Chapter 32 Emulsions
Introduction
An emulsion consists of two immiscible liquids, one of which is uniformly dispersed throughout the other as fine droplets normally of diameter 0.1–100 μm. To prepare a stable emulsion, a third ingredient, an emulsifying agent, is required. Oral emulsions are stabilized oil-in-water dispersions that may contain one or more active ingredients. They are a useful way of presenting oils and fats in a palatable form. Emulsions for external use are known as lotions, applications or liniments if liquid, or creams if semi-solid in nature. Some parenteral products may also be formulated as emulsions. Most important of these is total parenteral nutrition (TPN), which is discussed in detail in Chapter 41. Pharmaceutically, the term ‘emulsion’, when no other qualification is used, is taken to mean an oil-in-water preparation for internal use. Information about other types of emulsion, together with some of the science of emulsions, can be found in Aulton (2007).
Pharmaceutical applications of emulsions
Emulsions have a wide range of uses, including:
Examples of emulsions for oral use are cod liver oil emulsion (see Example 32.3), liquid paraffin oral emulsion (see Example 32.4) and castor oil emulsion. Examples of emulsions for external use are Turpentine Liniment BP (see Example 33.3) and Oily Calamine Lotion BP (see Example 32.5).
Example 32.1
Calculate the quantities for a primary emulsion for the following:
 |
||
| Cod liver oil | 30 mL | |
| Water | to 100 mL | |
| Primary emulsion quantities: | ||
| Cod liver oil is a fixed oil, therefore the primary emulsion proportions are 4:2:1. Hence: | ||
| Cod liver oil | 30 mL | 4 parts |
| Water | 15 mL | 2 parts |
| Powdered acacia gum | 7.5 g | 1 part |
Example 32.2
 Calciferol solution, 0.15 mL per 5 mL dose.
Calciferol solution, 0.15 mL per 5 mL dose.
The percentage of oil in each dose is 3%. The oil content must be made up to at least 20% to produce a stable emulsion.
Since 20% of 5 mL = 1 mL, the volume of bland oil required is 1.0−0.15 = 0.85 mL.
Formula for primary emulsion (for 50 mL):
| Calciferol solution | 1.5 mL | 4 parts |
| Cottonseed oil | 8.5 mL | |
| Water | 5 mL | 2 parts |
| Acacia | 2.5 g | 1 part |
Example 32.3
 Prepare 200 mL cod liver oil emulsion to the following formula:
Prepare 200 mL cod liver oil emulsion to the following formula:
| Cod liver oil | 60 mL |
| Chloroform | 0.4 mL |
| Cinnamon water | to 200 mL |
Emulsion types
Emulsions may be oil-in-water (o/w) emulsions, where oil is the disperse phase in a continuous phase of water, or water-in-oil (w/o) emulsions, where water is the disperse phase in a continuous phase of oil. It is also possible to form a multiple emulsion, e.g. a water droplet enclosed in an oil droplet, which is itself dispersed in water – a w/o/w emulsion. These may be used for delayed-action drug delivery systems.
If the emulsion is for oral or intravenous administration it will always be oil-in-water. Intramuscular injections may be water-in-oil for depot therapy. When selecting emulsion type for preparations for external use, the therapeutic use, texture and patient acceptability will be taken into account. Oil-in-water emulsions are less greasy, easily washed off the skin and more cosmetically acceptable than water-in-oil emulsions. They have an occlusive effect, which hydrates the upper layers of the skin (called an emollient, see Ch. 33). Water-in-oil emulsions rub in more easily.
Identification of emulsion type
There is a range of tests available to identify the emulsion type. Some of the tests that can be used are outlined below.
Miscibility test. An emulsion will only mix with a liquid that is miscible with its continuous phase. Therefore an o/w emulsion is miscible with water, a w/o emulsion with an oil.
Conductivity measurement. Systems with an aqueous continuous phase will conduct electricity, while systems with an oily continuous phase will not.
Staining test. A dry filter paper impregnated with cobalt chloride turns from blue to pink on exposure to stable o/w emulsions.
Dye test. If an oil-soluble dye is used, o/w emulsions are paler in colour than w/o emulsions. If examined microscopically, an o/w emulsion will appear as coloured globules on a colourless background while a w/o emulsion will appear as colourless globules against a coloured background.
Formulation of emulsions
An ideal emulsion has globules of disperse phase that retain their initial character, that is the mean globule size does not change and the globules remain evenly distributed. The formulation of emulsions involves the prevention of coalescence of the disperse phase (often called ‘cracking’) and reducing the rate of creaming.
Emulsifying agents
Emulsifying agents help the production of a stable emulsion by reducing interfacial tension and then maintaining the separation of the droplets by forming a barrier at the interface. Most emulsifying agents are surface-active agents. Emulsion type is determined mainly by the solubility of the emulsifying agent. If the emulsifying agent is more soluble in water (i.e. hydrophilic) then water will be the continuous phase and an o/w emulsion will be formed. If the emulsifying agent is more soluble in oil (i.e. lipophilic), oil will be the continuous phase and a w/o emulsion will be formed. If a substance is added which alters the solubility of the emulsifying agent, this balance may be altered and the emulsion may change type. The process is called phase inversion. The ideal emulsifying agent is colourless, odourless, tasteless, non-toxic, non-irritant and able to produce stable emulsions at low concentrations.
Emulsifying agents can be classed into three groups: naturally occurring, synthetic surfactants and finely divided solids.
Naturally occurring emulsifying agents
These agents come from vegetable or animal sources. Therefore the quality may vary from batch to batch and they are susceptible to microbial contamination and degradation.
Polysaccharides. Acacia is the best emulsifying agent for extemporaneously prepared oral emulsions as it forms a thick film at the oil–water interface to act as a barrier to coalescence. It is too sticky for external use. Tragacanth is used to increase the viscosity of an emulsion and prevent creaming. Other polysaccharides, such as starch, pectin and carrageenan, are used to stabilize an emulsion.
Semi-synthetic polysaccharides. Low-viscosity grades of methylcellulose (see Example 32.4) and carboxymethylcellulose will form o/w emulsions.
Sterol-containing substances. These agents act as water-in-oil emulsifying agents. Examples include beeswax, wool fat and wool alcohols (see Ch. 33).
Synthetic surfactants
These agents are classified according to their ionic characteristics as anionic, cationic, non-ionic and ampholytic. The latter are used in detergents and soaps but are not widely used in pharmacy.
Anionic surfactants. These are organic salts which, in water, have a surface-active anion. They are incompatible with some organic and inorganic cations and with large organic cations such as cetrimide. They are widely used in external preparations as o/w emulsifying agents. They must be in their ionized form to be effective and emulsions made with anionic surfactants are generally stable at more alkaline pH.
Many different ones are used pharmaceutically. Some examples include:
Cationic surfactants. These are usually quaternary ammonium compounds which have a surface-active cation and so are sensitive to anionic surfactants and drugs. They are used in the preparation of o/w emulsions for external use and must be in their ionized form to be effective. Emulsions formed by a cationic surfactant are generally stable at acidic pH. The cationic surfactants also have antimicrobial activity. Examples include cetrimide and benzalkonium chloride.
Non-ionic surfactants. These are synthetic materials and make up the largest group of surfactants. They are used to produce either o/w or w/o emulsions for both external and internal use. The non-ionic surfactants are compatible with both anionic and cationic substances and are highly resistant to pH change. The type of emulsion formed depends on the balance between hydrophilic and lipophilic groups which is expressed as the HLB (hydrophilic–lipophilic balance) number (see below). Examples of the main types include glycol and glycerol esters, macrogol ethers and esters, sorbitan esters and polysorbates.
The HLB (hydrophilic–lipophilic balance) system. An HLB number, usually between 1 and 20, is allocated to an emulsifying agent and represents the relative proportions of the lipophilic and hydrophilic parts of the molecule. The lower the number, the more oil soluble the emulsifying agent. Higher numbers (8–18) indicate a hydrophilic molecule which produces an o/w emulsion. Low numbers (3–6) indicate a lipophilic molecule which produces a w/o emulsion. Oils and waxy materials have a ‘required HLB number’ which helps in the selection of appropriate emulsifying agents when formulating emulsions. Liquid paraffin, for example, has a required HLB value of 4 to obtain a w/o emulsion and 12 for an o/w emulsion. Two or more surfactants can be combined to achieve a suitable HLB value and often give better results than one surfactant alone. (See Aulton (2007) or the Pharmaceutical Codex for more details.) HLB values of some commonly used emulsifying agents are given in Table 32.1.
Table 32.1 HLB values of emulsifying agents
| Emulsifying agent | HLB value |
| Acacia | 8.0 |
| Sorbitan laurate (Span 20®) | 8.6 |
| Sorbitan stearate (Span 60®) | 4.7 |
| Polysorbate 20 (Tween 20®) | 16.7 |
| Polysorbate 80 (Tween 80®) | 15.0 |
| Sodium lauryl sulphate | 40.0 |
| Sodium oleate | 18.0 |
| Tragacanth | 13.2 |
| Triethanolamine oleate | 12.0 |
Finely divided solids
Finely divided solids can be adsorbed at the oil–water interface to form a coherent film that prevents coalescence of the dispersed globules. If the solid particles are preferentially wetted by oil, a w/o emulsion is formed. Conversely, if the particles are preferentially wetted by water, an o/w emulsion is formed. They form emulsions with good stability which are less prone to microbial contamination than those formed with other naturally derived agents. Examples are bentonite, aluminium magnesium silicate and colloidal silicon dioxide. Colloidal aluminium and magnesium hydroxides are used for internal preparations. For example liquid paraffin and magnesium hydroxide oral emulsion is stabilized by the magnesium hydroxide.
Choosing an emulsifying agent
The active ingredients that are to be emulsified and the intended use of the product will determine the choice of emulsifying agent. Because they are non-toxic and non-irritant, the natural polysaccharides (acacia) and non-ionic emulsifying agents are useful for internal emulsions. Quillaia can be used in low concentrations, but soap emulsions irritate the gastrointestinal tract and have a laxative effect. The taste should be bland and palatable, again suggesting the use of natural polysaccharides. Polysorbates have a disagreeable taste, therefore flavouring ingredients are necessary. Only certain non-ionic emulsifying agents are suitable for parenteral use including lecithin, polysorbate 80, methylcellulose, gelatin and serum albumin. A wider range of emulsifying agents can be used externally, although the polysaccharides are normally considered too sticky.
Antioxidants
Some oils are liable to degradation by oxidation and therefore antioxidants may be added to the formulation. They should be preferentially soluble in the oily phase.
Antimicrobial preservatives
Emulsions contain water, which will support microbial growth. Microbes produce unpleasant odours, colour changes and gases. In addition they may affect the emulsifying agent, possibly causing the breakdown of the emulsion. Other ingredients in emulsions can provide a growth medium for microbes. Examples include arachis oil which supports Aspergillus species and liquid paraffin which supports Penicillium species. Contamination may be introduced from a variety of sources including:
Antimicrobial preservative agents should be free from toxic effects, odour, taste (for internal use) and colour. They should be bactericidal rather than bacteriostatic, have a rapid action and wide antibacterial spectrum over a range of temperatures and pH. Additionally emulsion ingredients should not affect their activity and they should be resistant to attack by microorganisms. The effect of the partition coefficient is also important. Microbial growth normally occurs in the aqueous phase of an emulsion, therefore it is important that a sufficient concentration of preservative is present in the aqueous phase. A preservative with a low oil/water partition coefficient will have a higher concentration in the aqueous phase. A combination of preservatives may give the best preservative cover for an emulsion system. The ratio of the disperse phase volume to the total volume is known as the phase volume or phase volume ratio. If, for example, a preservative is soluble in the oil and if the proportion of oil is increased, the concentration of preservative in the aqueous phase decreases. This could reduce the concentration in the aqueous phase below an effective concentration.
Colours and flavourings
Colour is rarely needed in an emulsion, as most have an elegant white colour and thick texture. Emulsions for oral use will usually contain some flavouring agent.
Stability of emulsions
Phase inversion
This is the process in which an emulsion changes from one type to another, say o/w to w/o. The most stable range of disperse phase concentration is 30–60%. As the amount of disperse phase approaches or exceeds a theoretical maximum of 74% of the total volume, so the tendency for phase inversion to occur increases. Addition of substances which alter the solubility of an emulsifying agent may also cause phase inversion. The process is irreversible.
Creaming
The term ‘creaming’ is used to describe the aggregation of globules of the disperse phase at the top or bottom of the emulsion, similar to cream on milk. The process is reversible and gentle shaking redistributes the droplets throughout the continuous phase. Creaming is undesirable because it is inelegant and inaccurate dosing is possible if shaking is not thorough. Additionally, creaming increases the likelihood of coalescence of globules and therefore the breakdown of the emulsion due to cracking.
Cracking
Cracking is the coalescence of dispersed globules and separation of the disperse phase as a separate layer. It is an irreversible process and redispersion cannot be achieved by shaking.
Causes and prevention of cracking or creaming
Dispensing emulsions
Emulsions can be extemporaneously prepared on a small scale using a mortar and pestle. Electric mixers can also be used, although incorporation of excess air may be a problem. All equipment used must be thoroughly clean and dry. All oil-soluble and water-soluble components of the emulsion are separately dissolved in the appropriate phase. A suitable emulsifying agent must then be used.
Emulsions for oral use
Acacia gum is usually used when making extemporaneous o/w emulsions for oral use, unless otherwise specified. A primary emulsion should be prepared first. This is a thick, stable emulsion prepared using optimal proportions of the ingredients. These vary with the nature of the oil.
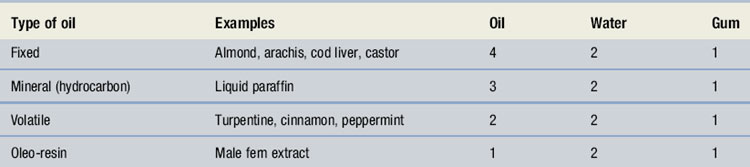
Calculating quantities for primary emulsions
Proportions or ‘parts’ for preparation of primary emulsions are given in Table 32.2. These refer to parts by volume for the different types of oil and water and weight for the acacia gum. If more than one oil is to be incorporated, the quantity of acacia for each is calculated separately and the sum of the quantities used.
Variations to primary emulsion calculations
If the proportion of oil is too small, modifications must be made. Acacia emulsions containing less than 20% oil tend to cream readily. A bland, inert oil, such as arachis, sesame, cottonseed or maize oil, should be added to increase the amount of oil and so prevent this from happening. Care should be taken in selection of the bulking oil because of the increasing incidence of nut allergy. It is often, therefore, advisable to avoid oils such as arachis, especially for children.
Methods of preparation of extemporaneous emulsions
There are two possible methods, the dry gum method being the more popular.
Dry gum method of preparation
Wet gum method of preparation
Water is added to the acacia gum and quickly triturated until the gum has dissolved to make a mucilage. Oil is added to this mucilage in small portions, triturating the mixture thoroughly after each addition until a thick primary emulsion is obtained. The primary emulsion should be stabilized by mixing for several minutes and then completed in the same way as for the dry gum method.
Problems when producing the primary emulsion
The primary emulsion may not form and a thin oily liquid is formed instead. Possible causes are:
Emulsions for external use
Liquid or semi-liquid emulsions may be used as applications, liniments and lotions (see Ch. 33). The extemporaneous preparation of emulsions for external use does not require the preparation of a primary emulsion. Soaps are commonly used as the emulsifying agent and some are prepared ‘in situ’ by mixing the oily phase containing a fatty acid and the aqueous phase containing the alkali. Alternatively the emulsifying agent can be dissolved in the oily or aqueous phase and the disperse phase added to the continuous phase, either gradually or in one portion.
Creams are semi-solid emulsions which may be o/w (e.g. aqueous cream) or w/o (e.g. oily cream). These are considered in more detail in Chapter 33.
Shelf life and storage
Emulsions should be stored at room temperature and will either be recently or freshly prepared. Some official preparations will have specific expiry dates. They should not be frozen.
Containers
An amber medicine bottle is used, plain for internal use and ribbed for external use, with an airtight child-resistant closure. Containers with a wide mouth are useful for very viscous preparations.
Special labelling and advice for emulsions
Action and uses. A rich source of vitamins A and D.
Formulation notes. Cod liver oil is a fixed oil that requires the addition of acacia gum as an emulsifying agent. The proportions are 4 oil : 2 water : 1 gum. Therefore 60 mL cod liver oil, 30 mL of cinnamon water and 15 g of acacia gum will be used to prepare the primary emulsion. Cinnamon water acts as a flavouring agent and vehicle. It may need to be prepared from concentrated cinnamon water, at a dilution of 1 part to 39 parts of water. Since 60 mL of the emulsion is the cod liver oil, it is not necessary to prepare 200 mL of cinnamon water, so 160 mL is adequate. Therefore, 4 mL of concentrated cinnamon water will be diluted to 160 mL with water. Chloroform is dense and only slowly soluble and acts as a preservative.
Method of preparation. Use the dry gum method. Weigh 15 g of acacia, measure 60 mL of cod liver oil and 30 mL of cinnamon water, which will be used to create the primary emulsion. Place the cod liver oil in a dry, flat-bottomed mortar. Add the acacia and mix very lightly and briefly. Immediately add the cinnamon water, mixing vigorously until a clicking sound is heard and a white primary emulsion is formed. Continue mixing for a few minutes to stabilize the primary emulsion. Scrape the mortar and pestle with a spatula to ensure that all the oil is incorporated. Add the chloroform by pipette and mix thoroughly. Gradually add most of the remainder of the cinnamon water to the emulsion in the mortar, stirring well between additions. Transfer the emulsion to a 200 mL measure, rinsing the mortar with cinnamon water, adding these washings to the measure. Make up to volume with cinnamon water and pack in an amber medicine bottle with a child-resistant closure. Polish and label the bottle and give a 5 mL medicine spoon with the medicine.
Shelf life and storage. Store in a cool, dry place. It is recently prepared, therefore a shelf life of 2–3 weeks is applicable.
Advice and labelling. This is an unofficial formula, and should be labelled ‘Cod liver oil 30% v/v emulsion’. ‘Shake well before use’. A normal dose is 10 mL three times a day, with or after food.
Action and uses. A lubricant laxative for chronic constipation.
Formulation notes. Methylcellulose 20 at a concentration of 2% acts as an emulsifying agent for the mineral oil, liquid paraffin. A primary emulsion is not required. Benzoic acid and chloroform act as preservatives and vanillin and saccharin sodium act as flavouring and sweetening agent respectively. The amount of saccharin sodium is not weighable on a dispensing balance and will be obtained by trituration using water as the diluent (since this is the vehicle for the emulsion).
Trituration for saccharin sodium:
| Saccharin sodium | 100 mg |
| Water | to 100 mL |
5 mL of water will contain 5 mg of saccharin sodium.
Method of preparation. Firstly, prepare a mucilage by mixing the methylcellulose 20 with about six times its weight of boiling water and allow to stand for 30 minutes to hydrate. Add an equal weight (about 15 g) of ice and stir mechanically until the mucilage is homogeneous. Dissolve the vanillin in the benzoic acid solution and chloroform. Add this mixture to the mucilage and stir for 5 minutes. Make up the saccharin sodium trituration and stir in the appropriate volume of solution to the mucilage. Make the volume of the mucilage up to 50 mL, taking care to ensure that there is no entrapped air in the mucilage. Make the emulsion by mixing together 50 mL of liquid paraffin and 50 mL of prepared mucilage with constant stirring. The emulsion is more stable if passed through a hand homogenizer. Pack in an amber medicine bottle with a child-resistant closure. Shake well to ensure that the emulsion is thoroughly mixed. Polish and label the bottle and give a 5 mL medicine spoon with the medicine.
Shelf life and storage. Store in a cool, dry place. This is an official preparation and should remain stable on storage, however a 4-week expiry date is recommended.
Advice and labelling. ‘Shake well before use’. The emulsion should not be taken within 30 minutes of meal times and preferably on an empty stomach. It should not be taken at bedtime. The importance of fibre and fluid intake in the diet should be emphasized.
Action and uses. Soothing lotion for the treatment of eczema, sunburn and other inflammatory conditions.
Formulation notes. The emulsifying agent for the arachis oil is the soap calcium oleate produced from the calcium hydroxide and oleic acid when they are shaken together. Wool fat is included as an emulsion stabilizer. This is a w/o emulsion.
Method of preparation. The wool fat, oleic acid and arachis oil should be warmed gently together in an evaporating basin (using a water bath or heating block) until melted. Mix them thoroughly. The calamine should be sieved and weighed and placed on a warm ointment tile. Add a little of the oily mixture and rub in with a large spatula until smooth. Gradually add more of the oily mixture until it is fluid. Transfer back to the evaporating basin and stir to evenly distribute the calamine powder. Pour into a previously tared, amber ribbed bottle and add the calcium hydroxide solution to the bottle in small amounts, shaking well between additions. Make up to volume and seal with a child-resistant closure. Polish and label the bottle.
Shelf life and storage. Store in a cool, dry place. It is unpreserved, therefore a shelf life of 2–3 weeks is applicable.
Advice and labelling. ‘Shake well before use’ and ‘For external use only’.