KEY POINTS
•
The endocrine system is part of the regulatory system of the body and works in conjunction with the nervous system. The nervous system produces an immediate response while the endocrine system produces a slower but longer-lasting effect.
•
Endocrine glands secrete hormones, which are carried by the blood to specific target organs.
•
Each target organ responds only to a particular hormone or to a group of hormones and is unaffected by other hormones.
•
Hormonal secretion is controlled by different mechanisms, e.g. levels of a chemical in the blood, or by a feedback loop.
•
Each hormone has a specific effect and many interrelate with other hormones to create a complex network that acts to maintain the body in a state of equilibrium.
Basic functions and hormones
The endocrine system forms part of the regulatory system of the body and works in conjunction with the other regulatory mechanism, the nervous system. A series of endocrine glands secrete chemical messengers known as hormones, which are carried by the blood to their target organs. These may be some distance away from the gland. In contrast, exocrine glands produce secretions that are released via ducts and lie close to their effector organs, e.g. sweat glands, gastric glands.
Chemically, hormones may be steroids, proteins or amines (derived from amino acids). They regulate the activity of the target organ, which responds to that particular hormone. All other organs are unaffected. The response produced by hormones is slower and lasts longer, and complements the rapid and relatively short-lived responses produced by the nervous system.
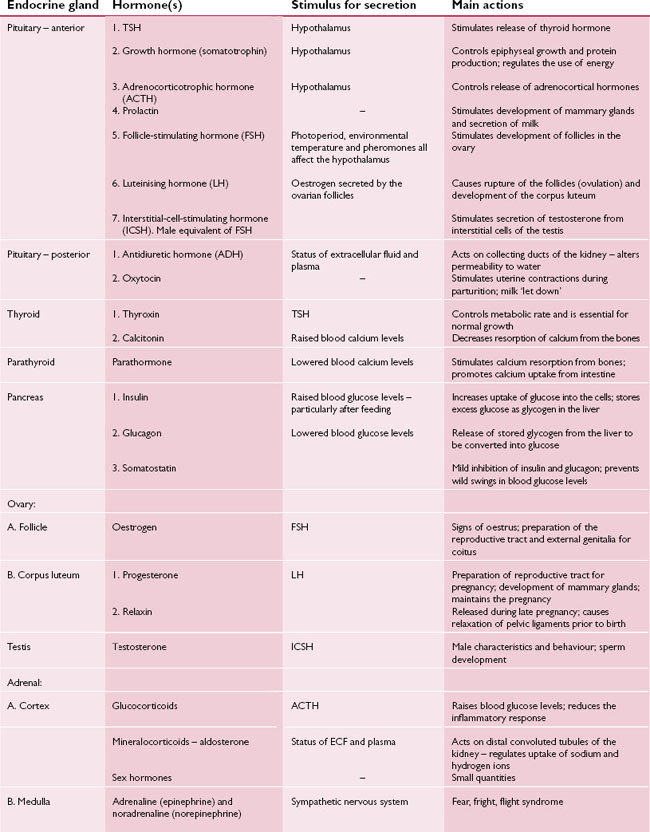
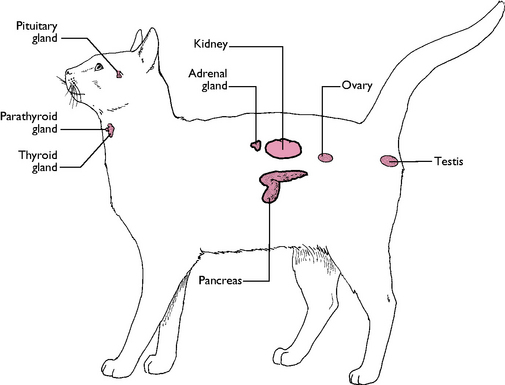
The endocrine glands are distributed throughout the body and may secrete more than one hormone (Fig. 6.1).
The glands are:
Secretion of a hormone occurs in response to a specific stimulus (Table 6.1). Stimuli may be:
•
Nerve impulses, e.g. adrenaline (epinephrine) is released from the adrenal medulla in response to nerve impulses from the sympathetic nervous system.
•
A stimulating or releasing hormone, e.g. TSH (thyrotrophic/thyroid-stimulating hormone) from the anterior pituitary gland activates the thyroid gland.
•
Levels of certain chemicals in the blood, e.g. raised blood glucose levels stimulate the release of insulin from the pancreas.
•
Feedback loops, which prevent oversecretion or reduce secretion once the effect has been achieved, e.g. oestrogen from the ovarian follicles prevents further secretion of follicle-stimulating hormone from the anterior pituitary gland, so preventing further follicular development (see
Fig. 6.4).
Not all hormones are secreted by endocrine glands – some are produced from tissue within another organ, including:
•
Gastrin – produced by the wall of the stomach. As food enters the stomach via the cardiac sphincter, gastrin stimulates the release of gastric juices from the gastric glands and digestion begins.
•
Secretin – produced by the wall of the small intestine. As food enters the duodenum from the stomach, secretin stimulates the secretion of intestinal and pancreatic juices which continue the process of digestion.
•
Chorionic gonadotrophin – produced during pregnancy by the ectodermal layer of the chorion surrounding the conceptus. It helps to maintain the corpus luteum in the ovary throughout gestation.
•
Erythropoietin or
erythropoietic-stimulating factor – produced by the kidney in response to low levels of blood oxygen. It stimulates the bone marrow to produce erythrocytes or red blood cells.
Endocrine glands
Pituitary gland
This is a small gland lying ventral to the hypothalamus in the forebrain (Fig. 6.1). It is also known as the hypophysis and is divided into two lobes, each of which acts as a separate gland. The pituitary gland is often referred to as the ‘master gland’ as its hormones control the secretions of many of the other endocrine glands.
Anterior pituitary gland
Also known as the adenohypophysis, this produces:
•
Thyrotrophic/thyroid stimulating hormone (TSH) – stimulates the thyroid gland.
•
Growth hormone or
somatotrophin – controls the rate of growth in young animals by:

Controlling the rate of growth at the epiphyses of the bones

Being involved in protein production from amino acids

Regulating the use of energy during periods of poor food supply. Glucose is conserved for use by the nervous system and fat is broken down to be used as a source of energy by the rest of the body
•
Adrenocorticotrophic hormone (ACTH) – stimulates the adrenal cortex. Oversecretion may cause the symptoms of Cushing’s disease.
•
Prolactin – stimulates the development of the mammary glands and the secretion of milk during the latter half of pregnancy. The milk cannot be released unless oxytocin is produced at the end of the gestation period.
•
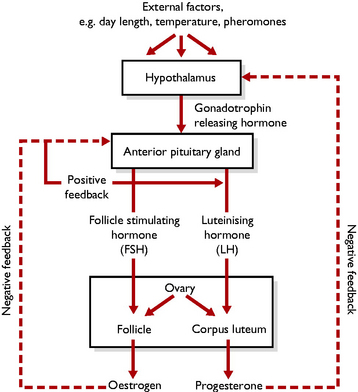
Follicle stimulating hormone (FSH) – at the start of the oestrous cycle, or at puberty, external factors, e.g. day length (photoperiod), temperature or pheromones secreted by the male or other females, affect the hypothalamus. This secretes
gonadotrophin-releasing hormone which stimulates the anterior pituitary gland to secrete FSH. FSH stimulates germ cells in the ovary to develop into follicles, each containing an ovum
Fig. 6.4.
•
Luteinising hormone (LH) – secretion is stimulated by the presence of oestrogen in the blood. LH stimulates the ripe follicles in the ovary to rupture and release their ova (ovulation). The remaining tissue becomes ‘luteinised’ to form the corpus luteum
Fig. 6.4.
•
Interstitial cell stimulating hormone (ICSH) – stimulates the interstitial cells or cells of Leydig in the testis to secrete testosterone. This is the male equivalent of FSH.
Posterior pituitary gland
The posterior pituitary gland is also known as the neurohypophysis. The hormones associated with this part of the pituitary gland are secreted by the hypothalamus and only stored here. They are:
•
Antidiuretic hormone (ADH) – also called vasopressin. This hormone alters the permeability of the collecting ducts of the kidney to water. It is secreted in response to the changing volume of extracellular fluid (ECF) and helps maintain homeostasis (see
Ch. 10).
•
Oxytocin – this has two effects:

It acts on the mammary glands during late pregnancy and causes the milk to be released or ‘let down’ in response to suckling by the neonate

At the end of gestation, oxytocin causes the contraction of the smooth muscle of the uterus, resulting in parturition and delivery of the fetuses.
Thyroid glands
These lie in the midline on the ventral aspect of the first few rings of the trachea (Fig. 6.1). They are controlled by TSH from the anterior pituitary gland and secrete three hormones:
•
Thyroxin (or T
4) and
tri-iodothyronine (or T
3) – have a similar effect. Tri-iodothyronine contains a high proportion of the trace element iodine – a lack of iodine in the diet can have a dramatic effect. Both hormones affect the uptake of oxygen by all the cells in the body and are essential for normal growth.
Undersecretion – hypothyroidism – is more common in dogs. In young animals, hypothyroidism causes dwarfism (stunted growth). In older animals, the condition is known as myxoedema: the dog becomes fat and sluggish, alopecic, the skin feels cold and clammy and the heart rate slows – all due to a reduced metabolic rate.
Oversecretion – hyperthyroidism – is more common in old cats. The affected animal is thin, active, often aggressive, has a good appetite and a fast heart rate – all due to a raised metabolic rate.
•
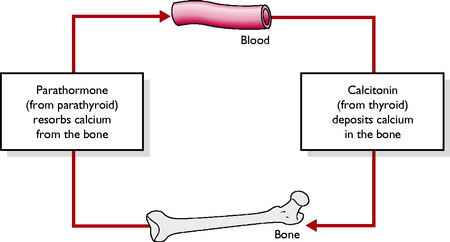
Calcitonin – lowers the levels of blood calcium by decreasing the rate of bone resorption. When levels of blood calcium are high, e.g. if a calcium rich diet is eaten, calcium is deposited in the bone and acts as a reservoir for later use (
Fig. 6.2). Calcitonin has an opposite effect to parathormone but is of less importance.
Parathyroid glands
These glands lie on either side of the thyroid gland and secrete the hormone parathormone (Fig. 6.1). Secretion is dependent on the levels of calcium in the blood – if levels are low, calcium is resorbed from the bones and absorption of calcium from the intestine is increased (Fig. 6.2).
Oversecretion (hyperparathyroidism) occurs in:
•
Primary hyperparathyroidism – due to neoplasia of the parathyroid glands. This causes bone resorption, bone weakness and pathological fractures.
•
Secondary hyperparathyroidism – as seen in chronic renal failure. The calcium:phosphate ratio in the blood is altered by impaired kidney function. This leads to increased output of parathormone and consequently increased resorption of bone in an effort to maintain blood calcium levels. There is preferential resorption from the mandible and maxilla, producing a condition known as ‘rubber jaw’ – the jaw becomes pliable and fragile and the teeth may fall out.
•
Nutritional hyperparathyroidism – results from feeding low calcium diets, e.g. an all-meat diet. Parathormone is produced in an attempt to raise the blood calcium levels by bone resorption.
Pancreas
The pancreas is a pinkish lobular gland lying in the loop of the duodenum in the abdominal cavity (Fig. 6.1). It has an exocrine part and an endocrine part and is described as being a mixed gland. The exocrine secretions, which are digestive juices, enter the duodenum via the pancreatic duct (see Ch. 9). The endocrine secretions are produced by discrete areas of tissue within the exocrine tissue, known as the islets of Langerhans.
The islets of Langerhans secrete three hormones, each from a different type of cell:
•
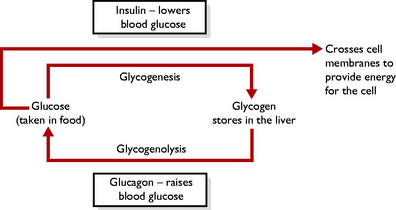
Insulin (from the beta cells) – secreted in response to high blood glucose levels. Insulin lowers blood glucose levels by:

Increasing the uptake of glucose into the cells, where it is metabolised to provide energy

Storing excess glucose as glycogen in the liver. Conversion of glucose to glycogen occurs by a process known as
glycogenesis (
Fig. 6.3).
Lack of insulin leads to a condition known as diabetes mellitus, in which the animal suffers from hyperglycaemia and glucosuria (the presence of glucose in the urine). If left untreated, the condition may progress to a stage where the body uses its protein and fat stores as a source of energy. Daily insulin injections and dietary control are necessary to control the condition.
•
Glucagon (from the alpha cells) – secreted in response to low blood glucose levels. Glucagon raises blood glucose levels by breaking down the glycogen stores in the liver. Conversion of glycogen to glucose occurs by a process known as
glycogenolysis (
Fig. 6.3).
•
Somatostatin (from the delta cells) – this is mildly inhibitory to the secretions of insulin and glucagon and prevents wild fluctuations in blood glucose levels, which may damage the tissues. It also decreases gut motility and the secretion of digestive juices, which serve to reduce the efficiency of the digestive and absorptive processes.
The ovary
Female mammals have two ovaries, which lie one on each side of the dorsal abdominal cavity caudal to the kidneys. At the onset of sexual maturity, the two ovaries become capable of secreting two hormones:
•
Oestrogen – produced by the walls of the developing
ovarian follicles. Development of germ cells in the ovary into ripe follicles is the result of the secretion of FSH from the anterior pituitary gland. Oestrogen causes the behaviour associated with the oestrous cycle and prepares the reproductive tract and external genitalia for mating (see
Ch. 11). Oestrogen also exerts negative feedback on the anterior pituitary gland, preventing further secretion of FSH and further follicular development (
Fig. 6.4).
•
Progesterone – secreted by the
corpus luteum, which develops from the remaining follicular tissue after the follicle has ovulated. The corpus luteum develops as a result of the production of LH from the anterior pituitary gland. Progesterone prepares the reproductive tract for pregnancy and maintains the pregnancy (see
Ch. 11). During pregnancy, progesterone exerts negative feedback on the hypothalamus and prevents secretion of
gonadotrophin-releasing hormone and so prevents further oestrous cycles until parturition occurs.
It also causes development of the mammary glands during pregnancy (
Fig. 6.4).
In the later stages of pregnancy, the corpus luteum also secretes a hormone known as relaxin. This causes the sacroiliac and other ligaments around the birth canal to soften and relax in preparation for parturition.
The testis
Male mammals possess a pair of testes, which are carried external to the abdominal cavity within the scrotum. At the start of sexual maturity, the testes begin to secrete two hormones:
•
Testosterone – produced by the
interstitial cells or
cells of Leydig in response to the secretion of ICSH from the anterior pituitary gland. Testosterone is responsible for:

The development of male characteristics such as penis development, development of the barbs on the feline penis, muscle development, jowls on the face of a tomcat, size

Male behaviour patterns, e.g. sexual drive, aggression, territorial behaviour, courtship displays and mating behaviour
^
Development of spermatozoa
•
Oestrogen – produced in small quantities by the
Sertoli cells in the seminiferous tubules of the testes.
Adrenal glands
There is a pair of adrenal glands, one lying close to the cranial pole of each kidney (Fig. 6.1). Each gland has an outer cortex and an inner medulla. There is no connection between the two parts and they can be considered as two separate glands.
Adrenal cortex
The hormones produced are known as steroids and have a similar structure based on lipid. There are three groups, each one being secreted by a different layer:
•
Glucocorticoids – secretion is regulated by ACTH from the anterior pituitary gland. The hormones are known as
corticosteroids; the most important are
cortisol and
corticosterone. In the normal animal they are present in low levels but increase in response to stress. They have two main actions:

They increase blood glucose levels by reducing glucose uptake by the cells, increasing the conversion of amino acids to glucose in the liver (a process known as
gluconeogenesis) and mobilising fatty acids from the adipose tissue ready for conversion to glucose

When present in large quantities, they depress the inflammatory reaction, which delays healing and repair. This property is used therapeutically to reduce swelling and inflammation.
Oversecretion of glucocorticoids, or hyperadrenocorticalism, leads to symptoms of Cushing’s disease. These include polydipsia, polyuria, polyphagia and bilateral symmetrical alopecia.
•
Mineralocorticoids – the most important is
aldosterone. This acts on the distal convoluted tubule of the kidney where it regulates acid–base balance of the plasma and ECF by excretion of H
+ ions and also controls the excretion of Na
+ and K
+ ions (see
Ch. 10).
•
Adrenal sex hormones – both male and female animals produce all types of sex hormones. They are secreted in insignificant quantities but may be the reason why some animals show a certain level of sexual behaviour despite being neutered.
Adrenal medulla
This produces two hormones with similar actions: adrenaline (epinephrine) and noradrenaline (norepinephrine). These hormones prepare the body for emergency action, known as the ‘fear, flight, fight’ syndrome, and are controlled by the sympathetic nervous system. Their actions are to:
•
Raise blood glucose levels by the breakdown of glycogen stored in the liver –
glycogenolysis. This increases the body’s energy levels
•
Increase the heart rate and the rate and depth of respiration – this increases the amount of oxygen reaching the tissues
•
Dilate the blood vessels of the skeletal muscles – this enables the supply of glucose and oxygen to reach the areas where it is needed
•
Decrease the activity of the gastrointestinal tract and the bladder – in an emergency their functions are less important.
 Storing excess glucose as glycogen in the liver. Conversion of glucose to glycogen occurs by a process known as glycogenesis (Fig. 6.3).
Storing excess glucose as glycogen in the liver. Conversion of glucose to glycogen occurs by a process known as glycogenesis (Fig. 6.3). The development of male characteristics such as penis development, development of the barbs on the feline penis, muscle development, jowls on the face of a tomcat, size
The development of male characteristics such as penis development, development of the barbs on the feline penis, muscle development, jowls on the face of a tomcat, size They increase blood glucose levels by reducing glucose uptake by the cells, increasing the conversion of amino acids to glucose in the liver (a process known as gluconeogenesis) and mobilising fatty acids from the adipose tissue ready for conversion to glucose
They increase blood glucose levels by reducing glucose uptake by the cells, increasing the conversion of amino acids to glucose in the liver (a process known as gluconeogenesis) and mobilising fatty acids from the adipose tissue ready for conversion to glucose