Systemic Complications
The therapeutic use of drugs is commonplace in dentistry, with the administration of local anesthetics considered essential whenever potentially painful procedures are contemplated. It is estimated (conservatively) that dental professionals in the United States administer in excess of 6 million dental cartridges per week, or more than 300 million per year.
Local anesthetics are extremely safe drugs when used as recommended. However, whenever any drug, including local anesthetics, is used, the potential for unwanted and undesirable responses exists. In this chapter, systemic adverse reactions to drugs in general, and local anesthetics in particular, are reviewed.
Several general principles of toxicology (the study of the harmful effects of chemicals or drugs on biological systems) are presented to further an understanding of the material in this chapter.
Harmful effects of drugs range from those that are inconsequential to the patient and entirely reversible once the drug is withdrawn, to those that are uncomfortable but not seriously harmful, to those that can seriously incapacitate or prove fatal to the patient.
Whenever any drug is administered, two types of actions may be observed: (1) desirable actions, which are clinically sought and usually beneficial; and (2) undesirable actions, which are additional and are not sought.
• Principle 1: No drug ever exerts a single action. All drugs exert many actions, desirable and undesirable. In ideal circumstances, the right drug in the right dose is administered via the right route to the right patient at the right time for the right reason and does not produce any undesirable effects.1 This ideal clinical situation is rarely, if ever, attained, because no drug is so specific that it produces only the desired actions in all patients.
• Principle 2: No clinically useful drug is entirely devoid of toxicity. The aim of rational drug treatment is to maximize the therapeutic and to minimize the toxic effects of any given drug. No drug is completely safe or completely harmful. All drugs are capable of producing harm if handled improperly; conversely, any drug may be handled safely if proper precautions are observed.
• Principle 3: The potential toxicity of a drug rests in the hands of the user. A second factor in the safe use of drugs (after the drug itself) is the person to whom the drug is being administered. Individuals react differently to the same stimulus. Therefore, patients vary in their reactions to a drug. Before administering any drug, the doctor must ask the patient specific questions about his or her medical and drug history. Physical evaluation and the ensuing dialogue history related to local anesthetic administration are presented in Chapters 4 and 10.
Classification of Adverse Drug Reactions
Classifying adverse drug reactions, in the past, has been the object of much confusion; reactions were labeled as side effects, adverse experiences, drug-induced disease, diseases of medical progress, secondary effects, and intolerance. The term adverse drug reaction (ADR) is preferred at this time.
Box 18-1 outlines the three major methods by which drugs produce adverse reactions.
Overdose reactions, allergy, and idiosyncrasy are important topics in relation to local anesthetics and pain control in dentistry. A brief overview of each is presented, followed by an in-depth look at overdose and allergy.
Overdose reactions are those clinical signs and symptoms that manifest as a result of an absolute or relative overadministration of a drug, which leads to elevated blood levels of the drug in its target organs (places in the body where the drug exerts a clinical action). Signs and symptoms of overdose are related to direct extension of the normal pharmacologic actions of the drug in its target organs. Local anesthetics are drugs that act to depress excitable membranes (e.g., the central nervous system [CNS] and myocardium are the target organs for local anesthetics). When administered properly and in therapeutic dosages, they cause little or no clinical evidence of CNS or cardiovascular system (CVS) depression. However, signs and symptoms of selective CNS and CVS depression develop with increased blood levels in the cerebral circulation or myocardium. Toxic reaction is a synonym for overdose. Toxins are poisons. All drugs are poisons when administered to excess, thus the term toxic reaction.
Allergy is a hypersensitive state acquired through exposure to a particular allergen (a substance capable of inducing altered bodily reactivity), re-exposure to which brings about a heightened capacity to react. Clinical manifestations of allergy vary and include the following:
In stark contrast to the overdose reaction, in which clinical manifestations are related directly to the normal pharmacology of the causative agent, the clinically observed reaction in allergy is always produced by an exaggerated response of the patient’s immune system. Allergic responses to a local anesthetic, an antibiotic, latex, shellfish, bee sting, peanuts, or strawberries are produced by the same mechanism and may present clinically similar signs and symptoms. All allergies require the same basic management. Overdose reactions to these substances appear clinically dissimilar, necessitating entirely different modes of emergency management.
Another point of contrast between overdose and allergy relates to the amount of “drug” necessary to produce or provoke the reaction. For an overdose reaction to develop, a large enough amount of the drug must be administered to result in excessive blood levels in the drugs target organ(s). Overdose reactions are dose related. In addition, the degree of intensity (severity) of the clinical signs and symptoms relates directly to the blood level of the drug. The greater the dose administered, the higher the blood level, and the more severe the reaction. By contrast, allergic reactions are not dose related. A large dose of a drug administered to a nonallergic patient does not provoke an allergic response, whereas a minuscule amount (e.g., 0.1 mL or less) of a drug to which the patient is allergic can provoke life-threatening anaphylaxis.
Idiosyncrasy, the third category of true adverse drug reactions, is a term used to describe a qualitatively abnormal, unexpected response to a drug, differing from its usual pharmacologic actions and thus resembling hypersensitivity. However, idiosyncrasy does not involve a proven, or even suspected, allergic mechanism. A second definition considers an idiosyncratic reaction to be any adverse response that is neither overdose nor an allergic reaction. An example is stimulation or excitation that develops in some patients after administration of a CNS-depressant drug (e.g., a histamine blocker). Unfortunately, it is virtually impossible to predict which persons will have idiosyncratic reactions or the nature of the resulting idiosyncrasy.
It is thought that virtually all instances of idiosyncratic reaction have an underlying genetic mechanism. These aberrations remain undetected until the individual receives a specific drug, which then produces its bizarre (nonpharmacologic) clinical expression.
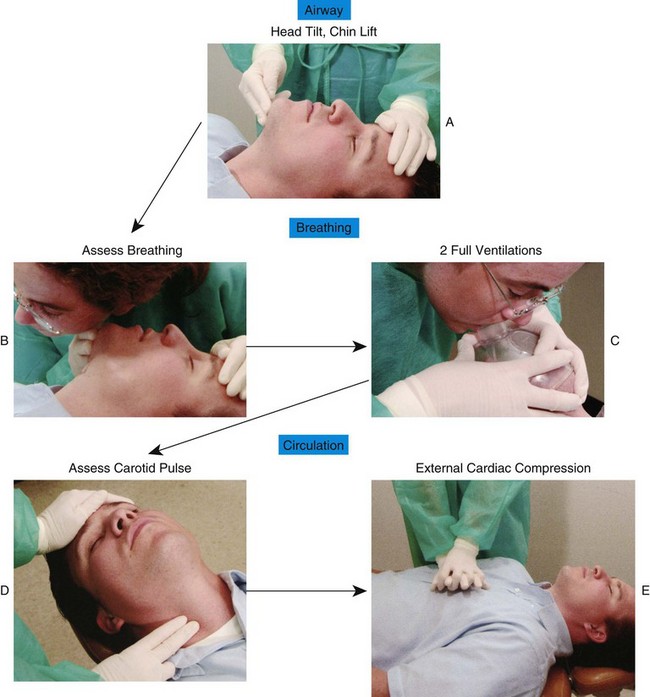
Specific management of idiosyncratic reactions is difficult to discuss because of the unpredictable nature of the response. Treatment is necessarily symptomatic and includes positioning, airway, breathing, circulation, and definitive care.
Table 18-1 compares allergy versus overdose.
Overdose
A drug overdose reaction is defined as those clinical signs and symptoms that result from an overly high blood level of a drug in various target organs and tissues. Overdose reactions are the most common of all true ADRs, accounting for up to 99% in some estimates.2
For an overdose reaction to occur, the drug first must gain access to the circulatory system in quantities sufficient to produce adverse effects on various tissues of the body. Normally, both constant absorption of the drug from its site of administration into the circulatory system and steady removal of the drug from the blood as it undergoes redistribution (e.g., to skeletal muscle and fat) and biotransformation in other parts of the body (e.g., liver) are noted. Overly high drug levels in the blood and target organs rarely occur (Fig. 18-1) in this situation.
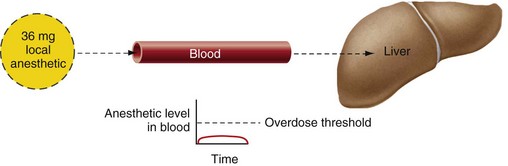
Figure 18-1 Under normal conditions, both constant absorption of local anesthetic from the site of deposition into the cardiovascular system and constant removal of the drug from the blood by the liver occur. Local anesthetic levels in the blood remain low and below the threshold for overdose.
However, this “steady state” can be altered in various ways, leading to rapid or more gradual elevation of the drug’s blood level. In either case, a drug overdose reaction is caused by a level of a drug in the blood that is sufficiently high to produce adverse effects in various organs and tissues of the body in which the drug exerts a clinical action (these are termed the target organs of the drug). The reaction continues for only as long as the blood level of the drug in the target organs remains above its threshold for overdose.
Predisposing Factors
Overdose to local anesthetics is related to the blood level of the local anesthetic that occurs in certain tissues after the drug is administered. Many factors influence the rate at which this level is elevated and the length of time it remains elevated. The presence of one or more of these factors predisposes the patient to the development of overdose. The first group of factors relates to the patient, the second group to the drug and the area into which the drug is administered (Box 18-2).
Patient Factors
Age: Although ADRs, including overdose, can occur in persons of any age, individuals at both ends of the age spectrum experience a higher incidence of such reactions.3-8 The functions of absorption, metabolism, and excretion may be imperfectly developed in very young persons and may be diminished in older-old persons, thereby increasing the half-life of the drug, elevating circulating blood levels, and increasing the risk of overdose.9
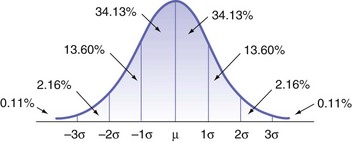
Weight: The greater the (lean) body weight of a patient (within certain limits), the larger the dose of a drug that can be tolerated before overdose reactions occur (providing the patient responds “normally” to the drug). Most drugs are distributed evenly throughout the body. Larger individuals have a greater blood volume and consequently a lower level of the drug per milliliter (mL) of blood. Maximum recommended doses (MRDs) of local anesthetics normally are calculated on the basis of milligram of drug per kilogram or pound of body weight. One of the major factors involved in producing local anesthetic overdose in the past was lack of consideration of this extremely important factor. Determination of maximum doses according to milligram per kilogram or milligram per pound of body weight is based on the responses of the “normal-responding” patient, which are calculated from the responses of many thousands of patients. An individual patient’s response to drug administration, however, may demonstrate significant variation. The normal distribution curve (Fig. 18-2) illustrates this fact. The usual cerebral blood level of lidocaine necessary to induce seizure activity is approximately 7.5 µg/mL. However, patients on the hyporesponding side of this curve may not convulse until a significantly higher brain–blood level is reached, whereas others (hyperresponders) may convulse at a brain–blood level considerably lower than 7.5 µg/mL.
Other Medications: Administration of concomitant medications may influence local anesthetic drug levels. Patients taking meperidine (Demerol), phenytoin (Dilantin), quinidine (an antidysrhythmic), or desipramine (a tricyclic antidepressant) have increased local anesthetic blood levels and thus may experience toxic actions of the local anesthetic at lower administered doses because of protein binding competition. The H2-histamine blocker cimetidine slows the biotransformation of lidocaine by competing with the local anesthetic for hepatic oxidative enzymes, leading to somewhat elevated lidocaine blood levels.10-12
Sex: Studies in animals have shown that sex is a factor in drug distribution, response, and metabolism, although it is not of major significance in humans. In humans, the only instance of sexual difference affecting a drug response is pregnancy. During pregnancy, renal function may be disturbed, leading to impaired excretion of certain drugs, their accumulation in the blood, and increased risk of overdose. However, local anesthetic seizure thresholds for the fetus, newborn, and mother are significantly different.11-15 In the adult woman, the seizure threshold is reported to be 5.8 mg/kg, in the newborn 18.4 mg/kg, and in the fetus 41.9 mg/kg. This is thought to be a result of the efficient placental clearance of lidocaine into the mother’s plasma.
Presence of Disease: Disease may affect the ability of the body to transform a drug into an inactive by-product. Hepatic and renal dysfunction impairs the body’s ability to break down and excrete the local anesthetic, leading to an increased anesthetic blood level, whereas heart failure decreases liver perfusion (the volume of blood flowing through the liver during a specific period), thereby increasing the half-lives of amide local anesthetics and increasing the risk of overdose.16,17
Genetics: Genetic deficiencies may alter a patient’s response to certain drugs. A genetic deficiency in the enzyme serum pseudocholinesterase (serum cholinesterase, plasma pseudocholinesterase, plasma cholinesterase) is an important example. This enzyme, produced in the liver, circulates in the blood and is responsible for biotransformation of the ester local anesthetics. A deficiency in this enzyme quantitatively or qualitatively can prolong the half-life of an ester local anesthetic, thereby increasing its blood level. Approximately 1 in 2820 individuals, or 6% to 7% of patients in most surgical populations, possesses atypical serum pseudocholinesterase.18
Mental Attitude and Environment: A patient’s psychological attitude influences the ultimate effect of a drug. Although of greater importance with regard to antianxiety or analgesic drugs, it is also important with regard to local anesthetics. Psychological attitude affects the patient’s response to various stimuli. The apprehensive patient who overreacts to stimulation (experiencing pain when gentle pressure is applied) is more likely to receive a larger dose of local anesthetic, which would seemingly increase his or her risk of local anesthetic overdose. However, a recent study in rats demonstrated that stress-induced changes in arterial carbon dioxide tension (decreased paCO2) and in partial pressure of oxygen in arterial blood (increased paO2) significantly raised the seizure threshold for both lidocaine and articaine.19 Stress significantly increased the latency period for the first tonic–clonic seizure induced by toxic doses of both lidocaine and articaine.19
Drug Factors
Vasoactivity: All local anesthetics currently used by injection in dentistry are vasodilators. Injection into soft tissues increases perfusion in the area, leading to an increased rate of drug absorption from the site of injection into the cardiovascular system. This causes two undesirable effects: a shorter duration of clinical anesthesia and an increased blood level of the local anesthetic.
Concentration: The greater the concentration (percent solution injected) of the local anesthetic administered, the greater the number of milligrams per milliliter of solution and the greater the circulating blood volume of the drug in the patient. For example, 1.8 mL of a 4% solution is 72 mg of the drug, but 1.8 mL of a 2% solution represents only 36 mg. If the drug is clinically effective as a 2% concentration, higher concentrations should not be used. The lowest concentration of a given drug that is clinically effective should be selected for use. For commonly used local anesthetics in dentistry, these “ideal” concentrations have been determined and are represented in the commercially available forms of these drugs.
Dose: The larger the volume of a local anesthetic administered, the greater the number of milligrams injected and the higher the resulting circulating blood level. The smallest dose of a given drug that is clinically effective should be administered. For each of the injection techniques discussed in this book, a recommended dose has been presented. Where possible, this dose should not be exceeded. Although “dental” doses of local anesthetics are relatively small compared with those used in many nondental nerve blocks, significantly high blood levels of the local anesthetic can be achieved in dental situations because of the greater vascularity of the intraoral injection site or inadvertent intravascular injection.
Route of Administration: Local anesthetics, when used for pain control, exert their clinical effects in the area of deposition. Ideally then, a local anesthetic drug should not enter into the cardiovascular system. Almost all other therapeutic agents must enter the CVS and achieve a minimum therapeutic blood level before their clinical action(s) occur. Local anesthetics administered for antidysrhythmic purposes must reach such a therapeutic blood level to be effective. Indeed, one factor involved in terminating pain control by a local anesthetic consists of its diffusion out of the nerve tissue and its subsequent entry into the CVS and removal from the site of deposition.
A factor in local anesthetic overdose in dentistry is “inadvertent” intravascular injection. Extremely high drug levels can be obtained in a short time, leading to serious overdose reactions.
Absorption of local anesthetics through oral mucous membranes is also potentially dangerous because of the rate at which some topically applied anesthetics enter the circulatory system. Lidocaine HCl and tetracaine HCl are absorbed well after topical application to mucous membranes. Benzocaine, which is not water soluble, is poorly absorbed.
Rate of Injection: The rate at which a drug is injected is a very important factor in the causation or prevention of overdose reactions. (According to the author, rate of injection is the single most important factor.) Whereas intravascular injection may or may not produce signs and symptoms of overdose (indeed, lidocaine is frequently administered intravenously in doses of 1.0 to 1.5 mg/kg to treat ventricular ectopy), the rate at which the drug is injected is a major factor in determining whether drug administration will prove clinically safe or hazardous. Malagodi and associates demonstrated that the incidence of seizures with etidocaine went up when the rate of intravenous (IV) infusion was increased.20
Rapid IV administration (15 seconds or less) of 36 mg of lidocaine produces greatly elevated levels and virtually ensures an overdose reaction. Slow (60-second or more) IV administration produces significantly lower levels in the blood, with a lesser risk that a severe overdose reaction will develop.
Vascularity of the Injection Site: The greater the vascularity of the injection site, the more rapid the absorption of the drug from that area into the circulation. Unfortunately (as regards local anesthetic overdose) for dentistry, the oral cavity is one of the most highly vascular areas of the entire body. However, some areas within the oral cavity are less well perfused (e.g., the site for the Gow-Gates nerve block), and these usually are more highly recommended than other, better-perfused, sites (e.g., those for the inferior alveolar or posterior superior alveolar nerve block).
Presence of Vasoconstrictors: The addition of vasoconstrictor to a local anesthetic produces a decrease in the perfusion of an area and a decreased rate of systemic absorption of the drug. This, in turn, decreases the clinical toxicity of the local anesthetic (see Table 3-1).
Causes
Elevated blood levels of local anesthetics may result from one or more of the following:
1. Biotransformation of the drug is unusually slow.
2. The unbiotransformed drug is too slowly eliminated from the body through the kidneys.
3. Too large a total dose is administered.
Biotransformation and Elimination
Ester local anesthetics, as a group, undergo more rapid biotransformation in the liver and blood than the amides. Plasma pseudocholinesterase is primarily responsible for their hydrolysis to para-aminobenzoic acid.
Atypical pseudocholinesterase occurs in approximately 1 out of every 2820 individuals, or 6% to 7% of patients in a surgical population.18 Patients with a familial history of this disorder may be unable to biotransform ester agents at the usual rate, and subsequently, higher levels of ester anesthetics may develop in their blood.
Atypical pseudocholinesterase represents a relative contraindication to the administration of ester local anesthetics. Amide local anesthetics may be used without increased risk of overdose in patients with pseudocholinesterase deficiency.
Amide local anesthetics are biotransformed in the liver by hepatic microsomal enzymes. A history of liver disease, however, does not absolutely contraindicate their use. In an ambulatory patient with a history of liver disease (American Society of Anesthesiologists [ASA] Physical Status classification system 2 or 3), amide local anesthetics may be used judiciously (relative contraindication) (Fig. 18-3).
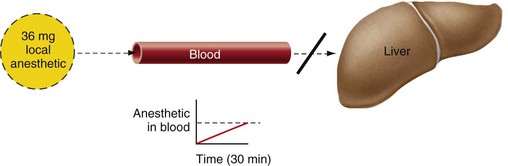
Figure 18-3 In patients with significant liver dysfunction, removal of a local anesthetic from the blood may be slower than its absorption into the blood, leading to a slow but steady rise in the blood anesthetic level.
Minimum effective volumes of anesthetic should be used. Average, even low-average, doses may be capable of producing an overdose if liver function is compromised to a great enough degree (ASA 4 or 5); however, this situation is unlikely to occur in an ambulatory patient.17
Renal dysfunction also can delay elimination of the active local anesthetic from the blood. A percentage of all anesthetics is eliminated unchanged through the kidneys: 2% procaine, 10% lidocaine, 5% to 10% articaine, and 1% to 15% mepivacaine and prilocaine. Renal dysfunction may lead to a gradual increase in the level of active local anesthetic in the blood.16
Excessive Total Dose
Given in excess, all drugs are capable of producing signs and symptoms of overdose (Fig. 18-4). Precise milligram dosages or the blood levels at which clinical effects are noted are impossible to predict. Biological variability has a great influence on the manner in which persons respond to drugs.
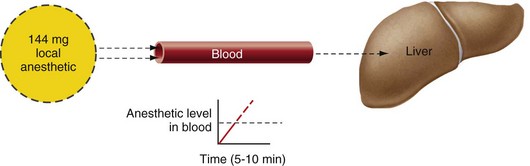
Figure 18-4 Even in a patient with normal liver function, a large dose of local anesthetic may be absorbed into the cardiovascular system more rapidly than the liver can remove it. This produces a relatively rapid elevation of the anesthetic blood level.
The MRD of parenterally administered (injected) drugs is commonly calculated after consideration of a number of factors, including the following:
1. Patient’s age. Individuals at either end of the age spectrum may be unable to tolerate normal doses, which should be decreased accordingly.
2. Patient’s physical status. For medically compromised individuals (ASA 3, 4, and 5) the calculated MRD should be decreased.
3. Patient’s weight. The larger the person (within limits), the greater is the volume of distribution of the drug. With a usual dose, the blood level of the drug is lower in the larger patient, and a larger milligram dose can be administered safely. Although this rule is generally valid, there are always exceptions; care must be exercised whenever any drug is administered.
MRDs of local anesthetics should be determined after consideration of the patient’s age, physical status, and body weight. Table 18-2 provides maximum recommended doses based on body weight for lidocaine, mepivacaine, prilocaine, and articaine.
TABLE 18-2
Maximum Recommended Doses of Local Anesthetics
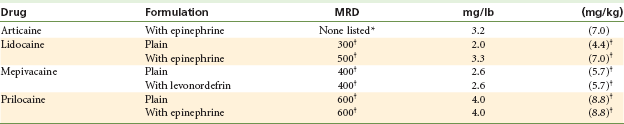
*Manufacturer’s recommendation: Prescribing information, New Castle, Del, 2000.
†Manufacturer’s recommendation: Prescribing information, dental, Westborough, Mass, 1990, Astra Pharmaceutical Products.
It is highly unlikely that the maximum figures indicated in Table 18-2 will be reached in the typical dental practice. There is rarely an occasion to administer more than three or four cartridges during a dental appointment. Regional block anesthesia is capable of obtunding the full mouth in an adult with six cartridges, and with two cartridges in the primary dentition. Yet despite this ability to achieve widespread anesthesia with minimum volumes of anesthetic, the administration of excessive volumes is the most frequently seen cause of local anesthetic overdose.21,22
Rapid Absorption Into the Circulation
Vasoconstrictors are considered an integral component of all local anesthetics whenever depth and duration of anesthesia are important. There are but few indications for the use of local anesthetics without a vasoconstrictor in dentistry. Vasoconstrictors increase both the depth and the duration of anesthesia and reduce the systemic toxicity of most local anesthetics by delaying their absorption into the CVS. Vasoconstrictors should be included in local anesthetic solutions unless specifically contraindicated by the medical status of the patient or the duration of the planned treatment.23 The American Dental Association and the American Heart Association have summarized this as follows: “Vasoconstrictor agents should be used in local anesthetic solutions during dental practice only when it is clear that the procedure will be shortened or the analgesia rendered more profound. When a vasoconstrictor is indicated, extreme care should be taken to avoid intravascular injection. The minimum possible amount of vasoconstrictor should be used.”24 Rapid absorption of local anesthetics also may occur after their application to oral mucous membranes. Absorption of some topically applied local anesthetics into the circulation is rapid, exceeded in rate only by direct intravascular injection.25 Local anesthetics designed for topical application are used in a higher concentration than formulations suitable for parenteral administration.
From the perspective of overdose, amide topical anesthetics, when applied to wide areas of mucous membrane, increase the risk of serious reactions. Benzocaine, an ester anesthetic, which is poorly, if at all, absorbed into the cardiovascular system, is less likely to produce an overdose reaction than amides, although cases of methemoglobinemia from excessive benzocaine administration have been reported.26-28 The risk of allergy (more likely with esters than amides) must be addressed before any drug is used. Serious overdose reactions have been reported after topical application of amide local anesthetics.29-32
The area of application of a topical anesthetic should be limited. There are few indications for applying a topical to more than a full quadrant (buccal and lingual/palatal) at one time. Application of an amide topical to a wide area requires a large quantity of the agent and increases the likelihood of overdose.
When a spray topical anesthetic is needed, the use of metered dosage forms is strongly recommended. Disposable nozzles for metered sprays make maintenance of sterility simpler (Fig. 18-5). Ointments or gels, if used in small amounts (as on the tip of a cotton applicator stick), may be applied with minimal risk of overdose.
Intravascular Injection
Intravascular injection may occur with any type of intraoral injection but is more likely when a nerve block is administered33:
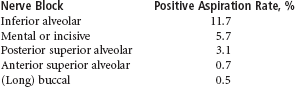
Both IV and intra-arterial (IA) injections are capable of producing overdose (Fig. 18-6). Aldrete demonstrated that a rapidly administered IA injection may cause retrograde blood flow in the artery as the anesthetic drug is deposited (Fig. 18-7).34 Intravascular injections of local anesthetic within the usual practice of dentistry should not occur. With knowledge of the anatomy of the site to be anesthetized and proper technique of aspiration before the anesthetic solution is deposited, overdose as a result of intravascular injection is minimized.
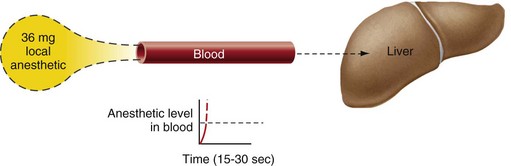
Figure 18-6 Direct rapid intravascular administration of one cartridge of local anesthesia produces marked elevation of the anesthetic blood level in a very short time.
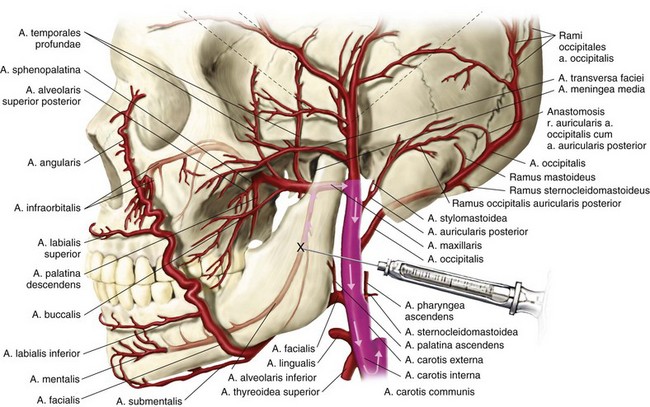
Figure 18-7 Reverse carotid blood flow. Rapid intra-arterial deposition of local anesthetic into the inferior alveolar artery (X) produces an overdose reaction. Blood flow in the arteries is reversed because of the high pressure produced by the rate of injection. Arrows indicate the path of the solution into the internal carotid artery and cerebral circulation.
Prevention: To prevent intravascular injection, use an aspirating syringe. In an unpublished survey conducted by the author, 23% of dentists questioned stated that they routinely use nonaspirating syringes to administer local anesthetics. There is no justification for the use of a nonaspirating syringe for any intraoral injection technique, because it is impossible to determine the precise location of the needle tip without aspirating.
Use a needle no smaller than 25 gauge when the risk of aspiration is high. Although aspiration of blood is possible through smaller-gauge needles, resistance to the return of blood into the lumen of smaller-gauge needles is increased, leading to an increased likelihood of an unreliable aspiration test. Therefore, injection techniques with a greater likelihood of positive aspiration dictate the use of a 25-gauge needle. A 27-gauge needle can be utilized in lieu of 25-gauge as it provides relatively reliable aspiration; however, 30-gauge needles should be avoided, if at all possible, when injections are administered into more vascular areas of the oral cavity.
Aspirate in at least two planes before injection. Figure 18-8 illustrates how an aspiration test may be negative even though the needle tip lies within the lumen of a blood vessel. The use of multiple aspiration tests before injection of solution, with the needle bevel in different planes, overcomes this potential problem. After the initial aspiration, rotate the syringe about 45 degrees to reorient the needle bevel relative to the wall of the blood vessel, and reaspirate.

Figure 18-8 Intravascular injection of local anesthetic. A, Needle is inserted into the lumen of the blood vessel. B, Aspiration test is performed. Negative pressure pulls the vessel wall against the bevel of the needle; therefore no blood enters the syringe (negative aspiration). C, Drug is injected. Positive pressure on the plunger of the syringe forces local anesthetic solution out through the needle. The wall of the vessel is forced away from the bevel, and anesthetic solution is deposited directly into the lumen of the blood vessel.
Slowly inject the anesthetic. Rapid intravascular injection of 1.8 mL of a 2% local anesthetic solution produces a blood level in excess of that necessary for overdose. Rapid injection is defined (by the author) as administration of the entire volume of a dental cartridge in 30 seconds or less. The same volume of anesthetic deposited intravascularly slowly (minimum, 60 seconds) produces slightly elevated blood levels that are still below the minimum for serious overdose (seizure). In the event that the level does exceed this minimum, onset of the reaction will be slower and signs and symptoms will be less severe than those observed after more rapid injection. Slow injection is the most important factor in preventing adverse drug reactions—it is even more important than aspiration. The ideal rate of local anesthetic administration is 1.0 mL/min. Given that many dentists administer LA more rapidly than this ideal, the recommended rate of LA administration is deposition of a 1.8-mL cartridge in not less than 60 seconds. Because the recommended volumes of local anesthetic for most intraoral injection techniques are considerably less than 1.8 mL, most injections can be administered safely (and comfortably) in less than 1 minute.
The truth about local anesthetic overdosage in dentistry35: Administration of too large an LA dose relative to the weight (and age) of the patient is the most common cause of serious local anesthetic overdose reactions in dentistry. Although some serious cases of local anesthetic overdose have occurred in adult patients,5 an overwhelming majority of problems commonly develop in the child who is young (2 to 6 years), lightweight (<30 kg [66 lb]), and well behaved; requires multiple procedures in four quadrants; and is managed in the office of an inexperienced general dentist.3
Review of many of the cases that resulted in serious morbidity or death reveals a number of shared factors, none of which in itself might pose a serious problem; however, when added together, they act to produce clinical signs and symptoms of local anesthetic overdose. These factors are presented in Box 18-3.
1. Treatment plan: In interviews with trained pediatric dentists, it has been the author’s experience that when presented with the patient described in the preceding section (young, lightweight, well behaved), the pediatric dentist (with few exceptions) will not treat all four quadrants at one visit using local anesthetic alone. Limiting treatment to one or two quadrants per visit represents a more rational approach to this patient’s needs, and enhances safety.
A dentist confronted with a (well-meaning) parent or grandparent who complains of the difficulties of getting to the dental office and the inconvenience of having to miss a half-day of work, and wanting to have the child’s dental care accomplished in one visit (not two or more), might feel pressured into agreeing to this request, thus increasing the risk for local anesthetic overdose. This is more likely to occur in offices of younger (by which I mean “inexperienced”) dentists who are developing their practice and wish to keep their patients “happy.”
2. Choice of local anesthetic: In most instances where serious LA overdose has occurred in children, the local anesthetic administered has been a “plain” drug, either mepivacaine HCl 3% (usually) or prilocaine HCl 4%. Both of these are excellent local anesthetics—when used properly. The rationale behind the clinician’s selection of a short-acting drug for children includes that (1) most pediatric appointments are of short duration, and (2) “plain” local anesthetics possess a shorter duration of residual soft tissue anesthesia, minimizing the likelihood of inadvertent soft tissue injury as the child bites or chews his or her numb lip or tongue.
As a rule, the pediatric dentist administers a “plain” local anesthetic only when treatment is limited to one quadrant. If treatment extends to two or more quadrants in one visit, a vasopressor-containing LA is selected. Prolonged posttreatment soft tissue anesthesia leads to the increased possibility of soft tissue damage; however, this risk is outweighed by benefits accrued through delayed absorption of the local anesthetic into the CVS (the risk of overdose is diminished). Postoperative soft tissue injury can be prevented in many ways, such as securing a cotton roll in the buccal fold and advising the parent to watch the child. (See Chapters 16 and 17.) Availability of the local anesthesia reversal agent—phentolamine mesylate—decreases residual soft tissue anesthesia duration significantly.36,37 Reversal of local anesthesia is discussed fully in Chapter 20.
Table 18-3 presents the local anesthetic of choice for 117 dentists who treat children.38
TABLE 18-3
Local Anesthetic of Choice for 117 Dentists Who Treat Children
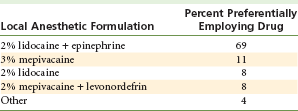
Data from Cheatham BD, Primosch RE, Courts FJ: A survey of local anesthetic usage in pediatric patients by Florida dentists, J Dent Child 59:401–407, 1992.
3. Volume of local anesthetic administered: Pain control for the entire primary dentition can be achieved with approximately two cartridges of local anesthetic. In the smaller child patient, there is rarely a compelling need to administer a 1.8-mL volume of local anesthetic in any one injection. Yet full cartridges are commonly administered when children receive local anesthetic administered by nonpediatric dentists. In many of the instances where a death resulted, a total of five, six, or seven cartridges were administered.3
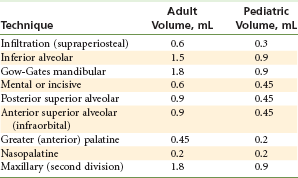
In those situations where LA must be administered to all four quadrants of a smaller child, pain control can be achieved with not more than two cartridges, as follows: one fourth of a cartridge each for the right and left incisive nerve blocks (anesthetizing all mandibular primary teeth); or one half of a cartridge each for right and left inferior alveolar nerve blocks; one quarter of a cartridge each for the right and left anterior superior alveolar nerve blocks. In lieu of the anterior superior alveolar nerve block, maxillary infiltrations may be administered with one sixth of a cartridge per injection (Table 18-4).
4. Local anesthetic administered to all four quadrants at one time: Administration, over 1 or 2 minutes, of four or more cartridges of a local anesthetic without a vasopressor to all four quadrants makes little therapeutic sense and considerably increases the risk of an overdose. Administration of local anesthetic to one quadrant, treating that area, then anesthetizing the next quadrant, and so on, makes considerably more sense from both a therapeutic and a safety perspective. For equal volumes of local anesthetic, administration over a longer time frame (e.g., 1 to 2 hours) results in a lower blood level when compared with administration of the entire dose at one time.
5. Exceeding the maximum dosage based on patient’s body weight: An important factor, especially when younger, lighter-weight patients are managed, is maximum recommended dose (MRD). Determine the weight of the patient (in kilograms [kg] or pounds [lb]) before the start of treatment. It is preferable to weigh the child on a scale, because parents frequently can offer only a rough estimate of their child’s weight (usually underestimating it). One must always remember that these figures are not absolutes. Exceeding the MRD of a drug does not guarantee that an overdose will happen (see Table 18-5 and discussion). On the other hand, administering dosages below the maximum calculated by body weight is no guarantee that adverse reactions will not be seen. The likelihood of ADRs developing is dose related. Smaller dosages minimize (but do not eliminate) this risk; larger doses increase (but do not guarantee) it.
TABLE 18-5
Maximum Recommended Dosages of Local Anesthetics
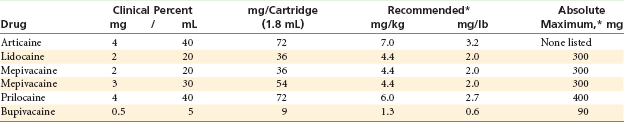
*Maximum recommended doses of local anesthetics are for local anesthetic solutions containing vasoconstrictors or without vasoconstrictors.
Maximum recommended dosages of commonly administered local anesthetics are summarized in Table 18-5.
The intrinsic safety of local anesthetics is illustrated in Table 18-6, which presents the volume of local anesthetic administered on 65 occasions by a general dentist who removed third molars from college-aged individuals.
TABLE 18-6
Local Anesthetic Administration for Removal of Third Molars
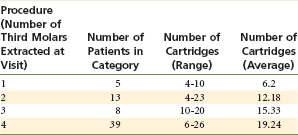
From Malamed SF: Unpublished data, 2002.
None of these patients experienced an adverse response to the local anesthetic, although many received dosages many times the MRD.39 This is one indication that local anesthetics are extremely safe drugs when administered to healthy, younger (teenage to mid-20s) adult patients. Unfortunately, when they are administered in overly large doses to younger, lightweight patients, overdose is a significant risk.
Virtually all local anesthetic overdose reactions are preventable if the clinician adheres to the very basic, simple recommendations presented in the preceding section. In the unlikely situation that an overdose reaction develops, adherence to the basic steps of emergency management will lead to a successful outcome in essentially all cases.
Clinical Manifestations
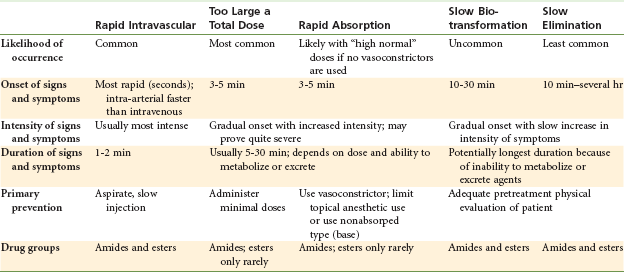
Clinical signs and symptoms of overdose appear whenever the blood level in that drug’s target organ(s) becomes overly high for that individual (Box 18-4). Target organs for local anesthetics include CNS and the myocardium. The rate of onset of signs and symptoms and, to an extent, their severity correspond to this level. Table 18-7 compares the various modes of local anesthetic overdose.
The clinical manifestations of LA overdose will persist until the anesthetic blood level in the affected organs (brain, heart) falls below the minimum value (through redistribution), or until clinical signs and symptoms are terminated through administration of appropriate drug therapy.
Pathophysiology
The blood or plasma level of a drug is the amount absorbed into the circulatory system and transported in plasma throughout the body. Levels are measured in micrograms per milliliter (µg/mL) (1000 µg equals 1 mg). Figure 18-9 illustrates clinical manifestations observed with increasing blood levels of lidocaine in the CNS and heart. Blood levels are estimates because significant individual variation can occur.
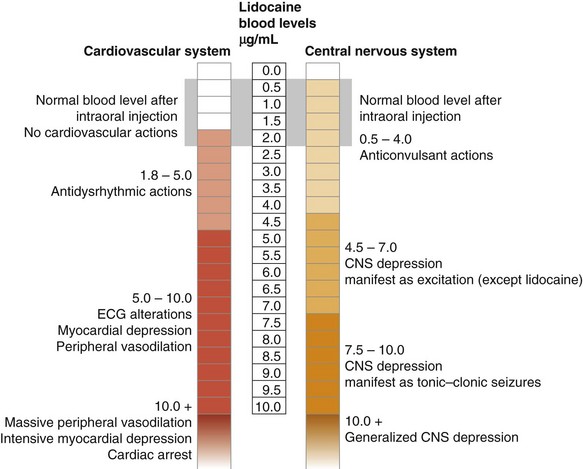
Figure 18-9 Local anesthetic blood levels and actions on cardiovascular and central nervous systems.
Local anesthetics exert a depressant effect on all excitable membranes. In the clinical practice of anesthesia, a local anesthetic is applied to a specific region of the body, where it produces its primary effect: reversible depression of peripheral nerve conduction. Other actions are related to its absorption into the circulation and its subsequent actions on excitable membranes, including smooth muscle, the myocardium, and the CNS.
Following intraoral administration of 40 to 160 mg of lidocaine, the blood level rises to a maximum of approximately 1 µg/mL. (The usual range is between 0.5 and 2 µg/mL, but remember that response to drugs varies according to the individual.) Adverse reactions to the anesthetic are extremely uncommon in most individuals at these normal blood levels.
Central Nervous System Actions
The CNS is extremely sensitive to the actions of local anesthetics. As the cerebral blood level of LA increases, clinical signs and symptoms are observed.
Local anesthetics cross the blood–brain barrier, producing CNS depression. At nonoverdose levels of lidocaine (<5 µg/mL), no clinical signs or symptoms of adverse CNS effects are noted. Indeed, therapeutic advantage may be taken at blood levels between 0.5 and 4 µg/mL, because in this range, lidocaine demonstrates anticonvulsant actions.41-43 The mechanism of this action is depression of hyperexcitable neurons found in the amygdala of seizing patients.
Signs and symptoms of CNS toxicity appear at a cerebral blood level greater than 4.5 µg/mL. Generalized cortical sensitivity is noted: agitation, talkativeness, and irritability. Tonic–clonic seizures generally occur at levels greater than 7.5 µg/mL. With further increases in the lidocaine blood level, seizure activity ceases and a state of generalized CNS depression develops. Respiratory depression and arrest (apnea) are manifestations of this. Chapter 2 describes the method through which a CNS-depressant drug, such as a local anesthetic, can produce clinical signs and symptoms of apparent CNS stimulation.
Cardiovascular System Actions
The CVS is considerably less sensitive to the actions of local anesthetics. Adverse CVS responses do not usually develop until long after adverse CNS actions have appeared.
Local anesthetics, primarily lidocaine, have been used in the management of cardiac dysrhythmias, especially ventricular extrasystoles (premature ventricular contractions [PVCs]) and ventricular tachycardia. The minimum effective level of lidocaine for this action is 1.8 µg/mL, and the maximum is 5 µg/mL—the level at which undesirable actions become more likely.44
Increased blood levels (5 to 10 µg/mL) lead to minor alterations on the electrocardiogram, myocardial depression, decreased cardiac output, and peripheral vasodilation. At levels above 10 µg/mL, these effects are intensified: primarily massive peripheral vasodilation, marked reduction in myocardial contractility, severe bradycardia, and possible cardiac arrest.45,46
Management
Management of all medical emergencies is predicated on keeping the victim alive until he or she recovers, or until help arrives on scene to take over management. With prompt implementation of the basic emergency management protocol, a local anesthetic overdose reaction will resolve within minutes. Management of the LA overdose is based on the severity of the reaction. In most cases, the reaction is mild and transitory, requiring little or no specific treatment beyond basic treatment. In other instances, however, the reaction may be more severe and longer lasting, in which case more aggressive therapy is warranted.
Most local anesthetic overdose reactions are self-limiting because the blood level in the target organs (e.g., brain and heart) continues to decrease over time as the reaction progresses and the local anesthetic is redistributed (if the heart is still pumping effectively—as it usually is). Only rarely will drugs other than oxygen be necessary to terminate a local anesthetic overdose. Whenever signs and symptoms of overdose develop, do not simply label the patient “allergic” to local anesthetics, because this will further complicate future treatment (see p. 326).
Mild Overdose Reaction
Signs and symptoms of a mild overdose include retention of consciousness, talkativeness, and agitation, along with increased heart rate, blood pressure, and respiratory rate, which usually develop slowly—approximately 5 to 10 minutes after injection(s).
Slow Onset (≥5 minutes after administration): Possible causes of reactions with a slow onset include unusually rapid absorption, and too large a total dose. Management follows the usual P→A→B→C→D algorithm used in the management of all medical emergencies. Box 18-5 summarizes basic emergency management.
Use the following protocol to deal with slow onset of symptoms.
P→A→B→C: Position the conscious patient comfortably. A, B, and C are assessed as adequate (patient is conscious and talking).
1. Reassure the patient that everything is all right and under control.
2. Administer oxygen via nasal cannula or nasal hood. This is indicated as a means of preventing acidosis, a situation during which the seizure threshold of the local anesthetic is decreased. The greater the arterial carbon dioxide tension, the lower the local anesthetic blood level necessary to induce or perpetuate tonic–clonic activity.47
3. Monitor and record vital signs. Postexcitation depression is usually mild, with little or no therapy necessary.
4. (optional) If trained and if equipment is available, establish an IV infusion. Use of anticonvulsants (e.g., midazolam) usually is not indicated at this time, although midazolam may be administered slowly intravenously and titrated at a rate of 1 mg/min if CNS stimulation appears to be intensifying toward a more severe reaction. If midazolam is administered, activate emergency medical services (dial 9-1-1).
5. Permit the patient to recover for as long as necessary. Dental care may or may not be continued after the patient’s physical and emotional status have been evaluated. The patient may leave the dental office unescorted only if you are convinced that full recovery has occurred. Vital signs should be recorded and compared with baseline values, and the patient evaluated thoroughly before discharge. If an anticonvulsant drug was administered, or if doubt exists as to the patient’s degree of recovery, do not permit the patient to leave the office alone; consider emergency medical assistance (e.g., dial 9-1-1).
Slower Onset (≥15 minutes after administration): Possible causes of reactions of a slower onset include abnormal biotransformation and renal dysfunction. Follow this protocol for dealing with the slower onset of signs and symptoms in a conscious patient.
P→A→B→C: Position the conscious patient comfortably. A, B, and C are assessed as adequate (patient is conscious and talking).
4. Administer an anticonvulsant. Overdose reactions caused by abnormal biotransformation or renal dysfunction usually progress somewhat in intensity and last longer (because the drug cannot be eliminated rapidly). If venipuncture can be performed and if equipment is available, titrate 1 mg of midazolam/min until the clinical signs and symptoms of overdose subside.
5. Summon medical assistance. When venipuncture is not practical, or when an anticonvulsant drug has been administered, seek emergency medical assistance as soon as possible. Postexcitement depression usually is moderate after a mild excitement phase. Administration of midazolam or any other anticonvulsant will intensify this depression to varying degrees. Monitoring of the patient’s status and adherence to the steps of basic life support are normally more than adequate for this situation.
6. After termination of the reaction, be sure that the patient is examined by a physician or a hospital staff member to determine possible causes. The examination could include blood tests and hepatic and renal function tests.
7. If the patient is not transported to a hospital by emergency medical services (EMS), do not let him or her leave the dental office alone. Arrangements should be made for an adult companion if hospitalization is deemed unnecessary.
8. Determine the cause of the reaction before proceeding with therapy requiring additional local anesthetics.
Severe Overdose Reaction
Rapid Onset (within 1 minute): Signs and symptoms include loss of consciousness with or without convulsions. The probable cause is intravascular injection.
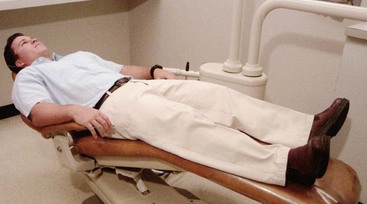
P→A→B→C: Place the unconscious patient in the supine position. A, B, and C are assessed and maintained, as necessary. Remove the syringe from the mouth (if still present), and place the patient supine with feet elevated slightly. Subsequent management is based on the presence or absence of convulsions.
D (definitive care): In the presence of tonic–clonic convulsions:
1. Protect the patient’s arms, legs, and head. Loosen tight clothing, such as ties, collars, and belts, and remove the pillow (or “doughnut”) from the headrest.
2. Immediately summon emergency medical assistance (i.e., 9-1-1).
3. Continue basic life support. Maintenance of an adequate airway and adequate ventilation are of the utmost importance during management of local anesthetic–induced tonic–clonic seizures. Increased oxygen utilization and hypermetabolism, with increased production of CO2 and lactic acid, occur during the seizure, leading to acidosis, which, in turn, lowers the seizure threshold (the blood level at which local anesthetic–induced seizures begin), prolonging the reaction.48 Cerebral blood flow during such a seizure is also increased, elevating still further local anesthetic blood levels within the CNS.
4. Administer an anticonvulsant. The blood level of the local anesthetic declines as the drug undergoes redistribution; if acidosis is not present, seizures cease usually within about 1 to 3 minutes. Anticonvulsant therapy is not indicated for most seizures. If the seizure is prolonged (4 to 5 minutes with no indication of terminating), consider administering an anticonvulsant, but only if trained in parenteral drug administration (IV, intramuscular [IM], intranasal [IN]) and ventilation of a possibly apneic patient. IV midazolam, titrated at a rate of 1 mg/min until seizures cease, is the preferred treatment.49,50 If venipuncture is not feasible, 5 mg/mL midazolam may be administered IM at a dose of 0.2 mg/kg for adult or pediatric patients.51,52 The vastus lateralis is the preferred site for IM injection. Intranasal (IN) midazolam can be administered in patients weighing less than 50 kg at a dose of 0.2 mg/kg (up to 10 mg).53 Seizures usually stop within 1 to 2 minutes after IN midazolam. Maintain basic life support, and obtain the assistance of emergency medical personnel.
Postseizure (Postictal) Phase: CNS depression is usually present at an intensity equal that of the excitation phase (Fig. 18-10). The patient may be drowsy or unconscious; breathing may be shallow or absent; the airway may be partially or totally obstructed; blood pressure and heart rate may be depressed or absent. A more intense postseizure state is noted when anticonvulsants have been administered to terminate the seizure.
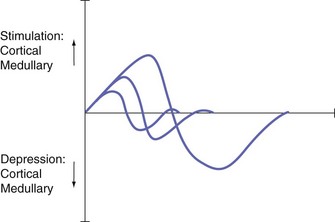
Figure 18-10 Effects of local anesthetics on the central nervous system. Notice that the intensity of depression is equal to the intensity of the preceding stimulation. (From Bennett CR: Monheim’s local anesthesia and pain control in dental practice, ed 7, St Louis, 1984, Mosby.)
P→A→B→C: Implementation of the steps of basic life support is crucial: airway, breathing, and circulation must be provided as needed. In all postictal situations, maintenance of an adequate airway is necessary; in some other cases, assisted or controlled ventilation may be indicated; for a small percentage of the most severe reactions, chest compression must be added to the first two steps of basic life support.
1. Additional management, such as use of a vasopressor (ephedrine) IM, is indicated if hypotension persists for extended periods (30 minutes). Preferred initial management for hypotension in this situation consists of positioning of the patient and administration of IV fluids.
2. Allow the patient to rest until recovery is sufficient to permit transfer to a hospital emergency department. This means a return of vital signs to baseline levels. In all situations in which local anesthetic–induced seizures occur and emergency medical services are necessary, evaluation of the patient in a hospital emergency department is necessary.
Slow Onset (5 to 15 minutes): Possible causes of severe reactions of slow onset include (1) too large a total dose, (2) rapid absorption, (3) abnormal biotransformation, and (4) renal dysfunction.
P→A→B→C: Provide basic life support (BLS) as necessary. As in the preceding protocol, prevention of acidosis and hypoxia through airway management and adequate pulmonary ventilation is of primary importance for a successful outcome.
1. Administer an anticonvulsant. If symptoms are mild at the onset but progress in severity, and if an IV line can be established, definitive treatment with IV anticonvulsants and continued oxygen administration are indicated. IM or IN midazolam may be considered when the IV route is not available.
2. Summon emergency medical assistance immediately if seizures develop.
3. Postseizure management includes BLS and IM or IV administration of a vasopressor for hypotension, as needed. Administration of IV fluids is recommended for management of hypotension.
4. Permit the patient to recover for as long as necessary before discharge to hospital. Completely evaluate the patient’s condition at future appointments before readministering a local anesthetic.
Overdose reactions are the most common “true” ADRs associated with administration of amide local anesthetics. Most overdose reactions are preventable through adequate pretreatment evaluation of the patient and sensible administration of these drugs. In the few instances in which clinical manifestations of overly high local anesthetic blood levels become evident, a successful outcome usually results if the condition is promptly recognized and the patient treated efficiently and effectively. Primary among the steps of management are maintenance of a patent airway and adequate oxygenation. Data indicate that if local anesthetic–induced seizures are brief and well managed, no permanent neurologic or behavioral sequelae remain postictally.54 In other words, ischemic CNS damage is not inevitable with well-managed, brief, local anesthetic–induced seizures.
Epinephrine Overdose
Precipitating Factors and Prevention
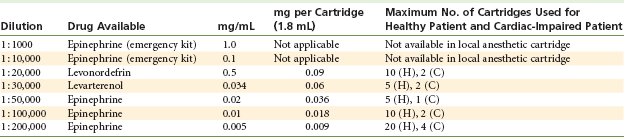
Epinephrine and levonordefrin are the vasoconstrictors presently included in dental local anesthetic cartridges in the United States and Canada. Table 18-8 outlines the milligram per milliliter concentrations of vasoconstrictors currently used in dentistry worldwide.
The optimum concentration of epinephrine for prolongation of pain control (with lidocaine) appears to be 1 : 400,000.55 Use of a 1 : 50,000 epinephrine concentration for pain control cannot be recommended. Epinephrine 1 : 50,000 or 1 : 100,000 is useful via local infiltration in the control of bleeding when applied directly into the surgical site. Epinephrine or local anesthetic overdose reactions occurring under these conditions are rare.
Epinephrine overdose is more common when used in gingival retraction cord before impressions are taken for a crown and bridge procedure. Currently available cords contain approximately 225.5 µg of racemic epinephrine per inch of cord.56 Epinephrine is readily absorbed through gingival epithelium that has been disturbed (abraded) by the dental procedure. About 64% to 94% of applied epinephrine is absorbed into the CVS.56 Variability in absorption is extreme, according to the degree and duration of vascular exposure (bleeding). With regard to vasoconstrictors used for gingival retraction purposes, the American Dental Association states the following in Accepted Dental Therapeutics: “Since effective agents which are devoid of systemic effects are available, it is not advisable to use epinephrine for gingival retraction, and its use is contraindicated in individuals with a history of cardiovascular disease.”57
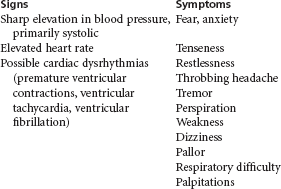
Clinical Manifestations
Clinical signs and symptoms of epinephrine overdose are listed in Box 18-6.
Management: Most instances of epinephrine overdose are of such short duration that little or no formal management is necessary. On occasion, however, the reaction may be prolonged and some management is desirable.
Terminate the Procedure: If possible, remove the source of epinephrine. Stopping the injection of local anesthetic does not remove epinephrine that has been deposited; however, release of endogenous epinephrine and norepinephrine from the adrenal medulla and nerve endings is lessened once the anxiety-inducing stimulus is eliminated. Epinephrine-impregnated gingival retraction cord, if present, should be removed.
Basic management follows the usual P→A→B→C→D algorithm used in management of all medical emergencies.
P→A→B→C: Position the conscious patient comfortably. The supine position often is not desired by the patient because it tends to accentuate the CVS effects. A semi-sitting or erect position minimizes any further elevation in cerebral blood pressure. A, B, and C are assessed as adequate (patient is conscious and talking).
1. Reassure the patient that the signs and symptoms are transient and will subside shortly. Anxiety and restlessness are common clinical manifestations of epinephrine overdose.
2. Monitor vital signs and administer oxygen. Blood pressure and heart rate should be checked every 5 minutes during the episode. Striking elevations in both parameters may be noted but gradually return toward baseline. Oxygen may be administered if necessary. The patient may complain of difficulty breathing. An apprehensive patient may hyperventilate (increased rate and depth of breathing). Oxygen is not indicated in the management of hyperventilation because it can exacerbate symptoms, possibly leading to carpopedal tetany.
3. Recovery. Permit the patient to remain in the dental chair as long as necessary to recover. The degree of postexcitation fatigue with depression noted varies but is usually prolonged. Do not discharge the patient if any doubt remains about his or her ability to provide self-care.
Allergy
Allergy is a hypersensitive state, acquired through exposure to a particular allergen, re-exposure to which produces a heightened capacity to react. Allergic reactions cover a broad spectrum of clinical manifestations ranging from mild and delayed responses occurring as long as 48 hours after exposure to the allergen, to immediate and life-threatening reactions developing within seconds of exposure (Table 18-9).
TABLE 18-9
Classification of Allergic Diseases (After Gell and Coombs)
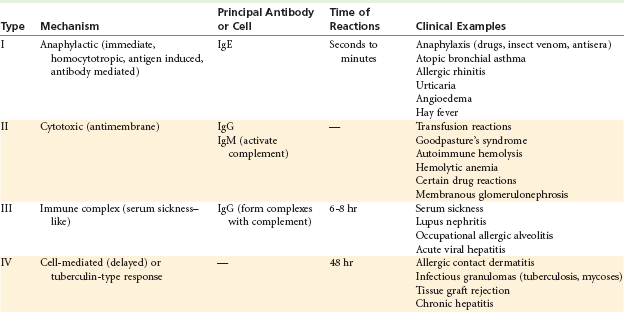
Adapted from Krupp MA, Chatton MJ: Current medical diagnosis and treatment, Los Altos, Calif, 1994, Lange Medical.
Predisposing Factors
The incidence of allergy in the population is not low: about 15% of patients with allergy have conditions severe enough to require medical management, and some 33% of all chronic disease in children is allergic in nature.58
Allergy to local anesthetics does occur, but its incidence has decreased dramatically since the introduction of amide anesthetics in the 1940s. Brown and associates stated, “The advent of the amino-amide local anesthetics which are not derivatives of para-aminobenzoic acid markedly changed the incidence of allergic type reactions to local anesthetic drugs. Toxic reactions of an allergic type to the amino amides are extremely rare, although several cases have been reported in the literature in recent years which suggest that this class of agents can on rare occasions produce an allergic type of phenomenon.”59
Allergic responses to local anesthetics include dermatitis (common in dental office personnel), bronchospasm (asthmatic attack), and systemic anaphylaxis. The most frequently encountered are localized dermatologic reactions. Life-threatening allergic responses related to local anesthetics are indeed rare.60,61
Hypersensitivity to the ester-type local anesthetics—procaine, propoxycaine, benzocaine, tetracaine, and related compounds such as procaine penicillin G and procainamide—is much more frequent.
Amide-type local anesthetics are essentially free of this risk. However, reports from the literature and from medical history questionnaires indicate that alleged allergy to amide drugs appears to be increasing, despite the fact that subsequent evaluation of these reports usually finds them describing cases of overdose, idiosyncrasy, or psychogenic reactions.62-65 Allergy to one amide local anesthetic does not preclude the use of other amides, because cross-allergenicity does not occur.66 With ester anesthetic allergy, however, cross-allergenicity does occur; thus all ester-type local anesthetics are contraindicated with a documented history of ester allergy.66
Allergic reactions have been documented for the various contents of the dental cartridge. Table 18-10 lists the functions of these components. Of special interest with regard to allergy is the bacteriostatic agent methylparaben. The parabens (methyl-, ethyl-, and propyl-) are included, as bacteriostatic agents, in all multiple-use formulations of drugs, cosmetics, and some foods. Their increasing use has led to more frequent sensitization to them. In evaluating local anesthetic allergy, Aldrete and Johnson demonstrated positive reactions to methylparaben but negative reactions to the amide anesthetic without the bacteriostatic agent.2 Table 18-11 presents Aldrete and Johnson’s dermal reaction findings in patients exposed to various ester and amide local anesthetic solutions. The authors reported no signs of systemic anaphylaxis occurring in any of the subjects. Dental local anesthetic cartridges available in the United States and Canada are single-use items and as such no longer contain paraben preservatives.
TABLE 18-10
Contents of Local Anesthetic Cartridge
| Ingredient | Function |
| Local anesthetic agent | Conduction blockade |
| Vasoconstrictor | Decreases absorption of local anesthetic into blood, thus increasing duration of anesthesia and decreasing toxicity of anesthetic |
| Sodium metabisulfite | Antioxidant for vasoconstrictor |
| Methylparaben* | Preservative to increase shelf life; bacteriostatic |
| Sodium chloride | Isotonicity of solution |
| Sterile water | Diluent |
*Methylparaben has been excluded from all local anesthetic cartridges manufactured in the United States since January 1984, although it is still found in multidose vials of medication.
TABLE 18-11
Frequency of Dermal Reactions in Patients Exposed to Various Local Anesthetic Agents
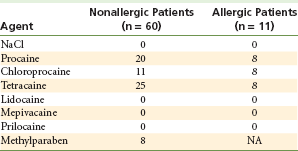
Data from Aldrete JA, Johnson DA: Evaluation of intracutaneous testing for investigation of allergy to local anesthetic agents, Anesth Analg 49:173–183, 1970.
Sodium Bisulfite Allergy
Allergy to sodium bisulfite or metabisulfite is being reported today with increasing frequency.67-70 Bisulfites are antioxidants that are commonly sprayed onto prepared fruits and vegetables to keep them appearing “fresh” for long periods of time. For example, apple slices sprayed with bisulfite do not turn brown (become oxidized). People who are allergic to bisulfites (most often steroid-dependent asthmatic individuals) may develop a severe response (bronchospasm).69,71 The U.S. Food and Drug Administration has enacted regulations that limit the use of bisulfites on foods. A history of allergy to bisulfites should alert the dentist to the possibility of this same type of response if sodium bisulfite or metabisulfite is included in the local anesthetic solution. Sodium bisulfite or metabisulfite is found in all dental local anesthetic cartridges that contain a vasoconstrictor, but is not found in “plain” local anesthetic solutions.
In the presence of a documented sulfite allergy, it is suggested that a local anesthetic solution without a vasopressor (“plain local anesthetic”) should be used (e.g., mepivacaine HCl 3%, prilocaine HCl 4%) if possible. No cross-allergenicity is present between sulfites and the “sulfa-” type antibiotics (sulfonamides).
Epinephrine Allergy
Allergy to epinephrine cannot occur in a living person. Questioning of the “epinephrine-allergic” patient (see “Dialogue History,” p. 329) immediately reveals signs and symptoms related to increased blood levels of circulating catecholamines (tachycardia, palpitation, sweating, nervousness), likely the result of fear of receiving injections (release of endogenous catecholamines [epinephrine and norepinephrine]). Management of the patient’s fear and anxiety over receipt of the injection is in order in most of these situations.
Latex Allergy
The thick plunger (also known as the stopper or bung) at one end of the local anesthetic cartridge and the thin diaphragm at the other end of the cartridge (see Fig. 7-1), through which the needle penetrates, at one time contained latex. Because latex allergy is a matter of concern among all health care professionals, the risk of provoking an allergic reaction in a latex-sensitive patient must be considered. A review of the literature on latex allergy and local anesthetic cartridges by Shojaei and Haas reveals that latex allergen can be released into the local anesthetic solution as the needle penetrates the diaphragm, but no reports or case studies have described an allergic response to the latex component of the cartridge containing a dental local anesthetic.70 Dental cartridges presently (January 2012) available in the United States and Canada are latex free.
Topical Anesthetic Allergy
Topical anesthetics possess the potential to induce allergy. The most commonly used topical anesthetics in dentistry are esters, such as benzocaine and tetracaine. The incidence of allergy to this classification of local anesthetics far exceeds that to amide local anesthetics. However, because benzocaine (an ester topical anesthetic) is poorly absorbed systemically, allergic responses that develop in response to its use normally are limited to the site of application.72 When other topical formulations, ester or amide, that are absorbed systemically are applied to mucous membranes, allergic responses may be localized or systemic. Many contain preservatives such as methylparaben, ethylparaben, or propylparaben.
Prevention
Most medical history questionnaires contain several questions related to allergy.
Question: Are you allergic to (e.g., have itching, rash, swelling of hands, feet, or eyes) or made sick by penicillin, aspirin, codeine, or any other medications?
Question: Have you ever had asthma, hay fever, sinus trouble, or allergies or hives?
These questions seek to determine whether the patient has experienced any adverse drug reactions. ADRs are not uncommon; those most frequently reported are labeled as allergy. If the patient mentions any unusual reaction to local anesthetics, the following protocol should be observed before use of the questionable drug is carried out. If the patient relates a history of alleged local anesthetic allergy, it is imperative that the dentist consider the following factors:
1. Assume that the patient is truly allergic to the drug in question and then take whatever steps are necessary to determine whether the alleged “allergy” is indeed an allergy. A recent paper on food allergy revealed that 30% of Americans have reported (alleged) one or more food allergies, but true food allergy in the U.S. population actually occurs at a rate of approximately 4% in adults and 5% in children.73
2. Any drug or closely related drug to which a patient claims to be allergic must not be used until the alleged allergy can be absolutely disproved.
3. For almost all drugs commonly implicated in allergic reactions, equally effective alternate drugs exist (e.g., antibiotics, analgesics).
4. The only drug group in which alternatives are not equally effective consists of local anesthetics.
Two major components are useful for determining the veracity of a claim of allergy: (1) dialogue history, whereby additional information is sought directly from the patient, and (2) consultation for a more thorough evaluation if doubt persists.
Dialogue History
The following questions are included in the dialogue history between the dentist and a patient with an alleged allergy to local anesthetics. The first two questions are the most critical, for they immediately establish in the evaluator’s mind a sense of whether allergy does or does not exist.74
Question: What treatment was given?
Following these two questions, the evaluator may consider others that will help elucidate the actual reaction.
Question: Can you provide the name, address, and telephone number of the doctor (dentist or physician) who was treating you when the incident occurred?
Answers to these questions provide enough information to permit a doctor to make an informed determination as to whether a true allergic reaction to a drug occurred. This is the initial step in managing alleged local anesthetic allergy. The dialogue history follows.
Question: Describe exactly what happened.
This is probably the most important question because it allows the patient to describe the actual sequence of events. The “allergy,” in most instances, is explained by the answer to this question. The symptoms described by the patient should be recorded and evaluated to help in formulating a tentative diagnosis of the adverse reaction. Did the patient lose consciousness? Did convulsions occur? Was there skin involvement or respiratory distress? The manifestations of allergic reactions are discussed in the following paragraph. Knowing them can aid the evaluator in rapidly determining the nature of the reaction that occurred.
Allergic reactions involve one or more of the following: skin (itching, hives, rash, edema), gastrointestinal system (cramping, diarrhea, nausea, vomiting), exocrine glands (runny nose, watery eyes), respiratory system (wheezing, laryngeal edema), and cardiovascular system (angioedema, vasodilation, hypotension). Most patients describe their local anesthetic “allergy” as one in which they experienced palpitations, severe headache, sweating, and mild shaking (tremor). Such reactions are almost always of psychogenic origin or are related to the administration of overly large doses of vasoconstrictor (e.g., epinephrine). They are not allergic in nature. Hyperventilation, an anxiety-induced reaction in which patients lose control over their breathing (inhaling and exhaling rapidly and deeply), is accompanied by dizziness, lightheadedness, and peripheral paresthesias (fingers, toes, and lips). Complaints of itching, hives, rash, or edema lead to the presumptive conclusion that an allergic reaction actually may have occurred.
Question: What treatment was given?
When the patient is able to describe his or her management, the evaluator usually can determine its cause. Were drugs injected? If so, what drugs? Epinephrine, histamine blockers, corticosteroids, or anticonvulsants? Was aromatic ammonia used? Oxygen? Knowledge of the specific management of these situations can lead to an accurate diagnosis.
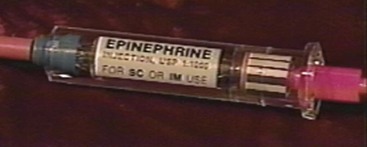
Drugs used in the management of allergic reactions include three categories: vasopressors (epinephrine [Adrenalin]), histamine blockers (diphenhydramine [Benadryl] or chlorpheniramine [Chlor-Trimeton]), and corticosteroids (hydrocortisone sodium succinate [Solu-Cortef] or dexamethasone [Decadron]).
Mention of the use of one or more of these drugs increases the likelihood that an allergic response did occur. Anticonvulsants, such as diazepam or midazolam, are administered intravenously to terminate seizures induced by overdose of local anesthetic. Aromatic ammonia is frequently used in the treatment of syncopal episodes. Oxygen may be administered in any or all of these reactions but is not specific for allergy.
Question: What position were you in when the reaction took place?
Injection of a local anesthetic into an upright patient is most likely to produce a psychogenic reaction (vasodepressor syncope). This does not exclude the possibility that another type of reaction may occur, but with the patient supine during the injection, vasodepressor syncope is a less likely cause, even though transient loss of consciousness may (on very rare occasions) occur in these circumstances.75 In some of the evaluations of allergy to local anesthetics that the author has carried out, the patient had been given an intracapsular injection of corticosteroid in the knee. Seated upright on a table in the physician’s treatment room, the patient was able to watch the entire procedure, which was profoundly disturbing. In an effort to make such injections more tolerable, lidocaine or another local anesthetic is added to the steroid mixture. In spite of this, however, the intracapsular injection of corticosteroid and lidocaine is extremely uncomfortable. Many patients experience their “allergic reaction” at this time. Therefore, the supine position is recommended as being physiologically best tolerated for the administration of all local anesthetic injections.
Question: What was the time sequence of events?
When, in relation to administration of the local anesthetic, did the reaction occur? Most adverse drug reactions associated with local anesthetic administration occur during or immediately (within seconds) after the injection. Syncope, hyperventilation, overdose, and (sometimes) anaphylaxis are most likely to develop immediately during the injection or within minutes thereafter, although all may occur later, during dental therapy. Also, seek to determine the amount of time that elapsed during the entire episode. How long was it before the patient was discharged from the office? Did dental treatment continue after the episode? The fact that dental treatment continued after this episode indicates that the response was probably minor and of a nonallergic nature.
Question: Were the services of a physician, emergency medical services, or a hospital necessary?
A positive response to this usually indicates the occurrence of a more serious reaction. Most psychogenic reactions are ruled out by a positive answer, although an overdose or allergic reaction indeed may have occurred.
Question: What local anesthetic was administered?
A patient who is truly allergic to a drug should be told the exact (generic) name of the substance. Many persons with documented allergic histories wear a medical alert tag or bracelet (Fig. 18-11) that lists specific items to which they are sensitive. However, some patients respond to this question with, “I’m allergic to local anesthetics” or “I’m allergic to Novocain” or “I’m allergic to all ‘caine’ drugs.” Of 59 patients reporting allergy to local anesthetics, 54 could name one or more local anesthetics they believed were responsible. Five referred to only caine drugs.76 Novocain (procaine) and other esters rarely are used today as injectable local anesthetics in dentistry (although the esters (primarily tetracaine) maintain some popularity in medicine); the amides have replaced the esters in clinical practice. Yet patients throughout the world frequently call the local anesthetics they receive “shots of Novocain.” Two reasons exist for this. First, many older patients at one time received Novocain as a dental local anesthetic, and its name has become synonymous with intraoral dental injections. Second, despite the fact that United States dentists do not inject procaine or procaine-propoxycaine, many still describe local anesthetics as Novocain when talking with their patients. Thus the usual response of a patient to this question remains, “I’m allergic to Novocain.” This response, received from a patient who has been managed properly in the past after an adverse reaction, indicates that the patient was sensitive to ester local anesthetics but not necessarily to amide local anesthetics. However, the answers usually are too general and vague for any conclusions to be drawn.77
Question: What amount of drug was administered?
This question seeks to determine whether there was a definite dose–response relationship, as might occur with an overdose reaction. The problem is that patients rarely know these details and can provide little or no assistance. The doctor who was involved in the prior episode(s) may be of greater assistance.
Question: Did the anesthetic solution contain a vasoconstrictor or preservative?
The presence of a vasoconstrictor might lead to the thought of an overdose reaction (relative or absolute) to this component of the solution. A preservative, such as methylparaben (if a multidose vial was used) or sodium bisulfite (if the solution contained a vasoconstrictor), in the solution might lead to the belief that an allergic reaction did occur to the preservative, not to the local anesthetic. Unfortunately, however, most patients are unable to furnish this information. Today, methylparaben is found only in multidose vials of local anesthetics (and most other drugs). Bisulfites are found in all dental local anesthetic cartridges containing a vasopressor.
Question: Were you taking any other drugs or medications at the time of the reaction?
This question seeks to determine the possibility of a drug–drug interaction or a side effect of another drugs being responsible for the reported adverse response. Reidenburg and Lowenthal, reporting in 1968 on adverse nondrug reactions, demonstrated that “adverse” effects and side effects, which so often are blamed on medications, occur with considerable regularity in persons who have received no drugs or medications for weeks.78 In other words, many so-called adverse drug reactions may be nothing more than a coincidental event: the person is becoming overly tired, irritable, nauseated, or dizzy for reasons unrelated to drugs. Unfortunately, however, it seems that whenever such symptoms develop in a patient taking a medication, the drug is immediately thought to be responsible, with the label “allergy” often applied.
Question: Can you provide the name and address of the doctor (dentist, physician, or hospital) who was treating you at the time of the incident?
If possible, it is usually valuable to speak to the person who managed the previous episode. In most instances, this person is able to locate patient records and describe in detail what transpired. If it is not possible to locate or contact the doctor, the patient’s primary care physician should be consulted. Direct discussion with the patient and the doctor can provide a wealth of information that the knowledgeable dentist can use to determine more precisely the nature of the previous reaction.
Consultation and Allergy Testing
Consultation should be considered if any doubt remains as to the cause of the reaction after the dialogue history. Referral to a doctor who will test for allergy to local anesthetics is recommended.
Although no form of allergy testing is 100% reliable, skin testing is the primary mode of assessing a patient for local anesthetic allergy. Intracutaneous injections are among the most reliable means available, because they are 100 times more sensitive than cutaneous testing, and involve depositing 0.1 mL of test solution into the patient’s forearm.2,76,79-82 In all such instances, the local anesthetic solutions should contain neither vasoconstrictor nor preservative. Methylparaben, if evaluated, should be tested separately.83
The protocol for intracutaneous testing for local anesthetic allergy used at the Ostrow School of Dentistry of U.S.C. for the past 35 years involves the administration of 0.1 mL of each of the following: 0.9% sodium chloride, 1% or 2% lidocaine, 3% mepivacaine, and 4% prilocaine, without methylparaben, bisulfites, or vasopressors. After successful completion of this phase of testing, 0.9 mL of one of the previously noted local anesthetic solutions that produced no reaction is injected intraorally via supraperiosteal infiltration atraumatically (but without topical anesthesia) above a maxillary right or left premolar or anterior tooth. This is called an intraoral challenge test, and it frequently provokes the “allergic” reaction: fainting, sweating, and palpitations.
After performing more than 210 local anesthetic allergy testing procedures, the author has encountered four allergic responses to the paraben preservative (before 1984, the protocol included testing for parabens) and none to the amide local anesthetic itself. Numerous psychogenic responses (syncope, hyperventilation, palpitations) have been observed during intracutaneous or intraoral testing phases.
Such testing may be carried out by any person who is knowledgeable about the procedure and is fully prepared to manage whatever adverse reactions may develop. It must be remembered that skin testing is not without risk. Severe immediate allergic reactions may be precipitated by as little as 0.1 mL of drug in a sensitized patient. Emergency drugs, equipment, and trained personnel always must be available whenever allergy testing is performed.
Intracutaneous allergy testing should be carried out only after an intensive dialogue history in which the evaluator has become convinced that the prior reaction to the local anesthetic was not allergy. The testing procedure is used to confirm this fact for the patient. The intraoral challenge test was added to the protocol when several patients with negative responses to intracutaneous testing stated, “But the dentist will give me a larger amount in the mouth.” It was intended to provide the patient with the psychological support needed to receive intraoral local anesthetic injections safely.
Informed consent is obtained before allergy testing. This consent includes, among other possible complications, acute allergy (anaphylaxis), cardiac arrest, and death.
A continuous intravenous infusion is started before all allergy testing procedures are performed, and emergency drugs and equipment are readily available throughout the testing.
Dental Management in the Presence of Alleged Local Anesthetic Allergy
When doubt persists concerning a history of allergy to local anesthetics, do not administer these drugs to the patient. Assume that allergy exists. Do not use local anesthetics, including topical anesthetics, unless and until allergy has been absolutely disproved – to the patient’s satisfaction.
Elective Dental Care
Dental treatment requiring local anesthesia (topical or injectable) should be postponed until a thorough evaluation of the patient’s “allergy” is completed. Dental care not requiring local anesthesia may be completed during this time.
Emergency Dental Care
Pain or oral infection presents a more difficult situation in the “I am allergic to Novocain” patient. Commonly, this patient is new to the dental office, requiring tooth extraction, pulpal extirpation, or incision and drainage (I&D) of an abscess, with an unremarkable medical history except for the alleged “allergy to Novocain.” If, after dialogue history, the “allergy” appears to have been a psychogenic reaction but some doubt remains, consider one of several courses of action.
Emergency Protocol No. 1: The most practical approach to this patient is to provide no treatment of an invasive nature. Arrange an appointment for immediate consultation and allergy testing. Do not carry out any dental care requiring the use of injectable or topical local anesthetics. For incision and drainage of an abscess, inhalation sedation with nitrous oxide and oxygen might be an acceptable alternative.
Acute pain may be managed with oral analgesics, infection with oral antibiotics. These constitute only temporary measures. After complete evaluation of the “allergy,” definitive dental care may proceed.
Emergency Protocol No. 2: Use general anesthesia in place of local anesthesia for management of a dental emergency. When properly used, general anesthesia is a highly effective and relatively safe alternative. Its lack of availability is a major problem in most dental practices.
When general anesthesia is used, be careful to avoid local anesthetics in these procedures:
1. Topical application (via spray) to the pharynx and tracheal mucosa immediately before intubation.
2. Infiltration of the skin with local anesthetic before venipuncture to decrease discomfort.
General anesthesia, administered in the dental office or in a hospital operating theater, is a viable short-term alternative to local anesthetic administration in managing the “allergic” patient, provided adequate facilities and well-trained personnel are available.
Emergency Protocol No. 3: Histamine blockers used as local anesthetics should be considered if general anesthesia is not available, and if it is deemed necessary to intervene physically in the dental emergency. Most injectable histamine blockers have local anesthetic properties. Diphenhydramine hydrochloride in a 1% solution with 1 : 100,000 epinephrine provides pulpal anesthesia for up to 30 minutes.84 Although the quality of soft and hard tissue anesthesia attained with diphenhydramine, lidocaine, or prilocaine is equivalent, an undesirable side effect frequently noted during injection of diphenhydramine is a burning or stinging sensation, which limits the use of this agent for most patients to emergency procedures only.85-87 Nitrous oxide and oxygen used along with diphenhydramine minimize patient discomfort while increasing the pain reaction threshold. Another (possibly positive) side effect of diphenhydramine and many histamine blockers is CNS depression (sedation, drowsiness), which may prove somewhat beneficial during treatment but mandates that a responsible adult guardian be available to take the patient home after treatment.
Management of the Patient With Confirmed Allergy
Management of the dental patient with a confirmed allergy to local anesthetics varies according to the nature of the allergy. If the allergy is limited to ester anesthetics, an amide anesthetic may be used (provided it does not contain a paraben preservative, which is closely related to the esters). No dental local anesthetic cartridge manufactured in the United States since January 1984 contains methylparaben.
If, in the exceedingly unlikely case, a documented allergy to an amide local anesthetic exists, other amide local anesthetics may be employed because cross-allergenicity between amide locals does not occur.66
If allergy does truly exist to an ester local anesthetic (a much more likely situation), dental treatment may be safely completed via one of the following:
On occasion, it is reported that a patient is “allergic to all ‘caine’ drugs.” Such a report should provoke close scrutiny by the dentist, and the method by which this conclusion was reached should be re-examined.
All too often, patients are mislabeled as “allergic to local anesthetics.” Such patients ultimately must have dental treatment carried out in a hospital setting, usually under general anesthesia, when a proper evaluation might have saved the patient time and money and decreased the risk of dental care.60,77
Clinical Manifestations
Table 18-9 lists the various forms of allergic reactions. It is also possible to classify allergic reactions by the time elapsing between contact with the antigen (allergen) and onset of clinical manifestations of allergy. Immediate reactions develop within seconds to hours of exposure. (They include types I, II, and III in Table 18-9.) With delayed reactions, clinical manifestations develop hours to days after antigenic exposure (type IV).
Immediate reactions, particularly type I, anaphylaxis, are significant. Organs and tissues involved in immediate allergic reactions include the skin, cardiovascular system, respiratory system, and gastrointestinal system. Generalized (systemic) anaphylaxis involves all these systems. Type I reactions may involve only one system, in which case they are referred to as localized allergy. Examples of localized anaphylaxis and their “targets” include bronchospasm (respiratory system) and urticaria (skin).
Time of Onset of Symptoms
The time elapsing between a patient’s exposure to the antigen and the development of clinical signs and symptoms is important. In general, the more rapidly signs and symptoms develop following antigenic exposure, the more intense the reaction is likely to be.88 Conversely, the more time between exposure and onset, the less intense the reaction. Cases have been reported of systemic anaphylaxis arising many hours after exposure.89
The rate of progression of signs and symptoms once they appear is also significant. Situations in which signs and symptoms rapidly increase in intensity are likely to be more life threatening than those progressing slowly or not at all once they appear.
Signs and Symptoms
The most common allergic drug reaction associated with local anesthetic administration consists of urticaria and angioedema. Urticaria is associated with wheals, which are smooth, elevated patches of skin. Intense itching (pruritus) frequently is present. Angioedema is localized swelling in response to an allergen. Skin color and temperature usually are normal (unless urticaria or erythema is present). Pain and itching are uncommon. Angioedema most frequently involves the face, hands, feet, and genitalia, but it can also involve the lips, tongue, pharynx, and larynx. It is more common following application of topical anesthetics to oral mucous membranes. Within 30 to 60 minutes, the tissue in contact with the allergen appears swollen.
Allergic skin reactions, if the sole manifestation of an allergic response, normally are not life threatening; however, those that occur rapidly after drug administration may be the first indication of a more generalized reaction to follow.
Respiratory Reactions
Clinical signs and symptoms of allergy may be solely related to the respiratory tract, or respiratory tract involvement may occur along with other systemic responses.
Signs and symptoms of bronchospasm, the classic respiratory allergic response, include the following:
Laryngeal edema, an extension of angioneurotic edema to the larynx, is a swelling of the soft tissues surrounding the vocal apparatus with subsequent obstruction of the airway. Little or no exchange of air from the lungs is possible. Laryngeal edema represents the effects of allergy on the upper airway, whereas bronchospasm represents the effects on the lower airway (smaller bronchioles). Laryngeal edema is a life-threatening emergency.
Generalized Anaphylaxis
The most dramatic and acutely life-threatening allergic reaction is generalized anaphylaxis. Clinical death can occur within a few minutes. Generalized anaphylaxis can develop after administration of an antigen by any route but is more common after parenteral administration (injection). Time of response is variable, but the reaction typically develops rapidly, reaching maximum intensity within 5 to 30 minutes. It is extremely unlikely that this reaction will ever be noted after administration of amide local anesthetics.
Signs and symptoms of generalized anaphylaxis, listed according to their typical progression, follow:
• Smooth muscle spasm of the gastrointestinal (cramping) and genitourinary tracts and of respiratory smooth muscle (bronchospasm)
In fatal anaphylaxis, respiratory and cardiovascular disturbances predominate and are evident early in the reaction. The typical reaction progression is shown in Box 18-7.
In rapidly developing reactions, all signs and symptoms may occur within a very short time with considerable overlap. In particularly severe reactions, respiratory and cardiovascular signs and symptoms may be the only ones present. The reaction or any part of it can last from minutes to a day or longer.88,90
With prompt and appropriate treatment, the entire reaction may be terminated rapidly. However, hypotension and laryngeal edema may persist for hours to days despite intensive therapy. Death, which may occur at any time during the reaction, usually is secondary to upper airway obstruction produced by laryngeal edema.91
Management
Management is predicated on the rate at which the reaction appears after antigenic challenge.
Delayed Skin Reactions: Signs and symptoms developing 60 minutes or longer after exposure usually do not progress and are not considered life threatening. Examples include a localized mild skin and mucous membrane reaction after application of topical anesthetic. In most instances, the patient already may have left the dental office and is calling back later describing these signs and symptoms, or the patient may still be in the dental office at the conclusion of his or her treatment.
Basic management follows the usual P→A→B→C→D algorithm used in management of all medical emergencies.
P→A→B→C: Position the conscious patient comfortably. A, B, and C are assessed as adequate (patient is conscious and talking).
1. Oral histamine blocker: 50 mg diphenhydramine or 10 mg chlorpheniramine; a prescription for diphenhydramine, 50 mg capsules, one q6h for 3 to 4 days should be given to the patient.
2. If still in the dental office, the patient should remain in the office under observation for 1 hour before discharge to ensure that the reaction does not progress.
3. Obtain medical consultation, if necessary, to determine the cause of the reaction. A complete list of all drugs and chemicals administered to or taken by the patient should be compiled for use by the allergy consultant.
4. If drowsiness occurs after oral histamine blocker administration, the patient should not be permitted to leave the dental office unescorted.
Immediate Skin Reactions: Signs and symptoms of allergy developing within 60 minutes require more vigorous management. Examples include conjunctivitis, rhinitis, urticaria, pruritus, and erythema.
P→A→B→C: Position the conscious patient comfortably. A, B, and C are assessed as adequate (patient is conscious and talking).
1. Administer parenteral (IM, IV) histamine blocker: 50 mg diphenhydramine (25 mg if less than 30 kg [66 lb]) or 10 mg chlorpheniramine (5 mg if less than 30 kg [66 lb]).
2. Monitor and record vital signs (blood pressure, heart rate and rhythm, respiratory rate) every 5 minutes for 1 hour.
3. Observe the patient a minimum of 60 minutes for evidence of recurrence. Discharge in the custody of a responsible adult if any parenteral drugs have been given.
4. Prescribe an oral histamine blocker for 3 days.
5. Fully evaluate the patient’s reaction before further dental care is provided.
6. If, at any time during this period, uncertainty exists as to the condition of the patient, activate EMS (9-1-1).
Respiratory Reactions
P→A→B→C: Position the conscious patient comfortably. Most persons experiencing respiratory distress prefer to be seated upright to varying degrees. A, B, and C are assessed. Airway is patent, although patient is exhibiting respiratory distress. C is assessed as adequate.
1. Terminate treatment (if started).
2. Administer oxygen via full face mask, nasal hood, or nasal cannula at a flow of 5 to 6 liters/min.
3. Administer epinephrine IM in the vastus lateralis muscle (0.3 mg if >30 kg; 0.15 mg if <30 kg) or another appropriate bronchodilator via metered dose inhaler (MDI) (albuterol) (Fig. 18-12). Dose may be repeated every 5 to 10 minutes until recovery or help (EMS) arrives on the scene to take over management.
4. Activate EMS (9-1-1). If alone with victim, it is important to administer epinephrine before activating EMS.
5. On recovery (bronchospasm resolves), administer histamine blocker to minimize risk of relapse (50 mg IM diphenhydramine [25 mg if <30 kg] or 10 mg IM chlorpheniramine [5 mg if <30 kg]).
6. EMS will evaluate the patient’s status and will determine whether transport to the hospital emergency department for observation or additional treatment is warranted.
Laryngeal Edema: Laryngeal edema may be present when movement of air through the patient’s nose and mouth cannot be heard or felt in the presence of spontaneous respiratory movements, or when it is impossible to carry out artificial ventilation in the presence of a patent airway (tongue not causing obstruction). Partial obstruction of the larynx produces stridor (a characteristic high-pitched crowing sound), in contrast to the wheezing associated with bronchospasm. A partial obstruction may gradually or rapidly progress to total obstruction accompanied by the ominous “sound” of silence (in the presence of spontaneous respiratory movements). The patient rapidly loses consciousness from lack of oxygen.
P→A→B→C: Position the unconscious patient supine. A, B, and C are assessed. If airway is maintained and the victim’s chest is making spontaneous respiratory movements but no air is being exchanged, immediate and aggressive treatment is mandatory to save the victim’s life.
1. Epinephrine. Administer 0.3 mg (if >30 kg) (0.15 mg if <30 kg) epinephrine IM in the vastus lateralis muscle. Epinephrine may be administered every 5 to 10 minutes as needed until recovery, or until help (9-1-1) arrives on the scene to take over management.
2. Following administration of epinephrine, activate EMS. Summon emergency medical assistance and administer oxygen.
3. Maintain the airway. If only partially obstructed, epinephrine may halt the progress of the edema through its vasoconstrictive actions.
4. Additional drug management: histamine blocker IM or IV (50 mg diphenhydramine or 10 mg chlorpheniramine), corticosteroid IM or IV (100 mg hydrocortisone sodium succinate to inhibit and decrease edema and capillary dilation).
5. Perform cricothyrotomy. If the preceding steps have failed to secure a patent airway, an emergency procedure to create an airway is critical for survival. Figures 18-13 and 18-14 both illustrate the anatomy of the region and the technique. Once established, the airway must be maintained, oxygen administered, and artificial ventilation used as needed. Monitor the patient’s vital signs. The patient definitely will require hospitalization following transfer from the dental office by paramedical personnel.
Generalized Anaphylaxis
Generalized anaphylaxis is highly unlikely to develop in response to local anesthetic administration. Its management is included here, however, for completeness. The most common causes of death from anaphylaxis are parenterally administered penicillin and stinging insects (the Hymenoptera: wasps, hornets, yellow jackets, and bees).
Signs of Allergy Present: When signs and symptoms of allergy (e.g., urticaria, erythema, pruritus, wheezing) are present, they should signal an immediate diagnosis of allergy. The patient usually is unconscious.
P→A→B→C: Position the unconscious patient supine. A, B, and C are assessed and performed as indicated (Fig. 18-15). If conscious, position the patient comfortably.
1. Administer epinephrine. The doctor should have previously called for the office emergency team. Epinephrine from the emergency kit (0.3 mL of 1 : 1000 for >30 kg, 0.15 mL for <30 kg, and 0.075 mL for <15 kg) is administered IM as quickly as possible, or IV (but only if available in a 1 : 10,000 solution). Because of the immediate need for epinephrine in this situation, a preloaded syringe of epinephrine is recommended for the emergency kit (Fig. 18-16). Epinephrine is the only injectable drug the author recommends that should be kept in a preloaded delivery system so as to prevent confusion when looking for it in this near-panic situation.
2. Summon medical assistance (9-1-1). As soon as a severe allergic reaction is considered a possibility, emergency medical care should be summoned. If alone with the victim, it is important to administer the epinephrine first, then activate EMS.
3. Should the clinical picture fail to improve or continue to deteriorate (increased severity of symptoms) within 5 to 10 minutes of the initial epinephrine dose, a second dose is administered. Subsequent doses may be administered as needed every 5 to 10 minutes. There is no absolute contraindication to epinephrine administration in anaphylaxis.88
5. Monitor vital signs. The patient’s cardiovascular and respiratory status must be monitored continuously. Blood pressure and heart rate (at the carotid artery) should be recorded at least every 5 minutes, with chest compression started if no palpable pulse (cardiac arrest) is detected.
During this acute, life-threatening phase of what is obviously an anaphylactic reaction, management consists of epinephrine administration (q5-10min), basic life support (as needed), administration of oxygen, and continual monitoring (and recording) of vital signs. Until improvement in the patient’s clinical status is noted, no additional drug therapy is indicated.
6. Additional drug therapy. Additional drug therapy may be started once clinical improvement (increased blood pressure, decreased bronchospasm) is noted. This includes administration of a histamine blocker and a corticosteroid (both drugs IM or, if available, IV). They function to prevent a recurrence of signs and symptoms, obviating the need for continued administration of epinephrine. They are not administered during the acute phase of the reaction because they are too slow in onset and they do not do enough immediate good to justify their use at this time. Epinephrine and oxygen are the only drugs that should be administered during the acute phase of the anaphylactic reaction.
No Signs of Allergy Present: If a patient receiving a local anesthetic injection loses consciousness and no signs of allergy are present, the differential diagnosis includes psychogenic reaction (vasodepressor syncope), cardiac arrest, overdose reaction, and allergic reaction involving only the cardiovascular system, among other possibilities.
P→A→B→C: Position the unconscious patient supine (see Fig. 18-15).
1. Terminate treatment, if started.
2. Position the patient. Management of this situation, which might prove to result from any of a number of causes (see earlier), requires immediate placement of the patient in the supine position with the legs elevated slightly. Low blood pressure (in the brain) is, far and away, the leading cause of unconsciousness in humans, and the supine position (with feet elevated) increases blood flow to the brain.
3. Provide basic life support, as indicated (Fig. 18-17). A, B, and C are assessed and performed as indicated. Victims of vasodepressor syncope or postural hypotension rapidly recover consciousness once properly positioned with a patent airway maintained. Patients who do not recover at this juncture should continue to have the elements of basic life support applied (breathing, circulation) as needed.
1. Summon EMS. If consciousness does not return rapidly after institution of the steps of basic life support, EMS should be sought immediately.
3. Monitor vital signs. Blood pressure, heart rate and rhythm, and respirations should be monitored and recorded, at least every 5 minutes, with the elements of basic life support started at any time necessary.
4. Provide additional management. On arrival, emergency medical personnel will seek to make a diagnosis of the cause of the loss of consciousness. If this is possible, appropriate drug therapy will be instituted and the patient stabilized and then transferred to a local hospital emergency department.
In the absence of definitive signs and symptoms of allergy, such as edema, urticaria, or bronchospasm, epinephrine and other allergy drug therapy (e.g., histamine blockers, corticosteroids) are not indicated. Any of a number of other situations may be the cause of the unconsciousness, for example, drug overdose, hypoglycemia, cerebrovascular accident, acute adrenal insufficiency, or cardiopulmonary arrest. Continued basic life support until medical assistance arrives is the most prudent course of action in this situation.
Summary
Systemic complications associated with local anesthetic drug administration and techniques are frequently preventable. Following is a summary of those procedures recommended to minimize their occurrence:
1. Preliminary medical evaluation should be completed before administration of any local anesthetic.
2. Anxiety, fear, and apprehension should be recognized and managed before administration of a local anesthetic.
3. All dental injections should be administered with the patient supine or semi-supine. Patients should not receive local anesthetic injections in the upright position unless special conditions (e.g., severe cardiorespiratory disease) dictate.
4. Topical anesthetic should be applied before all injections for a minimum of 1 minute.
5. The weakest effective concentration of local anesthetic solution should be injected at the minimum volume compatible with successful pain control.
6. The anesthetic solution selected should be appropriate for the dental treatment contemplated (duration of action).
7. Vasoconstrictors should be included in all local anesthetics unless specifically contraindicated by the desired duration of action (e.g., short duration procedure) or the patient’s physical status (e.g., ASA 4 as a result of cardiovascular disease).
8. Needles should be disposable, sharp, rigid, capable of reliable aspiration, and of adequate length for the contemplated injection techniques.
9. Aspirating syringes must always be used for all injections.
10. Aspiration should be carried out in at least two planes before injection.
11. Injection should be made slowly, over a minimum of 60 seconds if 1.8 mL of local anesthetic is deposited.
12. Observe the patient both during and after local anesthetic administration for signs and symptoms of undesirable reaction. Never give an injection and leave the patient alone while doing other procedures.
References
1. Pallasch, TJ. Pharmacology for dental students and practitioners. Philadelphia: Lea & Febiger; 1980.
2. Speca, SJ, Boynes, SG, Cuddy, MA. Allergic reactions to local anesthetic formulations. Dent Clin North Am. 2010;54:655–664.
3. Finder, RL, Moore, PA. Adverse drug reactions to local anesthesia. Dent Clin North Am. 2002;46:747–757.
4. Vinckier, F. Local anesthesia in children. Rev Belge Medec Dent. 2000;55:61–71.
5. Malamed, SF. Morbidity, mortality and local anesthesia. Prim Dent Care. 1999;6:11–15.
6. Meechan, J. How to avoid local anaesthetic toxicity. Br Dent J. 1998;184:334–335.
7. Meechan, J, Rood, JP. Adverse effects of dental local anaesthesia. Dent Update. 1997;24:315–318.
8. Davis, MJ, Vogel, LD. Local anesthetic safety in pediatric patients. N Y State Dent J. 1996;62:32–35.
9. Prince, BS, Goetz, CM, Rihn, TL, et al. Drug-related emergency department visits and hospital admissions. Am J Hosp Pharm. 1992;49:1696–1700.
10. Kishikawa, K, Namiki, A, Miyashita, K, et al. Effects of famotidine and cimetidine on plasma levels of epidurally administered lignocaine. Anaesthesia. 1990;45:719–721.
11. Shibasaki, S, Kawamata, Y, Ueno, F, et al. Effects of cimetidine on lidocaine distribution in rats. J Pharmacobiodynam. 1988;11:785–793.
12. Dailey, PA, Hughes, SC, Rosen, MA, et al. Effect of cimetidine and ranitidine on lidocaine concentrations during epidural anesthesia for cesarean section. Anesthesiology. 1988;69:1013–1017.
13. de Jong, RH. Bupivacaine preserves newborns’ muscle tone. JAMA. 1977;237:53–54.
14. Steen, PA, Michenfelder, JD. Neurotoxicity of anesthetics. Anesthesiology. 1979;50:437–453.
15. Hazma, J. Effect of epidural anesthesia on the fetus and the neonate. Cah Anesthesiol. 1994;42:265–273.
16. Shammas, FV, Dickstein, K. Clinical pharmacokinetics in heart failure: an updated review. Clin Pharmacokinet. 1988;15:94–113.
17. Hammermeister, KE. Adverse hemodynamic effects of antiarrhythmic drugs in congestive heart failure. Circulation. 1990;81:1151–1153.
18. Pedersen, NA, Jensen, FS. Clinical importance of plasma cholinesterase for the anesthetist. Ann Acad Med Singapore. 1994;23(Suppl 6):120–124.
19. Barcelos, KC, Furtado, DP, Ramacciato, JC, et al. Effect of PaCO2 and PaO2 on lidocaine and articaine toxicity. Anesth Prog. 2010;57:104–108.
20. Malagodi, MH, Munson, ES, Embro, MJ. Relation of etidocaine and bupivacaine toxicity to rate of infusion in rhesus monkeys. Br J Anaesth. 1977;49:121–125.
21. Hersh, EV, Helpin, ML, Evans, OB. Local anesthetic mortality: report of a case. ASDC J Dent Child. 1991;58:489–491.
22. Moore, PA. Preventing local anesthetic toxicity. J Am Dent Assoc. 1992;123:60–64.
23. Yagiela, JA. Local anesthetics. In Dionne RA, Phero JC, Becker DE, eds.: Management of pain and anxiety in the dental office, ed 2, Philadelphia: WB Saunders, 2002.
24. Kaplan EL, ed. Cardiovascular disease in dental practice. Dallas, Tex: American Heart Association, 1986.
25. Adriani, J, Campbell, D. Fatalities following topical application of local anesthetics to mucous membrane. J Am Med Assoc. 1956;162:1527.
26. Wilburn-Goo, D, Lloyd, LM. When patients become cyanotic: acquired methemoglobinemia. J Am Dent Assoc. 1999;130:826–831.
27. Moos, DD, Cuddeford, JD. Methemoglobinemia and benzocaine. Gastroenterol Nurs. 2007;30:342–345.
28. Trapp, L, Will, J. Acquired methemoglobinemia revisited. Dent Clin North Am. 2010;54:665–675.
29. Smith, M, Wolfram, W, Rose, R. Toxicity: seizures in an infant caused by (or related to) oral viscous lidocaine use. J Emerg Med. 1992;10:587–590.
30. Hess, GP, Walson, PD. Seizures secondary to oral viscous lidocaine. Ann Emerg Med. 1988;17:725–727.
31. Garrettson, LK, McGee, EB. Rapid onset of seizures following aspiration of viscous lidocaine. J Pediatr. 1992;30:413–422.
32. Rothstein, P, Dornbusch, J, Shaywitz, BA. Prolonged seizures associated with the use of viscous lidocaine. J Pediatr. 1982;101:461–463.
33. Bartlett, SZ. Clinical observations on the effects of injections of local anesthetics preceded by aspiration. Oral Surg Oral Med Oral Pathol. 1972;33:520.
34. Aldrete, JA, Narang, R, Sada, T, et al. Reverse carotid blood flow: a possible explanation for some reactions to local anesthetics. J Am Dent Assoc. 1977;94:1142–1145.
35. Malamed, SF. Allergic and toxic reactions to local anesthetics. Dent Today. 2003;22:114–121.
36. Tavares, M, Goodson, JM, Studen-Pavlovich, D, et al. Reversal of soft tissue anesthesia with phentolamine mesylate in pediatric patients. Local Anesthesia Reversal Group. J Am Dent Assoc. 2008;139:1095–1104.
37. Moore, PA, Hersh, EV, Papas, AS, et al. Pharmacokinetics of lidocaine with epinephrine following local anesthesia reversal with phentolamine mesylate. Anesth Prog. 2008;55:40–48.
38. Cheatham, BD, Primosch, RE, Courts, FJ. A survey of local anesthetic usage in pediatric patients by Florida dentists. J Dent Child. 1992;59:401–407.
39. Malamed SF: Report of a case, unpublished data, 2002.
40. Munson, ES, Tucker, WK, Ausinsch, B, et al. Etidocaine, bupivacaine, and lidocaine seizure thresholds in monkeys. Anesthesiology. 1975;42:471–478.
41. Rey, E, Radvanyi-Bouvet, MF, Bodiou, C, et al. Intravenous lidocaine in the treatment of convulsions in the neonatal period: monitoring plasma levels. Ther Drug Monit. 1990;12:316–320.
42. Aggarwal, P, Wali, JP. Lidocaine in refractory status epilepticus: a forgotten drug in the emergency department. Am J Emerg Med. 1993;11:243–244.
43. Pascual, J, Ciudad, J, Berciano, J. Role of lidocaine (lignocaine) in managing status epilepticus. J Neurol Neurosurg Psychiatr. 1992;55:49–51.
44. Jaffe, AS. The use of antiarrhythmics in advanced cardiac life support. Ann Emerg Med. 1993;22:307–316.
45. Bruelle, P, de La Coussaye, JE, Eledjam, JJ. Convulsions and cardiac arrest after epidural anesthesia: prevention and treatment. Cah Anesthesiol. 1994;42:241–246.
46. de La Coussaye, JE, Eledjam, JJ, Brugada, J, et al. Cardiotoxicity of local anesthetics. Cah Anesthesiol. 1993;41:589–598.
47. Bachmann, MB, Biscoping, J, Schurg, R, et al. Pharmacokinetics and pharmacodynamics of local anesthetics. Anaesthesiol Reanim. 1991;16:359–373.
48. Ryan, CA, Robertson, M, Coe, JY. Seizures due to lidocaine toxicity in a child during cardiac catheterization. Pediatr Cardiol. 1993;14:116–118.
49. Rivera, R, Segnini, M, Baltodano, A, et al. Midazolam in the treatment of status epilepticus in children. Crit Care Med. 1993;21:991–994.
50. Bertz, RJ, Howrie, DL. Diazepam by continuous intravenous infusion for status epilepticus in anticonvulsant hypersensitivity syndrome. Ann Pharmacother. 1993;27:298–301.
51. Lahat, E, Aladjem, M, Eshel, G, et al. Midazolam in treatment of epileptic seizures. Pediatr Neurol. 1992;8:215–216.
52. Wroblewski, BA, Joseph, AB. Intramuscular midazolam for treatment of acute seizures or behavioral episodes in patients with brain injuries. J Neurol Neurosurg Psychiatr. 1992;55:328–329.
53. Hanley, DF, Jr., Pozo, M. Treatment of status epilepticus with midazolam in the critical care setting. Int J Clin Pract. 2000;54:30–35.
54. Feldman, HS, Arthur, GR, Pitkanen, M, et al. Treatment of acute systemic toxicity after the rapid intravenous injection of ropivacaine and bupivacaine in the conscious dog. Anaesth Analg. 1991;73:373–384.
55. Daublander M: The role of the vasoconstrictor. Paper presented at: 3M ESPE Expert Conference, Munich, Germany, April 2011.
56. Kellam, SA, Smith, JR, Scheffel, SJ. Epinephrine absorption from commercial gingival retraction cords in clinical patients. J Prosthet Dent. 1992;68:761–765.
57. ADA/PDR. Ada guide to dental therapeutics, ed 5. Chicago: The American Dental Association; 2009.
58. Gomes, ER, Demoly, P. Epidemiology of hypersensitivity drug reactions. Curr Opin Allergy Clin Immunol. 2005;5:309–316.
59. Brown, DT, Beamish, D, Wildsmith, JA. Allergic reaction to an amide local anaesthetic. Br J Anaesth. 1981;53:435–437.
60. Aldrete, JA, O’Higgins, JW. Evaluation of patients with history of allergy to local anesthetic drugs. South Med J. 1971;64:1118–1121.
61. Boren, E, Teuber, SS, Nguwa, SM, et al. A critical review of local anesthetic sensitivity. Clin Rev Allergy Immunol. 2007;32:119–128.
62. Jackson, D, Chen, AH, Bennett, CR. Identifying true lidocaine allergy. J Am Dent Assoc. 1994;125:1362–1366.
63. Doyle, KA, Goepferd, SJ. An allergy to local anesthetics? The consequences of a misdiagnosis. ASDC J Dent Child. 1989;56:103–106.
64. Thyssen, JP, Menne, T, Elberling, J, et al. Hypersensitivity to local anaesthetics—update and proposal of evaluation algorithm. Contact Dermatitis. 2008;59:69–78.
65. Harboe, T, Guttormsen, AB, Aarebrot, S, et al. Suspected allergy to local anaesthetics: follow-up in 135 cases. Acta Anaesthesiol Scand. 2010;54:536–542.
66. Haas, DA. An update on local anesthetics in dentistry. J Can Dent Assoc. 2002;68:546–551.
67. Schwartz, HJ, Sher, TH. Bisulfite sensitivity manifesting as allergy to local dental anesthesia. J Allergy Clin Immunol. 1985;75:525–527.
68. Seng, GF, Gay, BJ. Dangers of sulfites in dental local anesthetic solutions: warnings and recommendations. J Am Dent Assoc. 1986;113:769–770.
69. Perusse, R, Goulet, JP, Turcotte, JY. Sulfites, asthma and vasoconstrictors. Can Dent Assoc J. 1989;55:55–56.
70. Shojaie, AR, Haas, DA. Local anesthetic cartridges and latex allergy: a literature review. J Can Dent Assoc. 2002;68:622–626.
71. Perusse, R, Goulet, JP, Turcotte, JY. Contraindications to vasoconstrictors in dentistry. Part II. Hyperthyroidism, diabetes, sulfite sensitivity, cortico-dependent asthma, and pheochromocytoma. Oral Surg Oral Med Oral Pathol. 1992;74:687–691.
72. Bruze, M, Gruvberger, B, Thulin, I. PABA, benzocaine, and other PABA esters in sunscreens and after-sun products. Photodermatol Photoimmunol Photomed. 1990;7:106–108.
73. Boyce, JA, Assa’ad, A, Burks, AW, et al. Guidelines for the diagnosis and management of food allergy in the United States: report of the NIAID-Sponsored Expert Panel. J Allergy Clin Immunol. 2010;126(Suppl 6):S1–S58.
74. Malamed, SF. Medical emergencies in the dental office, ed 6. St Louis: Mosby; 2007.
75. Peter, R. Sudden unconsciousness during local anesthesia. Anesth Pain Control Dent. 1993;2:140–142.
76. Chandler, MJ, Grammer, LC, Patterson, R. Provocative challenge with local anesthetics in patients with a prior history of reaction. J Allergy Clin Immunol. 1987;79:883–886.
77. Orr, DL, II. It’s not Novocain, it’s not an allergy, and it’s not an emergency!. Nev Dent Assoc J. 2009;11:3–6.
78. Riedenburg, MM, Lowenthal, DT. Adverse nondrug reaction. N Engl J Med. 1968;279:678–679.
79. Hodgson, TA, Shirlaw, PJ, Challacombe, SJ. Skin testing after anaphylactoid reactions to dental local anesthetics: a comparison with controls. Oral Surg Oral Med Oral Pathol. 1993;75:706–711.
80. Rozicka, T, Gerstmeier, M, Przybilla, B, et al. Allergy to local anesthetics: comparison of patch test with prick and intradermal test results. J Am Acad Dermatol. 1987;16:1202–1208.
81. Eggleston, ST, Lush, LW. Understanding allergic reactions to local anesthetics. Ann Pharmacother. 1996;30:851–857.
82. Canfield, DW, Gage, TW. A guideline to local anesthetic allergy testing. Anesth Prog. 1987;34:157–163.
83. Swanson, JG. An answer for a questionable allergy to local anesthetics. Ann Emerg Med. 1988;17:554.
84. Malamed, SF. The use of diphenhydramine HCl as a local anesthetic in dentistry. Anesth Prog. 1973;20:76–82.
85. Ernst, AA, Anand, P, Nick, T, et al. Lidocaine versus diphenhydramine for anesthesia in the repair of minor lacerations. J Trauma. 1993;34:354–357.
86. Uckan, S, Guler, N, Sumer, M, et al. Local anesthetic efficacy for oral surgery: comparison of diphenhydramine and prilocaine. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1998;86:26–30.
87. Willett, J, Reader, A, Drum, M, et al. The anesthetic efficacy of diphenhydramine and the combination diphenhydramine/lidocaine for the inferior alveolar nerve block. J Endod. 2008;34:1446–1450.
88. Lieberman, P, Kemp, SF, Oppenheimer, J, et al. The Diagnosis and Management of Anaphylaxis: An Updated Practice Parameter. Allerg Clin Immunol. 2005;115(3):S483–S523.
89. Oh, VM. Treatment of allergic adverse drug reactions. Singapore Med J. 1989;30:290–293.
90. Adkinson, NF, Jr., Busse, WW, Bochner, BS, et al. Middleton’s allergy: principles and practice, ed 7. St Louis: Mosby; 2009.
91. Stafford, CT. Life-threatening allergic reactions: anticipating and preparing are the best defenses. Postgrad Med. 1989;86:235–242. [245].