PELVIS AND PERINEUM
1. INTRODUCTION
The bowl-shaped pelvic cavity is continuous superiorly with the abdomen and bounded inferiorly by the perineum, the region between the thighs. The bones of the pelvic girdle demarcate the following two regions:
- Greater or false pelvis: the lower portion of the abdomen that lies between the flared iliac crests
- Lesser or true pelvis: demarcated by the pelvic brim, sacrum, and coccyx, and contains the pelvic viscera
The pelvis contains the terminal gastrointestinal tract and urinary system, and the internal reproductive organs. The perineum lies below the “pelvic diaphragm,” or muscles that form the pelvic floor, and contains the external genitalia. In reviewing the pelvis and perineum, we will focus on the musculoskeletal structures that support the pelvis and then study the viscera, blood supply, and innervation of these two regions.
2. SURFACE ANATOMY
Key Landmarks
Key landmarks of the surface anatomy include the following (Fig. 5-1):
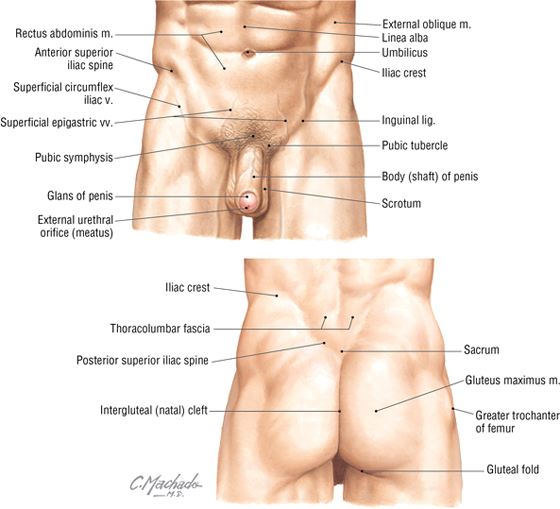
FIGURE 5-1 Surface Anatomy: Key Landmarks
- Umbilicus: site that marks the T10 dermatome, that lies at the level of the intervertebral disc between L3 and L4
- Iliac crest: rim of the ilium that lies at approximately the L4 level
- Anterior superior iliac spine: superior attachment point for the inguinal ligament
- Inguinal ligament: ligament formed by aponeurosis of the external abdominal oblique muscle; forms a line of demarcation separating the lower abdominopelvic region from the thighs
- Pubic tubercle: the inferior attachment point of the inguinal ligament
- Posterior superior iliac spine: often seen as a “dimpling” of the skin just above the intergluteal (natal) cleft; often more obvious in females
The surface anatomy of the perineum will be reviewed with that section later in this chapter.
3. MUSCULOSKELETAL ELEMENTS
Bony Pelvic Girdle
The pelvic girdle is the attachment point of the lower limb to the body’s trunk. (The pectoral girdle is its counterpart for the attachment of the upper limb.) The bones of the pelvis include the following (Fig. 5-2):
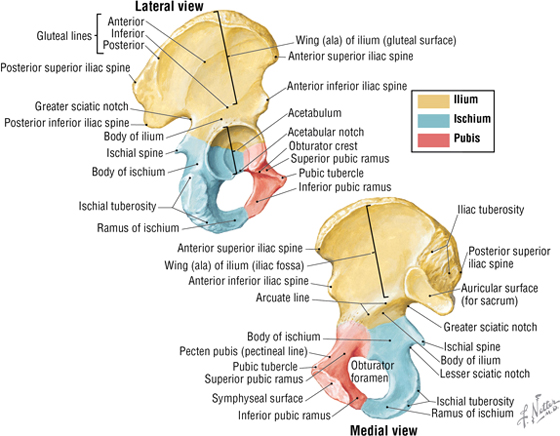
FIGURE 5-2 Right Pelvic (Coxal) Bone
- Right and left pelvic bones (coxal or hip bones): the fusion of three separate bones (i.e., the ilium, ischium, and pubis) that join in the acetabulum (cup-shaped surface where the pelvis articulates with the head of the femur)
- Sacrum: the fusion of the five sacral vertebrae; the two pelvic bones articulate with the sacrum posteriorly
- Coccyx: the terminal end of the vertebral column; a remnant of our embryonic tail
The pelvic girdle forms a stable articulation to support the transfer of weight from the lower limb to the body’s trunk. The joints and ligaments reflect this stability and are summarized in Figure 5-3 and Table 5-1. The sacrum and coccyx are reviewed in the Chapter 2 along with the vertebral column.
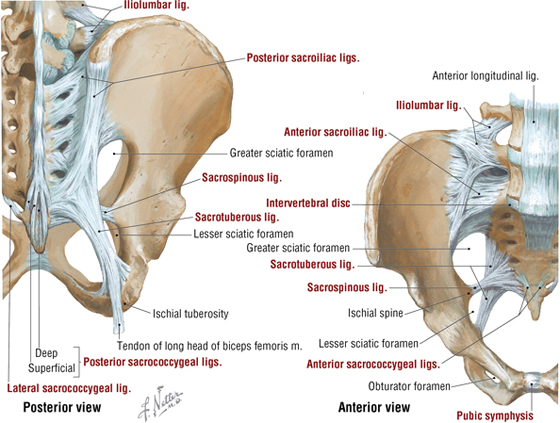
FIGURE 5-3 Bony Pelvis and Ligaments
|
TABLE 5-1 Joints and Ligaments of the Pelvis
|
 |
*Other ligaments include those binding any two vertebrae and facet joints
Anatomically, the female bony pelvis differs from the male pelvis, reflecting the adaptations for childbirth. The differences include the following:
- The bones of the pelvis usually are smaller, lighter, and thinner.
- The pelvic inlet is oval in the female and heart-shaped in the male.
- The pelvic outlet is larger due to everted ischial tuberosities.
- The pelvic cavity is wider and shallower.
- The pubic arch is larger and wider.
- The greater sciatic notch is wider.
- The sacrum is shorter and wider.
- The obturator foramen is oval or triangular in the female and round in the male
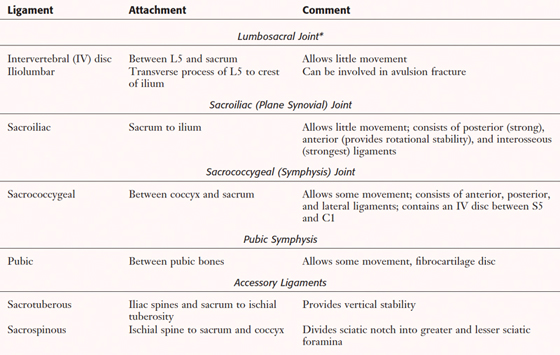
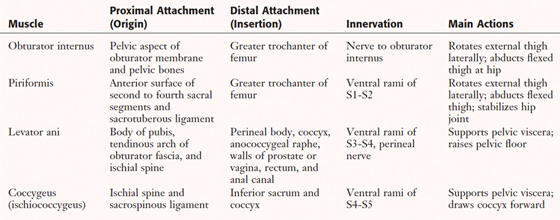
Muscles of the Pelvis
The muscles of the true pelvis line its lateral wall and form a floor over the pelvic outlet. (The pelvic inlet is demarcated by the pelvic brim.) Two muscles line the lateral wall (obturator internus and piriformis) and attach to the femur, and two muscles form the floor, or “pelvic diaphragm” (levator ani and coccygeus) (Fig. 5-4 and Table 5-2). The levator ani is really composed of three muscle groups intermingled to form a single sheet of muscle (iliococcygeus, pubococcygeus, and puborectalis). The levator ani muscle is a very important support structure for the pelvic viscera in bipeds (upright-walking humans) and also helps maintain closure of the vagina and rectum. Bipedalism places greater pressure on the lower pelvic floor, and these two muscles have been “co-opted” for a different use then originally intended in most land-dwelling quadruped mammals. Thus, the muscles once used to tuck the tail between the hind legs (coccygeus) and wag the tail (levator ani) now subserve a support function as we have evolved as bipeds and lost our tail.
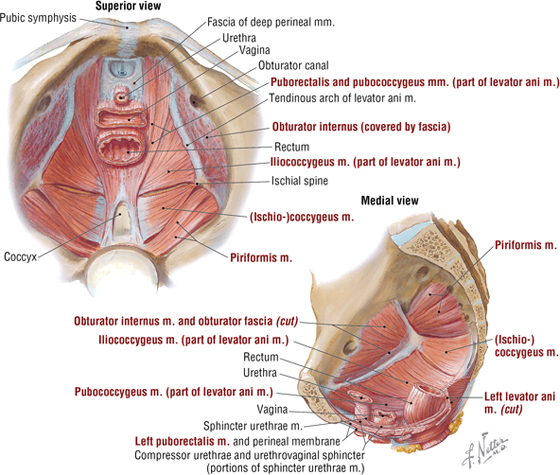
FIGURE 5-4 Muscles of the Female Pelvis
|
TABLE 5-2 Muscles of the Pelvis
|
 |
4. VISCERA
Distal Gastrointestinal Tract
In both sexes, the distal gastrointestinal tract passes into the pelvis as the rectum and anal canal. The rectosigmoid junction superiorly lies at about the level of the S3 vertebra, and the rectum extends inferiorly to become the anal canal just below the coccyx (Fig. 5-5). As the rectum passes through the pelvic diaphragm, it bends posteriorly at the anorectal flexure and becomes the anal canal. The anorectal flexure is important in maintaining fecal continence (via the muscle tone maintained by the puborectalis portion of the levator ani muscle). During defecation, this flexure straightens, and fecal matter can then move into the anal canal. Superiorly the rectum is covered on its anterolateral surface with peritoneum, which gradually covers only the anterior surface, while the distal portion of the rectum descends below the peritoneal cavity (subperitoneal) to the anorectal flexure. Features of the rectum and anal canal are summarized in Table 5-3.
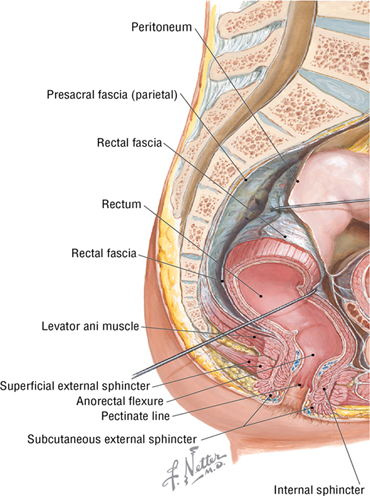
FIGURE 5-5 Rectum and Anal Canal
|
TABLE 5-3 Features of the Rectum and Anal Canal
|
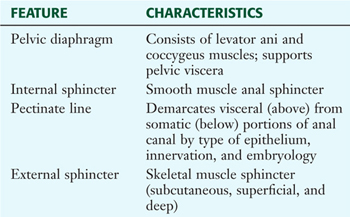 |
Distal Urinary Tract
The distal elements of the urinary tract lie within the pelvis. These include the following (Fig. 5-6):
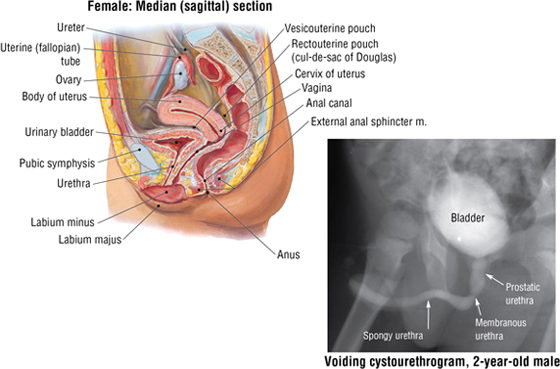
FIGURE 5-6 Distal Urinary Tract (Contd.)
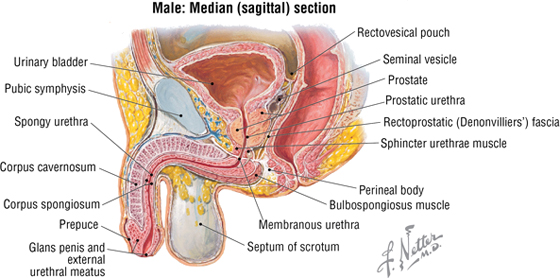
FIGURE 5-6 (Contd.) Distal Urinary Tract
- Distal ureters: pass retroperitoneally into the pelvic inlet and are crossed anteriorly by the uterine artery in females and the ductus deferens in males before terminating in the urinary bladder
- Urinary bladder: lies behind the pubic symphysis in a subperitoneal position; holds up to 800 to 1000 mL of urine and contains a smooth triangular area internally between the openings of the two ureters and the single urethral opening inferiorly (trigone of the bladder); the smooth muscle of the bladder wall is the detrusor muscle
- Urethra: short in the female (3 to 4 cm) and contains two small paraurethral mucous glands (Skene’s glands) at its aperture; longer in the male (20 cm) and divided into the prostatic, membranous, and spongy portions
Females have an external urethral sphincter composed of skeletal muscle under voluntary control and innervated by the somatic nerve fibers in the pudendal nerve (S2-S4). Males have the following urethral sphincters:
- Internal sphincter: smooth-muscle involuntary sphincter at the neck of the bladder and innervated by sympathetic fibers from L1 to L2; during ejaculation, it contracts and prevents semen from entering the urinary bladder
- External sphincter: skeletal muscle voluntary sphincter surrounding the membranous urethra and innervated by the somatic nerve fibers in the pudendal nerve (S2-S4)
Micturition (urination/voiding) occurs by the following sequence of events:
- Normally, the sympathetic fibers relax the bladder wall and constrict the internal urethral sphincter (smooth muscle around the bladder neck, present only in males), thus inhibiting emptying
- Micturition is initiated by the stimulation of stretch receptors (afferents enter the spinal cord via the pelvic splanchnic nerves, S2-S4) located in the detrusor (smooth) muscle of the bladder when it begins to fill
- Parasympathetic efferents (pelvic splanchnics) induce a reflex contraction of the detrusor muscle and relaxation of the internal sphincter (males only), enhancing the “urge” to void
- When appropriate (and sometimes not!), somatic efferents via the pudendal nerve (S2-S4) cause voluntary relaxation of the external urethral sphincter, and the bladder begins to empty
- When complete, the external urethral sphincter contracts (in males, the bulbospongiosus muscle contracts to expel the last few drops of urine from the spongy urethra), and the detrusor muscle relaxes under sympathetic control
C L I N I C A L F O C U S
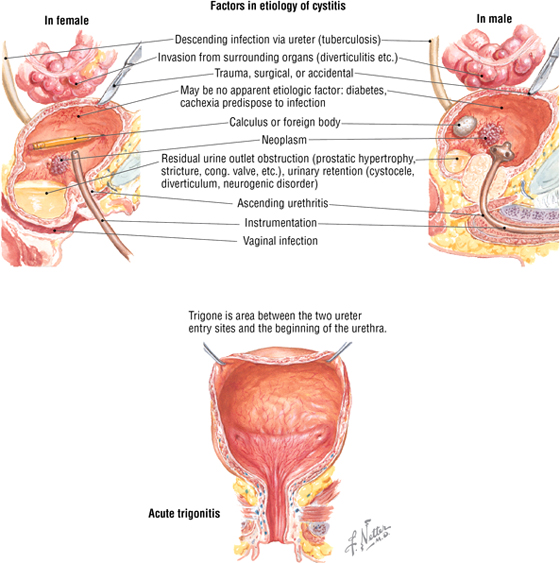
Urinary Tract Infections
Urinary tract infection (UTI) is more common in females, and this probably is directly related to their shorter urethras, urinary tract trauma, and exposure to pathogens in an environment that is conducive for growth and propagation. As illustrated, a number of other risk factors also may precipitate infections in either sex. Escherichia coli is the usual pathogen involved in infection. UTI may lead to urethritis, cystitis (bladder inflammation), and pyelonephritis. Symptoms of cystitis may include the following:
- Dysuria
- Frequency of urination
- Urgency of urination
- Suprapubic discomfort and tenderness
- Hematuria (less common)
C L I N I C A L F O C U S
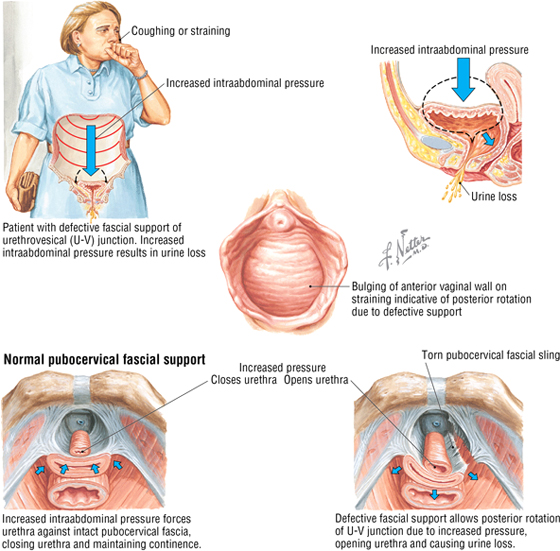
Stress Incontinence in Women
Involuntary loss of urine after an increase in intraabdominal pressure is often associated with a weakening of the support structures of the pelvic floor, including the following:
- Medial and lateral pubovesical ligaments
- Pubovesical fascia at the urethrovesical junction (blends with the perineal membrane and body)
- Levator ani (provides support at the urethrovesical junction)
- Functional integrity of the urethral sphincter
Common predisposing factors for stress incontinence include multiparity, obesity, chronic cough, and heavy lifting.
Reproductive Viscera in the Female
The female pelvic reproductive viscera include the midline uterus and vagina, and the adnexa (paired ovaries and uterine tubes). A double sheet of peritoneum (actually a mesentery), called the broad ligament, envelopes the ovaries, uterine tubes, and uterus (Figs. 5-7 and 5-8). During embryonic development, the ovaries are pulled into the pelvis by a fibromuscular band (homologue of the male gubernaculum), and this ovarian ligament attaches the inferomedial pole of the ovary to the uterus. It then reflects anterolaterally off the uterus as the round ligament of the uterus, enters the deep inguinal ring, courses down the inguinal canal, and ends in the labia majora of the perineum as a fibrofatty mass. Features of the female pelvic reproductive viscera are summarized in Table 5-4.
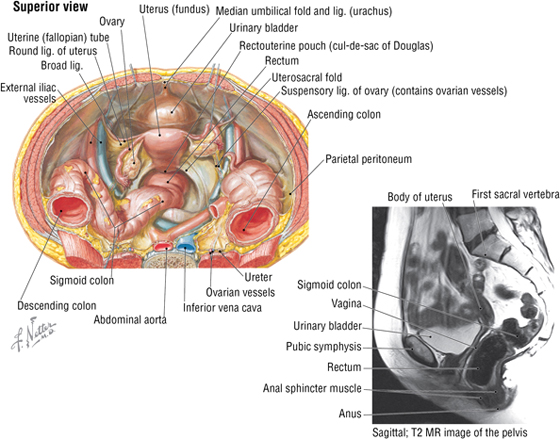
FIGURE 5-7 Peritoneal Relationships of the Female Pelvic Viscera. (MR reprinted with permission from Kelley LL, Petersen C: Sectional Anatomy for Imaging Professionals. Philadelphia, Mosby, 2007.)
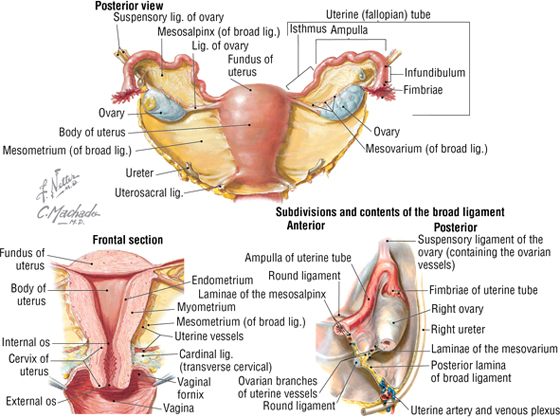
FIGURE 5-8 Uterus and Adnexa
|
TABLE 5-4 Features of the Female Pelvic Viscera
|
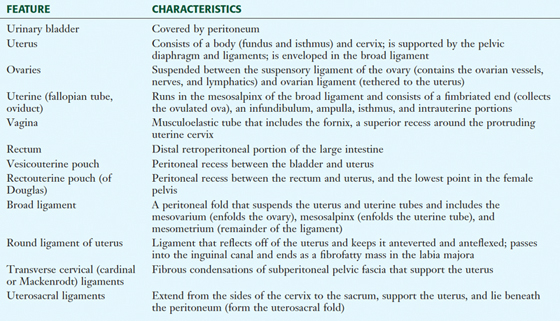 |
C L I N I C A L F O C U S
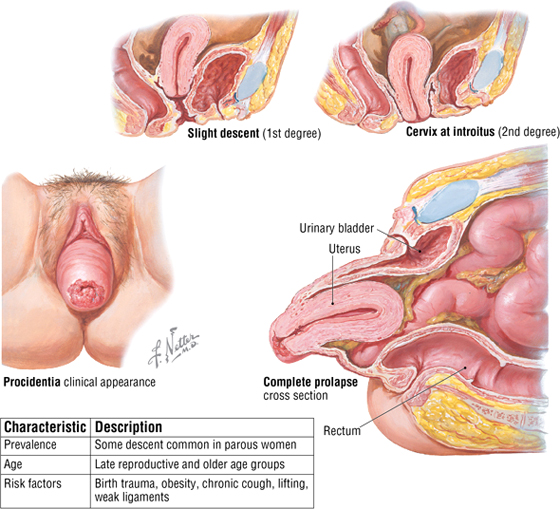
Uterine Prolapse
Uterine prolapse may occur when the support structures of the uterus, especially the cardinal ligaments, uterosacral ligaments, and levator ani, are weakened.
C L I N I C A L F O C U S
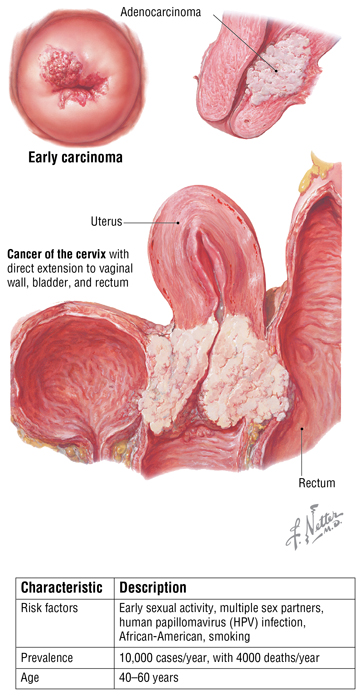
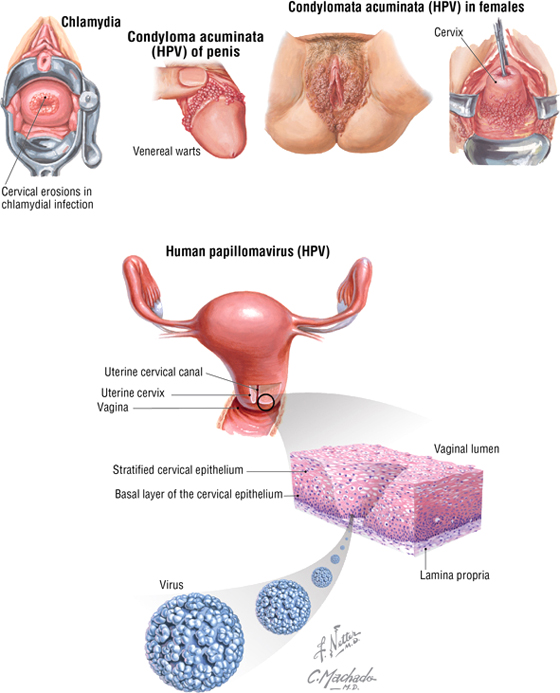
Cervical Carcinoma
Approximately 85% to 90% of cervical carcinomas are squamous cell carcinomas, whereas 10% to 15% are adenocarcinomas. Most carcinomas occur near the external cervical os, where the cervical epithelium changes from simple columnar to stratified squamous epithelium (the transformation zone). The most common cause of cervical carcinoma is contraction of human papillomavirus (HPV) during sexual intercourse.
C L I N I C A L F O C U S
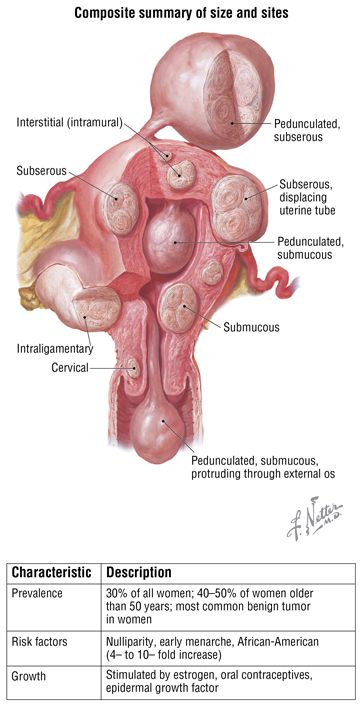
Uterine Leiomyomas (Fibroids)
Leiomyomas are benign tumors of smooth muscle and connective tissue cells of the myometrium of the uterus. They are firm, can range in size from 1 mm to 20 cm, and commonly are referred to as “fibroids.” This illustration is a composite drawing showing various sizes and sites of potential leiomyomas.
C L I N I C A L F O C U S
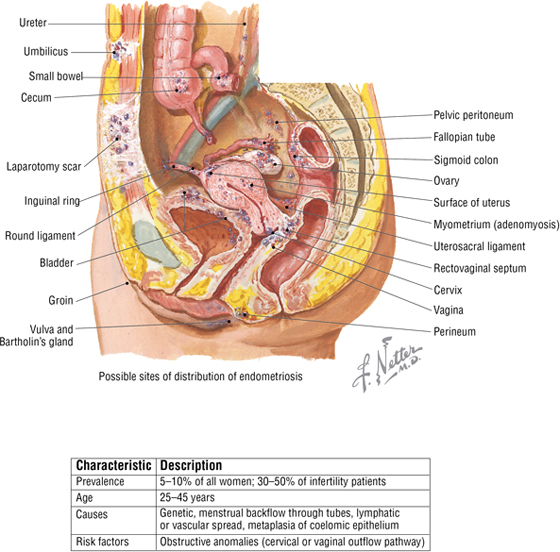
Endometriosis
Endometriosis is a progressive benign condition characterized by ectopic foci of endometrial tissue, called implants, that grow in the pelvis (on the ovaries, in the rectouterine pouch, uterine ligaments, uterine tubes) or in the peritoneal cavity. Like the lining of the uterus, these ectopic implants can grow and then break down and bleed in cycle with the woman’s normal menstrual cycle. (They are estrogen sensitive.)
C L I N I C A L F O C U S
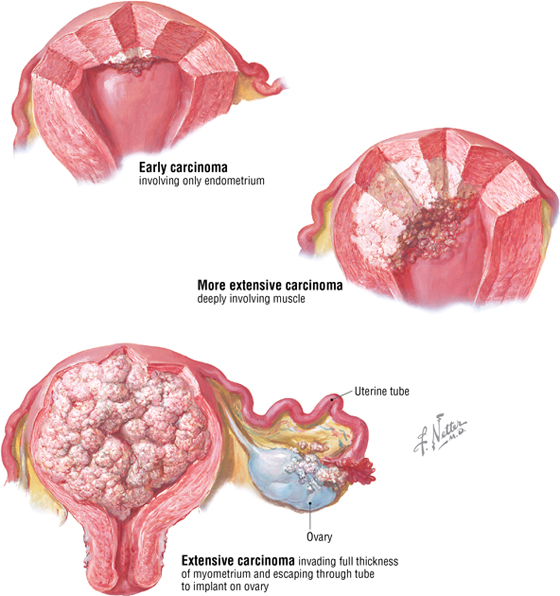
Uterine Endometrial Carcinoma
Endometrial carcinoma is the most common malignancy of the female reproductive tract. It often occurs between the ages of 55 and 65 years, and risk factors include the following:
- Obesity (increased estrogen synthesis from fat cells without concomitant progesterone synthesis)
- Estrogen replacement therapy without concomitant progestin
- Breast or colon cancer
- Early menarche or late menopause (prolonged estrogen stimulation)
- Chronic anovulation
- No prior pregnancies and/or periods of breastfeeding
- Diabetes
C L I N I C A L F O C U S
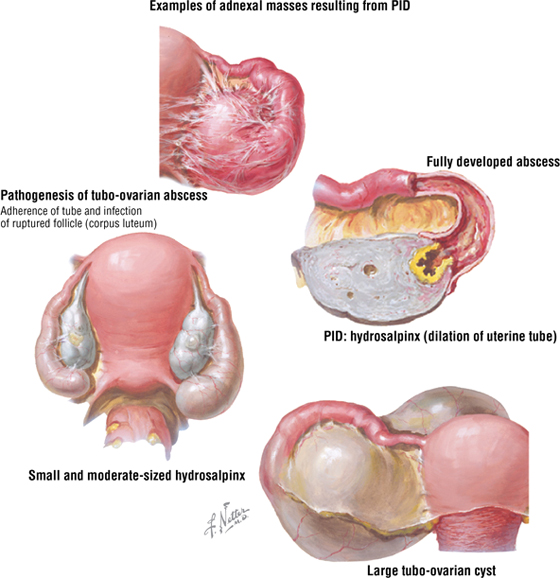
Chronic Pelvic Inflammatory Disease
Recurrent or chronic infections of the uterine tubes or other adnexa (uterine appendages) result in cystic dilation (hydrosalpinx) and can account for approximately 40% of female infertility. The inflammation can cause scarring, causing problems with fertility, pelvic pain, or tubal (ectopic) pregnancy. The most affected age group is 15 to 25 years of age, and risk factors include the following:
- Early sexual activity
- Failure to use condoms
- Multiple sexual partners
- Sexually transmitted diseases (STDs)
C L I N I C A L F O C U S
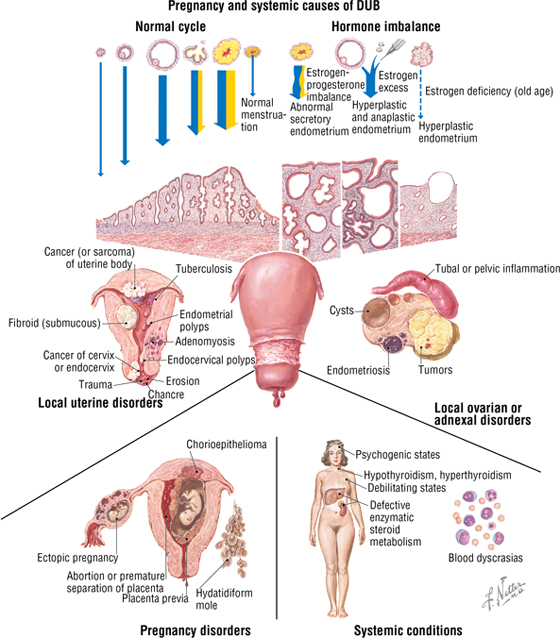
Dysfunctional Uterine Bleeding
Dysfunctional uterine bleeding (DUB) involves an irregular cycle or intermenstrual bleeding (painless) with no clinically identifiable cause. It accounts for approximately 10% to 15% of all gynecologic office visits. The etiology and pathogenesis are extensive and include local uterine, ovarian, or adnexal disorders, as well as systemic and pregnancy-related disorders. Hormonal imbalance is a common cause.
C L I N I C A L F O C U S
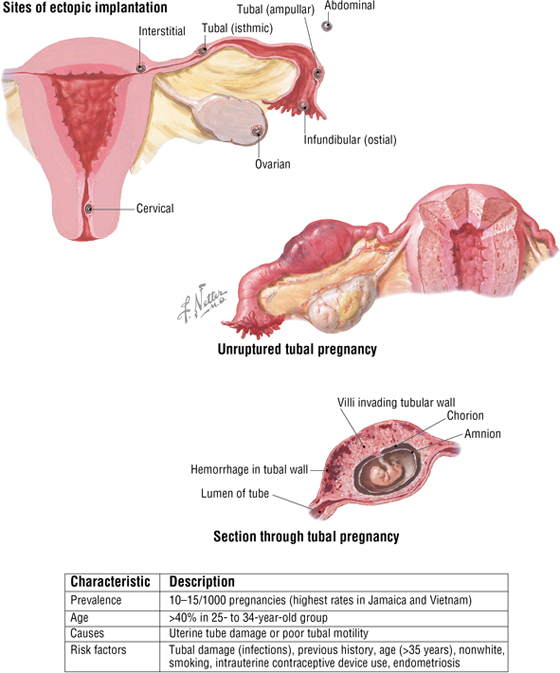
Ectopic Pregnancy
Ectopic pregnancy involves implantation of a blastocyst outside the uterine cavity, most commonly in the fallopian tube. Because of the potential medical danger of an ectopic pregnancy, the pregnancy is usually terminated medically (if detected early enough) or surgically (often laparoscopically).
C L I N I C A L F O C U S
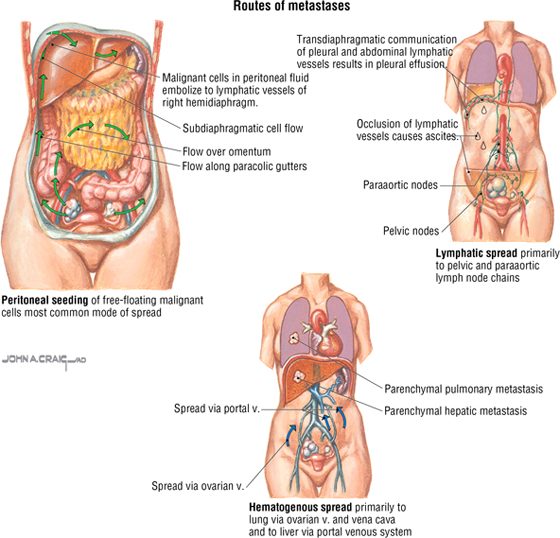
Ovarian Cancer
Ovarian cancer is the most lethal cancer of the female reproductive tract (about 16,000 deaths annually). Eighty-five percent to 90% of all malignancies occur from the surface epithelium, with cancerous cells often breaking through the capsule and seeding the peritoneal surface, invading the adjacent pelvic organs, or seeding the omentum, mesentery, and intestines. Additionally, the cancer cells spread via the venous system to the lungs (ovarian vein and IVC) and liver (portal system), and via lymphatics. Risk factors include the following:
C L I N I C A L F O C U S
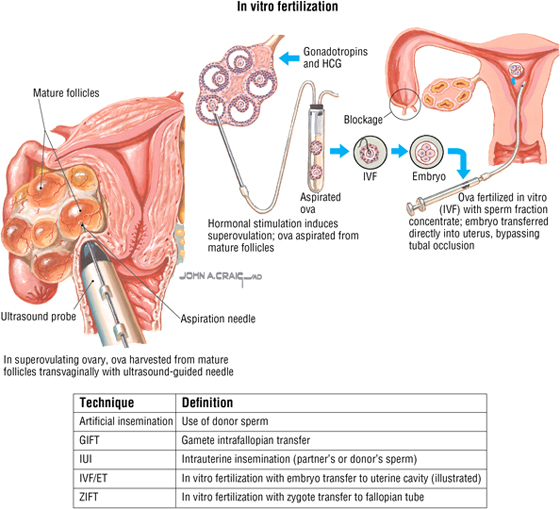
Assisted Reproduction
Approximately 10% to 15% of infertile couples may benefit from various assisted reproductive strategies.
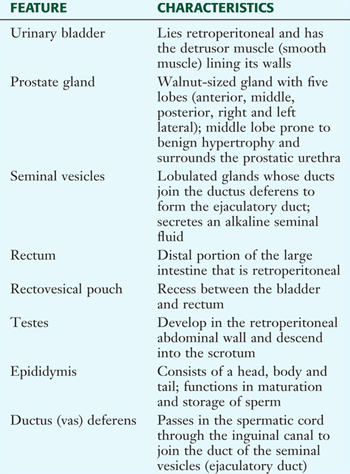
Reproductive Pelvic Viscera in the Male
The male pelvic reproductive viscera include the prostate gland and paired seminal vesicles. These structures lie in a subperitoneal position and are in close association with the urethra (Fig. 5-9). The testes descend into the scrotum late in human prenatal development and are connected to the seminal vesicles by the ductus (vas) deferens, which ascends in the scrotum, passes through the inguinal canal, and then courses retroperitoneally to join the duct of the seminal vesicles (ejaculatory ducts) (Table 5-5).
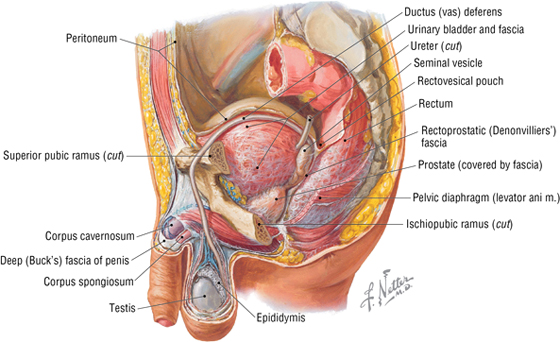
FIGURE 5-9 Male Reproductive Viscera
|
TABLE 5-5 Features of the Male Pelvic Viscera
|
 |
The testes are paired gonads that are about the size of a chestnut. They exhibit the following features (Fig. 5-10):
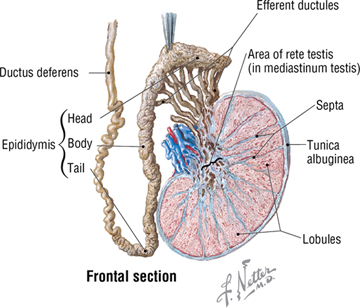
FIGURE 5-10 Testis, Epididymis, and Ductus Deferens
- During descent of the testes into the scrotum, a pouch of peritoneum called the tunica vaginalis attaches to the anterior and lateral aspect of the testes (has visceral and parietal layers)
- They are encased within a thick capsule, the tunica albuginea
- They are divided into lobules that contain seminiferous tubules
- The seminiferous tubules are lined with germinal epithelium that gives rise to spermatozoa
- They drain spermatozoa into the rete testes (straight tubules) and efferent ductules of the epididymis
- Sperm mature and are stored in the epididymis, a long coiled tube about 23 feet in length
The ductus deferens joins the ducts of the seminal vesicles to form the ejaculatory ducts, which empty into the prostatic urethra, the first portion of the male urethra leaving the urinary bladder (Fig. 5-11) (also see Fig. 5-9 and Table 5-5). The seminal vesicles exhibit the following features:
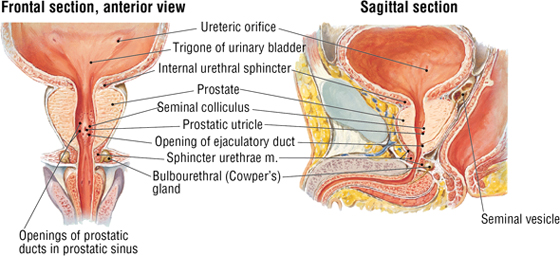
FIGURE 5-11 Bladder, Prostate, Seminal Vesicles, and Proximal Urethra. (MR reprinted with permission from Weber E, Vilensky J, Carmichael M: Netter’s Concise Radiologic Anatomy. Philadelphia, Saunders, 2009.) (Contd.)
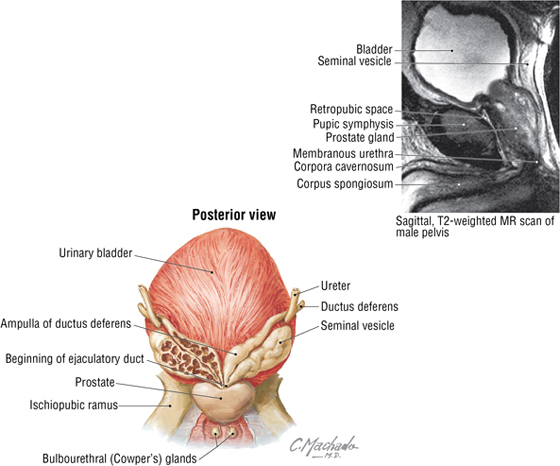
FIGURE 5-11 (Contd.) Bladder, Prostate, Seminal Vesicles, and Proximal Urethra. (MR reprinted with permission from Weber E, Vilensky J, Carmichael M: Netter’s Concise Radiologic Anatomy. Philadelphia, Saunders, 2009.)
- Contribute fluid to the ejaculate; produce about 70% of the ejaculate volume
- Produce a viscous and alkaline fluid that nourishes the spermatozoa and protects them from the acidic environment of the female vagina
The prostate is a walnut-sized gland (see Figs. 5-9 and 5-11 and Table 5-5) that surrounds the proximal urethra. The prostate exhibits the following features:
- Contributes fluid to the ejaculate; produces about 20% of the ejaculate volume
- Produces a thin, milky, slightly alkaline fluid that helps to liquefy coagulated semen after it is deposited in the female vagina; contains citric acid, proteolytic enzymes, sugars, phosphate, and various ions
There are about 2 to 6 mL of semen and approximately 150 to 600 million spermatozoa in each ejaculation. The pH is between 7 and 8.
C L I N I C A L F O C U S
Vasectomy
Vasectomy offers birth control with a failure rate below that of the pill, condom, intrauterine device, and tubal ligation. It can be performed as an office procedure with a local anesthetic. (Approximately 500,000 are performed each year in the United States.) One approach uses a small incision on each side of the scrotum to isolate the vas deferens; another uses a small puncture (no incision) in the scrotal skin to isolate both the right and left vas. The muscular vas is identified, and a small segment is isolated between two small metal clips or sutures. The isolated segment is resected, the clipped ends of the vas are cauterized, and the incision is closed (or, in the non-incisional approach, the puncture wound is left unsutured).
C L I N I C A L F O C U S
Testicular Cancer
Testicular tumors are heterogeneous neoplasms, 95% of them arising from germ cells and almost all being malignant. Of the germ cell tumors, 60% show mixed histological features, and 40% show a single histological pattern. Surgical resection usually is performed using an inguinal approach (radical inguinal orchiectomy) to avoid spread of the cancer to the adjacent scrotal tissues.
Additional figures available online. See Table of Contents for Instructions for online access.

C L I N I C A L F O C U S
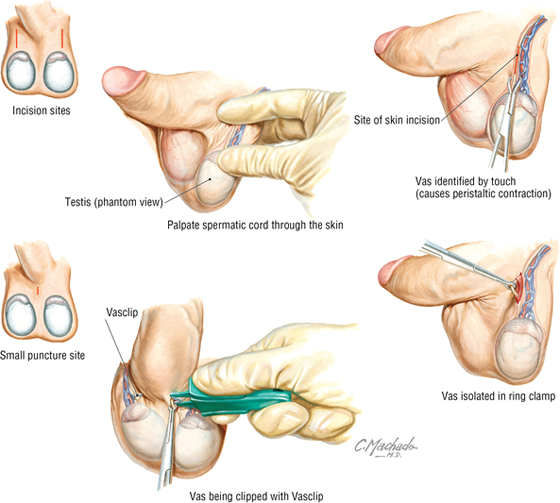
Hydrocele and Varicocele
The most common cause of scrotal enlargement is hydrocele, an excessive accumulation of serous fluid within the tunica vaginalis (usually a potential space). An infection in the testis or epididymis, trauma, or a tumor may lead to hydrocele, or it may be idiopathic. Varicocele is an abnormal dilation and tortuosity of the pampiniform venous plexus. Almost all varicoceles are on the left side. This is perhaps because the left testicular vein drains into the left renal vein (which has a slightly higher venous pressure) rather than into the larger inferior vena cava (as the right testicular vein does). A varicocele is evident at physical examination when a patient stands, but it usually resolves when the patient is recumbent.
C L I N I C A L F O C U S
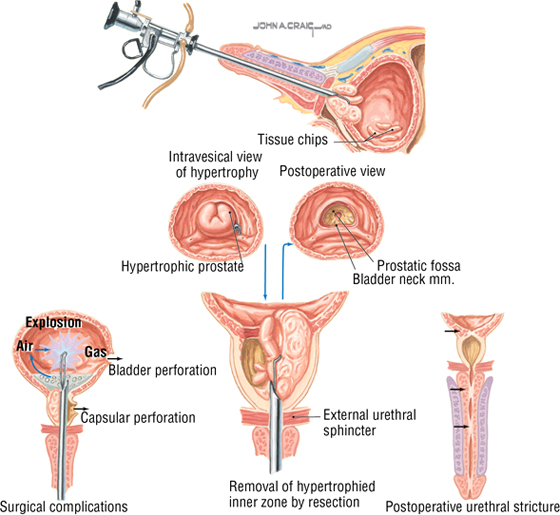
Transurethral Resection of the Prostate
Benign prostatic hypertrophy is fairly common (20% of males by the age of 40 years), and its occurrence increases with age (90% of males older than 80 years of age). It is really a nodular hyperplasia, not hypertrophy. It results from the proliferation of epithelial and stromal tissues, often in the periurethral area. This growth can lead to symptoms that may include urinary urgency, decreased stream force, frequency, and nocturia. Symptoms may necessitate transurethral resection of the prostate (TURP), in which the obstructing periurethral part of the gland is removed via a resectoscope. Although relatively rare, several surgical complications are illustrated.
C L I N I C A L F O C U S
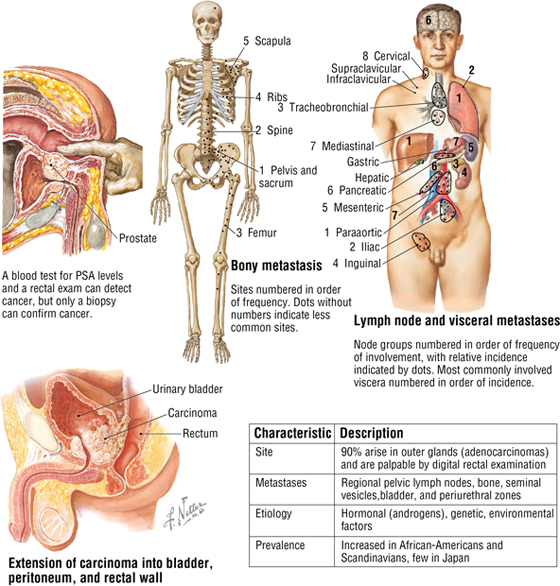
Prostatic Carcinoma
Prostatic carcinoma is the most common visceral cancer in males and the second leading cause of death in men older than 50 years of age. (Lung cancer is first.) Primary lesions invade the prostatic capsule and then spread along the ejaculatory ducts into the space between the seminal vesicles and bladder. The pelvic lymphatics and rich venous drainage of the prostate (prostatic venous plexus) facilitate the metastatic spread of the cancer to distant sites.
Pelvic Fascia in Both Sexes
The pelvic fascia covers the lateral pelvic walls, envelops the neurovascular bundles, and condenses around the pelvic viscera, forming significant support structures, especially in the female. The major fascial condensations in the female include the following (Fig. 5-12):
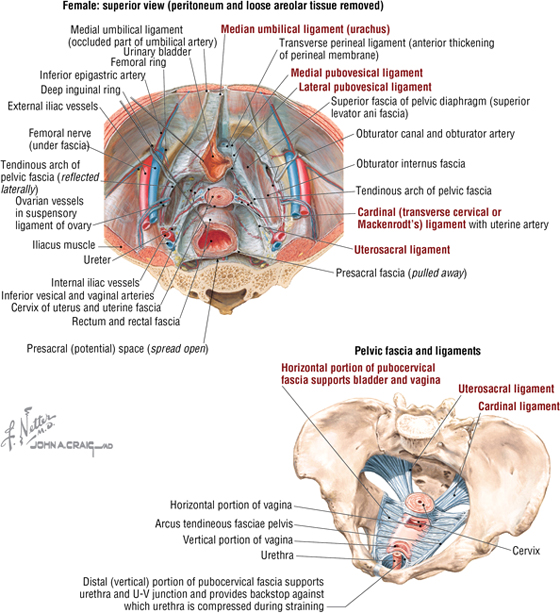
FIGURE 5-12 Endopelvic Fascia in the Female
- Median umbilical ligament: mid-sagittal anterior ligament in both sexes that extends to the umbilicus (a remnant of the urachus)
- Medial pubovesical ligament: connects the bladder to the pubis in both sexes
- Lateral ligament of the bladder (pubovesical): provides lateral support that conveys the superior vesical vessels in both sexes
- Pubocervical ligaments: fascial condensations that course from the cervix to the anterior pelvic wall
- Transverse cervical ligaments (also called cardinal, lateral cervical, or Mackenrodt ligaments): provide important posterolateral support of the uterus and convey the uterine vessels
- Uterosacral ligaments: fascial condensations that course from the cervix posteriorly to the pelvic walls
- Rectovaginal septum: fascial condensations between the rectum and vagina
The same ligaments that support the female urinary bladder also support the male bladder. Additionally, males have a fascial condensation called the prostatic fascia that surrounds the anterolateral aspect of the prostate gland, envelops the prostatic venous plexus, and extends posteriorly to envelop the prostatic arteries and nerve plexus (rectoprostatic septum or Denonvilliers’ fascia) (Fig. 5-9).
- Covers the pelvic viscera in both sexes and forms the broad ligament in females
- Forms the median umbilical (urachus) fold and the medial umbilical folds (remnants of the fetal umbilical arteries) in both sexes
- Forms the vesicouterine and rectouterine (pouch of Douglas) pouches in females
- Forms the rectovesical pouch in males
- Forms the uterosacral fold in females and the vesicosacral fold in males
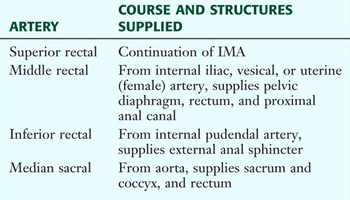
5. BLOOD SUPPLY
The arterial supply to the pelvis arises from the paired internal iliac arteries, which not only supply the pelvis but also send branches into the perineum, the gluteal region, and the medial thigh. The arteries in the female pelvis are shown in Figure 5-13 and summarized in Table 5-6.
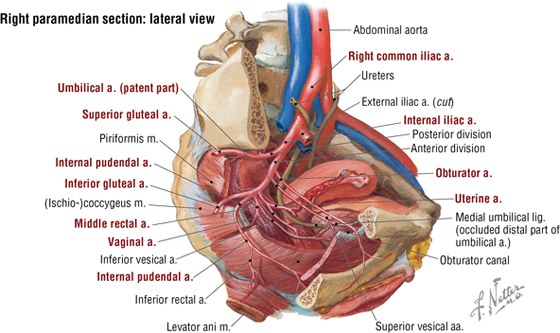
FIGURE 5-13 Pelvic Arteries in the Female
|
TABLE 5-6 Branches of the Female Pelvic Arteries
|
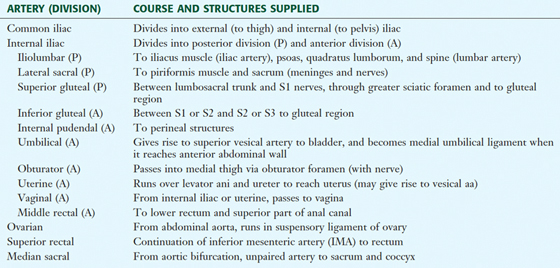 |
The arteries in the male are similar, except that the uterine, vaginal, and ovarian branches are replaced by arteries to the ductus deferens (from a vesical branch), the prostatic artery (from the inferior vesical artery), and the testicular arteries (from the abdominal aorta). Significant variability exists for these arteries, so they are best identified and named for the structure they supply. Corresponding veins, usually multiple, course with each of these arterial branches and drain into the internal iliac vein directly or into other larger veins. (Multiple connections among veins are common.) Extensive venous plexuses are associated with the bladder, rectum, vagina, uterus, and prostate (commonly just referred to as the pelvis plexus of veins). Those veins surrounding the rectum form an important portocaval anastomosis via the superior (portal) rectal and the middle and inferior (caval) rectal veins (see Figs. 4-26 and 5-18).
6. LYMPHATICS
Much of the lymphatic drainage of the pelvis parallels the venous drainage and drains into lymph nodes along the internal iliac vessels (Fig. 5-14 and Table 5-7). The major exception to this rule is the drainage from the ovaries and the adjacent uterine tubes and upper uterus, and the testes and scrotal structures, which flows directly back to the aortic (lumbar) nodes of the mid-abdomen.
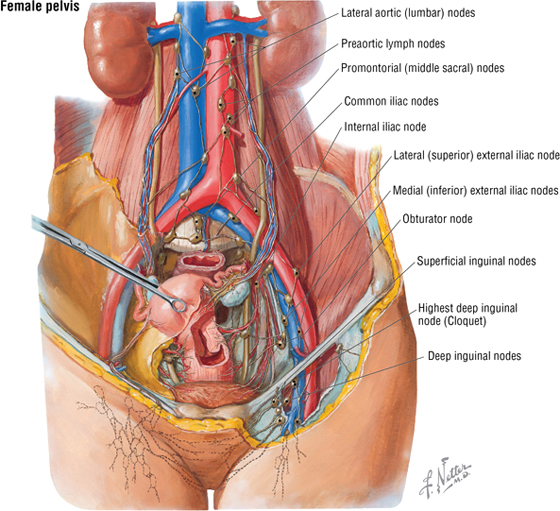
FIGURE 5-14 Lymphatics of the Pelvis
|
TABLE 5-7 Pelvic Lymphatics
|
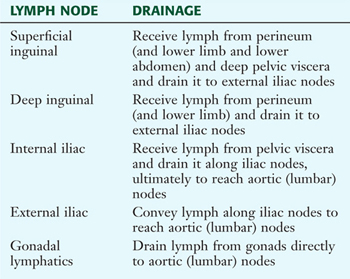 |
7. INNERVATION
The skin and skeletal muscle of the pelvis are innervated by the somatic division of the peripheral nervous system. The muscle innervation is reviewed in Table 5-2 and is derived from the ventral rami of the sacral (L4-S4) and coccygeal plexus. Although most of the sacral plexus is involved in innervation of the gluteal muscles and muscles of the lower limb, several small twigs innervate the pelvic musculature (nerve to the obturator internus and nerves to the pelvic diaphragm) and the perineum, which is supplied by the pudendal nerve (S2-S4). Somatic afferent fibers convey pain, touch, and temperature from the skin, skeletal muscle, and joints via nerves from these plexuses to the same relative spinal cord levels.
The smooth muscle and glands of the pelvis are innervated by the autonomic division of the peripheral nervous system via the pelvic splanchnics (S2-S4; parasympathetic) and the lumbar and sacral splanchnics (L1-L2; sympathetic) (Fig. 5-15 and Table 5-8).
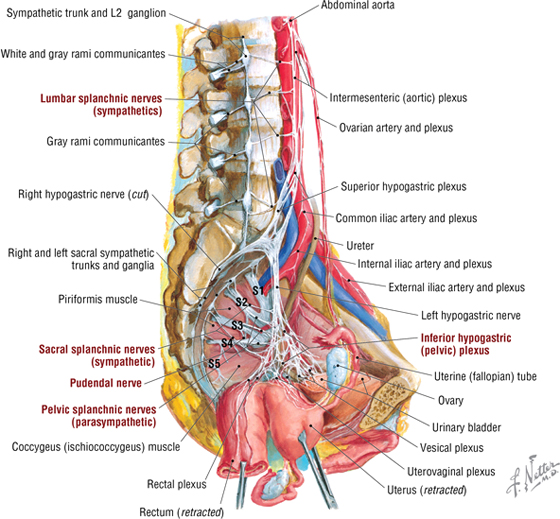
FIGURE 5-15 Nerves of the Pelvic Cavity
|
TABLE 5-8 Summary of Pelvic Nerves
|
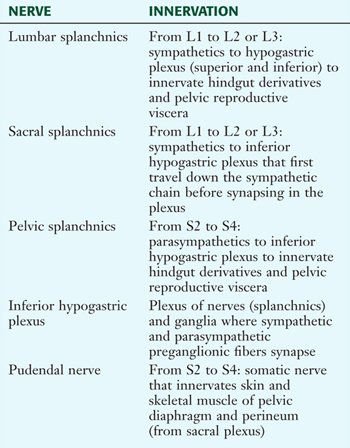 |
- Vasodilate
- Contract the bladder’s detrusor smooth muscle
- Stimulate engorgement of the erectile tissues
- Modulate the enteric nervous system’s control of the distal bowel (from splenic flexure to the rectum)
- Inhibit contraction of both the male internal urethral sphincter for urination and the internal anal sphincter for defecation in both sexes
The sympathetic efferent fibers generally do the following:
- Vasoconstrict and/or maintain vasomotor tone
- Increase secretion from sweat glands
- Contract the male internal urethral sphincter and the internal anal sphincters in both sexes
- Via smooth muscle contraction, move the sperm along the male reproductive tract and stimulate secretion from the seminal vesicles and prostate
- Stimulate secretion from the greater vestibular (Bartholin’s) glands in females and the bulbourethral (Cowper’s) glands in males, along with minor lubricating glands associated with the reproductive tract in both sexes
Visceral afferent fibers convey pelvic sensory information (largely pain) via both the sympathetic fibers (to the upper lumbar spinal cord [L1-L2] or lower thoracic levels [T11-T12]) and parasympathetic fibers (to the S2-S4 levels of the spinal cord).
8. FEMALE PERINEUM
The perineum is a diamond-shaped region between the thighs and is divided descriptively into an anterior urogenital (UG) triangle and a posterior anal triangle (Fig. 5-16). The boundaries of the perineum include the following:
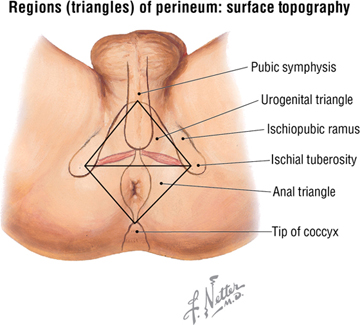
FIGURE 5-16 Subdivisions of the Perineum
- Pubic symphysis anteriorly
- Ischial tuberosities laterally (lateral margins are demarcated by the ischiopubic rami anteriorly and the sacrotuberous ligaments posteriorly) (see Fig. 5-3)
- Coccyx posteriorly
- Roof formed largely by the levator ani muscle
Anal Triangle (Both Sexes)
The key feature of the anal triangle is the anal opening and the external anal sphincter, which has the following attachments (Fig. 5-17):
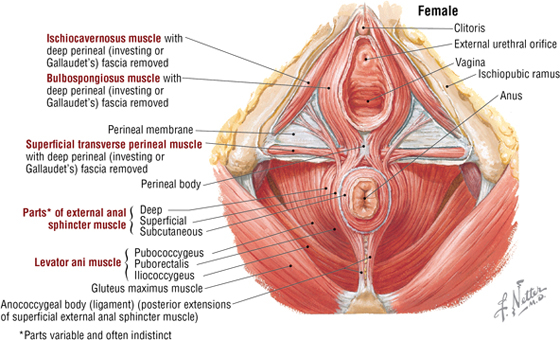
FIGURE 5-17 Muscles of the Female Perineum
- Subcutaneous part: just beneath the skin
- Superficial part: attaches to the perineal body and coccyx
- Deep part: surrounds the anal canal
Similar to the skin and all the skeletal muscles of the perineum, the external anal sphincter is innervated by the pudendal nerve (S2-S4) (inferior rectal branches) (see Fig. 5-22) from the sacral plexus and supplied by the internal pudendal artery (rectal branches), a branch of the internal iliac artery in the pelvis (see Fig. 5-13). The venous drainage of the lower rectum and anal canal provides an important portocaval anastomosis between the superior rectal vein (portal system) and the median sacral vein and middle and inferior rectal branches (caval system) (Fig. 5-18) (Table 5-9).
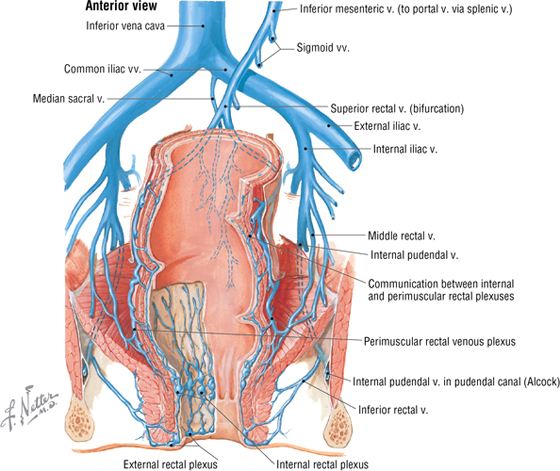
FIGURE 5-18 Veins of the Rectum and Anal Canal
|
TABLE 5-9 Rectal Portocaval Anastomoses
|
 |
The anal canal and external anal sphincter is flanked on either side by a wedge-shaped, fat-filled space called the ischioanal (ischiorectal) fossae (Fig. 5-19). This space allows for the expansion of the anal canal during defecation and accommodates the fetus during childbirth.
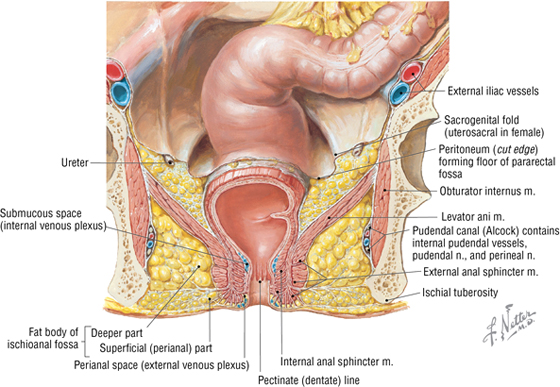
FIGURE 5-19 Anal Canal and Ischioanal Fossae
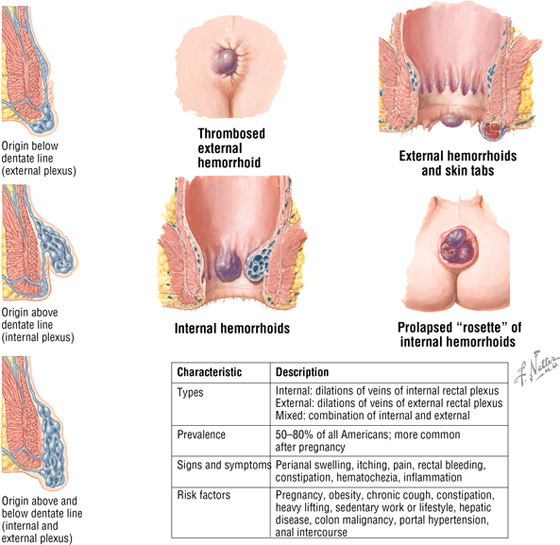
C L I N I C A L F O C U S
Hemorrhoids
Hemorrhoids are symptomatic varicose dilations of submucosal veins that protrude into the anal canal and/or extend through the anal opening (external hemorrhoid). Hemorrhoids can bleed, causing the blood to pool and clot, yielding a “thrombosed” hemorrhoid.
Urogenital Triangle
The UG triangle is divided into a superficial pouch (contains the external genitalia and associated skeletal muscles) and a deep pouch (largely occupied by the urethrovaginalis skeletal muscle sphincter complex surrounding the urethra and vaginal apertures). Superior to the deep pouch lies the levator ani muscle, with an intervening anterior extension of the ischioanal fossae (fat) separating the deep pouch and muscle. The female external genitalia (vulva) are shown in Figure 5-20 and summarized in Table 5-10.
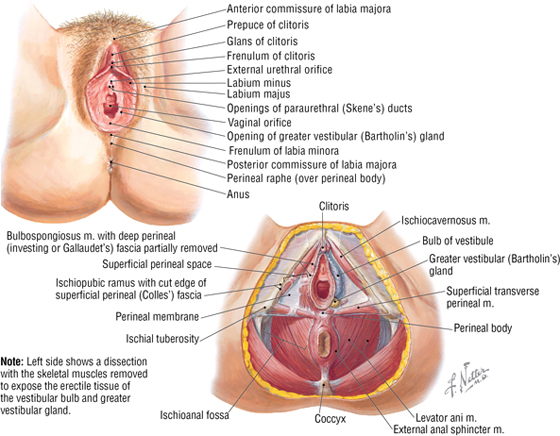
FIGURE 5-20 Female Perineum and Superficial Perineal Pouch
|
TABLE 5-10 Features of the Female External Genitalia
|
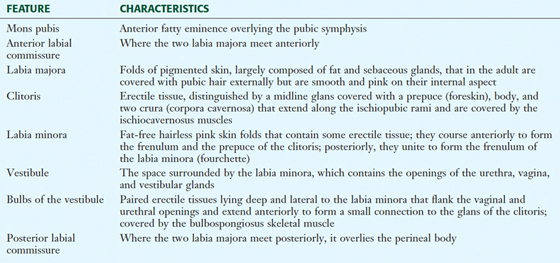 |
C L I N I C A L F O C U S
Episiotomy
Occasionally, if there is danger of tearing of the perineal body during childbirth, the physician may perform an incision, called an episiotomy, to enlarge the vaginal opening to accommodate the head of the fetus. The incision is easier to repair and heals better than a tear. Episiotomies usually are either directly in the midline through the perineal body or posterolateral, to avoid the perineal body.
Additional figures available online. See Table of Contents for Instructions for online access.

The perineal body (central tendon of the perineum) is an important fibromuscular support region lying just beneath the skin midway between the two ischial tuberosities and an important attachment point for the perineal muscles, especially the urethrovaginalis complex in women, and the levator ani superiorly (see Fig. 5-20).
The deep perineal pouch contains the following (Fig. 5-21):
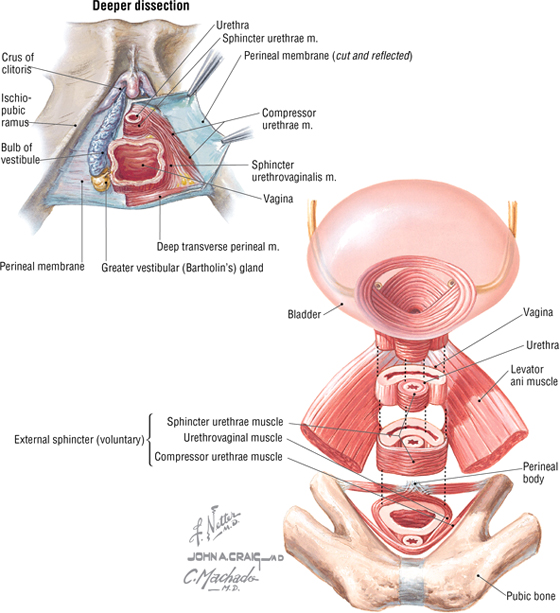
FIGURE 5-21 Female Perineum and Urethrovaginalis Sphincter Complex
- Urethra: extends from the bladder, runs through the deep pouch, and opens into the vestibule
- Vagina: distal portion passes through the deep pouch and opens into the vestibule
- External urethral sphincter: skeletal muscle sphincter
- Compressor urethrae: two thin skeletal muscle bands extend from the ischiopubic rami and fuse in the midline around the anterior aspect of the urethra
- Sphincter urethrovaginalis: extends from the perineal body around the lateral sides of the vagina and fuses in the midline around the anterior aspect of the urethra
- Deep transversus perineal muscles: extend from the ischiotuberosities and rami to the perineal body; stabilize the perineal body
These structures, along with their respective neurovascular bundles, lie between the perineal membrane (thick fascial sheath) and the fascia covering the inferior aspect of the levator ani. The neurovascular components include the following (Fig. 5-22):
- Pudendal nerve: somatic innervation (S2-S4) of the skin and skeletal muscles of the perineum; includes the inferior rectal (anal), perineal, labial, and dorsal clitoral branches
- Internal pudendal artery: arises from the internal iliac artery, passes out the greater sciatic foramen around the sacrospinous ligament and into the lesser sciatic foramen to enter the pudendal (Alcock’s) canal, and distributes to the perineum as the inferior rectal, perineal, labial, artery of the bulb, and dorsal clitoral branches
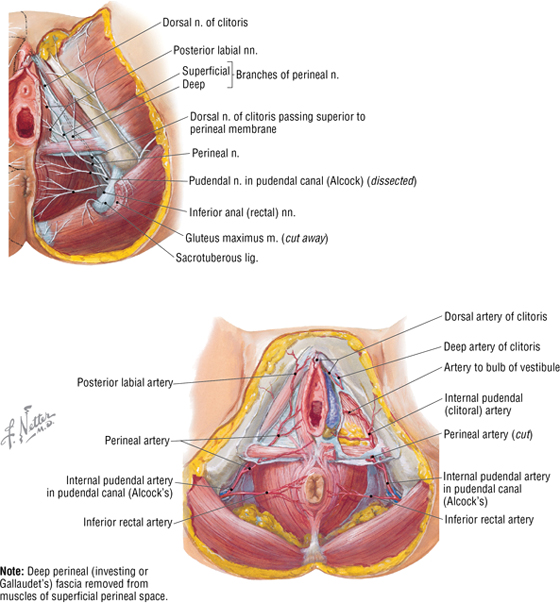
FIGURE 5-22 Neurovascular Supply to the Female Perineum
C L I N I C A L F O C U S
Sexually Transmitted Diseases
HPV (human papillomavirus) and Chlamydia trachomatis infections are the two most common STDs in the United States. HPV infections (>90% of which are benign) are characterized in both sexes by warty lesions caused most often by serotypes 6 and 11. The virus is commonly spread by skin-to-skin contact; the incubation period is 3 weeks to 8 months. HPV is highly associated with cervical cancer in women. Chlamydia is the most common bacterial STD, with antibodies present in up to 40% of all sexually active women (which suggests prior infection). Infected structures include the urethra, cervix, greater vestibular glands, and uterine tubes in females, and the urethra, epididymis, and prostate in males. A common risk factor for both STDs is having multiple sexual partners.
9. MALE PERINEUM
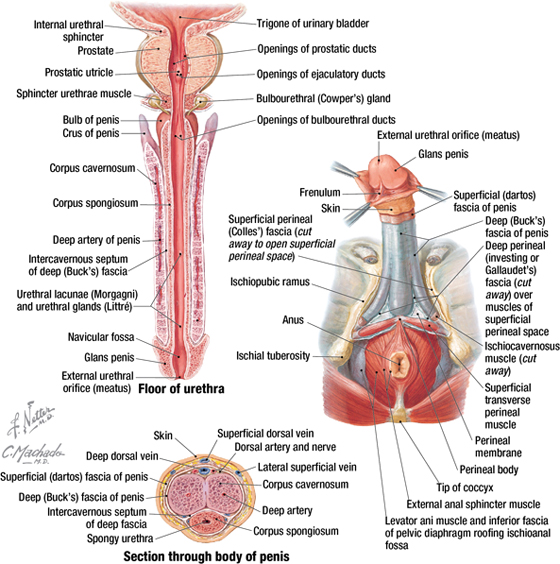
The boundaries of the perineum and the anal triangle in both sexes have been discussed in the previous section; this section will focus of the male UG triangle. The UG triangle is divided into a superficial pouch (contains the external genitalia and associated skeletal muscles) and a deep pouch (largely occupied by the external urethral sphincter surrounding the membranous urethra). The male external genitalia are shown in Figure 5-23 and summarized in Table 5-11.
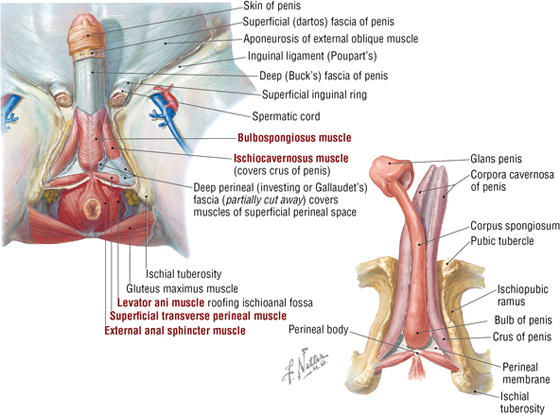
FIGURE 5-23 Male Perineum, Superficial Pouch, and Penis
|
TABLE 5-11 Features of the Male External Genitalia
|
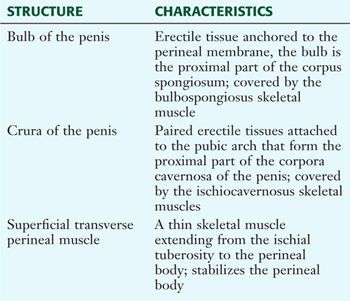 |
The bulb and crura form the root of the penis, whereas the corpus spongiosum and the two corpora cavernosa compose the shaft of the penis. They are bound tightly together by the investing deep (Buck’s) fascia of the penis and a superficial (dartos) fascia of the penis.
The superficial fascia (subcutaneous tissue) of the perineum includes a fatty and membranous layer (Colles fascia) similar to the anterior abdominal wall (Fig. 5-24). In the female, the fatty layer contributes to the labia majora and mons pubis, but it is minimal in the male. In the latter, the membranous layer of the superficial fascia (called Scarpa’s fascia on the abdominal wall but Colles fascia in the perineum) is continuous with the dartos (smooth muscle) fascia of the penis and scrotum and envelops the superficial perineal pouch, thus providing a potential conduit for fluids or infections from the superficial pouch to the lower abdominal wall. The deep perineal (Gallaudet) fascia invests the ischiocavernosus, bulbospongiosus, and superficial transverse perineal muscles in both sexes and is continuous with the deep (Buck’s) fascia of the penis and the deep investing fascia of the external abdominal oblique muscle and rectus sheath (Fig. 5-25).
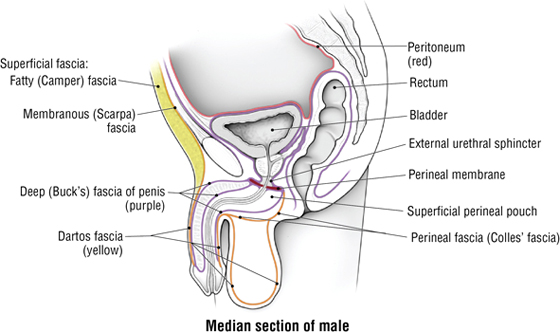
FIGURE 5-24 Fasciae of the Male and Female Pelvis and Perineum (Contd.)
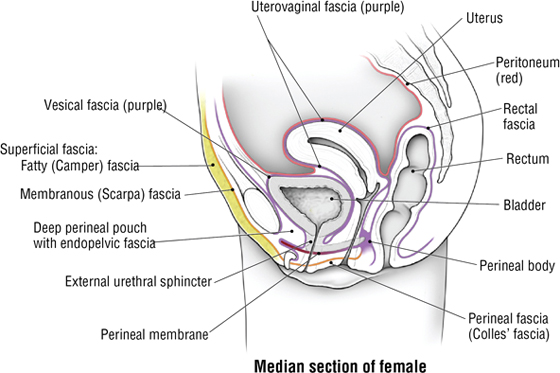
FIGURE 5-24 (Contd.) Fasciae of the Male and Female Pelvis and Perineum
FIGURE 5-25 Penis and Urethra
Features of the penis are summarized in Table 5-12 and illustrated in Figure 5-25.
|
TABLE 5-12 Features of the Penis
|
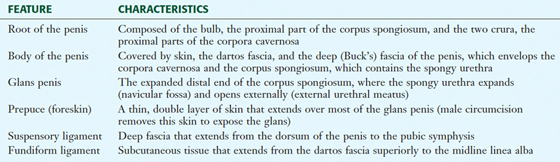 |
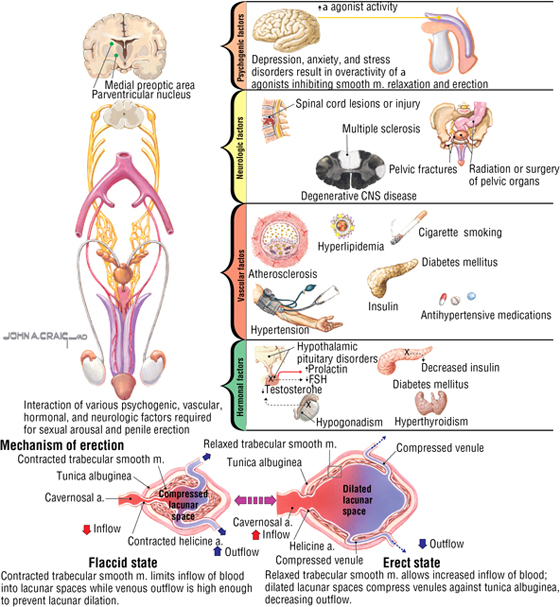
Erection of the penis (and clitoris in the female) and ejaculation involve the following sequence of events:
- Friction and sexual stimulation evokes the excitation of parasympathetic fibers (pelvic splanchnics S2-S4), which leads to vasodilation of the cavernous vessels and engorgement of the erectile tissue with blood
- Sympathetic fibers then initiate contraction of the smooth muscle of the epididymal ducts, ductus deferens, seminal vesicles, and prostate, in that order
- Sperm and the seminal and prostatic secretions enter the prostatic urethra, where they are combined with secretions of the bulbourethral and penile urethral glands (semen)
- Under sympathetic stimulation (L1-L2), the internal urethral sphincter contracts to prevent ejaculation into the urinary bladder; with rhythmic contractions of the bulbospongiosus muscle (via somatic stimulation from the pudendal nerve), the semen moves along the spongy urethra (parasympathetic stimulation of urethral smooth muscle helps move the semen through the spongy urethra) and is ejaculated (orgasm)
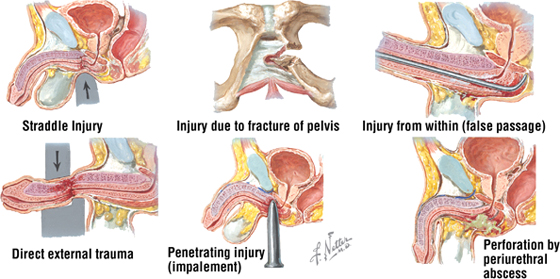
C L I N I C A L F O C U S
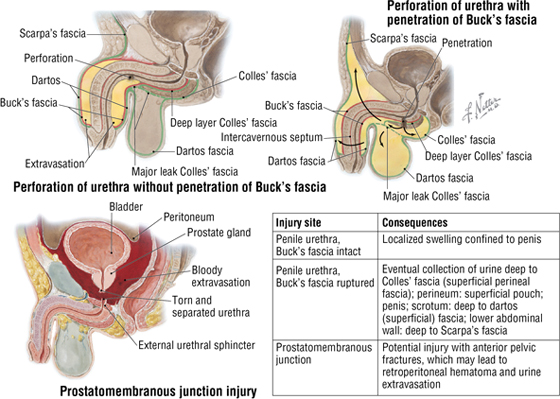
Urethral Trauma in the Male
Although rare, direct trauma to the corpora cavernosa can occur. Rupture of the thick tunica albuginea usually involves the deep fascia of the penis (Buck’s fascia), and blood can extravasate quickly, causing penile swelling. Urethral rupture is more common and involves one of three mechanisms:
- External trauma or a penetrating injury
- Internal injury (caused by a catheter, instrument, or foreign body)
- Spontaneous rupture (caused by increased intraurethral pressure or periurethral inflammation)
C L I N I C A L F O C U S
Urine Extravasation in the Male
Rupture of the male urethra can lead to urine extravasation into various pelvic or perineal spaces that are largely limited by the fascial planes.
C L I N I C A L F O C U S
Erectile Dysfunction
Erectile dysfunction (ED) is an inability to achieve and/or maintain penile erection sufficient for sexual intercourse. Its occurrence increases with age, and some of the probable causes are illustrated. Normal erectile function occurs when a sexual stimulus causes the release of nitric oxide from nerve endings and endothelial cells of the corpora cavernosa, thus relaxing the smooth muscle tone of the vessels and increasing blood flow into the erectile tissues. As the erectile tissue becomes engorged with blood, it compresses the veins in the tunica albuginea so that the blood remains in the cavernous bodies. The available drugs to treat ED aid in relaxing the smooth muscle of the blood vessels of the erectile tissues. Erectile dysfunction can also occur from damage to the nerves innervating the perineum (e.g., a complication of prostatic surgery). Afferent impulses conveying stimulation/arousal sensations are conveyed by the pudendal nerve (S2-S4, somatic fibers), whereas the autonomic efferent innervation of the cavernous vasculature is via the pelvic splanchnics (S2-S4, parasympathetic fibers).
The deep perineal space in males includes the following (Fig. 5-26):
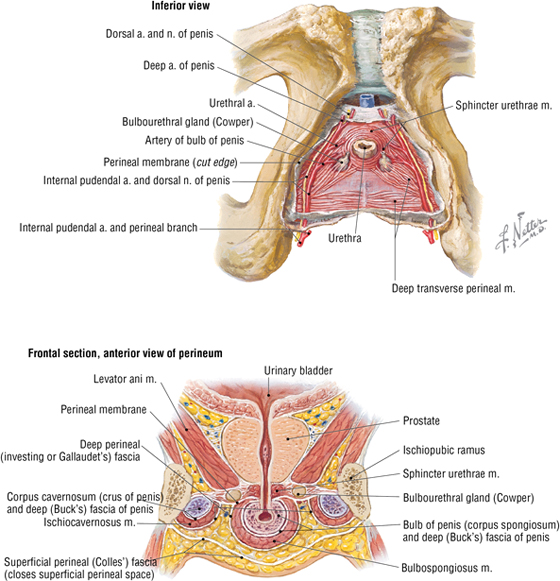
FIGURE 5-26 Deeper Structures of the Male Perineum
- Membranous urethra: a continuation of the prostatic urethra
- Deep transversus perineal muscles: extend from the ischiotuberosities and rami to the perineal body; stabilize the perineal body
- Bulbourethral glands: their ducts pass from the deep pouch to enter the proximal part of the spongy urethra; provide a mucus-like secretion that lubricates the spongy urethra
- External urethral sphincter: skeletal muscle that encircles the membranous urethra, is under voluntary control (via the pudendal nerve), and extends superiorly over the anterior aspect of the prostate gland but does not possess sphincter action on the gland
These structures, along with their respective neurovascular bundles, lie between the perineal membrane (thick fascial sheath) and the fascia covering the inferior aspect of the levator ani. The neurovascular components include the following:
- Pudendal nerve: somatic innervation (S2-S4) of the skin and skeletal muscles of the perineum; includes the inferior rectal (anal), perineal, scrotal, and dorsal nerves of the penis
- Internal pudendal artery: arises from the internal iliac artery; passes out the greater sciatic foramen with the pudendal nerve, around the sacrospinous ligament, and into the lesser sciatic foramen to enter the pudendal (Alcock’s) canal and distribute to the perineum as the inferior rectal, perineal, scrotal, and dorsal arteries of the penis as well as the artery of the bulb
10. EMBRYOLOGY
Development of the Reproductive Organs
The reproductive systems of the female and male develop from undifferentiated primordia and follow the sexual differentiation of each sex based on the genetic makeup of the embryo (XX for females and XY for males). In females, mesonephric ducts degenerate while the paramesonephric ducts develop into the uterine tubes, uterus, and upper portion of the vagina (Fig. 5-27 and Table 5-13). In males, the mesonephric ducts persist and become the ductus deferens, ejaculatory ducts, and seminal vesicles.
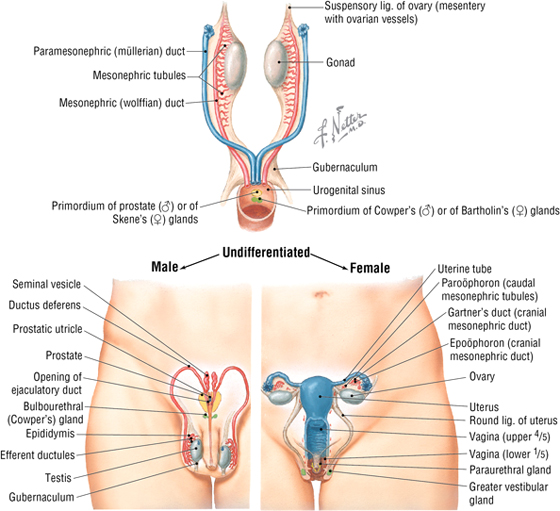
FIGURE 5-27 Derivation of the Reproductive Organs
|
TABLE 5-13 Derivatives of the Urogenital System
|
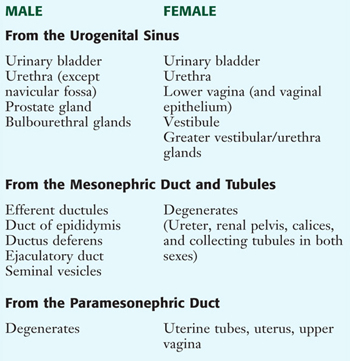 |
Development of the External Genitalia
The female and male external genitalia develop from the genital tubercle (the phallic structures), paired urogenital folds, and labioscrotal folds (Fig. 5-28 and Table 5-14).
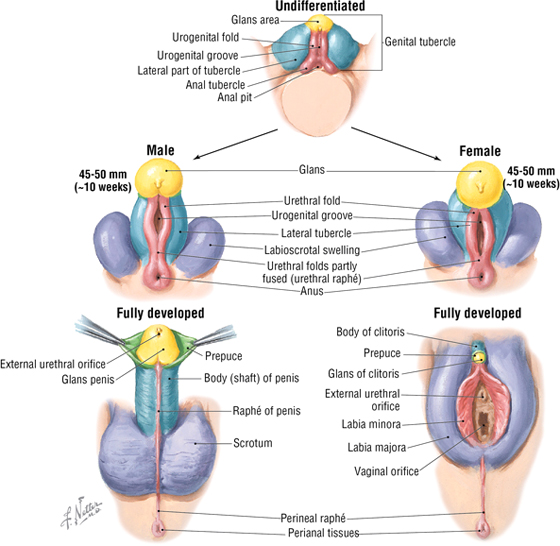
FIGURE 5-28 Development of the External Genitalia
|
TABLE 5-14 Homologues of the External Genitalia
|
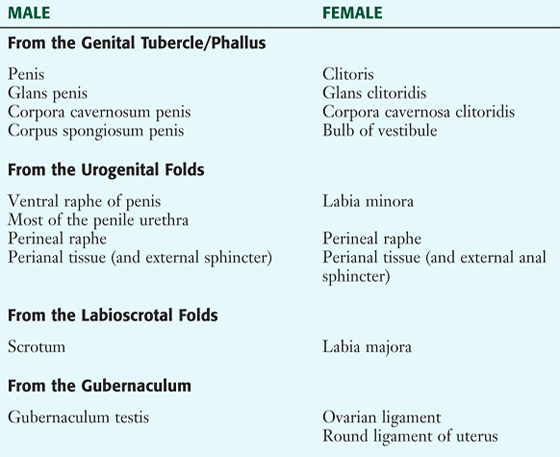 |
C L I N I C A L F O C U S
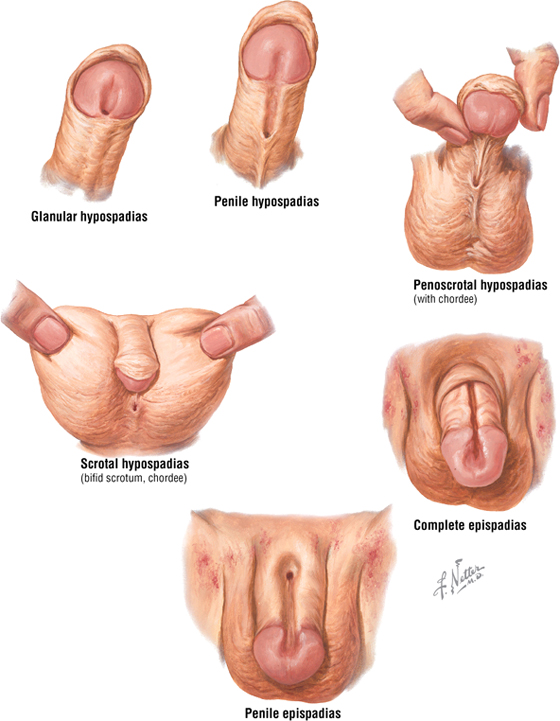
Hypospadias and Epispadias
Hypospadias and epispadias are congenital anomalies of the penis. Hypospadias is far more common (1 in 300 male births) and is characterized by failure of fusion of the urogenital folds, which normally seal the penile (spongy) urethra within the penis. The defect occurs on the ventral aspect of the penis (corpus spongiosum). Hypospadias may be associated with inguinal hernias and undescended testes. Epispadias (rare: 1 in 30,000 male births) is characterized by a urethral orifice on the dorsal aspect of the penis.
C L I N I C A L F O C U S
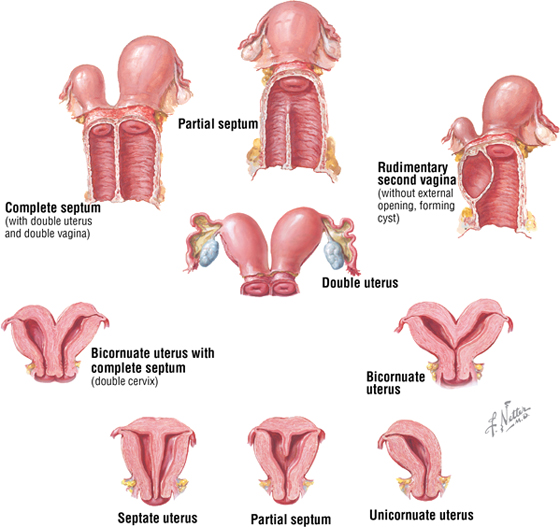
Uterine Anomalies
Incomplete fusion of the distal paramesonephric (müllerian) ducts can lead to septation of the uterus, or partial or complete duplication of the uterus (bicornuate uterus). The prevalence is up to 3% for septate uterine anomalies but only about 0.1% for bicornuate anomalies. If only one paramesonephric duct persists and develops, a unicornuate uterus results. These conditions seem to be transmitted by a polygenic or multifactorial pattern and carry a higher risk for recurrent spontaneous abortions (15% to 25%), premature labor, uterine pain, breech or transverse deliveries, and dysmenorrhea.
C L I N I C A L F O C U S
Online Figures
Ovarian tumors
Additional figures available online. See Table of Contents for Instructions for online access.