HEAD AND NECK
1. INTRODUCTION
3. SKULL
4. BRAIN
9. EAR
10. ORAL CAVITY
11. NECK
12. PHARYNX
13. LARYNX
16. EMBRYOLOGY
1. INTRODUCTION
The head and neck area offers a unique challenge for students because of the density of small neurovascular structures; the complexity of its bony features, especially the skull; and the compactness of its anatomy. The head protects the brain, participates in communication and expresses our emotions, and houses the special senses (sight, sound, balance, smell, and taste). The neck connects the head to the thorax and is the conduit for visceral structures passing cranially or caudally within tightly partitioned fascial sleeves.
The anatomy of the head is best understood if you think of it as a series of interconnected compartments, which include the following:
- Cranium: contains the brain and its meningeal coverings
- Orbits: contain the eye and the muscles that move the eye
- Nasal cavities: form the uppermost part of our respiratory system
- Ears: contain the apparatus for hearing and balance
- Oral cavity: forms the proximal end of the digestive tract
The anatomy of the neck is composed of a series of concentric-like compartments that provide a conduit for structures passing to the head or thorax. These compartments include the following:
- Musculofascial: a superficial compartment encompassing the outer boundary of the neck
- Visceral: an anterocentral compartment that contains the upper respiratory (pharynx, larynx, and trachea) and GI tracts (pharynx and esophagus), and the thyroid, parathyroid, and thymus glands
- Neurovascular: two anterolateral compartments called the carotid sheath, which contains the common carotid artery, internal jugular vein, and vagus nerve
- Prevertebral: posterocentral compartment that contains the cervical vertebrae and the associated paravertebral muscles
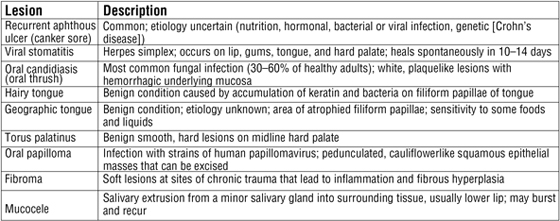
2. SURFACE ANATOMY
The key surface features of the head and neck are shown in Figure 8-1 and include the following:
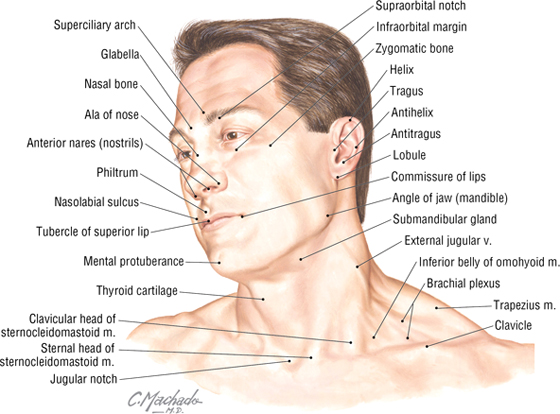
FIGURE 8-1 Key Surface Anatomy Landmarks
- Glabella: smooth prominence on the frontal bone above the root of the nose
- Zygomatic bone: the cheekbone, which protrudes below the orbit and is vulnerable to fractures from facial trauma
- Ear (auricle or pinna): skin-covered elastic cartilage with several consistent ridges, including the helix, antihelix, tragus, antitragus, and lobule
- Philtrum: midline infranasal depression of the upper lip
- Nasolabial sulcus: line between the nose and the corner of the lip
- Thyroid cartilage: the laryngeal prominence (“Adam’s apple”)
- Jugular (suprasternal) notch: midline depression between the two sternal heads of the sternocleidomastoid muscle
3. SKULL
The skull is composed of 22 bones (see Chapter 1, “Introduction to the Human Body”). Eight of these bones form the cranium (neurocranium, which contains the brain and meninges), and 14 of these form the face (viscerocranium). There are seven associated bones: the auditory ossicles (three in each middle ear) and the unpaired hyoid bone (Fig. 8-2 and Table 8-1).
FIGURE 8-2 Skull (Contd.)
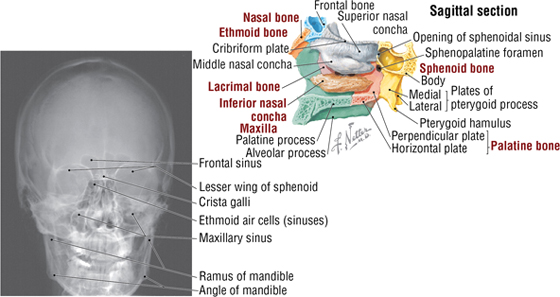
FIGURE 8-2 (Contd.) Skull
|
TABLE 8-1 Bones of the Skull
|
 |
Other features of the skull will be noted as we proceed through each region of the head. However, several general features of note include the following (see Fig. 8-2):
- Coronal suture: region between the frontal and two parietal bones
- Sagittal suture: region between the two parietal bones
- Lambdoid suture: region between the occipital bone and the two parietal bones
- Nasion: point at which the frontal and nasal bones meet
- Bregma: point at which coronal and sagittal sutures meet
- Lambda: point at which sagittal and lambdoid sutures meet
- Pterion: point at which frontal, sphenoid, temporal, and parietal bones meet; middle meningeal artery lies beneath this region
- Asterion: point at which temporal, parietal, and occipital bones meet
- Inion: the external occipital protuberance
Cranial Fossae
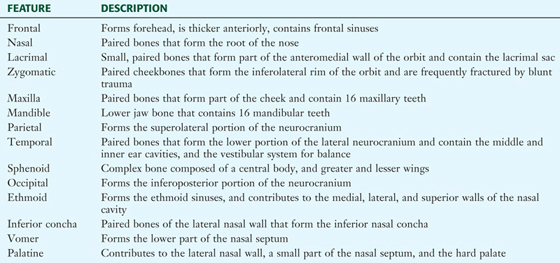
The cranial base (the floor of the neurocranium, which supports the brain) is divided into the following three cranial fossae, with each having numerous foramina (openings) for structures to pass in or out of the neurocranium (Fig. 8-3):
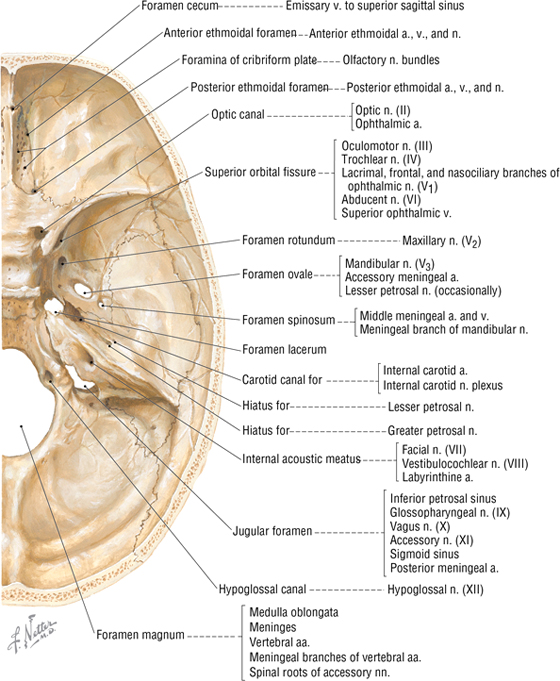
FIGURE 8-3 Superior Aspect of the Cranial Base (Cranial Fossae)
- Anterior: composes the roof of the orbits, and accommodates the frontal lobes of the brain
- Middle: accommodates the temporal lobes of the brain
- Posterior: accommodates the cerebellum, pons, and medulla oblongata of the brain
C L I N I C A L F O C U S
Skull Fractures
- Linear: presents with a distinct fracture line
- Comminuted: presents with multiple fragments (depressed if driven inward; can compress or tear the underlying dura mater)
- Diastasis: fracture along a suture line
- Basilar: fracture of the base of the skull
Any fracture that communicates with a lacerated scalp, a paranasal sinus, or the middle ear is termed a compound fracture. Compound depressed fractures must be treated surgically.
C L I N I C A L F O C U S
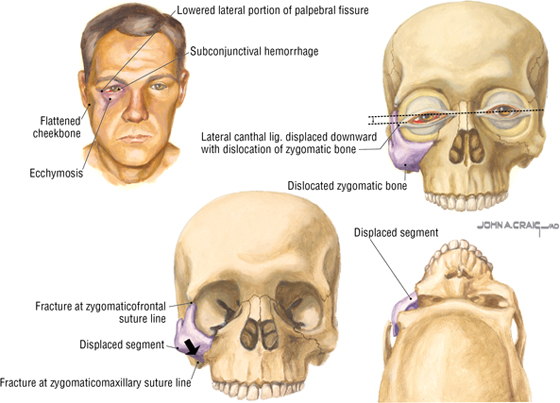
Zygomatic Fractures
Trauma to the zygomatic bone (cheekbone) can disrupt the zygomatic complex and its articulations with the frontal, maxillary, temporal, sphenoid, and palatine bones. Often, fractures involve suture lines with the frontal and maxillary bones, resulting in displacement inferiorly, medially, and posteriorly. The typical clinical presentation is illustrated. Ipsilateral ocular and visual changes may include diplopia (an upper outer gaze) and hyphema (blood in the anterior chamber of the eye), which requires immediate clinical attention.
C L I N I C A L F O C U S
Midface Fractures
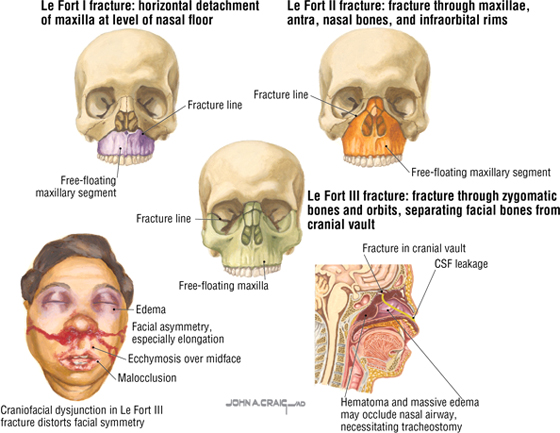
Midface fractures (of the maxilla, naso-orbital complex, and zygomatic bones) were classified by Le Fort as follows:
- Le Fort I: horizontal detachment of the maxilla at the level of the nasal floor
- Le Fort II: pyramidal fracture that includes both maxillae and nasal bones, medial portions of both maxillary antra, infraorbital rims, orbits, and orbital floors
- Le Fort III: includes Le Fort II and a fracture of both zygomatic bones; may cause airway problems, nasolacrimal apparatus obstruction, and cerebrospinal fluid (CSF) leakage
4. BRAIN
Meninges of the Brain
The brain and spinal cord are surrounded by three membranous connective tissue layers called the meninges, which include the following (Fig. 8-4):
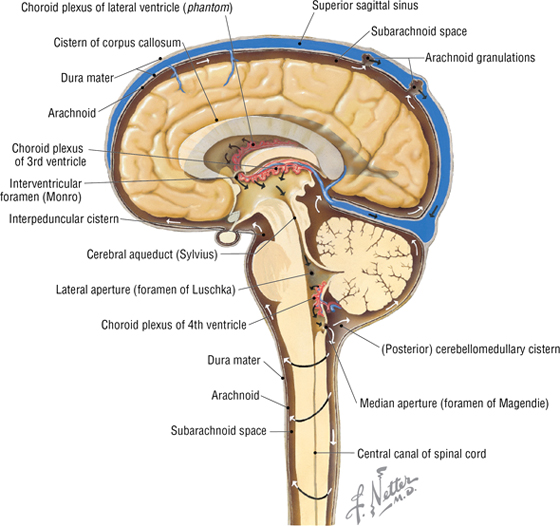
FIGURE 8-4 The CNS Meninges, CSF Circulation, and Arachnoid Granulations
- Dura mater: thick outermost meningeal layer that is richly innervated by sensory nerve fibers
- Arachnoid mater: fine, weblike avascular membrane directly beneath the dural surface; the space between the arachnoid and the underlying pia is called the subarachnoid space and contains CSF, which bathes and protects the CNS
- Pia mater: delicate membrane of connective tissue that intimately envelops the brain and spinal cord
The dura mater is richly innervated by meningeal sensory branches of the trigeminal nerve (CN III), the vagus nerve (CN X, specifically to the posterior cranial fossa), and the upper cervical nerves; the arachnoid and pia mater lack sensory innervation. The dura also forms thick connective tissue folds or layers that separate various brain regions and lobes (Figs. 8-4, 8-5, and 8-6):
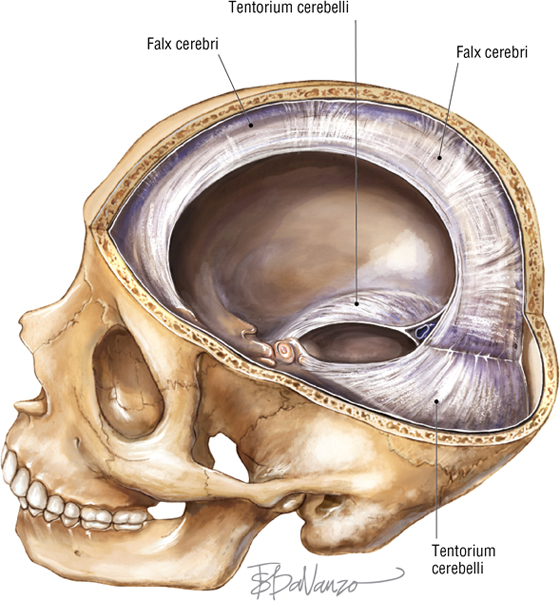
FIGURE 8-5 Dural Projections
- Falx cerebri: double layer of dura between the cerebral hemispheres
- Falx cerebelli: sickle-shaped layer of dura that projects between the two cerebellar hemispheres
- Tentorium cerebelli: fold of dura that covers the cerebellum and supports the occipital lobes of the cerebral hemispheres
- Diaphragma sellae: fold of dura that forms the roof of the sella turcica covering the pituitary gland
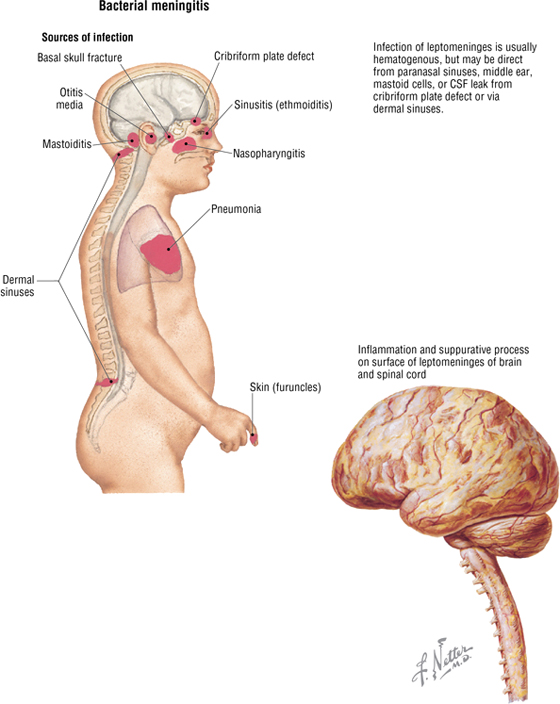
Dural Venous Sinuses
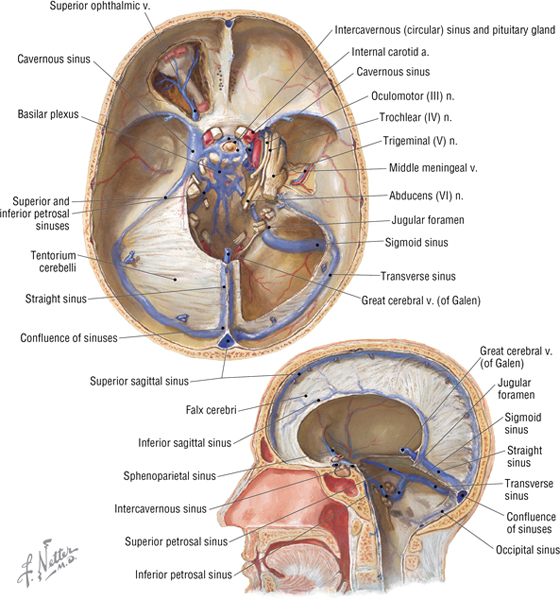
The dura also forms large venous channels between its periosteal and meningeal layers and elsewhere where two meningeal layers come together (Table 8-2 and Fig. 8-6). These dural venous sinuses drain blood from the brain, largely posteriorly and then into the internal jugular veins; however, these sinuses lack valves, so the direction of blood flow through them is pressure dependent.
|
TABLE 8-2 Dural Venous Sinuses
|
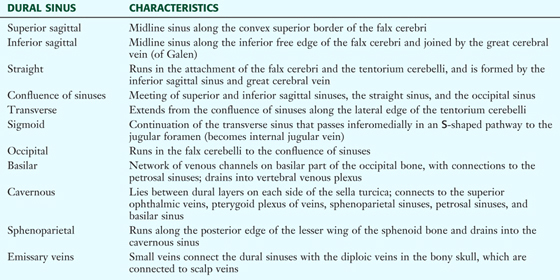 |
Subarachnoid Space
The subarachnoid space (between the arachnoid and pia mater) contains CSF, which performs the following functions (Figs. 8-4 and 8-7):
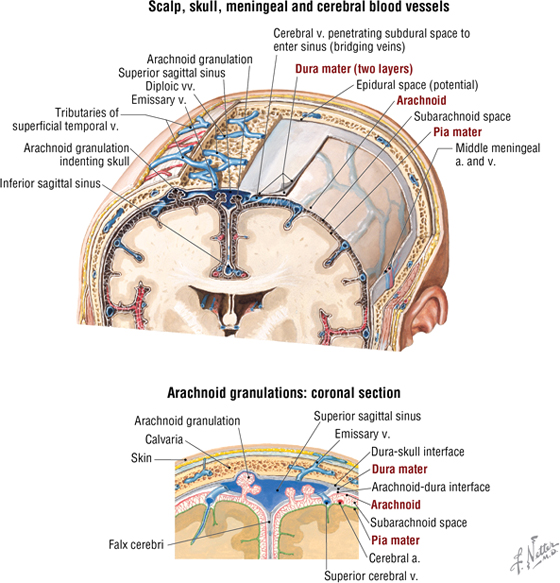
FIGURE 8-7 Relationship of Arachnoid Granulations and the Venous Sinus
- Supports and cushions the spinal cord and brain
- Fulfills some functions normally provided by the lymphatic system
- Occupies a volume of about 150 mL in the subarachnoid space
- Is produced by choroid plexuses in the brain’s ventricles
- Is produced at a rate of about 500-700 mL/day
- Is reabsorbed largely by arachnoid granulations and by small CNS capillaries
The arachnoid granulations absorb most of the CSF and deliver it to the dural venous sinuses (see Figs. 8-4 and 8-7). These granulations are composed of convoluted aggregations of arachnoid that extend as “tufts” into the superior sagittal sinus and function as one-way valves for the clearance of CSF. (CSF crosses into the venous sinus, but venous blood cannot enter the subarachnoid space.) Small, microscopic arachnoid cell herniations also occur along the spinal cord where CSF (which circulates at a higher pressure than venous blood) is delivered directly into spinal cord veins.
C L I N I C A L F O C U S
Meningitis
Meningitis is a serious condition defined as an inflammation of the arachnoid and pia mater. It results most often from bacterial or aseptic causes. Aseptic causes include viral infections, drug reactions, and systemic diseases. Patients with meningitis usually present with the following symptoms:
- Headache
- Fever
- Seizures
- Painful stiff neck
Diagnosis is made by performing a lumbar puncture and examining the CSF.
C L I N I C A L F O C U S
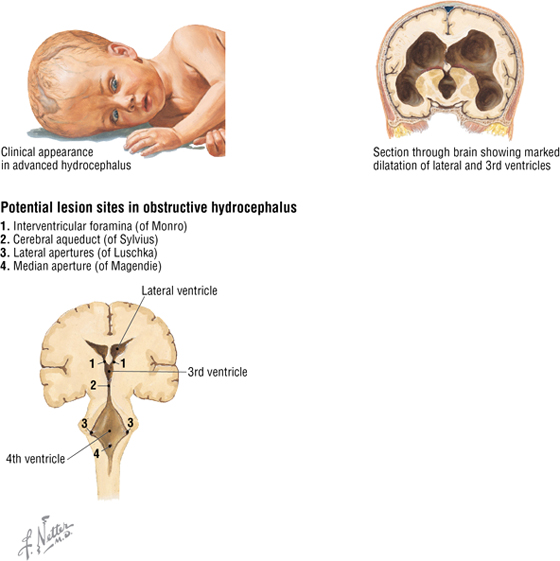
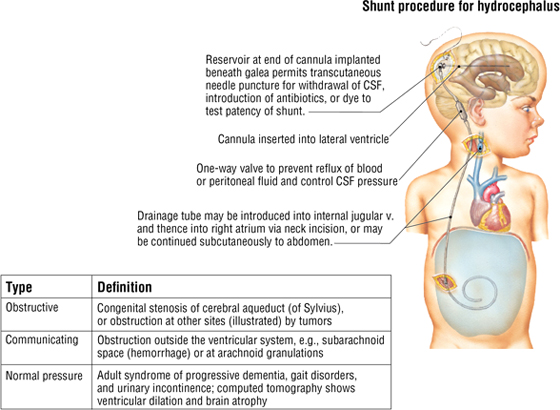
Hydrocephalus
Hydrocephalus is the accumulation of excess CSF within the brain’s ventricular system. It is caused by either overproduction or decreased absorption of CSF.
Gross Anatomy of the Brain
The most notable feature of the human brain is its large cerebral hemispheres (Figs. 8-8). Several circumscribed regions of the cerebral cortex are associated with specific functions, and key surface landmarks of the typical human cerebrum are used to divide it into lobes (four or five, depending on classification, with the fifth being either the insula or the limbic lobe). The lobes and their functions are as follows:
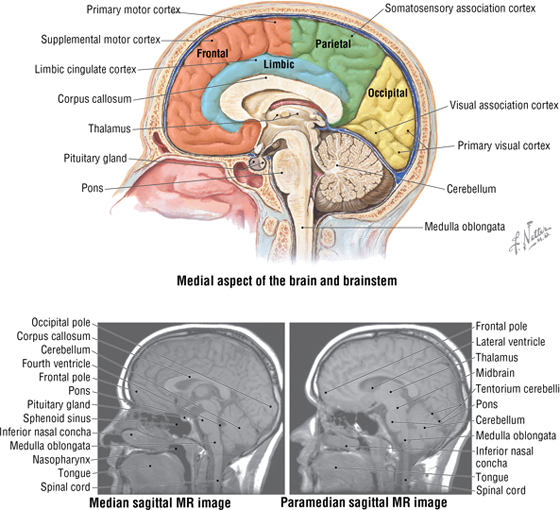
FIGURE 8-8 Brain and Brainstem
- Frontal: affects motor control, expressive speech, personality, and drive
- Parietal: affects sensory input, representation and integration, and receptive speech
- Occipital: affects visual input and processing
- Temporal: affects auditory input and memory integration
- Insula: a fifth deep lobe that lies medial to the temporal lobe (sometimes included as part of the temporal lobe); influences emotions and limbic functions
- Limbic: a fifth medial lobe (cingulate cortex); influences emotions and autonomic functions
Other key areas of the brain include the following components (see Fig. 8-8):
- Thalamus: gateway to the cortex; simplistically functions as an “executive secretary” to the cortex (relay center between cortical and subcortical areas)
- Cerebellum: coordinates smooth motor activities, and processes muscle position
- Brainstem: includes the midbrain, pons, and medulla oblongata; conveys motor and sensory information from the body and autonomic and motor information from higher centers to peripheral targets
Internally, the brain contains four ventricles, two lateral ventricles, and a central third and fourth ventricle (Fig. 8-9). CSF, which is produced by the choroid plexus (see Fig. 8-4), circulates through these ventricles and then enters the subarachnoid space through two lateral apertures (foramen of Luschka) or a median aperture (foramen of Magendie) in the fourth ventricle.
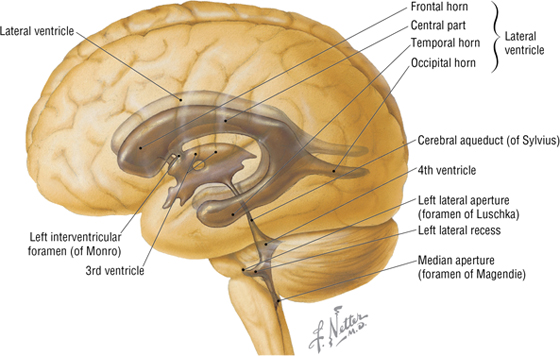
FIGURE 8-9 Ventricular System of the Brain
Blood Supply to the Brain
Arteries supplying the brain arise largely from the following two pairs of arteries (Fig. 8-10 and Table 8-3):
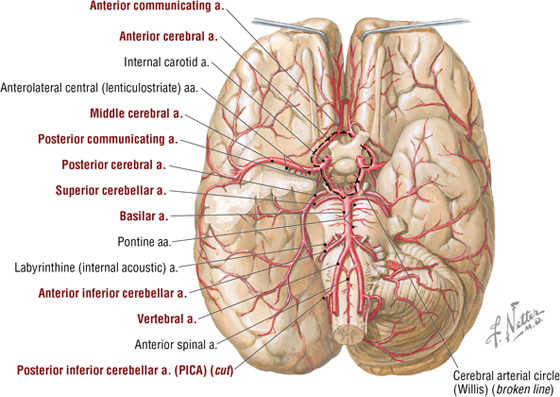
FIGURE 8-10 Arterial Circle on the Base of the Brain
|
TABLE 8-3 Blood Supply to the Brain
|
 |
- Vertebrals: arise from the subclavian artery, ascend through the transverse foramina of the C1-C6 vertebrae, and enter the foramen magnum of the skull
- Internal carotids: arise from the common carotid in the neck, ascend in the neck, enter the carotid canal, and traverse the foramen lacerum to terminate as the middle and anterior cerebral arteries, which anastomose with the arterial circle of Willis
C L I N I C A L F O C U S
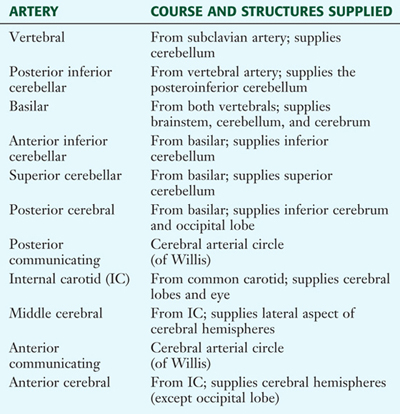
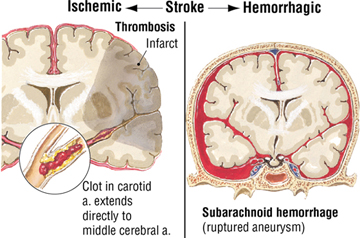
Subarachnoid Hemorrhage
Subarachnoid hemorrhage usually occurs from an arterial source and results in the collection of blood between the arachnoid and pia mater. The most common cause of subarachnoid hemorrhage is the rupture of a saccular, or berry, aneurysm.
C L I N I C A L F O C U S
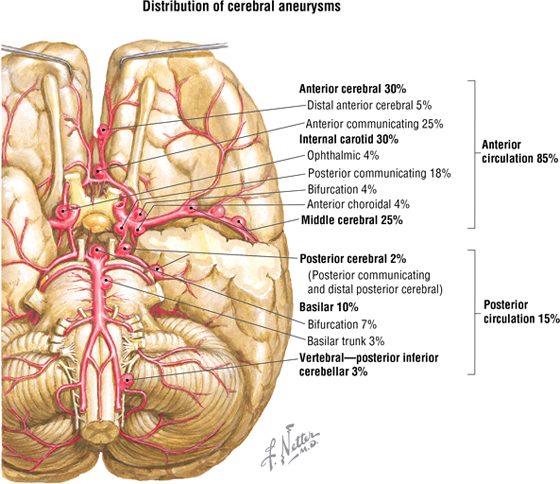
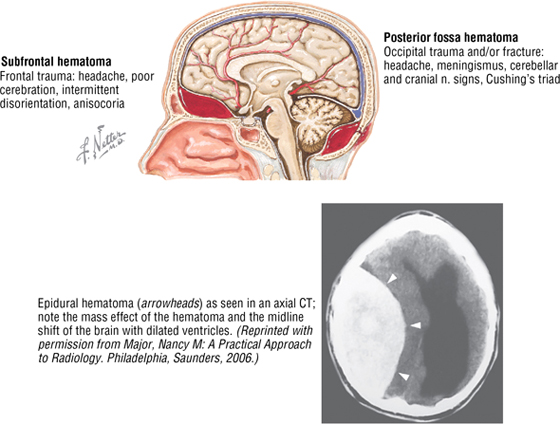
Epidural Hematomas
Epidural hematomas result most often from vehicular accidents, falls, and sports injuries. The blood collects between the periosteal dura and the bony cranium. The source of the bleeding is usually arterial (85%); common locations include the frontal, temporal (middle meningeal artery is very susceptible, especially where it lies deep to the pterion), and occipital regions.
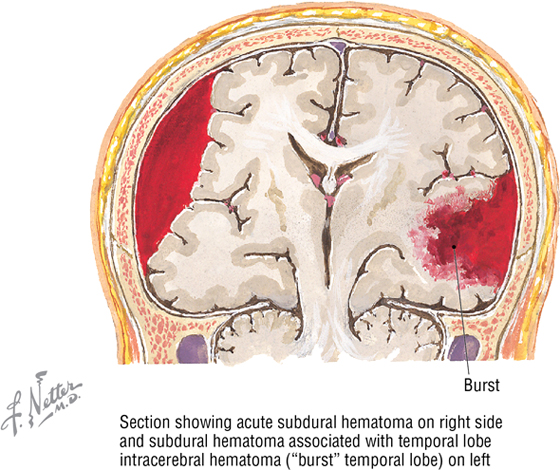
C L I N I C A L F O C U S
Subdural Hematomas
Subdural hematomas are usually due to an acute venous hemorrhage of the cortical bridging veins draining cortical blood into the superior sagittal sinus. Half are associated with skull fractures. In a subdural hematoma, the blood collects between the dura and the arachnoid mater. Clinical signs include a decreasing level of consciousness, ipsilateral pupillary dilation, headache, and contralateral hemiparesis. These hematomas may develop within 1 week after injury but often present with clinical signs within hours. Chronic subdural hematomas are most common in the elderly and chronic alcoholics who have some brain atrophy, which increases the space traversed by the bridging veins and renders the stretched vein susceptible to tearing.
C L I N I C A L F O C U S
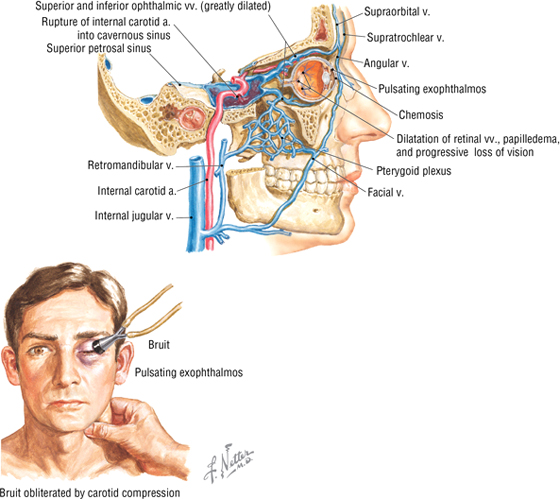
Carotid-Cavernous Sinus Fistula
More common than symptomatic intracavernous sinus aneurysms but less common than subarachnoid saccular (berry) aneurysms, carotid-cavernous sinus fistulas often result from trauma and are more common in men than in women. They are high-pressure (arterial), low-flow lesions characterized by an orbital bruit, exophthalmos, chemosis, and extraocular muscle palsies (involving cranial nerves III, IV, and VI). Blood collecting in the cavernous sinus drains by several venous pathways, as the sinus has connections with other dural venous sinuses as well as the ophthalmic veins and pterygoid plexus of veins in the infratemporal region.
C L I N I C A L F O C U S
Stroke
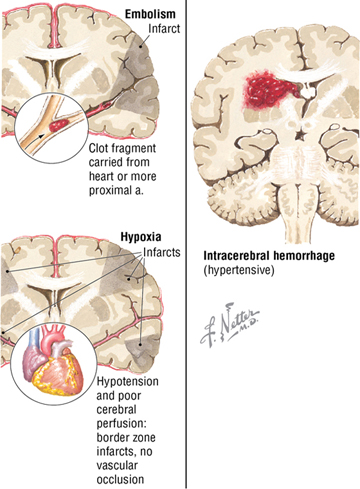
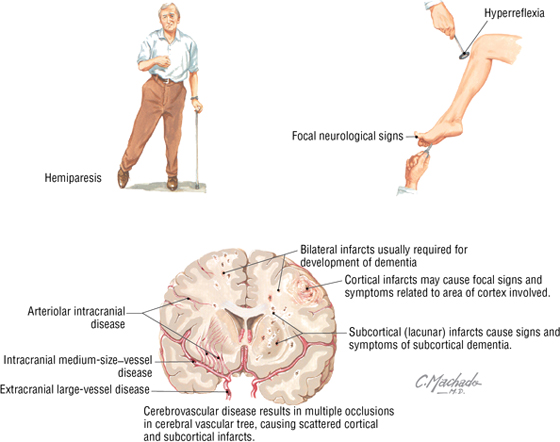
Stroke is a localized brain injury caused by a vascular episode that lasts more than 24 hours, whereas transient ischemic attacks (TIAs) are focal ischemic episodes that last less than 24 hours. Stroke is classified into the following two types:
- Ischemic (80%) (infarction): thrombotic or embolic, resulting from atherosclerosis of the extracranial (usually carotid) and/or intracranial arteries, or from underlying heart disease
- Hemorrhagic: occurs when a cerebral vessel weakens and ruptures (subarachnoid or intracerebral hemorrhage), which causes intracranial bleeding, usually affecting a larger brain area
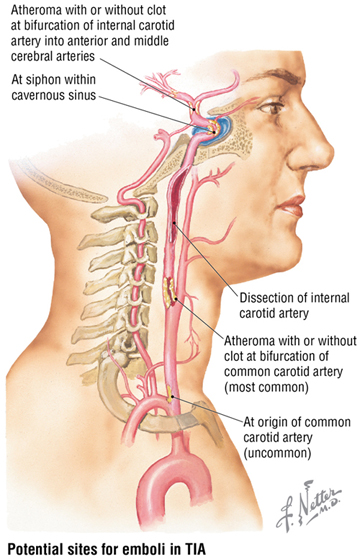
C L I N I C A L F O C U S
Transient Ischemic Attack (TIA)
A transient ischemic attack is a temporary interruption of focal brain circulation that results in a neurological deficit that lasts less than 24 hours (more commonly lasts 15 minutes to 1 hour). The most common cause of TIA is embolic disease from the heart, carotid, or cerebral vessels, which may temporarily block a vessel. The onset of the deficit is abrupt, and recovery is gradual; the most common deficits include the following:
- Hemiparesis
- Hemisensory loss
- Aphasia
- Confusion
- Hemianopia
- Ataxia
- Vertigo
C L I N I C A L F O C U S
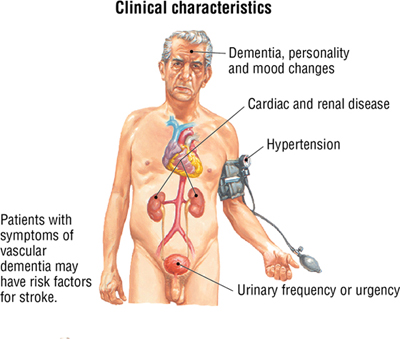
Vascular (Multi-infarct) Dementia
Dementia is an acquired neurological syndrome that presents with multiple cognitive deficits. By definition, it includes one or more of the following: short-term memory impairment, behavioral disturbance, and difficulties with daily functioning and independence. It can be classed as degenerative, vascular, alcoholic, or HIV related. Vascular dementias, resulting from anoxic damage from small infarcts, account for about 15% to 20% of dementia cases. Multi-infarct dementia is associated with heart disease, diabetes mellitus, hypertension, and inflammatory diseases.
C L I N I C A L F O C U S
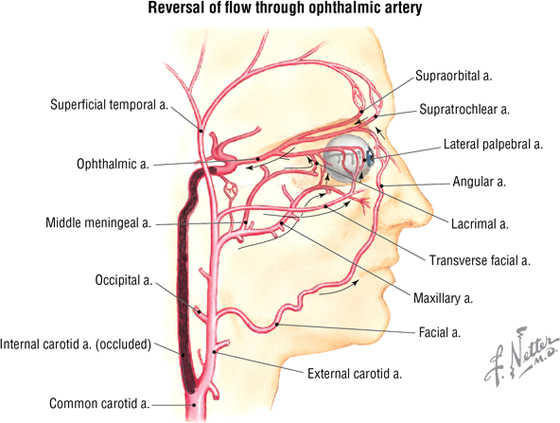
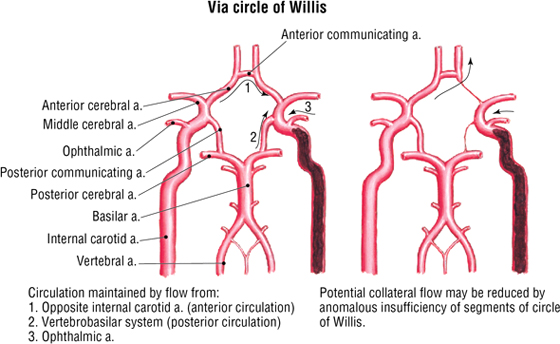
Collateral Circulation after Internal Carotid Artery Occlusion
If a major artery, such as the internal carotid artery, becomes occluded, extracranial and intracranial (circle of Willis) anastomoses may provide collateral routes of circulation. These routes are more likely to develop when occlusion is gradual (as in atherosclerosis) rather than acute (as in embolic obstruction).
C L I N I C A L F O C U S
Brain Tumors
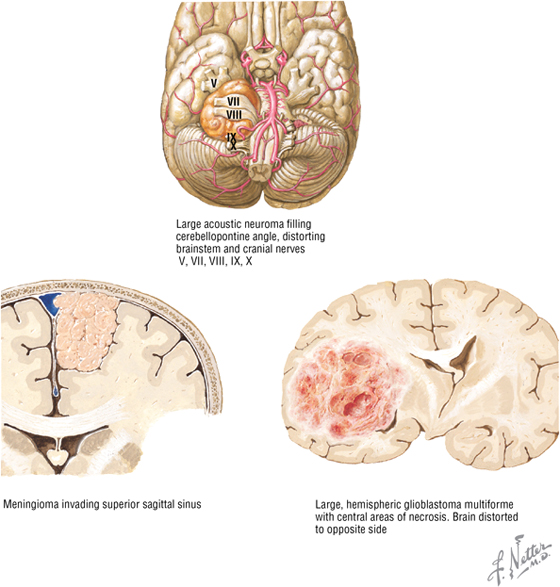
Clinical signs and symptoms of brain tumors depend on the location and the degree to which intracranial pressure (ICP) is elevated. Slow-growing tumors in relatively silent areas (e.g., frontal lobes) may go undetected and can become quite large before symptoms occur. Small tumors in key brain areas can lead to seizures, hemiparesis, or aphasia. Increased ICP can initiate broader damage by compressing critical brain structures. Early symptoms of increased ICP include malaise, headache, nausea, papilledema, and, less often, abducent nerve palsy and Parinaud’s syndrome; classic signs of hydrocephalus are loss of upward gaze, downward ocular deviation (“setting sun” syndrome), lid retraction, and light-near dissociation of pupils. Primary tumors include the following:
- Gliomas: arise from astrocytes or oligodendrocytes; glioblastoma multiforme is the most malignant form (astrocytic series)
- Meningiomas: arise from the arachnoid mater and can extend into the brain
- Pituitary tumors: can expand in the sella turcica and affect cranial nerves II, III, IV, V1, V2, and VI; about 15% of primary tumors
- Neuromas: acoustic neuroma, a benign tumor of CN VIII, is a common example; about 7% of primary tumors
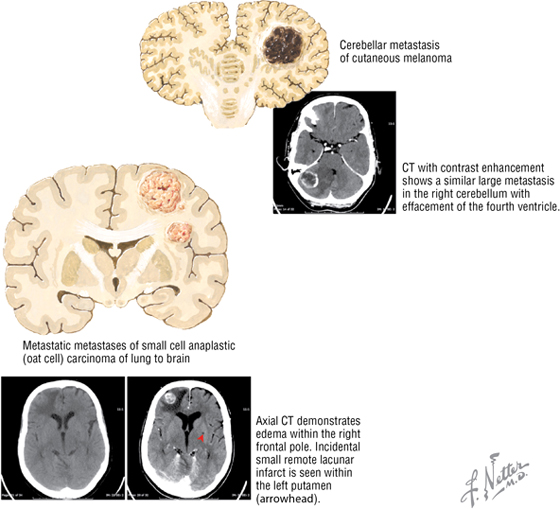
C L I N I C A L F O C U S
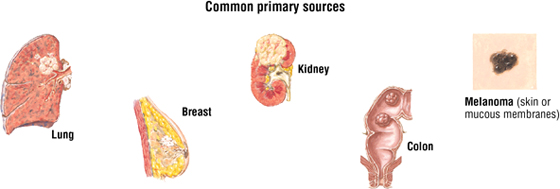
Metastatic Brain Tumors
Metastatic brain tumors are more common than primary brain tumors. Most spread via the bloodstream, with cells seeded between the white (fiber tract pathways) and gray (cortical neurons) matter. Some tumors metastasize directly from head and neck cancers, or by means of Batson’s vertebral venous plexus. Presentation often includes headache (50%), seizures (25%), and elevated intracranial pressure
Cranial Nerves
Please see Chapter 1, “Introduction to the Human Body,” for an overview of the general organization of the nervous system.
In addition to the 31 pairs of spinal nerves, 12 pairs of cranial nerves (CN) arise from the brain. They are identified both by name and by Roman numerals CN I to CN XII (Fig. 8-11). Cranial nerves are somewhat unique and may contain the following multiple functional components:
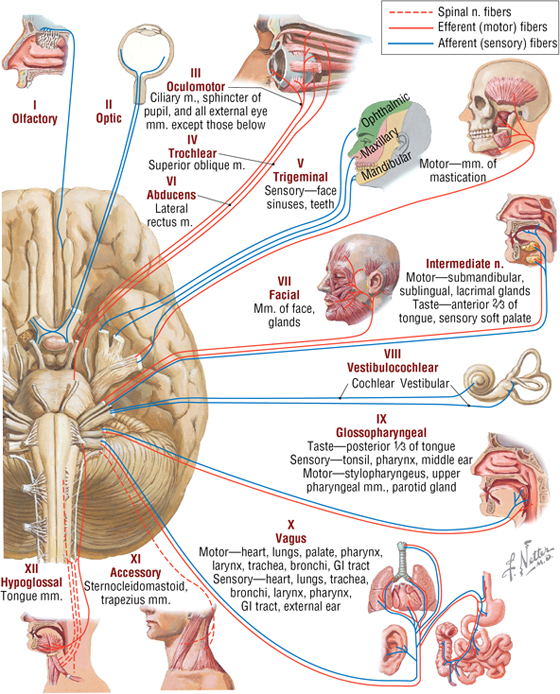
FIGURE 8-11 Overview of the Cranial Nerves (specific details omitted)
- General (G): same general functions as spinal nerves
- Special (S): functions found only in cranial nerves (special senses)
- Afferent (A) or efferent (E): sensory or motor functions, respectively
- Somatic (S) or visceral (V): related to skin and skeletal muscle innervation (somatic), or to smooth muscle, cardiac muscle, and glands (visceral)
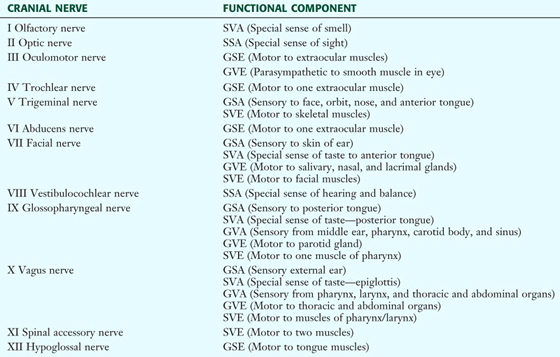
Each cranial nerve is classified as either general (G) or special (S), and then somatic (S) or visceral (V), and finally afferent (A) or efferent (E) (Table 8-4). For example, a cranial nerve that is classified GVE (general visceral efferent) means it contains motor fibers to visceral structures like a parasympathetic or sympathetic fiber from the spinal cord.
|
TABLE 8-4 Functional Components of the Cranial Nerves
|
 |
In general, cranial nerves are described as follows:
- CN I and II: arise from the forebrain; are really tracts of the brain for the special senses of smell and sight
- CN III, IV, and VI: move the extraocular skeletal muscles of the eyeball
- CN V: has three divisions; V1 and V2 are sensory, and V3 is both motor and sensory
- CN VII, IX, and X: are both motor and sensory
- CN VIII: is the special sense of hearing and balance
- CN XI and XII: are motor to skeletal muscle
- CN III, VII, IX, and X: also contain parasympathetic (visceral) fibers of origin, although many of these autonomic fibers “jump” onto branches of CN V to reach their targets
Rather than describe each cranial nerve and all its branches in detail at this time, we will review each nerve anatomically and clinically as we encounter it in the various regions of the head and neck. It may be helpful to refer back to this section each time you are introduced to a new region and its cranial nerve innervation.
5. SCALP AND FACE
Layers of the Scalp
The layers of the scalp spell “S-C-A-L-P” and include the following:
- Skin
- Connective tissue that contains the blood vessels of the scalp
- Aponeurosis (galea aponeurotica) of the epicranial muscles (frontalis and occipitalis)
- Loose connective tissue deep to the aponeurosis, which contains emissary veins that communicate with the cranial diploë and dural sinuses within the cranium
- Periosteum (pericranium) on the surface of the bony skull
Muscles of Facial Expression
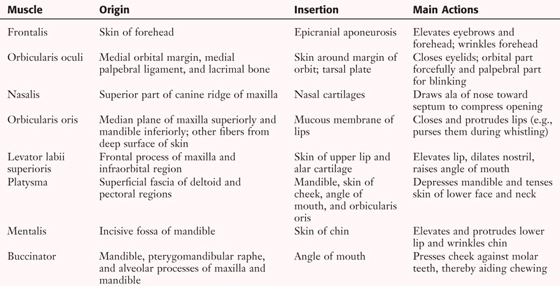
The muscles of facial expression are skeletal muscles that lie in the subcutaneous tissue of the face. They are all innervated by the terminal motor branches of the facial nerve (CN VII) and take origin from the underlying facial skeleton, but insert into the skin or facial cartilages (Fig. 8-12 and Table 8-5).
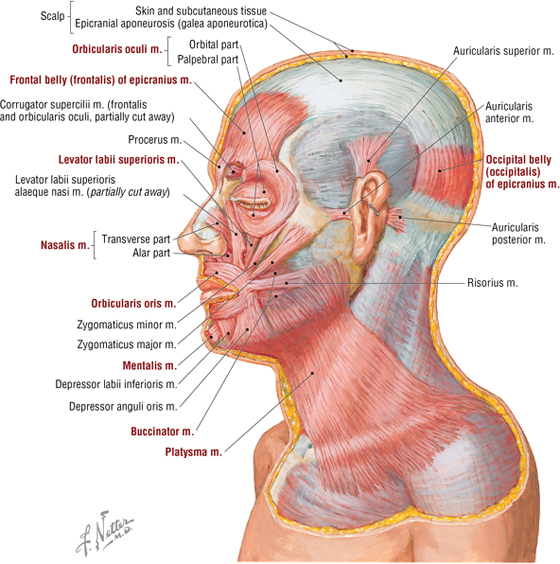
FIGURE 8-12 Muscles of Facial Expression
|
TABLE 8-5 Summary of Major Facial Muscles
|
 |
C L I N I C A L F O C U S
Scalp Wounds
Scalp wounds tend to bleed profusely for several reasons. The scalp is supplied by a rich arterial network, and the blood vessels reside in the tough connective tissue layer, which has a tendency to hold the small arteries open rather than let them retract into the subcutaneous tissue.
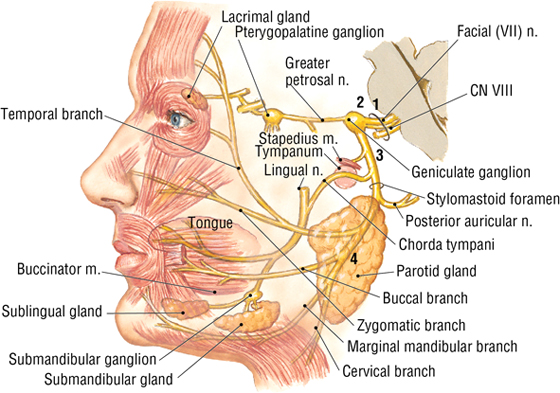
Innervation of the facial muscles is by the five terminal branches of CN VII. The facial nerve emerges from the stylomastoid foramen, passes through the parotid salivary gland, and then distributes over the face and neck (Fig. 8-13). The five terminal branches are as follows:
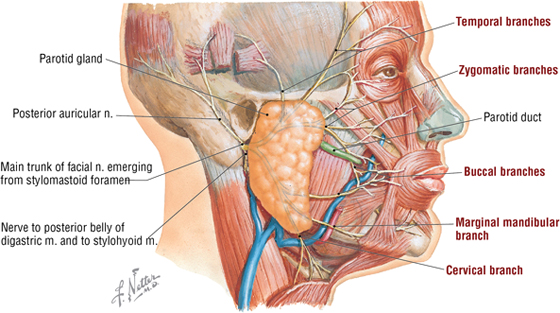
FIGURE 8-13 Terminal Branches of the Facial Nerve and Parotid Gland
- Temporal
- Zygomatic
- Buccal
- Marginal mandibular
- Cervical
The sensory innervation of the face is by the three divisions of the trigeminal nerve (CN V), with some contributions by the cervical plexus. (Figure 8-14 lists the specific nerves for each division.) The sensory neurons in CN V reside in the trigeminal (semilunar, gasserian) ganglion, which is divided as follows:
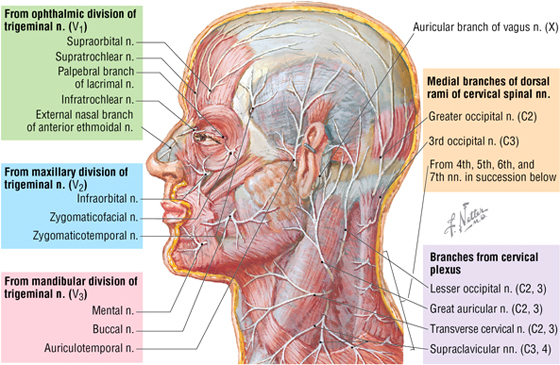
FIGURE 8-14 Cutaneous Nerves of the Face and Neck
- Ophthalmic (V1) division
- Maxillary (V2) division
- Mandibular (V3) division
The blood supply to the face includes the following vessels (Fig. 8-15):
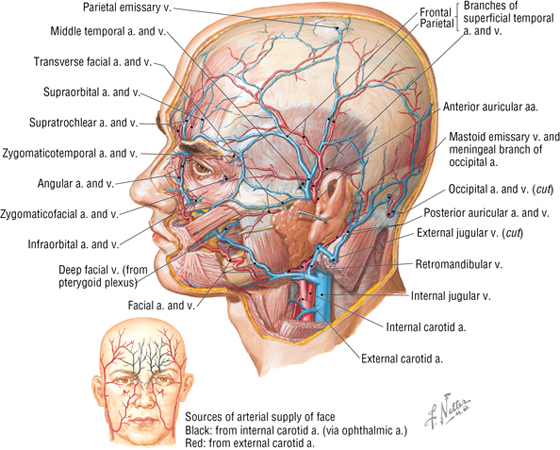
FIGURE 8-15 Arteries and Veins of the Face
- Facial artery: arises from the external carotid artery (ECA)
- Superficial temporal artery: arises from the ECA
- Ophthalmic artery: arises from the internal carotid artery, and distributes over the forehead
- Facial vein: drains into the internal jugular vein, directly or as a common facial vein
- Retromandibular vein: formed by the union of the maxillary and superficial temporal veins; ultimately drains into the external jugular vein
- Ophthalmic veins: tributaries from the forehead drain into superior and inferior ophthalmic veins in the orbit (and also anastomose with the facial vein) and then posteriorly into the cavernous dural sinus
C L I N I C A L F O C U S
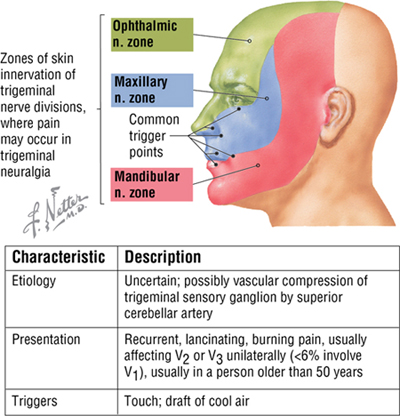
Trigeminal Neuralgia
Trigeminal neuralgia (or tic douloureux) is a neurological condition characterized by episodes of brief, intense facial pain over one of the three areas of distribution of CN V. The pain is so intense that the patient winces, which produces a facial muscle tic.
C L I N I C A L F O C U S
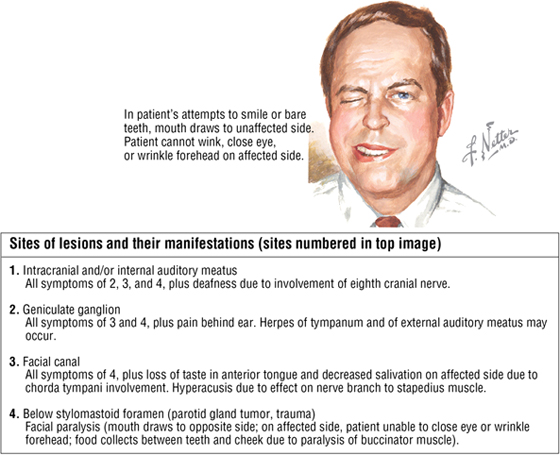
Facial Nerve (Bell’s) Palsy
Acute, unilateral idiopathic facial palsy is the most common cause of facial muscle weakness and cranial neuropathy. Facial nerve palsy also may be caused by herpes simplex virus (HSV) infection. Manifestations associated with lesions at various points along the path of CN VII are illustrated.
C L I N I C A L F O C U S
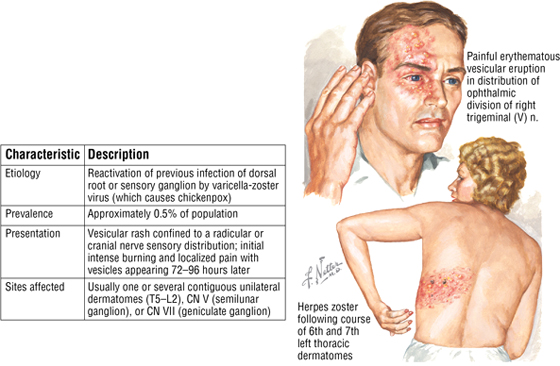
Herpes Zoster (Shingles)
Herpes zoster, or shingles, is the most common infection of the peripheral nervous system (PNS). It is an acute neuralgia confined to the dermatome distribution of a specific spinal or cranial sensory nerve root
C L I N I C A L F O C U S
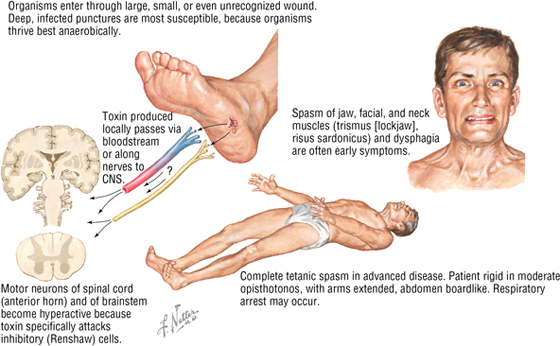
Tetanus
The PNS motor unit is vulnerable to three bacteria-produced toxins: tetanospasmin (motor neuron), diphtheria toxin (peripheral nerve), and botulin (neuromuscular junction). The hearty spore of Clostridium tetani is commonly found in soil, dust, and feces and can enter the body through wounds, blisters, burns, skin ulcers, insect bites, and surgical procedures. Symptoms include restlessness, low-grade fever, and stiffness or soreness. Eventually, nuchal rigidity, trismus (lockjaw), dysphagia, laryngospasm, and acute, massive muscle spasms can occur. Prophylaxis (immunization) is the best management.
6. ORBIT AND EYE
Bony Orbit
The bones contributing to the orbit include the following (Fig. 8-16):
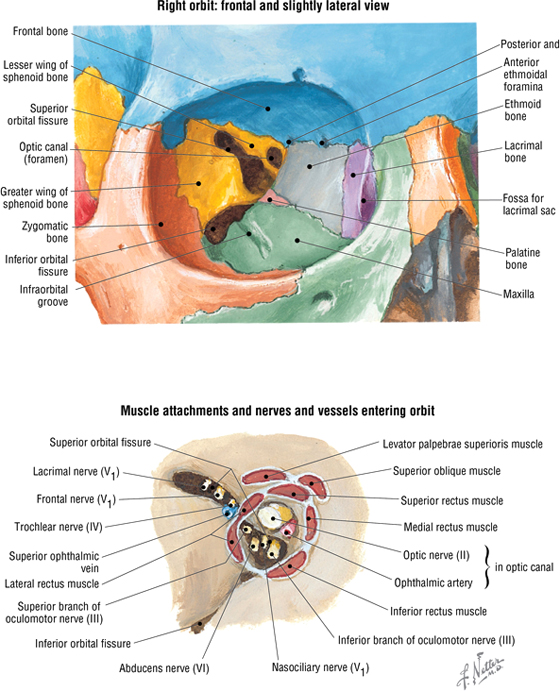
FIGURE 8-16 Bony Orbit and Its Openings
- Frontal (orbital surface)
- Maxillary (orbital surface)
- Zygomatic (orbital surface)
- Sphenoid
- Palatine (orbital plate)
- Ethmoid (orbital plate)
- Lacrimal
The back of the orbit has three large openings that include the following (see Fig. 8-16):
- Superior orbital fissure: CN III, IV, VI, and V1 (frontal, lacrimal, and nasociliary nerves) pass through the fissure along with the ophthalmic vein
- Inferior orbital fissure: CN V2 and infraorbital vessels pass through this fissure
- Optic canal: CN II and the ophthalmic artery pass through this canal
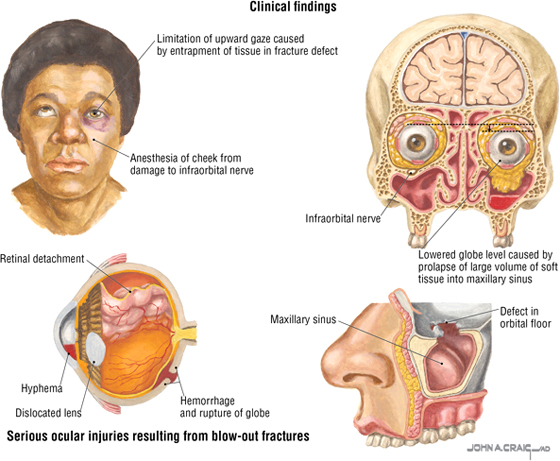
C L I N I C A L F O C U S
Orbital Blow-out Fracture
A massive zygomaticomaxillary complex fracture or a direct blow to the front of the orbit (e.g., by a baseball or a fist) may cause a rapid increase in intraorbital pressure and a resulting blow-out fracture of the thin orbital floor. In severe comminuted fractures of the orbital floor, the orbital soft tissues may herniate into the underlying maxillary paranasal sinus. Clinical signs include diplopia, infraorbital nerve paresthesia, enophthalmos, edema, and ecchymosis.
Eyelids and Lacrimal Apparatus
The eyelids protect the eyeballs and keep the corneas moist. Each eyelid contains a tarsal plate of dense connective tissue; tarsal glands that secrete an oily mixture into the tears; and a small slip of smooth muscle (superior tarsal [Müller’s] muscle) in the superior eyelid, which attaches to the tarsal plate along with the levator palpebrae superioris muscle (Fig. 8-17). The tears contain albumins, lactoferrin, lysozyme, lipids, metabolites, and electrolytes. The lacrimal apparatus includes the following (see Fig. 8-17):
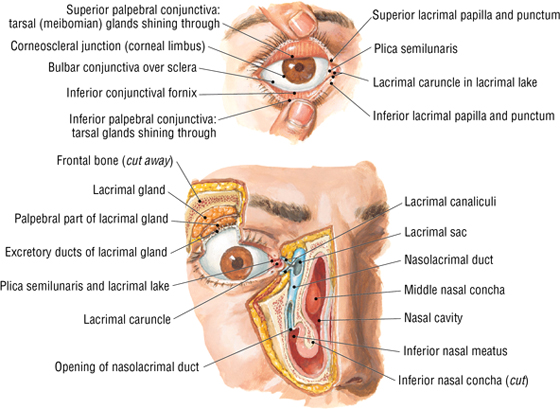
FIGURE 8-17 Eyelids and the Lacrimal Apparatus (Contd.)
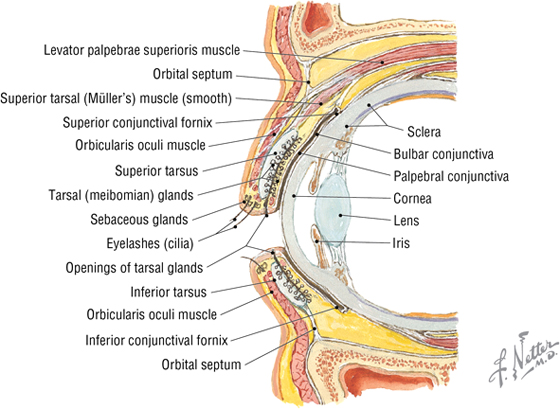
FIGURE 8-17 (Contd.) Eyelids and the Lacrimal Apparatus
- Lacrimal glands: secrete tears; innervated by the facial nerve parasympathetics
- Lacrimal ducts: excretory ducts of the glands
- Lacrimal canaliculi: collect tears into openings on the lids called the puncta, and convey them to the lacrimal sacs
- Lacrimal sacs: collect tears and release them into the nasolacrimal duct when one blinks (contraction of the orbicularis oculi muscle)
- Nasolacrimal ducts: convey tears from lacrimal sacs to the inferior meatus of the nasal cavity
The lacrimal glands receive secretomotor parasympathetic fibers from the facial nerve (CN VII) that originate in the superior salivatory nucleus; travel in the greater petrosal and vidian (nerve of the pterygoid canal) nerves; synapse in the pterygopalatine ganglion; and send postganglionic fibers via the maxillary, zygomatic, and lacrimal nerves to the lacrimal gland (see Fig. 8-65).
Muscles
The orbital muscles include six extraocular skeletal muscles that move the eyeball and one skeletal muscle that elevates the upper eyelid (Fig. 8-18 and Table 8-6). In addition to the movements of elevation, depression, abduction, and adduction, two muscles (superior rectus and oblique muscles) medially rotate (intorsion) the eyeball, and two muscles (inferior rectus and oblique muscles) laterally rotate (extorsion) the eyeball.
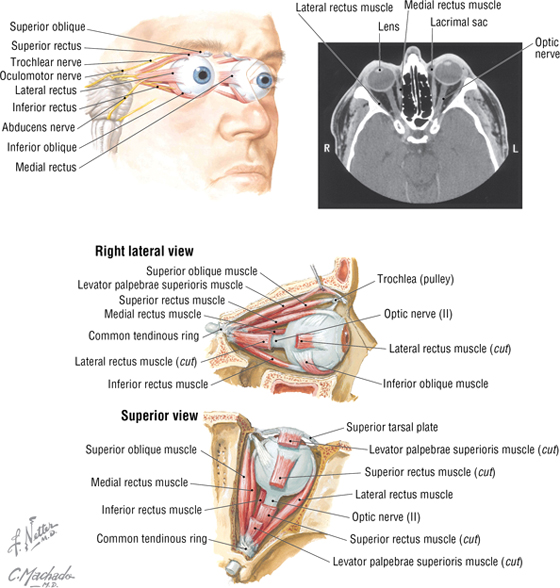
FIGURE 8-18 Orbital Muscles. (CT reprinted with permission from Kelley LL, Petersen C: Sectional Anatomy for Imaging Professionals. Philadelphia, Mosby, 2007.)
|
TABLE 8-6 Summary of Orbital Muscles
|
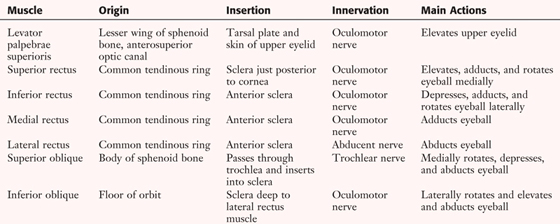 |
C L I N I C A L F O C U S
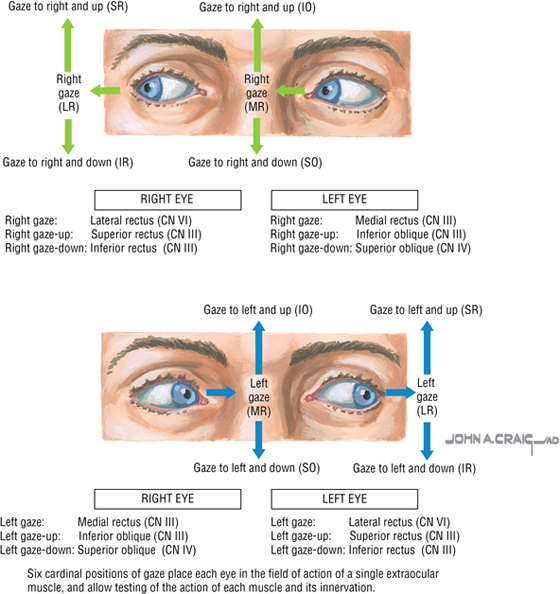
Clinical Testing of the Extraocular Muscles
Because extraocular muscles act as synergists and antagonists and may be responsible for multiple movements, it is difficult to test each muscle individually. However, the generalist physician can obtain an idea of extraocular muscle (or nerve) impairment by checking the ability of individual muscles to elevate or depress the globe with the eye abducted or adducted, thereby aligning the globe with the pull (line of contraction) of the muscle. Generally, intorsion and extorsion are too difficult to assess in a routine eye examination. One can use an H pattern to assess how each eye tracks movement of an object (the tester’s finger). For example, when the finger is held up and to the right of the patient’s eyes, the patient must primarily use the SR of the right eye and the IO of the left eye to focus on the finger. Pure abduction is done by the lateral rectus, and pure adduction is done by the medial rectus. In all other cases, two muscles elevate the eye (superior rectus [SR] and inferior oblique [IO], with minimal intorsion or extorsion) and two muscles depress the eye (inferior rectus [IR] and superior oblique [SO], with minimal intorsion or extorsion) in abduction and adduction, respectively. At the end of this test, the examiner can bring the finger directly to the midline to test convergence (medial rectus muscles). If an eye movement disorder is detected via this method, a clinical specialist may be consulted for further evaluation.
Nerves in the Orbit
Three cranial nerves innervate the extraocular skeletal muscles (Table 8-6), one cranial nerve mediates the special sense of sight (CN II), and one cranial nerve conveys general sensory information from the orbit and eye (CN V1) (Fig. 8-19). The major branches of the ophthalmic nerve (CN V1) include the following:
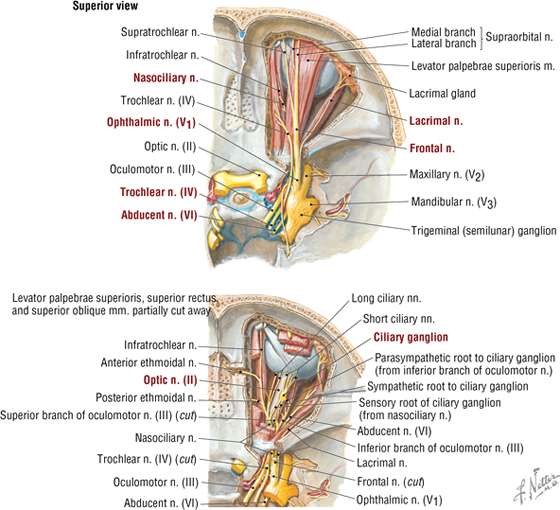
FIGURE 8-19 Nerves of the Orbit
- Frontal: runs on the superior aspect of the levator palpebrae superioris muscle and ends as the supratrochlear and supraorbital nerves; sensory to forehead, scalp, frontal sinus, and upper eyelid
- Lacrimal: courses laterally on the superior aspect of the lateral rectus muscle to the lacrimal gland; sensory to conjunctiva and skin of the upper eyelid
- Nasociliary: gives rise to short and long ciliary nerves, posterior and anterior ethmoidal nerves, and infratrochlear nerve; sensory to iris and cornea, sphenoid and ethmoid sinuses, lower eyelid, lacrimal sac, and skin of the nose
The optic nerve (CN II) is actually a brain tract that conveys sensory information from the retina, via the ganglion cell axons, to the brain (see Fig. 8-11). The optic nerve is covered by the same three dural layers as the CNS, and the retina is really our “window” into the brain (see the clinical focus box, “Papilledema,” later in this chapter).
In addition to supplying four of the seven skeletal muscles in the orbit (see Table 8-6), the oculomotor nerve (CN III) also provides parasympathetic fibers, which exhibit the following features (see Fig. 8-63):
- They arise centrally from the nucleus of Edinger-Westphal (preganglionic fibers), and course along CN III and its inferior division to synapse in the ciliary ganglion on postganglionic parasympathetic neurons
- Postganglionic fibers then course via short ciliary nerves to the eyeball
- These fibers innervate the sphincter muscle of the pupil (sphincter pupillae) and the ciliary muscle for accommodation
Sympathetic innervation to the eyeball is arranged as follows (see Figs. 8-62 and 8-63):
- It arises from the upper thoracic intermediolateral cell column of the spinal cord (T1-T2) and sends preganglionic fibers into the sympathetic trunk, where they ascend to synapse in the superior cervical ganglion (SCG)
- Postganglionic fibers course along the internal carotid artery, enter the orbit on the ophthalmic artery, and pass through the ciliary ganglion or along the long and short ciliary nerves to the eyeball
- They innervate the dilator muscle of the pupil (dilator pupillae) and the superior tarsal muscle of the upper eyelid
C L I N I C A L F O C U S
Loss of Innervation to Orbital Muscles
If the innervation of an eye muscle is compromised by direct trauma or by a CNS injury, infection, or tumor, the muscle will be weakened or paralyzed. Injury to CN III will result in ophthalmoplegia (inability to move the eye, or abduction and depression of the eye in normal straight gaze) on the affected side, involving four of the extraocular muscles and the levator palpebrae superioris (causing ptosis, or drooping of the upper eyelid). Injury to CN IV will paralyze the superior oblique muscle and the affected eye will be elevated and adducted, whereas injury to CN VI will paralyze the lateral rectus muscle, and the affected eye will be deviated medially (adducted) when in a normal straight gaze. The patient will be unable to abduct the affected eye when asked to look laterally. The patient also will present with diplopia (double vision).
C L I N I C A L F O C U S
Horner’s Syndrome
Horner’s syndrome occurs when there is a lesion somewhere along the pathway of the sympathetic fibers traveling to the head (usually from the sympathetic trunk distally). The cardinal signs are as follows:
- Ptosis: drooping of the upper eyelid on the affected side due to paralysis of the superior tarsal smooth muscle in the free edge of the levator palpebrae superioris muscle
- Miosis: pupillary constriction on the affected side due to the paralysis of the pupillary dilator smooth muscle in the iris
- Anhidrosis: loss of sweating on the affected side of the head due to loss of sweat gland innervation by the sympathetic fibers
- Flushed, warm dry skin: vasodilation of the subcutaneous arteries on the affected side due to a lack of sympathetic vasoconstriction tone and sweat gland innervation
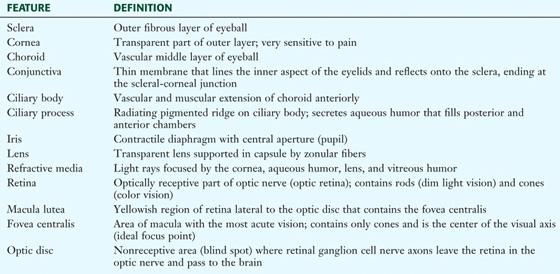
Eyeball (Globe)
The human eyeball measures about 25 mm in diameter, is tethered in the bony orbit by six extraocular muscles that move the globe, and is cushioned by fat that surrounds the posterior two thirds of the globe (Fig. 8-20). Features of the eyeball are summarized in Table 8-7.
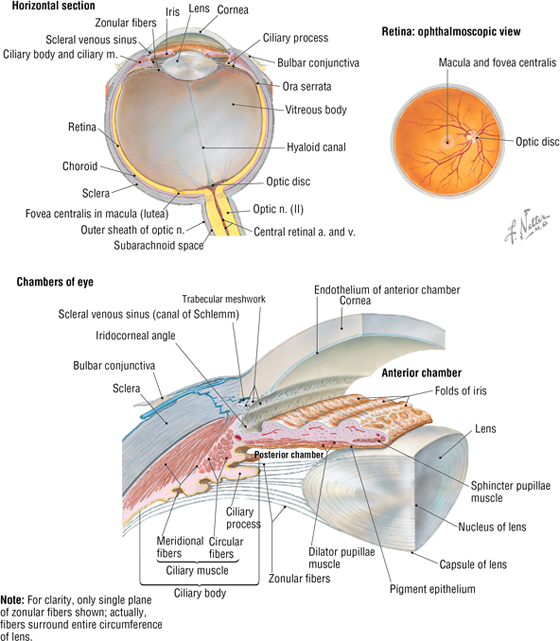
FIGURE 8-20 The Eyeball and Retina
|
TABLE 8-7 Features of the Eyeball
|
 |
The large chamber behind the lens is the vitreous chamber (body) and is filled with a gel-like substance called the vitreous humor, which helps cushion and protect the fragile retina during rapid eye movements (see Fig. 8-20).
The chamber between the cornea and the iris is the anterior chamber, and the space between the iris and lens is the posterior chamber (see Fig. 8-20). Both chambers are filled with aqueous humor, which is produced by the ciliary body and circulates from the posterior chamber, through the pupil, and into the anterior chamber, where it is absorbed by the trabecular meshwork into the scleral venous sinus (canal of Schlemm) at the angle of the cornea and iris.
Accommodation of the Lens
The ciliary body contains smooth muscle arranged in a circular fashion like a sphincter (see Fig. 8-20). When relaxed, it pulls a set of zonular fibers attached to the elastic lens taut and flattens the lens for viewing objects at some distance from the eye. When focusing on near objects, the sphincter-like ciliary muscle (parasympathetically innervated by CN III) contracts and constricts closer to the lens, relaxing the zonular fibers and allowing the elastic lens to round up for accommodation (near vision).
Blood Supply to the Orbit and Eye
The ophthalmic artery arises from the internal carotid artery just as it exits the cavernous sinus, and it supplies the orbit and eye by the following branches (Fig. 8-21):
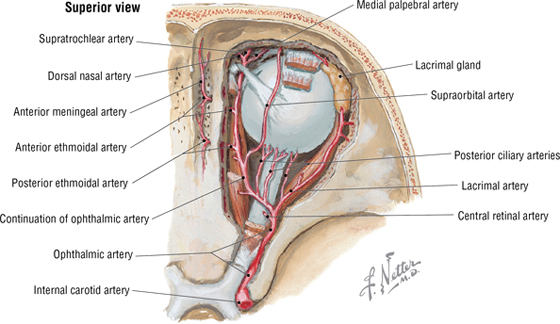
FIGURE 8-21 Branches of the Ophthalmic Artery
- Central artery of the retina: travels in the optic nerve; occlusion leads to blindness
- Short and long posterior ciliary arteries: pierce the sclera and supply the ciliary body, iris, and choroid
- Lacrimal arteries: supply the gland, conjunctiva, and eyelids
- Ethmoidal arteries: supply the ethmoid and frontal sinuses, nasal cavity, and external nose
- Medial palpebrae arteries: supply the eyelids
- Muscular arteries: supply skeletal muscles of the orbit and smooth muscles of the eyeball
- Dorsal nasal arteries: supply the lateral nose and lacrimal sac
- Supraorbital artery: passes through supraorbital notch and supplies the forehead and scalp
- Supratrochlear artery: supplies the forehead and scalp
The venous drainage is by the superior and inferior ophthalmic veins, with connections to the cavernous sinus posteriorly (principal drainage), the pterygoid plexus inferiorly, and the facial vein anteriorly (see Fig. 8-27).
C L I N I C A L F O C U S
Blink Reflex
A wisp of cotton or air on the cornea activates the sensory loop of the corneal blink reflex. Afferent fibers, whose nerve cell bodies reside in the trigeminal ganglion, course centrally in CN V1 (nasociliary nerve) and initiate a bilateral blink response, activating efferent fibers arising in the motor nucleus of CN VII that cause the orbicularis oculi muscle to contract (principally the palpebral portion of that muscle), thus closing the eyelid
C L I N I C A L F O C U S
Pupillary Light Reflex
Bright light stimulation causes a pupillary constriction response that is mediated by CN II afferents (from the retina) responding to the light stimulus and evoking a bilateral efferent response in the nucleus of Edinger-Westphal preganglionic parasympathetic fibers. These fibers synapse in the ciliary ganglion and send postganglionic fibers to the pupillary constrictor muscle of each iris, which constricts the pupils symmetrically and bilaterally, limiting the light’s effect on the retina.
C L I N I C A L F O C U S
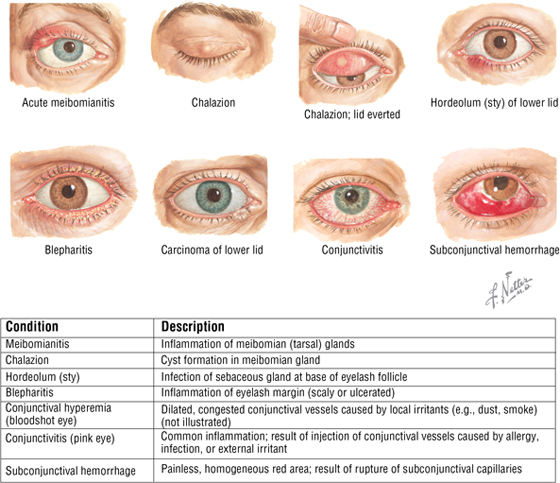
Eyelid Infections and Conjunctival Disorders
C L I N I C A L F O C U S
Papilledema
The optic nerve is a tract of the brain and is therefore surrounded by the three meningeal layers that cover the central nervous system. The subarachnoid space extends along the nerve to the point where it attaches to the posterior aspect of the eyeball. If there is an increase in intracranial pressure, this pressure also compresses the optic nerve and its venous return via the retinal veins. This results in edema of the optic disc (see Fig. 8-20), which can be detected by examining the disc with the ophthalmoscope.
C L I N I C A L F O C U S
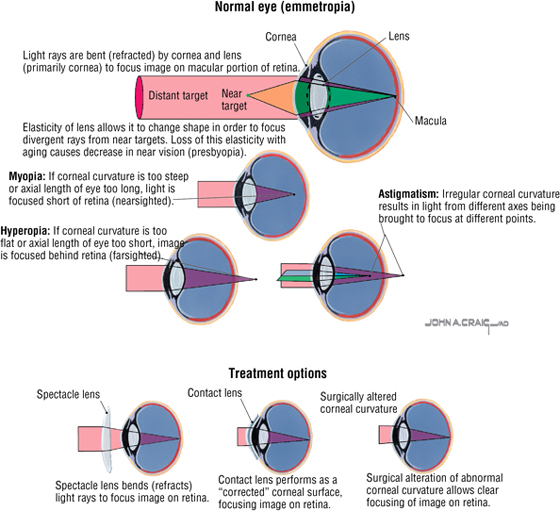
Ocular Refractive Disorders (Ametropias)
Ametropias are the aberrant focusing of light rays on a site other than the optimal site on the retina (macula). Optically, the cornea, lens, and axial length of the eyeball must be in precise balance to achieve sharp focus on the macula. Common disorders include the following:
- Myopia (nearsightedness): 80% of ametropias
- Hyperopia (farsightedness): age-related occurrence
- Astigmatism: nonspherical cornea causes focusing at multiple locations instead of at a single point; affects 25% to 40% of the U.S. population
- Presbyopia: age-related progressive loss of accommodative ability (lens is less flexible)
C L I N I C A L F O C U S
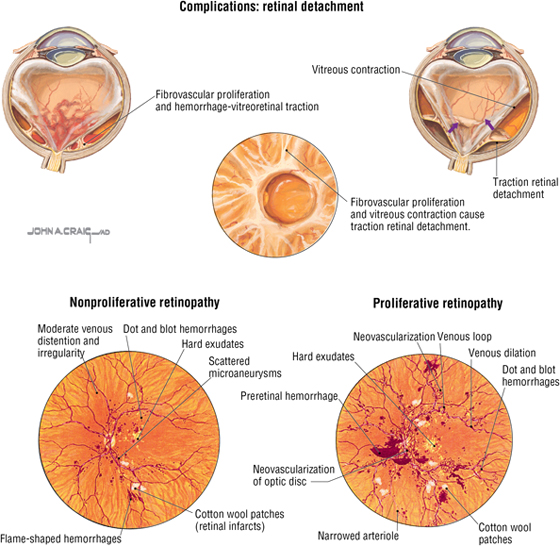
Diabetic Retinopathy
Diabetic retinopathy develops in nearly all patients with type 1 diabetes mellitus (DM) and in 50% to 80% of patients with type 2 DM of 20 years’ duration or more. It can progress rapidly in pregnant women with type 1 DM. Diabetic retinopathy is the number-one cause of blindness in middle-aged individuals and the fourth leading cause of blindness overall in the United States.
C L I N I C A L F O C U S
Glaucoma
Glaucoma is an optic neuropathy that can lead to visual field deficits and is often associated with elevated intraocular pressure (IOP).
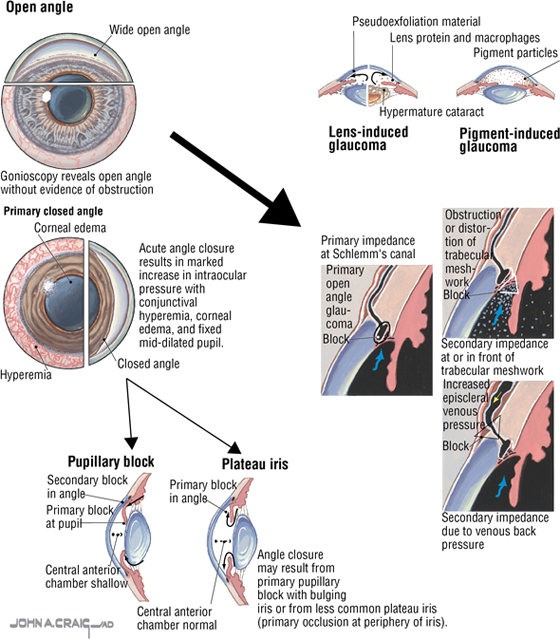
C L I N I C A L F O C U S
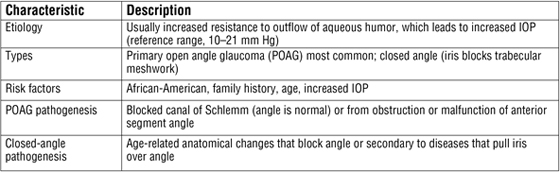
Cataract
A cataract is an opacity, or cloudy area, in the crystalline lens. Risk factors for cataracts include age, smoking, alcohol use, sun exposure, low educational status, diabetes, and systemic steroid use. Treatment is most often surgical, involving lens removal (patient becomes markedly farsighted), with vision corrected with glasses, contact lenses, and/or an implanted plastic lens (intraocular lens).
7. TEMPORAL REGION
This region includes the temporal bone region and infratemporal fossa, and focuses on the muscles of mastication, the mandibular division of the trigeminal nerve (CN V3), and the two terminal branches of the external carotid artery—the maxillary and superficial temporal arteries.
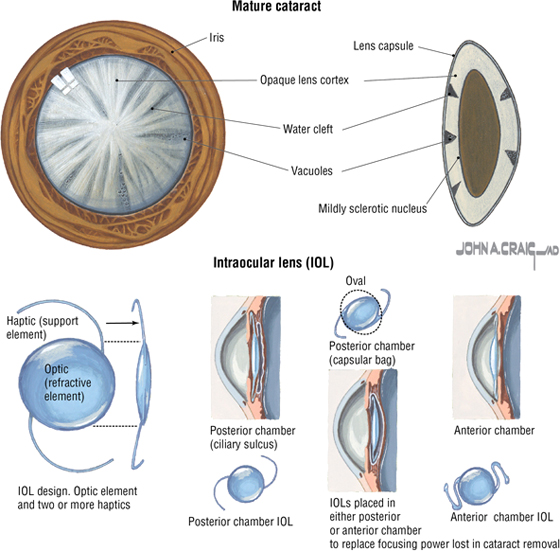
Muscles of Mastication
The muscles of mastication provide a coordinated set of movements that facilitate biting and chewing (the grinding action of the lower jaw). These muscles participate in movements of elevation, retrusion (retraction), and protrusion of the mandible. Embryologically, they are derived from the first branchial arch, and all are innervated by CN V3 (Fig. 8-22 and Table 8-8).
FIGURE 8-22 Muscles of Mastication
|
TABLE 8-8 Summary of the Muscles of Mastication
|
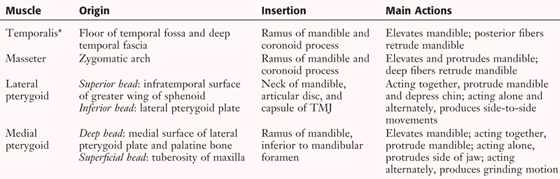 |
*All innervated by CN V3.
The temporomandibular joint (TMJ) is the articulation between the condylar process of the mandible and the squamous portion of the temporal bone (mandibular fossa) (Figs. 8-23 and 8-24 and Table 8-9). The TMJ is a modified hinge-type synovial joint.
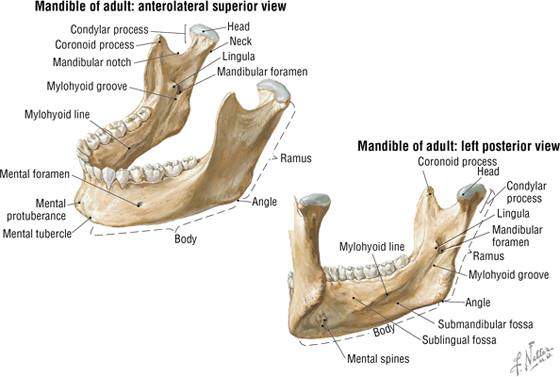
FIGURE 8-23 Mandible
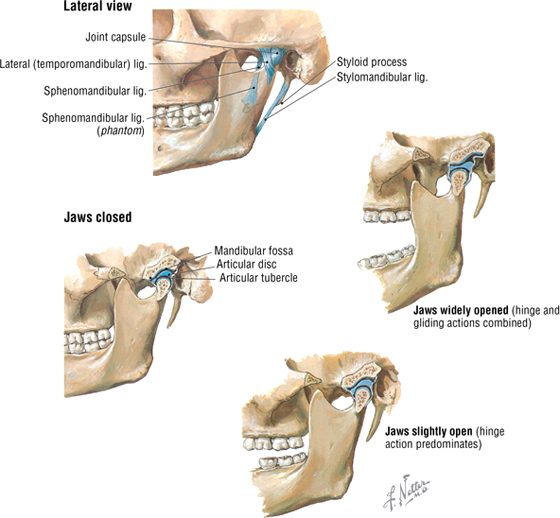
FIGURE 8-24 Temporomandibular Joint
|
TABLE 8-9 Features of the TMJ
|
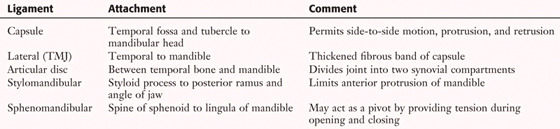 |
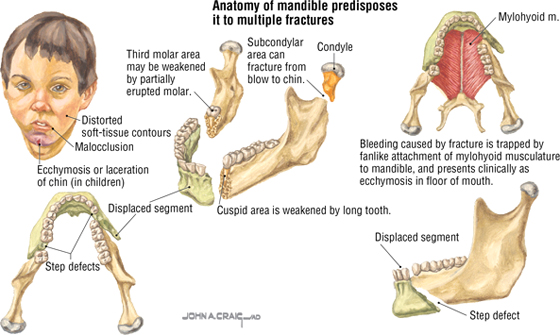
C L I N I C A L F O C U S
Mandibular Dislocation
Because of its vulnerable location, the mandible is the second most commonly fractured facial bone (the nasal bone is first). The mandible’s U shape renders it liable to multiple fractures (more than 50%). The most common sites are the cuspid (canine tooth) area and the third molar area. Oozing blood from the mandible collects in loose tissues of the mouth floor (ecchymosis) and is virtually pathognomonic of a fracture.
C L I N I C A L F O C U S
Mandibular Fractures
TMJ dislocation (subluxation) occurs when the mandibular condyle moves anterior to the articular eminence and the mouth has the appearance of being wide open. The dislocation can be quite painful and can occur from a variety of actions, including a large yawn. Once the ligaments are stretched, subsequent dislocations may occur more frequently.
Parotid Gland
The parotid gland is the largest of the three pairs of salivary glands and occupies the retromandibular space between the mandibular ramus and mastoid process (see Figs. 8-13, 8-15, and 8-66). It is encased within the parotid sheath, a tough extension of the deep cervical fascia. The parotid gland is innervated by secretomotor parasympathetic fibers from the glossopharyngeal nerve (CN IX), which we will review in the next section (see Fig. 8-66).
Infratemporal Fossa
The infratemporal fossa is the space inferior to the zygomatic arch, medial to the mandibular ramus and posterior to the maxilla. CN V3 (the largest division of CN V) exits the foramen ovale, and its branches in this region include the following (Fig. 8-25):
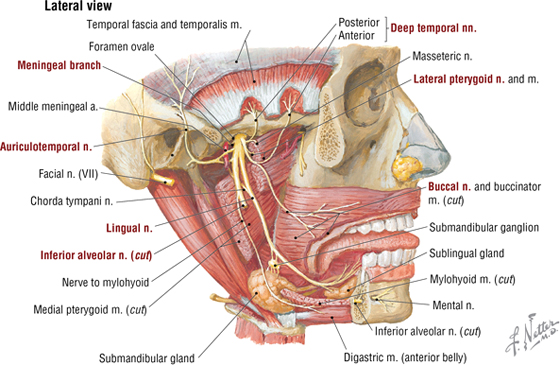
FIGURE 8-25 Infratemporal Fossa and the Mandibular Nerve (CN V3)
- Muscular: small motor nerves to the four muscles of mastication, and to the tensor veli palatini, mylohyoid, anterior belly of the digastric, and tensor tympani (in middle ear); embryologically, derived from the first branchial arch
- Meningeal: accompanies the middle meningeal artery through the foramen spinosum; sensory to the dura
- Auriculotemporal: conveys CN IX parasympathetics from otic ganglion to the parotid gland; sensory to the auricle and temple
- Buccal: sensory to the cheek
- Lingual: conveys CN VII parasympathetics of chorda tympani to the submandibular ganglion and taste fibers from the tongue to the geniculate ganglion of CN VII; sensory to the tongue
- Inferior alveolar: sensory to mandibular teeth, gums, and chin via the mylohyoid branch from the inferior alveolar
Parasympathetic preganglionic fibers from the glossopharyngeal nerve (CN IX) (inferior salivatory nucleus) run through the middle ear tympanic plexus and lesser petrosal nerve to synapse in the otic ganglion, which is located on the medial aspect of CN V3 as it exits the foramen ovale (see Figs. 8-64 and 8-66). Secretomotor postganglionic fibers join the auriculotemporal nerve and travel to the parotid gland, which they innervate.
Additionally, parasympathetic preganglionic fibers from CN VII (superior salivatory nucleus) pass through the middle ear and exit through a small fissure (petrotympanic) in the temporal bone as the chorda tympani nerve to join the lingual branch of CN V3 and pass to the submandibular ganglion, where they synapse (see Fig. 8-65). Secretomotor postganglionic fibers then innervate the submandibular and sublingual salivary glands.
Vascular Supply
The external carotid artery terminates as the superficial temporal and maxillary arteries (see Fig. 8-15). The temporal artery supplies the scalp and upper face (via its transverse facial branch), while the maxillary artery supplies the infratemporal region, nasal cavities, palate, and maxillary teeth (Fig. 8-26). It is divided for descriptive purposes into the following three parts:
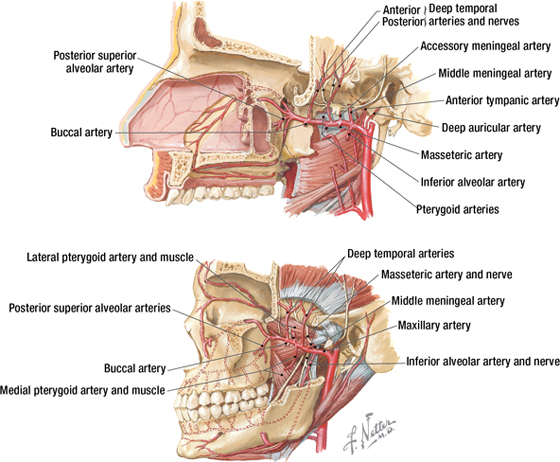
FIGURE 8-26 Branches of the Maxillary Artery
- Retromandibular: arteries enter foramina and supply dura, mandibular teeth and gums, ear, and chin
- Pterygoid: branches supply muscles of mastication and buccinator
- Pterygopalatine: branches enter foramina and supply maxillary teeth and gums, orbital floor, nose, paranasal sinuses, palate, auditory tube, and superior pharynx
Major branches of the maxillary artery include the inferior alveolar and middle meningeal branches (from the first part) to the muscles of mastication (from the second part), and the superior alveolar, infraorbital, greater palatine, and sphenopalatine branches (from the third part) (see Fig. 8-26).
The infratemporal fossa is largely drained by veins of the pterygoid plexus (Fig. 8-27), which have extensive anastomoses with dural, ophthalmic, and facial veins.
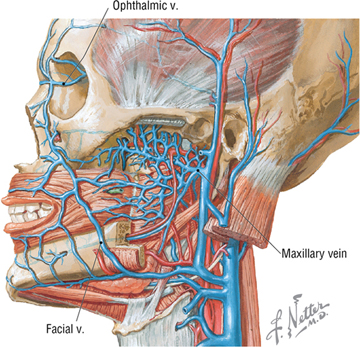
FIGURE 8-27 Pterygoid Plexus of Veins
8. PARANASAL SINUSES AND NASAL CAVITY
Paranasal Sinuses
The four paired paranasal sinuses are the frontal, ethmoid, maxillary, and sphenoid sinuses. They are named for the bones in which they reside (Fig. 8-28), and they surround the nose and orbits. These sinuses are lined with respiratory epithelium (pseudostratified columnar with cilia), lighten the weight of the facial skeleton, assist in warming and humidifying inspired air, add resonance to the voice, and drain mucus secretions into the nasal cavities. Sneezing and blowing the nose, as well as gravity, help to drain the paranasal sinuses of mucus.
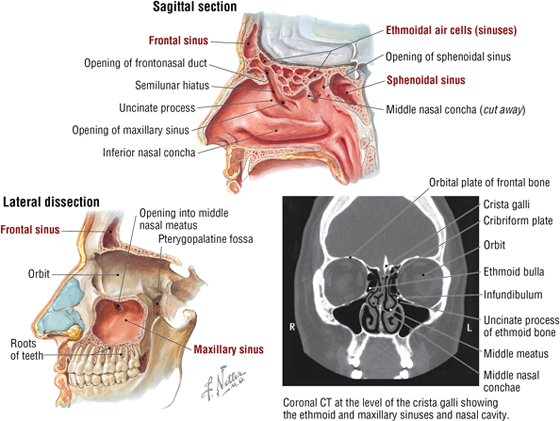
FIGURE 8-28 Paranasal Sinuses. (CT reprinted with permission from Kelley LL, Petersen C: Sectional Anatomy for Imaging Professionals. Philadelphia, Mosby, 2007.)
C L I N I C A L F O C U S
Lingual Nerve Trauma
Injury to the lingual nerve proximal to the point where the chorda tympanic joins it will result in loss of sensation from the anterior two-thirds of the tongue, the gums, and the lingual aspect of the mandibular oral mucosa and lower lip. The cheek mucosa is innervated by the buccal nerve, V3 (see Fig. 8-25). If the injury is distal to the point of union of the chorda tympani, then additional deficits will include loss of salivation from the submandibular and sublingual salivary glands and loss of taste from the anterior two-thirds of the tongue.
The innervation, blood supply, and drainage of the paranasal sinuses include the following (see Figs. 8-26, 8-27, 8-32, and 8-33):
- Frontal: sensory fibers from V1 (supraorbital); anterior ethmoidal arteries (from ophthalmic); drains via the frontonasal duct into the semilunaris hiatus (middle meatus)
- Ethmoid: sensory fibers from V1 (nasociliary nerve’s ethmoidal branches) and V2 (orbital branches); blood from ethmoidal arteries (from ophthalmic); anterior ethmoid drains into semilunaris hiatus (middle meatus), middle drains into the ethmoid bulla (middle meatus), and posterior drains into superior meatus
- Sphenoid: sensory fibers from V2 (orbital branches); pharyngeal arteries (from maxillary); drains into sphenoethmoidal recess above superior concha
- Maxillary: sensory fibers from V2 (infraorbital and alveolar branches); infraorbital and alveolar arteries (from maxillary); drains into semilunar hiatus (middle meatus)
Note also that the nasolacrimal duct drains tears into the inferior meatus. Thus, your nose “runs” when you cry!
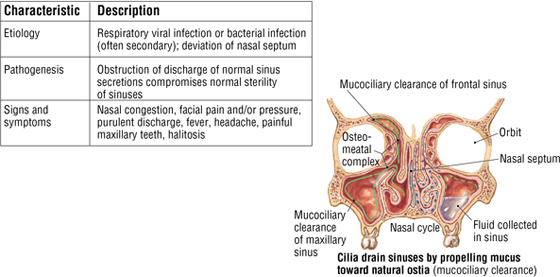
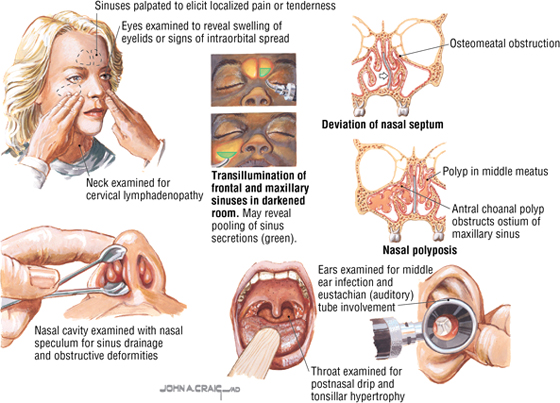
C L I N I C A L F O C U S
Rhinosinusitis
Rhinosinusitis is an inflammation of the paranasal sinuses (usually the ethmoid and maxillary sinuses) and the nasal cavity. Physical examination of the paranasal sinuses is usually sufficient to make the diagnosis, although a CT of the sinus may help in difficult cases.
Nasal Cavities
Air entering the nose passes through the following areas (Fig. 8-29):
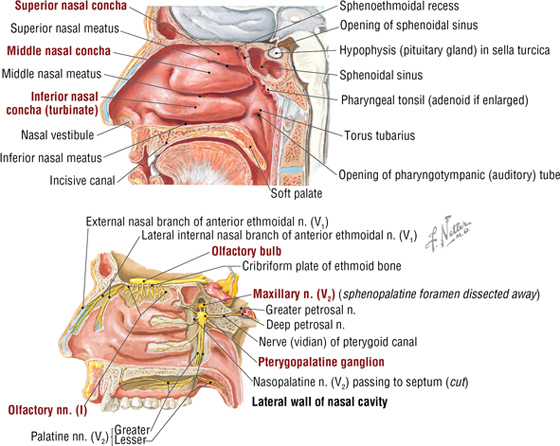
FIGURE 8-29 Lateral Wall of the Nasal Cavity
- Nares: anterior apertures or nostrils
- Vestibule: dilated portion of the nose inside each aperture; highly vascular epithelium with hair
- Respiratory region: nasal cavity proper, lined with highly vascular respiratory epithelium and three conchae, which increase the surface area for filtering, warming, and humidifying inspired air
- Olfactory region: small, apical region of nasal cavity where the olfactory receptors reside
- Choanae: posterior apertures where the nasal cavity communicates with the nasopharynx
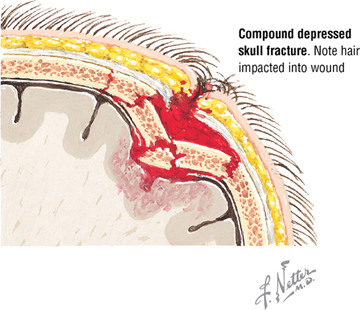
Bones of the nasal cavity include the following (Fig. 8-30):
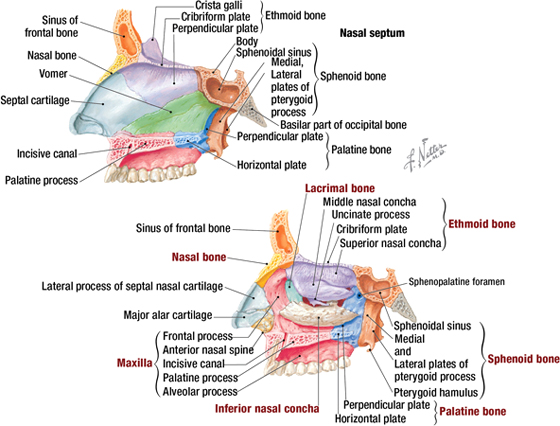
FIGURE 8-30 Bones Forming the Nasal Cavity
- Ethmoid: unpaired bone that contains the ethmoid air cells (sinuses) and contributes to the roof and the lateral and medial walls of the nasal cavity
- Sphenoid: unpaired bone that contains sphenoid sinus and forms the posterior part of the cavity
- Frontal: unpaired bone that contains frontal sinus, and forms part of the roof and septum of the cavity
- Vomer: unpaired bone that contributes to the septum
- Nasal: paired bones that form part of the anterior roof and lateral wall
- Maxillary: paired bones that form the floor, septum, and lateral walls of the cavity
- Palatine: paired bones that form the floor, septum, and lateral walls of the cavity
- Lacrimal: bone that forms part of the lateral wall of the nasal cavity
- Inferior nasal concha: paired bones that form part of the lateral wall
Most of the external nose is cartilaginous and is composed of the lateral processes of the septal cartilage, the septal cartilage, and the major and minor alar cartilages (Fig. 8-31):
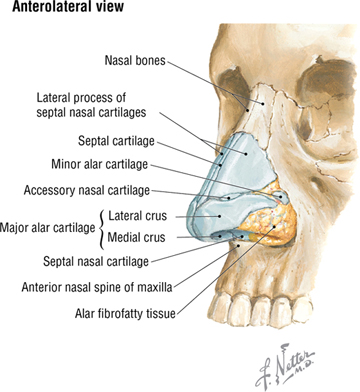
FIGURE 8-31 Structure of the External Nose
Blood Supply and Innervation
Blood supply to the nasal cavities originates from the following major arteries (Fig. 8-32):
- Ophthalmic: anterior and posterior ethmoidal arteries
- Maxillary: sphenopalatine (terminal branch of the maxillary) and greater palatine arteries
- Facial: lateral nasal and septal branches
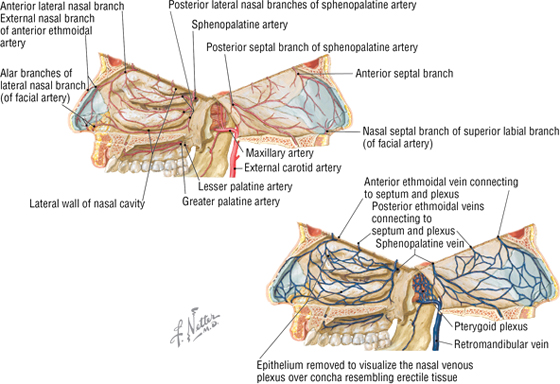
FIGURE 8-32 Arterial Supply and Venous Drainage of the Nasal Cavity (septum hinged open)
C L I N I C A L F O C U S
Nosebleed
A nosebleed, or epistaxis, is a common occurrence and often involves the richly vascularized region of the vestibule and the anteroinferior aspect of the nasal septum (Kiesselbach's area). Commonly, nosebleeds occur because of trauma involving the septal branch of the superior labial artery from the facial artery.
Corresponding veins drain the floor, lateral walls, and nasal septum, with most of the venous return passing into the pterygoid plexus of veins (see Fig. 8-32):
The innervation of the nasal cavity includes the following (Fig. 8-33):
- Olfactory: CN I olfactory receptors (special sense of smell) in the olfactory epithelium convey axons that synapse in the olfactory bulbs, which are actually brain tracts surrounded by the three meningeal layers, not unlike CN II
- Ophthalmic: CN V1 general afferents conveyed by the anterior and posterior ethmoidal nerves of the nasociliary nerve
- Maxillary: CN V2 general afferents conveyed to the trigeminal (sensory) ganglion via small nasal branches and the nasopalatine nerve on the septum
- Sympathetics: largely postganglionic vasomotor fibers from the SCG that reach the nose by traveling on blood vessels and existing nerves (mostly V2)
- Parasympathetics: secretomotor fibers to the mucosal glands of the nose and paranasal sinuses from CN VII via the greater petrosal nerve and the nerve of the pterygoid canal; synapse in the pterygopalatine ganglion; postganglionics distribute on existing nerves
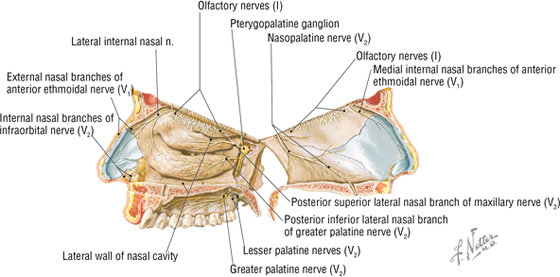
FIGURE 8-33 Nerve Supply of the Nose (septum hinged open)
9. EAR
The human ear consists of the following three parts (Fig. 8-34):
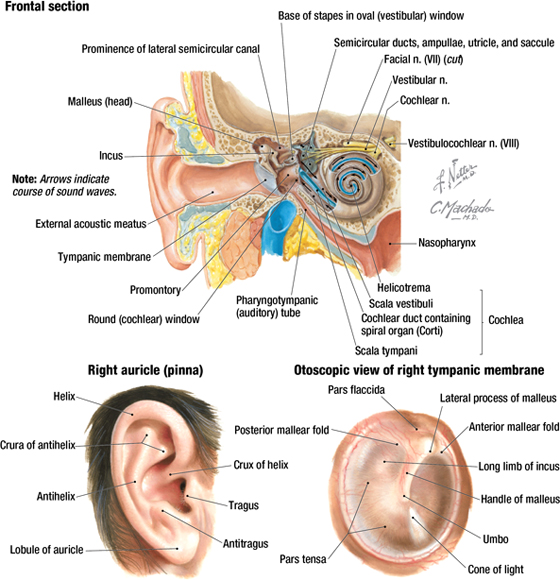
FIGURE 8-34 General Anatomy of the Right Ear
- External: the auricle (pinna), external acoustic meatus, and tympanic membrane (eardrum)
- Middle: the tympanic cavity between the eardrum and labyrinthine wall, which contains the three middle ear ossicles (malleus, incus, and stapes) and the stapedius and tensor tympani muscles; communicates posteriorly with the mastoid antrum and anteriorly with the auditory (eustachian) tube
- Internal (inner): acoustic apparatus (cochlea) and vestibular apparatus (vestibule with the utricle and saccule, and semicircular canals)
External Ear
The auricle is composed of skin and elastic cartilage and helps funnel sound waves into the external acoustic meatus. It is innervated by auricular branches from CN V3, VII, and X, and by the lesser occipital nerve. The external acoustic meatus is about 2.5 cm long and is composed of cartilage (lateral third) and bone. Its lining of skin contains hairs and modified sweat glands (ceruminous glands) that secrete an earwax that protects the skin. It is innervated mostly by CN V3 and X (minor contributions from CN VII and IX). The tympanic membrane lies at an oblique angle (see Fig. 8-34), sloping medially from posterosuperiorly to anteroinferiorly, and is attached on its medial side to the handle of the malleus, which creates a depression in its middle called the umbo. Because of its oblique position and the umbo, the tympanic membrane gives off a reflection of light when viewed with an otoscope (the cone of light). Its external surface is innervated by CN V3, VII, and X, and its internal surface is innervated by CN IX.
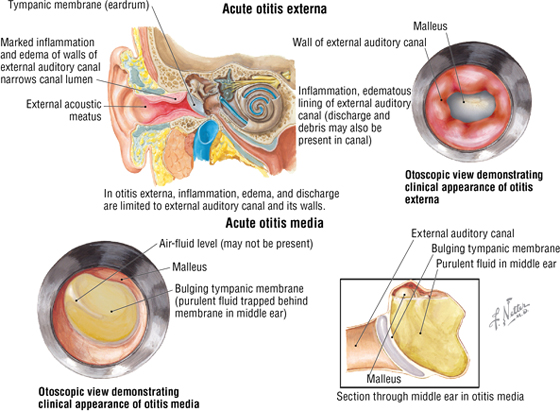
C L I N I C A L F O C U S
Acute Otitis Externa and Media
Acute otitis externa (swimmer's ear) involves inflammation or bacterial infection of the external acoustic meatus, usually because the protective earwax has been washed from the ear. Otitis media is an inflammation of the middle ear and is common in children younger than 15 years because the auditory tube is short and relatively horizontal at this age, which limits drainage by gravity and provides a route for infection from the nasopharynx. When viewed with an otoscope, the normal translucent appearance of the tympanic membrane is gone, the eardrum is erythematous and bulging, and the cone of light is absent.
Middle Ear
The middle ear cavity is like a box with six sides, and is air filled and lined with a mucous membrane. Its boundaries include the following (Fig 8-35):
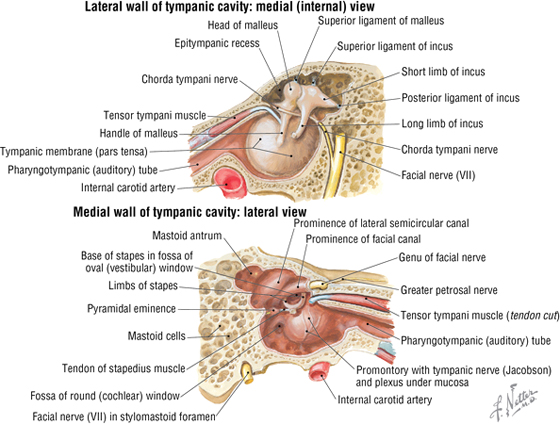
FIGURE 8-35 Walls of the Right Middle Ear
- Roof: tegmen tympani, a layer of bone that is part of the petrous portion of the temporal bone
- Floor: jugular fossa, a thin layer of bone separating the middle ear from the internal jugular vein
- Posterior wall: an incomplete wall with a small aperture (aditus ad antrum) leading to the mastoid air cells
- Anterior wall: an incomplete wall with a thin bony lower portion separating the cavity from the internal carotid artery (in the carotid canal), and superiorly an opening for the auditory (pharyngotympanic; eustachian) tube and tensor tympani muscle
- Lateral wall: the tympanic membrane and epitympanic recess above the eardrum (also note the chorda tympani branch of CN VII passing through the cavity)
- Medial wall: the labyrinthine wall exhibiting superiorly a prominence of the lateral semicircular canal and a second one for the CN VII; the oval (fenestra vestibuli) window for the base of the stapes; a promontory (basal turn of the cochlea), with the tympanic nerve plexus (CN IX) on its surface; and, most inferiorly, the round (fenestra cochlea) window covered with a membrane
Vibrations of the eardrum cause the three middle ear ossicles to vibrate, which causes the base of the stapes to vibrate against the oval window and thus initiates a wave action within the fluid-filled scala vestibuli (filled with perilymph) and scala tympani of the cochlea (described in the next section). The stapedius (smallest skeletal muscle in the body) and tensor tympani muscles dampen excessive vibrations in the stapes (stapedius) and eardrum (tensor) in response to loud noises.
Internal Ear
The internal ear houses the special senses of hearing and balance. The internal ear is composed of the following two elements (Fig. 8-36):
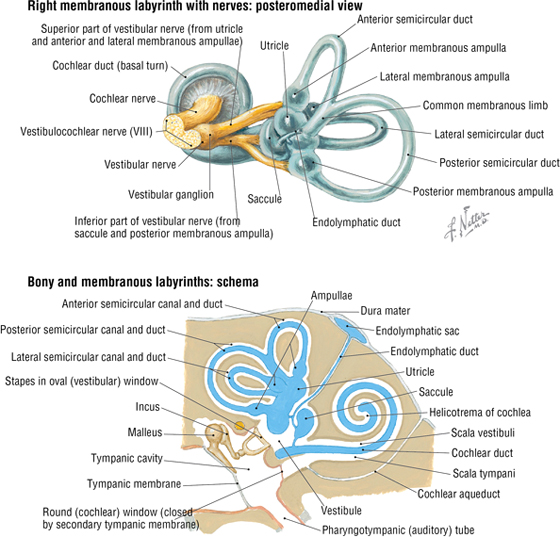
FIGURE 8-36 Structures of the Right Internal Ear
- Bony labyrinth: includes the vestibule, the three semicircular canals, and the cochlea, which are all housed within the temporal bone and filled with perilymph
- Membranous labyrinth: is suspended within the perilymph of the bony labyrinth and is filled with endolymph; consists of the cochlear duct (the organ of hearing) and the utricle, saccule, and semicircular ducts (the organs of balance)
Vibrations of the middle ear ossicles and the base plate of the stapes on the oval window initiate a wave action within the perilymph-filled scala vestibuli and scala tympani of the cochlea (see Fig. 8-34, top image). This wave action causes the deflection and depolarization of tiny hair cells within the organ of Corti (membranous labyrinth). This stimulates action potentials in the afferent axons of the spiral ganglion cells that are conveyed centrally to the brain, with final processing occurring in the auditory cortex of the temporal lobe.
A similar mechanism of depolarization also occurs in the endolymph of the vestibular system (hair cells and a single kinocilium), where the receptors for equilibrium involve the following two functional components:
- Static: a special receptor called the macula resides in each utricle and saccule; concerned with positioning of the head and linear acceleration, as well as gravity and low-frequency vibrations (saccule only)
- Dynamic: special receptors called the crista ampullaris reside in the ampulla of each semicircular canal (anterior, lateral, and posterior canals) and are concerned with angular (rotational) movements of the head
Vestibular afferents passing back to the CNS provide input to help modulate and coordinate muscle movement, tone, and posture, as well as regulate head and neck movements and coordinate eye movements.
C L I N I C A L F O C U S
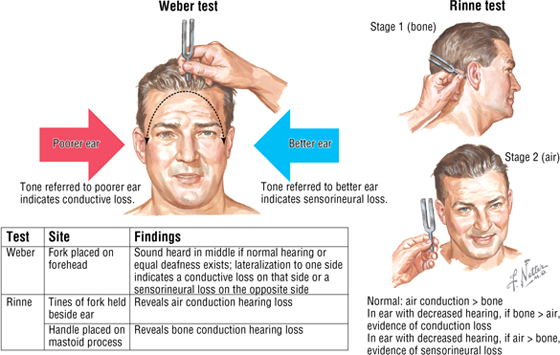
Weber and Rinne Tests
Sensorineural hearing loss suggests a disorder of the internal ear or the cochlear division of CN VIII. Conductive hearing loss suggests a disorder of the external or middle ear (eardrum, ear ossicles, or both). The Weber and Rinne tests offer an easy way to differentiate between sensorineural and conductive hearing loss.
C L I N I C A L F O C U S
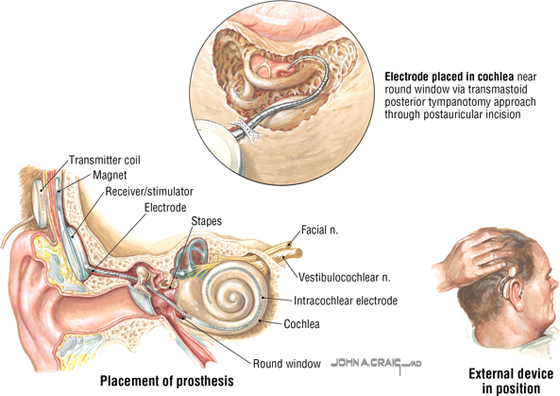
Cochlear Implant
Approximately two million Americans have profound bilateral deafness. One option available to them is a cochlear implant, which consists of a speech processor and implanted electrodes. An external microphone detects sound, which is converted by the processor into electrical signals transmitted to the cochlear implant and vestibulocochlear nerve.
C L I N I C A L F O C U S
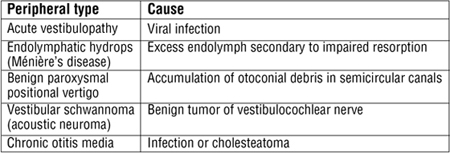
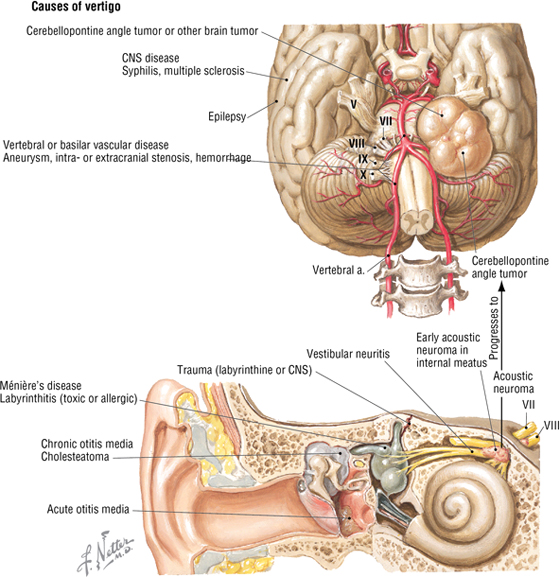
Vertigo
A condition involving the peripheral vestibular system or its CNS connections and characterized by the illusion or perception of motion is called vertigo. Central types of vertigo may be caused by multiple sclerosis, migraine, vascular disease (associated with the vestibulobasilar region), or brainstem tumors (especially at the cerebellopontine angle).
C L I N I C A L F O C U S
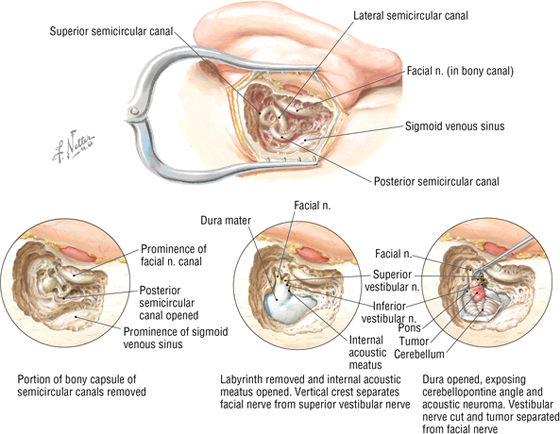
Removal of an Acoustic Neuroma
The translabyrinthine approach to acoustic neuroma removal takes advantage of the anatomy of CN VIII. The tumor often is encapsulated within the vestibular division of CN VIII in the internal acoustic meatus. The approach is via the mastoid air cells, with removal of the semicircular canals and resection of the tumor. Early treatment can spare the cochlear division of CN VIII, and thus hearing, and also spare the facial nerve from involvement.
10. ORAL CAVITY
The mouth consists of an oral vestibule, which is the space between the teeth and lips or cheeks, and the oral cavity proper internal to the teeth and gums. Features of the oral cavity proper include the palate (hard and soft), teeth, gums (gingivae), tongue, and salivary glands (see Fig. 8-40 and 8-41). The mucosa of the hard palate, cheeks, tongue, and lips contain numerous minor salivary glands that secrete directly into the oral cavity. Paired collections of lymphoid tissue called the palatine tonsils lie between the palatoglossal and palatopharyngeal folds (contain small skeletal muscles of the same name) and “guard” the entrance into the oropharynx.
Muscles
The tongue is a strong muscular organ (gram for gram, one of the strongest muscles in the body) consisting of intrinsic skeletal muscle arranged in four different planes (all innervated by the hypoglossal nerve, CN XII):
- Superior longitudinal
- Inferior longitudinal
- Transverse
- Vertical
Additionally, three extrinsic skeletal muscles originate outside the tongue and insert into it (Fig. 8-37 and Table 8-10).
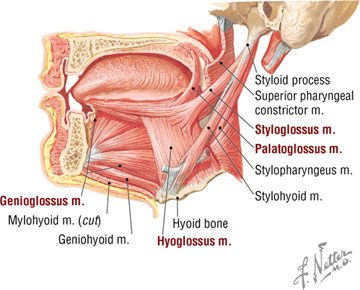
FIGURE 8-37 Tongue and Its Extrinsic Muscles
|
TABLE 8-10 Extrinsic Tongue Muscles
|
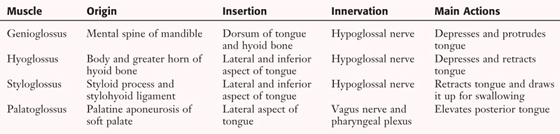 |
The surface of the tongue is characterized by small lingual papillae, divided into four types (Fig. 8-38).
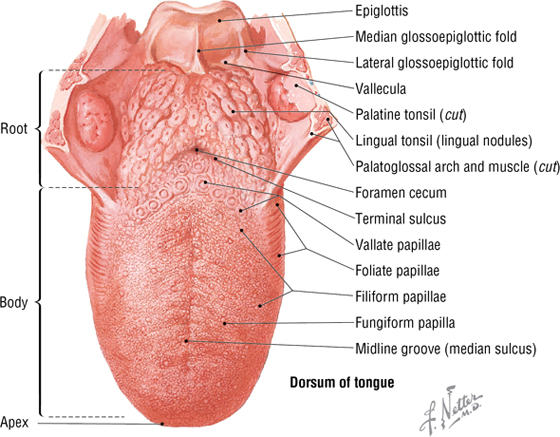
FIGURE 8-38 Dorsum of the Tongue
- Filiform: numerous slender projections that lack taste buds; give the tongue its rough feel
- Fungiform: larger mushroom-shaped papillae (may appear as red caps) scattered on the dorsum of the tongue's surface; possess taste buds
- Circumvallate: larger papillae that lie in a row just anterior to the sulcus terminalis; possess taste buds
- Foliate: lie along the sides of the tongue and are rudimentary in humans; possess taste buds
The tongue receives its blood supply largely by the lingual artery (from the external carotid artery) and is innervated by the following five cranial nerves (Fig. 8-39):
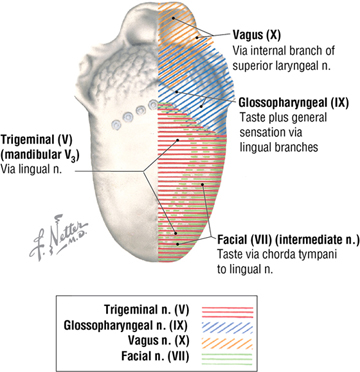
FIGURE 8-39 Sensory Innervation of the Tongue
- Mandibular: via lingual nerve; for general sensation to the anterior two-thirds of the tongue
- Facial: via chorda tympani nerve, which joins the lingual; for taste on the anterior two-thirds of the tongue
- Glossopharyngeal: general sensation and taste to the posterior one-third of the tongue
- Vagus: via the internal branch of the superior laryngeal nerve, for general sensation and taste on the base of the tongue at the epiglottic region
- Hypoglossal: motor to the intrinsic and extrinsic tongue muscles
Salivary Glands
Whereas there are thousands of microscopic minor salivary glands in the oral and lingual mucosa, there also are three pairs of larger salivary glands (Fig. 8-40 and Table 8-11).
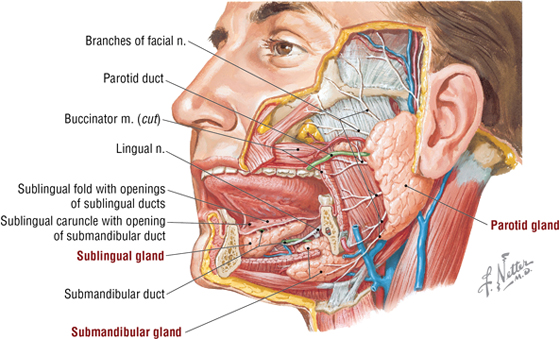
FIGURE 8-40 Major Salivary Glands
|
TABLE 8-11 Major Salivary Glands
|
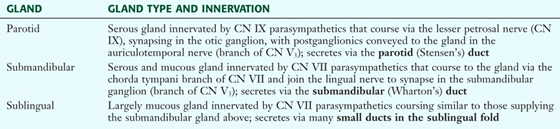 |
Palate
The palate forms the floor of the nasal cavity and the roof of the oral cavity. The palate is divided as follows (Figs. 8-41 and 8-42):
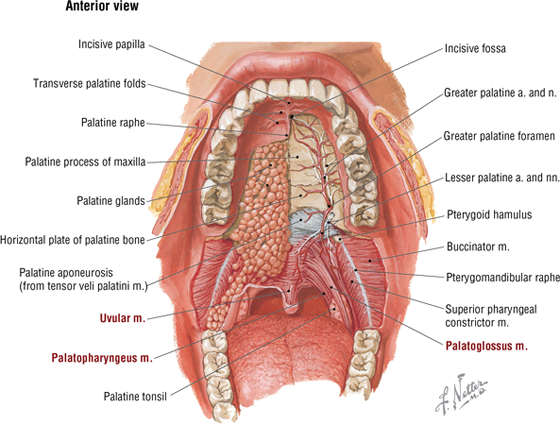
FIGURE 8-41 Oral Cavity with Partial Dissection of the Palate
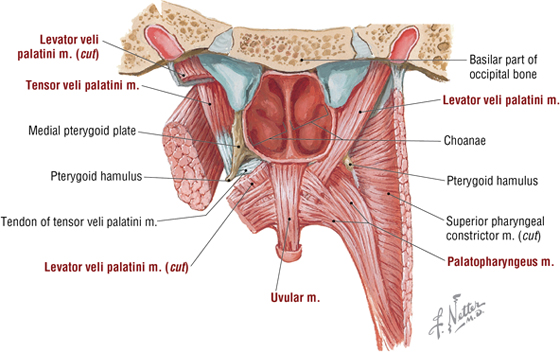
FIGURE 8-42 Posterior View of the Soft Palate Muscles
- Hard palate: bony anterior two-thirds of the palate; formed by the palatal process of the maxilla and horizontal process of the palatine bone; covered by a thick mucosa that overlies numerous mucus-secreting palatal glands
- Soft palate: posterior third of the palate; composed of a mucosa and mucus-secreting palatal glands with five muscles that contribute to the soft palate and its movements; closes off the nasopharynx during swallowing
Sensory innervation of the hard palate is via the nasopalatine and greater palatine nerves (CN V2), whereas sensory innervation of the soft palate is via the lesser palatine nerves (CN V2) (see Fig. 8-41).
The muscles of the soft palate are summarized in Figures 8-41 and 8-42, and Table 8-12.
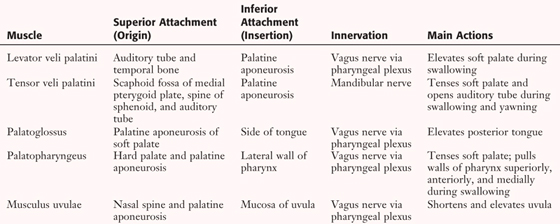
|
TABLE 8-12 Muscles of the Soft Palate
|
 |
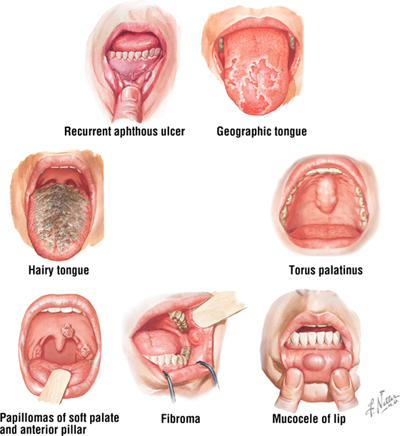
C L I N I C A L F O C U S
Common Oral Lesions
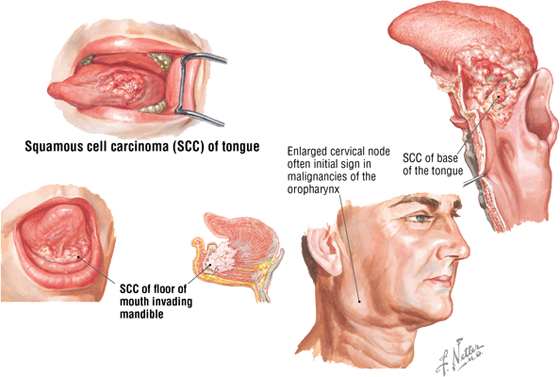
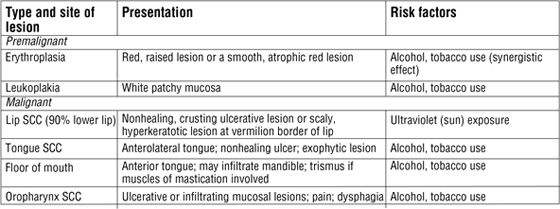
C L I N I C A L F O C U S
Cancer of the Oral Cavity
Squamous cell carcinoma (SCC) accounts for more than 90% of cancers in this region, so the information here focuses on SCC. All of these lesions may present with palpable submental, submandibular, and upper cervical lymph nodes.
C L I N I C A L F O C U S
Nerve Lesions
A lesion of the vagus nerve is easily detected by asking the patient to say “ahh.” If the nerve is intact, the soft palate and uvula will elevate symmetrically. If the vagus is lesioned on one side, the elevation will be asymmetrical, with the palate and uvula deviating away from the lesioned side.
Lesion of the hypoglossal nerve peripherally (lower motor neuron) will cause the tongue to deviate toward the side of the lesioned nerve when the patient is asked to stick out the tongue. The ipsilateral tongue will also show evidence of muscle atrophy.
11. NECK
The neck is divided descriptively into two major triangles. Each triangle contains key structures used as landmarks by anatomists and physicians operating in this area. The neck is a vertical conduit for structures entering or leaving the head. It is tightly bound in several fascial layers that divide the neck into descriptive compartments.
The two major triangles of the neck include the following (Fig. 8-43):
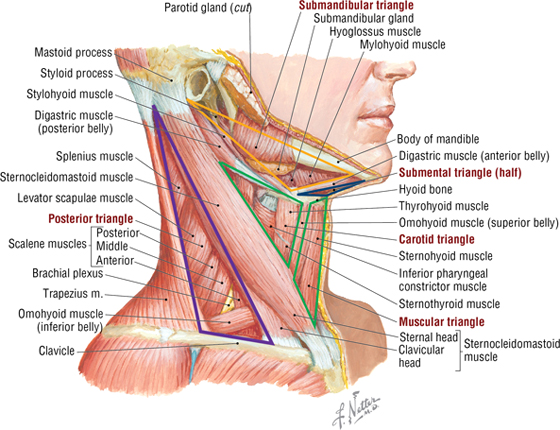
FIGURE 8-43 Triangles of the Neck
- Posterior: bounded by the posterior border of the sternocleidomastoid muscle (SCM), anterior border of the trapezius, and middle third of the clavicle
- Anterior: bounded by the anterior border of the SCM, inferior border of the mandible, and the midline of the neck; also subdivided into the following triangles:
- Submandibular
- Carotid
- Muscular
- Submental
The neck is surrounded by a superficial cervical fascia that lies deep to the skin and invests the platysma muscle (a muscle of facial expression). A second deep cervical fascia tightly invests the neck structures and is divided into the following three layers (Fig. 8-44):
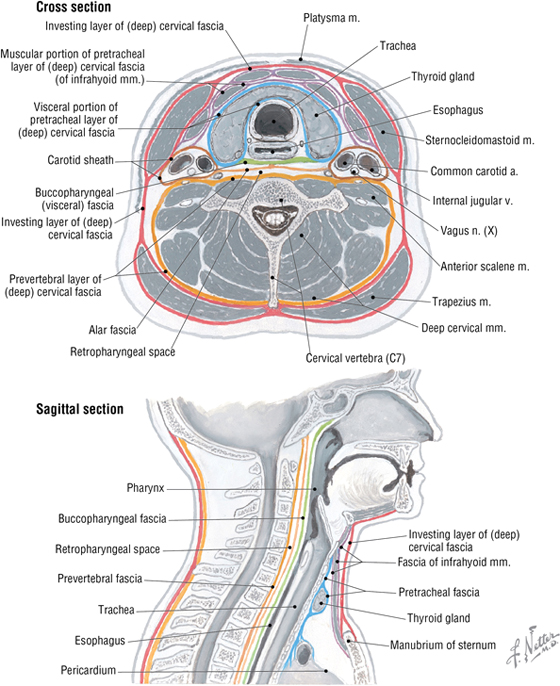
FIGURE 8-44 Cervical Fascial Layers and Spa
- Investing: surrounds the neck and invests the trapezius and SCM muscles
- Pretracheal (visceral): limited to the anterior neck; invests the infrahyoid muscles, thyroid gland, trachea, and esophagus; posteriorly called the buccopharyngeal fascia, as it covers the buccinator and pharyngeal constrictor muscles
- Prevertebral: tubular sheath that invests the prevertebral muscles and vertebral column; includes the alar fascia anteriorly
The carotid sheath blends with these three fascial layers but is distinct and contains the common carotid artery, internal jugular vein, and vagus nerve (see Fig. 8-44).
Muscles
The muscles of the anterior and posterior triangles are summarized in Figure 8-45 and Table 8-13).
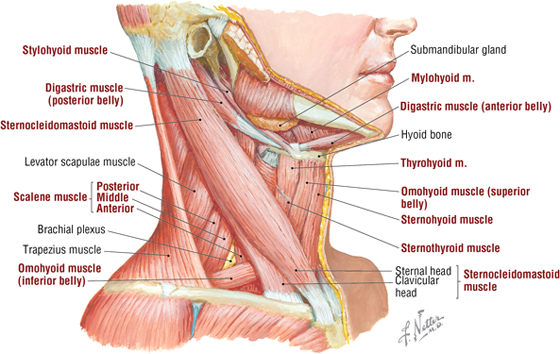
FIGURE 8-45 Muscles of the Neck
|
TABLE 8-13 Muscles of the Neck
|
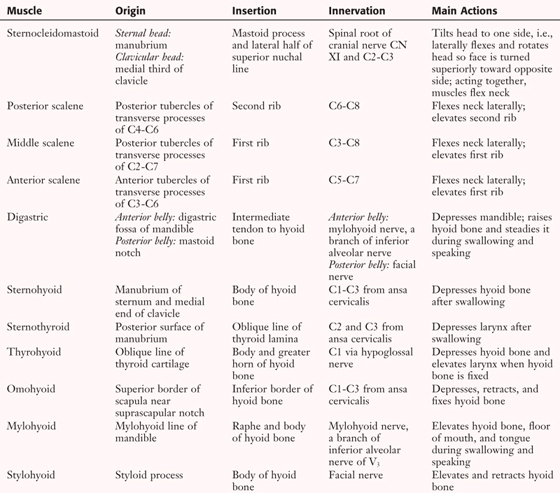 |
Cervical Plexus
The spinal accessory nerve (CN XI) exits the jugular foramen and crosses the posterior triangle, innervating the SCM and trapezius muscles (Fig. 8-46). However, the cervical plexus, composed of the ventral primary rami of C1-C4, innervates most of the neck muscles and provides sensory innervation to the anterior and lateral neck (see Fig. 8-46 and Table 8-14).
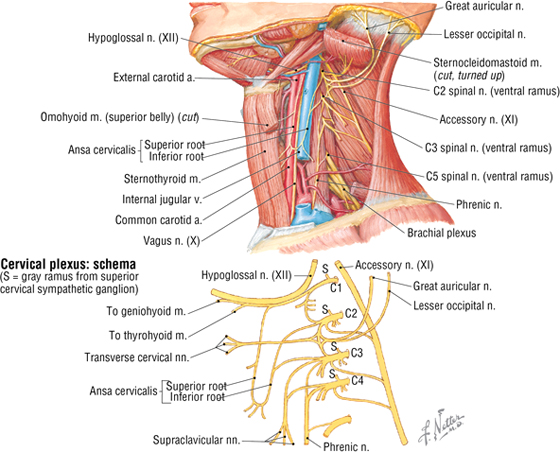
FIGURE 8-46 Cervical Plexus
|
TABLE 8-14 Cervical Plexus
|
 |
C L I N I C A L F O C U S
Fascial Planes
The neck is divided into relatively tight compartments by the fascial planes previously described. Infections may occur in these compartments and tend to spread within the planes limited by these fascial sleeves. Moreover, if significant edema occurs, it may compress some of the structures found within each of the fascial compartments (see Fig. 8-44).
C L I N I C A L F O C U S
Retropharyngeal Space
This space lies between the buccopharyngeal fascia (posterior portion of the pretracheal fascia) and the anterior aspect of the prevertebral fascia, and extends from the base of the skull into the proximal posterior mediastinum (see Fig. 8-44). Infections anywhere in this space may gain access to the thoracic cavity via the posterior mediastinum.
Blood Supply
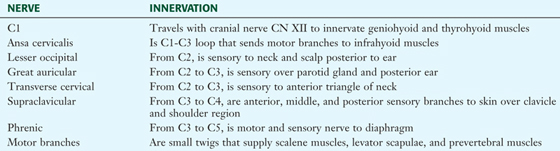
The arterial supply to the neck is by the subclavian artery (Fig. 8-47 and Table 8-15) and some of the branches of the external carotid artery (Fig. 8-48 and Table 8-16). The subclavian artery is divided for descriptive purposes into three parts: part 1 lies medial, part 2 lies posterior, and part 3 lies lateral to the anterior scalene muscle.
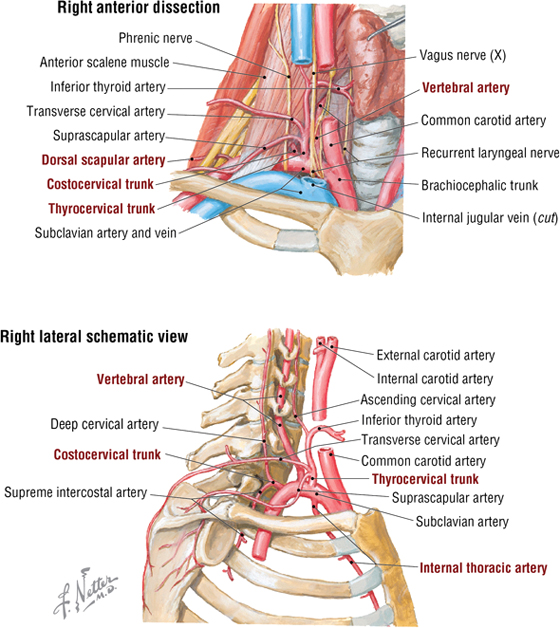
FIGURE 8-47 Subclavian Artery and Its Branches
|
TABLE 8-15 Branches of the Subclavian Artery
|
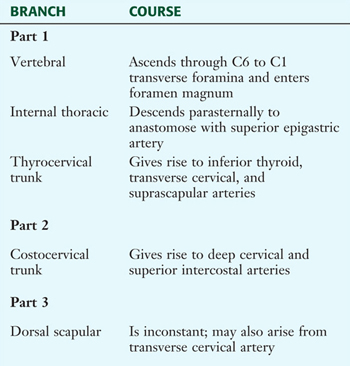 |
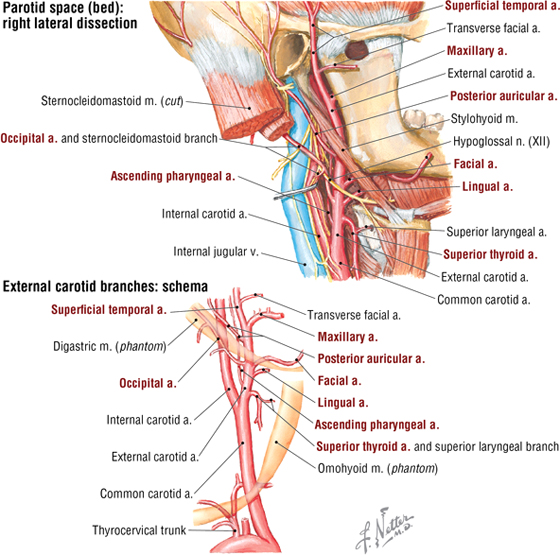
FIGURE 8-48 External Carotid Artery and Its Branches
|
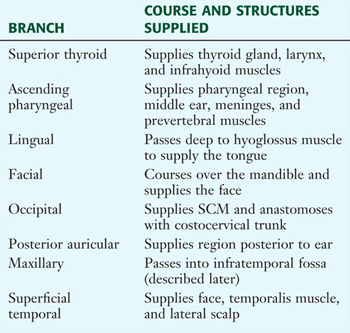
TABLE 8-16 Branches of the External Carotid Artery
|
 |
The venous drainage of the neck is highly variable, but most of the blood ultimately drains into tributaries of the external and internal jugular veins (Fig. 8-49). The external jugular vein is formed by the posterior auricular and posterior branch of the retromandibular veins, while the internal jugular vein begins at the jugular foramen as a continuation of the sigmoid dural sinus.
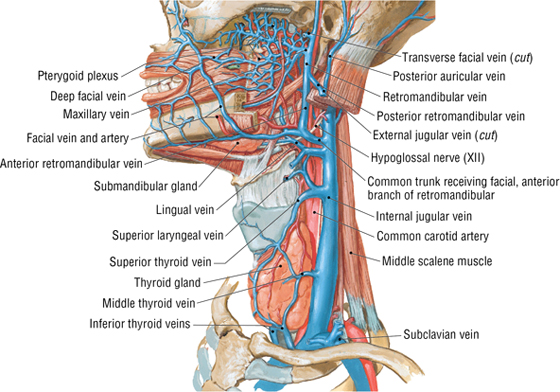
FIGURE 8-49 External and Internal Jugular Veins (Contd.)
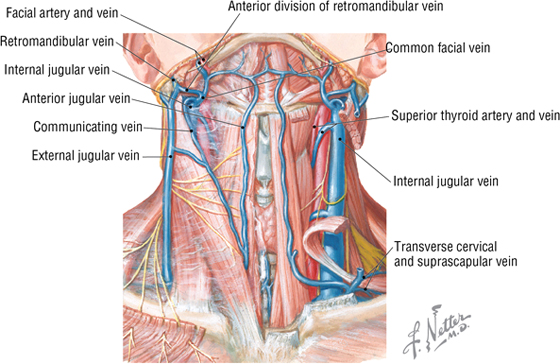
FIGURE 8-49 (Contd.) External and Internal Jugular Veins
C L I N I C A L F O C U S
Central Venous Access
When one wishes to place a large-bore catheter into a central vein, the subclavian or internal jugular veins may be used. Care must be exercised when introducing such a catheter because extensive bleeding and/or puncture of the apex of the pleural sac may occur. Ultrasonography is often used to help guide the catheter to the appropriate site.
C L I N I C A L F O C U S
Jugular Venous Pulses
The venous pulse is a normal pulse that can often be visualized in the right internal jugular vein in the lower neck. It is distinguished from an arterial pulse because it is impalpable (cannot be felt with your finger) unless there is an abnormality. The normal jugular venous pulse is visible just above the right clavicle in a patient lying supine at a 45° angle. The pulse ideally consists of the following two waves:
- A wave: results from the rebound of blood during atrial systole (contraction)
- V wave: results from the filling of the atria while the atrioventricular valve is still closed
The jugular venous pulse may be used to assess atrial filling and elevated or diminished venous pressures. Commonly, an elevated jugular venous pressure suggests congestive or right-sided heart failure, tricuspid valve regurgitation, pericardial tamponade, or several other abnormalities.
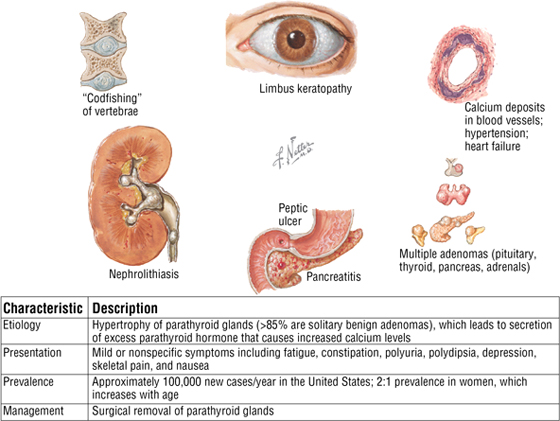
Thyroid and Parathyroid Glands
The thyroid gland lies at the C5-T1 vertebral level, anterior to the trachea, and is a ductless endocrine gland that weighs about 20 gm (Fig. 8-50 and Table 8-17). The thyroid gland secretes thyroxine (T4), triiodothyronine (T3), and calcitonin, and it performs the following functions:
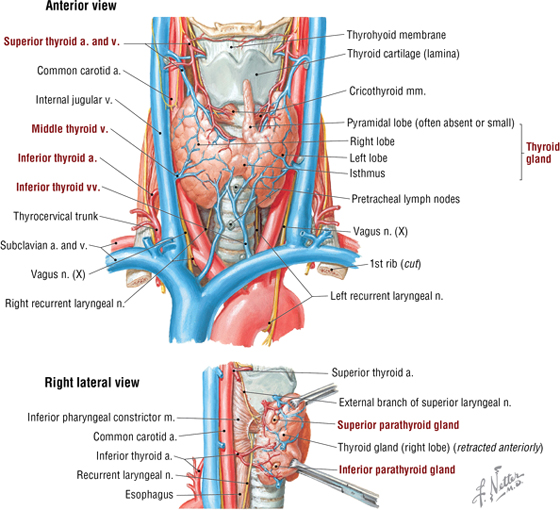
FIGURE 8-50 Thyroid and Parathyroid Glands and Their Blood Supply
|
TABLE 8-17 Features of the Thyroid Gland
|
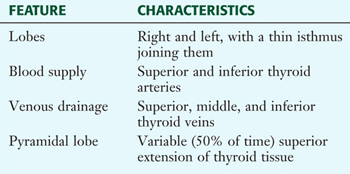 |
- Increases the metabolic rate of tissues
- Increases the consumption of oxygen
- Increases heart rate, ventilation, and renal function
- Is required for growth hormone production, and is important in CNS growth
- Increases the deposition of calcium and phosphate in bones (calcitonin)
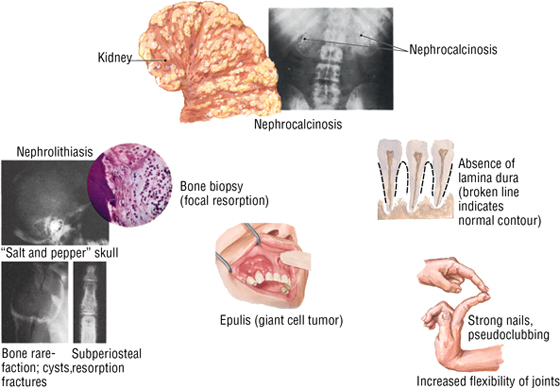
The parathyroid glands are paired superior and inferior glands (their number and location can vary) that are located on the posterior aspect of the thyroid gland (see Fig. 8-50). They secrete parathyroid hormone (PTH) in response to low calcium levels in the bloodstream and perform the following functions:
- Cause the resorption and release of calcium from bone
- Cause the resorption of calcium by the kidney
- Alter vitamin D metabolism, which is critical for calcium absorption from the GI tract
C L I N I C A L F O C U S
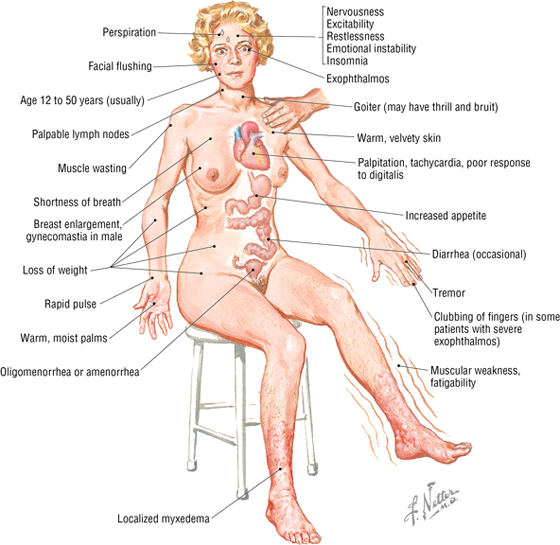
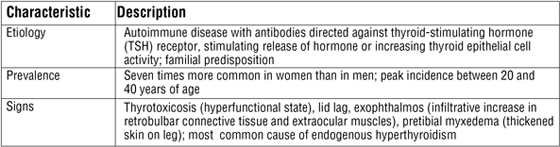
Hyperthyroidism with Diffuse Goiter (Graves’ Disease)
Graves’ disease is the most common cause of hyperthyroidism in patients younger than 40 years of age. Excess synthesis and release of thyroid hormone (T3 and T4) result in thyrotoxicosis, which upregulates tissue metabolism and leads to symptoms, indicating increased metabolism. Besides Graves’ disease, hyperthyroidism can be caused by benign growth of the thyroid gland, benign growth of the anterior pituitary gland, thyroiditis, the ingestion of excessive amounts of thyroid hormones and/or iodine, and tumors of the ovavies.
C L I N I C A L F O C U S
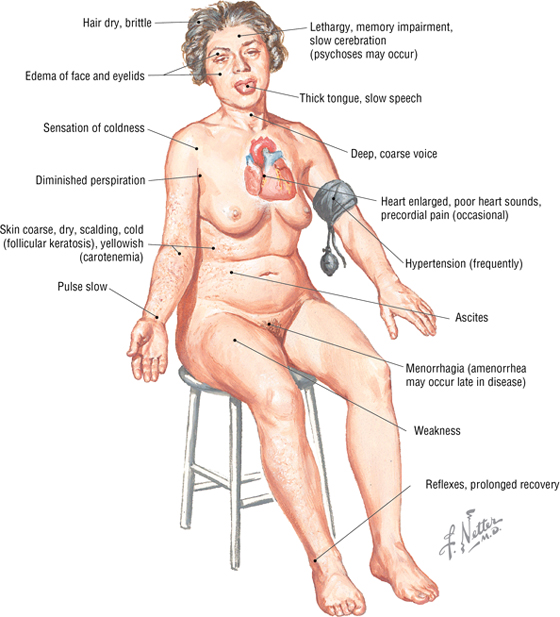
Primary Hypothyroidism
Primary hypothyroidism is a disease in which the thyroid gland produces inadequate amounts of thyroid hormone to meet the body’s needs. (Thyroid-stimulating hormone levels are elevated.) In addition to the autoimmune form of the disease, hypothyroidism also may occur from thyroidectomy and radiation-related damage.
C L I N I C A L F O C U S
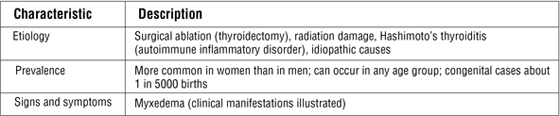
Manifestations of Primary Hyperparathyroidism
Prevertebral Muscles
A group of deep neck flexor muscles called the prevertebral muscles lie surrounded by the prevertebral fascia adjacent to the bodies of the cervical and upper thoracic vertebrae (Fig. 8-51 and Table 8-18).
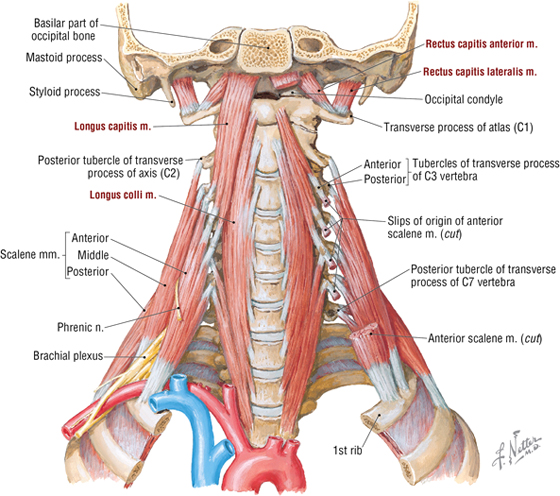
FIGURE 8-51 Prevertebral Muscles
|
TABLE 8-18 Prevertebral Muscles
|
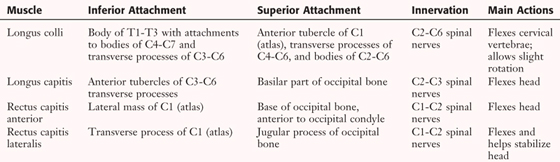 |
12. PHARYNX
The pharynx (throat), a fibromuscular tube, connects the nasal and oral cavities of the head with the larynx and esophagus in the neck (Fig. 8-52). The pharynx is subdivided as follows:
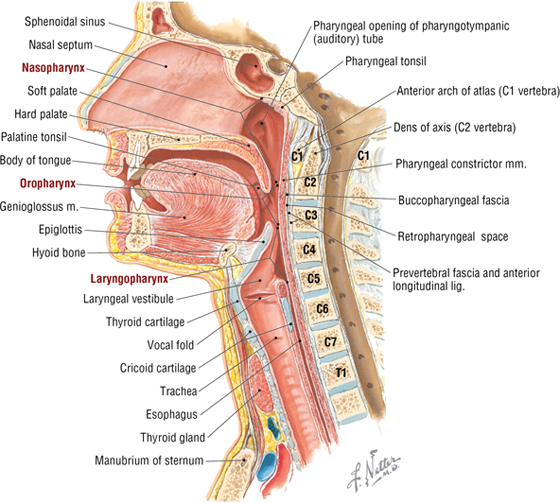
FIGURE 8-52 Subdivisions of the Pharynx
- Nasopharynx: lies posterior to the nasal cavity above the soft palate
- Oropharynx: extends from the soft palate to the superior tip of the epiglottis; lies posterior to the oral cavity
- Laryngopharynx: extends from the tip of the epiglottis to the inferior aspect of the cricoid cartilage; also known as the hypopharynx
The muscles of the pharynx (Fig. 8-53 and Table 8-19) participate in swallowing (deglutition) and contract serially from superior to inferior to move a bolus of food from the oropharynx and laryngopharynx into the proximal esophagus.
FIGURE 8-53 Pharyngeal Muscles
|
TABLE 8-19 Pharyngeal Muscles
|
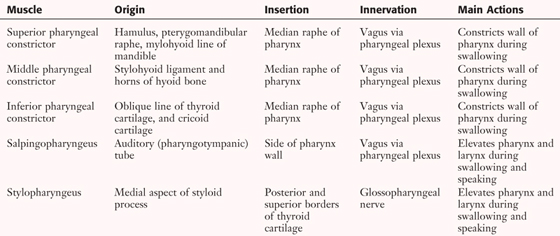 |
The blood supply to the pharynx is via branches of the thyrocervical trunk (subclavian) (see Fig. 8-47 and Table 8-15) and the external carotid artery (principally its superior thyroid, facial, ascending pharyngeal, and maxillary branches) (see Fig. 8-48 and Table 8-16). Venous drainage is via the pharyngeal venous plexus, the pterygoid plexus of veins, and the facial, lingual, and superior thyroid veins, which all drain primarily into the internal jugular vein (see Fig. 8-49).
Swallowing, or deglutition, includes the following sequence of events (Fig. 8-54):
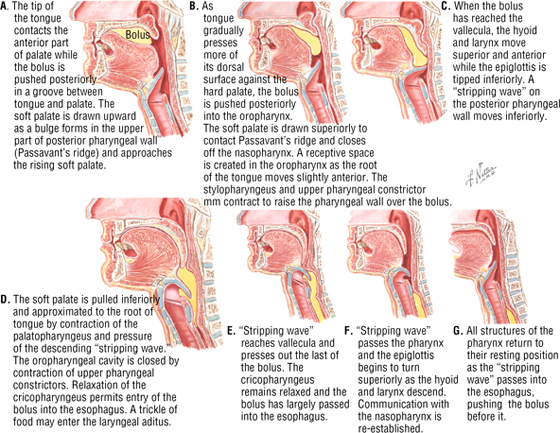
FIGURE 8-54 Deglutition (swallowing)
- The tongue pushes the bolus of food up against the hard palate.
- The soft palate elevates to close off the nasopharynx.
- The tongue pushes the bolus back into the oropharynx.
- As the bolus reaches the epiglottis, the larynx elevates and the tip of the epiglottis tips downward over the laryngeal opening (aditus).
- Contractions of the pharyngeal constrictors squeeze the bolus into two streams that pass on either side of the epiglottis and down along the piriform recesses and into the upper esophagus.
- The soft palate pulls downward to assist in moving the bolus around the epiglottis.
- The laryngeal vestibule and rima glottidis (space between the vocal folds) close to protect the larynx.
- Once the bolus is in the esophagus, all structures return to their starting positions.
The superior openings into the pharynx (nasal and oral cavities) are “guarded” by a ring of lymphoid tissue in the mucosa that composes Waldeyer’s tonsillar ring and includes the following (Fig. 8-55):
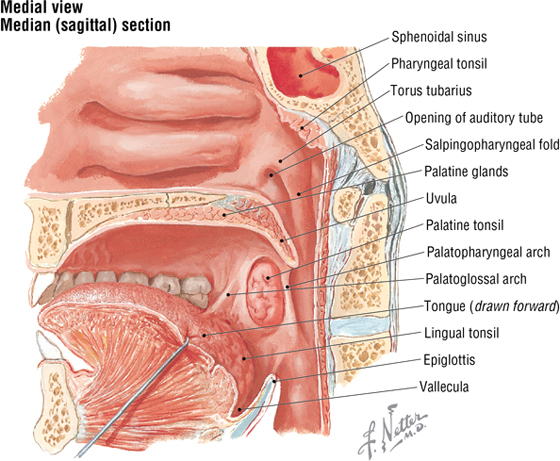
FIGURE 8-55 Tonsils
- Tubal tonsils: lymphoid tissue that is adjacent to the opening of the auditory tube; may be continuous with pharyngeal tonsils
- Pharyngeal tonsils: lie in the posterior wall and roof of the nasopharynx; called adenoids when enlarged
- Palatine tonsils: guard the oropharynx and lie between the palatoglossal and palatopharyngeal folds; receive a rich blood supply from branches of facial, lingual, ascending pharyngeal, and maxillary arteries of the external carotid
- Lingual tonsils: collection of lymphoid nodules on the posterior third of the tongue
13. LARYNX
The larynx (voice box) is a musculoligamentous and cartilaginous structure that lies at the C3-C6 vertebral level, just superior to the trachea. It functions both as a sphincter to close off the airway and as a “reed instrument” to produce sound. Its framework consists of nine cartilages joined by ligaments and membranes (Fig. 8-56 and Table 8-20).
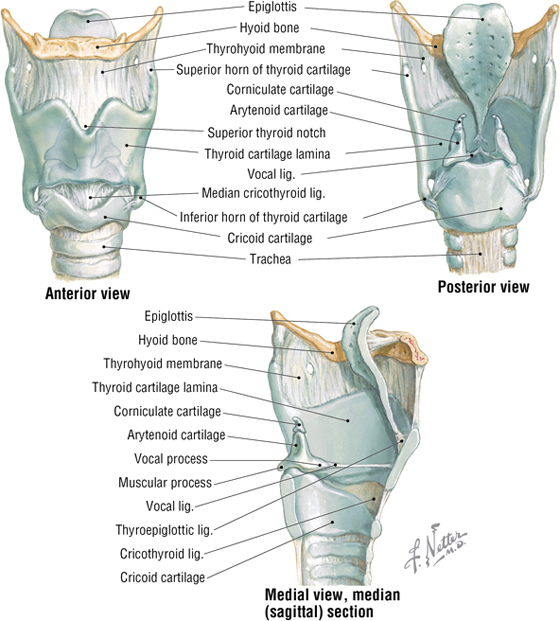
FIGURE 8-56 Laryngeal Cartilages, Ligaments, and Membranes
|
TABLE 8-20 Laryngeal Cartilages
|
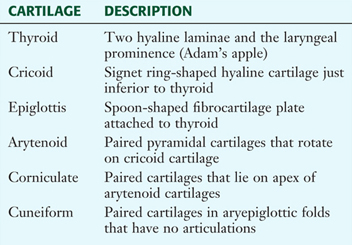 |
The intrinsic skeletal muscles of the larynx attach to the laryngeal cartilages and act largely to adjust the
tension on the vocal folds (ligaments, cords); to open or close the rima glottidis (space between the vocal folds); and to open or close the rima vestibuli, which is the space above the vestibular folds (false folds) (Fig. 8-57). The opening or closing of the rima vestibuli is important during swallowing (prevents aspiration into the trachea) but also adjusts the size of the vestibule during phonation, which enhances the quality of the sound. All of these muscles are innervated by the recurrent branch of CN X, except the cricothyroid muscle, which is innervated by the external branch of the superior laryngeal nerve (CN X). Sensation above the vocal folds is conveyed via the superior laryngeal nerve and by the recurrent laryngeal nerve below the vocal folds.
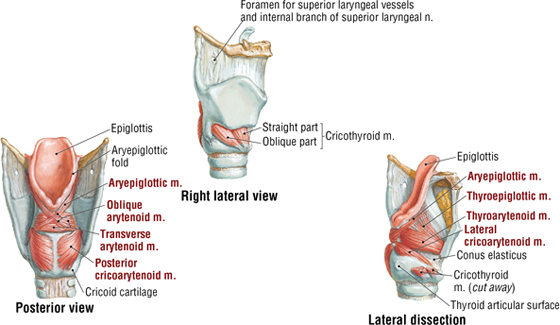
FIGURE 8-57 Muscles of the Larynx (Contd.)
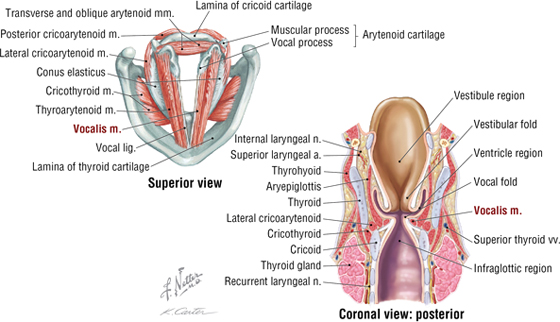
FIGURE 8-57 (Contd.) Muscles of the Larynx
C L I N I C A L F O C U S
Emergency Airway: Cricothyrotomy
When all other methods of establishing an airway have been exhausted or determined to be unsuitable, an incision can be made through the skin and the underlying cricothyroid membrane to gain access to the trachea. The site of the incision can be judged by locating the thyroid notch and sliding your finger inferiorly until the space between the thyroid and cricoid cartilages is palpated (about one fingerbreadth inferior to the thyroid notch). If the patient has a midline pyramidal lobe arising from the thyroid gland, this procedure may lacerate that tissue and cause significant bleeding.
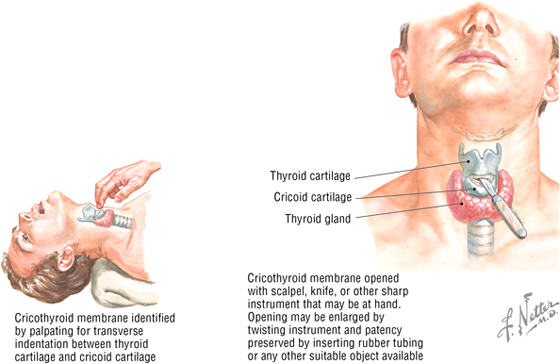
The vocal folds (vocal ligaments covered with mucosa) control phonation similar to a reed instrument. Vibrations of the folds produce sounds as air passes through the rima glottidis. The posterior cricoarytenoid muscles are important, as they are the only laryngeal muscles that abduct the vocal folds and maintain the opening of the rima glottidis. The vestibular folds are protective in function.
C L I N I C A L F O C U S
Manifestations of Hoarseness
Hoarseness can be due to any condition that results in improper vibration or coaptation of the vocal folds.
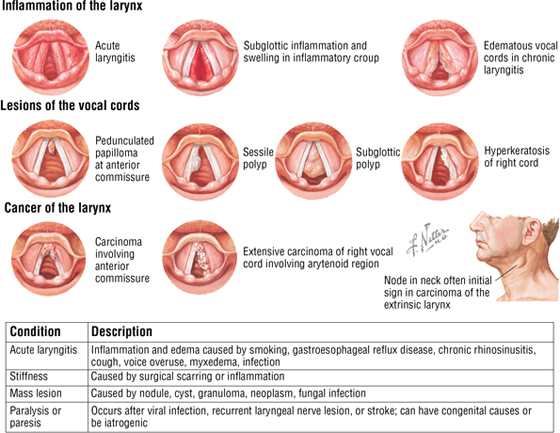
14. VASCULAR AND LYMPHATIC SUMMARY
Arteries of the head and neck largely include branches derived from the following major vessels (Fig. 8-58):
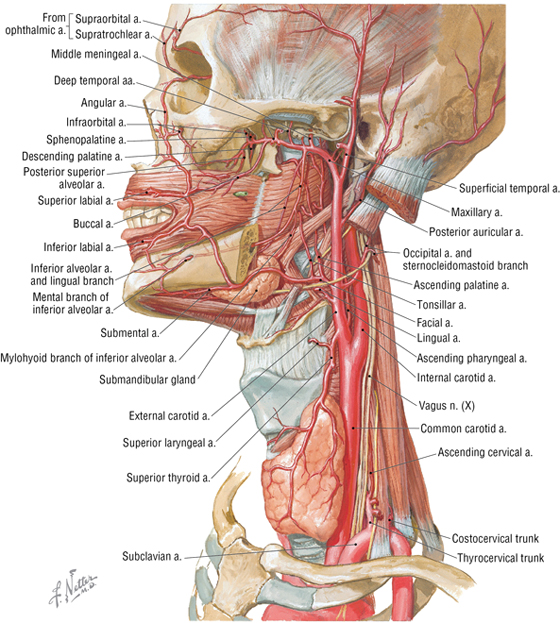
FIGURE 8-58 Major Arteries of the Head and Neck
- Subclavian: supplies the lower neck (thyrocervical and costocervical trunks), thoracic wall, shoulder, upper back, and brain (vertebral branches)
- External carotid: supplies the thyroid gland, larynx, pharynx, neck, oral cavity, face, nasal cavity, meninges, and temporal and infratemporal regions via its eight primary branches
- Internal carotid: supplies the brain, orbit, eyeball, lacrimal glands, forehead, and ethmoid sinuses
The venous drainage of the head and neck ultimately collects in the following major veins (numerous variations and anastomoses exist between these veins) (Fig. 8-59):
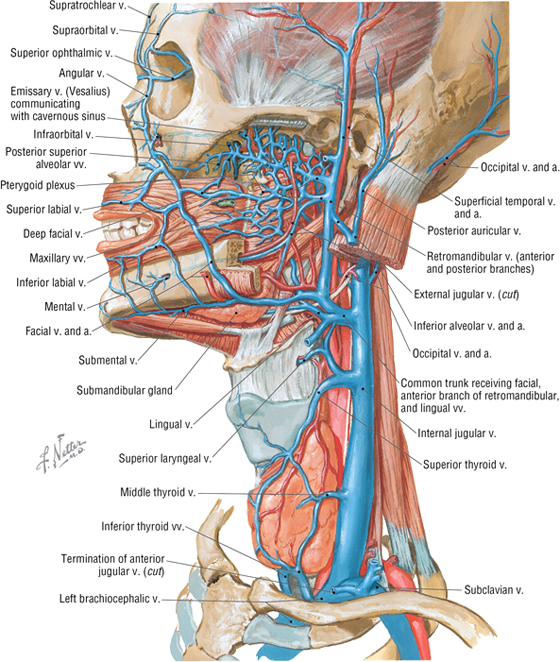
FIGURE 8-59 Major Veins of the Head and Neck
- Retromandibular: receives tributaries from the temporal and infratemporal regions (pterygoid plexus), orbit, nasal cavity, pharynx, and oral cavity
- Internal jugular: drains the brain (dural venous sinuses), face, thyroid gland, and neck
- External jugular: drains the superficial neck, lower neck and shoulder, and upper back (often communicates with the retromandibular vein) (see Fig. 8-49)
Lymph nodes and vessels of the head and neck tend to follow the venous drainage, with most of the lymph ultimately collecting in the deep cervical lymphatic chain (jugulodigastric and jugulo-omohyoid nodes), which courses along the internal jugular veins (Fig. 8-60). Superficial cervical nodes drain the superficial structures of the neck along lymphatic vessels that parallel the external jugular vein. The right side drains into the right lymphatic duct, and the left side drains into the thoracic duct (see Fig. 1-15).
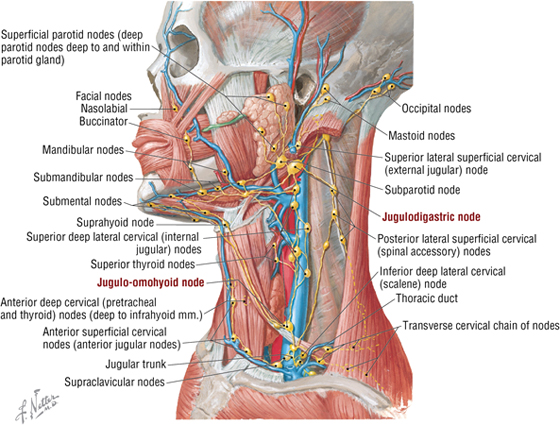
FIGURE 8-60 Major Lymphatics of the Head and Neck
15. CRANIAL NERVE SUMMARY
Autonomic Innervation
The autonomic distribution to the head involves preganglionic axons that arise from neurons in the CNS and synapse in peripheral ganglia (Fig. 8-61). Postganglionic axons then arise from neurons in these peripheral ganglia and course to their respective targets (smooth muscle and glands). The vagus nerve (not shown) provides parasympathetic innervation to the neck, thorax, and upper two-thirds of the abdominal viscera.
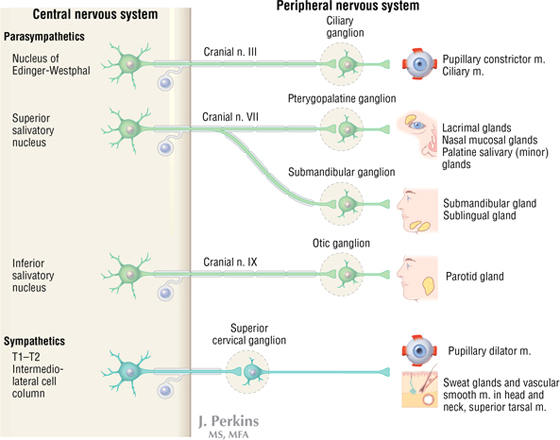
FIGURE 8-61 Autonomic Distribution to the Head
Preganglionic sympathetics from the upper thoracic spinal cord levels (T1-T2) ascend via the sympathetic trunk and synapse in the SCG. Postganglionic axons from the SCG then course along blood vessels or existing nerves to reach their targets (largely vasomotor, sweat glands, and some smooth muscle) (Fig. 8-62).
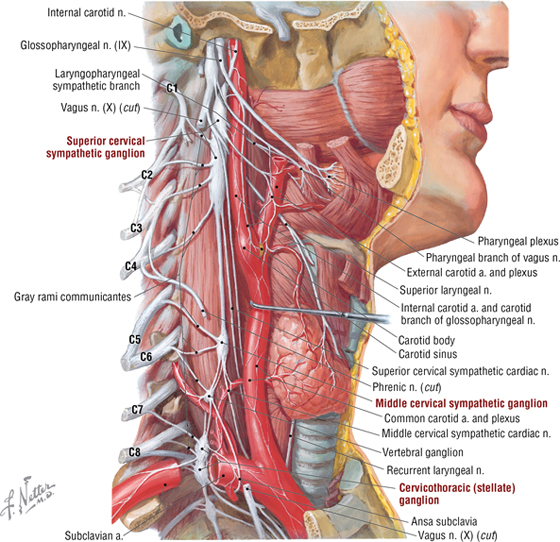
FIGURE 8-62 Sympathetic Ganglia and Nerves to the Head
Cranial Nerves
We reviewed the general components of the cranial nerves earlier in this chapter (see Table 8-4), so we will focus this summary selectively on the more complex cranial nerves.
Oculomotor, Trochlear, and Abducent Nerves
The oculomotor nerve (CN III) innervates five muscles in the orbit (general somatic efferents) and conveys parasympathetic preganglionics to the ciliary ganglion. (Postganglionics mediate pupillary constriction and accommodation.) The trochlear nerve (CN IV) innervates the superior oblique muscle, and the abducent nerve (CN VI) innervates the lateral rectus muscle (Fig. 8-63).
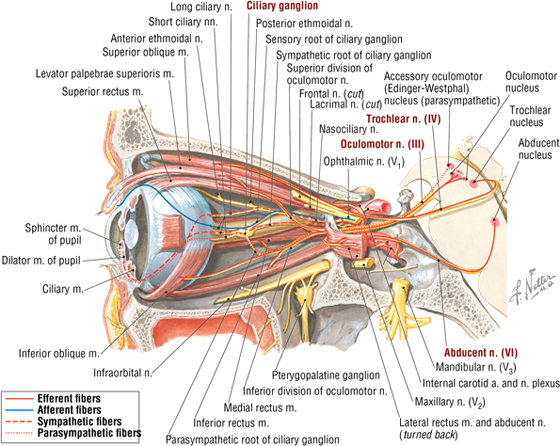
FIGURE 8-63 Pathway Summary for CN III, IV, and VI
Trigeminal Nerve
The trigeminal nerve (CN V), the major sensory nerve of the head, conveys general somatic afferents centrally to the trigeminal sensory ganglion via its ophthalmic, maxillary, and mandibular divisions. Its mandibular division also innervates muscles derived from the first embryonic branchial arch. Because of the trigeminal nerve’s extensive distribution, most of the parasympathetic fibers from CNs III, VII, and IX course with CN V to reach their targets (smooth muscle and glands) (Fig. 8-64).
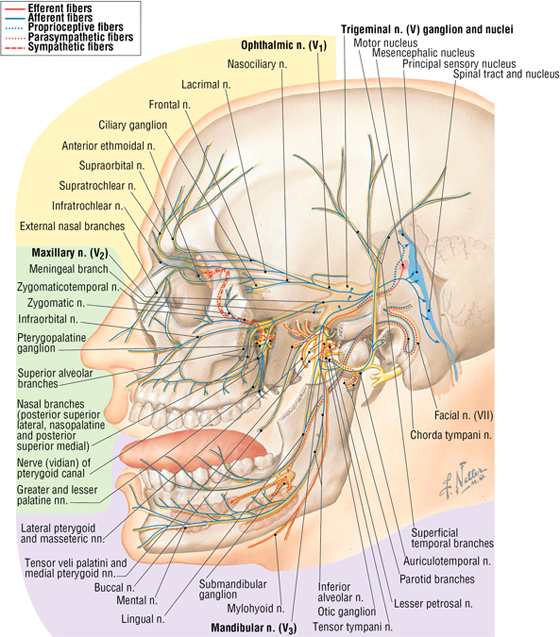
FIGURE 8-64 Pathway Summary for CN V
Facial Nerve
The facial nerve (CN VII), the major motor nerve of the head, conveys general somatic efferents to muscles derived from the second embryonic branchial arch. Additionally, it sends preganglionic parasympathetics from the superior salivatory nucleus via the intermediate nerve to the pterygopalatine (via greater petrosal and nerve of the pterygoid canal) and submandibular (via chorda tympani and lingual nerves) ganglia. It also conveys special visceral afferents from taste receptors on the anterior two-thirds of the tongue back along the chorda tympani to the geniculate sensory ganglion of CN VII (Fig. 8-65).
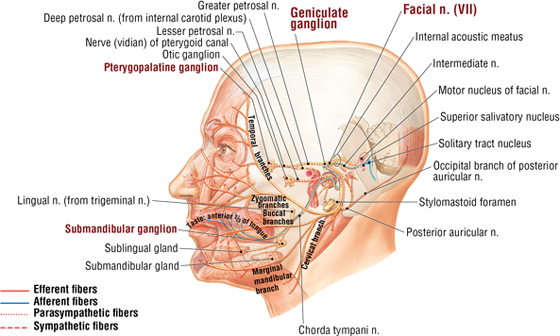
FIGURE 8-65 Pathway Summary for CN VII (Contd.)
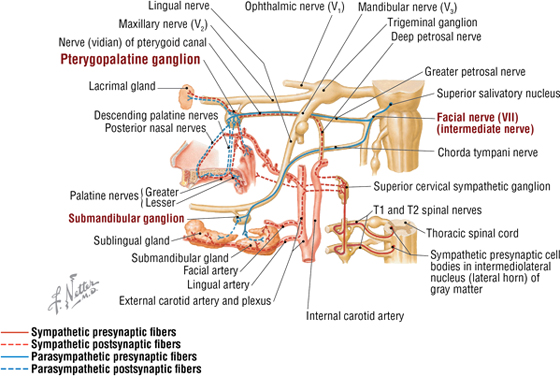
FIGURE 8-65 (Contd.) Pathway Summary for CN VII
Glossopharyngeal Nerve
The glossopharyngeal nerve (CN IX) innervates the stylopharyngeus muscle (derived from the third embryonic branchial arch), sends preganglionic parasympathetics from the inferior salivatory nucleus via the lesser petrosal nerve to the otic ganglion (innervates the parotid gland), and conveys special visceral afferents from taste receptors on the posterior third of the tongue to the sensory ganglia of CN IX. General visceral afferents also return from the carotid sinus (baroreceptors) and carotid body (chemoreceptors), tongue, pharynx, and middle ear (Fig. 8-66).
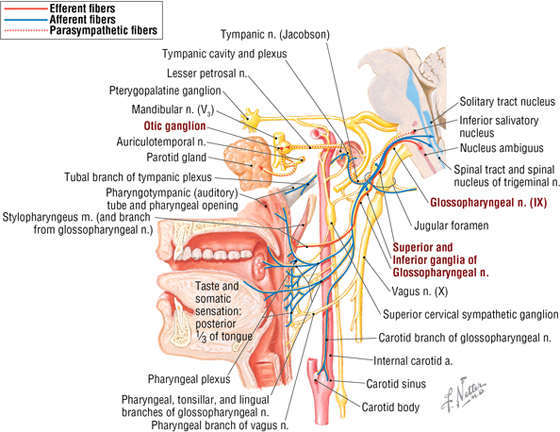
FIGURE 8-66 Pathway Summary for CN IX
Vagus Nerve
The vagus nerve (CN X) innervates the pharyngeal and laryngeal derivatives of the fourth embryonic branchial arch (via its superior laryngeal nerve) and sixth embryonic branchial arch (via the recurrent laryngeal nerve). It also sends preganglionic parasympathetic fibers to the neck, thorax, and proximal two-thirds of the abdominal GI tract, with its fibers synapsing in terminal ganglia in or very near the structures innervated. Afferents arise from visceral structures of the same regions and from taste on the epiglottis, and general afferents arise from skin around the ear and posterior dura mater (Fig. 8-67).
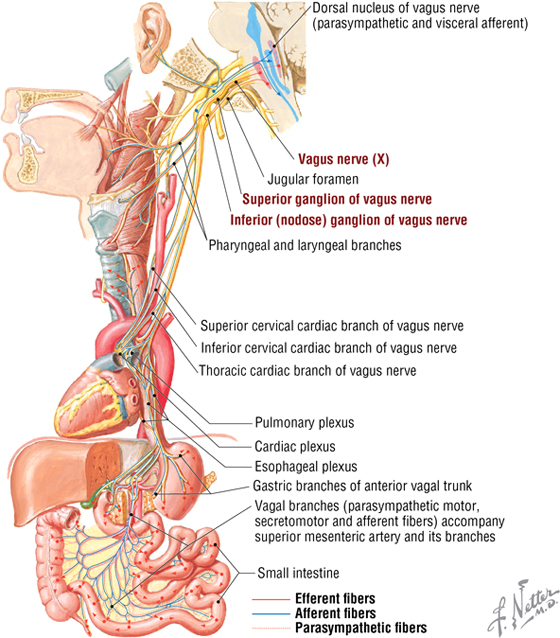
FIGURE 8-67 Pathway Summary for CN X
16. EMBRYOLOGY
Brain Development
The cranial end of the neural tube begins to expand into definitive swellings and characteristic flexures during the fourth week of development, giving rise to the forebrain, midbrain, and hindbrain (Fig. 8-68). By the fifth week, these three divisions subdivide into five regions that ultimately give rise to the definitive brain structures (Fig. 8-68).
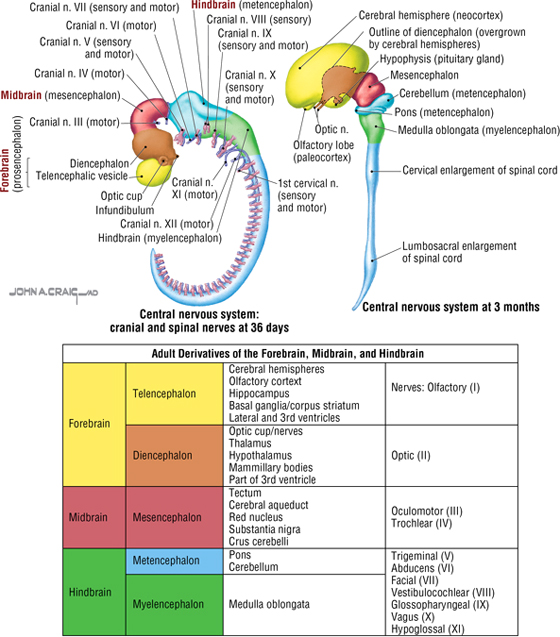
FIGURE 8-68 Brain Development at Five Weeks and Three Months
Cranial Nerve Development
The 12 pairs of cranial nerves develop from cranial to caudal (except for CN XI, which arises from the upper cervical spinal cord); as direct extensions of the neural tube (CN I and CN II); or as peripheral nerve outgrowths to surface placodes, somitomeres (head somites), and pharyngeal arches. Consequently, they innervate the structures and tissues derived from these targets (Fig. 8-69). The spinal accessory nerve (CN XI) is unique in that it lacks a cranial root and innervates two muscles derived from cervical somites—the trapezius and sternocleidomastoid.
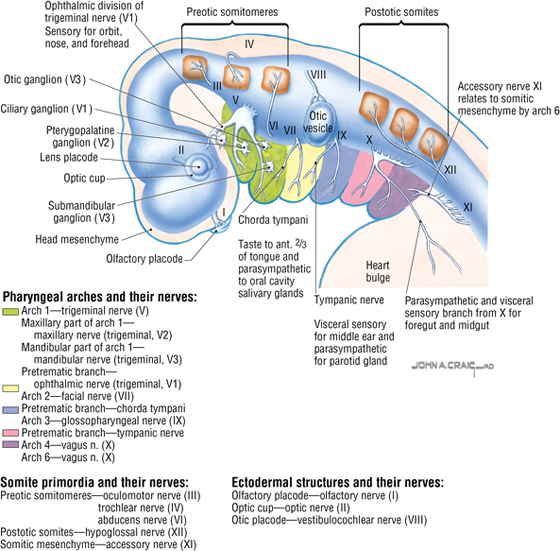
FIGURE 8-69 Cranial Nerve Primordia
C L I N I C A L F O C U S
Craniosynostosis
As the brain grows, so does the neurocranium, by bone deposition along suture lines. If this process is interrupted (because of unknown reasons or genetic factors), the cranium may compensate by depositing more bone along other sutures. If the sagittal suture closes prematurely, growth in width is altered, so growth occurs lengthwise and leads to a long, narrow cranium; coronal and lambdoid suture closure results in a short, wide cranium. The disorder occurs in about 1 in 2000 births and is more common in men than in women.
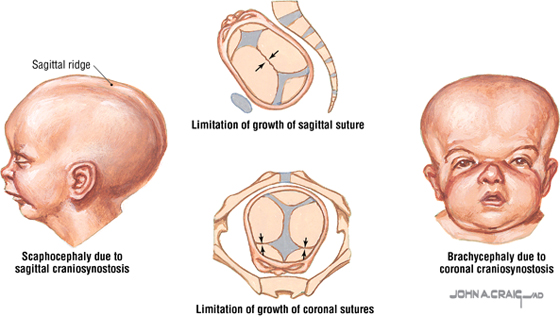
Pharyngeal Arch and Pouch Development
Pharyngeal arches develop from the human ancestral gill (branchial) arch system as an evolutionary adaptation to terrestrial life. The original six pairs of arches develop into four pairs, with a cranial nerve, the muscles it innervates, a cartilage/bone element, and an aortic arch associated with each arch (Fig. 8-70).
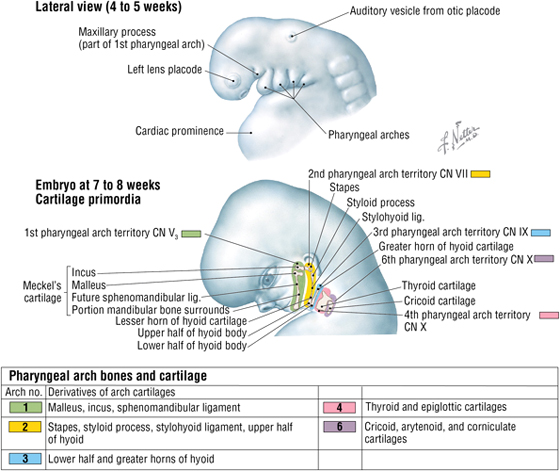
FIGURE 8-70 Pharyngeal Arches
Internally, each arch is also associated with an endoderm-derived pharyngeal pouch, an outpocketing of the foregut in the head and neck. The four pharyngeal pouches give rise to various important structures, but the thyroid gland develops as its own diverticulum from the tongue and migrates to its final position anterior to the trachea (Fig. 8-71).
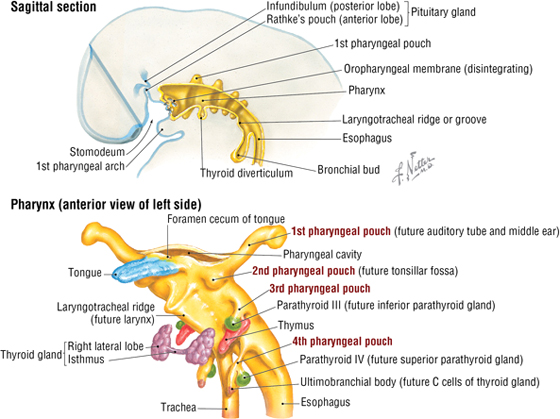
FIGURE 8-71 Pharyngeal Pouch Derivatives
C L I N I C A L F O C U S
Pharyngeal Arch and Pouch Anomalies
Most anomalies of the pharyngeal apparatus involve fistulas, cysts, or ectopic glandular tissue. Some common anomalies and their sources from the associated pharyngeal pouch or wall are shown here in a composite illustration.
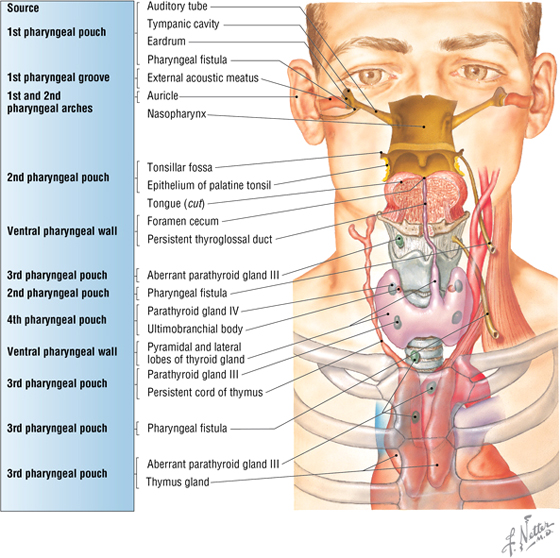
Facial Development
The face develops primarily from the neural crest by the fusion of an unpaired frontonasal prominence with bilateral maxillary, nasal (ectoderm-derived), and mandibular prominences that meet in the midline (Fig. 8-72). Fusion along the midline by portions of the maxilla and palatine bone gives rise to the hard palate, separating the nasal and oral cavities (Fig. 8-73).
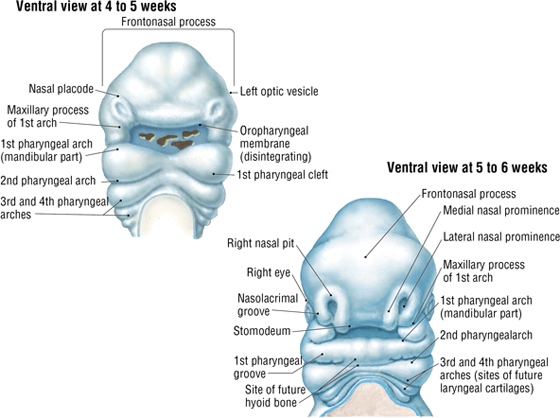
FIGURE 8-72 Development of the Face (Contd.)
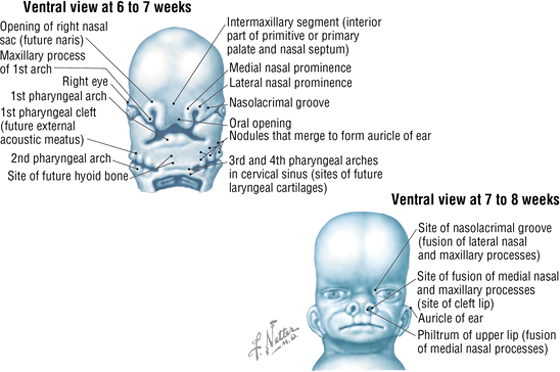
FIGURE 8-72 (Contd.) Development of the Face
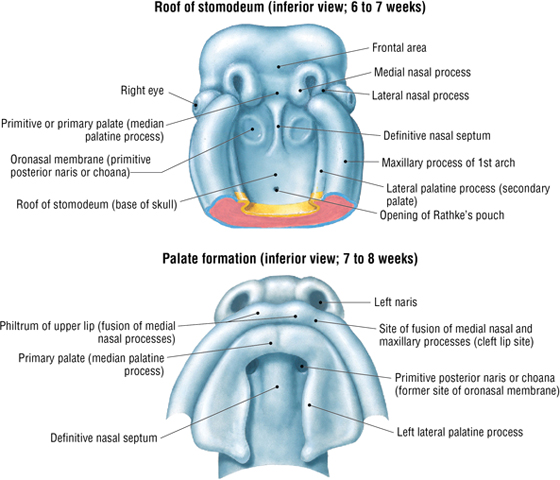
FIGURE 8-73 Development of the Hard Palate (Contd.)
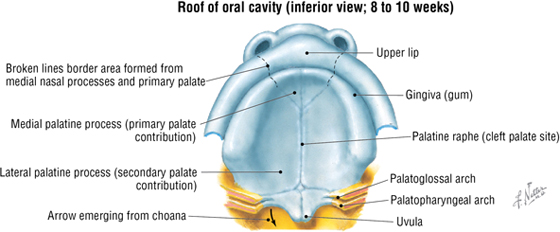
FIGURE 8-73 (Contd.) Development of the Hard Palate
C L I N I C A L F O C U S
Congenital Anomalies of the Oral Cavity
Because the face and oral cavity develop largely by midline fusion of various prominences, incomplete or failed fusion can lead to cleft formation (lips and palate) or anomalous features (ankyloglossia, torus formations). The etiology is multifactorial, but genetics appears to play some role.
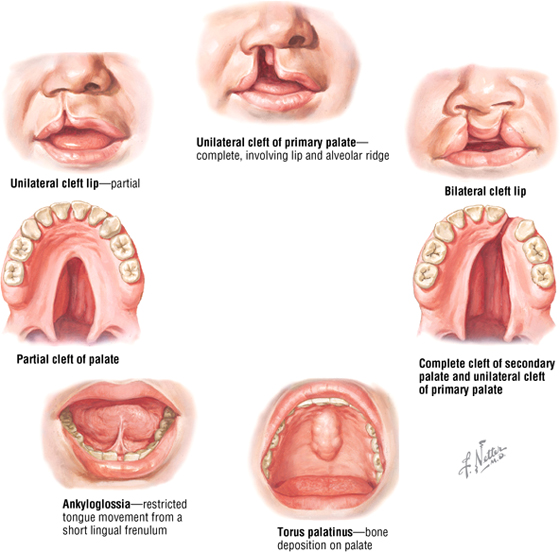
C L I N I C A L F O C U S
Online Figures
Scalp wounds
Papilledema
Mandibular dislocations
Nosebleed
Nerve lesions
Central venous access
Additional figures available online. See Table of Contents for Instructions for online access.