
ABDOMEN
1. INTRODUCTION
7. EMBRYOLOGY
1. INTRODUCTION
The abdomen is the region between the thorax superiorly and the pelvis inferiorly. The abdomen is composed of the following:
- Layers of skeletal muscle that line the abdominal walls and assist in respiration and (by increasing intra-abdominal pressure) facilitate micturition (urination), defecation (bowel movement), and childbirth
- The abdominal cavity, a peritoneal lined cavity that is continuous with the pelvic cavity inferiorly and contains the abdominal viscera (organs)
- Visceral structures that lie within the abdominal peritoneal cavity (intraperitoneal) and include the gastrointestinal (GI) tract and its associated organs, the spleen, and the urinary system (kidneys and ureters), which is located retroperitoneally behind and outside the cavity, but anterior to posterior abdominal wall muscles
In your study of the abdomen, first focus on the abdominal wall and note the continuation of the three muscle layers of the thorax (intercostal muscles) as they blend into the abdominal flank musculature.
Next, note the disposition of the abdominal organs. For example, you should know the region or quadrant of the abdominal cavity in which they reside; whether the organ is suspended in a mesentery or lies retroperitoneally (refer to embryology of the abdominal viscera [i.e., foregut, midgut, or hindgut derivatives]); the blood supply and autonomic innervation pattern to the organs; and features of the organs that will allow you to readily identify which organ or part of an organ you are viewing (particularly important in laparoscopic surgery). Also, you should understand the dual venous drainage of the abdomen by the caval and hepatic portal systems, and the key anastomoses between these two systems that facilitate venous return to the heart.
Finally, study the posterior abdominal wall musculature, and identify the components and distribution of the lumbar plexus of somatic nerves.
2. SURFACE ANATOMY
Key Landmarks
Key surface anatomy features of the anterolateral abdominal wall include the following (Fig. 4-1):
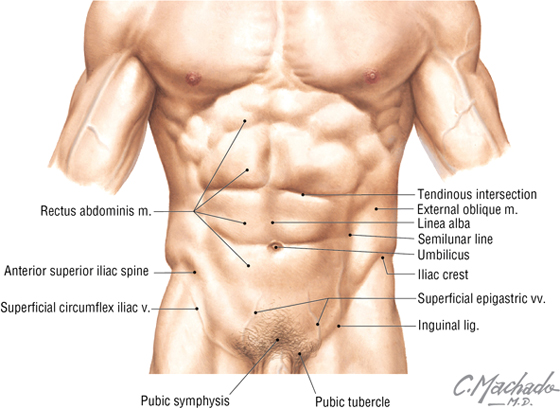
FIGURE 4-1 Key Landmarks of the Surface Anatomy of the Anterolateral Abdominal Wall
- Rectus sheath: a fascial sheath containing the rectus abdominis muscle, which runs from the pubic symphysis and crests to the xiphoid process and fifth to seventh costal cartilages
- Linea alba: literally the “white line”; a relatively avascular midline subcutaneous band of fibrous tissue where the fascial aponeuroses of the rectus sheath from each side interdigitate in the midline
- Semilunar line: the lateral border of the rectus abdominis muscle in the rectus sheath
- Tendinous intersections: transverse skin grooves that demarcate transverse fibrous attachment points of the rectus sheath to the underlying rectus abdominis muscle
- Umbilicus: the site that marks the T10 dermatome, lying at the level of the intervertebral disc between L3 and L4; the former attachment site of the umbilical cord
- Iliac crest: the rim of the ilium, which lies at about the level of the L4 vertebra
- Inguinal ligament: a ligament composed of the aponeurotic fibers of the external abdominal oblique muscle, which lies deep to a skin crease that marks the division between the lower abdominal wall and thigh of the lower limb
Surface Topography
Clinically, the abdominal wall is divided descriptively into quadrants or regions so that both the underlying visceral structures and the pain or pathology associated with those structures can be localized and topographically described. Common clinical descriptions use either quadrants or the nine descriptive regions (demarcated by two vertical midclavicular lines and two horizontal lines: the subcostal and intertubercular planes) shown in Figure 4-2 and Table 4-1.
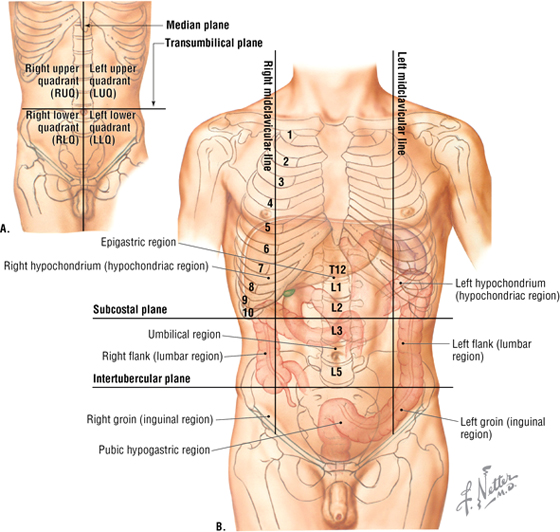
FIGURE 4-2 The Four-Quadrant (A) and Nine-Region (B) Descriptive Planes Used in Clinical Medicine
|
TABLE 4-1 Clinical Planes of Reference
|
 |
3. ANTEROLATERAL ABDOMINAL WALL
Layers
The layers of the abdominal wall include the following:
- Skin: epidermis and dermis
- Superficial fascia (subcutaneous tissue): below the umbilicus, this single layer divides into a more superficial fatty layer (Camper’s fascia) and a deeper membranous layer (Scarpa’s fascia) (see Fig. 4-11)
- Investing fascia: tissue that covers the muscle layers
- Abdominal muscles: three flat layers, similar to the thoracic wall musculature, except in the anterior mid-region where the vertically oriented rectus abdominis muscle lies in the rectus sheath
- Endoabdominal fascia: tissue that is unremarkable except for a thicker portion called the transversalis fascia, which commonly lines the inner aspect of the transversus abdominis muscle
- Extraperitoneal fat: connective tissue that is variable in thickness
- Peritoneum: thin serous membrane that lines the inner aspect of the abdominal wall (parietal peritoneum) and occasionally reflects off the walls as a mesentery to partially or completely invest various visceral structures (visceral peritoneum)
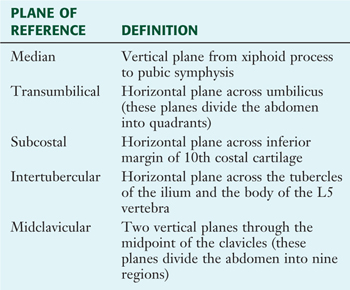
Muscles of the Anterolateral Abdominal Wall
The muscles of the anterolateral abdominal wall include three flat layers that are continuations of the three layers in the thoracic wall (Fig. 4-3). These include two abdominal oblique muscles and the transversus abdominis muscle. In the mid-region, a vertically oriented pair of rectus abdominis muscles lie within the rectus sheath and extend from the pubic symphysis and crest to the xiphoid process and costal cartilages 5 to 7 superiorly. The small pyramidalis muscle (Fig. 4-3B) is inconsistent and clinically insignificant. These muscles (except the pyramidalis) are summarized in Table 4-2.
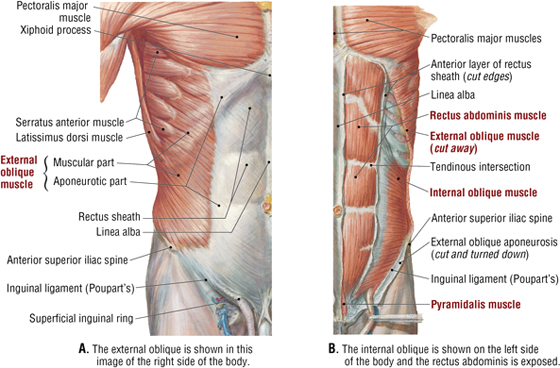
FIGURE 4-3 Muscles of the Anterolateral Abdominal Wall (Contd.)
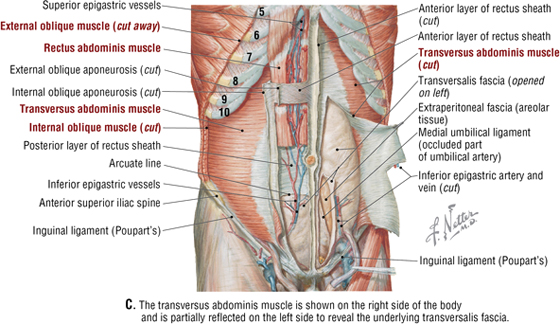
FIGURE 4-3 (Contd.) Muscles of the Anterolateral Abdominal Wall
|
TABLE 4-2 Principal Muscles of the Anterolateral Abdominal Wall
|
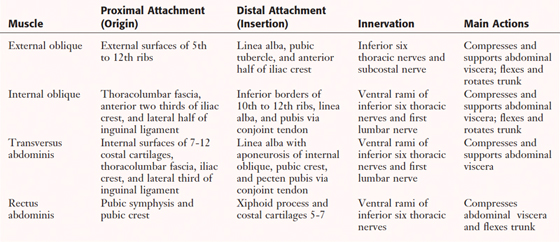 |
Rectus Sheath
The rectus sheath encloses the vertically running rectus abdominis muscle (and inconsistent pyramidalis) (Fig. 4-3B), the superior and inferior epigastric vessels, the lymphatics, and the ventral rami of T7-L1 nerves, which enter the sheath along its lateral margins (Fig. 4-3C). The superior three-quarters of the rectus abdominis is completely enveloped within the rectus sheath, while the inferior one-quarter is supported posteriorly only by the transversalis fascia, extraperitoneal fat, and the peritoneum; the site of this transition is called the arcuate line (Fig. 4-4 and Table 4-3).
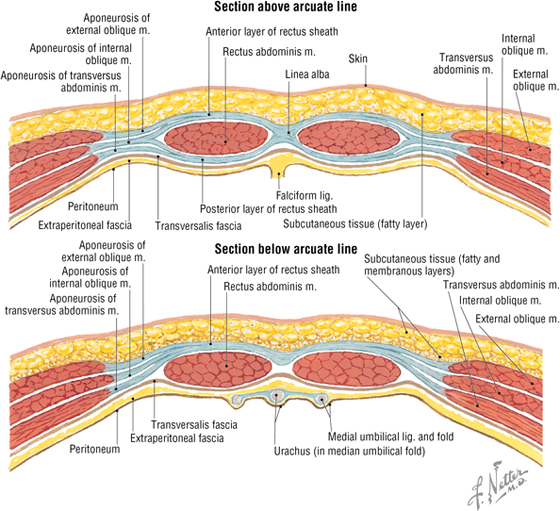
FIGURE 4-4 Features of the Rectus Sheath
|
TABLE 4-3 Aponeuroses and Layers Forming the Rectus Sheath
|
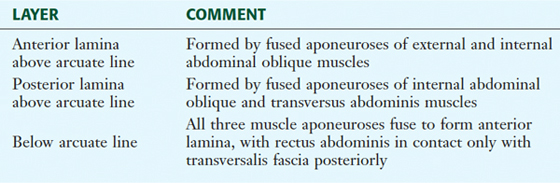 |
Innervation and Blood Supply
The segmental innervation of the anterolateral abdominal skin and muscles is by ventral rami of T6-L1. The blood supply includes the following arteries (Figs. 4-3C and 4-5):
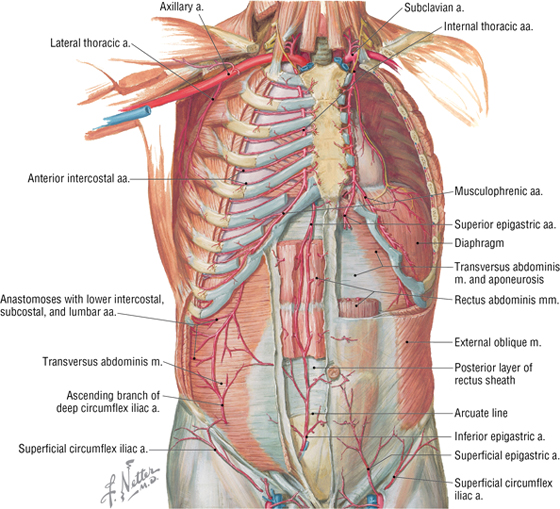
FIGURE 4-5 Arteries of the Anterolateral Abdominal Wall
- Musculophrenic: a terminal branch of the internal thoracic artery; it courses along the costal margin
- Superior epigastric: arises from the terminal end of the internal thoracic artery and anastomoses with the inferior epigastric artery at the level of the umbilicus
- Inferior epigastric: arises from the external iliac artery and anastomoses with the superior epigastric artery
- Superficial circumflex iliac: arises from the femoral artery and anastomoses with the deep circumflex iliac artery
- Superficial epigastric: arises from the femoral artery and courses toward the umbilicus
- External pudendal: arises from the femoral artery and courses toward the pubis
Superficial and deeper veins accompany these arteries, but, as elsewhere in the body, they form extensive anastomoses with each other to facilitate venous return to the heart (Fig. 4-6 and Table 4-4).
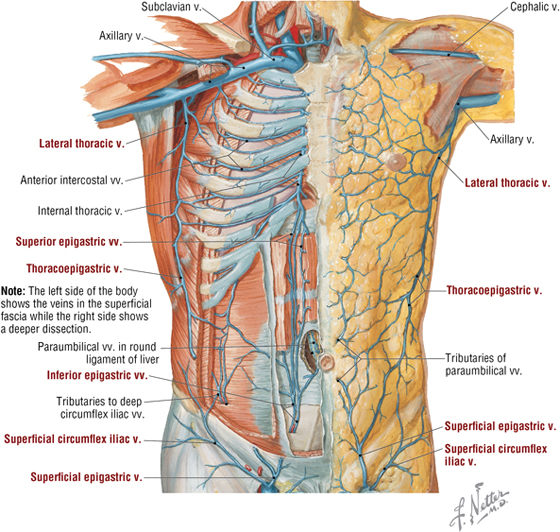
FIGURE 4-6 Veins of the Anterolateral Abdominal Wall
|
TABLE 4-4 Principal Veins of the Anterolateral Abdominal Wall
|
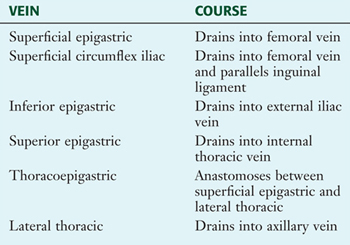 |
Lymphatic drainage of the abdominal wall parallels the venous drainage, with the lymph ultimately coursing to the following lymph node collections:
- Axillary nodes: superficial drainage above the umbilicus
- Superficial inguinal nodes: superficial drainage below the umbilicus
- Parasternal nodes: deep drainage along the internal thoracic vessels
- Lumbar nodes: deep drainage internally to the nodes along the abdominal aorta
- External iliac nodes: deep drainage along the external iliac vessels
C L I N I C A L F O C U S
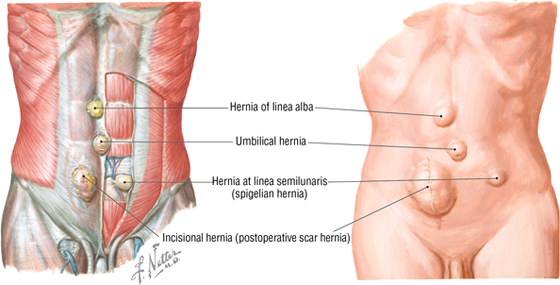
Abdominal Wall Hernias
To distinguish abdominal wall hernias, they often are called “ventral” hernias, so as not to be confused with inguinal hernias. However, all are technically abdominal wall hernias. Other than inguinal hernias, which are discussed separately, the most common types of abdominal hernias include:
- Umbilical hernia: usually seen up to the age of three and after the age of 40
- Linea alba hernia: often seen in the epigastric region, they are more common in males and rarely contain visceral structures (e.g., bowel)
- Linea semilunaris (spigelian) hernia: usually occurs in midlife and develops slowly
- Incisional hernia: occurs at the site of a previous laparotomy scar
C L I N I C A L F O C U S
Common Surgical Incisions
Although laparoscopic surgery is increasingly common, surgical access to the abdomen may still require a larger incision for some procedures. When necessary, these surgical exposures usually occur over the visceral structure of interest and may include one of the following incisions:
- Midline: a vertical incision over the linea alba; for access to the stomach, duodenum, transverse colon, or abdominal aorta
- Paramedian: a vertical incision about 1 to 1.5 inches lateral to the midline; for access to the same structures listed above
- Gridiron: usually short and in the right lower quadrant (McBurney’s point) for an appendectomy, where the muscle fibers of each layer are incised between rather than across (transection) their fibers to minimize muscle necrosis; a longer incision for access to the cecum and ascending colon
- Longer gridiron: on the left side; for access to the sigmoid colon and rectum
- Subcostal: along the inferior costal margin; for access to the gallbladder (right side) or spleen (left side)
- Suprapubic: a transverse incision just superior to the pubic hair line; for a hysterectomy or access to other pelvic viscera
4. INGUINAL REGION
The inguinal region, or groin, is the transition zone between the lower abdomen and the upper thigh. This region, especially in males, is characterized by a weakened area of the lower abdominal wall that renders this region particularly susceptible to inguinal hernias. Although inguinal hernias can occur in either sex, they are much more common in males because of the descent of the testes into the scrotum, which occurs along this boundary region.
The inguinal region is demarcated by the inguinal ligament, the inferior border of the external abdominal oblique aponeurosis, which is folded under upon itself and attaches to the anterior superior iliac spine and extends inferomedially to attach to the pubic tubercle (Figs. 4-1, 4-3B, and 4-7). Medially, the inguinal ligament flares into the crescent-shaped lacunar ligament that attaches to the pecten pubis of the pubic bone (Fig. 4-7). Fibers from the lacunar ligament also course internally along the pelvic brim as the pectineal ligament (see the clinical focus box, “Inguinal Hernias,” later in this chapter). A thickened inferior margin of the transversalis fascia, called the iliotibial tract, runs parallel to the inguinal ligament but deep to it and reinforces the medial portion of the inguinal canal (see next section).
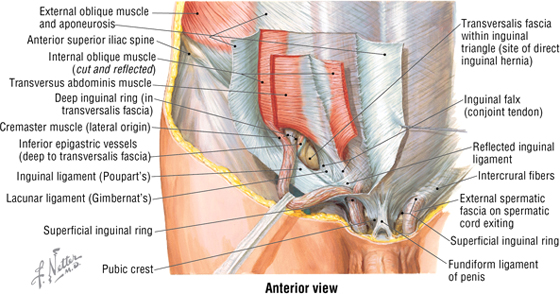
FIGURE 4-7 Adult Male Inguinal Canal and Retracted Spermatic Cord
Inguinal Canal
The gonads in both sexes initially develop retroperitoneally from a mass of intermediate mesoderm called the urogenital ridge. As the gonads begin to descend toward the pelvis, a peritoneal pouch called the processus vaginalis extends through the various layers of the anterior abdominal wall and acquires a covering from each layer except for the transversus abdominis muscle, because the pouch passes beneath this muscle layer. The processus vaginalis and its coverings form the fetal inguinal canal, a tunnel or passageway through the anterior abdominal wall. In the female, the ovaries are attached to the gubernaculum, whose other end terminates in the labioscrotal swellings (which will form the labia majora in females or the scrotum in males). The ovaries descend into the pelvis, where they remain, tethered between the lateral pelvic wall and the uterus medially (by the ovarian ligament, a derivative of the gubernaculum). The gubernaculum then reflects off the uterus as the uterine ligament, passes through the inguinal canal, and ends as a fibrofatty mass in the future labia majora.
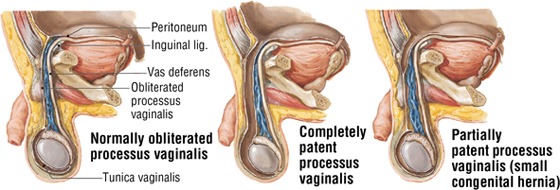
In males, the testes descend into the pelvis but then continue their descent through the inguinal canal (formed by the processus vaginalis) and into the scrotum, which is the male homologue of the female labia majora (Fig. 4-8). This descent through the inguinal canal normally occurs around the 26th week of development and usually takes several days. The gubernaculum terminates in the scrotum and anchors the testis to the floor of the scrotum. A small pouch of the processus vaginalis, called the tunica vaginalis, persists and partially envelops the testis. In both sexes, the processus vaginalis then normally seals itself and is obliterated. Sometimes this fusion doesn’t happen or is incomplete, especially in males, probably owing to the descent of the testes through the inguinal canal. Consequently, a weakness may persist in the abdominal wall that can lead to inguinal hernias.
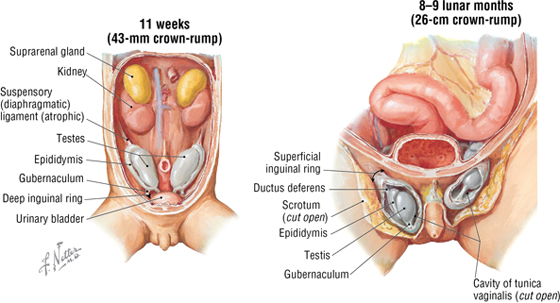
FIGURE 4-8 Fetal Descent of the Testes
As the testes descend, they bring their accompanying spermatic cord along with them and, as these structures pass through the inguinal canal, they too become ensheathed within the layers of the anterior abdominal wall (Fig. 4-9). The spermatic cord enters the inguinal canal at the deep inguinal ring (an outpouching in the transversalis fascia lateral to the inferior epigastric vessels) and exits the 4-cm-long canal via the superficial inguinal ring (superior to the pubic tubercle) before passing into the scrotum, where it suspends the testis. In the female, the only structure in the inguinal canal is the fibrofatty remnant of the round ligament of the uterus, which terminates in the labia majora. The contents in the spermatic cord include the following (see Fig. 4-9):
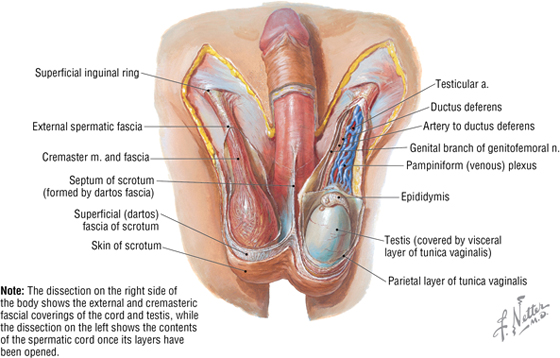
FIGURE 4-9 Layers Composing the Spermatic Cord and Its Contents
- Ductus (vas) deferens
- Testicular artery, artery of the ductus deferens, and cremasteric artery
- Pampiniform plexus of veins
- Autonomic nerve fibers (efferent and visceral afferents) coursing on the arteries and ductus deferens
- Genital branch of the genitofemoral nerve (innervates cremaster muscle)
- Lymphatics
Layers of the spermatic cord include the following (see Fig. 4-9):
- External spermatic fascia: derived from the external abdominal oblique aponeurosis
- Cremasteric (middle spermatic) fascia: derived from the internal abdominal oblique muscle
- Internal spermatic fascia: derived from the transversalis fascia
The features of the inguinal canal, including its anatomical boundaries, are shown in Figure 4-10 and summarized in Table 4-5. Note that the deep inguinal ring begins internally as an outpouching of the transversalis fascia lateral to the inferior epigastric vessels, and that the superficial inguinal ring is the opening in the aponeurosis of the external abdominal oblique muscle. Aponeurotic fibers at the superficial ring envelop the emerging spermatic cord medially (medial crus), over its top (intercrural fibers), and laterally (lateral crus) (see Fig. 4-10).
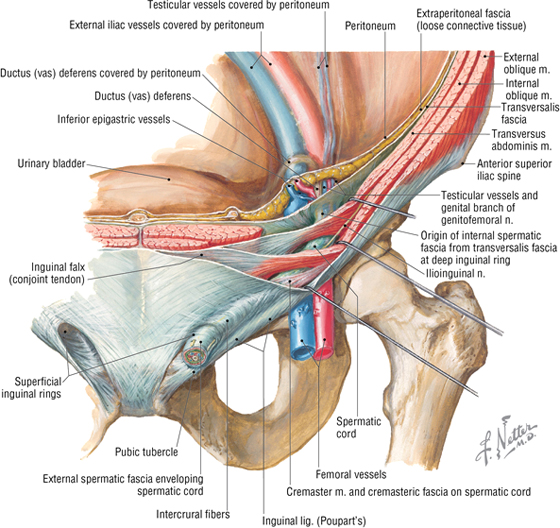
FIGURE 4-10 Features of the Inguinal Canal in the Male
|
TABLE 4-5 Features and Boundaries of the Inguinal Canal
|
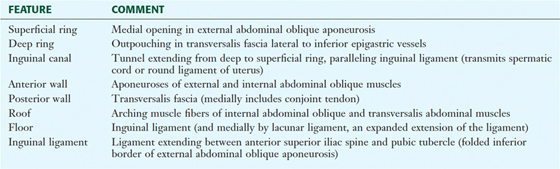 |
C L I N I C A L F O C U S
Inguinal Hernias
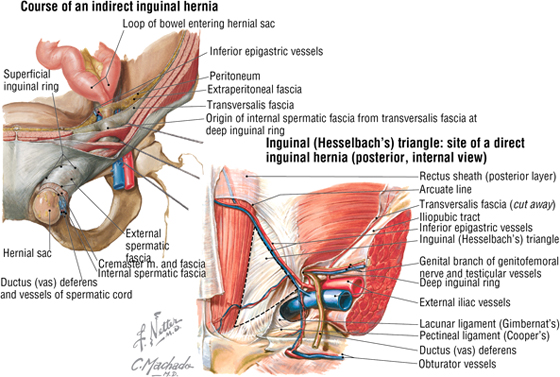
The protrusion of peritoneal contents (mesentery, fat, and/or a portion of bowel) through the abdominal wall in the groin region is termed an inguinal hernia. Inguinal hernias are distinguished by their relationship to the inferior epigastric vessels. There are two types of inguinal hernia:
Indirect (congenital) hernia: 75% of inguinal hernias occur lateral to the inferior epigastric vessels, pass through the deep inguinal ring and inguinal canal as a protrusion along the spermatic cord, and lie within the internal spermatic fascia
Direct (acquired): occurs medial to the inferior epigastric vessels, passes directly through the posterior wall of the inguinal canal, and is separate from the spermatic cord and its coverings derived from the abdominal wall
In many instances, indirect inguinal hernias arise from the incomplete closure of, or a weakness in, the processus vaginalis. The herniated peritoneal contents may extend into the scrotum (or the labia majora if it occurs in a female, although they are much less common in females) if the processus vaginalis is patent along its entire course.
Direct inguinal hernias pass through the inguinal (Hesselbach’s) triangle, demarcated internally by the inferior epigastric vessels laterally, the rectus abdominis muscle medially, and the inguinal ligament inferiorly. Often, direct hernias are more limited in the extent to which they can protrude through the inferomedial abdominal wall. They occur not because of a patent processus vaginalis but because of an “acquired” weakness in the lower abdominal wall.
C L I N I C A L F O C U S
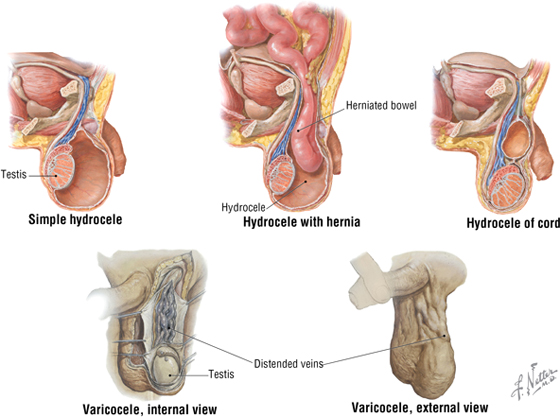
Hydrocele and Varicocele
The most common cause of scrotal enlargement is hydrocele, an excessive accumulation of serous fluid within the tunica vaginalis (usually a potential space). It is a small sack of peritoneum originally derived from the processus vaginalis that covers about two thirds of the testis. An infection (in the testis or epididymis), trauma, or a tumor may lead to a hydrocele, or it may be idiopathic.
Varicocele is an abnormal dilation and tortuosity of the pampiniform venous plexus within the spermatic cord. Almost all varicoceles are on the left side, perhaps because the left testicular vein drains into the left renal vein rather than the larger inferior vena cava, as the right testicular vein does. A varicocele is evident at physical examination when a patient stands, but it often resolves when the patient is recumbent.
5. ABDOMINAL VISCERA
Peritoneal Cavity
The abdominal viscera are contained either within a serous membrane–lined cavity called the abdominopelvic (sometimes just “abdominal” or “peritoneal”) cavity or lie in a retroperitoneal position adjacent to this cavity, often with only their anterior surface covered by peritoneum (e.g., the kidneys and ureters). The abdominopelvic cavity extends from the abdominal diaphragm inferiorly to the floor of the pelvis (Fig. 4-11).
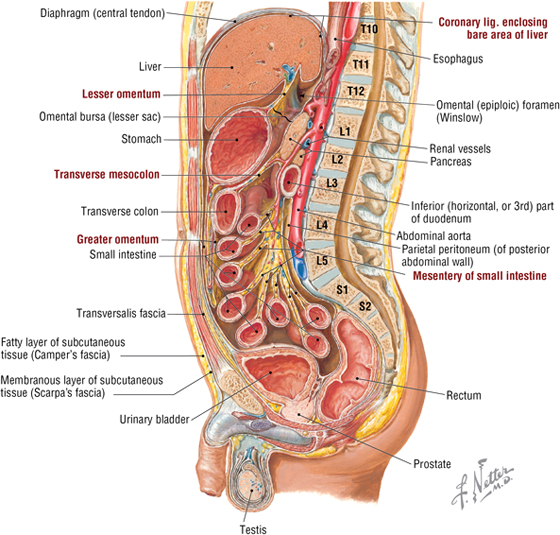
FIGURE 4-11 Sagittal Section of the Peritoneal Cavity. Observe the parietal peritoneum lining the cavity walls, the mesenteries suspending various portions of the viscera, and the lesser and greater sacs.
The walls of the abdominopelvic cavity are lined by parietal peritoneum, which can reflect off the abdominal walls in a double layer called a mesentery, which embraces and suspends a visceral structure. As the mesentery wraps around the viscera, it becomes visceral peritoneum. Viscera suspended by a mesentery are considered intraperitoneal, whereas viscera covered on only one side by peritoneum are considered retroperitoneal.
Anatomists refer to the peritoneal cavity as a “potential space,” since it normally contains only a small amount of serous fluid that lubricates its surface. If excessive amounts of fluid collect in this space due to edema (ascites) or hemorrhage, then it becomes a “real space.” Many clinicians, however, view the cavity only as a real space because it does contain serous fluid but qualify this distinction further when ascites or hemorrhage occurs.
The abdominopelvic cavity is further subdivided into the following (Figs. 4-11 and 4-12):
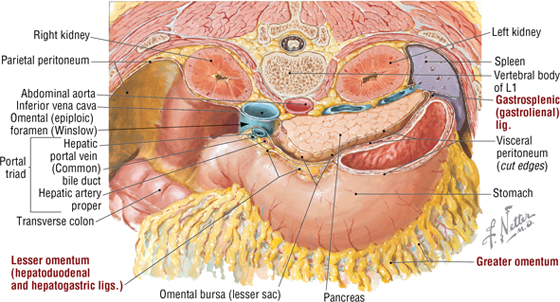
FIGURE 4-12 The Lesser Sac
- Greater sac: most of the abdominopelvic cavity
- Lesser sac: also called the omental bursa; it is an irregular part of the peritoneal cavity that forms a cul-de-sac space posterior to the stomach and anterior to the retroperitoneal pancreas; it communicates with the greater sac via the epiploic foramen (of Winslow)
C L I N I C A L F O C U S
Peritoneum: Clinical Importance
The peritoneal cavity, with its large, moist surface area and mobile visceral contents (especially the bowel), allows for the rapid and wide dissemination of infection and malignant cells throughout its extent. Moreover, if the peritoneal surfaces of the cavity become irritated and inflamed, they quickly react by forming scar tissue (peritoneal adhesions) between adjacent peritoneal layers. These adhesions can become extensive and compromise the normal mobility of visceral structures. Therefore, surgeons are careful to limit the trauma to the viscera and to keep the peritoneal surfaces moist and well-irrigated with sterile isotonic saline.
C L I N I C A L F O C U S
Peritoneal Dialysis
Because the peritoneal cavity is lined by an extensive serous membrane, clinicians can take advantage of this feature and use the peritoneal cavity as a semipermeable dialysis membrane (to exchange water and soluble substances) for patients who develop kidney failure; however, hemodialysis is more common. Dialysis fluid is intermittently introduced into and removed from the peritoneal cavity via an indwelling catheter, and molecules and electrolytes are exchanged across the peritoneal lining between this fluid and the blood based on their size and concentration gradient. Even with meticulous sterile technique, this approach often leads to infection when employed chronically.
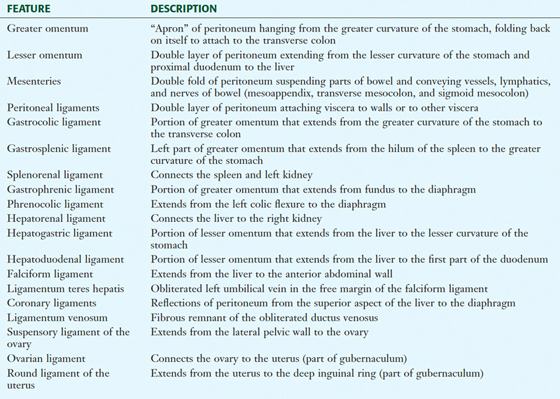
Additionally, the peritoneal cavity contains a variety of double-layered folds of peritoneum in addition to the mesenteries that suspend the bowel. These include the omenta (attached to the stomach) and peritoneal ligaments; these are not ligaments in the traditional sense, but are short, distinct mesenteries that connect structures (for which they are named) together or to the abdominal wall
(Table 4-6). Some of these structures are shown in Figures 4-11 and 4-12, and we will encounter the others later in the chapter as we describe the abdominal contents.
|
TABLE 4-6 Mesenteries, Omenta and Peritoneal Ligaments
|
 |
Abdominal Organs
Abdominal Esophagus and Stomach
The distal end of the esophagus passes through the right crus of the abdominal diaphragm at about the level of the T10 vertebra and terminates in the cardiac portion of the stomach (Fig. 4-13).
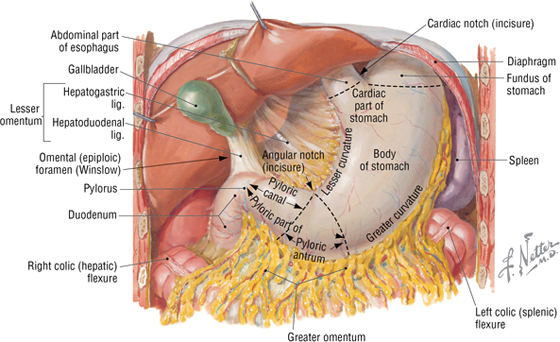
FIGURE 4-13 Abdominal Esophagus and Regions of the Stomach
The stomach is a dilated, saclike portion of the GI tract that exhibits significant variation in size and configuration, and terminates at the thick smooth muscle sphincter (pyloric sphincter) by joining the first portion of the duodenum. It is tethered superiorly by the lesser omentum (gastrohepatic ligament portion) (see Table 4-6) extending from its lesser curvature and is attached along its greater curvature to the greater omentum and the gastrosplenic ligament (see Figs. 4-12 and 4-13). Generally, the J-shaped stomach is divided into the following regions (see Fig. 4-13 and Table 4-7):
|
TABLE 4-7 Descriptive Features of the Stomach
|
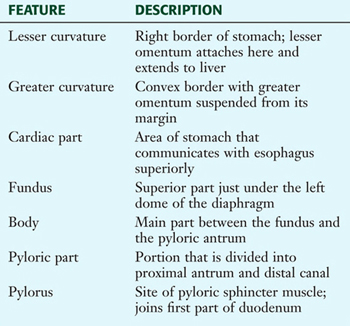 |
- Cardiac region
- Fundus
- Body
- Pyloric region (antrum and canal)
C L I N I C A L F O C U S
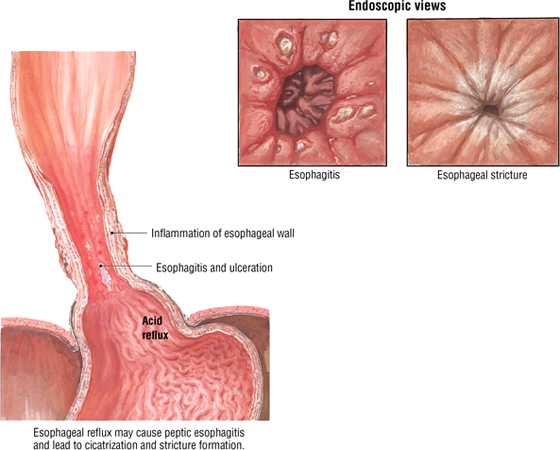
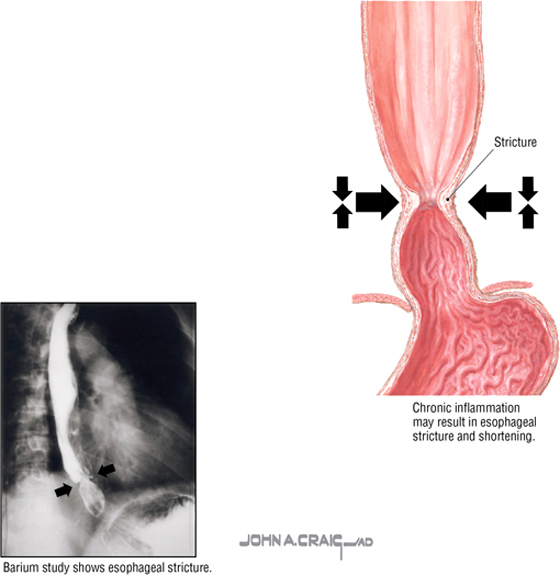
Gastroesophageal Reflux Disease (GERD)
The terminal end of the esophagus possesses a lower esophageal sphincter (specialized smooth muscle that is pharmacologically different from the smooth muscle lining the lower esophagus). It prevents the reflux of gastric contents into the lower esophagus. However, it can become compromised, usually by a loss of muscle tone or a sliding hiatal hernia, leading to GERD and inflammation of the esophageal lining. GERD often presents with upper abdominal pain, dyspepsia, gas, heartburn, dysphagia, bronchospasm (15% to 20%), or asthma (15% to 20%).
C L I N I C A L F O C U S
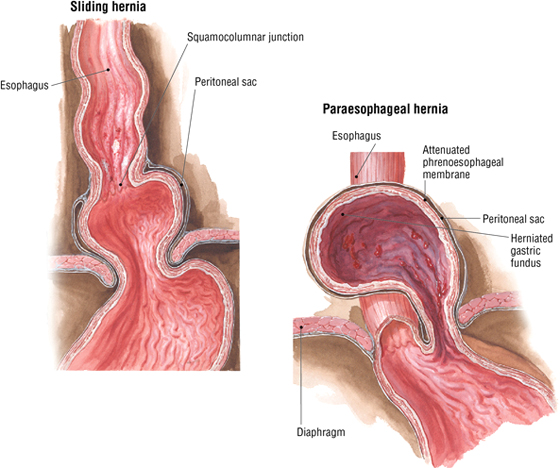
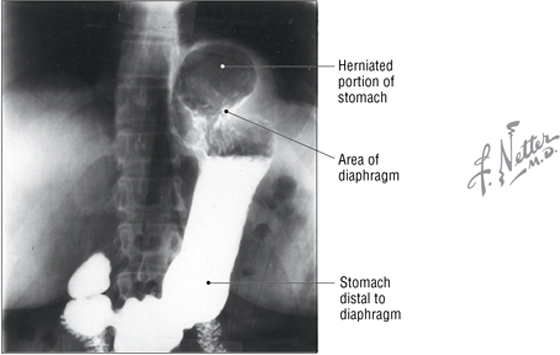
Hiatal Hernia
Herniation of the diaphragm that involves the stomach is referred to as a hiatal hernia. A widening of the space between the muscular right crus forming the esophageal hiatus allows protrusion of part of the stomach superiorly into the posterior mediastinum of the thorax. The two anatomical types are the following:
- Sliding, rolling, or axial hernia (95% of hiatal hernias): appears as a bell-shaped protrusion
- Paraesophageal, or nonaxial hernia: usually involves the gastric fundus
C L I N I C A L F O C U S
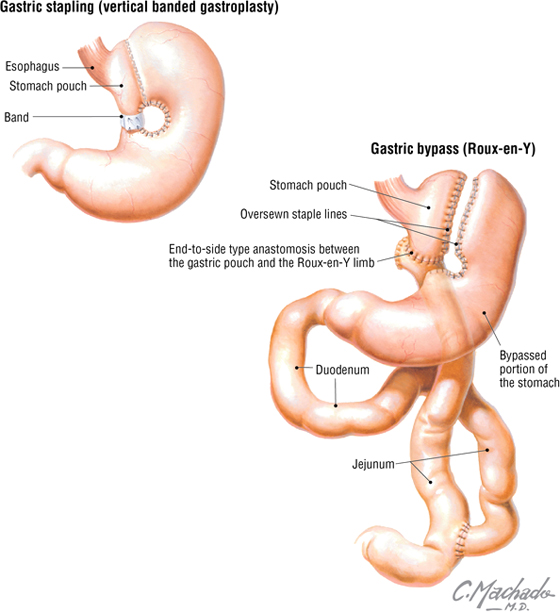
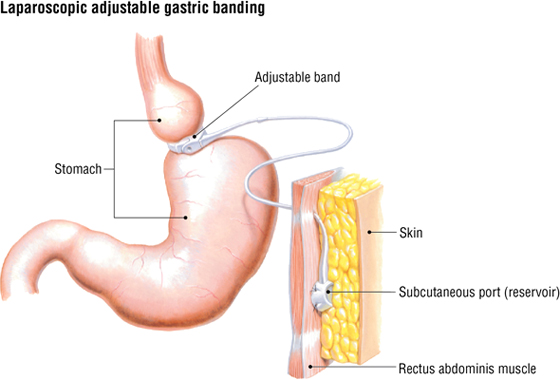
Bariatric Surgery
In some cases of morbid obesity, bariatric surgery may offer a viable alternative to failed dieting. The following three approaches may be considered:
- Gastric stapling (vertical banded gastroplasty) involves creating a small stomach pouch in conjunction with stomach stapling and banding; this approach is performed less frequently in preference to other options.
- Gastric bypass (Roux-en-Y) spares a small region of the fundus and attaches it to the proximal jejunum; the main portion of the stomach is stapled off, and the duodenum is reattached to a more distal section of jejunum, allowing for the mixture of digestive juices from the liver and pancreas.
- Adjustable gastric banding restricts the size of the proximal stomach, limiting the amount of food that can enter; the band can be tightened or relaxed via a subcutaneous access port if circumstances warrant.
The interior of the unstretched stomach is lined with prominent longitudinal mucosal gastric folds called rugae, which become more evident as they approach the pyloric region.
Small Intestine
The small intestine measures about 6 meters in length (somewhat shorter in the fixed cadaver) and is divided into the following three parts:
- Duodenum: about 25 cm long and largely retroperitoneal
- Jejunum: about 2.5 meters long and suspended by a mesentery
- Ileum: about 3.5 meters long and suspended by a mesentery
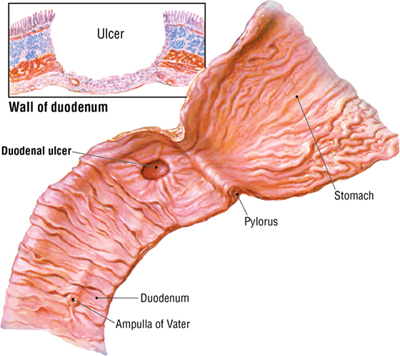
The duodenum is the first portion of the small intestine and descriptively is divided into four parts (Table 4-8). Most of the C-shaped duodenum is retroperitoneal and ends at the duodenojejunal flexure, where it is tethered by a musculoperitoneal fold called the suspensory ligament of the duodenum (ligament of Treitz) (Fig. 4-14).
|
TABLE 4-8 Features of the Duodenum
|
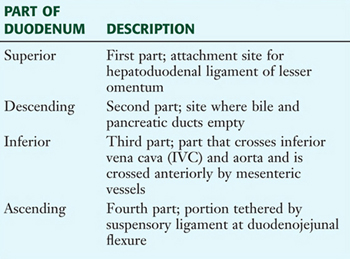 |
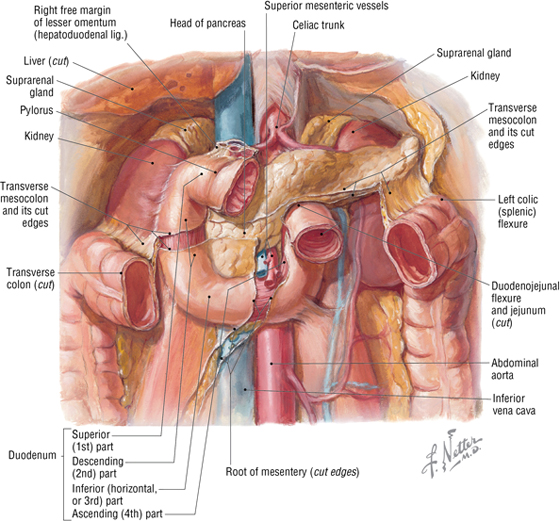
FIGURE 4-14 The Duodenum
The jejunum and ileum are both suspended from an elaborate mesentery. The jejunum is recognizable from the ileum owing to the following factors (Fig. 4-15):
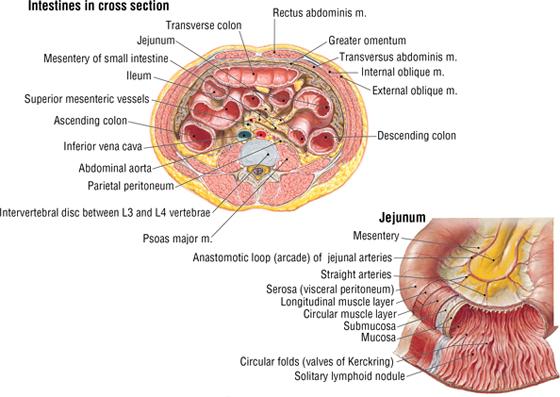
FIGURE 4-15 The Jejunum and Ileum (Contd.)
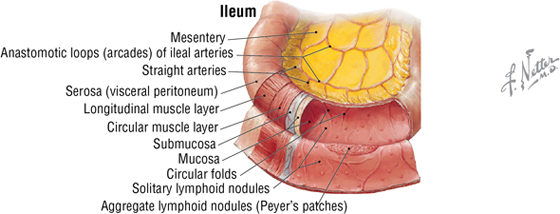
FIGURE 4-15 (Contd.) The Jejunum and Ileum
- It occupies the left upper quadrant of the abdomen.
- It is larger in diameter.
- Its walls are thicker.
- Its mesentery contains less fat.
- It has arterial branches with fewer arcades and longer vasa recta.
- Internally it has mucosal folds that are higher and more numerous, which increases the surface area for absorption.
C L I N I C A L F O C U S
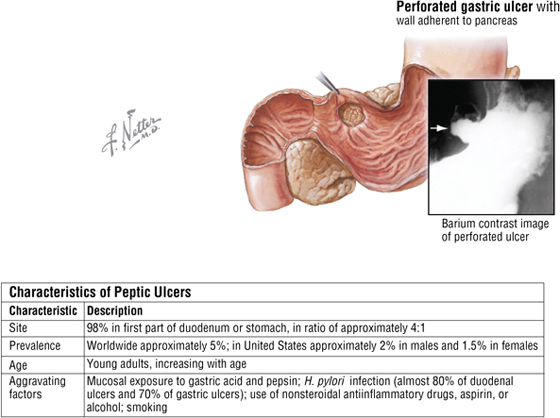
Peptic Ulcer Disease
Peptic ulcers are GI lesions that extend through the muscularis mucosae and are remitting, relapsing lesions. (Erosions, on the other hand, affect only the superficial epithelium.) Acute lesions are small and shallow, whereas chronic ulcers may erode into the muscularis externa or perforate the serosa. Although they may occur in the stomach, most occur in the first part of the duodenum, which is referred to by clinicians as the duodenal cap.
C L I N I C A L F O C U S
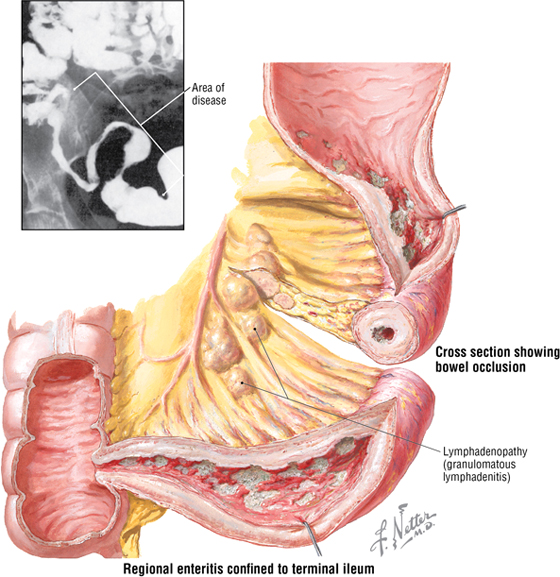
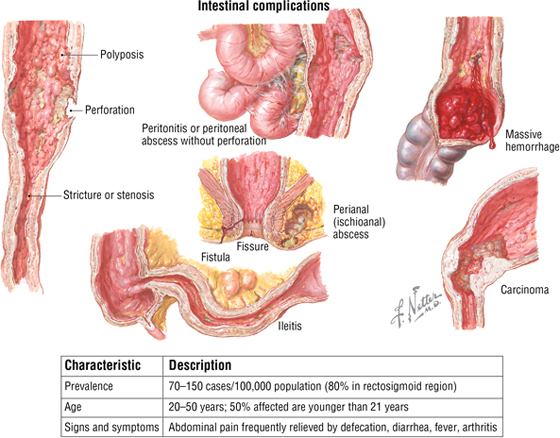
Crohn Disease
Crohn disease is an idiopathic inflammatory bowel disease that can affect any segment of the GI tract but usually involves the small intestine (terminal ileum) and colon. Young adults of northern European ancestry are more commonly affected. Transmural edema, follicular lymphocytic infiltrates, epithelioid cell granulomas, and fistulation characterize this disease. Signs and symptoms include the following:
- Diffuse abdominal pain (paraumbilical and lower-right quadrant)
- Diarrhea
- Fever
- Dyspareunia (pain during sexual intercourse)
- Urinary tract infection (UTI)
- Malabsorption
The small intestine ends at the ileocecal junction, where a sphincter called the ileocecal valve controls the passage of ileal contents into the cecum (Fig. 4-16). The valve is actually two internal mucosal folds that cover a thickened smooth muscle sphincter.
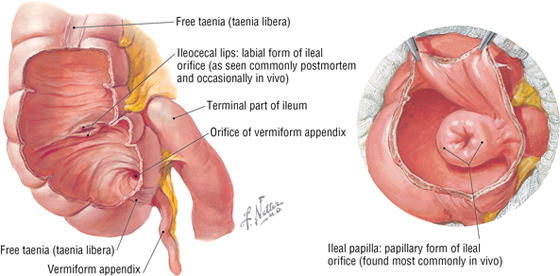
FIGURE 4-16 The Ileocecal Junction and Valve
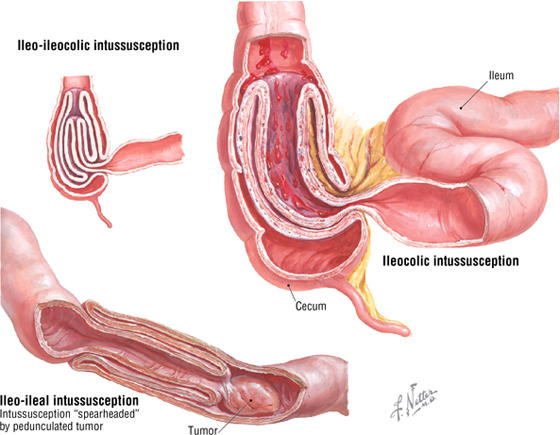
Large Intestine
The large intestine is about 1.5 meters long and extends from the cecum to the anal canal. It includes the following segments (Figs. 4-16 and 4-17):
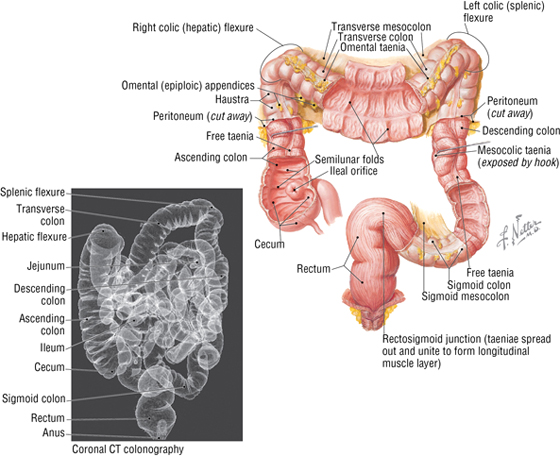
FIGURE 4-17 Features and Musculature of the Large Intestine. (CT reprinted with permission from Kelley LL, Petersen C: Sectional Anatomy for Imaging Professionals. Philadelphia, Mosby, 2007.)
- Cecum: a pouch that is connected to the ascending colon and the ileum; it extends below the ileocecal junction, although it is not suspended by a mesentery
- Appendix: a narrow tube of variable length (usually about 7 to 10 cm) that contains numerous lymphoid nodules and is suspended by mesentery called the mesoappendix
- Ascending colon: is retroperitoneal and ascends on the right flank to reach the liver, where it bends into the right colic (hepatic) flexure
- Transverse colon: is suspended by a mesentery, the transverse mesocolon, and runs transversely from the right hypochondrium to the left, where is bends to form the left colic (splenic) flexure
- Descending colon: is retroperitoneal and descends along the left flank to join the sigmoid colon in the left groin region
- Sigmoid colon: is suspended by a mesentery, the sigmoid mesocolon, and forms a variable loop of bowel that runs medially to join the midline rectum in the pelvis
- Rectum and anal canal: are retroperitoneal and extend from the middle sacrum to the anus (See Chapter 5, Pelvis and Perineum)
The colon (ascending colon through the sigmoid part) absorbs water and important ions from the feces. It then compacts the feces for delivery to the rectum. Features of the large intestine include the following (see Fig. 4-17):
- Taeniae coli: three longitudinal bands of smooth muscle that are visible on the cecum and colon’s surface and assist in peristalsis
- Haustra: sacculations of the colon created by the contracting taeniae coli
- Omental appendices: small fat accumulations that are covered by visceral peritoneum and hang from the colon
- Greater luminal diameter: the large intestine has a larger luminal diameter than the small intestine
C L I N I C A L F O C U S
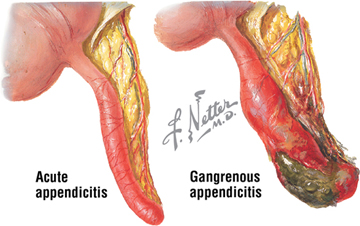
Acute Appendicitis
Appendicitis is a fairly common inflammation of the appendix, often caused by bacterial infection. Initially, diffuse pain is felt in the periumbilical region. However, as the appendix becomes more inflamed and irritates the parietal peritoneum, the pain becomes well localized to the right lower quadrant (circumscribed tenderness to palpation). Surgical resection is the treatment of choice to prevent more serious life-threatening complications (abscesses and peritonitis).
C L I N I C A L F O C U S
Ulcerative Colitis
Like Crohn disease, ulcerative colitis is an idiopathic inflammatory bowel disease that begins in the rectum and extends proximally. Usually the inflammation is limited to the mucosal and submucosal layers of the bowel.
C L I N I C A L F O C U S
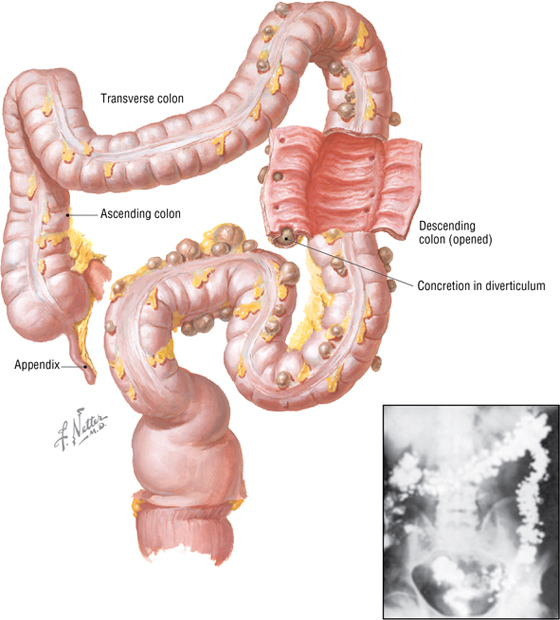
Diverticulosis
Diverticulosis is a herniation of colonic mucosa and submucosa through the muscular wall, with a diverticular expansion in the adventitia of the bowel visible on its external surface. Common sites of development occur where neurovascular bundles penetrate the muscular wall of the bowel.
C L I N I C A L F O C U S
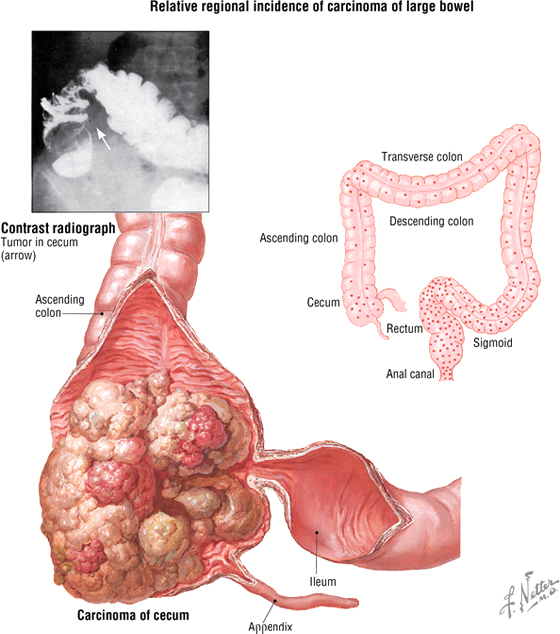
Colorectal Cancer
Colorectal cancer is second only to lung cancer in site-specific mortality and accounts for almost 15% of cancer-related deaths in the United States. The cancer appears as polypoid and ulcerating, and spreads by infiltration through the colonic wall, by regional lymph nodes, and to the liver through portal venous tributaries.
C L I N I C A L F O C U S
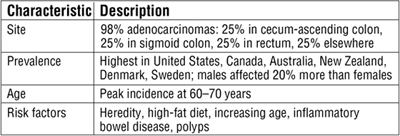
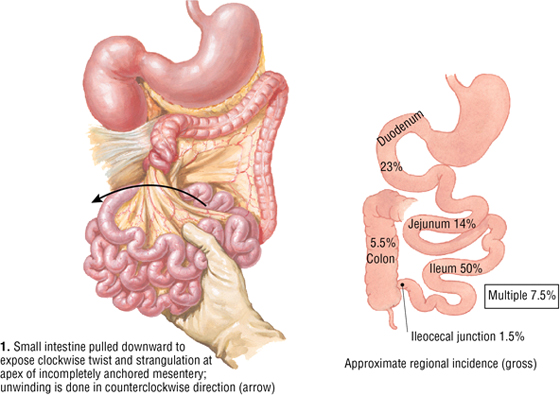
Volvulus
Volvulus is the twisting of a bowel loop that may cause bowel obstruction and constriction of its vascular supply, which may lead to infarction. Volvulus affects the small intestine more often than the large, and the sigmoid colon is the most common site in the large intestine; the mesenteric mobility of these portions of the bowel account for this higher occurrence at these sites. Volvulus is associated with dietary habits, perhaps a bulky vegetable diet that results in an increased fecal load.
C L I N I C A L F O C U S
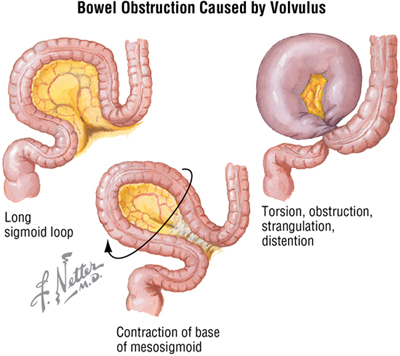
Intussusception
Intussusception is the invagination, or telescoping, of one bowel segment into a contiguous distal segment. In children, the cause may be linked to excessive peristalsis. In adults, an intraluminal mass, such as a tumor, may become trapped during a peristaltic wave and pull its attachment site forward into the more distal segment. Intestinal obstruction and infarction may occur.
Liver
The liver is the largest solid organ in the body and anatomically is divided into four lobes (Fig. 4-18):
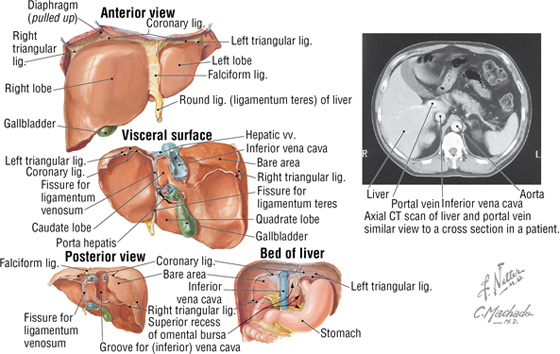
FIGURE 4-18 Various Views of the Liver and the Bed of the Liver. (CT reprinted with permission from Kelley LL, Petersen C: Sectional Anatomy for Imaging Professionals. Philadelphia, Mosby, 2007.) (Contd.)
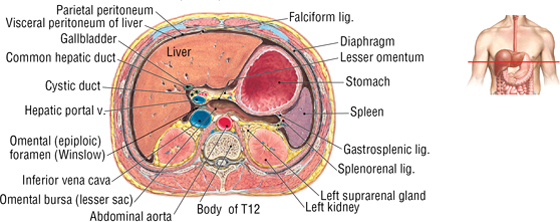
FIGURE 4-18 (Contd.) Various Views of the Liver and the Bed of the Liver. (CT reprinted with permission from Kelley LL, Petersen C: Sectional Anatomy for Imaging Professionals. Philadelphia, Mosby, 2007.)
- Right lobe (largest lobe)
- Left lobe
- Quadrate lobe (lies between the gallbladder and the round ligament of the liver)
- Caudate lobe (lies between the IVC, ligamentum venosum, and porta hepatis)
Functionally and surgically, the liver is divided into right and left halves. (The quadrate and caudate are part of the left half.) Surgeons often divide the liver further into eight independent vascular segments based on its vasculature, with each segment receiving a major branch of the hepatic artery, portal vein, hepatic vein (drains the liver’s blood into the IVC), and biliary drainage. The external demarcation of the two liver halves runs in an imaginary sagittal plane passing through the gallbladder and IVC. Features of the liver are summarized in Table 4-9.
|
TABLE 4-9 Features of the Liver and Its Ligaments
|
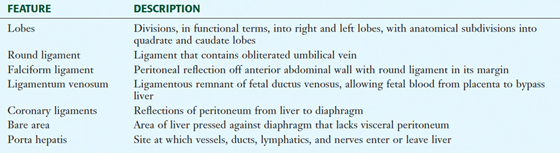 |
The liver is important as it receives the venous drainage from the GI tract, its accessory organs, and the spleen via the portal vein (see Fig. 4-25). The liver serves the following important functions:
- Storage of energy sources (glycogen, fat, protein, and vitamins)
- Production of cellular fuels (glucose, fatty acids, and keto acids)
- Production of plasma proteins and clotting factors
- Metabolism of toxins and drugs
- Modification of many hormones
- Production of bile acids
- Excretion of substances (bilirubin)
- Storage of iron and many vitamins
- Phagocytosis of foreign materials that enter the portal circulation from the bowel
Gallbladder
The gallbladder is composed of a fundus, body, and neck. Its function is to receive, store, and concentrate bile. Bile, which is secreted by the hepatocytes of the liver, passes through the extrahepatic duct system (Fig. 4-19) in the following way:
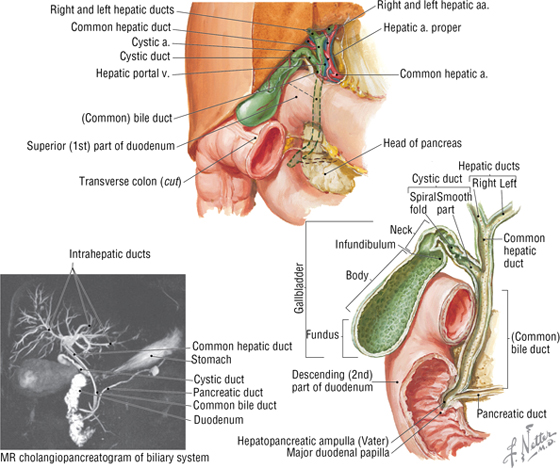
FIGURE 4-19 Gallbladder and Its Extrahepatic Ducts. (MR reprinted with permission from Kelley LL, Petersen C: Sectional Anatomy for Imaging Professionals. Philadelphia, Mosby, 2007.)
- Collects in the right and left hepatic ducts after draining the right and left liver lobes
- Enters the common hepatic duct
- Enters the cystic duct and is stored and concentrated in the gallbladder
- Upon stimulation (largely by vagal efferents and cholecystokinin [CCK]), leaves the gallbladder and enters the cystic duct
- Passes inferiorly down the common bile duct
- Enters the hepatopancreatic ampulla (of Vater)
- Empties into the second part of the duodenum (major duodenal papilla)
The liver produces about 900 mL of bile per day. Between meals most of the bile is stored in the gallbladder (which has a capacity of about 30 to 50 mL), where it is also concentrated. Consequently, bile that reaches the duodenum is a mixture of the more dilute bile directly flowing from the liver and the concentrated bile from the gallbladder.
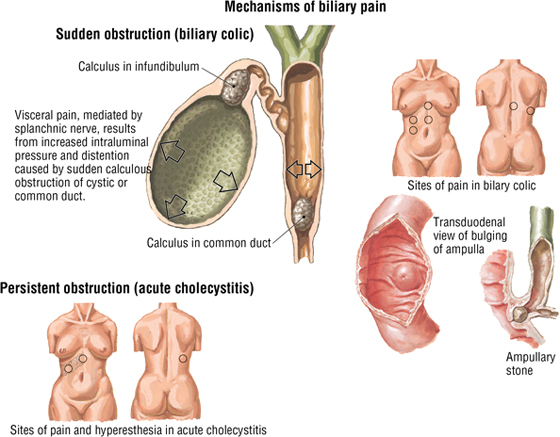
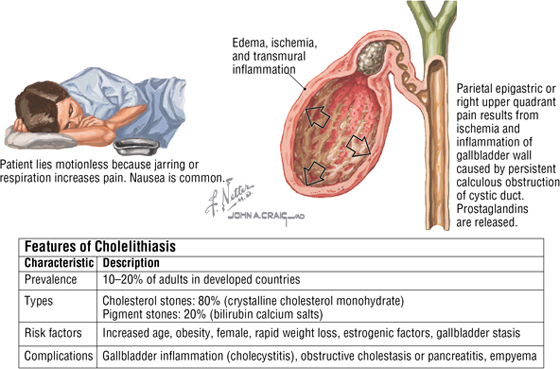
C L I N I C A L F O C U S
Gallstones (Cholelithiasis)
Cholelithiasis results from stone formation in the gallbladder and extrahepatic ducts. Acute pain (biliary colic) can be referred to several sites. Common sites include the back just below the right scapula (T6-T9 dermatomes) or even the right shoulder region, if an inflamed gallbladder (cholecystitis) irritates the diaphragm. Obstruction of bile flow (bile stasis) can lead to numerous complications and jaundice (yellow discoloration of the skin and sclera that is caused by bilirubin accumulation in the blood plasma).
Pancreas
The pancreas is an exocrine and endocrine organ that lies posterior to the stomach in the floor of the lesser sac. It is a retroperitoneal organ, except for the distal tail, which is in contact with the spleen (Fig. 4-20). The anatomical parts of the pancreas include the following:
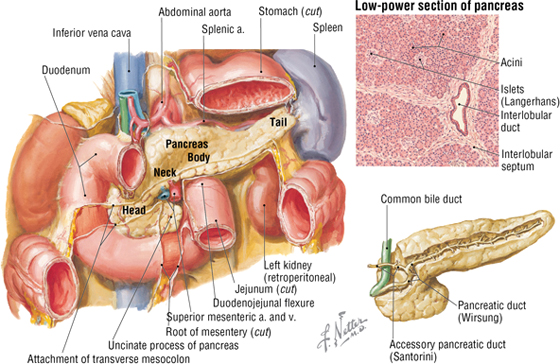
FIGURE 4-20 Pancreas
- Head: nestled within the C-shaped curve of the duodenum, with its uncinate process lying posterior to the superior mesenteric vessels
- Neck: lies anterior to the mesenteric vessels, deep to the pyloris of the stomach
- Body: extends above the duodenojejunal flexure and across the superior part of the left kidney
- Tail: terminates at the hilum of the spleen in the splenorenal ligament
The acinar cells of the exocrine pancreas secrete a number of enzymes that are necessary for digestion of proteins, starches, and fats. The pancreatic ductal cells secrete fluid with a high bicarbonate content that serves to neutralize the acid entering the duodenum from the stomach. Pancreatic secretion is under neural (vagus nerve) and hormonal (secretin and CCK) control, and the exocrine secretions empty primarily into the main pancreatic duct, which joins the common bile duct at the hepatopancreatic ampulla (of Vater). A smaller accessory pancreatic duct also empties into the second part of the duodenum above the major duodenal papilla (see Fig. 4-20).
The endocrine pancreas is represented by clusters of islet cells (of Langerhans), a heterogeneous population of cells responsible for the elaboration and secretion primarily of insulin, glucagon, somatostatin, and several lesser hormones.
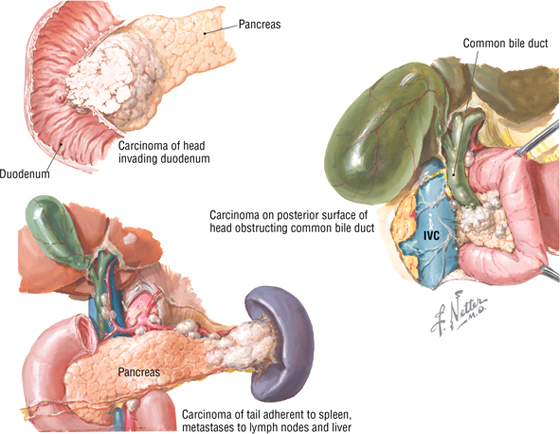
C L I N I C A L F O C U S
Pancreatic Cancer
Carcinoma of the pancreas is the fifth leading cause of cancer death in the United States. Pancreatic carcinomas, which are mostly adenocarcinomas, arise from the exocrine part of the organ (cells of the duct system); 60% of cancers are found in the pancreatic head (these often cause obstructive jaundice). Islet tumors of the endocrine pancreas are less common. Because of the anatomical position of the pancreas, adjacent anatomical sites may be directly involved (duodenum, stomach, liver, colon, spleen), and pancreatic metastases via the lymphatic network are common and extensive.
Spleen
The spleen is slightly larger than a clenched fist and weighs about 180 to 250 grams. It lies in the upper left quadrant of the abdomen and is tucked posterolateral to the stomach under the protection of the lower-left rib cage and diaphragm (Figs. 4-20 and 4-21). Simplistically, it is a large lymph node (and can become quite large during infections), although functionally it is much more and is involved in the following functions:
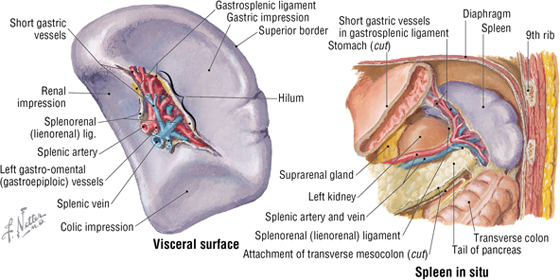
FIGURE 4-21 Spleen
- Lymphocyte proliferation (B and T cells)
- Immune surveillance and response
- Blood filtration
- Destruction of old or damaged red blood cells (RBCs)
- Destruction of damaged platelets
- Recycling iron and globin
- Providing a reservoir for blood
- Providing a source of RBCs in early fetal life
The spleen is tethered between the stomach by the gastrosplenic ligament and the left kidney by the splenorenal ligament. Vessels, nerves, and lymphatics enter or leave the spleen at the hilum (Fig. 4-21).
C L I N I C A L F O C U S
Rupture of the Spleen
Trauma to the left upper quadrant can lead to splenic rupture. The adventitial capsule of the spleen is very thin, making traumatic rupture a medical emergency, as the spleen receives a rich vascular supply and can bleed profusely.
Arterial Supply
The arterial supply and the innervation pattern of the abdominal viscera are directly reflected in the embryology of the GI tract, which we will discuss later in the chapter. The abdominal GI tract is derived from the following three embryonic gut regions:
- Foregut: gives rise to the abdominal esophagus, stomach, proximal half of the duodenum, liver, gallbladder, and pancreas
- Midgut: distal half of the duodenum, jejunum, ileum, cecum, appendix, ascending colon, and proximal two-thirds of the transverse colon
- Hindgut: distal third of the transverse colon, descending colon, sigmoid colon, rectum, and proximal anal canal
The following three large arteries arise from the anterior aspect of the abdominal aorta; each artery supplies the derivatives of the three embryonic gut regions (Fig. 4-22):
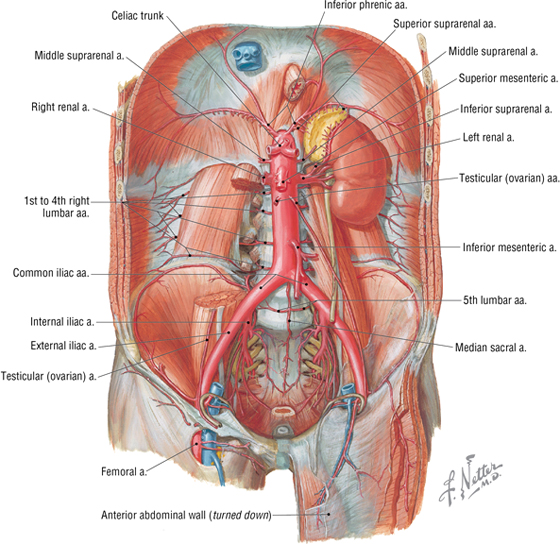
FIGURE 4-22 Abdominal Aorta and Its Branches
- Celiac trunk (artery): foregut derivatives and the spleen
- Superior mesenteric artery (SMA): midgut derivatives
- Inferior mesenteric artery (IMA): hindgut derivatives
The celiac trunk arises from the aorta immediately inferior to the diaphragm and divides into the following three main branches (Fig. 4-23):
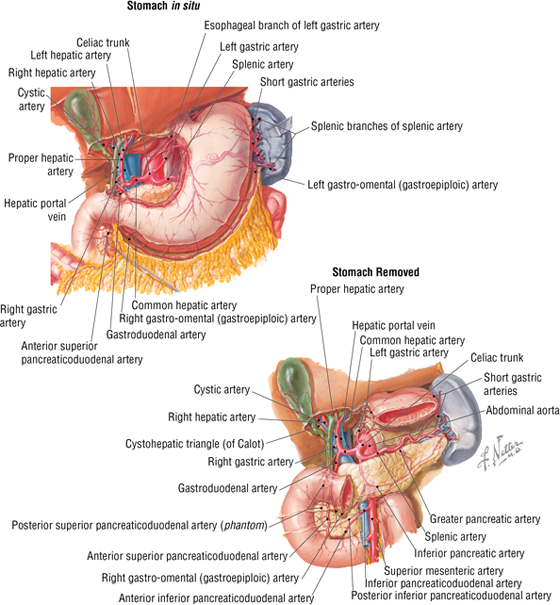
FIGURE 4-23 Celiac Trunk, Its Major Branches, and Their Secondary Branches
- Common hepatic: supplies the liver, gallbladder, stomach, duodenum, and pancreas (head and neck)
- Left gastric: the smallest branch; supplies the stomach and esophagus
- Splenic: the largest branch; takes a tortuous course along the superior margin of the pancreas, and supplies the spleen, stomach, and pancreas (neck, body, and tail)
The SMA arises from the aorta about one finger’s breadth inferior to the celiac trunk. It then passes posterior to the neck of the pancreas, and anterior to the distal duodenum. Its major branches include the following (Fig. 4-24):
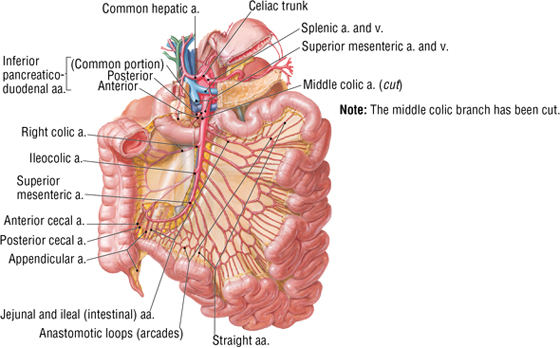
FIGURE 4-24 Superior and Inferior Mesenteric Arteries and Their Branches (Contd.)
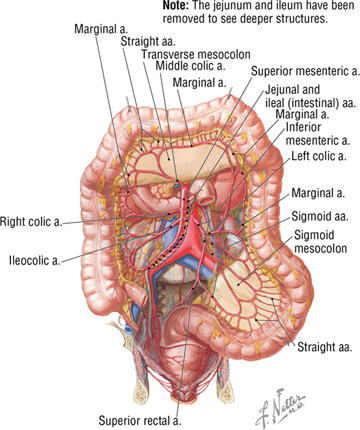
FIGURE 4-24 (Contd.) Superior and Inferior Mesenteric Arteries and Their Branches
- Inferior pancreaticoduodenal artery: supplies the head of the pancreas and duodenum
- Jejunal and ileal branches: give rise to 15 to 18 intestinal branches; run in the mesentery tethering the jejunum and ileum
- Middle colic artery: runs in the transverse mesocolon; supplies the transverse colon
- Right colic artery: courses retroperitoneally to the right side; supplies the ascending colon
- Ileocolic artery: passes to the right iliac fossa and supplies the ileum, cecum, appendix, and proximal ascending colon; terminal branch of the SMA
The IMA arises from the anterior aorta at about the level of the L3 vertebra (the aorta divides anterior to L4), angles to the left, and gives rise to the following branches (see Fig. 4-24)
- Left colic artery: courses to the left and ascends retroperitoneally; supplies the distal transverse colon (by an ascending branch that enters the transverse mesocolon) and the descending colon
- Sigmoid arteries: a variable number of arteries (2 to 4) that enter the sigmoid mesocolon; supply the sigmoid colon
- Superior rectal artery: a small terminal branch; supplies the distal sigmoid colon and proximal rectum
Along the extent of the abdominal GI tract, the branches of each of these arteries anastomose with each other, providing alternative routes of arterial supply. For example, the marginal artery (of Drummond) (see Fig. 4-24) is a large, usually continuous branch that interconnects the right, middle, and left colic branches supplying the large intestine.
Venous Drainage
The hepatic portal system drains the abdominal GI tract, pancreas, gallbladder, and spleen and ultimately drains into the liver and its sinusoids (Fig. 4-25). A portal system, by definition, implies that arterial blood flows into a capillary system (in this case the bowel and its accessory organs), then into larger veins (portal tributaries), and then again into another capillary (or sinusoids) system (the liver), before ultimately being collected into larger veins (hepatic veins and the IVC) that return the blood to the heart.
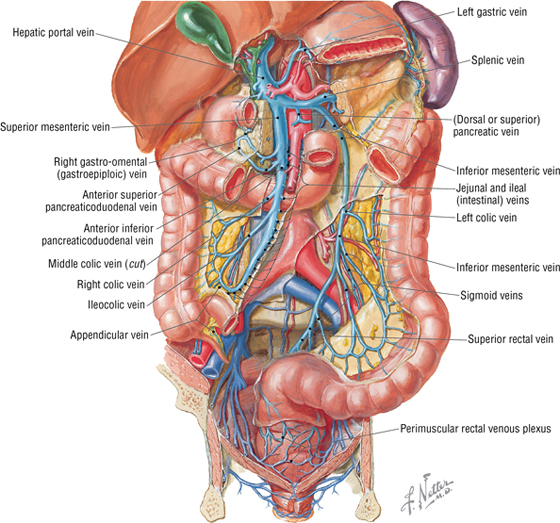
FIGURE 4-25 Venous Tributaries of the Hepatic Portal System
The portal vein ascends from behind the pancreas (superior neck) and courses superiorly in the hepatoduodenal ligament (which also contains the common bile duct and proper hepatic artery) to the hilum of the liver; it is formed by the following veins (Figs. 4-25 and 4-26):
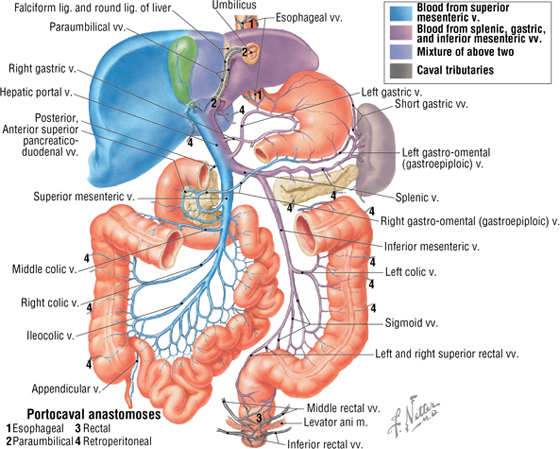
FIGURE 4-26 Hepatic Portal System and Important Portacaval Anastomoses
- Superior mesenteric vein (SMV): large vein that lies to the right of the SMA and drains portions of the foregut and all of the midgut derivatives
- Splenic vein: large vein that lies inferior to the splenic artery, parallels its course, and drains the spleen, pancreas, foregut, and, usually, hindgut derivatives (via the inferior mesenteric vein)
The inferior mesenteric vein (IMV), while usually draining into the splenic vein (see Fig. 4-25), also may drain into the junction of the SMV and splenic vein or drain directly into the SMV.
Typical of most veins in the body, the portal system has numerous anastomoses with other veins, specifically in this case with the tributaries of the caval system (the IVC and the azygos system of veins) (Fig. 4-26). These anastomoses allow for the rerouting of venous return to the heart (these veins do not possess valves) should a major vein become occluded.
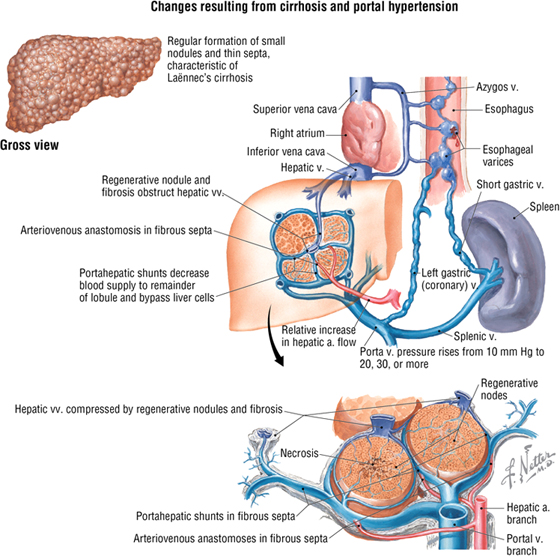
C L I N I C A L F O C U S
Cirrhosis of the Liver
Cirrhosis is a largely irreversible disease characterized by diffuse fibrosis, parenchymal nodular regeneration, and disturbed hepatic architecture. Progressive fibrosis disrupts the portal blood flow, leading to portal hypertension. Major causes of cirrhosis include the following:
- Alcoholic liver disease (60% to 70%)
- Viral hepatitis (10%)
- Biliary diseases (5% to 10%)
- Genetic hemochromatosis (5%)
- Cryptogenic cirrhosis (10% to 15%)
Portal hypertension can lead to esophageal and rectal varices (tortuous enlargement of the esophageal and rectal veins) as the portal venous blood is shunted into the caval system using portacaval anastomoses (see Figure 4-26). Additionally, the engorgement of the superficial venous channels in the subcutaneous tissues of the abdominal wall (see Fig. 4-6, via the paraumbilical portacaval route) can appear as a caput medusae (tortuous subcutaneous varices that resemble the snakes of Medusa’s head).
C L I N I C A L F O C U S
Portal Hypertension
If the portal vein becomes occluded or its blood cannot pass through the hepatic sinusoids, a significant increase in portal venous pressure will ensue, resulting in portal hypertension. Normal portal venous pressure is about 3 to 6 mm Hg, but it can exceed 12 mm Hg (portal hypertension), resulting in dilated, tortuous veins (varices) and variceal rupture. The following three major mechanisms are defined:
- Prehepatic: obstructed blood flow to the liver
- Posthepatic: obstructed blood flow from the liver to the heart
- Intrahepatic: cirrhosis or another liver disease, affecting hepatic sinusoidal blood flow
Clinical consequences of portal hypertension include:
- Ascites, usually detectable when 500 mL of fluid accumulates in the abdomen
- Formation of portacaval shunts via anastomotic channels (see Fig. 4-26)
- Congestive splenomegaly (becomes engorged with venous blood backing up from the splenic vein)
- Hepatic encephalopathy (neurological problems due to the inadequate removal of toxins in the blood by the diseased liver)
Additional figures available online. See Table of Contents for Instructions for online access.

Lymphatics
Lymphatic drainage from the stomach, portions of the duodenum, liver, gallbladder, pancreas, and spleen is largely from regional nodes associated with those organs to a central collection of lymph nodes around the celiac trunk (Fig. 4-27). Lymphatic drainage from the midgut derivatives goes largely to superior mesenteric nodes and hindgut derivatives to inferior mesenteric nodes (Fig. 4-28). These nodal collections often are referred to as the pre- or para-aortic nodes, and they ultimately drain to the celiac nodes and then to the cisterna chili (dilated proximal end of the thoracic duct), which is located adjacent to the celiac trunk.
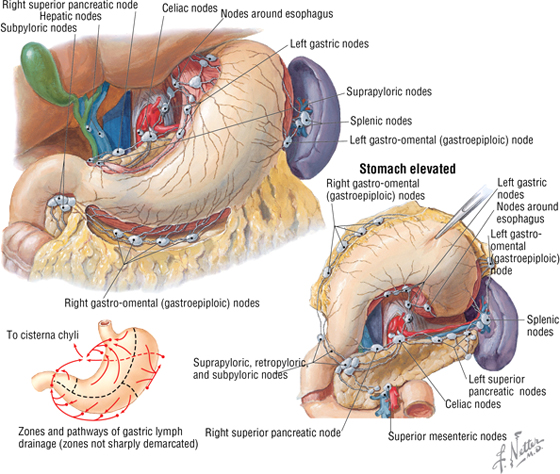
FIGURE 4-27 Lymphatics of the Epigastric Region
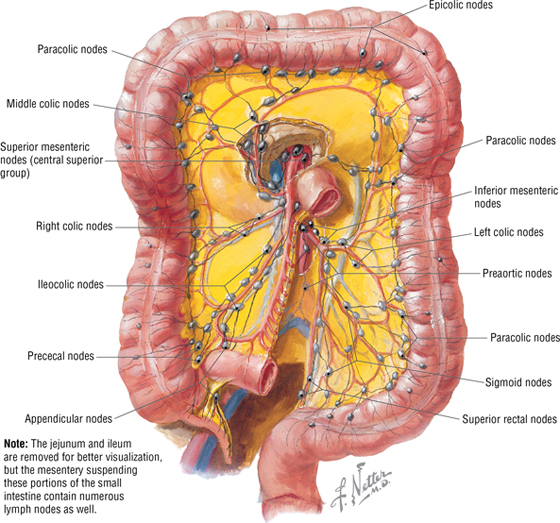
FIGURE 4-28 Lymphatics of the Intestines
Innervation
The abdominal viscera are innervated by the autonomic nervous system (ANS), and the pattern of innervation closely parallels the arterial supply to the various embryonic gut regions (see Table 4-14). Additionally, the enteric nervous system (see Chapter 1, “Introduction to the Human Body”) provides an “intrinsic” network of ganglia with connections to the ANS, which helps coordinate peristalsis and secretion.
The sympathetic innervation of the viscera is derived from the following nerves (see Table 4-14 and Figs. 4-29 and 4-30):
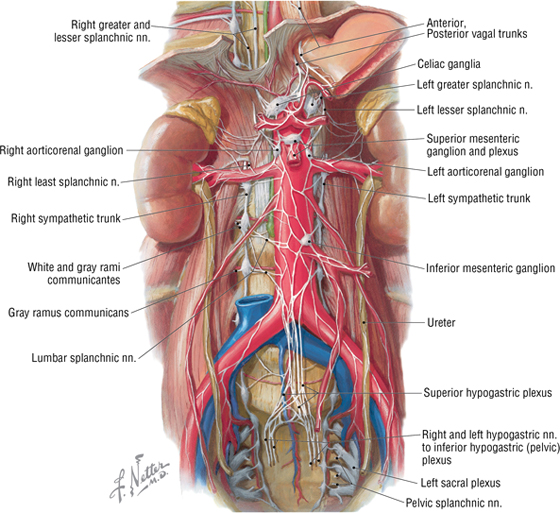
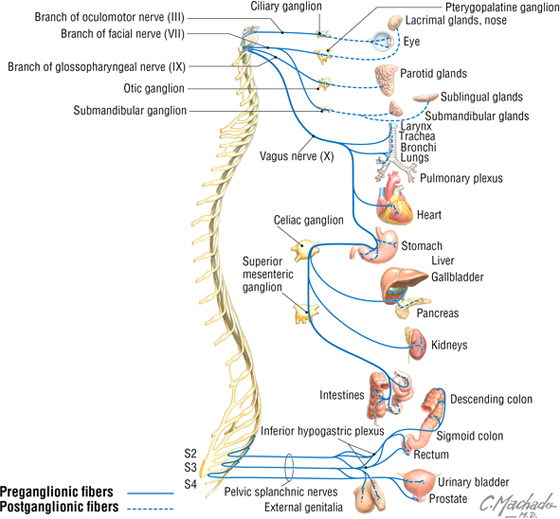
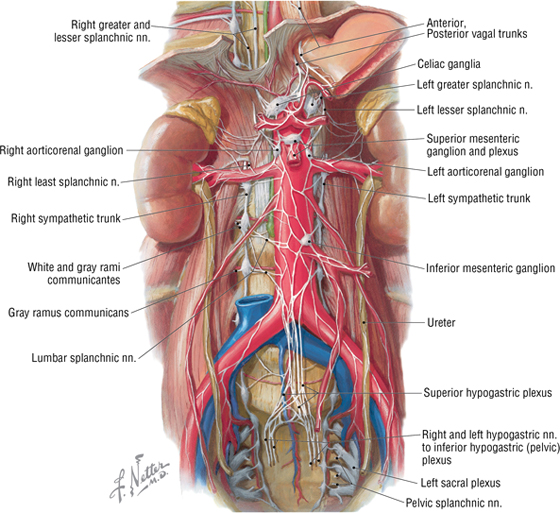
FIGURE 4-29 Abdominal Autonomic Nerves
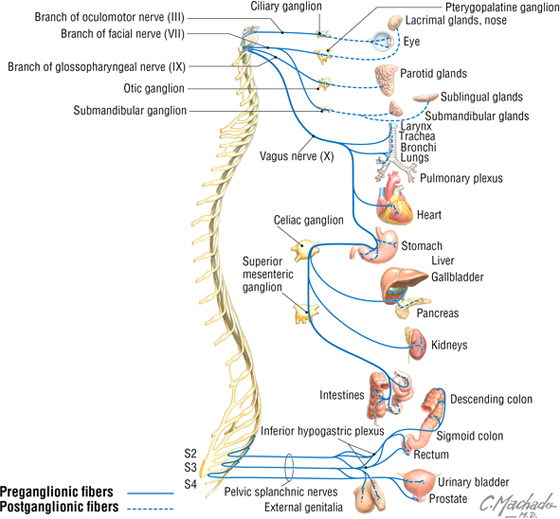
FIGURE 4-30 Parasympathetic Innervation of Abdominal Viscera
- Thoracic splanchnic nerves: greater (T5-T9), lesser (T10-T11), and least (T12) splanchnic nerves (the nerve branches from the thoracic ganglia from which these nerves arise is variable) that convey preganglionic axons to the prevertebral ganglia to innervate the foregut and midgut derivatives
- Lumbar splanchnic nerves: usually several lumbar splanchnic nerves (L1-L2 or L3) that convey preganglionic axons to the prevertebral ganglia and plexus to innervate the hindgut derivatives
Postganglionic sympathetic axons arise from the postganglionic neurons in the prevertebral ganglia and plexus and travel with the blood vessels to their target viscera. Generally, sympathetic stimulation leads to the following:
- Vasoconstriction to shunt blood to other parts of the body, thus inhibiting digestion
- Reduced bowel motility
- Reduced bowel secretion
The parasympathetic innervation of the viscera is derived from the following (see Table 4-14 and Figs. 4-29 and 4-30):
- Vagus nerves: anterior and posterior vagal trunks enter the abdomen on the esophagus and send preganglionic axons directly to postganglionic neurons in the walls of the viscera derived from the foregut and midgut
- Pelvic splanchnic nerves: preganglionic axons from S2-S4 travel via these splanchnic nerves to the prevertebral plexus and distribute to the postganglionic neurons of the hindgut derivatives. (Note: pelvic splanchnic nerves are not part of the sympathetic trunk; only sympathetic neurons and axons reside in the sympathetic trunk and chain ganglia.)
Many postganglionic parasympathetic neurons are in the myenteric and submucosal ganglia that compose the enteric nervous system (see Chapter 1, “Introduction to the Human Body”). Generally, parasympathetic stimulation leads to the following:
- Increased bowel motility
- Increased secretion
Visceral afferent fibers travel with the ANS components and can be summarized as follows:
- Pain afferents: include the pain of distension and ischemia, which is conveyed to the CNS largely by the sympathetic components to the spinal dorsal root ganglia associated with the T5-L2 spinal cord levels
- Reflex afferents: include information from chemoreceptors, osmoreceptors, and mechanoreceptors, which are conveyed to autonomic centers in the medulla oblongata via the vagus nerves
Finally, GI tract function is a coordinated effort carried out not only by the “hardwired” components of the ANS and enteric nervous system, as described earlier, but also by the immune and endocrine systems. In fact, the GI tract is considered by many to be the largest endocrine organ in the body, secreting and responding to dozens of GI hormones and other neuroimmune substances.
6. POSTERIOR ABDOMINAL WALL AND VISCERA
Posterior Abdominal Wall
The posterior abdominal wall and its visceral structures lie deep to the parietal peritoneum (retroperitoneal) lining the posterior abdominal cavity. This region contains skeletal structures, muscles, major vascular channels, adrenal glands, the upper urinary system, nerves, and lymphatics.
Fascia and Muscles
Deep to the parietal peritoneum, the muscles of the posterior abdominal wall are enveloped in a layer of investing fascia called the endoabdominal fascia, which is continuous laterally with the transversalis fascia of the transversus abdominis muscle. For identification, we name the fascia according to the structures it covers (Fig. 4-31). These structures are as follows:
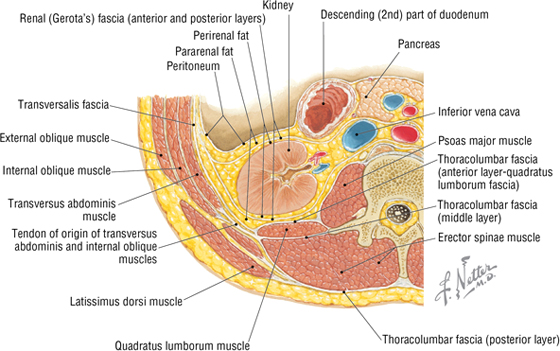
FIGURE 4-31 Transverse Section through the L2 Vertebra
- Psoas fascia: covers the psoas major muscle and is thickened superiorly, forming the medial arcuate ligament (see Figs. 4-31 and 4-32)
- Thoracolumbar fascia: anterior layer covers the quadratus lumborum muscle and is thickened superiorly, forming the lateral arcuate ligament (see Figs. 4-31 and 4-32); middle and posterior layers envelop the erector spinae muscles of the back
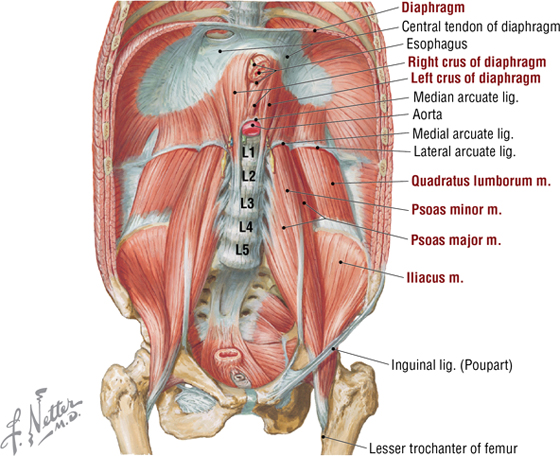
FIGURE 4-32 Muscles of the Posterior Abdominal Wall
The muscles of the posterior abdominal wall have attachments to the lower rib cage, the T12-L5 vertebrae, and bones of the pelvic girdle. These muscles are shown in Table 4-10 and Figure 4-32. Note that the diaphragm has a central tendinous portion and is attached to the lumbar vertebrae by a right and left crus (“leg”), which are joined centrally by the median arcuate ligament that passes over the emerging abdominal aorta (see Fig. 4-32).
|
TABLE 4-10 Muscles of the Posterior Abdominal Wall
|
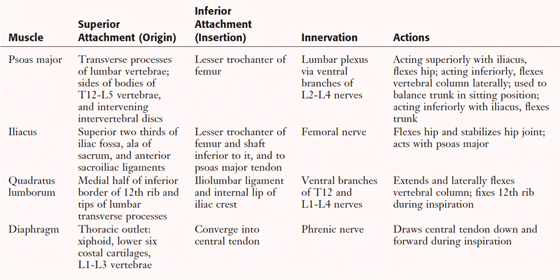 |
Kidneys and Adrenal (Suprarenal) Glands
The kidneys and adrenal glands are retroperitoneal organs that receive a rich arterial supply (Fig. 4-33). The right kidney usually lies somewhat lower than the left kidney because of the presence of the liver.
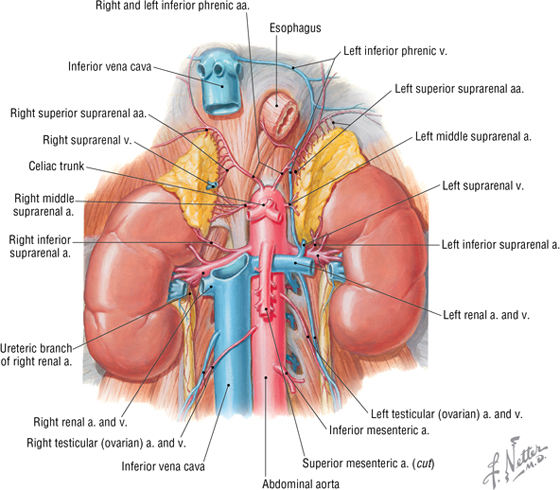
FIGURE 4-33 Kidneys and Adrenal Glands, and Their Blood Supply
Each kidney is enclosed in the following layers of fascia and fat (Figs. 4-31 and 4-34):
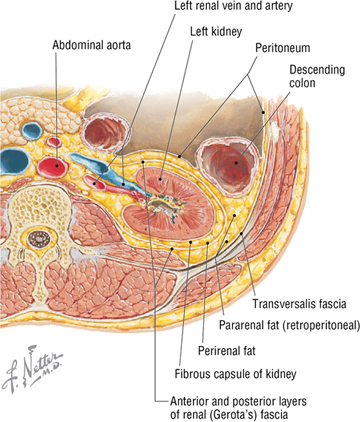
FIGURE 4-34 Renal Fascia and Fat
- Renal capsule: covers each kidney; a thick fibroconnective tissue capsule
- Perirenal (perinephric) fat: directly surrounds the kidney (and adrenal glands) and cushions it
- Renal fascia: surrounds the kidney (and adrenal glands) and perirenal fat; superiorly it is continuous with the fascia covering the diaphragm; inferiorly it may blend with the transversalis fascia
- Pararenal (paranephric) fat: an outer layer of fat that is variable in thickness and is continuous with the extraperitoneal (retroperitoneal) fat
The kidneys are related posteriorly to the diaphragm and muscles of the posterior abdominal wall, as well as the 11th and 12th (floating) ribs. They move with respiration, and anteriorly are in relation to the abdominal viscera and mesenteries shown in Figure 4-14. Variability in these relationships is common owing to the size of the kidneys and adjacent viscera, disposition of mobile portions of the bowel, and extent of the mesenteries.
Structurally, each kidney has the following gross features (Fig. 4-35):
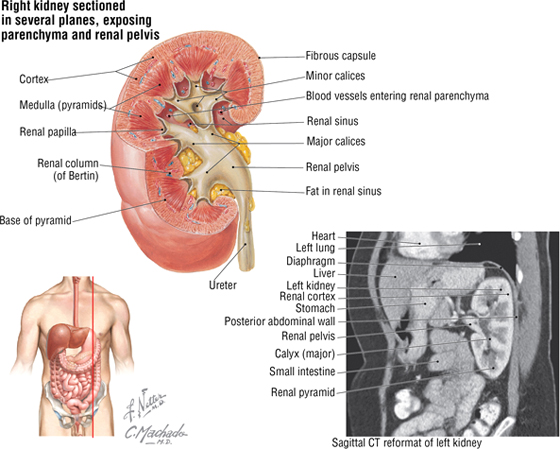
FIGURE 4-35 Features of the Right Kidney Sectioned in Several Planes. (CT reprinted with permission from Kelley LL, Petersen C: Sectional Anatomy for Imaging Professionals. Philadelphia, Mosby, 2007.)
- Renal capsule: a fibroconnective tissue capsule that surrounds the renal cortex
- Renal cortex: outer layer that surrounds the renal medulla and contains nephrons (units of filtration) and renal tubules
- Renal medulla: inner layer (usually appears darker in color) that contains renal tubules and collecting ducts that convey filtrate to minor calices; the renal cortex extends as renal columns in between the medulla, demarcating the distinctive “renal pyramids” whose apex (renal papilla) terminates with a minor calyx
- Minor calyx: structure that receives urine from the collecting ducts of the renal pyramids
- Major calyx: site at which several minor calices drain
- Renal pelvis: point at which several major calices unite; conveys urine to the proximal ureter
- Hilum: medial aspect of each kidney, where the renal pelvis emerges from the kidney and where vessels, nerves, and lymphatics enter or leave the kidney
The ureters are about 25 cm long, extend from the renal pelvis to the urinary bladder, are composed of a thick layer of smooth muscle, and lie in a retroperitoneal position.
The right adrenal (suprarenal) gland often is pyramidal in shape, whereas the left gland is semilunar (see Fig. 4-33). Each adrenal gland “caps” the superior pole of the kidney and is surrounded by perirenal fat and renal fascia. The right adrenal gland is in close proximity to the IVC and liver, whereas the stomach, pancreas, and even the spleen can lie anterior to the left adrenal gland.
C L I N I C A L F O C U S
Renal Stones (Calculi)
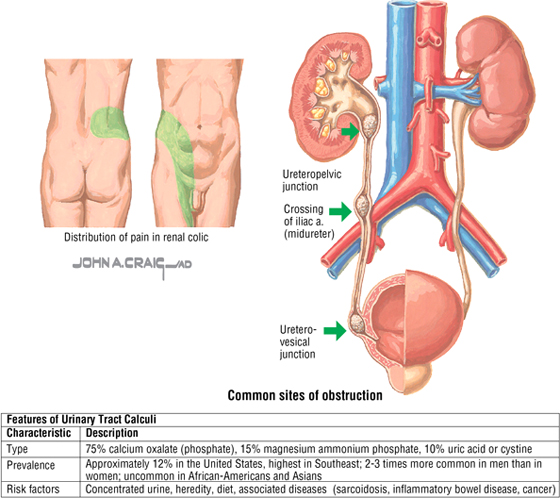
Renal stones may form in the kidney and remain there or, more commonly, pass down the ureters to the bladder. When the stones traverse the ureter, they cause significant pain (renal colic) that typically distributes on the side of the insult radiating from “loin to groin.” The ureters narrow at three points along their course to the bladder. This is a common location for renal stones to become lodged and cause pain. This pain distribution reflects the pathway of visceral pain afferents (pain is from distension of the ureter) that course to the spinal cord levels T11-L1 via the sympathetic splanchnic nerves. Complications of renal stones include obstruction to the flow of urine, infection, and destruction of the renal parenchyma.

C L I N I C A L F O C U S
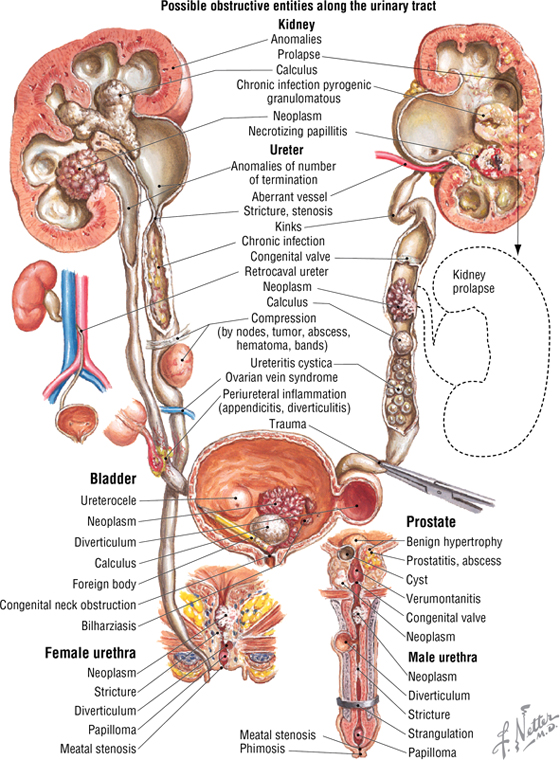
Obstructive Uropathy
Obstruction to the normal flow of urine, which may occur anywhere from the level of the renal nephrons to the urethral opening, can precipitate pathological changes that coupled with an infection can lead to serious uropathies. This composite figure shows a number of obstructive possibilities and highlights important aspects of the adjacent anatomy one sees along the extent of the urinary tract.
C L I N I C A L F O C U S
Malignant Tumors of the Kidney
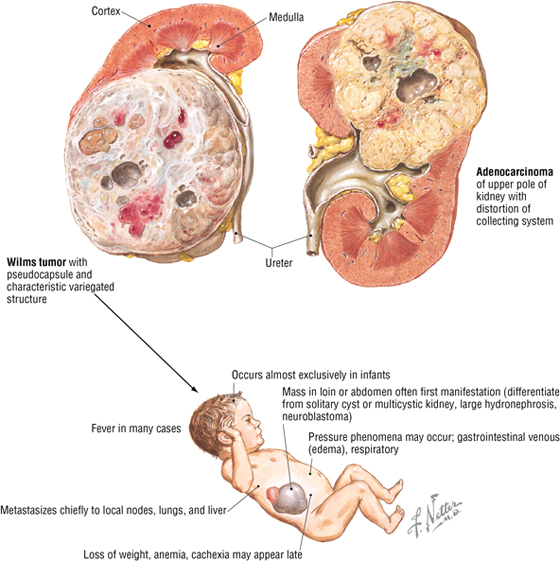
Of the malignant kidney tumors, 80% to 90% are adenocarcinomas that arise from the tubular epithelium. They account for about 2% of all adult cancers, often occur after 50 years of age, and occur twice as often in men as in women. Wilms tumor is the third most common solid tumor in young children (<10 years of age) and is associated with congenital malformations related to chromosome 11.
Abdominal Vessels
The abdominal aorta extends from the aortic hiatus (T12) to the lower level of L4, where it divides into the right and left common iliac arteries (Fig. 4-36). The abdominal aorta gives rise to the following three groups of arteries (Table 4-11 and Fig. 4-36):
|
TABLE 4-11 Branches of the Abdominal Aorta
|
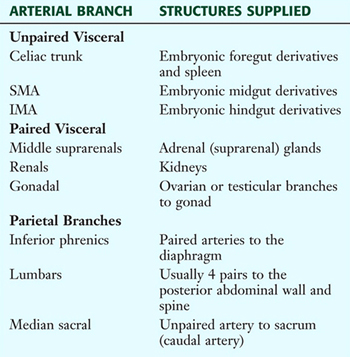 |
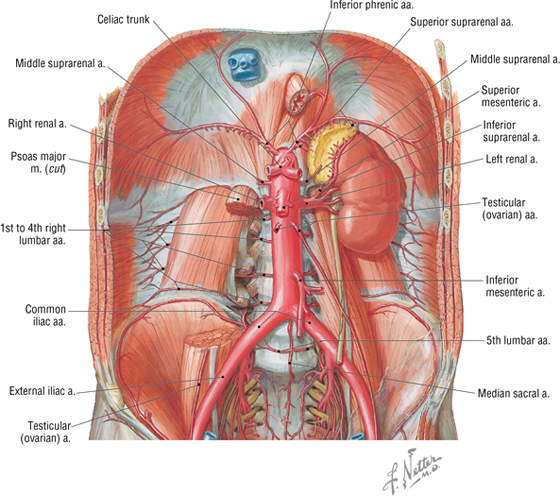
FIGURE 4-36 Abdominal Aorta
- Unpaired visceral arteries to the GI tract, spleen, pancreas, gallbladder, and liver
- Paired visceral arteries to the kidneys, adrenal glands, and gonads
- Parietal arteries to musculoskeletal structures
The inferior vena cava (IVC) (Fig. 4-37) drains abdominal structures other than the GI tract and the spleen, which are drained by the hepatic portal system. The IVC begins by the union of the two common iliac veins just to the right and slightly inferior of the midline distal abdominal aorta and ascends to pierce the diaphragm at the level of the T8 vertebral level, where it empties into the right atrium. Most of the IVC tributaries parallel the arterial branches of the aorta, but two or three hepatic veins also enter the IVC just inferior to the diaphragm. It is important to note that the ascending lumbar veins connect adjacent lumbar veins and drain superiorly into the azygos venous system (see Chapter 3, “Thorax”). This venous anastomosis is important if the IVC should become obstructed.
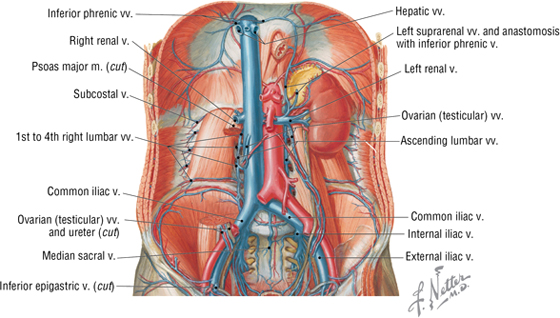
FIGURE 4-37 Inferior Vena Cava
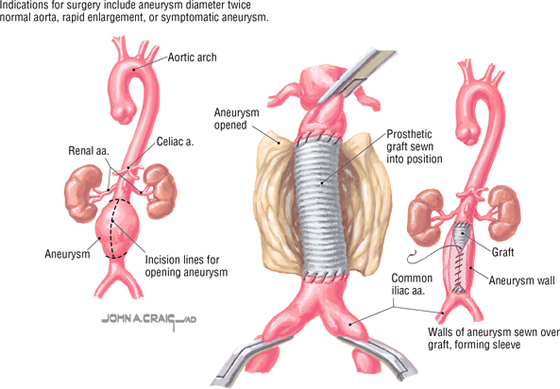
C L I N I C A L F O C U S
Surgical Management of Abdominal Aortic Aneurysm
Aneurysms (bulges in the arterial wall) usually involve the large arteries. The multifactorial etiology includes family history, hypertension, breakdown of collagen and/or elastin within the vessel wall (which leads to inflammation and weakening of the arterial wall), and atherosclerosis. The abdominal aorta (infrarenal segment) and iliac arteries are most often involved, but the thoracic aorta and the femoral and popliteal arteries can also have aneurysms. Symptoms include abdominal and/or back pain, nausea, and early satiety, but up to 75% of patients may be asymptomatic. If surgical repair is warranted, the procedure may be done in an open fashion using durable synthetic grafts (illustrated) or by an endovascular repair, in which a new synthetic lining is inserted using hooks or stents to hold the lining in place.
Lymphatic Drainage
Lymph from the posterior abdominal wall and retroperitoneal viscera drains medially following the arterial supply back to lumbar and visceral preaortic lymph nodes (Fig. 4-38). Ultimately, the lymph is collected into the cisterna chyli and conveyed to the venous system by the thoracic duct.
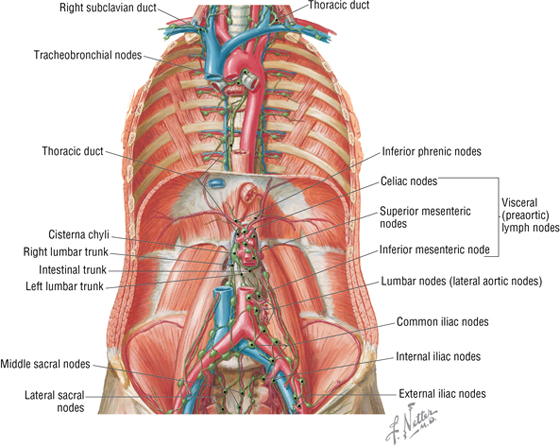
FIGURE 4-38 Abdominal Lymphatics
Innervation
Retroperitoneal visceral structures of the posterior abdominal wall (adrenal glands, kidneys, and ureters) are supplied by parasympathetic fibers from the vagus nerve (adrenals) and by the pelvic splanchnics (S2-S4) to the distal ureters (see Fig. 4-30). Sympathetics (secretomotor) to the adrenal medulla come from the lesser and least thoracic splanchnic nerves, and sympathetics to the kidneys and proximal ureters come from the lesser and least thoracic splanchnic nerves (T10-T12) and the lumbar splanchnics (L1-L2) (see Fig. 4-29).
Pain afferents from all of the abdominal viscera pass to the spinal cord largely by following the thoracic and lumbar splanchnic sympathetic nerves (T5-L2). The neuronal cell bodies of these afferents reside in the respective dorsal root ganglia of the spinal cord segment. Thus, visceral pain may be perceived as somatic pain over these dermatome regions, a phenomenon known clinically as referred pain. Pain afferents from pelvic viscera largely follow pelvic splanchnic parasympathetic nerves (S2-S4) into the cord, and the pain is largely confined to the pelvic region. Common sites of referred visceral pain are shown in Figure 4-39 and summarized in Table 4-12.
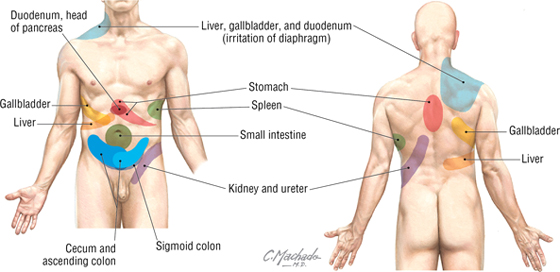
FIGURE 4-39 Sites of Visceral Referred Pain
|
TABLE 4-12 Summary of Spinal Cord Levels for Visceral Referred Pain
|
 |
*Irritation of the diaphragm leads to pain referred to the back (inferior scapula) and shoulder region.
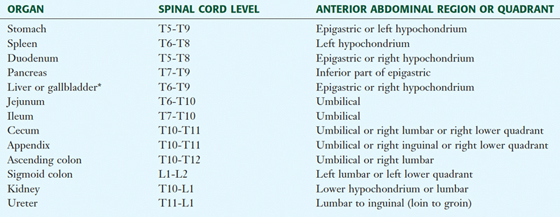
Somatic nerves of the posterior abdominal wall are derived from the lumbar plexus, which is composed of the ventral rami of L1-L4 (sometimes with a small contribution from T12) (Fig. 4-40). The branches of the lumbar plexus are summarized in Table 4-13.
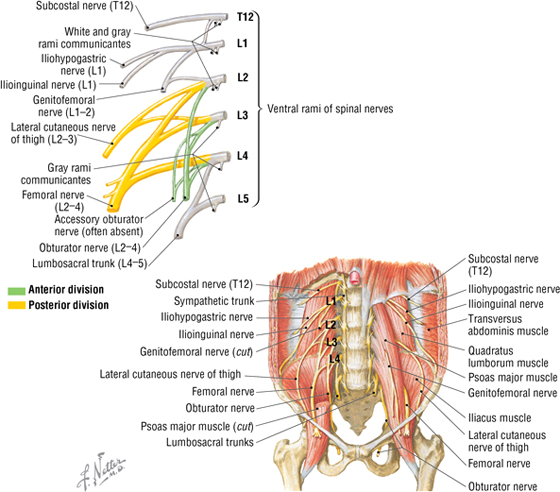
FIGURE 4-40 Lumbar Plexus
|
TABLE 4-13 Branches of the Lumbar Plexus
|
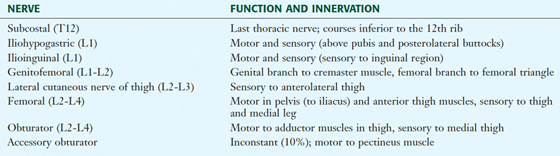 |
7. EMBRYOLOGY
Summary of Gut Development
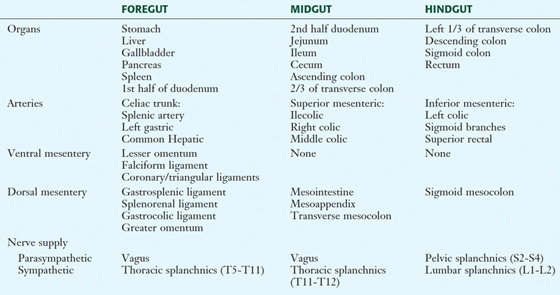
The embryonic gut begins as a midline endoderm-lined tube that is divided into foregut, midgut, and hindgut regions, each giving rise to adult visceral structures with a segmental vascular supply and autonomic innervation (Fig. 4-41 and Table 4-14). Knowing this pattern of distribution related to the three embryonic gut regions will help you better organize your thinking about the abdominal viscera and their neurovascular supply.
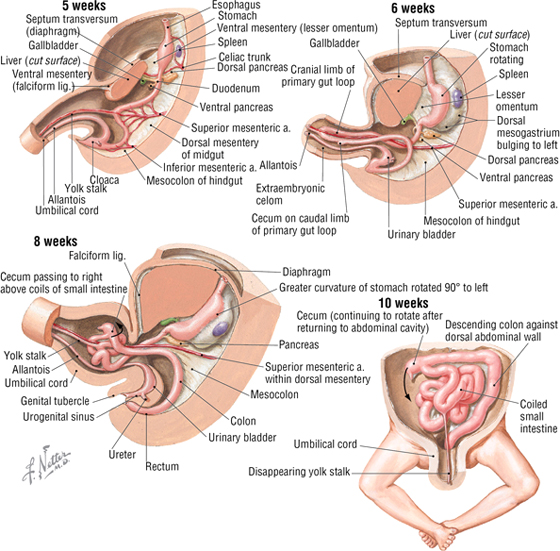
FIGURE 4-41 Sequence of Embryonic Gut Tube Rotations
|
TABLE 4-14 Summary of Embryonic Gut Development
|
 |
The gut undergoes a series of rotations and differential growth that ultimately contributes to the postnatal disposition of the abdominal GI tract (see Fig. 4-41). This sequence of events can be summarized as follows:
- The stomach rotates 90 degrees clockwise on its longitudinal axis so that the left side of the gut tube now faces anteriorly.
- As the stomach rotates, the duodenum swings to the right into its familiar C-shaped configuration and becomes largely retroperitoneal.
- The midgut forms an initial primary intestinal loop by rotating 180 degrees counterclockwise around the axis of the SMA (which supplies blood to the midgut) and, because of its fast growth, herniates out into the umbilical cord (6 weeks).
- By the 10th week, the gut loop returns into the abdominal cavity and completes its rotation with a 90-degree swing to the right lower quadrant.
- Thus, the midgut loop completes a 270-degree rotation about the axis of the SMA and undergoes significant differential growth to form the small intestine and proximal portions of the large intestine (see Table 4-14).
- The hindgut then develops into the remainder of the large intestine and proximal anal canal, supplied by the IMA, and ending in the cloaca (Latin for “sewer”).
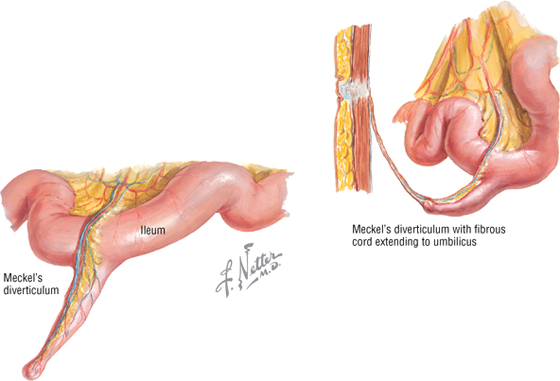
C L I N I C A L F O C U S
Meckel’s Diverticulum
Meckel’s diverticulum is the most common developmental anomaly of the bowel and occurs as a result of failure of the vitelline (yolk stalk) duct to involute once the gut loop has re-entered the abdominal cavity. It is often referred to as the “syndrome of twos” because of the following reasons:
- It occurs in approximately 2% of the population.
- It is about 2 inches long.
- It is located about 2 feet from the ileocecal junction.
- It often contains at least 2 types of mucosa.
Additional figures available online. See Table of Contents for Instructions for online access.

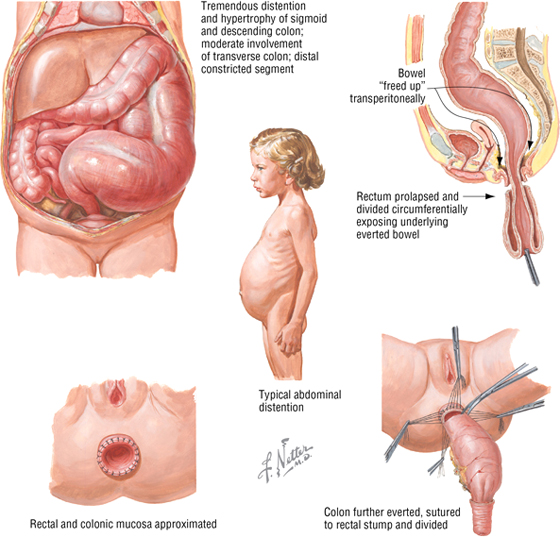
C L I N I C A L F O C U S
Congenital Megacolon
Congenital megacolon results from the failure of neural crest cells to migrate distally along the colon (usually the sigmoid colon and rectum). This leads to an aganglionic segment that lacks both Meissner’s submucosal and Auerbach’s myenteric plexuses. Distention proximal to the aganglionic region may occur shortly after birth or may cause symptoms in early childhood. Surgical repair involves prolapse and eversion of the segment.
C L I N I C A L F O C U S
Congenital Malrotation of the Colon
Many congenital lesions of the GI tract cause intestinal obstruction, which commonly results from malrotation of the midgut, atresia, volvulus, meconium ileus, or imperforate anus. Vomiting, absence of stool, and abdominal distention characterize the clinical picture. Intestinal obstruction can be life threatening, requiring surgical intervention. The corrective procedure for congenital malrotation with volvulus of the midgut is illustrated.
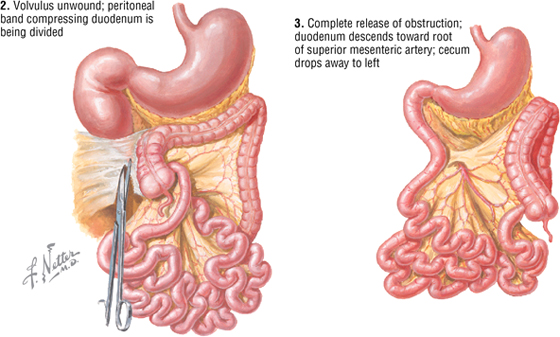
Liver, Gallbladder, and Pancreas Development
During the third week of development, an endodermal outpocketing of the foregut gives rise to the hepatic diverticulum (Fig. 4-42). Further development of this diverticulum gives rise to the liver, the biliary duct system, and the gallbladder. A little later, two pancreatic buds (ventral and dorsal) originate as endodermal outgrowths of the duodenum (see Fig. 4-42). As the duodenum swings to the right during rotation of the stomach, the ventral pancreatic bud (which will form part of the pancreatic head and the uncinate process) swings around and fuses with the dorsal bud to form the union of the two pancreatic ducts (main and accessory ducts) and buds. This fused pancreas embraces the SMV and SMA, which are in relationship to these developing embryonic buds (see Figs. 4-20 and 4-42). The endoderm of the pancreas gives rise to the exocrine and endocrine cells of the organ, whereas the connective tissue stroma is formed by mesoderm.
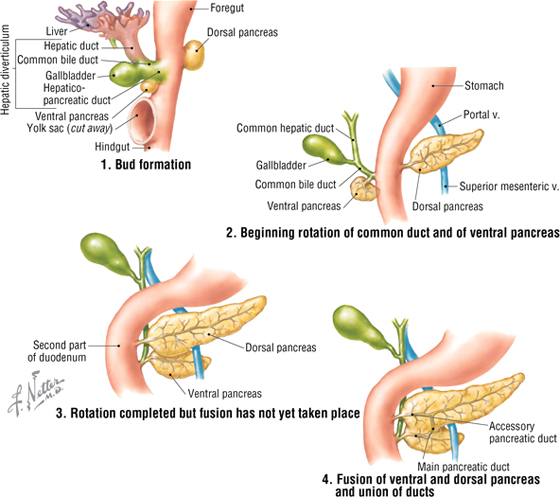
FIGURE 4-42 Development of the Hepatic Diverticulum and Pancreas
Urinary System Development
Initially, retroperitoneal intermediate mesoderm differentiates into the nephrogenic (kidney) tissue and forms the following (Fig. 4-43):
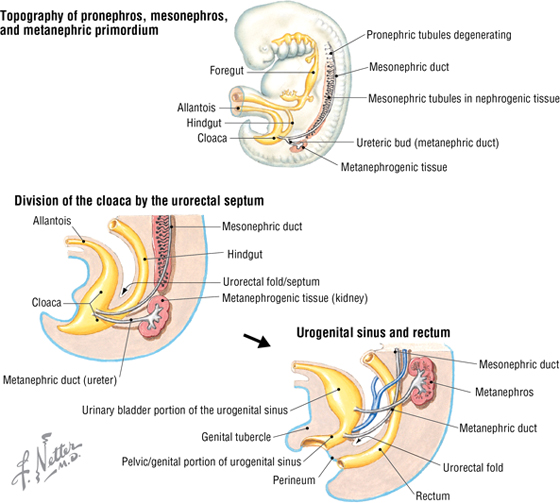
FIGURE 4-43 Development of the Kidney
- Pronephros, which degenerates
- Mesonephros with its mesonephric duct, which functions briefly before degenerating
- Metanephros, the definitive kidney tissue (nephrons and Loop of Henle) into which the ureteric bud (an outgrowth of the mesonephric duct) grows and differentiates into the ureter, renal pelvis, calyces, and collecting ducts
By differential growth and some migration, the kidney “ascends” from the sacral region, first with its hilum directed anteriorly and then medially, until it reaches its adult location (Fig. 4-44). Around the 12th week, the kidney becomes functional as the fetus swallows amniotic fluid, urinates into the amniotic cavity, and continually recycles fluid in this fashion. Toxic wastes, however, are removed via the placenta into the maternal circulation.
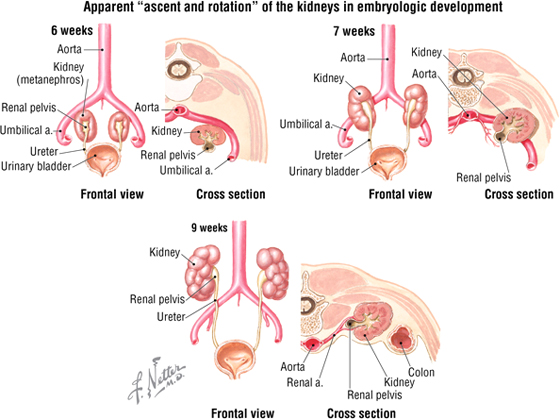
FIGURE 4-44 Ascent and Rotation of the Kidney
C L I N I C A L F O C U S
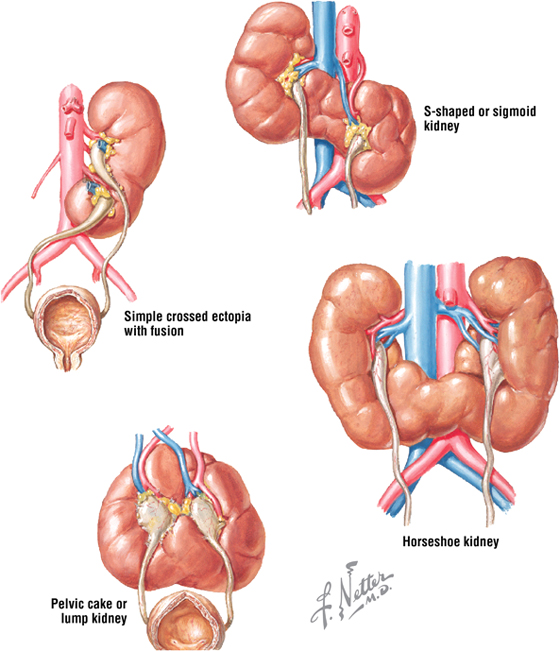
Renal Fusion
The term renal fusion refers to various common defects in which the two kidneys fuse to become one. The horseshoe kidney, in which developing kidneys fuse (usually the lower lobes) anterior to the aorta, often lies low in the abdomen and is the most common kind of fusion. Fused kidneys are close to the midline, have multiple renal arteries, and are malrotated. Obstruction, stone formation, and infection are potential complications.
Additional figures available online. See Table of Contents for Instructions for online access.

Adrenal (Suprarenal) Gland Development
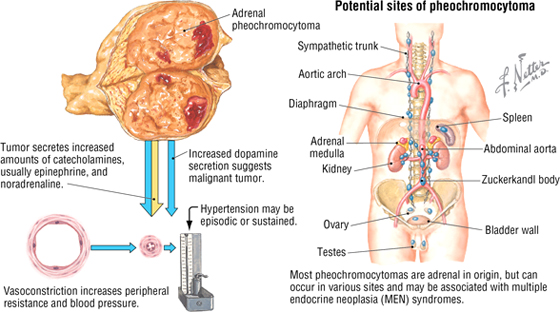
The adrenal cortex develops from mesoderm, whereas the adrenal medulla forms from neural crest cells, which migrate into the cortex and aggregate in the center of the gland. The cells of the medulla are essentially the postganglionic neurons of the sympathetic division of the ANS, but secrete mainly epinephrine and some norepinephrine into the blood as neuroendocrine cells.
C L I N I C A L F O C U S
Pheochromocytoma
Although pheochromocytomas are relatively rare neoplasms composed largely of adrenal medullary cells (which secrete excessive amounts of catecholamines), they can occur elsewhere throughout the body associated with the sympathetic chain or at other sites where neural crest cells typically migrate. Common clinical features include the following:
- Vasoconstriction and elevated blood pressure
- Headache, sweating, and flushing
- Anxiety, nausea, tremor, and palpitations or chest pain
Additional figures available online. See Table of Contents for Instructions for online access.

C L I N I C A L F O C U S
Online Figures
Acute abdomen: visceral etiology
Irritable bowel syndrome
Acute pyelonephritis
Additional figures available online. See Table of Contents for Instructions for online access.
