Chapter 47 Gas Exchange
1. The composition of a gas mixture can be described by the fractional composition or partial pressure.
2. Alveolar gas composition is determined by alveolar ventilation and the exchange of oxygen and carbon dioxide.
3. Exchange of oxygen and carbon dioxide between the alveolus and pulmonary capillary blood occurs by diffusion.
4. The exchange of gases between the tissues and blood also occurs by diffusion.
5. The amount of alveolar ventilation in relation to pulmonary capillary blood flow—the  /
/ ratio—determines the adequacy of pulmonary gas exchange.
ratio—determines the adequacy of pulmonary gas exchange.
6. The composition of the systemic arterial blood is determined by the composition of the capillary blood that drains each alveolus.
7. Right-to-left vascular shunts allow blood to bypass ventilated lung.
8. Part of each breath ventilates dead-space and does not participate in gas exchange.
9. Arterial oxygen (Pao2) and carbon dioxide (Paco2) tensions are measured to evaluate gas exchange.
The Composition of a Gas Mixture Can Be Described by the Fractional Composition or Partial Pressure
Understanding gas exchange requires an understanding of the measurement of gas composition and the forces causing gas movement within the lungs, blood, and tissues. For convenience, physiologists use many abbreviations when describing gas exchange (Table 47-1). Air contains 21% oxygen (the fraction of oxygen in inspired air, FIo2, is 0.21). High in the Andes Mountains, the air still contains 21% oxygen, but mammals develop hypoxia at those altitudes. Clearly, therefore, it is not only the fraction of oxygen that is important for gas exchange; the hypoxia at high altitude is a result of the low barometric pressure. At this lower barometric pressure, the oxygen molecules are less densely packed, and therefore the partial pressure of oxygen (Po2) in the air is decreased. It is this partial pressure (also called tension) and, of more importance, the partial pressure difference, that is important in gas transfer.
Table 47-1 Common Abbreviations Used in Gas Exchange
| Abbreviation | Definition |
|---|---|
| AaDO2 | Alveolar-to-arterial oxygen tension difference |
| FIO2 | Fraction of oxygen in inspired air |
| FO2 | Fraction of oxygen in the gas mixture |
| PaCO2 | Arterial carbon dioxide tension |
| PACO2 | Alveolar carbon dioxide tension |
| PaO2 | Arterial oxygen tension |
| PAO2 | Alveolar oxygen tension |
| PB | Barometric pressure |
| PcapCO2 | Capillary carbon dioxide tension |
| PcapO2 | Capillary oxygen tension |
| PCO2 | Carbon dioxide tension |
| PH2O | Partial pressure of water vapor |
| PIO2 | Inspired oxygen tension |
| PO2 | Oxygen tension |
| PvCO2 | Carbon dioxide tension of venous blood |
| PvO2 | Oxygen tension of venous blood |
 |
Perfusion |
| R | Respiratory exchange ratio |
 |
Ventilation |
 A A |
Amount of alveolar ventilation |
 co2 co2 |
Rate of carbon dioxide production |
 o2 o2 |
Rate of oxygen movement between alveolus and blood |
 / / |
Ratio of alveolar ventilation to pulmonary capillary blood flow |
The oxygen tension (Po2) of a dry gas mixture is determined by barometric pressure (PB) and the fraction of oxygen (Fo2) in the gas mixture, as follows:
In the atmosphere, FIo2 is 0.21, so Po2 in dry air at sea level when PB = 760 mm Hg is approximately 160 mm Hg:
Po2 decreases at higher altitudes because barometric pressure decreases.
During inhalation, air is warmed to body temperature and humidified in the larger air passages. The concentration of other gases is reduced by the presence of water vapor molecules; therefore, Po2 decreases. The Po2 of humidified gas is calculated as follows:
where PH2O is the partial pressure of water vapor at body temperature. The PH2O is determined by the temperature and percentage saturation of the air with water. In a mammal with a body temperature of 38.2°C, PH2O in saturated air equals 50 mm Hg; therefore the Po2 of warmed, completely humidified gas in the conducting airways is approximately 149 mm Hg:
Alveolar Gas Composition Is Determined by Alveolar Ventilation and the Exchange of Oxygen and Carbon Dioxide
Because there is only a negligible amount of carbon dioxide in the inspired air, PAco2 is determined by the rate of carbon dioxide production ( co2) in relation to the amount of alveolar ventilation (
co2) in relation to the amount of alveolar ventilation ( A):
A):
where K = PB − PH2O.
It is obvious from this equation that if  co2 increases, as occurs during exercise,
co2 increases, as occurs during exercise,  A must also increase if PACo2 is to remain constant. If
A must also increase if PACo2 is to remain constant. If  A does not increase sufficiently, PAco2 rises. Similarly, if
A does not increase sufficiently, PAco2 rises. Similarly, if  co2 remains constant and
co2 remains constant and  A halves, PAco2 doubles.
A halves, PAco2 doubles.
Po2 is lower in the alveolus than in inspired air because oxygen and carbon dioxide exchange occurs continually. During breathing, alveolar oxygen tension (PAo2) fluctuates around an average value, increasing during inhalation and decreasing during exhalation. The average oxygen tension in the alveoli of the lung can be calculated from the alveolar gas equation, a simplified version of which follows:
where R, the respiratory exchange ratio, is the ratio of the rate of carbon dioxide production to that of oxygen consumption. The respiratory exchange ratio is determined by the substrates being metabolized by the animal. This equation demonstrates that alveolar oxygen tension is determined by the inspired oxygen tension and the exchange of oxygen for carbon dioxide. Assuming an average R of 0.8 and an alveolar carbon dioxide tension (PAco2) of 4.0 mm Hg, PAo2 averages approximately 100 mm Hg at sea level, where PB is 760 mm Hg. The alveolar gas equation also shows that whenever PAco2 increases, PAo2 decreases, and vice versa.
Alveolar hypoventilation, a decrease in alveolar ventilation in relation to carbon dioxide production, elevates PAco2 and decreases PAo2. Figure 47-1 shows the causes of alveolar hypoventilation. It occurs when (1) the central nervous system is depressed by drugs or injury, (2) there is damage to the peripheral nerves, (3) there is damage to the thorax and respiratory muscles, (4) there is severe airway obstruction (e.g., in exercising horses with laryngeal hemiplegia) or (5) there is severe lung disease that decreases lung compliance.
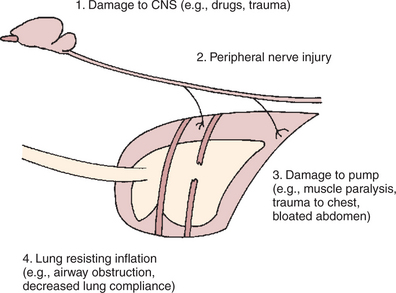
FIGURE 47-1 Diagrammatic representation of the brain, peripheral nerves, thorax, airways, and lung to show the causes of alveolar hypoventilation.
The converse of alveolar hypoventilation, alveolar hyperventilation, causes a decrease in PAco2 because ventilation is increased in relation to carbon dioxide production. Therefore, according to the alveolar gas equation, as PAco2 decreases, PAo2 increases. Hyperventilation occurs when the need to ventilate is increased by stimuli such as hypoxia, increased production of hydrogen ions (H+), or an increase in body temperature.
A modified form of the alveolar gas equation can be used to determine PAo2 for clinical purposes, as follows:
In this equation, arterial carbon dioxide tension (Paco2) is substituted for alveolar carbon dioxide tension (PAco2).
Exchange of Oxygen and Carbon Dioxide Between the Alveolus and Pulmonary Capillary Blood Occurs by Diffusion
Diffusion is the passive movement of gases down a concentration (partial pressure) gradient. The rate of gas movement between the alveolus and the blood ( o2) is determined by the physical properties of the gas (D), the surface area available for diffusion (A), the thickness of the air-blood barrier (x), and the driving pressure gradient of the gas between the alveolus and capillary blood (PAo2 − PcaPo2), as follows:
o2) is determined by the physical properties of the gas (D), the surface area available for diffusion (A), the thickness of the air-blood barrier (x), and the driving pressure gradient of the gas between the alveolus and capillary blood (PAo2 − PcaPo2), as follows:
D is determined by several factors, including the molecular weight and solubility of the gas. The alveolar surface area (A) available for diffusion is that occupied by perfused pulmonary capillaries. During exercise, more capillaries become perfused by blood, and thus the surface area available for diffusion increases.
In the lung the barrier separating air and blood is less than 1 μm thick (Figure 47-2). However, although thin, this barrier includes a layer of liquid and surfactant lining the alveolar surface; an epithelial layer, usually formed by type I epithelial cells; a basement membrane; variable-thickness interstitium; and a layer of endothelium. In addition to moving gases through this air-blood barrier, diffusion also moves gases within the plasma, allowing oxygen to gain access to erythrocytes and hemoglobin.
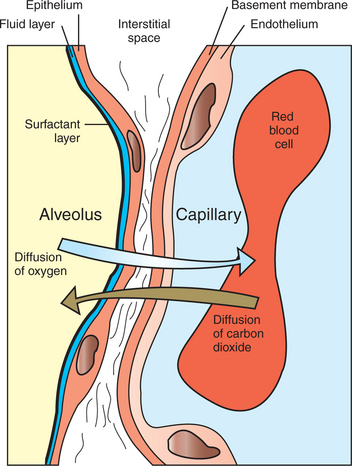
FIGURE 47-2 Diagrammatic representation of the air-blood barrier within the lung, showing the pathway for diffusion of oxygen and carbon dioxide between the alveolus and the erythrocyte within the pulmonary capillary.
Blood entering the alveolar capillary from the small pulmonary arteries is known as mixed venous blood because it is blood that has returned to the right side of the heart in veins from all parts of the systemic circulation. The driving pressure for gas diffusion is the difference in oxygen tension between the alveolus and the capillary blood. PAo2 averages 100 mm Hg; in a resting animal, blood entering the alveolar capillary—that is, mixed venous blood—has an oxygen tension (P⫫o2) of approximately 40 mm Hg. The driving pressure gradient of 60 mm Hg (100–40) causes rapid diffusion of oxygen into the capillary, where it combines with hemoglobin. Hemoglobin takes up oxygen from the plasma and helps maintain the gradient for oxygen diffusion.
Normally, equilibration between alveolar and capillary oxygen tensions occurs within 0.25 second, approximately one third of the time the blood is in the capillary (Figure 47-3). During strenuous exercise, muscles extract a large amount of oxygen from the blood, so the mixed venous blood returning to the lung contains little oxygen. In addition, during exercise the cardiac output is high, and the velocity of blood flow through the capillaries is rapid. More oxygen must therefore be transferred in less time than in the resting animal. Under these strenuous conditions, diffusion equilibrium may not occur, and the oxygen tension of blood leaving the lung and entering the systemic arteries (Pao2) may decrease during intense exercise. This exercise-associated hypoxemia is observed in racing Thoroughbred horses.
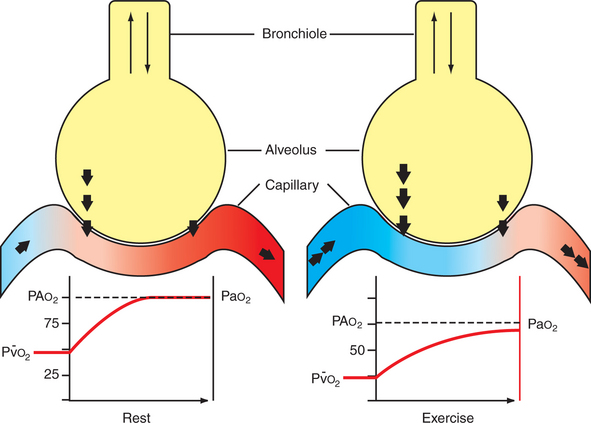
FIGURE 47-3 Schematic representation of alveolus and pulmonary capillary, showing the increase in oxygen (Po2) tension that occurs as blood passes through the capillaries. The shaded area within the alveolus represents mixing of gases by diffusion. The size of the arrows between the alveolus and the capillary represents the magnitude of the oxygen fluxes. In the resting animal, mixed venous oxygen tension (v—o2) is approximately 40 mm Hg, and blood and air equilibrate rapidly. In the exercising animal, mixed venous oxygen tension is low, and even though oxygen fluxes are high, the blood has not equilibrated with the alveolar oxygen tension before it leaves the alveolus. PAo2, Alveolar oxygen tension; Pao2, arterial oxygen tension.
In a diseased lung, diffusion of oxygen may be impeded as a result of inflammation and edema, which may thicken the air-blood barrier or reduce the surface area available for gas exchange. In these situations the therapeutic administration of oxygen can increase PAo2 and thereby provide a greater driving pressure to deliver oxygen into the blood.
The carbon dioxide tension of venous blood returning to the lungs averages 4.6 mm Hg, and alveolar carbon dioxide tension (PAco2) is 4.0 mm Hg. Thus the driving pressure for diffusion of carbon dioxide is only 6 mm Hg. Despite this small driving pressure, the amount of carbon dioxide that diffuses per minute between the capillaries and the alveoli is similar to the amount of oxygen. The 20-fold greater solubility of carbon dioxide compared with oxygen compensates for the small driving pressure gradient. For the same reason, carbon dioxide diffusion between the blood and the alveoli is rarely affected by lung disease.
The Exchange of Gases Between the Tissues and Blood Also Occurs by Diffusion
The Pao2 of blood entering the tissue capillaries from the systemic arteries is 85 to 1000 mm Hg, and the Paco2 is 40 mm Hg. As blood passes through the capillaries, it is exposed to the tissues that are consuming oxygen and producing carbon dioxide. Tissue oxygen tension is determined by the rate of delivery of oxygen in relation to its rate of consumption, but it averages 4.0 mm Hg. Similarly, tissue carbon dioxide tension is determined by the rate of tissue production in relation to the rate of removal by the blood, but it averages 46 mm Hg. As a result of the partial pressure differences between the tissues and capillaries, oxygen diffuses into the tissues and carbon dioxide diffuses into the blood until the partial pressures of blood and tissue are equal. Tissues with a high oxygen demand have more capillaries per gram of tissue. This provides a larger surface for diffusion and also means that the maximal distance between the tissue and the nearest capillary is less than in the poorly vascularized tissues (Figure 47-4).
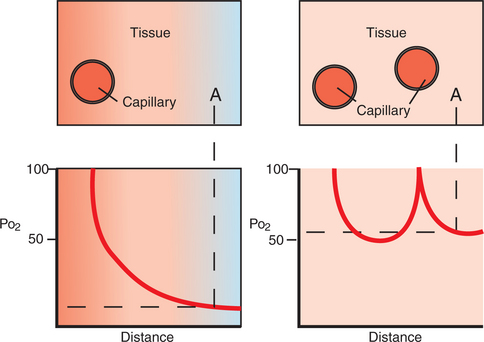
FIGURE 47-4 Effect of increasing capillary density on tissue oxygen tension (Po2). Oxygen tension is shown as a function of the distance from the capillary. Left, Point A has Po2 of approximately 10 mm Hg, whereas, right, point A has Po2 of approximately 50 mm Hg, because it is now closer to a second tissue capillary.
During exercise, muscle blood flow increases in part as a result of recruitment of capillaries that are not perfused in the resting animal. Capillary recruitment brings blood closer to the metabolizing tissues and slows the rate of blood flow, which allows more time for diffusion equilibrium. In addition, exercise lowers the Po2 and Pco2 of the muscle, which increases the driving pressure gradients for diffusion.
The Amount of Alveolar Ventilation in Relation to Pulmonary Capillary Blood Flow—the  /
/ . Ratio—Determines the Adequacy of Pulmonary Gas Exchange
. Ratio—Determines the Adequacy of Pulmonary Gas Exchange
In the alveoli, gas exchange is accomplished by the close approximation of air and blood. Ideally, each of the millions of alveoli should receive air and blood in amounts that are optimal for gas exchange; that is, ventilation ( ) and perfusion (
) and perfusion ( ) should be matched. In reality, this never occurs. Even in the young healthy animal, there is some
) should be matched. In reality, this never occurs. Even in the young healthy animal, there is some  /
/ mismatching, most likely resulting from branching patterns of bronchi and blood vessels and to some extent from gravitational forces. In disease, this
mismatching, most likely resulting from branching patterns of bronchi and blood vessels and to some extent from gravitational forces. In disease, this  /
/ mismatching becomes more extreme and leads to hypoxemia, a low Pao2.
mismatching becomes more extreme and leads to hypoxemia, a low Pao2.
Figure 47-5 shows schematic alveoli and capillaries with a variety of  /
/ ratios. The alveolus in the center is ideal: it receives ventilation and blood flow with a
ratios. The alveolus in the center is ideal: it receives ventilation and blood flow with a  /
/ ratio of 0.8. Venous blood arrives with a Pv–o2 and a Pv–co2 each of 46 mm Hg, is exposed to alveolar gas tensions (PAo2 and PAco2), and leaves with an end-capillary oxygen tension (PcaPo2) of 100 mm Hg and a capillary carbon dioxide tension (Pcapco2) of 40 mm Hg. The units toward the bottom have a low
ratio of 0.8. Venous blood arrives with a Pv–o2 and a Pv–co2 each of 46 mm Hg, is exposed to alveolar gas tensions (PAo2 and PAco2), and leaves with an end-capillary oxygen tension (PcaPo2) of 100 mm Hg and a capillary carbon dioxide tension (Pcapco2) of 40 mm Hg. The units toward the bottom have a low  /
/ ratio and are relatively overperfused and underventilated. The Po2 of blood leaving these units is low, and the Pco2 is high. Low
ratio and are relatively overperfused and underventilated. The Po2 of blood leaving these units is low, and the Pco2 is high. Low  /
/ units occur frequently in lung disease because ventilation is reduced by airway obstruction or by localized stiffening of the lung by inflammatory processes. The alveoli toward the top of Figure 47-5 have a high
units occur frequently in lung disease because ventilation is reduced by airway obstruction or by localized stiffening of the lung by inflammatory processes. The alveoli toward the top of Figure 47-5 have a high  /
/ ratio; ventilation is high in relation to blood flow. This can occur when pulmonary blood flow to part of the lung is reduced by vascular obstruction or by pulmonary hypotension. The blood leaving such units has a higher Po2 and a lower Pco2 than blood from the units with a
ratio; ventilation is high in relation to blood flow. This can occur when pulmonary blood flow to part of the lung is reduced by vascular obstruction or by pulmonary hypotension. The blood leaving such units has a higher Po2 and a lower Pco2 than blood from the units with a  /
/ ratio of 0.8.
ratio of 0.8.
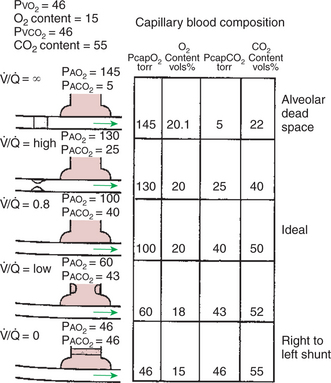
FIGURE 47-5 Diagrammatic representation of an alveolus and a capillary, showing the effect of differing ventilation/perfusion ( /
/ ) ratios on the partial pressure and gas content of blood leaving the alveolus. In the case of
) ratios on the partial pressure and gas content of blood leaving the alveolus. In the case of  /
/ ∞ (top), there is no bulk flow of blood past the alveolus, so capillary blood does not contribute to the arterial blood that leaves the left ventricle. See text for explanation and Table 47-1 for abbreviation definitions.
∞ (top), there is no bulk flow of blood past the alveolus, so capillary blood does not contribute to the arterial blood that leaves the left ventricle. See text for explanation and Table 47-1 for abbreviation definitions.
Extending the concepts demonstrated in Figure 47-5 to the whole lung with its multitude of alveoli requires computer simulation and the investigation of the frequency distribution of  /
/ ratios within the lung. In the normal animal the majority of alveoli have
ratios within the lung. In the normal animal the majority of alveoli have  /
/ ratios close to 1, and the range of ratios is small (Figure 47-6).
ratios close to 1, and the range of ratios is small (Figure 47-6).
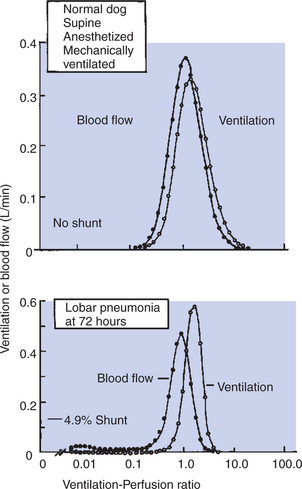
FIGURE 47-6 Distribution of ventilation and blood flow as a function of the ventilation/perfusion ( /
/ ) ratio. Top, In the normal dog, most of the blood flow and ventilation are received by gas exchange units with a
) ratio. Top, In the normal dog, most of the blood flow and ventilation are received by gas exchange units with a  /
/ ratio close to 1.0. No blood flow and no ventilation are received by units with extremely high or extremely low
ratio close to 1.0. No blood flow and no ventilation are received by units with extremely high or extremely low  /
/ ratios. Bottom, In the dog with pneumonia, a considerable portion of the blood flow is received by units with low
ratios. Bottom, In the dog with pneumonia, a considerable portion of the blood flow is received by units with low  /
/ ratios, that is, units with little ventilation. The amount of blood passing through right-to-left shunts is also increased in pneumonia.
ratios, that is, units with little ventilation. The amount of blood passing through right-to-left shunts is also increased in pneumonia.
(From Wagner PD, Laravuso RB, Goldzimmer E, et al: Distributions of ventilation-perfusion ratios in dogs with normal and abnormal lungs, J Appl Physiol 38:1099, 1975.)
The Composition of the Systemic Arterial Blood Is Determined by the Composition of the Capillary Blood That Drains Each Alveolus
Blood that returns from the lungs to the left ventricle for distribution to the tissues comes from capillaries associated with millions of alveoli, each of which may have a slightly different  /
/ ratio. The content of oxygen and carbon dioxide in blood that leaves each alveolus varies because of these differing
ratio. The content of oxygen and carbon dioxide in blood that leaves each alveolus varies because of these differing  /
/ ratios. Thus the composition of arterial blood is determined by distribution of
ratios. Thus the composition of arterial blood is determined by distribution of  /
/ ratios in the lung.
ratios in the lung.
Lung disease accentuates  /
/ mismatching because of obstruction of airways, flooding of alveoli with exudates, and local obstructions to blood flow. This mismatching has a major effect on oxygen exchange but little effect on the exchange of carbon dioxide. In the case of oxygen, overventilation of some alveoli does not compensate for underventilation of others. Because of the shape of the oxyhemoglobin dissociation curve (see Chapter 48) the overventilated (high
mismatching because of obstruction of airways, flooding of alveoli with exudates, and local obstructions to blood flow. This mismatching has a major effect on oxygen exchange but little effect on the exchange of carbon dioxide. In the case of oxygen, overventilation of some alveoli does not compensate for underventilation of others. Because of the shape of the oxyhemoglobin dissociation curve (see Chapter 48) the overventilated (high  /
/ ) alveoli with a high PAo2 cannot add enough oxygen to the blood to compensate for the deficiency that arises from the underventilated (low
) alveoli with a high PAo2 cannot add enough oxygen to the blood to compensate for the deficiency that arises from the underventilated (low  /
/ ) alveoli with a low PAo2. Therefore, hypoxemia occurs to varying degrees in most lung diseases. However, in contrast to oxygen, carbon dioxide is very soluble, and because its dissociation curve (see Chapter 48) is almost linear, the overventilated alveoli can compensate for those that are underventilated. For this reason, hypercarbia, also called hypercapnia (increased Paco2), rarely occurs in the presence of lung disease.
) alveoli with a low PAo2. Therefore, hypoxemia occurs to varying degrees in most lung diseases. However, in contrast to oxygen, carbon dioxide is very soluble, and because its dissociation curve (see Chapter 48) is almost linear, the overventilated alveoli can compensate for those that are underventilated. For this reason, hypercarbia, also called hypercapnia (increased Paco2), rarely occurs in the presence of lung disease.
As the degree of  /
/ mismatching increases and oxygen exchange becomes less efficient, the difference between the average PAo2 and Pao2 increases. Normally, this alveolar-to-arterial oxygen tension difference (AaDo2) averages 5 to 10 mm Hg, because there is a degree of
mismatching increases and oxygen exchange becomes less efficient, the difference between the average PAo2 and Pao2 increases. Normally, this alveolar-to-arterial oxygen tension difference (AaDo2) averages 5 to 10 mm Hg, because there is a degree of  /
/ inequality even in normal lungs, and because venous blood draining the bronchial and coronary circulations mixes with the oxygenated blood draining the alveoli. The AaDo2 increases when animals are anesthetized or when they have lung disease, because many poorly ventilated regions of the lung continue to receive blood flow; that is, the number of units with low
inequality even in normal lungs, and because venous blood draining the bronchial and coronary circulations mixes with the oxygenated blood draining the alveoli. The AaDo2 increases when animals are anesthetized or when they have lung disease, because many poorly ventilated regions of the lung continue to receive blood flow; that is, the number of units with low  /
/ increases (see Figure 47-6).
increases (see Figure 47-6).
Right-to-Left Vascular Shunts Allow Blood to Bypass Ventilated Lung
In a right-to-left shunt, blood from the right ventricle bypasses ventilated lung and returns to the left atrium (see Figure 47-5, bottom). Such blood does not pick up oxygen and, when it leaves the lung, has the same composition as the venous blood that entered the lung. Right-to-left shunts have a  /
/ ratio of zero and are formed when alveoli are collapsed (atelectasis), are unventilated because of complete airway obstruction, or are filled with exudates, as in acute pneumonia. Right-to-left shunts can also result from complex congenital cardiac defects, such as tetralogy of Fallot, which allow blood to flow directly from the right to the left chambers of the heart, bypassing the lungs. Such large right-to-left shunts cause a major impairment of oxygen exchange. In normal animals the venous blood (low Po2) from the bronchial and coronary veins enters the oxygenated blood leaving the lungs. This is equivalent to a right-to-left shunt and constitutes 5% of cardiac output.
ratio of zero and are formed when alveoli are collapsed (atelectasis), are unventilated because of complete airway obstruction, or are filled with exudates, as in acute pneumonia. Right-to-left shunts can also result from complex congenital cardiac defects, such as tetralogy of Fallot, which allow blood to flow directly from the right to the left chambers of the heart, bypassing the lungs. Such large right-to-left shunts cause a major impairment of oxygen exchange. In normal animals the venous blood (low Po2) from the bronchial and coronary veins enters the oxygenated blood leaving the lungs. This is equivalent to a right-to-left shunt and constitutes 5% of cardiac output.
Part of Each Breath Ventilates Dead-Space and Does Not Participate in Gas Exchange
Dead-space ventilation consists of the gas that does not participate in gas exchange. This includes both anatomic dead-space (see Chapter 45) and alveolar dead-space. The latter consists of alveoli that receive ventilation but no blood flow; that is, they have a  /
/ ratio of infinity (see Figure 47-5, top). Alveolar dead-space can form when the pulmonary arterial pressure is so low that many capillaries are unperfused, or when the vessels are obstructed by thrombi.
ratio of infinity (see Figure 47-5, top). Alveolar dead-space can form when the pulmonary arterial pressure is so low that many capillaries are unperfused, or when the vessels are obstructed by thrombi.
Arterial Oxygen (Pao2) and Carbon Dioxide (Paco2) Tensions Are Measured to Evaluate Gas Exchange
A systemic arterial blood sample is essential to evaluate pulmonary gas exchange because this blood has just passed through the lung. A venous blood sample is inadequate because its composition varies depending on the blood flow/metabolism ratio of the tissue of origin. Arterial blood gas tensions are the end result of the individual processes involved in gas exchange and thus are affected by the composition of inspired air, alveolar ventilation, alveolocapillary diffusion, and ventilation/perfusion matching. All these factors must be considered when evaluating a blood gas result.
Inspired air usually contains 21% oxygen (FIo2 = 0.21), but during anesthesia or oxygen therapy, the administration of oxygen increases FIo2, which causes an increase in inspired oxygen tension (PIo2). Although the daily fluctuations in PB cause only trivial changes in PIo2, the decrease in PB that occurs at higher altitudes results in a major decrease in PIo2. As a result, there is a decrease in PAo2 and thus a decrease in Pao2 as animals ascend in altitude. In the appropriate geographic locations, altitude-induced changes in Pao2 must always be considered when blood gas tensions are evaluated.
Adequacy of alveolar ventilation is assessed by examination of Paco2. It is elevated above the normal value of 40 mm Hg when animals hypoventilate and is decreased during hyperventilation. At the same time, hypoventilation decreases PAo2 and Pao2, and hyperventilation increases these tensions.
Diffusion abnormalities and  /
/ mismatching impair the transfer of oxygen from the alveolus to arterial blood, increase the AaDo2, and reduce Pao2. Paco2 is rarely elevated by these problems for two reasons. First, the high solubility of carbon dioxide allows easy diffusion across the remaining healthy lung. Second, the hypoxemia caused by lung disease stimulates ventilation. The resultant increase in alveolar ventilation keeps Paco2 normal or even reduces it below normal.
mismatching impair the transfer of oxygen from the alveolus to arterial blood, increase the AaDo2, and reduce Pao2. Paco2 is rarely elevated by these problems for two reasons. First, the high solubility of carbon dioxide allows easy diffusion across the remaining healthy lung. Second, the hypoxemia caused by lung disease stimulates ventilation. The resultant increase in alveolar ventilation keeps Paco2 normal or even reduces it below normal.
In animals with normal lungs, administering oxygen (increasing FIo2) elevates Pao2. As  /
/ mismatching becomes more extreme, oxygen administration increases Pao2 only modestly, especially in the presence of right-to-left shunts. Concurrently, the alveolar-arterial oxygen difference widens. The Pao2 response to oxygen is a good way to evaluate the severity of lung disease.
mismatching becomes more extreme, oxygen administration increases Pao2 only modestly, especially in the presence of right-to-left shunts. Concurrently, the alveolar-arterial oxygen difference widens. The Pao2 response to oxygen is a good way to evaluate the severity of lung disease.
Pao2 tends to be lower in newborn animals than in adults. This is because there is greater mismatching of ventilation and blood flow in the immature lungs.
CLINICAL CORRELATIONS
Hypoventilation in a Bulldog
History.
A 5-year-old bulldog is presented to you because it refuses to exercise. Normally the dog is willing to go for short, slow walks. Over the past 6 months, the dog has been making an increasing amount of noise when it breathes. When it is awake, it makes a rattling sound during inhalation; when it sleeps, it snores loudly and wakes frequently, standing up, turning around, and then lying down again. On one occasion the owner tried to get the dog to run, but the dog collapsed, making a loud noise in its throat as it struggled to inhale.
Clinical Examination.
The bulldog is in good condition, but even as you walk into the room, you notice the loud rattling noises being made by the dog during breathing. You also observe that the mucous membranes of the pendulous lips have a bluish tinge. The dog is standing when you walk into the room, but while you are talking to the owner, the dog lies down and apparently goes to sleep. This causes the breathing noises to become much louder.
Examination of the dog reveals no abnormalities in the heart or the digestive tract, but examination of the respiratory tract reveals multiple abnormalities. The external nares of the dog are extremely small, and it is difficult to introduce a speculum to examine the nasal cavity. When the dog’s mouth is opened, an excessive amount of loosely folded tissue is observed in the pharynx, and it is impossible to move this aside to examine the larynx. Listening to the lungs is not helpful because all the sounds being generated by the loose, vibrating tissue in the upper airway are transmitted to the lungs. Radiographs, however, reveal no abnormalities in the lungs, but the trachea is quite narrow. An arterial blood sample is taken for measurement of carbon dioxide and oxygen tensions. Pao2 is 50 mm Hg (normal, 95–100), and Paco2 is 75 mm Hg (normal, 40).
Comment.
This bulldog’s condition represents an extreme form of the brachycephalic syndrome, which is seen in short-nosed dogs, particularly bulldogs. The syndrome usually includes stenosis (narrowing) of the external nares and obstruction of the pharynx by pendulous folds of excessive soft tissue. In some of these dogs, the trachea is also very narrow. These dogs have difficulty breathing, particularly during inhalation, when the subatmospheric pressure within the upper airway sucks the loose folds of tissue into the airway lumen. This can result in total obstruction to ventilation. In general, these dogs make a lot of noise during inhalation as the loose folds of tissue vibrate. Exhalation presents less difficulty because the higher-than-atmospheric pressure in the pharynx tends to push back the loose tissue and open the airway. Over time the chronic, excessively subatmospheric pressure during inhalation can cause deformity of the larynx.
The upper airway obstruction in this bulldog is limiting ventilation so severely that the dog is suffering from alveolar hypoventilation. The elevated Paco2 indicates this. An elevation in Paco2 occurs when alveolar ventilation is not sufficient to remove the carbon dioxide being produced by the body. The accumulating carbon dioxide in the alveolus and the lack of ventilation also depress the PAo2, which leads to a decrease in Pao2, as in this dog. The hypoxemia then leads to hemoglobin desaturation, which accounts for the bluish color (cyanosis) of the mucous membranes of the dog.
Treatment.
The treatment for this dog is surgical removal of some of the excessive tissues of the upper airway and enlargement of the external nares. This will alleviate some of the obstruction and may improve ventilation. However, with the narrowing of the trachea observed in this dog, it is unlikely that the dog will ever be able to exercise to a significant degree, although its condition may be improved sufficiently that it can make a suitable pet.
Hypoxemia in an Anesthetized Clydesdale Horse
History.
A 2-year-old, 750-kg Clydesdale horse is presented for removal of a testicle that has been retained in the abdomen, a procedure that requires anesthesia. You know that anesthesia of heavy draft horses can lead to gas exchange problems, and therefore you have an anesthesia machine available to provide ventilation and to supplement the horse with extra oxygen. The horse is anesthetized with a short-acting intravenous anesthetic; an endotracheal tube is inserted; and the horse is connected to the anesthesia machine and allowed to breathe oxygen containing isoflurane for anesthesia. Ventilation is not assisted.
Thirty minutes after the induction of anesthesia, the veterinary technician takes an arterial blood sample to monitor the horse’s gas exchange. Pao2 is 70 mm Hg, and Paco2 is 65 mm Hg. Are you satisfied with the results of the blood gas analysis? If not, what can be done to improve gas exchange?
Comment.
The elevation of Paco2 from the normal value of 40 mm Hg to 65 mm Hg shows that the horse is suffering from alveolar hypoventilation; that is, the ventilation received by the alveoli is insufficient to remove the carbon dioxide being produced by the horse. This is probably a result of depression of the central nervous system by the anesthetic gases, so that the drive to breathe is reduced. In addition, the positioning of the horse on its back for removal of the retained testicle causes the heavy viscera to push on the diaphragm, making it difficult for the horse to ventilate. Alveolar hypoventilation in an anesthetized animal can be corrected by the use of positive-pressure ventilation. You have a ventilator as part of the anesthesia machine and choose to ventilate the horse to return the Paco2 to acceptable levels.
The Pao2 of 70 mm Hg shows that the horse has considerable problems in exchanging oxygen. Although a Pao2 of 70 mm Hg is sufficient almost to saturate hemoglobin and would not be considered particularly low in an animal breathing air, it is very low in an animal breathing 100% oxygen. When animals breathe oxygen, PAo2 is greater than 600 mm Hg:
If the lung is functioning ideally, arterial oxygen should also be close to 600 mm Hg. In this horse, Pao2 is only 75 mm Hg, so AaDo2 is 645 − 75, that is 570 mm Hg.
This huge AaDo2 is not unusual in large, anesthetized mammals. The positioning of the horse on its back with the consequent weight of the viscera pushing forward on the diaphragm and compressing the lungs can lead to severe  /
/ inequalities. Parts of the dependent lung are unable to ventilate, although they continue to receive blood flow and therefore become right-to-left shunts. These right-to-left shunts result in severe arterial hypoxemia. As long as the Pao2 is sufficient to saturate hemoglobin, the horse is in no danger. The dangerous point is during recovery from anesthesia. The horse must be supplemented with oxygen until it is sufficiently conscious to be able to rest on its sternum unaided and eventually to stand. Returning to these postures eliminates right-to-left shunts, restores the
inequalities. Parts of the dependent lung are unable to ventilate, although they continue to receive blood flow and therefore become right-to-left shunts. These right-to-left shunts result in severe arterial hypoxemia. As long as the Pao2 is sufficient to saturate hemoglobin, the horse is in no danger. The dangerous point is during recovery from anesthesia. The horse must be supplemented with oxygen until it is sufficiently conscious to be able to rest on its sternum unaided and eventually to stand. Returning to these postures eliminates right-to-left shunts, restores the  /
/ istribution to normal, and improves gas exchange.
istribution to normal, and improves gas exchange.
Boron WF. Ventilation and perfusion of the lungs. In: Boron WF, Boulpaep EL. Medical physiology: a cellular and molecular approach, updated edition. Philadelphia: Saunders, 2005.
Hlastala MP, Berger AJ. Physiology of respiration, ed 2. New York: Oxford University Press, 2001.
Leff AR, Schumacker PT. Respiratory physiology: basics and applications. Philadelphia: Saunders, 1993.
Lekeux P, Art T. The respiratory system: anatomy, physiology and adaptations to exercise and training. In: Hodgson DR, Rose RJ. The athletic horse. Philadelphia: Saunders, 1994.
West JB. Respiratory physiology: the essentials, ed 7. Baltimore: Lippincott Williams & Wilkins, 2005.
PRACTICE QUESTIONS
1. Calculate the alveolar oxygen tension (PAo2) of an anesthetized cow when the barometric pressure is 750 mm Hg, PH2O at body temperature = 50 mm Hg, and Paco2 = 80 mm Hg. The cow is breathing a mixture of 50% oxygen and 50% nitrogen. Assume the respiratory exchange ratio is 1.
2. Which of the following will decrease the rate of oxygen transfer between the alveolar air and the pulmonary capillary blood?
3. During exercise, recruitment of muscle capillaries that are unperfused in the resting animal results in all the following except:
4. Which of the following could potentially result in more low  /
/ regions within the lung?
regions within the lung?
5. Which of the following statements is correct?
 /
/ units in the lung.
units in the lung. /
/ units in the lung are not a cause of hypoxemia (low Pao2).
units in the lung are not a cause of hypoxemia (low Pao2).6. A horse has difficulty inhaling, especially during exercise. Arterial blood gas tensions at rest are Pao2 = 55 mm Hg and Paco2 = 70 mm Hg. After you give the horse oxygen to breathe, Pao2 increases to 550 mm Hg, and Paco2 remains unchanged. The cause of these gas tensions is: