant reduction in lameness caused by pain at the dorsal margin of the sole, but not at the angles of the sole.37 The horse is examined after 5 minutes.
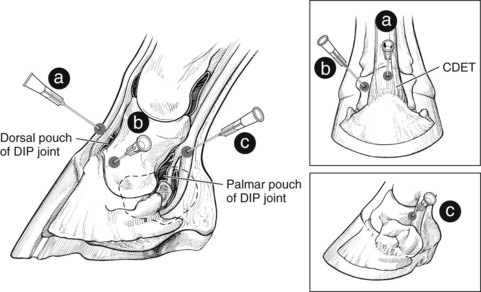
Fig. 10-14 Lateral view of the foot showing our preferred approach for arthrocentesis of the digital interphalangeal joint using a dorsal midline needle insertion site (a) and directing the needle slightly distally through the common (long) digital extensor tendon. Alternatively, the clinician approaches the digital interphalangeal joint using a site medial or lateral to the extensor tendon (b). The top inset shows the needle positions from the dorsal aspect. The clinician may use a palmar (plantar) approach by positioning the needle between the distal palmar (plantar) border of the middle phalanx and a palpable notch in the proximal border of the cartilage of the foot. The clinician directs the needle (c) in a palmaroproximolateral to dorsodistomedial direction. The lower inset shows the notch into which the needle is inserted. CDET, Common (long) digital extensor tendon; DIP, distal interphalangeal.
Alternatively, a lateral approach to the DIP joint can be used (see Figure 10-14). Landmarks include the distal palmar border of the middle phalanx dorsally and the palpable notch in the proximal border of the lateral cartilage of the foot distally. A 4-cm needle is inserted laterally and directed in a dorsodistomedial direction. This technique, however, is less reliable than the dorsal approach, because contrast material entered exclusively the DIP joint in only 13 of 20 specimens and in 7 specimens inadvertently entered the navicular bursa or DFTS.38
Proximal Interphalangeal Joint
Arthrocentesis of the proximal interphalangeal joint is most commonly performed in the dorsal pouch. Effusion is rarely present even in horses with severe lameness, a situation that makes arthrocentesis challenging. The injection site is just lateral (or medial) to the CDE tendon at a level of or just distal to the distal, palmar process of the proximal phalanx, located and easily palpable on the distopalmar aspect of this bone. With the horse in the standing position, a 20-gauge, 2.5-cm needle is directed slightly distally and medially (using the dorsolateral approach) and inserted until articular cartilage is encountered (Figure 10-15). Although a desirable sign, synovial fluid appearing in the hub of the needle is an unusual occurrence. Local anesthetic solution, 5 to 10 mL, is injected, and the horse is examined after 5 minutes.
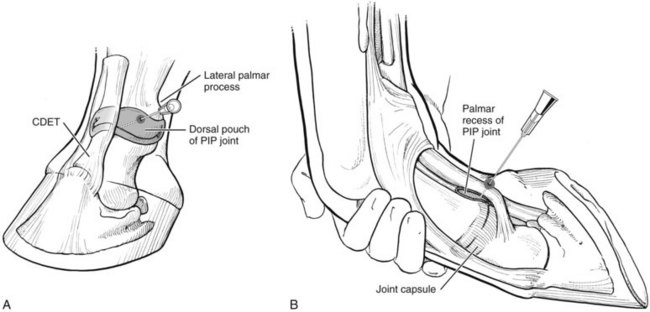
Fig. 10-15 A, Dorsolateral view of the digit showing the site for arthrocentesis of the dorsal pouch of the proximal interphalangeal joint. The clinician inserts the needle just abaxial to the common digital extensor tendon at a site level with the palpable distal palmar (plantar) process of the proximal phalanx. B, Flexed lateral view of the digit indicating the site for arthrocentesis of the palmar (plantar) aspect of the proximal interphalangeal joint. The clinician inserts the needle into the V-shaped notch formed by the distal palmar (plantar) aspect of the proximal phalanx dorsally, the bony eminence associated with the attachment of the lateral collateral ligament to the distal aspect of the proximal phalanx and proximal aspect of the middle phalanx distally, and the insertion of the lateral branch of the superficial digital flexor tendon palmarodistally (plantarodistally). The clinician directs the needle distomedially (in a slightly dorsal direction) at an angle of about 30 degrees from the transverse plane until fluid appears. CDET, Common (long) digital extensor tendon; PIP, proximal interphalangeal.
An alternative approach that one author (MWR) finds much easier to perform is approaching the proximal palmar pouch of the proximal interphalangeal joint from the lateral aspect. The injection location is a V-shaped notch, located dorsal to the neurovascular bundle and between the distal palmar process of the proximal phalanx and the insertion of the lateral branch of the SDFT (see Figure 10-15). The limb is held off the ground with the digit in flexion, and a 2.5- or 4-cm needle is directed distomedially (and slightly dorsally) at an angle of about 30 degrees from the transverse plane until fluid is collected (generally at a depth of 2 to 3 cm).39 Advantages of this compared with the dorsal approach include less needle manipulation, a larger injection volume, and more frequent recovery of synovial fluid. The technique is difficult to perform with the limb in an extended weight-bearing position, because the palmar or plantar aspect of the proximal interphalangeal joint is compressed. Furthermore, diffusion of local anesthetic solution into palmar soft tissue structures can confound interpretation of results.5
Metacarpophalangeal Joint
Four sites commonly used for arthrocentesis of the metacarpophalangeal joint include the dorsal, proximopalmar, and distopalmar sites and the approach through the collateral ligament of the proximal sesamoid bone. The two most commonly used, the dorsal and proximopalmar sites, have potential disadvantages compared with the less commonly used sites. The dorsal pouch can be prominent in horses with effusion, but inadvertently stabbing articular cartilage repeatedly is common when this approach is used. The proximopalmar pouch or recess is large and easily identified, but prominent synovial villi often occlude the needle end, complicating retrieval of synovial fluid, even in horses with severe effusion. Hemorrhage associated with large intracapsular vessels is also a common complication with the proximopalmar approach. The palmar pouch is located dorsal to the suspensory branch, palmar to the McIII, proximal to the collateral sesamoidean ligament, and distal to the bell of the splint bone (Figure 10-16). Arthrocentesis using the proximopalmar approach can be performed with the limb in the standing position or being held. An 18- to 22-gauge, 2.5- to 4-cm needle is inserted in the center of the pouch and directed slightly distally in the frontal plane until synovial fluid is recovered (Figure 10-17). It may be necessary to aspirate synovial fluid if the joint capsule is not distended.
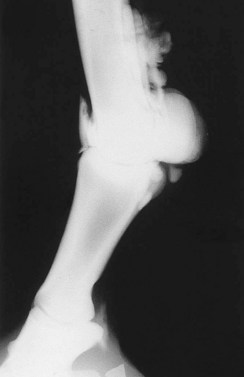
Fig. 10-16 Positive contrast arthrogram of the metacarpophalangeal joint showing the extensive nature of the palmar pouch that extends proximally to the level of the distal end of the splint bones. The distopalmar outpouchings are reliable sites for retrieval of synovial fluid and injection.
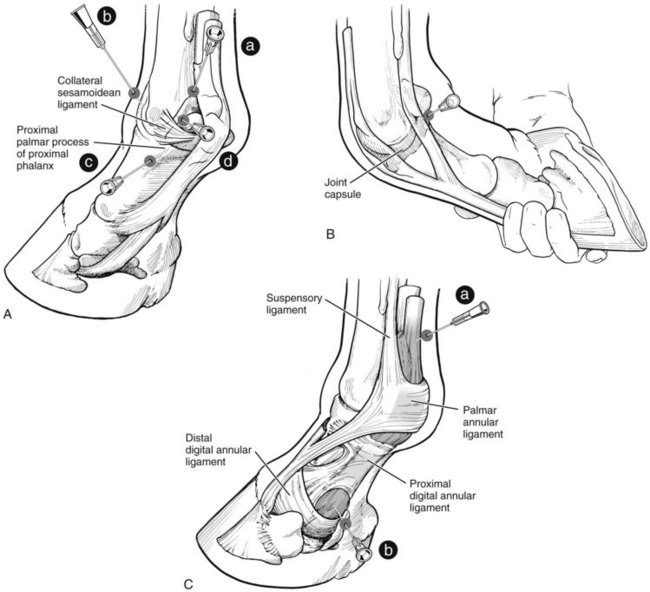
Fig. 10-17 A, Palmarolateral (plantarolateral) view of the left metacarpophalangeal (metatarsophalangeal) joint and digit showing the sites for arthrocentesis of the proximal palmar (plantar) pouch (a), the dorsal pouch (b), the distal palmar (plantar) pouch (c), and the palmar (plantar) pouch through the collateral ligament of the proximal sesamoid bone (d). B, Our preferred site for metacarpophalangeal (metatarsophalangeal) joint arthrocentesis, the distal palmar (plantar) approach, using a site just proximal to the lateral palmar (plantar) process of the proximal phalanx, is easily located in the standing or flexed position. C, Palmarolateral (plantarolateral) view of the digit indicating sites for synoviocentesis of the proximal (a) and distal (b) aspects of the digital flexor tendon sheath. Proximally, the clinician inserts the needle proximal to the palmar (plantar) annular ligament, and distally inserts the needle on the palmar (plantar) midline into an outpouching of the digital flexor tendon sheath between the proximal and distal digital annular ligaments.
Dorsally, arthrocentesis is performed medial or lateral to the CDE tendon (see Figure 10-17). With the limb in a standing or flexed position, the clinician can insert a needle in the distal aspect of the palmar pouch, through the collateral sesamoidean ligament, a less common but effective approach for arthrocentesis of the metacarpophalangeal joint. The technique is more easily performed with the joint held in flexion. This approach for arthrocentesis was shown to be associated with less subcutaneous and synovial inflammation than was the proximopalmar approach40 and is the technique routinely used by one of the Editors (SJD).
Under most circumstances we prefer to perform arthrocentesis of the metacarpophalangeal joint using the distopalmar approach. The injection site is in a small but reliable recess bounded by a triad of structures. Just proximal to the readily palpable proximal, palmar process of the proximal phalanx is a distinct depression. The dorsal aspect of the proximal sesamoid bone and the palmar condyle of the McIII complete the triad but are not readily palpable. The injection site is dorsal to the neurovascular bundle. Synovial fluid is consistently retrieved because the injection site is in the most distal aspect of the joint, and hemorrhage is rare. A large volume of fluid can be collected, if desired, because this area is devoid of the large synovial villi that complicate the proximopalmar approach. With the horse in a standing position, a 20-gauge, 2.5-cm needle is inserted, parallel to the ground, in a dorsomedial direction until fluid is obtained (see Figure 10-17). The needle can be advanced to the hub, but the joint is quite superficial in this location. This technique can also readily be performed with the limb being held in a flexed position.
Ten mL of local anesthetic solution are injected, and the horse is reexamined in 5 to 10 minutes. In horses with subchondral bone pain, additional time may be necessary, but perineural analgesia may be necessary to abolish lameness in these horses. Diffusion of local anesthetic solution may account for partial or complete improvement in lameness in horses with suspensory branch desmitis, sesamoiditis, or injury of the straight, cruciate, or oblique sesamoidean ligaments. Therefore timely evaluation of horses after metacarpophalangeal analgesia is necessary.
Carpal Joints
Arthrocentesis of the middle carpal or antebrachiocarpal joints is one of the easiest and most straightforward of all joint injection techniques. With the carpus in flexion, injection sites are easily identified, and large portals exist through which to access the joints. Portals can be found either medial to the extensor carpi radialis (ECR) tendon or between the ECR and the CDE tendons (Figure 10-18). The middle carpal and carpometacarpal joints always communicate, but a communication between the middle carpal and antebrachiocarpal joints rarely exists. A communication between the middle carpal joint and carpal sheath only rarely is encountered clinically, but was not seen in a study using cadaver limbs. Analgesia of the middle carpal and antebrachiocarpal joints should be performed separately to differentiate lameness between these independent cavities. However, even though gross anatomic communications rarely exist between these joints, a recent in vitro study revealed the potential for diffusion of mepivacaine from one joint to the other by 15 minutes after either was injected with 10 mL of 2% mepivacaine. In only a small percentage were the concentrations of mepivacaine in each joint at levels thought to produce clinical analgesia. How this translates to the live horse also remains unknown. Nonetheless, the clinician is reminded of the importance of prompt reevaluation to minimize misinterpretation of the results, but also to keep an open mind if results of diagnostic imaging do not seem compatible with the results of diagnostic analgesia.34 Distopalmar outpouchings of the carpometacarpal joint complicate interpretation of analgesic techniques, because these extend a mean distance of 2.5 cm distal to the carpometacarpal articulation and are closely associated with the suspensory ligament origin and the palmar metacarpal nerves (see Figures 10-8 to 10-10).41 Careful differential analgesic techniques and comprehensive imaging are necessary for accurate diagnosis of lameness in the carpal and proximal metacarpal regions.
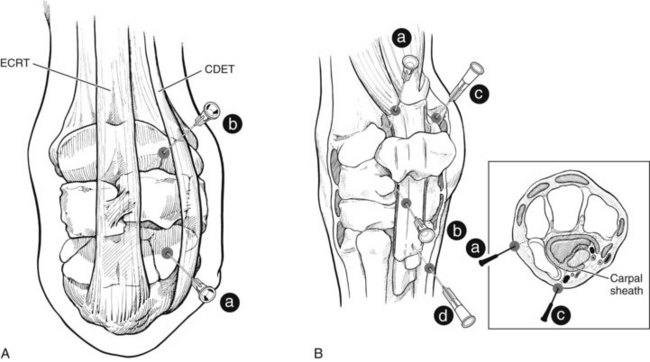
Fig. 10-18 A, Dorsal view of the left carpus in a flexed position showing the sites for arthrocentesis of the middle carpal (a) and antebrachiocarpal (b) joints. Needles are usually positioned between the extensor carpi radialis and common digital extensor tendons (as shown), but sites for injection of both joint cavities located medial to the extensor carpi radialis tendon can be used. B, Lateral view of the left carpus demonstrating sites for arthrocentesis of the proximal palmar pouch of the antebrachiocarpal joint (a), the palmarolateral pouch of the middle carpal joint (b), and the proximal (c) and distal (d) pouches of the distended carpal sheath. The inset shows the relative needle positions to enter the palmar pouch of the antebrachiocarpal joint and the carpal sheath. CDET, Common (long) digital extensor tendon; ECRT, extensor carpi radialis tendon.
Typically, a 20-gauge, 2.5-cm needle is used to inject 5 to 10 mL of local anesthetic solution into the middle carpal and antebrachiocarpal joints. If the skin can be prepared aseptically on the dorsal aspect, the injections are most commonly performed with the joint in 90 to 120 degrees of flexion. The clinician can maintain flexion, but having an assistant hold the limb securely is easier.
If the dorsal aspect of the carpus cannot be prepared aseptically, as occurs commonly in racehorses with chemically induced dermatitis (scurf), or if an additional site is needed for thorough lavage, the palmarolateral pouches of the middle carpal and antebrachiocarpal joints can be used. The palmar pouch of the antebrachiocarpal joint is bounded by the lateral digital extensor tendon dorsally and the ulnaris lateralis tendon palmarly. In horses with substantial effusion, this pouch is easily identified but must be differentiated from the lateral outpouching of the carpal sheath. Arthrocentesis can be performed either proximally or distally in the palmar pouch (see Figure 10-18). The distal injection site is located in a shallow recess between the distal lateral radius (ulna) and the ulnar carpal bone, just distal to the V-shaped convergence of the lateral digital extensor and ulnaris lateralis tendons. With the horse in a standing position, a 20-gauge, 2.5-cm needle is inserted perpendicular to the skin and advanced until synovial fluid is recovered.
The palmar pouch of the middle carpal joint is similarly accessed in a shallow depression between the ulnar and fourth carpal bones, located 2 to 2.5 cm distal to the recess palpated to access the antebrachiocarpal joint in the palmar aspect (see Figure 10-18). The shallow depression in the middle carpal joint is difficult to palpate, but in horses with severe effusion an outpouching of the joint is palpable. This approach is undertaken with the limb in a standing position, decreases the potential for iatrogenic cartilage injury, and is less dangerous to the clinician because the procedure is performed on the side rather than in front of the limb.42 The injection is more difficult and less commonly used, however.
Cubital (Elbow) Joint
Two sites are used for arthrocentesis of the elbow joint. The cranial pouch is accessed at the level of the radiohumeral articulation, just cranial to the lateral collateral ligament. The lateral collateral ligament courses between the palpable lateral tuberosity of the radius and the lateral epicondyle of the humerus (Figure 10-19). An 18- or 20-gauge, 6- to 9-cm needle is directed medially and slightly caudally to a depth of 5 to 6 cm, beginning in the adult horse, about 3.5 cm proximal to the lateral tuberosity of the radius and 2.5 cm cranial to the lateral collateral ligament.19 To account for differences in horse size, the injection site is generally located two thirds of the distance between the humeral epicondyle and the lateral tuberosity of the radius. This block may be more easily performed closer to the lateral collateral ligament, and at this site the joint is penetrated in a more superficial location.5 Before injection, every effort should be made to verify that the needle is actually in the joint. Periarticular deposition of local anesthetic solution in this location can induce temporary radial nerve dysfunction, and horses may lose the ability to extend the carpus and digit.43 Twenty to 25 mL of local anesthetic solution are used. An older approach relied on injection of local anesthetic solution into the ulnaris lateralis bursa, once universally thought to communicate with the elbow joint. The frequency of communication between the elbow joint and ulnaris lateralis bursa was determined to be 37.5%, and therefore this approach is no longer recommended.44
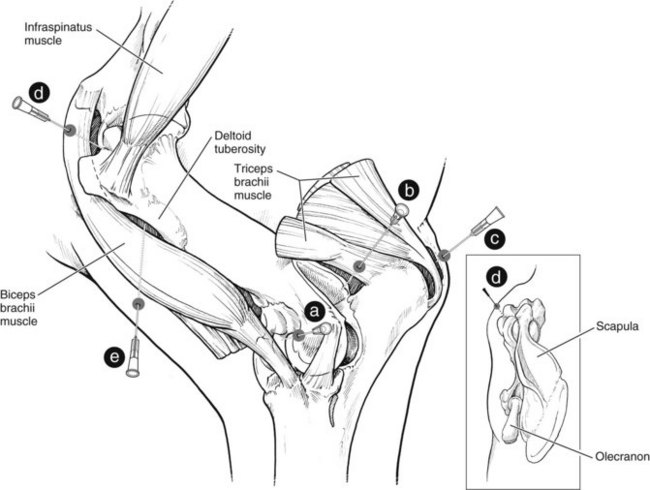
Fig. 10-19 Lateral view of the left elbow and shoulder regions. For arthrocentesis of the cranial pouch of the elbow (cubital) joint, the clinician directs the needle (a) medially and slightly caudally to a depth of about 5 to 6 cm at a point about 3.5 cm proximal to the lateral tuberosity of the radius and 2.5 cm cranial to the lateral collateral ligament. Arthrocentesis of the proximal, caudal pouch (b) is performed at a site in the palpable depression between the cranial aspect of the olecranon and the caudal aspect of the lateral epicondyle of the humerus. One injection site is for the rarely performed technique of synoviocentesis of the olecranon bursa (c). Proximally is the site for arthrocentesis of the scapulohumeral joint (d). A needle is inserted cranial to the infraspinatus tendon in the notch between the cranial and caudal eminences of the greater tubercle of the humerus and advanced in a caudomedial direction, roughly parallel to the ground and about 45 degrees to the long axis of the body (inset). For the bicipital bursa (e), the clinician inserts the needle at a point about 4 cm proximal to the palpable distal aspect of the deltoid tuberosity of the humerus (or alternatively, a point about 3 to 4 cm distal and 6 to 7 cm caudal to the palpable aspect of the cranial process of the greater tubercle) and directs it proximally and medially, and in some patients slightly cranially.
We prefer to perform arthrocentesis in the proximolateral aspect of the caudal pouch in the palpable depression cranial to the olecranon process and caudal to the lateral epicondyle of the humerus. In most horses the site of needle penetration is 3 to 3.5 cm caudal to the lateral epicondyle (see Figure 10-19). In small horses and ponies, an 18- or 20-gauge, 4-cm needle is sufficient, but in large horses a 9-cm spinal needle is often necessary because the injection site is at the distal extent of the lateral head of the triceps muscle. The needle is advanced for 5 to 7 cm in a distal, slightly cranial, and medial direction until synovial fluid is recovered. However, this technique is often less well tolerated by difficult horses compared with the cranial pouch technique.
Elimination of skin sensitivity at the site of needle insertion by depositing a small volume of local anesthetic solution may facilitate elbow arthrocentesis, because numerous attempts may be necessary. Synovial fluid is consistently retrievable from the joint with proper needle positioning.
Scapulohumeral (Shoulder) Joint
The shoulder joint is frequently blamed for lameness in many horses but, based on the results of diagnostic analgesia, is an uncommon source of pain. Arthrocentesis of this joint is most commonly performed at a site between the cranial and caudal prominences of the greater tubercle of the humerus, just cranial to the infraspinatus tendon. This tendon is easily palpated in most horses and serves as the primary landmark. Firm, careful palpation between the cranial and caudal prominences reveals a depression or notch, which is the point of needle insertion (see Figure 10-19). Identification of landmarks is easier in horses with muscle atrophy resulting from chronic lameness.
In most horses an 18- to 20-gauge, 9-cm spinal needle is preferred, although using the entire length is not necessary. Elimination of skin sensitivity is usually not necessary. The needle is inserted in a caudomedial direction (about 45 degrees from lateral), and directed slightly distally. Attaching a syringe to aspirate synovial fluid is sometimes necessary, because in joints with minimal effusion, confirming intraarticular position of the needle may be difficult. A total of 25 to 30 mL of local anesthetic solution is used, and the horse is assessed 10 and 30 minutes after injection, because severe pain associated with osteochondrosis may resolve slowly. Analgesia of the suprascapular nerve and subsequent supraspinatus and infraspinatus muscle paralysis were reported after attempts at intraarticular shoulder analgesia.43 This complication is uncommon, in our experience, and may result from proximal periarticular injection of local anesthetic solution. An alternative explanation is anesthetic solution diffusion to nerves of the brachial plexus.5 Trauma from numerous needle insertions or injection of large volumes of local anesthetic solution (>30 mL) may increase the likelihood of this complication. In fact, some have recommended using only 8 to 10 mL, but false-negative results from the block would likely occur.43 Our opinion is that the most likely cause of this rare complication is malposition of the needle or iatrogenic trauma. Rarely, a communication between the bicipital bursa and the shoulder joint occurs.45 Thinking a horse has shoulder joint pain is possible then, but in reality the diagnosis is bicipital bursitis or tendonitis. Rather than a communication between the structures, the most likely explanation is inadvertent penetration of the bicipital bursa from a misdirected needle.
Analgesia of Forelimb Bursae and Tendon Sheaths
In most instances, analgesia of bursae and tendon sheaths is achieved using perineural techniques, but in some horses, selective intrasynovial analgesia is indicated. Pain sensation from bursae and sheaths is likely complex, and lameness after intrabursal or intrathecal (within a sheath) analgesia may improve but not completely resolve. In fact, horses with severe lameness resulting from bursitis or tenosynovitis often have other associated soft tissue damage, a fact that explains partial improvement after intrasynovial analgesia. Extra time is usually given, after blocking, to reassess the horse’s clinical signs.
Podotrochlear (Navicular) Bursa
As was noted previously (see DIP joint analgesia), analgesia of the navicular bursa has generally been regarded as the most specific block for diagnosis of navicular syndrome. Although likely still true, the results of at least two studies suggest there is potential for misinterpretation of the results of analgesia of the navicular bursa, and we question the specificity of the block. With a setscrew model used to induce solar pain, it was shown that injection of 3.5 mL of local anesthetic solution into the navicular bursa significantly reduced lameness scores in horses with pain at the dorsal aspect of the sole (but not the palmar aspect) within 15 minutes.29 In a complementary study using endotoxin-induced synovitis of the DIP joint, injection of the navicular bursa with 3.5 mL of local anesthetic solution had no effect on lameness score at 10 minutes, but lameness was substantially decreased 20 minutes after injection (though not to a statistically significant degree [P = .07]).30 Nonetheless, the clinical experience of one of the Editors (SJD) indicates that intrathecal analgesia of the navicular bursa is reasonably reliable in improving pain associated with lesions of the navicular bone, navicular bursa, and distal aspect of the DDFT, whereas pain associated with the collateral ligaments of the DIP joint is not affected.
A palmar midline approach is most commonly used for analgesia of the navicular bursa. Because needle position is difficult to assess and fluid recovery varies, radiographs should be used to confirm proper needle position. Alternatively radiodense contrast medium can be injected together with the local anesthetic solution, and a lateromedial radiographic image can then be obtained to determine that the injection was into the navicular bursa. Positioning the foot on a wooden block can minimize the problems of manipulation at the bulbs of the heel and helps to maintain aseptic technique. Subcutaneous deposition of a small volume (1 to 2 mL) of local anesthetic solution can improve horse compliance during this procedure. An 18- to 20-gauge, 9-cm spinal needle is inserted on the palmar midline, just proximal to the hairline, and directed parallel to the sole until the needle contacts bone (Figure 10-20).25,27,46 Others describe a similar approach, although they direct the needle parallel to the coronary band.21,47,48 Because redirection of the needle proximally or distally often is necessary, these approaches differ little. Success depends most on personal experience, but radiographs can be critical in confirming successful entry into the navicular bursa. The direction in which the needle is inserted is often dictated by the shape of the horse’s foot and the projected position of the navicular bone.5 Plotting and marking the navicular position on the hoof wall can be helpful in determining needle direction and depth of insertion. The navicular position is located at a site 1 cm distal to and halfway between the dorsal and palmar aspects of the coronary band.48,49 However, with experience and after identifying the navicular position, the procedure can be done blindly. In most horses the flexor surface of the navicular bone will be contacted at a depth of 4 to 5 cm. The needle is likely improperly positioned if resistance is encountered at a depth of less than 3 to 4 cm or if the needle can be advanced more than 6 to 7 cm. Spontaneous retrieval of synovial fluid is rare and usually indicates that the needle is in the DIP joint capsule or the DFTS. To avoid penetrating these structures, the needle should be placed in the middle of the flexor surface of the navicular bone.5 Three to 5 mL of local anesthetic solution are used. If navicular syndrome is suspected, some clinicians combine injection of local anesthetic solution with a corticosteroid. Alternatively, navicular bursography50 can be performed in combination with diagnostic analgesia by adding 1 to 2 mL of sterile, iodinated contrast material (see Chapter 30). Because in the standing horse the navicular bursa is under compression by the DDFT, suspending the foot or placing the toe in a “navicular block” as if for radiography, with the foot in partial flexion during actual injection, are useful. Without using radiographs, being confident of accurate needle placement is difficult.
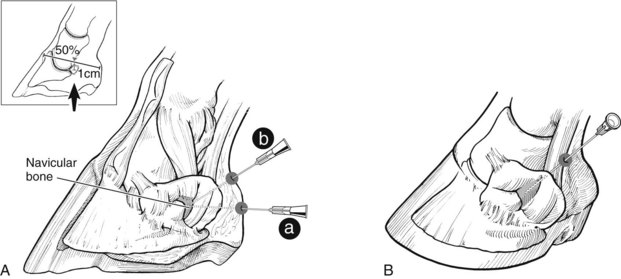
Fig. 10-20 A, Lateral view showing two techniques for synoviocentesis of the navicular bursa of the foot. In the palmar (plantar) approach (a) the needle is placed just proximal to the hairline between the bulbs of the heel and inserted to the navicular bursa using the navicular position as a guide. The navicular position (arrow) is located by determining the point on the outside of the hoof wall that is 50% of the distance from the dorsal to the palmar (plantar) extent of the coronary band and 1 cm below (inset). An approach slightly more proximal (b) requires placing the needle in the depression between the heel bulbs and advancing the needle in a dorsodistal direction, about 30 degrees from horizontal toward the navicular position. B, Palmarolateral (plantarolateral) view of the digit showing the lateral approach for synoviocentesis of the navicular bursa. The needle is inserted just proximal to the cartilage of the foot between the digital neurovascular bundle and the digital flexor tendon sheath and directed axially, distally, and slightly dorsally.
A proximal, palmar injection technique has been described. A needle is inserted into the deepest part of the hollow between the heel bulbs and advanced dorsodistally, about 30 degrees from horizontal, until contact with the bone is made.45,51 A lateral (or medial) approach is also described. A needle is inserted just proximal to the cartilage of the foot, between the neurovascular bundle and the DFTS and directed axially, distally, and slightly dorsally until contact with bone is made (see Figure 10-20).46,48,52 These five techniques were compared in an in vitro study. The most reliable technique was determined to be the distal palmar approach, with the needle being directed to the navicular position and the limb in a non–weight-bearing position.53
Digital Flexor Tendon Sheath
Two sites for intrasynovial injection of the DFTS are just proximal to the palmar (plantar) annular ligament (PAL) or in the palmar aspect of the pastern region in an outpouching of the sheath located between the proximal and distal digital annular ligaments (see Figure 10-17). Effusion facilitates identification of these sites, and rarely would an intrathecal injection be contemplated without the presence of effusion. Proximal to the PAL, villous hypertrophy of synovial membrane can complicate the procedure, because even with severe distention of the sheath, synovial fluid may be difficult to retrieve. For this reason we favor the palmar pastern approach. In some horses the sheath appears to be compartmentalized and distended proximal to the PAL but not below, and therefore injections are easier to perform proximally. A 20-gauge, 2.5-cm needle and 10 to 15 mL of local anesthetic solution are used (see also Figure 124-1). In contrast to intrasynovial analgesia in other locations in the digit, analgesia of the DFTS appears to be quite specific for lameness associated with pain arising from structures contained within it.54 In other words, unless local anesthetic solution is inadvertently injected outside of the DFTS or leaks from it after injection, analgesia of nearby digital nerves and structures appears unusual. However, local diffusion may result in alleviation of pain from the oblique or straight sesamoidean ligaments.55
Alternatives to these approaches for intrasynovial injection of the DFTS are described. The procedure can be performed at a site just distal to the PSBs, between the distal aspect of the PAL and the proximal aspect of the proximal digital annular ligament (see Figure 10-17). A palmar axial sesamoidean approach has been described. With the metacarpophalangeal joint held in flexion (225-degree angle between the McIII and the proximal phalanx), a 20-gauge, 2.5-cm needle is inserted at an angle of 45 degrees, 3 mm axial to the palmar border of the PSB (midbody) and just palmar to the neurovascular bundle. Putative advantages included more reliable access to the DFTS when effusion is absent and reduced time required for successful entry.56
Carpal Sheath
The carpal sheath (carpal flexor sheath) envelops the SDFT and DDFT in the carpal canal. Distention of the carpal sheath is most easily recognized laterally, just proximal to the accessory carpal bone, between the lateral digital extensor and ulnaris lateralis tendons (see Figure 10-18). Effusion of the carpal sheath must be differentiated from that of the antebrachiocarpal joint. Concurrent distention of the dorsal aspect of the antebrachiocarpal joint or distention of the distal aspect of the carpal sheath (lateral or medial, distal to the flexor retinaculum on the palmar aspect of the metacarpal region) is a sign that is helpful in determining this. Ultrasonographic evaluation or positive contrast radiography can be useful adjunct diagnostic techniques. Synoviocentesis can be performed in either the proximal or the distal aspect of the sheath, using a 20-gauge, 2.5-cm needle and 10 to 15 mL of local anesthetic solution.
Olecranon Bursa
This technique is mentioned to be complete, but we have never found an indication to perform analgesia of this bursa (see Figure 10-19). If distended, this bursa could be entered using the same techniques described for other bursae. Rarely, local analgesia over implants used to repair olecranon process fractures is necessary to investigate whether implant removal is indicated.
Bicipital Bursa
Bicipital bursitis and shoulder lameness are frequently diagnosed but in reality are uncommon causes of lameness, if the clinician religiously adheres to the principles of diagnostic analgesia. However, bicipital bursitis and tendonitis and proximal humeral osteitis, fractures, or osseous cystlike lesions can cause lameness and are diagnosed using analgesia of the bicipital bursa. The bicipital bursa is located between the greater and lesser tubercles of the humerus and the overlying tendon of origin of the biceps brachii muscle. Synoviocentesis of the bicipital bursa is routinely performed from a lateral approach, but if severe effusion exists, the bursa can be accessed medially. The injection site is located just cranial to the humerus, 4 cm proximal to the distal aspect of the deltoid tuberosity.46 Alternatively, the site can be located by finding a point 3 to 4 cm distal and 6 to 7 cm caudal to the cranial process of the greater tubercle (see Figure 10-19).19 Subcutaneous infiltration of local anesthetic solution at the site can be used but is rarely needed. An 18-gauge, 9-cm needle is directed in a proximal, medial, and slightly cranial direction and can be “walked off” (shaft of the needle in contact with the bone) the cranial cortex of the humerus. A change in resistance is felt, and synovial fluid may be seen in the needle hub or can be aspirated. Ten to 20 mL of local anesthetic solution are used. If injection is difficult, synovial fluid cannot be retrieved, and retrieving local anesthetic solution already injected is not possible, the bursa likely has not been entered. A recent study showed a high failure rate of injection with either technique.57 Moreover, false-negative results also occur, despite retrieval of synovial fluid, in association with severe lesions of the tendon of biceps brachii or in the presence of dystrophic mineralization or ossification.58 An alternative is to use an ultrasound-guided technique, which may be more accurate.
Perineural Analgesia in the Hindlimb
Perineural analgesia in the distal aspect of the hindlimb is similar to that described for the forelimb. Minor differences in innervation and anatomy must be taken into consideration, however. Technical differences in whether, or how, the limb is held and other intangible differences exist. Most clinicians are not as familiar, or frankly as comfortable, with performing hindlimb analgesic techniques, and this is particularly true with perineural analgesia. It takes a dedicated lameness detective to be enthusiastic about hindlimb analgesia, particularly in fractious or highly strung horses. Obviously, safety for the veterinarian and assistants is paramount, and physical and chemical restraint become important. Performing intraarticular analgesia is far easier, but the clinician must keep in mind that perineural techniques are much more effective in abolishing subchondral bone pain. Therefore false-negative results will likely be obtained if one is limited to only intraarticular procedures. We generally recommend that most perineural techniques distal to the tarsus be performed with the limb held off the ground by an experienced assistant, but personal preference can of course prevail. In some instances, such as when plantar digital analgesia is performed, the anatomy is much easier to identify when the limb is bearing weight. One of the Editors (SJD) routinely performs the majority of hindlimb local analgesic techniques with the limb bearing weight, and with the horse restrained in wooden stocks. The hindlimb can be positioned behind or just in front of the back wooden post; the clinician is then protected by the post if the horse kicks.
To limit the number of hindlimb injections in horses that lack clinical signs referable to the digit, starting with the low plantar block (low 4 point or 6 point block) may be reasonable, in lieu of performing sequential blocks starting with plantar digital analgesia. Of course, performing blocks distal to this site at another time may be necessary if baseline lameness is discovered using this approach. The clinician should take care when testing the efficacy of hindlimb blocks, and using a pole or similar device may be safer than using forceps.5 Complete abolition of skin sensation in the hindlimb is less likely than in the forelimb because the distribution of cutaneous innervation varies.
Plantar Digital Analgesia
The technique for plantar digital analgesia is essentially the same as in the forelimb (see Figure 10-5). The prevalence of lameness abolished by plantar digital analgesia in the hindlimb is considerably lower than palmar digital analgesia in the forelimb but is not zero, and therefore this block should still represent a good starting point for a horse with undiagnosed hindlimb lameness. Because of the reciprocal apparatus, the digit is constantly flexed when the limb is held off the ground, and this block can be slightly more difficult to perform in this position. However, just as in the forelimb, results can be misleading with abolition of pastern or fetlock region pain.
Dorsal Ring Block of the Pastern
The section on the dorsal ring block of the pastern in the forelimb describes this technique (see Figure 10-5). This block requires several needle insertions and can be difficult to perform if the limb is held off the ground, because the dorsal aspect of the pastern is constantly flexed, making subcutaneous injection difficult.
Basisesamoid and Abaxial Sesamoid Blocks
Basisesamoid and abaxial sesamoid blocks present no essential differences between the forelimbs and hindlimbs (see Figure 10-5). Our philosophical points about the basisesamoid block (see forelimb) hold true in the hindlimb as well. The abaxial sesamoid block is avoided, if possible, in racehorses, because the high prevalence of lameness involving the metatarsophalangeal joint may lead to inadvertent misdiagnosis (a positive response to the block will be interpreted as lameness in the foot, when in reality lameness involves the metatarsophalangeal joint).
Low Plantar Block
Analgesia of the metatarsophalangeal joint region is achieved using the low plantar block, a procedure similar to the low palmar block (see Figure 10-7). This block is one of the most overlooked but most useful of all perineural techniques. It is essential to block the medial and lateral and plantar and the medial and lateral plantar metatarsal, and in some horses the dorsal metatarsal nerves. For routine diagnostic analgesia we do not block the dorsal metatarsal nerves, but for therapeutic analgesia they should be blocked. Anecdotal information suggests that some practitioners may not include the plantar metatarsal nerves when performing this block. The plantar metatarsal nerves supply innervation to the subchondral bone of the distal aspect of the third metatarsal bone (MtIII), and to provide analgesia to this important area, these nerves need to be blocked. In fact, a modification of this technique can be used in horses suspected of having subchondral, maladaptive, or nonadaptive remodeling of the MtIII, a common diagnosis in Standardbred and Thoroughbred racehorses (see Chapters 106 to 109). A positive response to an independent block of the lateral plantar metatarsal nerve can help establish this syndrome as the cause of lameness. Other causes of pain arising from the lateral aspect of the metatarsophalangeal joint, including fractures of the lateral condyle of the MtIII or of the PSBs, can be abolished using this modified technique.
The only difference between the low palmar and low plantar blocks involves the dorsal aspect of the limb (see Figure 10-7). Skin sensation laterally and medially is retained after this block, unless a circumferential, subcutaneous ring block is used. In the forelimb, it is necessary to use subcutaneous infiltration only to the dorsal midline. Alternatively, the dorsal metatarsal nerves can be blocked individually.
High Plantar Nerve Block
The high plantar or subtarsal block is one of the most important but often overlooked perineural analgesic procedures in the horse. This block is used to diagnose suspensory desmitis, arguably one of the most important lameness conditions in the hindlimb. However, suspensory desmitis can be a catchall diagnosis in some horses with occult hindlimb lameness, and the high plantar block must be done to confirm the authentic location of pain. The high plantar block should be done after completion of lower limb blocks such as low plantar analgesia to rule out other common sources of pain. Practitioners should be wary of a recent trend to complete only a subtarsal block to diagnose, erroneously in some horses, proximal suspensory desmitis, when sequential distal-to-proximal analgesic techniques may have revealed an alternative source of pain. The tarsometatarsal joint has distoplantar outpouchings (similar to but less extensive than the distopalmar outpouchings of the carpometacarpal joint) that may complicate tarsometatarsal intraarticular or high plantar analgesic techniques (Figure 10-21). However, this is certainly less of a problem in the hindlimb than in the forelimb. For example, inadvertent penetration of the tarsometatarsal joint occurred in only 5% of limbs in which high plantar analgesia was performed, at a level of 1.5 cm distal to the tarsometatarsal joint. However, contrast material was found in the tarsal sheath in 40% of limbs, adding yet another dimension to this already somewhat difficult blocking technique. False-negative results have been attributed to inadvertent injection into blood or lymphatic vessels.59 The clinician should take care in preparing the limb for this procedure and interpreting the results. It is possible, although not likely, that when a high plantar block is performed, local anesthetic solution could be inadvertently placed in the tarsometatarsal joint. A good chance also exists, however, of inducing analgesia of the tarsal sheath. Comprehensive evaluation using numerous imaging modalities is needed when attempting to differentiate causes of lameness in this important area.

Fig. 10-21 Positive contrast arthrogram of the tarsometatarsal joint showing short, distoplantar outpouchings extending distally toward the origin of the suspensory ligament. Inadvertent penetration of these pouches occurs during subtarsal or high plantar analgesic techniques.
The medial and lateral plantar and the medial and lateral plantar metatarsal nerves are blocked, and a circumferential dorsal ring block provides complete analgesia to the metatarsal region. Blocking only the plantar metatarsal nerves can abolish pain associated with the suspensory ligament. Most clinicians do not include the dorsal ring block, but it is necessary to do so to eliminate lameness resulting from injury of the dorsal cortex of the MtIII or to suture lacerations in this area. This block is performed most commonly and safely with the limb held off the ground. Although uncommon to rare, needle breakage is a complication during high plantar analgesia, and for this reason we prefer to use needles no smaller than 18 to 20 gauge and 4 cm long. At this level on the plantar aspect of the limb, it is impossible to palpate nerves, and unlike with the high palmar block, only one injection site exists for each, on the medial and lateral aspects of the limb. The needle is placed just distal to the tarsometatarsal joint and axial to the fourth metatarsal bone (MtIV) and inserted until contact is made with the MtIII (Figure 10-22). A minimum of 5 mL of local anesthetic solution is deposited at this deep location, and an additional 5 mL are deposited as the needle is withdrawn, leaving a definite bleb in the subcutaneous tissues. Some clinicians prefer lower volumes of local anesthetic solution. Additional local anesthetic solution can be used without risk, and a common modification is flooding the origin of the suspensory ligament with an additional 5 to 10 mL of local anesthetic solution. The procedure is then repeated medially, and the needle is inserted axial to the second metatarsal bone (MtII). To complete the block, a circumferential subcutaneous ring block is performed. The clinician must take care not to lacerate the dorsal metatarsal artery or the saphenous vein during this procedure.
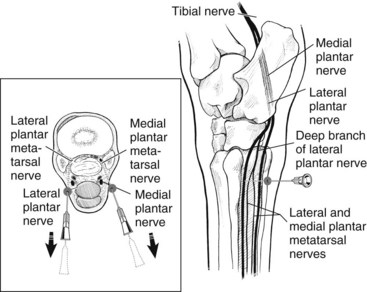
Fig. 10-22 The high plantar block is performed at a level 4 cm distal to the proximal aspect of fourth metatarsal bone and on the medial side 3 cm distal to the proximal aspect of second metatarsal bone. The needles are inserted axial to the respective splint bone and advanced deep to contact the plantar surface of the third metatarsal bone. Local anesthetic solution is deposited in this location to block the lateral (medial) plantar metatarsal nerves and in a more superficial position as the needle is withdrawn blocks the lateral (medial) plantar nerves (inset).
An alternative technique to alleviate pain from the proximal aspect of the suspensory ligament is to block the deep branch of the lateral plantar nerve. This can be performed with the limb bearing weight or lifted, according to personal preference. A 20-gauge needle is inserted perpendicular to the skin just plantar to the MtIV at the junction where its contour changes from oblique to vertical. The needle is inserted to a depth of approximately 1 cm, and 3 mL of local anesthetic solution are deposited. This block is quick and easy to perform and is generally well tolerated but may not remove pain associated with entheseous reaction.5 See the following text for a discussion of alternative techniques to block the suspensory origin.
Fibular (Peroneal) and Tibial Nerve Blocks
Analgesia of the distal crus and tarsus or entire distal aspect of the hindlimb is induced using the fibular and tibial nerve blocks. These blocks are used most commonly in horses with distal hock joint pain, in which intraarticular analgesia is difficult or impossible to perform. The fibular and tibial nerve blocks, when completed successfully, are more effective in eliminating pain from the complex hock joints than is intraarticular analgesia. The fibular and tibial nerve blocks also are useful in eliminating pain associated with subchondral trauma of the distal aspect of the tibia and talus, distally located tibial stress fractures, the tarsal sheath, the distal aspect of the common calcaneal tendon, the calcaneal bursa, and the plantar aspect of the hock. The clinician should keep in mind that if the high plantar block has not already been performed, the fibular and tibial nerve blocks eliminate pain associated with proximal suspensory desmitis.
The deep fibular nerve is blocked at a site located laterally, 10 cm proximal to the point of the hock (tuber calcanei), in the groove between the long and lateral digital extensor muscles (Figure 10-23). In this groove the superficial fibular nerve is easily palpated and can be rolled against the fascia of the crus. An 18- to 22-gauge, 4-cm needle is inserted to the hub or until it contacts the lateral tibial cortex, and 10 to 15 mL of local anesthetic solution are injected, beginning deep and continuing as the needle is withdrawn. The needle can be redirected in a fan-shaped pattern if desired to ensure complete block of the deep branch of the fibular nerve. Seeing blood in the needle hub is common, a reliable sign of accurate needle placement, because the cranial tibial vein and artery are located close to the deep fibular nerve.60 Performing the tibial block first is therefore preferable, as is warning the client that blood may appear.5 The superficial fibular nerve is blocked as the needle is withdrawn from deep within the injection site. Additional local anesthetic solution (5 to 10 mL) is placed in this subcutaneous location.
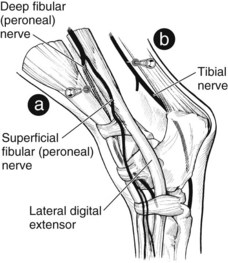
Fig. 10-23 Lateral view of the left crus and tarsus showing the fibular (peroneal) and tibial nerve block. The deep and superficial fibular nerves are blocked by finding the groove between the long and lateral digital extensor muscles, 10 cm proximal to the tarsus, in which the superficial fibular nerve is palpable. The needle (a) is advanced deep to block the deep branch and withdrawn to a more superficial position to deposit local anesthetic solution subcutaneously to block the superficial branch. The tibial nerve block (b) is performed by palpating the nerve just cranial to the common calcaneal tendon (from either a lateral or a medial approach) in a location about 10 cm proximal to the tuber calcanei.
The tibial nerve is blocked at a site 10 cm proximal to the tuber calcanei, cranial to the common calcaneal tendon, and caudal to the DDFT (see Figure 10-23). The nerve can be palpated as a firm cordlike structure with the limb in a flexed position. For this reason, performing this block may be easier with the limb not bearing weight. Although the tibial nerve is slightly more superficial medially, the injection can be performed either medially or laterally. A 20-gauge, 2.5-cm needle is inserted laterally, and 15 mL of local anesthetic solution are injected over the nerve. The needle tip should be palpated under the skin, medially, to ensure the proper depth of penetration. Local anesthetic solution can be placed using a fan-shaped injection technique, but the horse will object if the tibial nerve is penetrated. Although deep pain will be abolished if these nerves are successfully blocked, superficial sensation persists on the medial aspect and occasionally in the caudal (plantar) aspect of the limb. To use the fibular and tibial nerve blocks therapeutically, it is necessary to perform a circumferential subcutaneous ring block to completely abolish skin sensation. After the fibular and tibial nerve blocks, paradoxically, preexisting toe drag may persist or increase, despite resolution of weight-bearing lameness.5 Some horses stumble or knuckle, indicating loss of extensor muscle function, but this is not common and certainly not a necessary sign to suggest that complete analgesia has been obtained. However, exercising a horse at speed or over fences should be avoided. Because of nerve size and depth, we suggest that additional time be given, as much as 20 to 30 minutes, to evaluate the effect of this block before a final conclusion is reached. Dyson has recognized improvement in horses up to 1 hour after blocking and warns that proceeding with a stifle block too soon leads to false-positive results.5 The fibular and tibial nerve blocks are not commonly performed in practice, at least in the United States, and at best may result in only 50% to 80% improvement in lameness score, particularly in those horses with severe distal hock joint pain, although in some horses lameness is abolished completely. Allowing more time for maximal response and taking a realistic approach to the percent improvement expected are warranted when using the fibular and tibial nerve blocks. Intrasynovial analgesic techniques are certainly more specific than are the fibular and tibial nerve blocks, and although the fibular and tibial nerve blocks have limitations, the lameness diagnostician should become familiar and comfortable with this procedure. Proficiency in performing these blocks is a must for accurate diagnosis of hindlimb lameness. Performing the fibular and tibial components can independently improve specificity of the fibular and tibial nerve blocks.
Intraarticular Analgesia in the Hindlimb
Analgesia of the DIP and proximal interphalangeal joints in the hindlimb is exactly the same as that described for the forelimb. Performing intraarticular analgesia of the metatarsophalangeal joint is the same as that described for the metacarpophalangeal joint. Perineural analgesic techniques should be used whenever possible, because subchondral bone pain is more completely abolished with these techniques, and false-negative results are less likely.
Tarsus
Tarsometatarsal Joint
The most reliable site for arthrocentesis of the tarsometatarsal joint is a lateral approach, just proximal to the MtIV. At this site is a subtle but consistent depression that can reliably be palpated. A 20-gauge, 2.5-cm needle is inserted in a dorsomedial and slightly distal direction (Figure 10-24). The needle can usually be inserted to the hub, but occasionally it hits articular cartilage. Synovial fluid is consistently retrieved, but we find it interesting that even in horses without lameness of the tarsometatarsal joint, the fluid is generally watery, lacking what is thought to be normal viscosity. In most horses, up to 4 mL of local anesthetic solution can usually be injected without encountering elevated intraarticular pressures and horse discomfort. Be aware that beyond 2 mL the horse may start to feel uncomfortable, raise the limb, or even kick. Anecdotal reports of a subtle pop or sudden decrease in pressure have been attributed to communication between the tarsometatarsal and centrodistal (distal intertarsal) joints. In reality, this most often results from rupture of the tarsometatarsal joint capsule and subsequent deposition of local anesthetic solution (or medication) extraarticularly into the tarsal space and not the centrodistal joint. We recommend using no more than 4 mL of local anesthetic solution or injecting only that amount of local anesthetic solution necessary to develop moderate intraarticular resistance to avoid inadvertent deposition into the intertarsal space. Periarticular extravasation of local anesthetic solution from excessive volume may inadvertently block the nearby lateral plantar nerve and deep branch, potentially alleviating pain associated with the suspensory ligament attachment or other structures. An alternative site for tarsometatarsal arthrocentesis is a medial approach, similar to that described for the centrodistal joint.
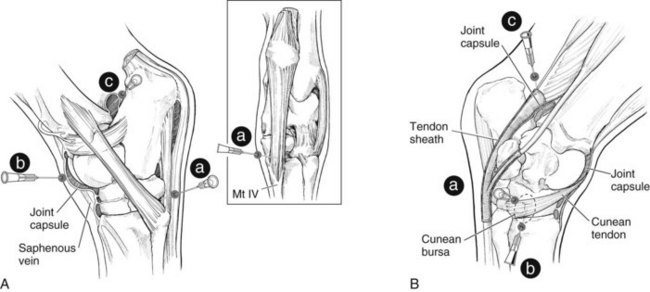
Fig. 10-24 A, Lateral and plantar (inset) views of the left tarsus showing sites for tarsal arthrocentesis. The tarsometatarsal joint is entered by locating the depression just proximal to the proximal aspect of the fourth metatarsal bone (Mt IV) and inserting a needle (a) in the plantar aspect of this depression, directing it dorsomedially. The dorsomedial pouch of the tarsocrural joint (b) is entered either just lateral or medial to the dorsal branch of the saphenous vein or, alternatively, using the plantarolateral pouch (c). B, Medial view of the left tarsus. The centrodistal joint is entered by placing the needle (a) in the depression formed between the fused first and second tarsal bones, the third tarsal bone, and the central tarsal bone, which is at the proximal edge or just slightly distal to the proximal edge of the cunean tendon. The cunean bursa (dashed ellipse) is entered by locating the distal border of the cunean tendon and inserting the needle (b) under the tendon from the distal aspect or placing it directly through the tendon. The distended tarsal sheath (c) can be entered proximal, just caudal to the tarsocrural joint capsule or distal (not shown) to the tarsus.
The issue of communication between the distal tarsal joints is important from diagnostic and therapeutic standpoints. Studies have shown that the tarsometatarsal and centrodistal joints communicate in 8% to 35% of normal horses.59,61,62 Communication between the tarsometatarsal joint (and presumably the centrodistal joint) and the talocalcaneal-centroquartal (proximal intertarsal) and tarsocrural joints was shown to be about 4% in an in vivo study, after injection of latex in the tarsometatarsal joint.62 Some concern and confusion exist regarding whether or not a single injection into the tarsometatarsal joint also provides analgesia or treats the centrodistal joint. Some clinicians even preferentially inject a large volume of local anesthetic solutions or drugs, hoping to block or medicate the tarsometatarsal and centrodistal joints. A recent in vitro study found that, although gross anatomic communications exist in only a minority of horses, diffusion of mepivacaine between the distal tarsal joints (as well as between the distal tarsal joints and the tarsocrural joint) occurs with a much higher frequency. Fifteen minutes after injection of 5 mL of 2% mepivacaine into either the tarsometatarsal or the centrodistal joint, mepivacaine was detected in the alternate joint at concentrations >300 mg/L in 64% and 60% of specimens, respectively.63 Whether or not this holds true in the live horse remains undetermined. For that reason, and based on our clinical experience, we believe the clinician should still consider the tarsometatarsal and centrodistal joints to be separate synovial cavities. However, it is clear that in some horses analgesia or treatment of the tarsometatarsal joint will relieve centrodistal joint pain. Because the tarsometatarsal joint has distoplantar outpouchings, abolishing pain associated with the proximal suspensory attachment or lesions involving the proximal aspect of the MtIII is also possible when performing tarsometatarsal analgesia. Accurate differential diagnosis for pain involving the lower hock joints and proximal metatarsal region depends on careful interpretation of response to diagnostic analgesia and evaluation of ancillary images.
Centrodistal Joint
Compared with the tarsometatarsal joint, arthrocentesis of the centrodistal joint is relatively difficult. The centrodistal joint is small, and in fact inserting a needle any larger than 22 to 25 gauge into this joint is difficult, even in horses with normal width of joint space. We have tried several alternative sites, including dorsomedial and dorsolateral approaches. Anecdotal reports suggest that the dorsomedial approach, about 1 cm distal to the distal end of the medial trochlear ridge, is a consistent, reliable injection site, but we often enter the proximal intertarsal joint from this approach. An outpouching of the centrodistal joint exists dorsolaterally, but we reasoned that the perforating tarsal artery precluded use of this site in vivo. A recent study described the use of this dorsolateral approach. The site is identified as a point 2 to 3 mm lateral to the long digital extensor tendon and 6 to 8 mm proximal to a line drawn perpendicular to the long axis of the MtIII at the level of the proximal aspect of the MtIV. The success rate for arthrocentesis at this site was equal to that for the traditional medial approach, with purported advantages being improved safety for the clinician and easily identified landmarks. In vivo, iatrogenic injury to the dorsal pedal artery or penetrating tarsal artery was not encountered.64
We still preferentially use a medial approach at the distal aspect of, or through, the cunean tendon (medial tendon of insertion of the tibialis cranialis muscle), a structure that can be readily palpated. With a fingertip, the distal edge of the cunean tendon is moved proximally to reveal an ill-defined concavity, the articulation of the fused first and second tarsal bones, with the third and central tarsal bones (see Figure 10-24). This depression is sometimes located in a slightly more proximal location. This injection technique is one of the few commonly performed by standing on the opposite side of the horse. A skin bleb is useful because in most horses inserting a needle directly into the joint is difficult, and numerous attempts may be necessary. A 22- to 25-gauge, 2.5-cm needle is inserted directly in a lateral direction, horizontally, roughly parallel to the central and third tarsal articulation, perpendicular to the skin. Slight redirection of the needle may be necessary, and in many horses joint fluid is not obtained. If the needle can be inserted to a depth of 1 to 1.5 cm, it is likely properly positioned even if synovial fluid cannot be retrieved. Fluid retrieved in a more superficial location likely indicates penetration of the cunean bursa. In horses in which diagnostic information or therapeutic injection is critical and any question of needle placement exists, radiographs are warranted. A maximum of 4 to 5 mL can be injected. If a larger volume can be comfortably injected, the needle tip is likely in the tarsal space or in the proximal intertarsal joint, or a communication with the tarsometatarsal joint exists. If the injection is difficult to perform, the needle is likely malpositioned in the subcutaneous tissues, or the needle tip is touching articular cartilage. Most clinicians attempt injection of the centrodistal joint after first injecting the tarsometatarsal joint, and in some instances, medication or local anesthetic solution readily flows from the needle. The typical response is, “There must be a communication between the tarsometatarsal and centrodistal joints.” However, this clinical finding most often results from inadvertent penetration of the distended medial pouch of the tarsometatarsal joint. Fluid accumulation in the tarsal space from the tarsometatarsal joint injection can cause the same result, if the needle enters the tarsal space rather than the centrodistal joint space.
In horses with advanced osteoarthritis or even in horses with early distal hock joint pain, it may be difficult or impossible to be confident that intraarticular analgesia has been achieved. An alternative approach for providing tarsal analgesia is first to perform sequential, intraarticular analgesia of the tarsometatarsal and tarsocrural joints, and then to perform the fibular and tibial nerve blocks if lameness persists. If lameness abates after the fibular and tibial nerve blocks, a presumptive diagnosis of centrodistal joint pain can be made, assuming other sources of pain abolished by this block can be ruled out.
Tarsocrural Joint
Arthrocentesis of the tarsocrural joint is straightforward and easy compared with some joints, because of extensive and multiple dorsal and plantar outpouchings. In horses with moderate to severe effusion, identifying four distinct outpouchings—the dorsolateral, dorsomedial, plantarolateral, and plantaromedial pouches—is easy. The clinician must keep in mind that the tarsocrural and proximal intertarsal joints communicate through a large fenestration at the dorsal aspect of the joints in adult horses, although in weanlings and yearlings the fenestration often cannot be seen during arthroscopic examination. Any one of the tarsocrural joint pouches can be used, but the most common site of entry is on either side of the saphenous vein, in the dorsomedial pouch (see Figure 10-24). This particular site is preferred in horses without obvious effusion. An alternative site is the plantarolateral pouch. The most consistent site to use is the distal aspect of the dorsomedial pouch, just distal to the medial malleolus of the tibia and medial to the saphenous vein. An 18- to 20-gauge, 2.5- or 4-cm needle is used to deposit 20 to 30 mL of local anesthetic solution into the tarsocrural joint. In horses with severe osteoarthritis of the tarsocrural joint or those with subchondral bone pain, use of as much as 30 to 50 mL of local anesthetic solution is necessary to abolish pain. In these horses, a false-negative result is common if only 10 to 20 mL of local anesthetic solution is used.
The plantar pouches can be useful alternative sites for arthrocentesis if the dorsomedial pouch is unsuitable, as sometimes occurs with a wound, swelling associated with trauma of the fibularis (peroneus) tertius, or superficial dermatitis. The plantar pouches must be differentiated from distention of the tarsal sheath or other forms of thoroughpin. Although the dorsal and plantar pouches freely communicate, anatomically, flushing from one aspect of the tarsocrural to the other when the horse is in a weight-bearing position may be difficult. Fluid flow between articular surfaces and joint spaces under collateral ligaments is likely restricted when horses are in a weight-bearing position. This same phenomenon occurs in other joint spaces.
Stifle Joint
The three compartments of the equine stifle joint are the medial femorotibial, lateral femorotibial, and femoropatellar joint compartments. Most consider that the femoropatellar and medial femorotibial joints communicate in almost all horses and that the lateral femorotibial compartment is solitary, but recent anatomical studies have shed new light on this time-honored concept. The frequency of communication between the medial femorotibial and femoropatellar compartments was found to be 60% to 74% in normal horses when the injection was performed from the femoropatellar compartment.65,66 The frequency of communication was higher (80%) when the injection was performed in the medial femorotibial compartment.65 It is important to realize, however, that the medial femorotibial and femoropatellar compartments did not communicate in all horses. Inconsistency in communication depending on which compartment was injected was attributed to directionality in the normal foramen or slit between the two compartments (flow easier from the medial femorotibial to the femoropatellar compartment).
The time-honored assumption that the lateral femorotibial joint is a solitary compartment was also challenged. The lateral femorotibial joint communicated with the femoropatellar joint in 3% to 18% of horses but was indeed solitary in the majority of normal horses.65,66 Communication may be more frequent after trauma and certainly after arthroscopic surgical procedures.
Similar to the digit, carpus, and tarsus, there is clinically important evidence that mepivacaine diffuses between the compartments of the stifle joint. The proportion of synovial compartments with mepivacaine concentration >300 mg/L 15 minutes after injection of an adjacent compartment with 10 mL of 2% mepivacaine ranged from 5% to 40%.63 Of note, functional (diffusion) communication between the medial femorotibial and femoropatellar joints was lower than previous estimates (25% to 40% versus 60% to 80%). Volume of local anesthetic solution (10 mL) was considerably lower than is commonly used in clinical practice for intraarticular analgesia of the stifle joints, and it remains undetermined if results of in vitro studies translate to actual clinical relevance.
We recommend that each compartment of the stifle joint be injected independently, either sequentially or simultaneously, to avoid confusing results during stifle analgesia. The variable degree of communication will obviously cause some degree of uncertainty in diagnosis. The same principle is recommended for therapy as well. Needle insertion in the stifle joints is complicated by a natural tendency of horses to react inappropriately to manipulation compared with other areas of the limbs. Horses seem to object to simple palpation of the stifle and may become fractious during arthrocentesis. To avoid excessive manipulation during injection, we have found it useful to attach an extension set to the needle, a procedure that obviates the need to touch the needle or skin when attaching the syringe. If necessary, the extension set may be useful for many diagnostic procedures, particularly in the hindlimbs. In general, 20 to 30 mL of local anesthetic solution are used in each of the medial femorotibial, lateral femorotibial, and femoropatellar compartments. A common misconception is that long needles are needed to perform arthrocentesis of the stifle joint compartments. In fact, some racehorse trainers will insist that “the long needles, Doc” are necessary to achieve success in medicating the femoropatellar joint. If arthrocentesis is performed with the limb in a weight-bearing position, the joint capsules can easily be penetrated with needles no longer than 4 cm. In the flexed position, use of a spinal needle when performing femoropatellar arthrocentesis is necessary. We prefer to have the horse in a weight-bearing position, with the limb slightly ahead of the contralateral limb, a position that allows the clinician to palpate landmarks readily without undue tension on patellar and collateral ligaments.
Arthrocentesis of the medial femorotibial joint is performed at a site located just caudal to the medial patellar ligament, cranial to the medial collateral ligament, and 1 to 2 cm proximal to the medial tibial plateau (Figure 10-25). In a normal horse a distinct depression occurs at this location, but in horses with effusion, a considerable bulge in the joint capsule can be present. An 18-gauge, 4-cm needle is inserted perpendicular to the skin and can be redirected or rotated if synovial fluid is not immediately retrieved. A common mistake is to insert the needle too far distally, and in this position the needle tip enters ligaments or the medial meniscus.
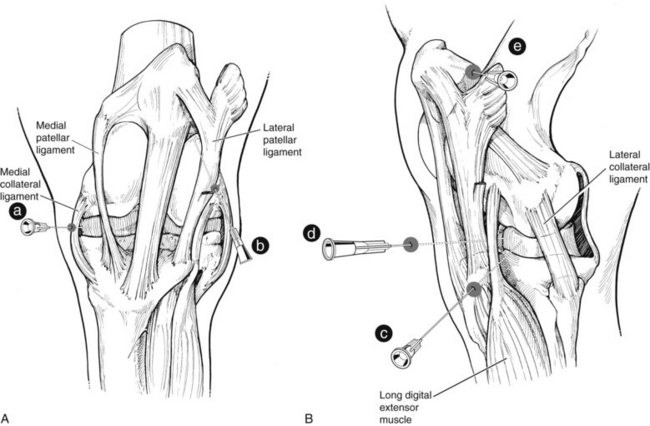
Fig. 10-25 A, Cranial view of the left stifle. The medial femorotibial joint (a) is approached from a site between the medial patellar and medial collateral ligaments, about 2 cm proximal to the proximal aspect of the tibia. The femoropatellar joint (b) most commonly is injected either between the lateral and middle patellar ligaments or between the middle and medial patellar ligaments (not shown). The needle is directed proximally in this subpatellar position. B, Lateral view of the left stifle. The lateral femorotibial joint can be approached by placing the needle caudal to the long digital extensor tendon and cranial to the lateral collateral ligament (c) or inserting it between the lateral patellar ligament and the cranial edge of the long digital extensor tendon (d). An alternative site for arthrocentesis of the femoropatellar joint (e) can be used by passing the needle through the lateral femoropatellar ligament.
Arthrocentesis of the lateral femorotibial joint is more challenging than for the other two compartments, because the lateral joint pouch is small and located deep within tissue. The site is caudal to the long digital extensor tendon and cranial to the lateral collateral ligament, just proximal to the lateral tibial plateau (see Figure 10-25). These landmarks are easily palpated, but distention of the joint capsule is not, in contrast to the medial femorotibial joint. An 18-gauge, 4-cm needle is inserted horizontally and directed in a slight caudomedial direction. Retrieval of synovial fluid varies, and redirecting or rotating the needle is often necessary. An alternate site can be used, located caudal to the lateral patellar ligament and cranial to the long digital extensor tendon, and just proximal to the tibial plateau.
Arthrocentesis of the femoropatellar joint is most commonly performed at a sub-patellar site and either lateral or medial to the middle patellar ligament. The joint capsule can be easily palpated even in most normal horses, if the horse is in a weight-bearing position. With the horse in a weight-bearing position, an 18-gauge, 4-cm needle is inserted perpendicular to the skin, or directed slightly proximally, until joint fluid is obtained or the needle tip contacts articular cartilage of the distal femur (see Figure 10-25). The clinician does not need to angle the needle sharply proximally using this technique. What is sometimes frustrating is that even in horses with obvious femoropatellar effusion, a steady flow of synovial fluid cannot be obtained, and attempting aspiration of fluid with a syringe is seldom helpful, because synovial villi readily plug the needle, making aspiration impossible. Some clinicians perform femoropatellar arthrocentesis with the limb in a non–weight-bearing position, in which case a 9-cm spinal needle is used and the needle is directed proximally, between the patella and distal aspect of the femur. An alternative lateral approach to the femoropatellar joint has been described.67 An 18-gauge, 4-cm needle is inserted into the lateral cul-de-sac of the femoropatellar compartment, located about 5 cm proximal to the lateral tibial plateau, caudal to the lateral patellar ligament and the lateral trochlear ridge of the femur. The needle is directed perpendicular to the long axis of the femur until bone is contacted (about 1.5 to 2 cm in most horses) and then is withdrawn slightly until synovial fluid is collected. Proposed advantages of this approach are a reduced potential for iatrogenic injury to the articular cartilage and more reliable recovery of synovial fluid compared with the subpatellar approach.68
Coxofemoral (Hip) Joint
Although the coxofemoral joint is relatively large and the landmarks for needle insertion are consistent, injection is considered to be a daunting task. Few of us perform this injection technique on a regular basis, and depth of penetration makes accurate needle placement difficult. An 18-gauge, 15-cm (6-inch) spinal needle is adequate for all but the largest of draft horses. A needle of this length should be inserted carefully, and if the horse is moving or fractious, it may be necessary to provide sedation. The site is in the angle formed between the long caudal and short cranial processes of the greater trochanter of the femur (Figures 10-26 and 10-27). This site can be difficult to palpate in heavily muscled horses, and ultrasonographic evaluation can be useful to identify the injection site. The most difficult landmark to palpate consistently, but an important one nonetheless, is the cranial process. The site is between the two processes, closer to the cranial process and not caudal to the trochanter.
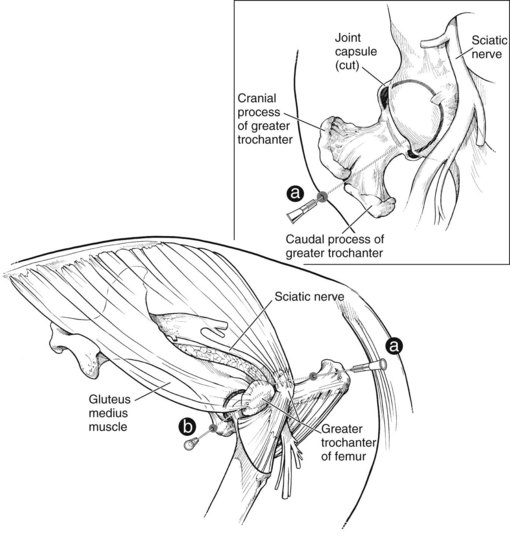
Fig. 10-26 Lateral and dorsal (inset) views of the left coxofemoral joint. Arthrocentesis of the coxofemoral joint is performed by inserting the needle (a) in the angle formed between the caudal and cranial processes of the greater trochanter of the femur. The needle is inserted slightly cranially, distally, and medially just dorsal to the shaft of the femoral neck (inset). This view (b) shows the seldom used diagnostic technique of synoviocentesis of the trochanteric bursa.

Fig. 10-27 Arthrocentesis of the right coxofemoral joint. Using an extension set between needle and syringe, a technique that reduces the amount of manipulation necessary during the procedure, facilitates arthrocentesis of this and other joints.
Before the needle is inserted, blocking the injection site may be useful. Because the shaft of the needle is handled, sterile gloves are recommended. Needle direction is important. The needle is inserted in a slightly craniomedial direction and slightly distally and directed just dorsal to the femoral neck, until the joint capsule is penetrated. In most horses, a subtle pop can be felt as this occurs. “Walking” the needle off the femoral neck may be useful, using the bone as a guide to the coxofemoral joint. In most adult light-breed horses, this occurs within 3 to 5 cm of the hub of the needle. Synovial fluid is reliably retrieved from the coxofemoral joint, spontaneously or by aspiration. A large volume of local anesthetic solution should not be injected if synovial fluid is not readily obtained, but injecting a small volume and attempting retrieval with a syringe is useful. It is possible inadvertently to inject local anesthetic solution around the sciatic nerve, causing temporary paresis, if the needle is caudally malpositioned, and therefore local anesthetic solution should not be injected if any doubt exists that the needle is correctly positioned. The amount of local anesthetic solution used is 25 to 30 mL. Most horses are evaluated in 20 to 30 minutes, but in horses with fractures of the acetabulum the clinician should expect only 50% improvement in lameness score, and improvement may be short-lasting (15 to 30 minutes). An alternative ultrasound-guided technique has been described and is particularly valuable in large overweight horses in which the landmarks are difficult to palpate.69
Analgesia of Hindlimb Bursae and Tendon Sheaths
Analgesia of the navicular bursa and DFTS in the hindlimb is the same as in the forelimb.
Cunean Bursa
Occasionally, injecting the cunean bursa is necessary to assess the role of the cunean bursa and tendon in horses with distal hock joint pain, to perform cunean tenectomy, or to medicate the structure. The cunean bursa is seldom the sole source of distal hock joint pain but can play a role, so analgesia or medication of this structure is sometimes combined with other injections.
The cunean bursa is between the distal tarsal bones and the medial branch of the cranialis tibialis tendon (called the jack tendon or cord) but is seldom palpable (see Figure 10-24). The distal aspect of the cunean tendon is usually easily palpated, however, by starting at the distal aspect of the hock and sliding the fingertip in a proximal direction. Retrieving synovial fluid is unusual but possible, but during injection the clear outline of the bursa can be seen as it distends. A 20- to 22-gauge needle is inserted deep to the distal edge of the cunean tendon and directed in a proximal direction, and 3 to 5 mL of local anesthetic solution is injected. We prefer this approach, but alternatively the needle can be inserted perpendicular to the skin and directly through the tendon itself until bone is contacted.
Tarsal Sheath
Analgesia of the tarsal sheath is performed to confirm the structure as a source of lameness associated with traumatic and infectious tenosynovitis (although the response may be limited in the face of infection) and various osseous lesions, such as those involving the sustentaculum tali, or unusual exostoses (osteochondroma). The tarsal sheath surrounds the DDFT from a point approximately level with the tuber calcanei and extends to a point 2 to 3 cm distal to the tarsometatarsal joint. Distention of the tarsal sheath is commonly called thoroughpin, but occasionally thoroughpin appears as fluid swelling proximal to the tarsus that does not involve the tarsal sheath. The DDFT is located medial to the calcaneus as it crosses the sustentaculum tali. The heavy tarsal retinaculum medially and the calcaneus laterally restrict outpouching of the tarsal sheath to the proximal and distal aspects. The clinician should take care to differentiate tarsal sheath effusion from distention of the plantar pouches of the tarsocrural joint. A 20-gauge, 2.5-cm needle is used to inject 10 to 15 mL of local anesthetic solution.
Calcaneal Bursa
Indications for analgesia of the calcaneal bursa include traumatic and infectious bursitis, tendonitis of the gastrocnemius or SDFT at this level, and osseous lesions of the tuber calcanei. The bursa is located between the SDFT and tuber calcanei. Proximal to the tuber calcanei, the bursa is interposed between the SDFT and the gastrocnemius tendon. When distended, an unusual clinical finding, the bursa is palpable as medial and lateral outpouchings just proximal to the tuber calcanei. Smaller outpouchings are often discernable just distal to the tuber calcanei but are inconsistent. The bursa can be accessed for injection at any of these outpouchings. A 20- to 22-gauge, 2.5- or 4-cm needle is used to inject 10 mL of local anesthetic solution, after retrieval of fluid for analysis if indicated. Pain may take 20 to 30 minutes to abate in horses with osseous lesions or with severe lameness.
Trochanteric Bursa
Seldom does an indication exist to block the trochanteric bursa, although injections in this region are commonly performed to manage bursitis and muscle pain (see Chapter 47). The trochanteric bursa is located between the tendon of insertion of the gluteus accessorius muscle and the cranial process of the greater trochanter of the femur (see Figure 10-26; see also Chapter 47). In normal horses this bursa is small and likely has minimal synovial fluid. Synoviocentesis is performed using an 18- to 20-gauge, 4-cm needle, although in larger, more heavily muscled horses, a longer needle may be necessary. The needle is inserted perpendicular to the skin, directly over the cranial aspect of the greater trochanter until contact with bone is made. We have had difficulty retrieving fluid even in lame horses that have a positive response to analgesia. Generally, 5 to 10 mL of local anesthetic solution are injected until pressure is felt. If local anesthetic solution can be aspirated, the needle was likely in the bursa, but if not, the injection was likely performed in the surrounding tissues.
Local Infiltration in the Forelimb and Hindlimb
Local infiltration of local anesthetic solution in painful soft tissues or over painful bony swellings can be performed at any location, although some areas deserve special mention. Any localized area of pain, into which a needle can be inserted safely, is fair game for local analgesia.
The clinician must be aware, however, that local infiltration may not provide total analgesia to the region, mostly because the entire nerve supply to the region cannot be blocked. Incomplete analgesia is common in horses with bony lesions, such as bucked shins, because deep pain from the cortex of the McIII is difficult if not impossible to eliminate using subcutaneous infiltration of local anesthetic solution. In most instances, perineural analgesia for this particular condition is preferred. Local infiltration is performed in many horses in lieu of perineural technique, or in horses in which perineural analgesia has localized pain to a general region, but conflicting or numerous clinical problems exist. An advantage of local infiltration is that proprioception is not lost, and horses can be moved at speed for reevaluation after this form of analgesia. Efficacy can be assessed by deep, direct digital palpation, to confirm that the previously identified source of pain was eliminated by local analgesia.
Splints
A common suspected cause of lameness in many horses are exostoses associated most commonly with the second (McII) and fourth (McIV) metacarpal bones or the MtII or MtIV, or in combination with the McIII or MtIII. A 20- to 22-gauge, 2.5- to 4-cm needle is used to deposit 5 mL of local anesthetic solution subcutaneously over the painful exostosis. The needle is slid directly alongside the proliferative lesion, between skin and bone. For splints involving the McII or MtII and the McIV or MtIV, it is important to deposit local anesthetic solution abaxial and axial (between the suspensory ligament and splint bones) to the lesion. In some horses proliferative changes involve only the axial aspect of the McII, MtII, McIV, or MtIV (blind splints), and it is critical to block in this location. In others with primary proliferation between the McII or MtII, McIV or MtIV, and the McIII or MtIII, subcutaneous injection will suffice. When local anesthetic solution is infiltrated on the axial aspect of the splint bones, the palmar or plantar metacarpal or metatarsal nerves are likely blocked, making it possible to abolish pain from a more distal site and leading to misinterpretation of results. In horses with extensive adhesions between the axial aspects of the McII or MtII and the McIV or MtIV, the suspensory ligament pain may be incompletely abolished using a local infiltration technique, and the palmar or plantar nerves and palmar or plantar metacarpal or metatarsal nerves above the site may need to be blocked individually for pain to be abolished.
Suspensory Ligament Origin
Local infiltration or flooding the palmar metacarpal or plantar metatarsal regions at the origin of the suspensory ligament is often done in lieu of perineural analgesia, as described previously. This is also referred to by some as a subtarsal or subcarpal block. An 18- to 22-gauge, 2.5- to 4-cm needle can be used to distribute 5 to 15 mL of local anesthetic solution in a fan-shaped pattern, usually from a lateral injection site just axial to the McIV or MtIV. It is important to use adequate restraint and have the limb in a flexed position when performing this technique. In the hindlimb an 18- to 19-gauge needle should be used to minimize the potential for needle breakage, should the horse kick during the procedure.
False-positive results, attributed to inadvertent analgesia of palmar metacarpal or plantar metatarsal nerves, penetration of the distal outpouchings of the carpometacarpal and tarsometatarsal joints, or penetration of the tarsal sheath can occur.25,56 Compared with high palmar analgesia, the incidence of inadvertent injection of the distal palmar outpouchings of the carpometacarpal joint was highest when local infiltration of the suspensory origin was performed.25 A single injection technique was recently developed for diagnostic analgesia of the suspensory ligament origin in the hindlimb that should both limit the incidence of the previously mentioned complication, and also may be more specific for pain originating from the origin of the suspensory ligament. The technique involves blocking the deep branch of the lateral plantar nerve. The clinician holds the limb with the stifle and tarsus at 90 degrees of flexion and with the digit fully flexed. While the SDFT is deflected medially, a 2.5-cm needle is inserted to the hub, perpendicular to the skin, at a site 15 mm distal to the proximal aspect of the MtIV on the plantarolateral aspect of the limb. The needle is advanced between the lateral aspect of the SDFT and MtIV, at which point local anesthetic solution is injected.70 It is important to understand that from the deep branch of the lateral plantar nerve originate the lateral and medial plantar metatarsal nerves that continue distally, axial to the MtIV and MtII, to provide important innervation to the fetlock joint (see previous discussion). Failure to eliminate fetlock region pain by first performing low plantar analgesia could lead to erroneous interpretation of the results of analgesia of the deep branch of the lateral plantar nerve. If only the deep branch of the lateral plantar nerve is blocked, a diagnosis of proximal plantar metatarsal pain could be made even though fetlock region pain could be the true source of pain causing lameness.
Curb
Curb, the term used for swelling of the distal, plantar aspect of the tarsus, is a complex condition involving SDF tendonitis, long plantar desmitis, subcutaneous swelling, or various combinations of these soft tissue injuries (see Chapter 78). Local infiltration can partially abolish pain associated with curb and usually involves depositing local anesthetic solution subcutaneously. Completely blocking deep pain associated with the long plantar ligament or SDFT is not possible without using the fibular and tibial nerve blocks. A tibial nerve block may be more specific.5 A 20-gauge, 2.5- to 4-cm needle is used to inject 15 to 20 mL of local anesthetic solution with the limb in a flexed position. Adequate restraint and the help of an assistant are mandatory. Local anesthetic solution is infiltrated subcutaneously along the plantar, medial, and lateral aspects of the swelling, but deep injection into or between the SDFT and long plantar ligament is avoided. The medial injection is most comfortably and safely performed by standing on the opposite side of the horse.
Dorsal Spinous Process Impingement
Infiltration of local anesthetic solution around impinging dorsal spinous processes is a technique that is performed when attempting to confirm or rule out lameness or poor performance associated with back pain caused by impingement or other pain originating from the dorsal spinous processes of the thoracolumbar vertebrae.71 The horse is usually evaluated under saddle or in harness or on a lunge line, because lameness associated with this condition may be subtle and only manifested under these conditions. The hair along the dorsal midline is clipped, and the site or sites are prepared aseptically. We prefer to use 22-gauge, 9-cm spinal needles, although in most instances shorter needles can easily reach the tops of the dorsal spinous processes. Needles are inserted on the dorsal midline and directed ventrally to the dorsal spinous processes or the interspinous space. Markers placed after scintigraphic or radiographic examination are helpful to determine the precise location for blocking or to administer medication. The interspinous space can be located by redirecting the needle in a cranial or caudal direction. If impingement of the dorsal spinous processes exists, it may be impossible to infiltrate between them, but placing local anesthetic solution around the processes is satisfactory.5 Seven to 10 mL (per site) of local anesthetic solution are deposited as the needle is slowly withdrawn, and the horse is reevaluated 10 to 15 minutes later.
Using ultrasound guidance, intraarticular or periarticular injections of the cervical, thoracic, or lumbar facet joints can be performed using a 9-cm spinal needle. Injection techniques for the sacroiliac joints are described in Chapters 50 and 51.
Orthopedic Implants
Occasionally, pain associated with orthopedic implants is suspected to cause lameness. This is most commonly seen in horses after distal McIII or MtIII condylar fracture repair but can occur after repair of proximal phalanx or olecranon process fractures. Low-grade lameness is most common. Differentiating pain arising from negative interaction of implants with bone or surrounding soft tissue is nearly impossible based on the results of any diagnostic analgesia technique, because innervation to the joint or surrounding tissues is complex. Local anesthetic solution can be injected around screw heads, next to pins and wires or bone plates, and the horse is then reevaluated. Because lameness is often subtle, improvement is often difficult to judge. A combination of clinical findings and those from ancillary diagnostic techniques is used to determine the role of implant pain.