Characteristics of Microorganisms
After completing this chapter, the student should be able to do the following:
 Describe the general structure of bacteria, viruses, and fungi.
Describe the general structure of bacteria, viruses, and fungi.
 Describe what bacteria need for growth and how to control their growth.
Describe what bacteria need for growth and how to control their growth.
 Describe how bacteria are cultured.
Describe how bacteria are cultured.
 Describe how bacteria make acids from sugar.
Describe how bacteria make acids from sugar.
 Describe the life cycle of viruses.
Describe the life cycle of viruses.
 Describe the most important fungus in dentistry.
Describe the most important fungus in dentistry.
Four groups of microorganisms have varying degrees of importance in the field of dentistry and allied dental health. These groups are bacteria, viruses, fungi, and protozoa. Although each group has a different life cycle and each group is composed of many different types, the bacteria share two common characteristics: they are too small to be seen by the naked eye, and many members of each group can live on or in the human body, which may result in development of harmful infections.
BACTERIA
Bacterial Names and Differentiation
Bacteria are named like most other life forms, with a first name (genus) and a last name (species). Each genus is composed of one or more species, and some species may be subdivided further into types and strains. For example, the genus Streptococcus is composed of about 21 different species, and the oral species S. mutans is divided into 8 subtypes (A to H).
Bacteria have different characteristics and activities that allow them to be distinguished from one another. These include cell morphology (size and shape), staining characteristics, colony characteristics (appearance during growth on agar media), metabolic properties, immunologic properties, and DNA and RNA characteristics.
All sizes and shapes are determined by observation under a microscope that magnifies about 1000 times normal size. Because bacteria are difficult to see even under a regular light microscope, procedures for staining the cells with special dyes were developed to aid visualization. A staining procedure developed by Dr. Christian Gram differentiates bacteria into one of two groups. Those bacteria that appear blue or purple are called gram-positive, and those that appear pink or red are called gram-negative. Gram-positive and gram-negative bacteria have other important differences, which will be described later. Other staining procedures also aid in identifying bacteria. For example, the Ziehl-Neelsen or Kinyoun acid-fast stain helps visualize acid-fast bacilli and greatly aids in the identification of Mycobacterium tuberculosis, the causative agent of tuberculosis.
Another way to visualize bacteria is to place (inoculate) them onto the surface of a semisolid growth medium, called agar, contained in a covered dish, called a petri plate (described later). If the agar medium contains all the proper nutrients and is incubated at the proper temperature, each bacterium begins to multiply into a small mass of cells (a colony) that can be seen with the naked eye (Figure 2-1). Each visible colony contains hundreds of thousands of bacterial cells and frequently has an appearance (shape, color, size, consistency) different from that of another species. Thus colony morphology is one aspect used to differentiate bacteria.
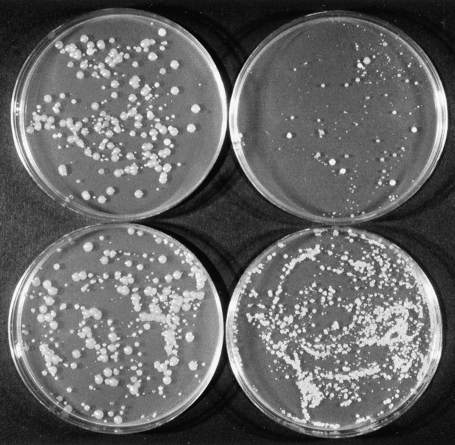
FIGURE 2-1 Colonies of different bacteria on an agar growth medium in petri plates. Colonies of different bacteria vary in size and appearance. Each plate contains a different number of colonies, and each colony contains thousands of cells.
Metabolism refers to the physical and chemical changes that occur during bacterial growth (multiplication or increase in numbers of cells). Different bacteria have different metabolic properties, which distinguish one species from another. Detecting these differences may involve performing many tests; for example, determining the nutrients (e.g., sugars and amino acids) used for growth, the requirements for oxygen or carbon dioxide during growth, the waste materials (e.g., acids) produced during growth, and the enzymes (i.e., catalysts that chemically change a substance such as breaking down proteins into amino acids) made during growth.
Table 2-1 assists in understanding the characteristics of microorganisms by describing various macromolecules and their subunits. Bacteria having different chemical substances on their surfaces or that make different extracellular substances (substances that are released from the cell to the outside environment) cause the synthesis of different antibodies (special proteins in serum) when bacteria are placed into animals. These antibodies are part of the immune defense system of human beings and lower animals and will be explained further in Chapter 3. Antibodies formed against one bacterium usually will bind only to that bacterium and not to others, and this binding can be visualized in the laboratory by a variety of techniques. Thus, exposing an animal to a known bacterium, allowing the animal to make antibodies to that bacterium, mixing the serum of the animal with unknown bacteria in the laboratory, and looking for a visualized positive reaction can help determine the identity of the unknown bacteria.
TABLE 2-1
| Macromolecule | Basic Composition | Examples or Occurrence |
| Protein | Amino acids (e.g., tryptophan, leucine) | Enzymes, viral capsid, cell walls, cytoplasmic membranes, flagella |
| Polysaccharide | Monosaccharides (e.g., glucose, fructose) | Capsules, storage granules, dextran |
| Lipid | Fatty acids, glycerol | Cytoplasmic membranes, viral envelopes |
| Nucleic acid | Adenine, guanine, cytosine, thymine, ribose | DNA, RNA |
| Glycoprotein | Polysaccharide, protein | Fimbriae, viral envelope |
| Lipoprotein | Lipid, protein | Cell wall |
| Lipopolysaccharide | Lipid, polysaccharide | Endotoxin |
All of the properties of bacteria are controlled by specific genes in their DNA. Thus, because different bacteria have different properties, they also have different DNA and RNA. Several techniques can be used to detect differences in these nucleic acids, and these techniques greatly aid in differentiating and identifying bacteria.
Cell Morphology and Structure
Bacteria are single cells with one of three basic shapes. Spherical cells are called cocci (singular coccus); rod-shaped cells are called bacilli (singular bacillus); and curved or spiral cells are called spirilla (singular spirillum). The cocci and bacilli may exist as single cells, or they may exist in small clusters or in chains (Figure 2-2). The average diameter of a coccus is about 1 micrometer (μm). Common bacilli are about 1 μm wide and 5 to 10 μm long.
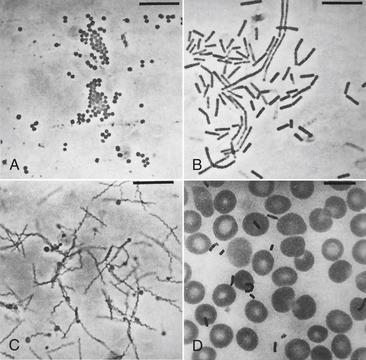
FIGURE 2-2 The common morphologies of prokaryotic cells as revealed by phase-contrast photomicrographs of unstained (A) Staphylococcus aureus (cocci), (B) Bacillus subtilis (rods), and (C) Treponema denticola (spirals) compared with (D) human red blood cells. Bacillus subtilis has been mixed with the red blood cells in D for size comparison. Bar is 10 μm. (From Slots J, Taubman MA: Contemporary oral microbiology and immunology, St Louis, 1992, Mosby.)
Spirilla are 0.2 to 1.0 μm wide and up to 30 μm long. A micrometer is 1 millionth of a meter or 1 thousandth of a millimeter, and a millimeter is the smallest division on a metric ruler. Approximately 25,000 cocci laid side by side would create a line just 1 inch long. In comparison, a human red blood cell is about 7 μm in diameter.
STRUCTURE
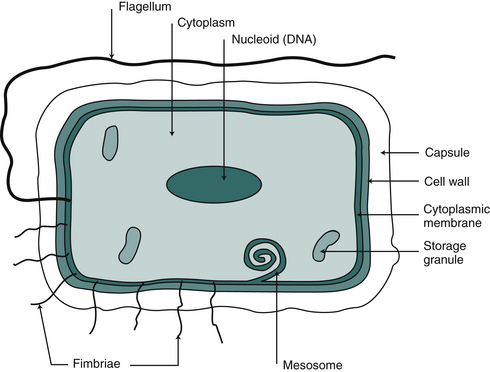
Although bacterial species differ in shape, size, and activity, their structure is similar. Understanding this structure helps explain their role in causing diseases, their resistance to methods of killing, and their activities that are beneficial to the human race. Figure 2-3 shows the structures of a representative bacterial cell; Table 2-2 lists the functions of these structures.
TABLE 2-2
Bacterial Structure and Function
| Structure | Function/Activity |
| Cytoplasmic membrane | Transport of nutrients; energy metabolism; secretion of wastes; DNA synthesis; cell wall synthesis |
| Cell wall | Cell shape; protection from mechanical damage |
| Outer membrane of gram-negative bacteria | Contains endotoxin; transport of nutrients |
| Capsule | Protection from drying; antiphagocytic; attachment to surfaces |
| Flagella | Locomotion |
| Fimbriae (pili) | Attachment to surfaces; transport of DNA between cells |
| Nucleoid | DNA control of cell activities |
| Endospore | Protection against adverse conditions |
CYTOPLASM: The cytoplasm is contained within the cytoplasmic membrane and is a viscous material consisting of water, enzymes and other proteins, carbohydrates, lipids, nucleic acids, essential nutrients, oxygen, and waste products. Embedded in the cytoplasm is the bacterial nucleoid, which consists of a single, long chromosome of DNA that contains most of the genes (approximately 2500) controlling cell activities. The nucleoid usually is diffused throughout the cytoplasm rather than well defined as in mammalian cells. Some bacteria also have extrachromosomal DNA in small units in the cytoplasm called plasmids. Plasmids frequently carry genes that express special activities such as resistance to chemical and physical agents and antibiotics.
The cytoplasm also contains submicroscopic particles called ribosomes that serve as physical sites for the synthesis of proteins from amino acids. Some bacteria may have granules in the cytoplasm that consist of stored substances such as starch, lipids, or iron.
CYTOPLASMIC MEMBRANE: The cytoplasmic membrane surrounds the cytoplasm and is composed of lipids and protein substances. Its structure is similar to that of mammalian cells, and its functions include regulating the entrance and exit of nutrient materials and waste products, maintaining proper pressure within the cell to keep it from bursting, containing the enzymes responsible for synthesizing the outer cell wall, serving as the physical site for attachment and allocation of newly formed chromosomal DNA during cell division, controlling release of certain extracellular enzymes, and serving as the site of many metabolic reactions through which the cell gains energy for growth.
Mesosomes, present mostly in gram-positive bacteria, are inward foldings of the cytoplasmic membrane. Mesosomes house many hydrolytic enzymes that are released into the extracellular environment and break down macromolecules into their subunits, which are taken into the cell as food.
Antimicrobial agents in many disinfectants, handwashing agents, and mouth rinses kill or inhibit the growth of bacteria by acting on the cytoplasmic membrane. Chlorhexidine gluconate, present in handwashing products and mouth rinses, is thought to affect the cell membrane and interfere with energy metabolism and uptake of nutrients by the cells.
CELL WALL: The bacterial cell wall is a rigid structure that gives the cell its characteristic shape (coccus, rod, spirillum) and is not present in mammalian cells. The cell wall is a complex structure in which its basic components (peptidoglycan) form a tight-knit “net” over the entire surface of the cell. Peptidoglycan (peptide, small protein; glycan, polysaccharide) consists of long polysaccharide chains with short side chains of peptides. The peptides of one polysaccharide chain are linked to the peptides of other polysaccharide chains, forming a large continuous macromolecule. Besides giving the cell its characteristic shape, the peptidoglycan also protects the cell from mechanical crushing. Gram-positive bacteria have several layers of peptidoglycan in their cell walls and are much more resistant to external physical forces than gram-negative bacteria, because the latter have only a few layers of peptidoglycan.
The peptidoglycan of the cell wall is the site of action of several antimicrobial agents. Lysozyme is an enzyme present in saliva, tears, nasal secretions, and other body secretions and is present inside white blood cells (e.g., phagocytes, which are described later) that destroy bacteria. This enzyme lyses susceptible bacteria by breaking the bond between the subunits of the polysaccharide chain in peptidoglycan. The antibiotic penicillin and its many derivations act by preventing cross-linking of the peptidoglycan units as the cell wall is being synthesized during cell division. Other antibiotics such as vancomycin and the cephalosporins also prevent cell wall synthesis. The action of all of these antimicrobial agents results in “holes” forming in the peptidoglyan that cause a loss of the cytoplasm into the external environment (lysis) and cell death.
OUTER MEMBRANE: Gram-negative (but not gram-positive) bacteria have an outer membrane just external to the cell wall. This membrane covers the entire cell surface, and its basic structure and composition are like the cytoplasmic membrane. The outer membrane, however, contains an important component called endotoxin that is composed of lipid, polysaccharide, and protein (lipopolysaccharide-protein complex). When endotoxin is released from bacteria present in the body (after cell death and lysis, or in some instances during its synthesis), it can cause damage to nearby body cells and stimulate several reactions in the body, including fever, inflammation, bone destruction, hemorrhage, and vomiting. The action of endotoxin is thought to play a role in many infectious diseases, including periodontal diseases, dysentery, meningitis, typhoid fever, gonorrhea, and cholera.
CAPSULE: Some gram-positive and gram-negative bacteria contain another structure called the capsule, which also is referred to as a slime layer or glycocalyx. The capsule covers the entire outer surface external to the cell wall in some gram-positive bacteria or external to the outer membrane in some gram-negative bacteria. The capsule is produced by the cytoplasmic membrane and secreted through the cell wall and remains associated with the cell surface in the form of a gelatinous covering. Usually the capsule consists of polysaccharide, but in a few instances it may contain proteins. Some species may have large capsules, such as Streptococcus pneumoniae (the cause of lobar pneumonia and middle ear infections); others may have only a thin layer of capsular material, such as S. mutans (a cause of dental caries).
Capsules contain a large amount of water (hydrated) and may help bacteria survive in dry environments. The presence of a capsule also influences how bacteria interact with cells and other surfaces in the human body. Surface polysaccharides in the microcapsule of S. mutans are involved in sucrose-induced plaque formation on tooth surfaces (see Chapter 5). The presence of capsules also reduces the ability of white blood cells to surround, engulf, and destroy the bacterium through a process called phagocytosis (eating cells) and digestion (see Chapter 3). Thus bacteria with capsules tend to escape these early body defense mechanisms against bacterial disease agents. Bacteria without capsules are engulfed and destroyed more easily.
FLAGELLA: Some bacteria have long, threadlike appendages called flagella (singular flagellum). These protein structures are attached to the cytoplasmic membrane extending through the cell wall and, if present, the outer membrane and capsule. They have a whiplike motion and allow the bacterium to move through fluids. The number of flagella per bacterial cell may range from one to many, exhibiting different arrangements over the cell surface.
FIMBRIAE AND PILI: Fimbriae and pili are hairlike protein appendages projecting from the cytoplasmic membrane into the external environment. They are much shorter than flagella and have two major functions. Sex pili, found mainly on gram-negative bacteria, serve as a tube through which DNA can be passed directly from a donor cell to a recipient cell during a process called conjugation. This process permits properties expressed by the DNA genes of one cell to be transferred to and expressed by another cell. Fimbriae, also called pili, serve as mechanisms by which cells can attach to other cells or environmental surfaces. The fimbriae act as a bridge between the cell and other surfaces. Attachment fimbriae provide an important virulence property. Almost all bacteria that cause harmful infections on or through mucous membranes must first attach to the epithelial cells of the mucous membrane, or they will be washed away by secretions of the body. Attachment fimbriae provide the mechanisms of attachment in diseases such as “strep throat,” scarlet fever, gonorrhea, and diphtheria and cause some bacteria to attach to each other during the formation of dental plaque.
ENDOSPORES: Some bacteria have developed a defense mechanism against death caused by adverse environmental conditions. When available nutrients become depleted, cells of Bacillus, Geobacillus, and Clostridium form a large internal structure that contains the DNA and other substances surrounded by several coats of protein. This dense, thick-walled structure is called a spore or endospore and is one of the most resistant forms of life against heat, drying, and chemicals (Figure 2-4). Once formed, the spore can remain dormant for years and then, when exposed to the proper nutrients and other growth requirements, it can germinate into an actively dividing (vegetative) cell. Only one endospore forms within a bacterial cell, and it germinates into only one vegetative bacterial cell. This is in contrast to fungal spores, in which several spores may form a single cell. Bacterial spores are particularly important in the field of infection control because of their high resistance to heat and antimicrobial chemicals. Spores of Geobacillus stearothermophilus and Bacillus atrophaeus are used biologically to monitor the use and functioning of heat or ethylene oxide gas sterilizers (see Chapter 11). Also, spores of B. atrophaeus and Clostridium sporogenes are used to test the antimicrobial effectiveness of liquid sterilants used at room temperature.
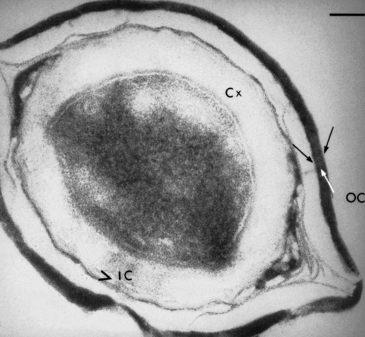
FIGURE 2-4 Thin section of a Bacillus megaterium spore showing two spore coats (IC, inner coat; OC, outer coat). The germ cell wall of the spore coat is seen immediately underlying the thick cortex (Cx). Bar is 100 nm. (From Aaronson AI, Fitz-James P: Structure and morphogenesis of the bacterial spore coat. Bacteriol Rev 40:360-402, 1976.)
Growth and Control
Bacterial growth is defined as an increase in cell numbers; it also is referred to as multiplication. The cells divide by a process called binary fission, in which each cell divides into two daughter cells (Figure 2-5). In the next generation, each of these daughter cells divides into two similar cells, and this continues until the environmental conditions no longer support growth because of a lack of nutrients; a buildup of toxic products; changes in pH, temperature, and availability of oxygen; or the application of physical or chemical agents that kill the bacteria.
Bacteria have a tremendous ability to multiply, and under optimal growth conditions a population of some bacteria such as Escherichia coli can double in number (go from one generation to the next) in just 20 minutes. If such growth continues for just 24 hours, one cell can multiply to a mass of cells that is equal to the size of Earth (more than 3 trillion billion cells). This of course can never happen because nutrients soon become depleted and growth stops. To be more realistic, 10 mL of an overnight broth culture of a bacterium seldom achieves a total population of more than 10 billion cells.
GROWTH REQUIREMENTS
Bacteria are influenced by a variety of physical and chemical conditions of the environments in which they exist. Each bacterial species requires certain conditions for growth, and, if those conditions do not exist at a given site, the bacterium will not be found at that site. Even subtle differences are important. For example, the differences in the physical and the chemical environments between the buccal surface of a tooth and a periodontal pocket just a few millimeters away are sufficient to result in important differences in the types and numbers of bacteria that are found at these two sites (see Chapter 5). The greater the differences among environmental sites, the greater the differences in the types and number of bacteria present. Thus, the bacteria that survive and grow in the human body can be different from those that survive in the oceans. Conversely, some bacterial species can survive and grow in widely different environments. Five major chemical or physical conditions influence growth of bacteria.
TEMPERATURE: Bacteria can be divided into three groups based on the temperature required for optimal growth. Thermophiles grow best at 56° C (132.8° F) with a range of 45° C to 70° C (113° F to 158° F). Such bacteria were found in the hot waters of the “Old Faithful” geyser in Yellowstone National Park. More importantly, the spore-forming thermophilic bacterium G. stearothermophilus was selected many years ago to test the use and functioning of heat sterilizers because of its resistance to heat. Mesophiles grow at temperatures ranging from 22° C to 45° C (71.6° F to 113° F) with optimal growth at body temperature, 37° C (98.6° F). Most of the bacteria that grow and survive in the human body, including those that cause infectious diseases (such as dental caries, periodontal diseases, tuberculosis, bacterial pneumonia, tetanus, and many others), are mesophiles. Psychrophiles grow between temperatures of 1° C and 22° C (33.8° F and 71.6° F), with optimal growth at the typical refrigerator temperature, 7° C (44.6° F). The bacteria present in the oceans, as well as many of those that spoil food stored in a refrigerator, are psychrophiles. Refrigeration has long been used to maintain the freshness of food or extend the storage life of many items that may be contaminated with microorganisms. Refrigeration slows down or prevents the growth of many bacteria and molds, but refrigeration cannot be considered a means of killing microorganisms. If psychrophiles are present, they will continue to grow at normal rates at these low temperatures. If fresh pasteurized milk or high-quality hamburger is purchased at the food market and stored unopened in the refrigerator, it will eventually spoil because microorganisms, some of which may be psychrophiles, will grow using the nutrients in the milk or meat and will produce physical and chemical changes associated with food spoilage.
Thus, if an item or solution becomes contaminated with microorganisms, placing it in the refrigerator or freezer cannot be relied on to kill the microorganisms to make it “safe” for use.
ACIDITY: pH is a measure of acidity, and the pH scale ranges from 0 (high acidity) to 14 (high alkalinity). Values from 0 to 7 are acidic, and values from 7 to 14 are basic or alkaline. The neutral pH of 7 indicates an equal amount of acid and base or no acid or base present. Examples of acidic solutions are stomach acid (pH 1.5) and orange juice (pH 2.9). Examples of basic or alkaline solutions are household ammonia cleaners (pH 11.9) and human blood (about pH 7.4). Pure water has a pH of 7.0.
Most bacteria that survive in the human body grow over a pH range of 5.5 to 8.5, with optimal growth at pH 7.0. Bacteria that produce acids during growth are called acidogenic; those that survive and grow in an acidic environment (usually below pH 5.5) are called aciduric. Acidogenic and aciduric bacteria are important in the initiation and progression of dental caries, as described in Chapter 5.
NUTRIENTS: Bacteria, like mammalian cells, must synthesize all of the macromolecules of protein, polysaccharides, lipids, and nucleic acids (DNA and RNA) needed to grow. These macromolecules are synthesized from the building blocks of amino acids, monosaccharides, fatty acids, and purines/pyrimidines, respectively. Bacteria also must use a variety of smaller molecules such as vitamins and inorganic substances (e.g., sodium, potassium, iron, chlorine, manganese, magnesium, sulfur, phosphorus, calcium, and trace elements). If a bacterium cannot synthesize a given building block such as an amino acid or a vitamin such as niacin, these substances must be available from the environment for the bacterium to survive and grow. Just as we require “eight essential vitamins,” bacteria also require nutrients for growth.
Different bacteria have different nutritional requirements. For example, S. mutans may require six amino acids, five vitamins, all four purines and pyrimidines, and other small molecules plus an energy source, nitrogen, oxygen, inorganic salts, and trace elements from its environment. Conversely, some types of E. coli need only carbon dioxide, a nitrogen source, and trace elements and from this meager “diet” can synthesize all of the macromolecules needed for growth.
Many organic nutrients available for growth may not be in a form that can be used by the bacteria. For example, amino acids are the building blocks for proteins, and many bacteria require certain amino acids to synthesize their own proteins needed for growth. In many instances, proteins rather than the amino acid building blocks are present in the environment, but the entire protein molecules are too large to get into bacterial cells. Thus many bacteria make extracellular proteases, which are enzymes released into the environment that break down proteins into amino acids that can enter the cell. Bacteria also may produce extracellular enzymes that degrade polysaccharides into monosaccharides or lipids into fatty acids, which then can be taken into the cell and be used for growth.
Unfortunately, when these extracellular bacterial enzymes are produced in the human body during a bacterial infection, they may degrade proteins, polysaccharides, or lipids that are important components of body cells, causing damage to these cells. This is one of the mechanisms by which bacteria cause disease.
OXYGEN METABOLISM: Bacteria are divided into four groups based on their requirement for oxygen:
• Obligate aerobes require the presence of oxygen at concentrations of about 20% and cannot grow at low oxygen concentrations.
• Microaerophiles can tolerate only low concentrations of oxygen at no more than 4%.
• Obligate anaerobes cannot tolerate oxygen and grow only in its absence.
• Facultative anaerobes can grow in the presence or absence of oxygen.
Almost all bacteria (regardless of their growth requirement for oxygen) have enzymes that produce toxic substances (e.g., superoxide and hydrogen peroxide) from oxygen that can kill the bacteria. These toxic substances also are produced by white blood cells and help these cells kill bacteria after phagocytosis (see Chapter 3). Some bacteria that produce these toxic substances in the presence of oxygen have mechanisms to remove them to prevent death. One mechanism involves the enzyme superoxide dismutase that converts superoxide to hydrogen peroxide and molecular oxygen. Hydrogen peroxide is converted to water and oxygen by the enzyme catalase.
Obligate aerobes, microaerophiles, and facultative anaerobes, all of which can grow in the presence of oxygen, have superoxide dismutase and catalase to detoxify the oxygen metabolites. Obligate anaerobes do not have these enzymes and therefore cannot tolerate the presence of oxygen. About 99% of the bacteria that live in the mouth are obligate anaerobes or facultative anaerobes.
CULTURING BACTERIA
All of the nutritional and physical growth requirements must be met to culture (grow) bacteria in the laboratory. Culture media in the form of a liquid (broth medium) or in a semisolid (JELL-O–like) form (agar medium) provide the nutrients. Agar is a polysaccharide from seaweed that is liquid at boiling temperatures and turns semisolid when it cools to room temperature. Agar is added to a solution of nutrients, brought to a boil, sterilized, and poured into covered dishes (petri plates) or into tubes to cool and solidify. Samples of bacteria then are placed into sterilized broth media or onto the surface of sterile agar media and incubated under the appropriate atmospheric conditions (anaerobically, without air; aerobically, in air) at the proper temperature.
If bacteria grow in the broth culture, the broth becomes turbid (cloudy). If bacteria grow on the surface of agar media, visible colonies of bacteria appear that may be well separated from each other (see Figure 2-1), or, if a large number of bacteria were originally placed on the agar, a confluent solid mass of growth (lawn) may appear all over the surface.
An agar medium is used primarily to separate bacterial cells physically from each other to obtain a pure culture (growth of only one type of bacterium). Most samples taken from the human body or from nature that are cultured for the presence of bacteria contain many different species. When the sample is spread or streaked (inoculated) over the surface of an agar medium, individual cells or small groups of cells, called colony-forming units (CFUs), are deposited at different sites on the surface. As the agar plate is incubated, each cell or CFU begins to multiply into a pure colony (clone). Thus all of the cells in the colony are derived from the cells or CFUs originally deposited at that site and exist as a pure culture that can be picked off the agar medium and kept separate from all other bacteria. Occasionally, more than one type of bacterial cell can be deposited next to another on the agar surface during inoculation, and both will grow into a mixed, rather than a pure, colony. Such colonies must be picked off and restreaked on a fresh agar plate to separate the types into pure colonies.
Agar plates also provide a means to quantitate the number, or CFUs, of bacterial cells present in a sample. Each single colony that develops on the agar plate after incubation represents 1 CFU present in the original sample.
Most bacteria can survive and grow separately from other cells if the environment is appropriate. Special bacteria can grow only while inside other living cells. Their general structures and mechanisms for growth are the same as those of the free-living bacteria, but they lack some of the metabolic machinery necessary to exist separately. Thus they use the machinery of other cells to grow. Examples of these special bacteria are members of the genera Rickettsia, which can cause diseases such as Rocky Mountain spotted fever, typhus, and ehrlichiosis, and Chlamydia, which can cause sexually transmitted diseases, pneumonia, and trachoma (disease of the eye).
METABOLIC ACTIVITIES
Metabolism is the sum of chemical reactions that occur in the cell. Metabolism involves the uptake of nutrients into the cell, converting them to substances needed by the cells for survival and multiplication and release of waste products (Figure 2-6). Metabolism includes two phases: catabolism, or the breakdown of nutrients to smaller or more easily usable molecules, and anabolism, or the synthesis of new molecules. Catabolism provides the building blocks or carbon skeletons and the energy needed for anabolism. Anabolism provides the macromolecules needed to make cell components, such as cell walls, DNA, cytoplasmic membranes, fimbriae, flagella, cytoplasmic granules, and capsules. Catabolic and anabolic reactions require biologic catalysts called enzymes.
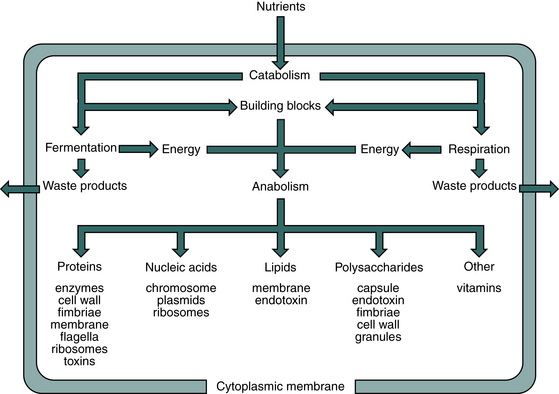
FIGURE 2-6 General bacterial metabolism. Nutrients are taken into the cell and processed through catabolic reactions that generate the building blocks and energy needed to synthesize macromolecules through anabolic reactions. Waste products generated exit the cell.
ENZYMES: Metabolism occurs through the action of enzymes, which are catalysts made of protein. Catalysts speed up chemical reactions and are used over and over because they are not changed during the reaction. Action of some enzymes requires small molecules such as magnesium or calcium, called cofactors; other enzymes require organic molecules such as vitamins, called coenzymes. An enzyme (E) molecule binds to a specific molecule referred to as the substrate (S), and the enzyme binds to the part of the substrate molecules that will be changed. This binding causes the breaking of chemical bonds or the formation of new chemical bonds in the substrate molecule, changing the substrate to a new substance called the product (P). This reaction is written as follows:
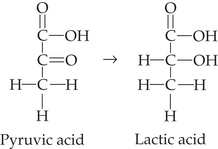
A bacterial cell has about 1000 different enzymes, and the enzyme names all end with the suffix -ase (e.g., protease and hydrolase). Some enzymes break down extracellular substrates into subunits (products) that then can be taken into the cell and used for growth. Other enzyme reactions may change one small molecule into another small molecule. In the example given, pyruvic acid (produced in the cells from the metabolism of sugar) is changed into lactic acid by the enzyme lactate dehydrogenase. Lactic acid produced by streptococci and lactobacilli in dental plaque leaves the cell as a waste product and can cause demineralization of the tooth surface, producing dental caries (see Chapter 5).
CATABOLISM: Bacterial multiplication requires the synthesis of new cell components, and these anabolic reactions require energy. Catabolism provides some of the building blocks for the macromolecules and the energy needed to drive anabolism. All bacteria require nutrients that can serve as sources of energy, and the energy is released from the nutrients as they are processed through catabolic reactions. Two major catabolic pathways that generate energy in bacteria are fermentation and respiration. The pathway used depends on the types of enzymes and metabolic machinery present in the bacterial cell.
ENERGY PRODUCTION: A common energy source for many bacteria is glucose. After glucose is transported into the cells, it is processed through one of two major catabolic pathways known as fermentation or respiration (described later). These reactions are associated with the release of energy from the glucose, but the energy cannot be used to drive anabolic reactions unless it is transferred to special molecules such as adenosine triphosphate (ATP). The ATP then participates in the energy-requiring anabolic reactions such as the synthesis of polysaccharides from monosaccharides and proteins from amino acids.
FERMENTATION: Fermentation is an anaerobic process that usually involves the breakdown of sugars (called glycolysis) with end products of organic acids or alcohols. During fermentation of sugars, hydrogen atoms (also referred to as electrons) are released from the sugar breakdown products. These electrons then bind to organic molecules, changing their structure. In respiration, these electrons bind to oxygen or inorganic substances (as described later). During the fermentation of glucose, pyruvic acid usually accepts the released electrons, changing to lactic acid as a final end product. This is the metabolic pathway that is responsible for dental caries formation, and it is active in caries-conducive oral bacteria such as S. mutans and Lactobacillus spp. The metabolic machinery present in these oral bacteria gives the cells only one metabolic choice, the generation of building blocks and energy for anabolism through the fermentation of sugar mainly to lactic acid. Other bacteria may produce other products from fermentation, depending on the species and the nutrients available.
RESPIRATION: Respiration by infectious bacteria also involves glycolysis of sugars to pyruvic acid as described for fermentation. The electrons released from the sugar breakdown products, however, are transferred to oxygen in aerobic respiration through a series of molecular processes called the electron transport chain. The pyruvic acid, rather than being changed to an end product lactic acid as in fermentation, is processed further through a series of reactions that yield considerably more energy in the form of ATP.
CONTROLLING GROWTH
Controlling the growth of bacteria is accomplished by preventing their multiplication or by killing them. Such control is important to prevent damage that they may cause by growing where they should not (e.g., in our bodies, on food, in drinking water).
PREVENTING GROWTH: Prevention of growth can be achieved by changing or eliminating a physical or nutritional requirement for growth or by using a chemical agent that interferes with cell division. Agents or conditions that prevent bacterial growth without killing them are called bacteriostatic.
Storing items in the refrigerator stops or slows down bacterial growth, unless the bacteria are psychrophiles. Freezing bacteria stops their growth and, because of formation of ice crystals inside the cell, can rupture the cell membrane. Usually, some cells survive, however, and may begin to grow when thawed.
Eliminating the availability of oxygen prevents the growth of aerobes. Adding oxygen prevents growth of anaerobes. Changing the pH beyond optimal values stops growth except for bacteria that can survive extreme pH values, such as aciduric bacteria in the mouth. Treating bacterial diseases with antibiotics can result in inhibiting growth or in killing the cells, depending on the bacterium and the antibiotic used. Antibiotics are chemicals that interfere with some metabolic activity of the bacterium but usually do not affect the metabolic activity of human body cells. This effect is referred to as selective toxicity. For example, penicillins prevent the formation of the cell wall in certain bacteria, which prevents their growth and usually kills the bacterium. Penicillins do not affect the growth of human body cells because our cells do not have cell walls.
KILLING BACTERIA: Killing of bacteria is accomplished by physical or chemical means and is an important aspect of disease prevention and infection control. Agents or conditions that kill microorganisms rather than just prevent their growth are called bactericidal, virucidal, or fungicidal agents or conditions. Probably the surest way to kill bacteria (or any other type of microorganisms) in the shortest amount of time is to expose them to high temperatures such as those achieved in a steam, dry heat, or unsaturated chemical vapor sterilizer (see Chapter 11). The heat may destroy proteins, break down DNA and RNA, or cause structural damage to the cell membrane.
Several chemicals can kill bacteria and other microorganisms, and the type of chemical used frequently is determined by location of the microorganisms to be killed. Strong chemicals cannot be used to kill microorganisms on or in the body, whereas inanimate objects, such as operatory surfaces, can withstand treatment by such agents. Chemicals kill microorganisms by several mechanisms, depending on the properties of the chemical.
VIRUSES
Viruses cause many different diseases in human beings (e.g., measles, mumps, common cold, severe acute respiratory syndrome, hemorrhagic fevers, and encephalitis). Viruses can also infect lower animals, plants, fungi, bacteria, algae, and protozoa. Viruses are important in dentistry because they can cause the following:
• Specific oral diseases (e.g., herpes infections and hand-foot-and-mouth disease)
• Diseases elsewhere in the body that may result in lesions occurring in the mouth (e.g., measles)
• Blood-borne diseases (e.g., hepatitis B and acquired immunodeficiency syndrome)
• Other types of diseases that may be transmitted in the dental office without use of proper infection control procedures
Structure
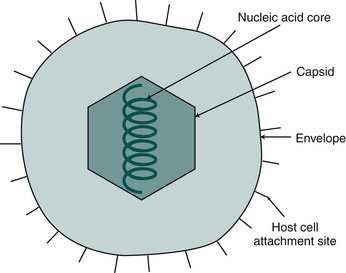
Human viruses are smaller than bacteria, ranging from 0.02 to 0.3 μm. They may have many different shapes, but their general structure consists of a nucleic acid core (DNA or RNA) surrounded by a protein coat called a capsid. Some viruses also have an outer structure of lipids, proteins, and polysaccharides called the envelope (Figure 2-7).
Life Cycle
Unlike most bacteria, viruses are not free-living in that they do not have the metabolic machinery to synthesize new protein coats and nucleic acids. Viruses must use the nutrients and the metabolic machinery of living cells to multiply (replicate themselves). Thus viruses, like the special bacteria Rickettsia and Chlamydia, are called obligate intracellular parasites and multiply only inside of living cells. Table 2-3 summarizes their life cycle.
TABLE 2-3
| Step | Activity |
| Adsorption | Virus particle attaches to host cell surface. |
| Penetration | Virus enters host cell. |
| Uncoating | Capsid is degraded to release nucleic acid. |
| Replication∗ | Host cell machinery is used to synthesize new viral nucleic acid and protein capsid. |
| Assembly | Capsid is assembled around nucleic acid. |
| Release | Viral particle migrates to cytoplasmic membrane for budding, or the host cell lyses to release all internal contents. |
∗Some viruses will incorporate their nucleic acid into the host cell chromosomal DNA, resulting in (1) delay of the viral replication through the lytic cycle or (2) changing of host cell properties through transformation without host cell lysis.
To replicate after entering the body, a virus must first adsorb to a surface of a living cell. This attachment is specific for each type of virus, and the virus attaches to certain host cells through special receptors on the capsid or on the envelope. After adsorption, the virus is taken into the cell, and the capsid is removed to release the nucleic acid and a few molecules of enzymes that help initiate replication. At this point in the life cycle, the nucleic acid of the virus (depending on the virus involved) may induce the lytic cycle, a persistent infection, or cell transformation.
Lytic Cycle
In the lytic cycle the nucleic acid takes over the metabolic machinery of the cell and directs it to produce more virus particles inside the cell. The macromolecules of the host cell are broken down to provide the nutrients needed to synthesize new virus capsids and virus nucleic acids. These elements then are assembled into new virus particles that are released when the host cell lyses. Each infected host cell may produce thousands of new viruses, each of which can infect a new host cell to produce more viruses. Some viruses are released slowly from their host cells by budding through the host cell cytoplasmic membrane, acquiring a portion of the cell membrane as their envelope.
Persistent Infection
A persistent virus infection may be latent, chronic, or slow. A latent persistent infection may occur if the nucleic acid of the virus is incorporated into the DNA of the host cell chromosomes. This incorporated viral nucleic acid is replicated along with the host cell chromosomes during normal cell division and is carried to each newly formed host cell. The viral nucleic acid may be reactivated later to induce a lytic cycle. This type of latent persistent infection is caused by herpesviruses such as herpes simplex, which causes cold sores. A chronic persistent infection such as hepatitis B is caused by lysis of the infected cells, but the symptoms are often unrecognized. Slow persistent infections are those in which the virus replicates slowly, causing recognizable damage only after several years.
Host Cell Transformation
Some viruses infect host cells and cause changes in the properties of cells without causing lysis of the cell. These new properties may result in uncontrolled cell growth such as the formation of certain tumors such as warts caused by the human papillomavirus.
Controlling Virus Replication
Viruses cause diseases by killing or changing the cells of our body. Artificially controlling the growth of viruses inside the body with chemicals is impossible in most cases. Antimicrobial chemicals (including antibiotics) act by inhibiting the metabolic machinery of the microorganisms. Because viruses use the metabolic machinery of the host cell to replicate, such chemicals would cause damage to the host cells. Thus because most virus diseases cannot be treated, the approach is to prevent them from occurring through immunization or infection control procedures.
Viruses can be killed when outside of the body by exposure to heat or chemicals as described for bacteria.
FUNGI
Fungi include mushrooms, molds, and yeasts, with certain members of the latter two types capable of causing diseases in human beings. Such diseases may involve the lungs or other organs or tissues (e.g., histoplasmosis, coccidioidomycosis, blastomycosis, cryptococcosis, and phycomycoses) or the skin (e.g., athlete’s foot, ringworm, and candidiasis) and infections of the nails, scalp, and hair. In dentistry, the most important fungal infection is oral candidiasis (e.g., thrush or denture stomatitis). The infection is caused by the fungus Candida albicans, which may exist as a yeast cell or as a filamentous fungus (mold). This organism also may cause skin infections, vaginal infections, or widespread infection in the body.
Candida albicans occurs as a member of the normal oral microbiota in about 30% of adults. The fungus is an opportunistic pathogen in that it usually causes harmful infections only when given a special opportunity resulting from depressed body defenses, immature body defenses as in the newborn, changes in the physiology of the body, trauma to tissues (e.g., poor-fitting dentures), debilitating systemic diseases, and long-term antibacterial therapy.
Oral infections with C. albicans usually are treated easily with topical antifungal agents, and the yeast cells can be killed outside the body by exposure to heat and certain chemicals as described for bacteria and viruses.
Bagg, J., MacFarlane, T.W., Poxton, I.R., Smith, A.J. Essentials of microbiology for dental students, ed, 2. Oxford: Oxford University Press; 2006.
Lamont, R.J., Burne, R.A., Lantz, M.S., LeBlanc, D.J. Oral microbiology and immunology. Herdon, PA: ASM Press; 2006.
Sompayrac, L. How pathogenic viruses work. Boston: Jones and Bartlett; 2002.
Review Questions
MULTIPLE CHOICE QUESTIONS
______1. Candida albicans is a:
______2. Which of the following microbes do not need to multiply inside of living cells?
______3. Amino acids are linked together to form:
______4. Which type of bacterium is shaped like a sphere?
______6. What bacterial cell structure protects the cell from being crushed?
______7. A special form of bacterium that is dormant and highly resistant to heat and chemicals is a:
______8. Bacteria that make acids are called:
______9. Bacteria that can survive and grow in the presence of acids are called:
______10. Bacteria that die in the presence of oxygen are called:
______11. Structures that allow certain bacteria to attach to surfaces are called:
______12. What bacterial structure inhibits phagocytosis and allows bacteria to escape death caused by white blood cells?
______13. What part of the name Streptococcus mutans is the species name?
______14. Which of the following best describes a psychrophilic bacterium?
a. a chemical substance produced by a microorganism that can inhibit the growth of or destroy some other microorganisms
b. a protein that is produced by the body in response to an antigen and is capable of binding specifically to that antigen
c. a chemical agent used to kill microorganisms on contaminated operatory surfaces