Orthodontics II
Management of occlusal problems
Overview
The management of malocclusion comprises a substantial part of orthodontic practice. It ranges from interception of developing occlusal problems through to comprehensive correction of established malocclusion in the adolescent or adult. It also encompasses the special requirements in orthodontic care of those with cleft lip and/or palate.
This chapter describes the management of the developing dentition and of all major anomalies of established malocclusion, including surgical correction. The occlusal problems particular to cleft lip and/or palate together with their management are also outlined.
10.1 Problem solving in the developing dentition
Although most orthodontic treatment is undertaken when the permanent dentition is established, some aspects of the developing occlusion may be better dealt with in the mixed dentition. Such interception may eliminate the need for, or simplify, later treatment. Systematic and regular screening of the developing dentition is essential to this process.
Anomalies of eruption and exfoliation
Both eruption and exfoliation of primary and permanent teeth may be premature or delayed.
Natal teeth: Natal teeth are usually lower incisors that are erupted at birth or appear soon after. Removal is indicated only if they interfere with suckling or if they are so mobile as to be at risk of inhalation.
Eruption of teeth: Other than natal teeth, the following points should be borne in mind:
• There is greater variation in the eruption sequence of primary teeth between races than there is in eruption times.
• Poor diet and chronic ill-health in child populations may alter eruption sequence.
• Eruption times of permanent teeth tend to be later in Caucasians than in Mongoloids, who in turn tend to be later than Negroids.
• Females tend to erupt their permanent teeth earlier than males, particularly second and third molars.
Factors causing premature exfoliation or delay in the eruption and exfoliation of primary or permanent teeth are given in Table 10.1.
Table 10.1
Causes of premature or delayed eruption of primary or permanent teeth
| Causes | |
| Premature eruption | Familial tendency Primary dentition: high birthweight Permanent dentition: early-onset puberty, excess growth or thyroid hormone secretion |
| Delayed eruption | Primary dentition: very low birthweight, premature birth General causes: Down or Turner syndromes, severe nutritional deficiency, hypothyroidism/hypopituitarism, cleidocranial dysplasia, hereditary gingival hyperplasia, cleft lip and palate Local causes: ectopic crypt position, supernumerary or odontome, congenital absence, retention of primary tooth, dilaceration, primary failure of eruption, crowding |
| Premature exfoliation | Commonly caries or trauma Rarely hereditary hypophosphatasia, congenital neutropenia, cyclic neutropenia, Chediak–Higashi syndrome, histiocytosis X |
| Delayed exfoliation | Congenital absence of permanent successor Ectopic position of permanent successor Trauma Severe periradicular infection of primary tooth |
To ensure that any deviation in the normal eruption sequence is detected early, clinical vigilance is required during the developing dentition, supported by radiographic investigations where necessary. Particular attention should be given to the permanent maxillary incisors and canines, as early recognition of an anomaly in their eruption improves the prognosis.
Hypodontia
The most common missing teeth are:
Absent third molars: Extraction of a second molar, either to facilitate distal movement of the upper buccal segments or to relieve posterior crowding, should not be considered in the absence of a third molar. These start to calcify any time between 8 and 14 years.
Absent upper lateral incisors: Management options for the space created by absent upper lateral incisors are:
The final decision depends on:
• the patient’s attitude to orthodontic treatment
• the anteroposterior and vertical skeletal relationships
• amount of exposure of the upper canines and incisors on smiling
• the colour, size, shape and inclination of the canine and incisor teeth
The possible plans are best assessed by carrying out a trial set-up of each on duplicate study models, followed by joint consultation with a restorative colleague.
Space opening: In uncrowded or mildly crowded arches, when the buccal segment occlusion is class I or, at most, half unit class II, or in class III where proclination of the incisors is likely to correct an anterior crossbite, space opening is best. In addition, in patients with low Frankfort–mandibular plane angle (FMPA) or where the maxillary canine is considerably darker than the incisors, it may be best to open rather than close the anterior spaces. A fixed appliance may be needed to localise space for the missing units, followed by at least 3–6 months of removable appliance retention ensuring that the space is maintained by placing wire spurs in contact with the adjoining teeth. If it is possible to reposition the incisors and canines into their desired locations by tipping movements, a removable rather than a fixed appliance may be used. In selected cases, autotransplantation of lower premolars (extracted for relief of crowding) to the upper lateral incisor area may be possible. The prognosis is best when the root of the lower premolars is half to two-thirds formed; surgery must also be deftly planned and carried out to ensure optimal preparation of the donor site and prevent root surface damage. More commonly, the missing units may be replaced on resin-retained bridgework, and occasionally by implants at a later date. If bridgework is planned, it is important to ensure that sufficient interocclusal clearance exists for placement of the metal framework; if not, this should be created during appliance therapy.
Space closure: In crowded mouths, early extraction of the primary canines should be carried out to encourage mesial drift of the posterior teeth, but a later phase of fixed appliance therapy is usually needed to align and approximate the upper anterior teeth, followed by bonded retention. Recontouring of the canines in addition to composite build-up of their mesio-incisal aspects is advisable before treatment starts to assist with definitive tooth positioning; final restorations are placed following appliance removal. Bleaching of the canines may also be required to enhance aesthetics. Overjet reduction by space closure may be more favourable than resorting to midarch extractions and space opening. Space closure is likely to be facilitated in patients with increased FMPA, crowding and where the buccal segment relationship is a full unit class II.
Absent second premolars: The primary second molar should be retained where the arch is uncrowded or aligned. If the tooth starts to submerge, an occlusal onlay may be placed to maintain it in function. Removal of the lower second primary molar shortly after eruption of the lateral incisors will encourage spontaneous space closure in mildly crowded mouths, but in those with marked crowding, its extraction should be delayed until orthodontic treatment commences so that the resulting space may be used for arch alignment. In the upper arch, extraction of the second primary molar is again best deferred until orthodontic treatment is about to start. Rarely, a lower second premolar develops late and necessitates an alteration in the original treatment plan.
Absent lower central incisors: In the absence of permanent lower central incisors, root resorption and progressive incisal wear may lead to loss of the primary incisors in the late mixed dentition, although occasionally they can last for longer. A fixed appliance may be needed to close incisor spacing in a crowded mouth or to align the lateral incisors prior to placement of resin-retained bridgework in an uncrowded arch. Where one or both lower central incisors is missing and the space is closed orthodontically, mild crowding may result in the upper labial segment as six anterior teeth are arranged around four or five lower teeth.
Supernumerary teeth
Teeth additional to the normal number are termed ‘supernumerary’. Most commonly, they occur in the premaxilla (mesiodens) but they often also develop distal to the last tooth in each dental series (lateral incisor, second premolar and third molar) as an exuberant growth of the dental lamina, perhaps representing a tertiary dentition. They are more common:
• in the permanent than in the primary dentition (respective incidences 2% and 1%)
• in children with cleft of the lip and alveolus and cleidocranial dyostosis.
Those in the premaxilla can be categorised into three groups: conical, tuberculate and supplemental.
Conical teeth: Conical teeth occur between the upper permanent central incisors; they are often singular but can sometimes occur in combination with others of similar form. They may have no effect if they are well above the apices of the incisors. If there is no risk of damage to adjacent teeth with tooth movement, they can be left in place and observed. Often, however, they may displace the adjacent teeth, perhaps creating a large diastema, or they may delay eruption. In these instances, removal is indicated. Occasionally, a conical supernumerary tooth erupts and can be extracted.
Tuberculate teeth: Tuberculate teeth are the most common cause of an unerupted permanent maxillary central incisor. Suspicion should be raised if the lateral incisors erupt in advance of the centrals. In these cases, a radiograph of the premaxilla should be taken to allow early detection and localisation of any supernumerary, which should then be surgically removed. An attachment with gold chain or a magnet should be bonded to the unerupted incisor to allow provision for orthodontic alignment if the tooth fails to erupt spontaneously within 12 months of surgery. In conjunction with surgery, space to accommodate the unerupted tooth must be maintained or opened by appliance therapy; the latter may entail extraction of the upper primary canines.
Supplemental teeth: The supplemental tooth resembles the normal tooth in morphology and commonly produces crowding or displacement of adjacent teeth. Usually, the tooth, which is similar to the contralateral tooth, is better retained (provided it is not severely malpositioned) and the other incisor is extracted.
Anomalies of development
First permanent molars with poor long-term prognosis
The first permanent molar is never the extraction of choice for orthodontic reasons but is invariably enforced because of poor prognosis resulting from caries and/or enamel hypoplasia. Enamel decalcification on the lingual aspect of lower first permanent molars or on the buccal aspect of upper first permanent molars should be treated seriously, as it is often a hallmark of a high caries rate and possible limited lifespan of these teeth. When a two-surface or deep occlusal restoration is indicated in one molar 2–3 years after eruption, careful assessment of the malocclusion and the condition of the other first permanent molars should be made. Timely removal may lead to considerable spontaneous correction of the malocclusion in certain patients but it does little for relief of incisor crowding or correction of an incisor relationship unless appliance therapy is instituted.
A ‘cook book’ approach to each patient with poor-quality first permanent molars is not possible but some guidelines are listed in Box 10.1.
Infraoccluded primary molars
Between 1–9% of children are likely to exhibit this anomaly but estimates regarding its incidence vary. A genetic tendency has been suggested with absent premolars, ectopic position of the first permanent molars and palatal canine displacement identified as associated factors. Infraocclusion results from ankylosis of the tooth while alveolar growth and eruption of the adjacent teeth continues. Provided the permanent successor is present, exfoliation will occur eventually, but removal is indicated in its absence and where the infraocclusion is marked, with the crown of the tooth just visible, or where root development of the unerupted premolar is almost complete.
Impaction of the maxillary first permanent molar
Impaction of the maxillary first permanent molar occurs in 2–6% of children. It may correct spontaneously (unlikely after the upper lateral incisors erupt) or it may require disimpaction of the molar either by placing a brass wire separator between the adjacent teeth (in mild problems) or by appliance therapy (in more marked impaction). Extraction of the second primary molar is required if the impaction produces symptomatic resorption with pulpal involvement or to facilitate restoration of the first permanent molar. Crowding is exacerbated by the subsequent mesial drift of the first permanent molar, but this can be treated later.
Aberrant position of second premolars
Occasionally, the second premolars appear in slightly unfavourable positions when viewed on a radiograph, but generally this is of no long-term consequence and their final position is usually satisfactory. A grossly ectopic second premolar is rare and may be observed or surgically removed.
Posterior crossbite with mandibular displacement
Sometimes, a unilateral crossbite of the buccal segment teeth with mandibular displacement follows a prolonged finger- or thumb-sucking habit. In some children, grinding the primary canines can lead to correction and prevent perpetuation of the crossbite from the mixed to the permanent dentition; where this is not effective, arch expansion by using either a removable appliance and a midline screw or a quadhelix is required to reduce the chance of the crossbite being present in the permanent dentition. Alternatively, correction may be deferred until the premolars erupt (Fig. 10.1).
Treatment of anomalies by serial extractions
In 1948, Kjellgren, a Swedish orthodontist, ascribed the term ‘serial extractions’ to the following three-stage procedure:
• Extraction of the primary canines at age 8.5–9.5 years to encourage alignment of the permanent incisors.
• Extraction of the first primary molars approximately 1 year later to encourage eruption of the first premolars.
• Extraction of the first premolars as the permanent canines are erupting.
This approach works best in children with class I malocclusion at about 9 years, with moderate crowding, average overbite and a full complement of teeth and where there is no doubt about the long-term prognosis of the first permanent molars. It was originally intended to remove the need for appliance therapy but, in practice, this is seldom the case. In addition, extractions under general anaesthesia is an unpleasant and often frightening introduction to dentistry for any child, which may psychologically scar their attitude to subsequent dental treatment. As a result, the full extent of the original technique is never adopted in contemporary orthodontic practice, but consideration is often given to the need to extract the primary canines in the following instances:
• To allow labial movement of a permanent upper lateral incisor erupting palatal to the permanent upper central incisors and in potential crossbite.
• To create space in the upper labial segment for proclination of an instanding permanent lateral incisor or the eruption of a permanent incisor, where a supernumerary tooth has delayed its appearance.
• To promote alignment of a displaced permanent maxillary canine; this is particularly beneficial where the canine is displaced palatally.
• To facilitate lingual movement of a labially placed permanent lower incisor with reduced periodontal support or of the lower labial segment to aid anterior crossbite correction in class III malocclusion.
Other developmental problems
Early loss of primary teeth is most commonly caused by caries but, occasionally, it results from premature exfoliation, often when there is severe crowding, or it may be planned (e.g. to encourage space closure by mesial drift of the buccal segments in children who are missing one or more permanent teeth). In all cases, consideration should be given to balancing (extraction of the same tooth on the opposite side of the arch) or to compensating (extraction of the equivalent opposing tooth) for an extraction. Premature loss of a primary tooth does not inevitably lead to premature eruption of the permanent successor.
The effects of early loss of a primary tooth depend on several factors including:
All of these influence the potential for crowding to be concentrated at the extraction site. In general, this potential is greatest in a young child with pre-existing crowding when a maxillary posterior tooth is removed with poor buccal segment intercuspation.
Incisors: Early loss of a primary incisor tends to have minimal effect as it usually exfoliates in the early mixed dentition. Premature loss of a primary incisor through trauma may, however, lead to dilaceration of the permanent successor.
Canines: Unilateral loss of a primary canine invariably leads to movement of the centreline and should be balanced to prevent this occurring.
First molars: Occasionally, displacement of the centreline follows early extraction of a first primary molar, but the need for a balancing extraction is best assessed by checking the midlines at subsequent reviews.
Second primary molars: Where the second primary molar is extracted, the first permanent molar migrates mesially and may lead to considerable space loss if the extraction is carried out before the permanent molar erupts; hence, it is preferable to delay extraction until the first permanent molar has erupted. The need for a lower compensating extraction should be considered carefully if removal of an upper second primary molar of poor prognosis would allow the first permanent molar to move forward to become a full unit class II from a half class II relationship.
Space maintenance for early tooth loss: Space maintenance is indicated:
• when premature loss of a tooth promotes crowding in an otherwise acceptable occlusion
• in severely crowded mouths where all of the extraction space is required for alignment of the remaining teeth
A removable appliance will usually suffice in the upper arch but a lingual arch soldered to bands cemented to molar teeth is best in the lower.
Upper median diastema
Upper median diastema is a normal phase of dental development and usually reduces as the permanent maxillary canines erupt. It may, however, also result from:
• a midline supernumerary tooth
• missing or small upper lateral incisors
• incisor proclination in class II division 1 malocclusion (Section 10.3) or due to a digit-sucking habit
• a more generalised spacing condition due to mismatch in tooth/arch size (Section 10.2).
A radiograph of the upper incisor area should be taken to exclude the presence of a supernumerary tooth in those with a large midline diastema. Rarely, a low-lying attachment of the labial frenum is a primary cause, as the attachment usually recedes as the incisors approximate. In a spaced arch, this does not occur, indicating that the frenum is associated with, but not causative of, the diastema.
Where the frenum is implicated in causing a diastema, blanching of the incisive papilla usually occurs when the lip is pulled upwards or outwards, with characteristic V-shaped notching of the alveolar bone between the two central incisors visible radiographically. The need for fraenectomy should be assessed after eruption of the permanent canines and is preferably undertaken during space closure as the scar tissue will aid approximation of the incisors. Treatment of the diastema in the early mixed dentition may be necessary if there is insufficient space for the lateral incisors and the diastema exceeds 3 mm but vigilance is needed to ensure that the lateral incisor roots are not moved into the path of the erupting canines. A fixed appliance is usually required to close an upper midline space, with bodily approximation of the incisors followed by palatal bonded retention.
Dilaceration
Dilaceration is a sudden angular alteration in the long axis of the crown or in the root of a tooth. Most commonly it results from intrusion of a primary incisor driving the crown of the permanent successor palatally, and it leads to enamel and dentine hypoplasia. On occasion, dilaceration is developmental in origin, with a characteristic labial and superior coronal deflection of the affected tooth. Usually, a dilacerated incisor remains unerupted and requires surgical removal but, if the dilaceration is mild, surgical exposure and orthodontic alignment may be feasible when the root apex is destined not to perforate the cortical plate.
Traumatic loss of an upper permanent central incisor
As the adjacent teeth tend to tilt toward the site of loss in the first days following trauma, the space must be maintained, ideally by immediate reimplantation of the tooth or by fitting a denture carrying a replacement tooth. Later, autotransplantation of a premolar or adhesive bridgework may be considered. This is generally preferable to space closure, as a lateral incisor rarely gives an optimum appearance in a central incisor position, even with coronal build-up and gingival recontouring.
Incisors in crossbite
Early correction of a crossbite involving a permanent incisor is essential to prevent displacing occlusal forces compromising the periodontal support of the lower anterior teeth and to allow the occlusion to develop around an undisplaced condylar position. Provided there is likely to be adequate overbite of 2–3 mm, an upper removable appliance with a double-cantilever spring to procline the instanding incisor and posterior capping to disengage the occlusion will usually suffice (see Section 10.5 and Fig. 10.2). It may be necessary to remove the upper primary canines to facilitate crossbite correction on a permanent upper lateral incisor or the lower primary canines to allow alignment of a labially placed permanent lower incisor.
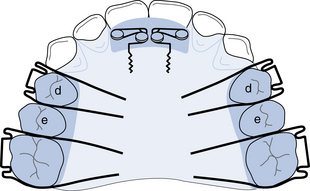
Fig. 10.2 Upper removable appliance to procline 1|1 in the early mixed dentition, assuming all primary teeth are in good condition.
Double cantilever springs 1|1 (0.5 mm SS wire); Adams’ clasps d|d (0.6 mm SS wire) and 6|6 (0.7 mm SS wire); posterior capping 2–3 mm in height to disengage the anterior occlusion.
Habits
Depending on the positioning of a finger(s) or thumb, the frequency and intensity of a sucking habit may:
Gentle persuasion to discontinue the habit should be given and simple measures adopted to effect this. An upper removable ‘reminder’ appliance may be fitted if the child is eager to stop.
Increased overjet
Where the overjet is greater than 3 mm, the risk of incisor trauma is more than doubled; trauma is more common in boys and the risk is greater with incompetent lips. An initial phase of functional appliance therapy to retract the incisors may be beneficial in these children but seldom produces complete correction of the malocclusion. Often, it is necessary to proceed to a second phase of treatment when the permanent dentition is fully erupted. This usually involves fixed appliances to detail the occlusion in combination with premolar extractions for relief of crowding. An early start to overjet correction can lead to protracted treatment, as the functional appliance will need to be worn as a retainer at least until a possible second phase of treatment commences and most likely until growth is complete. As this places considerable demands on patient co-operation, the likely benefits of early treatment must be deemed to outweigh any potential disadvantages before commencing on this course. There is also a potential risk of upper incisor root resorption if these teeth are retracted into the upper canine eruption path.
In recent years, the results of a randomised controlled clinical trial in North America have indicated that early skeletal effects produced by either functional or headgear therapy in the preadolescent period were not maintained long term. In addition, little or no differences existed following fixed appliance therapy in the permanent dentition between those who had been treated earlier or who had been observed until the permanent dentition erupted. A multicentre randomised controlled trial in the UK found that children treated at 8–10 years of age by a functional appliance had higher self-concept scores when evaluated 15 months later compared to those allocated to the control group. Many clinicians now prefer to wait until the permanent dentition is established before considering possible extractions for overjet correction and relief of crowding. A mixed dentition functional appliance phase, however, is beneficial to psychosocial wellbeing where the child is being teased because of the dentofacial anomaly; interestingly, a reduction in the risk of incisor trauma may not follow based on the findings of recent randomised clinical trials. The need for a custom-made mouthguard for sports, therefore, should be emphasised to those where treatment is deferred until the permanent dentition and in others following functional treatment.
Ectopic maxillary canines
The maxillary canine is ectopic in approximately 2% of the population, with 15% of these buccal and 85% palatal to the arch. Development of the maxillary canine begins about 4–5 months after birth and the crown is complete around 6–7 years of age. From an initial position high in the maxilla, the tooth moves buccally downwards and forwards to be guided into its final position by the distal aspect of the lateral incisor root. For this reason, absence or diminution in the size of the lateral incisor increases the incidence of displacement (×2.4). There also appears to be a greater incidence of palatal canine displacement where the maxillary arch is spaced or in class II division 2 malocclusion; a genetic link has been suggested and palatal displacement has a familial tendency, is more common in females than males, occurs bilaterally more than seems likely and is associated with absent or small teeth. Buccal displacement is more common in crowded arches. Where routine palpation of the buccal sulcus at 10 years fails to detect a canine prominence, the path of eruption is likely to be abnormal. In addition, considerable delay in the eruption of a canine compared with the opposite side of the arch points to canine displacement.
Transposition: Transposition is when the position of the canine is interchanged with that of an adjacent tooth. In the upper arch, the maxillary canine and first premolar, or the lateral incisor and canine, are involved, although the former arrangement is more common. In the lower arch, this anomaly affects solely the lateral incisor and canine teeth.
Estimating the maxillary canine position:
Clinical estimate: Buccal and palatal palpation along with observation of the lateral incisor inclination give a hint to the canine position. When it is lying low and palatal or high and buccal, the lateral incisor is likely to be labially inclined.
Radiographic estimation: Although a dental panoramic tomogram is helpful in initial assessment of canine position, further radiographic views are needed to locate the position of the tooth. Most commonly an upper anterior occlusal view or two periapical films taken with a tube shift are needed to allow localisation, using vertical or horizontal parallax respectively. The axial inclination, apex location and the vertical and mesiodistal position of the canine relative to the incisor roots should be assessed. The permanent incisors should be checked carefully to exclude resorption, and the root length of the primary canine noted. Resorption of incisors is more common in females than males and there is a 50% greater risk of its occurrence should the canine be at a greater than 25° angulation to the midline when viewed on a dental panoramic tomogram. If incisor resorption is detected, urgent treatment is indicated. Removal of the impacted canine may arrest the resorption but extraction of the incisor may be required in those with severe resorption. Cone beam computed tomography (CBCT) can reveal the full extent of resorption.
Management of canine displacement: The management of buccal or palatal maxillary canine displacement including transposition is described in Table 10.2.
Table 10.2
Management of maxillary canine displacementa
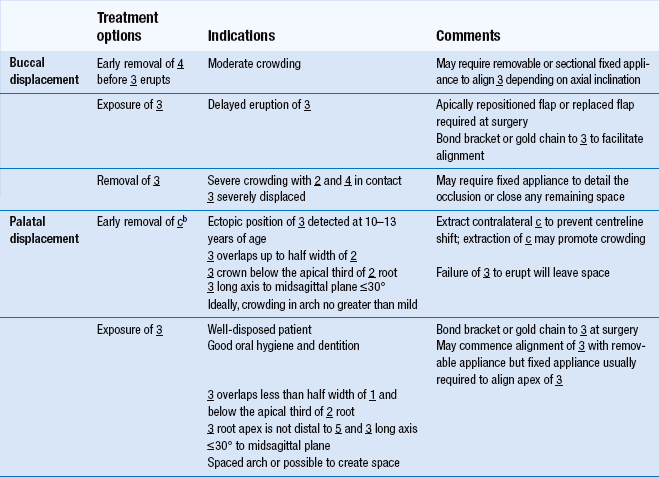
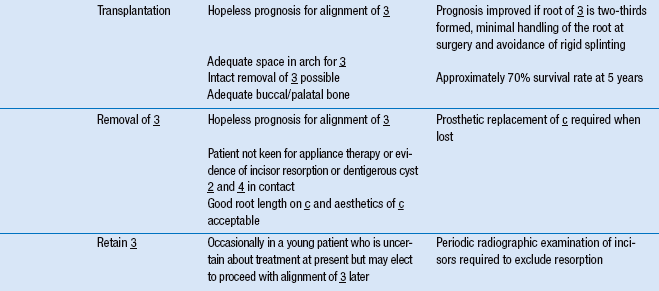
aIn each case, the patient’s interest in orthodontic treatment, their level of dental awareness and general features of the malocclusion (including the degree of crowding or spacing and the condition of the primary canine (if present) and adjacent teeth) must be assessed before the final treatment plan can be devised
b91% chance of normalisation of eruption path of 3 with extraction of c where 3 is mesially positioned and overlaps < half of root of 2; 64% chance of normal eruption of 3 if > half of 2 root overlapped. Recent evidence shows significant improvement in success rate of eruption of 3 with the use of RME and headgear (or headgear only) compared to untreated controls.
Anomalies of size and form
Teeth of a size that is greater or less than the norms for gender and for a given population are described as ‘megadont’ or ‘microdont’ respectively.
Megadontia has a prevalence of 1.1% in the permanent dentition, with maxillary central incisors most frequently affected, although lower second premolars are affected occasionally. The normal shape and absence of incisor notching distinguishes megadont maxillary incisors from ‘double teeth’. Megadont teeth may be found unilaterally on the affected side in unilateral facial hyperplasia, but more generalised megadontia is associated with gigantism. A megadont upper incisor may produce crowding, an increased overjet or both. If the tooth is only slightly enlarged, removal of about 1 mm of enamel from each proximal surface and appliance therapy to close the resultant space may suffice. In gross enlargement, extraction of the affected tooth and placement of a pontic following any appliance treatment may be necessary.
Microdontia is frequently seen in association with hypodontia, in Down syndrome and in ectodermal dysplasia. The prevalence is 0.2–0.5% in the primary dentition and 2.5% in the permanent dentition, with diminutive upper lateral incisors accounting for 1–2% of the latter. Short roots are often found on these teeth, which may be a factor in the aetiology of palatally displaced canines. In crowded mouths, where the lateral incisor is peg-shaped on one side of the arch and of normal size on the opposite side, removal of both lateral incisors may be optimal to achieve symmetry in the upper labial segment. If the diminutive lateral incisor is retained, orthodontic treatment should first create sufficient space to ensure that the tooth can be restored to normal dimensions. This space is maintained for at least 3 months with metal spurs on a removable retainer prior to final restoration.
Form
• Have a prevalence of 0.1–0.2% in the permanent dentition.
Clinical appearance can vary from an incisal notch in a tooth of enlarged mesiodistal width to an anomaly resembling two separate crowns. Treatment is best delayed until the pulp has receded. Separation may be possible if there are two separate pulp chambers and root canals, but recontouring of the crown to resemble two separate teeth or reduction of its mesiodistal width may be possible where one pulp chamber exists.
Prevalence in the primary dentition is 0.5–1.6% in Caucasians and it affects teeth mostly in the mandibular labial segment. In the presence of hypodontia, double primary teeth are followed usually by absence of permanent teeth, but supernumerary teeth are more common in the permanent dentition if all of the primary teeth are present. Occasionally, eruption of the permanent successor is delayed if a double primary tooth exists, and its removal, possibly in conjunction with that of permanent supernumeraries, may be indicated to allow eruption of the permanent teeth.
Accessory cusps and evaginated teeth
In the primary dentition, the maxillary molars are most commonly affected by additional cusps whereas the incisors, particularly the upper incisors, premolars and molars may be affected in the permanent dentition. An additional cusp on a maxillary incisor is termed a ‘talon’ cusp. As well as being unsightly, it may produce an occlusal interference or predispose to caries between the cusp and the palatal surface of the incisor. Treatment may be either by removal of the cusp and localised pulpotomy or by progressive grinding to encourage secondary dentine formation.
Evagination is characterised by a conical tuberculated prominence on the occlusal surface of a tooth and affects premolars most commonly. Treatment is as recommended for talon cusps.
10.2 Class I malocclusion
Aetiology
Skeletal factors: The skeletal pattern may be class I, class II or class III with the incisors compensating for any underlying skeletal discrepancy. An increase in lower anterior face height or a mild transverse skeletal discrepancy may also occur, creating an anterior open bite or buccal segment crossbite, respectively.
Soft tissues factors: Apart from bimaxillary proclination, where labial movement of the incisors may result from tongue pressure in the presence of unfavourable lip tone, the soft tissues are not prime aetiological factors.
Dental factors: A tooth/dental arch size discrepancy leading to crowding or spacing is the principal cause of class I malocclusion. Other factors, however, such as early loss of primary teeth, large or small teeth, supernumerary or absent teeth, can also influence any inherent dento-alveolar disproportion.
There are several typical occlusal features:
• ‘The lower incisor edges occlude with, or lie immediately below, the cingulum plateau of the upper central incisors’ (British Standards Institute classification). Not all of the incisors, however, may relate in this manner. Provided the overall anteroposterior labial segment relationship is normal, even where a crossbite exists on one or two upper incisors, the incisor relationship may be regarded as class I.
• The molar relationship is variable and depends on whether mesial drift has followed any previous extractions.
• Crowding is often concentrated in the upper canine and lower second premolar areas as these teeth often erupt last in each arch.
• Crowding may also displace one or more teeth into crossbite and create a premature contact on closure, with associated mandibular displacement and centreline shift.
Treatment
The need for treatment on dental health grounds is most commonly related to the presence of crowding or displacement of teeth; the latter may be caused by crowding, although ectopic developmental position, the presence of a supernumerary, retention of a primary tooth or, rarely, a pathological cause may be responsible. Treatment may be indicated also for spacing or for the management of vertical or transverse problems (see Sections 10.1 and 10.5).
Treatment planning
The basic principles of treatment planning have already been outlined in Section 9.4.
Crowding: The possible measures to be considered in relation to the management of crowding have been presented in Sections 9.4 and 10.1. Some basic guidelines, however, regarding the management of crowding in class I malocclusion are as follows:
• Mild crowding, often present as the permanent incisors erupt, may resolve with some increase in intercanine width and use of leeway space. If present when the permanent dentition is established, it is best accepted.
• Moderate crowding is usually dealt with by first premolar extractions. Where this is undertaken in a growing patient, considerable spontaneous improvement in labiolingual alignment of the incisors and canines will ensue in the following 6 months provided the canines are mesially inclined and movement is not hindered by the occlusion. Thereafter, the potential for further spontaneous change is much less, and fixed appliances are usually required to correct residual occlusal discrepancies.
• Severe crowding often may be managed expediently by the removal of the most displaced teeth or, on occasion, by the extraction of more than one tooth per quadrant. Anchorage planning is most critical in this group and the placement of space maintainers prior to any proposed extractions is almost always necessary.
• Late lower labial segment crowding occurs commonly in late teens and gradually increases throughout the third and fourth decades, representing largely an adaptation to growth changes in the facial skeleton. Other factors have also been implicated (see Table 9.2, p. 261), but the evidence associating the mandibular third molar with late lower incisor crowding is weak. Mild crowding is best accepted and monitored.
• Where the posterior occlusion is class I and the arches otherwise aligned with a mildly increased overbite, moderate-to-severe lower incisor crowding may be dealt with by extraction of one incisor (usually the most malpositioned) followed by alignment and approximation of the remaining units using a sectional fixed appliance. A bonded lingual retainer is advisable to maintain the result, but lingual movement of the lower labial segment may produce reciprocal palatal movement of the upper incisors and lead to their misalignment. This must be drawn to the patient’s attention before treatment starts.
Bimaxillary proclination
Bimaxillary proclination (proclination of upper and lower incisors) is seen typically in Negros, where it can be regarded as normal, but it may occur also in Caucasians in association with class I, class II division 1 or class III malocclusions. In class I, the overjet is increased because of the incisor angulation. Treatment to retract the upper and lower labial segments is generally unstable, as lingual movement of the lower incisors away from their zone of labiolingual balance tends to relapse post-treatment unless retained permanently. The prospect of stability may be improved where the lips have good muscle tone and become competent following incisor retroclination. Where the soft tissue factors are unfavourable (e.g. grossly incompetent lips), treatment is inadvisable.
Spacing
In Caucasians, a generally spaced dentition is rare and is caused by a disproportion in the size of the teeth relative to the arch size or by absence of teeth. Where the spacing is mild, acceptance is usually best. Alternatively, consideration may be given to composite additions or porcelain veneers to increase the mesiodistal width of all the labial segment teeth. In more marked spacing, orthodontic treatment to concentrate the space at specific sites prior to fitting of a prosthesis or implant placement may be necessary.
Space between the upper central incisors is more common. Although this often exists in the early mixed dentition, it usually reduces considerably as the permanent maxillary canine erupts. Other factors that may cause an upper median diastema are given in Section 10.1. On average, the mesiodistal width of the upper lateral incisor is 80% that of the central incisor. Where the lateral incisor is narrower, it should be enlarged by composite or porcelain additions to assist maintenance of diastema closure.
In patients with missing upper permanent lateral incisors, the resulting space may be opened, closed or accepted (Section 10.1).
10.3 Class II malocclusion
Class II malocclusions are divided into divisions 1 and 2.
Division 1
The following factors contribute to the production of a class II division 1 malocclusion.
Skeletal relationships: Although the skeletal relationship is usually class II, class II division 1 malocclusion may exist on a class I or mild class III skeletal pattern. Where a class II skeletal pattern is present, mandibular deficiency is almost entirely the primary cause, although excessive maxillary growth or a combination of the two may be factors in other instances. In contrast, the developmental position or inclination of the teeth resulting from soft tissue or digit-sucking influences are to blame where the skeletal pattern is class I or mildly class III. The anterior vertical proportions of the face vary, and where these are greatly increased or reduced, treatment is likely to be difficult.
Lips, tongue and habits: The effects of the lips and tongue on the incisor position are determined principally by the skeletal pattern and thereafter by the manner in which an anterior oral seal is achieved. Where the skeletal pattern is class II, an acceptable incisor relationship may be achieved by proclination of the lower incisors under the influence of the tongue. In general, however, the greater the class II skeletal discrepancy, the more likely the lips are to be incompetent and to contribute to upper incisor proclination. Where lip incompetence exists along with a class II skeletal pattern and a reduced lower facial height, an anterior oral seal is likely to be produced by the lower lip lying under the upper incisors. This worsens the overjet by proclining the upper and retroclining the lower incisor teeth. In rare cases, the lower lip may be hyperactive and contribute to a class II division 1 malocclusion by solely retroclining the lower incisors. Where the lower facial height is increased, an anterior oral seal is often produced largely by forward positioning of the tongue, thus tending to reduce the overbite further and compensate for the class II discrepancy by proclining the lower incisors.
In very rare instances, a primary atypical swallowing behaviour will cause an overjet increase, but distinguishing this from an adaptive tongue thrust is difficult. The effect of a digit-sucking habit is to procline the upper incisors and retrocline the lower incisors although the overjet increase may be asymmetric depending on the positioning of the digit.
Occlusal characteristics
As forward mandibular posturing to disguise the overjet increase is seen in some patients, it is important to ensure that the mandible is in centric relation before recording the occlusal features.
• ‘The lower incisor edges lie posterior to the cingulum plateau of the upper incisors; there is an increase in overjet and the upper incisors are usually proclined’ (British Standards Institute classification).
• This malocclusion is seen in about 15–20% of Caucasians and the upper incisors are often traumatised because of the increased overjet: the likelihood increasing more than two-fold where the overjet exceeds 3 mm compared to where it is less than 3 mm.
• Drying of the gingivae labial to the upper incisors may occur with grossly incompetent lips, and this will aggravate an established gingivitis.
• The overbite varies depending on the skeletal pattern, the presence or absence of an adaptive tongue thrust on swallowing, or the existence of a digit-sucking habit. It is commonly increased and complete, and sometimes traumatic, with the lower incisors impinging on the gingivae palatal to the upper incisors. It may also be incomplete or tend to an anterior open bite.
• Usually the molar relationship is class II, provided mesial drift following early loss of primary teeth has not occurred.
Treatment
There is little need for treatment where the overjet is mildly increased and the arches are aligned (overjet 3.5–6 mm with competent lips; dental health component of the Index of Orthodontic Treatment Need (IOTN) (grade 2)). In such cases, the facial and dental appearance as well as the risks to dental health are minimal and acceptance of the malocclusion is reasonable. Where the overjet increase is between 6–9 mm or greater than 9 mm, the need for treatment on dental health grounds is great or very great, respectively. The factors that must be considered regarding any potential treatment are discussed in Section 9.4.
Special considerations in treatment planning:
Skeletal pattern and profile: In general, the more the anteroposterior and vertical skeletal relationships deviate from normal, the more likely the profile is to be compromised and the more difficult treatment is likely to be. Where the nasolabial angle is obtuse or there is a marked ‘gummy smile’ or a short upper lip, treatment mechanics must ensure that overjet reduction does not worsen facial aesthetics; a combined orthodontic surgical approach may be best. Non-extraction treatment may be preferable to address mild-to-moderate crowding and avoid potential compromise to facial profile from extraction-based treatment.
Mandibular growth: The amount and pattern of mandibular growth can aid or detract from correction of a class II division 1 malocclusion in the growing patient. A forward mandibular growth pattern is favourable and is generally associated with situations where the lower facial height is reduced. A backward pattern of mandibular growth seen in individuals with increased lower facial height is unfavourable because the class II skeletal pattern is aggravated and the likelihood of lip competence post-treatment is reduced. In the non-growing patient, correction of both overbite and overjet of skeletal origin is difficult, and surgical correction may be required.
Form and relationship of the lips and tongue at rest and in function: It is important to assess the likely impact of the lips and tongue in the aetiology of the malocclusion and, more importantly, whether a stable correction is possible by altering or correcting their influence. As a digit-sucking habit may affect the swallowing pattern and the incisor position, it should be ceased before treatment commences.
Space requirements: Space is required in the lower and upper arches for overbite reduction and overjet correction, respectively (the former always preceding the latter), in addition to that needed for possible relief of crowding (see Section 9.4). On occasion, this may necessitate the loss of four units in the upper arch, usually where the lower labial segment is crowded and the buccal segment relationship is more than class II. Sometimes, in these cases, treatment may be started with a functional appliance to correct the molar relationship to class I, followed then by extractions for relief of crowding.
Where the lower arch is aligned, the buccal segment relationship typically half a unit class II and the overjet increase modest, space for overjet reduction may be obtained by moving the upper buccal segments distally using headgear or with the assistance of temporary anchorage devices (TADs) (screws or implants). Removal of the upper second permanent molars may be required.
Treatment in class I or mild class II skeletal relationship: Rarely, will treatment by tipping movements and upper removable appliance therapy alone be possible. Where the FMPA is average or slightly reduced, the arches are aligned and uncrowded and the upper incisors sufficiently proclined that, when the overjet is reduced, they will form no less than a 95° angle to the maxillary plane, then this may be considered. The highest quality outcome, however, is to be obtained with fixed appliances. Where occlusal factors (in particular, the inclination of the canines and maxillary incisors) are not amenable to tipping movements, fixed appliances are indicated (often in combination with extractions to allow relief of crowding) for correction of the incisor and buccal segment relationships. Removal of lower second and upper first premolars often favours the attainment of these occlusal goals. In the mixed dentition with a mild/moderate class II pattern, overjet reduction may be carried out using a functional appliance, although this is often followed by a phase of fixed appliance treatment, sometimes in combination with extractions, to optimise the final occlusal result (see Section 10.1).
Treatment in moderate-to-severe class II skeletal relationship: Three possibilities exist in relation to treatment in moderate-to-severe class II skeletal relationships.
Growth modification: Growth modification is only possible in the growing child. Ideally the arches should be uncrowded. Treatment should be undertaken just before and/or during the pubertal growth spurt. Success depends on creating a differential in the rate of growth of the maxilla and mandible. Depending on the relative contribution of maxillary prognathism or mandibular retrusion to the skeletal class II malocclusion, an attempt may be made to restrain horizontal and/or vertical maxillary growth, stimulate mandibular growth or both. While headgear restrains maxillary growth with forces of up to 1000 g in total, a functional appliance accelerates mandibular growth; the final mandibular size, however, with functional appliance treatment is little if any greater than it would have been without treatment. Wear of either headgear or a functional appliance or both for 14–16 hours per day, in conjunction with favourable growth, is necessary for a successful outcome. The correction achieved in the early mixed dentition with functional appliance or headgear has not been upheld long term; in addition, there were only minor, if any, differences following fixed appliance treatment in the permanent dentition between those who received early treatment and those allocated initially to the observation group. Consequently, in current practice, early treatment is only considered in those cases with psychosocial handicap.
When functional appliance treatment is planned, assessing standing height and secondary sexual characteristics assists in determining if a patient has begun the pubertal growth spurt. The stage of cervical vertebral maturation (CVM) viewed on a lateral cephalometric film has also been shown to be useful in assessment of optimal treatment timing. Following overjet correction, wear of the appliance as a retainer until growth has reduced to adult levels is required, unless a second phase of treatment to align the arches with fixed appliances and possibly extractions is considered.
Orthodontic camouflage: The skeletal discrepancy can be disguised by orthodontic tooth movement; this corrects the incisor relationship but the class II skeletal pattern remains. Invariably, treatment involves upper arch extractions, most commonly first premolars, and fixed appliance therapy to bodily retract the incisors. The effect of repositioning the teeth must not have a detrimental effect on the facial profile, otherwise ‘camouflage’ will have failed. Realistically this option is only acceptable where the class II skeletal pattern is no worse than moderate, the vertical facial proportions are good and the arches are reasonably well aligned so that the extraction spaces can be used for overjet reduction and not for relief of crowding. Where the lower incisors are retroclined by a habit, lip trap or deep overbite, it may be possible for them to be proclined by treatment and for this ‘camouflage’ to be stable.
Orthognathic surgery: Where growth is complete and camouflage would not produce optimal facial and dental aesthetics, surgical correction of the malocclusion is best (see Section 10.6). In such an individual, an overjet >10 mm is the best indicator that successful correction by camouflage is unlikely. This is especially so if the mandibular incisors are proclined relative to a short and deficient mandible and/or the total face height is increased.
Retention and post-treatment stability: The interincisal angle should be within normal limits, the overjet completely reduced with the upper incisors in soft tissue balance (i.e. no tongue thrust) and the lower lip covering at least one-third of their labial surface. Where these criteria are met, the prospect of stability is good. Retention planning is discussed elsewhere (see Section 11.4) but retention until growth is complete is required following functional appliance treatment.
Division 2
Skeletal relationships: The skeletal pattern in division 2 malocclusion is usually mildly class II, although it may be class I or mildly class III. A reduced lower facial height is common with an associated anterior mandibular growth rotation, which tends to increase the overbite. A relatively wide maxillary base may lead to a lingual crossbite of the first premolars.
Soft tissues: The high lower lip line (covering more than one-third of the upper incisor crowns) and resting pressure (about 2.5 times greater than that of the upper lip) are the most significant aetiological factors in retroclination of the upper incisors. The lower lip level depends largely on the lower anterior facial height; the more reduced the lower anterior facial height, the higher the lower lip line. Where the lower lip is also hyperactive, bimaxillary retroclination will result.
Dental factors: The upper incisor cingulum is often reduced or absent, which may exacerbate the overbite. In addition, there is an increased likelihood of the teeth being smaller than normal, as is the chance of a more acute crown/root angulation. Retroclination of the upper, and commonly of the lower, incisors also makes existing crowding worse.
Occlusal features
The main occlusal features are the following:
• ‘The upper central incisors are retroclined. The overjet is minimal but may be increased’ (British Standards Institute classification).
• The upper lateral incisors are often proclined and mesiolabially rotated but they may also be retroclined.
• Occasionally upper and lower incisors are retroclined, usually associated with a high lower lip line where the lip is hyperactive.
• The overbite may be traumatic: palatal to the upper incisors, labial to the lowers or, in severe cases, in both locations.
• Because of the discrepancy in arch widths and the class II skeletal relationship, a scissors bite is often present in the first premolar area.
Treatment
Treatment planning: The following factors in particular must be considered in relation to treatment planning.
The underlying skeletal discrepancy, both anteroposteriorly and vertically: In general, the more class II the skeletal pattern and the lower the FMPA, the more difficult treatment is likely to be to achieve a normal incisor relationship.
The growth potential and pattern of facial growth: In a growing patient, correction of both a class II skeletal pattern and deep overbite is facilitated by favourable facial growth. Although a forward mandibular growth rotation aids correction of a class II skeletal discrepancy, it tends to increase the overbite.
Profile considerations: Occasionally, a non-extraction approach may be adopted, usually in those with bimaxillary retroclination, to prevent the proposed risk of adverse profile change that may result from an extraction-based plan. There is, however, little difference in lip fullness with either approach. When the profile is particularly unfavourable in an adult, usually with a marked class II pattern and very reduced FMPA, a combined orthodontic/surgical approach will be required.
The presence and degree of crowding: Lower arch extractions should only be considered where the crowding is marked. There is a risk of a deep overbite becoming traumatic as the lower incisors are allowed to drop lingually if extractions are undertaken in the presence of mild-to-moderate crowding. In addition, as the lower labial segment is constricted by the upper labial segment, some stable expansion of the lower intercanine width and proclination of the lower incisors may be feasible, thereby providing space for relief of mild-to-moderate crowding. Where extractions are necessary, a lower fixed appliance should be used to close residual spacing and prevent retroclination of the lower labial segment. In these cases, consideration should be given also to upper arch extractions and correction of the incisor relationship.
The lower lip level: Where the lower lip level is at the gingival third of the upper incisor crowns or higher, correction of the incisor relationship without recourse to indefinite retention is unlikely.
The depth of overbite and inclination of the upper incisors: The depth of overbite and the inclination of the upper incisors determine the two approaches to treatment: either acceptance or correction of the incisor relationship.
Overbite reduction may be achieved by various means, including:
In addition, proclination of the upper incisors, followed by a functional appliance to correct the overjet created, will reduce the overbite.
In a growing patient, use of a flat anterior bite plane on an upper removable appliance will retard lower incisor eruption while allowing the lower posterior teeth to erupt, thereby reducing the overbite. Facial growth then accommodates the increase in lower facial height. Extrusion of the upper molars by cervical headgear, or of lower molars using intraoral elastics attached to a fixed appliance, is only advisable in a growing patient as a means of overbite reduction. Attempts to intrude the incisors, for example by utility arches, are effective to a limited extent; however, the molars are also extruded somewhat. More apparent than real intrusion is likely.
Lower incisor proclination is not usually stable unless the lower incisors have been held in a retroclined position behind the cingulum of the upper incisors. Fitting an upper removable appliance with a flat anterior bite plane will allow spontaneous labial movement of the lower incisors to adopt a position of labiolingual balance. Careful planning by a specialist is required if active proclination of the lower incisors is considered.
A combined orthodontic/surgical approach is best in adults where the overbite is deep and the skeletal pattern is markedly class II.
Acceptance of the incisor relationship: Where the upper labial segment crowding and retroclination are mild and the overbite onto tooth tissue, it is reasonable that no active treatment be undertaken. If treatment is indicated, however, it is confined to relief of upper arch crowding and alignment of the upper labial segment alone.
Correction of the incisor relationship: The interincisal angle and the overbite must be reduced for stable correction. The interincisal angle must be reduced to at least 135° (preferably less) to allow for an effective occlusal stop.
Adjustment of incisor root torque/lower labial segment proclination: Usually fixed appliances are used to effect palatal root torque and reduce the overbite, sometimes by proclination of the lower incisors. Planning the final incisor positions requires considerable expertise, as proclination of the lower labial segment may stress the labial periodontium and create gingival recession, while the possible degree of palatal/labial root torque required is limited by the thickness of the alveolar processes. Anchorage demands are also increased because of the torquing movements.
Proclination of the labial segment or extractions will provide space for relief of mild-to-moderate or severe lower arch crowding, respectively, while in the upper arch, space to correct the incisor relationship may be created by moving the buccal segments distally (either by headgear or an alternative means) or by extractions. To prevent lingual movement of the lower incisors, second premolar extractions are preferred; upper first or second premolars may be chosen depending on the anchorage demands and space requirements. Permanent lower retention may be required depending on the amount of lower incisor proclination, and the addition of a flat anterior bite plane to an upper Hawley retainer is advisable to prevent overbite relapse. This should be worn until at least growth has reduced to adult levels.
Growth modification: In a growing child with a mild to moderate class II skeletal pattern, with ideally a well-aligned lower arch, a functional appliance may be used to modify growth and correct the incisor relationship. To allow the mandible to be postured forward for the construction bite and to ensure favourable arch co-ordination post-treatment, the retroclined maxillary incisors must be proclined and the upper arch expanded prior to the functional appliance phase; the amount of upper arch expansion required, however, is often of a very modest nature due to the tendency for the maxillary arch form to be wider than that of the lower. If a twin block functional appliance is used, this has a midline screw for upper arch expansion and springs may be incorporated in the upper appliance for incisor proclination (or their alignment may be undertaken simultaneously with a sectional fixed appliance), thereby avoiding the need for a preliminary separate phase of treatment. After functional treatment, detailing of the occlusion is usually completed by fixed appliances ideally followed by retention until the late teens.
Orthognathic surgery: Where the facial profile is poor because of the marked skeletal discrepancy anteroposteriorly and/or vertically, and particularly in the adult with a deep traumatic overbite, a surgical approach in conjunction with orthodontics is best. A class II division 1 incisor relationship is created presurgically but the increased curve of Spee is maintained. Following mandibular advancement to correct the overjet and facial profile, the lower buccal segment teeth are extruded to level the arch and close the lateral open bites.
Post-treatment stability: Two features of class II division 2 malocclusion are particularly prone to relapse:
Rotational correction early in treatment and pericision should be undertaken to help to prevent relapse, but as these do not guarantee stability, bonded palatal retention long term is advisable, ensuring that this is supervised appropriately.
An increase in lower facial height and inferior movement of the lower lip away from the upper labial segment aids correction of the interincisal angle but is dependent on favourable vertical facial growth. Even where these features are evident, the closing pattern of mandibular growth tends to increase the overbite into adulthood. Following overbite correction, an upper removable retainer incorporating a flat anterior bite plane is recommended until growth is complete, but in many cases long-term retention is advisable.
10.4 Class III malocclusion
Aetiology
Skeletal pattern: The skeletal pattern is most usually class III although it may be class I with the class III malocclusion due to incisor position or inclination. Mandibular, maxillary and cranial base factors often make a combined contribution to the underlying class III skeletal relationship. The mandible is longer; the glenoid fossa positioned more forward, the maxilla shorter and/or retrognathic in addition to a shorter anterior cranial base. The vertical relationship of the skeletal bases varies from increased to average or reduced and is generally reflected in the depth of overbite, which may alter depending on the pattern of facial growth. Where this is vertical rather than horizontal, an anterior open bite is likely.
Commonly, a transverse discrepancy exists in the dental base relationship because of the narrow maxillary and wider mandibular bases, although this is often worsened by the class III skeletal pattern.
Soft tissues: The soft tissues contribute little to the aetiology of the malocclusion. Instead, where the lips are competent, the lips and tongue induce retroclination of the lower and proclination of the upper incisors (dento-alveolar compensation); as a result, the incisor relationship masks the true severity of the skeletal pattern. Where the lower anterior facial height is increased, however, the lips are frequently incompetent, with an adaptive tongue thrust on swallowing which may procline the lower incisors.
• ‘The lower incisor edges lie anterior to the cingulum plateau of the upper incisors, the overjet is reduced or reversed’ (British Standards Institute classification).
• The overbite may be increased, average or reduced. Where the vertical facial proportions are increased, there is often an anterior open bite.
• Frequently, the upper incisors are proclined and the lower incisors retroclined, compensating for the underlying class III skeletal pattern.
• Upper arch crowding is common, often because of a short and narrow dental base, while the lower arch is more commonly aligned or spaced.
• Crossbites of the labial and/or buccal segments are common, resulting from the underlying class III occlusal discrepancy as well as from differences in the length and width of the arches. Crossbites may be associated with a mandibular displacement (see Section 9.3), particularly where a unilateral buccal segment crossbite exists. In the case of an anterior crossbite, the possibility of displacement should be assessed by checking if the patient can bite with the upper and lower central incisal edges contacting. Lower incisor mobility and occasionally gingival recession may be associated with the anterior crossbite.
Treatment
Account must be taken of the following factors.
The degree of anteroposterior and vertical skeletal discrepancy: The degree of anteroposterior and vertical skeletal discrepancy is the most important factor in planning treatment and assessing the prognosis. As it is usually directly reflected in the facial and dental appearance, it will influence also the complexity of treatment undertaken through the patient’s perception of these features.
The potential direction and extent of future facial growth: The general trend for downward and forward mandibular growth to surpass that of the maxilla is unfavourable for class III correction. Relevant family history, the age and gender of the patient, together with assessment of the vertical facial proportions, may help in making a ‘guesstimate’ as to the likely changes with growth. A reduced or average anterior facial height is often associated with a closing mandibular growth rotation, and a horizontal pattern of mandibular growth worsening the reverse overjet. With an increased vertical facial height, there is a tendency for a backward mandibular rotation to increase the likelihood of anterior open bite.
The incisor inclinations: The incisor inclinations indicate the degree of dento-alveolar compensation; if this is already marked, further compensation by orthodontic means is unlikely to be stable or to produce an aesthetic result.
The amount of overbite: It is essential that there is an adequate overbite post-treatment to improve the prospects of stable overjet correction. Where the overbite is average or increased pretreatment, stability is more likely than where the overbite is reduced. Proclination of the upper incisors reduces the overbite while retroclination of the lower incisors increases it. Both movements may be necessary in some cases.
The ability to achieve an edge-to-edge incisor relationship: If it is not possible to achieve an edge-to-edge incisor relationship, correction of the incisor relationship by simple means is unlikely.
The degree of upper and lower arch crowding: The following should be borne in mind. Upper arch extractions should be delayed until a reverse overjet and/or buccal crossbites have been corrected. This may provide space for relief of mild-to-moderate upper arch crowding. Where extractions are undertaken in the upper arch only, the reverse overjet may worsen with palatal movement of the upper labial segment. Where mid upper arch extractions are necessary, extraction of lower first premolars is usually advisable to allow correction of the incisor relationship.
Treatment
No treatment is an option when the skeletal pattern is mildly class III and/or the incisor relationship is acceptable, with minimal crowding and no mandibular displacement.
Treatment in class I or mild class III skeletal pattern: Where the lower anterior facial height is increased, the overbite is usually minimal and the incisor relationship should be accepted. Treatment should focus on aligning the arches, with possible extractions. Upper arch expansion for crossbite correction will create space for relief of crowding. When this is indicated, fixed appliance mechanics must be used to minimise unfavourable dropping of the palatal cusps of the premolars and molars, as this will reduce the overbite further.
Provided the lower anterior facial height is average or reduced, with a normal or increased overbite and upright upper incisors, proclination of the upper labial segment may be undertaken. This is often best carried out in the early mixed dentition before the permanent canines move labial to the lateral incisor roots, thereby increasing the risk of resorption if their proclination is attempted. In such cases, treatment is best deferred until the canines have been retracted, removing the obstruction to crossbite correction of the lateral incisors. An upper removable appliance, incorporating a screw or Z-springs and posterior capping, may be used to correct the anterior crossbite (Fig. 10.2), but a fixed appliance may be indicated depending on the presence of other occlusal features.
The need for upper arch extractions should be reassessed after the incisor relationship has been corrected, as some additional space for relief of crowding will be forthcoming from anteroposterior expansion. Movement of the upper buccal segments distally is not a favoured option as restraint of maxillary growth is likely. Often, extraction of the lower primary canines in the early mixed dentition, or of first premolars in a crowded lower arch in the permanent dentition, is advantageous in allowing the lower labial segment to drop lingually and increase the overbite.
Treatment in mild-to-moderate class III skeletal pattern: Where the overbite is average or increased, two options exist: growth modification or orthodontic camouflage.
Growth modification: In general, attempts to modify growth in class III malocclusion are disappointing, largely because the inherent tendency for growth is unfavourable. Where the underlying skeletal problem is mild, however, caused by either maxillary deficiency or mandibular excess, an effort may be made in the early mixed dentition to augment forward maxillary growth or ‘restrain’ mandibular growth. Maxillary protraction facemask treatment applies tension to the posterior and superior maxillary sutures, typically via a bonded or banded rapid maxillary expansion splint, and is ideal where maxillary retrognathia exists in combination with average or reduced vertical facial proportions, and upright, or slightly proclined, upper incisors.
Treatment must be started in the early mixed dentition, definitely before 10 years of age and preferably younger, to maximise the chances for successful forward movement. Forces of ~350–450 g per side are applied for 12–14 hours per day with a slight downward direction (~30°) from the maxillary splint to the facemask frame. The expansion device is usually turned once per day, until the upper palatal cusps approximate the lower buccal cusps. The overall skeletal correction is brought about by moving the maxilla down and forward which rotates the mandible down and back. Additionally, the mandibular teeth are displaced backward and the maxillary teeth forward. There is often rebound of mandibular growth when treatment is discontinued and surgical correction may be required after adolescence. Results of a recent randomised controlled trial indicate maxillary protraction treatment in children under 10 years to be 70% successful (i.e. a positive overjet was achieved). There was, however, no discernible psychosocial improvement. Longer-term follow-up of cases treated with maxillary protraction to late adolescence also found ~70% success. To maximise the skeletal changes, it is now possible to use mini-plates in the infrazygomatic crest of the maxillary buttress and between the lower canine and lateral incisors with class III intermaxillary elastic traction. Results so far are promising but long-term follow-up is required.
Compressive forces applied to the condylar area via a chin cup have never been very successful, but if the force is aimed below the condyle, redirection rather than restraint of mandibular growth occurs. In essence, a downward and backward mandibular rotation is effected which increases the lower anterior facial height and reduces chin prominence. Lingual tipping of the lower incisors helps to correct the incisor relationship.
A functional appliance, particularly a Frankel III, may also be used for correction of mandibular prognathism, although only limited posterior mandibular posturing is possible. Mandibular growth is not restrained and the effects are similar to chin cup therapy where the force is directed below the condyle. For both chin cup and functional appliance therapy, the skeletal pattern should ideally be mildly class III with reduced vertical facial proportions, and the ability should exist to achieve an edge-to-edge incisor relationship with upright or proclined lower incisors. In all class III situations where growth modification is attempted, there is a need for prolonged follow-up during and after adolescence in order to monitor mandibular growth.
Orthodontic camouflage: Orthodontic camouflage may be considered where the overbite is mildly reduced. Treatment aims to correct the incisor relationship by retroclination of the lower labial segment and/or proclination of the upper labial segment. Lower arch extractions, preferably of first premolars, are usually necessary in conjunction with class III intermaxillary traction to upper and lower fixed appliances. Expansion of the upper arch will tend to compromise the overbite (as the palatal cusps tend to drop down) unless undertaken with rectangular wire incorporating additional torque to upright the premolar and molars. Extrusion of the upper molars ought to be avoided as this will also reduce the overbite. Lower arch extractions must only be undertaken where the likelihood of achieving successful overjet correction is favourable. Should the result relapse with further mandibular growth, surgical correction may be required. Any decompensation will need to be undone as part of presurgical orthodontics, which will result in opening up of the extraction spaces.
In some cases, proclination of the upper labial segment may be aided by reverse-pull headgear to the upper fixed appliance. More commonly, this technique is reserved for use in cleft lip and palate or maxillary hypodontia to augment anchorage during upper arch space closure.
Treatment in severe class III skeletal pattern:
Orthognathic surgery: Where the skeletal discrepancy is more marked in the anteroposterior and/or vertical dimension, and therefore not amenable to satisfactory correction by orthodontic camouflage, the arches may be aligned and the incisor relationship accepted or correction may be brought about by orthognathic surgery. ANB <40 and lower incisor inclination less than 830 to the mandibuar plane have been suggested as indicators for surgery rather than camouflage. The former is preceded by fixed appliance therapy to decompensate the arches. Then, often a combination of maxillary advancement and/or posterior impaction with mandibular set back, and possibly a reduction genioplasty, is necessary to attain the optimal profile change.
10.5 Open bite and crossbite
Open bite
An open bite may exist anteriorly or posteriorly in the arch.
Anterior open bite
The incisors do not overlap vertically when the posterior teeth are in occlusion.
Skeletal pattern: An increase in lower facial height and high FMPA leads to an increase in the distance between the upper and lower incisors. Where it is not possible for the incisors to erupt sufficiently to compensate for this, an incomplete or anterior open bite results. This is worsened by the downward and backward pattern of mandibular growth, which contributes to the likely additional class II skeletal pattern.
Soft tissues: Rarely an open bite is caused by the action of the tongue. The forward positioning of the tongue to achieve an anterior oral seal is usually adaptive in those with increased vertical skeletal proportions, as there is a greater tendency for the lips to be incompetent. A similar swallowing pattern is often observed in children with an anterior open bite caused by a digit-sucking habit. Where a tongue thrust is endogenous/primary (which is rare), there is often a lisp and some proclination of upper and lower incisors.
Habits and open mouth breathing: A persistent digit-sucking habit inhibits eruption of the incisors, often producing an asymmetric anterior open bite. Occasionally, a posterior crossbite is produced through unopposed action of the cheek muscles as the tongue is lowered by the presence of the digit during sucking. Research shows that, in the main, open mouth breathing, due to nasal obstruction or habit and which may lead to altered head posture and increased lower facial height, does not have a major role in aetiology of anterior open bite.
Treatment: With the exception of an anterior open bite caused by a habit, treatment is complex and is best managed by a specialist.
Monitor and/or accept: The open bite may be monitored/accepted if it is mild or where the prospect of stability is poor because of adverse skeletal and/or soft tissue factors, notably grossly incompetent lips and/or the suspicion of a primary tongue thrust.
Orthodontic and surgical management: The aim is to increase or at least maintain the overbite. Extrusion of molars, which may occur through use of a flat anterior bite plane on an upper removable appliance or cervical-pull headgear, must be avoided. Expansion of the upper arch, which is likely to extrude the palatal cusps and ‘prop open’ the bite, should also be avoided.
Assuming that there are no adverse growth or soft tissue factors, growth modification may be possible using high-pull headgear to the upper molars in mild open bite, or by attaching high-pull headgear to a removable or functional appliance with buccal capping where a class II skeletal pattern and a more marked anterior open bite exists. Where an anterior open bite is associated with a ‘gummy smile’, high-pull headgear to a full-coverage maxillary splint is indicated. As extrusion of the incisors to close an anterior open bite is unstable, the aim in all cases is to attempt to maintain the vertical position of the maxilla while preventing eruption of the upper posterior teeth. Attempts to intrude the maxilla and modify growth require excellent patient co-operation, with a minimum of 14–16 hours per day wear of the headgear and any other appliance. Following correction of the anterior open bite, fixed appliances are often required, sometimes in conjunction with extractions, to detail the occlusion.
Occasionally, camouflage by incisor retraction following relief of crowding can be stable if the lips become competent post-treatment. The contention that extraction of molars may aid overbite increase is unproven.
Where the anterior open bite is severe, a combined orthodontic/surgical approach is best when growth is complete.
Treatment of open bite caused by habits: Gentle discouragement of a digit-sucking habit in the early mixed dentition often leads to spontaneous correction of an anterior open bite, although it may take up to 3 years for the overbite to be regained. Fitting an upper removable appliance may act as a habit breaker and allow incisor retraction once the habit has ceased.
Posterior open bite
Posterior open bite exists where there is no contact between the buccal segment teeth when the remainder of the dentition is in occlusion.
It is very rare and the exact aetiology often incompletely understood. Causes include unilateral condylar hyperplasia. Here removal of the condyle is required if growth is excessively active. It is also caused, rarely, when the molar teeth fail to erupt despite apparent bone resorption in advance of the teeth (primary failure of eruption), or eruption is arrested at a certain occlusal level while adjacent teeth maintain contact with the opposing teeth. In both cases, extraction of the molar is the only treatment option. A lateral open bite is occasionally seen in the buccal segments with infraocclusion or following early loss of primary molars. In the latter situation, lateral tongue spread has been given as a possible cause, but it is likely that other factors are involved. Any attempt to extrude the teeth into occlusion usually relapses. Lateral open bites usually occur bilaterally as a transient feature during twin-block therapy but resolve as the buccal blocks are trimmed and the posterior teeth erupt into occlusion.
Crossbite
A crossbite is a buccolingual malrelationship of the upper and lower teeth. It can be anterior or posterior, unilateral or bilateral and may be associated with a mandibular displacement on closing such that an occlusal contact deflects the mandible laterally or anteriorly to allow maximum interdigitation. With a lateral displacement, there is often a centreline shift. By convention, the lower teeth are described relative to the upper so where the lower teeth occlude buccal to the opposing teeth, a buccal crossbite exists. Conversely, where the lower teeth occlude lingual to the palatal cusps of the upper teeth, a lingual (scissors) crossbite exists.
Aetiology
Skeletal factors: A mismatch in the widths of the dental arches or an anteroposterior skeletal discrepancy may produce a crossbite of a complete arch segment – a lingual crossbite commonly found in class II – whereas a buccal and/or anterior crossbite is often associated with a class III malocclusion.
Growth restriction of the maxilla following cleft repair or of the mandible secondary to condylar trauma can lead also to buccal segment crossbite.
Soft tissue factors: With a digit-sucking habit, the tongue position is lowered and contraction of the cheeks during sucking is unopposed. This displaces the upper posterior teeth palatally and often creates a crossbite.
Treatment
It is important to realise that where a crossbite is associated with a mandibular displacement, there is a functional indication for its correction, as displacing occlusal contacts may predispose to temporomandibular joint problems in susceptible individuals. In addition, a traumatic displacing anterior occlusion may deflect a lower incisor labially and compromise periodontal support.
Treatment of anterior crossbite: Where one or two incisors are in crossbite. there is usually a mandibular displacement, and correction early in the mixed dentition is advisable provided adequate overbite exists to maintain correction. Space must be present in the arch (or can be created by extraction) to allow alignment of the tooth. If the tooth inclination is amenable to tipping, an upper removable appliance with buccal capping to free the occlusion and a Z-spring for proclination may be used (see Fig. 10.2). Anterior retention must be good to resist the displacing force caused by the action of the spring. Alternatively, an appliance with a screw section, clasping the teeth to be moved, overcomes this problem. Where insufficient overbite is likely to exist post-treatment, or the incisor is bodily displaced, treatment is better carried out with a fixed appliance in the permanent dentition. Treatment of anterior crossbite involving two or more incisors is considered in Section 10.4.
Treatment of unilateral buccal crossbite: An upper removable appliance incorporating a T-spring or screw section may often be considered for correcting a crossbite on a premolar or molar, respectively (Figs 10.3 and 10.4). However, where reciprocal movement of opposing teeth is needed, fixed attachments should be placed and cross-elastics used to achieve the desired movement. Where a single tooth is mildly displaced from the arch, relief of crowding may be necessary to aid crossbite correction. In those with more marked tooth displacement, extraction rather than orthodontic alignment may be a better option.
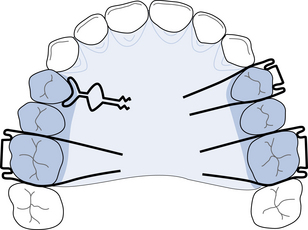
Fig. 10.3 Correction of crossbite on a premolar – upper removable appliance to move 4| buccally.
T-spring 4| (0.5 mm SS wire); Adams’ clasps 6|46 (0.7 mm SS wire); buccal capping relieved over 4|.
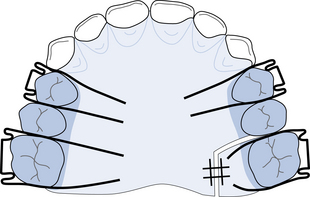
Fig. 10.4 Correction of a crossbite on a molar – upper removable appliance to move |6 buccally.
Screw section to move |6 buccally; Adams’ clasps 64|64 (0.7 mm SS wire); buccal capping.
Where a unilateral buccal segment crossbite is associated with a mandibular displacement, this usually results from a mild mismatch in widths of the dental bases, sometimes as a result of narrowing of the upper arch caused by digit sucking. Grinding of the relevant primary teeth, where a premature contact results in a mandibular displacement, is advised to prevent the associated posterior crossbite from being carried forward to the permanent dentition. Otherwise, upper arch expansion using a removable appliance with midline expansion screw and buccal capping to disengage the occlusion, or by a quadhelix appliance, may be used for correction provided the teeth are not tilted buccally already. The quadhelix consists of a 1 mm stainless steel wire with four coils; it is attached to bands cemented to a molar tooth on each side of the arch. Alternatively, a preformed appliance may be slotted into welded attachments on the palatal aspect of the molar bands. Differential slow arch expansion anteriorly and/or posteriorly may be achieved following customary activation of half a tooth width per side. Slight overcorrection is advised to compensate for the relapse tendency. Although, treatment with an upper removable appliance or quadhelix produced similar results, treatment with a quadhelix has been shown to be more economical.
Treatment of bilateral buccal crossbite: A bilateral buccal crossbite is seldom associated with functional problems. Generally, as its existence indicates an underlying symmetrical transverse skeletal discrepancy, it is best accepted unless correction is planned as part of overall treatment, when rapid expansion of the midpalatal suture should be attempted only by a specialist. This is achieved by turning a midline screw, connected to bands cemented on first premolar and molar teeth, twice daily for 2 weeks. Expansion of the suture must be carried out no later than in early teenage years but, based on limited data, it appears that only 25% of the expansion achieved is stable long term. Surgically-assisted rapid palatal expansion (SARPE) (see Section 10.6) may be considered in the adult.
Treatment of lingual crossbite: Crowding may displace a single tooth into lingual crossbite. Once the crowding is relieved, the crossbite may be corrected, often by palatal movement of the upper unit using a buccally approaching spring on a removable appliance, provided the occlusion is disengaged. Where a complete unilateral lingual crossbite is associated with a mandibular displacement, lower arch expansion and upper arch contraction with either removable or fixed appliances can produce a stable result provided a good buccal intercuspation is achieved. Surgical correction may be indicated to correct a complete bilateral lingual crossbite or unilateral lingual crossbite with no displacement.
10.6 Adult and surgical–orthodontic treatment
Adult orthodontics
Orthodontic treatment in adults is the most rapidly expanding area of contemporary orthodontic practice. The increased focus on facial and dental appearance allied with improved awareness of the potential of orthodontic tooth movement to improve dental aesthetics and greater social acceptability of appliances account for this.
Special consideration in adults
There are a number of factors that are specific for orthodontic procedures in adults:
• Adults are generally highly motivated orthodontic patients, able to specify their concerns, but they tend to have higher expectations of the final result than younger patients.
• The dentition may be compromised because of periodontal disease, tooth loss or extensive restorative treatment. Careful pretreatment assessment is required and all systemic and dental disease must be controlled before orthodontic treatment starts. Occasionally existing bridgework may need to be removed to allow tooth movement to proceed. Often, input from a variety of other disciplines (restorative, periodontal, prosthodontic and surgical) is necessary to achieve the best result, and integrated treatment planning must be co-ordinated in a logical sequence.
• There is also a greater likelihood of systemic illness impacting on the treatment plan in adults.
• Due to the absence of growth, skeletal discrepancies (other than mild) are best dealt with by orthodontics in combination with surgery rather than by camouflage.
• Where camouflage is considered, overbite reduction by intrusion of the incisors rather than by extrusion of the molars is necessary.
• Anchorage planning is often more demanding than in the younger patient because of previous tooth loss and the possibility of reduced bony support of the remaining teeth. Headgear is not a realistic treatment option and alternatives such as palatal arches or bone anchor devices must be considered.
• Because of the reduced cell population and often reduced vascularity of the alveolar bone, the initial response to orthodontic forces is slow; however, once tooth movement starts it tends to progress as efficiently as in adolescents. The bone remodelling process necessary for tooth movement, however, is slower in those taking oral bisphosphonates for osteoporosis (see Section 9.3).
• Some pain is common for 3–4 days following appliance adjustment, and light forces should be applied initially in all cases and throughout treatment where periodontal support is compromised.
• To improve the appearance of the appliance, aesthetic brackets or lingual appliances are options. In selected cases, treatment by a series of clear vacuum-formed thermoplastic aligners may be considered.
• Bands should be avoided in those with periodontal breakdown; fully bonded appliances should be used instead. Indeed there is an increasing trend to use bonded attachments on all teeth in adults due to longer clinical crowns.
Adjunctive or comprehensive orthodontic treatment in the adult
Adjunctive treatment: Adjunctive treatment involves carrying out tooth movement to correct one aspect of the occlusion to improve dental health or function, although the final occlusal result may not be necessarily ideal or class I. Treatment duration is usually about 6 months and typically is integrated with periodontal or advanced restorative procedures. Uprighting of teeth that have tilted into an extraction space prior to bridgework, extrusion of teeth with a subgingival fracture margin to allow placement of a coronal restoration on sound root surface and anterior alignment to facilitate the best appearance of restorative work are examples of some adjunctive treatments.
Comprehensive treatment: The aim of comprehensive treatment is to achieve the optimal aesthetic and functional occlusal result. Where the skeletal discrepancy is mild, camouflage by dento-alveolar movement is possible using fixed appliances. The principles of treatment planning and treatment follow similar lines to those adopted for class I, class II division 1 and division 2 and class III malocclusions (see Sections 10.2–4) but overbite reduction must be achieved by intrusion of incisors rather than by extrusion of molars. In those with a more marked skeletal discrepancy, a combined orthodontic and surgical approach is required to ensure that the best facial and occlusal results are achieved (see below).
Where significant periodontal breakdown has occurred, comprehensive treatment may still be possible provided disease is controlled and a regular maintenance scheme operates throughout orthodontic treatment. Because of the reduced periodontal ligament area, forces should be as light as possible, and anchorage planning is critical. Fixed appliances using a sectional arch approach are often indicated, and permanent retention with a bonded retainer is usual.
Surgical–orthodontic treatment
Surgical–orthodontic treatment involves correction of dentofacial deformity through a combined surgical and orthodontic approach. In contemporary practice, surgery to correct a jaw deformity (orthognathic surgery) is rarely undertaken independent of concurrent orthodontic treatment, as otherwise the final result is likely to be compromised.
Timing of treatment: Treatment is usually deferred until growth is essentially completed, which is generally in late teens in males and slightly earlier in females. This delay is most important where growth is excessive, particularly in class III cases, as it safeguards against relapse brought about by further growth. Where the temporomandibular joint is ankylosed or the dentofacial deformity is causing severe psychological distress, earlier intervention may be considered.
Planning surgical–orthodontic treatment
A team approach is required, involving the orthodontist and oral and maxillofacial surgeons. Input from a plastic surgeon, restorative specialist, speech therapist and clinical psychologist may be required.
First, the patient’s complaint must be ascertained. This may relate to their dental and/or facial appearance, masticatory (including temporomandibular joint) function, speech or a combination of these. Occasionally, a patient may be overly concerned about some relatively minor skeletal or dental anomaly, which is blamed for lack of success in some aspect of life. In these instances, there is often a deep-rooted psychological problem and referral to an appropriate counsellor may be indicated.
A detailed medical and dental history together with a thorough examination must then be performed, including an analysis of facial form in full face and profile. The height and width proportions of the face including, among others, the alar base width, nasolabial angle, upper incisor exposure at rest and when smiling, relation of the upper dental midline to the other facial midlines and the location of any cranial, maxillary, nasal, mandibular or chin deformities should be noted. Temporomandibular joint signs or symptoms must be documented. Dental and periodontal health, the degree of upper and lower arch crowding and any dento-alveolar compensation should be noted.
Facial and dental photographs, panoramic and lateral cephalometric films and dental casts should be obtained. A posteroanterior cephalometric film is indicated if facial asymmetry is apparent. Where available, cone-beam CT and 3D facial images may be taken for more detailed evaluation.
Record analysis and planning: The patient’s cephalometric film should be traced or digitised and then a ‘standard’ skull template (e.g. Bolton standard, representing the norm) is superimposed to indicate sites of discrepancy. These templates, however, are composites for males and females. Formerly, planning involved enlargement of the photographic negative profile to match 1:1 with the cephalometric film and then ‘cutting and pasting’ to simulate the desired surgical changes.
Newer techniques allow superimposition of the patient’s soft tissue profile, from a digital photograph, on the cephalometric tracing; then, the image is adjusted in line with proposed orthodontic/surgical moves. The patient may view the predicted impact on the soft tissue profile of various ‘simulated’ treatment options, the risks and benefits of which should be explained to facilitate decision making. It should be emphasised that these ‘predictions’ are not an assurance of the likely outcome. 3D planning combining CT scans, 3D facial images with incorporation of digital models is now being refined.
Surgical movement may also be simulated on a duplicate set of dental casts. Where a maxillary procedure is planned, the casts should be mounted on a semiadjustable articulator.
The impact of presurgical decompensation, which usually worsens facial appearance, must also be understood. It may, on occasion, be helpful for a prospective patient to have an opportunity to discuss the process with another individual where a successful outcome has been achieved.
Orthodontic management
Presurgical orthodontics and at surgery: All dental and periodontal disease must be managed before treatment can get underway. Presurgical orthodontics allows the jaws to be positioned in their desired location without interference from tooth positions. This phase of treatment takes about 1 year but may be slightly longer where there is severe crowding or protrusion. It aims to align and co-ordinate the arches or arch segments as well as to establish the vertical and anteroposterior position of the incisors. Usually, this involves placing the incisors at a normal inclination to their respective bases, decompensating for any existing dento-alveolar compensation (nature’s attempt to camouflage a skeletal discrepancy). The full extent of the skeletal problem is thus revealed so maximum surgical correction can then be achieved. Intermaxillary traction for class III or II cases is often used to aid decompensation. Depending on the crowding and space requirements, extractions may be necessary to allow the tooth movements required. Consideration should also be given to removal of impacted third molars at this stage.
In some cases, it is not possible or advisable to decompensate fully for the incisor position because of anatomical constraints (e.g. a narrow symphysis or thin labial gingival tissue in a class III malocclusion). Marked gingival recession is likely in the latter if the lower incisors are proclined.
Space must be created interdentally to allow access for surgical cuts when a segmental procedure is planned. Some tooth movements (e.g. levelling of a curve of Spee in patients with a short face) are managed in a more expeditious manner postsurgically while other movements (e.g. correction of a bilateral skeletal crossbite of the upper arch) can be managed simultaneously with Le Fort I correction for other skeletal problems at the time of surgery.
When presurgical orthodontics is completed, photographic images, radiographs (including a lateral cephalometric film) and impressions should be taken. Arch co-ordination, and the other desired tooth movements, should be checked on a set of work casts. Adjustment to tooth position(s) may be necessary and, in some cases the surgical plan, may require slight amendment. Rigid rectangular stabilising archwires with ball hooks, to allow for intermaxillary fixation, should be placed. An interocclusal acrylic wafer, made from casts positioned to simulate the desired occlusal result, is recommended routinely to ensure accuracy of the postsurgical result. If maxillary or bimaxillary surgery is planned, a facebow recording is necessary to allow the casts to be positioned on a semiadjustable articulator. At surgery, the interocclusal wafer is used to locate the jaws or jaw segments accurately; these are then usually fixed semirigidly in position by either mini-plates in the maxilla or lag screws in the mandible. Intermaxillary fixation may also be required.
Surgical procedures
Surgery may be carried out on the maxilla, mandible or on both jaws depending on the nature and severity of the skeletal problem.
Le Fort I osteotomy: The Le Fort I osteotomy is the most common maxillary orthognathic procedure. Access is usually provided by an incision in the buccal sulcus from left to right first molar areas, or by vertical incisions and tunnelling of the mucosa in those for whom the adequacy of the palatal blood supply may be in doubt. The maxilla is sectioned above the apices of the teeth so that it can be ‘downfractured’ from its anterior wall, tuberosities, lateral nasal walls and nasal septum but remain pedicled on the palate. Superior, inferior or forward movement of the maxilla is then possible; posterior repositioning is not realistic.
Le Fort II osteotomy: With the Le Fort II procedure, the incisions pass through the bridge of the nose and lower border of the orbit, allowing the correction of marked maxillary retrognathism and nasal retrusion.
Le Fort III osteotomy: Via a bicoronal flap, the whole mid-face including the zygomas is separated from the cranium. This is most frequently employed in correction of rare craniofacial anomalies (e.g. Crouzon’s syndrome where the coronal and orbital sutures fuse early, leading to cessation of forward maxillary growth).
Segmental procedures: The Wassmund osteotomy involves separating the premaxilla by vertical cuts distal to the canines; the cuts are then extended horizontally across the palate. It may be used for overjet correction in the presence of premaxillary prominence or correction of a ‘gummy smile’ but is now rarely used. Lack of interdental space for surgical cuts and damage to the adjacent teeth are potential problems with this procedure.
Sagittal split osteotomy: A sagittal split osteotomy is the most frequently undertaken mandibular procedure. The inner and outer parts of the ramus are split through a cut made horizontally above the lingula and obliquely across the retromolar area. These cuts are extended vertically through the buccal cortical plate to the inferior aspect of the mandible. The tooth-bearing part can then be moved forwards or backwards or rotated slightly, but inferior alveolar nerve damage is a common complication.
Vertical subsigmoid osteotomy: The mandible is sectioned via an extra- or intraoral incision by a vertical cut through the sigmoid notch, passing behind the lingula, to the mandibular angle. This procedure is used for correction of mandibular prognathism.
Bimaxillary procedures: Correction of the skeletal problems in many individuals involves surgery to both the maxilla and mandible to produce optimal dentofacial harmony.
Distraction osteogenesis: Based on manipulation of a healing bone, this technique stretches an osteotomised site in advance of calcification to induce the generation of new bone formation and investing soft tissue. Where large distances of movement are required and/or deficient jaws increased in size at an early age, this technique has its greatest applications. The maxilla or mandible can be moved forward with distraction but it lacks the precision of standard orthognathic procedures in terms of placement of the jaws or teeth in preplanned positions. Patients with craniofacial syndromes, for example moderately severe hemifacial microsomia with a rudimentary ramus on the affected side or those with severe maxillary deficiency as found in Apert or Crouzon syndrome, are prime candidates for distraction. The mandibular symphysis may also be widened by this procedure.
Adjunctive facial procedures: To improve the soft tissue contours beyond those attainable by orthognathic surgery, several adjunctive facial procedures can be employed. These include chin augmentation, rhinoplasty, implants for facial soft tissue contours, liposuction and platysma lift procedures. Injection of collagen or Botox™ tends to produce a temporary aesthetic improvement.
Postsurgical orthodontics and follow-up: Once adequate bone healing and a satisfactory range of mandibular movement has been achieved, the wafer is removed and light round archwires placed to allow occlusal settling. Light elastic traction is used to guide the teeth into the desired position and ensure that good interdigitation is achieved so the appliances can be removed within 6 months of surgery. This is followed by a retention regimen that usually follows standard fixed appliance therapy. Surgical follow-up should be for a minimum of 2 years.
Stability and relapse
In general, stability is enhanced and relapse minimised when:
• surgical and orthodontic plans are correct and realistic, well-integrated and executed competently
• surgical movement is modest – no greater than 5–6 mm vertically or anteroposteriorly in the maxilla or 8 mm in the mandible; does not place the soft tissues under tension and the condyles are not distracted at surgery
• aberrant soft tissue factors are absent (e.g. tongue thrust or previous surgical scarring, as may occur in repaired cleft palate) and lips are competent
• teeth have been placed in soft tissue balance and not extruded presurgically
• patient is compliant with all aspects of treatment, particularly postsurgical wear of elastic traction
10.7 Cleft lip and palate
Management of patients with cleft lip and palate is best undertaken in special centres. The general practitioner should, however, understand the timing and sequence of treatment for these patients and the importance of providing a high standard of preventive and routine dental care.
Aetiology
Whether a cleft occurs in isolation or as part of a syndrome, both genetic and environmental factors interact in its aetiology. A distinct family history exists in 40% of those with cleft lip (with or without palate involvement) and in 20% of those with cleft palate only. Environmental factors such as folic acid deficiency, maternal infections, nicotine, anticonvulsant drug therapy, aspirin and cortisone may act synergistically in a susceptible, genetically predisposed individual to promote clefting. Clefting of the lip and primary palate follows from failure of fusion of the medial nasal, lateral nasal and maxillary processes at around the sixth week of intrauterine life. Clefts of the secondary palate follow failure of fusion of the palatal shelves from 8–10 weeks. Elevation of the palatal shelves from a vertical to a horizontal position occurs later in females than males, allowing for more lateral facial growth, which possibly contributes to the greater prevalence of isolated cleft palate in females.
Classification: Several classification systems exist, but the cleft is easiest described as involving the primary (lip and alveolus to the incisive foramen) and/or secondary palate (hard palate from incisive foramen back and soft palate) as being unilateral or bilateral, complete or incomplete (Fig. 10.5). A submucous cleft may not be detected for some time as the overlying mucosa is unaffected, but it is usually noticed when speech development is poor.
Prevalence
Clefts of the lip and/or palate occur in 65% of all craniofacial deformities, with a prevalence of 1 in 750 live births for cleft lip and palate in Caucasians, and 1 in 2000 live births for isolated cleft of the secondary palate. Cleft lip and palate more frequently affects males and is more common on the left than on the right side, while females are more often affected by cleft palate alone. Occasionally the latter is a feature of other syndromes such as Pierre Robin, Treacher Collins and Down syndrome.
Common clinical features
• Both the maxilla and mandible tend to be retrognathic (particularly with cleft palate only) relative to non-cleft individuals; the maxillary position is partly attributable to growth restriction postsurgically.
• Upper facial height tends to be reduced but the lower facial height tends to be increased, with an excess freeway space.
• Class III skeletal relationship often results from the retrusion of maxilla and mandible but is aggravated by mandibular overclosure to allow posterior tooth contact.
Dental and occlusal features: On the side of the cleft, the following anomalies often exist:
• The lateral incisor is absent, of abnormal size and/or shape, hypoplastic or appears as two conical teeth on the medial and lateral side of the cleft.
• A supernumerary or supplemental tooth may be present on either side of the cleft.
• The central incisor is often rotated and tilted toward the cleft and may be hypoplastic, particularly in bilateral clefts.
Elsewhere in the mouth, tooth size tends to be smaller and eruption delayed, with a greater prevalence of hypodontia, enamel hypoplasia and abnormal tooth shape than in unaffected individuals.
A class III incisor relationship is common with a crossbite of one or both buccal segments and occasionally a lateral open bite.
Growth: Postsurgical scarring in those with cleft lip and palate restricts anteroposterior, vertical and transverse growth of the midface. These changes do not seem to occur to any significant extent in unrepaired clefts.
Hearing and speech: Where the cleft involves the posterior palate, the action of tensor palati on the Eustachian tube is impaired, often leading to hearing difficulties. This, in addition to palatal fistulae and adverse palatopharyngeal function, means that speech is often defective. Regular assessment of hearing and speech is essential before and during school years.
Care management
Care management is best co-ordinated in a specialised centre by a team usually comprising an orthodontist, speech therapist, health visitor and plastic, ear–nose–throat and maxillofacial surgeons. General dental care must be monitored regularly by a caring and interested general dental practitioner.
Neonatal period: Maternal support, with discussion of the potential of what current treatment offers, should be provided by designated individual(s) from the cleft team. Emphasis should also be placed on the importance of a high standard of dental care for later treatment. The mother must be instructed in feeding using special bottles and teats (e.g. Rosti bottle and Gummi teat). A specialised health visitor should be available for provision of ongoing advice and support.
Repositioning of the displaced cleft segments by removable appliances, often with extraoral strapping to facilitate surgical repair (presurgical orthopaedics), is now undertaken less frequently than before owing to its dubious benefits.
Lip closure is usually undertaken at around 3 months, with the Millard technique (often with modifications) adopted most commonly. The extent of alar cartilage dissection and the simulataneous use of the vomer flap are disputed. In bilateral clefts, both sides are now mostly repaired together but doing each side separately is still practised in some centres. Repair of the hard and soft palate is usually carried out between 9 and 12 months, most commonly by means of a von Langenbeck procedure. Delaying until at least 5 years, as practiced in some European centres, is inadvisable due to the detrimental effects on speech development.
Primary dentition: Preventive advice including dietary counselling and possibly provision of fluoride supplements is essential. Speech should be assessed formally at about 18 months and speech and hearing assessed regularly. Speech therapy can be instituted as necessary. Pharyngoplasty and/or lip revision may be required prior to starting school.
Mixed/permanent dentition: In preparation for alveolar bone grafting at 9–10 years of age, upper incisor(s) alignment and arch expansion is usually undertaken to facilitate access. Extraction of any primary teeth in the upper arch should take place at least 3 weeks prior to surgery to allow healing. Bone is harvested from the iliac crest or the chin, placed in the cleft site and the wound closed with keratinised flaps. The graft, in addition to allowing eruption of the permanent canine and space closure, supports the alar base and helps to close oronasal fistulae; in bilateral cases, it also stabilizes the premaxilla.
Once the permanent canine has erupted (~10–15% require exposure), further treatment usually involves centreline correction and space closure by mesial movement of the buccal segment teeth so that the canine replaces a missing or diminutive lateral incisor. The treatment plan should be finalised with input from a restorative colleague. Crowding should be relieved in the non-cleft quadrant if necessary and in the lower arch if orthodontic correction of the malocclusion is likely. Otherwise, lower arch extractions should be delayed until surgical correction of the malocclusion is planned.
Where gross midface retrusion is present in late teenage years, a Le Fort I or II surgical advancement is likely, with possible mandibular setback and/or genioplasty depending on the severity of the skeletal problem. Presurgical orthodontics proceeds along conventional lines (see Section 10.6). Rhinoplasty may be required as a later procedure to optimise the facial profile.
![]() Self-assessment: questions
Self-assessment: questions
Multiple choice questions (True/False)
a. Affects the upper permanent lateral incisors in 20% of cases
b. Affects lower second premolars more so than upper second premolars
c. Is more common in males than females
e. Of third molars can be determined definitively by 8 years of age
a. Occur in about 10% of the population
b. Are more common in females than males
3. Removal of a  deemed of poor prognosis in a class I (incisors and molars) malocclusion with generalised moderate premolar crowding where all other teeth are sound:
deemed of poor prognosis in a class I (incisors and molars) malocclusion with generalised moderate premolar crowding where all other teeth are sound:
a. Is advisable when the bifurcation of the  is calcifying, to maximise the potential for spontaneous correction of malocclusion in that quadrant
is calcifying, to maximise the potential for spontaneous correction of malocclusion in that quadrant
4. Extraction of cs may be indicated:
a. To allow spontaneous correction of potential crossbite on erupting 2s
b. To allow space to be created for an unerupted upper central incisor whose eruption has been inhibited by the presence of a supernumerary
c. To allow the lower incisors to drop lingually in a developing class III malocclusion
d. To encourage improvement in the position of a displaced 3
e. Along with bs in early mixed dentition to encourage space closure in children in whom 2s are absent
5. Extraction of a lower right first primary molar:
a. Is described as balanced when extraction of the upper left first primary molar is requested also
b. Is described as compensated when extraction of the lower left first primary molar is requested also
c. Should be compensated to prevent a centreline shift
d. Should be balanced to prevent overbite reduction
e. Should be requested if the crown of the tooth is submerged level with the gingival margin
6. A persistent thumb-sucking habit may produce:
7. Buccal displacement of 3/ may be contributed to by:
a. Represents inclination of the upper/lower incisors less than the mean for Caucasians
c. Results when lip pressure is higher than tongue pressure
9. Factors that may aggravate an already increased overjet include:
a. A persistent thumb-sucking habit
c. A bilateral buccal segment crossbite
10. Prognosis for stable correction of a 10 mm overjet in a 12-year-old female patient with normal overbite is enhanced when:
a. The underlying anteroposterior skeletal pattern is class I
b. There is a backward pattern of mandibular growth
c. The lower lip lies under the upper incisors post-treatment
11. A functional appliance for correction of a class II division 1 malocclusion:
a. Works by maintaining the mandible in its rest position
b. Is least effective during active growth
c. Is ideal for treating irregularities in tooth alignment
d. Requires 14–16 hours per day wear to be effective
e. Requires post-treatment retention until growth has ceased
12. Deep overbite in class II division 2 malocclusion is associated with:
a. A reduced interincisal angle
c. Normal cingulum thickness on the upper incisors
13. Relative to class I malocclusion, cephalometric features of class III malocclusion may include:
b. A more posterior position of the glenoid fossa
c. A reduced mandibular length
14. An anterior open bite may be caused by:
a. A low Frankfort mandibular planes angle
b. An endogenous tongue thrust
15. A buccal crossbite on 5/ may result from:
16. In a 30-year-old adult male patient:
a. Overbite reduction is generally easier than in an adolescent
b. Molar extrusion is the approach of choice for overbite reduction orthodontically
c. Lighter forces are desirable for tooth movement if the dentition is periodontally compromised
d. Anchorage demands may be less if teeth have been lost
e. Significant skeletal discrepancies may be addressed by growth modification
17. Factors associated with dental and/or skeletal relapse following mandibular advancement osteotomy include:
a. Mandibular advancement greater than 8 mm
b. Condylar distraction during surgery
18. Common dental anomalies in a 10-year-old child with a left unilateral cleft of lip and palate include:
19. Alveolar bone grafting in patients with cleft lip and palate:
Extended matching items questions
For each of the clinical problems (a–e), select from the list below (1–13) the most appropriate course of action (more than one may be correct). Each item can be used once, more than once or not at all.
1. Removal of lower second primary molars after eruption of the permanent lateral incisors.
2. Early removal of the associated upper primary canine.
3. Retention of a lower second primary molar.
4. Observe but take no specific action.
6. Carry out a balancing extraction.
7. Extraction of the same tooth type in contralateral quadrants.
8. Autotransplant a lower premolar.
9. Prescribe a radiograph to check if a supernumerary tooth is present.
10. Upper permanent incisor proclination with an upper removable appliance.
11. Fit an upper removable appliance space maintainer.
12. Extraction of the upper left second primary molar.
13. Prescribe a dental panoramic tomogram and an upper anterior occlusal radiograph.
a. A 9-year-old boy with class I incisor and molar relationships who has large carious lesions in the upper left and lower right first permanent molars (all permanent teeth are developing on a dental panoramic tomogram).
b. A 10-year-old girl with a class II division 2 malocclusion where the upper right permanent canine is not palpable buccally; subsequent radiographic assessment reveals the tooth to overlap less than half the width of the upper right permanent lateral incisor and to be located at the mid-third of its root; the long axis of the unerupted right maxillary canine is <30° to the midsagittal plane.
c. An 18-year-old girl with a class III malocclusion and generalised mild crowding who is not keen to proceed with fixed appliance orthodontic treatment; a single conicle supernumerary is identified radiographically well above the apices of the upper incisors.
d. A 9-year-old boy with the upper permanent incisors fully erupted and a median diastema of 4 mm.
e. An 8.5-year-old girl presents with caries on the medial aspect of the upper left first permanent molar which is impacted into the upper left second primary molar producing resorption of half the width of its distobuccal root resulting in pain.
Case history questions
An 8-year-old girl presents with her mother, who is very concerned about her daughter’s large (5 mm) upper median diastema.
Case history 3
A 7-year-old boy presents with 1/1 in crossbite but otherwise has features of a class I malocclusion.
1. What is the possible aetiology of the crossbite?
2. When is early treatment advisable?
3. What factors must be considered regarding treatment possibilities?
4. List the desirable features in the design of an upper removable appliance to correct the incisor relationship.
Picture questions
Figure 10.6 is a radiograph.
Picture 4
Figure 10.9 is a dental panoramic tomogram.
2. What factors may account for this?
3. How would you aid localisation?
4. What interceptive method may have helped to avoid this problem developing?
5. What factors determine whether orthodontic alignment is possible?
Picture 6
Figure 10.11 shows the frontal view of a 22-year-old female who presented for orthodontic treatment with an obvious facial anomaly, which she reported to be gradually worsening.
1. What obvious facial anomaly is present?
2. What investigation is shown in Figure 10.12? What does this show?
 are calcifying (aged approximately 8.5–9.5 years) and moderate premolar crowding is present.
are calcifying (aged approximately 8.5–9.5 years) and moderate premolar crowding is present.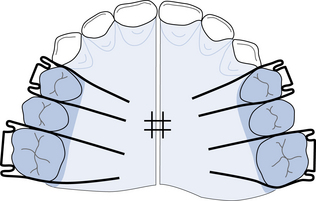
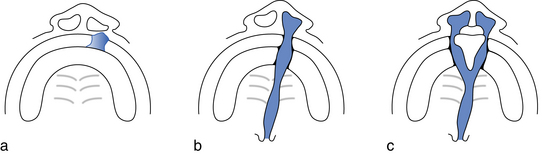







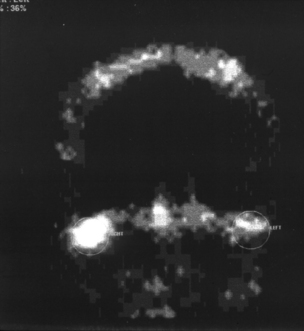
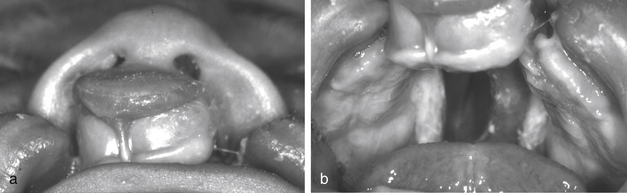
 is calcifying.
is calcifying. as all other teeth are sound; however, an extraction
as all other teeth are sound; however, an extraction
 s may be considered to facilitate lingual movement of a lower incisor that is being displaced labially by a crossbite relationship with the upper incisor teeth, or of the whole lower labial segment lingually in a class III malocclusion.
s may be considered to facilitate lingual movement of a lower incisor that is being displaced labially by a crossbite relationship with the upper incisor teeth, or of the whole lower labial segment lingually in a class III malocclusion. ,
, most commonly. Management involves acceptance of the transposition if it is complete, extraction of the most displaced tooth if crowding is present or orthodontic alignment where sufficient space exists in the arch. The apical positions of the transposed teeth will determine whether alignment is carried out with the teeth in their transposed positions or if these can be corrected.
most commonly. Management involves acceptance of the transposition if it is complete, extraction of the most displaced tooth if crowding is present or orthodontic alignment where sufficient space exists in the arch. The apical positions of the transposed teeth will determine whether alignment is carried out with the teeth in their transposed positions or if these can be corrected.