Chapter 10 Urinary system
If the metabolic processes of the body are to function effectively, the chemical composition and volume of the tissue fluid must be kept constant. The most important function of the urinary system – and principally that of the kidney – is to maintain this constant internal environment, described as homeostasis.
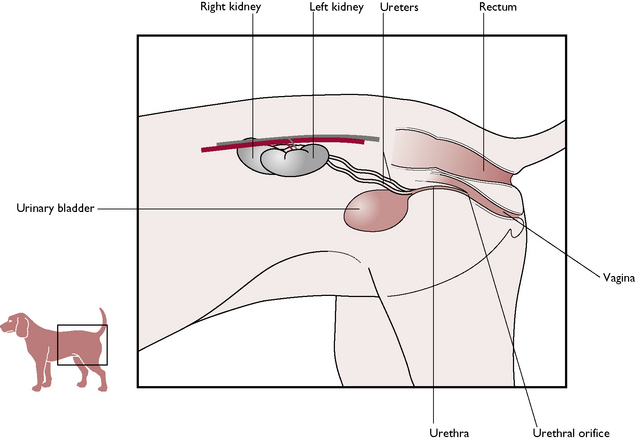
The urinary system lies in the abdominal and pelvic cavities. It is anatomically linked with the genital or reproductive system and may be referred to as the urogenital system. Both systems share the urethra which runs through the penis of the male and joins the vagina of the female.
The parts of the urinary system are:
The functions of the urinary system are:
The kidney
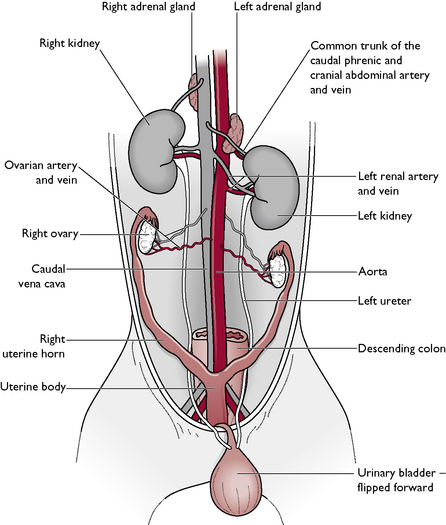
There are two kidneys lying in the cranial abdominal cavity, one on each side of the midline ventral to the lumbar hypaxial muscles (Fig. 10.1). Each kidney is closely attached to the lumbar muscles by a covering of parietal peritoneum. There is no mesenteric attachment, as seen in other abdominal organs, and the kidney is described as being retroperitoneal. The right kidney lies slightly cranial to the left because the stomach has evolved to lie on the left side of the abdomen, pushing the left kidney out of position. Lying close to the cranial pole of each kidney are the ovaries of the female and the adrenal glands (Fig. 10.2).
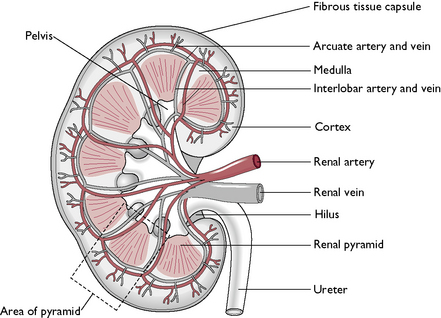
Macroscopic structure
The kidneys of the cat and dog have a characteristic bean shape and the indented area is known as the hilus. This is the point at which blood vessels, nerves and the ureters enter and leave the kidney. The kidneys are normally a deep reddish-brown but the colour may be affected by any substance filtering through them. On a lateral radiograph of the abdomen, a normal kidney can be seen to be equivalent in size to approximately 2.5 vertebrae (Fig. 10.3). The outer surface may be surrounded by a layer of fat, which acts as an energy reserve and protects the kidney from external damage.
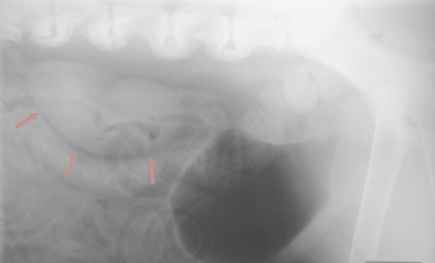
Fig. 10.3 Radiograph of the kidney area. The bladder has been inflated with air for contrast and the kidney (arrows) can be seen to measure about 2.5 times the length of the lumbar vertebrae.
When examining the cut surface of a normal kidney cut longitudinally, it is possible to see four layers (Fig. 10.4). From the outside inwards these are:
Blood supply
Arterial blood is carried from the aorta in a single renal artery to each kidney (Fig. 10.4). This carries 20% of cardiac output. Within the tissue of the kidney, the renal artery divides into several interlobar arteries, which pass between the renal pyramids and into the cortex. Here capillaries supply the renal tubules and also give off numerous capillary networks known as glomeruli (sing. glomerulus) (Fig. 10.5). Each glomerulus supplies an individual nephron. The capillaries then recombine to form interlobar veins, which enter the single renal vein. This carries venous blood to the caudal vena cava.
Blood entering the kidney carries oxygen, nutrients and waste products from the tissues of the body; blood leaving the kidney carries carbon dioxide produced by the kidney tissues, but the nitrogenous waste products have been removed via the glomeruli.
Microscopic structure
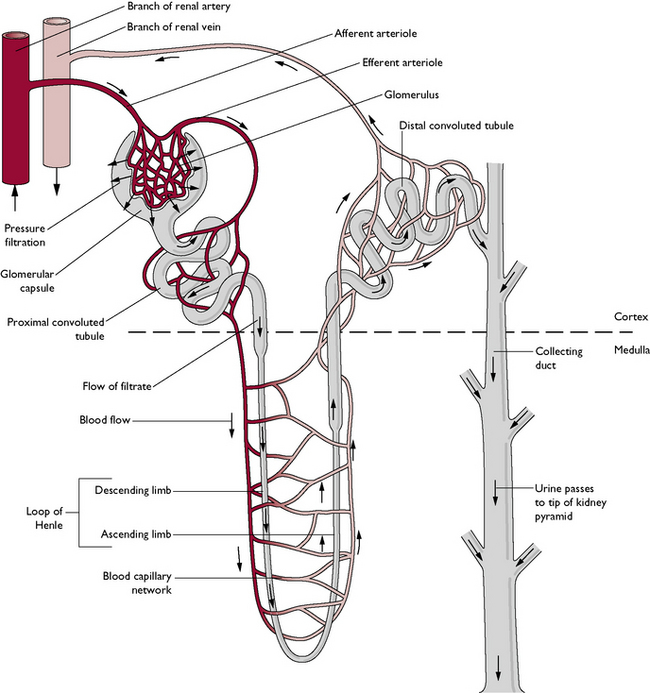
The functional unit of the kidney is the nephron (Fig. 10.5). Each kidney contains about a million nephrons, which are closely packed together. They are responsible for the filtration of blood and the production of urine. Each nephron is a long tubule divided into several parts:
Renal function – the formation of urine
Blood is filtered by the kidneys and the resulting filtrate undergoes a series of modifications within the renal tubules to produce urine. This urine is very different in composition and volume from the original filtrate. For every 100 L of fluid filtered from the blood only 1 L is produced as urine – 99% of the original filtrate is reabsorbed back into the blood. The changes made to the filtrate reflect the status of the extracellular fluid (ECF) and in particular that of the blood plasma.
The physiological processes occurring in the renal nephrons are:
Blood enters the kidney and is carried to the capillaries forming the glomeruli.
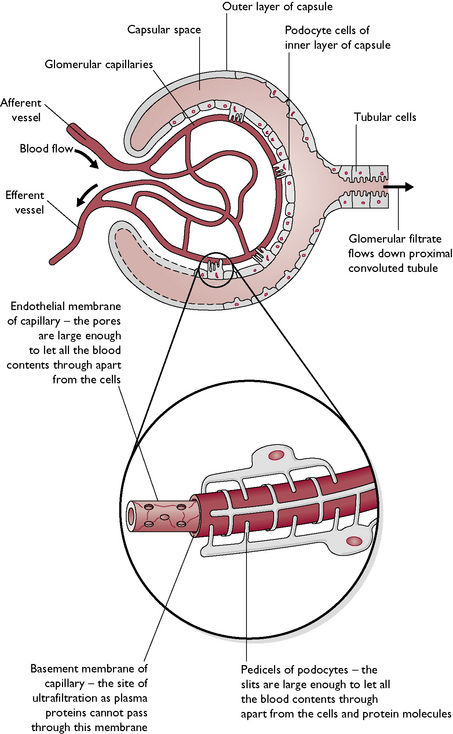
Glomerulus
Blood pressure within each glomerulus is high because:
High pressure in the glomerulus forces fluid and small molecules out of the blood through the pores of the basement membrane into the capsule lumen. Larger-sized particles such as red blood cells, plasma proteins and any substance bound to protein molecules, e.g. hormones are retained in the blood. This process is known as ultrafiltration and the filtrate is referred to as the glomerular filtrate or primitive urine. The glomerular filtrate is very dilute and contains 99% water and 1% chemical solutes.
Proximal convoluted tubule
Approximately 65% of all the resorptive processes take place here (Fig. 10.7). These are:
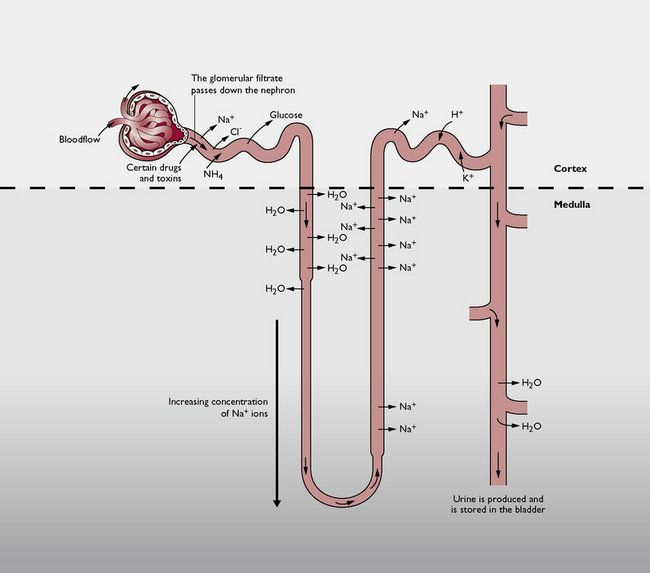
Fig. 10.7 Diagrammatic representation of the processes occurring in the different parts of the nephron.
In cases of diabetes mellitus, there is too much glucose in the blood (hyperglycaemia). This overflows into the glomerular filtrate and the tubules reabsorb it up to the limit of the renal threshold. The excess passes on down the tubules and out in the urine – glucosuria is a diagnostic sign of diabetes mellitus.
Loop of Henle
The function of the loop of Henle is to regulate the concentration and volume of the urine according to the status of the ECF. The glomerular filtrate flows first into the descending loop and then into the ascending loop, both of which lie in the medulla (Fig. 10.7).
The net result of this mechanism is that the filtrate is the same concentration when it enters the loop of Henle as it is when it leaves and passes into the distal convoluted tubule, but it is reduced in volume as water has been removed. This water is reabsorbed into the blood – it has been conserved for use by the body. If the animal is dehydrated, more water is reabsorbed; if it is overhydrated, more water will be lost in the filtrate.
Distal convoluted tubule
It is here that the final adjustments are made to the chemical constituents of the urine in response to the status of the ECF. This is achieved by:
Collecting duct
Here the final adjustments are made to the volume of water in the urine in response to the status of the ECF (Fig. 10.7). The hormone antidiuretic hormone (ADH), produced by the posterior pituitary gland, is able to change the permeability of the duct walls to water.
Diuretics are drugs used to increase the volume of urine produced and so reduce the volume of fluid in the body. One of the most commonly used – furosemide – is a ‘loop diuretic’, which acts on the loops of Henle. It prevents reabsorption of Na+ so water is not resorbed by osmosis and remains in the urine as it flows through the tubules.
As a result of the above processes, the ultrafiltrate that passed through the glomerular capsule has now become concentrated urine by the repeated effects of reabsorption and secretion.
Osmoregulation – control of renal function
Osmoregulation ensures that the volume of the plasma and the concentration of dissolved chemicals in the plasma and other tissue fluids remains constant. Homeostasis is maintained and the body can function normally. Several factors are involved in the control of osmoregulation (Table 10.1) and it is achieved in two ways:
Table 10.1 Factors involved in osmoregulation
| Controlling factor | Function |
|---|---|
| Renin (hormone) | Produced by the glomeruli of the kidney in response to low arterial pressure |
| Angiotensinogen (plasma protein) | Converted to angiotensin by the action of renin |
| Angiotensin (protein) | Causes vasoconstriction; stimulates the release of aldosterone from the adrenal cortex |
| Aldosterone (hormone – mineralocorticoid) | Secreted by the cortex of the adrenal gland; acts mainly on the distal convoluted tubules but has a lesser effect on the collecting ducts; regulates the reabsorption of Na+ ions |
| Antidiuretic hormone (ADH or vasopressin) | Secreted by the posterior pituitary gland; mainly affects the collecting ducts by changing their permeability to water; also has an effect on the distal convoluted tubules |
| Baroreceptors | Found in the walls of the blood vessels; monitor arterial blood pressure |
| Osmoreceptors | Found in the hypothalamus; monitor the osmotic pressure of the plasma; affect the thirst centre of the brain and influence the secretion of ADH |
Control of water loss
Water is lost by the healthy animal in urine, faeces, sweat and in respiration. Very small amounts may also be lost in vaginal secretions and tears. If this water loss is not replaced by food and drink, or if the water loss is excessive, e.g. in vomiting, diarrhoea or haemorrhage, the total volume of ECF falls and the animal is described as being dehydrated.
A dehydrated patient will show:
Note: Osmotic pressure is the pressure needed to prevent osmosis from occurring. It is dependent on the number of particles of undissolved molecules and ions in a solution. Blood pressure is the pressure exerted on the inside of the walls of the arterial blood vessels by the blood. It is detected by baroreceptors in the walls of the vessels.
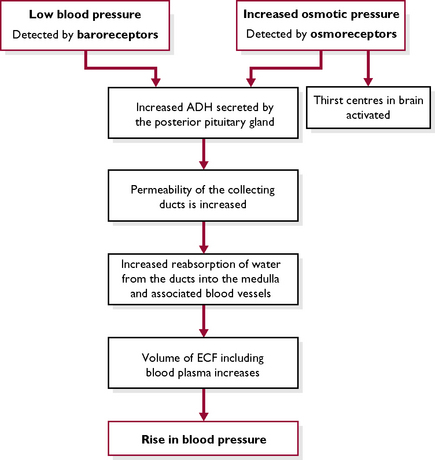
In dehydration, osmoregulatory mechanisms will start to work (Fig. 10.8). The fall in blood pressure and rise in osmotic pressure ultimately result in an increase in the reabsorption of water from the collecting ducts, under the control of the hormone ADH (see Ch. 6). The osmoreceptors also stimulate the thirst centre in the brain and the animal feels the need to drink. Both of these pathways result in a rise in plasma volume and an increase in arterial blood pressure. Dehydrated animals should be given fluid parenterally (intravenously) or, in less severe cases, provided with access to drinking water. They will excrete reduced quantities of concentrated urine.
Raised blood pressure will result in the opposite effect, and the animal will produce increased quantities of more dilute urine.
Control of sodium levels
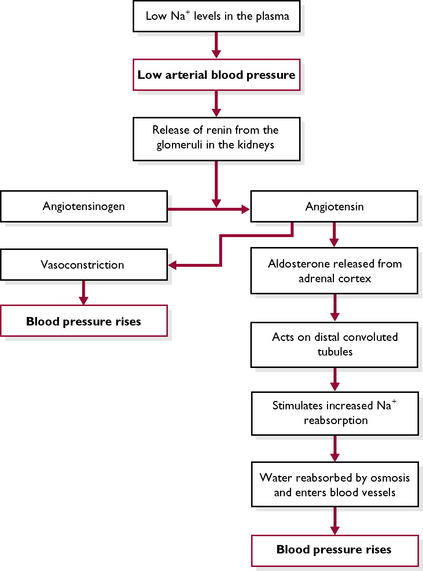
Sodium is taken into the body in the form of salt (NaCl) in food. It is lost in sweat, faeces and urine. Sodium is found in the ionised form Na+ in all the body fluid compartments and plays a fundamental part in determining arterial blood pressure. High Na+ levels in the diet draw water into the plasma by osmosis. This raises blood volume and blood pressure also rises. Conversely, if an animal has a low level of Na+, less water is drawn into the plasma and blood volume falls – this lowers the arterial blood pressure. The osmoregulatory mechanisms take steps to correct this, resulting in a compensatory rise in blood pressure (Fig. 10.9).
Regulation of Na+ in the plasma occurs mainly in the distal convoluted tubule and is controlled by the hormone aldosterone, secreted by the cortex of the adrenal gland (see Ch. 6).
Excretion
Excretion is the removal of waste products from the body. These are formed within the tissues as a result of metabolic processes and are useless, surplus to the requirements of the body or potentially harmful to the body tissues. Excretion by the kidneys removes:
Urea passes into the circulation and is carried to the kidney where it is excreted in the urine.
Kidney disease can present in many forms and the symptoms are related to the fact that all kidney functions are affected and the homeostatic mechanisms cease to work. Chronic renal failure commonly occurs in older cats and dogs and develops when the nephrons are gradually replaced by fibrous connective tissue as a normal ‘old age’ change. Symptoms, many of which are related to rising levels of urea in the blood, develop when 75% of the nephrons have ceased to function.
Other parts of the urinary system
The ureters
Urine formed by the nephrons leaves each kidney by a single ureter at a point known as the hilus (Fig. 10.4). Each ureter is a narrow muscular tube running caudally towards the bladder, one on each side of the midline in the dorsal abdomen (Figs 10.2, 10.3). Each ureter is suspended from the dorsal body wall by a fold of visceral peritoneum, the mesoureter.
Urine is pushed along the tube towards the bladder by peristaltic waves brought about by contraction of the smooth muscle fibres forming the ureter walls. Transitional epithelium lines the ureters and allows for expansion as urine passes along.
The bladder
Each ureter enters the single bladder close to the neck. The ureters underrun the bladder mucosa for a short distance before opening into the lumen at an oblique angle. This area, known as the trigone, acts as a valve preventing the backflow of urine along the ureter (Fig. 10.2).
The bladder is a pear-shaped hollow organ. The rounded end points cranially, while the narrow end or neck points caudally and usually lies within the pelvic cavity. Its function is to collect and store urine. When full, the bladder extends into the abdomen, pulling the neck ventrally over the edge of the pelvic brim with the ventral surface of the bladder touching the abdominal floor; when empty most of the bladder lies in the pelvic cavity.
In cross-section, the bladder consists of an inner lining of transitional epithelium, which enables the walls to expand when filling with urine. A submucosal layer of elastic tissue and smooth muscle is arranged in folds to allow expansion. The smooth muscle fibres are continuous with those of the internal bladder sphincter. The bladder is surrounded by a layer of peritoneum, which covers only the cranial end lying in the abdomen. All organs in the pelvic cavity are surrounded by connective tissue and muscle and are not covered in peritoneum.
Urolithiasis is the formation of mineral ‘stones’ known as uroliths or calculi in the bladder. These may cause a blockage in the urinary tract. The most common site for blockage in the cat is at the tip of the penis; the most common site in the male dog is as the urethra bends over the ischial arch and as it passes through the os penis. Blockage is rare in the female animal because the urethra is shorter and more distensible.
The neck of the bladder ends in the bladder sphincter, whose function is to control the flow of urine out of the bladder and down the urethra. It consists of two concentric parts:
The urethra
The urethra is a tube which conveys urine caudally from the bladder through the pelvic cavity to the outside. Its structure varies according to the sex of the animal, and in the case of the male animal, between cats and dogs.
From the point at which the deferent ducts join it, the urethra conveys both urine and sperm to the outside of the body.
Micturition
Micturition (often incorrectly referred to as urination) is the act of expelling urine from the bladder. It is normally a reflex activity but can be overridden by voluntary control from the brain. The steps involved are:
If it is inappropriate for the animal to micturate, the brain overrides the reflex pathway and prevents the bladder sphincter from relaxing. At a more appropriate time, the brain stimulates both the external and internal sphincters: they relax and urine is released. Voluntary control develops as the young animal matures – in puppies and kittens it is not fully developed until the animal is about 10 weeks old.
Urinalysis
Urine is derived from the ultrafiltrate of plasma so it reflects the health status of the whole animal. The analysis of urine, or urinalysis, is a useful diagnostic tool. Normal urine contains only water, salts and urea. The clinical parameters used to evaluate a sample of urine are shown in Table 10.2.
Table 10.2 Normal values shown by the urine of the dog and cat
| Clinical parameter | Normal value | Comments |
|---|---|---|
| Daily volume | Dog: 20–100 ml/kg body weight | Polyuria – increased volume of urine |
| Oliguria – reduced volume of urine | ||
| Cat: 10–12 ml/kg body weight | Anuria – absence of urine | |
| Appearance | Clear, yellow, characteristic smell | Tomcat urine has an unpleasant strong smell; old samples smell ammoniacal |
| pH | 5–7 | Carnivorous diet produces acid urine; herbivorous diet produces alkaline urine |
| Specific gravity (s.g.) | Dog: 1.016–1.060 | Reflects the concentration of urine; exercise, high environmental temperatures and dehydration will cause a rise in specific gravity |
| Cat: 1.020–1.040 | ||
| Protein | None | Proteinuria – presence of protein. |
| May indicate damage to nephrons, chronic renal failure, inflammation of the urinary tract | ||
| Blood | None | Haematuria – presence of blood |
| Haemoglobinuria – presence of haemoglobin, due to rupture of red cells | ||
| May indicate damage or infection to the urinary tract. | ||
| Glucose | None | Glucosuria – presence of glucose |
| May indicate diabetes mellitus; levels of glucose in the filtrate exceed the renal threshold and excess is excreted in the urine | ||
| Ketones | None | Ketonuria – presence of ketones |
| May be accompanied by acid pH and smell of ‘peardrops’ in urine and on the breath | ||
| Bile | None | Bilirubinuria – presence of bile |
| Indicator of some form of liver disease | ||
| Crystals and casts | In small quantities, these may be considered to be normal | Crystalline or colloidal material coalesce to form a cast of the renal tubules and are flushed out by the urine; in large quantities crystals may form calculi or uroliths and block the tract |