Physical and Psychological Evaluation
Before starting any dental procedure, the doctor or hygienist must determine whether the patient can tolerate the planned dental procedure in relative safety. If this is not the case, the specific treatment modifications necessary to decrease the risk presented by the patient must be determined. This is especially important whenever drugs are to be administered during treatment, such as analgesics, sedatives, inhalation sedation (N2O-O2) agents, and local anesthetics. Before administering local anesthetics, the administrator must determine the relative risk presented by the patient. This is important because local anesthetics, like all drugs, exert actions on many parts of the body (see Chapter 2). Actions of local anesthetics include depressant effects on excitable membranes (e.g., central nervous system [CNS], cardiovascular system [CVS]). Because local anesthetics undergo biotransformation primarily in the liver (amides) or blood (esters) the functional status of these systems must be determined before drug administration. Because a small percentage of all injected local anesthetic is excreted in an active (unmetabolized) form in the kidneys, kidney function must be evaluated. Other questions should be asked: Has the patient ever received a local anesthetic for medical or dental care? If so, were any adverse reactions observed?
Most undesirable reactions to local anesthetics are produced not by the drugs themselves but as a response to the act of drug administration.1 These reactions are commonly psychogenic and have the potential to be life threatening if not recognized and managed promptly. The two most commonly occurring psychogenic reactions are vasodepressor syncope and hyperventilation. Other psychogenically induced reactions noted as a response to local anesthetic administration may include tonic–clonic convulsions, bronchospasm, and angina pectoris.
However, local anesthetics are not absolutely innocuous drugs, nor is the act of local anesthetic administration entirely benign. The doctor must seek to uncover as much information as possible concerning the patient’s physical and mental status before administration of a local anesthetic. Fortunately the means to do so exist in the form of the medical history questionnaire, the dialogue history, and the physical examination of the patient. Adequate use of these tools can lead to an accurate determination of a patient’s physical status and can prevent up to 90% of all life-threatening medical emergencies in dental practice.2
Goals of Physical and Psychological Evaluation
In the following discussion, a comprehensive but easy-to-use program of physical evaluation is described.3,4 Used as recommended, it allows the dental team to accurately determine any potential risk presented by the patient before the start of treatment. This system can be used to meet the following goals:
1. To determine the patient’s ability to tolerate physically the stresses involved in the planned dental treatment
2. To determine the patient’s ability to tolerate psychologically the stresses involved in the planned dental treatment
3. To determine whether treatment modification is indicated to enable the patient to better tolerate the stresses of dental treatment
4. To determine whether the use of psychosedation is indicated
5. To determine which technique of sedation is most appropriate for the patient
6. To determine whether contraindications exist to (a) the planned dental treatment or (b) any of the drugs to be used.
The first two goals involve the patient’s ability to tolerate the stress involved in the planned dental care. Stress may be of a physiologic or psychological nature. Patients with underlying medical problems may be less able to tolerate the usual levels of stress associated with various types of dental care. These patients are more likely to experience an acute exacerbation of their underlying medical problem(s) during periods of increased stress. Such disease processes include angina pectoris, seizure disorders, asthma, and sickle cell disease. Although most of these patients will be able to tolerate the planned dental care in relative safety, it is the obligation of the dental team to determine whether a problem does exist and the severity of the problem and to decide how it might impact the proposed dental treatment plan.
Excessive stress can prove detrimental to the non–medically compromised (i.e., “healthy”) patient. Fear, anxiety, and acute pain produce abrupt changes in the homeostasis of the body that may prove detrimental. Many “healthy” patients suffer from fear-related emergencies, including hyperventilation and vasodepressor syncope (also known as vasovagal syncope and “fainting”).
The third goal is to determine whether the usual treatment regimen for a patient should be modified to enable the patient to better tolerate the stress of treatment. In some cases, a healthy patient will be psychologically unable to tolerate the planned treatment. Treatment may be modified to minimize the stress faced by this patient. The medically compromised patient will also benefit from treatment modification aimed at minimizing stress. The stress reduction protocols (SRPs) outlined in this chapter are designed to aid the dentist and the hygienist in minimizing treatment-related stress for both healthy and medically compromised patients.
When it is believed that the patient will require some assistance in coping with his or her dental treatment, the use of psychosedation should be considered. The last three goals involve determination of the need for use of psychosedation, selection of the most appropriate technique, and selection of the most appropriate drug(s) for patient management.
Physical Evaluation
The term physical evaluation is used to describe the steps involved in fulfilling the aforementioned goals. Physical evaluation in dentistry consists of the following three components:
With the information (database) collected from these three steps, the dentist and the hygienist will be better able to (1) determine the physical and psychological status of the patient (establish a risk factor classification for the patient); (2) seek medical consultation, if indicated; and (3) appropriately modify the planned dental treatment, if indicated. Each of the three steps in the evaluation process is discussed in general terms, with specific emphasis placed on its importance in the evaluation of the patient for whom local anesthesia is to be administered.
Medical History Questionnaire
The use of a written, patient-completed medical history questionnaire is a moral and legal necessity in the practice of both medicine and dentistry. Such questionnaires provide the dentist and the hygienist with valuable information about the physical and in some cases the psychological condition of the prospective patient.
Many types of medical history questionnaires are available; however, most are simply modifications of two basic types: the “short” form and the “long” form. The short form medical history questionnaire provides basic medical history information and is best suited for use by a dentist or hygienist with considerable clinical experience in physical evaluation. When using the short-form history, the dentist or hygienist must have a firm grasp of the appropriate dialogue history required to aid in determination of the relative risk presented by the patient. The dentist or the hygienist should be experienced in the use of techniques of physical evaluation and interpretation of findings. Unfortunately, most dentist offices use the short form or a modification of it primarily as a convenience for their patient and themselves. The long form, on the other hand, results in a more detailed database concerning the physical condition of the prospective patient. It is used most often in teaching situations and represents a more ideal instrument for teaching physical evaluation.
In recent years, computer-generated medical history questionnaires have been developed.5 These questionnaires permit patients to enter their responses to questions electronically on a computer. Whenever a positive response is given, the computer asks additional questions related to the positive response. In effect, the computer asks the questions called for in the dialogue history.
Any medical history questionnaire can prove to be extremely valuable or entirely worthless. The ultimate value of the questionnaire resides in the ability of the dentist or hygienist to interpret the significance of the answers and to elicit additional information through physical examination and dialogue history.
In this sixth edition of Local Anesthesia, the prototypical adult health history questionnaire that has been developed by the University of the Pacific (UOP) School of Dentistry in conjunction with MetLife has been included (Fig. 10-1).6 Figure 10-2 is an example of a pediatric medical history questionnaire.
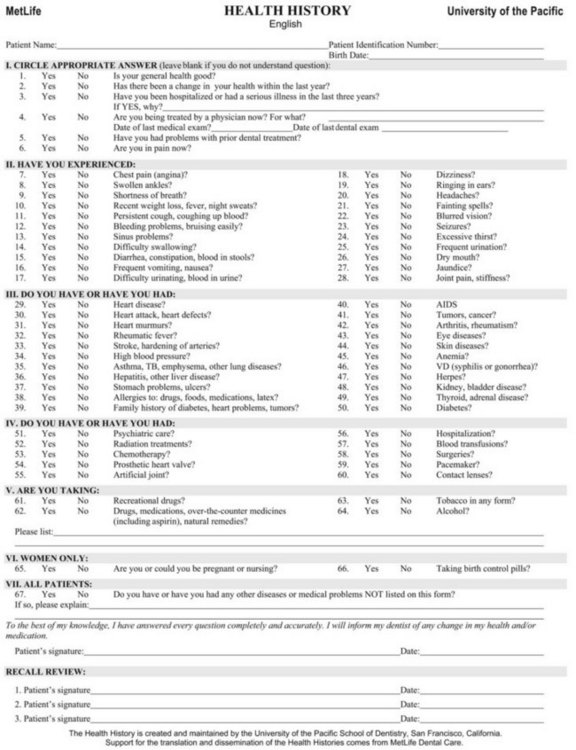
Figure 10-1 Adult health history questionnaire. (Reprinted with permission from University of the Pacific Arthur A. Dugoni School of Dentistry, San Francisco.)
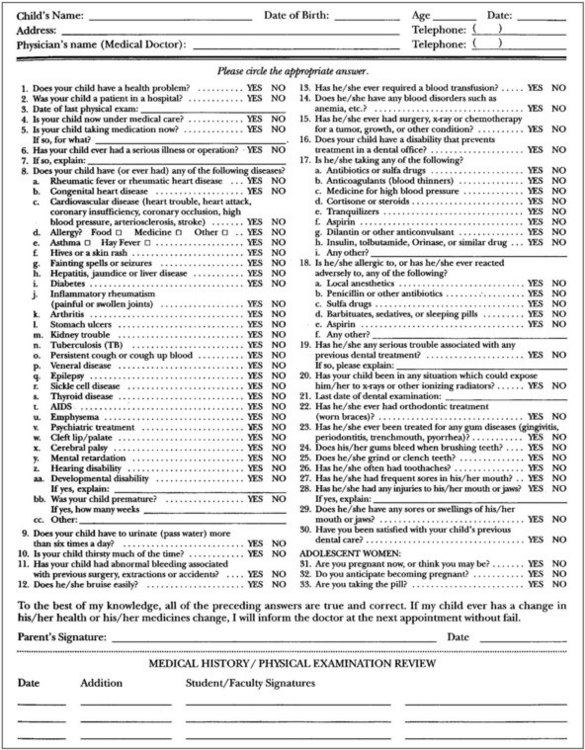
Figure 10-2 Pediatric medical history questionnaire. (From Malamed SF: Medical emergencies in the dental office, ed 6, St Louis, 2007, Mosby.)
This health history has been translated into 36 different languages, constituting the languages spoken by 95% of the persons on this planet. The cost of the translation was supported by several organizations including the California Dental Association, but most extensively by MetLife Dental. The health history (see Fig. 10-1), translations of the health history (Fig. 10-3), the interview sheet (Fig. 10-4), the medical consultation form (Fig. 10-5), and protocols for the dental management of medically complex patients may be found on the University of the Pacific Website at www.dental.pacific.edu under “Dental Professionals” and then under “Health History Forms.” Protocols for the management of medically complex patients can be found at the same Website under “Pacific Dental Management Protocols.” Translations of the medical history form can be found at www.metdental.com under “Multilanguage Medical Health History Forms Available.”
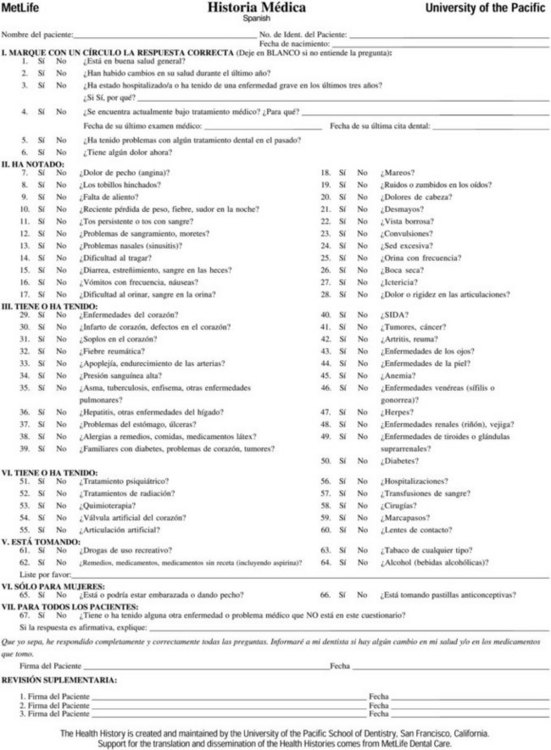
Figure 10-3 Spanish health history questionnaire. (Reprinted with permission from University of the Pacific Arthur A. Dugoni School of Dentistry, San Francisco.)
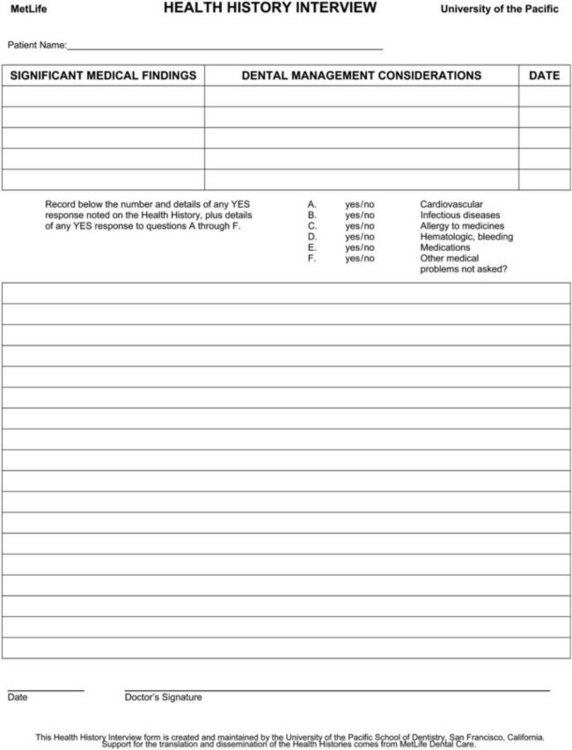
Figure 10-4 Health history interview sheet. (Reprinted with permission from University of the Pacific Arthur A. Dugoni School of Dentistry, San Francisco.)
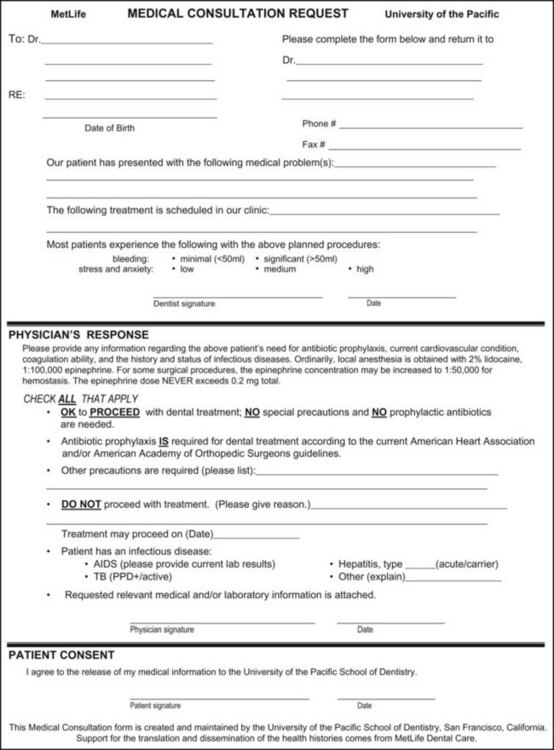
Figure 10-5 Medical consultation form. (Reprinted with permission from University of the Pacific Arthur A. Dugoni School of Dentistry, San Francisco.)
The health history has been translated while keeping the same question numbering sequence. Thus a dentist who speaks English and is caring for a patient who does not can ask the patient to complete the health history in his or her own language. The dentist then compares the English health history with the patient’s translated health history, scanning the translated version for YES responses. When a YES is found, the dentist is able to look at the question number and match it to the question number on the English version. For example, the dentist would know that a YES response to question No. 34 on the non-English version is the same as this response to question No. 34 on the English version, which relates to high blood pressure (HBP). For that matter, a Mandarin Chinese–speaking dentist could use the multilanguage health history with an English-speaking patient and have the same cross-referenced information. A dentist who speaks Spanish could use the multilanguage health history with a patient who speaks French. With the uniform health history question sequence, these health history translations can serve patients and dentists all around the world.
The health history is divided into sections related to signs and symptoms (“Have you experienced?”), diagnosed diseases (“Do you have or have you had?”), medical treatments (including drugs and other physiologically active compounds), and several other questions.
Although both long- and short-form medical history questionnaires are valuable in determining a patient’s physical condition, one criticism of most available health history questionnaires is the absence of questions related to the patient’s attitudes toward dentistry. It is recommended therefore that one or more questions be included that relate to this all-important subject:
Question Nos. 5 and 6 on the UOP medical history questionnaire address these points.
Following is the UOP medical history questionnaire with a discussion of the significance of each point.
I Circle Appropriate Answer: (Leave blank if you do not understand the question.)
1 Is Your General Health Good?
Comment: General survey questions seek patients’ general impression of their health. Studies have demonstrated that a YES response to this question does not necessarily correlate with the patient’s actual state of health.7
2 Has There Been a Change in Your Health Within the Last Year?
3. Have You Been Hospitalized or Had a Serious Illness in the Last 3 Years?
4 Are You Being Treated by a Physician Now? For What?
Comment: Question Nos. 2, 3, and 4 seek information regarding recent changes in the patient’s physical condition. In all instances of a positive response, an in-depth dialogue history must ensue to determine the precise nature of the change in health status, the type of surgical procedure or illness, and the names of any medications the patient may now be taking to help manage the problem.
5 Have You Had Problems With Prior Dental Treatment?
Comment: Many adults are reluctant to verbally admit to the dentist, hygienist, or assistant their fears about treatment, for fear of being labeled a “baby.” This is especially true of young men in their late teens or early twenties; they attempt to “take it like a man” or “grin and bear it” rather than admit their fears. Because the most common fear mentioned by dental patients is fear of injection (the “shot,” in their words), all too often, such macho behavior results in an episode of vasodepressor syncope. Whereas many such patients will not offer verbal admissions of fear, many of these same patients will volunteer this information in writing.
6 Are You in Pain Now?
Comment: The primary aim of this question is related to the need for immediate dental care. Its purpose is to determine what prompted the patient to seek dental care. If pain is present, the dentist may need to treat the patient immediately on an emergency basis, whereas in the more normal situation, treatment can be delayed until future visits. This may affect the use of local anesthesia, in that effective pain control can be more difficult to achieve in the presence of infection and chronic, albeit, now acute, pain in the fearful patient.
II Have You Experienced
7 Chest Pain (Angina)?
Comment: A history of angina (defined, in part, as chest pain brought on by exertion and alleviated by rest) usually indicates the presence of coronary artery disease with attendant ischemia of the myocardium. The risk factor for the typical patient with stable angina is ASA 3 (American Society of Anesthesiologists’ [ASA] physical status classification system).* In the presence of dental fears, sedation is absolutely indicated in the anginal patient. Inhalation sedation with N2O-O2 is preferred. Effective pain control—local anesthesia with vasoconstrictor included—is absolutely indicated. Patients with unstable or recent-onset angina represent ASA 4 risks.
8 Swollen Ankles?
Comment: Swollen ankles (pitting edema or dependent edema) indicate possible heart failure (HF). However, varicose veins, pregnancy, and renal dysfunction are other causes of ankle edema. Healthy persons who stand on their feet for long periods (e.g., mail carriers, dental staff members) may develop ankle edema that is not life threatening, merely esthetically unpleasing.
9 Shortness of Breath?
Comment: Although the patient may respond negatively to specific questions (questions No. 29 to No. 35 in Section III) regarding the presence of various heart and lung disorders (e.g., angina, HF, pulmonary emphysema), clinical signs and symptoms of heart or lung disease may be evident. A positive response to this question does not always indicate that the patient suffers such a disease. To more accurately determine the patient’s status before the start of dental care, further evaluation is suggested.
10 Recent Weight Loss, Fever, Night Sweats?
Comment: The question refers primarily to an unexpected gain or loss of weight, not to intentional weight loss (e.g., dieting). Unexpected weight change may indicate HF, hypothyroidism (increased weight), hyperthyroidism, widespread carcinoma, uncontrolled diabetes mellitus (weight loss), or a number of other disorders. The presence of fever and/or night sweats should be pursued to determine whether they are innocent or perhaps clues to the presence of a more significant problem, such as tuberculosis.
11 Persistent Cough, Coughing Up Blood?
Comment: A positive response mandates an in-depth dialogue history to determine the cause of the persistent cough or hemoptysis (blood-tinged sputum). The most common causes of hemoptysis are bronchitis and bronchiectasis, neoplasms, and tuberculosis.
A chronic cough can indicate active tuberculosis or other chronic respiratory disorders, such as chronic bronchitis. Cough associated with an upper respiratory infection confers an ASA 2 classification on the patient, whereas chronic bronchitis in a patient who has smoked more than one pack of cigarettes daily for many years may indicate chronic lung disease and confer on the patient an ASA 3 risk.
12 Bleeding Problems, Bruising Easily?
Comment: Bleeding disorders, such as hemophilia, are associated with prolonged bleeding or frequent bruising and can lead to modification of certain forms of dental therapy (e.g., surgery, technique of local anesthetic administration, venipuncture) and therefore must be made known to the dentist before treatment is begun.
Before a needle is inserted into the vascular soft tissues of the oral cavity, it should be determined whether the patient is at risk of excessive bleeding. In the presence of coagulopathies or other bleeding disorders, injection techniques with a greater incidence of positive aspiration should be avoided, if possible, in favor of supraperiosteal, periodontal ligament (PDL), intraosseous (IO), or other techniques less likely to produce bleeding. Techniques that might be avoided when bleeding disorders are present include the maxillary (V2) nerve block (high tuberosity approach), the posterior superior alveolar nerve block (PSA), the inferior alveolar nerve block (IANB), and probably both the Gow-Gates and the Akinosi-Vazirani mandibular nerve blocks. Although the latter two techniques have relatively low positive aspiration rates, bleeding following their administration is likely to occur deep in the tissues and therefore may be more difficult to manage. Modifications should be listed in the patient’s chart.
13 Sinus Problems?
Comment: Sinus problems can indicate the presence of an allergy (ASA 2), which should be pursued in the dialogue history, or an upper respiratory tract infection (URI) (ASA 2), such as a common cold. The patient may experience some respiratory distress when placed in a supine position; distress may also be present if a rubber dam is used. Specific treatment modifications—postponing treatment until the patient is able to breathe more comfortably, limiting the degree of recline in the dental chair, and foregoing use of a rubber dam—are advisable.
15 Diarrhea, Constipation, Blood in Stools?
Comment: This is an evaluation to determine whether gastrointestinal (GI) problems are present, many of which require patients to be medicated. Causes of blood in feces can range from benign, self-limiting events to serious life-threatening disease. Common causes include anal fissures, aspirin-containing drugs, bleeding disorders, esophageal varices, foreign body trauma, hemorrhoids, neoplasms, use of orally administered steroids, the presence of intestinal polyps, and thrombocytopenia.
16 Frequent Vomiting, Nausea?
Comment: A multitude of causes can lead to nausea and vomiting. Medications, however, are among the most common causes of nausea and vomiting.8-10 Opiates, digitalis, levodopa, and many cancer drugs act on the chemoreceptor trigger zone in the area postrema to induce vomiting. Drugs that frequently induce nausea include nonsteroidal anti-inflammatory drugs (NSAIDs), erythromycin, cardiac antidysrhythmics, antihypertensive drugs, diuretics, oral antidiabetic agents, oral contraceptives, and many GI drugs, such as sulfasalazine.8-10
GI and systemic infections, viral and bacterial, are the second most common cause of nausea and vomiting.
18 Dizziness?
Comment: A positive response may indicate chronic postural (orthostatic) hypotension, symptomatic hypotension or anemia, or transient ischemic attack (TIA), a form of pre-stroke. In addition, patients with certain types of seizure disorders, such as the “drop attack,” may report fainting or dizzy spells. The dentist may be advised to perform further evaluation, including a consultation with the patient’s primary care physician. A transient ischemic attack represents an ASA 3 risk, whereas chronic postural hypotension normally represents an ASA 2 or 3 risk.
19 Ringing in Ears?
Comment: Tinnitus (an auditory sensation in the absence of sound heard in one or both ears, such as ringing, buzzing, hissing, or clicking) is a common side effect of certain drugs including salicylates, indomethacin, propranolol, levodopa, aminophylline, and caffeine. It may be seen with multiple sclerosis, tumor, and ischemic infarction.
20 Headaches?
Comment: The presence of headache should be evaluated to determine the cause. Common causes include chronic daily headaches, cluster headaches, migraine headaches, and tension-type headaches. If necessary, consultation with the patient’s primary care physician is warranted. Determine the drug(s) used by the patient to manage his or her symptoms, because many of these agents can have an effect on the clotting of blood that could influence choice of local anesthetic technique (e.g., avoidance of those with a higher positive aspiration rate).
21 Fainting Spells?
Comment: Fainting (vasodepressor syncope) is the most common medical emergency in dentistry. It is most likely to occur during administration of a local anesthetic as a result of needle phobia (trypanophobia11). Prior recognition of needle phobia can usually result in prevention of the syncopal episode.
22 Blurred Vision?
Comment: Blurred vision is an increasingly common finding as patients age. Leading causes of blurred vision and blindness include glaucoma, diabetic retinopathy, and macular degeneration. Double vision, or diplopia, usually results from extraocular muscle imbalance, the cause of which must be sought. Common causes include damage to third, fourth, or sixth cranial nerves secondary to myasthenia gravis, vascular disturbance, and intracranial tumor.
23 Seizures?
Comment: Seizures are common emergencies in the dental environment. The most likely candidate to have a seizure is the epileptic patient. Even epileptics who are well controlled with antiepileptic drugs may suffer seizures in stressful situations, such as might occur in the dental office. The dentist must determine the type of seizure, the frequency of occurrence, and the drug(s) used to prevent the seizure before starting dental treatment. Treatment modification using SRPs (discussed later in this chapter) is desirable for patients with known seizure disorders. Sedation is highly recommended in the fearful epileptic dental patient as a means of preventing a seizure from developing during treatment. Epileptics whose seizures are under control (occur infrequently) are ASA 2 risks; those with more frequent seizures represent ASA 3 or 4 risk. A classic overdose of local anesthetic manifests as tonic–clonic seizure activity.
27 Jaundice?
Comment: Jaundice, or yellowness of skin, the whites of the eyes, and mucous membranes, is due to deposition of bile pigment resulting from an excess of bilirubin in the blood (hyperbilirubinemia). It is frequently caused by obstruction of bile ducts, excessive destruction of red blood cells (hemolysis), or disturbances in the functioning of liver cells. Jaundice is a sign that might be indicative of a benign problem, such as a gallstone obstructing the common bile duct, or it may be due to pancreatic carcinoma involving the opening of the common bile duct into the duodenum. Because amide local anesthetics undergo primary biotransformation in the liver, the presence of significant hepatic dysfunction (e.g., ASA 4) may represent a relative or absolute contraindication to administration of these drugs. Articaine HCl, which undergoes biotransformation both in the liver and in the blood (plasma cholinesterase), is preferred in these patients because it has an elimination half-life of 27 minutes (vs. 90 minutes for most other amide local anesthetics).
28 Joint Pain, Stiffness?
Comment: A history of joint pain and stiffness (arthritis) may be associated with long-term use of salicylates (aspirin) or other NSAIDs, some of which may alter blood clotting. Arthritic patients who are receiving long-term corticosteroid therapy may suffer increased risk of acute adrenal insufficiency, especially the patient who has recently stopped taking the steroid. Such patients may require a short course of steroid therapy or a modification (increase) in corticosteroid dose during dental treatment, so that their body is better able to respond to any additional stress that might be associated with the treatment.
Because of possible difficulties in positioning the patient comfortably, modifications may be necessary to accommodate the patient’s physical disability. Most patients receiving corticosteroids are categorized as ASA 2 or 3 risk depending on the reason for the medication and the degree of disability present. Patients with significantly disabling arthritis are ASA 3 risks. Problems secondary to arthritis may require modification in positioning during local anesthetic injection.
III Do You Have or Have You Had
29 Heart Disease?
Comment: This represents a survey question seeking to detect the presence of any and all types of heart disease. In the presence of a YES answer, the dentist must seek more specific detailed information as to the nature and severity of the problem and a list of any medications taken by the patient to manage the condition. Because many forms of heart disease are exacerbated in the presence of stress, consideration of the SRP becomes increasingly important.
30 Heart Attack, Heart Defects?
Comment: Heart attack is the lay term for myocardial infarction (MI). The dentist must determine the time that has elapsed since the patient suffered the MI, the severity of the MI, and the degree of residual myocardial damage to decide whether treatment modifications are indicated. Elective dental care traditionally has been withheld for the first 6 months after an MI,12 although recent evidence demonstrates that many patients are able to tolerate stress in as few as 3 to 4 weeks after experiencing an MI.13,14 Most post-MI patients are considered to be ASA 3 risks 6 months or more after the event; however, a patient who has experienced an MI within 6 months before the planned dental treatment should be considered an ASA 4 risk until medical consultation with his or her cardiologist is obtained. When little or no residual damage to the myocardium is present, the patient may be considered an ASA 2 risk after 6 months.
Heart failure: The degree of heart failure (weakness of the “pump”) present must be assessed through the dialogue history. When a patient has a more serious condition, such as congestive heart failure (CHF) or dyspnea (labored breathing) at rest, specific treatment modifications are warranted. In this situation, the dentist must consider whether the patient requires supplemental O2 during treatment. Whereas most HF patients are classified according to the ASA physical status classification system as ASA 2 (mild HF without disability) or ASA 3 (disability developing with exertion or stress) risks, the presence of dyspnea at rest represents an ASA 4 risk. Effective pain control is essential in the ASA 2 and 3 HF patient, but care must be taken in selecting the appropriate drugs and technique to prevent significant increases in the cardiac workload. Local anesthetics containing vasopressors are definitely indicated in these patients because they are more likely to provide successful pain control for dental procedures compared with “plain” local anesthetics.
Congenital heart lesions: An in-depth dialogue history is required to determine the nature of the lesion and the degree of disability present. Patients can represent ASA 2, 3, or 4 risk. The dentist may recommend medical consultation, especially for the pediatric patient, to judge the severity of the lesion. Some dental treatments require prophylactic antibiotics.
31 Heart Murmurs?
Comment: Heart murmurs are common, but not all murmurs are clinically significant. The dentist should determine whether a murmur is functional (nonpathologic, or ASA 2), whether clinical signs and symptoms of valvular stenosis or regurgitation are present (ASA 3 or 4), and whether antibiotic prophylaxis is warranted. A major clinical symptom of a significant (organic) murmur is undue fatigue. Table 10-1 provides guidelines for antibiotic prophylaxis (most recently revised in 2007).15 Box 10-1 categorizes cardiac problems as to their requirements for antibiotic prophylaxis, and Box 10-2 addresses prophylaxis and dental procedures specifically. As noted in the Guidelines, antibiotic prophylaxis is NOT indicated for the administration of routine dental injection techniques through noninfected tissues. Guidelines for antibiotic prophylaxis in orthopedic patients with total joint replacements were published initially in 200316 and were last revised in 2010.17
TABLE 10-1
Antibiotic Prophylaxis 2007*
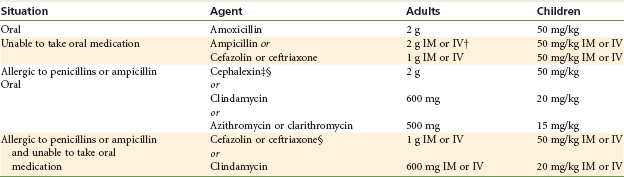
*Regimen: single dose 30 to 60 minutes before procedure.
†IM, Intramuscular; IV, intravenous.
‡Or other first- or second-generation oral cephalosporin in equivalent adult or pediatric dosage.
§Cephalosporins should not be used in an individual with a history of anaphylaxis, angioedema, or urticaria with penicillins or ampicillin.
From Wilson W, Taubert KA, Gewitz M, et al: Prevention of infective endocarditis: guidelines from the American Heart Association: a guideline from the American Heart Association Rheumatic Fever, Endocarditis, and Kawasaki Disease Committee, Council on Cardiovascular Disease in the Young, and the Council on Clinical Cardiology, Council on Cardiovascular Surgery and Anesthesia, and the Quality of Care and Outcomes Research Interdisciplinary Working Group, Circulation 116:1736–1754, 2007.
32 Rheumatic Fever?
Comment: A history of rheumatic fever should prompt the dentist to perform an in-depth dialogue history for the presence of rheumatic heart disease (RHD). In the presence of RHD, antibiotic prophylaxis may be indicated as a means of minimizing the risk of developing subacute bacterial endocarditis (SBE). Depending on the severity of the disease and the presence of a disability, RHD patients can be an ASA 2, 3, or 4 risk. Additional treatment modifications may be advisable.
33 Stroke, Hardening of Arteries?
Comment: The dentist must pay close attention to stroke, cerebrovascular accident (CVA), or “brain attack” (the term increasingly used to confer on the lay public and health care professionals the urgency needed in prompt management of the victim of a CVA). A patient who has suffered a CVA is at greater risk of suffering another CVA or a seizure should he or she become hypoxic. The importance of effective pain control, through administration of local anesthetic solutions with vasopressors, cannot be overstated. Epinephrine concentrations should be minimized (e.g., 1 : 200,000) but this agent should be included as it increases anesthetic effectiveness. The dentist should be especially sensitive to the presence of transient cerebral ischemia (TCI), a precursor to CVA; TCI represents an ASA 3 risk. The post-CVA patient is an ASA 4 risk within 6 months of the CVA, becoming an ASA 3 risk 6 or more months after the incident (if the recovery is uneventful). In rare cases, the post-CVA patient can be an ASA 2 risk.
34 High Blood Pressure?
Comment: Elevated blood pressure (BP) measurements are frequently encountered in the dental environment secondary to the added stress that many patients associate with a visit to the dental office. With a history of HBP, the dentist must determine the drugs the patient is taking, the potential side effects of those medications, and any possible interactions with other drugs that might be used during dental treatment. Guidelines for clinical evaluation of risk (ASA categories) based on adult BP values are presented later in this chapter. The SRP is a significant factor in minimizing further elevation in BP during treatment.
35 Asthma, Tuberculosis (TB), Emphysema, Other Lung Disease?
Comment: Determining the nature and severity of respiratory problems is an essential part of patient evaluation. Many acute problems developing in the dental environment are stress related, increasing the workload of the cardiovascular system and the O2 requirements of many tissues and organs in the body. The presence of severe respiratory disease can greatly influence the planned dental treatment and the choice of drugs and technique if sedation is required.
Asthma (bronchospasm) is marked by a partial obstruction of the lower airway. The dentist must determine the nature of the asthma (intrinsic [allergic] vs. extrinsic [nonallergic]), the frequency of acute episodes, causal factors, the method of management of acute episodes, and drugs the patient may be taking to minimize the occurrence of acute episodes. Stress is a common precipitating factor in acute asthmatic episodes. The well-controlled asthmatic patient represents an ASA 2 risk, whereas the well-controlled but stress-induced asthmatic patient is an ASA 3 risk. Patients whose acute episodes are frequent and/or difficult to terminate (requiring hospitalization [status asthmaticus]) are ASA 3 or 4 risk.
With a history of tuberculosis, the dentist must first determine whether the disease is active or arrested. (Arrested tuberculosis represents an ASA 2 risk.) Medical consultation and dental treatment modification are recommended when such information is not easily determined.
Emphysema is a form of chronic obstructive pulmonary disease (COPD), also called chronic obstructive lung disease (COLD). The emphysematous patient has a decreased respiratory reserve from which to draw if cells of the body require additional O2, which they do during stress. Supplemental O2 therapy during dental treatment is recommended in severe cases of emphysema; however, the severely emphysematous (ASA 3 and 4) patient should not receive more than 3 L of O2 per minute.18 This flow restriction helps to ensure that the dentist does not eliminate the hypoxic drive, which is the emphysematous patient’s primary stimulus for breathing. The emphysematous patient is an ASA 2, 3, or 4 risk, depending on the degree of disability.
36 Hepatitis, Other Liver Disease?
Comment: Liver diseases may be transmissible (hepatitis A and B) or may indicate the presence of hepatic dysfunction. A history of blood transfusion or of past or present drug addiction should alert the dentist to a probable increase in the risk of hepatic dysfunction. (Hepatic dysfunction is a common finding in the parenteral drug abuse patient.) Hepatitis C is responsible for more than 90% of cases of posttransfusion hepatitis, but only 4% of cases are attributable to blood transfusion; up to 50% of cases are related to IV drug use. Incubation of hepatitis C averages 6 to 7 weeks. The clinical illness is mild, usually asymptomatic, and characterized by a high rate (>50%) of chronic hepatitis.19 Because most drugs undergo biotransformation in the liver, care must be taken when specific drugs and techniques of administration are selected for the patient with significant hepatic dysfunction. In general, local anesthetics and vasopressors are indicated for use, with consideration of minimizing the dose in patients with severe hepatic dysfunction (e.g., ASA 4).
37 Stomach Problems, Ulcers?
Comment: The presence of stomach or intestinal ulcers may be indicative of acute or chronic anxiety and the possible use of medications such as tranquilizers, H1-inhibitors, and antacids. Knowledge of which drugs are taken is important before additional drugs are administered in the dental office. A number of H1-inhibitors are now over-the-counter (OTC) drugs. Because many patients do not consider OTC drugs “real” medications, the dentist must specifically question the patient about them. The presence of ulcers does not itself represent increased risk during treatment. In the absence of additional medical problems, the patient may represent an ASA 1 or 2 risk.
38 Allergies to: Drugs, Foods, Medications, Latex?
Comment: The dentist must evaluate a patient’s allergies thoroughly before administering dental treatment or drugs. The importance of this question and its full evaluation cannot be overstated. A complete and vigorous dialogue history must be undertaken before any dental treatment is begun, especially when a presumed or documented history of drug allergy is present. Adverse drug reactions (ADRs) are not uncommon. Many, if not most, ADRs are labeled as “allergy” by the patient and also on occasion by his or her health care professional. However, despite the great frequency with which allergy is reported, true documented and reproducible allergic drug reactions are relatively rare. A recent review of food allergy revealed 30% self-reporting of “food allergy” by the studied population, when the reality is that true food allergy is seen in 8% of children and 5% of adults.20
All ADRs must be evaluated thoroughly, especially when the dentist plans to administer or prescribe closely related medications for the patient during dental treatment. Alleged “allergy to Novocaine” is frequently reported.
The incidence of true, documented, reproducible allergy to the amide local anesthetics is virtually nil.21,22 However, reports of alleged allergy to local anesthetics is common.23,24 Thorough investigation of the alleged allergy is essential if the patient is not to be assigned the label of “allergic to all -caine drugs,” thereby precluding dental (and surgical) care in a normal manner. Avoidance of dental care or receipt of care under general anesthesia is the alternative in these cases.
Reports of allergy to “epinephrine” or “adrenaline” also must be carefully evaluated. Most often, such reports prove to be simply an exaggerated physiologic response by the patient to the injected epinephrine or, more commonly, to endogenous catecholamine release in response to the act of receiving the injection (the “adrenal squeeze,” as a colleague called it recently).
Two essential questions that must be asked in all instances of alleged allergy are these: (1) Describe your reaction, and (2) How was it managed?
The presence of allergy alone represents an ASA 2 risk. No emergency situation is as frightening to health care professionals as the acute, systemic allergic reaction known as anaphylaxis. Prevention of this life-threatening situation is more gratifying than treatment of anaphylaxis once it develops.
Investigation into a patient’s report of “allergy to local anesthesia” is so important that it is discussed in depth in Chapter 18.
40 Acquired Immunodeficiency Syndrome (AIDS)?
Comment: Patients who have a positive test result for human immunodeficiency virus (HIV) are representative of every area of the population. The usual barrier techniques should be employed to minimize risk of cross-infection for both patient and staff members. Patients who are HIV positive are considered ASA 2, 3, 4, or 5 risk depending on the current status of their infection.
Proper care and handling of the local anesthetic syringe/needle must be observed, as in all situations, to avoid accidental needle-stick injury.
41 Tumors, Cancer?
Comment: The presence or prior existence of cancer of the head or neck may require specific modification of dental therapy. Irradiated tissues have decreased resistance to infection, diminished vascularity, and reduced healing capacity. No specific contraindication exists to administration of drugs for the management of pain or anxiety in these patients; however, techniques of local anesthetic drug administration may, on rare occasion, be contraindicated if the tissues in the area of deposition have been irradiated. Many persons with cancer may be receiving long-term therapy with CNS depressants, such as antianxiety drugs, hypnotics, and opioids. Consultation with the patient’s oncologist is recommended before dental treatment is begun. A past or current history of cancer does not necessarily increase ASA risk status. However, patients who are cachectic or hospitalized or are in poor physical condition may represent ASA 4 or 5 risk.
43 Eye Disease?
Comment: For patients with glaucoma, the need to administer a drug that diminishes salivary gland secretions will have to be addressed. Anticholinergics, such as atropine, scopolamine, and glycopyrrolate, are contraindicated in patients with acute narrow angle glaucoma because these drugs produce an increase in intraocular pressure. Patients with glaucoma are usually ASA 2 risks. There is no contraindication to local anesthetic administration with or without vasopressors.
44 Skin Diseases?
Comment: Skin represents an elastic, rugged, self-regenerating, protective covering for the body. The skin also represents our primary physical presentation to the world and as such displays a myriad of clinical signs of disease processes, including allergy and cardiac, respiratory, hepatic, and endocrine disorders.25
45 Anemia?
Comment: Anemia is a relatively common adult ailment, especially among young adult women (iron deficiency anemia). The dentist must determine the type of anemia present. The ability of the blood to carry O2 or to give up O2 to other cells is decreased in anemic patients. This decrease can become significant during procedures in which hypoxia is likely to develop. There is no contraindication to local anesthetic administration with or without vasopressors.
Sickle cell anemia is seen exclusively in black patients. Periods of unusual stress or of O2 deficiency (hypoxia) may precipitate sickle cell crisis. Administration of supplemental O2 during treatment is strongly recommended for patients with sickle cell disease. Persons with sickle cell trait represent ASA 2 risk, whereas those with sickle cell disease are 2 or 3 risks.
In addition, congenital or idiopathic methemoglobinemia, although rare, represents a relative contraindication to administration of the amide local anesthetic prilocaine.26
46 VD (Syphilis or Gonorrhea)?
Comment: When treating patients with sexually transmitted diseases (STDs), dentists and staff members are at risk of infection. In the presence of oral lesions, elective dental care might be postponed. Standard barrier techniques, such as protective gloves, eyeglasses, and masks, provide operators with a degree of (but not total) protection. Such patients usually represent ASA 2 and 3 risks but may be 4 or 5 risks in extreme situations.
48 Kidney, Bladder Disease?
Comment: The dentist should evaluate the nature of the renal disorder. Treatment modifications including antibiotic prophylaxis may be appropriate for several chronic forms of renal disease. Functionally anephric patients are ASA 3 or 4 risks, whereas patients with most other forms of renal dysfunction may be ASA 2 or 3 risks. Box 10-3 shows a sample dental referral letter for a patient on long-term hemodialysis treatment as the result of chronic kidney disease.
49 Thyroid, Adrenal Disease?
Comment: The clinical presence of thyroid or adrenal gland dysfunction—hyperfunction or hypofunction—should prompt the dentist to use caution in administering certain drug groups (e.g., epinephrine to hyperthyroid patients, CNS depressants to hypothyroid patients). In most instances, however, the patient has previously seen a physician and has undergone treatment for thyroid disorder by the time he or she seeks dental treatment. In this case, the patient is likely to be in a euthyroid state (normal blood levels of thyroid hormone) because of surgical intervention, irradiation, or drug therapy. The euthyroid state represents an ASA 2 risk, whereas clinical signs and symptoms of hyperthyroidism or hypothyroidism represent ASA 3 or, in rare instances, ASA 4 risk. Patients who are clinically hyperthyroid are more likely to hyper-respond to “usual” doses of epinephrine (e.g., develop tachycardia, have elevated blood pressure). Vital signs should be monitored preoperatively, perioperatively, and postoperatively in these situations.
Patients with hypofunctioning adrenal cortices have Addison disease and receive daily replacement doses of glucocorticosteroids. In stressful situations, their body may be unable to respond appropriately, leading to loss of consciousness. Hypersecretion of cortisone, Cushing syndrome, rarely results in an acute life-threatening situation. Consideration of sedation, in the presence of dental anxiety, is recommended.
50 Diabetes?
Comment: A patient who responds positively to this question requires further inquiry to determine the type, severity, and degree of control of his or her diabetic condition. A patient with type 1 (insulin-dependent diabetes mellitus, or IDDM) or type 2 (non–insulin-dependent diabetes mellitus, or NIDDM) diabetes mellitus is rarely at great risk from dental care or commonly administered dental drugs (e.g., local anesthetics, epinephrine, antibiotics, CNS depressants). The NIDDM patient is usually an ASA 2 risk; the well-controlled IDDM patient, an ASA 3 risk; and the poorly controlled IDDM patient, an ASA 3 or 4 risk.
The greatest concerns during dental treatment relate to the possible effects of the dental care on subsequent eating and development of hypoglycemia (low blood sugar). Patients leaving a dental office with residual soft tissue anesthesia, especially in the mandible (e.g., tongue, lips), usually defer eating until sensation returns, a period potentially of 5 (lidocaine, mepivacaine, articaine, prilocaine with vasoconstrictor) or more (up to 12) hours (bupivacaine with vasoconstrictor). Diabetic patients have to modify their insulin doses if they do not maintain normal eating habits. Administration of the local anesthetic reversal agent, phentolamine mesylate, at the conclusion of dental treatment can significantly minimize the duration of residual soft tissue anesthesia.27,28
IV Do You Have or Have You Had
51 Psychiatric Care?
Comment: The dentist should be aware of any nervousness (in general or specifically related to dentistry) or history of psychiatric care before treating the patient. Such patients may be receiving a number of drugs to manage their disorders that might interact with drugs the dentist uses to control pain and anxiety (Table 10-2). Medical consultation should be considered in such cases. Extremely fearful patients are ASA 2 risks, whereas patients receiving psychiatric care and drug therapy represent ASA 2 or 3 risk.
TABLE 10-2
Dental Drug Interactions With Local Anesthetics and Vasopressors*
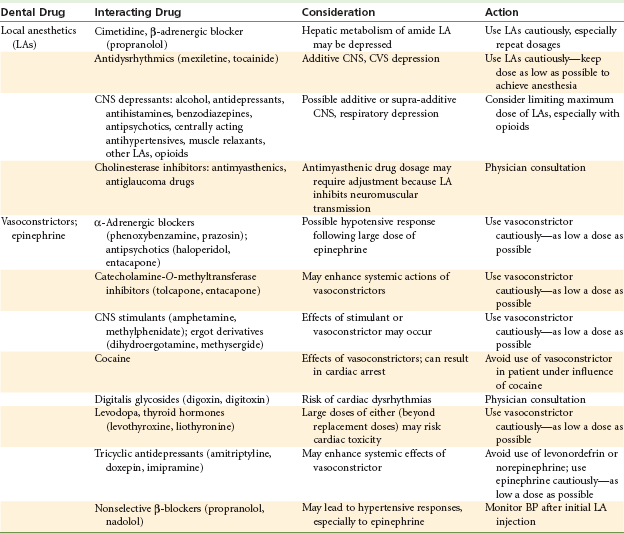
BP, Blood pressure; CNS, central nervous system; CVS, cardiovascular system.
*Drug–drug interactions of greater clinical significance are emboldened for emphasis.
From Ciancio SG: ADA/PDR guide to dental therapeutics, ed 5, Chicago, 2010, American Dental Association.
54 Prosthetic Heart Valve?
Comment: Patients with prosthetic (artificial) heart valves are no longer uncommon. The dentist’s primary concern is to determine whether antibiotic prophylaxis is required. Antibiotic prophylactic protocols were presented earlier in this chapter.15 The dentist should be advised to consult with the patient’s physician (e.g., the cardiologist, the cardiothoracic surgeon) before providing treatment. Patients with prosthetic heart valves usually represent ASA 2 or 3 risk. Administration of local anesthetic drugs and vasopressors is indicated for these patients. Antibiotic prophylaxis is not indicated for the administration of routine dental injection techniques through noninfected tissues.15
55 Artificial Joint?
Comment: More than 1,000,000 total joint arthroplasties are performed annually in the United States.17 An expert panel of dentists, orthopedic surgeons, and infectious disease specialists convened by the American Dental Association (ADA) and the American Academy of Orthopaedic Surgeons performed a thorough review of available data to determine the need for antibiotic prophylaxis to prevent hematogenous prosthetic joint infection in dental patients who have undergone total joint arthroplasty. The panel concluded that antibiotic prophylaxis is not recommended for dental patients with pins, plates, and screws, or for those who have undergone total joint replacement. However, dentists should consider antibiotic premedication in a small number of patients who may be at increased risk for the development of hematogenous total joint infection (Table 10-3).16
TABLE 10-3
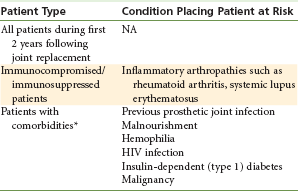
HIV, Human immunodeficiency virus; NA, not applicable.
*Patients potentially at increased risk of experiencing hematogenous total joint infection.
Data from American Dental Association, American Academy of Orthopedic Surgeons: Antibiotic prophylaxis for dental patients with total joint replacements, J Am Dent Assoc 134:895-898, 2003.
58 Surgeries?
Comment: Determine the reason for hospitalization, the duration of the hospital stay, and any medications prescribed that the patient may currently be taking.
Determine the reason for the blood transfusion (e.g., prolonged bleeding, accident, type of surgery).
Determine the nature (elective, emergency) and type of surgery (cosmetic, GI, cardiac, etc.) and the patient’s physical status at the present time.
59 Pacemaker?
Comment: Cardiac pacemakers are implanted beneath the skin of the upper chest or the abdomen with pacing wires extending into the myocardium. The most frequent indication for the use of a pacemaker is the presence of a clinically significant dysrhythmia. Fixed-rate pacemakers provide a regular, continuous heart rate regardless of the heart’s inherent rhythm, whereas the more commonly used demand pacemaker is activated only when the rhythm of the heart falls into an abnormal range. Although there is little indication for antibiotic administration in these patients, medical consultation is suggested before the start of treatment to obtain the specific recommendations of the patient’s physician. The patient with a pacemaker is commonly an ASA 2 or 3 risk during dental treatment.
In recent years, persons who represent a significant risk of sudden unexpected death (e.g., cardiac arrest) as a result of electrical instability of the myocardium (e.g., ventricular fibrillation) have had implantable cardioverter-defibrillators (ICDs) placed below the skin of their chest. Medical consultation is strongly recommended for these patients.
60 Contact Lenses?
Comment: Contact lenses are commonly worn by persons with visual disturbances. Dental considerations for patients with contact lenses include removal of the lenses during administration of any sedation technique. Sedated patients may not close their eyes as frequently as unsedated patients, thereby increasing the likelihood of irritating the sclera and cornea of the eye. This is particularly recommended when inhalation sedation (N2O-O2) is employed because any leakage of gases from the nasal hood is likely to irritate the eyes.
V Are You Taking
61 Recreational Drugs?
Comment: Although most patients will not admit to the use of recreational drugs, it is important to ask the question. This becomes particularly important when the dentist is considering the use of CNS-depressant drugs for sedation or local anesthetics with or without a vasoconstrictor, such as epinephrine.
62 Drugs, Medications, Over-the-Counter Medicines (Including Aspirin), Natural Remedies?
Comment: Because many patients make a distinction between the terms drug and medication, questionnaires should use both terms to determine what drugs (pharmaceutically active substances) a patient has taken. Unfortunately, in today’s world, the term drug often connotes the illicit use of medications (e.g., opioids). In the minds of many patients, people “do” drugs but “take” medications for the management of medical conditions. Additionally, natural remedies contain active substances, some of which may interact with drugs commonly used in dentistry.29,30
The dentist must be aware of all medications and drugs that their patients take to control and treat medical disorders. Frequently, patients take medications without knowing the condition the medications are designed to treat; many patients do not even know the names of drugs that they are taking. It becomes important therefore for dentists to have available one or more means of identifying these medications and of determining their indications, side effects, and potential drug interactions. Many excellent sources are available, including online services, such as MD Consult,* Lexi-Comp,† and Epocrates.‡ The Physicians’ Desk Reference (PDR),31 both in hard copy and online, offers a picture section that aids in identification of commonly prescribed drugs. The PDR also offers the Physicians’ Desk Reference for Herbal Medicines.31 The ADA Guide to Dental Therapeutics is another valuable reference to those drugs commonly employed in dentistry and to the medications most often prescribed by physicians. Potential complications and drug interactions are stressed.31a
Knowledge of the drugs and medications patients are taking permits dentists to identify medical disorders, possible side effects—some of which may be of significance in dental treatment (e.g., postural hypotension)—and possible interactions between those medications and the drugs administered during dental treatment (see Table 10-2).
VI Women Only
65 Are You or Could You Be Pregnant or Nursing?
66. Taking Birth Control Pills?
Comment: Pregnancy represents a relative contraindication to extensive elective dental care, particularly during the first trimester. Consultation with the patient’s obstetrician-gynecologist (OBGYN) is recommended before the start of any dental treatment. Administration of local anesthetics with or without epinephrine is acceptable during pregnancy. Food and Drug Administration (FDA) pregnancy categories are presented in Box 10-4, and known fetal effects of local anesthetics and vasopressors are presented in Table 10-4.
TABLE 10-4
| Drug | Effect |
| Anesthetics, local | No adverse effects in dentistry |
| Articaine | No adverse effects reported in dentistry |
| Bupivacaine | Does not cross placenta readily; no adverse effects in dentistry |
| Epinephrine | No adverse effects reported for dental use |
| Lidocaine | No adverse effects reported in dentistry |
| Mepivacaine | No adverse effects reported in dentistry |
| Prilocaine | No adverse effects reported in dentistry |
VII All Patients
67 Do You Have or Have You Had Any Other Diseases or Medical Problems Not Listed on This Form?
Comment: The patient is encouraged to comment on specific matters not previously mentioned. Examples of several possibly significant disorders include acute intermittent porphyria, methemoglobinemia, atypical plasma cholinesterase, and malignant hyperthermia.
To the best of my knowledge, I have answered every question completely and accurately. I will inform my dentist of any change in my health and/or medication.
Comment: This final statement is important from a medicolegal perspective because although instances of purposeful lying on health histories are rare, they do occur. This statement should be accompanied by the date on which the history was completed and the signatures of both the patient (or the parent or guardian if the patient is a minor or is not legally competent) and the dentist who reviews the history. This in effect becomes a contract obliging the patient, parent, or guardian to report any changes in the patient’s health or medications. Brady and Martinoff7 demonstrated that a patient’s analysis of personal health frequently is overly optimistic, and that pertinent health matters sometimes are not immediately reported.
The medical history questionnaire should be updated on a regular basis, approximately every 3 to 6 months or after any prolonged lapse in treatment. In most instances, the entire medical history questionnaire need not be redone. The dentist or dental hygienist need only ask the following questions:
1. Have you experienced any change in your general health since your last dental visit?
2. Are you now under the care of a physician? If so, what is the condition being treated?
3. Are you currently taking any drugs, medications, or over-the-counter products?
If any of these questions elicits a positive response, a detailed dialogue history should follow. For example, a patient may answer that no change has occurred in general health but may want to notify the dentist of a minor change in condition, such as the end of a pregnancy (It’s a girl!) or a recent diagnosis of NIDDM or asthma.
In either situation, a written record of having updated the history should be appended to the patient’s progress notes or on the health history form. When the patient’s health status has changed significantly since the last history was completed, the entire history should be redone (e.g., if a patient was recently diagnosed with cardiovascular disease and is managing it with a variety of drugs that he or she was not previously taking).
In reality, most persons do not undergo significant changes in their health with any regularity. Thus one health history questionnaire can remain current for many years. Therefore the ability to demonstrate that a patient’s medical history has been updated on a regular basis becomes all the more important.
The medical history questionnaire should be completed in ink. Corrections and deletions are made by drawing a single line through the original entry without obliterating it. The change is then added along with the date of the change. The dentist initials the change.
A written notation should be placed in the chart whenever a patient reveals significant information during the dialogue history. As an example, when a patient answers affirmatively to the question about a “heart attack”, the dentist’s notation may read “2008” (the year the MI occurred).
Physical Examination
The medical history questionnaire is quite important to the overall assessment of a patient’s physical and psychological status. However, the questionnaire has limitations. For the questionnaire to be valuable, the patient must (1) be aware of the presence of any medical condition and (2) be willing to share this information with the dentist.
Most patients do not knowingly deceive their dentist by omitting important information from the medical history questionnaire, although cases in which such deception has occurred are on record. A patient seeking treatment for an acutely inflamed tooth decides to withhold from the dentist that he had an MI 2 months earlier because he knows that to tell the dentist would mean that he would likely not receive the desired treatment (e.g., extraction).
The other factor, a patient’s knowledge of his or her physical condition, is a much more likely cause of misinformation on the questionnaire. Most “healthy” persons do not visit their physician regularly for routine checkups. Recent information has suggested that annual physical examination should be discontinued in the younger healthy patient because it has not proved as valuable an aid in preventive medicine, as was once thought.32a In addition, most patients simply do not visit their physician on a regular basis, doing so instead whenever they become ill. From this premise, it stands to reason that the true state of the patient’s physical condition may be unknown to the patient. Feeling well, although usually a good indicator of health, is not a guarantor of good health.7 Many disease entities may be present for a considerable length of time without exhibiting overt signs or symptoms that alert the patient of their presence (e.g., HBP, diabetes mellitus, cancer). When signs and symptoms are present, they are frequently mistaken for other, more benign problems. Although they may answer questions on the medical history questionnaire to the best of their knowledge, patients cannot give a positive response to a question unless they are aware that they have the condition. The first few questions on most histories refer to the length of time since the patient’s last physical examination. The value of the remaining answers, dealing with specific disease processes, can be gauged from the patient’s responses to these initial questions.
Because of these problems, which are inherent in the use of a patient-completed medical history questionnaire, the dentist must look for additional sources of information about the physical status of the patient. Physical examination of the patient provides much of this information. This consists of the following:
2. Visual inspection of the patient
3. Function tests, as indicated
4. Auscultation of heart and lungs and laboratory tests, as indicated
Minimal physical evaluation for all potential patients should consist of (1) measurement of vital signs and (2) visual inspection of the patient.
The primary value of the physical examination is that it provides the dentist with important (up-to-the-minute) information concerning the physical condition of the patient immediately before the start of treatment, as contrasted with the questionnaire, which provides historical (dated) information. The patient should undergo a minimal physical evaluation at the initial visit to the office before the start of any dental treatment. Readings obtained at this time, called baseline vital signs, are recorded on the patient’s chart.
The six vital signs are as follows:
Vital signs and guidelines for their interpretation follow.
Blood Pressure
Technique: The following technique is recommended for the accurate manual determination of BP.33 A stethoscope and a sphygmomanometer (blood pressure cuff) are the required equipment. The most accurate and reliable of these devices is the mercury-gravity manometer. The aneroid manometer, probably the most frequently used, is calibrated to be read in millimeters of mercury (mm Hg) and is quite accurate if well maintained. Rough handling of the aneroid manometer may lead to erroneous readings. It is recommended that the aneroid manometer be recalibrated at least annually. Use of automatic BP monitors has become common because their accuracy has increased while their cost has decreased, ranging from well under $100 to several thousand dollars. Likewise, their accuracy varies. The use of automatic monitors simplifies the monitoring of vital signs, but dentists should be advised to check the accuracy of these devices periodically (comparing values with those of the more accurate mercury or aneroid manometer).
Although they are most accurate, the use of mercury manometers has become increasingly rare because they are too bulky for easy carrying and mercury spills are potentially dangerous.34 Aneroid manometers are easy to use, are somewhat less accurate than mercury manometers, and are more delicate, requiring recalibration at least annually or when dropped or bumped.34
Automatic devices containing all equipment in one unit negate the need for a separate stethoscope and manometer. Most are easy to use, whereas more expensive devices have automatic inflation and deflation systems and readable printouts of both BP and heart rate. As with the aneroid manometer, automatic BP systems are somewhat fragile, requiring recalibration on a regular schedule or when bumped or dropped. Body movements may influence accuracy, and even the most accurate devices do not work on certain people.34
Automatic BP monitors that fit on the patient’s wrist are available and easy to use. However, BP measurements at the wrist may not be as accurate as those taken at the upper arm, and systematic error can occur as a result of differences in the position of the wrist relative to the heart (see later discussion).35,36 The technique of blood pressure monitoring is discussed in extensive detail in other textbooks.37
For the adult patient with a baseline BP in the ASA 1 range (<140/<90 mm Hg), it is suggested that BP be recorded every 6 months unless specific dental procedures demand more frequent monitoring. The parenteral administration of any drug (local anesthesia; IM, IV, or inhalation sedation; or general anesthesia) mandates more frequent recording of vital signs.
Patients with BPs in the ASA 2, 3, or 4 category should be monitored more frequently (e.g., at every appointment), as outlined in Table 10-5. Patients with known HBP should have their BP monitored at each visit to determine whether BP is adequately controlled. It is impossible to gauge BP by “looking” at a person, or by asking, “How do you feel?” Routine monitoring of BP in all patients according to treatment guidelines will effectively minimize the occurrence of acute complications of HBP (e.g., hemorrhagic CVA).
TABLE 10-5
Guidelines for Blood Pressure (Adult)
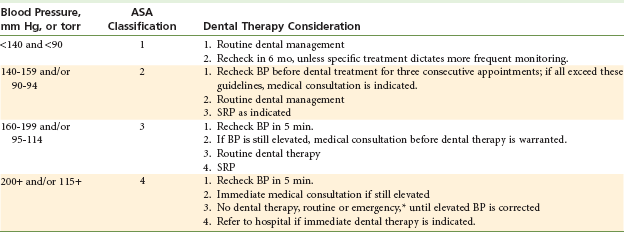
ASA, American Society of Anesthesiologists; BP, blood pressure; SRP, stress reduction protocol.
*When the BP of the patient is slightly above the cutoff for category 4 and anxiety is present, inhalation sedation may be employed in an effort to diminish the BP (via the elimination of stress).
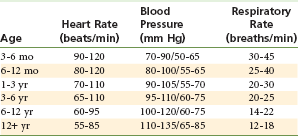
The normal range of BP in younger patients is somewhat lower than that in adults. Table 10-6 presents a normal range of BP in infants and children.
Technique: Heart rate (pulse) and rhythm may be measured at any readily accessible artery. Most commonly used for routine measurement are the brachial artery, which is located on the medial aspect of the antecubital fossa, and the radial artery, which is located on the radial and ventral aspects of the wrist.
Guidelines for Clinical Evaluation: Three factors should be evaluated while the pulse is monitored:
The heart rate should be evaluated for a minimum of 30 seconds, ideally for 1 minute. The normal resting heart rate for an adult ranges from 60 to 110 beats per minute. It is often lower in a well-conditioned athlete (physiologic [sinus] bradycardia) and elevated in the fearful individual (sinus tachycardia). However, clinically significant disease may also produce slow (bradycardia [<60 per minute]) or rapid (tachycardia [>110 per minute]) heart rates. It is suggested that any heart rate below 60 or above 110 beats per minute (adult) should be evaluated (initially via dialogue history). Where no obvious cause is present (e.g., endurance sports, anxiety), medical consultation should be considered.
The healthy heart maintains a relatively regular rhythm. Irregularities in rhythm should be confirmed and evaluated via dialogue history and/or medical consultation before the start of treatment. The occasional premature ventricular contraction (PVC) is so common that it is not necessarily considered abnormal. Clinically, PVCs detected by palpation appear as a break in a generally regular rhythm in which a longer-than-normal pause (a “skipped beat”) is noted, followed by resumption of regular rhythm. PVCs may be produced by smoking, fatigue, stress, various drugs (e.g., epinephrine, caffeine), and alcohol. Frequent PVCs are usually associated with a damaged or an ischemic myocardium.
Disturbances in the regularity of heart rhythm should be evaluated before the start of dental treatment, particularly when drugs (e.g., local anesthetics, sedatives) are to be administered. Table 10-6 presents the range of normal heart rates in children of various ages.
Administration of epinephrine-containing local anesthetics is relatively contraindicated in patients with ventricular dysrhythmias unresponsive to medical therapy. Dysrhythmias frequently are induced by an ischemic or irritable myocardium. Epinephrine and other catecholamines may provoke further irritability, leading to potentially more serious, possibly fatal dysrhythmias.
Guidelines for Clinical Evaluation: Normal respiratory rate for an adult is 14 to 18 breaths per minute. Bradypnea (abnormally slow rate) may be produced by, among other causes, opioid administration, whereas tachypnea (abnormally rapid rate) is seen with fever, fear (hyperventilation), and alkalosis. The most common change in ventilation noted in the dental environment is hyperventilation, an abnormal increase in the rate and depth of respiration. It is also seen, but much less frequently, in diabetic acidosis. The most common cause of hyperventilation in dental and surgical settings is extreme psychological stress, which is not infrequent during local anesthetic administration (e.g., “the shot”).
Any significant variation in respiratory rate should be evaluated before treatment. Table 10-6 presents the normal range of respiratory rates at different ages.
BP, heart rate and rhythm, and respiratory rate provide information about the functioning of the cardiorespiratory system. It is recommended that they be recorded as part of the routine physical evaluation for all potential dental patients. Recording of the remaining vital signs—temperature, height, and weight—although desirable, may be considered optional. However, when parenteral drugs are to be administered, including local anesthetics, especially in lighter-weight, younger, or older patients, actual recording of a patient’s weight becomes considerably more important.
Technique: Patients should be asked to state their height and weight. The range of normal height and weight is quite variable and is available on charts developed by various insurance companies. New guidelines for range of normal height and weight have been published (Table 10-7).
TABLE 10-7
Acceptable Weight (in Pounds) for Men and Women*
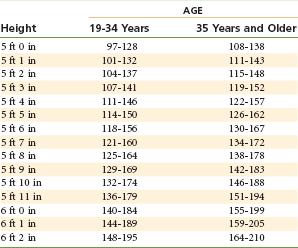
*Weights based on weighing in without shoes or clothes.
Department of Health & Human Services (HHS) and Department of Agriculture (USDA): Dietary guidelines for Americans, Washington, DC, 2005, HHS/USDA.
In pediatric patients, especially those weighing less than 30 kg (66 lb), it is strongly suggested that the patient be weighed before receiving local anesthetic or CNS-depressant drugs (e.g., sedatives).
For the dentist who treats younger, lighter-weight (less than 30 kg [66 lb]) patients, it is strongly suggested that a scale be available in the office. If the child will not willingly step onto the scale for measurement, the doctor can, after weighing himself or herself, hold the patient, obtain their combined weight, then subtract his or her own weight to accurately calculate the patient’s weight. Parents are not usually accurate informers about their child’s weight.
Visual Inspection of the Patient
Visual observation of the patient provides the dentist with valuable information concerning the patient’s medical status and level of apprehension toward the planned treatment. Observation of the patient’s posture, body movements, speech, and skin can assist in the diagnosis of possibly significant disorders that may have gone undetected previously. The reader is referred to other textbooks for a more detailed discussion of visual inspection of the dental patient.37-39
Additional Evaluation Procedures
Following completion of these three steps (medical history questionnaire, vital signs, and physical examination), it occasionally will be necessary to follow up with additional evaluation for specific medical disorders. This examination may include auscultation of the heart and lungs, testing for blood glucose levels, retinal examination, function tests for cardiorespiratory status (e.g., breath-holding test, match test), electrocardiographic examination, and blood chemistries. Many of these tests are used in dental offices but do not represent a standard of care in dentistry.
Dialogue History
After patient information has been collected, the dentist reviews with the patient any positive responses on the questionnaire, seeking to determine the severity of these disorders and any potential risk that they might represent during the planned treatment. This process, the dialogue history, is an integral part of patient evaluation. The dentist must put to use all available knowledge of the disease to assess the degree of risk to the patient.
One example of dialogue history is presented below. For a more in-depth description of dialogue history for specific disease states, the reader is referred to Medical Emergencies in the Dental Office, 6th edition.37
The following is a dialogue history to be initiated with a positive reply to angina pectoris:
1. What precipitates your angina?
2. How frequently do you experience anginal episodes?
3. How long do your anginal episodes last?
4. Describe a typical anginal episode.
5. How does nitroglycerin affect the anginal episode?
6. How many tablets or sprays do you normally need to terminate the episode?
7. Are your anginal episodes stable (similar in nature), or has there been a recent change in their frequency, intensity, radiation pattern of pain, or response to nitroglycerin (seeking unstable or preinfarction angina)?
Dialogue history should be completed for every positive response noted on the medical history. A written note should be included on the questionnaire that summarizes the patient’s response to the questions. For example, “heart attack” is circled. Written by the dentist next to this on the questionnaire is the statement “June 2008,” implying that the patient stated that the heart attack occurred in June 2008.
Dialogue history related to the administration of local anesthetic in patients with alleged allergy is presented in Chapter 18.
Determination of Medical Risk
Having completed all components of the physical evaluation and a thorough dental examination, the dentist next takes all of this information and answers the following questions:
1. Is the patient capable, physically and psychologically, of tolerating in relative safety the stresses involved in the proposed treatment?
2. Does the patient represent a greater risk (of morbidity or mortality) than normal during this treatment?
3. If the patient does represent an increased risk, what modifications will be necessary in the planned treatment to minimize this risk?
4. Is the risk too great for the patient to be managed safely as an outpatient in the medical or dental office?
In an effort to answer these questions, the Herman Ostrow School of Dentistry of USC developed a physical evaluation system that attempts to assist the dentist in categorizing patients from the standpoint of risk factor orientation.40 Its function is to assign the patient an appropriate risk category so that dental care can be provided to the patient in comfort and with increased safety. The system is based on the ASA physical status classification system, which is described next.
Physical Status Classification System
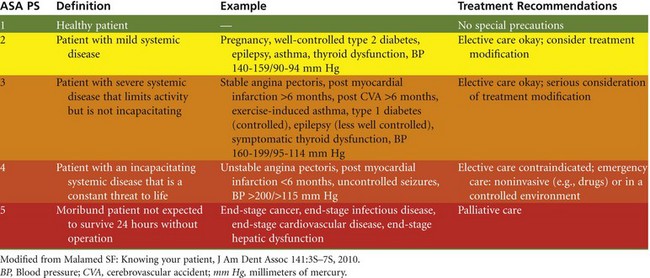
In 1962 the American Society of Anesthesiologists (ASA) adopted what is now referred to as the ASA physical status (ASA PS) classification system.41 This system represents a means of estimating medical risk presented by a patient undergoing a surgical procedure. The system has been in continual use since 1962, virtually without change, and has proved to be a valuable method of determining surgical and anesthetic risk before the actual procedure.42,43 The classification system follows:
Class 1. A healthy patient (no physiologic, physical, or psychological abnormalities)
Class 2. A patient with mild systemic disease without limitation of daily activities
Class 3. A patient with severe systemic disease that limits activity but is not incapacitating
Class 4. A patient with incapacitating systemic disease that is a constant threat to life
Class 5. A moribund patient not expected to survive 24 hours with or without the operation
Class 6. A brain-dead patient whose organs are being removed for donor purposes
When this system was adapted for use in a typical outpatient dental or medical setting, ASA 5 and 6 were eliminated and an attempt made to correlate the remaining four classifications with possible treatment modifications for dental treatment. Figure 10-6 illustrates the USC physical evaluation form on which a summary of the patient’s physical and psychological status is presented along with planned treatment modifications.
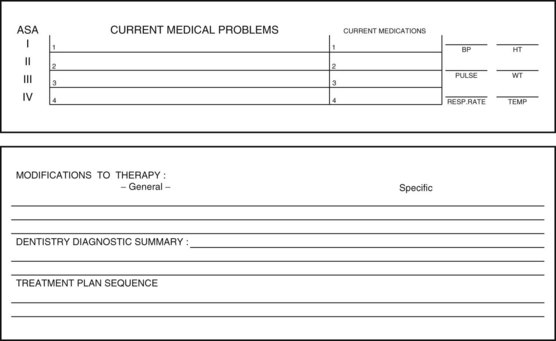
Figure 10-6 The Herman Ostrow School of Dentistry of University of Southern California (USC) physical evaluation (PE) summary form.
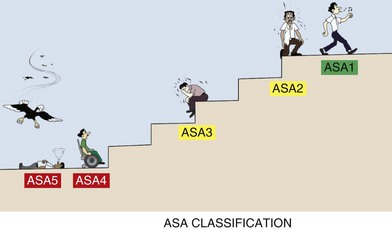
In the discussion of the ASA categories to follow, the term normal or usual activity is used along with the term distress. Definitions of these terms follow: Normal or usual activity is defined as the ability to climb one flight of stairs or to walk two level city blocks; distress is defined as undue fatigue, shortness of breath, or chest pain. Figure 10-7 illustrates the ASA classification system based on the ability to climb one flight of stairs.
ASA 1
A patient in the ASA 1 category is defined as normal and healthy. After reviewing the available information, the dentist determines that the patient’s heart, lungs, liver, kidneys, and central nervous system are healthy and that his or her blood pressure is below 140/90 millimeters of mercury. The patient is not unduly phobic and is younger than 60 years. A patient in the ASA 1 category is an excellent candidate for elective surgical or dental care, with minimal risk of experiencing an adverse medical event during treatment.
ASA 2
Patients in the ASA 2 category have a mild systemic disease or are healthy patients (ASA 1) who demonstrate extreme anxiety and fear toward dentistry or are older than 60 years. Patients classified as ASA 2 generally are somewhat less able to tolerate stress than are patients classified as ASA 1; however, they still are at minimal risk during dental treatment. An ASA 2 classification represents a yellow light for the dentist (proceed with caution). Elective dental care is warranted, with minimal increased risk to the patient during treatment. However, the dentist should consider possible treatment modifications.
ASA 3
A patient in the ASA 3 category has severe systemic disease that limits activity but is not incapacitating. At rest, a patient in the ASA 3 category does not exhibit signs and symptoms of distress (such as undue fatigue, shortness of breath, and chest pain); however, when stressed, physiologically or psychologically, the patient does exhibit such signs and symptoms. An example is a patient with angina who is pain free while in the waiting room but develops chest pain when seated in the dental chair. Similar to ASA 2, the ASA 3 classification indicates that the dentist should proceed with caution. Elective dental care is not contraindicated, although the patient is at increased risk during treatment. The dentist should give serious consideration to implementing treatment modifications.
ASA 4
A patient in the ASA 4 category has an incapacitating systemic disease that is a constant threat to life. Patients with this classification have a medical problem or problems of greater significance than the planned dental treatment. The dentist postpones elective dental care until the patient’s physical condition has improved to at least an ASA 3 classification. A patient in the ASA 4 category exhibits clinical signs and symptoms of disease at rest. This classification represents a red light, a warning that the risk involved in treating the patient is too great to permit elective care. In dental emergencies, such as cases of infection or pain, clinicians should treat patients conservatively in the dental office until their medical condition improves. When possible, emergency treatment should be noninvasive, consisting of drugs such as analgesics for pain and antibiotics for infection. When the dentist believes that immediate intervention is required (e.g., incision and drainage, extraction, pulpal extirpation), it is suggested that the patient receive care in an acute care facility (i.e., a hospital) whenever possible.
ASA 5
An ASA 5 classification indicates a moribund patient not expected to survive 24 hours without surgery. Patients in this category almost always are hospitalized and terminally ill. In many institutions, these patients are not to be resuscitated if they experience respiratory or cardiac arrest (they are termed “DNR” [“Do Not Resuscitate”]. Elective dental treatment is contraindicated; however, emergency care in the realm of palliative treatment (i.e., relief of pain and/or infection) may be necessary. An ASA 5 classification is a red light with regard to dental care.
The ASA PS classification system is not meant to be inflexible; rather, it is meant to function as a relative value system based on a dentist’s clinical judgment and assessment of available relevant clinical data.40 When the dentist is unable to determine the clinical significance of one or more diseases, consultation with the patient’s physician or other medical or dental colleagues is recommended. In all cases, however, the treating dentist makes the final decision regarding whether to treat or postpone treatment. The ultimate responsibility for the health and safety of a patient lies solely with the dentist, who decides to treat or not treat the patient.
Table 10-8 summarizes the ASA physical status classification system as modified for use in dentistry.
Drug–Drug Interactions and Contraindications
Potential drug–drug interactions involving local anesthetics or vasopressors, and three relative contraindications to the administration of local anesthetics—malignant hyperthermia (malignant hyperpyrexia), atypical plasma cholinesterase, and idiopathic or congenital methemoglobinemia—are detailed in the following discussion. A fourth—allergy (an absolute contraindication)—is discussed in Chapter 18.
The importance of each potential interaction is listed in its significance rating as designed by Moore and associates.44 The rating system is defined in Box 10-5.
Drug–Drug Interactions
Amide Local Anesthetics With Inhibitors of Metabolism (e.g., Cimetidine, Lidocaine) (Significance Rating = 5)
The H2-receptor blocker cimetidine (Tagamet) modifies the biotransformation of lidocaine by competing with it for binding to hepatic oxidative enzymes. Other H2-receptor blockers, such as ranitidine and famotidine, do not inhibit lidocaine biotransformation.45,46 The net result of this interaction with cimetidine is an increase in the half-life of the circulating local anesthetic. With typical dental practice usage of local anesthetics, this interaction is of little clinical significance. The interaction between amide local anesthetics and cimetidine might be of greater clinical significance in the presence of a history of HF (ASA 3 or greater), where the percentage of cardiac output delivered to the liver falls while the percentage of cardiac output delivered to the brain increases.47 With greater blood levels of lidocaine secondary to cimetidine, and an increased percentage in blood being delivered to the brain, the risk of local anesthetic overdose is increased. Inhibition of local anesthetic metabolism has little effect on peak plasma levels of the local anesthetic when given as a single injection.48 This combination of factors—cimetidine and ASA 3 + HF—represents a relative contraindication to the use of amide local anesthetics. Minimal doses of amide local anesthetics should be administered.
Summation Interactions With Local Anesthetics (Significance Rating = 1)
Combinations of local anesthetics may be administered together without unnecessary increase in risk of development of a toxic reaction (overdose). Toxicity of local anesthetics is additive when they are administered in combination. To minimize this risk, the total dose of all local anesthetics administered should not exceed the lowest of the maximum recommended therapeutic doses (MRTD) of each of the administered local anesthetics.
Sulfonamides and Esters (Significance Rating = 5)
Ester local anesthetics, such as procaine and tetracaine, may inhibit the bacteriostatic action of the sulfonamides. With the uncommon use of sulfonamides today, along with the extremely rare administration of ester local anesthetics in dentistry, this potential drug interaction is unlikely to be noted. As a rule, ester local anesthetics should not be administered to patients receiving sulfonamides.
Local Anesthetics With Opioid Sedation (Significance Rating = 1)
Sedation with opioid analgesics may increase the risk of local anesthetic overdose. This is of primary concern in younger, lighter-weight children. Therefore the dosage of local anesthetic should, as always, be minimized.
Local Anesthetic–Induced Methemoglobinemia (Significance Rating = 4)
Methemoglobin may result when prilocaine is administered in excessive dosages.49 Local anesthetic–induced methemoglobinemia is discussed later in this chapter.
Vasoconstrictor and Tricyclic Antidepressant (e.g., Levonordefrin and Amitriptyline) (Significance Rating = 1)
Tricyclic antidepressants (TCAs) are commonly prescribed in the management of major depression. TCAs may enhance the cardiovascular actions of exogenously administered vasopressors. This enhancement of activity is approximately fivefold to tenfold with levonordefrin and norepinephrine, but is only twofold with epinephrine and phenylephrine.50 This interaction has been reported to have resulted in a series of hypertensive crises, one of which led to the death of a patient (after a small dose of norepinephrine [norepinephrine is not available in dental local anesthetics in North America]).51 Administration of norepinephrine and levonordefrin should be avoided in patients receiving TCAs. Patients receiving epinephrine-containing local anesthetics should be administered the smallest effective dose. Yagiela and associates recommend limiting the epinephrine dose to patients receiving TCAs in a dental appointment to 0.05 mg or 5.4 mL of a 1 : 100,000 epinephrine concentration.52 Commonly prescribed TCAs are listed in Box 10-6.
Vasoconstrictors and Nonselective β-Adrenoceptor Antagonist (β-Blocker) (e.g., Propranolol and Epinephrine) (Significance Rating = 1)
Administration of vasopressors in patients being treated with nonselective β-blockers increases the likelihood of a serious elevation in blood pressure accompanied by a reflex bradycardia. Several cases have been reported in the medical literature and appear to be dose related.53,54 Reactions have occurred with epinephrine doses ranging from 0.04 to 0.32 mg, the equivalent of the administration of 4 to 32 mL of local anesthetic with a 1 : 100,000 epinephrine concentration.55 Box 10-7 lists both nonselective and cardioselective β-blockers.
Monitoring of preoperative vital signs—specifically, blood pressure, heart rate, and rhythm—is strongly recommended for all patients, but is especially recommended in patients receiving β-blockers. Re-recording these vital signs at 5 to 10 minutes after administration of a vasopressor-containing local anesthetic is strongly suggested.
Vasoconstrictor With Hydrocarbon Inhalation Anesthetic (e.g., Halothane or Enflurane and Epinephrine) (Significance Rating = 1)
There is an increased possibility of cardiac dysrhythmias when patients receiving certain halogenated general anesthetic gases are administered epinephrine.56,57 Discussion with the anesthesiologist before local anesthetic administration during general anesthesia is suggested.
Vasoconstrictor With Cocaine (Significance Rating = 1)
Cocaine is a local anesthetic drug that possesses significant stimulatory properties on the CNS and CVS. Cocaine stimulates norepinephrine release and inhibits its reuptake in adrenergic nerve terminals, thus producing a state of catecholamine hypersensitivity.58,59 Tachycardia and hypertension frequently are observed with cocaine administration, both of which increase cardiac output and myocardial oxygen requirements.60 When this results in myocardial ischemia, potentially lethal dysrhythmias, anginal pain, myocardial infarction, or cardiac arrest may ensue.61-63 The risk of such problems is elevated in dentistry when a local anesthetic containing a vasopressor is accidentally administered intravascularly in a patient with already high cocaine blood levels. After intranasal application of cocaine, peak blood levels develop within 30 minutes and usually disappear after 4 to 6 hours.64 Whenever possible, local anesthetics containing vasopressors should not be administered to patients who have used cocaine on the day of their dental appointment.65 Unfortunately, it is the rare abuser of cocaine who will volunteer this vital information to the dentist. The use of epinephrine-impregnated gingival retraction cord, although not recommended for use in any dental patient, is absolutely contraindicated in the cocaine abuser.
Administration of local anesthetics to cocaine abusers also can increase the risk of local anesthetic overdose. If there is any suspicion about a patient having used cocaine recently, the patient should be questioned directly. If cocaine has been used within 24 hours of the dental appointment, or if it is suspected that cocaine has been used within 24 hours, the planned dental treatment should be postponed.66,67
Vasoconstrictor With Antipsychotic or Another α-Adrenoceptor Blocker (Significance Rating = 4)
α-Adrenoceptor blockers such as phenoxybenzamine and prazosin (Minipress), and antipsychotic drugs such as haloperidol (Haldol) and thioridazine (Mellaril), may produce significant hypotension as a result of overdose. This hypotensive effect may be intensified with large doses of vasoconstrictors. Vasoconstrictors should be used with caution.68
Vasoconstrictor With Adrenergic Neuronal Blocker (Significance Rating = 4)
Sympathomimetic effects may be enhanced. The vasoconstrictor should be used cautiously.69 Phenothiazines are psychotropic drugs usually prescribed for the management of serious psychotic disorders. The most commonly observed side effect of phenothiazines involving the cardiovascular system is postural hypotension. Phenothiazines suppress the vasoconstricting actions of epinephrine, permitting its milder vasodilating actions to work unopposed. This response is not likely to develop when local anesthetics are administered extravascularly; however, accidental intravascular administration of a vasopressor-containing local anesthetic could lead to hypotension in patients receiving phenothiazines.67
Local anesthetics containing vasopressors are not contraindicated in patients receiving phenothiazines; however, it is recommended that the smallest volume of vasopressor-containing local anesthetic that is compatible with clinically adequate pain control be administered.
Commonly prescribed phenothiazines include chlorpromazine (Thorazine) and promethazine (Phenergan).
Vasoconstrictor With Thyroid Hormone (e.g., Epinephrine and Thyroxine) (Significance Rating = 4)
Summation of effects is possible when thyroid hormones are taken in excess. Vasoconstrictors should be used with caution when clinical signs and symptoms indicating hyperthyroidism are present.70,71
Vasoconstrictor and Monoamine Oxidase Inhibitors (Significance Rating = 5)
Monoamine oxidase inhibitors (MAOIs) are prescribed in the management of major depression, certain phobic-anxiety states, and obsessive-compulsive disorders (Box 10-8).67 They are capable of potentiating the actions of vasopressors used in dental local anesthetics by inhibiting their biodegradation by the enzyme monoamine oxidase (MAO) at the presynaptic neuron level.58
Historically, the administration of local anesthetics containing vasopressors has been absolutely contraindicated for patients receiving MAOIs because of the increased risk of hypertensive crisis. However, Yagiela and others demonstrated that such an interaction among epinephrine, levonordefrin, norepinephrine, and MAO did not occur.52,67 Such a response, hypertensive crisis, did develop with phenylephrine, a vasopressor not used at present in dental local anesthetic solutions.
Therefore, it seems appropriate to state, “there seems to be no restriction, from a theoretical basis, to use local anesthetic with vasoconstrictor other than phenylephrine in patients currently treated with MAOIs.”67
For a thorough review of potentially significant drug interactions occurring in dentistry, the reader is referred to the excellent series of papers that appeared in 1999 in the Journal of the American Dental Association.44,48,72-74
Most known drug–drug interactions involving local anesthetics or vasopressors occur with CNS and CVS depressants. Whenever a potential drug–drug interaction is known, doses of local anesthetics should be decreased. There is no formula for the correct degree of reduction. Prudence dictates, however, that the smallest dose of local anesthetic or vasopressor that is clinically effective should be used.
Knowledge of all drugs and medications, including prescription and nonprescription drugs, as well as herbal remedies, being taken by a patient better enables the doctor to evaluate the patient’s overall physical and psychological well-being. Drug references such as Mosby’s Drug Consult, Compendium of Pharmaceuticals and Specialties (CPS) (Canada), Lexi-Comp,* and Epocrates.com† are valuable resources in determining drug information, including the potential for drug–drug interactions. Current medications should be listed in the dental record.
Malignant Hyperthermia
Malignant hyperthermia (MH; malignant hyperpyrexia) is one of the most intense and life-threatening complications associated with the administration of general anesthesia. It is rare: 1 : 15,000 incidence among children receiving general anesthesia and 1 : 50,000 incidence in adults.75 The syndrome is transmitted genetically by an autosomally dominant gene. Reduced penetrance and variable expressivity in siblings of families inheriting the syndrome are also characteristic of its genetic transmission. MH is seen more frequently in males than females—a finding that increases with increasing age. To date, the youngest reported case of MH occurred in a boy aged 2 months and the oldest in a 78-year-old man.
Reports of MH in North America appear to be clustered in three regions: Toronto (in Canada) and Wisconsin and Nebraska (in the United States). Most persons with MH are functionally normal, the presence of MH becoming known only when the individual is exposed to triggering agents or through specific testing.
For many years, it was thought that MH could be triggered when susceptible patients were exposed to amide local anesthetics.76 Indeed, in both the first and second editions of this textbook, MH was considered an absolute contraindication to amide local anesthetics. However, recent findings77-79 and publications by the Malignant Hyperthermia Association of the United States (MHAUS)80 have demonstrated that amide local anesthetics are not likely to trigger such episodes; thus MH has been re-categorized as a relative contraindication in the third and subsequent editions.
Causes
All reported cases of MH (associated with drug administration) have developed during the administration of general anesthesia.81 No association with the type of surgical procedure being performed has been noted. Several cases of MH have been reported among patients receiving general anesthesia for dental care, including one case in a dental office.82,83
Anesthetic agents that have been associated with cases of MH are as follows (several of these drugs, such as lidocaine and mepivacaine, have been associated with MH only anecdotally): succinylcholine, halothane, enflurane, isoflurane, desflurane, and sevoflurane.
Two drugs have been associated with a preponderance of MH cases: succinylcholine, a skeletal muscle relaxant (77% of all cases), and the inhalation anesthetic halothane (60%).84 Of significance to dentistry is the fact that the two most commonly used (amide) local anesthetics, lidocaine and mepivacaine, had been administered along with other potential trigger agents in cases in which MH developed. At one time, a history of documented MH or a high risk of MH was considered to be an absolute contraindication to the administration of all amide local anesthetics. However, recent evidence demonstrates that MH is not a likely occurrence with amide local anesthetics as used in dentistry, and therefore should be considered a relative contraindication. The Malignant Hyperthermia Association of the United States (MHAUS; www.mhaus.org) has a policy statement on the use of local anesthetics85: “Based on limited clinical and laboratory evidence, all local anesthetic drugs appear to be safe for MH susceptible individuals.” This statement followed several reports in the literature, including one by Adragna,86 which stated, “After an extensive search of the literature, I have been unable to find any reports of any malignant hyperthermic crisis caused solely by the use of amide local anesthetics without epinephrine…In fact, lidocaine has been used successfully to treat the arrhythmias of a severe MH reaction and, in fact, lidocaine has been used routinely as a local anesthetic without problems on [MH syndrome] MHS patients in at least one institution…The question I am posing is clear. Is there any evidence that amide local anesthetics are contraindicated in MHS patients, or is our habit of avoiding them just a habit?” Because the MH syndrome has yet to be reported in a situation in which local anesthetic was the sole drug administered, it is reasonable for the dentist to manage the dental needs of such patients using amide or ester local anesthetics. Prior consultation with the patient’s physician is strongly suggested.
Adriani and Sundin reported that in susceptible patients, MH may be precipitated by factors other than the drugs just listed.87 These include emotional factors (excitement and stress) and physical factors (mild infection, muscle injury, vigorous exercise, and elevated environmental temperatures). It appears then that the dental office could be a site where the susceptible patient, exposed to excessive stresses such as pain and fear, might exhibit symptoms of MH.
Recognition of the High-Risk Malignant Hyperthermia Patient
No questions on medical history questionnaires currently used in dentistry specifically address MH. The only ones on the health history questionnaire that might elicit this information are as follows: Question No. 56: Do you have, or have you had hospitalization? Question No. 58: Do you have, or have you had surgeries? And question No. 67: Do you have, or have you had any other diseases or medical problems NOT listed on this form? The patient with MH or a family member at risk usually will volunteer this information to his or her doctor at an early visit.
Family members are usually evaluated for their risk after the occurrence of MH. Initial evaluation involves determination of the blood levels of creatinine phosphokinase (CPK).88 Elevated CPK levels are seen when muscle damage has occurred. With an elevated CPK, a second phase of evaluation is required, involving the histologic examination of a biopsy specimen taken from the quadriceps muscle (with the patient under a type of anesthesia known to be safe) and testing of the specimen for an increased contracture response when exposed to halothane and caffeine.
Dental Management of the Malignant Hyperthermia Patient
On disclosure of the presence of MH, or when the risk of its occurrence is high, it is recommended that the dentist contact the patient’s primary care physician to discuss treatment options.
Dental management on an outpatient basis with local anesthetics as the only drugs administered is indicated in most cases, but with higher-risk patients, it might be prudent to conduct such treatment within the confines of a hospital, where immediate emergency care is available should the MH syndrome be triggered. “Normal” doses of amide local anesthetics may be used with little increase in risk.85 Vasoconstrictors may be included to provide longer periods of pain control or hemostasis.
Box 10-9 lists the MHAUS list of safe anesthetic agents for MH patients.
Atypical Plasma Cholinesterase
Choline–ester substrates, such as the depolarizing muscle relaxant succinylcholine and the ester local anesthetics, are hydrolyzed in the blood by the enzyme plasma cholinesterase, which is produced in the liver. Hydrolysis of these chemicals is usually quite rapid, their blood levels decreasing rapidly, thereby terminating the drug’s action (succinylcholine) or minimizing the risk of overdose (ester local anesthetics).
Approximately 1 out of every 2820 persons possesses an atypical form of plasma cholinesterase, transmitted as an inherited autosomal recessive trait.89 Although many genetic variations of atypical plasma cholinesterase are identifiable, not all produce clinically significant signs and symptoms.
Determination
In most cases, the presence of atypical plasma cholinesterase is determined through the patient’s response to succinylcholine, a depolarizing skeletal muscle relaxant. Succinylcholine is commonly administered during the induction of general anesthesia to facilitate intubation of the trachea. Apnea is produced for a brief time with spontaneous ventilation returning as the succinylcholine is hydrolyzed by plasma cholinesterase. When atypical plasma cholinesterase is present, the apneic period is prolonged from minutes to many hours. Patient management simply involves the maintenance of controlled ventilation until effective spontaneous respiratory efforts return. After recovery, the patient and family members are tested for a serum cholinesterase survey. The dibucaine number is determined from a sample of blood. Normal patients have dibucaine numbers between 66 and 86. Atypical plasma cholinesterase patients exhibiting prolonged response to succinylcholine have dibucaine numbers as low as 20, with other genetic variants exhibiting intermediate values. Patients with low dibucaine numbers are more likely to exhibit prolonged succinylcholine-induced apnea.90
Significance in Dentistry
The presence of atypical plasma cholinesterase should alert the doctor to the increased risk of prolonged apnea in patients receiving succinylcholine during general anesthesia. Also, and of greater significance in the typical ambulatory dental patient not receiving general anesthesia or succinylcholine, is the increased risk of developing elevated blood levels of the ester local anesthetics. Signs and symptoms of local anesthetic overdose are more apt to be noted in these patients, even with “normal” dosages. Because injectable ester local anesthetics are rarely used in dentistry anymore, the presence of atypical plasma cholinesterase represents a relative contraindication to their administration. Because they undergo biotransformation in the liver, amide local anesthetics do not present an increased risk of overly high blood levels in these patients. Ester anesthetics may be administered, if deemed necessary by the doctor, but their doses should be minimized.
Methemoglobinemia
Methemoglobinemia is a condition in which a cyanosis-like state develops in the absence of cardiac or respiratory abnormalities. When the condition is severe, blood appears chocolate brown, and clinical signs and symptoms, including respiratory depression and syncope, may be noted. Death, although unlikely, can result. Methemoglobinemia may occur through inborn errors of metabolism or may be acquired through administration of drugs or chemicals that increase the formation of methemoglobin. The local anesthetic prilocaine has been shown to produce clinically significant methemoglobinemia when administered in large doses to patients with subclinical methemoglobinemia.91,92
Administration of prilocaine to patients with congenital methemoglobinemia or other clinical syndromes in which the oxygen-carrying capacity of blood is reduced should be avoided because of the increased risk of producing clinically significant methemoglobinemia. The topical anesthetic benzocaine also can induce methemoglobinemia, but only when administered in very large doses.93,94
Causes
Iron is normally present in the reduced or ferrous state (Fe++) in the hemoglobin molecule. Each hemoglobin molecule contains four ferrous atoms, each loosely bound to a molecule of oxygen. In the ferrous state, hemoglobin can carry oxygen that is available to the tissues. Because hemoglobin in the erythrocyte is inherently unstable, it is continuously being oxidized to the ferric form (Fe+++), in which state the oxygen molecule is more firmly attached and cannot be released to the tissues. This form of hemoglobin is called methemoglobin. To permit an adequate oxygen-carrying capacity in the blood, an enzyme system is present that continually reduces the ferric form to the ferrous form. In usual clinical situations, approximately 97% to 99% of hemoglobin is found in the more functional ferrous state, and 1% to 3% is found in the ferric state. This enzyme system is known commonly as methemoglobin reductase (erythrocyte nucleotide diaphorase), and it acts to reconvert iron from the ferric to the ferrous state at a rate of 0.5 g/dl/hr, thus maintaining a level of less than 1% methemoglobin (0.15 g/dl) in the blood at any given time. As blood levels of methemoglobin increase, clinical signs and symptoms of cyanosis and respiratory distress may become noticeable. In most instances, they are not observed until a methemoglobin blood level of 1.5 to 3.0 g/dl (10% to 20% methemoglobin) is reached.95
Acquired Methemoglobinemia
Although prilocaine can produce elevated methemoglobin levels, other chemicals and substances can also do this, including acetanilid, aniline derivatives (e.g., crayons, ink, shoe polish, dermatologicals), benzene derivatives, cyanides, methylene blue in large doses, nitrates (antianginals), para-aminosalicylic acid, and sulfonamides.26 Sarangi and Kumar reported the case of a fatality that occurred because of a chemically induced methemoglobinemia from writing ink.96 Daly and associates reported the case of a child born with 16% (2.3 g/dl) methemoglobin that supposedly resulted because the mother, while still pregnant, had stood with wet bare feet on a bath mat colored with aniline dye.97 In these situations, nitrates in the pen and dye were absorbed and converted to nitrites, which oxidized the ferrous atoms to ferric atoms and thus produced methemoglobinemia.
Acquired Methemoglobinemia—Prilocaine
The production of methemoglobin by prilocaine is dose related. Toluene is present in the prilocaine molecule, which as the drug is biotransformed becomes o-toluidine, a compound capable of oxidizing ferrous iron to ferric iron and of blocking the methemoglobin reductase pathways. Peak blood levels of methemoglobin develop approximately 3 to 4 hours after drug administration and persist for 12 to 14 hours.
Clinical Signs and Symptoms and Management
Signs and symptoms of methemoglobinemia usually appear 3 to 4 hours after administration of large doses of prilocaine to healthy patients, or of smaller doses in patients with the congenital disorder. Most dental patients will have left the office by this time, thus provoking a worried telephone call to the doctor. Although signs and symptoms vary with blood levels of methemoglobin, typically the patient appears lethargic and in respiratory distress; mucous membranes and nail beds will be cyanotic and the skin pale gray (ashen). Diagnosis of methemoglobinemia is made on the presentation of cyanosis unresponsive to oxygen administration and a distinctive brown color of arterial blood.86 Administration of 100% oxygen does not lead to significant improvement (ferric atoms cannot surrender oxygen to tissues). Venous blood (gingival puncture) may appear chocolate brown and will not turn red when exposed to oxygen. Definitive treatment of this situation requires the slow IV administration of 1% methylene blue (1.5 mg/kg or 0.7 mg/lb). This dose may be repeated every 4 hours if cyanosis persists or returns. Methylene blue acts as an electron acceptor in the transfer of electrons to methemoglobin, thus hastening conversion of ferric to ferrous atoms. However, methylene blue, if administered in excess, can itself cause methemoglobinemia.
Another treatment, although not as rapid-acting as methylene blue and therefore not as popular, is the IV or IM administration of ascorbic acid (100 to 200 mg/day). Ascorbic acid accelerates the metabolic pathways that produce ferrous atoms.
Methemoglobinemia should not develop in a healthy ambulatory dental patient, provided doses of prilocaine HCl remain within recommended limits. The presence of congenital methemoglobinemia remains a relative contraindication to the administration of prilocaine. Although prilocaine may be administered, if absolutely necessary, its dose must be minimized. Whenever possible, alternate local anesthetics should be used.
The maximum recommended dose of prilocaine is listed by the manufacturer as 8.0 mg/kg (3.6 mg/lb). Methemoglobinemia is unlikely to develop at doses below this level.
References
1. Daublander, M, Muller, R, Lipp, MD. The incidence of complications associated with local anesthesia in dentistry. Anesth Prog. 1997;44:132–141.
2. McCarthy, FM. Essentials of safe dentistry for the medically compromised patient. Philadelphia: WB Saunders; 1989.
3. McCarthy, FM. Stress reduction and therapy modifications. J Calif Dent Assoc. 1981;9:41–47.
4. McCarthy, FM, Malamed, SF. Physical evaluation system to determine medical risk and indicated dental therapy modifications. J Am Dent Assoc. 1979;99:181–184.
5. Berthelsen, CL, Stilley, KR. Automated personal health inventory for dentistry: a pilot study. J Am Dent Assoc. 2000;131:59–66.
6. Jacobsen, PL, Fredekind, R, Budenz, AW, et al. The medical health history in dental practice: MetLife quality resource guide. Bridgewater, NJ: MetLife; July 2003.
7. Brady, WF, Martinoff, JT. Validity of health history data collected from dental patients and patient perception of health status. J Am Dent Assoc. 1980;101:642–645.
8. Jeske AH, ed. Mosby’s dental drug reference, ed 9, St Louis: Mosby, 2009.
9. Fukuda, K. Intravenous anesthetics. In Miller RD, ed.: Miller’s anesthesia, ed 6, Philadelphia: Elsevier, 2005.
10. Skidmore-Roth, L. Mosby’s 2010 nursing drug reference. St Louis: Mosby; 2010.
11. Hamilton, JG. Needle phobia—a neglected diagnosis. J Fam Pract. 1995;41:169–175.
12. Gottlieb, SO, Flaherty, JT. Medical therapy of unstable angina pectoris. Cardiol Clin. 1991;9:19–98.
13. Little, JW. Ischemic heart disease. In Little JW, Falace DA, Miller CS, et al, eds.: Dental management of the medically compromised patient, ed 7, St Louis: Mosby, 2007.
14. Shah, KB, Kleinman, BS, Sami, H, et al. Reevaluation of perioperative myocardial infarction in patients with prior myocardial infarction undergoing noncardiac operations. Anesth Analg. 1990;71:231–235.
15. Wilson, W, Taubert, KA, Gewitz, M, et al. Prevention of infective endocarditis: guidelines from the American Heart Association: a guideline from the American Heart Association Rheumatic Fever, Endocarditis, and Kawasaki Disease Committee, Council on Cardiovascular Disease in the Young, and the Council on Clinical Cardiology, Council on Cardiovascular Surgery and Anesthesia, and the Quality of Care and Outcomes Research Interdisciplinary Working Group. Circulation. 2007;116:1736–1754.
16. American Dental Association, American Academy of Orthopedic Surgeons. Antibiotic prophylaxis for dental patients with total joint replacements. J Am Dent Assoc. 2003;134:895–898.
17. Public Relations Department, American Academy of Orthopedic Surgeons. Information statement 1033: antibiotic prophylaxis for bacteremia in patients with joint replacements. Rosemont, Ill: American Academy of Orthopedic Surgeons; February 2009. [Revised June 2010].
18. National Collaborating Centre for Chronic Conditions, Chronic Obstructive Pulmonary Disease. National clinical guideline on management of chronic obstructive pulmonary disease in adults in primary and secondary care. Thorax. 2004;59(Suppl 1):1–232.
19. Yakahane, Y, Kojima, M, Sugai, Y, et al. Hepatitis C virus infection in spouses of patients with type C chronic liver disease. Ann Intern Med. 1994;120:748–752.
20. Chafen, JJ, Newberry, SJ, Riedl, MA, et al. Diagnosing and managing common food allergies: a systematic review. JAMA. 2010;303:1848–1856.
21. Haas, DA. An update on local anesthetics in dentistry. J Can Dent Assoc. 2002;68:546–551.
22. Yagiela, JA, Injectable and topical local anesthetics. ADA/PDR guide to dental therapeutics, ed 5. . American Dental Association: Chicago, 2010.
23. Jackson, D, Chen, AH, Bennett, CR. Identifying true lidocaine allergy. J Am Dent Assoc. 1994;125:1362–1366.
24. Shojaei, AR, Haas, DA. Local anesthetic cartridges and latex allergy: a literature review. J Can Dent Assoc. 2002;68:622–626.
25. Seidel HM, Ball JW, Dains J, eds. Mosby’s guide to physical examination. St Louis: CV Mosby, 2012.
26. Wilburn-Goo, D, Lloyd, LM. When patients become cyanotic: acquired methemoglobinemia. J Am Dent Assoc. 1999;130:826–831.
27. Hersh, EV, Moore, PA, Papas, AS, et al. and the Soft Tissue Anesthesia Recovery Group: Reversal of soft tissue local anesthesia with phentolamine mesylate. J Am Dent Assoc. 2008;139:1080–1093.
28. Malamed, SF. Reversing local anesthesia. Inside Dent. 2008;4:2–3.
29. DerMarderosian A, Beutler JA, eds. The review of natural products. St Louis: Facts and Comparisons, 2005.
30. Fetrow, CH, Avila, JR. Professional’s handbook of complementary and alternative medicine. Philadelphia: Lippincott Williams & Wilkins; 2003.
31. 2011 Physicians’ desk reference, ed 65. Medical Economics: Oradell, NJ, 2011.
31a. Gruenwald J, Brendler T, Jaenicke C, eds. 2011 Physicians’ desk reference for herbal medicines. Oradell, NJ: Medical Economics, 2011.
32. American Dental Association. ADA/PDR guide to dental therapeutics, ed 5. Chicago: The Association; 2010.
32a. Smith, DM, Lombardo, JA, Robinson, JB. The preparticipation evaluation, primary care. Clin Off Pract. 1991;18:777–807.
33. American Heart Association. Recommendations for human blood pressure determination by sphygmomanometry. Dallas: The Association; 1967.
34. Pickering, TG, Hall, JE, Appel, LJ, et al. Recommendations for blood pressure measurement in humans and experimental animals. Part 1. Blood pressure measurement in humans: a statement for professionals from the Subcommittee of Professional and Public Education of the American Heart Association Council on High Blood Pressure Research. Hypertension. 2005;45:142–161.
35. Mitchell, PT, Parlin, RW, Blackburn, H. Effect of vertical displacement of the arm on indirect blood pressure measurement. N Engl J Med. 1964;271:72–74.
36. Wonka, F, Thummler, M, Schoppe, A. Clinical test of a blood pressure measurement device with a wrist cuff. Blood Press Monit. 1996;1:361–366.
37. Malamed, SF. Prevention. In Malamed SF, ed.: Medical emergencies in the dental office, ed 6, St Louis: Mosby Elsevier, 2007.
38. Little, JW, Falace, DA, Miller, CS, et al. Dental management of the medically compromised patient, ed 7. St Louis: Mosby; 2007.
39. Seidel, HM, Ball JW, Dains J, eds. Mosby’s guide to physical examination. St Louis: CV Mosby, 2006.
40. McCarthy, FM, Malamed, SF. Physical evaluation system to determine medical risk and indicated dental therapy modifications. J Am Dent Assoc. 1979;99:181–184.
41. American Society of Anesthesiologists. New classification of physical status. Anesthesiology. 1963;24:111.
42. Lagasse, RS. Anesthesia safety: model or myth? A review of the published literature and analysis of current original data. Anesthesiology. 2002;97:1609–1617.
43. Fleisher, LA. Risk of anesthesia. In Miller RD, Fleisher LA, Johns RA, eds.: Miller’s anesthesia, ed 6, New York: Churchill Livingstone, 2005.
44. Moore, PA, Gage, TW, Hersh, EV, et al. Adverse drug interactions in dental practice: professional and educational implications. J Am Dent Assoc. 1999;130:17–54.
45. Kishikawa, K, Namiki, A, Miyashita, K, et al. Effects of famotidine and cimetidine on plasma levels of epidurally administered lignocaine. Anaesthesia. 1990;45:719–721.
46. Wood, M. Pharmacokinetic drug interactions in anaesthetic practice. Clin Pharmacokinet. 1991;21:85–307.
47. Wu, FL, Razzaghi, A, Souney, PE. Seizure after lidocaine for bronchoscopy: case report and review of the use of lidocaine in airway anesthesia. Pharmacotherapy. 1993;13:12–78.
48. Moore, PA. Adverse drug interactions in dental practice: interactions associated with local anesthetics, sedatives and anxiolytics. Part IV of a series. J Am Dent Assoc. 1999;130:441–554.
49. Wilburn-Goo, D, Lloyd, LM. When patients become cyanotic: acquired methemoglobinemia. J Am Dent Assoc. 1999;130:26–31.
50. Jastak, JT, Yagiela, JA. Vasoconstrictors and local anesthesia: a review and rational use. J Am Dent Assoc. 1983;107:623–630.
51. Boakes, AJ, Laurence, DR, Lovel, KW, et al. Adverse reactions to local anesthetic vasoconstrictor preparations: a study of the cardiovascular responses to xylestesin and hostcain with noradrenalin. Br Dent J. 1972;133:137–140.
52. Yagiela, JA, Duffin, SR, Hunt, LM. Drug interactions and vasoconstrictors used in local anesthetic solutions. Oral Surg. 1985;59:565–571.
53. Hansbrough, JF, Near, A. Propranolol-epinephrine antagonism with hypertension and stroke. Ann Intern Med. 1980;92:717. [(letter)].
54. Kram, J, Bourne, HR, Melmon, KL, et al. Propranolol. Ann Intern Med. 1974;80:282. [(letter)].
55. Foster, CA, Aston, SJ. Propranolol-epinephrine interaction: a potential disaster. Reconstr Surg. 1983;72:74–78.
56. Ghoneim, MM. Drug interactions in anaesthesia: a review. Can Anaesthet Soc J. 1971;18:353–375.
57. Reichle, FM, Conzen, PF. Halogenated inhalational anaesthetics: best practice and research. Clin Anaesthesiol. 2003;17:19–46.
58. Hardman JG, Limbird LE, eds. Goodman and Gilman’s the pharmacological basis of therapeutics, ed 10, New York: McGraw-Hill, 2001.
59. Hoffman, BB, Lefkowitz, RJ, Taylor, P, Neurotransmission: the autonomic and somatic motor nervous systems. Goodman and Gilman’s the pharmacological basis of therapeutics, ed 9. . McGraw-Hill: New York, 1996.
60. Benzaquen, BS, Cohen, V, Eisenberg, MJ. Effects of cocaine on the coronary arteries. Am Heart J. 2001;142:302–410.
61. Gradman, AH. Cardiac effects of cocaine: a review. Biol Med. 1988;61:137–141.
62. Vasica, G, Tennant, CC. Cocaine use and cardiovascular complications. Med J Austral. 2002;177:260–262.
63. Hahn, IH, Hoffman, RS. Cocaine use and acute myocardial infarction. Emerg Med Clin North Am. 2001;19:493–510.
64. Myerburg, RJ. Sudden cardiac death in persons with normal (or near normal) hearts. Am J Cardiol. 1997;79:3–9.
65. Van Dyke, D, Barash, PG, Jatlow, P, et al. Cocaine: plasma concentrations after intranasal application in man. Science. 1976;191:859–861.
66. Friedlander, AH, Gorelick, DA. Dental management of the cocaine addict. Oral Surg. 1988;65:45–48.
67. Perusse, R, Goulet, J-P, Turcotte, J-Y. Contraindications to vasoconstrictors in dentistry. Part III. Pharmacologic interactions. Oral Surg Oral Med Oral Pathol. 1992;74:592–697.
68. Debruyne, FM. Alpha blockers: are all created equal? Urology. 2000;56(5 Suppl 1):20–22.
69. Emmelin, N, Engstrom, J. Supersensitivity of salivary glands following treatment with bretylium or guanethidine. Br J Pharmacol Chemother. 1961;16:15–319.
70. McDevitt, DG, Riddel, JG, Hadden, DR, et al. Catecholamine sensitivity in hyperthyroidism and hypothyroidism. Br J Clin Pharmacol. 1978;6:97–301.
71. Johnson, AB, Webber, J, Mansell, P, et al. Cardiovascular and metabolic responses to adrenaline infusion in patients with short-term hypothyroidism. Clin Endocrinol. 1995;43:647–751.
72. Yagiela, JA. Adverse drug interactions in dental practice: interactions associated with vasoconstrictors. Part V of a series. J Am Dent Assoc. 1999;130:501–709.
73. Hersh, EV. Adverse drug interactions in dental practice: interactions involving antibiotics. Part II of a series. J Am Dent Assoc. 1999;130:236–251.
74. Haas, DA. Adverse drug interactions in dental practice: interactions associated with analgesics. Part III of a series. J Am Dent Assoc. 1999;130:397–407.
75. Rosenberg, H, Fletcher, JE. An update on the malignant hyperthermia syndrome. Ann Acad Med Singapore. 1994;23(Suppl 6):84–97.
76. Carson, JM, Van Sickels, JE. Preoperative determination of susceptibility to malignant hyperthermia. J Oral Maxillofac Surg. 1982;40:432–435.
77. Gielen, M, Viering, W. 3-in-1 lumbar plexus block for muscle biopsy in malignant hyperthermia patients: amide local anaesthetics may be used safely. Acta Anaesthesiol Scand. 1986;30:581–583.
78. Paasuke, RT, Brownell, AKW. Amine local anaesthetics and malignant hyperthermia. Can Anaesth Soc J. 1986;33:126–129. [(editorial)].
79. Ording, H. Incidence of malignant hyperthermia in Denmark. Anesth Analg. 1985;64:700–704.
80. Malignant Hyperthermia Association of the United States. Anesthetic list for MH-susceptible patients. www.mhaus.org. [Accessed September 9, 2011].
81. Jurkat-Rott, K, McCarthy, T, Lehmann-Horn, F. Genetics and pathogenesis of malignant hyperthermia. Muscle Nerve. 2000;23:1–17.
82. Steelman, R, Holmes, D. Outpatient dental treatment of pediatric patients with malignant hyperthermia: report of three cases. ASDC J Dent Child. 1992;59:12–65.
83. Amato, R, Giordano, A, Patrignani, F, et al. Malignant hyperthermia in the course of general anesthesia in oral surgery: a case report. J Int Assoc Dent Child. 1981;12:15–28.
84. The European Malignant Hyperpyrexia Group. A protocol for the investigation of malignant hyperpyrexia (MH) susceptibility. Br J Anaesth. 1984;56:1267–1269.
85. Malignant Hyperthermia Association of the United States. MHAUS Professional Advisory Council adopts new policy statement on local anesthetics. Communicator. 1985;3:4.
86. Adragna, MG. Medical protocol by habit: avoidance of amide local anesthetics in malignant hyperthermia susceptible patients. Anesthesiology. 1985;62:99–100. [(letter)].
87. Adriani, J, Sundin, R. Malignant hyperthermia in dental patients. J Am Dent Assoc. 1984;108:180–184.
88. Kaus, SJ, Rockoff, MA. Malignant hyperthermia. Pediatr Clin North Am. 1994;41:121–237.
89. Williams, FM. Clinical significance of esterases in man. Clin Pharmacokinet. 1985;10:392–403.
90. Abernethy, MH, George, PM, Herron, JL, et al. Plasma cholinesterase phenotyping with use of visible-region spectrophotometry. Clin Chem. 1986;32(1 Pt 1):194–197.
91. Prilocaine-induced methemoglobinemia-Wisconsin, 1993. MMWR Morb Mortal Wkly Rep. 1994;43:555–657.
92. Bellamy, MC, Hopkins, PM, Hallsall, PJ, et al. A study into the incidence of methaemoglobinaemia after “three-in-one” block with prilocaine. Anaesthesia. 1992;47:1084–1085.
93. Guertler, AT, Pearce, WA. A prospective evaluation of benzocaine-associated methemoglobinemia in human beings. Ann Emerg Med. 1994;24:426–630.
94. Rodriguez, LF, Smolik, LM, Zbehlik, AJ. Benzocaine-induced methemoglobinemia: a report of a severe reaction and review of the literature. Ann Pharmacother. 1994;28:543–649.
95. Eilers, MA, Garrison, TE. General management principles. In Marx J, Hockberger R, Walls R, eds.: Rosen’s emergency medicine: concepts and clinical practice, ed 5, St Louis: Mosby, 2002.
96. Sarangi, MP, Kumar, B. Poisoning with writing ink. Indian Pediatr. 1994;31:756–857.
97. Daly, DJ, Davenport, J, Newland, MC. Methemoglobinemia following the use of prilocaine. Br J Anaesth. 1964;36:737–739.
*The ASA physical status classification system is discussed in detail later in this chapter.
*MD Consult: www.mdconsult.com.
†Lexi-Comp: www.lexi.com.
‡Epocrates: www.epocrates.com.
*Lexi-Comp (www.lexi.com).
†Epocrates.com.