 CHAPTER 35 Sodium Disorders
CHAPTER 35 Sodium Disorders
The kidney regulates sodium balance and is the principal site of sodium excretion. Sodium is unique among electrolytes because water balance, not sodium balance, usually determines its concentration. When the sodium concentration increases, the resultant higher plasma osmolality causes increased thirst and increased secretion of antidiuretic hormone (ADH), which leads to renal conservation of water. Both of these mechanisms increase the water content of the body, and the sodium concentration returns to normal. During hyponatremia, the fall in plasma osmolality decreases ADH secretion, and consequent renal water excretion leads to an increase in the sodium concentration. Although water balance usually is regulated by osmolality, volume depletion stimulates thirst, ADH secretion, and renal conservation of water. Volume depletion takes precedence over osmolality; volume depletion stimulates ADH secretion, even if a patient has hyponatremia.
The excretion of sodium by the kidney is not regulated by the plasma osmolality. The patient’s effective plasma volume determines the amount of sodium in the urine. Effective plasma volume is controlled by a variety of regulatory systems, including the renin-angiotensin-aldosterone system and intrarenal mechanisms. In hyponatremia or hypernatremia, the underlying pathophysiology determines the urinary sodium concentration, not the serum sodium concentration.
HYPONATREMIA
Etiology
Different mechanisms can cause hyponatremia (Fig. 35-1). Pseudohyponatremia is a laboratory artifact that is present when the plasma contains high concentrations of protein or lipid. It does not occur when a direct ion-selective electrode determines the sodium concentration, a technique that is increasingly used in clinical laboratories. In true hyponatremia, the measured osmolality is low, whereas it is normal in pseudohyponatremia. Hyperosmolality, resulting from mannitol infusion or hyperglycemia, causes a low serum sodium concentration because water moves down its osmotic gradient from the intracellular space into the extracellular space, diluting the sodium concentration. For every 100 mg/dL-increment of the serum glucose, the serum sodium decreases by 1.6 mEq/L. Because the manifestations of hyponatremia are due to the low plasma osmolality, patients with hyponatremia caused by hyperosmolality do not have symptoms of hyponatremia and do not require correction of hyponatremia.
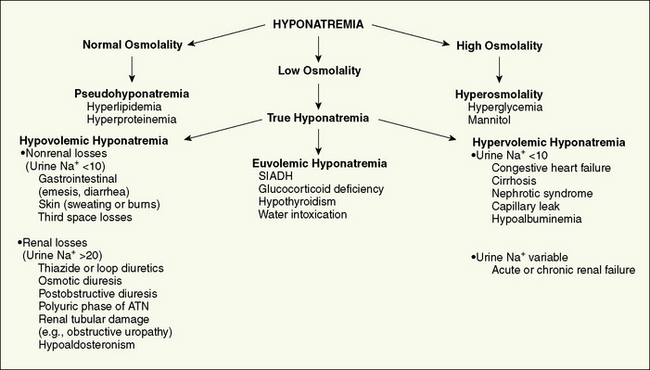
Figure 35-1 Differential diagnosis of hyponatremia. Assessment of hyponatremia is a three-step process: (1) Determine if the osmolality is low; if yes, the patient has true hyponatremia. (2) Evaluate the patient’s volume status. (3) Determine the urine sodium concentration to help narrow the differential diagnosis. ATN, acute tubular necrosis; SIADH, syndrome of inappropriate secretion of antidiuretic hormone.
Classification of true hyponatremia is based on the patient’s volume status (see Fig. 35-1). In hypovolemic hyponatremia, the child has lost sodium from the body. Water balance may be positive or negative, but there has been a higher net sodium loss than water loss; this is due to oral or intravenous (IV) water intake, with water retention by the kidneys to compensate for the intravascular volume depletion. If the sodium loss is due to a nonrenal disease, the urine sodium concentration is very low, as the kidneys attempt to preserve the intravascular volume by conserving sodium. In renal diseases, the urine sodium is inappropriately elevated.
Patients with hyponatremia and no evidence of volume overload or volume depletion have euvolemic hyponatremia. These patients typically have an excess of total body water and a slight decrease in total body sodium. Some of these patients have an increase in weight, implying that they are volume overloaded. Nevertheless, they usually appear normal or have only subtle signs of fluid overload. In syndrome of inappropriate ADH (SIADH), there is secretion of ADH that is not inhibited by either low serum osmolality or expanded intravascular volume. Retention of water causes hyponatremia, and the expansion of the intravascular volume results in an increase in renal sodium excretion. Hyponatremia in hospitalized patients is often due to inappropriately produced ADH secondary to stress in the presence of hypotonic fluids. SIADH is associated with pneumonia, mechanical ventilation, meningitis, and other central nervous system disorders (trauma). Ectopic (tumor) production of ADH is rare in children. Infants also can develop euvolemic hyponatremia as a result of excessive water consumption or inappropriately diluted formula.
In hypervolemic hyponatremia, there is an excess of total body water and sodium, although the increase in water is greater than the increase in sodium. In renal failure, there is an inability to excrete sodium or water; the urine sodium may be low or high, depending on the cause of the renal insufficiency. In other causes of hypervolemic hyponatremia, there is a decrease in the effective blood volume because of either third space fluid loss or poor cardiac output (see Chapter 145). Regulatory systems sense this decrease in effective blood volume and retain water and sodium to correct the problem. ADH causes renal water retention, and the kidneys, under the influence of aldosterone and other intrarenal mechanisms, retain sodium, leading to a low urine sodium concentration. The patient’s serum sodium concentration decreases because water intake exceeds sodium intake, and ADH prevents the normal loss of excess water.
Clinical Manifestations
Hyponatremia causes a fall in the osmolality of the extracellular space. Because the intracellular space then has a higher osmolality, water moves from the extracellular space to the intracellular space to maintain osmotic equilibrium. The increase in intracellular water may cause cells to swell. Brain cell swelling is responsible for most of the symptoms of hyponatremia. Neurologic symptoms of hyponatremia include anorexia, nausea, emesis, malaise, lethargy, confusion, agitation, headache, seizures, coma, and decreased reflexes. Patients may develop hypothermia and Cheyne-Stokes respirations. Hyponatremia can cause muscle cramps and weakness. Symptoms are more severe when hyponatremia develops rapidly; chronic hyponatremia can be asymptomatic because of a compensatory decrease in brain cell osmolality, which limits cerebral swelling.
Treatment
Rapid correction of hyponatremia can produce central pontine myelinolysis. Avoiding more than a 12-mEq/L increase in the serum sodium every 24 hours is prudent, especially if the hyponatremia developed gradually. Treatment of hypovolemic hyponatremia requires administration of IV fluids with sodium to provide maintenance requirements and deficit correction, as well as to replace ongoing losses (see Chapter 33). For children with SIADH, water restriction is the cornerstone of therapy. Children with hypothyroidism or cortisol deficiency need specific hormone replacement. Acute water intoxication rapidly self-corrects with transient restriction of water intake, which is followed by introduction of a normal diet. Treatment of hypervolemic hyponatremia centers on restriction of water and sodium intake, but disease-specific measures, such as dialysis in renal failure, also may be necessary.
Emergency treatment of symptomatic hyponatremia, such as seizures, uses IV hypertonic saline to increase the serum sodium concentration rapidly, which leads to a decrease in brain edema. One milliliter per kilogram of 3% sodium chloride increases the serum sodium by approximately 1 mEq/L. A child often improves after receiving 4 to 6 mL/kg of 3% sodium chloride.
HYPERNATREMIA
Etiology
There are three basic mechanisms of hypernatremia (Fig. 35-2). Sodium intoxication is frequently iatrogenic in a hospital setting resulting from correction of metabolic acidosis with sodium bicarbonate. In hyperaldosteronism, there is renal retention of sodium and resultant hypertension; the hypernatremia is mild.
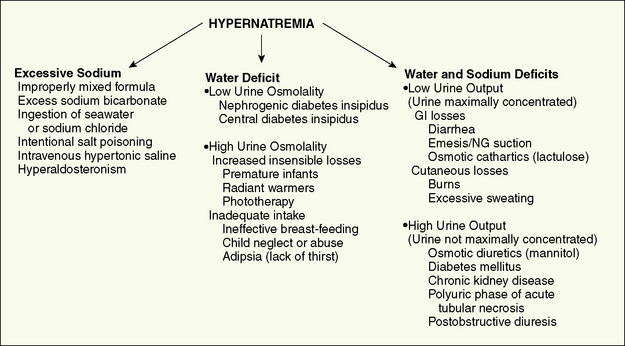
Figure 35-2 Differential diagnosis of hypernatremia by mechanism. GI, gastrointestinal; NG, nasogastric.
Hypernatremia resulting from water losses develops only if the patient does not have access to water or cannot drink adequately because of neurologic impairment, emesis, or anorexia. Infants are at high risk because of their inability to control their own water intake. Ineffective breastfeeding, often in a primiparous mother, can cause severe hypernatremic dehydration. High insensible losses of water are especially common in premature infants; the losses increase further as a result of radiant warmers or phototherapy for hyperbilirubinemia. Children with extrarenal causes of water loss have high levels of ADH and very concentrated urine.
Children with diabetes insipidus have inappropriately diluted urine. Hereditary nephrogenic diabetes insipidus causes massive urinary water losses. Because it is most commonly an X-linked disorder, it usually occurs in boys, who may have episodes of severe hypernatremic dehydration and failure to thrive. The defect is in the gene for the ADH receptor in the X-linked form of nephrogenic diabetes insipidus. Acquired nephrogenic diabetes insipidus may be secondary to interstitial nephritis, sickle cell disease, hypercalcemia, hypokalemia, or medications (lithium or amphotericin). If the defect is due to central diabetes insipidus, the urine output decreases, and the urine osmolality increases in response to administration of an ADH analog. Central causes of ADH deficiency include tumor, infarction, or trauma. There is no response to an ADH analog in a child with nephrogenic diabetes insipidus.
Diarrhea results in sodium and water depletion. Most children with gastroenteritis do not develop hypernatremia because they drink enough hypotonic fluid to compensate at least partially for stool water losses. Hypernatremia is most likely in a child with diarrhea who has inadequate intake because of emesis, lack of access to water, or anorexia. Some renal diseases, including obstructive uropathy, renal dysplasia, and juvenile nephronophthisis, can cause losses of sodium and water, potentially producing hypernatremia if the patient consumes insufficient water.
In situations with combined sodium and water deficits, analysis of the urine differentiates renal and nonrenal etiologies. When the losses are extrarenal, the kidney responds to volume depletion with low urine volume, a concentrated urine, and sodium retention (urine sodium <10 mEq/L). With renal causes, the urine volume is not appropriately low, the urine is not maximally concentrated, and the urine sodium may be inappropriately elevated.
Clinical Manifestations
Most children with hypernatremia are dehydrated and have the typical signs and symptoms of dehydration (see Chapter 33). Children with hypernatremic dehydration tend to have better preservation of intravascular volume owing to the shift of water from the intracellular space to the extracellular space. Blood pressure and urine output are maintained, and hypernatremic infants potentially become more dehydrated before seeking medical attention. Probably because of intracellular water loss, the pinched abdominal skin of a dehydrated, hypernatremic infant has a doughy feel.
Hypernatremia, even without dehydration, causes central nervous system symptoms that tend to parallel the degree of sodium elevation and the acuity of the increase. Patients are irritable, restless, weak, and lethargic. Some infants have a high-pitched cry and hyperpnea. Alert patients are very thirsty, although nausea may be present. Hypernatremia causes fever, although many patients have an underlying process that contributes to the fever. Hypernatremia is associated with hyperglycemia and mild hypocalcemia; the mechanisms are unknown.
Brain hemorrhage is the most devastating consequence of hypernatremia. As the extracellular osmolality increases, water moves out of brain cells, resulting in a decrease in brain volume. This decrease in volume can result in tearing of intracerebral veins and bridging blood vessels as the brain moves away from the skull and the meninges. Patients may have subarachnoid, subdural, and parenchymal hemorrhage. Seizures and coma are possible sequelae of the hemorrhage.
Treatment
As hypernatremia develops, the brain generates idiogenic osmoles to increase the intracellular osmolality and prevent the loss of brain water. This mechanism is not instantaneous and is most prominent when hypernatremia has developed gradually. If the serum sodium concentration is lowered rapidly, there is movement of water from the serum into the brain cells to equalize the osmolality in the two compartments. The resultant brain swelling manifests as seizures or coma.
Because of the dangers of overly rapid correction, hypernatremia should be corrected slowly. The goal is to decrease the serum sodium by less than 12 mEq/L every 24 hours, a rate of 0.5 mEq/L/hr. The most important component of correcting moderate or severe hypernatremia is frequent monitoring of the serum sodium to allow adjustment of fluid therapy and provide adequate correction that is neither too slow nor too fast. If a child develops seizures from brain edema secondary to rapid correction, administration of hypotonic fluid should be stopped, and an infusion of 3% saline should be used to increase the serum sodium acutely.
In a child with hypernatremic dehydration, as in any child with dehydration, the first priority is restoration of intravascular volume with isotonic fluid. Table 33-8 outlines a general approach for correcting hypernatremic dehydration secondary to gastroenteritis. If the hypernatremia and dehydration are secondary to water loss, as occurs with diabetes insipidus, a more hypotonic IV fluid is appropriate. A child with central diabetes insipidus should receive an ADH analog to prevent further excessive water loss. A child with nephrogenic diabetes insipidus requires a urine replacement solution to offset ongoing water losses. Chronically, reduced sodium intake, thiazide diuretics, and nonsteroidal anti-inflammatory drugs can decrease water losses in nephrogenic diabetes insipidus.
Acute, severe hypernatremia, usually secondary to sodium administration, can be corrected more rapidly because idiogenic osmoles have not had time to accumulate; this balances the high morbidity and mortality from severe, acute hypernatremia with the dangers of overly rapid correction. When hypernatremia is due to sodium intoxication, and the hypernatremia is severe, it may be impossible to administer enough water to correct the hypernatremia rapidly without worsening volume overload. Some patients require use of a loop diuretic or dialysis.