Orthodontics III
appliances and tooth movement
Overview
Central to the success of any orthodontic treatment is selection of the appropriate appliance and competence in its handling. It is, therefore, necessary to be aware of the scope and limitations of each appliance system and the care required with its use.
In this chapter, removable, fixed, functional and headgear appliances are discussed. Histological aspects of tooth movement are then addressed and the factors that must be considered in planning retention are presented.
11.1 Removable appliances
Aside from clear vacuum-formed thermoplastic appliances that may be used in the upper and lower arches, removable appliances consisting primarily of wire and acrylic components are used almost exclusively in the upper arch. Lower appliances of the latter components are poorly tolerated because of encroachment on tongue space and the difficulty in achieving satisfactory retention due to the lingual tilt of the molars; they are, however, usually used for the sole purpose of retention post-treatment. Clear thermoplastic appliances may also be used in either arch as retainers; they are also capable of minor tooth alignment and have gained acceptance by adults for this purpose. Although functional appliances are also composed of wire and acrylic, they have a different mode of action and are dealt with in Section 11.3.
Indications for removable appliance therapy
In the contemporary management of malocclusion, the role of ‘traditional’ removable appliances composed of wire and acrylic is much more restrictive than it has been formerly; a greater awareness of their limitations and the widespread use of fixed appliances account mainly for this. Removable appliances, however, may be considered in the following situations:
• Where tilting movement of teeth is desirable and acceptable.
• To maintain space in the mixed or early permanent dentition.
• To help to transmit forces to groups of teeth, e.g. for arch expansion or distal movement of buccal segments (possibly with intrusion); extraoral traction may be applied quite easily to the appliance to produce the latter movements.
• To free the buccal occlusion and facilitate crossbite correction or other tooth movement.
• To produce overbite reduction.
• As an adjunct to fixed appliance treatment.
• As a retainer following removable or fixed appliance treatment.
Designing a removable appliance
Some important points should be remembered in relation to appliance design for those that involve acrylic and wire components:
• Always design the appliance with the patient in the dental chair; this helps to avoid design errors.
• Keep the design as simple as possible: aim to carry out a few tooth movements with each appliance.
• Use the acronym ARAB to help to design the appliance in a logical sequence, ensuring nothing is overlooked: A, activation; R, retention; A, anchorage; and B, base plate.
Springs: The force (F) delivered by a spring is expressed by the formula F α dr4/l3, where d is the deflection of the spring when activated, r is the radius of the wire and l is the length of the spring. Radius and wire length, therefore, have most effect on wire stiffness.
Retention component: The retention component maintains the appliance in the mouth, and it is generally advisable to have the clasps located to optimise retention. The following components are commonly used.
Adams’ clasp: Retention is achieved by the arrowheads, which engage about 1 mm of the mesial and distal undercuts on the tooth. This clasp is the most common means of gaining posterior retention. For molars, 0.7 mm wire is used, but 0.6 mm wire is advisable for premolars and primary molars. The clasp is easily modified to incorporate two teeth for retention, hooks for elastic traction or soldered tubes for extraoral anchorage. To move the arrowhead towards the tooth and to engage more gingivally, adjustment should be made in the middle of the flyover; otherwise close to the arrowhead is all that may be necessary.
Southend clasp: This 0.7 mm clasp is recommended anteriorly with the U-loop engaging the undercut between the incisors. Pushing the loop towards the base plate is the only adjustment usually required.
Long labial bow: This bow is constructed from 0.7 mm (0.8 mm if designed with reverse loops) wire and is useful in preventing buccal drifting of teeth during mesial or distal movement. Alternatively it may be fitted to the teeth as a retainer.
Adjustment depends on the design, but for a U-looped bow it is usual to squeeze the legs of the U-loop, followed by an upward adjustment anteriorly to restore its optimal vertical position.
Anchorage: Anchorage is the resistance to the force of reaction generated by the active components and is best thought of in terms of the available space for the intended tooth movement. The anchorage demands should be assessed before treatment commences and may be classified as:
• low: where the space from an extraction will provide excess space to achieve the desired result. Revision of the treatment plan would seem advisable, or methods used to encourage space closure
• moderate: where some residual extraction space is likely to remain following the intended tooth movement but this should be kept under surveillance during the treatment period
• high: where all the space from an extraction is needed to align the remaining teeth or reduce an overjet; anchorage must be reinforced from the start of treatment
• very high: the extraction space will not allow successful achievement of the desired tooth movement and either additional extractions and/or extraoral traction is required to gain further space. The treatment aims may need amendment.
Patients for whom anchorage demands are high or very high are best treated by a specialist.
The anchorage demands are influenced by the following:
• How many teeth are being moved and the intended final tooth positions: greater demand is placed on anchorage when several teeth, rather than one tooth, are being moved and when the intended final tooth position requires teeth to be moved large distances.
• The force applied: greater forces place greater demand on anchorage; bodily movement requires greater force (~100–150 g) than tipping movement (~30–60 g) and hence the former is more ‘anchorage straining’.
• The root surface area (RSA): teeth with larger RSA or a block of teeth with a large RSA will resist anchorage loss more than those with a smaller RSA.
• Mesial drift tendency: this is greater in the upper than in the lower arch.
• Frankfort mandibular planes angle (FMPA): space loss is easier with increased than with reduced FMPA which may be related to the different musculature associated with each facial form.
• Occlusal interdigitation: where this is good, mesial drift is less likely.
Intraoral reinforcement of anchorage: Anchorage may be reinforced:
• intramaxillarily using teeth in the same arch by incorporating the maximum number of teeth in the anchor unit or by making bodily movement only possible for the anchor teeth; palatal or lingual arches link molar teeth across the arch which increases RSA of the anchor unit to resist mesial movement of the molars
• by mucosal coverage: the palatal coverage of the base plate provides greater anchorage in removable than in fixed appliances
• intermaxillarily using teeth in the opposing arch; this is not recommended with removable appliances as elastic traction tends to displace the appliance, but it is suitable with fixed appliances, the direction of the elastic traction depending on the malocclusion: class II traction pulls backward on the upper labial segment and forward on the lower buccal segment; class III traction pulls forward on the upper molars and backward on the lower labial segment
• using temporary anchorage devices (TADs): the placement of temporary bone screws or mini-plates; these are used in conjunction with fixed appliances (see Section 11.2).
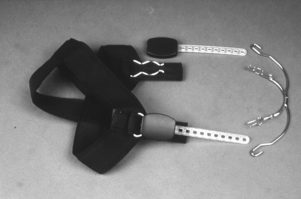
Extraoral reinforcement of anchorage: Headgear may be used to pull upward and backward on a facebow attached to an upper removable, upper fixed or functional appliance, against the cranial vault. Forces of 200–250 g for 10–12 hours per day are needed. If distal molar movement is required, extraoral traction is necessary with forces of 400–500 g for 14–16 hours or more per day.
Safety with headgear: Safety is a priority because of the potential hazards to the eyes and face. Two safety mechanisms must be fitted to each headgear assembly, preferably a facebow with locking device (e.g. Ni Tom®) and a safety release spring mechanism attached to the headcap. Verbal and written instructions must be issued to the patient and parent or guardian emphasising that:
• the headgear is only to be assembled and removed in the way demonstrated by the orthodontist
• no horseplay is permissible when the headgear is attached
• if the headgear ever comes out at night, discontinue wear and contact the orthodontist as soon as possible
• if it ever damages the face or eyes, contact the local hospital immediately; discontinue wear and contact the orthodontist.
Base plate: The base plate connects the other components of the appliance and may be passive or active.
Anterior bite plane: An anterior bite plane is required when overbite reduction is necessary or when removal of an occlusal interference is required to allow tooth movement. Three essential elements must be addressed:
• The bite plane should be flat: if inclined, it may procline or retrocline the lower incisors.
• It must have sufficient extention posteriorly to contact the lower incisors; to ensure this, a measurement of the overjet (+3 mm) should be forwarded to the laboratory at the time of appliance fabrication.
• It should separate the molar teeth by about 2 mm; it will be necessary, in most cases, to add cold-cure acrylic to the flat anterior bite plane during treatment to continue overbite reduction.
Posterior bite planes: Posterior bite planes are required to remove occlusal interferences and facilitate tooth movement when overbite reduction is unnecessary. This is commonly the case when correcting a unilateral buccal crossbite with mandibular displacement or an incisor crossbite. The acrylic coverage should be just sufficient to disengage the occlusion but must be adjusted to give even contact of the posterior teeth. The bite planes should be removed when the malocclusion is corrected and the appliance should then be worn as a retainer while the posterior occlusion settles.
Common tooth movements required
Table 11.1 summarises the common desired tooth movements and the active components to achieve these. Box 11.1 describes the technique involved in fitting a removable appliance.
Table 11.1
Common tooth movements and related active components
| Tooth movement required | Component and wire diameter | Activation |
| Retraction of 3 buccal | Buccal canine retractor: 0.5 mm sleeved with coil or 0.7 mm with U-loop | For 0.5 mm spring, bend anterior leg about 2–3 mm around the round beak of a spring-forming plier For 0.7 mm spring, cut 1 mm of wire from the free end, ensuring that the spring is curved into contact with the mesial surface of the canine |
| palatal | Palatal finger spring 0.5 mm | Ensure that spring is just above the gingival margin on the tooth and that movement tangential to the point of contact will keep the tooth in the line of the arch Bend in the free arm in the area between the coil and guardwire Half tooth width for single rooted teeth (3 mm) |
| Buccal movement of 4, 5 or 6 | Single tooth: T-spring, 0.5 mm Two or more teeth: screw |
Pull spring away from the base plate ~2 mm and at 45° to direction of desired movement Instruct the patient to turn screw once or twice per week |
| Palatal movement of single tooth other than 3 | Buccal retractor either 0.5 mm sleeved with coil or 0.7 mm with U-loop | As per buccal canine retractor but activation may be greater or less depending on root surface area of the tooth |
| Distal movement of upper first permanent molar (FPM) | 0.6 mm palatal finger springs to retract banded FPMs | 1–2 mm activation of springs, with headgear worn 12–16 hours per day with a force 200–250 g per side Must fit with two safety mechanisms (e.g. ‘Ni Tom®’ facebow and ‘Snap-away’ headcap) |
| Proclination of incisors | Z-spring 0.5 mm Double cantilever springs 0.6/0.7 mm Screw appliance |
Pull the spring 1–2 mm away from the base plate at ~45° angle to direction of wanted movement As for Z-spring Instruct patient to turn screw one or two turns per week |
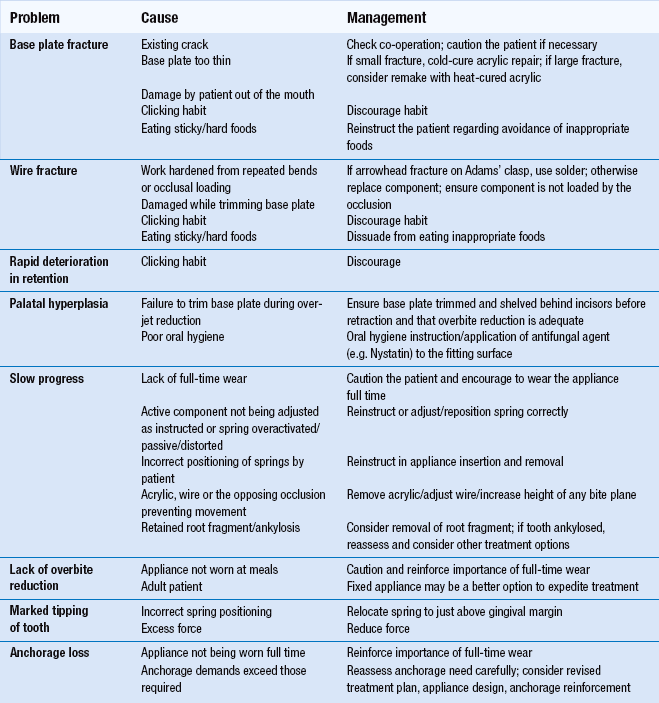
Managing problems during treatment
Problems that arise commonly during treatment are listed in Table 11.2 together with the most likely causes and necessary treatment.
Clear aligner therapy
This form of treatment involves creating a series of aligners (clear vacuum-formed thermoplastic appliances). Scanned dental casts are used to create a digital model to which small changes are then made to produce a stereolithographic cast on which the aligner is made. Subsequent incremental changes to the digital model are used to produce a matching series of altered casts for construction of a sequence of aligners. Currently, these appliances have been shown to perform well, particularly in adults, in the following circumstances: mild-to-moderate crowding in conjunction with interproximal stripping or expansion; lower incisor extraction for severe crowding; closure of mild-to-moderate spacing; posterior dental expansion; and intrusion of one or two teeth. Severely rotated canines and premolars, high canines, overbite reduction by relative intrusion and molar uprighting do not lend themselves to correction by these appliances. In conjunction with fixed attachments, however, it is possible to extend their use to closure of premolar extraction spaces, extrusion of incisors and molar translation.
These are fitted active following construction on a model to which minor tooth movement has been made. Further activation can be brought about by creating a divot in the aligner using a special plier heated to the correct temperature or by adding hard plastic bumps that snap into the aligner.
11.2 Fixed appliances
A fixed appliance is attached to the teeth.
Components
The appliance is composed of three elements: the attachments (brackets/bonded molar tubes/bands, the archwires and the accessories.
Brackets, bonded molar tubes and bands: It is becoming increasingly popular to place bonded attachments (brackets and molar tubes) on all teeth. Currently this is mostly undertaken using composite resin following acid etching of the enamel although self-etching primers (SEPs; which combine etchant and primer to avoid the need to wash the etchant away) may also be used. Resin-modified glass ionomer cements, which release and uptake fluoride in an attempt to prevent enamel demineralisation, are also available. These newer systems, however, are not as popular as the two-stage etch and prime systems due in part to reports of associated higher bond failure rates. Adhesive precoated brackets, claimed to minimise excess composite to save on clean-up time and give a more consistent bond, are also available.
The bonded brackets and molar tubes allow the teeth to be directed by the active components comprising the archwire and/or accessories. Brackets may be made from stainless steel, titanium, polycarbonate, ceramic or a combination of polycarbonate/ceramic. Molar tubes are made from stainless steel or titanium. Ceramic brackets are more aesthetic than metal but have disadvantages. They are hard and brittle so may wear the opposing teeth, increase friction with the archwire and can cause enamel fracture at debond due to the strong bond to the adhesive (common with the early-marketed types). These latter problems have now been overcome by a polycarbonate base on a ceramic-faced bracket with a metal insert in the bracket slot.
Despite the trend to use bonded tubes instead of bands on molars, bands are particularly indicated for the upper molars especially if headgear or a palatal arch is being used. Other indications include teeth with short clinical crowns, as placement of bonded attachments is difficult, and teeth with repeated bond failure. Bands are usually cemented using a glass ionomer cement. Separation of the teeth, commonly with elastomeric rings, is required for up to 1 week to facilitate band placement and guarantee best fit.
Archwires: Archwires may be round or rectangular.
With its easy formability, good stiffness and reasonable cost, stainless steel is the most popular archwire material; however, nickel–titanium, cobalt–chromium and beta-titanium – all with greater flexibility than stainless steel – have gained increasing popularity in contemporary practice. Nickel–titanium has two unique properties – shape memory and superelasticity – that relate to phase transitions between the martensitic and austenitic alloy forms. Even with a large deflection, a relatively constant low force is applied, making these archwires an excellent choice for initial alignment. They are, however, more expensive than stainless steel archwires, which because of the properties given above, are especially suitable later in treatment.
Cobalt–chromium alloy (Elgiloy) may be shaped while in a soft state and then hardened by heat treatment.
Beta-titanium has excellent strength and springiness, midway between nickel–titanium and stainless steel, making it ideal for intermediate and finishing stages of treatment.
Elastics, elastomeric modules/chain/thread, wire ligatures: Latex elastics produced for orthodontic purposes may be used for intra- or intermaxillary traction. A range of sizes is available. Elastomeric modules are used to maintain an archwire in an edgewise bracket slot (see below) while elastomeric chain or thread may be used to move teeth along an archwire, or for derotation. Stainless steel wire ligatures continue to be used particularly when maximum contact is desired between the wire and the bracket slot or to maintain space closure.
Indications for fixed appliances
Anchorage control
Because the palate is not covered by a base plate, anchorage control is more critical with a fixed than with a removable appliance. In addition, bodily rather than tipping movement places greater strain on anchorage.
Anchorage may be reinforced by:
• increasing the anchorage unit by bonding more teeth and ligating them together
• preventing forward tipping of the molars by anchor bends in the archwire (placed between premolar and molar at 30° to the occlusal plane)
• placing torque in the archwire ensuring that the anchor teeth can only move bodily, thereby increasing resistance to unwanted movement; a twist is placed in the plane of the wire so that on insertion in a rectangular bracket slot, it exerts a buccolingual force on the root apex
• palatal and/or lingual arches: prevent molar tipping
• intermaxillary traction (see Section 11.1): as well as reinforcing anchorage, the incisor relationship (either increased or reverse overjet) may be corrected
• placement of a TAD; may be an implant, mini-plate attached with screws to maxillary or mandibular basal bone or a screw in the alveolus
• extraoral means, including reverse headgear (see Sections 10.4 and 11.1).
Appliance types
Preadjusted appliances: The preadjusted edgewise appliance uses an individual bracket with a rectangular slot for each tooth to give it ‘average’ tip, torque and buccolingual position and to allow the placement of flat archwires; some individual adjustment bends, however, are often required to the wire to compensate for these ‘average’ values. 0.018 and 0.022 systems (which describes the bracket slot width in inches) exist and bracket prescriptions by Andrews, Roth and MBT are available. Round flexible wires are used for initial alignment and rectangular wires are required for precise apical control. Clinical time is saved and good occlusal results are achieved consistently with these appliances but costs are increased due to the need for an individual attachment per tooth.
Tip-edge appliance: This uses special brackets with rectangular slots and was developed from the Begg appliance to overcome some of its deficiencies. That appliance system uses a bracket with a vertical slot and round wires exclusively held in place loosely with brass pins. Tipping movement is facilitated and auxiliaries are necessary for rotational and apical movement. With the Tip-edge appliance, although round wire is used for most of the treatment as with the Begg technique, the facility exists to place rectangular wire in the final stages, affording greater control of tooth positions.
Lingual appliance: Brackets are bonded to the lingual or palatal surfaces of the teeth and specially configured archwires are used. Recent advances include the construction, from laser scans of the study models, of customised precious metal pads to which low-profile brackets are attached, and the use of computer-controlled wire bending devices to individualise archwire fabrication.
Self-ligating appliances: These remove the need for elastomeric or stainless steel wire ligation of the archwire to the bracket. Available systems include Damon®, Speed® and Smartclip®. Because the archwire is not pressed firmly against the base of the bracket, as is the case with use of an elastomeric module or wire ligature, friction is reduced. Claims that overall treatment time is significantly shorter than with conventional preadjusted edgewise appliances have not been upheld.
Appliance management: An excellent standard of oral hygiene is essential prior to and during fixed appliance treatment. All patients must be instructed specifically in relation to diet and optimal oral hygiene practices following placement of the appliance to minimise the risk of enamel demineralisation. Mucosal ulceration is common in the early stages of treatment and it is wise to give the patient some soft ribbon wax to place over any components that are causing minor trauma. Adjustment visits are usually at intervals of 4–6 weeks. Repairing fixed appliances occupies more chair-side time than does removable appliances. Some discomfort is normal for a few days following adjustment and is usually overcome by mild analgesics.
11.3 Functional appliances
Functional appliances correct malocclusion by using, removing or modifying the forces generated by the orofacial musculature, tooth eruption and dentofacial growth.
Mechanism of action
How functional appliances work is not completely understood. They are generally devoid of active components, such as springs, and are incapable of moving teeth individually. Instead, they operate by applying or eliminating forces that are generated through the facial and masticatory musculature and by harnessing those that occur through natural growth processes. They are, therefore, only effective in growing children, preferably just prior to their pubertal growth spurt.
The specific force system set up by any appliance will depend on its particular design. Essentially, forces are developed by posturing the mandible – either downward and forward in class II or downward and backward in class III. This applies intermaxillary traction between the arches, as can be produced by elastics with fixed appliances. As the scope for posturing the mandible backward is far less than for posturing it forward, functional appliances are more successful in, and are indicated almost exclusively for, class II malocclusion. For this reason, the possible mechanisms of action will only be considered for class II malocclusion. In these cases, the result is a forward tipping of the lower incisors and the entire mandibular dentition, with acceleration of mandibular growth, as well as a backward tipping of the upper incisors and restraint of maxillary growth. Overall mandibular growth is modified – the total amount is unaffected but the expression of growth is altered.
Indications
Where used for correction of class II malocclusion, the following should ideally be present:
• Patient should be actively growing, preferably just prepubertal.
• Mild-to-moderate skeletal class II owing to mandibular retrusion.
• Lower incisors upright or slightly retroclined; proclined lower incisors usually contraindicates functional appliance therapy.
In most cases, a further phase of fixed appliances is required to detail the occlusion. In moderate class II malocclusion with crowding, this may involve extractions also (see Section 10.1). In more severe cases, the prospect of successful correction of the malocclusion by functional appliance therapy alone is limited (~20–30%); if this is undertaken, the likely need for subsequent extractions and fixed appliances or even combined surgical–orthodontic treatment should be explained.
Practical management of patients with a functional appliance
Box 11.2 outlines the general steps involved in using a functional appliance. The orthodontist must be confident about the ability of the appliance to work and relay this enthusiastically to both the patient and parent.
Types of functional appliance
The following account describes some standard functional appliances. However, current thinking regarding design is to ‘pick and mix’ the components that are necessary for the specific correction of a particular malocclusion. Such a ‘components approach’ to design requires considerable insight into the working of these appliances which necessitates specialist knowledge and expertise. Functional appliances may be removable or fixed, tooth borne or tissue borne.
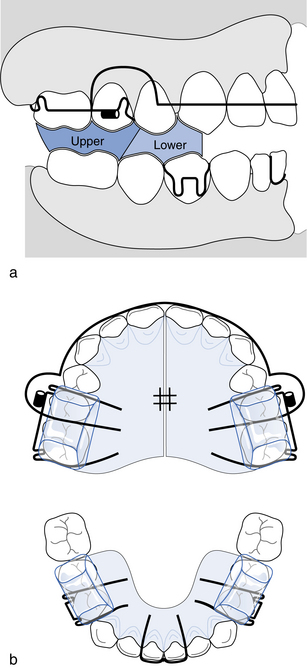
Twin-block appliance: The twin-block appliance consists of upper and lower appliances incorporating buccal blocks, with interfacing inclined planes at 70° that posture the mandible forward on closure (Fig. 11.1; the labial bow on the upper appliance is optional). The construction bite is taken with the mandible postured forward, ideally to an edge-to-edge incisor relationship and open 2–3 mm (some operators recommend 5–6 mm). Full-time wear is facilitated by the two-part design. Where the mandible needs to be postured further forward during treatment to reactivate, acrylic may be added to the inclined bite planes. When the overjet is corrected, trimming of the upper buccal blocks or a modified retainer with a steep anterior inclined plane is required to close the lateral open bites that develop, especially evident where the overbite is deep to start with. Variants for treatment of class II division 2 and class III malocclusions also exist.
Herbst appliance: This fixed-functional appliance consists of splints cemented to the upper and lower buccal segment teeth connected by a rigid arm to posture the mandible forward. Although costly and subject to breakages, speaking and eating are reported to be easier than with the twin-block.
Bionator: A labial bow is extended back to hold the cheeks out of contact with the buccal segment teeth and allow arch expansion, while a thick palatal loop takes the place of acrylic. Full-time wear is advisable except for meals.
Medium opening activator: Particularly useful where deep overbite correction is required, this appliance has molar clasping, a palatal base plate, acrylic extensions lingual to the lower incisors and no buccal capping; acrylic struts link the upper to the lower and the lower buccal segment teeth have scope to erupt. Full-time wear with the usual exceptions is possible.
Frankel appliance: Originally termed a ‘function regulator’, this has particular use in the management of abnormal soft tissue pattern, for example hyperactive mentalis muscle. Buccal shields hold the cheeks away from the teeth and stretch the mucoperiosteum at the sulcus depth, intending to expand the arches and widen the alveolar processes. There are three types: FR 1 for class I and class II division 1 malocclusions; FR 2 for class II division 2 malocclusion; and FR 3 for class III malocclusion. Wear is built up over the first weeks until full-time, apart from sports and while eating. Frankel appliances are complex in design, expensive to make and repair and easy to damage and distort. They can, however, be reactivated by sectioning the buccal shields and repositioning them forward.
Headgear addition to functional appliances: In cases where maximal anteroposterior and vertical maxillary restraint is desirable, occipital-pull headgear may be added to tubes incorporated in the acrylic or soldered to the clasp bridges. Forces of about 500 g should be used for 14–16 hours per day and the usual headgear safety precautions and instructions should be followed (see Section 11.1). If the FMPA is increased, molar capping is essential to promote a closing rotation of the mandible and prevent molar eruption, thereby facilitating an increase in overbite. The addition of high-pull headgear to the appliance will facilitate this process.
Effects of functional appliances
For class II malocclusion with deep overbite:
• Retroclination of the upper incisors and proclination of the lower incisors are usual, although the latter is not found consistently and is best minimised by placing acrylic capping on the lower anterior teeth.
• Inhibition of lower incisor eruption and promotion of eruption of the posterior teeth leads to levelling of the curve of Spee. This process is facilitated by lower incisor capping on the appliance.
• Guidance of eruption of the lower posterior teeth in an upward and forward direction while preventing eruption and forward movement of the upper posterior teeth encourages correction of a class II buccal relationship.
• Arch expansion is intended through the buccal shields of the Frankel appliance, the buccal wire of the Bionator or by adjustment of the midline screw of the twin-block.
• Enhancement of mandibular growth is brought about by movement of the mandibular condyle out of the fossa, promoting growth of the condylar cartilage and forward migration of the glenoid fossa. This effect is very variable.
• Restraint of forward maxillary growth.
• An increase in lower facial height is mediated by the alterations in the eruption of the posterior teeth, as described above.
These skeletal effects only account for a small portion of the treatment effects even when efforts are made to limit the amount of tooth movement. The skeletal changes, produced by early mixed dentition treatment by these appliances, appear to be diminished or lost by subsequent growth. For most class II children, early treatment by functional appliances has been shown to be no more effective than later treatment undertaken in the permanent dentition. The primary indication suggested, however, for early class II treatment by a functional appliance is a child with psychosocial problems due to dentofacial appearance (see Section 9.4 and 10.1). The limited indications, use and effects of functional appliances in class III malocclusion are dealt with in Section 10.4
11.4 Orthodontic tooth movement and retention
Orthodontic tooth movement
The biological response to a sustained force is determined mainly by the force magnitude and duration, which generate zones of pressure and tension within the periodontal ligament, their extent and location depending on the intended movement.
Pressure zones: The cellular response relates to whether a light or heavy force is applied. With a light sustained force, movement occurs within a few seconds as periodontal ligament fluid is squeezed out and the vascular supply is compressed, setting off a complex biochemical response. Osteoclastic invasion occurs within 2 days and frontal resorption follows.
When a heavy sustained force is applied, the periodontal ligament is compressed to such a degree that the blood flow is cut off completely, producing an area of sterile necrosis (hyalinisation). Small zones of hyalinisation are inevitable even with light forces, but the area of hyalinisation is extended with forces of greater magnitude. Osteoclastic differentiation is impossible within the necrotic periodontal ligament space but, after several days, osteoclasts appear adjacent to and within the adjacent cancellous spaces. From there, they invade the bone adjacent to the hyalinised area and tooth movement eventually occurs by undermining resorption.
Tension zones: Following initial application of a light force, the blood vessels vasodilate and the periodontal ligament fibres are stretched, while fibroblast and preosteoblast proliferation occurs. The stretched fibres become embedded in osteoid, which later mineralises. The normal periodontal ligament width is eventually regained by simultaneous collagen fibre remodelling.
With heavy forces, rupture of blood vessels and severing of the periodontal ligament fibres are likely, but these are restored with the remodelling processes.
Mechanisms of tooth movement: Although the histological response to an applied orthodontic force has been investigated extensively, the mechanism by which a mechanical stimulus effects a cellular response is complex and at present unclarified. It is likely that vascular changes in the periodontal ligament in areas of pressure and tension, electrical signals generated in response to flexing of alveolar bone following force application, prostaglandins and cytokine release interact in the process.
Types of tooth movement, force magnitude and duration: Although it was previously thought that tipping of a single-rooted tooth (Fig. 11.2) occurred about a point almost midway along the root, rotation now appears to take place near the apical third within an elliptically-shaped area. Half of the periodontal ligament is stressed, with maximum pressure created at the alveolar crest in the direction of movement and at the diagonally opposite apical area. For bodily movement and rotation, a force couple must be applied, loading uniformly the whole of the periodontal ligament in the direction of translation so both crown and root move in the same direction by equal amounts (Fig. 11.3). With extrusion, all of the periodontal ligament is tensed, but when a tooth is intruded, the force is concentrated at the apex. An element of tipping is unavoidable with extrusion, intrusion and rotation.
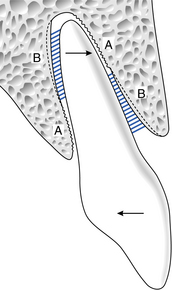
Fig. 11.2 The effect of tipping movement.
A = area of periodontal ligament compression/alveolar bone resorption; B = area of periodontal ligament tension/alveolar bone deposition.
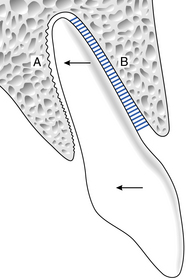
Fig. 11.3 The effect of bodily movement.
A = area of periodontal ligament compression/alveolar bone resorption; B = area of periodontal ligament tension/alveolar bone deposition.
For tooth movement to occur optimally, the force per unit area within the periodontal ligament should ideally not occlude the vascular supply yet be sufficient to induce a cellular response. A force should, therefore, be as light as possible for the movement intended, taking into account the root surface area over which it is spread. Optimal force ranges for various tooth movements are:
Although tooth movement can occur in response to heavy forces, these should not be applied continuously; intermittent application may be clinically acceptable. Not only must a force be of sufficient magnitude to effect the movement desired, but it must also be sustained for sufficient time. For successful movement, a force must be applied for about 6 out of 24 hours, and continuous application of light forces is optimal. This is favoured, because control of tooth movement and anchorage is facilitated while the risks of pulpal and radicular damage are minimised. Excessive mobility is avoided and movement is more efficient with less discomfort. Movement of the order of 1 mm in a 4-week period is regarded as optimal, with faster progress recorded in children than in adults. This is largely a consequence of the greater cellularity of the periodontal ligament, more cancellous alveolar bone and faster tissue turnover in a growing patient, which ensure a more rapid response to an applied force.
Undesirable sequelae of orthodontic force
Pulpal damage: A mild pulpitis following initial force application is common, but has no effect long term. Where the apical blood vessels are severed by the use of heavy continuous force or by injudicious root movement through the alveolar plate, pulp death is likely, although this is usually associated with previous trauma.
Root resorption: Areas of cementum resorbed during tooth movement are usually repaired. Some permanent loss of root length is found, however, on nearly all teeth following bodily movement over long distances. The maxillary incisors, then the mandibular incisors and first permanent molars, are primarily affected. Fortunately, in most instances, loss of 0.5–1.0 mm of root length is of no long-term significance. Suggested risk factors include: root resorption before treatment, a history of previous trauma, roots that are pipette-shaped, blunt or demonstrate a marked apical curvature, use of excessive forces and apical contact with cortical bone. Genetic risk factors are also involved. Recent evidence indicates that comprehensive orthodontic treatment increases the severity and incidence and that heavy forces produce most root resorption.
Loss of alveolar bone height: With fixed appliance treatment, 0.5–1 mm loss of crestal alveolar height is common, with the greatest loss occurring at extraction sites. In the presence of good oral hygiene, this appears of little concern.
Pain and mobility: Even with appropriate force magnitude, ischaemic areas develop in the periodontal ligament after activation of an orthodontic appliance, leading to mild discomfort and pressure sensitivity. These usually last for 2–4 days and return when the appliance is reactivated. Some increase in mobility is common, as the periodontal ligament space widens and the fibres reorganise in response to the applied force. With heavy orthodontic forces, however, the likelihood of almost immediate onset of pain and marked mobility is increased, as the periodontal ligament is crushed and further undermining resorption occurs.
Retention
Following tooth movement, a period of retention is usually required to hold the teeth passively, preventing them returning to their pre-treatment position while the periodontal fibres and alveolar bone adapt to their new locations. The retention phase should be planned and discussed fully with the patient before treatment starts. The following factors are likely to destabilise the final result.
Forces from the supporting tissues: Reorganisation of the principal periodontal ligament fibres and supporting alveolar bone occurs within 4–6 months, but at least 7–8 months is required for the supracrestal fibres to reorganise because of the slow turnover of the free gingival fibres. Rotational correction is, therefore, liable to relapse, but this tendency may be reduced by surgical sectioning (pericision) of the supracrestal fibres. Overcorrection of the rotation early in treatment may help to minimise relapse; however, irrespective of strategy, bonded retention is required to guarantee alignment.
Where periodontal support is compromised, indefinite retention will be necessary following orthodontic treatment. When the maxillary labial frenum is suspected in the aetiology of a diastema (see Section 10.1), a fraenectomy is recommended. This is best undertaken during space closure so incisor approximation is aided by scar formation, although indefinite retention is required.
Soft tissues: Following appliance therapy, the teeth should be in a position of soft tissue balance. The original mandibular archform should remain unchanged, as markedly altering the angulation of the lower incisors will promote relapse. Limited proclination of the lower labial segment may be stable, however, where the lower incisors have been retroclined by a digit-sucking habit, a lower lip trap or by retroclined upper incisors. In addition, some retroclination of the lower incisors may be stable in class III correction where the upper incisors have been proclined and, as a result, the labiolingual position of the incisors is, in effect, interchanged.
In class II division 1, a pre-treatment assessment of the degree of lip incompetence and mechanism of achieving an anterior oral seal should be made, followed by an estimate of the likely post-treatment coverage of the upper incisors by the lower lip. One-third to one-half of the labial surface of the upper incisors should be covered to give the best chance of stable overjet correction.
Occlusal factors: A good buccal segment interdigitation, although unproven, and an interincisal angulation of about 135° promote stability. In addition, following incisor proclination, a positive overbite is necessary to prevent relapse
Facial growth: Continuing growth in the original pattern that contributed to the malocclusion is particularly likely to occur post-treatment in class III, open bite and deep bite cases. Some overcorrection of these incisor relationships is recommended, and retention should be continued until growth is complete. To prevent facial growth impacting on the development of late lower incisor crowding, permanent retention to the lower labial segment is now widely advocated.
Retention strategies
There are no specific rules as to the most appropriate retention strategy for each patient; this must be devised on an individual basis. The following guidelines are useful.
• After crossbite correction, where there is adequate overbite or good buccal segment interdigitation, no retention is necessary.
• On completion of removable appliance therapy, with the exception of space maintenance, a period of 3 months’ nocturnal wear of a Hawley retainer or a passive existing appliance is usually sufficient.
• At least 1 year of night-only retention is required following comprehensive treatment with fixed appliances. Hawley or vacuum-formed thermoplastic retainers may be used; although equally effective at preventing relapse in the upper arch, vacuum-formed are superior in the lower arch. Often this retainer type is prescribed for the upper arch only and a bonded retainer placed lingual to the lower labial segment, sometimes with a vacuum-formed retainer to wear over it in the event of partial debond. Because of the tendency for lower incisor crowding to occur, even when orthodontic treatment has been undertaken, prolonged retention to the lower labial segment by leaving the bonded retainer in place is recommended. Lengthy retention by a bonded retainer is advisable also following correction of rotations.
• Where growth modification has been used to correct a malocclusion, retention should continue until growth has ceased.
• In periodontally compromised dentitions, indefinite retention is recommended.
• In adults, the duration of retention should be longer than in adolescents because of the slower nature of the remodelling processes.
• Guidance in relation to the retention strategy following correction of other occlusal anomalies is given in the relevant sections.
![]() Self-assessment: questions
Self-assessment: questions
Multiple choice questions (True/False)
a. Is indicated for bodily tooth movement
b. Is particularly effective as a lower arch space maintainer in the mixed dentition
c. May act as a retainer following active tooth movement
2. When designing an upper removable appliance:
a. It is not recommended to do so with the patient in the dental chair
b. It is advisable to incorporate as many active components as possible
c. Using the acronym ARAB is helpful
d. The overjet measurement minus 2 mm gives an accurate indication of the required extent of a flat anterior bite plane
e. It is advisable to specify the wire dimensions of the appliance components
3. A flat anterior bite plane:
a. Is indicated for lower incisor proclination
b. Is an aid to correction of anterior open bite
c. Should contact at least two lower incisors
d. Should separate the molar teeth by 5 mm
e. Should allow the lower incisors to occlude posterior to it
4. Retention of an upper removable appliance may be improved by:
5. The following removable appliance components are usually made from 0.6 mm stainless steel wire:
6. The force exerted by a typical 0.5 mm palatal finger spring to retract a maxillary canine is:
a. Directly proportional to the length of the wire
b. Inversely proportional to the wire diameter
c. Inversely proportional to the deflection of the spring at activation
d. Directly proportional to the thickness of acrylic covering the terminal end of the spring in the base plate
e. Inversely proportional to the number of retention components on the appliance
7. A fixed appliance is indicated for:
c. Bodily retraction of upper incisors for overjet reduction
8. Active components on a fixed appliance may be:
9. The following are types of functional appliance:
10. The twin-block appliance for class II correction:
a. Cannot be worn while eating
b. Has buccal shields to allow arch expansion
d. Is usually constructed using a wax registration with the patient opened 2 mm in the first permanent molar region
11. There is a greater likelihood of anchorage loss:
a. When light forces are used to move teeth
b. On average, in the upper than in the lower arch
c. When few teeth are being moved in an intact arch
d. When the buccal interdigitation is good
e. In the upper arch with a full arch fixed appliance than with a removable appliance
12. Anchorage may be reinforced with an upper removable appliance by:
Extended matching items questions
Theme: Appliance components and appliance types
For each of the patients (a–e) that you might be asked to assess, select from the list below (1–16) the most appropriate appliance components to incorporate in an appliance or a specific appliance type (more than one may be correct) for correction of the occlusal problem(s) given. Each item can be used once, more than once or not at all.
a. An 8-year-old boy with both permanent upper central incisors in crossbite; there is an anterior mandibular displacement on closure on 1/1 and a 5 mm overbite on these incisors. 6edc21 are present in each quadrant.
b. A 13-year-old girl who has completed upper fixed appliance treatment for her class I malocclusion; there were no incisor rotations pretreatment; 7 to 1 are erupted in each quadrant.
c. A 12-year-old boy with an uncrowded class II division 1 malocclusion on a class II skeletal base with average FMPA.
d. An 11-year-old girl scheduled for fixed appliance therapy where slightly more space than that provided by extraction of upper first premolars will be required for upper arch alignment.
e. A 12.5-year-old boy where all the extraction space from lower second primary molar extractions (both lower second premolars are absent) will be needed for relief of crowding and fixed appliance alignment of the remaining teeth.
Case history questions
A 14-year-old male patient presents complaining of slow progress of upper removable appliance therapy to retract 3/3 following extraction of 4/4. Treatment commenced 8 months ago and the canine teeth are still not in a class I relationship. On examination, 3/3 only appeared to have moved 3 mm in the past 8 months.
Picture questions
Figure 11.4 shows a patient wearing an upper removable appliance.
Short note questions
2. disadvantages of removable appliances
4. preadjusted edgewise fixed appliances
5. optimal force range for tipping, bodily movement, rotation, intrusion
7. the histological effects that occur with a tipping movement to retract a maxillary canine
8. retention procedures to minimise/prevent rotational relapse.
Viva questions
1. What instructions would you give a patient who was issued with an upper removable appliance to procline /1?
2. How would you know if a passive removable appliance you had issued 4 weeks previously was being worn full time?
a. Classify functional appliances.
b. Outline your management of a class II division 1 malocclusion to be treated by a functional appliance.
c. Explain the mode of action and effects of a functional appliance in such a case.
4. Define what is meant by the term ‘anchorage’. Classify anchorage and describe how anchorage can be preserved and monitored during removable appliance therapy. What special measures may need to be taken with anchorage reinforcement?