Descriptions and relationships based on a person standing erect, facing forward, with arms at the sides, palms facing forward, legs together, and feet directed forward.
Equal right and left halves: Median plane
Anterior and posterior parts: Coronal (frontal) section
Unequal right and left halves: Sagittal or parasagittal section
Superficial fascia (hypodermis), which is subcutaneous tissue.
Skull, vertebral column, ribs, and sternum.
Synovial joint.
Skeletal, cardiac, and smooth.
Insertion (of the muscle).
Superior and inferior venae cavae.
Larger veins of the limbs and lower neck.
Angina pectoris. Atherogenesis of the coronary arteries can compromise the blood supply to the myocardium and precipitate an ischemic episode that is felt as chest pain (angina).
11. What body regions are ultimately drained of lymph by the thoracic duct?
Left upper body quadrant and both lower body quadrants.
Nasopharynx, oropharynx, and laryngopharynx (hypopharynx).
Efferent (motor) neuron.
In brain ventricles and the subarachnoid space.
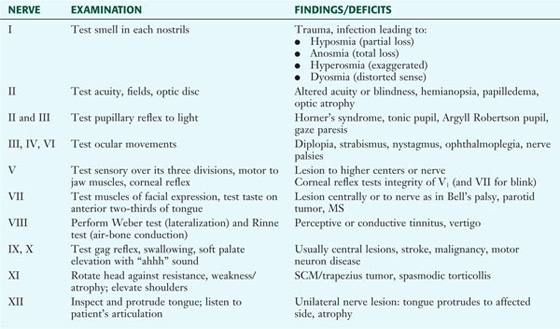
Use the mnemonic: On (Olfactory) Old (Optic) Olympus’ (Oculomotor) Towering (Trochlear) Top (Trigeminal), A (Abducens) Finn (Facial) And (Auditory-Vestibulocochlear) German (Glossopharyngeal) Viewed (Vagus) Some (Accessory-Spinal Accessory) Hops (Hypoglossal).
8 cervical pairs, 12 thoracic pairs, 5 lumbar pairs, 5 sacral pairs, and 1 coccygeal pair.
Sympathetic (thoracolumbar) and parasympathetic (craniosacral) divisions.
Sympathetic division.
FSH: Anterior pituitary gland
T4: Thyroid gland
Inhibin: Ovary
GH: Anterior pituitary gland
Cortisol: Adrenal cortex
ANP: Atria of the heart
Insulin: Pancreas
Testosterone: Testis
Renin: Kidney
Melatonin: Pineal
Oxytocin: Hypothalamus
Prolactin: Anterior pituitary gland
Cecum, ascending colon, transverse colon, descending colon, sigmoid colon, rectum, and anal canal.
The paired ureters drain the urine from the kidney to the urinary bladder, lie in a retroperitoneal position, extend about 24 to 34 cm in length, and possess a thick smooth muscle wall.
Sperm travel in the ductus (vas) deferens.
A thin mesothelial membrane that lines the body cavity walls (parietal peritoneum), reflects off the walls to form a double layer of peritoneum called a mesentery, and reflects onto the abdominal organs as a visceral peritoneal layer. It secretes a small amount of serous fluid to lubricate the peritoneal surfaces and reduce friction.
Gastrulation.
Notochord: Mesoderm
Epidermis: Ectoderm
Neurons: Ectoderm
Lining of GI tract: Endoderm
Nails and hair: Ectoderm
Heart: Mesoderm
Skeletal muscle: Mesoderm
Dermis: Mesoderm
Lining of airways: Endoderm
Ganglia: Ectoderm
Spinous process of L4 and the intervertebral disc of L4-L5.
It is a useful landmark for a lumbar puncture or epidural block.
Lordosis: Swayback
Kyphosis: Hunchback
Scoliosis: Curved back
Spinous process.
Synovial joints between the atlas and occipital bone (atlantooccipital joint) and between the atlas and axis (atlantoaxial joint).
L4-L5 or L5-S1.
Notochord.
L5.
Atlantoaxial joint.
Ligamentum flavum.
Into three groups: superficial (upper limb muscles), intermediate (muscles of respiration), and deep (postural muscles).
Deep intrinsic back muscles.
Iliocostalis, longissimus, and spinalis muscles.
Vertebral artery, a branch of the subclavian in the neck.
8 cervical, 12 thoracic, 5 lumbar, 5 sacral, and 1 coccygeal pair.
Somatic efferent (motor) axons, afferent (sensory) axons, and postganglionic sympathetic axons.
Dermatome.
In the brain ventricles, spinal central canal, and subarachnoid space of the brain and spinal cord.
A single anterior artery and two posterior arteries run the length of the spinal cord.
Sclerotome.
Spina bifida.
Neural tube.
It is the articulation of the manubrium and body of the sternum, and it marks the dividing point of the superior mediastinum from the inferior mediastinum. It also overlies the tracheal bifurcation and aortic arch and is useful for counting intercostal spaces. (Second ribs articulate here.)
Axillary lymph nodes (75% of all lymph).
Upper outer quadrant and the axillary tail of Spence. The most common type is infiltrating ductal carcinoma (70% to 80%).
External intercostals, as they elevate the ribs and, along with the diaphragm, increase the volume of the thoracic cavity.
Visceral pleura.
Lung extends to the eighth rib and the pleura to the tenth rib.
Anteroinferior to the pulmonary arteries and bronchi.
Compression of one or more of the structures passing out of the thoracic outlet. The subclavian artery or vein or the lower portion of the brachial plexus is often involved.
The right main bronchus is wider, shorter, and more vertical than the left bronchus, and aspirated infective agents can gain easier access to the right lung.
Postganglionic sympathetic fibers (to the heart) and visceral afferents from the heart.
Right, usually via its SA nodal branch.
Visceral afferents from the ischemic heart are conveyed to the upper thoracic spinal cord levels, which also receive somatic afferents from the T1-T4 dermatomes. Both groups of afferents converge in the dorsal horn of the spinal cord, and angina may be perceived as localized to the somatic distribution (T1-T4) rather than identified with the heart.
The pulmonary and aortic valves. Each has three semilunar cusps or leaflets. (They share a common embryologic origin.)
SA node to AV node to common AV bundle (of His) to the right and left bundle branches and subendocardial Purkinje system.
Drainage is largely by tributaries of the azygos system of veins (intercostal veins).
It has important connections with tributaries of the inferior vena cava and portal system, which normally drains most of the venous blood from below the diaphragm back to the heart. If this drainage is compromised, the connections with the azygos system provide alternative routes of venous return to the heart.
Laryngotracheal diverticulum.
On the right side, the right subclavian artery; on the left side, the aortic arch.
VSD, which usually occurs in the membranous portion of the interventricular septum.
Pulmonary stenosis or narrowing of the right ventricular outflow, transposed aorta, right ventricular hypertrophy, and VSD.
T10.
Spleen, splenic flexure of the transverse colon, pancreatic tail, stomach (variable), and part of the left kidney.
Skin; subcutaneous tissue (fatty Camper’s fascia and membranous Scarpa’s fascia in lower abdomen); external oblique, internal oblique, and transversus abdominis muscles; transversalis fascia; extraperitoneal fascia (preperitoneal fat); and peritoneum.
Genital branch of the genitofemoral nerve. It innervates the cremaster muscle.
A hernia that occurs lateral to the inferior epigastric vessels, passes through the deep inguinal ring and inguinal canal, and may appear at the superficial inguinal ring.
The epiploic foramen (of Winslow), just posterior to the hepatoduodenal ligament and anterior to the IVC.
In the lumen of the second, or descending, part of the duodenum.
Left gastric, common hepatic, and splenic. They supply the spleen and the foregut derivatives of the GI tract.
The jejunum compared to the ileum is larger in diameter; its mesentery contains less fat; its arterial arcades are fewer; and it has a longer vasa recta.
Midgut derivatives of the GI tract.
One third of the way along a line connecting the anterior superior iliac spine to the umbilicus. It is a good landmark for locating an inflamed appendix (point of tenderness).
Ascending colon, descending colon, and rectum.
The portion that is pressed against the diaphragm and is not covered with visceral peritoneum. It will have a dull appearance rather than a glistening appearance.
Esophageal, paraumbilical, rectal, and retroperitoneal.
Right and left hepatic ducts to the common hepatic duct to the cystic duct to the gallbladder. From the gallbladder to the cystic duct to the common bile duct to the hepatopancreatic ampulla (of Vater) to the second part of the duodenum.
In the abdomen at the cisterna chyli, which is the dilated beginning of the duct that receives lymph from lumbar and interstitial lymphatic glands.
At the ureteropelvic junction; at the point where the ureter crosses the external iliac vessels; and at the ureterovesical junction.
The right vein empties into the IVC, and the left vein empties into the left renal vein.
They distribute to the foregut and midgut derivatives of the GI tract by synapsing in the celiac and superior mesenteric ganglia and sending postganglionic fibers to the viscera on the vessels of the celiac artery and SMA.
Afferent axons conveying pain pass via the thoracic and lumbar splanchnic nerves to the dorsal root ganglia (site of the afferent neurons) and into the spinal cord between the T5 and L2 levels, where they synapse in the dorsal horn (gray matter).
Femoral nerve, which innervates the anterior compartment muscles of the thigh (largely knee extensors), and obturator, which innervates medial compartment muscles of the thigh (largely hip adductors).
Foregut and midgut derivatives are innervated by the vagus nerve; the hindgut is innervated by the pelvic splanchnic nerves (S2-S4).
The superior mesenteric artery (SMA).
The mesoderm into which the ureteric bud grows and differentiates to form the definitive human kidney.
The pelvic brim, sacrum, and coccyx.
The female pubic arch is larger and wider.
The greater and lesser sciatic foramina. They provide an avenue for structures to pass from the pelvis to the gluteal region and posterior thigh, and for the pudendal vessels and nerves to enter the pudendal canal and pass to the perineum.
Levator ani and coccygeus.
The body (fundus and isthmus) and cervix.
It is the lowest point in the female pelvis (where peritoneal fluids may collect), and access to drain these fluids is possible via the posterior vaginal fornix.
Mesovarium (surrounds and suspends ovary), mesosalpinx (surrounds and suspends uterine tubes), and mesometrium (surrounds and supports the uterus).
Stress incontinence may result from a loss of functional integrity of the pubovesical ligaments, vesicocervical fascia, levator ani, and/or urethral sphincter.
The transverse cervical (cardinal) and uterosacral ligaments, and the levator ani muscle.
Iliolumbar, lateral sacral, and superior gluteal arteries.
Appropriate central nervous system reflexes initiate voiding via stimulation of pelvic splanchnic nerves to the bladder; this causes contraction of the detrusor smooth muscle of the bladder wall. Voluntary relaxation of external sphincter urethrae muscle tone occurs in conjunction with the detrusor contraction, but it is mediated by the somatic nervous system. In males, sympathetic relaxation of the internal sphincter (females lack an internal sphincter) also occurs with detrusor muscle contraction.
Prostatic, membranous, and spongy (penile).
Into the prostatic urethra via the ejaculatory ducts.
Inferior anal (rectal) nerves from the pudendal nerve (S2-S4).
The inferior and middle rectal veins (tributaries of the internal iliac vein—caval system) anastomose with the superior rectal vein from the inferior mesenteric vein, a tributary of the portal venous system.
Parasympathetic preganglionic fibers arise from S2-S4 via pelvic splanchnic nerves that course to the inferior hypogastric plexus (pelvic), synapse there, and then innervate pelvic viscera (smooth muscle and glands).
The lymphatic vessels of the ovary follow the ovarian artery directly back to the abdominal aorta and infiltrate aortic nodes in this region.
The pubic symphysis anteriorly, the ischial tuberosities laterally, and the coccyx posteriorly.
It anchors the perineum because it provides for the attachment of many skeletal muscles of the perineum as well as fascial layers.
Loss of functionality in the nerves that relax the smooth muscle tone of the corpus cavernosum, which impedes blood flow into cavernous erectile tissue. Current medications facilitate smooth muscle relaxation and increase blood flow.
The bulb of the vestibule.
The greater trochanter of the femur.
Ilium, ischium, and pubis. All come together in the acetabulum.
The iliofemoral ligament, which forms an inverted Y ligament (of Bigelow) that limits hyperextension.
Primarily the retinacular arteries of the medial and lateral femoral circumflex, and the acetabular branch of the obturator artery, which runs in the ligament of the femoral head (less important in adults).
Superior gluteal nerve. Weakness of abductors (gluteus medius and minimus) on the weight-bearing limb can lead to a gluteal lurch during walking; this is known as a positive Trendelenburg sign.
Ventral primary rami of L1-L4.
Tibial and common fibular nerves.
Iliopsoas muscle.
Femoral nerve (L2-L4). These muscles are largely extensors of the leg at the knee.
Semitendinosus, semimembranosus, and long head of the biceps femoris. They extend the thigh at the hip and flex the leg at the knee.
To avoid injury to the large sciatic nerve, which runs through the lower half of the gluteal region.
An attachment arrangement of tendons of the semitendinosus, gracilis, and sartorius muscles to the medial tibial condyle (looks like a goose’s foot).
Anterior drawer sign, where the tibia moves anteriorly in relation to the femur. The ACL normally prevents hyperextension of the knee and is injured more than the posterior cruciate ligament.
Injury to the ACL, tibial collateral ligament, and medial meniscus.
Anterior tibial artery.
| Gastrocnemius | Tibial |
| Fibularis longus | Superficial fibular |
| Tibialis anterior | Deep fibular |
| Plantaris | Tibial |
| Flexor hallucis longus | Deep fibular |
| Flexor digitorum brevis | Medial plantar (from tibial) |
| Soleus | Tibial |
| Abductor digiti minimi | Lateral plantar (from tibial) |
| Plantar and dorsal interossei | Lateral plantar (from tibial) |
Deep fibular nerve (if weakened eversion is also present, then it is the common fibular nerve).
Talocrural joint, a uniaxial synovial hinge (ginglymus) joint.
The longitudinal and transverse arches.
Plantar calcaneonavicular ligament, which supports the head of the talus and medial longitudinal arch of the foot. It is fairly elastic, hence its name.
Calcaneus. Most are intra-articular fractures in which the talus is driven down on the calcaneus, as in a fall from a great height, with a landing on the heel.
The patellar tendon reflex (L3-L4) and the calcaneal tendon reflex (S1-S2).
Medial and lateral plantar arteries derived from the posterior tibial artery.
The swing phase and the stance phase.
Inguinal region: L1
Knee: L4
Second toe: L5
Posterior leg and thigh: S1-S2
Rotates medially 90°, while the upper limb rotates laterally 90°. Thus, the limbs are 180° out of phase with each other (knee anterior and big toe medial versus elbow posterior and thumb lateral).
Median cubital vein in the cubital fossa.
Multiaxial synovial ball-and-socket joint; capable of flexion, extension, abduction, adduction, protraction and retraction, and circumduction.
Fibrocartilaginous glenoid labrum.
Subscapularis, supraspinatus, infraspinatus, and teres minor muscles.
Axillary nerve.
Dorsal scapular, suprascapular, and subscapular arteries.
Axillary: Deltoid and teres minor
Dorsal scapular: Levator scapulae and rhomboids
Medial pectoral: Pectoralis minor and major
Upper subscapular: Subscapularis
Lower subscapular: Subscapularis and teres major
Long thoracic: Serratus anterior
Thoracodorsal: Latissimus dorsi
Axillary, musculocutaneous, radial, median, and ulnar nerves.
Biceps brachii muscle.
C7 and C8 (radial nerve). C5 and C6 (musculocutaneous nerve).
Radial nerve.
Anular ligament.
Medial epicondyle of the humerus.
Flexor carpi radialis: Flex and abduct hand at wrist
Flexor digitorum superficialis: Flex middle phalanges of medial four digits
Flexor digitorum profundus: Flex distal phalanges of medial four digits
Brachioradialis: Flex forearm at elbow
Extensor carpi ulnaris: Extend and adduct hand at wrist
Extensor digitorum: Extend medial four digits at metacarpophalangeal (MCP) joint
Extensor pollicis brevis: Extend proximal phalanx of thumb at MCP joint
Abductor pollicis longus: Abduct and extend thumb at MCP joint
Extensors of wrist and/or digits, and supinator of the forearm; radial nerve.
Scaphoid.
A common extension-compression fracture of the distal radius that results in a typical dinner fork deformity.
Lumbrical and interosseous muscles.
Median (recurrent branch) nerve.
Osseofascial tunnel consisting of the carpal arch and overlying flexor retinaculum (transverse carpal ligament). It contains nine muscle tendons and the median nerve.
Median nerve: Palmar (volar) tip of the index finger
Ulnar nerve: Palmar (volar) tip of the little finger
Radial nerve: Dorsal web space between the thumb and index finger
Thenar atrophy: Median
Hypothenar atrophy: Ulnar
Claw hand: Ulnar
Wrist drop: Radial
First dorsal interosseous atrophy: Ulnar
Paresthesia along lateral forearm: Musculocutaneous
Paresthesia over lateral deltoid: Axillary
Weakened finger adduction: Ulnar
Winging of scapula: Long thoracic
The hypomere (hypaxial muscles); these include all the muscles of the upper limb.
Shoulder: C5-C6
Middle finger: C7
Little finger: C8
Elbow: C7-C8
Medial arm: T1
| Superior orbital fissure | Oculomotor, trochlear, abducent, and V1 |
| Rotundum | V2 |
| Ovale | V3, lesser petrosal (occasionally) |
| Internal acoustic meatus | Facial and vestibulocochlear |
| Jugular | Glossopharyngeal, vagus, and spinal accessory |
About 500 mL/day is produced; CSF is reabsorbed by the arachnoid granulations (most significant site) and small capillaries along the brainstem and spinal cord.
Superior petrosal sinus to sigmoid sinus to internal jugular vein to brachiocephalic vein (right or left) to superior vena cava to right atrium.
| Epidural | Arterial, usually the middle meningeal or its branches |
| Subdural | Venous, often the cortical bridging veins |
| Subarachnoid | Arterial, often from saccular (berry) aneurysms |
GSA: sensory to the skin of the ear
SVA: special sense of taste to the anterior two-thirds of the tongue
GVE: motor to glands; salivary, nasal, and lacrimal
SVE: motor to muscles of facial expression and those from the second pharyngeal arch
Lacrimal gland (CN VII secretomotor fibers) to lacrimal ducts to bulbar conjunctival and corneal surfaces, then to lacrimal lake, to lacrimal punctum (superior and inferior) to lacrimal canaliculi to lacrimal sac, down the nasolacrimal duct and into the inferior meatus of the inferior nasal concha.
SR (CN III) and IO (CN III), in abduction and adduction, respectively.
Myopia: Nearsightedness; difficulty seeing distant objects clearly
Hyperopia: Farsightedness; difficulty seeing close objects clearly
Presbyopia: Progressive loss of ability to accommodate the lens and clearly focus on close objects
Resistance to the outflow of aqueous humor, usually primary open angle, resulting from impedance at the canal of Schlemm or of the trabecular meshwork, or from venous backpressure.
Ptosis: loss of innervation of superior tarsal (smooth) muscle (distal part of levator palpebrae muscle of upper eyelid)
Miosis: loss of innervation of dilator muscle of the pupil
Anhydrosis: loss of innervation of sweat glands
Flushed face: unopposed vasodilation of cutaneous vessels
(Each sign represents loss of sympathetic innervation)
Preganglionic parasympathetic fibers from CN IX (inferior salivatory nucleus) innervate the gland and travel via the lesser petrosal nerve to the otic ganglion, where they synapse. Postganglionic fibers then jump onto the auriculotemporal branch of V3 and pass to the parotid gland (secretomotor fibers).
Loss of salivary secretion in the submandibular and sublingual salivary glands, and loss of taste from the anterior two-thirds of the tongue.
Frontal, maxillary, and anterior and middle ethmoid sinuses.
Motor: CN XII; sensory: CN V3 (anterior), CN IX (posterior), and CN X (epiglottis); taste: CN VII (anterior) and CN IX (posterior).
Ansa cervicalis (C1-C3) of the cervical plexus.
The phrenic nerve (C3-C5) appears on the anterior surface of the anterior scalene muscle and innervates the diaphragm.
Inferior thyroid, transverse cervical, and suprascapular.
Recurrent laryngeal nerve, which innervates the muscles of the larynx.
Nasopharynx, oropharynx, and laryngopharynx (called hypopharynx by many clinicians).
A potential space between the alar and prevertebral fascial layers. An infection in this space can spread superiorly to the base of the skull or inferiorly into the posterior mediastinum.
A ring of lymphoid tissues around the oropharynx including the palatine, lingual, and nasopharyngeal tonsils.
Superior cervical ganglion.
Metencephalon (pons and cerebellum) and myelencephalon (medulla oblongata).
CN IX (innervates the stylopharyngeus muscle); the inferior half and greater horns of the hyoid bone are derived from the third arch.