Chapter 5 Movement System Syndromes of the Hand and Wrist
Introduction
Hand dysfunctions may be caused by an acute injury or injury as a result of prolonged or repetitive activities. Effective treatment requires managing the acute tissue injury as well as the underlying movement impairments. Based on years of clinical observations, we have classified the patterns of movement deviations associated with hand dysfunctions. The classifications are labeled as movement system syndromes (Box 5-1). This chapter describes two categories of movement system syndromes: (1) those based on the source or region of the injury, and (2) those based on the principal movement system impairment.
BOX 5-1 Movement System Syndromes of the Hand
Conditions that may fall under the regional impairment diagnosis of the hand when the pathoanatomical source diagnosis is not provided on the referral documentation are as follows:
Injuries
Postoperative
A diagnosis based on the source or pathoanatomy is most commonly used for acute hand dysfunction and is often provided in the referral documentation. In these cases, a complete movement system examination is not possible. The source diagnosis guides physical therapy treatment based on established protocols. These protocols are based on stages of tissue healing because they identify the source (pathoanatomical tissue) that is affected and the degree of the injury.1 A regional diagnosis, hand impairment is used when the referral documentation does not state the pathoanatomical or source diagnosis for an acute injury (see Box 5-1). After resolution of this early or severe stage of tissue injury, a complete movement system examination should be performed to establish a diagnosis of the principal movement impairment.
A diagnosis based on the principal movement system impairment should also be used for hand dysfunction caused by prolonged or repetitive activities. These types of slowly developing conditions do not have a protocol for treatment or even an established standardized examination, particularly one that assesses movement. The repetitive movements that induce the pain conditions result in slight deviations from precise movement and thus an examination to assess movement characteristics is essential.2
In addition to the movement system impairment, or source or regional diagnosis (see Box 5-1), assignment of a stage helps guide the development of the treatment plan. The staging system is described in Chapter 2.
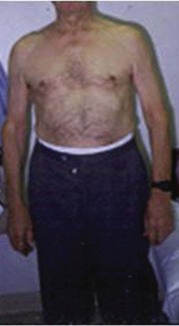
Movement system impairments are influenced by a variety of factors, including age, structural variations, and body type. For example, a patient who is obese may have a resting alignment of shoulder abduction. This shoulder alignment results in increased wrist ulnar deviation (UD) when typing on a keyboard. Repetitive wrist ulnar and radial deviation may cause tissue injury at the wrist such as is found in de Quervain’s disease. Another example of the influence of structural variation is the musician whose anthropometrics may influence choices made regarding an instrument. A musician with short arms and fingers may compensate by using a slightly different movement pattern compared to a musician with longer extremities playing the same instrument.
For any of the movement system syndromes, the most important movement pattern to address in treatment may be the result of either hypomobility (physiological and accessory motion), hypermobility (excessive motion), force production deficit (decreased strength), or movement pattern coordination deficit (impaired motor control: timing, magnitude, or duration).3
The movement system syndromes of insufficient finger or thumb flexion, insufficient finger or thumb extension, and insufficient thumb abduction and/or opposition are used to teach the principles of examination and treatment of the hand to physical therapy students and therapists who have not specialized in hand therapy. The content within these three syndromes is not new to the experienced hand therapist, but it is organized in a unique way to facilitate teaching therapists who do not specialize in the hand how to determine the cause of the dysfunction (referred to as the source of signs and symptoms in the Chapter 5 Appendix). A major objective of the systematic examination of the hand for these syndromes is to identify the cause of the dysfunction instead of only identifying isolated impairments, such as decreased active range of motion (AROM). For example, for the movement system syndrome, insufficient finger or thumb flexion, there are several potential causes of the limitation of movement, including flexor or extensor tendon adhesion (hypomobility), extensor muscle shortness (hypomobility), weakness or rupture of the finger flexors (force production deficit), shortened ligaments (hypomobility), and so on. Treatment should address the cause of dysfunction instead of the isolated impairments. If treatment is based on goniometric measurement of AROM without taking into account the cause of the limitation, the treatment may not be the most effective or efficient.
The movement system syndromes, thumb carpometacarpal (CMC) accessory hypermobility and finger flexion with and without rotation, are unique and have not been previously described this way. CMC accessory hypermobility syndrome is based on information available in the literature, as well as clinical experience observing and treating the movement impairments associated with thumb pain. Young patients with hypermobile joints and patients with early osteoarthritis (OA) or degenerative joint disease (DJD) of the CMC of the thumb are often assigned this syndrome.
Knowledge of normal alignment, movement, and muscle function guides the therapist in identifying alignment and movement impairments and prescribing treatment to correct those impairments. Unique to the movement system examination of the hand is the emphasis on first evaluating the patient’s preferred pattern of movement and correlating this with the onset of symptoms (referred to as the primary test). The examiner focuses on identifying the joint that is relatively most flexible and is the cause of the patient’s chief complaint. The primary test is immediately followed by a secondary test in which the symptom-provoking preferred pattern of movement is modified to determine the effect on the symptoms. This sequence of testing is performed throughout the examination, as well as during the observation of functional activities. Identifying and modifying the functional activities is a critical aspect in the physical therapy management of the patient’s pain.
Key elements in the examination and treatment of the hand for all diagnostic groups presented in this chapter that may be unique are as follows:
Symptoms in the hand may be referred from the neck, thoracic outlet,5 elbow, forearm, or wrist.9-11 Therefore the examination of the hand should include differentiating whether the source of the symptoms is from the hand or referred from one of these regions.
Edema and scar are impairments that may exist in any of the syndromes and must be addressed for treatment to be effective, but identification of the edema and scar is not critical for assigning the movement system diagnosis.
Examination and Key Tests
Subjective Examination
During the history, particular attention is paid to questioning the patient regarding the daily activities that are performed repeatedly and which of those are associated with increasing and decreasing the symptoms.
Objective Examination
Synthesize the findings from the movement testing (AROM, PROM, and resistive tests) to determine the reason for the loss of motion (source of signs). For example, insufficient finger flexion may be because of the following:
See the description of the movement system syndromes in the Chapter 5 Appendix for specific test findings.
Alignment of the Hand and Wrist
Prolonged postures or repeated movements performed by the patient result in adaptations in the tissues (tissue impairments). These tissue impairments (i.e., short, stiff, long, overused, or weak muscles) result in imprecise movement patterns that eventually result in tissue injury.2 The identification of impairments in alignment provides insight into possible existing impairments in the tissues that will be verified later in the examination.
Normal Standing Alignment
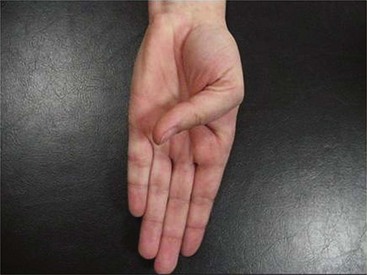
Normal alignment gives an indication of the preferred patterns of muscle use and resting muscle lengths. Normal alignment of the hand at rest includes the following:


Figure 5-4 A, Normal resting alignment of wrist in slight extension, front view. B, Normal resting alignment of wrist in slight ulnar deviation, side view.
Examining the alignment of the forearm, elbow, and shoulder girdle is an important component of evaluation of hand dysfunction. Visual appraisal of muscle and tendon development should also be examined when assessing alignment. Muscles should be equally defined between muscles on the same side or symmetrical when compared to the same muscle on the opposite side.
Impaired Alignment
Impaired alignment provides important clues regarding the source of the signs or symptoms and indicates the preferred patterns of muscle use and resting muscle stiffness or lengths. However, assessment of alignment is only the first step in the objective examination and any clues obtained need to be confirmed via the rest of the tests.
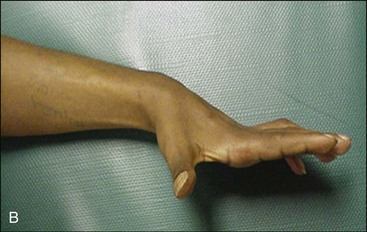
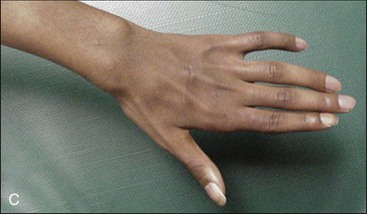
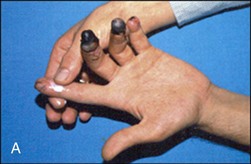
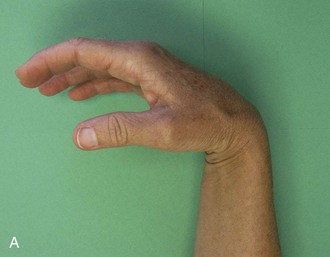
Impaired alignment of the hand includes clawing (Figure 5-6), stiff hand position (wrist flexion, finger MP extension, IP flexion, and thumb adduction); rotation of the fingers (Figure 5-7); boutonnière (Figure 5-8) or swan neck alignment of the thumb or fingers (Figure 5-9); mallet, radial deviation (RD), or UD of the IP joints of the fingers or thumb (Figure 5-10); flexion of the DIP joints of the fingers (Figure 5-11); deviations in the longitudinal arch of increased flexion (Figure 5-12) or extension (Figure 5-13) as a whole or at individual joints (arch no longer smooth); deviations of the transverse arch (increased or decreased) (see Figure 5-13, B); increased UD of the MP joints (see Figure 5-8, C); and adduction and/or flexion (Figure 5-14; see Figure 5-10, B) or abduction of the CMC joint of the thumb.24

Figure 5-7 Impaired alignment: Rotation (supination) of MP joints of index fingers right greater than left.


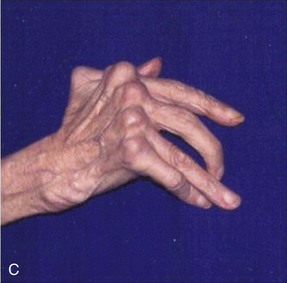
Figure 5-8 A, Classic boutonnière posture of proximal interphalangeal (PIP) joint flexion and distal interphalangeal (DIP) joint hyperextension. B, Impaired alignment: Tendency toward boutonnière of thumb (MP flexion with IP extension). C, Impaired alignment: Subluxation and ulnar deviation of MP joints and intrinsic plus (increased flexion of MP joints and extension of IP joints); boutonnière of thumb (MP flexion with IP extension).
(A, From DeLee JC, Drez D, Miller MD: DeLee and Drez’s orthopaedic sports medicine, Philadelphia, 2010, Saunders.)




Figure 5-9 A, Impaired alignment: Swan neck (PIP hyperextension with MP and DIP flexion) of fingers. B, Impaired alignment: Swan neck of thumbs left greater than right.


Figure 5-10 A, Impaired alignment: Radial deviation of IP of thumb and adduction of CMC of thumb early stages of degeneration. B, Impaired alignment: Radial deviation of IP of thumb and adduction of CMC of thumb late stages of degeneration.


Figure 5-13 A, Impaired alignment: Alteration of longitudinal arch of fingers of decreased flexion (left elbow injury). B, Impaired alignment: Alteration of longitudinal arch of fingers of decreased flexion and decreased transverse arch (ulnar nerve injury).
Many of these impaired alignments are classically thought of as a result of an acute injury or a chronic disease process. Some impaired alignments may be due to prolonged position of immobilization required for tissue healing after an injury or surgery. However, people that have not had an injury or a chronic disease may have a mild version of these impairments in alignment. These may be due to genetics, as well as the repeated movement patterns used during daily activities. Theoretically, modification of these impaired alignments may help to prevent tissue injury or alleviate pain in the presence of tissue injury.
Clawing, a resting position of flexion of the IP joints of the fingers with MP joint hyperextension (see Figure 5-6, B and C), is classically a sign of ulnar or combined ulnar and median nerve injury and is due to loss of function of the interossei and lumbricals (intrinsics). Insufficient function of the intrinsics results in an imbalance at the MP joint where the extensors (extensor digitorum [ED]) predominate over the flexors (intrinsics, flexor digitorum profundus [FDP], and flexor digitorum superficialis [FDS]) because the intrinsics are no longer functioning. The predominance of the ED at the MP joint results in increased passive tension on the FDP further contributing to the flexion of the IP joints. Clawing also results in flattening of the transverse arches of the hand. Ulnar nerve injury affects the hypothenar muscles and median nerve injury the thenar muscles, contributing to the flattening of the transverse arches.25,26 The static alignment of the posttraumatic stiff hand is similar to the claw hand position: wrist flexion, finger MP extension, IP flexion, and thumb adduction.24
A classic boutonnière deformity (see Figure 5-8, A), PIP flexion with DIP hyperextension, is a sign of injury to the central slip of the extensor mechanism. With rupture to the central slip, the extensor mechanism retracts increasing the tension on the terminal tendon, thus contributing to hyperextension of the DIP joint. Over time, the lateral bands migrate anteriorly and thus become PIP joint flexors instead of extensors. However, this same alignment can be seen with a PIP flexion contracture without injury to the extensors (pseudoboutonnière). Prolonged positioning in this alignment may also result in shortening of the oblique retinacular ligament. Shortness of the ORL then contributes further to the deformity.27-29
A swan neck deformity (see Figure 5-9, A) is described as PIP hyperextension with MP and DIP flexion. This can be due to anything that increases tension on the central slip of the extensor mechanism (ED, intrinsics) but most often may be caused by shortness or increased activity of the finger intrinsics. A prerequisite for the PIP hyperextension to occur is laxity of the volar plate at the PIP joint. As the PIP hyperextends, the lateral bands migrate farther from the axis of rotation in a posterior direction, increasing their efficiency as PIP extensors. PIP hyperextension places increased passive tension on the FDP resulting in DIP flexion. A nonfunctional FDS may also contribute to PIP hyperextension. A swan neck deformity may also result secondary to a mallet finger injury. When the terminal tendon of the extensor mechanism is ruptured in a mallet finger injury, the extensor mechanism retracts, increasing the tension on the central slip that is still attached. This results in PIP hyperextension if the PIP volar plate is lax.30-33
RD or UD of the IP joints of the fingers or thumb (see Figure 5-10) is usually either an indication of an injury to the collateral ligaments or of degeneration as a result of OA.17,34,35 Abnormal UD of the MP joints of the fingers is usually an indicator of inflammatory arthritis (e.g., rheumatoid or lupus). As the fingers deviate, muscle function changes. With UD of the fingers at the MP joints, the FDP and FDS may become ulnar deviators of the joint if the pulleys no longer hold the tendons centrally on the bone.36-38 Likewise, the ED may become a deviator of the joint if it slips in a radial or ulnar direction off the head of the metacarpal.
UD of the MP joints of the fingers (see Figure 5-8, C) may be suggestive of inflammatory arthritis. However, some people that have laxity of the joints and little muscle stiffness may also have increased UD of the MP joints21 that is associated with their symptoms and can be modified with patient education.
Flexion of the DIP joints of the fingers is usually either an indicator of a mallet finger injury or the result of OA of the DIP joints (see Figure 5-11).17
Adduction (see Figure 5-10, B) or abduction of the CMC joint of the thumb is usually associated with degeneration of the CMC joint of the thumb. Adduction of the CMC is usually associated with flexion26 and may indicate shortness or relative stiffness of the adductor pollicis and the flexor pollicis brevis (FPB) and insufficient function or excessive length of the abductor pollicis longus (APL), abductor pollicis brevis (APB), opponens pollicis (OP), and first dorsal interossei (DI) muscles. Abduction of the CMC indicates shortness, relative stiffness, or excessive recruitment of the APL, and if associated with MP flexion, shortness or stiffness of the FPB, and lengthened or insufficient recruitment of the extensor pollicis brevis (EPB). The adducted or abducted positions of the CMC joint of the thumb are also associated with compensatory impairments in alignment of the MP39 and IP joints of the thumb, either a boutonnière (MP flexion with IP hyperextension) (Figure 5-8, B and C) or swan neck (MP hyperextension with IP flexion) deformity (see Figure 5-9, B).6,40,41
Rotation of the fingers at the MP or PIP joints (see Figure 5-7), deviations in the longitudinal arch of increased flexion (see Figure 5-12) or extension (see Figure 5-13, A and B) as a whole or at individual joints (arch no longer smooth), or deviations of the transverse arch (increased or decreased) may indicate an imbalance of the muscular forces on opposing sides of the joints (in the absence of a structural change or nerve injury from trauma). Rotation may be the result of overuse or increased stiffness of the interossei on one side of the finger and underuse or use in a lengthened position of the interossei on the opposite side of the finger. The FDP, FDS, and ED may be underused and the intrinsics overused (intrinsic plus position of MP flexion and IP extension). Alteration of the longitudinal arch of increased finger MP flexion and decreased IP flexion may be the result of overuse of the finger intrinsics and underuse of the FDP, FDS, and ED (see Figure 5-9, A2). Clawing, boutonnière, swan neck, and mallet are all disruptions in the longitudinal arch. These are usually attributed to a nerve injury or injury to the extensor mechanism. However, when similar alignments are identified in the absence of a specific nerve or extensor mechanism injury, the therapist should identify the muscles that may be under or overused, contributing to the impaired alignment. Similarly, muscles that contribute to increasing the transverse arch are the opponens pollicis and digiti minimi, APB, abductor digiti minimi (ADM), flexor digiti minimi (FDM), FPB, and the interossei. The transverse arch is decreased when the ED, extensor pollicis longus (EPL), is dominant compared to the interossei.
An increase in the longitudinal arch of the fingers and thumb is indicative of overuse or relative stiffness of the FDS, FDP, and FPL (see Figure 5-12). A decrease in the longitudinal arch is associated with relative decreased muscle stiffness of the FDS, FDP, and flexor pollicis longus (FPL) (see Figure 5-13, A).
The most common wrist alignment impairment is wrist flexion (Figure 5-15, A and B), but RD or UD may also be present. Wrist flexion may be due to obesity and secondary abduction of the shoulder. The effect of gravity then is to flex the wrist. A resting alignment of wrist flexion may also be the result of repeated use of the finger or wrist flexors with the wrist in a flexed position. The finger or wrist flexors may be relatively stiff, short, or overused compared to the wrist extensors. A resting alignment of wrist RD with extension is indicative of stiffness, shortness or overuse of the extensor carpi radialis longus (ECRL) or extensor carpi radialis brevis (ECRB) relative to the extensor carpi ulnaris (ECU). Wrist radial deviation with wrist flexion is indicative of overuse of the flexor carpi radialis (FCR) relative to the flexor carpi ulnaris (FCU). Overuse of the FCU may result in wrist UD with wrist flexion and overuse of the ECU, wrist UD with extension. Prolonged alignment with the wrist in UD may contribute to injury of the tissues on the ulnar side of the wrist such as the triangular fibrocartilage complex (TFCC) (Figure 5-15, C).



Figure 5-15 A, Impaired alignment: Wrist flexion secondary to elbow hypomobility and lack of elbow extension. B, Impaired resting alignment of wrist flexion secondary to wide thorax and shoulder abduction (without pain or injury). C, Impaired alignment of wrist in ulnar deviation resulting in left ulnar-sided wrist pain.
Shoulder alignment must be considered in making the determination of elbow, forearm, wrist, and hand alignment impairments. If distal impairments are noted, then scapular and humeral alignment should be corrected to determine if the origin of this malalignment is distal or proximal. Impairments in shoulder girdle alignment may affect patterns of muscle use in the hand or cause proximal or distal nerve compression with symptoms radiating into the hand.5,42
Visual appraisal of muscle and tendon development should also be examined when assessing alignment. Asymmetry of muscle bulk between muscles on the same side or compared to the same muscle on the opposite side is another indicator of impaired patterns of muscle use or of nerve injury (Figure 5-16).
An important component of examination of the hand is assessment of appearance, including skin, creases, web spaces, scar, circulation, temperature, edema, sympathetic changes, and nodules. These are not described in detail in this chapter because they are covered well in other texts. However, a brief description of the examination of edema and scar is provided in Box 5-2.
BOX 5-2 Examination and Treatment of Scar and Edema
Scar Classification2
Treatment of Scar2
General treatment guidelines for superficial scar
Treatment of hypersensitive scar
Treatment of immobile or adhered scar
Treatment of raised scar1
Treatment of scar with splinting5
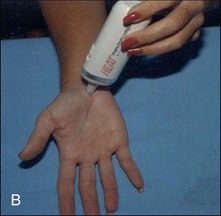
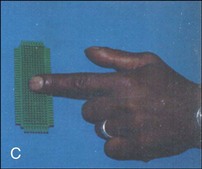
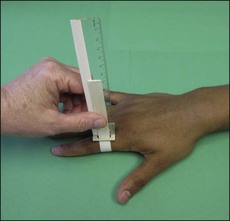
Procedures for Measurement of Edema
Treatment of Edema
General Principles of Positioning the Swollen Hand7
Exercise
AROM, Active range of motion; DIP, distal interphalangeal; IP, interphalangeal; MP, metacarpophalangeal; PIP, proximal interphalangeal; PROM, passive range of motion.
1 Schneider LH, Feldscher SB: Tenolysis: dynamic approach to surgery and therapy. In Mackin EJ, Callahan AD, Osterman AL, et al, eds: Rehabilitation of the hand and upper extremity, ed 5, St Louis, 2002, Mosby.
2 Mustoe TA, Cooter RD, Gold MH, et al: International clinical recommendations on scar management, Plast Reconstr Surg 1102:560-571, 2002.
3 Skirven TM, Callahan AD: Therapist’s management of peripheral nerve injuries. In Mackin EJ, Callahan AD, Osterman AL, et al, eds: Rehabilitation of the hand and upper extremity, ed 5, St Louis, 2002, Mosby.
4 Walsh MT, Muntzer E: Therapist’s management of complex regional pain syndrome reflex sympathetic dystrophy. In Mackin EJ, Callahan AD, Osterman AL et al, eds: Rehabilitation of the hand and upper extremity, ed 5, St Louis, 2002, Mosby.
5 Grigsby DE, Linde L, Knothe B: Therapist’s management of the burned hand. In Mackin EJ, Callahan AD, Osterman AL, et al, eds: Rehabilitation of the hand and upper extremity, ed 5, St Louis, 2002, Mosby.
6 Colditz JC: Anatomic considerations for splinting the thumb. In Mackin EJ, Callahan AD, Osterman AL, et al, eds: Rehabilitation of the hand and upper extremity, ed 5, St Louis, 2002, Mosby.
7 Villeco JP, Mackin EJ, Hunter JM: Edema: therapist’s management. In Mackin EJ, Callahan AD, Osterman AL, et al, eds: Rehabilitation of the hand and upper extremity, ed 5, St Louis, 2002, Mosby.
8 Brand PW, Hollister AM: Clinical mechanics of the hand, ed 3, St Louis, 1999, Mosby.
9 van Velze CA, Kluever I, van der Merwe CA, et al: The difference in volume of dominant and nondominant hands, J Hand Ther 46:6-9, 1991.
10 Artzberger SM: Manual edema mobilization: treatment for edema in subacute hand. In Mackin EJ, Callahan AD, Osterman AL, et al, eds: Rehabilitation of the hand and upper extremity, ed 5, St Louis 2002, Mosby.
11 Innis PC: Surgical management of the stiff hand. In Mackin EJ, Callahan AD, Osterman AL, et al, eds: Rehabilitation of the hand and upper extremity, ed 5, St Louis 2002, Mosby.
Normal Motions of the Hand and Wrist
Wrist Motions
Normally, the wrist extends with slight radial deviation and flexes with slight UD during functional wrist motion.26
Wrist flexion occurs in the sagittal plane around a medial to lateral axis through the capitate.20 Full range is approximately 65 to 80 degrees.43 During wrist flexion if the fingers and thumb are relaxed, finger and thumb extension will occur secondary to tenodesis43 or passive tension on the finger and thumb extensors. During wrist flexion, the proximal carpal row glides posteriorly on the distal radius43,44 and articular disc, the scaphoid and lunate volarflex, and the triquetrum dorsiflexes.45 Relative volarflexion of the scaphoid “unlocks” the midcarpal joint so most of the motion during wrist flexion occurs at the midcarpal joint.45 The articular surface of the distal end of the radius has an inclination anteriorly that allows for greater wrist flexion than extension ROM.43
Wrist extension occurs in the sagittal plane around a medial to lateral axis through the capitate.20 Full range is approximately 55 to 70 degrees.43 During wrist extension if the fingers and thumb are relaxed, finger and thumb flexion will occur secondary to tenodesis of the finger and thumb flexors.43 During wrist extension, the proximal carpal row glides anteriorly on the distal radius43,44 and on the articular disc, the scaphoid and lunate dorsiflex, and the triquetrum volarflexes.45 Relative dorsiflexion of the scaphoid “locks” the midcarpal joint so most of the motion during wrist extension occurs at the radiocarpal joint.45
Radial deviation occurs in the coronal plane around an anterior-to-posterior axis through the capitate. Full range is approximately 15 degrees,43 and maximum range is achieved with the wrist in neutral with respect to flexion and extension. During wrist radial deviation, the proximal carpal row glides ulnarly44 and the scaphoid and lunate volarflex.43,45
Ulnar deviation occurs in the coronal plane around a anterior-to-posterior axis through the capitate. Full range is approximately 30 degrees,43 and maximum range is achieved with the wrist in neutral with respect to flexion and extension. Ulnar deviation is greater than radial deviation because of the medial inclination of the articular surfaces of the distal radius and ulna.43 The radial styloid process extends distally farther than the ulnar styloid process. During wrist UD, the proximal carpal row glides radially44 and the scaphoid and lunate dorsiflex.45 Normally there are greater compressive forces on tissues of the ulnar side of the wrist during wrist UD with the forearm pronated than with the forearm supinated because of a dynamic change in the relative length of the radius and ulna.46 During pronation, the ulna moves slightly distally, whereas during supination it moves slightly proximally.47
Finger Motions
Finger Flexion
MP, PIP, and DIP flexion occurs in the sagittal plane around a medial-to-lateral axis. Full range is approximately 90 degrees for the MP joint. The range increases progressively toward the ulnar side of the hand to about 110 degrees.43 Manual workers with fingers that have a greater circumference tend to have less ROM compared to nonmanual workers.4 Normal range for the PIP is 100 to 120 degrees and 70 to 90 degrees for the DIP.43 Rotation of the MP joints contributes to the fingers being oriented toward the scaphoid at the end of the range of finger flexion (Figure 5-17).20 Normally, the fingers adduct as they flex. Although movement at the CMC and gliding of the intermetacarpal joints are not usually measured clinically, normal finger flexion range and deepening of the arches of the hand require slight flexion at the CMC and gliding at the intermetacarpal joints. There is increased movement at the CMC and intercarpal joints on the ulnar side of the hand compared to the second and third CMC and intercarpal joints. Usually the PIP and DIP joints flex simultaneously.48 The normal total active motion (TAM) of the fingers is 270 degrees. Normally, the fingertips make a large arc of motion20,49 with the PIPs flexing first, followed by MP, and last by DIP flexion20 (Figure 5-18, A). During active finger flexion, the wrist should extend slightly.20,43 During finger flexion at the MP, PIP, and DIP joints, the direction of the glide of the distal articular surface on the proximal articular surface is anterior.44
Finger Rotation
Finger MP and IP rotation occurs in a transverse plane about a longitudinal axis. Average range of passive MP rotation is 30 to 40 degrees and is greatest for the ring and little fingers.20,43 Rotation during active finger MP flexion varies from 1 to 13 degrees of supination.50 The direction of MP rotation of the index finger is variable.50,51 Rotation during active finger PIP flexion varies from 1 to 6 degrees of pronation for the index and middle fingers and 8 to 9 degrees of supination for the ring and small fingers. Rotation of the DIP joints of all fingers vary from 1 to 5 degrees of pronation.50
Finger Extension
MP, PIP, and DIP extension occurs in the sagittal plane around a medial to lateral axis. Full range is approximately 0 to 45 degrees for the MP joint.52 Normal range for the PIP and DIP joints is 0 degrees.52 Although movement at the CMC and gliding of the intermetacarpal joints are not usually measured clinically, normal finger extension range and a decrease of the arches of the hand require extension at the CMC and gliding at the intermetacarpal joints. The sequence of finger extension occurs first at the MP followed by PIP and DIP.4 Normally, the PIP and DIP always extend together.43,48 During finger extension, the wrist should not flex excessively but should stay relatively stable, the IP joints of the fingers should extend through full ROM, and the MP joints should extend at least to neutral (0 degrees). During finger extension at the MP, PIP, and DIP joints, the direction of the glide of the distal articular surface on the proximal articular surface is posterior.44
Finger Abduction
Finger MP abduction occurs in the coronal plane about an anterior-to-posterior axis. To our knowledge, there are no normal values for AROM for MP abduction. Normal passive range is 9 to 19 degrees of radial deviation and 20 to 43 degrees of UD.21 Normal finger abduction should occur without MP extension beyond neutral (0 degrees).43 The direction of the glide of the proximal phalanx on the metacarpal during finger abduction at the MP joints is radial for the index, radial and ulnar for the middle, and ulnar for the ring and small fingers.44 Pronation (medial rotation) occurs at the MP joints during finger radial deviation, and supination occurs during finger UD.21
Thumb Motions
During isolated movements of the thumb, the wrist and fingers should stay stable.
Thumb Flexion
Normal motion occurs around an anterior-to-posterior axis in the coronal plane. Normal range of thumb MP flexion is highly variable but normally about 50 degrees.43 IP flexion is 70 degrees.43 The thumb CMC also flexes 15 degrees52 but is usually not measured clinically. Our observation is that the sequence of movements of the joints of the thumb during flexion from a resting alignment are CMC flexion first followed by MP and IP flexion. During thumb flexion, the thumb medially rotates slightly (pronates).20 The IP joint pronates and adducts during pinch.53 The glide of the distal articular surface on the proximal articular surface at the MP and CMC joints is in an anteroulnar direction.44
Thumb Extension
Normal motion occurs around an anterior-to-posterior axis in the coronal plane. Normal range of thumb MP and IP extension is 0 degrees. The IP has varying degrees of hyperextension and should be compared with the opposite thumb. The CMC joint extends to 10 to 15 degrees from anatomical position.43 Our observation is that the sequence of movements of the joints of the thumb during extension from a resting alignment are CMC extension first followed by MP and IP extension. Thumb extension (also known as radial abduction) should occur without excessive adduction or abduction. During thumb extension, the thumb laterally rotates slightly (supinates). The glide of the distal articular surface on the proximal articular surface at the MP and CMC joints is in a posteroradial direction.44
Thumb Palmar Abduction
Normal motion occurs around a medial to lateral axis in the sagittal plane. A slight amount of abduction occurs at the MP joint, but the primary movement occurs at the CMC joint and is about 45 degrees.43,48 During thumb abduction the MP and IP joints should stay in a fairly neutral position.54 During thumb abduction, the wrist should stay stable and the CMC joint should not extend.4,20 The direction of the glide of the distal articular surface on the proximal articular surface at the MP joint is radial and at the CMC joint is dorsal.43 The CMC joint is most stable in abduction and extension.7,20 It is in abduction and extension that most of the supporting ligaments of the CMC joint are taut.7
Thumb Adduction
Thumb adduction occurs around a medial-to-lateral axis in the sagittal plane. A slight amount of adduction occurs at the MP joint, but the primary movement occurs at the CMC joint.43,48 Normal movement is to be able to adduct the thumb against the radial side of the second metacarpal and index finger.43 The direction of the glide of the distal articular surface on the proximal articular surface at the MP joint is ulnar and at the CMC joint is volar.43,44
Thumb Opposition
Thumb opposition consists of thumb flexion, abduction, and medial rotation (pronation) bringing the tip of the thumb toward the tip of the small finger to line up the fingernails.7,43 During opposition, the CMC and MP joints flex simultaneously throughout the motion. The CMC and MP abduct simultaneously only at the beginning of the movement.54 Often, opposition is not measured goniometrically in the clinic but instead is assessed qualitatively.
Assessment of Range of Motion
AROM assesses the contractile and noncontractile structures.14 When assessing movement of the hand, the patient’s preferred pattern of active ROM is assessed first and correlated with the timing and onset of symptoms. If symptoms are produced and impairments are noted, the movement is immediately modified (when possible) to determine the effect on symptoms. During AROM, the timing of onset of muscle activity and increases and decreases relative to the normal ROM should be noted. A joint that moves relatively too much can be just as or more problematic than a joint with limited motion.
Besides noting the quantity of motion at each joint (increased or decreased), particular emphasis is placed on noting the quality of motion during the composite motion. Impairments to be noted during the assessment of the quality of active finger and thumb flexion and extension include the following:
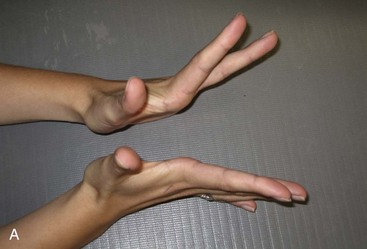

Figure 5-19 A, Excessive MP extension during active finger extension; left worse than the right. B, Insufficient MP extension with excessive IP extension during active finger extension (increased used of intrinsic).
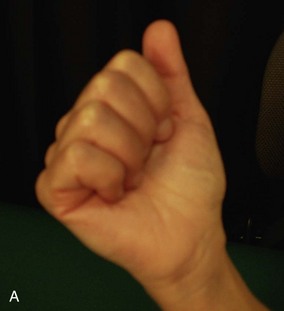

Figure 5-20 A, Decreased mobility on the ulnar side of the hand. B, Normal mobility on ulnar side of hand noted during strong grip.

Figure 5-21 Excessive MP extension instead of IP extension (clawing with finger extension without nerve injury).
In addition, impairments during AROM of the thumb include (1) insufficient or excessive thumb CMC, MP or IP extension or flexion relative to the other joints of the thumb; (2) insufficient or excessive CMC or MP abduction relative to the other joint (CMC or MP); (3) flexion of one joint of the thumb with extension of another or vice versa; and (4) wrist movement during active thumb motion (Figures 5-22 to 5-28).
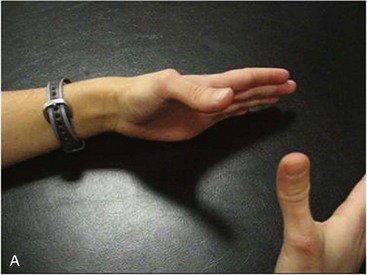

Figure 5-22 A, Insufficient thumb MP extension and excessive IP and CMC extension. B, Insufficient thumb MP extension and excessive IP and CMC extension.


Figure 5-23 A, Insufficient thumb CMC extension with excessive thumb MP extension. B, Insufficient CMC extension and too much MP extension on right hand.


Figure 5-28 Wrist flexes instead of maintaining neutral wrist position during active thumb palmar abduction.
When observing active finger flexion and extension, the alignment and movement of the wrist should also be noted. During active finger extension, the wrist should not flex excessively (Figure 5-29). During active finger flexion, the wrist should not flex but instead should extend slightly (Figure 5-30). During active wrist extension and flexion, the fingers should flex and extend, respectively, as the result of tenodesis4,20,55 (Figure 5-31). For example, during active wrist extension, the fingers should stay relaxed in a relatively flexed position instead of extending.

Figure 5-30 Wrist flexion instead of slight wrist extension during active finger flexion.
(Used with permission from Ann Kammien, PT, CHT, St Louis, Mo.)
Resistance may provoke movement impairments when AROM is normal or may exaggerate the impairment noted during AROM (Figures 5-32 to 5-39).

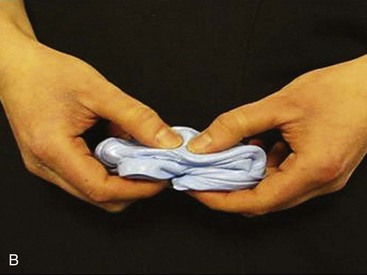


Figure 5-32 A, Normal longitudinal arc of thumb during pinch and good thenar muscle bulk. B, Collapse of first MC into flexion and adduction during pinch (left worse than right). C, Excessive thumb CMC adduction and flexion with wrist flexion during pinch. D, Excessive thumb IP extension and MP flexion during pinch (boutonnière).


Figure 5-34 A, Correct pattern of pinch: Maintaining arch of the first metacarpal. B, Collapse of first MC into flexion and adduction (swan neck) during pinch.


Figure 5-36 A, Dorsal view of impaired arc of movement: Excessive MP flexion and PIP extension (swan neck) index finger during resisted finger flexion. B, Radial or lateral view.
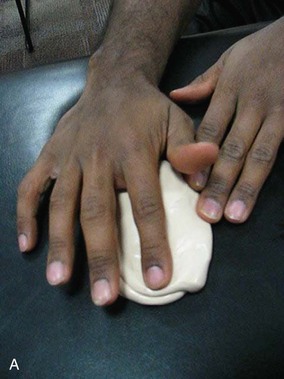


Figure 5-37 Impaired movement: Excessive MP adduction and/or rotation (supination = lateral rotation) of the index finger during resisted finger flexion. A, Starting position. B and C, MP adduction with rotation.

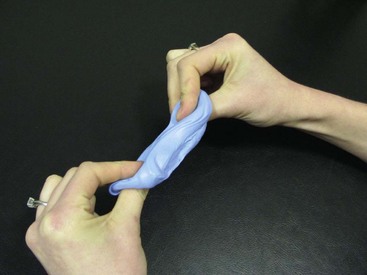

Figure 5-38 Impaired arc of movement: Increased PIP flexion and DIP hyperextension (boutonnière) of index finger during resisted finger flexion.

Figure 5-39 Impaired arc of movement: Excessive MP extension during resisted finger flexion indicating insufficient use of interossei.
Finally, during AROM or resistive ROM of the fingers or thumb, the examiner should also note the alignment and movement of the proximal upper extremity (forearm, elbow, and shoulder). The source of symptoms in the hand may come from the cervical spine, the thoracic outlet,5 elbow, forearm, wrist, or the hand.9-11 When the shoulder girdle is impaired, the distal muscles may generate excessive force to compensate for the proximal impairments.4,42,56,57 Decreased strength of the scapular muscles and poor scapular alignment may result in compression of nerves proximally causing symptoms in the hand or predisposing injury to the nerves distally (double crush).5 Ideal alignment and strength of the shoulder girdle provides a stable base on which the distal upper extremity can function.
Following AROM, PROM should be assessed, paying particular attention to identifying the cause of the impairments. For example, what is the reason for the limited AROM?
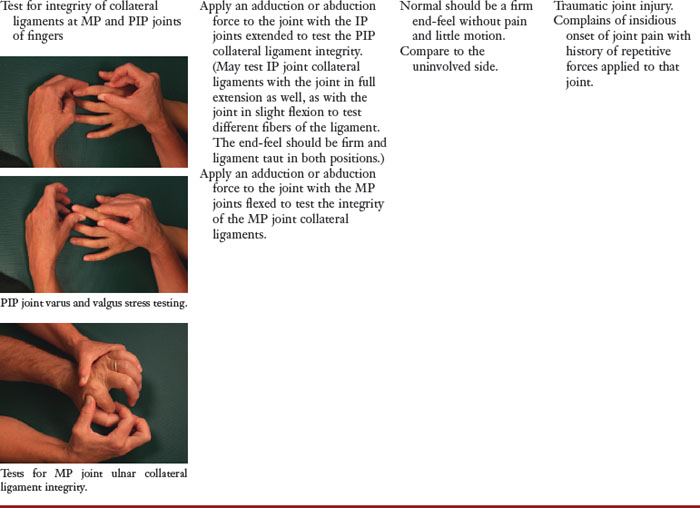
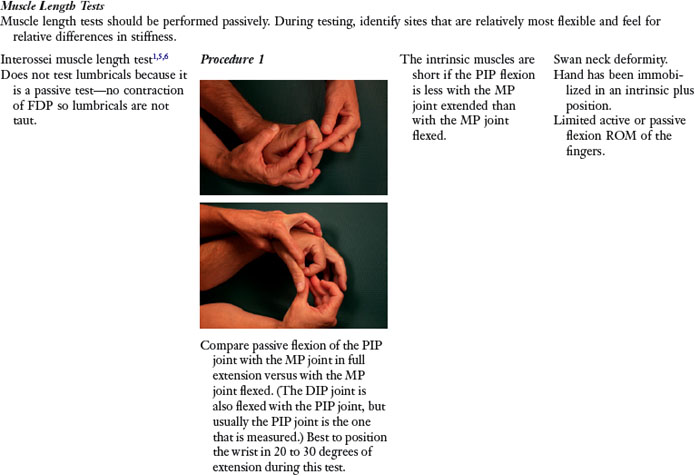
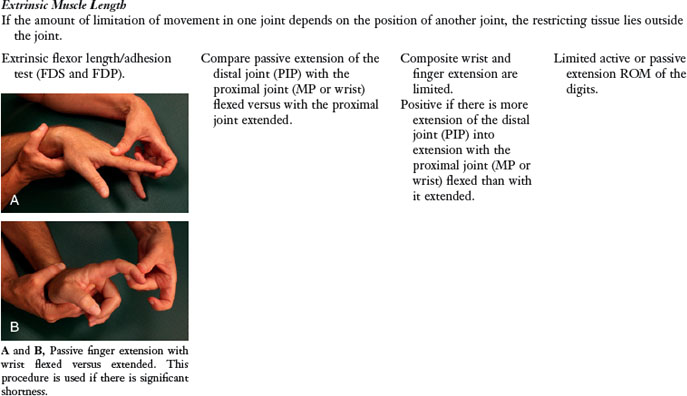
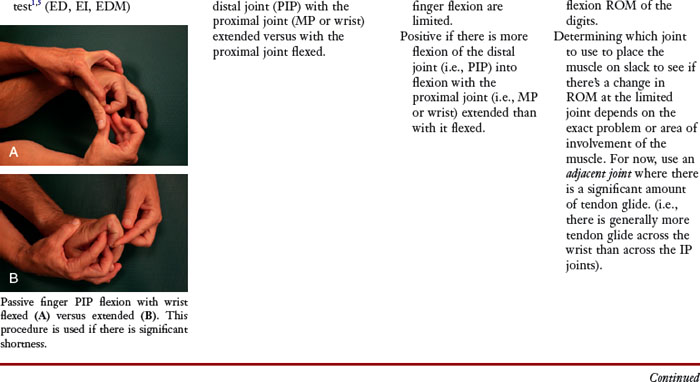
Of particular interest during assessment of PROM is the resistance felt to passive motion (stiffness). Passive tests should include tests of muscle length, ligament integrity, joint capsular pattern, joint accessory motion, and ligament length. When assessing muscle length, particular attention is paid to relative flexibility and stiffness not just absolute length. Stiffness is compared between one muscle or group relative to another and between muscles on one side compared to the same muscles on the opposite side. The onset of pain should also be noted during PROM and compared to the pain behavior during AROM. This helps determine whether the contractile or noncontractile structures are involved.14
PROM can then be followed by resistive testing to identify involvement of the contractile structures and to determine strength of individual or groups of muscles. Although a muscle may test strong in the midrange, it might test weak in the shortened range. The findings from the AROM, PROM, and resisted tests are evaluated to determine the cause of the movement impairments. This evaluation helps focus the treatment.
Functional Activities of the Hand and Wrist
Subjective Examination
During the history, the patient should be questioned about those daily activities that are performed repeatedly and which of those are associated with either increasing and decreasing the symptoms. These activities include work, leisure, and activities of daily living (ADLs).
The patient must be asked to describe and demonstrate the preferred alignment and movement patterns they use repeatedly during their daily activities. Attention is given to the entire upper quarter and trunk and the potential effect of those areas on the distal symptoms. Any impairments that are identified are immediately modified to determine the effect the modification has on the patient’s symptoms.
Assessment of the person’s preferred pattern of performance of functional activities is a crucial part of examining the patient with symptoms in the hand. Activities or postures that are used frequently during the day or during sleep are assessed. Simulation of the posture or movement should be performed during the examination. Attention should be paid to onset of symptoms, alignment and movement patterns of the entire upper extremity. If symptoms are present and impairments are noted in the posture or movement pattern, the posture or movement pattern should be immediately modified to determine if the modification alleviates the symptoms. The patient should then be educated regarding the impaired posture or movement pattern, and practice of the modified movement pattern should be done during the therapy session until the patient is able to adequately perform the modification independently. The modification must be easy enough for the patient to perform so that he or she can perform it correctly. If the patient is having difficulty, the examiner should prescribe a different modification that is easier. Symptoms should not be produced or increased during the modification of the movement or posture. Frequently, patients with symptoms in the hand also need modifications to the alignment or movement of the shoulder to alleviate the symptoms.5 Taking breaks frequently to improve the performance of the opposing muscles from those used repeatedly is often beneficial.
Examples of modifications in functional activities that may be necessary are detailed in the next sections.
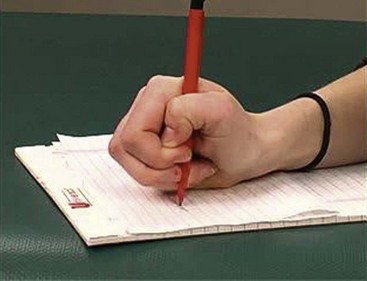
Writing
Modifications in writing focus on restoring the normal arch of the thumb and fingers used in grip, and correcting the alignment of the wrist, trunk, and shoulder girdle. The thumb CMC should be in relatively more abduction and pronation instead of adduction, flexion, and supination. Avoiding prolonged positioning with the joints at end-ranges may decrease stresses on the joint structures. At times, compensatory techniques may be useful such as using a writing utensil with a larger diameter or taping or splinting to facilitate correct alignment. Writing using a prehensile pattern of a 3-point grip with the DIP joint of the index finger in hyperextension and the PIP joint flexed may increase the compressive forces on the dorsal surfaces of the DIP joint and increase the tensile forces on the volar structures. With this type of grip the FDP is underused and the FDS may be overused. The ORL may become shortened and may need stretching. Writing with the thumb CMC positioned in adduction places the CMC joint in a less stable position and may result in stiffness or shortness of the adductor pollicis and insufficient use of the APB and the OP (Figures 5-40 to 5-44).
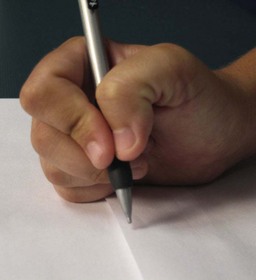

Figure 5-41 Writing: Impaired alignment. Excessive CMC adduction, thumb IP flexion, and index DIP extension.
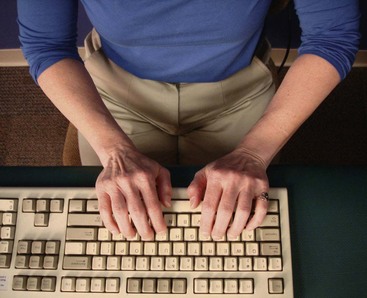
Using a Computer Mouse and Typing
The computer mouse and keyboard should be positioned on the desk so they can be reached while maintaining good alignment of the proximal upper extremity. The upper extremity should be supported to maintain the trunk and shoulder girdle in ideal alignment, the elbow flexed slightly less than 90 degrees, the forearms supported, and the wrists in very slight extension. The fingers should rest in the normal longitudinal arch (Figure 5-45) and in a relatively neutral position regarding ulnar or radial deviation (Figures 5-46 to 5-48).58 Consideration of alternate keyboard or mouse styles, adjustable chair armrests, and adjusting chair and monitor height are often helpful to achieve the ideal alignment. In our experience, in most cases the preferred alignment of the shoulder girdle is in scapular depression. Adjustments need to be made to the arm support to elevate the shoulder girdle to ideal alignment. At times, placing the keyboard on the desk instead of using the computer tray is optimal. This positioning may require moving the monitor back on the desk so the keyboard can be placed a few inches away from the edge of the desk, allowing the distal one-half to two-thirds of the forearms to be supported by the desk. A preferred alignment of some shoulder abduction can result in increased wrist UD and extension contributing to symptoms on the ulnar side of the wrist. Taking breaks to stand with the back against the wall and performing shoulder flexion, as well as stretching the finger flexors and extensors can be helpful.
Lifting
Lifting with the elbow flexed and the forearm supinated instead of pronated often helps decrease symptoms for patients with lateral epicondylitis (wrist extension with forearm pronation syndrome).
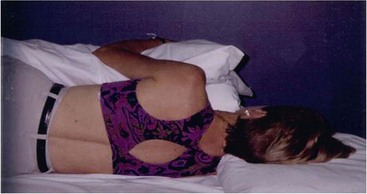
Sleeping
Particular attention should be paid to sleeping position when the alignment of the shoulder girdle is a factor contributing to the patient’s symptoms in the distal upper extremity. At times, a wrist or hand splint may be necessary to maintain the proper alignment of those joints. For example, in patients who have carpal tunnel syndrome (CTS), the wrist should be kept in a neutral position. Splinting the wrist is used to maintain the wrist position in patients with CTS, but proper support of the arm may also be helpful (Figure 5-49).
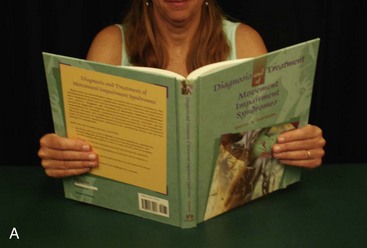
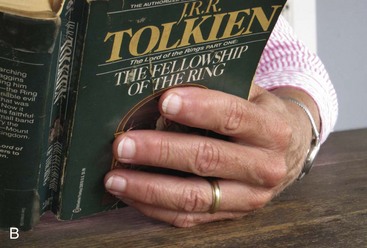
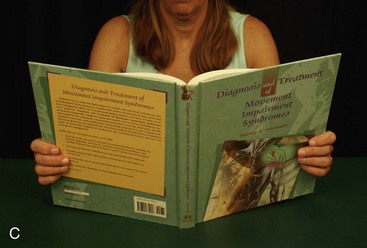
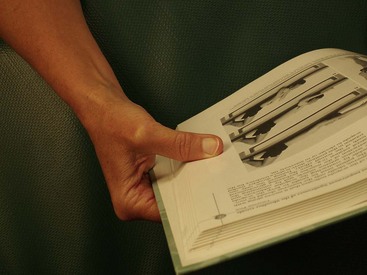
Reading
The pattern of grip used to hold the book while reading and the alignment of the proximal upper extremity, neck, and trunk should be noted. Resting and propping the reading material up on pillows and tilting it helps maintain the correct alignment of the head and decreases the need for prolonged gripping of the reading material (Figure 5-50).
Gripping Objects
Identification of repeated use of a particular preferred pattern of grip or pinch directs treatment. The pattern is modified either by varying the pattern or by alternating the pattern with one that uses a different set of muscles. For example, if a person tends to grip using an intrinsic plus type grip (MP flexion with IP extension; see Figure 5-50, A and B), instruction to use a style of grip that uses the extrinsic finger flexors more (hook- or power-type grip48; see Figure 5-50, C) may be beneficial. If an intrinsic plus grip must be used repeatedly, then taking breaks to stretch those muscles is necessary. Gripping objects so that a prolonged force is placed on the joints into ulnar or radial deviation should be avoided (Figure 5-51).
Playing an Instrument
Maintaining the ideal alignment of the trunk, neck, shoulder girdle, and distal upper extremity while playing an instrument is important. Particular attention is paid to subtle deviations in the alignment of the fingers (rotation, UD, or loss of the arch) and wrist, especially during functional use as force is increased. Small changes in the alignment of the shoulder girdle and elbow can result in beneficial decreases in the stresses on the hand.4,56 For example, while playing the harp with the scapula aligned in excessive abduction, the musician may excessively flex the elbow or extend the wrist to reach the close strings. Adducting the scapula slightly results in less extension of the wrist and less elbow flexion.
Manual Therapy
When the therapist applies force using the fingers or thumbs during joint mobilization techniques or massage, repeated or prolonged positioning of the therapist’s joints at end-ranges should be avoided. A common impairment noted with the thumb position is collapse of the CMC into adduction and flexion and the MP and IP into excessive flexion or excessive extension. Modification of this alignment to a more neutral position may help reduce stresses on the tissues (Figure 5-52).


Figure 5-52 A, Preferred pattern of motion of physical therapy student performing simulated functional activity of joint mobilization. B, Modified pattern of motion of physical therapy student performing simulated functional activity of joint mobilization intended to decrease stresses on thumb joints.
Many other functional activities may need to be addressed depending on those used by the patient. Examples may be eating, cooking, driving, other work activities, fitness, and hygiene.
Muscular actions of the Hand and Wrist
Muscles of the Wrist
The ECRL and ECRB are wrist extensors and radial deviators.13 They are in the second extensor compartment.59 The ECRL is a better radial deviator than the ECRB. The ECRL may also help flex the elbow13 and supinate the forearm.26
During finger flexion, gripping, or pinching, it is critical that the ECRL and ECRB are active to ensure the correct length tension capabilities of the finger flexors.20,43,60 During contraction of the finger flexors as with attempted gripping or pinching, weakness of the wrist extensors will result in the wrist flexing. Wrist flexion decreases the mechanical advantage of the finger flexors, limiting the ability to grip or pinch.20 Another example of compensatory wrist flexion occurring during active finger flexion is when finger flexion is limited by stiffness, shortness, or adhesions. Maximizing active finger flexion ROM requires that the wrist be maintained in 20 to 30 degrees of extension.20
During active wrist extension, if the wrist extensors are weak, the fingers may extend, indicating substitution by the ED. This is common after a wrist fracture. To strengthen the wrist extensors, it is critical to keep the fingers relaxed in flexion to avoid substitution by the ED.
The ECRL may often become overused, stiff, short, or painful. The ECRL has a good moment arm for elbow flexion49 in any forearm position but is the greatest with the forearm pronated.61 Repeated flexion of the elbow with the forearm pronated contributes to overuse of the ECRL. This is often the case with patients with lateral epicondylosis. During forearm pronation, compensatory humeral medial rotation will allow the ECRL to remain stiff or short. Humeral medial rotation should be avoided during exercises designed to increase the extensibility of the ECRL. If the ECRL is overused because the elbow is repeatedly flexed with the forearm in pronation, an important part of treatment is educating the patient to increase the use of the biceps by flexing the elbow with the forearm supinated instead of pronated. In addition, the ECRL also tends to be overused because it is active as a synergist during any gripping or pinching activities, which includes most daily functional activities.43
When performing resisted tests to differentiate between the ECRL or ECRB as the source of the symptoms, modification of elbow position can be helpful.13 Symptomatic resisted wrist extension with the elbow flexed implicates the ECRB, whereas the elbow extended implicates the ECRL.
Flexibility and strengthening exercises are often beneficial for patients with lateral elbow pain associated with overuse of the wrist extensors. Combined wrist flexion, forearm pronation, and elbow extension11 with the humerus stabilized places maximal stretch on the ECRL and ECRB. Shortness of the ECRL and ECRB results in a resting alignment of wrist extension and radial deviation.13 Stiffness of the ECRL and ECRB is identified by increased resistance to stretch during wrist flexion and ulnar deviation when the forearm is pronated with the elbow extended and the humerus stabilized. Progression of exercises should take into consideration the multiple joints that the muscle crosses when the goal is to avoid excessive stresses on the ECRL and ECRB.62 For example, performing wrist extension and flexion exercises with the forearm in neutral rotation and the elbow flexed places less tensile stress on the ECRL than with the forearm pronated and elbow extended.
The ECU extends and ulnarly deviates the wrist.13 The ECU is in the sixth extensor compartment.59 It is a better wrist extensor with the forearm supinated than with the forearm pronated because the tendon slips anteriorly during forearm pronation.48,49 The ECU is active as an antagonist during wrist flexion63 and stabilizes the wrist during thumb abduction.20 The ECU works along with the ECRL and ED during wrist extension. Through the attachments of its sheath to the TFCC,45 the ECU contributes to the stability of the distal radioulnar joint (DRUJ)43 and the ulnar carpals. Repeated use of the wrist in UD47 and wrist extension causes increased compression on the TFCC potentially resulting in tissue injury and symptoms. A resting alignment of slight shoulder abduction while typing on a standard computer keyboard has been observed to contribute to increased wrist extension and UD, with symptoms on the ulnar side of the wrist. Shortness of the ECU results in a resting alignment of UD with slight wrist extension.13 Stiffness of the ECU is identified by increased resistance to stretch during wrist flexion and radial deviation with the forearm pronated, elbow extended, and humerus stabilized.
The FCR flexes and radially deviates the wrist. The FCR may also assist in pronation of the forearm and elbow flexion.13,26 The FCR contracts during RD to counterbalance the extensor component of the ECRL.43 During movements of the wrist, the FCR also plays a role in stabilizing the distal pole of the scaphoid.64 Shortness of the FCR results in a resting alignment of wrist flexion and RD.13 Stiffness of the FCR is identified by increased resistance to stretch during wrist extension and ulnar deviation with the forearm supinated, elbow extended and humerus stabilized.
The FCU flexes and ulnarly deviates the wrist. It also assists with elbow flexion.13 The FCU is a very strong muscle with a large cross-sectional area.43,49 The FCU is less active as an ulnar deviator than the ECU.49 The FCU stabilizes the pisiform during contraction of the ADM.65 An imbalance between the forces of the FCU and ADM caused by repeated abduction of the small finger with the wrist in excessive extension may result in pain in the region of the pisiform or pisotriquetral joint. Overuse, stiffness, or shortness of the FCU may contribute to ulnar nerve compression at the elbow.11 Shortness of the FCU results in a resting alignment of wrist flexion with UD.13 Stiffness of the FCU is identified by increased resistance to stretch during wrist extension and radial deviation with the forearm supinated, elbow extended, and humerus stabilized.
The palmaris longus is a pure wrist flexor. It is absent in about 10% of people.43 It tenses the palmar fascia and assists with elbow flexion.13
Extrinsic Muscles of the Fingers
Finger Extensors
The extensor digitorum communis (EDC), extensor indicis (EI), and extensor digiti minimi (EDM) extend the MP joints of the fingers via their attachment into the sagittal bands.20 No other muscles can extend the MP joints of the fingers.19,20 All three muscles assist with IP extension if the MPs are not fully extended. The ED assists with abduction of the index, middle, and ring fingers, and both the ED and the EDM assist with abduction of the small finger.13 If the DI are weak, the ED and EDM may substitute for finger abduction. The EI assists with adduction of the index finger.13 The EI also allows independent extension of the index finger with the other fingers flexed.19 The juncturae between the tendons of the ED and sharing of the muscle bellies of the ED in the forearm contribute to limited independence of finger motion.20,66 The ED also assists with wrist extension and RD.13,43,63 The ED and EI are in the fourth extensor compartment, whereas the EDM is in the fifth.59,66
Normally, the finger extensor tendons should remain centered over the dorsum of the head of the metacarpal if the sagittal bands are intact.66 Normally during finger flexion, the ED tendons move ulnarly slightly because of the increased mobility on the ulnar side of the hand.20 Laxity of the sagittal bands allows the extensor tendons to sublux, usually to the ulnar side of the joint, during finger flexion.49,66
During normal active finger extension when the forces of the MP flexors (FDP, FDS interossei and lumbricals) and MP extensors (ED) are balanced, the ED extends the MP but does not cause MP hyperextension. If some of the MP flexors (interossei and lumbricals) are weak, the ED causes increased MP hyperextension, which prevents the ED from being able to extend the IP joints fully.24,26 This pattern of movement (mild “clawing”) is often observed in musicians such as pianists.
During finger flexion, when applying pressure to a surface (i.e., piano keys), or any type of pinch, the PIP joint should not hyperextend, but the finger should maintain its normal longitudinal arch. Maintenance of the arch requires the balanced action between the intrinsic long finger flexors and the ED. Overuse of the intrinsics results in a swan neck–type posture.30,31
During active finger extension, if the forces between the intrinsics and long finger extensors are balanced, the fingertips should move through a wide arc of motion. If the extensors (ED) dominate, the arc of motion is smaller.67
During active finger extension, the wrist flexors should stabilize the wrist to prevent excessive wrist extension by the ED.65 If the wrist flexors are overused during active finger extension, the wrist flexes because the wrist flexors are no longer just stabilizing but are overactive, flexing the wrist.
An example of the finger extensors (ED) dominating is displayed when the ECRL and/or ECRB is weak (i.e., after a Colles’ fracture). As the patient attempts wrist extension, the fingers extend instead of remaining relaxed in a flexed position.
During cylindrical grip, such as in holding a hammer, the ED helps stabilize the MP joint. Acting with MP flexors, the ED increases joint stability and compression. During spherical grip, such as in holding a baseball, the role of the finger extensors is to balance the finger flexors. The finger extensors also function to open the hand and release objects.48
During the passive length test for the ED, shortness or stiffness of the ED results in the MP and IP joints of the fingers extending if the wrist is flexed, or if the MP and IP joints are flexed, the wrist will extend. Shortness13 or stiffness of the finger extensors may also contribute to subluxation of the tendon over the head of the metacarpal during finger flexion.
Finger Flexors
The primary action of the FDS is to flex the PIP joints of the fingers. However, the FDS also assists with flexion of the CMC, MP, and wrist joints.13 The FDS powers most individual finger motion49 and crosses the elbow joint, whereas the FDP does not. The primary action of the FDP is flexion of the distal interphalangeal joints of the fingers. However, the FDP also assists with wrist, CMC, MP, and PIP flexion.13 In the normal hand, the flexor tendons cross the MP joint slightly from the ulnar side. However, the flexor tendons do not ulnarly deviate the MP joint unless the annular ligaments are lax or damaged, allowing the flexors to become ulnar deviators.49 During finger flexion, the FDP assists adduction of the index, ring, and small MP joints of the fingers. Interconnections of the muscle fibers of the FDP in the forearm inhibit the independent function of the individual tendons of the FDP.49 Therefore, to prevent the FDP from working on the finger being tested during MMT of the FDS, the other fingers are stabilized.68 After surgical repair of the FDP, uninvolved fingers adjacent to the involved finger may need to be immobilized to prevent forces from the adjacent fingers being transferred to the repaired tendon.
Good gliding of the FDS and FDP tendons relative to each other and to the bone is critical to good hand function. Restoring normal gliding of these tendons is often a focus of therapy in patients with traumatic hand injuries.69 Good hand function also requires normal length of the FDS and FDP. Shortness,13 stiffness, or adhesion of the FDS will result in flexion of the MP and PIP joints of the fingers if the wrist is extended or flexion of the wrist if the fingers are maintained in extension. Shortness,13 stiffness, or adhesion of the FDP will result in MP, PIP, and DIP flexion if the wrist is extended or wrist flexion if the finger is maintained in extension. Findings from flexor muscle length testing in patients with overuse syndromes often reveal that the absolute length of the muscles is normal, but the involved side is noticeably stiffer through the range than the uninvolved side. Caution should be used when stretching the FDS and FDP to prevent the MP and IP joints from flexing. Overstretching should also be avoided. Combined stretching of the wrist and fingers should not exceed 80 degrees of wrist extension and zero degrees of finger extension.
During cylindrical gripping, the FDP is more active during the dynamic phase of flexion movements of the fingers, whereas the FDS is more active during the static phase.48 During types of prehension that require DIP flexion, such as picking up a pin, the FDP is active.48 The FDS is active when the DIP is extended during PIP flexion.
There is a decrease in tension of the FDS and FDP at the more distal joints of the fingers when the wrist flexes.65 Thus when the focus of treatment is regaining finger flexion, the wrist should be maintained in at least 20 to 30 degrees of extension. The benefit of wrist extension for the length-tension properties of the flexor tendons has been discussed previously in the “Muscles of the Wrist” section.
CTS may be aggravated during gripping or prehension when using the finger flexors with the wrist flexed because this movement pattern results in anterior movement of the flexor tendons. The anterior movement of the flexor tendons decreases the distance between the finger flexor tendons and the flexor retinaculum relative to using the finger flexors with the wrist in extension, thus increasing the pressure on the median nerve at the wrist.70 Maintaining the wrist in neutral-to-slight extension during contraction of the finger flexors prevents the anterior movement of the flexor tendons.70 A movement impairment of wrist flexion during active finger extension has also been observed in patients with CTS (see Figure 5-29). Repeated use of the wrist flexors with the wrist in flexion may result in an impairment of the wrist flexors noted during active finger extension. Normally during active finger extension, the wrist flexors should stabilize the wrist against the wrist extensor force provided by the finger extensors. However, if the wrist flexors have been used repeatedly in a position of wrist flexion, the wrist flexors may flex the wrist during finger extension instead of stabilizing the wrist. Patients with this movement pattern should be instructed to practice active finger extension, maintaining the wrist in slight extension.
During finger flexion while applying pressure to a surface (such as playing the piano or any type of pinch), the fingers maintain a longitudinal arch when the actions of the FDS and FDP are balanced by the actions of the ED and the finger intrinsics.4 During open-chain active finger flexion, the fingertips should move through a wide arc of motion if there is balanced action between the intrinsics and long finger flexors. If the long finger flexors dominate, the arc of motion is decreases20,49 (see Figure 5-18). More details regarding specific movement impairments related to imbalances between these muscles are described later in this chapter in the discussion on the movement system syndromes.
The median nerve may become compressed as it travels under the proximal edge of the FDS producing symptoms in the anterior forearm and hand. Contraction of the FDS to the middle finger increases the compression, aggravating the symptoms.71
During active finger flexion in end-range power gripping, we have observed a movement impairment of an excessive increase in the ulnar side of the distal transverse arch and UD of the fingers at the MP joint in some patients. This movement impairment may also contribute to subluxation of the finger extensors over the head of the metacarpals and is more likely to be observed in the patient with hypermobile joints. Manually supporting the MP heads to prevent the excessive increase in the transverse arch abolishes the popping of the finger extensors over the heads of the metacarpals. Treatment may include limiting the finger flexion ROM, using splinting to assist avoiding excessive UD and increase in the transverse arch, exercising to increase the stiffness of the radial deviators of the MP joints of the fingers, and actively practicing the corrected movement pattern.
Intrinsic Muscles of the Fingers
The intrinsic muscles of the fingers include the DI and palmar interossei (PI) and the lumbricals.19 The DIs abduct the fingers away from the midline of the hand, which is through the middle finger and third metacarpal.72 The first DI assists with adduction of the thumb13 and may assist with stabilizing the first CMC joint.49 The three palmar interossei adduct the fingers.13 All of the interossei and the four lumbricals flex the MP and extend the IP joints of the fingers.19 The lumbricals are good extensors of the IP joints, regardless of the position of the MP joint.20 Because both of the lumbrical attachments are into tendons and the lumbricals have many sensory organs, the lumbricals balance the tension between the finger extensor mechanism and the finger flexors (FDP).20 When the lumbricals contract, the FDP tension is released and tension on the extensor mechanism is increased, facilitating finger IP extension.20 The lumbricals are relatively silent during cylindrical grip (gripping a tennis racket), whereas the interossei are very active.48 The interossei become more efficient as MP flexors as the fingers move farther into flexion.49 The role of the interossei during cylindrical grip and pad-to-pad prehension is to help flex, abduct, and adduct the MP joints of the fingers.48 The interossei contribute to ulnarly deviating all of the MP joints during gripping.48 The function of the interossei is critical for normal active finger flexion and extension. Weakness results in “clawing,” which has already been described (see sections on ED and impaired alignment). Absence of interossei function for the small finger results in a resting alignment of MP abduction and extension as a result of the unopposed action of the ED, which is referred to as Wartenberg’s sign.12,73
Shortness or stiffness of the intrinsics may result from overuse or immobilization at a shortened length. Shortness may not be evident when making a fist, but PIP and DIP flexion may be severely limited with the MP joint maintained in extension.19,20 Subtle differences in the length of the interossei may be identified only by abduction or adduction of the finger while maintaining the MP joint in extension and the IP joints in flexion. Shortness, stiffness, or overuse of the interossei on one side of the finger relative to the interossei on the opposite side of the finger may result in a rotation impairment of the MP or PIP joint of the finger. For example, if the first DI is underused and the first palmar interosseous is overused, the patient may present with the index finger resting in increased supination compared to the opposite side. The patient might present with pain in the area of the MP joint or PIP joint, depending on which joint is most affected by the rotation. A repeated activity that might contribute to this impairment is using the number keys on the right side of the computer keyboard instead of using the keys at the top of the keyboard. This movement impairment is described further in the “Movement System Syndromes” section.
Some patients that have normal ulnar nerve function demonstrate a movement impairment of mild clawing of the fingers only during functional use. MP hyperextension is noted presumably because the ED (MP extensor) is no longer counterbalanced by intrinsics (MP flexors) at the MP joint even though the intrinsics may test normal during strength testing. The ED cannot effectively extend IP joints because it is actively insufficient because of MP hyperextension. MP hyperextension puts passive tension on long finger flexors pulling the IPs into flexion. Teaching these patients to modify their preferred movement pattern may help prevent or relieve symptoms.
Weakness of the finger intrinsics has been described as common in patients who are performing artists, so strengthening the intrinsics is recommended.57 However, we find the muscles do not necessarily test weak when testing the strength of the intrinsics with MMT. We have observed instead that the preferred pattern of movement used by the patient is not ideal, and modification of that movement pattern results in relieving the patient’s symptoms. The focus of the modification is to maintain the longitudinal arch of the hand and fingers and neutral rotation of the fingers while playing an instrument, balancing the use of the long finger flexors and intrinsics.4 Changing the movement pattern is required to achieve a reduction of symptoms and strengthening alone is not as effective. To learn the correct movement pattern, patients need to perform the motion with decreased resistance and difficulty. If resistance is added before learning the new movement pattern, patients will resort to using the preferred impaired pattern of movement.
Thenar Muscles
The thenar muscles are crucial for positioning the thumb during functional grasping and manipulating objects.4,48 Contraction of the APB and the OP deepen the concavity or transverse arches of the hand facilitating grasp. The activity of these muscles varies, depending on whether the thumb is being opposed to the radial or ulnar fingers and on the force applied.48
The APB palmarly abducts the CMC and MP joints of the thumb13 and assists thumb IP joint extension through its attachments to the extensor mechanism. Most of the thumb abduction occurs at the CMC joint. The APB may assist flexion and medial rotation of the MP joint and assists with opposition of the CMC joint.13 The APB is often underused compared to the adductor pollicis and FPB, but in the absence of a nerve injury, the APB rarely tests weak during MMT. The APB is active during pinch of thumb with any finger and increases to equal the activity of the adductor pollicis during firm pinch with the small finger.48 Shortness or stiffness of this muscle is rare.
The OP flexes, abducts and medially rotates the CMC joint of the thumb. Cupping the hand, the APB and OP deepen the transverse arch at the carpal tunnel. Opposition of the thumb also results in deepening the proximal transverse arch of the hand. The OP and the APB originate on the flexor retinaculum.13 Weakness of the opponens results in the inability to oppose the tip of the thumb to the tip of the small finger, lining up the fingernails and making prehensile types of grip difficult if not impossible.13 Substitution using the FPB may allow the patient to touch the tip of the small finger to the thumb, but the patient will be unable to rotate the first metacarpal to line up the fingernails.74 During pinch, the activity of the opponens increases as the pinch with the thumb moves from the index to the small finger.48 The OP is often underused compared to the adductor pollicis and FPB, but in the absence of a nerve injury, rarely tests weak with MMT. Shortness or stiffness of this muscle is rare.
The FPB flexes the MP and CMC joints of the thumb. The FPB assists in opposition of the thumb and helps extend the IP joint via the extensor mechanism.13 The FPB has increased activity with increased force of pinch.48 The FPB is often overused along with the adductor pollicis. Shortness or stiffness of the FBP results in MP flexion of the thumb.
The adductor pollicis adducts the CMC and MP joints of the thumb and assists with MP flexion. It also assists with IP extension through its attachments to the extensor mechanism.13 The adductor pollicis has the largest torque potential of any muscle affecting the CMC joint of the thumb7 This muscle is active during all types of strong pinch but especially active during key or lateral pinch.48 During key pinch, if the adductor is weak, the FPL will substitute for the adductor pollicis, resulting in thumb IP flexion (positive Froment’s sign).49 If the adductor pollicis is nonfunctional, by using tenodesis,43 the thumb can be positioned for key pinch by extending the wrist. Because the adductor is used in all types of strong pinch and grip and the thumb is usually flexed and adducted during functional use,75 the adductor pollicis is frequently overused, stiff, or short. Overuse, stiffness, or shortness of the adductor contributes to alignment impairments, imprecise movement, and symptoms at the CMC joint of the thumb. An extreme example is OA with subluxation of the CMC joint of the thumb. During prehensile gripping, because of the distal attachment of the adductor pollicis on the first metacarpal, the adductor pollicis contributes to adduction, flexion, and lateral rotation (supination) of the thumb instead of helping maintain the longitudinal arch of the thumb.
Extrinsic Muscles of the Thumb
The APL abducts and extends the CMC joint of the thumb. Although it is named as an abductor, the movement it performs is really more extension of the thumb.49 The APL assists with radial deviation and flexion of the wrist.13 The APL is in the first extensor compartment with the EPB.66 The APL is the key muscle to maintain the arch of the pinch in the absence of deformity49 and thereby provides stability to the CMC joint.7 It is opposed by the adductor pollicis.49 The APL will substitute for the APB when the APB is weak, resulting in thumb extension with abduction instead of pure thumb palmar abduction. Increased stresses are placed on the tendons in the first extensor compartment with repeated RD of the wrist with the thumb stabilized, forceful wrist RD with abduction and extension of thumb, rapid rotational movements of forearm, and forceful UD of the wrist.76
The APL and the EPB can be the source of symptoms in two different locations: at the wrist over the first extensor compartment (deQuervain’s disease) and more proximally where the muscle crosses the ECRL and ECRB (intersection syndrome).77 The APL and the EPB must glide freely through the retinacular compartment to be symptom-free and function well. Shortness or stiffness results in wrist RD when the thumb is flexed or thumb extension when the wrist is ulnarly deviated. The length test for this muscle (similar to Finkelstein’s test) may provoke symptoms at the first extensor compartment if the APL or EPB is the source of the symptoms.
The EPL extends the IP joint of the thumb and assists with MP and CMC extension.13 The EPL assists with adducting the thumb CMC joint49 and extending and radially deviating the wrist.13 The EPL is in the third extensor compartment.66 Although the EPL is the primary thumb IP extensor, the deep head of the FPB, adductor pollicis, and the APB may assist in extending the IP joint of the thumb via their attachments into the extensor mechanism on the thumb.13 During thumb extension, if adduction occurs during extension, the EPL may be overused compared to the EPB and APL (see Figure 5-25). The APL, EPL, and EPB are synergists during thumb extension. Excessive thumb adduction during thumb extension indicates overuse of the EPL relative to the APL and EPB. Shortness of the EPL results in thumb extension when the wrist is ulnarly deviated with flexion or wrist extension and RD when the thumb is flexed. The ability to extend and adduct the thumb off the table when the hand is resting on the table with the palm down verifies that the EPL is intact.19
The EPB extends the MP joint of the thumb, extends and abducts the CMC, and assists with wrist RD.13 The EPB tendon is in the first extensor compartment of the wrist with the APL66 but is generally weaker than the APL. Weakness of the EPB is common. During thumb extension, if adduction occurs with extension, the EPB and APL may be underused compared to the EPL. Modifying the extension so the patient extends with more abduction will increase the use of the EPB and APL versus the EPL. During active thumb extension, other movement impairments involving the EPB can occur and are described in detail in the treatment section of the Chapter 5 Appendix for the thumb CMC accessory hypermobility syndrome. Shortness, stiffness, or adhesion of the EPB results in thumb MP extension when the thumb is flexed and the wrist is ulnarly deviated.
The FPL flexes the IP joint of the thumb, assists with MP and CMC flexion, and may assist with wrist flexion.13 The FPL is active during cylindrical grip along with the thenar muscles.48 During pad-to-pad and tip-to-tip prehension, the FPL is important to control IP flexion.48 The function of the FPL along with the APL is essential to maintain the longitudinal arch of the thumb. The patient is unable to form a circle with tip-to-tip pinch between the thumb and the index finger with severe weakness of the FPL. This is referred to as a positive circle sign.78 Shortness, stiffness, or adhesion of the FPL results in flexion of the thumb IP joint when the thumb and wrist are extended.
Hypothenar Muscles
During cylindrical grip, the muscles of hypothenar eminence are active.48 When working with patients that have limited flexion of the ulnar fingers caused by stiffness of the joints, there is often insufficient recruitment of the hypothenar muscles. Specific cues to contract these muscles, especially the FDM, help the patient recruit these muscles. We have not observed shortness of these muscles. All of the hypothenar muscles help cup or deepen the concavity of the palm,13,19 which is required for grasping objects and normal functional use of the hand.
The ADM abducts the MP joint of the small finger and assists in opposition and flexion of the small finger. The ADM also assists in extension of the IP joints through its attachment into the extensor expansion.13 The FCU stabilizes the pisiform during contraction of the ADM.65 An imbalance between the forces of the FCU and ADM caused by repeated abduction of the small finger with the wrist in excessive extension may result in pain in the region of the pisiform or pisotriquetral joint.
The opponens digiti minimi (ODM) opposes the small finger (flexion with slight rotation of the CMC joint) so it is possible to perform tip-to-tip prehension between the little finger and the thumb. The ODM also helps deepen the transverse arch or “cup” the palm.13
The FDM flexes the MP joint of the small finger and assists in opposing the little finger to the thumb.13
Movement System Syndromes of the Hand
The proposed movement system syndromes of the hand have been developed based on clinical experience and examination of the literature but are still a “work-in-progress” and need testing and refining based on feedback from other clinicians with expertise in treating patients with hand problems.
To our knowledge, no other classification systems have been described to guide physical therapy management of the patient with hand dysfunction. Commonly, it is the physician’s diagnoses related to the pathoanatomical source of pain, established protocols, and isolated impairments that guide treatment. The premise of this chapter is that syndromes are composed of clusters of impairments and when identified, more effectively guide physical therapy management of patients with hand problems than if no movement system diagnosis has been made. The physician’s diagnosis, while important and helpful, is not sufficient to guide the physical therapy management of the patient with hand problems. For patients whose treatment is guided by protocols, it is still important for the therapist to identify the cause (source) of the symptoms and signs. Thus the diagnoses presented here have two parts: one that identifies the principal movement that is impaired and the second that identifies the tissue that is the source of the impaired movement.
Some patients with hand symptoms have problems that are not guided by established protocols. Based on the premise that the physical therapist has primary expertise in analysis of the movement system, we have developed a set of movement system–based syndromes for the hand to guide physical therapy treatment of these patients. The syndromes are named either for the alignments and movements that appear to be related to the patient’s symptom behavior or for the primary cause of the patient’s impairments. The focus of the diagnoses is on the movement that produces the symptoms rather than the pathoanatomical source of the symptoms. In many cases, the symptom is associated with movement, thus we believe that alterations in the precision of movement are the cause of the tissue irritation and need to be corrected to achieve optimal outcomes. A patient might be assigned more than one syndrome, but usually, one syndrome is primary.
This section of the chapter focuses on the overall description of each syndrome and on symptoms and history, key tests and signs, and source of signs and symptoms (the first three columns of the Chapter 5 Appendix). The Chapter 5 Appendix includes a complete description of each syndrome, as well as associated signs or contributing factors and differential diagnosis for each syndrome.
Insufficient Finger and/or Thumb Flexion Syndrome
The principal impairment of insufficient finger and/or thumb flexion syndrome is limited finger or thumb flexion AROM, but the key to prescribing the appropriate treatment is differentiating between the sources causing the limited flexion. The sources of the limited flexion can be broadly classified into two main categories: hypomobility (physiological and accessory motion) and force production deficit (decreased strength). Insufficient finger and/or thumb flexion syndrome is most commonly secondary to a trauma or injury or after a period of immobilization to allow for tissue healing. In the acute stage, these patients may be assigned a hand impairment diagnosis Stage 1, but an underlying movement system diagnosis of insufficient finger or thumb flexion may help guide treatment. As the tissues heal, the diagnosis may change from pathoanatomical source or regional hand impairment to another movement system diagnosis. Items 1 to 11 in the following list are the potential causes (source of signs and symptoms) of insufficient finger or thumb flexion. The identified cause of insufficient finger and/or thumb flexion is the second part of the name of the syndrome. Insufficient finger or thumb flexion may be caused by the following:
Symptoms and History
Patients with insufficient finger and/or thumb flexion may complain of (1) the inability to make a fist, (2) difficulty gripping objects, and (3) difficulty using the involved hand for functional activities such as feeding, dressing, and writing. They usually report symptoms in the hand or forearm and may report swelling in the hand, wrist or forearm. They may also report numbness and tingling. Patients that have insufficient finger and/or thumb flexion may be referred to physical therapy with the following common referring diagnoses: status/postsynovectomy for arthritis, extensor or flexor tendon repair, tendon adhesion, ligament sprain (grade I or II), stiffness after fracture, or nerve injury. Patients with insufficient finger and/or thumb flexion may also be in the later healing stages after any of the surgical procedures listed for the hand impairment diagnosis in Box 5-1.
Key Tests and Signs
Alignment Analysis
Impairments in alignment and appearance for patients with this syndrome include joints that are red and swollen compared to the opposite hand, scar on flexor or extensor surface, resting alignment of decreased flexion of one or more joints of the involved finger, resting alignment of MPs in extension with increased IP flexion, and adducted thumb (typical stiff-hand posture). See Box 5-2 for examination and treatment for scar and edema.
Movement Impairment Analysis
Movement impairments noted in this syndrome include (1) the joint adjacent to the joint with the limited flexion flexes more readily than the joint that is limited; (2) during finger flexion; the wrist or fingers move into extension if the finger extensors are short13 or adhered; and (3) during finger flexion the wrist flexes if the finger joint structures are the source of the limited finger flexion and the wrist is relatively less stiff or the wrist extensors are weak.
Joint Integrity
Active and passive finger and/or thumb ROM should be assessed; and active flexion will be limited at one or more joints. Passive flexion and extension of the fingers and/or thumb may or may not be limited; depending on the cause of the limitation. The onset of pain is often at the end-range of the flexion ROM (see the “Source of Signs and Symptoms” section for further explanation). Table 5-1 includes the procedure for restricted joint motion testing.
TABLE 5-1 Procedures for Testing Restricted Joint Motion and Muscle Length
Ligament integrity and/or length.
One of the sources of limitation of finger and/or thumb flexion can be the joint structures, including the MP collateral ligaments, the ORL, and the dorsal capsule.19,79 Examination of the hand should include testing for integrity and length of the ligaments and differentiating whether the limitation of flexion ROM is the result of the joint structures or other causes. See Table 5-1 for specific procedures for these tests.
Muscle Length Tests
Tests of muscle length must be performed passively. Particular attention is paid to the amount of resistance to stretch (stiffness) throughout the ROM during the test and to which joint moves most easily. The length tests provide information regarding whether the limitation of flexion ROM is due to shortness or adhesion of the respective muscle and/or tendon. The tests of muscle length that should be performed are extrinsic finger or thumb flexors, extrinsic finger or thumb extensors, and the interossei muscles (see Table 5-1 for specific procedures).
Muscle Strength/Performance Impairments
Assessing strength is important to determine the source of the signs assuming there are no precautions regarding risk of injury to the tissues. Tests of strength include: grip and pinch strength using a grip dynamometer and a pinch gauge and MMT of the finger and/or thumb flexors.13,19 Strength may be decreased as the result of weakness of the extrinsic finger and/or thumb flexors or intrinsics or decreased gliding of the tendons.13,68,79 When performing these tests, the examiner should note the preferred pattern of movement and any impairments compared to normal. Impairments include limited ROM or an alteration in the sequencing and timing of joint movement.
Source of Signs and Symptoms
Based on the findings from a comprehensive examination, impairments are identified. Determination of the source of the signs and symptoms requires knowledge of and recognition of the cluster of impairments that are characteristic of each source. Identifying the source will guide management of the patient more effectively and efficiently than treating isolated impairments. For example, if treatment is focused on isolated impairments one could conclude that weakness is the cause of AROM into flexion being less than PROM (when PROM into flexion is normal). The appropriate treatment for weakness would be to overload the muscle to build strength. However, if the source of the limitation of AROM into flexion is flexor tendon adhesion, the initial focus of treatment would instead be restoring gliding of the flexor tendons. The clusters of impairments for each potential source and/or cause of insufficient finger or thumb flexion are as follows.
Hypomobility
Flexor Tendon Adhesion (Figure 5-53)
Extensor Tendon Adhesions (Figure 5-54, p. 213)
Extensor Muscle Shortness (Figure 5-55, p. 213)
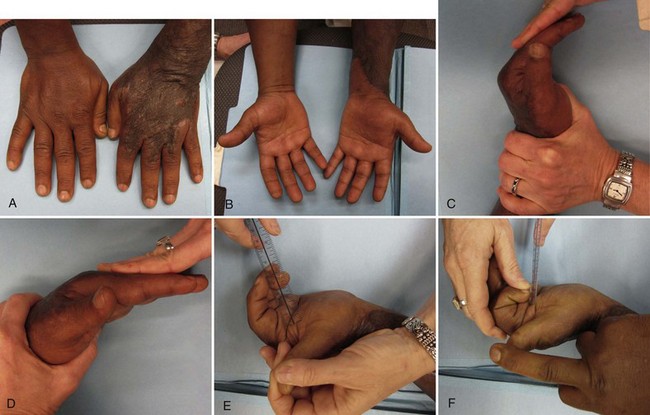
Figure 5-55 Insufficient finger flexion caused by extrinsic extensor shortness and dorsal scar. A, Appearance of dorsal scar. B, Appearance of anterior surface of hands and forearms. C to D, Passive range of MP flexion with wrist extended greater than passive MP flexion with wrist flexed. E, Active range of composite finger flexion. F, Passive range of composite finger flexion.
Metacarpophalangeal Collateral Ligament Shortness or Adhesion (Figure 5-56)
Interphalangeal Joint Dorsal Capsule Shortness or Adhesion (see Figure 5-56)
Shortness of Oblique Retinacular Ligament (Figure 5-57)
Shortness of Interossei and Lumbricals (Figure 5-58)
Swan Neck Deformity33 (see Figure 5-9)
Force Production Deficit
Insufficient finger flexion caused by force production deficit is likely the result of either weakness caused by ulnar or median nerve injury or rupture of the extrinsic flexor tendons.
Weakness of Finger and/or Thumb Flexors
Rupture of Finger and/or Thumb Flexors (see Figure 5-59)
Associated Signs or Contributing Factors
Patients with insufficient finger flexion usually present with associated edema and scarring of the hand or forearm and less frequently loss of sensation. Although these impairments are important to identify and treat, they are not key findings that help differentiate between diagnoses. For this reason, edema, scar, and sensation are listed as “associated signs or contributing factors.” See the Chapter 5 Appendix and Box 5-2 for the tests and treatment used to manage edema and scar. The Chapter 5 Appendix includes the complete listing of associated signs or contributing factors for this syndrome.
Differential Diagnosis
The movement system diagnoses, finger flexion with or without rotation syndrome and hand impairment, are those syndromes that most closely overlap with insufficient finger and/or thumb flexion and should therefore be ruled out during the examination of the patient. Source or regional impairment of the hand is discussed briefly in this chapter as it relates to patients with hand injuries, but Chapter 2 describes those diagnoses in more detail. Finger rotation with or without rotation syndrome is discussed in more detail later in this chapter, as well as the Chapter 5 Appendix.
Potential diagnoses requiring referral, as suggested by the patient’s signs and symptoms, are diagnoses of neuromusculoskeletal, visceral, or systemic origin that indicate that the patient should be referred to the physician for further evaluation. Refer to the Chapter 5 Appendix for the listing of these conditions.
Treatment
The Chapter 5 Appendix includes a description of treatment for each of the causes of insufficient finger and/or thumb flexion. Box 5-2 includes description of the treatment of scar and edema. Treatment for sensory deficits is not be covered here because it is covered well in other texts.74
The usual expectation is that AROM should increase by a minimum of 10 degrees per week except when the cause of the limitation is due to profound weakness or rupture. If ROM is not improving by at least 10 degrees per week, then more aggressive treatment, such as passive stretching or splinting, should be considered. However, pain and edema should be decreasing gradually over the course of treatment. If pain and edema are not decreasing, one reason could be that the treatment is too aggressive, resulting in the lack of progress with ROM (see Box 5-2).