Insufficient Finger and/or Thumb Extension Syndrome
The principal impairment of insufficient finger and/or thumb extension syndrome is limited finger or thumb extension AROM, but the key to prescribing the appropriate intervention is differentiating between the sources causing the limited extension. The identified cause of insufficient finger and/or thumb extension is the second part of the name of the syndrome. Insufficient finger or thumb extension may be caused by the following:
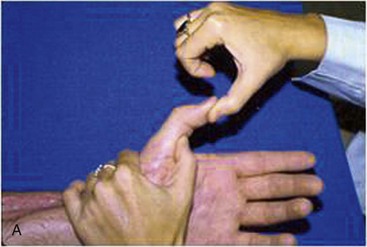

Figure 5-60 Insufficient thumb extension caused by adhered flexor pollicis longus. A, Limited passive range of thumb IP extension with MP extended. B, Normal IP extension with thumb MP flexed.
(Used with permission from Ann Kammien, PT, CHT, St Louis, Mo.)

Figure 5-61 Insufficient finger extension caused by extensor adhesion (PIP extensor lag).
(Used with permission from Ann Kammien, PT, CHT, St Louis, Mo.)


Figure 5-62 Insufficient finger extension caused by extrinsic flexor shortness. A, Normal range of PIP and DIP extension with MP and wrist flexed. B, Limited PIP extension with MP and wrist extended.

Figure 5-63 Insufficient finger extension caused by contracture of volar plate and accessory collateral ligaments.
(Used with permission from Ann Kammien, PT, CHT, St Louis, Mo.)
Insufficient finger and/or thumb extension syndrome is not be described further here because the principles for understanding it are the same as for insufficient finger and/or thumb flexion syndrome. See the Chapter 5 Appendix for additional details related to examination and treatment for this syndrome.
Insufficient Thumb Palmar Abduction and/or Opposition Syndrome
The principal impairment of insufficient thumb palmar abduction and/or opposition syndrome is limited thumb AROM into thumb palmar abduction and/or opposition, but the key to prescribing the appropriate intervention is differentiating between the sources causing the limited opposition and/or abduction. The sources of the limited thumb palmar abduction and/or opposition can be broadly classified into two main categories: hypomobility (physiological and accessory motion) or force production deficit (decreased strength). Pain may or may not be associated with the limited movement. Contracture resulting in insufficient thumb palmar abduction and/or opposition (hypomobility) is most commonly secondary to a trauma or injury or after a period of immobilization to allow for tissue healing.81 Acutely, these patients may be assigned a pathoanatomical source diagnosis or hand impairment Stage 1, but the underlying movement system diagnosis of insufficient thumb palmar abduction and/or opposition syndrome may help guide treatment. As the tissues heal, the diagnosis may change from a pathoanatomical source or regional hand impairment to insufficient thumb palmar abduction and/or opposition syndrome. Contracture resulting in insufficient thumb palmar abduction and/or opposition (hypomobility) may also be secondary to paralysis caused by a median nerve injury.81 However, if there is any active function of the median nerve innervated muscles, then the diagnosis force production deficit would guide treatment. A third reason for insufficient thumb palmar abduction and/or opposition (hypomobility) is joint subluxation and deformity secondary to the later stages OA of the CMC joint of the thumb.7,82 The “Source of Signs and Symptoms” section provides key information regarding the cluster of findings identifying the cause of the insufficient thumb palmar abduction and/or opposition for this syndrome.
Symptoms and History
The patient with insufficient thumb palmar abduction and/or opposition may complain of difficulty gripping objects, pain in the hand and/or the forearm, and a history of median nerve injury or trauma.81 If patients have had a nerve injury, they may also report a loss of sensation. Patients with DJD of the CMC of the thumb may report slowly developing joint pain, stiffness and limitation of motion, and difficulty with functional activities caused by pain. Activities related to DJD of the CMC joint of the thumb include needlework or repetitive use of scissors (e.g., a hairdresser). DJD of the CMC of the thumb is more common in women than men, and the onset is usually in the fifth to seventh decades of life.83 Common referring diagnoses may include status/postfracture after immobilization, median nerve injury, crush injury, spinal cord injury, brachial plexus injury, hand pain, or DJD of the CMC joint of the thumb.
Key Tests and Signs
Alignment Analysis
Impairments in alignment and appearance for patients with this syndrome include decreased first web space (thumb resting in more adduction than normal), scar, and muscle atrophy. In addition, patients in the later stages of DJD of the CMC joint of the thumb may have swelling at the CMC joint of thumb, prominence, and subluxation and an adduction deformity of the thumb CMC joint (see Figures 5-9, B, and 5-10, B). Associated alignment impairments of flexion or hyperextension at the thumb MP joint may also be noted.7,82
Movement Impairment Analysis
Movement impairments noted in this syndrome include decreased thumb CMC joint abduction during functional activities requiring opening of the hand in preparation for pinch or grip, inability maintaining the normal longitudinal arch of the thumb, and in some cases the MP joint may abduct excessively to compensate for the lack of CMC joint abduction.
Joint Integrity
Active and passive thumb ROM should be assessed. Findings will be limited active CMC palmar abduction, opposition, or extension. The onset of pain will likely be at the end of the ROM. If there is paralysis caused by a median nerve injury, there will be no active thumb palmar abduction or opposition. Passive thumb abduction and opposition ROM may or may not be limited. Crepitus may be palpable during PROM in patients with DJD of the CMC of thumb.82 See the “Source of Signs and Symptoms” section for further details.
Muscle Length Tests
Tests of muscle length should be performed for the adductor pollicis and FPB (see Table 5-1). These tests should be performed passively with particular attention paid to the amount of resistance to passive stretch (stiffness) throughout the ROM during the test and to which joint moves most easily. The purpose of the test is to identify whether decreased muscle length is contributing to the limitation of the thumb abduction and/or opposition ROM. Differentiating whether the limitation of motion is due to the adductor pollicis muscle length versus joint structures may not be possible.
Other special tests.
Two special tests have been described to help determine if the source of the signs and symptoms is degeneration at the CMC joint of the thumb. The first test, Swanson’s crank and grind test,84 will be positive as articular degeneration advances, and pain, crepitus, or instability will be present.82 The second test, the shoulder sign,85 will also be positive.
Muscle Strength/Performance Impairments
Assessing muscle strength is important to determine whether the insufficient thumb abduction and/or opposition is caused by decreased muscle strength. A quick test of strength72 can be done by having the patient oppose the tip of the thumb to the tip of the small finger. If weakness of the thenar muscles is suspected, follow-up testing should be done using MMT. Three-point or lateral pinch strength can be assessed with a pinch gauge and compared to the uninvolved side. When performing these tests, the examiner should note the preferred pattern of movement and any impairments compared to normal. Impairments include limited ROM or an alteration in the sequencing and timing of joint movement. Patients with DJD of CMC of thumb may have decreased pinch strength with collapse of the first metacarpal and weakness of the OP, APL, and APB.
Palpation.
Tenderness of the CMC joint along the entire joint line is characteristic of patients that are having pain caused by DJD of the CMC of the thumb.82
Source of Signs and Symptoms
The clusters of impairments for each potential source or cause of insufficient thumb abduction and/or opposition follow.
Force Production Deficit
If the patient has insufficient thumb abduction and/or opposition because of a median nerve injury, the following signs may be seen:
Hypomobility
Contracture caused by thumb adductor muscles, CMC joint structures, or scar may have the following signs:
CMC subluxation and/or deformity (see Figure 5-9, B, and Figure 5-10, B):
Associated Signs or Contributing Factors
Patients with insufficient thumb abduction and/or opposition caused by contracture secondary to soft tissue injury will often present with associated edema and scarring of the hand. See the Chapter 5 Appendix for the complete listing of associated signs or contributing factors, differential diagnoses, and treatment for this syndrome, as well as Box 5-2 for tests and treatment used to manage edema and scar.
Case Presentation
Insufficient Thumb Abduction and/or Opposition Syndrome
Symptoms and History
Patient is a retired 60-year-old overweight female with a medical history of juvenile rheumatoid arthritis (JRA). She was referred to physical therapy 1 month after bilateral thumb CMC arthroplasties with carpal tunnel releases. Her past medical history includes attention deficit hyperactivity disorder (ADHD), multiple surgeries to her cervical (fusion) and lumbar spine, bilateral total knee arthroplasties, and vasculitic neuropathy. The patient had multiple deformities, especially in her hands, and atrophy of the muscles in all extremities, greater on the right side compared to the left.
The patient reported difficulty using her hands for daily activities and complained of clumsiness in her hands. She reported dropping things frequently. She also complained of decreased strength and the inability to use her hands functionally because of decreased thumb motion. She reported requiring assistance from her husband for opening jars and other functional activities. At the time of the initial visit, the patient did not report much pain in her hands.
Alignment Analysis
The patient had significant deformity of thumbs with prominence of the CMC joint and MP joint hyperextension. Both thumb CMC joints were adducted with atrophy of the thenar muscles.
Movement Analysis
The patient had insufficient thumb abduction and opposition for gripping objects such as a large coffee cup. Also noted was decreased thumb CMC abduction and extension resulting in compensatory excessive thumb MP and IP extension (they were in hyperextension) when trying to grasp objects, as well as occasional excessive wrist flexion during grasping activities.
Muscle Length and Strength Analysis
The patient had stiffness and shortness in the thumb CMC adductors and joint structures and excessive laxity of the volar plate at both MP and IP joints of the thumbs. Strength of specific muscles, grip, or pinch were not tested at the initial examination due to the recent thumb surgery. Generalized weakness of bilateral hands was noted when examining the patient performing functional activities.
Diagnosis
Insufficient thumb opposition and/or palmar abduction syndrome, Stage 2 for rehabilitation was assigned because the patient did not have any pain but was more limited in the functional use of her hands as a result of weakness and deformity.
Treatment
A static hand-based splint was fabricated for the patient for both hands to be used at night to attempt to increase thumb CMC abduction and opposition ROM without increasing MP and IP hyperextension. The patient was also instructed to use the splint when using her hands for most functional activities to protect the structures of the CMC joint from injurious stresses.
In the later stages of rehabilitation, attempts were made using resistive putty to strengthen her thumb MP and IP flexors without increasing the deformity. General grip strengthening was also added to her home exercise program.
Correcting postural habits
Patient education was provided that focused on extending the CMC joint and avoiding MP and IP extension during grasping activities throughout the day.
Outcome
The patient was seen for a total of 8 visits over 3 months for ROM, strengthening, and correction of movement impairments during functional activities. She was able to increase the functional use of her hands through gentle ROM and strengthening of hand muscles and mostly with patient education to decrease the stresses on the thumb CMC joints. She reported decreased frequency of dropping objects; however, she was still unable to perform activities, such as opening jars, that require more strength.
Thumb Carpometacarpal Accessory Hypermobility Syndrome
Patients with thumb CMC accessory hypermobility syndrome have pain at the CMC joint, but the alignment and movement impairments occur at all joints of the thumb. The CMC joint may be either extended/abducted or adducted/flexed. The impairments at the CMC joint are associated with either (1) MP flexion with IP extension or (2) MP hyperextension with IP flexion and result in loss of the normal longitudinal arch of the thumb. This movement pattern is due to an inability to coordinate the timing and sequencing of the movements between the IP, MP, and CMC joints of the thumb and adaptive changes in the tissues. Correction of the impairments during the secondary test decreases the symptoms. The adductor pollicis and FPB are frequently overused relative to the APL, APB, opponens pollicis, EPB, and FPL. Patients assigned to this diagnosis must have a modifiable movement pattern. This diagnosis is not intended for patients with neurological injury or later stages of arthritis.
Symptoms and History
Patients with thumb CMC accessory hypermobility syndrome may complain of pain in the area of the CMC joint of thumb that is exacerbated by pinching activities. They may also complain of weakness secondary to the pain that occurs with use of the thumb. Populations in which this is seen include patients who perform activities requiring repetitive pinch or gripping with the thumb adducted such as those who write by hand, hairdressers using scissors, and surgeons. Patients with this syndrome are often young with hypermobile joints or middle aged with early stages of DJD of the CMC of the thumb. DJD of the CMC of the thumb is more common in women than in men.7,87 Common referring diagnoses include thumb pain, wrist pain, DJD of CMC of the thumb (Eaton’s stages I or II82), thumb arthritis, and basal joint arthritis or pain. Others have classified and described thumb deformities and the progression through the stages of degeneration.6,88
Key Tests and Signs
Alignment Analysis
The impairments in alignment and appearance that have been observed for patients with this syndrome include a CMC joint resting alignment of: extension/abduction or adduction/flexion. The impairments at the CMC joint are associated with either (1) MP flexion with IP extension or (2) MP hyperextension with IP flexion.6,39-41
Movement Impairment Analysis
A common movement impairment noted in this syndrome is the inability to maintain the arc of pinch during functional activities that produces symptoms (see Figures 5-32, B to D; 5-34, B; 5-41 to 44; and 5-52). The CMC joint remains in an extended/abducted position with associated MP joint flexion and IP joint hyperextension (see Figure 5-32, D) or the CMC joint collapses into adduction/flexion with associated MP flexion with IP extension or MP hyperextension with IP flexion (see Figure 5-32, B). Correction of arc of pinch decreases or abolishes the symptoms at the CMC joint.
Two different preferred patterns of movement may be noted during active thumb extension: (1) the CMC joint extending relatively more (amount and timing) than the MP joint (boutonnière = MP flexion with IP extension)6 (see Figure 5-22, A and B), or (2) the MP joint extending relatively more than the CMC joint (swan neck = MP hyperextension with IP flexion)6 (see Figure 5-23). During active thumb flexion, the impaired patterns of movement include the CMC joint flexing more readily than the MP joint (see Figure 5-26), or the CMC remains in a relatively abducted and extended position while the MP joint flexes excessively and the IP joint remains extended or hyperextends (see Figure 5-27). During thumb palmar abduction, the MP joint abducts relatively more than the CMC joint. Correction of these movement impairments during the secondary test decreases or abolishes the symptoms at the CMC joint for the patient with thumb CMC accessory hypermobility syndrome. Correction of the alignment or movement pattern at the CMC joint may not be optimal without simultaneous correction at adjacent joints such as the MP and IP.
Joint Integrity
Range of motion/muscle length.
Although active and passive thumb ROM should be assessed, in this syndrome, limitation of ROM is generally not a problem. More commonly, excessive ROM is noted. However, if the ROM is limited, the limitation is slight. Active ROM is usually equal to PROM. During PROM, particular attention is paid to differences in stiffness compared to the opposite side. Thumb active and passive abduction14 and extension may be slightly limited and painful at CMC joint. The limitation in PROM indicates a relatively stiff or short adductor pollicis and/or FPB. In some cases, MP extension may be stiff or limited and IP extension excessive. In other cases, MP flexion may be stiff or limited and IP flexion excessive.
Joint Accessory Mobility
The CMC joint of the thumb may be hypermobile in a variety of directions but commonly in the dorsoradial direction.49
Other Special Tests
Swanson’s crank and grind test17,84 (Figure 5-64) involving compression of the CMC joint has been described to help determine if the source of the signs and symptoms is degeneration at the CMC joint of the thumb. Swanson’s test will be positive as articular degeneration advances, and pain, crepitus, or instability are present. However, in the early stages of DJD of the CMC joint of the thumb, as seen in thumb CMC accessory hypermobility syndrome, distraction instead of the compression and rotation of the MC on the trapezium may reproduce pain.82
Muscle Strength/Performance Impairments
The main impairment in muscle strength and performance in thumb CMC accessory hypermobility syndrome is insufficient muscle performance of the OP, APL, and APB relative to the adductor pollicis and the FPB. The first dorsal interosseous muscle may also help stabilize the base of the first metacarpal at the CMC joint when there is excessive motion of the base of the metacarpal dorsally and radially.49 Impairments in muscle performance may not be detectable on MMT but identified based on the functional pattern of use. Pinch strength may be decreased and painful.
Source of Signs and Symptoms
The structures of the CMC joint of the thumb are the source of the signs and symptoms for thumb CMC accessory hypermobility syndrome. The cluster of impairments identifying the CMC joint as the source are listed in the following.
CMC Joint
See the Chapter 5 Appendix for the complete listing of associated signs or contributing factors, differential diagnoses, and treatment for this syndrome.
Treatment
The primary focus of treatment is to educate the patient to maintain the arc of the thumb during active, functional, and resisted isometric thumb movements (see Figures 5-32, A; 5-34, A; 5-40; and 5-52, B). During therapy, the therapist must work with the patient correcting and practicing the movement pattern used during the functional activity that is causing the symptoms. The symptoms should not be reproduced with correct alignment and movement patterns.
In addition, specific exercises are prescribed to increase the performance (motor recruitment and strength) of the muscles required to correct the movement pattern (often the APB, APL, and OP). Others have recommended specific exercises with a focus on thumb abduction because abduction contributes to the stability of the CMC joint.7,88,89 However, in addition to strengthening of the abductors, we emphasize the precision of movement with the exercise. Working on thumb abduction simultaneously increases the extensibility (stretching) of the antagonistic muscle. The exercises are performed with particular attention to the relative amount and timing of movement between joints. For example, during abduction of the thumb, most of the motion should occur at the CMC joint with the MP and IP joints in a fairly neutral position. Resistive exercises are not performed until the patient is first able to move the thumb actively with the correct pattern of movement. As resistance is added, special care is taken to maintain the correct pattern of movement. The patient is instructed to take frequent breaks to stretch throughout the day to help increase the extensibility of stiff muscles, especially during the functional activity that is contributing to the impairment. The focus is on stretching the muscles that are used the most, usually the adductors and flexors. Stretching helps to relax the muscles in addition to increasing muscle extensibility.
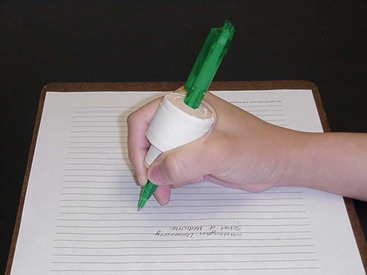
Modification of tools used at work or adaptive equipment is often helpful to facilitate use of the correct alignment and movement pattern17 (Figure 5-65).
Although not the mainstay of treatment, use of splinting or taping part of the time may be helpful for increasing the extensibility or length of tissues such as the adductor pollicis. See the Chapter 5 Appendix for the specific treatment for this syndrome.
Case Presentation
Thumb Metacarpophalangeal Flexion with Carpometacarpal Accessory Hypermobility Syndrome
Symptoms and History
A 50-year-old female violin teacher, who is right-hand dominant, presented to her initial physical therapy visit with bilateral thumb pain and a referring diagnosis of hyperflexible joints. She reported the symptoms had been present for the past 10 years. Previous treatment consisted of two types of neoprene splints. One splint had a strap holding the CMC in abduction and the other provided some support to the MP and wrapped around the hand. The patient’s goal was to play an orchestral concert and a “gig” on the same day without increasing her symptoms.
The location of symptoms was the MP joint area of bilateral thumbs. Her symptoms were aggravated by playing the piano, prolonged playing of the violin, and lifting. The initial onset of her symptoms followed lifting a container of hand bells. She had to discontinue playing the viola because of her thumb pain. The patient also reported that her thumb pain was aggravated by pulling files, twisting, lifting cases containing hand bells, typing, and playing the piano. The patient reported having obtained an ergonomic keyboard before the initial visit to physical therapy. At the time of the initial examination, she rated the intensity of her resting pain on a verbal numeric scale with 0 being no pain and 10 being severe pain, at 1/10 on the right and 0.5/10 on the left.
Alignment Analysis
Visual appraisal revealed no obvious swelling, scars, or discoloration of either thumb. Bilateral thumb resting alignment was CMC flexion/adduction (right > left), MP flexion, and IP extension (left > right) increased relative to normal. Bilateral ring finger alignment was increased flexion compared to normal. In general, her muscles were not bulky or well defined. There was no obvious atrophy (Figure 5-66).
Movement Analysis
Active ROM into flexion of the right thumb MP/IP was decreased slightly compared to the left (Figure 5-67).
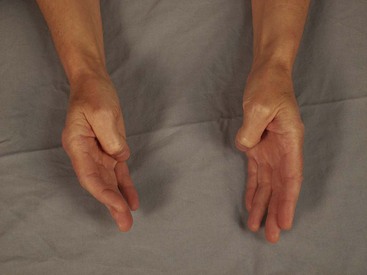
Figure 5-67 Active thumb flexion: Slight decreased range right thumb MP and IP joints compared to left.
During active thumb extension, the patient’s preferred pattern of movement was insufficient thumb MP extension and excessive IP extension. In addition, the CMC joint adducted during thumb extension (Figure 5-68). During functional activities, the thumbs assumed a supinated/adducted position rather than an abducted/pronated position. Modification of the preferred movement pattern by instructing the patient to maintain the arch of the thumb during functional use decreased her thumb symptoms.


Figure 5-68 Active thumb extension. A, Insufficient MP extension and excessive IP extension. B, CMC adduction.
When playing the violin, the patient’s preferred pattern of use was the right hand holding the bow with the thumb CMC adducted, the MP joint extended, and IP joint flexed instead of maintaining the arch of the thumb (Figure 5-69, A and C). Her left hand held the neck of the violin with slight pressure into thumb CMC adduction (Figure 5-69, D). In addition, when playing the violin, the left scapula anteriorly tilted and abducted more than the right scapula (Figure 5-69, E and F).








Figure 5-69 Preferred alignment and movement pattern. A, Anterior view of decreased arch of right thumb holding bow. B, Anterior view of corrected alignment of right thumb holding bow. C, Anterolateral view of decreased arch of right thumb holding bow. D, Left thumb CMC adduction during holding neck of violin. E, Posterolateral view of left scapular anterior tilt and abduction. F, Posterior view of left scapular anterior tilt and abduction. G, Posterolateral view of corrected scapular alignment. H, Posterior view of corrected scapular alignment.
With ligament integrity testing, there was a firm end-feel but increased laxity of the collateral ligaments of the thumb MP joint with symptoms reproduced with stress to the ulnar collateral ligament.
Muscle Length and Strength Analysis
MMT was performed as described by Kendall et al.13 Findings were as follows:
The finger flexors and extensors and the thumb MP flexors were relatively stiffer than the patient’s other muscles as determined during the length tests. No muscle shortness was found except possibly the finger extensors (ED). As the thumb was passively extended during the length test of the thumb flexors, stiffness was felt throughout the range and wrist RD occurred more readily than thumb extension, indicating possible increased stiffness of the FPB.
Initial Disabilities of the Arm, Shoulder, and Head (DASH) score: 17.24% overall, 18.75% on work, and 0% performing arts for violin.
Diagnosis
The movement system diagnosis was thumb MP flexion with CMC accessory hypermobility syndrome, Stage 2.
Treatment
The primary focus of the treatment was correction of the patient’s alignment and movement impairments. The initial treatment included patient education, splinting, and exercises. The patient was educated to maintain the arch of the thumb during functional use (e.g., typing, writing, and playing the violin (Figure 5-69, B). She was also educated about correct scapulae alignment while playing the violin (Figure 5-69, G and H).
Hand-based, custom-made static thumb splints designed to stabilize the thumb MP joints in extension and prevent UD or RD of the MP joints were fabricated (Figure 5-70). The purpose of the splints was to provide added stability to the thumb MP joint during functional use, including playing the violin. Other splint options were discussed with the patient such as silver ring or a more supportive thermoplastic thumb splint immobilizing the CMC and MP joints. The patient was not interested in other splint options. On the patient’s last visit, the patient requested neoprene splints, in addition to the thermoplastic splints, because of the possible impact of the thermoplastic splints on her violin while playing. After discussing various splint options, the patient chose the Comfort Cool thumb CMC restriction splint (North Coast Medical, Inc., Morgan Hill, Calif.) (Figure 5-71).


Figure 5-70 Hand-based, custom-made thumb splints designed to stabilize the thumb MP joints in more extension and prevent ulnar or radial deviation of the MP joints. A, Lateral view. B, Anterior view.
In addition to patient education and splinting, the patient was instructed in home exercises for improving the performance of the EPB, opponens, and APB. During the exercise for the EPB, the patient was instructed to focus on moving at the MP joint instead of the IP joint and to avoid thumb CMC adduction during active thumb extension (avoiding overuse of EPL). When exercising the opponens and the APB, the patient was educated to focus on moving at the CMC joint instead of the MP joint of the thumb during active opposition and abduction. The patient used the lid of a jar as a guide for proper movement into thumb opposition. Once the patient was able to perform the exercise actively with the correct movement pattern, the exercise was progressed by adding rubber band resistance.
Outcome
The patient was seen for a total of 4 visits over a 7-week period. At the last visit, the patient reported that she was playing her violin for 45 minutes at a time and wearing the Comfort Cool splints most of the time to control her symptoms. Playing the viola continued to aggravate her symptoms.
Final DASH score: 13.79% overall, 0% work, and performing arts (violin) modules.
Overall, the patient reported being very pleased with her outcomes from physical therapy. She reported an overall 75% improvement in her symptoms when using the splints, which she was doing most of the time. She also reported being pain-free most of the time, as long as she complied with correcting her movement impairments during functional activities such as while playing her instruments. After several months of using the thermoplastic and neoprene splints, the patient decided to be measured for thumb silver ring splints. She has continued performing the exercises prescribed in physical therapy and uses the thumb splints regularly. She reports no longer having thumb pain.
Finger (or Thumb) Flexion Syndrome
The movement system syndrome finger (or thumb) flexion is a preferred pattern of movement in which the normal alignment of the finger is not maintained during finger flexion. This includes one or more of the following: the longitudinal arch, neutral rotation, or neutral abduction/adduction of the finger (see Figures 5-36 to 5-39, 5-41, 5-42, and 5-46). The movement impairment occurs during the pain-provoking functional or occupational activity involving grip or resisted isometric finger flexion. The movement pattern may be due to an inability to coordinate the timing and sequencing of the movements, an alteration of the relative amount of motion between the IP and MP joints of the finger, or overuse during a repetitive activity. Finger MP or PIP joint pain associated with rotation is due to insufficient performance of one interossei muscle and overuse of the antagonistic interossei muscle at the same joint.90 The overused muscle is relatively stiffer than its antagonist. This results in the principal impairment of rotation at the painful joint and results from a repetitive activity. Finger AROM and strength are usually normal. Correction of the movement impairments does not always immediately modify symptoms but instead symptoms modify over time. Patients assigned to this diagnosis must have a modifiable movement pattern. This diagnosis is not intended for patients with neurological injury or later stages of arthritis. This syndrome can be associated with a scapular movement syndrome, but the symptoms are not referred from the shoulder or neck structures. Restoration of normal scapular alignment is believed to provide proximal stability, allowing distal segments to work optimally by decreasing excessive stresses on distal tissues.
Finger (or Thumb) Flexion Syndrome with Rotation
Symptoms and History
Patients with finger (or thumb) flexion syndrome with rotation may have a history of repetitive activity involving use of the finger intrinsic muscles. They may complain of pain at the MP or PIP joints of the finger. This has been observed most commonly in the index and small fingers.
Patients with finger (or thumb) flexion syndrome with rotation may report performance of repetitive activities such as typing on a computer, carrying a bag by the handle with the finger in UD, grasping a golf club, cutting hair (hairdresser), and playing a musical instrument.
Finger MP or PIP joint pain is a common referring diagnosis for patients with finger flexion syndrome with rotation.
Key Tests and Signs
Alignment/Appearance Analysis
The key impairment in alignment/appearance is a relative increase in the amount of rotation (supination or pronation) of the joint compared to the same finger or another uninvolved finger on the uninvolved side (see Figure 5-7).
Movement Impairment Analysis
The key movement impairment is noted during the pain-provoking functional or occupational activities involving grip or resisted isometric finger flexion and the patient does not maintain the finger in neutral rotation and in the normal longitudinal arc. Correction of the rotation and restoration of the normal longitudinal arc of the finger decreases or abolishes the symptoms. Three different impairments may be noted, as follows:
Ligament Integrity
Patients with finger (or thumb) flexion syndrome with rotation may have laxity of the collateral ligament on one side of the joint compared to the same finger on the uninvolved side (see Table 5-1).
Muscle Length Tests
The length of the interossei, extrinsic finger flexors, and extensors should be assessed. Table 5-1 lists the specific procedures for these length tests. Findings on the interossei muscle length test include shortness or relative increased stiffness of the interossei on one side of the involved finger and a long or relatively less stiff interossei on the opposite side of the involved finger. Stretch of the overused interossei may produce or aggravate symptoms.
Muscle Strength/Performance Impairments
Resisted tests for soft tissue differential diagnosis should be performed on the contractile structures in the symptomatic area. Contraction of the overused interossei may produce or aggravate symptoms (painful and weak or strong and painful). Pinch strength may be normal, but the movement impairments noted in the section on movement impairments previously may be evident during the test.
MMT of the extrinsic finger flexors, extensors, and interossei should also be performed. Often, no weakness will be detected with MMT. The relative performance between muscle groups is usually the impairment versus weakness detected on MMT. Findings from MMT of the interossei are relative strength or recruitment differences (timing and amount) for the interossei on opposite sides of involved finger. The ED, FDS, and FDP are usually strong but may be recruited relatively less than the interossei (depending on the pattern of impaired movement) as determined by the preferred pattern of movement used during the test.
Source of Signs and Symptoms
The source of the symptoms in finger flexion syndrome with rotation is usually the joint structures of the symptomatic joint, but the overused contractile tissues directly affecting the alignment and movement of that joint, such as the interossei, may also be a source of symptoms, as well as a source of the signs.
Case Presentation
Finger Flexion with Rotation Syndrome, Wrist Flexion Syndrome, and Scapular Depression
History and Symptoms
A 13-year-old female reported left wrist pain that started after increasing practice time on her cello for an audition. She reported that she was right-hand dominant and a serious cellist with auditions to join junior orchestras in the near future. Her symptoms started a few months before her initial physical therapy evaluation. She had seen an occupational therapist for this problem previously, but the progress had plateaued so she was referred to a therapist trained to treat musicians. The patient reported practicing at least 4 hours per day, but she experienced pain during practice, which required taking breaks from playing. The diagnosis provided by an orthopedic surgeon was flexor tendonitis.
The patient reported pain in the area of the left anterior wrist crease only when playing her cello. The production of the pain depended on the position of her wrist and hand when reaching for different notes, and the patient reported that the pain persisted after playing, depending on the number of hours spent practicing.
Alignment Analysis
The patient is a very slender, thin (including her fingers) teenager with little muscle definition. Her preferred sitting alignment when not playing the cello is extreme lumbar and thoracic flexion.
Movement Impairment Analysis
The principal movement impairments noted with her preferred pattern of playing the cello included the following:
Muscle Length and Strength Analysis
Muscle strength
| Muscle | Result |
|---|---|
| Interossei | 4/5 |
| FDS and FDP | 5/5 |
| EDC, ECRL, and ECRB | 5/5 |
| FCU and FCR | 5/5 (Patient reported resistance to these muscles would have been painful previously.) |
| Trapezii: Middle and lower | 3/5 |
Diagnosis
Stage 3 for rehabilitation was assigned because the patient had symptoms only with playing the cello and not with functional activities. Her symptoms increased with increased practice time on the cello.
Treatment
The primary focus of treatment was the redistribution of motion during function (playing the cello) by minimizing the amount of wrist flexion, UD, and finger abduction by increasing the movement of the hand up or down the neck of the cello and moving more at the elbow and shoulder. To achieve this correction, a cue was given to decrease wrist flexion by abducting the glenohumeral joint, which resulted in an immediate decrease in pain. In addition, the therapist worked with the patient to maintain the longitudinal arch of the finger and neutral rotation while maintaining correct scapular alignment. Strategies for treatment included correcting proximal impairments to facilitate better distal function and correcting distal impairments. Correcting the proximal impairments included patient education regarding avoiding scapular depression and abduction during playing the cello and exercises for the trapezius.
Exercises to improve the performance of the trapezius were as follows:
Exercises to correct distal impairments were as follows:
Finger (or Thumb) Flexion Syndrome without Rotation
Symptoms and History
Patients with finger flexion syndrome without rotation may report symptoms that are poorly localized in the hand, wrist, or forearm. Patients also may report symptoms while performing repetitive activities such as playing string instruments or the piano, writing, or any kind of grip or pinch activity.
Key Tests and Signs
Alignment Analysis
The patient with finger flexion syndrome without rotation may have impairments with use of the finger, but the resting finger alignment is often normal. However, associated impairments in scapular alignment may be noted such as scapular depression, abduction, anterior tilt, internal rotation, or downward rotation.
Movement Impairment
The key movement impairment is noted during the pain-provoking functional or occupational activity involving grip or resisted isometric finger flexion, and the patient does not maintain the normal longitudinal arc of finger, transverse arch of hand, and scapular alignment. Correction by restoration of the normal longitudinal arc of the finger and scapular alignment decreases symptoms over time. Movement impairments of the scapula include depression, abduction, internal rotation, downward rotation, or tilt. Restoration of normal scapular alignment is believed to provide proximal stability, allowing the distal segments to work optimally by decreasing excessive stresses on distal tissues.42
In addition to the scapular impairments, the following three different finger movement impairments may be noted:
Ligament Integrity
Patients with finger flexion syndrome without rotation that have a boutonnière type pattern of movement may have shortness of the ORL or laxity of the PIP or DIP volar plates, so the length of these structures should be assessed (see Table 5-1).
Muscle Length Tests
The length of the interossei, extrinsic finger flexors, and extensors should be assessed. Table 5-1 has the specific procedures for these length tests. Muscle length may be normal, but the muscle may be relatively stiffer than on the unaffected side.
Muscle Strength/Performance Impairments
Pinch strength should be assessed and may be normal, but the impairments noted in the section on movement impairments may be evident during the test. MMT of the extrinsic finger flexors, extensors, and interossei should be performed. However, often no weakness is detected. The relative recruitment (timing and amount) between muscle groups is usually the impairment rather than weakness detected on a MMT.
Source of Signs and Symptoms
The source of the symptoms is usually the joint and soft tissue structures of the symptomatic region. However, it is often difficult to reproduce the symptoms with any test during the examination. The impaired pattern of movement is believed to contribute to increased stresses on the tissues in the symptomatic area and correction of the pattern of movement decreases these stresses, thereby reducing the symptoms over time. See the Chapter 5 Appendix for the complete listing of associated signs or contributing factors, differential diagnoses, and treatment for this syndrome.
Treatment
The primary focus of treatment is to educate the patient to maintain the arc and neutral rotation of the fingers during functional activities and active and resisted isometric finger movements. The therapist must work with the patient during the therapy visits on correcting and practicing the movement pattern during the functional activity that is causing the problem. The symptoms should not be reproduced with correct alignment and movement patterns.
In addition, specific exercises are prescribed to increase the performance (motor recruitment and strength) of the muscles required to correct the movement pattern. Thus the extensibility of the antagonistic muscle is simultaneously increased (stretched). The exercises are performed with particular attention paid to the relative amount and timing of movement between joints. Resistive exercises are not performed until the patient is first able to move the fingers actively with the correct pattern of movement. As resistance is added, special care is taken to maintain the correct pattern of movement. The patient is instructed to take frequent breaks to stretch throughout the day to help increase the extensibility of stiff muscles, especially during the functional activity that is contributing to the impairment. The focus on stretching is on the muscles that are used the most. Besides increasing extensibility, stretching helps with relaxation of the muscle.
Modification of tools used at work, musical instruments, or adaptive equipment is often helpful to facilitate use of the correct alignment and movement pattern.
Although not the mainstay of treatment, use of splinting or taping part of the time may be helpful for increasing extensibility or length of tissues and facilitating recruitment of underused tissues. See the Chapter 5 Appendix for specific treatment for this syndrome.
Case Presentation
Finger Flexion without Rotation Syndrome with a Secondary Diagnosis of Scapular Depression and Shoulder Medial Rotation
History and Symptoms
The patient is a 17-year-old female high school student who plays the bassoon (primarily), violin, and trombone, and loves drawing, writing, and typing. She plays in the youth symphony, and also reports working occasionally on ceramics. She has no history of other medical or musculoskeletal problems. At the time of the initial physical therapy examination, the patient was on summer break so she had not practiced or typed as much as during the school year. Initial movement system examination occurred 6 months after onset of symptoms.
The patient reported generalized bilateral dorsal and volar wrist and hand pain (right more than left). She also reported occasional pain in her right elbow antecubital crease area and upper back pain. She reported her pain was aggravated with playing the bassoon and typing for school but did subside within a few minutes after cessation of those activities. The quality of the pain was described as aching. She reported no problems with sleeping and stated she awakened without any symptoms.
Alignment Analysis
Standing
Movement Analysis
Cervical ROM was normal without symptom reproduction. Shoulder ROM was also normal but movement impairments of insufficient scapular elevation, downward rotation, and slight scapular abduction bilaterally were noted. Arm elevation did not reproduce the patient’s symptoms at the time of the initial physical therapy examination.
Rocking back had noted movement impairments of cervical extension with insufficient elevation of scapulae. While playing the bassoon, the preferred pattern of playing was with the wrist flexed and the ring and small fingers in the intrinsic plus position (MP flexion with IPs extended). When instructions were provided to correct the movement impairments, the patient’s fingers assumed the “boutonnière” position (PIP flexion with DIP hyperextension). The scapulae were depressed while playing.
Muscle Length and Strength Analysis
| Shoulder | Right | Left |
|---|---|---|
| Lateral rotation | 3/5 | 3+/5 |
| Medial rotation | 3/5 | 3+/5 |
| Middle and lower trapezii | 3/5 | 3+/5 |
Movement impairments noted during the MMT of the trapezii included humeral medial rotation, scapular depression, and anterior tilt.
MMT of the wrist and hand did not reproduce the patient’s symptoms. The right hand was generally weaker than left by one muscle grade. The long finger flexors (FDP and FDS) of the right index and middle fingers were stronger than the long finger flexors of the ring and small fingers.
Scapular depression, shoulder medial rotation, wrist flexion, finger flexion without rotation syndrome.
Exercises were provided to correct the movement impairments noted during the movement system examination. The patient was instructed to do the following:
Source or Regional Impairment of the Hand
Patients in the regional impairment of the hand category usually have a history of acute trauma or injury to the hand or the patient is in the early postoperative phase. When known, the pathoanatomical or source diagnosis assigned by the physician, followed by the name of the operative procedure provided on the referral, is used as the diagnosis that will guide the physical therapy treatment. For example, flexor tendon laceration, flexor tendon repair, Stage 1. If the referral does not state the pathoanatomical or source diagnosis or the procedure that was performed by the physician, the regional diagnosis, hand impairment, will be used.
The focus of treatment is protecting the injured tissues. Usually, there is a history of acute trauma or injury to the hand or it is early in the postoperative phase. Medical precautions have often been issued. Because of the acuity of the condition, the patient’s typical movement pattern cannot be assessed at this time. The prognosis of tissue healing and normal movement is expected. The determination of the use of component versus compensatory treatment methods depends on the expectations of the final outcome. Initially, while precautions are required, compensatory methods may be necessary. The guidelines provided in the Chapter 5 Appendix are intended to be general, therefore the consulting physician’s protocols for specific precautions and progressions are necessary. Appropriate application of the protocols, however, requires that the therapist be familiar with the tissues that are affected by the surgical procedure, the specific surgical approach, and the variables that need to be considered while applying stresses to the healing tissues. This knowledge, as well as communication with the physician, allows the therapist to make appropriate adjustments in the protocol as needed.
See the source or regional impairment of the hand diagnosis in the Chapter 5 Appendix and Box 5-3 for more specific information regarding common referring diagnoses, examination, and general treatment guidelines for this diagnosis. Underlying movement system syndromes that should be considered are insufficient finger or thumb flexion, insufficient finger or thumb extension, insufficient thumb abduction and/or opposition, thumb CMC accessory hypermobility, or finger (or thumb) flexion syndrome with or without rotation.
BOX 5-3 General Treatment Guidelines
Patient Education
Pain
Scar
Range of Motion
Strength
Function
Using the hand in functional activities throughout the course of treatment is critical. The ideal pattern of movement should be encouraged as the patient is able. Examples of functional activities include writing, driving, work, eating, sleeping, and hygiene.
Tissue Factors
Bone
Nerve
Tendon
Guidelines for Treatment of Hypersensitivity
Desensitization
AAROM, Active assistive range of motion; AROM, active range of motion; IP, interphalangeal; MP, metacarpophalangeal; PROM, passive range of motion.
Movement System Diagnoses for the Wrist
To date, movement system diagnoses for the wrist have not been described in the detail presented here for the hand. However, suggested names for wrist diagnoses would follow the principles for naming the diagnoses in other regions. Suggested names are wrist flexion, wrist extension, a combination of wrist flexion or extension with RD or UD, wrist hypomobility, and wrist accessory hypermobility. For example, a patient with CTS who has symptoms that are provoked by repeated activity performed with the wrist in flexion might be assigned the diagnosis of wrist flexion syndrome.
Conclusion
Effective physical therapy treatment of hand dysfunction requires managing the acute tissue injury as well as the underlying movement impairments. In this chapter, we have described movement system diagnoses for hand dysfunctions in detail, and we have proposed the names for some movement system diagnoses for the wrist. These diagnoses need further testing in the clinic and by well-designed studies.