CHAPTER 61 Anterior abdominal wall
The anterior abdominal wall extends from the costal margins and xiphoid process superiorly to the iliac crests, pubis and pubic symphysis inferiorly. It overlaps and is connected to both the posterior abdominal wall and paravertebral tissues. It forms a continuous but flexible sheet of tissue across the anterior and lateral aspects of the abdomen. The anterior abdominal wall is composed of the integument, muscles and connective tissue lining the peritoneal cavity (Figs 61.1-61.5). It has an important role in maintaining the form of the abdomen and is involved in many physiological activities. Anterior abdominal wall tissues form the inguinal canal that connects the abdominal cavity to the scrotum in men or labia majora in women, and also form the umbilicus; both of these sites are of considerable clinical importance.
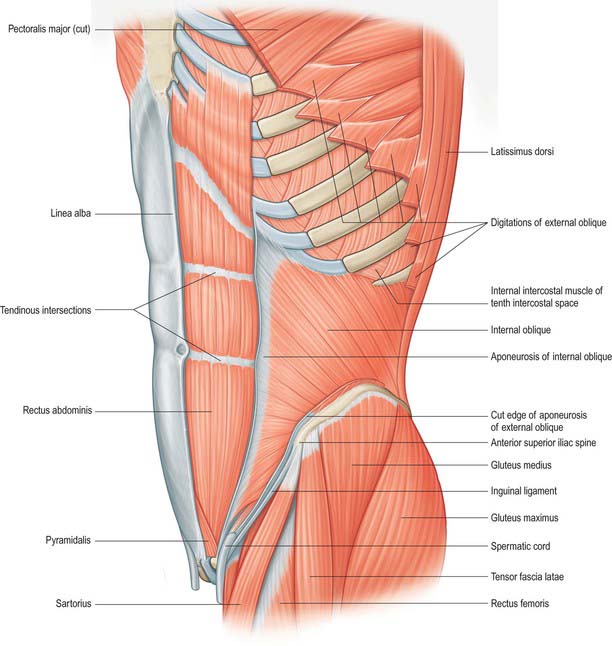
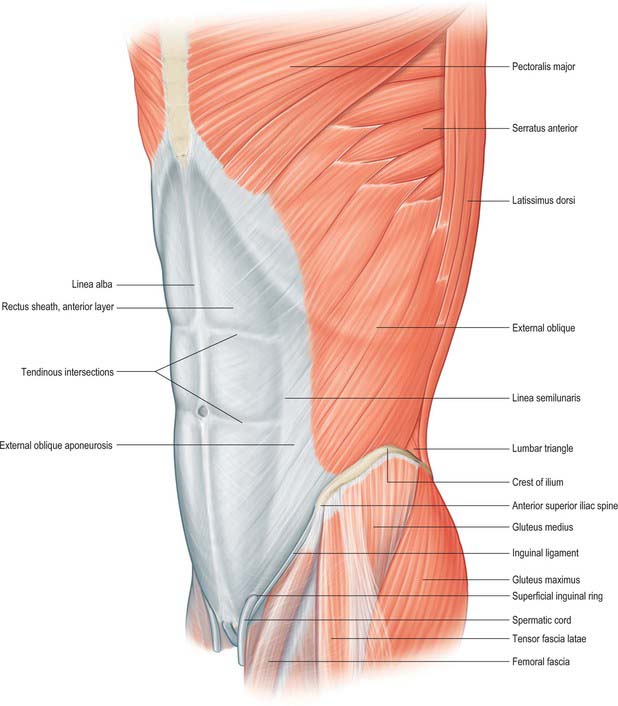
Fig. 61.2 Muscles of the left side of the trunk. External oblique has been removed to show internal oblique, but its digitations from the ribs have been preserved. The sheath of rectus abdominis has been opened and its anterior lamina removed.
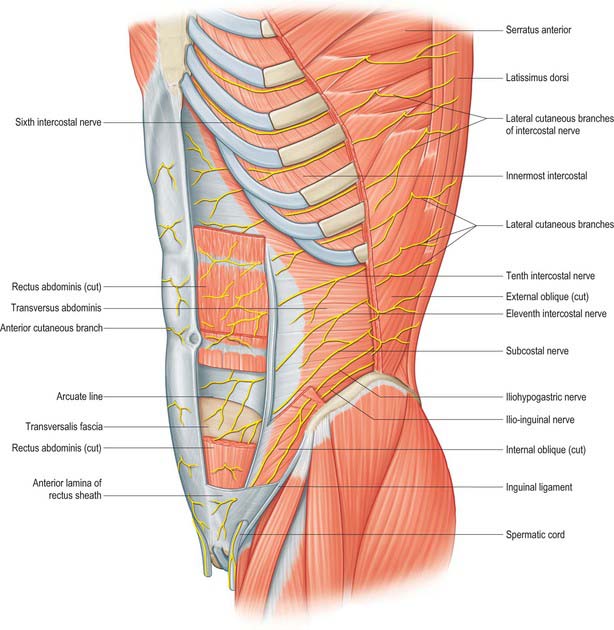
Fig. 61.3 The cutaneous branches of the lower intercostal and lumbar nerves. Portions of the muscles of the anterior abdominal wall have been removed, including most of the anterior layer of the rectus sheath and parts of rectus abdominis.
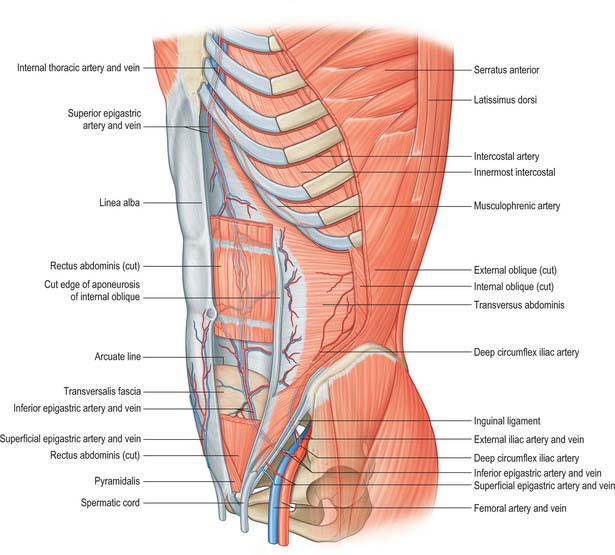
Fig. 61.4 Deep muscles and arterial supply of the anterolateral abdominal wall. The greater part of the left rectus abdominis has been removed to show the superior and inferior epigastric vessels.
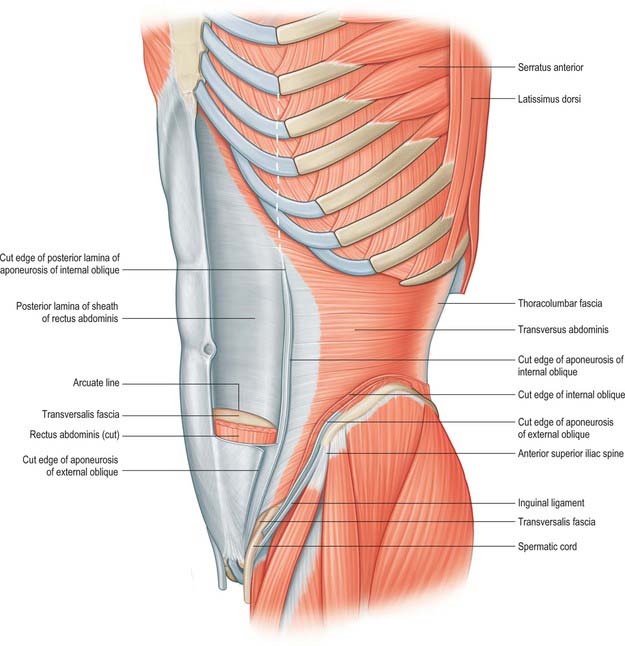
Fig. 61.5 Left transversus abdominis. The aponeurosis of transversus abdominis fuses into the posterior layer of the rectus sheath above the arcuate line. The position of lateral border of rectus abdominis is shown by the white dotted line.
SKIN AND SOFT TISSUE
The integument of the anterior abdominal wall comprises skin, soft tissues, lymphatic and vascular structures, and segmental nerves. The outer layer is formed from the skin and subcutaneous fat. The skin is non-specialized and variably hirsute, depending on the sex and race. All post-pubertal individuals have some extension of the pubic hair onto the anterior abdominal wall skin, although this is commonly most pronounced in males, in whom the hair may extend almost up to the umbilicus in a triangular pattern. The subcutaneous fat of the abdominal wall is highly variable in thickness and is one of the areas where excess fat is stored during periods of obesity, particularly in males.
VASCULAR SUPPLY AND LYMPHATIC DRAINAGE
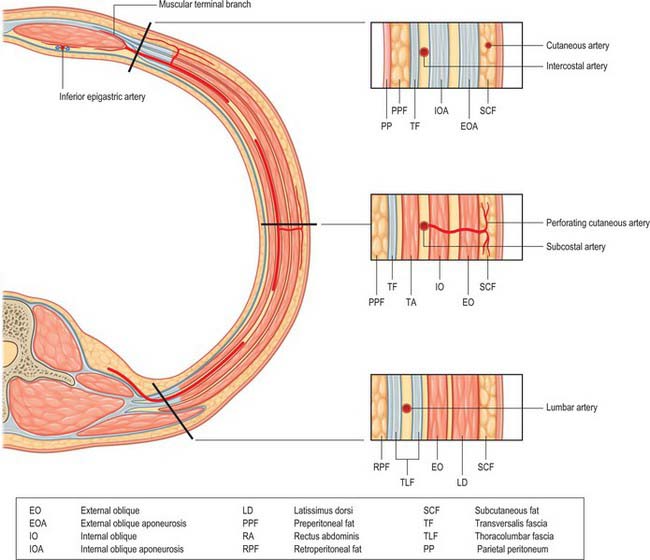
The anterior abdominal wall receives its blood supply from paired superior and inferior epigastric arteries running vertically through the tissues, and from paired posterior intercostal, subcostal and lumbar vessels running obliquely around the anterolateral aspects of the abdomen.
Superior epigastric artery and veins
The superior epigastric artery is a terminal branch of the internal thoracic artery. It descends between the costal and xiphoid slips of the diaphragm, accompanied by two or more veins (Fig. 61.4). The vessels pass anterior to the lower fibres of transversus thoracis and the upper fibres of transversus abdominis. The artery enters the rectus sheath behind rectus abdominis and runs down to anastomose with the inferior epigastric artery usually above the level of the umbilicus. Branches supply rectus abdominis and perforate the sheath to supply the abdominal skin. A branch given off in the upper rectus sheath passes anterior to the xiphoid process of the sternum and anastomoses with the same contralateral branch. This vessel may give rise to troublesome bleeding during surgical incisions that extend up to and alongside the xiphoid process. The superior epigastric artery supplies small branches to the anterior part of the diaphragm. On the right, small branches reach the falciform ligament, where they anastomose with branches arising from the hepatic artery.
Inferior epigastric artery and veins
The inferior epigastric artery originates from the external iliac artery posterior to the inguinal ligament (Fig. 61.6). Its accompanying veins, usually two, drain into the external iliac vein. It curves forwards in the anterior extraperitoneal tissue and ascends obliquely along the medial margin of the deep inguinal ring. It lies posterior to the spermatic cord, but is separated from it by the transversalis fascia. It pierces the transversalis fascia which forms the flimsy posterior support of rectus abdominis, and ascends between the muscle and the fascia and overlying pre-peritoneal connective tissue. In this part of its course, it raises the parietal peritoneum of the anterior abdominal wall as the lateral umbilical fold but has little supporting tissue posteriorly. Disruption of the artery, by surgical incisions e.g. for laparoscopic ports or drains, is not uncommon and the resulting haematoma may expand to considerable size because of the lack of tissue against which the bleeding is effectively compressed. The artery divides into numerous branches. Those which anastomose with branches of the superior epigastric artery do so posterior to rectus abdominis at a variable height above the umbilicus. The inferior epigastric vessels are usually significantly larger than the superior vessels and provide the ‘dominant’ supply to rectus abdominis. Preparatory ligation of the inferior epigastric artery is often performed for myo(cutaneous) flaps using the mid or lower rectus abdominis based on the superior epigastric artery to allow expansion of the superior arterial flow to improve viability of the flap. Branches anastomose with terminal branches of the lower six posterior intercostal arteries posterior to rectus abdominis at the lateral border close to the sheath. The artery is an important inferomedial relation of the deep inguinal ring, and may be damaged during extensive medial dissection of the deep ring during hernia repair, particularly when this is performed in the preperitoneal plane. The vas deferens in the male, or round ligament in the female, wind laterally round it. It has the following branches: the cremasteric artery, a pubic branch, and muscular and cutaneous branches.
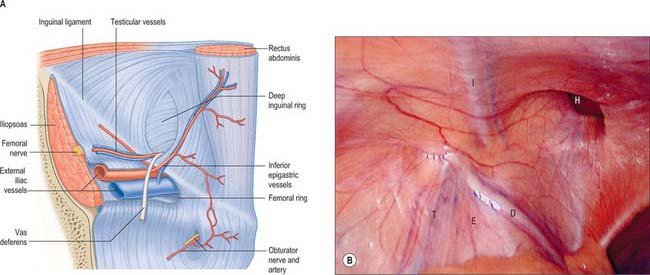
Fig. 61.6 A, The deep aspect of the lower part of the abdominal wall of the left side with the thinner posterior wall of the rectus sheath. The femoral and deep inguinal rings are displayed, together with the vessels and other structures in relation to them and also the opening into the obturator canal. B, Laparoscopic view showing the parietal peritoneum covering the area. I, inferior epigastric vessels; H, hernia orifice; D, ductus deferens; T, testicular vessels; E, external iliac vessels.
(B From Drake, Vogl and Mitchell 2005.)
The cremasteric artery accompanies the spermatic cord in males and supplies the cremaster and other coverings of the cord. It anastomoses with the testicular artery. In females it is small and accompanies the round ligament. A pubic branch, near the femoral ring, descends posterior to the pubis and anastomoses with the pubic branch of the obturator artery. Occasionally, the pubic branch of the inferior epigastric artery is larger than the main obturator artery origin, and it supplies the majority of flow into the obturator artery in the thigh. It is then referred to as the aberrant obturator artery. It lies close to the medial border of the femoral ring and may be damaged in medial dissection of the ring during femoral hernia repair. Muscular branches supply the abdominal muscles and peritoneum, and anastomose with the circumflex iliac and lumbar arteries. Cutaneous branches perforate the aponeurosis of external oblique, supply the skin and anastomose with branches of the superficial epigastric artery.
Sometimes the inferior epigastric artery arises from the femoral artery. It then ascends anterior to the femoral vein into the abdomen to follow its course as above. It occasionally arises from the external iliac artery, in common with an aberrant obturator artery and, rarely, from the obturator artery.
The superior and inferior epigastric arteries are important sources for a potential collateral circulation between the internal thoracic artery and the external iliac artery in situations where flow in the thoracic or abdominal aorta is compromised. Small tributaries of the inferior epigastric vein drain the skin around the umbilicus and anastomose with the terminal branches of the umbilical vein, draining the inner surface of the umbilicus via the falciform ligament. These anastomoses may open widely in cases of portal hypertension, when portal venous blood may drain into the systemic circulation via the inferior epigastric vessels. The radiating dilated veins seen under the umbilical skin are referred to as the ‘caput medusae’.
Posterior intercostal, subcostal and lumbar arteries
The 10th and 11th posterior intercostal arteries and the subcostal artery emerge from under the subcostal groove of their respective ribs and pass into the tissues of the anterior abdominal wall. They run through the aponeurosis of transversus abdominis and lie deep to the fibres of internal oblique. The lumbar arteries also cross the aponeurosis of transversus abdominis and lie deep to internal oblique. The arteries on either side run forward, giving off muscular branches to the overlying internal and external oblique, before anastomosing with the lateral branches of the superior and inferior epigastric arteries at the lateral border of the rectus sheath (Fig. 61.7). Perforating cutaneous vessels run vertically through the muscles to supply the overlying skin and subcutaneous tissue. A small contribution to the supply of the lower abdominal muscles comes from branches of the deep circumflex iliac arteries.
Lymphatic drainage
The lymphatic vessels of the anterior abdominal wall lie both superficial and deep to the deep fascia.
Superficial vessels
The superficial lymphatic vessels accompany the subcutaneous blood vessels. Vessels from the lumbar and gluteal regions run with the superficial circumflex iliac vessels. Those from the infra-umbilical skin run with the superficial epigastric vessels. Both drain into the superficial inguinal nodes. The supra-umbilical region is drained by vessels running obliquely up to the pectoral and subscapular axillary nodes, and there is some drainage to the parasternal nodes.
Deep vessels
The deep lymphatic vessels accompany the deep arteries. The vessels from the posterior portion of the abdominal wall pass with the lumbar arteries to drain into the lateral aortic and retro-aortic nodes. Vessels from the upper anterior abdominal wall run with the superior epigastric vessels to the parasternal nodes. Vessels of the lower abdominal wall drain into the circumflex iliac, inferior epigastric and external iliac nodes.
SEGMENTAL NERVES
The seventh to the 12th lower thoracic ventral rami continue anteriorly from the intercostal spaces into the abdominal wall (Fig. 61.3). Approaching the anterior ends of their respective spaces, the seventh and eighth nerves curve superomedially across the deep surface of the costal cartilages between the digitations of transverse abdominis. They reach the deep aspect of the posterior layer of the aponeurosis of internal oblique. Both the seventh and eighth nerves then run through this aponeurosis, pass posterior to rectus abdominis and supply branches to the upper portion of the muscle. They pass through the muscle near its lateral edge and pierce the anterior rectus sheath to supply the skin of the epigastrium.
The ninth to 11th intercostal nerves pass from their intercostal spaces between digitations of the diaphragm and transversus abdominis. They enter the layer between transversus abdominis and internal oblique. Here, the ninth nerve runs forwards almost horizontally, whereas the tenth and 11th pass inferomedially. At the lateral edge of rectus abdominis, the nerves pierce the posterior layer of the aponeurosis of internal oblique and pass behind the muscle to end, like the seventh and eighth intercostal nerves, with cutaneous branches. The ninth nerve supplies skin above the umbilicus, the tenth supplies skin, which includes the umbilicus, and the 11th supplies skin below the umbilicus (see Fig. 15.12 and Chapters 42, 45 and 79). The 12th thoracic nerve (subcostal nerve) connects with the first lumbar ventral ramus (dorsolumbar nerve). It accompanies the subcostal vessels along the inferior border of the 12th rib, passing behind the lateral arcuate ligament and kidney and anterior to the upper part of the quadratus lumborum. It perforates the transversus abdominis fascia, running deep to the internal oblique, to be distributed like the lower intercostal nerves. It supplies the anterior gluteal skin reaching down to the greater trochanter.
The seventh to 12th intercostal nerves supply the intercostal, subcostal and abdominal muscles. The tenth, 11th and 12th supply serratus posterior inferior. All six nerves also provide sensory fibres to the costal parts of the diaphragm and related parietal pleura and peritoneum. Like the upper intercostal nerves, they give off collateral and lateral cutaneous branches before they reach the costal angles. The collateral branch may rejoin its parent nerve but, if it does, it leaves it again near the lateral border of rectus abdominis. It then runs forward, through the muscle and its anterior sheath near the linea alba to supply the overlying skin. The lateral cutaneous branches pierce the intercostal muscles and external oblique and divide into anterior and posterior branches. These branches supply the skin of the abdomen and back. The anterior branches supply external oblique. The posterior branches pass back to supply the skin over latissimus dorsi. Each lateral cutaneous nerve descends as it pierces external oblique and the superficial fascia and reaches the skin on a level with the anterior and posterior cutaneous nerves of the segment.
SOFT TISSUE
Superficial fascia
The superficial fascia of the abdominal wall consists mostly of a single layer that contains a variable amount of fat. It lies between the skin and muscles of the anterior abdominal wall. In the lower part, the fascia differentiates into superficial and deep layers between which lie superficial vessels and nerves and, in the region of the groin, superficial inguinal lymph nodes.
Superficial layer
Where present, the superficial layer is thick, areolar in texture and contains a variable amount of fat. It is often greatly thickened in obese individuals. Inferiorly, it lies superficial to the inguinal ligament and is continuous with the superficial fascia of the thigh. In the male, this layer continues over the penis and outer surface of the spermatic cord into the scrotum, where it changes its character. In this region it is generally thin, with very little adipose tissue present and is pale red in colour. In the scrotum it also contains smooth muscle fibres, which form the dartos muscle. From the scrotum it may be traced backwards into continuity with the superficial fascia of the perineum. In the female, it continues from the suprapubic skin of the abdomen into the labia majora and perineum.
Deep (membranous) layer
When present as a distinct entity, the deep layer of the fascia is more membranous than the superficial, and contains elastic fibres. It is loosely connected by areolar tissue to the aponeurosis of external oblique, but in the midline it is intimately adherent to the linea alba and symphysis pubis. In the male, it extends onto the dorsum of the penis and forms part of the superficial ligament of the penis. Superiorly, it is continuous with the superficial fascia over the remainder of the trunk. Inferiorly, it lies superficial to the inguinal ligament and fuses with the overlying superficial layer and the underlying fascia lata in the inguinal flexure line or skin crease of the thigh.
In the male, the deep layer of the fascia continues inferiorly and medially over the penis and spermatic cord to the scrotum, where it becomes continuous with the membranous layer of the superficial fascia of the perineum. In the female, it continues into the labia majora and is continuous with the fascia of the perineum.
In the child, the testis can frequently be retracted out of the scrotum into the loose areolar tissue between external oblique and the deep layer of superficial fascia over the inguinal canal. This ‘space’ is sometimes called the superficial inguinal pouch.
Transversalis fascia
The transversalis fascia is a thin layer of connective tissue lying between the inner surface of transversus abdominis and the extraperitoneal fat. It is part of the general layer of fascia between the peritoneum and the abdominal wall. Posteriorly, it is continuous with the anterior layer of the thoracolumbar fascia, and it forms a continuous sheet anteriorly. Inferiorly, it is continuous with the iliac and pelvic fasciae, and superiorly it blends with the fascial covering of the inferior surface of the diaphragm. It is attached to the entire length of the iliac crest between the origins of transversus abdominis and iliacus and to the posterior margin of the inguinal ligament between the anterior superior iliac spine and the femoral vessels. In the inguinal region it is thick and dense, and augmented by the aponeurosis of transversus abdominis. Medial to the femoral vessels it is thin and fused to the pubis behind the conjoint tendon. Anterior to the femoral vessels, fascia extends down from the fascia transversalis to form the anterior part of the femoral sheath. The fascia is strengthened here by fibres, which arch transversely. Some fibres spread laterally towards the anterior superior iliac spine, some fibres run medially behind rectus abdominis, and some descend to the pubis behind the conjoint tendon. These arched fibres constitute the deep crural arch. The curved fibres of the deep crural arch thicken the inferomedial part of the rim of the deep inguinal ring. The spermatic cord in the male, or the round ligament of the uterus in the female, pass through the transversalis fascia at the deep inguinal ring. This opening is not visible during dissection through the skin because the transversalis fascia is prolonged on these structures as the internal spermatic fascia, but it can be seen from within the abdomen once the peritoneum has been stripped off. The internal spermatic fascia surrounds the testis and blends with the areolar tissue on the parietal layer of the tunica vaginalis: it may contain smooth muscle fibres.
Extraperitoneal connective tissue
The extraperitoneal connective tissue is a layer of areolar tissue lying between the peritoneum and the fasciae lining the abdominal and pelvic cavities. The amount of extraperitoneal tissue varies: it is especially abundant on the posterior wall of the abdomen, particularly around the kidneys, where it contains much adipose tissue; variable in thickness on the anterolateral wall, where it is thin in children and normal adults but often thickened in the obese, particularly in males; scanty in the suprapubic region, above the iliac crest and in the pelvis. Extraperitoneal tissue is continuous with the epimysium of the muscles of the abdominal wall.
MUSCLES
ANTEROLATERAL MUSCLES OF THE ABDOMEN
Rectus abdominis, pyramidalis, external oblique, internal oblique and transversus abdominis constitute the anterolateral muscles of the abdomen. They act together to perform a range of functions, some of which involve the generation of a positive pressure within one or more body cavities. Although many of these activities may occur with no ‘forced assistance’, activities such as expiration, defecation and micturition may be aided by the generation of a positive intra-abdominal pressure. Parturition, coughing and vomiting always require such a positive pressure. Under resting conditions, the tone developed within the muscles provides support for the abdominal viscera and retains the normal contour of the abdomen. The consequences of lack of muscular support can be seen in conditions such as ‘prune belly syndrome’, where there is congenital absence of these muscles.
Active contraction of the muscles provides an important role in the maintenance of abdominal wall tone when the intra-abdominal pressure is increased. The compression of the abdominal cavity required to increase the internal pressure is brought about mainly by the contraction of the diaphragm. The bony pelvis and lower thoracic cage provide an almost incompressible structure to part of the abdominal wall. During the generation of positive intra-abdominal pressure, the abdominal wall acts to hold the position of the wall fixed, rather than to generate pressure directly: because the majority of the abdominal wall is muscular, the anterolateral abdominal wall muscles must be synchronously contracted to prevent displacement of the viscera and the resultant loss of pressure. The oblique muscles, acting through the anterior aponeurosis and the rectus sheath, provide the majority of this tension, although transversus abdominis and rectus abdominis also contribute.
The lateral muscles, external oblique, internal oblique and transversus abdominis, have the greatest roles in these functions, tensing the rectus sheath and linea alba. The anterolateral abdominal muscles contribute little to the movements of the trunk during normal sitting and standing, which are movements controlled predominantly by the paravertebral and spinal muscles. However, movements of the trunk against resistance or when the individual is supine require the anterolateral abdominal muscles. Rectus abdominis is the most important in these situations, causing anterior flexion of the trunk. If the pelvic girdle is fixed, flexion of the thorax and pectoral girdle occurs. With a fixed thoracic cage, contraction of rectus abdominis causes the pelvis to lift and tilt to lie more nearly in a horizontal plane. Lateral flexion and rotation of the trunk against resistance is provided by unilateral contraction of the oblique muscles.
Rectus abdominis
Rectus abdominis is a long, strap-like muscle that extends along the entire length of the anterior abdominal wall. It is widest in the upper abdomen and lies just to the side of the midline. The paired recti are separated in the midline by the linea alba (Fig. 61.4).
The muscle fibres of rectus abdominis are interrupted by three fibrous bands or tendinous intersections. One is usually situated at the level of the umbilicus, another opposite the free end of the xiphoid process and a third about midway between the other two. These intersections pass transversely or obliquely across the muscle in a zigzag manner. They are rarely full-thickness and may extend only half-way through the body of the muscle. They usually fuse with the fibres of the anterior lamina of the sheath of the muscle. Sometimes, one or two incomplete intersections are present below the umbilicus. The intersections may occur during development or may represent the myosepta delineating the myotomes that form the muscle.
The medial border of rectus abdominis is closely related to the linea alba. Its lateral border may be visible on the surface of the anterior abdominal wall as a curved groove, the linea semilunaris, which extends from the tip of the ninth costal cartilage to the pubic tubercle. In a muscular individual it is readily visible, even when the muscle is not actively contracting, but in many normal and obese individuals it may be completely obscured.
Rectus abdominis arises by two tendons. The larger, lateral tendon is attached to the crest of the pubis and may extend beyond the pubic tubercle to the pectineal line. The medial tendon interlaces with the contralateral muscle and blends with the ligamentous fibres covering the front of the symphysis pubis. Additional fibres may arise from the lower part of the linea alba. Superiorly, rectus abdominis is attached by three slips of muscle to the fifth, sixth and seventh costal cartilages. The most lateral fibres are usually attached to the anterior end of the fifth rib. Sometimes this slip is absent, and occasionally it may extend to the fourth and third ribs. The most medial fibres are occasionally connected to the costoxiphoid ligaments and the side of the xiphoid process. In males, the pubic attachment of rectus abdominis may run over the anterior surface of the symphysis pubis and become continuous with the attachment of the gracilis and the fascia lata to the pubis.
Rectus abdominis is supplied principally by the superior and inferior epigastric arteries. The inferior epigastric artery tends to be larger in calibre than the superior. Small terminal branches from the lower three posterior intercostal arteries, the subcostal artery, the posterior lumbar arteries and the deep circumflex artery may provide some contribution, particularly to the lateral edges and the lower attachments, and they form small anastomoses with the lateral branches of the epigastric arteries. Rectus abdominis provides an excellent myocutaneous flap, either pedicled or free, because of the excellent vascularity provided by the epigastric vessels and because the muscle belly is separated from surrounding tissue within the rectus sheath. The upper half of the muscle may be used for breast reconstruction or augmentation of tissue loss on the anterior thorax. The lower half may be used in the region of the thigh and may be rotated on its lower attachments, passed through the pelvis and delivered into the perineum for reconstruction after radical pelvic and perineal resections.
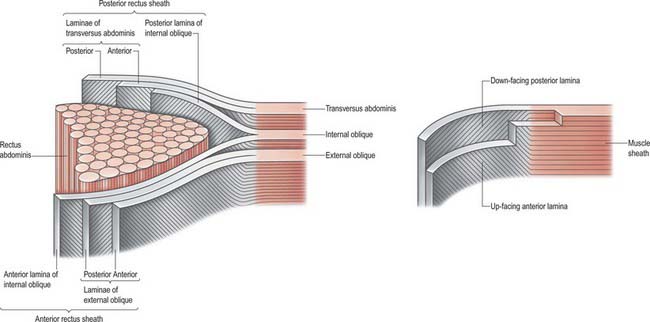
Rectus sheath
Rectus abdominis on each side is enclosed by a fibrous sheath. The anterior portion of this sheath extends the entire length of the muscle and fuses with the periosteum of the muscle attachments. Posteriorly, the sheath is complete in the upper two-thirds of the muscle. In the lower one-third, the posterior layer of the sheath stops approximately midway between the umbilicus and the pubis. In most individuals this is a clearly defined line, although the transition may not always be clear-cut in others. The lower border of the posterior sheath is called the arcuate line. Below this level, rectus abdominis is enclosed posteriorly by the transversalis fascia and extraperitoneal connective tissue (Figs 61.8 and 61.9). The rectus sheath is formed from decussating fibres from all three lateral abdominal muscles. External oblique, internal oblique and transversus abdominis each forms a bilaminar aponeurosis at their medial borders. The fibres from all three anterior leaves run obliquely upwards, whereas the posterior leaves run obliquely downwards at right angles to the anterior leaves.
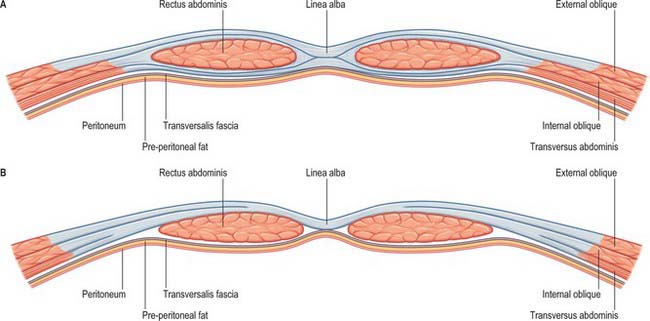
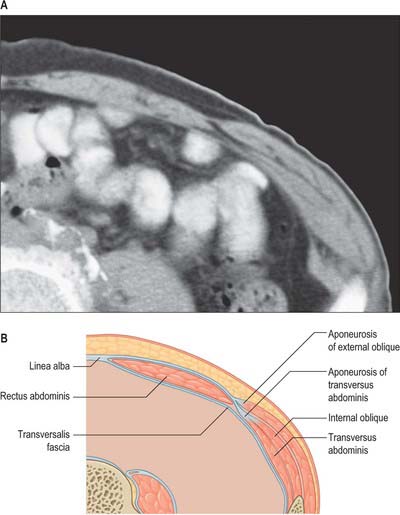
Fig. 61.8 Transverse sections through the anterior abdominal wall: A, immediately above the umbilicus; B, below the arcuate line. The bilaminar nature of each muscular aponeurosis is difficult to illustrate in cross-section. The fibres appear to fuse into a single sheet during formation of the rectus sheath. Note that rectus is supported directly by the transversalis fascia below the arcuate line.
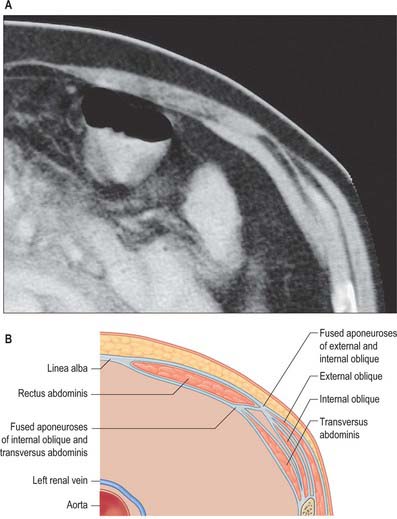
Fig. 61.9 Rectus sheath. Computed tomography scan (A) and diagram (B) of the anterior abdominal wall, demonstrating the formation of the rectus sheath above the umbilicus. The anterior rectus sheath is composed of both leaves of the aponeurosis of external oblique and the anterior leaf of the aponeurosis of internal oblique, fused together. The posterior rectus sheath is composed of the posterior leaf of the aponeurosis of internal oblique and both leaves of the aponeurosis of transversus abdominis.
The anterior rectus sheath is composed of both leaves of the aponeurosis of external oblique and the anterior leaf of the aponeurosis of internal oblique fused together. The posterior rectus sheath is composed of the posterior leaf of the aponeurosis of internal oblique and both leaves of the aponeurosis transversus abdominis (Fig. 61.10). Because of this arrangement, both the anterior and posterior layers of the rectus sheath consist of three layers of fibres with the middle layer running obliquely at right angles to the other two. At the midline, the anterior and posterior layers are closely approximated. Fibres of each layer decussate to the opposite side of the sheath, forming a continuous aponeurosis with the contralateral muscles (Fig. 61.11). Fibres also decussate anteroposteriorly, crossing from anterior sheath to posterior sheath. The dense fibrous line caused by this decussation is called the linea alba. The external oblique, internal oblique and transversus abdominis muscles can thus be regarded as paired, digastric muscles with a central tendon in the form of the linea alba. These decussating fibres maybe used to identify the midline during surgical incisions, since they can be seen as oblique fibres crossing at right angles. Below the level of the arcuate line, the fibres forming the posterior rectus sheath rapidly cease running behind the rectus and all leaves pass into the anterior rectus sheath.
Linea alba
The linea alba is a tendinous raphe extending from the xiphoid process to the symphysis pubis and pubic crest. It lies between the two recti and is formed by the interlacing and decussating aponeurotic fibres of external oblique, internal oblique and transversus abdominis. It is visible only in the lean and muscular, as a slight groove in the anterior abdominal wall. A fibrous cicatrix, the umbilicus, lies a little below the midpoint of the linea alba, and is covered by an adherent area of skin. Below the umbilicus, the linea alba narrows progressively as the rectus muscles lie closer together. Above the umbilicus, the rectus muscles diverge from one other and the linea alba is correspondingly broader. The linea alba has two attachments at its lower end: its superficial fibres are attached to the symphysis pubis, and its deeper fibres form a triangular lamella that is attached behind rectus abdominis to the posterior surface of the pubic crest on each side. This posterior attachment of linea alba is named the ‘adminiculum lineae albae’. The linea alba is crossed from side to side by a few minute vessels.
In the fetus, the umbilicus transmits the umbilical vessels, urachus and, up to the third month, the vitelline or yolk stalk. It closes a few days after birth, but the vestiges of the vessels and urachus remain attached to its deep surface. The remnant of the fetal left umbilical vein forms the round ligamentum of the liver. The obliterated umbilical arteries form the medial umbilical ligaments, enclosed in peritoneal folds of the same name. The partially obliterated remains of the urachus persist as the median umbilical ligament.
Divarication of the recti
Thinning and widening of the upper linea alba may occur, most commonly as a result of obesity or chronic straining. This process disrupts the arrangement of the fibres of the bilaminar aponeurosis. Contraction of the anterolateral abdominal muscles fails to be transmitted across the midline through the linea alba and increased intra-abdominal pressure causes the abdominal viscera to protrude beneath the thinned tissue as a broad midline bulge. The recti become widely separated or divaricated. This is not true herniation, as all the layers of the abdominal wall in that region are intact.
Umbilical hernia
There are three varieties of umbilical hernia. In true congenital herniation, a defect is present from birth. This is usually simply the result of failure of closure of the umbilicus after retraction of the umbilical gut loop. Less commonly, the gut loop does not retract and remains, in part, outside the abdominal cavity. An infantile umbilical hernia is caused by stretching of the umbilical scar tissue, associated with increased intra-abdominal pressure. An acquired umbilical or paraumbilical hernia actually occurs through small areas of weakness in the linea alba, above or below the umbilical scar.
Pyramidalis
Pyramidalis is a triangular muscle that lies in front of the lower part of rectus abdominis within the rectus sheath. It is attached by tendinous fibres to the front of the pubis and to the ligamentous fibres in front of the symphysis. The muscle diminishes in size as it runs upwards, and ends in a pointed apex that is attached medially to the linea alba. This attachment usually lies midway between the umbilicus and pubis, but may occur higher. The muscle varies considerably in size. It may be larger on one side than on the other, absent on one or both sides, or even doubled.
Pyramidalis is supplied by branches of the inferior epigastric artery, with some contribution from the deep circumflex iliac artery. A small artery frequently crosses the midline posterior to the belly of the muscle to anastomose with the contralateral vessel. This may cause troublesome bleeding during surgical incisions that run down as far as the lower rectus sheath above the symphysis pubis.
External oblique
External oblique is the largest and the most superficial of the three lateral abdominal muscles (Fig. 61.1). It curves around the lateral and anterior parts of the abdomen and is attached to the external surfaces and inferior borders of the lower eight ribs. The attachments rapidly become muscular and interdigitate with the lower attachment of serratus anterior and latissimus dorsi along an oblique line that extends downwards and backwards. The upper attachments are close to the cartilages of the corresponding ribs, the middle ones arise from the ribs at some distance from their cartilages and the lowest are close to the apex of the cartilage of the 12th rib. The fibres of external oblique diverge as they pass to their lower attachments. Those from the lower two ribs pass nearly vertically downwards and are attached to the anterior half or more of the outer lip of the anterior segment of the iliac crest. The middle and upper fibres pass downwards and forwards and end in the anterior aponeurosis, along a line drawn vertically from the ninth costal cartilage to a little below the level of the umbilicus. The muscle fibres rarely descend beyond a line from the anterior superior iliac spine to the umbilicus. The posterior border of the muscle is free.
The inguinal ligament is formed by the margin of the aponeurosis of external oblique extending between the anterior superior iliac spine and the pubic tubercle. The deep fibres of the aponeurosis of external oblique are not initially parallel to the long axis of the inguinal ligament: they approach the ligament obliquely at an angle of 10–20°. On reaching the ligament, fibres turns medially, and most run along the ligament to reach the pubic tubercle. The deepest fibres of the aponeurosis spread out posteromedially to insert into the pectineal line.
The upper and lower rib attachments of the muscle may be absent. Digitations or even the entire muscle may be reduplicated. The upper attachments of the muscle are sometimes continuous with pectoralis major or serratus anterior.
External oblique is supplied by branches from the lower posterior intercostal and subcostal arteries, the superior and inferior epigastric arteries, the superficial and deep circumflex arteries and the posterior lumbar arteries.
Inguinal ligament
The inguinal ligament is the thick, inrolled lower border of the aponeurosis of external oblique and stretches from the anterior superior iliac spine to the pubic tubercle. Its grooved abdominal surface forms the ‘floor’ of the inguinal canal. The ligament is not linear and has an inferior and an anterior convexity. At its lower border, it is continuous with the fascia lata. The lateral half is rounded and lies more obliquely than the medial half. The latter gradually widens towards its attachment to the pubis, where it becomes more horizontal and supports the spermatic cord. At the medial end, some fibres do not attach to the pubic tubercle but extend in two directions. Some expand posteriorly and laterally to attach to the pectineal line, forming the lacunar ligament complex. Other fibres pass upwards and medially behind the superficial inguinal ring and external oblique to join the rectus sheath and the linea alba. These constitute the reflected part of the inguinal ligament. Fibres from either side decussate in the linea alba, similarly to the aponeurosis of the abdominal muscles.
Internal oblique
Internal oblique lies deep to external oblique for the majority of its course (Fig. 61.2). It is thinner and less bulky than external oblique. Its fibres arise from the lateral two-thirds of the grooved upper surface of the inguinal ligament, where they form a common attachment with the iliac fascia to the inguinal ligament. Laterally, internal oblique is also attached to the anterior two-thirds of the intermediate line of the anterior segment of the iliac crest, and posteriorly some fibres are attached to the thoracolumbar fascia. The fibres originating from the posterior end of the iliac attachment pass upwards and laterally and are attached to the inferior borders and tips of the lower three or four ribs and their cartilages. Here, the attachments merge with those of the internal intercostals. The uppermost of these fibres form a short, free superior border. The fibres attached to the anterior iliac crest diverge and end in the anterior aponeurosis, which gradually broadens from below upwards. The uppermost part of the aponeurosis is attached to the cartilages of the seventh, eighth and ninth ribs. The fibres that originate from the inguinal ligament arch downwards and medially across the spermatic cord in the male and the round ligament of the uterus in the female. They become tendinous, fuse with the corresponding part of the aponeurosis of transversus abdominis, and attach to the crest and medial part of the pectineal line, forming the conjoint tendon.
Internal oblique is supplied by branches from the lower posterior intercostal and subcostal arteries, the superior and inferior epigastric arteries, the superficial and deep circumflex arteries and the posterior lumbar arteries.
Internal oblique is innervated by the terminal branches of the lower five intercostal nerves and the subcostal nerve from the ventral rami of the lower six thoracic spinal nerves, in addition to a small contribution from the iliohypogastric and ilioinguinal nerves from the ventral ramus of the first lumbar spinal nerve.
Cremaster
Cremaster consists of loosely arranged muscle fasciculi lying along the spermatic cord. It is variable in thickness and is thickest in young men. It may form an incomplete coating around the cord, known as the cremasteric fascia, which extends around the testis but lies within the external spermatic fascia. The attachment of the muscle arises mainly from the inferomedial border of internal oblique and transversus abdominis. A separate tendinous attachment may also occur to the middle of the inguinal ligament, extending as far as the anterior superior iliac spine. The medial portion is attached to the pubic tubercle and lateral pubic crest. The fibres spread out over the lateral aspect of the spermatic cord as it approaches the superficial inguinal ring. The shortest and most superior fasciculi turn inwards in front of the cord to join the medial part. The longer, lateral fasciculi blend with the fascia over the cord and upper part of the tunica vaginalis. In the female, a few fibres descending on the round ligament of the uterus represent the lateral part of cremaster. The medial part of the muscle is variably developed, and may be absent. It is attached to the pubic tubercle and the lateral pubic crest, the conjoint tendon and lower border of transversus abdominis. These fasciculi loop on the posteromedial aspect of the cord, interlacing with those of the lateral part. The entire muscle appears to form continuous loops that pass from the middle of the inguinal ligament as far as the tunica vaginalis, and then return to attach to the pubic tubercle.
Cremaster is innervated by the genital branch of the genitofemoral nerve, derived from the first and second lumbar spinal nerves.
Cremaster pulls the testis up towards the superficial inguinal ring. Although its fibres are striated, it is not usually under voluntary control. Stroking the skin of the medial side of the thigh evokes a reflex contraction of the muscle, the cremasteric reflex, which is most pronounced in children. It may represent a protective reflex, and the cremaster may also have a role in testicular thermoregulation.
Transversus abdominis
Transversus abdominis is the deepest of the lateral abdominal muscles (Fig. 61.5). It is attached to the lateral one-third of the inguinal ligament and the associated iliac fascia, the anterior two-thirds of the inner lip of the anterior segment of the iliac crest, the thoracolumbar fascia between the iliac crest and the 12th rib, and the internal aspects of the lower six costal cartilages. The costal attachments interdigitate with the attachment of the diaphragm. The muscle ends in an anterior aponeurosis. The lower fibres curve downwards and medially, together with those of the aponeurosis of internal oblique, and insert into the pubic crest and pectineal line to form the conjoint tendon. A band of fibres, sometimes muscular, may run from the lower border of the muscle to the inguinal ligament and is called the inter-foveolar ligament. The remainder of the aponeurosis passes medially and the fibres decussate at, and blend with, the linea alba. The upper costal and anterior iliac fibres of transversus abdominis are short. The lower costal and posterior iliac fibres are longer, and the thoracolumbar fibres are longest. Near the xiphoid process, the aponeurosis is formed only 2–3 cm from the linea alba, so the muscular part of transversus abdominis extends behind rectus into the posterior layer of the rectus sheath. The medial edge of the muscle, at the start of the aponeurosis, curves first downwards and laterally, and is furthest from the lateral edge of the rectus sheath at the level of the umbilicus. It then curves downwards and medially towards the middle of the superior crus of the superficial inguinal ring.
Occasional defects filled with fascia may occur in the lower muscular and aponeurotic parts of both internal oblique and transversus abdominis. The two muscles are sometimes fused and, rarely, transversus abdominis may be absent.
Transversus abdominis is supplied by branches from the lower posterior intercostal and subcostal arteries, the superior and inferior epigastric arteries, the superficial and deep circumflex arteries and the posterior lumbar arteries.
Conjoint tendon
The conjoint tendon is formed from the lower fibres of internal oblique and the lower part of the aponeurosis of transversus abdominis. It is attached to the pubic crest and pectineal line. It descends behind the superficial inguinal ring and acts to strengthen the medial portion of the posterior wall of the inguinal canal. The attachment to the pectineal line is frequently absent. Medially, the upper fibres of the tendon fuse with the anterior wall of the rectus sheath, and laterally some fibres may blend with the interfoveolar ligament.
Inguinal canal
The inguinal canal is a natural hiatus in the tissues of the anterior abdominal wall, and is formed from the various layers of the wall in the region of the groin (Figs 61.12, 61.13, 61.14, 61.15, and see Fig. 76.2). Its size and form vary with age, and although it is present in both sexes it is most well developed in the male. The canal is an oblique tunnel, with deep and superficial openings or rings. It contains the spermatic cord in males, the round ligament of the uterus in females, and the ilioinguinal nerve in both sexes.
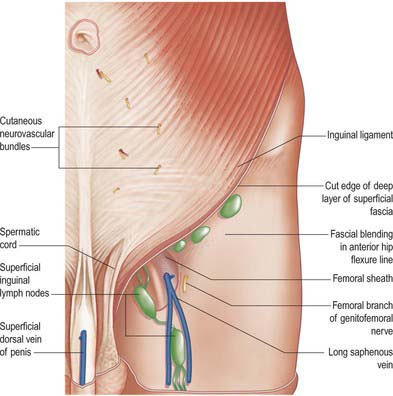
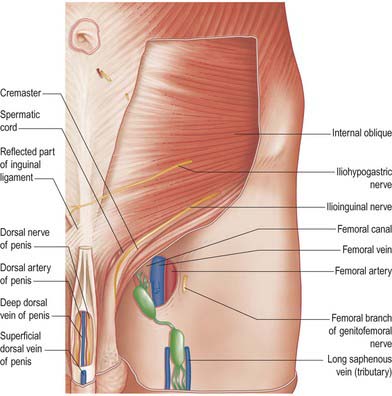
Fig. 61.12 Superficial structures of the inguinal region and lower part of the anterior abdominal wall on the left side.
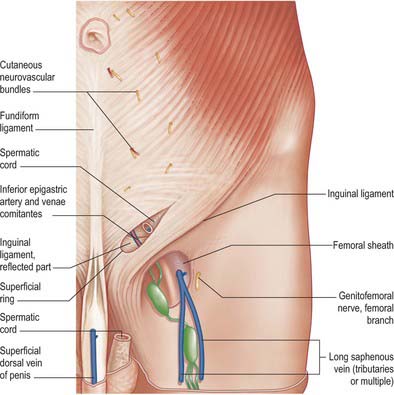
Fig. 61.13 Superficial structures of the inguinal region and lower part of the anterior abdominal wall on the left side: superficial aponeurotic layer removed.
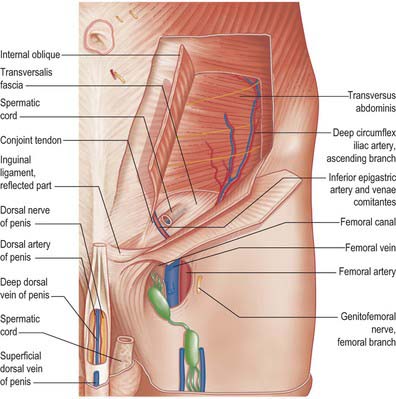
Fig. 61.15 Dissection of the regions shown in Fig. 61.13, with parts of external and internal oblique muscles removed.
Superficial inguinal ring
The superficial inguinal ring is a hiatus in the aponeurosis of external oblique, just above and lateral to the crest of the pubis. The ring is actually triangular, and its apex points along the line of the deep fibres of the aponeurosis. Although it varies in size, it does not usually extend laterally beyond the medial one-third of the inguinal ligament – the ring is smaller in the female. The base lies along the crest of the pubis and its sides are the crura of the opening in the aponeurosis. The lateral crus is the stronger and is reinforced by fibres of the inguinal ligament inserted into the pubic tubercle. The medial crus is thin. The fibres attach to the front of the symphysis pubis and interlace with fibres from the opposite side. In the external layer of the investing fascia of external oblique, some fibres arch above the apex of the superficial inguinal ring as intercrural fibres. In the male, the lateral crus is curved to form a groove, in which the spermatic cord rests. Fibres from the aponeurosis of external oblique and overlying fascia continue downwards from the crura of the ring, and form a delicate tubular prolongation of fibrous tissue around the spermatic cord and testis. This is the external spermatic fascia and constitutes the outermost covering of the cord. The superficial inguinal ring is only a distinct aperture when the continuity of this fascia with the aponeurosis is interrupted.
Deep inguinal ring
The deep inguinal ring is situated in the transversalis fascia, midway between the anterior superior iliac spine and the symphysis pubis approximately 1.25 cm above the inguinal ligament. It is oval, with an almost vertical long axis. Its size varies between individuals, and it is always much larger in the male. It is related above to the arched lower margin of transversus abdominis, and medially to the inferior epigastric vessels and the interfoveolar ligament, when that is present. Traction on the fascial ring exerted by internal oblique may constitute a valve-like safety mechanism when intra-abdominal pressure is increased.
Boundaries
The inguinal canal is a virtual space lying between the various layers formed from the lower tissues of the anterior abdominal wall. It lies obliquely and slants downwards and medially, parallel with and a little above the inguinal ligament. It extends from the deep to the superficial inguinal rings: the length depends on the age of the individual, but in the adult is between 3 and 5 cm long. The canal is bounded anteriorly by the skin, superficial fascia and aponeurosis of external oblique. In its lateral one-third, the anterior wall is reinforced by the muscular fibres of the internal oblique just above their origin from the inguinal ligament. Posteriorly lie the reflected inguinal ligament, the conjoint tendon and the transversalis fascia, which separate it from extraperitoneal connective tissue and peritoneum. Superiorly lie the arched fibres of internal oblique and transversus abdominis, forming the conjoint tendon, and inferiorly is the union of the transversalis fascia with the inguinal ligament and, at the medial end, the lacunar ligament.
In the newborn, the deep and superficial rings are nearly superimposed and the canal is extremely short. This creates an approximately oval defect in the abdominal wall. As the child grows, the anterior abdominal wall muscles grow rapidly, causing the positions of the rings to separate and the canal to lengthen. The defect thus becomes progressively more oblique until, in adulthood, the presence of separate anterior and posterior canal walls forms a ‘flap valve’ effect. Increases in intra-abdominal pressure transmitted through the posterior wall and the deep ring are supported by the presence of the thickest part of the overlying anterior wall. At the superficial ring and medial end of the anterior wall, where it is weakest, the posterior wall is strengthened by the conjoint tendon and the reflected inguinal ligament. The fibres of internal oblique and transversus abdominis, which form the conjoint tendon, are constantly active in standing; this activity increases during episodes of increased intra-abdominal pressure.
Relations
The inferior epigastric vessels are important posterior relations of the medial end of the canal (Fig. 61.16). They lie on the transversalis fascia as they ascend obliquely behind the conjoint tendon into the posterior portion of the rectus sheath.
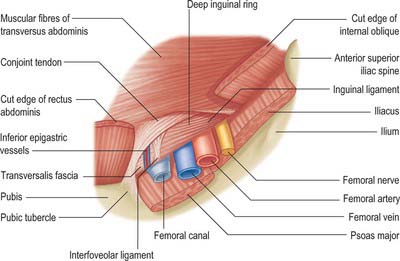
Fig. 61.16 Deep structures of the inguinal canal. The aponeurosis of external oblique has been removed. For clarity, the fibres of internal oblique and rectus abdominis have been divided and the structures passing posteroinferiorly to the inguinal ligament have been excluded.
The inguinal triangle lies in the posterior wall of the canal. It is bounded inferiorly by the medial half of the inguinal ligament, medially by the lower lateral border of rectus abdominis and laterally by the inferior epigastric artery, and overlies the medial inguinal fossa and, in part, the supravesical fossa.
Lacunar ligament
The lacunar ligament is a thick triangular band of tissue lying mainly posterior to the medial end of the inguinal ligament. It measures approximately 2 cm from base to apex and is a little larger in the male. It is formed from fibres of the medial end of the inguinal ligament and fibres from the fascia lata of the thigh, which join the medial end of the inguinal ligament from below. The inguinal fibres run posteriorly and laterally to the medial end of the pectineal line and are continuous with the pectineal fascia. They form a near horizontal, triangular sheet with a curved lateral border which forms the medial border of the femoral canal. The apex of the triangle is attached to the pubic tubercle. A strong fibrous band, the pectineal ligament of Astley Cooper, extends laterally along the pectineal line from the pectineal attachment. The fibres from the fascia lata join the inferior/posterior border of the inguinal ligament; the latter, in combination with fibres from the transversalis fascia, fuses with the pectineal fascia as it joins the thickened periosteum of the pectineal line. This portion of the lacunar ligament forms the lower extension of the medial border of the femoral canal and femoral sheath.
HERNIAS OF THE ANTERIOR ABDOMINAL WALL
INGUINAL HERNIA
Although the inguinal canal is arranged such that the weaknesses in the anterior abdominal wall caused by the deep and superficial inguinal rings are supported, the region remains a potential cause of herniation. An inguinal hernia involves the protrusion of a viscus through the tissues of the inguinal region of the abdominal wall.
Indirect inguinal hernia
An indirect hernia is defined as arising lateral to the inferior epigastric vessels. Many indirect hernias are related to the congenital abnormal persistence of the vaginal process, others are acquired as a result of progressive weakening of the lateral and posterior walls of the canal. The hernia may pass through the deep ring or may expand the deep ring such that it is no longer a clear entity. Small indirect hernias tend to lie below and lateral to the fibres of the conjoint tendon, but larger hernias often distort and thin the tendon superiorly. Small hernias, which do not protrude beyond the inguinal canal, are covered by the same inner layers as the spermatic cord, including the internal spermatic fascia and cremaster. If the hernia extends through the superficial inguinal ring it is additionally covered by external spermatic fascia.
In hernias related to a persistent fully patent vaginal process, the hernia contents descend in front of the testis into the tunica vaginalis (complete congenital hernia) and the vaginal process and tunica form part of the hernial sac. Where the vaginal process is sealed off from the tunica vaginalis, the hernia contents descend to the top of the testis (incomplete congenital hernia). Although both types are related to a congenital abnormality, actual herniation into the potential sac may not occur until adult life, when it may happen as a consequence of increased intra-abdominal pressure or sudden muscular strain.
Direct inguinal hernia
A direct inguinal hernia is defined as arising medial to the inferior epigastric vessels. Direct hernias are always caused by an acquired weakness of the inguinal triangle in the medial posterior wall of the canal, and frequently extend through the anterior wall of the canal or superficial ring. The hernia may protrude through the transversalis fascia, between the conjoint tendon and the inferior epigastric vessels, and enter the inguinal canal. It may closely resemble an indirect hernia, in that the coverings are similar. Its clinical presentation can also mimic an indirect inguinal hernia. Other direct hernias arise either between the fibres of the conjoint tendon or by eventration of the tendon such that it forms a thin covering to the hernia. In either case, a hernia enters the lower end of the canal, protruding through the superficial ring medial to the cord, and is covered by external spermatic fascia.
Clinical features of inguinal hernias
Indirect hernias often descend from lateral to medial in the same oblique angle as the canal, because of their origin in the lateral end of the inguinal canal. This is particularly true for congenital hernias. Direct hernias arise from the medial end of the canal and tend to protrude more directly anteriorly. With the patient in the supine position and the hernia reduced, pressure applied over the region of the deep inguinal ring may prevent appearance of an indirect hernia on standing or straining. This method of determining the type of hernia is fraught with difficulties. Indirect hernias may have a wide neck, and occlusion of the deep ring may not be possible with simple digital pressure. An acquired indirect hernia may arise medial to the deep ring. The angle of the descent of the hernia is also an unreliable guide, as it depends on the size of the defect in the posterior wall of the canal, the length of the canal and whether the hernia protrudes through the anterior wall. Direct hernias are more likely to have a wide-necked origin, making strangulation less likely.
FEMORAL HERNIA
A femoral hernia protrudes through the femoral ring. The femoral ring is normally closed by a femoral septum of modified extraperitoneal tissue, and is therefore a weak spot. In females, the ring is relatively large and subject to profound changes during pregnancy, which explains why femoral hernias are more common in women. When a section of intestine bulges through the ring, it pushes out a hernial sac of peritoneum. It is covered by extraperitoneal tissue (the femoral septum) and descends along the femoral canal to the saphenous opening. It is prevented from descending further along the femoral sheath by the narrow saphenous opening, by the vessels and by the close attachment of the superficial fascia and sheath to the lower part of the rim of the saphenous opening. The hernia hence turns forwards, distending the cribriform fascia and curving upwards over the inguinal ligament and the lower part of the aponeurosis of external oblique. While in the canal the hernia is usually small, because of the resistance of surrounding tissues, but it enlarges as it escape into the inguinal loose connective tissue. A femoral hernia first descends and then ascends forwards: pressure to reduce it should therefore be directed in the reverse order, with the thighs passively flexed for greatest relaxation.
The coverings of a femoral hernia are, from within outwards: the peritoneum, femoral septum, femoral sheath, cribriform fascia, superficial fascia and skin. A fibrous covering, the fascia propria, may lie outside the peritoneal sac and is frequently separated from it by adipose tissue. It represents a femoral septum which has been thickened to form a membranous sheet by hernial pressure. The fascia propria may easily be mistaken for the sac, and its contained extraperitoneal fat for omentum; the fat may resemble a lipoma, but dissection will reveal the true hernial sac in its centre. The intestine reaches only to the saphenous opening in incomplete femoral hernia, in contradistinction to complete hernia, in which it passes through the opening. The small size of an incomplete hernia renders it difficult to detect and therefore dangerous, especially in the corpulent. The site of strangulation varies: it may be at the neck of the hernial sac, more often it is at the junction of the falciform margin of the saphenous opening with the free edge of the pectineal part of the inguinal ligament, or it may be at the saphenous opening. The site of narrowing should be divided superomedially for a distance of 4–6 mm to avoid all normally positioned vessels and other important structures. Occasionally the obturator artery is replaced by an enlarged pubic branch of the inferior epigastric artery descending almost vertically to the obturator foramen. This vessel sometimes curves along the edge of the lacunar part of the inguinal ligament, encircling the neck of a hernial sac, and may be inadvertently cut during enlargement of the femoral ring in reducing a femoral hernia.
The pubic tubercle is an important landmark in distinguishing inguinal from femoral hernias; the neck of the hernia is superomedial to it in inguinal hernia, but inferolateral in the femoral form.
LESIONS OF THE INTERCOSTAL NERVES
Lesions of individual intercostal nerves do not produce any appreciable clinical effects. The anterolateral muscles are innervated by a number of different nerves: injury to a single nerve will not reduce the tone of the muscle wall. The overlap between sequential dermatomes means that significant cutaneous anaesthesia is appreciated only after sectioning of at least two sequential nerves.
Cormack GC, George B, Lamberty H. The Arterial Anatomy of Skin Flaps, 2nd edn., London, Edinburgh: Churchill Livingstone; 1994:168-172.
Lytle WJ. Inguinal anatomy. J Anat. 1979;128:581-594.
Rizk NN. A new description of the anterior abdominal wall in man and mammals. J Anat. 1980;131:373-385.
Shafik A. The cremasteric muscle. In: Johnson AD, Gomes WR. The Testis. New York: Academic Press, 1977.