Oral Microbiology and Plaque-associated Diseases
After completing this chapter, the student should be able to do the following:
 Describe the general nature of the normal oral microbiota.
Describe the general nature of the normal oral microbiota.
 Define biofilm and describe how it forms on teeth.
Define biofilm and describe how it forms on teeth.
 List the types of dental caries.
List the types of dental caries.
 Describe the consequences of untreated dental caries.
Describe the consequences of untreated dental caries.
 Describe the mechanism of dental caries formation.
Describe the mechanism of dental caries formation.
 Differentiate the types of periodontal diseases.
Differentiate the types of periodontal diseases.
 Describe the mechanism of periodontal diseases.
Describe the mechanism of periodontal diseases.
 List the microbes most important in causing dental caries and periodontal diseases.
List the microbes most important in causing dental caries and periodontal diseases.
 List the general approaches to preventing plaque-associated diseases.
List the general approaches to preventing plaque-associated diseases.
The mouth contains the normal oral microbiota that have colonized and continually are maintained on the teeth and soft tissues and in saliva. These microorganisms usually cause no harm except when they are allowed to accumulate in the form of dental plaque or are displaced from the mouth to deeper tissues such as the tooth pulp or to other body sites such as the bloodstream.
NORMAL ORAL MICROBIOTA
The human mouth usually is first exposed to microorganisms at birth during passage through the birth canal. Most of the mother’s vaginal bacteria that enter the child’s mouth are transient (short-lived) and do not establish themselves as regular members of the oral microbiota. With time, the child is exposed to microorganisms from the environment, and the main sources of microorganisms that colonize the child’s mouth appear to be the mouths of other persons, particularly the mother and other close family members.
For microorganisms to become established members of the oral microbiota, they must attach to oral surfaces and be able to multiply in the oral environment. Eruption of the primary teeth results in a major change in this environment, now providing tooth surfaces, gingival crevices, and more opportunity for bleeding into the mouth. New bacteria, such as Streptococcus mutans, appear that can survive only on the teeth. Anaerobes increase in number because of the added anaerobic sites around the teeth. Thus different sites in the mouth (tongue, buccal epithelium, supragingival tooth surfaces, subgingival tooth surfaces, and crevicular epithelial surfaces) support different combinations of microorganisms. As one grows older, more and more microorganisms colonize the mouth, and in general the composition stabilizes by the early teen years.
The normal oral microbiota consists mostly of bacteria, although about one third of the population also has the yeast Candida albicans in their mouth. The oral microbiota is complex, with about 40 genera of bacteria represented (Box 5-1), although not every person has all of these genera present all of the time. Each genus may be represented by several species, resulting in a complex group of gram-positive and gram-negative bacteria. A gram of dental plaque (about one quarter of a teaspoonful) contains almost 200 billion bacteria, and saliva contains 10 million to 100 million bacteria per milliliter.
MICROBIOLOGY OF CARIES
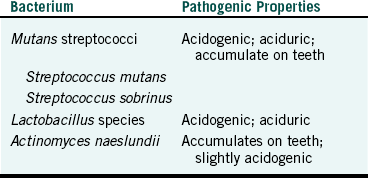
Dental caries is an infectious disease and is caused by a demineralization of tooth structure by acids produced during metabolism of dietary sugars by bacteria associated with the tooth surfaces (Figure 5-1). As with any infectious disease, four factors are necessary for caries to occur: susceptible host, microorganisms, substrate, and time.
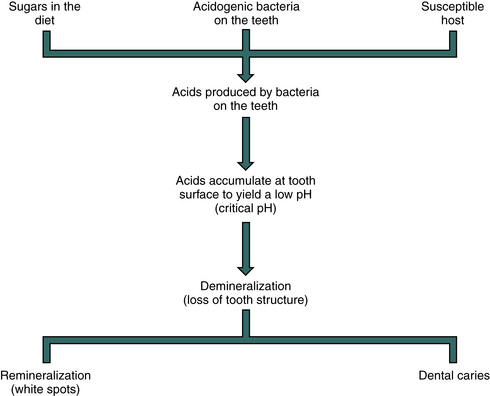
FIGURE 5-1 Formation of dental caries. In a person susceptible to dental caries the acidogenic bacteria on the teeth ferment sugars in the diet to acids (mainly lactic acid). The acids accumulate on the tooth surface, lowering the pH to a critical level of about 5.2. At this pH the minerals in the tooth start to dissolve, causing loss of tooth structure (demineralization). A natural body defense mechanism called remineralization attempts to restore the lost calcium and phosphate in the tooth, which will appear as a white spot on the tooth. If remineralization occurs more slowly than demineralization, dental caries occurs.
Susceptible Host
Not all individuals are susceptible to all infectious diseases. Resistance may be attributable to many factors (other than specific immunity) that are not well understood. In the case of caries-free persons, resistance has not been explained clearly but may involve characteristics of saliva, anatomic differences in the teeth, or the nature of the oral microbiota. Nevertheless, for caries to occur, the person must be susceptible to the disease.
Microorganisms
Bacteria capable of causing caries must be present in the mouth and must be associated closely with the teeth. This association may be in the form of dental plaque, a microbial mass that accumulates on the teeth in the absence of oral hygiene, or may result from an impaction of bacteria and food in the non–self-cleansing areas of the dentition (pits and fissures, interproximal sites, gingival crevices).
DENTAL PLAQUE (ORAL BIOFILM)
Plaque is a biofilm composed of bacterial cells embedded in an intercellular matrix (Figure 5-2). The matrix contains macromolecules and small molecules that (1) are produced by the multiplying bacteria, (2) may enter the mouth in the diet, and (3) originate from mammalian cells, saliva, or blood.

FIGURE 5-2 Relatively thin predominantly coccal flora (plaque) on the enamel surface associated with nondisease gingival tissue. E, Enamel; M, columnar microcolony. (From Listgarten MA: Structure of surface coatings of teeth. J Periodontol 47:3, 1976.)
Plaque begins to reform within seconds after the teeth are cleaned. Glycoproteins from saliva are first absorbed onto the tooth surface to a thin proteinaceous layer called the pellicle that coats all tooth surfaces exposed to saliva. Next, the bacteria attach to the pellicle, and these serve as an initial “layer” to which other bacterial cells attach. These other cells may come from saliva, or they may be the daughter cells formed from previously attached cells that are multiplying. Plaque accumulates most rapidly in the non–self-cleansing areas of the dentition where the tip of the tongue, the musculature of the cheeks, and the occlusion of the teeth cannot remove the accumulating bacteria. As the plaque accumulates in the absence of oral hygiene, potentially harmful products from the multiplying bacteria accumulate and may cause damage to the teeth (caries) or to the nearby periodontal tissues (gingivitis or periodontitis).
Many are the mechanisms by which bacteria attach to tooth surfaces or to each other during plaque formation. Some mechanisms involve interactions of the bacteria with glycoproteins or calcium from saliva or the pellicle, some involve fimbriae or special receptors on the surfaces of the bacteria, and others involve extracellular macromolecules produced by the bacteria that then can bind to cell surfaces. One approach to prevention of plaque-associated diseases (caries, periodontal diseases) other than brushing and flossing is to develop special mouth rinses that interfere with bacterial attachment to the teeth to prevent plaque from accumulating.
CARIES-CONDUCIVE BACTERIA
Although dental plaque contains many different species of bacteria, some are more important than others in directly contributing to the initiation or progression of dental caries (Table 5-1).
A group of closely related streptococci called the mutans streptococci consist of the most caries-conducive bacteria in the mouth. Members of this group that are most commonly present in the human mouth are S. mutans and S. sobrinus. Other species in this group occur in the mouth less frequently. The mutans streptococci have all three pathogenic properties important for caries formation:
The mutans streptococci are thought to be the most important oral bacteria in initiating caries, particularly on smooth tooth surfaces (buccal and lingual) where plaque that can resist the cleansing action of the tongue and cheeks “rubbing” against the teeth is needed for caries to develop. Mutans streptococci are important plaque formers and can accumulate rapidly in plaque in the presence of sucrose (table sugar). The mutans streptococci have special enzymes (glucosyltransferases) that split sucrose, linking together the glucose units of the sucrose molecules to form polysaccharides called glucans (Figure 5-3). The remaining fructose part of sucrose is taken into the cell and processed through catabolic fermentation reactions to produce energy with mainly lactic acid as a waste product (see Chapter 2). The glucans bind to the cells and act as bridges that bind to other cells. This binding permits new daughter cells to attach to the cell mass and accumulate in the developing dental plaque. The mutans streptococci not only produce acids (are acidogenic) from sugar metabolism but also are capable of surviving and metabolizing in the presence of these acids at a low pH (are aciduric), whereas most bacteria die at a low pH.
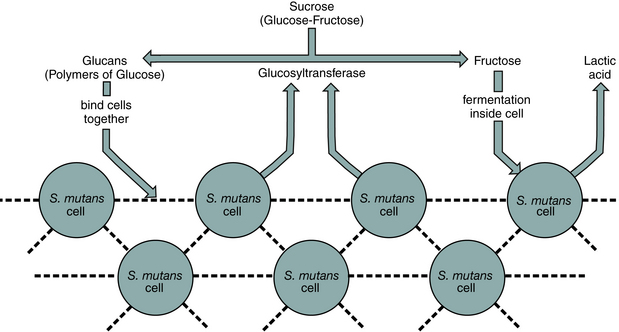
FIGURE 5-3 Plaque formation: Streptococcus mutans. Streptococcus mutans produces enzymes called glucosyltransferases that degrade sucrose into free fructose and polymers of glucose called glucans. The glucans bind to the surfaces of the S. mutans cells, linking them together into a mass in the plaque. The cells take in the fructose and metabolize it through fermentation with production of energy for multiplication and lactic acid as a waste product. Dashed lines indicate glucans.
Lactobacillus species such as L. acidophilus and L. casei are thought to be more important in the progression of a carious lesion after other bacteria (mainly mutans streptococci) have initiated the tooth destruction. Although lactobacilli are highly acidogenic and aciduric, they do not have effective attachment mechanisms to allow them to accumulate in plaque that develops over noncarious teeth. Thus the other bacteria present in plaque (e.g., mutans streptococci) are more important in the initial attack on the tooth. Low numbers of lactobacilli, however, are accidentally “trapped” in plaque as it develops and may be present in saliva. If the plaque bacteria produce acids, causing demineralization of the tooth, the aciduric bacteria such as lactobacilli and mutans streptococci are given an advantage to multiply more rapidly. The nonaciduric bacteria begin to die, leaving more nutrients available for the aciduric bacteria. The best place for lactobacilli to thrive is within the highly acidic carious lesion itself. As the lactobacilli thrive, they and the mutans streptococci produce even more acids, if sugars are present, causing the lesion to progress.
Actinomyces naeslundii is a good plaque former and can accumulate to high numbers in plaque. The bacteria is not as conducive to caries as the mutans streptococci, likely because they are only slightly acidogenic and not aciduric. However, A. naeslundii is important in root caries formation but the mechanisms of its involvement have not been defined clearly.
Substrate
The third factor needed for caries development is a dietary substrate that oral bacteria metabolize through catabolic fermentation to produce acids. Sucrose is the most caries-conducive component of our diet, but other sugars such as fructose, glucose, lactose, and starch also can be fermented by bacteria and can contribute to the disease.
Time
As with any infectious disease, time is needed for the disease to become recognized. This time can be called the incubation time, as described in Chapter 3. Dental checkups are scheduled frequently at 6-month intervals because this approximates the usual incubation time for clinically detectable caries.
MICROBIOLOGY OF PERIODONTAL DISEASES
Like dental caries, periodontal diseases are also infectious diseases caused by members of the normal oral microbiota that have been allowed to accumulate in gingival sulcus plaque (Figure 5-4). As the bacteria multiply, they produce histolytic enzymes, toxic metabolites, exotoxins, endotoxins, and immunosuppressive and antiphagocytic factors (which are described in Chapter 3). The accumulation of these bacteria and their potentially harmful products and antigens then produce periodontal diseases by the following mechanisms:
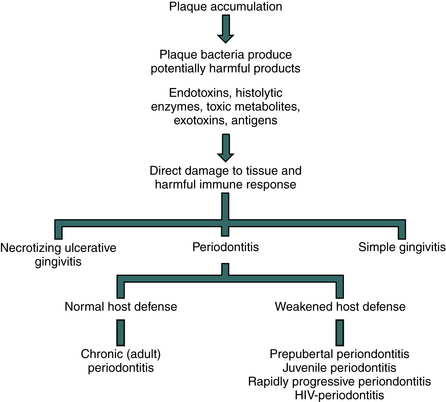
FIGURE 5-4 Development of plaque-associated periodontal diseases. As plaque accumulates in the gingival crevice, the bacteria multiply and produce harmful products that can cause direct damage to the periodontal tissues and that continually stimulate the immune system, resulting in tissue damage. The types of bacteria in the plaque and the nature of the body defense mechanisms combating the infection determine which form of periodontal disease may result.
• Interference with some host defense mechanisms
• Stimulation of the immune response in the periodontal tissues, which can cause damage
Types of Periodontal Diseases
If the disease process affects only the gingival tissue, resulting in an inflammatory response, including swelling, redness, and maybe spontaneous bleeding, the disease is called simple or acute gingivitis. This disease is reversible. When the plaque (and its tissue damaging products) is removed, the gingival tissue returns to normal. Another gingivitis, called necrotizing ulcerative gingivitis or trench mouth, is associated with plaque accumulation and predisposing factors such as stress. This gingivitis also is reversible if the predisposing factors are eliminated and plaque accumulation is controlled.
If the disease process affects the bone in which the teeth are set, the disease is called periodontitis. The disease involves the development of periodontal pockets around the teeth where the gingival tissue has separated from the teeth. These pockets are filled with plaque bacteria and limit access to cleaning. Some of the plaque products directly or indirectly destroy the periodontal tissues and the alveolar bone, which can result in a loosening or loss of the teeth involved. Periodontitis is not reversible. Removal and subsequent control of the plaque, however, can stop further progress of the disease in many instances.
The type of periodontal disease that develops from the accumulation of plaque is influenced by the specific types of bacteria present in the plaque and by how the body responds to the infection. For example, the continuous presence of plaque in persons with normal body defense mechanisms likely leads to chronic periodontitis, a slowly progressing destruction of the bone in which the teeth are set that occurs over a period of years. This is the most common form of periodontitis that usually occurs in persons older than age 35.
In those with some defect in body defenses (usually decreased phagocytosis), the bone destruction that occurs in periodontitis may occur rapidly, within months or weeks, as in rapidly progressive periodontitis (most commonly seen in those younger than age 35), juvenile periodontitis (most common during the early teen years), or prepubertal periodontitis (occurring in those with primary teeth). Immunosuppression resulting from human immunodeficiency virus infection also may predispose individuals to a rapidly progressing periodontitis.
Microorganisms in Periodontal Diseases
Subgingival plaque associated with all forms of periodontal disease contains many bacteria that possess a wide variety of pathogenic properties. Thus, many species can contribute to the disease processes, but some appear to be more important than others and often are called periodontopathogens (Box 5-2). Although caries-conducive bacteria are gram-positive, most of the periodontopathogens are gram-negative; the exceptions include Peptostreptococcus, Streptococcus, and Actinomyces. The latter two genera are associated mostly with gingivitis rather than with periodontitis. Although some research has discovered strong associations of specific species with specific types of periodontitis (e.g., Aggregatibacter actinomycetemcomitans with juvenile periodontitis and Porphyromonas gingivalis with chronic periodontitis), this is not always true in every case of the diseases.
PREVENTION OF PLAQUE-ASSOCIATED DISEASES
Regular brushing and flossing have long been used for preventing plaque-associated diseases. Fluoride and pit and fissure sealants also are effective against caries. Fluoride has three principal topical mechanisms of action: inhibiting bacterial metabolism after diffusing into the bacteria as hydrogen fluoride; inhibiting demineralization when present at the crystal surfaces of teeth during an acid challenge; and enhancing remineralization. Caries and periodontal diseases still occur, however, and other preventive approaches are being used or studied. A current approach involving microbiology is the use of antimicrobial mouth rinses. Other approaches still under investigation include more effective means of delivering antimicrobial agents to sites of infection, development of new antimicrobial agents, replacement of oral pathogens with nonpathogenic strains, and use of vaccines or other chemical agents that may prevent bacterial attachment or disrupt preformed plaque.
ACUTE DENTAL INFECTIONS
As carious lesions progress and approach the tooth pulp, microbial by-products may enter the pulp and cause inflammation called pulpitis. As the disease continues, the bacteria enter the pulp chamber, enhancing the inflammation and destroying the pulp tissue. Further progression may extend the infection through the tooth apex, causing a periapical infection. Depending on the host response and probably the types of bacteria involved, the surrounding facial tissues may become infected, producing a cellulitis. In general, endodontic treatment involves removing necrotic (dead) pulp tissue, killing and removing the remaining bacteria in the root canals, and filling the canals with inert material to prevent further access of bacteria to the periapical tissues. Treatment with antibiotics also may be necessary to slow down bacterial growth involved with periapical infections and cellulitis. Thus the normal oral bacteria present in carious lesions that extend to the pulp tissues become the causative agents of these acute dental infections.
OTHER INFECTIONS
Members of the normal oral flora may be involved in other harmful infections if given the opportunity to invade tissues, as in pulpitis. For example, Actinomyces israelii, a gram-positive anaerobic, rod-shaped bacterium, or other Actinomyces species found in plaque may cause a harmful infection in the jaw and neck area called cervicofacial actinomycosis. This disease is rare, resulting from entrance of these bacteria into oral tissues as a result of tooth extractions or some other trauma. Actinomycosis of the lung is another rare disease that results from aspiration (breathing in) of Actinomyces species into the lung from the mouth.
The slightest trauma in the mouth that results in bleeding (e.g., toothbrushing, biting the cheek, and dental procedures) may permit members of the normal oral microbiota to enter the bloodstream, causing a transient bacteremia. Normally, the phagocytes in the blood rapidly destroy these bacteria before they have a chance to cause problems. If a person has had previous damage to the heart valves, however, such as in rheumatic heart disease, certain oral bacteria in the blood may induce further damage to these valves or cause subacute bacterial endocarditis (inflammation of the inside of the heart). For this reason, some dental patients with previous heart damage must be given antibiotics prophylactically (for prevention) when they receive dental care. When bacteria do enter the bloodstream and cause damage to tissues, the condition is referred to as septicemia rather than bacteremia.
Other harmful infections caused by oral microorganisms are those resulting from a bite or a puncture or cut with a contaminated dental instrument. Several microorganisms are implanted through the skin in these instances, which can lead to a harmful infection that sometimes needs antibiotic treatment. Thus many members of the normal oral microbiota have pathogenic potential if they are allowed to gain entrance to deeper tissues or if they gain entrance to the bodies of others.
Bagg, J., MacFarlane, T.W., Poxton, I.R., Miller, C.H. Essentials of microbiology for dental students. Oxford: Oxford University Press; 1999.
Centers for Disease Control and Prevention. Recommendations for using fluoride to prevent and control dental caries in the United States. MMWR. 2001;50(RR-14):1–42.
Featherstone, J.D.B. The science and practice of caries prevention. J Am Dent Assoc. 2000;131:887–899.
Lamont R.J., Burne R.A., Lantz M.S., LeBlanc D.J., eds. Oral microbiology and immunology. Herndon, PA: ASM Press, 2006.
Review Questions
______1. The most important bacterium in causing dental caries is:
______3. Which of the following dietary components are most important in the cause of dental caries?
______4. Which is true about periodontal diseases?
a. Gingivitis involves the bone in which the teeth are set.
b. The same bacteria that cause dental caries also cause periodontal diseases.
______5. Which is true about the normal oral microbiota?
a. Dental plaque has about 200 billion bacteria per gram.
b. Usually only four different species of bacteria can exist in the human mouth.
c. All the bacteria in the mouth are cocci.
d. The oral microbiota are not involved in causing dental caries or periodontal diseases.
______6. Which of the following bacteria is the most important in causing the progression of a carious lesion after the lesion has been initiated?
______7. Which of the following bacteria is most important in causing periodontal diseases?
______8. Sucrose is converted to what polysaccharide that causes bridging between cells of Streptococcus mutans during plaque formation?
______9. Which of the following periodontal diseases is not related to weakened host defenses?
______10. Inflammation of the tissue in the root canal of a tooth is called: