Development of Infectious Diseases
After completing this chapter, the student should be able to do the following:
 List the steps in the development of an infectious disease.
List the steps in the development of an infectious disease.
 Describe the various stages of an infectious disease and describe how each stage is involved in the spread of the disease to others.
Describe the various stages of an infectious disease and describe how each stage is involved in the spread of the disease to others.
 Differentiate between direct, indirect, droplet, and airborne spread of disease agents.
Differentiate between direct, indirect, droplet, and airborne spread of disease agents.
 List the ways microbes can enter the body and describe how the route of entry may relate to disease development.
List the ways microbes can enter the body and describe how the route of entry may relate to disease development.
 List disease-producing properties of microbes.
List disease-producing properties of microbes.
 List the four mechanisms by which we defend ourselves against pathogenic microbes.
List the four mechanisms by which we defend ourselves against pathogenic microbes.
 Differentiate between antigens and antibodies.
Differentiate between antigens and antibodies.
 Define immunity and describe how it is involved in protecting against infectious diseases and how it can cause damage to the body.
Define immunity and describe how it is involved in protecting against infectious diseases and how it can cause damage to the body.
Diseases in the body have several causes. Some causes are associated with microorganisms, but others result from malfunctioning of an organ (e.g., hyperthyroidism and diabetes), a nutritional deficiency (e.g., rickets and scurvy), an allergic reaction (e.g., hay fever, asthma, and poison ivy), and abnormal growth of cells (e.g., cancer and tumors).
An infectious disease occurs when a microorganism in the body multiplies and causes damage to the tissues. The microorganisms that cause infectious diseases are called pathogens.
Two types of infectious diseases are endogenous and exogenous. These terms refer to the source of the microorganism. Endogenous diseases are caused by microorganisms that are normally present on or in the body without causing harm, but something happens that allows them to express their disease-producing potential. Examples of oral endogenous infectious diseases caused by members of the normal oral flora are dental caries, pulpitis, periodontal diseases, and cervicofacial actinomycosis. The causative agents of these diseases are called opportunistic pathogens. The agents cause diseases only when given a special opportunity to enter deeper tissues of the body or to accumulate to levels that can harm the body.
An exogenous disease is caused by microorganisms that are not normally present on or in the body but contaminate the body from the outside. Most infectious diseases are exogenous diseases (e.g., hepatitis B, “strep throat,” acquired immunodeficiency syndrome, measles, chickenpox, the common cold, and influenza).
Some exogenous microorganisms also can cause disease without entering and multiplying in the body. These are called toxigenic diseases and occur after eating food in which microorganisms have multiplied and produced toxins or poisons (e.g., Staphylococcus food poisoning and botulism).
STEPS IN DISEASE DEVELOPMENT
Box 3-1 lists the steps for development of exogenous infectious diseases. Exogenous infectious diseases develop through six basic steps, each of which may be modified slightly, depending on the specific microorganism involved and the related environmental conditions. The basic steps are described next as related to disease development in a dental office environment. Prevention of disease development occurs by interfering with one of the basic steps as described in Part 2, Infection Control (see Chapters 6 to 17 ).
Source of the Microorganism
The major sources of disease agents in the dental office are the mouths of the patients. Although microorganisms can be present almost anywhere in the office (surfaces, dust, water, air, and the dental team), microorganisms of greatest concern are in the mouths of patients. These microorganisms are described more fully in Chapters 5 and 7 and include those that may be present in saliva, respiratory secretions, and blood that may escape from the mouth during dental care. Members of the dental team also may harbor pathogenic microorganisms, but the chances for the spread of these agents in the office are much lower than for those involving microorganisms in patients. Nevertheless, spread of microorganisms from the dental team to patients is an important concern and is described in Chapter 8.
Although the patient’s mouth is in general the most important source of pathogens in the dental office, accurate detection of which patients may indeed be harboring these pathogens is not possible. Therefore, to successfully prevent the spread of pathogens in the office, the dental team must apply infection control procedures during the care of all patients using the concept of standard precautions. Standard precautions combines the concept of universal precautions (the need to treat blood and other body fluids from all patients as potentially infectious) with body substance isolation (designed to reduce the risk of transmission of pathogens from moist body surfaces) into one set of standards. Thus standard precautions means to consider blood, all body fluids, including secretions and excretions (except sweat), nonintact skin, and mucous membranes as potentially infectious in all patients. The importance of standard precautions is based on an understanding of asymptomatic carriers of disease agents and an analysis of the four stages of the infectious disease process in the body as related to spread of disease agents to others.
ASYMPTOMATIC CARRIER
Persons who have disease agents on or in their bodies but have no recognizable symptoms of the diseases are called asymptomatic carriers. These persons are probably the most important source for spread of disease agents because they may spread pathogens to others and may not even be aware that they are infected. Also, the dental team will not be aware of the potentially infectious nature of patients because carrier patients may look normal, with no recognizable symptoms.
An asymptomatic carrier state may occur at different stages during an infectious disease.
STAGES OF AN INFECTIOUS DISEASE
The four stages of an infectious disease are incubation, prodromal, acute, and convalescent. Pathogens may be spread to others during each of these stages.
INCUBATION STAGE: The incubation stage of an infectious disease is the period from the initial entrance of the infectious agent into the body to the time when the first symptoms of the disease appear. During this time, the disease agent simply is surviving in the body or is multiplying and producing harmful products that ultimately damage the body. This incubation period may range from a few hours to years, depending on the disease-producing potential of the microorganism, the number of microorganisms that enter the body, and the resistance of the body to the microorganism. All infectious diseases have an incubation stage, because we seldom, if ever, are exposed to a sufficient number of microorganisms to cause immediate symptoms. The entering microorganisms must multiply to sufficient numbers that overwhelm local or bodywide defense systems before enough damage occurs to result in a recognizable symptom (e.g., fever, swelling, skin discoloration, ulceration, pain, bleeding, watery eyes, and runny nose). The length of the incubation stage varies. For influenza, incubation is usually 2 to 3 days, whereas for hepatitis B, incubation is usually several weeks. Persons infected with the human immunodeficiency virus serotype 1 (HIV-1) may be free of recognizable symptoms for 10 years or longer after the virus initially enters the body.
PRODROMAL STAGE: The prodromal (“running before”) stage of a disease involves the appearance of early symptoms. The microorganism multiplies to numbers just large enough to cause the first symptoms commonly called malaise (not feeling well). These symptoms may include slight fever, headache, and upset stomach.
ACUTE STAGE: The acute stage is when the symptoms of the disease are maximal and the person is obviously ill. Although this person certainly has a potential to spread disease agents, the person may not be the most important source in the dental office. The acutely ill are not likely to come to the dental office for care except in an emergency. Their presence in the office also may depend on the severity of their symptoms and the nature of the disease.
CONVALESCENT STAGE: The convalescent stage of a disease is the recovery phase. The number of microorganisms may be declining, or the harmful microbial products are being destroyed rapidly as the body defenses successfully combat the disease. Nevertheless, infectious agents are present and may be spread during this stage. Although the patient is aware of the disease, the declining symptoms may not be recognizable by others.
Some persons may never recover fully from an infectious disease. The symptoms may occur over a long period or may occur intermittently. The chronic (long-term) stages may occur in diseases such as hepatitis B and tuberculosis, in which the disease agent may be retained in the body for long periods. As more fully described in Chapter 6, some persons may be infected with the hepatitis B virus and not experience any symptoms until 25 or more years later, with development of severe liver damage. Yet the virus was present in their bodies all of this time and may have been spread to others.
NORMAL PATIENT
A normal patient in this context is one who has no infectious diseases and is not a carrier of obvious pathogens. Normal and asymptomatic patients appear the same with no recognizable symptoms, however. This fact substantiates the need for standard precautions because one cannot always differentiate between normal patients and those capable of spreading harmful microorganisms.
Even normal patients have opportunistic pathogens in their mouths, as more fully described in Chapter 5.
Escape from the Source
Step 2 in the development of an infectious disease is the escape of microorganisms from the source. Microorganisms escape from the mouth during natural mechanisms such as coughing, sneezing, and talking. These modes are indeed how respiratory diseases such as the common cold, measles, chickenpox, and influenza normally are spread. Providing dental care results in several artificial mechanisms by which microorganisms can escape from the patient’s mouth.
Anything that is removed from a patient’s mouth is contaminated (hands, instruments, handpieces, x-ray film, cotton products, needles, teeth, saliva, tissue, appliances, and temporaries). In addition, microorganisms can escape from the mouth in spatter droplets and aerosol particles generated by use of the handpiece, ultrasonic scaler, and air/water syringe. Spatter droplets are the larger droplets that may contain several microorganisms and can hit the skin, eyes, nostrils, lips, and mouth of the dental team. These droplets settle rapidly from the air and can contaminate nearby surfaces. Aerosol particles are mostly invisible but contain a few microorganisms that may be inhaled or remain airborne for some time, depending on their size and on the air currents in the office.
Spread of Microorganisms to Another Person
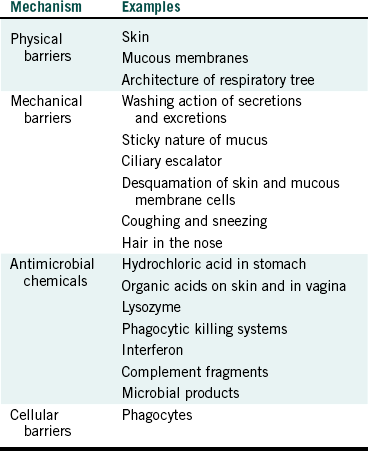
Microorganisms that have escaped from a patient’s mouth may be spread to others by four basic modes of disease transmission: direct contact, indirect contact, droplet infection, and airborne infection (Table 3-1).
TABLE 3-1
| Mode | Example |
| Direct contact | Contact with microorganisms at the source such as in the patient’s mouth |
| Indirect contact | Contact with items contaminated with a patient’s microorganisms such as surfaces, hands, contaminated sharps |
| Droplet infection | Contact with the larger droplets in sprays, splashes, or spatter-containing microorganisms |
| Airborne infection | Contact with the smaller droplet nuclei (aerosol particles) containing microorganisms |
DIRECT CONTACT
Touching soft tissue or teeth in the patient’s mouth results in direct contact with microorganisms with immediate spread from the source. This gives microorganisms an opportunity to penetrate the body through small breaks or cuts in the skin and around the fingernails of ungloved hands. Transference may involve diseases such as herpes infections of the fingers, other skin diseases, and sexually transmitted diseases.
INDIRECT CONTACT
A second mode of spread called indirect contact can result from injuries with contaminated sharps (e.g., needlesticks) and contact with contaminated instruments, equipment, surfaces, and hands. These items and tissues can carry a variety of pathogens such as hepatitis B and C viruses, usually because of the presence of blood, saliva, or other secretions from a previous patient. Skin infection and the common cold also are spread by this mode.
DROPLET INFECTION
A third mode of spread is droplet infection. This mode encompasses large-particle droplet spatter (larger than 5 mm) that is transmitted by close contact. Spatter generated during dental care may contact unprotected broken skin or mucous membranes of the eyes, noses, and mouths of members of the dental team. This contact delivers microorganisms directly to the body. Regular surgical masks, eyeglasses, and face shields interrupt this mode of transmission, which can involve the influenza, mumps, and rubella viruses and herpesviruses.
AIRBORNE INFECTION
A fourth mode of spread is airborne infection that involves small particles (sometimes referred to as droplet nuclei or aerosol particles) of a size smaller than 5 mm. These particles can remain airborne for hours and can be inhaled. Tuberculosis, chickenpox, and measles are spread by this mode, and surgical masks are not designed to protect against airborne spread. A particulate respirator (e.g., N-95 respirator) would be needed to afford such protection.
Entry into a New Person
Microorganisms that are spread to a new person frequently cause no damage unless they actually enter the body. The four basic routes of entry have been mentioned already (Table 3-2).
TABLE 3-2
Routes of Entry of Microorganisms into the Body
| Routes | Examples |
| Inhalation | Breathing aerosol particles generated from use of prophylaxis angle |
| Ingestion | Swallowing droplets of saliva/blood spattered into the mouth |
| Mucous membranes | Droplets of saliva/blood spattered into the eyes, nose, or mouth |
| Breaks in the skin | Directly touching microorganisms or being spattered with saliva/blood onto skin with cuts or abrasions; punctures with contaminated sharps |
Microorganisms at the surface of the skin can enter through small cuts or abrasions that often are unnoticed. Injuries with contaminated sharp items cause direct penetration through the skin into the body. Also, microorganisms in spatter or aerosols may contact and enter the body through mucous membranes of the eye, nose, and mouth, or they may be inhaled. Ingestion is another route of entry.
Infection
Infection is the multiplication and survival of microorganisms on or in the body. An infection does not always indicate disease, but disease seldom results without infection (the exception is toxigenic diseases). Our bodies are infected constantly with large numbers of bacteria multiplying and surviving in our mouths, nose, eyes, intestines, and skin on a normal basis.
Damage to the Body
As mentioned previously, infecting microorganisms usually must multiply to a harmful level for disease to occur. Thus harmful infection is the final step in development of an infectious disease. The final two steps of infection and damage are complex and involve a battle between the infecting microorganism and the defenses of the body, as described in the next section.
HOST-MICROORGANISM INTERACTIONS
Microorganisms present on or in the body multiply if the conditions are appropriate. Bacteria and fungi take in available nutrients, metabolize, multiply, and produce extracellular products that may damage the body. Viruses invade appropriate host cells, replicate, and damage the host cell during the process. The body attempts to restrict microbial invasion and multiplication and to counteract harmful microbial products. The result of these interactions is health or disease.
Pathogenic Properties of Microorganisms
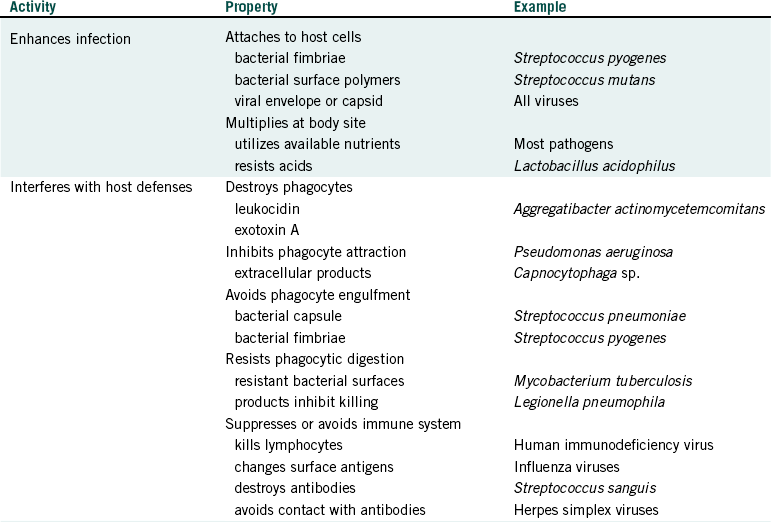
Pathogenic properties of microorganisms are properties that facilitate development of disease and are categorized as those that enhance infection, interfere with host defenses, and cause direct damage to the body (Table 3-3).
ENHANCEMENT OF INFECTION
Properties that enhance the initial survival and multiplication of microorganisms in the body are the surface fimbriae on bacteria and host cell attachment sites on viral envelopes or capsids. These features allow the microorganism to attach to host cells or other surfaces; for viruses, this attachment is required before the viruses can multiply.
Attachment to host surfaces is also necessary for infection by many bacteria, especially if they are to establish themselves on mucosal surfaces such as in the mouth. Bacteria that do not attach to or are not mechanically trapped in oral sites are washed off surfaces by saliva and swallowed. The accumulation of dental plaque is an example of the result of bacterial attachment to host surfaces, in this case leading to dental caries. Other examples of diseases requiring initial attachment by bacteria are streptococcal pharyngitis, genitourinary gonorrhea, gonococcal pharyngitis, conjunctivitis, Salmonella gastroenteritis, and shigellosis.
Bacteria that attach to specific body sites must be able to multiply in the environment of that site to become established and eventually cause damage. Thus, their nutritional requirements must be compatible with the specific host site. For this reason, only specific bacteria can survive at and damage specific sites in the body. For example, lactobacilli and many strains of Streptococcus mutans can survive in an environment high in acid (they are aciduric), such as within a carious lesion. Thus, although many other oral bacteria cannot multiply under these conditions, these aciduric species continue to thrive in the lesion and contribute to the progression of caries.
INTERFERENCE WITH HOST DEFENSES
Many microorganisms are pathogenic because they interfere with host defense mechanisms. Bacteria with capsules, such as Streptococcus pneumoniae, which causes lobar pneumonia, resist phagocytic engulfment, whereas other bacteria, such as Mycobacterium tuberculosis, which causes tuberculosis, may be engulfed but resist phagocytic digestion. Such bacteria gain a foothold during infection because they evade destruction by phagocytes, one of the early lines of defense. The same is true for bacteria such as Aggregatibacter actinomycetemcomitans, an important periodontal pathogen that produces a toxin (leukocidin) that kills certain phagocytes. Other microorganisms interfere with the latter stages of host defense, cell-mediated and antibody-mediated immunity. For example, HIV-1 can destroy certain T lymphocytes that are involved in regulating the immune response. Also, some streptococci can produce protease enzymes that destroy antibody molecules.
DIRECT DAMAGE TO THE BODY
As bacteria or fungi multiply in the body, they produce extracellular enzymes that can degrade macromolecules. If these macromolecules are parts of host cell surfaces or are tissue components, this process can kill cells or damage the tissue. Examples of such histolytic enzymes are the collagenase produced by the bacterial species of Porphyromonas, Bacteroides, and Clostridium; hyaluronidase produced by some streptococci; and a variety of proteolytic enzymes produced by many bacteria.
Bacteria also produce waste products, many of which are cytotoxic, such as ammonia, acids, and hydrogen sulfide, or cause demineralization of enamel and dentin, such as lactic acid and other organic acids. Gram-negative bacteria contain endotoxin that, when released, affects phagocytes and blood platelets and can induce an inflammatory response. Other bacteria may produce exotoxins that interfere with cell or body functions, such as food poisoning toxins and tetanus toxins.
Viruses cause damage by killing or interfering with the normal functions of the host cells they invade, and all types of microorganisms contain or produce substances that stimulate an inflammatory response or an immune response. These host responses are protective, but, if they are stimulated continually by persistence of the microorganism, these responses may produce more damage than protection. One example is the damage that occurs in periodontal disease with the long-term presence of plaque and its antigens in periodontal pockets.
Host Defense Mechanisms
Host defense against harmful infections are grouped into two categories: innate defenses that are always active and acquired defenses that must be stimulated to become active.
INNATE HOST DEFENSES
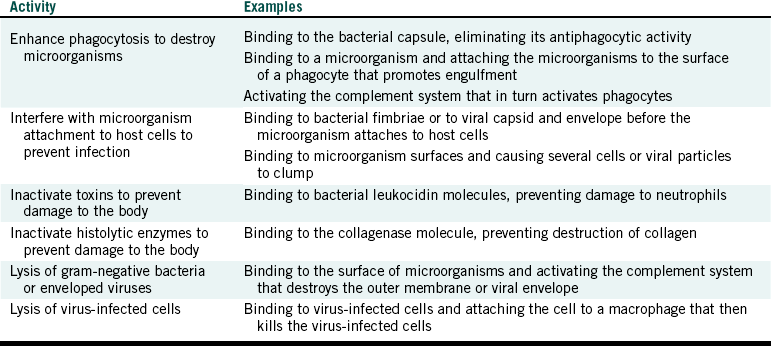
Innate host defenses consist of four groups of properties or activities of the body that guard against infection by contaminating microorganisms (Table 3-4). Although these defenses are formidable, they do not prevent all diseases.
TABLE 3-4
Innate Host Defense Mechanisms
Adapted from Miller CH, Cottone JC: The basic principles of infectious diseases as related to dental practice. Dent Clin North Am 37:1-20, 1993.
PHYSICAL BARRIERS: The unbroken skin serves as an excellent barrier and prevents microorganisms from penetrating to deeper tissues where multiplication and spread to other body sites may occur. The mucous membranes of the eyes, nose, mouth, respiratory tree, vagina, and intestinal tract also provide resistance to penetration by microorganisms. The architecture of the skin with its many layers and the arrangement of cells of mucous membranes serve as the mechanisms that resist penetration.
Another physical barrier is the architecture of the respiratory tree, which prevents particles of 5 µm and greater in size from reaching the alveoli (air sacs) of the lung. This restricts entrance of many microorganisms that may be present in large droplets or dust particles that are inhaled.
MECHANICAL BARRIERS: Mechanical barriers include the cleansing action of secretions such as saliva and tears and excretions such as urine that wash away microorganisms present at these respective body sites. Innate protection of the respiratory tree also includes the secretion of “sticky” mucus that tends to trap inhaled particles that then are moved up and away from the lungs by the ciliary escalator (movement of the hairlike cilia on the surface of mucosal epithelial cells that moves the mucus toward the throat). The natural reflexes of coughing and sneezing also expel particles from the respiratory tree.
Another mechanical barrier involves the desquamation (shedding) of skin cells and mucous membrane cells. As these outer surface cells are lost, microorganisms attached to these cells also are removed from the body.
ANTIMICROBIAL CHEMICALS: A variety of antimicrobial chemicals are present in the body that kill or inhibit the multiplication of microorganisms. Hydrochloric acid in the stomach and organic acids on the skin and in the vagina can prevent bacterial multiplication. The enzyme lysozyme can lyse and kill some bacteria and is present in saliva, tears, nasal secretions, intestinal secretions, colostrum, and inside phagocytes. Other antimicrobial mechanisms of phagocytes involve oxygen products, peroxidase, and lactoferrin. Many of our body cells produce a substance called interferon when the cells are infected with a virus. Interferon is released from infected cells and makes nearby cells resistant to virus replication.
A special group of proteins called the complement system is present in blood and tissue fluids and can participate in antimicrobial activities by working in concert with the immune response (it “complements” the immune system). The complement system may attract phagocytes to a site of infection, enhance phagocytosis of microorganisms, lyse certain gram-negative bacteria, and destroy the envelope of some viruses.
CELLULAR BARRIERS: As previously described, certain white blood cells such as neutrophils and macrophages can destroy microorganisms through the process of phagocytosis. These phagocytes first engulf (swallow up) microorganisms and then kill and digest them using enzymes that degrade the microbial structures. Phagocytes provide an important defense system and are present throughout the body in connective tissue, tissue and lymphatic fluid, lymph nodes, blood, and many organs.
ACQUIRED IMMUNITY
Immunity is a state of being resistant to the harmful effects of specific microorganisms. If a microorganism invades the body, it usually activates a special host defense system directed specifically against that invading microorganism. After this system is activated, it attempts to prevent serious harm from that microorganism and may provide protection against subsequent invasion of the body by that same microorganism. This defense system is called acquired immunity because this system is always ready to respond to microbial infections but does not actually do so until after an infection has occurred. In contrast, the innate body defenses are always active, even before infection has occurred.
ACTIVATION OF THE IMMUNE RESPONSE: The immune response is activated by antigens (sometimes referred to as immunogens). Examples of antigens are bacteria, viruses, fungi, protozoa, extracellular macromolecules produced by these microorganisms, and other macromolecules or cells that are normally not present in the body. During an infection, while the innate body defenses are trying to kill or limit the spread of the invading microorganism, the body recognizes the microorganism and its macromolecular products (antigens) as being foreign to the body. This recognition is accomplished by special macrophages distributed throughout the body that process antigens through phagocytosis and then interact with the cells of the immune system: B lymphocytes and T lymphocytes. This interaction causes these lymphocytes to multiply and yield large numbers of cells that can recognize the specific invading antigens. These lymphocytes then begin a series of activities that can destroy the microorganism or interfere with its pathogenic properties. These activities are grouped into two categories: cell-mediated response and antibody-mediated response.
CELL-MEDIATED RESPONSE: The activated T lymphocytes develop into several different types of T lymphocytes that can (1) regulate the antibody-mediated response, (2) destroy virus-infected host cells in an attempt to stop further multiplication of the virus in the body, (3) produce chemicals called lymphokines that in general activate other types of cells (e.g., phagocytes) to be more active in killing the invading microorganism, and (4) destroy certain nonmicrobial cells in the body that have changed and become recognized as foreign to the body (e.g., cancer cells).
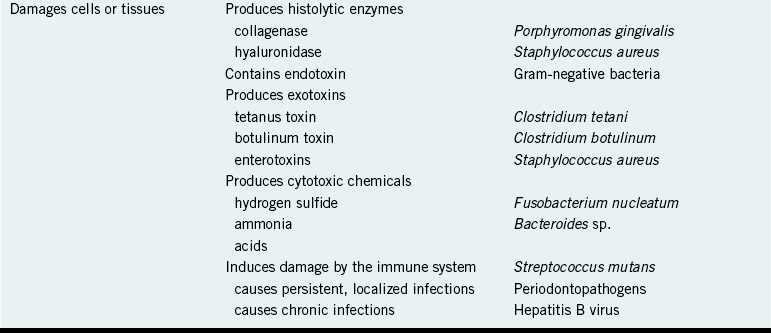
ANTIBODY-MEDIATED RESPONSE: The activated B lymphocytes develop into different types of B lymphocytes that produce lymphokines (that act like those produced from T lymphocytes) and into plasma cells that produce antibodies. Antibodies are protein molecules that can bind to the specific antigens that originally stimulated their formation. When the antibodies bind to these antigens, the antigens (e.g., microorganisms or their harmful products) are destroyed, inactivated, or more easily removed from the body, depending on the nature of the antigen (Table 3-5).
LONG-TERM IMMUNITY
The initial immune response to an invading microorganism usually results in an increased number of lymphocytes that can respond to that microorganism if it attempts to invade the body again. During subsequent invasions, the body “remembers” that microorganism and, because of the large number of specific lymphocytes now present, can respond rapidly to destroy the microorganism before it can damage the body. Thus once we have had an infectious disease, we frequently do not get that same disease again. Notable exceptions include dental caries, periodontal disease, and gonorrhea. Also, in some instances different microorganisms can cause the same disease. For example, more than 100 viruses can cause the common cold, and an immune response to one microorganism seldom protects against another.
ARTIFICIAL IMMUNITY
Artificial immunity involves being immunized or vaccinated against a specific disease. We are inoculated with an antigen (e.g., a dead microorganism, a weakened microorganism, the antigenic part of a microorganism, or an inactivated toxin) that will not cause disease or damage to the body but will stimulate the immune system. On receiving the vaccine, the body is deceived and, reacting as if the infection were real, mounts an immune response for protection. In most instances, this protection lasts for many years (e.g., hepatitis B vaccination), but in some cases booster inoculations are needed periodically to maintain protection (e.g., tetanus vaccinations). Chapter 9 describes diseases for which vaccines are available in the United States, including hepatitis B.
DAMAGE BY THE IMMUNE SYSTEM
Activation of the immune system by certain antigens can cause damage to the body. About 10% of the population is allergic to substances that can serve directly as an antigen or are changed into antigens after they enter the body. The immune response to the antigen (in these cases called an allergen) results in damage to the body, usually occurring at the body site exposed to the allergen. For example, some persons who breathe in pollens have antibody-mediated allergic reactions in the nose and eyes, called hay fever, or in the respiratory tree, called asthma. Allergies to foods (e.g., chocolate) are usually expressed as hives on the skin. Allergy to a substance that is distributed throughout the body (e.g., penicillin inoculation) may result in a widespread reaction affecting the blood system, lungs, and heart and is called systemic anaphylactic shock.
Cell-mediated allergic reactions also occur in some persons with chronic infections such as may occur in hepatitis B, syphilis, and tuberculosis. Oils from the poison ivy plant, nickel from jewelry, and chemicals in latex gloves also may cause cell-mediated allergic reactions, called contact dermatitis.
Skin testing is used to determine which specific allergens are causing problems. In many instances, an allergic person outgrows the allergy, but some persons remain allergic for life and must take special precautions to avoid contact with the allergens.
Abbas, A.K. Cellular and molecular immunology, ed 6. Philadelphia: Elsevier; 2007.
Bagg, J., MacFarlane, T.W., Poxton, I.R., Miller, C.H. Essentials of microbiology for dental students. Oxford: Oxford University Press; 1999.
Miller, C.H., Cottone, J.C. The basic principles of infectious diseases as related to dental practice. Dent Clin North Am. 1993;37:1–20.
Sompayrac, L. How pathogenic viruses work. Boston: Jones and Bartlett; 2002.
Review Questions
______1. The most important source of potentially infectious microbes in the dental office is:
______2. Microbes spreading from a patient’s mouth to your hand and then to another patient’s mouth represents what type of spread from patient to patient?
______3. The best definition of an asymptomatic carrier is a patient who is infected with a microorganism and:
______4. During the development of an infectious disease, what has to happen before the step “spread to a new host”?
______5. Antibodies are best defined as:
a. the active ingredients in antimicrobial handwashing products
b. microbes that can enter the body and stimulate an immune response
c. different types of chemicals such as penicillin that can kill microbes
d. proteins made in the body that bind to and destroy microbes and other antigens
______6. Allergies are best defined as:
a. infectious diseases caused by harmful infections with viruses
b. reactions to harsh chemicals that directly damage tissues
______7. The incubation stage of an infectious disease occurs:
______8. Infection is best defined as the:
______9. The difference between droplet and airborne infections is that:
a. airborne infections are caused by smaller infectious particles
b. droplet infections are caused by smaller infectious particles
c. airborne infections are caused by larger infectious particles
______10. Destruction of collagen in periodontal tissue by collagenase from Porphyromonas gingivalis is an example of what type of bacterial pathogenic property?
______11. Mucous membranes of the mouth represent what type of innate host defense barrier of the human body?
______12. The material in a vaccine that stimulates an immune response is called an:
______13. Which of the following is an infectious disease?