Small Intestine
• Adjust the patient so that the midsagittal plane is centered to the grid.
• For a sthenic patient, center the IR at the level of L2 for radiographs taken within 30 minutes after the contrast medium is administered (Fig. 17-58).
• For delayed radiographs, center the IR at the level of the iliac crests.
• Respiration: Suspend at the end of expiration unless otherwise requested.
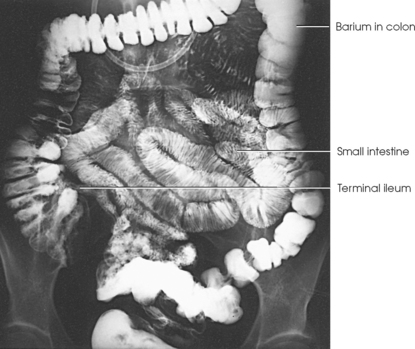
Structures shown: The PA or AP projection shows the small intestine progressively filling until the barium reaches the ileocecal valve (Figs. 17-59 to 17-62). When the barium has reached the ileocecal region, fluoroscopy may be performed, and compression radiographs may be obtained (Fig. 17-63). The examination is usually completed when the barium is visualized in the cecum, typically in about 2 hours for a patient with normal intestinal motility.
COMPLETE REFLUX EXAMINATION
For a complete reflux examination of the small intestine,1, 2 the patient’s colon and small intestine are filled by administering a BE to show the colon and small bowel. Before the examination, glucagon may be administered to relax the intestine. Diazepam (Valium) may also be given to diminish patient discomfort during the initial filling of the bowel. A 15% ± 5% weight/volume barium suspension is often used, and a large amount of the suspension (about 4500 mL) is required to fill the colon and small intestine.
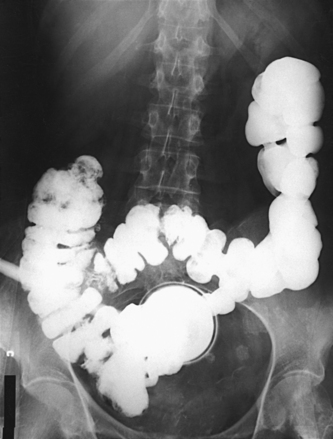
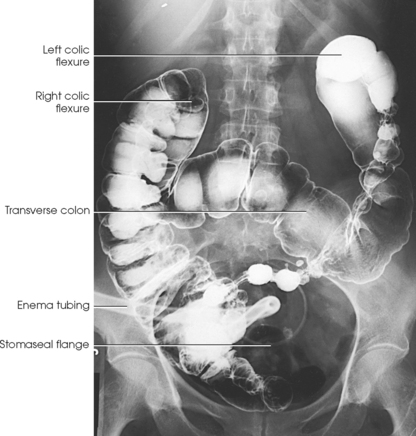
A retention enema tip is used, and the patient is placed in the supine position for the examination. The barium suspension is allowed to flow until it is observed in the duodenal bulb. The enema bag is lowered to the floor to drain the colon before radiographs of the small intestine are obtained (Fig. 17-64).
ENTEROCLYSIS PROCEDURE
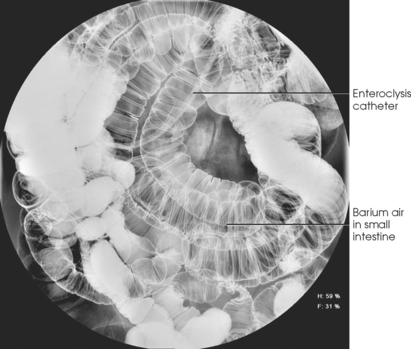
Enteroclysis (the injection of nutrient or medicinal liquid into the bowel) is a radiographic procedure in which contrast medium is injected into the duodenum under fluoroscopic control for examination of the small intestine. The contrast medium is injected through a specially designed enteroclysis catheter, historically a Bilbao or Sellink tube.
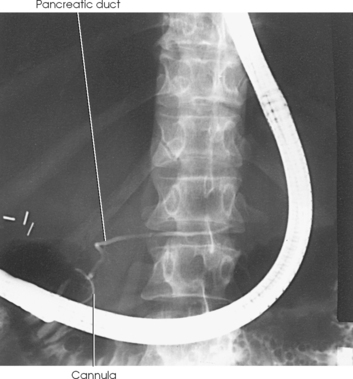
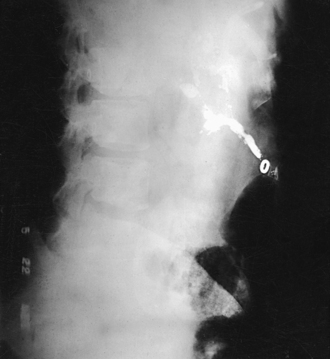
Before the procedure is begun, the patient’s colon must be thoroughly cleansed. Enemas are not recommended as preparation for enteroclysis because some enema fluid may be retained in the small intestine. Under fluoroscopic control, the enteroclysis catheter with a stiff guidewire is advanced to the end of the duodenum at the duodenojejunal flexure, near the ligament of Treitz. The retention balloon, if present, is filled with sterile water or saline. Barium is instilled through the tube at a rate of approximately 100 mL/min (Fig. 17-65). Spot radiographs, with and without compression, are taken as required. In some patients, air is injected after the contrast fluid has reached the distal small intestine (Fig. 17-66). When CT is to be performed, an iodinated contrast medium (Figs. 17-67 and 17-68) or tap water (Figs. 17-69 and 17-70) may be used.

Fig. 17-67 Enteroclysis with iodinated contrast medium. Filled retention balloon is seen in duodenum (arrow). (Courtesy Michelle Alting, AS, RT[R].)
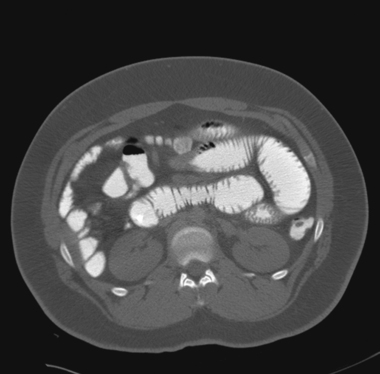
Fig. 17-68 Axial CT enteroclysis of the patient in Fig. 17-67.

Fig. 17-69 Axial CT enteroclysis with tap water and intravenous iodinated contrast medium. Intraluminal water (dark gray) is clearly delineated from bowel wall (light gray).
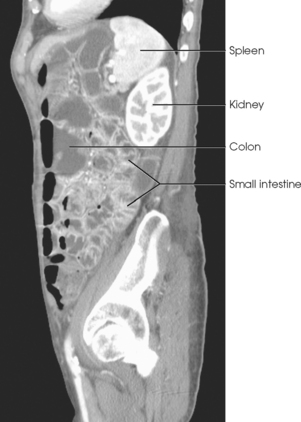
Fig. 17-70 Sagittal reconstruction of CT enteroclysis from Fig. 17-69.
After fluoroscopic examination of the patient’s small intestine, radiographs of the small intestine may be requested. The projections most often requested include AP, PA, obliques, and lateral. Recumbent and upright images may be requested. (Positioning descriptions involving the abdomen are presented in Chapter 16.)
INTUBATION EXAMINATION PROCEDURES
Gastrointestinal intubation is a procedure in which a long, specially designed tube is inserted through the nose and passed into the stomach. From there the tube is carried inferiorly by peristaltic action. Gastrointestinal intubation is used for therapeutic and diagnostic purposes.
When gastrointestinal intubation is used therapeutically, the tube is connected to a suction system for continuous siphoning of the gas and fluid contents of the gastrointestinal tract. The purpose of the maneuver is to prevent or relieve postoperative distention or to deflate or decompress an obstructed small intestine.
Although used much less frequently than in the past, a Miller-Abbott double-lumen, single-balloon tube (or other similar tubing) can be used to intubate the small intestine. Just above the tip of the Miller-Abbott tube is a small, thin rubber balloon. Marks on the tube, beginning at the distal end, indicate the extent of the tube’s passage and are read from the edge of the nostril. The marks are graduated in centimeters up to 85 cm and are given in feet thereafter. The lumen of the tube is asymmetrically divided into (1) a small balloon lumen that communicates with the balloon only and is used for the inflation and deflation of the balloon and for the injection of mercury to weight the balloon and (2) a large aspiration lumen that communicates with the gastrointestinal tract through perforations near and at the distal end of the tube. Gas and fluids are withdrawn through the aspiration lumen, and liquids are injected through it.
The introduction of an intestinal tube is an unpleasant experience for a patient, especially one who is acutely ill. Depending on the condition of the patient, the tube is more readily passed if the patient can sit erect and lean slightly forward or if the patient can be elevated almost to a sitting position.
With the intestinal tube in place, the patient is turned to an RAO position, a syringe is connected to the balloon lumen, and the mercury is poured into the syringe and allowed to flow into the balloon. The air is slowly withdrawn from the balloon. The tube is secured with an adhesive strip beside the nostril to prevent regurgitation or advancement of the tube. The stomach is aspirated, either by syringe or by attaching the large position of the lumen to the suction apparatus.
With the tip of the tube situated close to the pyloric sphincter and the patient in the RAO position (a position in which gastric peristalsis is usually more active), the tube should pass into the duodenum in a reasonably short time. Without intervention, this process sometimes takes many hours. Having the patient drink ice water to stimulate peristalsis is often successful. When this measure fails, the examiner guides the tube into the duodenum by manual manipulation under fluoroscopic observation. After the tube enters the duodenum, it is inflated again to provide a bolus that the peristaltic waves can more readily move along the intestine.
When the tube is inserted for decompression of an intestinal obstruction and possible later radiologic investigation, the adhesive strip is removed and replaced with an adhesive loop attached to the forehead. The tube can slide through the loop without tension as it advances toward the obstructed site. The patient is then returned to the hospital room. Radiographs of the abdomen may be taken to check the progress of the tube and the effectiveness of decompression. Simple obstructions are sometimes relieved by suction; others require surgical intervention.
If the passage of the intestinal tube is arrested, the suction is discontinued, and the patient is returned to the radiology department for a Miller-Abbott tube study. The contrast medium used for studies of a localized segment of the small intestine may be either a water-soluble, iodinated solution (Fig. 17-71, A) or a thin barium sulfate suspension. Under fluoroscopic observation, the contrast agent is injected through the large lumen of the tube with a syringe. Spot and conventional radiographs are obtained as indicated.
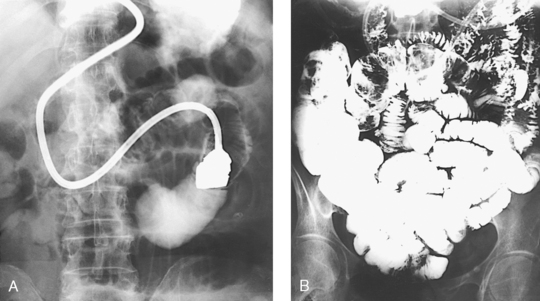
Fig. 17-71 A, Miller-Abbott tube study with water-soluble medium. B, Small bowel examination by Miller-Abbott tube with injection of barium sulfate.
When the intestinal tube is introduced for the purpose of performing a small intestine enema, the tube is advanced into the proximal loop of the jejunum and secured at this level with an adhesive strip taped beside the nose. Medical opinion varies regarding the quantity of barium suspension required for this examination (Fig. 17-71, B). The medium is injected through the aspiration lumen of the tube in a continuous, low-pressure flow. Spot and conventional radiographs are exposed as indicated. Except for the presence of the tube in the upper jejunum, the resultant radiographs resemble those obtained by the oral method.
CONTRAST MEDIA STUDIES
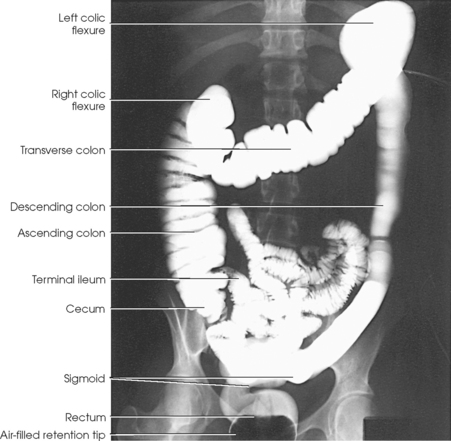
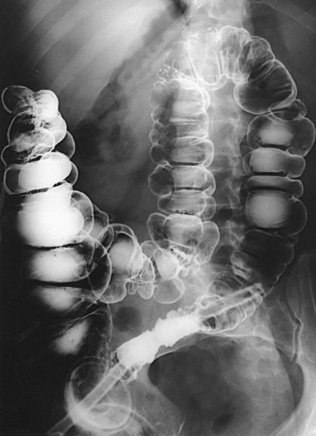
The two basic radiologic methods of examining the large intestine by means of contrast media enemas are (1) the single-contrast method (Fig. 17-72), in which the colon is examined with a barium sulfate suspension or water-soluble iodide only, and (2) the double-contrast method (Fig. 17-73), which may be performed as a two-stage or single-stage procedure. In the two-stage, double-contrast procedure, the colon is examined with a barium sulfate suspension and then, immediately after evacuation of the barium suspension, with an air enema or another gaseous enema. In the single-stage, double-contrast procedure, the fluoroscopist selectively injects the barium suspension and the gas.
The positive contrast medium shows the anatomy and tonus of the colon and most of the abnormalities to which it is subject. The gaseous medium serves to distend the lumen of the bowel and to render visible, through the transparency of its shadow, all parts of the barium-coated mucosal lining of the colon and any small intraluminal lesions, such as polypoid tumors.
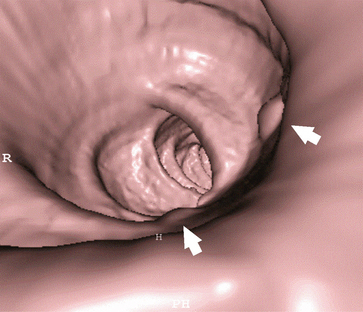
A more recent development in radiographic examination of the large intestine is computed tomography colonography (CTC), also called virtual colonoscopy (VC), a procedure used as a primary screening tool for colorectal cancer or after a failed conventional colonoscopy. This software-driven technique combines helical CT and virtual-reality software to create three-dimensional and multiplanar images of the colonic mucosa. Examples of currently available CTC techniques include the perspective filet or virtual dissection view, three-dimensional topographic view, multiplanar reformatted (MPR) view, and the colonoscopic-like endoluminal view (Figs. 17-74 to 17-76).
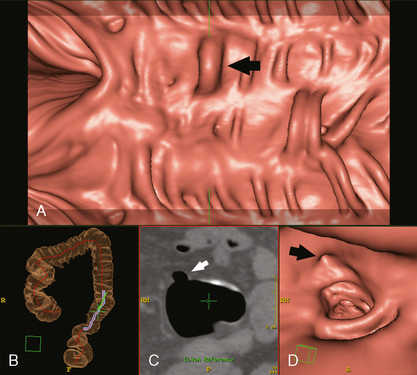
Fig. 17-74 Examples of CTC or VC. A, Perspective filet or virtual dissection view, showing diverticulum (arrow). B, Three-dimensional topographic view: Purple line in the sigmoid shows length of filet in A. C, Axial MPR, showing same diverticulum as in A (arrow). D, Endoluminal view showing opening (arrow) of diverticulum from A. (D, Courtesy J. Louis Rankin, BS, RT[R][MR].)
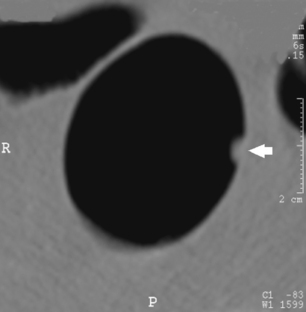
Fig. 17-76 Axial MPR image of upper tubular adenoma (arrow) from Fig. 17-75.
Contrast media
Commercially prepared barium sulfate products are generally used for routine retrograde examinations of the large intestine. Some of these products are referred to as colloidal preparations because they have finely divided barium particles that resist precipitation, whereas others are referred to as suspended or flocculation-resistant preparations because they contain some form of suspending or dispersing agent.
The newest barium products available are referred to as high-density barium sulfate. These products absorb a greater percentage of radiation, similar to older “thick” barium products. High-density barium is particularly useful for double-contrast studies of the alimentary canal in which uniform coating of the lumen is required.
Air is the gaseous medium usually used in the double-contrast enema study. The procedure is generally called an aircontrast study. Carbon dioxide may also be used because it is more rapidly absorbed than the nitrogen in air when evacuation of the gaseous medium is incomplete. Use of air as a contrast medium for radiographic evaluation of the colon is not limited to the double-contrast enema procedure. Air or carbon dioxide insufflation of the colon is used to perform CTC or VC.
Water-soluble, iodinated contrast media enemas are performed when colon perforation or leak is suspected. These iodinated contrast agents are administered orally to selected patients when retrograde filling of the colon with barium is impossible or is contraindicated. A disadvantage of iodinated solutions is that evacuation often is insufficient for satisfactory double-contrast visualization of the mucosal pattern. When a patient is unable to cooperate for a successful enema study, orally administered iodinated medium allows satisfactory examination of the colon. With these oral agents, transit time from ingestion to colonic filling is fast, averaging 3 to 4 hours. Iodinated solutions are practically nonabsorbable from the gastrointestinal mucosa. As a result, the oral dose reaches and outlines the entire large bowel. In contrast to an ingested barium sulfate suspension, this medium is not subject to drying, flaking, and unequal distribution in the colon. It frequently delineates the intestine almost as well as the BE does.
Preparation of intestinal tract
Medical opinion about preparation measures varies. Members of the medical profession usually agree, however, that the large intestine must be completely emptied of its contents to render all portions of its inner wall visible for inspection. When coated with a barium sulfate suspension, retained fecal masses are likely to simulate the appearance of polypoid or other small tumor masses (Fig. 17-77); this makes thorough cleansing of the entire colon a matter of prime importance. Preliminary preparation of the intestinal tract of patients who have a condition such as severe diarrhea, gross bleeding, or symptoms of obstruction is limited. Other patients are prepared, with modification as indicated, according to the specifications established by the examining physician. The preliminary preparation usually includes dietary restrictions (“clear” liquids only) and a bowel cleansing regimen. The methods of bowel cleansing include the following:
Standard barium enema apparatus
Disposable soft plastic enema tips and enema bags are commercially available in different sizes. A soft rubber rectal catheter of small caliber should be used in patients who have inflamed hemorrhoids, fissures, a stricture, or other abnormalities of the anus.
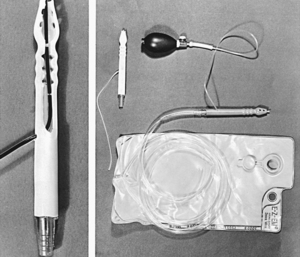
Disposable rectal retention tips (Fig. 17-78) have replaced the older retention catheters, such as the Bardex or Foley catheter. The retention tip is a doublelumen tube with a thin balloon at its distal end. Because of the danger of intestinal wall damage, the retention tip must be inserted with extreme care. The enema retention tip is used in a patient who has a relaxed anal sphincter or another condition that makes it difficult or impossible to retain an enema. Some radiologists routinely use retention enema tips and inflate them if necessary.
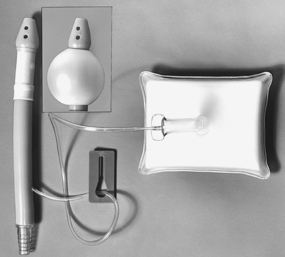
Fig. 17-78 Disposable retention enema tip. Uninflated balloon fits snugly. Inset: Balloon cuff inflated with 90 mL of air (one complete squeeze of inflator).
The disposable rectal retention tip has a balloon cuff that fits snugly against the enema nozzle before inflation and after deflation so that it can be inserted and removed with little discomfort to the patient. A reusable squeeze inflator is recommended to limit the air capacity to approximately 90 mL. One complete squeeze of the inflator provides adequate distention of the retention balloon without danger of overinflation. Disposable retention tips are available for double-contrast and single-contrast enemas. For the safety of the patient, any retention balloon must be inflated with caution, using fluoroscopy, just before the examination.
For the performance of a doublecontrast BE examination, a special rectal tip is necessary to instill air in the colon (Fig. 17-79). Alternatively, air can simply be pumped into the colon using a sphygmomanometer bulb. Double-contrast retention tips are also available.
Most enema bags have a capacity of 3 qt (3000 mL) when completely filled and have graduated quantity markings on the side. A filter may be incorporated within the bag to prevent the passage of any unmixed lumps of barium. The tubing is approximately 6 ft (1.8 m) long. Smaller enema bags (500 mL) with short, large-diameter tubing have been developed for double-contrast BE procedures.
Preparation of barium suspensions
The concentration of the barium sulfate suspensions used for single-contrast colonic enemas varies considerably. The often recommended range is 12% to 25% for weight/volume. For double-contrast examinations, a relatively high-density barium product is used. A 75% to 95% weight/volume ratio is common.
Commercial BE preparations are available as premixed liquids that can be poured into the disposable enema kit bag. Powdered barium is also available in single-contrast disposable kit bags. Water is added, and the solution is mixed by shaking the bag. Instructions for mixing a barium preparation vary according to the manufacturer and the type of barium used. The best recommendation is to follow the manufacturer’s instructions precisely.
If warm BEs are administered, the temperature should be below body temperature—about 85° F to 90° F (29° C to 30° C). In addition to being unpleasant and debilitating, an enema that is too warm is injurious to intestinal tissues and produces so much irritation that it is difficult, if not impossible, for the patient to retain the enema long enough for a satisfactory examination.
Preparation and care of patient
In no radiologic examination is the full cooperation of the patient more essential to success than in the retrograde examination of the colon. Few patients who are physically able to retain the enema fail to do so when they understand the procedure and realize that in large measure the success of the examination depends on them. The radiographer should observe the following guidelines in preparing a patient for retrograde examination of the colon:
• Take time to explain the procedural differences between an ordinary cleansing enema and a diagnostic enema: (1) With the diagnostic enema, the fluoroscopist examines all portions of the bowel as it is being filled with contrast medium under fluoroscopic observation; (2) this part of the examination involves palpation of the abdomen, rotation of the body as required to visualize the different segments of the colon, and the taking of spot radiographs without and, when indicated, with compression; (3) a series of large radiographs are taken before the colon can be evacuated.
• Assure the patient that retention of the diagnostic enema preparation is comparatively easy because its flow is controlled under fluoroscopic observation.
• Instruct the patient to (1) keep the anal sphincter tightly contracted against the tubing to hold it in position and prevent leakage, (2) relax the abdominal muscles to prevent intra-abdominal pressure, and (3) concentrate on deep oral breathing to reduce the incidence of colonic spasm and resultant cramps.
• Assure the patient that the flow of the enema would be stopped for the duration of any cramping.
A patient who has not had a previous colonic examination is usually fearful of being embarrassed by inadequate draping and failure to retain the enema for the required time. The radiographer can dispel or greatly relieve the patient’s anxiety by taking the following steps:
• Assure the patient that he or she will be properly covered.
• Assure the patient that although there is little chance of “mishap,” he or she will be well protected and there is no need to feel embarrassed should one occur.
• Keep a bedpan in the examining room for a patient who cannot or may not be able to make the trip to the toilet.
The preliminary preparation required for a retrograde study of the colon is strenuous for the patient. The examination itself further depletes the patient’s strength. Feeble patients, particularly elderly patients, are likely to become weak and faint from the exertion of the preparation, the examination, and the effort made to expel the enema. The strenuous nature of these procedures presents an increased risk for patients with a history of heart disease. An emergency call button should be available in the lavatory so that the patient can summon help if necessary. Although the patient’s privacy must be respected, the radiographer or an aide should frequently inquire to ensure that the patient is all right.
Insertion of enema tip
In preparation for insertion of the enema tip, the following steps are taken:
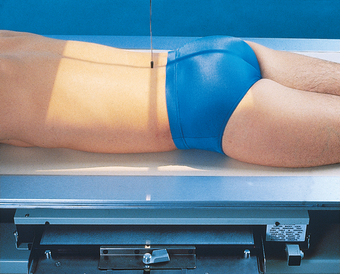
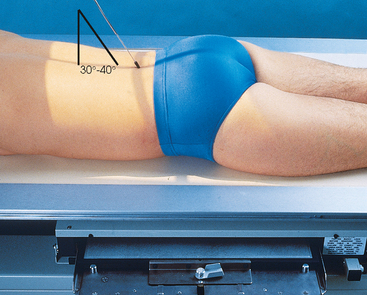
• Instruct the patient to turn onto the left side, roll forward about 35 to 40 degrees, and rest the flexed right knee on the table, above and in front of the slightly flexed left knee (Sims position). This position relaxes the abdominal muscles, which decreases intraabdominal pressure on the rectum and makes relaxation of the anal sphincter less difficult.
• Adjust the IV pole so that the enema contents are no higher than 24 inches (61 cm) above the level of the anus.
• Adjust the overlapping back of the gown or other draping to expose the anal region only, but keep the patient otherwise well covered. The anal orifice is commonly partially obscured by distended hemorrhoids or a fringe of undistended hemorrhoids. Sometimes there is a contraction or other abnormality of the orifice. It is necessary for the anus to be exposed and sufficiently well lighted for the orifice to be clearly visible so that the enema tip can be inserted without injury or discomfort.
• Run a little of the barium mixture into a waste basin to free the tubing of air, and then lubricate the rectal tube well with a water-soluble lubricant.
• Advise the patient to relax and take deep breaths so that no discomfort is felt when the tube is inserted.
• Elevate the right buttock laterally to open the gluteal fold.
• As the abdominal muscles and anal sphincter are relaxed during the expiration phase of a deep breath, insert the rectal tube gently and slowly into the anal orifice. Following the angle of the anal canal, direct the tube anteriorly 1 to 1½ inches (2.5 to 3.8 cm). Then following the curve of the rectum, direct the tube slightly superiorly.
• Insert the tube for a total distance of no more than 4 inches (10 cm). Insertion for a greater distance not only is unnecessary but also may injure the rectum.
• If the tube does not enter easily, ask the patient to assist if he or she is capable.
• Never forcibly insert a rectal tube because the patient may have distended internal hemorrhoids or another condition that makes forced insertion of the tube dangerous.
• After the enema tip is inserted, hold it in position to prevent it from slipping while the patient turns to the supine or prone position for fluoroscopy, according to the preference of the fluoroscopist. The retention cuff may be inflated at this time.
• Adjust the protective underpadding, and relieve any pressure on the tubing so that the enema mixture flows freely.
SINGLE-CONTRAST BARIUM ENEMA
Administration of contrast medium
After preparing the patient for the examination, the radiographer observes the following steps:
• Notify the radiologist as soon as everything is ready for the examination.
• If the patient has not been introduced to the radiologist, make the introduction at this time.
• At the radiologist’s request, release the control clip and ensure the enema flow.
• When occlusion of the enema tip occurs, displace soft fecal material by withdrawing the rectal tube about 1 inch (2.5 cm). Before reinserting the tip, temporarily elevate the enema bag to increase fluid pressure.
The rectal ampulla fills slowly. Unless the barium flow is stopped for a few seconds after the rectal ampulla is full, the suspension flows through the sigmoid and descending portions of the colon at a fairly rapid rate, frequently causing a severe cramp and acute stimulation of the defecation impulse. The flow of the barium suspension is usually stopped for several seconds at frequent intervals during fluoroscopically controlled filling of the colon.
During the fluoroscopic procedure, the radiologist rotates the patient to inspect all segments of the bowel. The radiologist takes spot radiographs as indicated and determines the positions to be used for subsequent radiographic studies. On completion of the fluoroscopic examination, the enema tip is usually removed so that the patient can be maneuvered more easily and so that the tip is not accidentally displaced during the imaging procedure. A retention tube is not removed until the patient is placed on a bedpan or the toilet.
After the IRs have been exposed (Fig. 17-80), the patient is escorted to a toilet or placed on a bedpan and instructed to expel as much of the barium suspension as possible. A postevacuation radiograph is then taken (Fig. 17-81). If this radiograph shows evacuation to be inadequate for satisfactory delineation of the mucosa, the patient may be given a hot beverage (tea or coffee) to stimulate further evacuation.
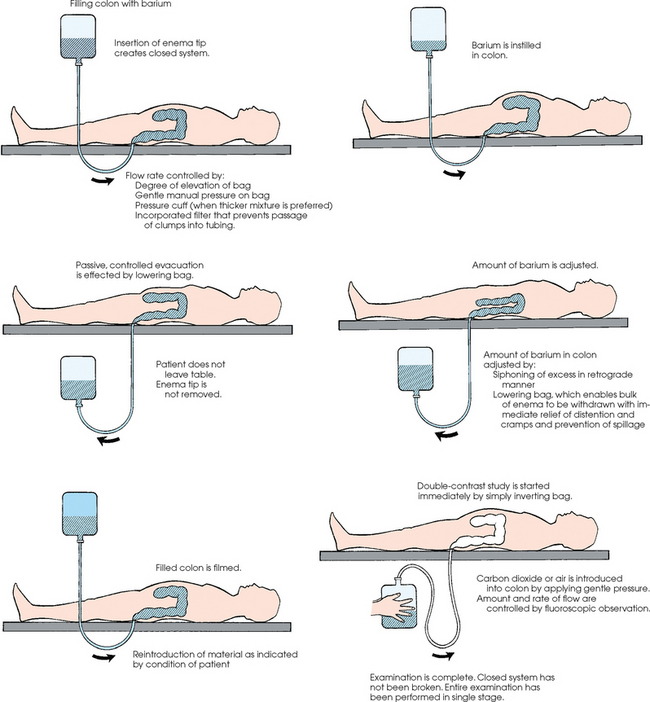
DOUBLE-CONTRAST BARIUM ENEMA
Two approaches to administering double-contrast BEs are currently in use. The first technique is a two-stage procedure, described by Welin,1 in which the entire colon is filled with a barium suspension. After administration of the enema, the patient evacuates the barium and immediately returns to the fluoroscopic table where air or another gaseous medium is injected into the colon. The second approach is the single-stage, doublecontrast examination. The popularity of this approach can be attributed primarily to more recent advancements in the manufacture of high-density barium sulfate.
Single-stage procedure
In performing the single-stage, double-contrast enema, certain requirements must be met to ensure an adequate examination. The most important requirement is that the patient’s colon be exceptionally clean. Residual fecal material can obscure small polyps or tumor masses. A second requirement is that a suitable barium suspension be used. A barium mixture that clumps or flakes neither clearly shows the lumen nor properly drains from the colon.
Currently available, premixed liquid barium products are generally more uniform for radiographic use than most barium suspensions mixed in the health care institution. A barium product with a density of 200% weight/volume may be used for a single-stage, double-contrast examination of the colon. The most important criterion is that the barium flows sufficiently to coat the walls of the colon.
With advances in the manufacture of high-density barium, high-quality double-contrast colon radiographs can be consistently obtained during one filling of the colon. In the single-stage procedure, the barium and air are instilled in a single procedure. Miller1 described a 7-pump method for performing single-stage, double-contrast examinations. This method reduces cost, saves time, and reduces radiation exposure to the patient. (A more complete description of the 7-pump method is provided in the seventh edition or earlier editions of this atlas.)
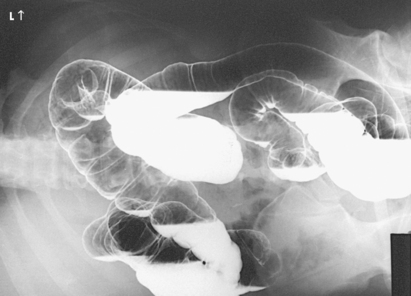
Fluoroscopy is performed to check the location of the barium, and additional air is instilled under fluoroscopic control. The patient is slowly rotated 360 degrees and placed in the supine position. Spot radiographs and overhead radiographs are then taken (Figs. 17-82 and 17-83).
In addition to the 7-pump method, a single-stage, double-contrast examination can be performed using a technique that does not employ a special air-contrast enema tip. With this technique, the barium and air are instilled through the closed enema bag system (Fig. 17-84).
Welin method
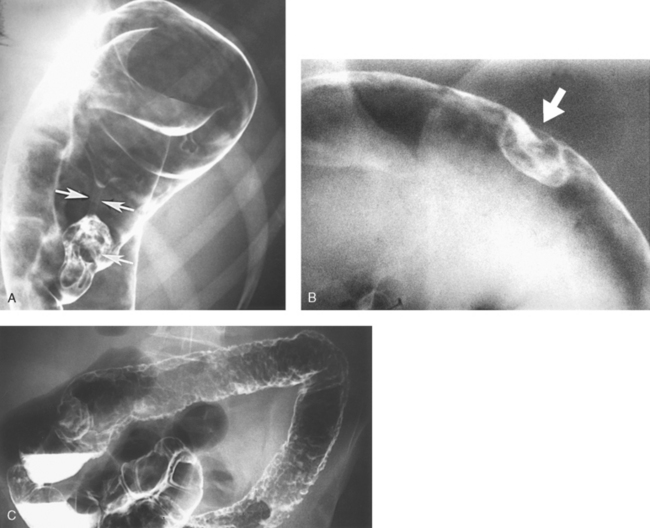
Welin1, 2 developed a technique for double-contrast enemas that reveals even the smallest intraluminal lesions (Figs. 17-85 and 17-86). He stated that this method of examination is extremely valuable in the early diagnosis of conditions such as ulcerative colitis, regional colitis, and polyps.
Welin stressed the importance of preparing the intestine for the examination, stating that (1) the colon must be cleansed as thoroughly as possible, and (2) the colonic mucosa must be prepared in such a way that an extremely thin, even coating of barium can adhere to the colonic wall. He recommended regulation of evacuation so that the two stages of the examination can be carried out at short intervals to avoid unnecessary waiting time, and the patient does not have to be in the examining room for more than 20 to 25 minutes.
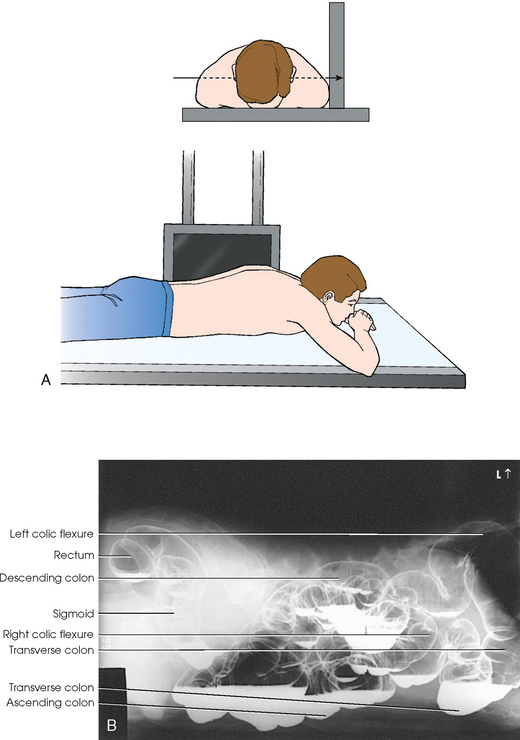
Stage 1: With the patient in the prone position to prevent possible ileal leak, the colon is filled to the left colic flexure, after which a conventional radiograph is taken (i.e., a right lateral projection of the barium-filled rectum). The patient is sent to the lavatory to evacuate the barium. Afterward, if the patient feels the need to do so, he or she is allowed to lie down and rest.
Stage 2: When the patient returns to the examining table, the enema tip is inserted, and the patient is again turned to the prone position. The prone position not only prevents ileal leakage with resultant opacification and overlap of the small intestine on the rectosigmoid area, but it also aids in adequate drainage of excess barium from the rectum.
The radiologist allows the barium mixture to run up to the middle of the sigmoid colon (slightly farther if the sigmoid is long). The patient is turned onto the right side, and air is instilled through the enema tip. The air forces the barium along, distributing it throughout the colon, and the patient is turned as required for even coating of the entire colon. Spot radiographs are made as indicated. If barium flows back into the rectum, it is drained out through the enema tip. More air is then instilled. Welin stressed the importance of instilling enough air (≥1800 to 2000 cc) to obtain proper distention of the colon.
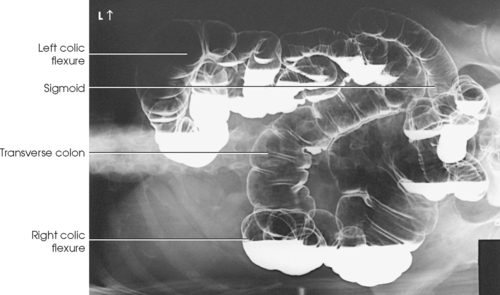
When sufficient distention of the colon has been obtained, 14- × 17-inch (35- × 43-cm) radiographs are obtained (Fig. 17-87) to include the rectum, using the following sequence: PA projection, PA oblique (LAO and RAO) projections, and right lateral projection 10 × 12 inches (24 × 30 cm). The patient is then turned to the supine position for an AP projection and two AP oblique (LPO and RPO) projections, all to include the transverse colon and its flexures. These studies are followed by AP projections in the right and left lateral decubitus positions to include the rectum. Finally, the patient is placed in the erect position for PA and PA oblique (RAO and LAO) projections of the horizontal colon and the left and right colic flexures.
OPACIFIED COLON
Radiographic studies of the adult colon are made on 14- × 17-inch (35- × 43-cm) IRs. Except for axial projections, these IRs may be centered at the level of the iliac crests on patients of sthenic build—higher for hypersthenic patients and lower for asthenic patients. AP and PA projections of the colon and abdomen may require two exposures, with the IRs placed crosswise: The first is centered high enough to include the diaphragm, and the second is centered low enough to include the rectum. Localized studies of the rectum and rectosigmoid junction are often exposed on 10- × 12-inch (24- × 30-cm) IRs centered at or slightly above the level of the pubic symphysis. Preevacuation radiographs of the colon include one or more images to show otherwise obscured flexed and curved areas of the large intestine.
Depending on the preference of the radiologist, the radiographic projections taken after fluoroscopy vary considerably. Any combination of the following images may be taken to complete the examination.
 PA PROJECTION
PA PROJECTION
• Center the midsagittal plane to the grid.
• Adjust the center of the IR at the level of the iliac crests (Fig. 17-88).
• In addition to positioning for the PA projection, place the fluoroscopic table in a slight Trendelenburg position if necessary. This table position helps separate redundant and overlapping loops of the bowel by “spilling” them out of the pelvis.
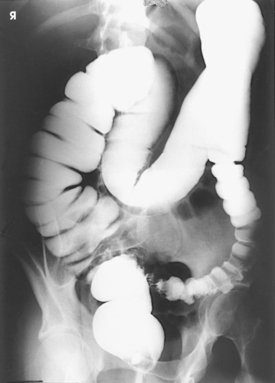
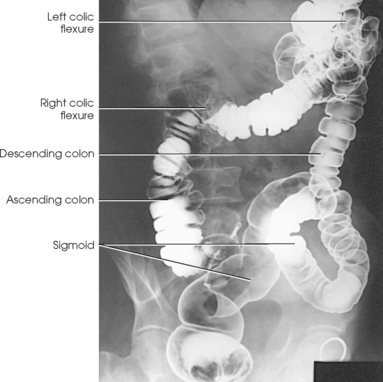
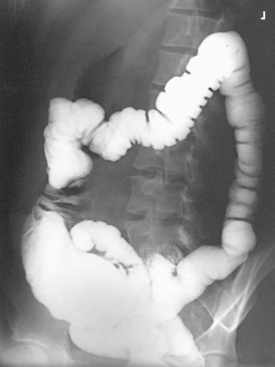
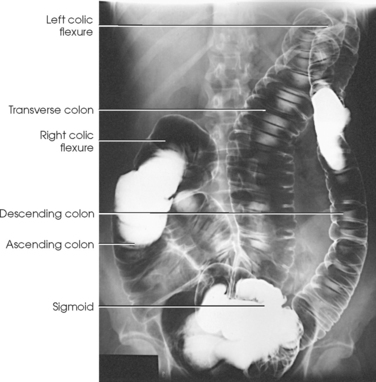
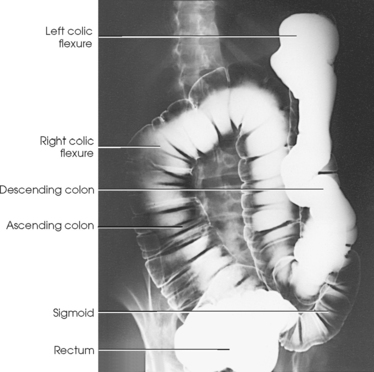
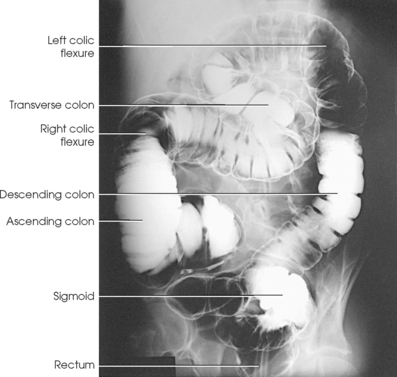
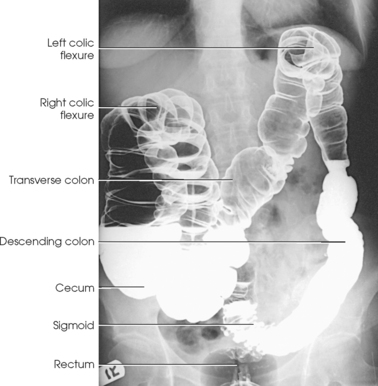
Structures shown: The PA projection shows the entire colon with the patient prone (Figs. 17-89 to 17-91).
 PA AXIAL PROJECTION
PA AXIAL PROJECTION
• Center the midsagittal plane to the grid.
• Adjust the center of the IR at the level of the iliac crests (Fig. 17-92).
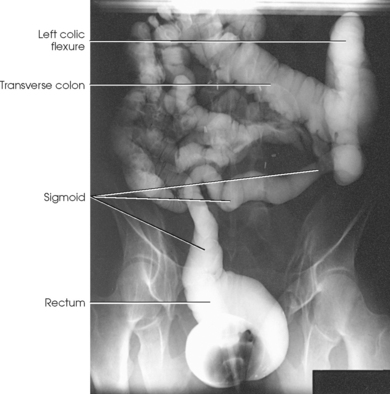
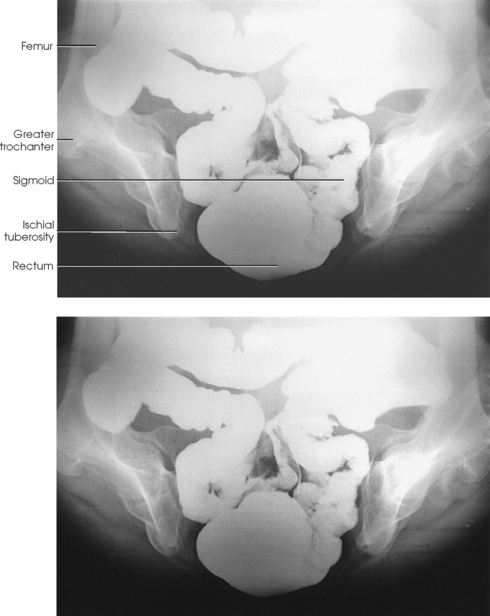
Structures shown: The PA axial projection best shows the rectosigmoid area of the colon (Figs. 17-93 and 17-94).
NOTE: This axial projection is sometimes performed with the patient in the RAO position, to further reduce superimposition in the rectosigmoid area.
 PA OBLIQUE PROJECTION
PA OBLIQUE PROJECTION
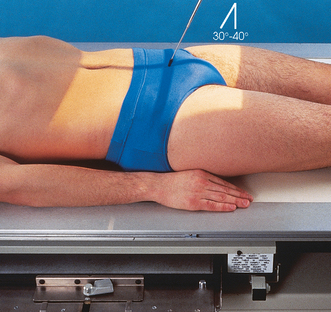
• With the patient’s right arm by the side of the body and the left hand by the head, have the patient roll onto the right hip to obtain a 35- to 45-degree rotation from the radiographic table.
• Flex the patient’s left knee to provide stability.
• Center the patient’s body to the midline of the grid.
• Adjust the center of the IR at the level of the iliac crests (Fig. 17-95).
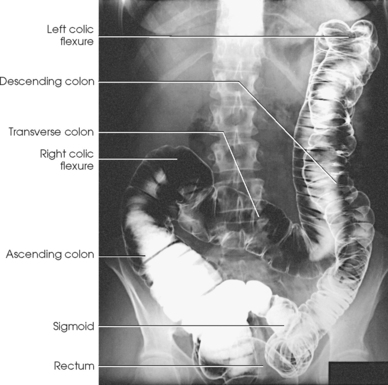
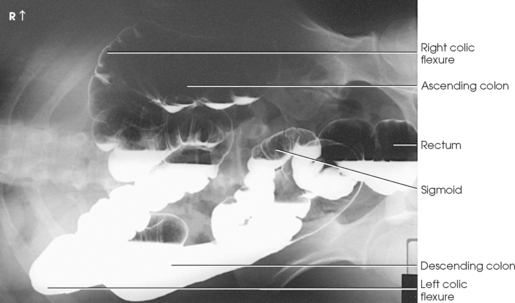
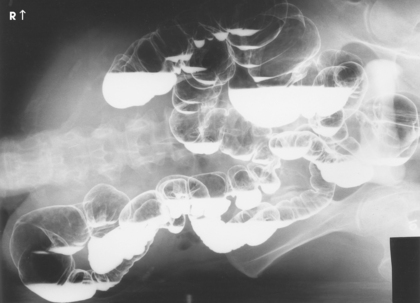
Structures shown: The RAO position best shows the right colic flexure, the ascending portion of the colon, and the sigmoid portion of the colon (Figs. 17-96 and 17-97).
 PA OBLIQUE PROJECTION
PA OBLIQUE PROJECTION
• With the patient’s left arm by the side of the body and the right hand by the head, have the patient roll onto the left hip to obtain a 35- to 45-degree rotation from the radiographic table.
• Flex the patient’s right knee to provide stability.
• Center the patient’s body to the midline of the grid.
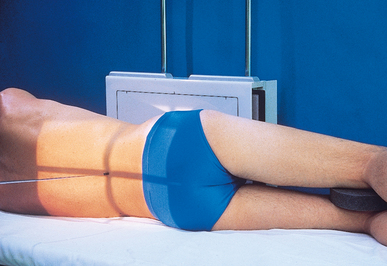
• Adjust the center of the IR at the level of the iliac crest (Fig. 17-98).
Structures shown: The LAO position best shows the left colic flexure and the descending portion of the colon (Figs. 17-99 and 17-100).
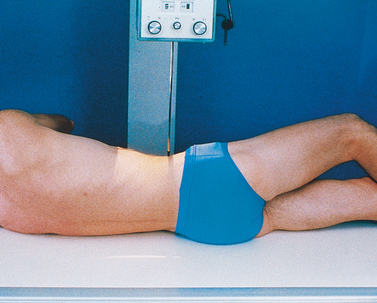
 LATERAL PROJECTION
LATERAL PROJECTION
• Center the midcoronal plane to the center of the grid.
• Flex the patient’s knees slightly for stability, and place a support between the knees to keep the pelvis lateral.
• Adjust the patient’s shoulders and hips to be perpendicular (Fig. 17-101).
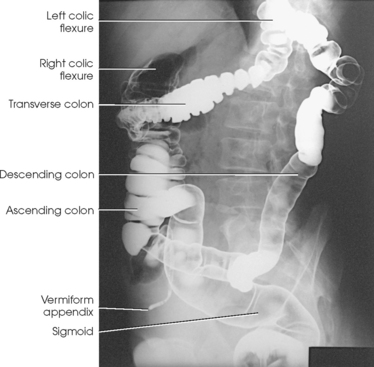
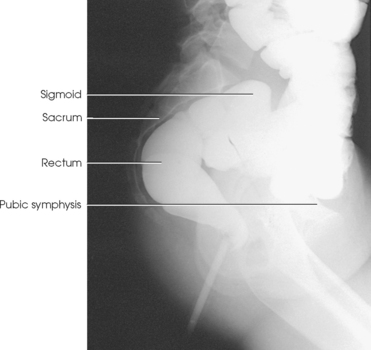
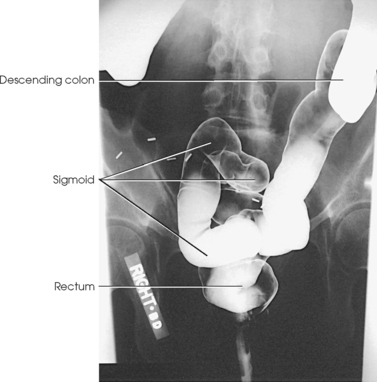
Structures shown: The lateral projection best shows the rectum and distal sigmoid portion of the colon (Figs. 17-102 and 17-103).
 AP PROJECTION
AP PROJECTION
• Center the midsagittal plane to the grid.
• Adjust the center of the IR at the level of the iliac crests (Fig. 17-104).
Structures shown: AP projection shows the entire colon with the patient supine (Figs. 17-105 and 17-106).
 AP AXIAL PROJECTION
AP AXIAL PROJECTION
• Center the midsagittal plane to the grid.
• Adjust the center of the IR at a level approximately 2 inches (5 cm) above the level of the iliac crests (Fig. 17-107).
Structures shown: The AP axial projection best shows the rectosigmoid area of the colon (Figs. 17-108 and 17-109). A similar image is obtained when the patient is prone (see Fig. 17-92).
NOTE: This axial projection is sometimes performed with the patient in the LPO position, to further reduce superimposition in the rectosigmoid area.
 AP OBLIQUE PROJECTION
AP OBLIQUE PROJECTION
• With the patient’s left arm by the side of the body and the right arm across the superior chest, have the patient roll onto the left hip to obtain a 35- to 45-degree rotation from the table.
• Use a positioning sponge and flex the patient’s right knee for stability, if necessary.
• Center the patient’s body to the midline of the grid.
• Adjust the center of the IR at the level of the iliac crests (Fig. 17-110).
Structures shown: The LPO position best shows the right colic flexure and the ascending and sigmoid portions of the colon (Figs. 17-111 and 17-112).
 AP OBLIQUE PROJECTION
AP OBLIQUE PROJECTION
• With the patient’s right arm by the side of the body and the left arm across the superior chest, have the patient roll onto the right hip to obtain a 35- to 45-degree rotation from the radiographic table.
• Use a positioning sponge and flex the patient’s right knee for stability, if needed.
• Center the patient’s body to the midline of the grid.
• Adjust the center of the IR at the level of the iliac crests (Fig. 17-113).
Structures shown: RPO position best shows the left colic flexure and the descending colon (Figs. 17-114 and 17-115).
Decubitus Positions
When a patient is being prepared for an examination in a decubitus position, the following general guidelines are observed:
• Take all decubitus radiographs (1) with the patient lying on the fluoroscopic table and a grid IR firmly supported behind the patient’s body, (2) with the patient lying on a patient cart with the body against an upright table or chest device, or (3) with the patient lying on a table or cart and a specially designed vertical grid device behind the patient.
• To ensure the side on which the patient is lying is shown, elevate the patient on a suitable radiolucent support. If this is not done, the radiograph records artifacts from the mattress or the table edge and superimposes these images over the portion of the patient’s colon on the “down” side.
• For all decubitus procedures, exercise extreme caution to ensure that the wheels of the cart are securely locked so that the patient will not fall.
• For lateral decubitus radiographs, have the patient put the back or abdomen against the vertical grid device. Most patients find it more comfortable to have their back against the vertical grid device than to have their abdomen against the same device.
• If both lateral decubitus radiographs are requested (which is often the case with air-contrast examinations), take one radiograph with the patient’s anterior body surface against the vertical grid device and the second radiograph with the posterior body surface against the vertical grid device.
 AP OR PA PROJECTION
AP OR PA PROJECTION
Right lateral decubitus position
• With the patient lying on an elevated radiolucent support, center the midsagittal plane to the grid.
• Adjust the center of the IR to the level of the iliac crests (Fig. 17-116).
Structures shown: The right lateral decubitus position shows an AP or PA projection of the contrast-filled colon. This position best shows the “up” medial side of the ascending colon and the lateral side of the descending colon when the colon is inflated with air (Figs. 17-117 and 17-118).
 COMPENSATING FILTER
COMPENSATING FILTER
Image quality can be improved on larger patients with the use of a special decubitus filter.
 PA OR AP PROJECTION
PA OR AP PROJECTION
Left lateral decubitus position
• With the patient lying on an elevated radiolucent support, center the midsagittal plane to the grid.
• Adjust the center of the IR at the level of the iliac crests (Fig. 17-119).
Structures shown: The left lateral decubitus position shows a PA or AP projection of the contrast-filled colon. This position best shows the “up” lateral side of the ascending colon and the medial side of the descending colon when the colon is inflated with air (Figs. 17-120 and 17-121).
LATERAL PROJECTION
R or L ventral decubitus position
Structures shown: The ventral decubitus position shows a lateral projection of the contrast-filled colon. This position best shows the “up” posterior portions of the colon and is most valuable in double-contrast examinations (Fig. 17-122).
 AP, PA, OBLIQUE, AND LATERAL PROJECTIONS
AP, PA, OBLIQUE, AND LATERAL PROJECTIONS
Upright AP, PA, oblique, and lateral projections may be taken as requested. The positioning and evaluation criteria for upright radiographs are identical to criteria required for the recumbent positions. The IR is placed at a lower level, however, to compensate for the drop of the bowel because of the effect of gravity (Figs. 17-123 to 17-125).
AXIAL PROJECTION
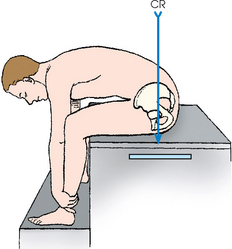
The Chassard-Lapiné method is used to show the rectum, rectosigmoid junction, and sigmoid. This projection, which is made at almost a right angle to the AP projection, shows the anterior and posterior surfaces of the lower portion of the bowel and permits the coils of the sigmoid to be projected free from overlapping.1, 2, 3 The projection may be exposed after evacuation of the large intestine, although a preevacuation radiograph can be exposed when the patient has reasonable sphincteric control.1
• Instruct the patient to sit well back on the side of the table so that the midcoronal plane of the body is as close as possible to the midline of the table.
• If necessary, shift the transversely placed IR forward in the Bucky tray so that its transverse axis coincides as nearly as possible with the midcoronal plane of the body.
• Instruct the patient to abduct the thighs as far as the edge of the table permits so that they do not interfere with flexion of the body.
• Center the IR to the midline of the pelvis, and ask the patient to lean directly forward as far as possible (Fig. 17-126).
The exposure required for this projection is approximately the same as that required for a lateral projection of the pelvis.
Structures shown: The Chassard-Lapiné image shows the rectum, rectosigmoid junction, and sigmoid in the axial projection (Fig. 17-127).
COLOSTOMY STUDIES
Enterostomy (Greek enteron, “intestine” + stoma, “opening”) is the general term applied to the surgical procedure of forming an artificial opening to the intestine, usually through the abdominal wall, for fecal passage. The regional terms are colostomy, cecostomy, ileostomy, and jejunostomy.
The colon is the most common site of disease in the large intestine, and surgical procedures are often performed on this structure. Loop colostomy is sometimes performed to divert the fecal column, either temporarily or permanently, from areas of diverticulitis or ulcerative colitis. Most colostomies are performed because of malignancies of the lower bowel and rectum. When a tumor is present, the lower carcinomatous part of the bowel is resected, and the end of the remaining part of the bowel is brought to the surface through the abdominal wall. This passage, or stoma, has no sphincter.
Preparation of intestinal tract
Postoperative contrast enema studies are performed at suitable intervals to determine the efficacy of treatment in a patient with diverticulitis or ulcerative colitis and to detect new or recurrent lesions in a patient who has had a tumor. Adequate cleansing of the bowel, which is as important in the presence of a colostomy as otherwise, is crucial to show polyps and other intraluminal lesions. In a patient with a colostomy, the usual preparation is irrigation of the stoma the night before the study and again on the morning of the examination.
Colostomy enema equipment
Although equipment must be scrupulously clean, and nondisposable items must be sterilized after each use, sterile technique is not required because the stoma is part of the intestinal tract. Except for a suitable device to prevent stomal leakage of the contrast material, the equipment used in a patient with a colostomy is the same as that used in routine contrast enema studies. The same barium sulfate formula is used, and gas studies are made. The opaque and double-contrast studies can be performed in a single-stage examination with the use of a disposable enema kit.
A device must be used to prevent spillage of contrast enema material in a patient with a colostomy. Otherwise, because of the absence of sphincter control, the contrast enema may escape through the colostomy almost as rapidly as it is injected. If this happens, bowel filling is unsatisfactory, and shadows cast by barium soilage of the abdominal wall and the examining table obscure areas of interest. Abdominal stomas must be effectively occluded for studies made by retrograde injection, and leakage around the stomal catheter must be prevented for studies made by injection into either an abdominal or a perineal colostomy. Numerous devices are available for this purpose.
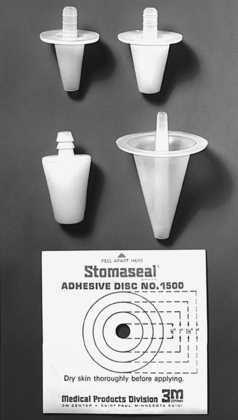
DIAGNOSTIC ENEMA
Diagnostic enemas may be given through a colostomy stoma with the use of tips and adhesive disks designed for the patient’s use in irrigating the colostomy (Fig. 17-128). The tips are available in four sizes to accommodate the usual sizes of colostomy stomas. These tips usually have a flange to prevent them from slipping through the colostomy opening. An adhesive disk is placed over the flange to minimize reflux soilage. The enema tubing is attached directly to the tip, which the patient holds in position to prevent the weight of the tubing from displacing the tip to an angled position. In addition to keeping a set of Laird tips on hand, it is recommended that the patient be asked to bring an irrigation device.
Retention catheters are also used in colostomy studies. Some radiologists use them alone, and others insert them through a device to prevent slipping and to collect leakage. Colostomy stomas are fragile and are subject to perforation by any undue pressure or trauma. Perforations have occurred during the insertion of an inflated bulb into a blind pouch and from overdistention of the stoma.
Preparation of patient
If the patient uses a special dressing, colostomy pouch, or stomal seal, he or she should be advised to bring a change for use after the examination. When fecal emission is such that a pouch is required, the patient should be given a suitable dressing to place over the stoma after the device has been removed.
The radiographer observes the following steps:
• Clothe the patient in a kimono type of gown that opens in front or back, depending on the location of the colostomy.
• Place the patient on the examining table in the supine position if he or she has an abdominal colostomy and in the prone position if he or she has a perineal colostomy.
• Before taking the preliminary radiograph and while wearing disposable gloves, remove and discard any dressing.
• Cleanse the skin around the stoma appropriately.
• Place a gauze dressing over the stoma to absorb any seepage until the physician is ready to start the examination.
• Lubricate the stomal catheter or tube well (but not excessively) with a water-soluble lubricant. The catheter should be inserted by the physician or the patient. If a catheter is forced through a stoma, the colon may be perforated.
Spot radiographs are taken during the examination. Postfluoroscopy radiographs are taken as needed. The projections requested depend on the location of the stoma and the anatomy to be shown (Figs. 17-129 to 17-132).
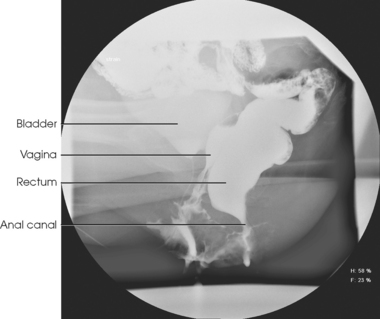
DEFECOGRAPHY
Defecography, evacuation proctography, or dynamic rectal examination is a relatively new radiologic procedure performed on patients with defecation dysfunction. No preparation of the patient is necessary, and cleansing enemas are not recommended because water remaining in the rectum dilutes the contrast medium.
Early investigators1 mixed a diluted suspension of barium sulfate, heated it, and added potato starch to form a smooth barium paste that was semisolid and malleable.2, 3 Barium manufacturers now package prepared barium products (100% weight/volume barium sulfate paste) with a special injector mechanism to instill the barium directly into the rectum. In addition, viscous barium may be introduced into the vagina and the bladder filled with aqueous iodinated contrast media.
After the contrast medium is instilled, the patient is usually seated in the lateral position on a commercially available radiolucent commode in front of a fluoroscopic unit. A special commode chair is recommended so that the anorectal junction and the zone of interest on the radiograph are not overexposed. Lateral projections are obtained during defecation by spot filming at the approximate rate of 1 to 2 frames per second. Video recording of the defecation process may be used, but the special equipment necessary to interpret the images is not always available, and a hard copy of the images is unavailable.1 The resulting images are then evaluated (Fig. 17-133). This evaluation includes measurements of the anorectal angle and the angle between the long axes of the anal canal and rectum. These measurements are compared with normal values. In addition, changes in proximity of the rectum to the vagina and bladder during defecation are assessed when these structures have been filled with contrast media (Fig. 17-134).
Biliary Tract and Gallbladder
Several techniques can be used to examine the gallbladder and the biliary ductal system. In many institutions, sonography is the modality of choice. This section of the atlas discusses the radiographic techniques currently available.
Table 17-1 lists some of the prefixes associated with the biliary system. Cholegraphy is the general term for a radiographic study of the biliary system. More specific terms can be used to describe the portion of the biliary system under investigation. Cholecystography is the radiographic investigation of the gallbladder, and cholangiography is the radiographic study of the biliary ducts.
TABLE 17-1
Biliary system combining forms
| Root forms | Meaning |
| Chole- | Relationship with bile |
| Cysto- | Bag or sac |
| Choledocho- | Common bile duct |
| Cholangio- | Bile ducts |
| Cholecyst- | Gallbladder |
Advances in sonography, CT, MRI, and nuclear medicine have reduced the radiographic examination of the biliary tract primarily to direct injection procedures including percutaneous transhepatic cholangiography (PTC), postoperative (T-tube) cholangiography, and endoscopic retrograde cholangiopancreatography (ERCP). The contrast agent selected for use in the direct-injection techniques may be any one of the water-soluble iodinated compounds employed for intravenous urography.
Percutaneous Transhepatic Cholangiography
PTC1 is another technique employed for preoperative radiologic examination of the biliary tract. This technique is used for patients with jaundice when the ductal system has been shown to be dilated by CT or sonography, but the cause of the obstruction is unclear. The performance of this examination has greatly increased because of the availability of the Chiba (“skinny”) needle. In addition, PTC is often used to place a drainage catheter for the treatment of obstructive jaundice. When a drainage catheter is used, diagnostic and drainage techniques are performed at the same time.
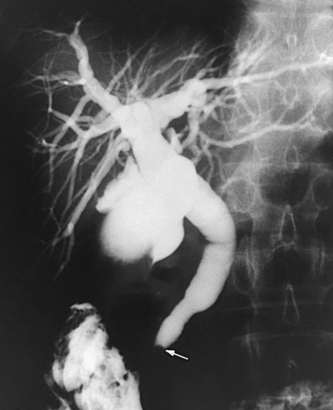
PTC is performed by placing the patient on the radiographic table in the supine position. The patient’s right side is surgically prepared and appropriately draped. After a local anesthetic is administered, the Chiba needle is held parallel to the floor and inserted through the right lateral intercostal space and advanced toward the liver hilum. The stylet of the needle is withdrawn, and a syringe filled with contrast medium is attached to the needle. Under fluoroscopic control, the needle is slowly withdrawn until the contrast medium is seen to fill the biliary ducts. In most instances, the biliary tree is readily located because the ducts are generally dilated. After the biliary ducts are filled, the needle is completely withdrawn, and serial or spot AP projections of the biliary area are taken (Figs. 17-135 to 17-137).
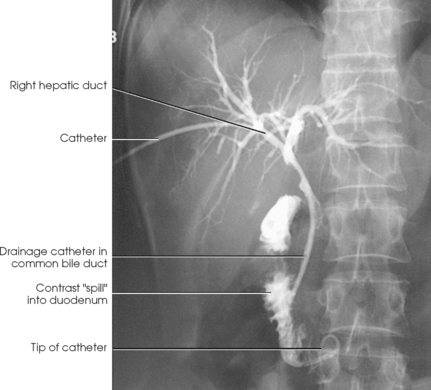
BILIARY DRAINAGE PROCEDURE AND STONE EXTRACTION
If dilated biliary ducts are identified by CT, PTC, or sonography, the radiologist, after consultation with the referring physician, may elect to place a drainage catheter in the biliary duct.1, 2 A needle larger than the Chiba needle used in the PTC procedure is inserted through the lateral abdominal wall and into the biliary duct. A guidewire is passed through the lumen of the needle, and the needle is removed. After the catheter is passed over the guidewire, the wire is removed, leaving the catheter in place.
The catheter can be left in place for prolonged drainage, or it can be used for attempts to extract retained stones if they are identified. Retained stones are extracted using a wire basket and a small balloon catheter under fluoroscopic control. This extraction procedure is usually attempted after the catheter has been in place for some time (Figs. 17-138 and 17-139).
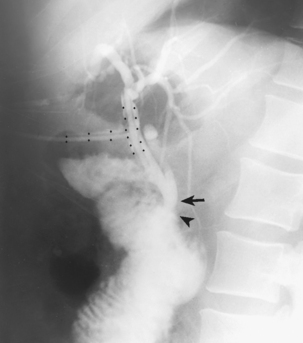
Postoperative (T-Tube) Cholangiography
Postoperative, delayed, and T-tube cholangiography are radiologic terms applied to the biliary tract examination that is performed via a T-shaped or pigtail-shaped catheter left in the common hepatic and common bile ducts for postoperative drainage (Fig. 17-140). A pigtail catheter is required for laparoscopic biliary procedures because it can be placed percutaneously. The T-tube catheter can be placed only during an open surgical procedure. This examination is performed to show the caliber and patency of the ducts, the status of the sphincter of the hepatopancreatic ampulla, and the presence of residual or previously undetected stones or other pathologic conditions.
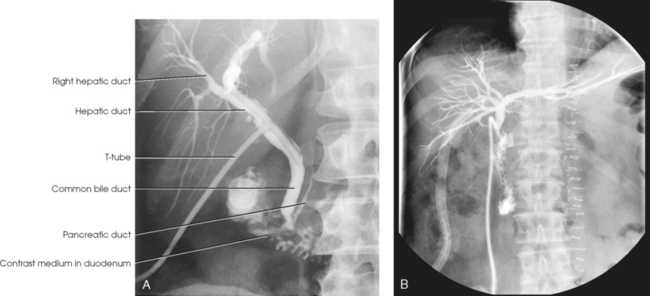
Fig. 17-140 A, Postoperative cholangiogram with T-tube catheter. B, Postoperative cholangiogram with pigtail catheter.
Postoperative cholangiography is performed in the radiology department. Preliminary preparation usually consists of the following:
1. The drainage tube is clamped the day before the examination to let the tube fill with bile as a preventive measure against air bubbles entering the ducts, where they would simulate cholesterol stones.
2. The preceding meal is withheld.
3. When indicated, a cleansing enema is administered about 1 hour before the examination. Premedication is not required.
The contrast agent used is one of the water-soluble iodinated contrast media. The density of the contrast medium used in postoperative cholangiograms is recommended to be no more than 25% to 30% because small stones may be obscured with a higher concentration.
After a preliminary radiograph of the abdomen has been obtained, the patient is adjusted in the RPO position (AP oblique projection) with the RUQ of the abdomen centered to the midline of the grid (Fig. 17-141).
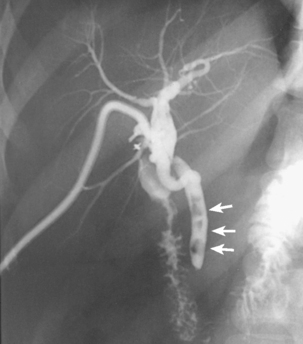
Fig. 17-141 AP oblique postoperative cholangiogram, RPO position, showing multiple stones in common bile duct (arrows).
With universal precautions employed, the contrast medium is injected under fluoroscopic control, and spot and conventional radiographs are made as indicated. Otherwise, 10- × 12-inch (24- × 30-cm) IRs are exposed serially after each of several fractional injections of the medium and then at specified intervals until most of the contrast solution has entered the duodenum.
Stern et al.1 stressed the importance of obtaining a lateral projection to show the anatomic branching of the hepatic ducts in this plane and to detect any abnormality not otherwise shown (Fig. 17-142). The clamp generally is not removed from the T-tube before the examination is completed. The patient may be turned onto the right side for this study.
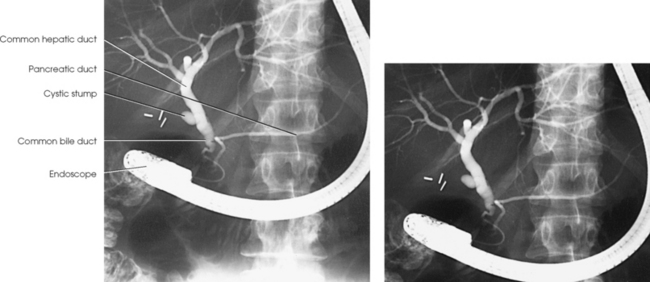
Endoscopic Retrograde Cholangio-pancreatography
ERCP is a procedure used to diagnose biliary and pancreatic pathologic conditions. ERCP is a useful diagnostic method when the biliary ducts are not dilated and when no obstruction exists at the ampulla.
ERCP is performed by passing a fiberoptic endoscope through the mouth into the duodenum under fluoroscopic control. To ease passage of the endoscope, the patient’s throat is sprayed with a local anesthetic. Because this causes temporary pharyngeal paresis, food and drink are usually prohibited for at least 1 hour after the examination. Food may be withheld for 10 hours after the procedure to minimize irritation to the stomach and small bowel.
After the endoscopist locates the hepatopancreatic ampulla (ampulla of Vater), a small cannula is passed through the endoscope and directed into the ampulla (Fig. 17-143). When the cannula is properly placed, the contrast medium is injected into the common bile duct. The patient may then be moved, fluoroscopy performed, and spot radiographs taken (Figs. 17-144 and 17-145). Oblique spot radiographs may be taken to prevent overlap of the common bile duct and the pancreatic duct. Because the injected contrast material should drain from normal ducts within approximately 5 minutes, radiographs must be exposed immediately.
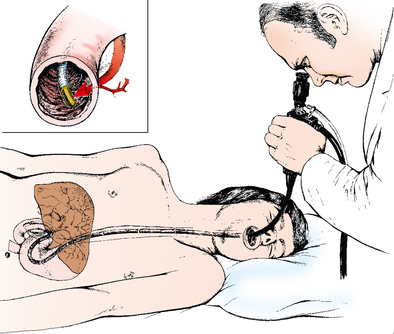
Fig. 17-143 Cannulation procedure. Procedure is begun with the patient in left lateral position. This schematic diagram gives an overview of location of the examiner and position of scope and its relationship to various internal organs. Inset: Magnified view of tip of scope with cannula in papilla. (From Stewart ET et al: Atlas of endoscopic retrograde cholangiopancreatography, St Louis, 1977, Mosby.)
The contrast medium that is used depends on the preference of the radiologist or gastroenterologist. Dense contrast agents opacify small ducts well, but they may obscure small stones. If small stones are suspected, use of a more dilute contrast medium is suggested.1 A history of patient sensitivity to an iodinated contrast medium in another examination (e.g., intravenous urography) does not contraindicate its use for ERCP. The patient must be watched carefully, however, for a reaction to the contrast medium during ERCP.
ERCP is often indicated when clinical and radiographic findings indicate abnormalities in the biliary system or pancreas. Sonography of the upper part of the abdomen before endoscopy is often recommended to assure the physician that no pancreatic pseudocysts are present. This step is important because contrast medium injected into pseudocysts may lead to inflammation or rupture.
Abdominal Fistulae and Sinuses
To show radiographically the origin and extent of fistulae (abnormal passages, usually between two internal organs) and sinuses (abnormal channels leading to abscesses), the following steps are taken:
• Fill the tract with a radiopaque contrast medium, usually under fluoroscopic control.
• Obtain right-angle projections. Oblique projections are occasionally required to show the full extent of a sinus tract.
• To explore fistulae and sinuses in the abdominal region, have the intestinal tract as free of gas and fecal material as possible.
• Unless the injection is made under fluoroscopic control, take a scout radiograph of the abdomen to check the condition of the intestinal tract before beginning the examination.
• When more than one sinus opening is present, occlude each accessory opening with sterile gauze packing to prevent reflux of the contrast substance and to identify every opening with a specific lead marker placed over the dressing (Figs. 17-146 to 17-148).
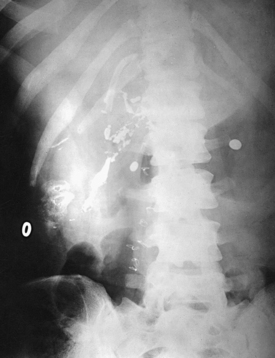
Fig. 17-146 AP abdomen showing contrast media–filled sinus tract with lead circular ring on body surface.
• Dress and identify the primary sinus opening in a similar manner if the catheter is removed after the injection.
• When a reflux of the contrast medium occurs, cleanse the skin thoroughly before making an exposure.
• When fluoroscopy is not employed, place the patient in position for the first projection before the injection to prevent drainage of the opaque substance by unnecessary movement. An initial radiograph is taken and evaluated before the examination is started or the patient’s position is changed.
To show a fistula involving the colon, barium is instilled by enema. If a fistula involving the small bowel is suspected, the patient ingests a thin barium suspension, which is followed by fluoroscopy or radiography until it reaches the suspected region. The bladder is filled with an iodinated contrast media when involvement of this structure is evaluated. Cutaneous fistulae and sinus tracts are opacified by introduction of an iodinated contrast medium through a small-diameter catheter. The procedures are performed using fluoroscopic observation, with images taken as indicated.
1Scukas J: Contrast media. In Margulis AR, Burhenne HJ, editors: Alimentary tract radiology, vol 1, ed 4, St Louis, 1989, Mosby.
1Cockerill EM et al: Optimal visualization of esophageal varices, AJR Am J Roentgenol 126:512, 1976.
1Skucas J: Contrast media. In Margulis AR, Burhenne HJ, editors: Alimentary tract radiology, vol 1, ed 4, St Louis, 1989, Mosby.
1Liotta D: Pour le diagnostic des tumeus du pancréas: la duodénographic hypotonique, Lyon Chir 50:445, 1955.
1Gugliantini P: Utilitá delle incidenze oblique caudocraniali nello studio radiologico della stenosi congenita ipertrofica del piloro, Ann Radiol [Diagn] 34:56, 1961. Abstract, AJR Am J Roentgenol 87:623, 1962.
1Gordon SS: The angled posteroanterior projection of the stomach: an attempt at better visualization of the high transverse stomach, Radiology 69:393, 1957.
1Wolf BS, Guglielmo J: Method for the roentgen demonstration of minimal hiatal herniation, J Mt Sinai Hosp NY 23:738, 741, 1956.
1Wolf BS, Guglielmo J: The roentgen demonstration of minimal hiatus hernia, Med Radiogr Photogr 33:90, 1957.
1Fitch D: The small-bowel see-through: an improved method of radiographic small bowel visualization, Can J Med Radiat Technol 26:167, 1995.
1Miller RE: Complete reflux small bowel examination, Radiology 84:457, 1965.
2Miller RE: Localization of the small bowel hemorrhage: complete reflux small bowel examination, Am J Dig Dis 17:1019, 1972.
1Welin S: Modern trends in diagnostic roentgenology of the colon, Br J Radiol 31:453, 1958.
1Miller RE: Barium pneumocolon: technologist-performed “7-pump” method, AJR Am J Roentgenol 139:1230, 1982.
1Welin S: Modern trends in diagnostic roentgenology of the colon, Br J Radiol 31:453, 1958.
2Welin S: Results of the Malmo technique of colon examination, JAMA 199:369, 1967.
1Raap G: A position of value in studying the pelvis and its contents, South Med J 44:95, 1951.
2Cimmino CV: Radiography of the sigmoid flexure with the Chassard-Lapiné projection, Med Radiogr Photogr 30:44, 1954.
3Ettinger A, Elkin M: Study of the sigmoid by special roentgenographic views, AJR Am J Roentgenol 72:199, 1954.
1Burhenne HJ: Intestinal evacuation study: a new roentgenologic technique, Radiol Clin (Basel) 33:79, 1964.
2Mahieu P et al: Defecography: I. Description of a new procedure and results in normal patients, Gastrointest Radiol 9:247, 1984.
3Mahieu P et al: Defecography: II. Contribution to the diagnosis of defecation disorders, Gastrointest Radiol 9:253, 1984.
1Mahieu PHG: Defecography. In Margulis AR, Burhenne H, editors: Alimentary tract radiology, vol 1, ed 4, St Louis, 1989, Mosby.
1Evans JA et al: Percutaneous transhepatic cholangiography, Radiology 78:362, 1962.
1Molnar W, Stockum AE: Relief of obstructive jaundice through percutaneous transhepatic catheter—a new therapeutic method, AJR Am J Roentgenol 122:356, 1974.
2Hardy CH et al: Percutaneous transhepatic biliary drainage, Radiol Technol 56:8, 1984.
1Stern WZ et al: The significance of the lateral view in T-tube cholangiography, AJR Am J Roentgenol 87:764, 1962.
1Cotton P, William C: Practical gastrointestinal endoscopy, Oxford, England, 1980, Blackwell.