The Abdomen, Pelvis, and Pelvic Limb
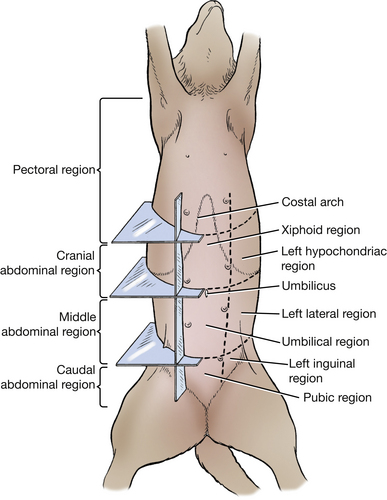
The surface anatomy of the abdomen is divided into cranial, middle, and caudal regions (Fig. 4-1). Reflect the skin from the right abdominal wall, leaving the mammary papillae in the female, the prepuce in the male, and the cutaneus trunci. Extend a perpendicular incision from the ventral midline to the middle of the medial surface of the right thigh and thence to its cranial border. Continue this incision dorsally along the cranial edge of the thigh past the crest of the ilium to the mid-dorsal line. Starting on the medial surface of the thigh, reflect or remove the skin of the right side of the abdomen.
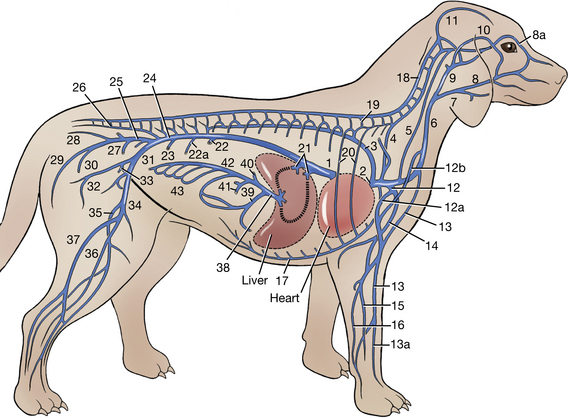
VESSELS AND NERVES OF THE VENTRAL AND LATERAL PARTS OF THE ABDOMINAL WALL
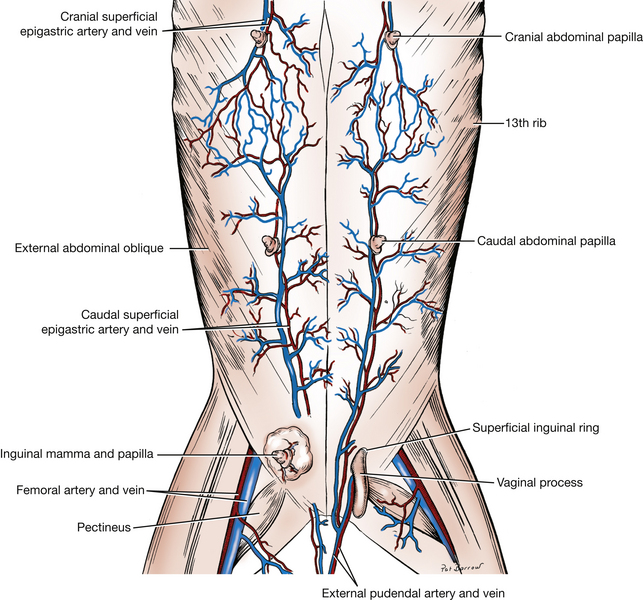
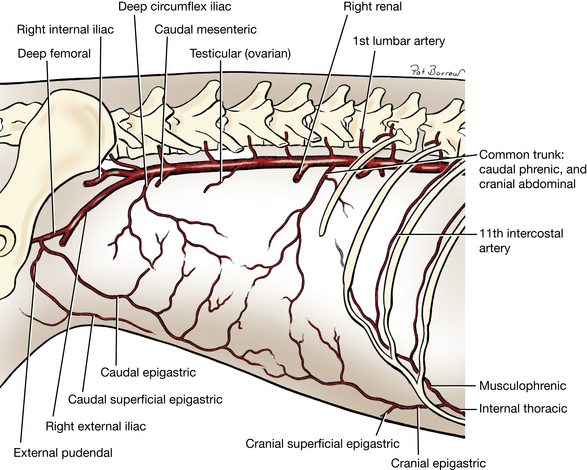
The arteries that supply the superficial part of the ventral abdominal wall are branches of the superficial epigastric arteries (Fig. 4-2). The origin of the cranial superficial epigastric artery is from the cranial epigastric (Fig. 4-33).
The subcutaneous tissue of the ventral abdominal wall contains the abdominal and inguinal mammae and the vessels and nerves that supply them. In the female, the cranial superficial epigastric vessels are seen subcutaneously near the cranial abdominal papilla. By blunt dissection, separate the right row of mammae from the fascia and turn them laterally.
Dissect the external pudendal artery (Figs. 2-79, 4-2, 4-33, 4-40), which emerges from the superficial inguinal ring. Its origin from the pudendoepigastric trunk, a branch from the deep femoral artery, will be seen later. The external pudendal artery courses caudoventrally to the cranial border of the gracilis. The caudal superficial epigastric artery is large and appears as a direct continuation of the external pudendal artery dorsal to the superficial inguinal lymph node. The caudal superficial epigastric artery (Fig. 4-2) runs cranially to the deep surface of the inguinal mamma and supplies the mammary branches. The artery continues, to supply the caudal abdominal mamma and anastomose with branches of the cranial superficial epigastric artery. In the male it supplies the prepuce. A small branch of the external pudendal artery courses caudally to supply the labia in the female and scrotum in the male.
Expose the superficial inguinal lymph nodes (Fig. 4-40), which lie adjacent to the caudal superficial epigastric vessels and cranial to their origin from the external pudendal vessels. The afferent lymphatics of these nodes drain the mammae, the prepuce, the scrotum, and the ventral abdominal wall as far cranially as the umbilicus. Their efferent lymphatics course through the inguinal canal to reach lymph nodes in the sublumbar region.
The abdominal wall receives its vascular supply primarily from four vessels (Fig. 4-33): cranial abdominal artery (craniodorsal), cranial epigastric artery (cranioventral), caudal epigastric artery (caudoventral), and deep circumflex iliac artery (caudodorsal).
Reflect the superficial fascia from the lateral abdominal wall. Emerging from the dorsolateral abdominal wall, caudal to the last rib, are superficial branches of the cranial abdominal artery (Fig. 4-33). The latter arises from a common origin with the caudal phrenic artery off the aorta and perforates the abdominal musculature, which it supplies, to reach the skin.
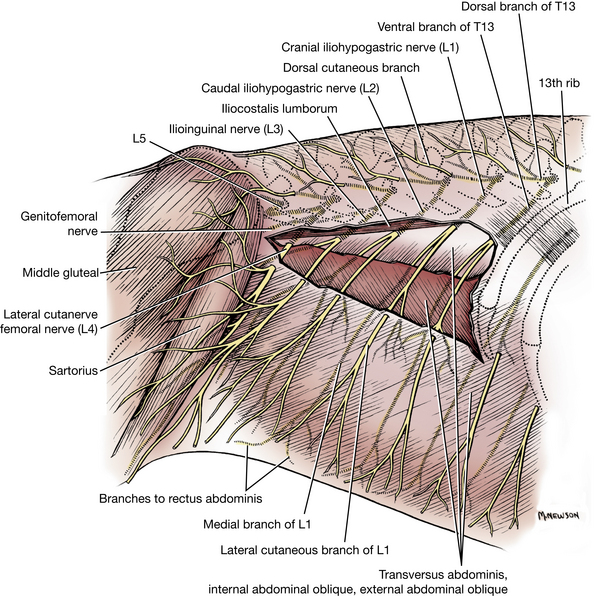
The cutaneous nerves of the abdomen differ somewhat from those of the thorax. The lateral cutaneous branches from the last five thoracic nerves do not follow the convexity of the costal arch but run in a caudoventral direction and supply the ventral and ventrolateral parts of the abdominal wall (Fig. 4-3). The cutaneous branches of the first three lumbar nerves perforate the lateral part of the abdominal wall and, as small nerves, run caudoventrally. They supply the skin of the caudolateral and caudoventral abdominal wall and the thigh in the region of the stifle. Do not dissect these cutaneous nerves. Cranial to the cranioventral iliac spine, the lateral cutaneous femoral nerve (Fig. 4-3) and the deep circumflex iliac artery and vein (Fig. 4-33) perforate the internal abdominal oblique and appear superficially. The nerve arises from the fourth lumbar spinal nerve and is cutaneous to the cranial and lateral surfaces of the thigh. The artery arises from the aorta and supplies the caudodorsal abdominal wall. Dissect these vessels and trace the nerve as far as the present skin reflection will allow.
Transect the lumbar origin of the external abdominal oblique and reflect it ventrally.
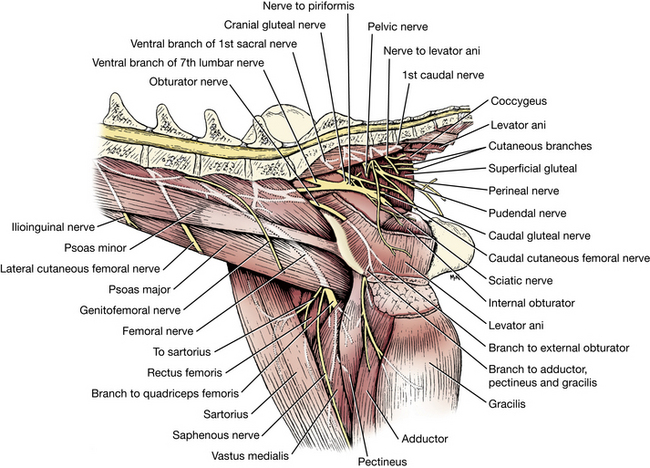
Transect the internal abdominal oblique at the origin of the muscle fibers from the thoracolumbar fascia. Extend the transection caudally to the level of the deep circumflex iliac vessels and lateral cutaneous femoral nerve. Separate the internal abdominal oblique muscle from the underlying transverse muscle and reflect it ventrally to expose the ventral branches of the last few thoracic spinal nerves and the first four lumbar spinal nerves. These are parallel to each other and supply the ventral and lateral parts of the thoracic and abdominal wall. The ventral branches of the first four lumbar nerves form the cranial iliohypogastric, caudal iliohypogastric, ilioinguinal, and lateral cutaneous femoral nerves, respectively. It may be difficult to differentiate between the ventral branches of T13 and L1 without tracing them to the intervertebral foramina, which is not necessary. Usually the ventral branch of T13 courses along the caudal aspect of the thirteenth rib.
The cranial and caudal iliohypogastric and ilioinguinal nerves (Fig. 4-3) pass through the aponeurosis of origin of the transversus abdominis. Each has a medial branch that descends between the transversus abdominis and the internal abdominal oblique to the rectus abdominis. The medial branches supply these muscles and the underlying peritoneum. The lateral branches of these nerves perforate the internal abdominal oblique and descend between the oblique muscles. They may be seen on the deep surface of the external abdominal oblique. Each lateral branch supplies these muscles, perforates the external abdominal oblique, and terminates subcutaneously as the lateral cutaneous branch to the abdominal wall in that region.
Inguinal Structures
Dissect the structures in the male that pass through the inguinal canal and the superficial inguinal ring (Figs. 2-79, 2-80, 4-5 through 4-7). Review structures on pages 84 to 87.
Male
The external pudendal artery and vein leave the superficial inguinal ring caudal and medial to the structures that extend to the testis. Their branches have been dissected.
The genitofemoral nerve (Figs. 4-3, 4-60, 4-65, 4-66, 4-69) arises from the ventral branches of the third and fourth lumbar nerves. It is bound by fascia to the external pudendal vein medial to the spermatic cord. It innervates the cremaster muscle and the skin covering the inguinal region and proximal medial thigh of both sexes and part of the prepuce in the male.
The spermatic fascia, a continuation of abdominal and transversalis fascia, surrounds the structures emerging from the superficial inguinal ring. This includes the vaginal tunic (spermatic cord) and cremaster muscle (Figs. 4-4 through 4-7).
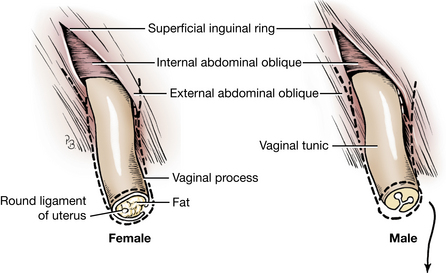
Fig. 4-4 Diagram of transected vaginal process in female and vaginal tunic in male. (Dotted lines indicate spermatic fascia. In the male the contents of the vaginal tunic are not shown. See Fig. 4-5.)
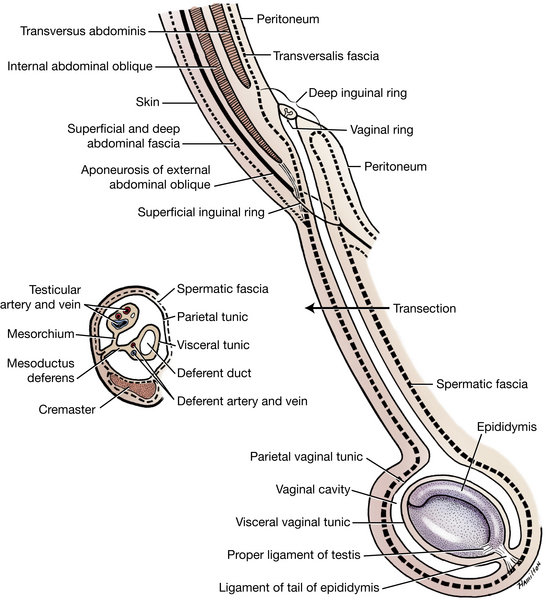
Fig. 4-5 Schema of the vaginal tunic in the male. (The visceral vaginal tunic is actually in contact with the surface of the testis.)
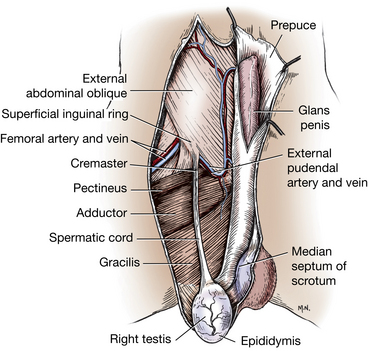
Fig. 4-6 Male genitalia, ventral view. As the vaginal tunic with the spermatic cord leaves the superficial inguinal ring, it is joined by muscle fibers of the internal abdominal oblique, which form the cremaster muscle.
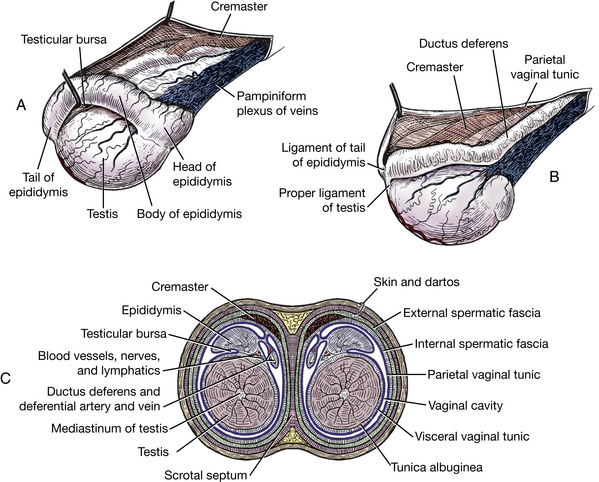
Fig. 4-7 Structures of testes and scrotum. A, Right testis, lateral aspect. B, Left testis, medial aspect. C, Schematic cross section through scrotum and testes.
The cremaster muscle is surrounded by this spermatic fascia as it courses along the caudal part of the vaginal tunic. The cremaster muscle arises from the caudal free border of the internal abdominal oblique and attaches to the vaginal tunic near the testis (Figs. 2-80, 4-40). Reflect the spermatic fascia to expose the vaginal tunic, which can be seen extending from its emergence through the superficial inguinal ring to the testis.
The vaginal process (Figs. 4-4 to 4-7) is a diverticulum of the peritoneum present in both sexes. In the male it envelops the testis and structures of the spermatic cord and is referred to as the vaginal tunic. It consists of the parietal, visceral, and connecting parts.
The parietal vaginal tunic, the outer layer of this diverticulum, extends from the deep inguinal ring to the bottom of the scrotum. Incise this parietal tunic along the most ventral part of the testis and along the cranial border of the vaginal tunic to the superficial inguinal ring to expose the visceral vaginal tunic. The cavity entered is a continuation of the peritoneal cavity.
The visceral vaginal tunic is closely fused to the testis and epididymis and surrounds the ductus deferens. The mesorchium is the connecting mesentery of the testis that contains the vessels and nerves of the testis. The mesoductus deferens is the connecting mesentery that attaches the ductus deferens to the body wall proximally and the mesorchium distally. It contains the artery, vein, and nerve of the ductus deferens (Figs. 4-5 through 4-7).
The spermatic cord (Figs. 2-80, 4-4 through 4-7) is carried through the inguinal canal by the descent of the testis and is composed of two distinct parts: the ductus deferens and the testicular artery and vein.
The ductus deferens carries the spermatozoa from the epididymis to the urethra. It arises from the tail of the epididymis at the caudal end of the testis and is attached to the mesorchium by the mesoductus deferens. The small deferent artery and vein accompany the deferent duct.
The testicular artery and vein, as well as the testicular lymph vessels and the testicular plexus of autonomic nerves, are closely associated with each other. These vessels and nerves are covered by a fold of peritoneum, the mesorchium, that is continuous with the parietal and visceral vaginal tunics. The artery is tortuous, and woven around it are the nerve plexus and the venous plexus. The venous plexus is the pampiniform plexus. The testicular artery and vein are branches of the aorta and caudal vena cava, respectively. They enter the testis at its cranial end. The nerve plexus is autonomic and sensory and contains postganglionic sympathetic axons, which arise from the third to fifth lumbar sympathetic ganglia.
The testis and the associated epididymis and ductus deferens (Figs. 2-80, 4-5 through 4-7) are intimately covered by the visceral vaginal tunic. At the caudal extremity of the epididymis, the visceral peritoneum leaves the tail of the epididymis at an acute angle and becomes the parietal layer. Thus there is a small circumscribed area on the epididymis not covered by peritoneum. The connective tissue that attaches the epididymis to the vaginal tunic and spermatic fascia at this point is the ligament of the tail of the epididymis. Reflect the skin of the scrotum caudally to observe it.
The epididymis (Figs. 2-80, 4-5 through 4-7) lies more on the lateral side of the testis than on its dorsal border. For descriptive purposes it is divided into a cranial extremity, or head, where the epididymis communicates with the testis; a middle part, or body; and a caudal extremity, or tail, which is continuous with the ductus deferens. The tail is attached to the testis by the proper ligament of the testis and to the vaginal tunic and spermatic fascia by the ligament of the tail of the epididymis. The ductus deferens passes cranially over the testis medial to the epididymis.
Lay the previously reflected skin back over the inguinal region and examine the scrotum. The scrotum is a pouch divided by an external raphe and an internal median septum into two cavities, each of which is occupied by a testis, an epididymis, and the distal part of the spermatic cord.
Female
In the female locate the external pudendal blood vessels and the genitofemoral nerve emerging from the superficial inguinal ring. The vaginal process (Figs. 4-2, 4-4) is the peritoneal diverticulum that is accompanied by the round ligament of the uterus. (The origin of this ligament from the mesometrium within the abdomen will be seen later.) These two structures, enclosed in fascia and surrounded by fat, may extend as far as the vulva.
The Inguinal Canal
The inguinal canal (Figs. 2-80, 4-5 through 4-7) is a short fissure filled with connective tissue between the abdominal muscles. It extends between the deep and superficial inguinal rings. It is bounded laterally by the aponeurosis of the external abdominal oblique; cranially by the caudal border of the internal abdominal oblique; caudally by the caudal border of the aponeurosis of the external abdominal oblique (inguinal ligament); and medially, in part, by the superficial surface of the rectus abdominis. The vaginal tunic and spermatic cord in the male and the vaginal process and round ligament of the uterus in the female pass obliquely caudoventrally through the canal. In both sexes the external pudendal vessels and genitofemoral nerve traverse the canal. Notice as many of these boundaries as possible before opening the abdomen.
Abdominal and Peritoneal Cavities
The abdominal cavity is formed by the muscles of the abdominal wall, the ribs, and the diaphragm. It is lined by peritoneum, which encloses the peritoneal cavity.
The peritoneal cavity, like the pleural and pericardial cavities, is a closed space. It is lined by a serous membrane. Serous membranes are thin layers of loose connective tissue covered by a layer of mesothelium. The peritoneum is derived from the somatic and splanchnic mesodermal layers lining the embryonic coelom.
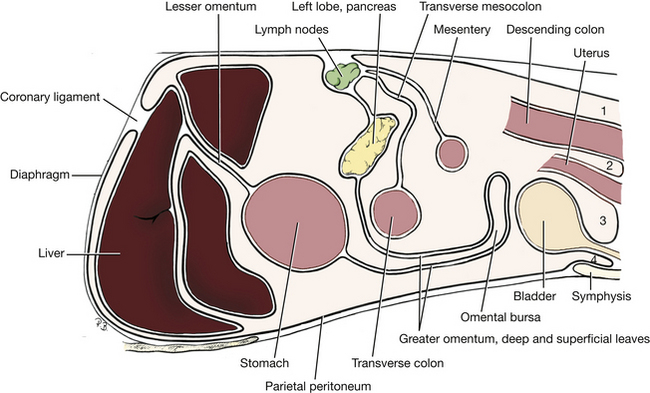
The parietal peritoneum is the layer that lines the body wall and has to be incised to open the peritoneal cavity. The visceral peritoneum surrounds all organs of the abdominal cavity. Therefore there are no organs “within” the peritoneal cavity because they are all covered by visceral peritoneum. (Only an oocyte when it ovulates is within the peritoneal cavity before it enters the uterine tube.) The connecting peritoneum extends between the parietal and visceral peritoneums and forms a mesentery that suspends the organs of the abdominal cavity and contains their blood vessels and nerves (Fig. 4-8).
The transversalis fascia reinforces the parietal peritoneum and attaches it to the abdominal muscles and diaphragm. Make a sagittal incision through the abdominal wall on each side dorsal to the rectus abdominis from the costal arch to the level of the inguinal canal. Connect the cranial ends of these incisions and reflect the ventral abdominal wall. Observe the following structures:
The falciform ligament is a fold of peritoneum that passes from the umbilicus to the diaphragm. It is also attached to the liver between the left medial and quadrate lobes. In obese specimens a large accumulation of fat is found in this remnant of the embryonic ventral mesentery. In young animals the round ligament of the liver may still be visible in the free border of the falciform ligament. Caudal to the umbilicus, the fold of peritoneum is the median ligament of the bladder. In the fetus the umbilical vein courses cranially in the free border of the falciform ligament to enter the liver, whereas the urachus and umbilical arteries are in the free border of the median ligament of the bladder.
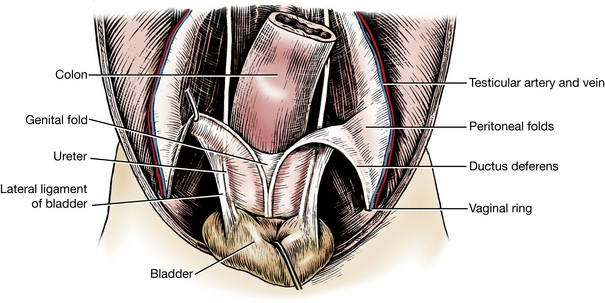
Examine the caudoventral aspect of the inside of the peritoneal cavity at the level of the inguinal canal and observe the vaginal ring.
The vaginal ring (Figs. 4-5, 4-11, 4-43) is the opening formed by the parietal peritoneum as it leaves the abdomen and enters the inguinal canal to form the vaginal process or tunic. It marks the position of the deep inguinal ring, which is formed by the reflection of the transversalis fascia outside the vaginal ring (Fig. 4-60). A deposit of fat is usually present in the transversalis fascia around the vaginal ring.
In the male the ductus deferens is attached to the abdominal and pelvic walls by a fold of peritoneum, the mesoductus deferens. At the vaginal ring, this fold joins the mesorchium, which contains the testicular artery and vein and the testicular nerve plexuses (Figs. 4-11, 4-43). The ductus deferens courses from the vaginal ring dorsally over the edge of the lateral ligament of the bladder and caudally to the urethra just beyond the neck of the bladder. In the female a fold of peritoneum from the mesometrium, which suspends the uterus, passes into the vaginal ring (Fig. 4-12). This contains the round ligament of the uterus, which is the remnant of the caudal part of the fetal gubernaculum. In the male this becomes the ligament of the tail of the epididymis.
The caudal epigastric artery and vein course cranially on the deep face of the caudal part of the rectus abdominis. The origin of the artery from the pudendoepigastric trunk of the deep femoral artery will be dissected later (Fig. 4-33).
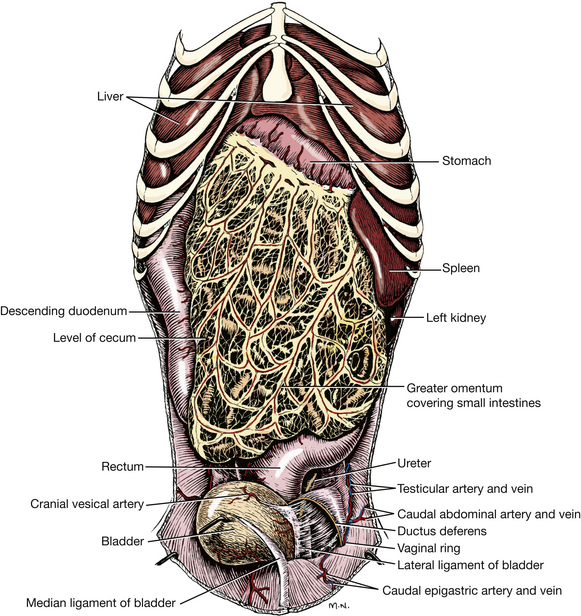
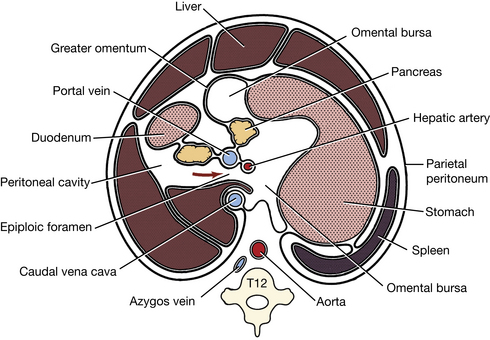
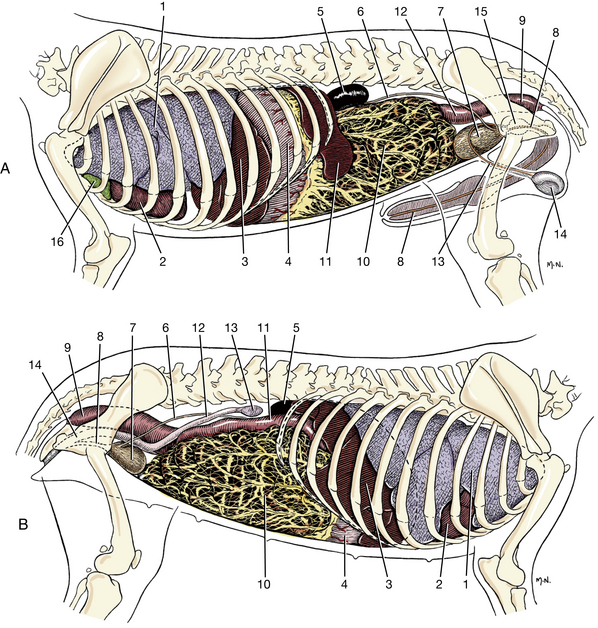
ABDOMINAL VISCERA
The greater omentum (Figs. 4-8 through 4-11) is the first structure seen after reflecting the abdominal wall. It is a caudoventral extension of the two layers of connecting peritoneum that pass from the dorsal body wall to the greater curvature of the stomach, the dorsal mesogastrium. As the stomach forms and rotates to its definitive position in the embryo, this mesogastrium grows extensively and forms a double-layered sac that extends caudoventrally beneath many of the abdominal organs. The space contained within the folded mesogastrium is the omental bursa. The fold adjacent to the ventral body wall is the superficial leaf. The deep leaf is adjacent to the abdominal organs. The greater omentum is lacelike, with depositions of fat along the vessels. The greater omentum covers the jejunum and ileum, leaving the descending colon exposed on the left, the bladder exposed caudally, and the descending duodenum exposed on the right. Reflect the omentum and, using your fingers on opposite sides, separate its superficial and deep walls to expose its cavity, the omental bursa. Follow the greater omentum from its ventral attachment on the greater curvature of the stomach to its dorsal attachment to the dorsal body wall. The spleen is enclosed in the superficial leaf of the greater omentum on the left side, and the left lobe of the pancreas is enclosed in the deep leaf dorsally.
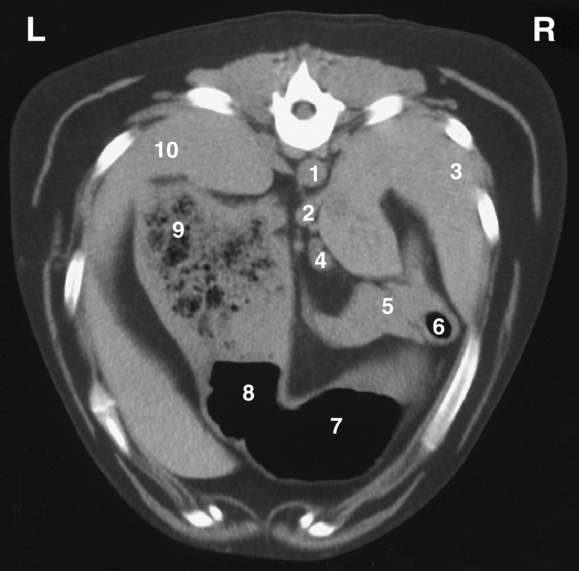
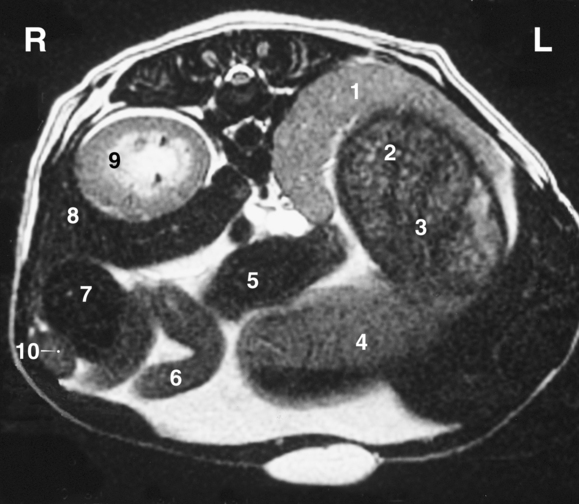
Three organs in the abdomen that are capable of considerable variation in size are the stomach, the urinary bladder, and the uterus. If one or more of these are distended, the relations of the organs will be altered.
The urinary bladder (Figs. 4-9, 4-11), when empty, is contracted and lies on the floor of the pelvic inlet. When distended, it lies on the floor of the abdomen and conforms in shape to the caudal part of the abdominal cavity because it displaces all freely movable viscera. It frequently reaches a transverse plane through the umbilicus.
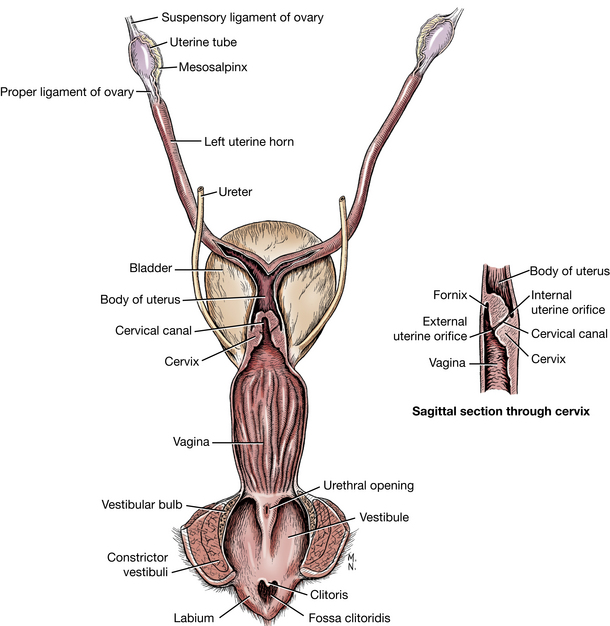
The nonpregnant uterus (Fig. 4-9, B; Fig. 4-12) is remarkably small even in a bitch that has had several litters. The uterus consists of a short cervix and body and two long horns. The gravid uterus lies on the floor of the abdomen during the second month or last half of pregnancy. As the uterus enlarges, the middle parts of the horns gravitate cranially and ventrally and come to lie medial to the costal arches; thus the uterus bends on itself because the ovarian and vaginal ends move very little during enlargement.
The spleen (Figs. 4-9 through 4-11, 4-13, 4-14) lies in the superficial leaf of the greater omentum to the left of the median plane along the greater curvature of the stomach. Its position, shape, and degree of distention are variable. Its lateral surface lies against the parietal peritoneum of the left lateral abdominal wall and the liver. Its caudal part may reach to a transverse plane through the midlumbar region. Its cranial limit is usually marked by a plane passing between the twelfth and thirteenth thoracic vertebrae. It may reach the floor of the abdomen. The part of the greater omentum that attaches the spleen to the stomach is the gastrosplenic ligament. If your specimen was anesthetized with a barbiturate, the spleen may be abnormally enlarged.
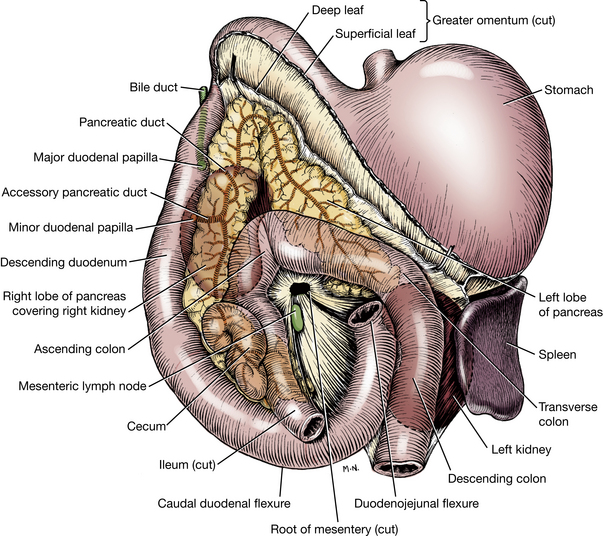
Fig. 4-13 Duodenum and transverse colon in relation to the root of the mesentery. Pancreas in situ and position of kidneys indicated by dotted line.
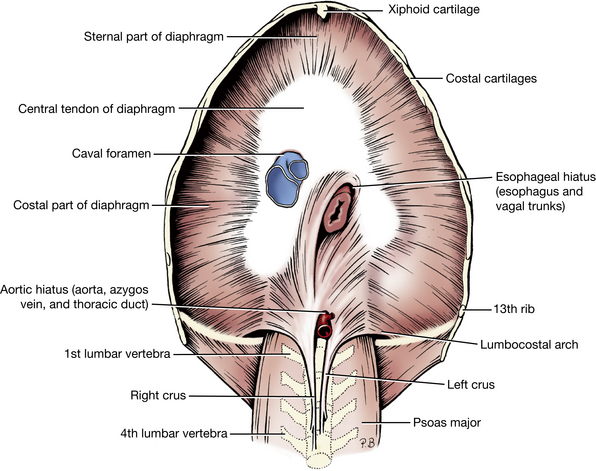
The diaphragm (Fig. 4-15), the muscular partition between the thoracic and the abdominal cavities, is a muscle of inspiration. It has an extensive muscular periphery and a small, V-shaped tendinous center. The muscular part of the diaphragm is divided into three parts according to its attachments: lumbar, costal, and sternal. The lumbar part forms the left and right crura that attach to the bodies of the third and fourth lumbar vertebrae by large tendons. The right crus is larger than the left. The costal part of the diaphragm arises from the medial surfaces of the eighth to thirteenth ribs. It interdigitates with the transversus abdominis muscle. The sternal part is narrow and arises from the dorsal surface of the sternum cranial to the xiphoid cartilage. The cupula is the most cranial extent of the dome-shaped diaphragm that bulges into the thorax. The extensions of the V-shaped tendinous center run dorsally between the lumbar and costal parts of each side. The caudal mediastinum may be severed to expose the tendinous part of the muscle.
The aortic hiatus is a dorsal passageway between the crura for the aorta, the azygos vein, and the thoracic duct. The more centrally located esophageal hiatus is in the muscular part of the right crus and transmits the esophagus, vagal nerve trunks, and esophageal vessels. The caval foramen is located at the junction of the tendinous and muscular parts of the right side of the diaphragm. The caudal vena cava passes through it.
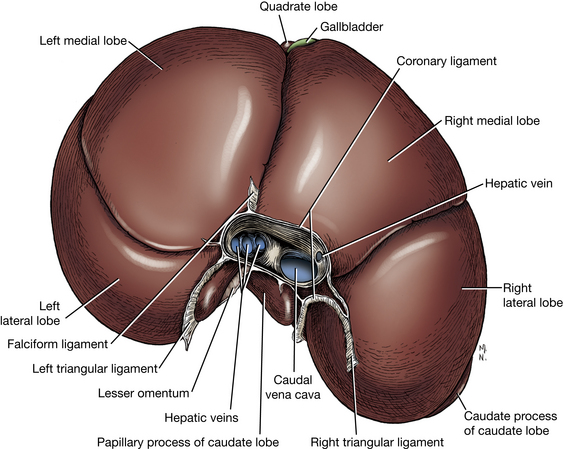
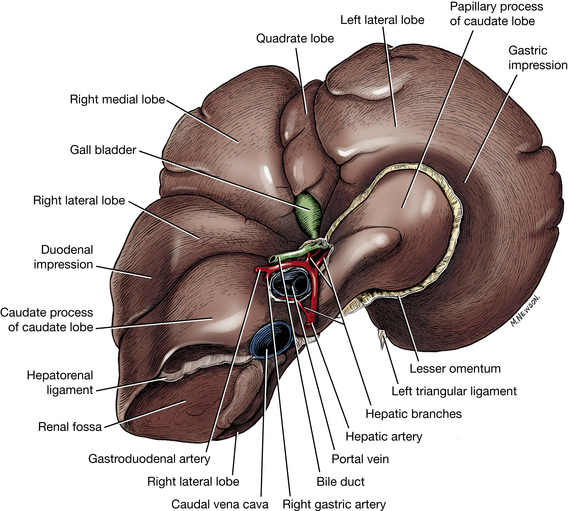
The liver (Figs. 4-8, 4-9, 4-11, 4-16, 4-17) has six lobes, and its parietal surface conforms to the abdominal surface of the diaphragm. The visceral surface of the liver is related on the left to the stomach and sometimes to the spleen; on the right to the pancreas, right kidney, and duodenum; and ventrally to the greater omentum and through this to the small intestine. Its most caudal part covers the cranial extremity of the right kidney and reaches a transverse plane through the thirteenth thoracic vertebra. The liver rarely projects caudal to the costal arch. It undergoes slight longitudinal movement with each respiration.
The right medial lobe of the liver contains a fossa for the gallbladder. The right lateral lobe, which is smaller, is located next to the caudate lobe, which embraces the cranial end of the right kidney. The quadrate lobe is narrow and is located between the right and left medial lobes. It forms the left boundary of the fossa of the gallbladder. The left medial lobe is separated by a fissure from the right medial and quadrate lobes. The umbilical vein enters the liver through this fissure. The left lateral lobe is separated by a fissure from the left medial lobe. The free margin of the left lateral lobe is frequently notched. The visceral surface of the left lateral lobe is concave where it contacts the stomach. The caudate lobe is indistinctly separated from the central mass of the liver, which is cranial to it. It lies transversely, but it is mainly to the right of and dorsal to the main bulk of the organ. It is constricted in its middle where the portal vein enters the liver ventral to it and the caudal vena cava crosses dorsal to it. Its extremities are in the form of two processes. The caudate process caps the cranial end of the right kidney and thus contains the deep renal impression. The papillary process can be seen through the lesser omentum if the liver is tipped forward. It lies in the lesser curvature of the stomach.
Biliary Passages
Much of the biliary duct system within the liver is microscopic. The bile, which is secreted by the liver cells, is collected into the canaliculi, which drain into interlobular ducts. The interlobular ducts of each lobe unite to form hepatic ducts (Fig. 4-18), which emerge from each lobe. The arrangement of the hepatic ducts is variable.
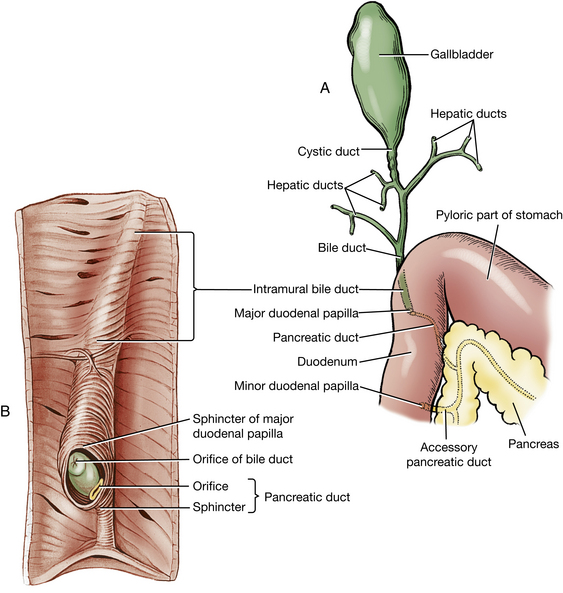
Fig. 4-18 Biliary and pancreatic ducts. A, Topographic relations, ventral view. B, Interior of the duodenum with the tunica mucosa removed to show musculus proprius in relation to the ducts and major duodenal papilla. (After Eichorn E, Boyden E: The choledochoduodenal junction in the dog: a restudy of Oddi’s sphincter, Am J Anat 97:431, 1955. Copyright 1955 Wiley-Liss. Reprinted by permission of Wiley-Liss, Inc., a subsidiary of John Wiley & Sons, Inc.)
The gallbladder (Figs. 4-16 to 4-18) is located in a fossa between the quadrate and right medial lobes of the liver. A full gallbladder extends through the liver and contacts the diaphragm (which is often stained green in preserved specimens). The neck of the gallbladder is continued as the cystic duct.
The main duct formed by the union of the hepatic ducts and the cystic duct from the gallbladder is the bile duct (ductus choledochus). It courses through the wall of the descending duodenum and terminates on the major duodenal papilla alongside the pancreatic duct. There are no valves in the biliary ducts, and bile may flow in either direction. Observe the duct system in your specimen.
The stomach (Figs. 4-8, 4-9, 4-11, 4-13, 4-14, 4-19, 4-20) is divided into parts that blend imperceptibly with one another. The cardiac part is the smallest part of the stomach and is situated nearest the esophagus. The fundus is dome shaped and lies to the left of and dorsal to the cardia. The body of the stomach is the large middle portion. It extends from the fundus on the left to the pyloric part on the right. The body joins the pyloric part at the angular incisure, which is the relatively sharp bend on the lesser curvature. The pyloric part is the distal third of the stomach as measured along the lesser curvature. The initial thin-walled portion is the pyloric antrum, which narrows to a pyloric canal before joining the duodenum at the sphincter, the pylorus.
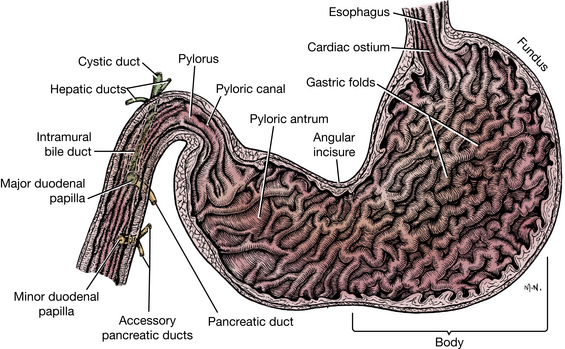
Fig. 4-19 Longitudinal section of stomach and proximal duodenum. Dog in dorsal recumbency: caudal to cranial view.
The stomach is bent so that its greater curvature faces mainly to the left and its lesser curvature faces mainly to the right; its parietal surface faces cranioventrally toward the liver, and its visceral surface caudodorsally faces the intestinal mass. Its position changes depending on its fullness.
The empty stomach is completely hidden from palpation and observation by the liver and diaphragm cranioventrally and the intestinal mass caudally. It lies to the left of the median plane. The empty stomach is cranial to the costal arch and sharply curved, so that it is more V-shaped than C-shaped. The greater curvature faces ventrally, caudally, and to the left. This curvature lies above and to the left of the mass of the small intestine. The lesser curvature is strongly curved around the papillary process of the liver and faces craniodorsally and to the right. The left lobe of the pancreas and transverse colon are dorsocaudal to it.
The full stomach lies in contact with the ventral abdominal wall and protrudes beyond the costal arches. It displaces the intestinal mass. Open the stomach along its parietal surface, remove the contents, and observe the longitudinal folds of mucosa, the rugae.
The duodenum (Figs. 4-9 through 4-11, 4-13, 4-14, 4-19, 4-20) is the most fixed part of the small intestine. It is suspended by the mesoduodenum, which will be studied later. Reflect the greater omentum cranially and the jejunum to either side to expose the duodenum. The duodenum begins at the pylorus to the right of the median plane. After a short dorsocranial course, it turns as the cranial duodenal flexure. It continues caudally on the right as the descending part, where it is in contact with the parietal peritoneum. Farther caudally the duodenum turns, forming the caudal duodenal flexure, and continues cranially as the ascending part. The ascending part lies to the left of the root of the mesentery, where it forms the duodenojejunal flexure.
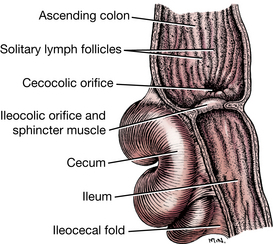
The jejunum forms the coils of the small intestine (Figs. 4-9 through 4-11), which occupy the ventrocaudal part of the abdominal cavity. They receive their nutrition from the cranial mesenteric artery, which is in the root of the mesentery. The root of the mesentery attaches the jejunum and ileum to the dorsal body wall. The mesenteric lymph nodes lie along the vessels in the mesentery. The jejunum begins at the left of the root of the mesentery and is the longest portion of the small intestine. Trace it from the duodenojejunal flexure on the left to its termination at the ileum on the right side of the abdomen. The ileum is the terminal portion of the small intestine (Figs. 4-13, 4-21, 4-29, 4-31). It is short and passes cranially on the right side of the root of the mesentery and joins the ascending colon at the ileocolic orifice. This narrow orifice is surrounded by a sphincter. There is no clear demarcation between jejunum and ileum. Note the vessel that courses on the antimesenteric side of the ileum from the cecum toward the jejunum. This approximates the length of the ileum (10 cm).
The cecum (Figs. 4-13, 4-21, 4-29, 4-31), a part of the large intestine, is an S-shaped, blind tube located to the right of the median plane at the junction of the ileum and colon. It is ventral to the caudal extremity of the right kidney, dorsal to the small intestine, and medial to the descending part of the duodenum. The cecum communicates with the ascending colon at the cecocolic orifice. Open the cecum, terminal ileum, and adjacent ascending colon and observe the ileocolic and cecocolic orifices.
The colon (Figs. 4-9, 4-10, 4-13, 4-20, 4-21, 4-29, 4-31) is located dorsally in the abdomen, suspended by a mesocolon. It is divided into a short ascending colon, which lies on the right of the root of the mesentery; a transverse colon, which lies cranial to the root of the mesentery; and a long descending colon, which lies at its beginning on the left of the root of the mesentery. The bend between the ascending and transverse colons is known as the right colic flexure, and that between the transverse and descending colons is known as the left colic flexure. The descending colon terminates at a transverse plane through the pelvic inlet. It is continued by the rectum.
The pancreas (Figs. 4-13, 4-14, 4-18, 4-29) is lobulated and is composed of a body and two lobes. The body lies at the pylorus. The right lobe lies dorsomedial to the descending part of the duodenum enclosed by the mesoduodenum. It is ventral to the right kidney. Pull the descending duodenum ventrally and to the left to expose this right lobe of the pancreas in the mesoduodenum. The left lobe of the pancreas lies between the peritoneal layers that form the deep leaf of the greater omentum. It is caudal to the stomach and liver and cranial to the transverse colon. Reflect the greater omentum cranially and the small intestine and transverse colon caudally to observe the pancreas.
The pancreatic duct system (Figs. 4-13, 4-18, 4-19) is variable. Most dogs have two ducts; these open separately in the duodenum but communicate in the gland. The pancreatic duct is the smaller of the two ducts and is sometimes absent. It opens close to the bile duct on the major duodenal papilla. Make an incision through the free border of the descending part of the duodenum. Scrape away the mucosa with the scalpel handle and identify the major duodenal papilla. This is on the side where the mesoduodenum attaches. The larger accessory pancreatic duct opens into the duodenum on the minor duodenal papilla 2 or 3 cm caudal to the major papilla. Locate the accessory duct by blunt dissection in the mesoduodenum between the right lobe of the pancreas and the descending duodenum.
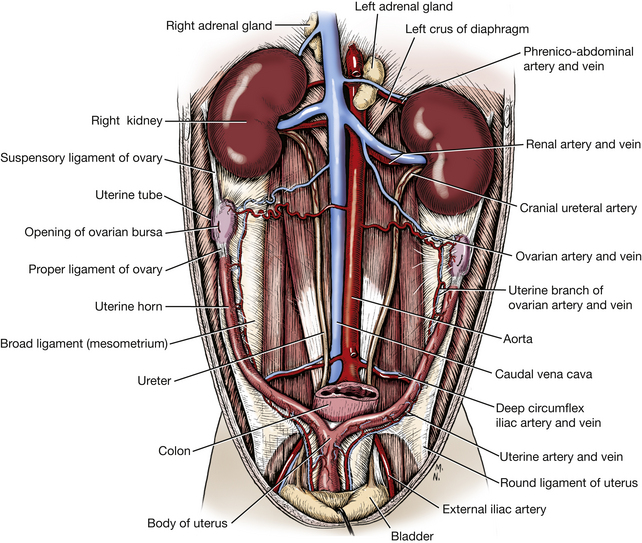
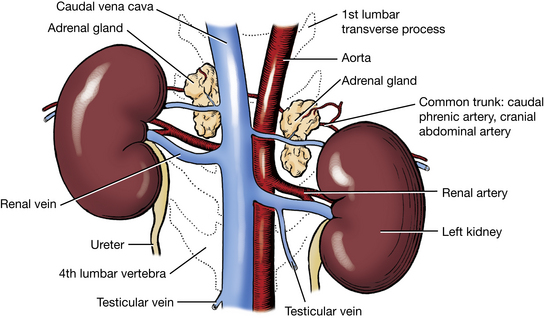
The adrenal glands (Figs. 4-12, 4-22, 4-27) are light colored and are located at the cranial aspect of each kidney. Each gland is crossed ventrally by the common trunk of the caudal phrenic and cranial abdominal veins, which leaves a deep groove on its ventral surface.
The right adrenal gland lies between the caudal vena cava and the caudate lobe of the liver ventrally and the sublumbar muscles dorsally. Expose the gland by dissection between the caudal vena cava and the kidney cranial to the renal vein. The left adrenal gland lies between the aorta and the left kidney. Transect each adrenal and note the lighter-colored cortex and darker medulla.
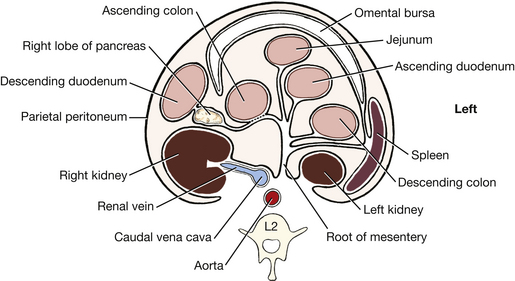
The kidneys (Figs. 4-9 through 4-12, 4-20, 4-22, 4-23) are dark brown. They are partly surrounded by fat and are covered only on their ventral surface by peritoneum. For this reason they are considered to be retroperitoneal organs. The lateral border is strongly convex, and the medial, nearly straight. At the middle of the medial border is an indention, the hilus of the kidney, where the renal vessels and nerves and the ureter communicate with the organ.
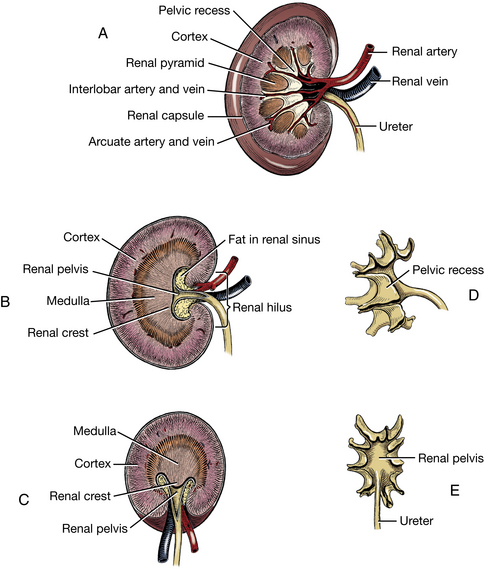
Fig. 4-23 Details of kidney structure. A, Sectioned in dorsal plane, off center. B, Sectioned in mid-dorsal plane. C, Transverse section. D, Cast of renal pelvis, dorsal view. E, Cast of renal pelvis, medial view.
The right kidney lies opposite the first three lumbar vertebrae. It is farther cranial than the left kidney by the length of half a kidney. The right kidney is more extensively related to the liver than to any other organ. Its cranial third is covered by the caudate process of the caudate lobe of the liver. The remaining ventral surface is related to the descending duodenum, the right lobe of the pancreas, the cecum, and the ascending colon. The caudal vena cava is on the medial border of the right kidney.
The left kidney lies opposite the second, third, and fourth lumbar vertebrae. It is related ventrally to the descending colon and the small intestine. The spleen is related to the cranial extremity of the kidney. The medial border is close to the aorta.
The expanded part of the ureter within the kidney is the renal pelvis. The ureter courses caudally in the sublumbar region. It opens into the dorsal part of the neck of the urinary bladder. Throughout this course it is enveloped by a fold of peritoneum from the dorsal body wall. Follow the course of the ureter. The renal sinus is the fat-filled space that contains the renal vessels and surrounds the renal pelvis.
Free the left kidney from its covering peritoneum and fascia. Do not cut its vascular attachment. Make a dorsal plane longitudinal section of the left kidney from its lateral border to the hilus, dividing it into dorsal and ventral halves. Note the granular appearance of the peripheral portion of the renal parenchyma. This is the renal cortex, which contains primarily the renal corpuscles and convoluted portions of the tubules. The more centrally positioned parenchyma is the medulla. It has a striated appearance owing to numerous collecting ducts. The vessels that are apparent at the corticomedullary junction are the arcuate branches of the renal vessels. The longitudinal ridge projecting into the renal pelvis is the renal crest, through which collecting tubules of the kidney excrete urine into the renal pelvis. Make a second longitudinal section parallel to the first and note the renal pyramids formed by the medulla. The pelvic recesses of the renal pelvis project outward between the renal pyramids.
Free the right kidney from its peritoneum and fascia and make a transverse section through it. Note the renal cortex, medulla, crest, and pelvis.
The ovaries (Figs. 4-9, 4-12, 4-24, 4-25) are located near the caudal pole of the kidneys. The right ovary lies cranial to the left ovary and is dorsal to the descending duodenum. The left ovary is between the descending colon and the abdominal wall. Each ovary is enclosed in a thin-walled peritoneal sac, the ovarian bursa (Fig. 4-25), formed by the mesovarium and mesosalpinx. The ovarian bursa is open to the peritoneal cavity by means of a slitlike orifice on the medial surface.
The uterine tube oviduct courses cranially and then caudally through the lateral wall of the bursa on its way to the uterine horn. Examine the surface of the bursa and observe the small cordlike thickening within its wall. This is the uterine tube. Open the bursa by a lateral incision dorsal to the uterine tube and examine the ovary and the infundibulum. The infundibulum is the dilated ovarian end of the uterine tube. It has a fimbriated margin and functions to engulf the oocyte after ovulation. Note that several of the fimbriae protrude into the peritoneal cavity from the opening of the ovarian bursa. In life, these fimbriae function to close the opening into the peritoneal cavity at the time of ovulation and thus prevent transperitoneal migration of oocytes. The entrance of the infundibulum into the uterine tube is spoken of as the abdominal ostium, and it is in this region that fertilization takes place. The uterine tube is short and slender. It opens into the much wider uterine horn at the tubouterine junction. This region is of physiological importance because it is here that sperm and ova are regulated in their transit.
The broad ligaments of the uterus (Figs. 4-12, 4-25) are the peritoneal folds on each side that attach to the lateral sublumbar region. They suspend all the internal genitalia except the caudal part of the vagina, which is not covered by peritoneum. Each ligament is divided into three parts: The mesometrium arises from the lateral wall of the pelvis and the lateral part of the sublumbar region and attaches to the lateral part of the cranial end of the vagina, uterine cervix, and uterine body, and the corresponding uterine horn. The mesovarium, a continuation of the mesometrium, is the cranial part of the broad ligament. It begins at a transverse plane through the cranial end of the uterine horn and attaches the ovary and the ligaments associated with the ovary to the lateral part of the sublumbar region. The mesosalpinx is the peritoneum that attaches the uterine tube to the mesovarium and forms with the mesovarium the wall of the ovarian bursa.
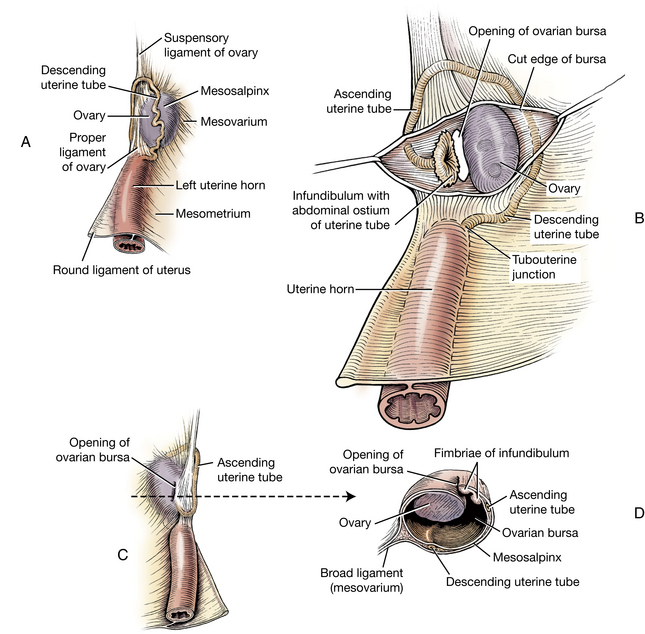
Fig. 4-25 Relations of left ovary and ovarian bursa. A, Lateral aspect. B, Lateral aspect, bursa opened. C, Medial aspect. D, Section through ovary and bursa.
The suspensory ligament of the ovary joins the transversalis fascia medial to the dorsal end of the last rib (Figs. 4-12, 4-24). It functions to hold the ovary in a relatively fixed position. In ovariohysterectomy this ligament is freed from its attachment to the body wall to facilitate removal of the ovary. The proper ligament of the ovary is short and attaches the ovary to the cranial end of the uterine horn. From this point caudolaterally to the inguinal canal, there is a fold from the lateral layer of the mesometrium that contains the round ligament of the uterus in its free border (Figs. 4-12, 4-25). The round ligament, a homologue of the embryonic gubernaculum, has no function in the adult. It passes through the inguinal canal and is wrapped by the vaginal process and adipose tissue.
Peritoneum
The peritoneum is a mesothelial layer that can be divided into three regional components. The parietal peritoneum covers the inner wall of the abdominal, pelvic, and scrotal cavities. The visceral peritoneum covers the organs suspended in these cavities. The connecting peritoneum is a double sheet of peritoneum that connects between the parietal and visceral layers or between the visceral layers of adjacent organs forming peritoneal folds referred to as mesenteries, omenta, or ligaments.
In the embryo the dorsal common mesentery is a double layer of peritoneum that passes from the dorsal abdominal wall to the digestive tube. It serves as a route by which the nerves and vessels reach the organs. In the dog the dorsal common mesentery persists as the greater omentum, mesoduodenum, mesentery, and mesocolon.
An omentum (epiploon) is the connecting peritoneum that attaches the stomach to the body wall or other organs. It is an extended mesogastrium.
The greater omentum (Figs. 4-8 through 4-11, 4-13, 4-26), an extended fold of dorsal mesogastrium, attaches the greater curvature of the stomach to the dorsal body wall. From the greater curvature of the stomach, it extends caudally as the superficial leaf over the floor of the abdomen. It turns dorsally on itself near the pelvic inlet and returns as the deep leaf dorsal to the stomach, where it contains the left lobe of the pancreas between its peritoneal layers. It attaches to the dorsal abdominal wall. Caudal and to the left of the fundus of the stomach is the spleen, which lies largely in an outpocketing of the superficial leaf of the greater omentum.
The lesser omentum (Figs. 4-8, 4-16, 4-17), a part of the ventral mesogastrium, loosely spans the distance from the lesser curvature of the stomach to the porta of the liver. Between the liver and the cardia of the stomach, it attaches for a short distance to the diaphragm. The papillary process of the liver is loosely enveloped by the lesser omentum. On the right the free edge of the lesser omentum is the hepatoduodenal ligament, which attaches the liver to the duodenum. It contains the portal vein, the hepatic artery, and the bile duct.
The omental bursa (Figs. 4-8, 4-10, 4-26) is formed by the omenta and the adjacent organs. It has an epiploic foramen opening into the main peritoneal cavity. This opening lies dorsally to the right of the median plane at the level of the cranial duodenal flexure, caudomedial to the caudate lobe of the liver. It is bounded dorsally by the caudal vena cava, ventrally by the portal vein, caudally by the hepatic artery in the mesoduodenum, and cranially by the liver. Find this foramen and insert a finger through it.
The mesoduodenum originates at the dorsal abdominal wall and the root of the mesentery and extends to the duodenum. On the right side it passes to the descending duodenum and encloses the right lobe of the pancreas between its layers. Cranially, it is continuous with the greater omentum across the ventral surface of the portal vein. Caudally, the mesoduodenum passes from the root of the mesentery to the caudal flexure of the duodenum. On the left, it is attached to the ascending duodenum, and at the duodenojejunal flexure, it is continuous with the mesentery of the jejunum. The ascending duodenum is secondarily attached to the mesocolon of the descending colon by the duodenocolic fold.
The mesentery (mesojejunoileum) attaches to the abdominal wall opposite the second lumbar vertebra by a short peritoneal attachment known as the root of the mesentery. Vessels and nerves pass in the mesentery to supply the large and small intestines. The peripheral border of the mesentery attaches to the jejunum and the ileum. At the ileocolic junction, the mesentery is continuous with the ascending mesocolon. The ascending, transverse, and descending mesocolons connect the ascending, transverse, and descending colons to the dorsal body wall. They are continuous with each other from right to left.
There are a few short peritoneal folds that serve more to fix organs in position than as channels for blood vessels. These are called ligaments: The right triangular ligament extends from the right crus of the diaphragm above the central tendinous part to the right lateral lobe of the liver. The left triangular ligament extends from the left crus of the diaphragm to the left lateral lobe of the liver.
The coronary ligament is a sheet of peritoneum that passes between the diaphragm and the liver around the caudal vena cava and hepatic veins. On the right it is continuous with the right triangular ligament, and on the left it is continuous with the left triangular ligament. Ventrally, right and left parts of the coronary ligament converge to form the falciform ligament.
The falciform ligament (Fig. 4-16) extends from the liver to the diaphragm and ventral abdominal wall to the umbilicus. The round ligament of the liver, which is the remnant of the umbilical vein of the fetus, may be found in the young animal as a small fibrous cord lying in the free edge of the falciform ligament. It enters the fissure for the round ligament of the liver between the quadrate and left medial lobes. In adult dogs the falciform ligament is filled with fat, and it persists only from the diaphragm to the umbilicus.
Vessels and Nerves of the Abdominal Viscera
The vagus nerve, or tenth cranial nerve (Figs. 3-20, 4-27, 5-52), carries both sensory and motor fibers from and to the viscera. About 20 percent are visceral motor (preganglionic parasympathetic efferent fibers), and about 80 percent are visceral sensory (afferents from all of the thoracic and most of the abdominal organs). The vagus nerve leaves the cranial cavity via the tympano-occipital fissure and traverses the neck in the carotid sheath with the sympathetic trunk. At the thoracic inlet, the vagus separates from the sympathetic trunk and continues over the base of the heart where the recurrent laryngeal nerve branches from it. Right and left vagus nerves divide caudal to the root of the lung into dorsal and ventral branches. The dorsal branches unite near the diaphragm to form the dorsal vagal trunk. The ventral branches unite caudal to the root of the lung to form the ventral vagal trunk. These trunks lie on the dorsal and ventral surfaces of the terminal part of the esophagus. From the trunks, as well as from the dorsal and ventral branches of the vagi, nerves arise to supply the esophagus. The vagal trunks pass through the esophageal hiatus of the diaphragm and course along the lesser curvature of the stomach.
Transect the left crus of the diaphragm at the esophageal hiatus and reflect it to expose the vagal trunks. Observe the ventral vagal trunk. It supplies the liver, the parietal surface of the stomach, and the pylorus. The terminal branches need not be dissected.
The dorsal vagal trunk (Fig. 4-27) gives off a celiac branch that passes dorsocaudally and contributes to the formation of the celiac and cranial mesenteric plexuses. These abdominal aortic plexuses are nerve networks lying on, around, and passing along abdominal vessels for which they are named. Parasympathetic axons in these plexuses follow the terminal branching of the respective blood vessels to the intestines at least as far caudally as the left colic flexure. The dorsal vagal trunk continues along the lesser curvature of the stomach to supply the visceral surface of the stomach, including the pylorus. All of these parasympathetic preganglionic axons will synapse with a second neuron within the wall of the organ where they terminate. The abdominal aortic plexuses are named for the branch of the aorta with which they are associated or, in some instances, for the adjacent organ. They include the coeliac, cranial mesenteric, caudal mesenteric, adrenal, and aorticorenal plexuses. The first three will be dissected.
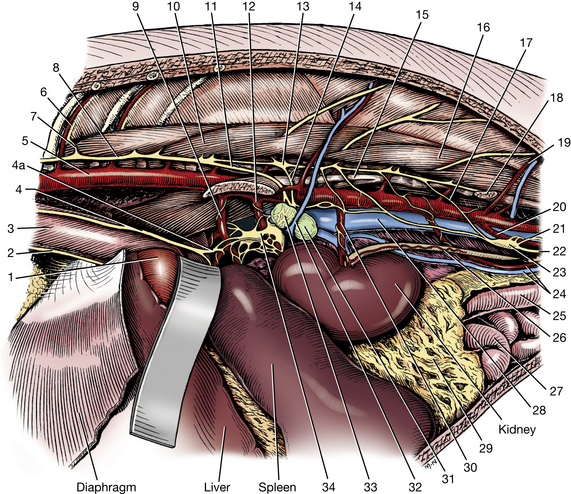
Fig. 4-27 Exposure of abdominal autonomic nervous system on left side.
In addition to the parasympathetic preganglionic axons described earlier, these plexuses contain sympathetic visceral efferent processes and numerous visceral afferent processes. Associated with many of these plexuses are abdominal sympathetic ganglia that contain cell bodies of sympathetic postganglionic axons. Within these ganglia are synapses with preganglionic sympathetic neurons that are destined to innervate the abdominal viscera.
Sympathetic Trunk
To expose the caudal thoracic and lumbar parts of the sympathetic trunk on the left side, reflect the abdominal and caudal thoracic walls so that the kidney and the crura of the diaphragm are freely accessible. Reflect the left kidney toward the median plane. The deep circumflex iliac artery and vein arise from the aorta and caudal vena cava in the caudal part of the lumbar region and may be transected and turned aside. These vessels will be described later with the branches of the abdominal aorta and caudal vena cava.
The psoas minor arises from the fascia of the muscle dorsal to it, the quadratus lumborum, and from the last thoracic and the first five lumbar vertebral bodies. It is ventral and medial to the quadratus lumborum and psoas major (Figs. 2-51, 4-27, 4-65). It inserts on the arcuate line of the ilium dorsal to the iliopubic eminence. Transect the tendon of the psoas minor caudal to the deep circumflex iliac vessels. Remove the muscle from its vertebral origins. Examine the psoas major and its union with the iliacus to form the iliopsoas muscle.
Identify the thoracic and lumbar parts of the sympathetic trunk as it passes along the vertebral bodies. Because most of the preganglionic axons in the sympathetic trunk at levels T10 to T13 pass into the major splanchnic nerve rather than into the lumbar region of the trunk, there is a distinct narrowing of the trunk caudal to the major splanchnic nerve. The trunk widens again as lumbar rami communicantes and splanchnic components enter it (Fig. 4-27).
Splanchnic Nerves
The splanchnic nerves contain sympathetic neurons that run between the sympathetic trunk and the abdominal autonomic ganglia as well as visceral afferents coursing to the spinal cord.
The major splanchnic nerve (Fig. 4-27) leaves the sympathetic trunk at the level of the twelfth or thirteenth thoracic sympathetic ganglion. It passes dorsal to the crus of the diaphragm, enters the abdominal cavity, and courses to the adrenal and celiacomesenteric ganglia and plexuses.
The minor splanchnic nerves (Fig. 4-27), generally two, usually leave the last thoracic and first lumbar sympathetic ganglia. They supply nerves to the adrenal gland, ganglion, and plexus, and they terminate in the celiacomesenteric ganglia and plexus. Dissect the origin of these nerves and their course to the adrenal gland.
The lumbar splanchnic nerves (Fig. 4-27) arise from the second to the fifth lumbar sympathetic ganglia. In general, they are distributed to the aorticorenal, cranial mesenteric, and caudal mesenteric ganglia and plexuses. Observe the origin of these nerves.
Abdominal Aortic Nerve Plexuses and Ganglia
As noted previously, branches of the vagus and splanchnic sympathetic nerves intermingle around the major abdominal arteries to form nerve plexuses in the abdomen. The plexuses supply the musculature of the artery and arterioles, and the viscera supplied by the branches of that artery.
Several sympathetic ganglia are located in the abdomen in close association with the plexuses. These ganglia are collections of cell bodies of postganglionic axons. Preganglionic axons of sympathetic splanchnic nerves must synapse in one of these ganglia. Preganglionic vagal axons (parasympathetic) do not synapse here but pass through the ganglia and plexuses to the wall of the organ innervated, where they synapse on a cell body of a postganglionic axon.
The celiac ganglia (Fig. 4-27) lie on the right and left surfaces of the celiac artery close to its origin. They are often interconnected, and numerous nerves from the ganglia follow the terminal branches of the celiac artery as a plexus.
The cranial mesenteric ganglion (Fig. 4-27) is located caudal to the celiac ganglion on the sides and caudal surface of the cranial mesenteric artery, which it partly encircles. Most of its nerves continue distally on the cranial mesenteric artery as the cranial mesenteric plexus. Because of the close relationship of the celiac and cranial mesenteric plexuses and ganglia, they are referred to as the celiacomesenteric ganglion and plexus.
The caudal mesenteric ganglion (Fig. 4-27) is located ventral to the aorta around the caudal mesenteric artery, which is an unpaired branch of the aorta caudal to the kidneys that supplies a portion of the colon. Lumbar splanchnic nerves enter the ganglion on each side. Branches may also come from the aortic and celiacomesenteric plexuses. Some of the nerves leaving the ganglion continue along the artery as the caudal mesenteric plexus.
The right and left hypogastric nerves leave the caudal mesenteric ganglion and course caudally near the ureters. They run in the mesocolon, incline laterally, and enter the pelvic canal. Their connections with the pelvic plexuses will be described later.
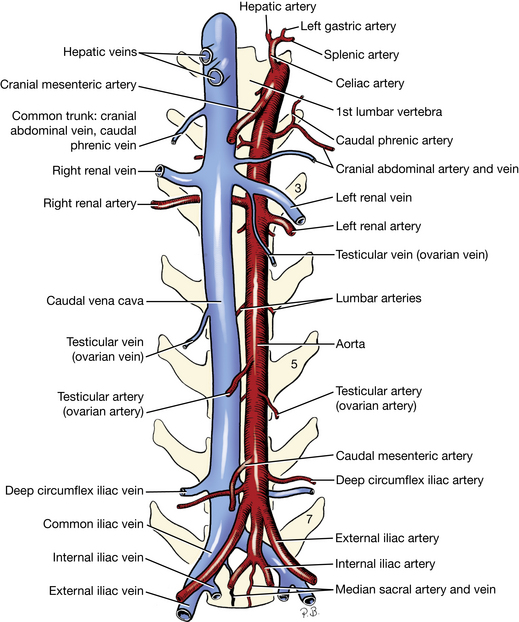
Branches Of The Abdominal Aorta
1. The paired lumbar arteries (Figs. 4-27, 4-28, 4-33) leave the dorsal surface of the aorta. Each extends dorsally and terminates in a spinal and a dorsal branch. The spinal branches pass through the intervertebral foramina into the vertebral canal whence they penetrate the dura and arachnoid that surround the spinal cord. Here they anastomose with the ventral spinal artery that is within the subarachnoid space and supply part of the spinal cord. The dorsal branches supply the muscles and skin above the lumbar vertebrae.
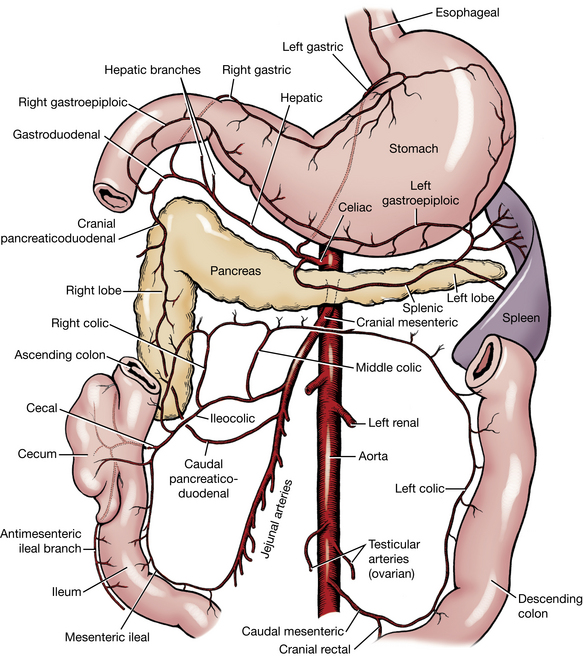
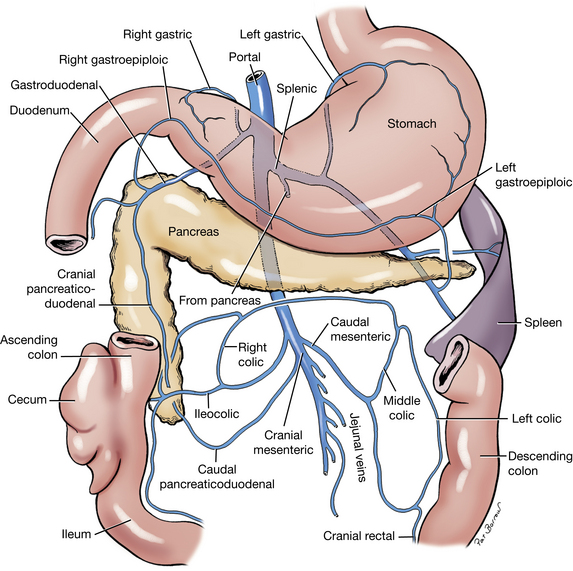
2. The celiac artery (Figs. 4-27 through 4-29) is short and arises from the aorta between the crura of the diaphragm. It has three branches: the hepatic artery, the left gastric artery, and the splenic artery. The celiac plexus of nerves covers the artery in its course through the mesentery.
The hepatic artery (Figs. 4-28, 4-29) is the first branch to leave the celiac artery. Find its origin. It courses cranially in the cranial border of the mesoduodenum, which is the caudal boundary of the epiploic foramen. It passes to the liver in the hepatoduodenal ligament. Follow this vessel dorsal to the pylorus between the lesser curvature of the stomach and the liver. One to five hepatic branches leave the hepatic artery and enter the liver. (These branches are covered with nerves and are closely associated with the hepatic lymph nodes.) The cystic artery leaves the last hepatic branch and supplies the gallbladder. It need not be dissected. After giving off branches to the liver, the hepatic artery terminates as the right gastric and the gastroduodenal arteries. This occurs in the lesser omentum.
The right gastric artery is a small artery that extends from the pylorus toward the cardia to supply the lesser curvature of the stomach. It anastomoses with the left gastric artery. It need not be dissected.
The gastroduodenal artery supplies the pylorus and terminates as the right gastroepiploic and cranial pancreaticoduodenal arteries. This occurs at the junction of the greater omentum and the mesoduodenum.
The right gastroepiploic artery enters and runs in the greater omentum along the greater curvature of the stomach. It supplies the stomach and the greater omentum. The right gastroepiploic artery anastomoses with the left gastroepiploic, a branch of the splenic artery.
The cranial pancreaticoduodenal artery follows the mesenteric border of the descending duodenum, where it supplies the duodenum and adjacent right lobe of the pancreas. It anastomoses with the caudal pancreaticoduodenal artery, which is a branch of the cranial mesenteric artery.
The left gastric artery (Figs. 4-28, 4-29) runs in the greater omentum to the lesser curvature of the stomach near the cardia and supplies both surfaces of the stomach. One or more esophageal rami pass cranially on the esophagus. It extends toward the pylorus, where it anastomoses with the right gastric artery.
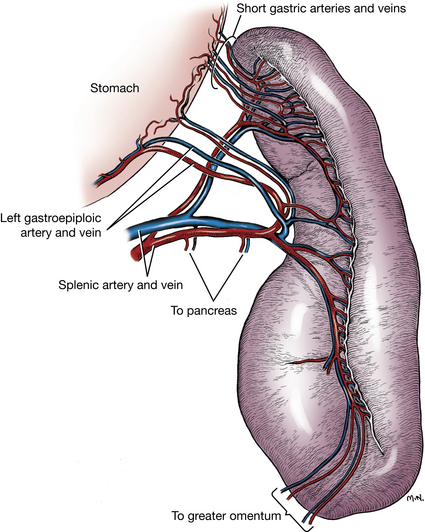
The splenic artery (Figs. 4-28 through 4-30) crosses the dorsal surface of the left lobe of the pancreas in the deep leaf of the greater omentum—to which it may supply branches—before dividing into dorsal and ventral splenic branches that enter the hilus of the spleen on its visceral surface. The dorsal branch gives rise to several arteries that enter the dorsal end of the spleen and a few short gastric arteries that course in the gastrosplenic ligament to the greater curvature of the stomach on the left side. The dorsal splenic branch continues as the left gastroepiploic artery on the greater curvature of the stomach. At the pyloric end of the stomach, the left gastroepiploic artery anastomoses with the right gastroepiploic artery, a branch of the hepatic artery. The ventral splenic branch supplies the rest of the spleen by numerous branches that enter at the hilus. Variations in this pattern exist, and you may find that the ventral branch of the splenic, rather than the dorsal branch, gives rise to the left gastroepiploic artery.
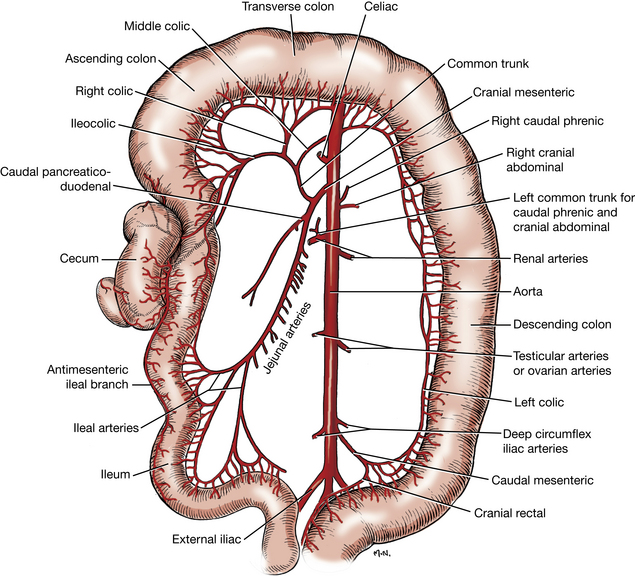
3. The cranial mesenteric artery (Figs. 4-28, 4-29, 4-31) leaves the aorta caudal to the celiac artery. It is surrounded proximally by the cranial mesenteric plexus of nerves and partly by the cranial mesenteric ganglion. Peripheral to the ganglion are the mesenteric lymph nodes and branches of the portal vein. Reflect these from the vessel. Observe the branches of the cranial mesenteric artery.
The middle, right, and ileocolic arteries arise from a common trunk from the cranial mesenteric artery and course through the mesocolon. Reflect the small intestine caudally and expose the colon cranial to the root of the mesentery. Dissect its blood supply within the mesocolon.
The middle colic artery, the first branch from the common trunk, runs cranially in the mesocolon to the mesenteric border of the left colic flexure and descending part of the colon. It bifurcates near the left colic flexure. One branch runs distally in the descending mesocolon, supplies the descending colon, and then anastomoses with the left colic artery, a branch of the caudal mesenteric artery. The other branch passes to the right and forms an arcade with the smaller right colic artery and supplies the transverse colon.
The right colic artery runs in the right mesocolon toward the right colic flexure, giving off branches to the distal part of the ascending colon and the adjacent transverse colon. It forms arcades with the middle colic artery and the colic branch of the ileocolic artery.
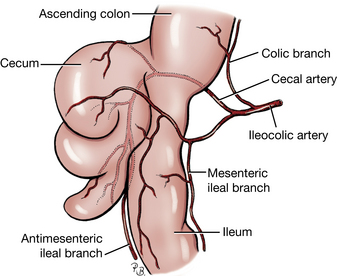
The ileocolic artery (Figs. 4-29, 4-31, 4-32) supplies the ileum, cecum, and ascending colon. It is closely associated with the right colic lymph node. The ascending colon is supplied by the colic branch. The cecal artery crosses the dorsal surface of the ileocolic junction and supplies the cecum and antimesenteric side of the ileum. The ileocolic artery continues as the mesenteric ileal branch to anastomose with ileal arteries of the cranial mesenteric artery.
The caudal pancreaticoduodenal artery (Figs. 4-29, 4-31) arises from the cranial mesenteric artery close to the common trunk for the colon. It runs to the right in the mesoduodenum to the descending portion of the duodenum near the caudal flexure. It supplies the descending duodenum and the right lobe of the pancreas and anastomoses with the cranial pancreaticoduodenal artery.
The jejunal arteries arise from the caudal side of the cranial mesenteric artery. They form arcades in the mesentery close to the jejunum.
The cranial mesenteric artery is terminated by ileal arteries, the last of which anastomoses with a branch of the ileocolic artery.
4. The common trunk of the caudal phrenic and cranial abdominal arteries (Figs. 4-22, 4-28, 4-31, 4-33) is paired and arises from the aorta between the cranial mesenteric and renal arteries. This common trunk crosses the ventral surface of the psoas muscles dorsal to the adrenal gland. The caudal phrenic artery runs cranially to supply the diaphragm. The cranial abdominal artery continues into the abdominal wall and ramifies between the transversus abdominis and the internal abdominal oblique, where it was previously dissected.
The adrenal gland may receive branches from the aorta or caudal phrenic, renal, or lumbar arteries.
5. The renal arteries (Figs. 4-12, 4-22, 4-27, 4-28) leave the aorta at different levels. The right one arises cranial to the left, in conformity with the more cranial position of the right kidney. It is longer than the left and lies dorsal to the caudal vena cava.
6. The ovarian artery (Figs. 4-12, 4-28, 4-33) of the female is homologous to the testicular artery of the male. This paired vessel arises from the aorta about halfway between the renal and external iliac arteries. The ovarian artery varies in size, position, and tortuosity, depending on the degree of development of the uterus. Each ovarian artery divides into two or more branches in the mesovarium just medial to the ovaries. Branches supply the ovary and its bursa and the uterine tube and horn. The branch to the uterine horn anastomoses with the uterine artery, a branch of the vaginal artery that runs cranially in the mesometrium.
The testicular artery (Figs. 4-27 through 4-29, 4-33) leaves the aorta in the midlumbar region and crosses the ventral surface of the ureter. The testicular artery, vein, and nerve plexus lie in a peritoneal fold, the mesorchium, which can be followed to the level of the vaginal ring. Their course in the spermatic cord has been dissected.
The right testicular and ovarian veins enter the caudal vena cava near the origin of the artery from the aorta. However, the left testicular and ovarian veins usually enter the left renal vein. This is important surgically.
7. The caudal mesenteric artery (Figs. 4-28, 4-29, 4-31) is unpaired and arises near the termination of the aorta. It enters the descending mesocolon and runs caudoventrally to the mesenteric border of the descending colon, where it terminates in two branches of similar size. The left colic artery follows the mesenteric border of the descending colon cranially to anastomose with the middle colic artery. The cranial rectal artery descends along the rectum and anastomoses with the middle rectal artery from the prostatic or vaginal artery.
8. The deep circumflex iliac artery (Figs. 4-12, 4-27, 4-28, 4-33) is paired and arises from the aorta close to the origin of the external iliac artery. It crosses the sublumbar muscles laterally, and at the lateral border of the psoas major it supplies the musculature of the caudodorsal portion of the abdominal wall. The deep circumflex iliac artery perforates the abdominal wall and becomes superficial ventral to the tuber coxae. It supplies the skin of the caudal abdominal area, the flank, and the cranial thigh. This vessel was transected when the psoas minor muscle was removed.
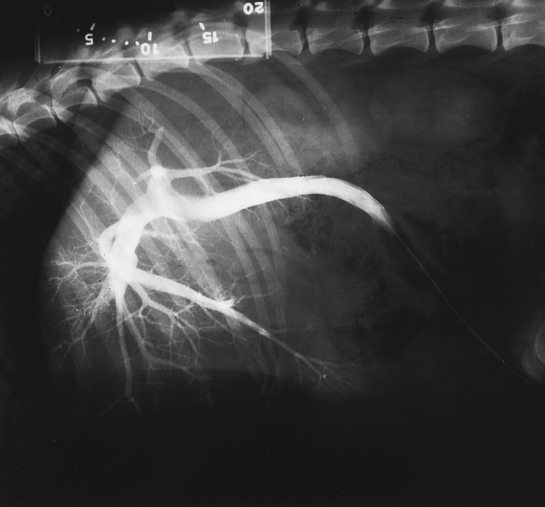
Portal Venous System
A venous portal system consists of a capillary bed interposed between veins returning blood to the heart. The portal vein (Figs. 4-17, 4-34, 4-35) carries venous blood to the liver from abdominal viscera such as the stomach, the small intestine, the cecum, the colon, the pancreas, and the spleen. The liver has a capillary bed of sinusoids through which the blood passes before it exits through large hepatic veins to enter the caudal vena cava and then the heart on the right side (Fig. 4-16). Separate the caudate process of the caudate lobe of the liver from the cranial duodenal flexure. Find the portal vein in the hepatoduodenal ligament at the ventral border of the epiploic foramen. Reflect the peritoneum and fat from the surface of the vein as far caudally as the root of the mesentery and expose its branches.
1. The gastroduodenal vein is a small, proximal branch of the portal vein in the mesoduodenum. It enters the portal vein from the right side near the body of the pancreas and drains the pancreas, the stomach, the duodenum, and the greater omentum.
2. The splenic vein enters the portal vein from the deep leaf of the greater omentum on the left side just caudal to the gastroduodenal branch. It is a large branch that receives blood from the spleen, the stomach, the pancreas, and the greater omentum. It receives the left gastric vein, which drains the lesser curvature of the stomach.
3. The cranial and caudal mesenteric veins are the distal terminal branches of the portal vein. The cranial mesenteric vein arborizes in the mesentery and collects blood from the jejunum, the ileum, the caudal duodenum, and the right lobe of the pancreas. The caudal mesenteric vein in the mesocolon drains the cecum and the colon.
As the portal vein enters the liver in the hepatoduodenal ligament, it divides into a short right and a long left branch. The right branch supplies the right lateral lobe and caudate process of the caudate lobe. The left branch supplies the other lobes. Within these lobes the portal venous branches give rise to a large array of hepatic sinusoids (Fig. 4-36) that form an extensive capillary bed. These are drained by larger branches that give rise to a variable number of hepatic veins that enter the caudal vena cava as it traverses the dorsal aspect of the liver (Fig. 4-16). Open this part of the caudal vena cava and observe the entrance of these hepatic veins.
PELVIC VISCERA, VESSELS, AND NERVES
To reflect the left pelvic limb, first reflect the penis and scrotum to the right. Cut through the pelvic symphysis with a cartilage knife, saw, or bone cutters. Locate the wing of the left ilium and sever all muscles that attach to its medial and ventral surfaces. Apply even but constant lateral pressure to the left os coxae by abducting the limb and at the same time cut through the cranioventral aspect of the sacroiliac joint. Cut the attachment of the penis to the left ischiatic tuberosity. Leave the limb attached. All structures more easily traced from the left should be dissected from this side.
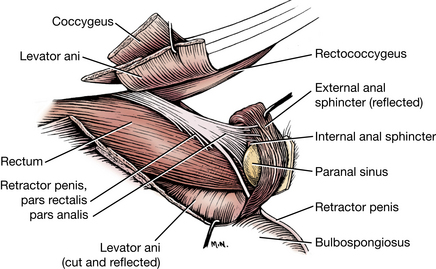
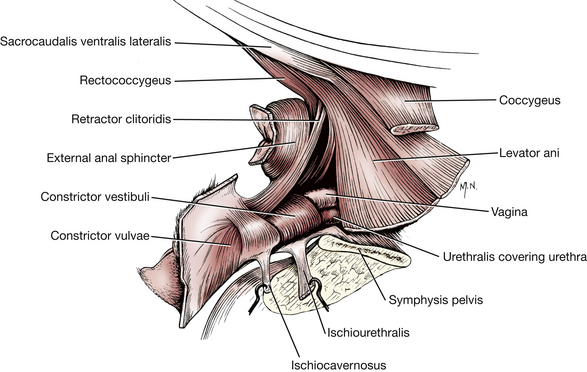
The levator ani muscle (Figs. 4-37, 4-45 through 4-47, 4-54, 4-65) lies medial to the coccygeus muscle. It is a broad, thin muscle originating on the medial edge of the body of the ilium and the dorsal surface of the pubis and the pelvic symphysis. It covers the cranial part of the internal obturator. The muscle appears caudal to the coccygeus, where it inserts on caudal vertebrae 3 to 7. Transect this muscle on the left side near its origin and reflect it.
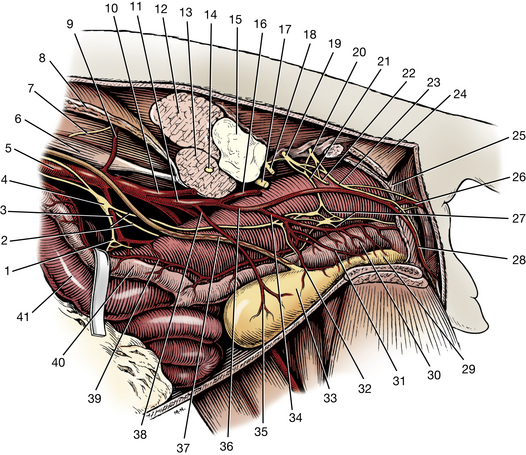
Fig. 4-37 Autonomic nerves and vessels of pelvic region, left lateral view.
The coccygeus muscle (Figs. 4-37, 4-45 through 4-47, 4-54, 4-65) lies lateral to the levator ani muscle. It is shorter and thicker and arises from the ischiatic spine and inserts on the transverse processes of caudal vertebrae 2 to 4. Transect the muscle at its origin. The levator ani and coccygeus muscles of each side form a pelvic diaphragm through which the genitourinary and digestive tracts open to the outside.
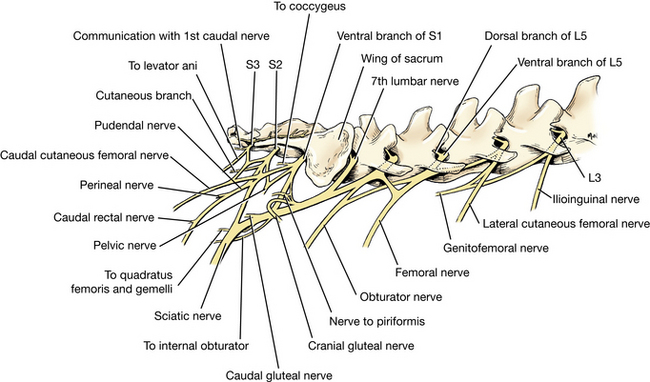
The pelvic plexus (Fig. 4-37) lies caudal to a plane passing through the pelvic inlet and dorsal to the prostate. It is closely applied to the surface of the rectum and the vaginal/prostatic artery. It can be identified by tracing the left hypogastric nerve to it. Occasionally, ganglia are large enough to be recognized in the plexus. The pelvic plexus contains sympathetic fibers from the hypogastric nerve and parasympathetic fibers from the pelvic nerve.
The pelvic nerve (Figs. 4-37, 4-58, 4-65, 4-66) is formed by parasympathetic preganglionic axons that leave the ventral branches of the three sacral spinal nerves. Find the left pelvic nerve on the lateral wall of the distal portion of the rectum. It is a very small nerve. Attempt to trace it proximally to its origin. It supplies branches to the urogenital organs, the rectum, and the descending colon. The branches to the urogenital organs join the pelvic plexus and follow the vaginal/prostatic vessels to these organs.
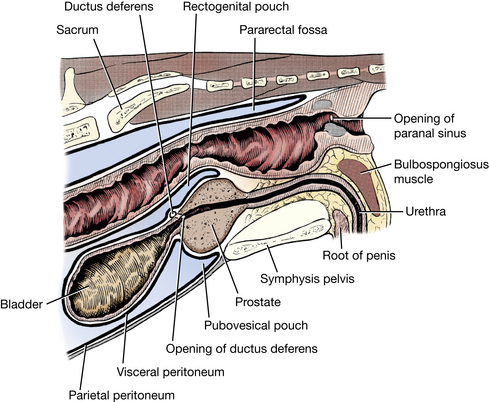
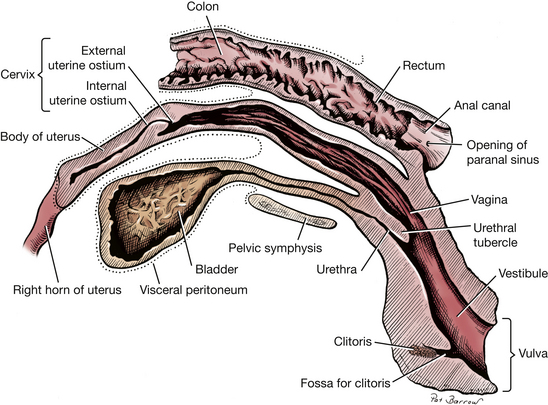
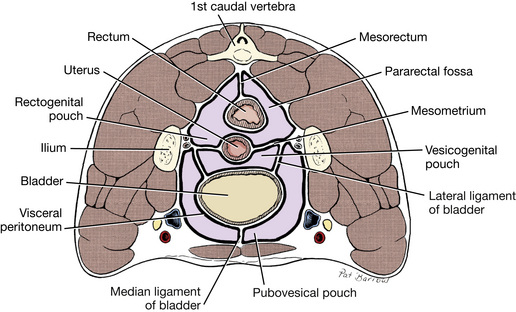
The extension of the peritoneal cavity dorsal to the rectum on either side of the mesorectum is the pararectal fossa (Figs. 4-8, 4-41, 4-53). Caudally, it extends approximately to the plane of the second caudal vertebra (Fig. 4-41). The pararectal fossa is continuous ventrally with the common peritoneal space between the rectum and uterus or prostate. This is the rectogenital pouch. In the female the rectogenital pouch communicates ventrally on either side of the uterus with the vesicogenital pouch between the uterus and bladder. The vesicogenital pouch in the female and the rectogenital in the male communicate with the short pubovesical pouch between the bladder and ventral body wall and pubis. This is divided by the median ligament of the bladder.
Iliac Arteries
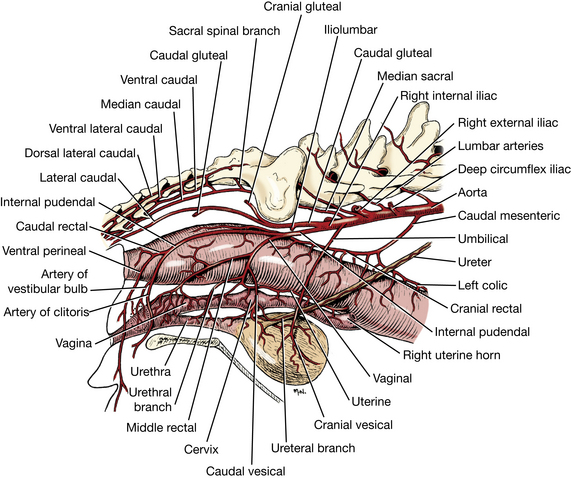
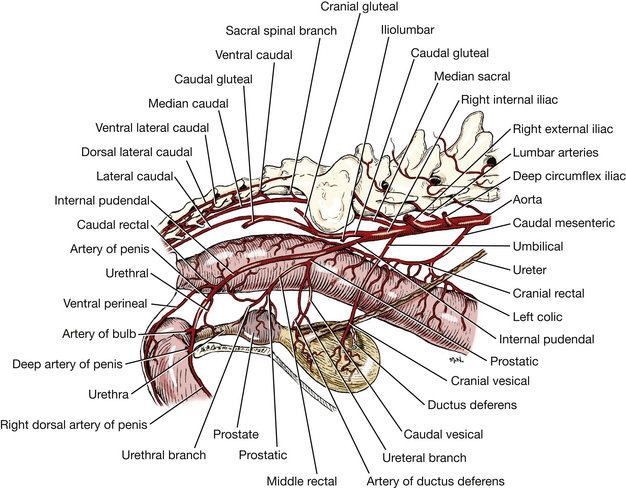
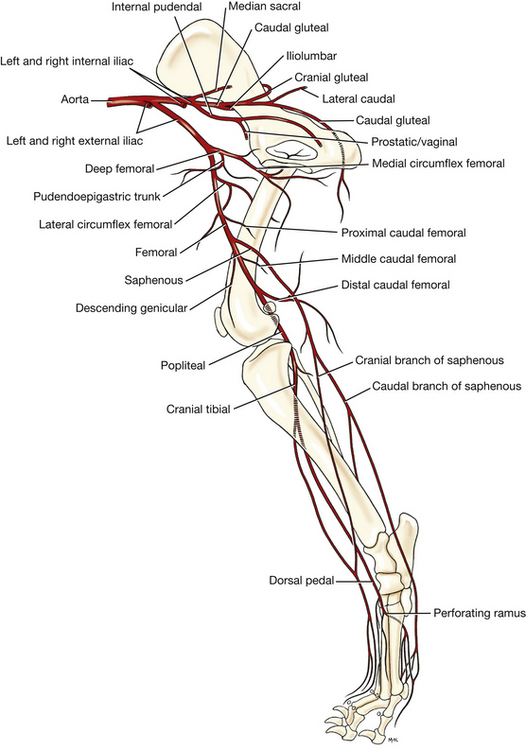
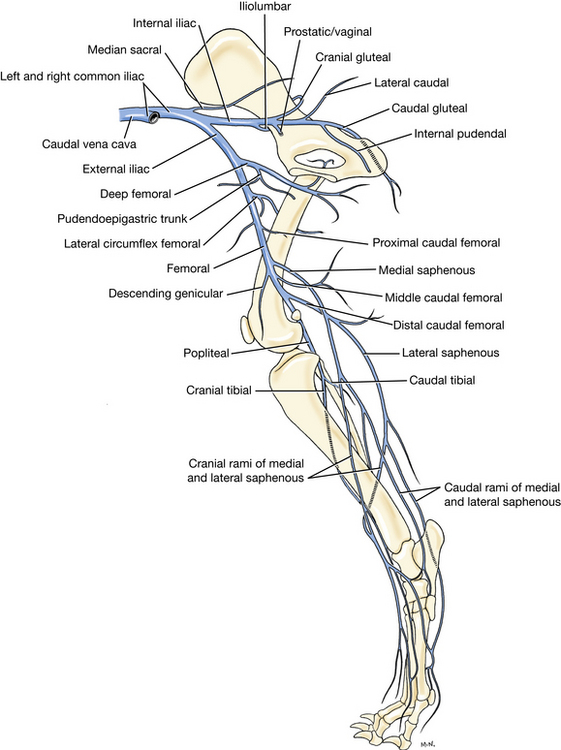
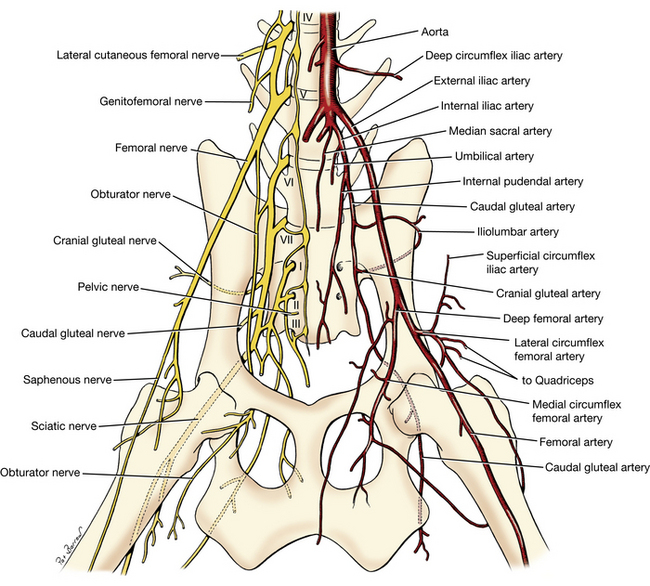
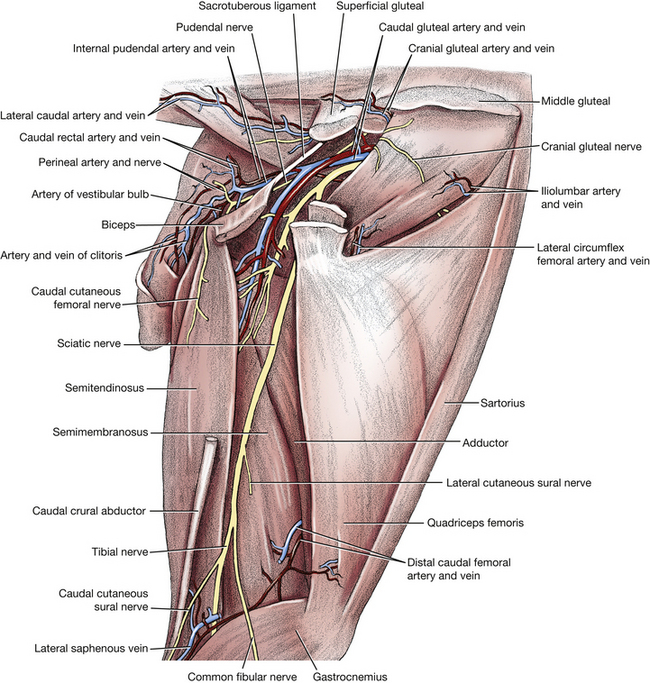
The paired iliac arteries (Figs. 4-28, 4-33, 4-37 through 4-39, 4-58) supply the pelvis and pelvic limb. The external iliac runs ventrocaudally and becomes the femoral artery as it leaves the abdomen through the vascular lacuna. The internal iliac arises caudal to the external iliac and passes caudolaterally into the pelvis.
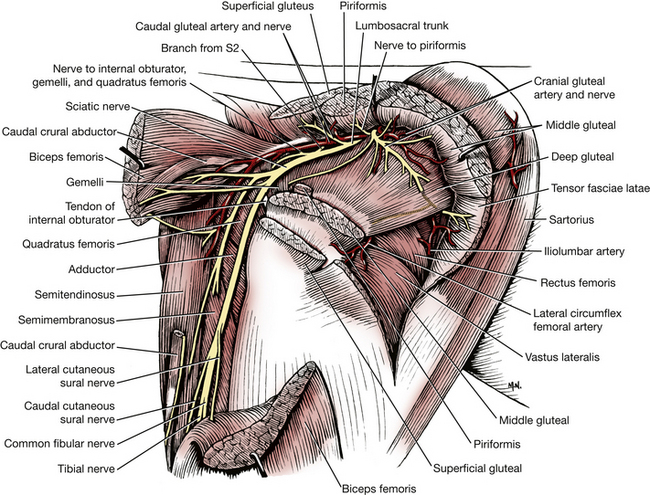
The internal iliac arteries and the smaller, unpaired median sacral artery terminate the aorta. Find the origin of these vessels. The internal iliac artery gives off the rudimentary umbilical artery and terminates cranial to the sacroiliac joint as the caudal gluteal and internal pudendal arteries. The caudal gluteal primarily supplies muscles on the outside of the pelvis and in the caudal thigh. The internal pudendal is distributed to the pelvic viscera and external genitalia at the ischial arch. Dissect the following vessels on the left side.
In the fetus the umbilical artery is a large, paired vessel that carries blood from the aorta to the placenta through the umbilicus. Find the remnant of this vessel, the round ligament of the bladder. It arises near the origin of the internal iliac artery and courses to the apex of the bladder in its lateral ligament. In some specimens it remains patent this far and supplies the bladder with cranial vesical arteries. Distal to the bladder the vessel is obliterated. There are no visible remnants in the median ligament of the bladder.
Find the origin of the internal pudendal artery (Figs. 4-37 through 4-39) from the internal iliac and dissect its branches. It is the smaller, more ventral branch that runs caudally on the terminal tendon of the psoas minor. At the level of the sacroiliac joint, the internal pudendal gives rise to the vaginal or prostatic artery.
The vaginal or prostatic artery forms an angle of about 45 degrees with the internal pudendal. It passes ventrally in an arch and terminates in cranial and caudal branches. In the female the cranial branch is the uterine artery. The uterine artery supplies a caudal vesical artery to the bladder and has ureteral and urethral branches. The uterine artery courses cranially along the body and horn of the uterus in the broad ligament and anastomoses with the uterine branch of the ovarian artery in the mesometrium. (This artery must be located on each side and ligated in an ovariohysterectomy procedure.) The caudal branch of the vaginal artery is the middle rectal artery, which supplies branches to the rectum and vagina. In the male the prostatic artery passes caudoventrally from the internal pudendal toward the prostate gland. Its cranial branch is the artery of the ductus deferens, which gives off a caudal vesical artery to the bladder, with ureteral and urethral branches. It then continues along the ductus deferens, which it supplies. The caudal branch is the middle rectal artery, which supplies the rectum, prostate, and urethra.
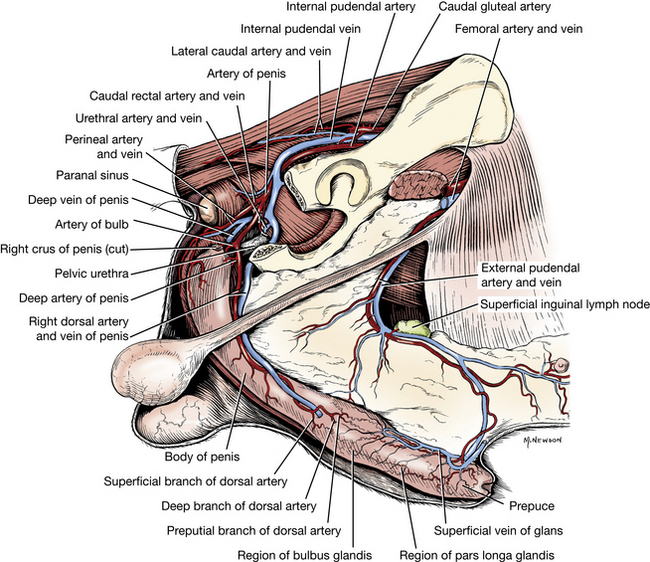
Reflect the skin and fat from the right ischiorectal fossa. The internal pudendal artery (Figs. 4-37 through 4-40, 4-68) passes obliquely across the greater ischiatic notch. It continues along the dorsal border of the ischiatic spine lateral to the coccygeus muscle and medial to the gluteal muscles and sacrotuberous ligament. It then courses medially into the ischiorectal fossa accompanied by the pudendal nerve. Here it terminates as a ventral perineal artery, a variable urethral artery, and an artery of the penis or clitoris. These vessels may be dissected on either side.
The ventral perineal artery may be seen passing caudally. It supplies a caudal rectal artery to the rectum and anus and terminates in the skin of the perineum and the scrotum or vulva.
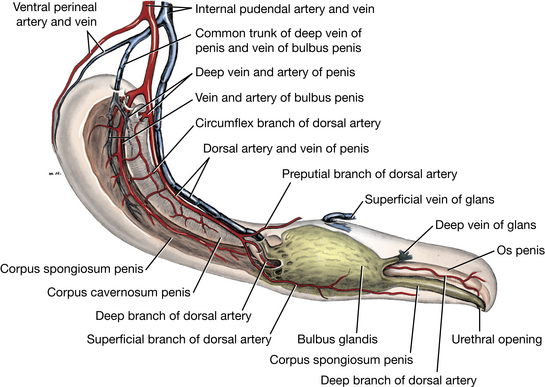
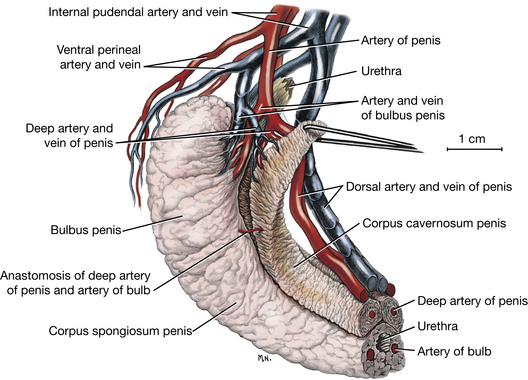
The artery of the penis (Figs. 4-39, 4-40) courses caudoventrally and terminates at the level of the ischial arch as three branches. The artery of the bulb of the penis arborizes in the bulb and continues to supply the corpus spongiosum and penile urethra. Observe this artery as it enters the bulb. The deep artery of the penis arises close to the artery of the bulb and enters the corpus cavernosum at the crus. This is at the level of the ischial arch lateral to the penile bulb. The dorsal artery of the penis runs on the dorsal surface to the level of the bulbus glandis, where it divides and sends branches to the prepuce and pars longa glandis. The penile arteries are accompanied by veins that have an important role in the mechanism of erection (Fig. 4-40).
In the female the artery of the clitoris courses caudoventrally to supply the clitoris and vestibular bulb.
Pelvic Viscera
The urinary bladder (Figs. 4-11, 4-41 through 4-43, 4-53) has an apex, a body, and a neck. Three connecting peritoneal folds (ligaments), are reflected from the bladder on the pelvic and abdominal walls. The median ligament of the bladder (Figs. 4-11, 4-53) leaves the ventral surface of the bladder and attaches to the abdominal wall as far cranial as the umbilicus. In the fetus it contains the urachus and umbilical arteries. These degenerate and leave no ligamentous remnant in the adult. The lateral ligament of the bladder passes to the pelvic wall and often contains an accumulation of fat along with the ureter and umbilical artery.
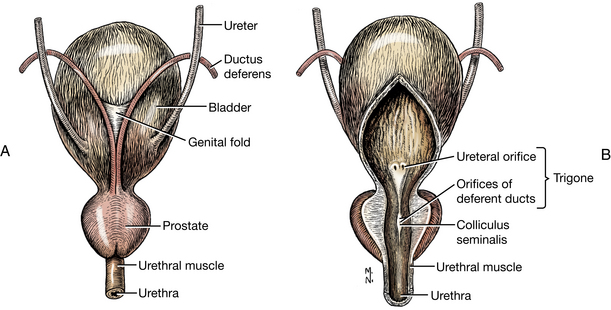
Fig. 4-42 Bladder, prostate, and associated structures. A, Dorsal view. B, Ventral view with bladder and urethra opened on the midline.
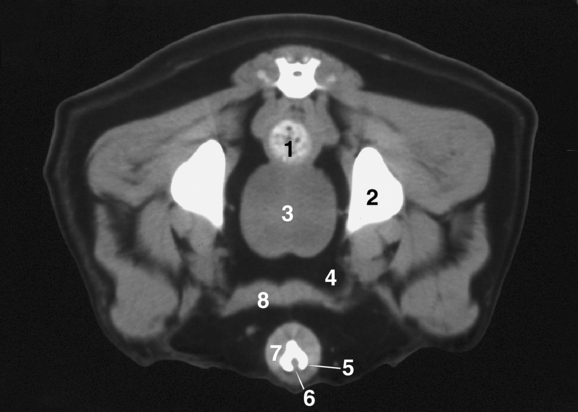
Observe the pattern of the bundles of smooth muscle on the surface of the bladder. These smooth muscle bundles pass obliquely across the neck of the bladder and the origin of the urethra. The muscle is innervated by the pelvic nerve (sacral parasympathetic neurons). No gross anatomical sphincter is present in the neck of the bladder, but a physiological sphincter of smooth muscle is maintained by sympathetic visceral efferent innervation.
The urethral muscle is striated and is confined to the pelvis, where it surrounds the pelvic urethra and serves as a voluntary sphincter to retain the urine. It is innervated by the pudendal nerve (sacral somatic efferent neurons). Make a midventral incision through the bladder wall and the urethra. In the male this should include the prostate gland.
Examine the mucosae of the bladder and urethra. If the bladder is contracted, its mucosa will be thrown into numerous folds, or rugae, as a result of its inelasticity.
Observe the entrance of the ureters into the bladder. These lie opposite each other near the neck of the organ. The trigone of the bladder is the dorsal triangular area located within lines connecting the ureteral openings into the bladder and the urethral exit from it.
The rectum (Figs. 4-41, 4-46, 4-52) continues the descending colon through the pelvis. It begins at the pelvic inlet. The anal canal is a continuation of the rectum to the anus. It consists of three zones and begins with the columnar zone, where the mucosa of the rectum forms longitudinal folds. The longitudinal ridges are called anal columns. They terminate at the intermediate zone, or anocutaneous line, where small pockets, anal sinuses, are formed between the columns. Distal to this line is the larger cutaneous zone of the anal canal, which has fine hairs, microscopic circumanal glands, and, on each side, the prominent ventrolateral opening of the paranal sinus (anal sac). The anal canal is surrounded by both a smooth internal and a striated external sphincter muscle (Figs. 4-45, 4-46). The external opening of the anal canal is the anus. Transect the external sphincter on the left and reflect it from the paranal sinus. This muscle receives its nerve supply from the caudal rectal nerve (pudendal) and its blood supply from the caudal rectal branch of the internal pudendal artery.
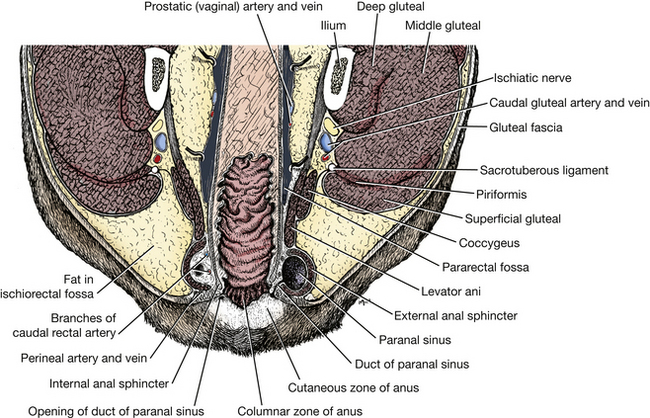
Fig. 4-46 Section through anus, dorsal plane. (Right side cut at lower level through duct of paranal sinus).
Observe the paranal sinus (Figs. 4-45, 4-46), expose its duct, and find the opening in the cutaneous zone of the anal canal. In the wall of this sinus are microscopic glands, the secretion of which accumulates in the lumen. The secretion is discharged through the duct of the paranal sinus. Open the sinus and examine its interior.
The internal sphincter muscle of the anus is an enlargement of the smooth circular muscle coat of the anal canal. It is not as distinct as the external sphincter.
The rectococcygeus muscle (Figs. 4-45, 4-47, 4-54) continues the longitudinal smooth muscle of the rectum to the ventral surface of the tail. Reflect the levator ani and coccygeus muscles from the left side of the rectum. Observe the rectococcygeus muscle arising from the dorsal surface of the rectum cranial to the sphincter muscles. Trace it caudally to its insertion on the caudal vertebrae.
Male
The prostate gland (Figs. 4-39, 4-41, 4-42, 4-44) completely surrounds the neck of the bladder and the beginning of the urethra. Examine the surface, form, size, and location of the prostate on several specimens. The normal size and weight of the prostate vary greatly. The organ generally lies at the pelvic inlet. It is larger and extends farther into the abdomen in older dogs. The prostate is flattened dorsally and rounded ventrally and on the sides. It is heavily encapsulated. Muscle fibers from the bladder run caudally on its dorsal surface. A longitudinal septum leaves the ventral part of the capsule and reaches the prostatic part of the pelvic urethra, thus partially dividing the gland ventrally into right and left lobes. This is indicated on the ventral surface by a shallow but distinct longitudinal furrow. Notice that the urethra runs through the center of the gland. Open the urethra and examine its lumen from the ventral aspect.
The male urethra is composed of a pelvic part within the pelvis and a penile part within the penis. The pelvic part has preprostatic and prostatic components. The urethral crest (Fig. 4-42) protrudes into the lumen from the dorsal wall of the prostatic part of the pelvic urethra. Near its middle and protruding farthest into the lumen of the urethra is a hillock, the colliculus seminalis. On each side of this eminence the deferent ducts open. Many prostatic openings are found on both sides of the urethral crest and can usually be seen if the gland is compressed.
On the dorsal surface of the bladder, locate the two deferent ducts where they are joined by the genital fold (Figs. 4-42, 4-43). Ventral to this fold is the vesicogenital pouch of the peritoneal cavity.
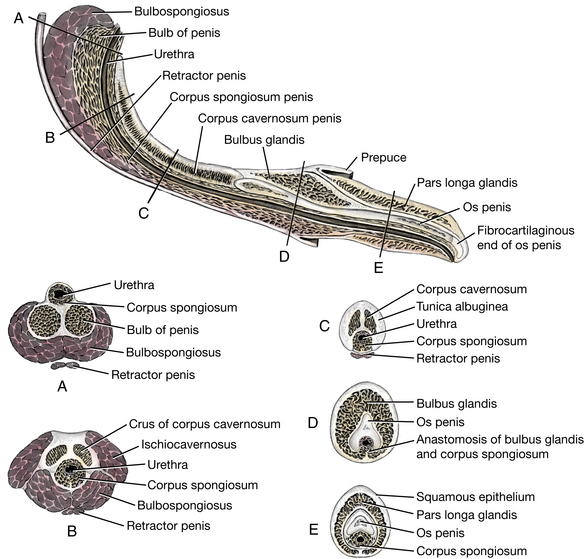
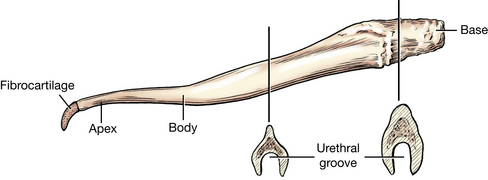
The penis is composed of a root, a body, and a glans (Figs. 4-40, 4-47 through 4-50). The dorsal surface of the penis faces the pelvic symphysis and the abdominal wall. In the nonerect state the glans is entirely withdrawn into the prepuce.
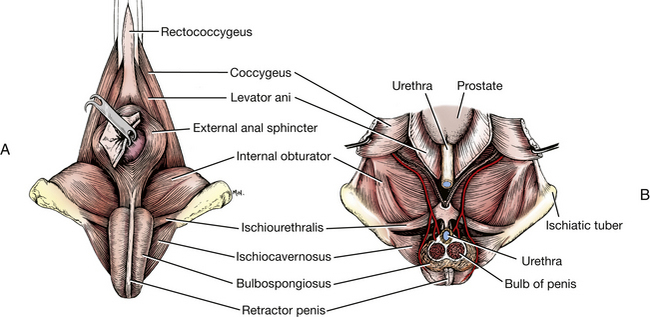
Fig. 4-47 Male perineum. A, Superficial muscles, caudal aspect. B, Dorsal section through pelvic cavity. The bilobed bulb of the penis is transected and the proximal portion is removed.
The prepuce is a tubular sheath or fold of integument that is continuous with the skin of the ventral abdominal wall and is reflected over the glans (Figs. 4-40, 4-50). It has a smooth internal layer and a haired external layer, which meet at the preputial orifice. At its deepest recess, the fornix of the prepuce, the internal layer is reflected onto the glans as the skin of the glans. In the erect state the fornix is eliminated, because the internal layer of the prepuce is closely applied to the body of the penis. Open the prepuce by a midventral incision from the orifice to the fornix. Continue the midventral skin incision to the anus so as to expose the entire length of the penis.
The root of the penis is formed by right and left crura, which originate on the ischiatic tuberosity of each side. The root ends where the crura blend with each other on the midline to form the body. Each crus is composed of vascular cavernous tissue, corpus cavernosum penis, supplied by the deep artery of the penis and surrounded by a thick fibrous tunic, the tunica albuginea. Examine the root. The left crus was transected when the limb was reflected. The trabeculae and vascular spaces can be seen on the cut surface. Note the firm attachment of the right crus to the ischiatic tuberosity. The root of the penis includes the two crura and the bulb. The ischiocavernosus muscle (Figs. 4-47, 4-50) arises from the ischiatic tuberosity, covers the origin of the crus, and inserts distally on the crus.
The retractor penis muscle (Figs. 4-45, 4-47, 4-50) is an elongated slip of mixed smooth and striated muscle fibers. It originates from the ventral surface of the sacrum, or first two caudal vertebrae, blends with the external anal sphincter, and extends distally on the ventral surface of the penis to the level of the glans, where it inserts. In the region of the anal sphincter, there is muscle fiber exchange between the retractor penis muscle and the external anal sphincter. Observe the retractor muscle on the body of the penis.
The bulbospongiosus muscle (Figs. 4-47, 4-50) bulges between the ischiocavernosus muscles ventral to the external anal sphincter. The fibers of the bulbospongiosus are transverse proximally, where they cover the bulb of the penis, and longitudinal distally, where they pass onto the body of the penis.
At the root of the penis between the crura is the bulb of the penis (Figs. 4-47 through 4-50) covered by the bulbospongiosus muscle. This bilobed dorsal expansion of the corpus spongiosum penis surrounds the urethra and is located at the ischial arch. It is supplied by the artery of the bulb. Observe the penile bulb and its relationship to the urethra at the root of the penis. Make one or two transverse sections through the root of the penis to observe its components. A thin layer of corpus spongiosum surrounds the entire length of the urethra in the penis.
The ischiourethralis muscle (Fig. 4-47) is a small transverse muscle that arises from the dorsal surface of the ischial tuberosity laterally and forms a fibrous ring with the opposing muscle at the pelvic symphysis that encircles the common trunk of the left and right dorsal veins of the penis. Contraction of the two muscles controls the venous return from the penis and helps maintain penile tumescence.
The body of the penis extends from the root, where the crura blend with each other, to the glans covering the os penis in the caudal portion of the prepuce (Figs. 4-40, 4-48, 4-50). Note that the region at the beginning of the body of the penis is compressed from side to side and wrapped by a thick tunic. It is capable of being bent without twisting when the male dismounts during coitus and remains “locked” for a variable period.
The corpus cavernosum penis (Figs. 4-48 through 4-50) of each crus converges toward the midline and the two corpora extend side by side throughout the body to the os penis. A median septum completely separates the two corpora, and each is covered by a thick white capsule (tunica albuginea) throughout its length. The two corpora cavernosa form a groove ventrally that contains the urethra and the thin corpus spongiosum that surrounds the urethra. Make several incomplete transections through the body of the penis to study these structures.
The glans of the penis is composed of two parts, the proximal bulbus glandis and the distal, more elongate pars longa glandis (Figs. 4-40, 4-44, 4-48, 4-50). The bulbus glandis, surrounding the proximal end of the os penis, is a dorsal extension of the corpus spongiosum. It is an expansile vascular structure that is largely responsible for retaining the penis within the vagina during copulation. The pars longa glandis is a cavernous tissue structure that overlaps the distal half of the bulbus glandis and continues to the distal end of the penis, partially encircling the os penis and the urethra. The pars longa glandis has no direct arterial communication with the corpus spongiosum penis and is separated from the bulbus glandis by a layer of connective tissue. Venous channels drain the pars longa glandis into the bulbus glandis through this layer. Make a longitudinal incision on the dorsum of the penis through the glans to observe its structure.
The os penis (Figs. 4-50, 4-51) is a long, ventrally grooved bone that lies almost entirely within the glans penis. It forms about a month after birth as an ossification of the fused distal ends of the corpora cavernosa. The expanded, rough, truncate base of the bone originates in the tunica albuginea of the corpora cavernosa. The body of the os penis extends through the glans penis. The base and body are grooved ventrally by the urethral groove, which surrounds the urethra and the corpus spongiosum on three sides. The bone ends as a long, pointed fibrocartilage in the tip of the glans, dorsal to the urethral opening.
At the level of the collar-like bulbus glandis of the glans of the penis, there is a communication between the corpus spongiosum penis and the bulbus glandis. The dorsal artery of the penis courses to the glans, where it supplies the prepuce, corpus spongiosum, and pars longa glandis.
Female
The cervix (Figs. 4-24, 4-37, 4-38, 4-52) is the constricted caudal portion of the uterus. It forms a small palpable enlargement just caudal to the short body of the uterus. The cervical canal is in a nearly vertical position, with the uterine opening (internal uterine ostium) dorsal and the vaginal opening (external uterine ostium) ventral in position.
The vagina (Figs. 4-24, 4-37, 4-38, 4-52) is located between the uterine cervix and the vestibule. The most cranial part of the vagina is the fornix, which extends cranial to the cervix along its ventral margin. The mucosal lining of the remaining part of the vagina is thrown into longitudinal folds that have small transverse folds. These are evidence of its ability to enlarge in both diameter and length. The longitudinal folds end dorsally at the level of the urethral orifice, where the vagina joins the vestibule. A prominent dorsal longitudinal fold in the cranial vagina nearly obscures the external uterine os and makes catheterization difficult. Note the caudoventral inclination of the vagina and the vestibule.
The vestibule (Figs. 4-24, 4-52) is the cavity that extends from the vagina to the vulva. Open the vestibule and vagina by a dorsal, midline longitudinal incision. The urethral tubercle projects from the floor of the cranial part of the vestibule. The urethra opens on this tubercle. This tubercle is at the level of the ischial arch. Note its relationship to the more ventrally placed vulva.
In the floor and ventrolateral wall of the vestibule, deep to the mucosa, are two elongated masses of erectile tissue, the vestibular bulbs. They are homologous to the bulbs of the penis of the male and lie in close proximity to the body of the clitoris. They are difficult to distinguish unless your incision passed through them.
The clitoris (Figs. 4-24, 4-52) is the female homologue of the penis. It is a small structure located in the floor of the vestibule near the vulva. It is composed of paired crura, a short body, and a glans clitoridis, which are difficult to distinguish. The glans clitoridis is a very small erectile structure that lies in the fossa clitoridis. The fossa is a depression in the floor of the vestibule and should not be mistaken as the urethral opening. The dorsal wall of the fossa partly covers the glans clitoridis and is homologous to the male prepuce. Identify the fossa and glans clitoridis. Only rarely is an os clitoridis present in the glans.
The retractor clitoridis muscle (Fig. 4-54), a homologue of the retractor penis in the male, originates on the first two caudal vertebrae, joins the external anal sphincter, blends with the constrictor vulvae, and continues onto the ventral surface of the clitoris.
The vulva includes the two labia and the external urogenital orifice that they bound, the rima pudendi. The labia fuse above and below the rima pudendi to form dorsal and ventral commissures. The dorsal commissure is ventral to a dorsal plane through the pelvic symphysis. The ventral commissure is directed caudoventrally.
Observe the course of the female urethra by passing a flexible probe through it. It extends from the bladder caudodorsally over the cranial edge of the pelvic symphysis to the genital tract caudal to the vaginovestibular junction. It ends at the external urethral orifice on the urethral tubercle, which is dorsal to the rima pudendi at the level of the ischial arch.
LIVE DOG: Abdominal palpation is an art that takes considerable experience to develop. It is dependent on your knowledge of the topographical anatomy of abdominal organs. Not all organs are palpable, and some cannot be felt in all dogs. In the standing dog, grasp the caudal abdomen gently with one hand and palpate the bladder ventrally and the descending colon above it. In the female the nonpregnant uterus can sometimes be felt between them. As the uterus enlarges with advanced gestation, it will be felt in the ventral abdomen. Dorsal to the colon, lumbar and iliac lymph nodes that are enlarged from disease can be felt.
Stand over or beside the standing dog and palpate the two sides simultaneously, starting cranially at the costal arch and progressing caudally. The liver is not usually felt. On the left side the empty stomach is not palpable, but the full stomach will be felt. The spleen should be felt on the left behind the costal arch. The left kidney is deeper but usually palpable. Cranially on the right, no specific organ is palpable. If pain is elicited, the organs to be considered as a source of irritation include the liver, pancreas, pylorus, and right kidney. Sometimes the descending duodenum can be felt on the right. The right kidney is not usually felt. Remember its close relationship with the caudate process of the caudate lobe of the liver. The descending colon can be felt on the left. In the ventral midabdominal region, you should be able to feel the coils of small intestine slip through your fingers. The ileum and cecum are not usually palpable. Deep in the midabdominal region, you may feel mesenteric lymph nodes, but only if they are enlarged from disease.
In the male palpate the root of the penis. Feel the ischiocavernosus muscles covering the crura on either side of the bulbospongiosus muscle that covers the penile bulb. Feel the slightly compressed, firm body of the penis formed by the paired corpora cavernosa and the groove ventrally that contains the urethra and corpus spongiosum penis. Bend the body of the penis and note its flexibility. In normal canine mating, the male will step over the female with one hind limb and face in the opposite direction while still “locked” in copulation. The penis bends without twisting at the level of the penile body. Palpate the junction of the corpora cavernosa of the penis with the os penis. This is sometimes the site of blockage of the urethra with calculi. Palpate the length of the os penis and the two parts of the glans penis that cover it. Palpate the superficial inguinal lymph nodes in the skin fold that suspends the penis at the level of the bulbus glandis. These are normally flat and difficult to feel. Palpate the spermatic cord from the superficial inguinal ring to the testes. Palpate the testes and epididymis in the scrotum.
In the female open the vulva and observe the clitoral fossa. The urethral opening on its tubercle is dorsal to this at the level of the ischial arch and is not visible.
Gently extend the tail and observe the cutaneous zone of the anal canal. Find the openings of the paranal sinuses on either side of the cranial part of this zone. Feel the tense coccygeus and levator ani muscles. Press your finger into the ischiorectal fossa.
VESSELS AND NERVES OF THE PELVIC LIMB (TABLE 4-1)
Table 4-1
Vessels and Nerves of the Pelvic Limb
| Cranial Thigh Muscle | Vessels | Nerve |
| Extension of stifle: | Lateral circumflex femoral | Femoral |
| Quadriceps femoris | ||
| Medial Thigh Muscles | ||
| Adductors of pelvic limb: | Deep femoral | Obturator |
| Gracilis | Caudal femorals | |
| Adductor | ||
| Pectineus | ||
| Caudal Thigh Muscles | ||
| Flexors and extensors of stifle, extensors of hip: | Deep femoral | Sciatic |
| Biceps femoris | Caudal gluteal | |
| Semimembranosus | Caudal femorals | |
| Semitendinosus | ||
| Cranial Muscles of Crus | ||
| Flexors of tarsus: | Cranial tibial | Fibular |
| Cranial tibial | ||
| Fibularis longus | ||
| Extensor of digits: | ||
| Long digital extensor | ||
| Caudal Muscles of Crus | ||
| Rotator of stifle: | Popliteal | Tibial |
| Popliteus | Distal caudal femoral | |
| Extensor of tarsus: | ||
| Gastrocnemius | ||
| Flexors of digits: | ||
| Superficial digital flexorDeep digital flexors | ||
| Deep digital flexors |
The caudal gluteal artery (Figs. 4-38, 4-39, 4-55, 4-58) is the larger of the two terminal branches of the internal iliac artery. It arises opposite the sacroiliac joint and passes caudally across the greater ischiatic notch and over the ischiatic spine lateral to the coccygeus muscle, parallel to the internal pudendal artery. The branches of the caudal gluteal are the iliolumbar, cranial gluteal, lateral caudal, and dorsal perineal arteries (Fig. 4-55). The veins (Figs. 4-56, 4-57) will not be dissected. Observe the origin of the caudal gluteal artery on the medial aspect of the right ilium at the pelvic inlet. Pull the caudal gluteal artery away from the ilium and observe the iliolumbar branch coursing cranial to the wing of the ilium and the cranial gluteal branch coursing caudal to the wing of the ilium across the greater ischiatic notch (Fig. 4-55).
Make a skin incision on the medial surface of the right thigh to the stifle. Encircle the stifle and reflect the skin from the lateral pelvis, rump, and thigh.
Expose the insertion of the superficial gluteal deep to the proximal edge of the biceps femoris. Transect the insertion at this level. Reflect the proximal portion of the superficial gluteal to its origin. Transect the middle gluteal muscle 1 cm from the crest of the ilium. Start at the cranial border of the bone and detach the muscle from the gluteal surface.
The cranial gluteal artery and nerve (Figs. 4-55, 4-58, 4-59, 4-65, 4-66, 4-70) pass across the cranial part of the greater ischiatic notch of the ilium and between the middle and deep gluteal muscles, which they supply. The cranial gluteal nerve also continues into and innervates the tensor fasciae latae.
The iliolumbar artery (Figs. 4-38, 4-39, 4-55, 4-58, 4-59, 4-68) arises close to the origin of the caudal gluteal artery or directly from the internal iliac. It passes across the cranioventral border of the ilium and supplies the psoas minor, iliopsoas, sartorius, tensor fasciae latae, and middle gluteal muscles. On the lateral side, observe its terminal distribution to the deep surface of the cranial end of the middle gluteal.
Transect the biceps femoris midway between its origin and the stifle. Transect the semitendinosus 1 cm distal to the transection through the biceps. Turn both muscles toward their origins. The caudal gluteal artery lies on the ventrocranial side of the sacrotuberous ligament and in this location gives off several small branches to adjacent muscles: the lateral caudal artery to the tail and the dorsal perineal artery to the perineum. These need not be dissected.
Follow the caudal gluteal artery as it passes over the ischiatic spine with the sciatic nerve ventral to the sacrotuberous ligament (Fig. 4-59). Here the artery supplies the superficial and middle gluteals, the rotators of the hip, and the adductor muscle. It divides into several branches, which supply the biceps femoris and the semitendinosus and semimembranosus muscles. Turn the biceps femoris caudally to expose the caudal gluteal artery lying deep to it, close to the sacrotuberous ligament and ischiatic tuberosity.
External Iliac Artery and Primary Branches
The right external iliac artery (Figs. 4-28, 4-33, 4-37 through 4-39, 4-55, 4-58, 4-60) arises from the aorta on a level with the sixth and seventh lumbar vertebrae. It runs caudoventrally and is related laterally near its origin to the common iliac vein and the psoas minor muscle. Farther distally it lies on the iliopsoas muscle. The external iliac on passing through the abdominal wall becomes the femoral artery. The opening through which the external iliac artery passes is the vascular lacuna, located between the caudal border of the aponeurosis of the external abdominal oblique (inguinal ligament) and the pelvis (Fig. 2-79).
The deep femoral artery is the only branch of the external iliac artery and arises inside the abdomen near the vascular lacuna and courses caudally. Two vessels leave the ventral surface of the deep femoral artery within the abdomen by a short pudendoepigastric trunk. These are the external pudendal and caudal epigastric arteries. The external pudendal artery passes through the inguinal canal and has already been dissected.
The caudal epigastric artery (Figs. 4-33, 4-60) arises from the pudendoepigastric trunk and passes cranially on the dorsal surface of the rectus abdominis. It supplies the caudal half of the rectus abdominis and the ventral parts of the oblique and transverse muscles.
Expose the femoral artery and vein and the saphenous nerve in the femoral triangle. This triangle is bounded cranially by the sartorius, laterally by the vastus medialis and rectus femoris, and caudally by the pectineus and adductor.
After giving off the pudendoepigastric trunk, the deep femoral artery continues as the medial circumflex femoral artery (Figs. 4-55, 4-58, 4-60, 4-63, 4-64), which leaves the abdomen through the vascular lacuna. It continues caudally between the quadriceps femoris and pectineus muscles and enters the adductor. Transect the pectineus at its origin and reflect it. Transect the origin of the gracilis and reflect the muscle caudally. Transect the origin of the adductor. Spare the branches of the medial circumflex femoral artery and obturator nerve that enter its cranial aspect. Remove portions of the adductor muscle to follow the distribution of the medial circumflex femoral artery.
As the medial circumflex femoral artery approaches the large adductor muscle, it gives off a deep branch that descends distally between the adductor and vastus medialis muscles, both of which it supplies. Small branches of the medial circumflex femoral supply the obturator muscles and the hip joint capsule. The transverse branch passes caudally through the adductor muscle, which it supplies, and terminates in the semimembranosus muscle.
The femoral artery (Figs. 4-55, 4-58, 4-60 through 4-64) is the continuation of the external iliac artery beyond the level of the vascular lacuna. The branches of the femoral artery in the order that they arise are superficial circumflex iliac, lateral circumflex femoral, proximal caudal femoral, saphenous, descending genicular, and middle and distal caudal femoral.
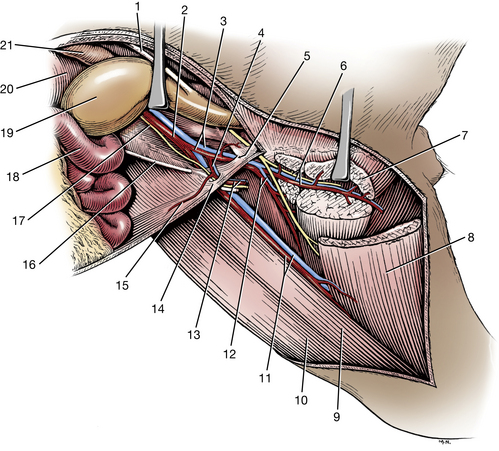
Fig. 4-60 Deep femoral artery, medial view, pectineus muscle removed, and adductor transected.
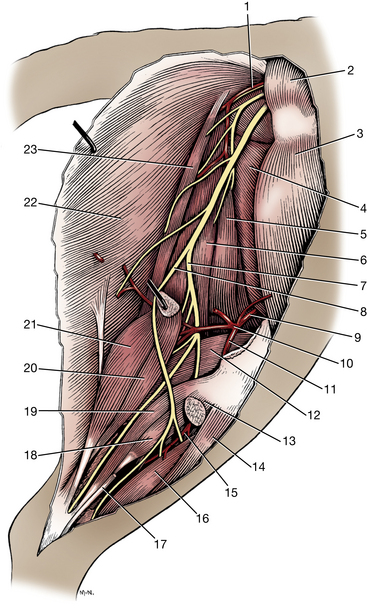
Fig. 4-61 Arteries and nerves of right thigh and crus, lateral view.
The superficial circumflex iliac artery (Fig.4-64) is a small branch that arises from the lateral side of the femoral artery near or with the lateral circumflex femoral artery. The superficial circumflex iliac artery courses cranially and supplies both parts of the sartorius, the tensor fasciae latae and the rectus femoris. It becomes superficial at the cranial ventral iliac spine of the tuber coxae. Transect both parts of the sartorius over the vessel and observe its branches.
The lateral circumflex femoral artery (Figs. 4-55, 4-58, 4-59, 4-64) is a large branch that passes between the rectus femoris and the vastus medialis. Although most of the vessel arborizes in the quadriceps, it also supplies the tensor fasciae latae, the superficial and middle gluteals, and the hip joint capsule.
The proximal caudal femoral artery (Figs. 4-55, 4-63) leaves the caudal surface of the femoral artery distal to the origin of the lateral circumflex femoral in the midthigh region.
It extends distocaudally over the pectineus and adductor muscles, which it supplies, and enters the deep surface of the gracilis.
Make a skin incision from the stifle to the claw of the second digit. Remove the skin as far distally as the metatarsal pad. Try to leave the subcutaneous vessels on the limb.
The saphenous artery (Figs. 4-55, 4-62 through 4-64), nerve, and medial saphenous vein continue distally between the converging borders of the caudal part of the sartorius and gracilis. Observe that the saphenous artery arises from the femoral artery, proximal to the stifle. The saphenous artery supplies the skin on the medial side of the stifle and terminates in a cranial and a caudal branch.
The cranial branch (Figs. 4-55, 4-63, 4-71) of the saphenous artery arises opposite the proximal end of the tibia, obliquely crosses the medial surface of the tibia, and passes distally on the cranial tibial muscle. It crosses the flexor surface of the tarsus with this muscle. At the proximal part of the metatarsus, it terminates as the dorsal common digital arteries.
The caudal branch (Figs. 4-55, 4-63, 4-73) of the saphenous artery arises at the proximal end of the tibia. It lies between the medial head of the gastrocnemius and the tibia. Distally, it is related to the flexors of the digits, and, with the tibial nerve, it crosses the medial plantar surface of the tarsus through the tarsal tunnel to enter the metatarsus. The vessel supplies branches to the tarsus and the deep structures of the proximal end of the metatarsus. In the metatarsus it supplies the paw by branches that give rise to the plantar common digital arteries. It also gives off deep branches that contribute to a deep plantar arch that is the source of plantar metatarsal arteries. These branches need not be dissected.
In some specimens the saphenous veins (Figs. 4-56, 4-57) may be congested enough to be identified. The medial saphenous vein is similar to the saphenous artery in its origin in the paw and termination in the femoral vein. The lateral saphenous vein has no comparable saphenous artery. It is formed by cranial and caudal branches in the leg that arise from venous arcades in the paw. It terminates in the distal caudal femoral vein. The cranial branch of the lateral saphenous vein is often used for venipuncture. It arises from an anastomosis with the cranial branch of the medial saphenous vein on the dorsal aspect of the tarsus and courses proximocaudally across the lateral surface of the leg.
After the saphenous artery arises from the femoral, the latter disappears lateral to the semimembranosus. Transect and turn the distal end of the semimembranosus craniomedially and trace the femoral artery to the gastrocnemius muscle.
The descending genicular artery (Figs. 4-55, 4-62, 4-64) arises from the femoral distal to the origin of the saphenous and supplies the medial surface of the stifle.
The middle caudal femoral artery (Figs. 4-55, 4-62, 4-64) arises distal to the descending genicular and saphenous arteries after the femoral artery passes lateral to the semimembranosus. It ramifies in the distal parts of the adductor and semimembranosus muscles.
The distal caudal femoral artery (Figs. 4-55, 4-61, 4-62) is a large vessel that arises from the caudal surface of the last centimeter of the femoral. The femoral is continued by the popliteal artery on entering the gastrocnemius. Reflect the insertions of the gracilis, semimembranosus, and semitendinosus to uncover the medial head of the gastrocnemius muscle. Transect the medial head of the gastrocnemius and reflect it. This will expose the distal caudal femoral artery and its branches, which supply the biceps femoris, the semimembranosus, the semitendinosus, the gastrocnemius, and the digital flexors.
The popliteal artery (Figs. 4-55, 4-61, 4-62), a continuation of the femoral artery, passes between the two heads of the gastrocnemius muscle, crosses the medial surface of the superficial digital flexor muscle, and courses over the flexor surface of the stifle and through the popliteal notch of the tibia. It inclines laterally under the popliteus muscle and perforates the lateral digital flexor to reach the interosseous space. The popliteal artery supplies the stifle, gastrocnemius, and popliteus muscles and terminates as cranial and caudal tibial arteries. The caudal tibial artery is a small vessel that leaves the caudal surface of the popliteal in the interosseous space. It need not be dissected.
Transect the popliteus where it covers the popliteal artery and follow the artery to the interosseous space.
The cranial tibial artery (Figs. 4-55, 4-61, 4-62, 4-71, 4-72) passes between the tibia and the fibula. Reflect the fascia on the cranial aspect of the stifle and leg where it serves for the insertion of the biceps femoris. Separate the cranial tibial and long digital extensor muscles throughout their length. Observe the cranial tibial artery between these two muscles. Transect the fibularis longus muscle at its origin and reflect it to expose the cranial tibial artery emerging from the interosseous space between the tibia and fibula. It supplies the fibularis longus, long digital extensor, and cranial tibial muscles. The termination of the artery will be dissected with the fibular nerves.
The lumbosacral plexus (Figs. 4-58, 4-65, 4-66) is diffuse and consists of the ventral branches of the lumbar and sacral spinal nerves. Of the nerves that arise from this plexus, the cranial and caudal iliohypogastric, the ilioinguinal, the lateral cutaneous femoral, and the genitofemoral have been dissected. The remainder will be dissected in the order of their accessibility.
1. The obturator nerve (Figs. 4-58, 4-65 through 4-69) arises from the fourth, fifth, and sixth lumbar spinal nerves. It is formed within the caudomedial portion of the iliopsoas muscle. It leaves the muscle dorsomedially, runs caudoventrally along the body of the ilium, penetrates the medial side of the levator ani muscle, and leaves the pelvis by passing through the cranial part of the obturator foramen. It supplies the adductor muscles of the limb: the external obturator, the pectineus, the gracilis, and the adductor. Locate this nerve on the medial side of the right ilium. Find it as it emerges ventrally from the obturator foramen and arborizes in the adductor muscles with the branches of the medial circumflex femoral artery.
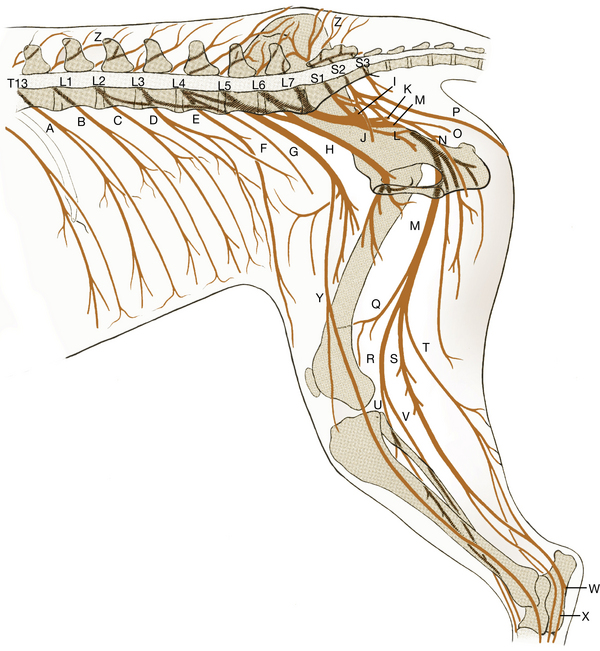
Fig. 4-66 Schematic medial view of right lumbar and sacral nerves.
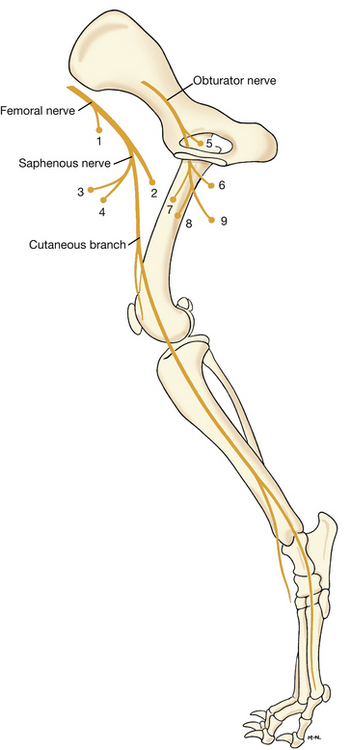
Fig. 4-67 Distribution of saphenous, femoral, and obturator nerves of right pelvic limb, schematic medial aspect.
Muscles innervated by numbered nerves
Femoral nerve
2. The femoral nerve (Figs. 4-58, 4-65 through 4-67, 4-69) arises primarily from the fourth, fifth, and occasionally the sixth lumbar spinal nerves. Find the femoral nerve with the lateral circumflex femoral artery. Observe its emergence from the iliopsoas muscle. Within the iliopsoas the saphenous nerve arises from the cranial side of the femoral nerve. The saphenous or femoral innervates the sartorius muscle. The cutaneous portion of the saphenous nerve supplies the skin on the medial side of the thigh, the stifle, leg, tarsus, and remainder of the paw. Follow this nerve as far distally as the tarsus.
The femoral nerve supplies branches to the iliopsoas muscle. It enters the quadriceps muscle between the rectus femoris and vastus medialis and supplies all four heads of the quadriceps. It is responsible for stifle extension to support weight in the pelvic limb.
In the right ischiorectal fossa, identify the coccygeus muscle. Reflect the already transected superficial and middle gluteals to uncover the greater ischiatic notch. Transect and reflect the sacral attachment of the sacrotuberous ligament. This exposes the caudal gluteal artery and the sciatic nerve. Deep to these are the internal pudendal artery and pudendal nerve and the ventral branches of the sacral nerves. These ventral branches emerge from the two pelvic sacral foramina and the sacrocaudal intervertebral foramen to form the sacral plexus.
3. The pudendal nerve (Figs. 4-65, 4-66, 4-68, 4-69) arises from all three sacral nerves. It passes caudolaterally, where it lies lateral to the levator ani and coccygeus muscles, medial to the superficial gluteal muscle and dorsal to the internal pudendal vessels. It appears superficially in the ischiorectal fossa after emerging from the medial side of the superficial gluteal muscle and courses caudomedially toward the pelvic symphysis at the ischial arch. The following branches arise from the pudendal nerve:
a. The caudal rectal nerve may arise from sacral nerves or may leave the pudendal nerve at the caudal border of the levator ani muscle. It innervates the external anal sphincter.
b. The perineal nerves arise from the dorsal surface of the pudendal nerve. They supply the skin of the anus and the perineum and continue to the scrotum or labium. Short nerves from the pudendal or perineal nerves supply the muscles of the penis or the vestibule and vulva.
c. The dorsal nerve of the penis in the male (or of the clitoris in the female) curves around the ischial arch and reaches the dorsal surface of the penis, where it courses cranially. It continues through the glans penis and ends in the skin covering the apex of the penis. It provides sensory nerves to the skin of the glans. In the female the smaller dorsal nerve of the clitoris runs ventrally to the ventral commissure of the vulva, where it terminates in the clitoris.
4. The caudal cutaneous femoral nerve (Figs. 4-65, 4-66, 4-68, 4-69) arises from the sacral plexus and is united to the pudendal for most of its intrapelvic course. The caudal cutaneous femoral nerve follows the caudal gluteal artery to the level of the ischiatic tuberosity, where it becomes superficial near the attachment of the sacrotuberous ligament and terminates in the skin on the proximal caudal half of the thigh.
The ventral branches of the sixth and seventh lumbar spinal nerves and the first two sacral spinal nerves unite to form a lumbosacral trunk adjacent to the greater ischiatic notch. The nerves that arise from this trunk are the caudal gluteal, cranial gluteal, and sciatic.
5. The caudal gluteal nerve (Figs. 4-58, 4-59, 4-65, 4-66) passes over the ischiatic notch medial to the middle gluteal muscle and enters the medial surface of the superficial gluteal muscle. It is the sole innervation to the superficial gluteal. It has a variable origin from the seventh lumbar and first two sacral spinal nerves.
6. The cranial gluteal nerve (Figs. 4-58, 4-59, 4-65, 4-66, 4-68 through 4-70) passes over the greater ischiatic notch, crosses the lateral surface of the ilium at the origin of the deep gluteal muscle, and innervates the middle and deep gluteal muscles and the tensor fasciae latae. It arises from the ventral branches of the sixth and seventh lumbar and first sacral spinal nerves. It was dissected with the cranial gluteal artery.
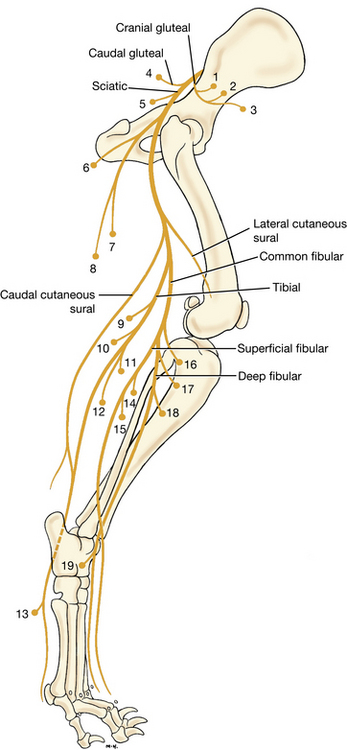
Fig. 4-70 Distribution of cranial and caudal gluteal nerves and sciatic nerve of right pelvic limb, schematic lateral view.
Muscles innervated by numbered nerves
Cranial gluteal nerve
7. The sciatic nerve (Figs. 4-58, 4-59, 4-61, 4-62, 4-65, 4-66, 4-68 through 4-70) arises from the last two lumbar and first two sacral spinal nerves. Isolate the nerve as it emerges from the lumbosacral trunk that passes over the greater ischiatic notch. Small branches leave within the pelvis to supply the internal obturator, gemelli, and quadratus femoris muscles. Do not dissect these branches. The sciatic nerve passes caudally over the hip medial to the greater trochanter, craniomedial to the tuber ischium and then distally, caudal to the femur on the lateral side of the adductor muscle. A branch leaves the nerve at the level of the hip and innervates the biceps femoris, semitendinosus, and semimembranosus muscles.
There are lateral and caudal cutaneous sural nerves (Figs. 4-59, 4-62, 4-66, 4-68, 4-70) that arise from the fibular and tibial components, respectively, of the sciatic nerve in the thigh and supply the skin on the lateral and caudal surfaces of the crus. The sciatic nerve terminates in the thigh as the common fibular and tibial nerves.
The common fibular nerve arises primarily from L6 and L7 spinal nerve ventral branches (Figs. 4-61, 4-62, 4-66, 4-68, 4-70). It is smaller than the tibial nerve and passes laterally, deep to the thin terminal part of the biceps femoris muscle. It crosses the lateral head of the gastrocnemius muscle and the fibula and passes between the lateral digital flexor muscle caudally and the fibularis longus muscle cranially to enter the muscles on the cranial side of the crus. Here the common fibular nerve divides into superficial and deep fibular nerves. These nerves innervate the flexor muscles of the tarsus and extensor muscles of the digits. These include the cranial tibial, fibularis longus, and long digital extensor muscles.
The superficial fibular nerve (Figs. 4-70, 4-71) leaves the lateral portion of the parent nerve below the stifle, where it lies between the lateral digital flexor caudally and the fibularis longus cranially. Expose the nerve and trace it as it curves distally, deep to the distal part of the fibularis longus. At the beginning of the distal third of the crus, it becomes subcutaneous and accompanies the cranial branch of the saphenous artery. Distal to the tarsus the superficial fibular nerve forms dorsal common digital nerves that innervate the paw (Fig. 4-71). The deep fibular nerve (Figs. 4-70, 4-71) arises from the cranial surface of the parent nerve. It enters the muscles on the cranial part of the crus and courses distally in association with the cranial tibial artery. In the proximal half of the tarsus, they both lie in a groove formed by the tendons of the long digital extensor muscle laterally and by the cranial tibial muscle medially. Expose them by cutting the extensor retinaculum. At the tarsus the nerve divides into dorsal metatarsal nerves that continue distally to innervate the dorsal aspect of the paw (Fig. 4-71) along with the dorsal common digital nerves from the superficial fibular nerve. Follow the deep fibular nerve as the termination of the cranial tibial artery is now dissected.
The cranial tibial artery is continued opposite the talocrural joint as the dorsal pedal artery (Figs. 4-55, 4-71, 4-73). Branches supply the tarsus, and the dorsal pedal artery terminates in the arcuate artery at the level of the tarsometatarsal joint. The arcuate artery runs transversely laterally through the ligamentous tissue at the proximal end of the metatarsus. It gives off dorsal metatarsal arteries that run distally to supply the paw dorsally. These need not be dissected.
A perforating branch (Figs. 4-71 through 4-73) leaves dorsal metatarsal artery II, a branch of the arcuate artery, and courses distally in the space between the second and third metatarsal bones. This perforating branch passes from the dorsal to the plantar surface of the metatarsus in the proximal end of this space. It anastomoses with the branches of the caudal branch of the saphenous artery to contribute to the plantar metatarsal arteries that supply the paw. This is the largest source of blood to the digits of the paw. Expose the arcuate artery and the perforating branch. Remove the proximal half of the interosseous muscle covering the plantar side of the second metatarsal bone to observe the perforating metatarsal branch that emerges between the second and third metatarsal bones (Fig. 4-73).
The tibial nerve arises primarily from L7 and S1 spinal nerve ventral branches and is the caudal portion of the sciatic nerve (Figs. 4-61, 4-62, 4-66, 4-68, 4-70, 4-73). It separates from the common peroneal nerve in the thigh. At the stifle it passes between the two heads of the gastrocnemius muscle. The tibial nerve supplies the muscles caudal to the tibia and fibula, which include the extensors of the tarsus and flexors of the digits, and sends branches to the stifle. It innervates both heads of the gastrocnemius muscle and the superficial digital flexor, the popliteus, and both deep digital flexor muscles. The tibial nerve is continued beyond these branches on the lateral digital flexor muscle. It emerges from the deep surface of the medial head of the gastrocnemius and continues distally along the medial side of the caudal surface of the tibia. Proximal to the tarsocrural joint, the tibial nerve divides into the medial and lateral plantar nerves. These cross the tarsus medial to the tuber calcanei through the tarsal tunnel and terminate as the plantar common digital and plantar metatarsal nerves, respectively, which are sensory to the plantar surface of the paw. The tarsal tunnel is formed by the sustentaculum tali dorsally, the calcanean tuber laterally, and the flexor retinaculum on the plantar side. It contains the tendon of the lateral digital flexor with its synovial sheath, the medial and lateral plantar nerves, and the caudal branch of the saphenous artery.
Blood supply and innervation of the digits of the pelvic limb are summarized in Table 4-2.
LIVE DOG
Place the palm of your hand over the cranial thigh with your fingers on the medial side and palpate the borders of the femoral triangle. Feel the pulse in the femoral artery. This is the most common site to determine the pulse rate and quality in a physical examination. The pulse can also be felt at two other sites in the pelvic limb. One is where the cranial branch of the saphenous artery crosses the medial side of the middle third of the tibia. Both the bone and the artery are subcutaneous here. The other is from the dorsal pedal artery, where it crosses the dorsal surface of the tarsus.
Trace the course of the sciatic nerve and appreciate where the nerve is close to bones that can fracture and injure it or close to the sites of intramuscular injections. The common fibular nerve is palpable where it crosses the proximal end of the fibula. Feel the head of the fibula and stroke the skin from proximal to distal to roll the nerve on the bone here. The tibial nerve can be felt proximal to the tarsus between the skin layers cranial to the common calcanean tendon. It is accompanied by saphenous vessels here.
Study Fig. 4-74 and identify the autonomous zones of the nerves in the pelvic limb on the live dog.
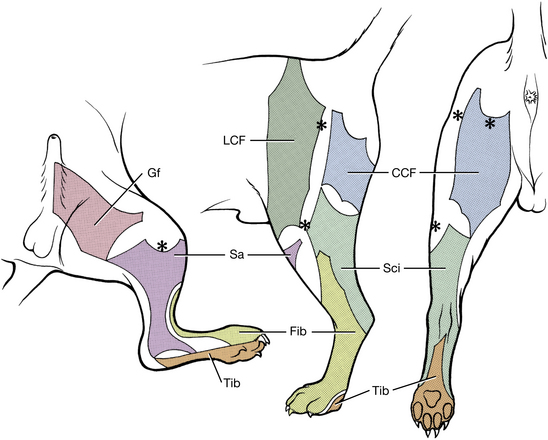
Fig. 4-74 Autonomous zones of cutaneous innervation of the pelvic limb. Medial, lateral, and caudal aspects. CCF, caudal cutaneous femoral; Gf, genitofemoral; LCF, lateral cutaneous femoral; fibular; Sa, saphenous; Sci, sciatic; Tib, tibial. Asterisks indicate palpable bony landmarks—medial and lateral tibial condyles, greater trochanter, and lateral end of tuber ischiadicum (from R. L. Kitchell). The sciatic nerve autonomous zone is for lesions proximal to the greater trochanter and includes the zones for the fibular and tibial nerves. For sciatic nerve lesions caudal to the femur, the autonomous zone varies, depending on how many of its cutaneous branches are affected.
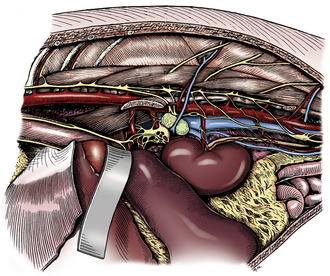 CHAPTER 4
CHAPTER 4