Chapter 47 Infection
Introduction
Infection is still a significant cause of abortion, fetal malformation, prematurity, infant death and long-term morbidity, especially in sick and preterm babies (Newell & Darling 2008). Normally the fetus is protected from infection during pregnancy (congenital infection) by the cervical mucus plug, intact amniotic sac and placenta, all of which act as a barrier to most bacterial conditions; but certain viruses and protozoa, because of their small molecular size, can cross the placenta, causing teratogenic (fetal malformation) effects and infections (Box 47.1).
Box 47.1
TORCH
The acronym TORCH can be used as an aide-mémoire for some infections that can affect the fetus in utero:
The fetus can also acquire infection around the time of birth (perinatal infection) due to exposure to maternal infection in the birth canal or birth trauma that causes abrasion of newborn skin, giving a potential portal of entry for infection. In the neonatal period (postnatal infection) infection may be acquired from the mother, other babies, hospital equipment; inadequate handwashing by health professionals, carers and parents; and droplet infections via the respiratory route. Puncturing the skin, such as during the Guthrie blood spot test, also provides a potential portal of entry for infection, and, in certain circumstances, infection can be acquired through breastfeeding.
Bacterial infections include those caused by group B streptococcus (GBS) and Listeria monocytogenes and sexually transmitted diseases such as chlamydia, gonorrhoea and syphilis. Viral infections include cytomegalovirus (CMV), herpes simplex virus (HSV), rubella, hepatitis, varicella–zoster and human immunodeficiency virus (HIV). Toxoplasmosis is a protozoal infection and candidiasis a fungal infection.
The effect of fetal infection depends upon the nature of the organism and the stage of gestation. For example, exposure to rubella in the first trimester of pregnancy is associated with a high risk of serious congenital defects, whereas exposure in late pregnancy poses little risk. In contrast, genital herpes infection in early pregnancy poses little risk, but if acquired at birth there is a high risk of neonatal infection. Exposure to primary CMV infection in pregnancy gives a risk of adverse neonatal outcome at any stage of pregnancy, but infection acquired during birth or in the postnatal period through breastfeeding is not associated with adverse neonatal outcome (Newell & McIntyre 2000).
Some infections have long-term sequelae which may not become apparent for months or even years. For example, the ophthalmic damage caused by chlamydia becomes apparent in the neonatal period but the pneumonia associated with chlamydia infection usually occurs months after delivery; deafness associated with congenital CMV, toxoplasmosis, syphilis and rubella infection often does not become apparent until later in childhood; and hepatitis B and C infection may result in an initial infection but chronic hepatitis develops later and after hepatitis B infection cirrhosis and carcinoma of the liver do not occur for several decades (Newell & McIntyre 2000).
Antenatal screening for infection
Currently, all women in early pregnancy in the UK are offered screening for syphilis, HIV, hepatitis B and rubella (UKNSC/HPA 2007). Women who present in labour without having received any antenatal care should be offered screening for these four infections in labour.
At initial booking, midwives must ensure sensitive questioning reveals any risk factors for infections. Immigrants and refugees from different countries may not have had rubella vaccinations or may come from areas with a high incidence of tuberculosis or HIV. Vaccination programmes address some conditions, such as hepatitis B and rubella, and research into vaccines for other pathogens, such as HIV and GBS, continues.
Newborn immunity
Both preterm and term infants are vulnerable to infection because they are naturally immunodeficient at birth. Also, because the immune system is not exposed to common organisms until birth, there is an initial delayed or diminished response to any invading organisms (Blackburn 2007).
Newborn term infants do have some degree of natural immunity at birth due to the following:
The complement system
The complement system is a major component of innate immunity. Complement consists of a series of plasma proteins and their fragments that, when activated, enhance other components of the immune system. For example, the effect of complement on the cell membrane of invading organisms enables their destruction by other defence mechanisms of the body (Blackburn 2007). Breast milk contains some components of the complement system but the overall action of complement is limited at birth.
Prevention of infection
Midwives must be vigilant in recognizing risk factors and early symptoms of maternal and neonatal infection. To do this effectively requires multidisciplinary working to prevent, diagnose and promptly treat infection in the mother, baby and, if necessary, the midwife.
The midwife needs to educate women to be aware of sources of potential infection that may affect her and/or her child and ensure that any infection during pregnancy is managed and treated promptly. As well as maternal transmission of infection, organisms can be introduced during invasive antenatal procedures, such as amniocentesis. Intrauterine pneumonia is the commonest effect, but it depends on the pathogens introduced. Strict aseptic techniques must be assured.
Newborn infants in maternity units are at risk of cross-infection and frequent, effective handwashing remains the single most important method of preventing the spread of infection (NPSA 2010: see website). Other strategies include newborn ‘rooming in’ with the mother, encouraging breastfeeding to increase immune protection, using individual equipment for each baby, and, if necessary, isolation of an infected infant. Visitors should be discouraged from sitting on beds and from visiting if they have an infection or feel unwell.
To avoid exposure to bloodborne infections, such as hepatitis B and HIV, midwives must integrate into their practice the Department of Health universal precautions (DH 1998) to reduce exposure to blood and other body fluids and tissue that may contain bloodborne pathogens. Universal precautions include covering any skin cuts/lesions with a waterproof dressing, wearing rubber gloves and other protective clothing as appropriate, avoiding needlestick injuries and disposing safely of sharps (needles) and other instruments and waste, and vaccination against hepatitis B.
Signs and symptoms of infection in the newborn
Newborn infection resulting from antenatal or intrapartum transmission of infections such as varicella, listeriosis, HSV, GBS, rubella, syphilis, chlamydia or gonorrhoea usually becomes apparent during the neonatal period. Early-onset infection occurs within the first 48 hours; late onset is after 72 hours.
The presentation of infection in the newborn is often subtle and difficult to recognize. It is important that midwives are alert to the possibility of infection so as to detect early signs and seek paediatric advice to enable prompt diagnosis and treatment.
When the membranes rupture, the fetus becomes susceptible to organisms from the birth canal; the infections most likely to be acquired in this way are pneumonia and/or meningitis due to GBS infection or Listeria monocytogenes, gonococcal and chlamydia conjunctivitis, Candida albicans (a fungal infection) and herpes simplex (Newell & Darling 2008).
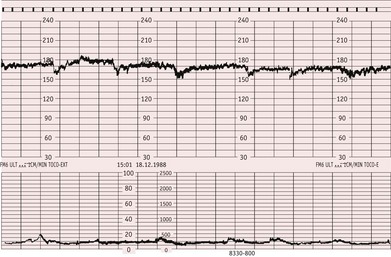
The possibility of neonatal infection should always be borne in mind if labour is preterm or there is prolonged rupture of the membranes, especially if chorioamnionitis has developed. Maternal pyrexia in labour, especially if preterm, and a cardiotocogragh (CTG) showing a fetal heart rate pattern of tachycardia with reduced variability, and no acclerations, can also be indicators of the possibility of fetal infection (Gibb & Arulkumaran 2008). The midwife should seek an obstetric clinical review because maternal investigations such as blood cultures and antibiotic treatment may be required and the baby should be screened at birth.
The baby at birth
Diagnosis of neonatal infection requires a high index of suspicion and if there is any doubt the baby should be seen by a paediatrician. A baby with infection at birth will often have an Apgar score that is within normal limits. A neonate with infection quickly becomes cold, and despite warming-up techniques being used, the temperature remains unstable. The baby appears lethargic and there is recurrent apnoea with pallor and mottling of the skin. The baby is reluctant to feed and a blood sugar, if tested, will be low.
Urgent referral to a paediatrician for further investigations is imperative as babies often deteriorate rapidly when ill. An infection screen will be carried out and includes a full blood count, blood culture, chest X-ray, and microscopy and culture of urine and cerebrospinal fluid. Treatment using broad-spectrum antibiotics will be started pending results of screening tests (Newell & Darling 2008).
Infections acquired during pregnancy
Listeriosis
Listeriosis is an uncommon but serious neonatal infection transmitted via the placenta. It is caused by the Gram-positive bacillus Listeria monocytogenes. Intrauterine infection can result in either spontaneous abortion or stillbirth; preterm labour and amnionitis are common. Listeriosis can cause a green staining of the liquor, which may be mistaken for meconium. Meconium is not normally passed prior to 34 weeks’ gestation; therefore, in a labour of less than 34 weeks’ gestation, green staining of the liquor should alert the midwife to the possibility of listeriosis. With listeriosis, the CTG will show a persistent tachycardia with markedly reduced variability and shallow decelerations (Fig. 47.1).
Listeriosis is usually apparent at birth or within the first few hours of life. The infant has a widespread rash with septicaemia, pneumonia and meningitis. The mortality rate is 30%. Late onset usually presents as meningitis between 1 to 8 weeks of age but has a better prognosis than early onset (Lissauer & Clayden 2007).
Syphilis
Syphilis is caused by the spirochaete Treponema pallidum and is acquired by direct sexual contact (see Ch. 57). Because Treponema pallidum crosses the placenta, all pregnant women in the UK are routinely screened for syphilis in early pregnancy. This prevents most cases of congenital syphilis because women with a confirmed positive result are referred to a sexual health clinic for assessment and treatment with parenteral penicillin which prevents mother-to-child transmission (National Collaborating Centre for Women’s and Children’s Health 2008). If women have a full course of treatment a month or more before birth, the infant does not require treatment and has an excellent prognosis; however, if there is any doubt about the adequacy of maternal treatment, the infant will be treated with penicillin (Lissauer & Clayden 2007).
If syphilis is not treated in pregnancy, 70% to 100% of neonates will be infected and up to one-third of these infants will be stillborn (National Collaborating Centre for Women’s and Children’s Health 2008). Infected infants may be asymptomatic at birth with clinical features not becoming apparent until 2 to 12 weeks after birth. Clinical features specific to congenital syphilis include a characteristic rash on the hands and soles of the feet, eye defects and microcephaly. On X-ray bone abnormalities will be seen. Congenital syphilis is very rare in the UK.
Hepatitis B virus
Intrauterine transmission of the hepatitis B virus (HBV) is uncommon because the virus does not readily cross the placenta; transmission generally occurs in the perinatal and postnatal period. Infected infants usually become asymptomatic carriers, with approximately 30–50% developing chronic HBV liver disease, which in 10% of children may progress to cirrhosis. There is a long-term risk of hepatocellular carcinoma.
Routine antenatal testing for the hepatitis B surface antigen (HBsAg) identifies those women at risk and babies of women who are HBsAg-positive should be given hepatitis B vaccination as soon as possible after birth (within 24 hours). Hepatitis B immunoglobulin (HBIG) is given as well if the mother is also hepatitis B e antigen (HBeAg)-positive because this indicates viral activity which can persist for weeks (Newell & McIntyre 2000). Babies with a birthweight of 1500 g or less born to hepatitis B-infected mothers should receive HBIG in addition to the vaccination regardless of the antigen status of the mother (UKNSC/HPA 2007). If two injections are required, they should be given on two different sites. Further injections are required to complete the vaccination programme and are usually given at 1 month and 6 months of age although vaccination programmes can vary according to area (Newell & McIntyre 2000).
Hepatitis C virus
Hepatitis C virus (HCV) is common amongst intravenous drug users. Mother-to-child transmission of HCV is rare unless there is co-infection with HIV. It seldom causes an acute infection but at least 50% of children will develop cirrhosis, hepatic carcinoma and eventually liver failure. Treatment is a combination of interferon and ribavirin therapy, which is successful in 50% of children (Lissauer & Clayden 2007).
HIV
Babies are usually affected by HIV type I; the usual route of infection in the Western world is vertical transmission from mother to infant during pregnancy, labour and the postnatal period (through breastfeeding) (see Ch. 57) but the incidence of vertical transmission in Western Europe and the USA has been reduced through HIV testing in pregnancy, retroviral treatment of women and the use of infant formula feeding (HIV I DNA is present in breast milk). This has resulted in fewer than 20 of the 1000 babies born each year in the UK to HIV-positive mothers being infected with the virus (Lissauer & Clayden 2007).
Diagnosis of neonatal HIV infection is complicated by the presence of passively acquired maternal antibody, which may persist for up to 18 months of age. Prior to 18 months of age, the most sensitive test for HIV is by detection of the viral genome by HIV DNA PCR (polymerase chain reaction). Two negative HIV DNA PCRs within the first 3 months of life, at least 2 weeks after completion of postnatal antiretroviral therapy, indicate the infant is not infected, although this cannot be confirmed until after 18 months of age (Lissauer & Clayden 2007).
Infected babies appear normal at birth; however, without prophylactic treatment, nearly 25% will develop acquired immunodeficiency syndrome (AIDS) or die in the first year of life; the remaining children may not show any signs of the disease until their teenage years. Common symptoms of AIDS developing in HIV-infected infants are failure to thrive, recurrent infections, diarrhoea and severe candida (thrush) infection (Newell & Darling 2008). Infants infected with HIV are susceptible to TB but BCG vaccination should not be given because it is a live mycobacterial vaccine (Lissauer & Clayden 2007).
Toxoplasmosis
The overall rate of fetal infection following exposure to maternal toxoplasmosis depends upon the timing of maternal infection. The rate of transmission is low (10%) during the first 2 weeks of pregnancy and increases to over 90% by the last 2 weeks of pregnancy; but the risk of adverse fetal outcome is highest following exposure to infection during the first trimester of pregnancy rather than in later pregnancy (Newell & McIntyre 2000). Clinical signs of neonatal toxoplasmosis include low birthweight, enlarged liver and spleen, hydrocephalus, jaundice and anaemia. Up to 85% of congenitally infected neonates are asymptomatic at birth, but most will develop complications, including seizures and reduced cognitive function, over time. Infected newborn infants are treated for 1 year with pyrimethamine and sulfadiazine (Lissauer & Clayden 2007). Regular blood tests are required during treatment because these drugs cause bone marrow suppression (Newell & McIntyre 2000).
Rubella (German measles)
The extent of fetal damage following maternal rubella infection is determined by gestational age at the onset of infection. Infection before 8 weeks’ gestation causes deafness, congenital heart disease and cataracts in over 80% of fetuses (Fig. 47.2). The fetus develops a viraemia which inhibits cell division and causes defects of the developing organs. Sometimes, spontaneous abortion occurs. Approximately 30% of fetuses infected between 13 and 16 weeks’ gestation will have impaired hearing. Beyond 18 weeks’ gestation, the risk to the fetus is minimal.
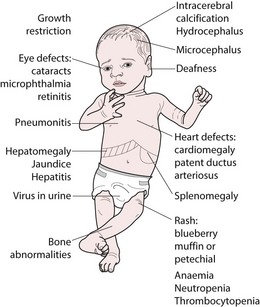
Figure 47.2 Clinical features of congenital rubella, cytomegalovirus (CMV), toxoplasmosis and syphilis.
(Lissauer & Claydon 2007:131.)
Babies with congenital rubella are very infectious and may excrete rubella virus in the urine for up to 12 months. They pose a cross-infection risk to other babies as well as to pregnant women. Isolation of mother and baby is necessary in hospital and great care required at home. Close follow-up is required, as neurological disorders, which are usually significant, may not be immediately obvious (Newell & McIntyre 2000).
Cytomegalovirus
Cytomegalovirus (CMV) is a herpes virus. After primary infection it remains latent but may become active if immunity is compromised. Exposure to primary CMV infection at any stage of pregnancy gives a risk of adverse neonatal outcome because viraemia occurs and the virus can cross the placenta. Congenital CMV infection affects 3–4/1000 live births in the UK (Lissauer & Clayden 2007). It can cause intrauterine death and stillbirth but infection acquired during birth or in the postnatal period through breastfeeding is not associated with adverse neonatal outcome unless the infant is premature (Newell & McIntyre 2000).
The majority of infected infants are asymptomatic at birth and develop normally; 5% will have clinical signs and symptoms associated with congenital CMV, such as microcephaly, cerebral palsy, pneumonitis, jaundice, thrombocytopenia and virus shedding. Approximately 5% of infected infants develop problems later in life, mainly hearing problems (Lissauer & Clayden 2007). Diagnosis of CMV can be confirmed by the isolation of CMV from throat swabs and urine samples (Newell & McIntyre 2000).
Varicella zoster
This virus is responsible for chickenpox. The effect of maternal varicella infection upon the fetus is determined by gestational age at the time of infection. Maternal varicella infection in the first 20 weeks of pregnancy results in congenital varicella syndrome in about 2% of neonates, causing chorioretinitis, skin lesions, skeletal abnormalities, encephalitis and neurological damage.
Maternal infection developing within 5 days before or 2 days after delivery has more serious implications for the neonate because the fetus is unprotected by maternal antibodies and the viral dose is high. About 25% of these infants will develop a vesicular rash. The mortality rate is 30%. These babies should be given varicella zoster immunoglobulin to reduce the risk of serious complications, including hepatic disorders and pneumonia. Aciclovir can also be given to the neonate prophylactically (Lissauer & Clayden 2007). Mother and baby should be isolated from other neonates.
Infections acquired during birth
Group B streptococcus (Streptococcus agalactiae)
Group B streptococcus (GBS) is commonly found in the gastrointestinal tract and colonizes the vagina in approximately 15% to 30% of women in the UK (Feldman 2001, UKNSC/HPA 2007).
The organism possesses an enzyme which can make microscopic holes in the amniotic sac, enabling it to reach the amniotic fluid and infect the fetus through the lung epithelium (Feldman 2001).
GBS is the commonest cause of overwhelming sepsis in the newborn, including pneumonia and meningitis, with an incidence in the UK of 1 : 1000 live births (Feldman 2001). Eighty percent of infections are early onset, most of which are clinically apparent at or immediately after birth. The mortality rate is 18% in premature infants and 6% in the term infant (UKNSC/HPA 2007).
Late onset occurs between 7 and 90 days. The infant is not colonized with GBS at birth but acquires it at a later stage, whereupon septicaemia rapidly develops, often accompanied by meningitis (Feldman 2001).
Diagnosis of GBS carriage in pregnancy
GBS carriage is asymptomatic but routine testing for GBS in pregnancy is not currently recommended in the UK (RCOG 2003, UKNSC/HPA 2007). Currently, a risk factor-based screening approach is used and intrapartum antibiotic prophylaxis is offered to women with recognized risk factors for early-onset GBS disease (HPA 2006a, RCOG 2003, UKNSC/HPA 2007). The risk factors are:
A multidisciplinary GBS Working Party set up by the Health Protection Agency published Interim ‘good practice’ recommendations for the prevention of early onset neonatal group B streptococcal (GBS) infection in UK (HPA 2006a) (see Figure 47.3 and website).
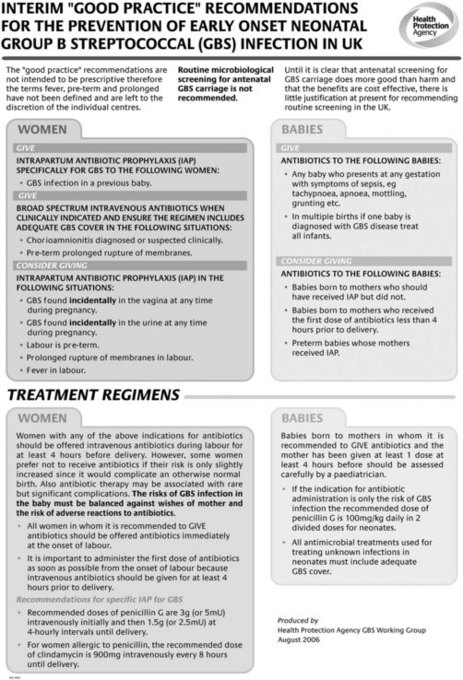
Figure 47.3 Group B Streptococcal (GBS) guidelines
(©Health Protection Agency. Reproduced with permission.)
Incidental diagnosis of GBS
Because there is no organized approach to GBS screening in the UK, carriage is usually found incidentally either through sending a midstream specimen of urine or a HVS (high vaginal swab) for culture during pregnancy. Using a HVS is unsatisfactory because it can give false negative results, but if GBS is detected incidentally from a HVS, intrapartum antibiotic prophylaxis should be considered.
Specific testing for GBS
The correct method is to take a low vaginal swab (from just inside the introitus) and then a rectal swab (the same swab or two separate swabs can be used) between 35 and 37 weeks’ gestation. Swabs taken at this time are effective in predicting whether or not there will be GBS carriage during labour. A special enrichment medium is used to culture the swabs to avoid overgrowth of other organisms to increase the likelihood of GBS isolation (HPA 2006b). Vaginal GBS carriage is not treated during pregnancy but intrapartum antibiotic prophylaxis is recommended.
GBS urine infection
If GBS is found in the urine during pregnancy, there is a higher risk of neonatal infection. The urinary infection should be treated at the time of diagnosis and intrapartum prophylaxis should also be offered (RCOG 2003).
GBS carriage and home birth
Women booked for a home birth may need to accept delivery in hospital if they have opted to receive intrapartum intravenous antibiotics. Routine community use of intravenous antibiotics may not be available and community midwives or GPs may be unwilling to accept the risk of anaphylaxis in the home environment.
The majority of research supporting the benefits of intrapartum prophylaxis relates to intravenous administration, but there is some evidence that the intramuscular route may be effective. If a woman fully understands that using the intramuscular route is based upon limited evidence, instead of intravenous therapy, benzyl penicillin 600 mg IM 8-hourly can be used; or erythromycin 100 mg IM 8-hourly if the woman is allergic to penicillin (UKNSC/HPA 2007).
Ophthalmia neonatorum
Ophthalmia neonatorum is defined as a purulent discharge from the eyes of an infant within 21 days of birth. It is a notifiable condition usually acquired during birth. Causative organisms include Staphylococcus aureus, Streptococcus pneumoniae, E. coli, Chlamydia trachomatis and Neisseria gonorrhoeae. A paediatrician must be notified immediately and swabs taken for culture and sensitivity – differential diagnosis of the organism is essential especially for chlamydial and gonococcal infections as these two organisms can cause conjunctival scarring, corneal infiltration and blindness.
Chlamydia trachomatis causes a purulent discharge with swelling of the eyelids that usually occurs within 10 days of life. Treatment is with oral erythromycin. Pneumonia can affect between 1% and 22% of infants. Symptoms (coughing and cyanosis) usually appear before 2 months of age (Newell & McIntyre 2000). Treatment is a broad-spectrum antibiotic given either intravenously or orally depending upon the severity of the illness (Lissauer & Clayden 2007) (see Fig. 47.4).

Figure 47.4 Purulent discharge together with swollen eyelids in an 8-day-old infant. This is the characteristic presentation of conjunctivitis from Chlamydia trachomatis. Neisseria gonorrhoeae was absent.
(From Lissauer & Clayden 2007:165.)
Gonococcal eye infection also manifests as a purulent discharge and swelling of the eyelids but within 48 hours of birth. Penicillin is the treatment of choice or intravenous cephalosporin if there is the possibility of penicillin resistance. For all eye infections, the eyes must be cleaned frequently and eye drops may also be prescribed (Lissauer & Clayden 2007) (see website).
Herpes simplex virus
Herpes simplex virus (HSV) is associated with active maternal genital herpes and is usually acquired during birth. HSV infection can be congenital and can cause a range of illnesses in the neonatal period, from skin blisters to overwhelming viraemia and encephalitis. Caesarean section may be the mode of delivery of choice when there are active herpetic lesions. Diagnosis requires culture of the virus from the affected skin, and once confirmed, treatment should be commenced as soon as the infection is identified. Infected neonates are treated with systemic aciclovir.
Candida (thrush)
Candida albicans is the commonest cause of fungal infections in infants. It may be acquired at delivery if the mother has a vaginal infection as a result of reduced resistance during antibiotic therapy or from inadequate hygiene practices.
Oral infection appears as white patches on the tongue, gums and palate; if the patches are removed, they leave a raw red area. If the mother is breastfeeding, her nipples should also be treated to prevent reinfection. Infection in the nappy area presents with a generalized papular or vesicular rash and antifungal preparations are effective treatments.
Disseminated candidiasis is an overwhelming septicaemia, usually found in preterm, very low birthweight babies. There is significant associated morbidity and mortality because this serious disease can affect all the major organs. Infection of the central nervous system has a poor outcome for extremely low birthweight babies, with over 40% having severe disabilities at 2 years of age (Friedman et al 2000). Prompt treatment is essential because this is a life-threatening condition. Aggressive intravenous treatments with both antifungal and antibacterial agents are required. The treatment of choice is intravenous fluconazole – an antifungal agent increasingly used, instead of amphotericin B and flucytosine, and which may be given orally or intravenously in the management of neonatal C. albicans infection.
Postnatal infections
Mild eye infections and ‘sticky eyes’ are not uncommon in the newborn and in many cases no bacteria are found. It is important to teach mothers good hygiene and care of the eyes. Handwashing is essential, and cool, boiled water, or sterile saline, and sterile cotton wool swabs are used to clean the eyes from the inner aspect to the outer, discarding the swab after one sweep.
Umbilical cord infection (Omphalitis)
Severe cord sepsis is uncommon and with good standards of hygiene can be prevented. The midwife must check the umbilicus regularly. Signs of infection include periumbilical inflammation, a moist, offensive smelling cord and delay in separation. Infection may be transported through the umbilical vein to the liver. The organism most commonly responsible is Staph. aureus, and, if found, antibiotics are required.
Pemphigus neonatorum
This is a potentially fatal staphylococcal infection. Because of its highly contagious character and severe effects, the midwife should consider any skin lesion associated with the formation of a blister or pus as a possible case of pemphigus.
Blisters, which fill with pus and burst leaving a raw surface, appear on the head or trunk. This is often called the staphylococcal scalded skin syndrome since the appearance mimics that of a scald. As the infection spreads in the superficial tissue, large areas become involved. Complications may arise since staphylococci can also affect the lungs, gut and liver.
Treatment is with systemic antibiotics such as flucloxacillin, which are given intravenously. It is also important to monitor for dehydration and other complications caused by fluid loss.
Gastroenteritis
This is highly infectious and carries a high risk of mortality for compromised babies. For this reason, an outbreak in a neonatal intensive care unit (NICU) or special care baby unit (SCBU) is a catastrophe. The neonate can quickly become very ill and dehydrated. Electrolyte imbalance, if not speedily treated, leads to tachycardia, hypotension and collapse. There are a number of possible causative organisms, including Salmonella, Shigella (a form of E. coli), echovirus type II and rotavirus. Isolation of infected babies is important to prevent cross-infection.
Preventive measures are of the utmost importance: high standards of hygiene must be maintained and effective handwashing practices are vital.
Prevention of newborn infection
A proactive approach should be taken regarding risk-identification, screening and treatment of infections in women, preconceptionally and antenatally, in order to reduce fetal and neonatal mortality and morbidity. The majority of these conditions are preventable, and midwives can do much to reduce their incidence and severity with education, awareness, early diagnosis and treatment.
Key Points
Blackburn ST. Maternal, fetal and neonatal physiology: a clinical perspective, ed 3. Philadelphia: Saunders Elsevier; 2007.
Dai D, Walker WA. Protective nutrients and bacterial colonization in the immature human gut. Advances in Pediatrics. 1999;46:353-382.
Department of Health (DH). Guidance for clinical health care workers: protection against infection with blood-borne viruses: recommendations of the Expert Advisory Group on AIDS and the Advisory Group on hepatitis. London: UK Health Departments; 1998.
Feldman RG. Group B streptococcus: prevention of infection in the newborn. The Practising Midwife. 2001;4(3):16-18.
Friedman S, Richardson SE, Jacobs SE, et al. Systemic candida infection in extremely low birth weight infants: short term morbidity and long term neurodevelopmental outcome. Pediatric Infectious Disease Journal. 2000;19(6):499-504.
Gibb D, Arulkumaran S. Fetal monitoring in practice, ed 3. London: Churchill Livingstone; 2008.
Health Protection Agency (HPA). Interim ‘good practice’ recommendations for the prevention of early onset neonatal group B streptococcal (GBS) infection in UK. London: London; 2006.
Health Protection Agency (HPA). Processing swabs for group B streptococcal carriage BSOP 58. London: HPA; 2006.
Jones JL, Lopez A, Wilson M, et al. Congenital toxoplasmosis: a review. Obstetrical & Gynecological Survey. 2001;56(5):296-305.
Kelly D, Coutts AG. Early nutrition and development of immune function in the neonate. Proceedings of the Nutrition Society. 2000;59(2):177-185.
Lissauer T, Clayden G. Illustrated textbook of paediatrics, ed 3. London: Elsevier; 2007.
National Collaborating Centre for Women’s and Children’s Health. Antenatal care: routine care for the healthy pregnant woman. London: RCOG; 2008.
National Patient Safety Agency (NPSA). Prevention of infection – correct washing hand technique. (website) www.npsa.nhs.uk/cleanyourhands/the-campaign/training-video/, 2010.
Newell SJ, Darling JC. Paediatrics, ed 8. Oxford: Blackwell Publishing; 2008.
Newell ML, McIntyre J. Congenital and perinatal infections: prevention, diagnosis and treatment. Cambridge: Cambridge University Press; 2000.
Oddy WH. Breastfeeding protects against illness and infection in infants and children: a review of the evidence. Breastfeeding Review. 2001;9(2):11-18.
Royal College of Obstetricians and Gynaecologists (RCOG). Prevention of early onset neonatal group B streptococcal disease. Guideline 36. London: RCOG; 2003.
UK National Screening Committee & Health Protection Agency (UKNSC/HPA). Briefing paper for health professionals to support the DH UK ‘screening for infectious diseases in pregnancy programme’ version 4. 2007.