1. Albarellos G.A., Landoni M.F. Current concepts on the use of antimicrobials in cats. Vet J. 2009;180(3) (Jun):):304-316.
2. United States Pharmacopeia (USP) Antibiotic Monographs. J Vet Pharmacol Ther. 26(Suppl 2), 2003.
3. Mattoes H.M., Kim M-K Kuti J.L., et al. Clinical advantage of continuous infusion β–lactams. Serious Hospital Infections. 2001;13(3):1-8.
4. Rice L.B. Genetic and biochemical mechanisms of bacterial resistance to antimicrobial agents. In: Lorian V., editor. Antibiotics in laboratory medicine. Baltimore: Williams & Wilkins; 2005:441-508.
5. Neu H.C. Principles of antimicrobial use. In: Brody T.M., Larner J., Minneman K.P., et al, editors. Human pharmacology: molecular to clinical. St Louis: Mosby; 1994:616-701.
6. Kapusnik J., Miller R.T., Sande M.A. Antibacterial therapy in critical care. In: Schoemaker W.C., Ayers S., Grenvik A., et al, editors. Textbook of critical care. ed 2. Philadelphia: Saunders; 1989:780-801.
7. Bush L.M., Calmon J., Johnson C. Newer penicillins and lactamase inhibitors. Infect Dis Clin North Am. 1989;3:571-594.
8. Donowitz G.R. Third generation cephalosporins. Infect Dis Clin North Am. 1989;3:595-612.
9. Vaden S., Riviere J. Penicillins. In: Adams R., editor. Veterinary pharmacology and therapeutics. ed 8. Ames, Iowa: Iowa State University Press; 2001:818-827.
10. Williams J.D., Naber K.G., Bryskier A., et al. Classification of oral cephalosporins. A matter for debate. Inter J Antimicro Agents. 2001;17:443-450.
11. Caprile K.A. The cephalosporin antimicrobial agents: a comprehensive review. J Vet Pharmacol Ther. 1988;11:1-32.
12. Bramhill D. Bacterial cell division. Annu Rev Cell Dev Biol. 1997;13:395-424.
13. Anonymous. Antimicrobial treatment guidelines for acute bacterial rhinosinusitis. Arch Otolaryngol Head Neck Surg. 2004;130:S1-S45.
14. Chambers H. Penicillin-binding protein - mediated resistance in pneumococci and staphylococci. J Infect Dis. 1999;179(Suppl 2):S353-S359.
15. Bywater R.J., Palmer G.H., Buswell J.F., et al. Clavulanate-potentiated amoxycillin: activity in vitro and bioavailability in the dog. Vet Rec. 1985;116(2):33-36.
16. Brown S.A. Treatment of gram-negative infections. Vet Clin North Am. 1988;18:1141-1166.
17. Papich M. Treatment of gram-positive bacterial infections. Vet Clin North Am. 1988;18:1267-1286.
18. Sobel J.D. Imipenem and aztreonam. Infect Dis Clin North Am. 1989;3:613-624.
19. Yigit H., Queenan A.M., Anderson G.J., et al. Novel carbapenem-hydrolyzing β-lactamase, KPC-1, from a carbapenem-resistant strain of Klebsiella pneumoniae. Antimicrob Agents Chemother. 2001;45(4):1151-1161.
19a. Human Drug Product Not Equivalent to Veterinary Ceftiofur; CVM Update, July 1997. Accessed June 2010, at http://www.fda.gov/AnimalVeterinary/NewsEvents/CVMUpdates/ucm127855.
20. Stegemann M.R., Passmore C.A., Sherington J., et al. Antimicrobial activity and spectrum of cefovecin, a new extended-spectrum cephalosporin, against pathogens collected from dogs and cats in Europe and North American. Antimicrob Agents Chemother. 2006;50(7):2286-2292.
21. Lowy F.D. Antimicrobial resistance: the example of Staphylococcus aureus. J Clin Invest. 2003;111:1265-1273.
22. Helfand M.S., Bonomo R.A. β-Lactamases: a survey of protein diversity. Curr Drug Targets Infect Disord. 2003;3:9-23.
23. Li X.Z., Mehrotra M., Ghimire S., et al. Beta-lactam resistance and beta-lactamases in bacteria of animal origin. Vet Microbiol 15. 2007;121(3-4):197-214.
24. Rodriguez-Banõ J., Navarro M.D., Romero L., et al. Clinical and molecular epidemiology of extended-spectrum β-lactamase–producing Escherichia coli as a cause of nosocomial infection or colonization: implications for control. Clin Infect Dis. 2006;42:37-45.
25. Dancer S.J. The problem with cephalosporins. J Antimicro Chemother. 2001;48:463-478.
26. Vree T.B., Dammers E., van Duuren E. Variable absorption of clavulanic acid after an oral dose of 25 mg/kg of Clavubactin and Synulox in healthy dogs. J Vet Pharmacol Therap. 2003;26:165-171.
27. Malik S., Christensen H., Peng H., et al. Presence and diversity of the β-lactamase gene in cat and dog staphylococci. Vet Microbiol. 2007;123:162-168.
28. Chaudhary U., Aggarwal R. Extended spectrum -lactamases (ESBL): an emerging threat to clinical therapeutics. Indian J Med Microbiol. 2004;22(2):75-80.
29. Jacoby G.A., Medeiros A.A., O’Brien T.F., et al. Broad-spectrum, transmissible beta-lactamases. N Engl J Med. 1988;319:723-724.
30. Jacoby G.A., Medeiros A.A. More extended-spectrum beta-lactamases. Antimicrob Agents Chemother. 1991;35:1697-1704.
31. Jacoby G.A. Extended-spectrum beta-lactamases and other enzymes providing resistance to oxyimino-beta-lactams. Infect Dis Clin North Am. 1997;11:875-887.
32. Decre D., Gachot B., Lucet J.C., et al. Clinical and bacteriologic spectrum of extended-spectrum beta-lactamase-producing strains of Klebsiella pneumoniae in a medical intensive care unit. Clin Infect Dis. 1998;27:834-844.
33. Sturenburg E., Mack D. Extended-spectrum beta-lactamases: implications for the clinical microbiology laboratory, therapy, and infection control. J Infect Dis. 2003;47:273-295.
34. Lee N., Yuen K.Y., Kumana C.R. Clinical role of beta-lactam/beta-lactamase inhibitor combinations. Drugs. 2003;63(14):1511-1524.
35. Antonio O., Weigel L.M., Rasheed K., et al. Mechanisms of decreased susceptibility to cefpodoxime in. Escherichia coli, Antimicrob Agents Chemother. 2002;46(12):3829-3836.
36. Tenover F.C., Raney P.M., Williams P.P. Confirmation methods for Escherichia coli with isolates the flqA locus and genetic evidence that Topoisomerase IV is the primary target and DNA gyrase is the secondary target. The Fluoroquinolone Toxicity Research Foundation, Collected during Project ICARE. J Clin Microbiol. 2003;41:3142-3146.
37. Queenan A.M., Bush K. Carbapenemases: the versatile β-lactamases. Clin Microbiol Rev. 2007;20(3):440-458.
38. Devriese L.A., Hermans K., Baele M., et al. Staphylococcus pseudintermedius versus Staphylococcus intermedius. Vet Microbiol. 2009;133(1-2):206-207.
39. Leonard F.C., Markey B.K. Methicillin-resistant Staphylococcus aureus in animals: a review. Vet J. 2008;75:27-36.
40. Kania S.A., Williamson N.L., Frank L.A. Methicillin resistance of staphyloccci isolated from the skin of dogs with pyoderma. J Am Vet Med Assoc. 2004;65:1268-1285.
40a. Faires M.C., Tater K.C., Weese J.S. An investigation of methicillin-resistant Staphylococcus aureus colonization in people and pets in the same household with an infected person or infected pet. J Am Vet Med Assoc. 2009;235(5):540-543.
41. Gortel K., Campbell K.L., Kakoma I., et al. Methicillin resistance among staphylococci isolated from dogs. Am J Vet Res. 1999;60(12):1526-1530.
42. Weese J.S., van Duijkeren E. Methicillin-resistant Staphylococcus aureus and Staphylococcus pseudintermedius in veterinary medicine. Vet Microbiol Jan 27:. 2010;140(3-4):418-429.
43. Walther B., Wieler L.H., Friedrich A.W., et al. Methicillin-resistant Staphylococcus aureus (MRSA) isolated from small and exotic animals at a university hospital during routine microbiological examinations. Vet Microbiol Feb 5:. 2008;127(1-2):171-178.
44. Strommenger B., Kehrenberg C., Kettlitz C., et al. Molecular characterization of methicillin-resistant Staphylococcus aureus strains from pet animals and their relationship to human isolates. J Antimicrob Chemother. 2006;57:461-465.
45. Devriese L.A., Hermans K., Baele M., et al. Staphylococcus pseudintermedius versus Staphylococcus intermedius,. Vet Microbiol. 2009;133(1-2):206-207.
46. Ruscher C., Lubke-Becker A., Wleklinski C.-G., et al. Prevalence of methicillin-resistant Staphylococcus pseudintermedius isolated from clinical samples of companion animals and equidaes. Vet Microbiol Apr 14:. 2009;136(1-2):197-201.
47. El Zubeir I.E.M., Kanbar T., Alber J., et al. Phenotypic and genotypic characteristics of methicillin/oxacillin-resistant Staphylococcus intermedius isolated from clinical specimens during routine veterinary microbiological examinations. Vet Microbiol. 2007;121:170-176.
48. Pottumarthy S., Schapiro J.M., Prentice J.L., et al. Clinical isolates of Staphylococcus intermedius masquerading as methicillin-resistant Staphylococcus aureus. J Clin Microbiol. 2004;42(12):5881-5884.
49. Guardabassi L., Loeber M.E., Jacobson A. Transmission of multiple antimicrobial-resistant Staphylococcus intermedius between dogs affected by deep pyoderma and their owners. Vet Microbiol. 2004;98:23-27.
49a. Methicillin-resistant Staphylococcus Aureus. Accessed January 1, 2010, at http://www.avma.org/reference/backgrounders/mrsa_bgnd.asp
50. Braga P.C. Antibiotic penetrability into bronchial mucus: pharmacokinetic and clinical considerations. Curr Ther Res. 1989;49(2):300-327.
51. Bergogne-Bérézin E. Pharmacokinetics of antibiotics in respiratory secretions. In: Pennington J.E., editor. Respiratory infections: diagnosis and management. ed 2. New York: Raven Press; 1988:608-631.
52. Bergan T. Pharmacokientics of tissue penetration of antibiotics. Rev Infect Dis. 1981;3:45-66.
53. Bolton G.C. Allen GD, Filer CW: Absorption, metabolism and excretion studies on clavulanic acid in the rat and dog. Xenobiotica. 1984;14(6):483-490.
54. Brown SA: Pfizer Animal Health, personal communication.
55. Garg R.C., Keefe T.J., Vig M.M. Serum levels and pharmacokinetics of ticarcillin and clavulanic acid in dog following parenteral administration of Timentin. J Vet Pharmacol Ther. 1987;10(4):324-330.
56. Barker C.W., Zhang W., Sanchez S., et al. Pharmacokinetics of imipenem in dogs. Am J Vet Res. 2003;64:694-699.
57. Bidgood T.L., Papich M.G. Comparison of plasma and interstitial fluid concentrations of doxycycline and meropenem following constant rate intravenous infusion in dogs. Am J Vet Res. 2003;64:1040-1046.
58. Bidgood T., Papich M.G. Plasma pharmacokinetics and tissue fluid concentrations of meropenem after intravenous and subcutaneous administration in dogs. Am J Vet Res. 2002;63:1622-1628.
59. Krueger W.A., Neeser G., Schuster H., et al. Correlation of meropenem plasma levels with pharmacodynamic requirements in critically ill patients receiving continuous veno-venous hemofiltration. Chemotherapy. 2003;49(6):280-286.
59a. Papich M.G., Davis J.L., Floerchinger A.M., et al. Cefpodoxime and cephalexin plasma pharmacokinetics, protein binding, and tissue distribution after oral administration to dogs. Accepted. Am J Vet Res. 2010. in press
60. Carli S., Anfossi P., Villa R., et al. Absorption kinetics and bioavailability of cephalexin in the dog after oral and intramuscular administration. J Vet Pharmacol Ther. 1999;22:308-313.
61. Prados A.P., Ambros L., Montoya L., et al. Chronopharmacological study of cephalexin in dogs. Chronobiol Int. 2007;24(1):161-170.
62. Campbell B.G., Rosin E. Effect of food on absorption of cefadroxil and cephalothin in dogs. J Vet Pharmacol Ther. 1998;21:418-420.
63. Richardson D.C., Aucoin D.P., DeYoung D.J., et al. Pharmacokinetic disposition of cefazolin in serum and tissue during canine total hip replacement. Vet Surg. 1992;21(1):1-4.
64. Marcellin-Little D.J., Papich M.G., Richardson D.C., et al. Pharmacokinetic model for cefazolin distribution during total hip arthroplasty in dogs. Am J Vet Res. 1996;57(5):720-723.
64a. WHO Food Additives Series: 49 Toxicological evaluation of certain veterinary drug residues in food. Accessed June 2010, at http://www.inchem.org/documents/jecfa/jecmono/v49je04.htm).
65. Jung H.-H., Mischkowsky T. Measurements of cefuroxime concentration in bone in dogs and man. Arch Orthop Trauma Surg. 1979;94:25-28.
66. Spurling N.W., Harcourt R.A., Hyde J.J. An evaluation of the safety of cefuroxime axetil during six months oral administration to beagle dogs. J Toxicol Sci. 1986;11:237-277.
67. Sakamoto H., Hirose T., Mine Y. Pharmacokinetics of FK027 in rats and dogs. J Antibot. 1985;38(4):496-504.
68. Rebuelto M., Albarellos G., Ambros L. Pharmacokinetics of Ceftriaxone administered by the intravenous, intramuscular or subcutaneous routes to dogs. Vet Pharm Therap. 2002;25:73-76.
69. Moore K.W., Trepanier L.A., Lautzenhiser S.J., et al. Pharmaocinetics of ceftazidime in dogs following subcutanoeus administration and continuous infusion and the association with in vitro susceptibility of Pseudomonas aeruginosa. Am J Vet Res. 2000;61:1204-1208.
70. Albarellos G.A., Ambros L.A., Landoni M.F. Pharmacokinetics of ceftazidime after intravenous and intramuscular administration to domestic cats. Veterinary Journal. 2008;178:238-243.
71. Brown S.A., Arnold T.S., Hamlow P.J., et al. Plasma and urine disposition and dose proportionality of ceftiofur and metabolites in dogs after subcutaneous administration of ceftiofur sodium. J Vet Pharmacol Ther. 1995;18(5):363-369.
72. Stegemann M.R., Sherington J., Blanchflower S. Pharmacokinetics and pharmacodynamics of cefovecin in dogs. J Vet Pharmacol Therap. 2006;29:501-511.
73. Stegemann M.R., Sherington J., Coati N., et al. Pharmacokinetics of cefovecin in cats. J Vet Pharmacol Therap. 2006;29:513-524.
73a. Harmoinen J., Mentula S., Heikkilä M., et al. Orally administered targeted recombinant beta-lactamase prevents ampicillin-induced selective pressure on the gut microbiota: a novel approach to reducing antimicrobial resistance. Antimicrob Agents Chemother. 2004;48:75-79.
74. Trautmann M., Zick R., Rukavina T., et al. Antibiotic-induced release of endotoxin: in-vitro comparison of meropenem and other antibiotics. J Antimicrob Chemother. 1998;41(2):163-169.
75. Kumar G.A.V., Kothari V.M., Kirsihman A., et al. Benzathine penicillin, metronidazole and benzyl penicillin in the treatment of tetanus: a randomized, controlled trial. Ann Trop Med Parasitol. 2004;98:59-63.
76. Semel J.D., Allen N. Seizures in patients simultaneously receiving theophylline and imipenem or ciprofloxacin or metronidazole. South Med J. 1991;84:465-468.
77. Rees C.A., Boothe D.M. Evaluation of the effect of cephalexin and enrofloxacin on clinical laboratory measurements of urine glucose in dogs. J Am Vet Med Assoc. 2004;224(9):1455-1458.
78. Ingerman M.J., Santoro J. Vancomycin: a new old agent. Infect Dis Clin North Am. 1989;3:641-652.
79. Walsh T.R., Howe R.A. The prevalence and mechanisms of vancomycin resistance in Staphylococcus aureus. Annu Rev Microbiol. 2002;56:657-675.
80. Chambers HF: Protein synthesis inhibitors and miscellaneous antibacterial agents. In Brunton LL, Lazo JS, Parker KL, editors: Goodman & Gilman’s the pharmacological basis of therapeutics, ed 11. Accessed January 2009, at http://www.accessmedicine.com/content.aspx?aID=949328.
81. Fillgrove K.L., Pakhomova S., Schaab M.R., et al. Structure and mechanism of the genomically encoded fosfomycin resistance protein, FosX, from Listeria monocytogenes. Biochemistry. 2007;46:8110-8120.
82. Marchese A., Bozzolasco M., Gualco L., et al. Effect of fosfomycin alone and in combination with N-acetylcysteine on E. coli biofilms. Int J Antimicrob Agents. 2003;22(Suppl 2):95-100.
83. Marchese A., Gualco L., Debbia E.A., et al. In vitro activity of fosfomycin against gram-negative urinary pathogens and the biological cost of fosfomycin resistance. Int J Antimicrob Agents. 2003;22(Suppl 2):53-59.
84. Sauermann R., Marsik C., Steiner I., et al. Immunomodulatory effects of fosfomycin in experimental human endotoxemia. Antimicrob Agents Chemother. 2007;51(5):1879-1881.
85. Olay T., Vicente M.V., Rodríguez A. Efficacy of fosfomycin + vancomycin or gentamicin in experimental endocarditis due to methicillin-resistant Staphylococcus aureus (MRSA). J Chemother. 1989;1(4 Suppl):391-392.
86. Schito G.C. Why fosfomycin trometamol as first line therapy for uncomplicated UTI? Int J Antimicrob Agents. 2003;22(Suppl 2):79-83.
87. Sack K., Schulz E., Marre R., et al. Fosfomycin protects against tubulotoxicity induced by Cis-diaminedichloroplatin and cyclosporin A in the rat. J Mol Med. 1987;65(11):525-527.
88. Gutierrez O.L., Ocampo C.L., Aguilera J.R., et al. Pharmacokinetics of disodium–fosfomycin in mongrel dogs. Res Vet Sci. 2008;85:156-161.
89. Kawaguchi K., Hasunuma R., Kikuchi S., et al. Time- and dose-dependent effect of fosfomycin on suppression of infection-induced endotoxin shock in mice. Biol Pharm Bull. 2002;25(12):1658-1661.
90. Riviere J., Spoo W. Aminoglycosides. In: Adams R., editor. Veterinary pharmacology and therapeutics. ed 8. Ames, Iowa: Iowa State University Press; 2001:828-840.
91. Bamberger D.M., Foxworth J.W., Bridwell D.L., et al. Extravascular antimicrobial distribution and the respective blood and urine concentrations in humans. In: Lorian V., editor. Antibiotics in laboratory medicine. Baltimore: Williams & Wilkins; 2005:799-809.
92. Vakulenko S.B., Mobashery S. Versatility of aminoglycosides and prospects for their future. Clin Microbiol Rev. 2003;16:430-450.
93. Maller R., et al. Once- versus twice-daily amikacin regimen: efficacy and safety in systemic gram-negative infections. J Antimicrob Chemother. 1993;31:939-948.
94. Jacqueline C., Caillon J., Le Mabecque V., et al. In vitro activity of linezolid alone and in combination with gentamicin, vancomycin or rifampicin against methicillin-resistant Staphylococcus aureus by time-kill curve methods. J Antimicrob Chemother. 2003;51(4):857-864.
95. Powell S.H., Thompson W.L., Luthe M.A., et al. Once-daily vs. continuous aminoglycoside dosing: efficacy and toxicity in animal and clinical studies of gentamicin, netilmicin, and tobramycin. J Infect Dis. 1983;147:918-932.
96. Blaser J. Efficacy of once- and thrice-daily dosing of aminoglycosides in in vitro models of infection. J Antimicrob Chemother. 1991;27(Suppl C):21-28.
97. Reiner N.E., Bloxham D.D., Thompson W.L. Nephrotoxicity of gentamicin and tobramycin given once daily or continuously in dogs. J Antimicrob Chemother. 1978;4(Suppl A):85-101.
98. Vanhaeverbeek M., Siska G., Douchamps J., et al. Comparison of the efficacy and safety of amikacin once or twice a day in the treatment of severe gram-negative infections in the elderly. Int J Clin Pharmacol Ther. 1993;31:153-156.
99. Blaser J., Stone B.B., Zinner S.H. Efficacy of intermittent versus continuous administration of netilmicin in a two-compartment in vitro model. Antimicrob Agents Chemother. 1985;27:343-349.
100. Roudebush P., Fales W.H. Antibacterial susceptibility of gentamicin resistant organisms recovered from small companion animals. J Am Anim Hosp Assoc. 1982;18:649-652.
101. Asseray N., Caillon J., Roux N., et al. Different aminoglycoside-resistant phenotypes in a rabbit Staphylococcus aureus endocarditis infection model. Antimicrob Agents Chemother. 2002;46(5):1591-1593.
102. Forgan-Smith W.R., McSweeney R.J. Gentamicin and amikacin—an in vitro comparison using 1000 clinical isolates. Intern Med J. 2008;8:383-386.
103. Barclay M.L., Begg E.J. Aminoglycoside adaptive resistance: importance for effective dosage regimens. Drugs. 2001;61(6):713-721.
104. Mealey K.L., Boothe D.M. Nephrotoxicosis associated with topical administration of gentamicin in a cat. J Am Vet Med Asso. 1994;204:1919-1921.
104a. Kihlström E., Andåker L. Inability of gentamicin and fosfomycin to eliminate intracellular Enterobacteriaceae. J Antimicrob Chemother. 1985;15(6):723-728.
105. Ling G.V., Conzelman G.M.Jr., Franti C.E., et al. Urine concentrations of gentamicin, tobramycin, amikacin, and kanamycin after subcutaneous administration to healthy adult dogs. Am J Vet Res. 1981;42(10):1792-1794.
106. Peters A.M. The kinetic basis of glomerular filtration rate measurement and new concepts of indexation to body size. Eur J Nucl Med Mol Imaging. 2004;31(1):137-149.
107. Riviere J.E., Coppoc G.L. Pharmacokinetics of gentamicin in the juvenile dog. Am J Vet Res. 1981;42(9):1621-1623.
108. Wilson R.C., Duran S.H., Horton C.R.Jr. Bioavailability of gentamicin in dogs after intramuscular or subcutaneous injections. Am J Vet Res. 1989;50(10):1748-1750.
109. Baggot J.D., Ling G.V., Chatfield R.C. Clinical pharmacokinetics of amikacin in dogs. Am J Vet Res. 1985;46(8):1793-1796.
110. Wright L.C., Horton C.R.Jr., Jernigan A.D., et al. Pharmacokinetics of gentamicin after intravenous and subcutaneous injection in obese cats. J Vet Pharmacol Ther. 1991;14(1):96-100.
111. Jernigan A.D., Hatch R.C., Wilson R.C. Pharmacokinetics of tobramycin in cats. Am J Vet Res. 1988;49(5):608-612.
112. Jernigan A.D., Wilson R.C., Hatch R.C. Pharmacokinetics of amikacin in cats. Am J Vet Res. 1988;49(3):355-358.
113. Kukanich B., Coetzee J.F. Comparative pharmacokinetics of amikacin in Greyhound and Beagle dogs. J Vet Pharmacol Ther. 2007;31:102-107.
114. Jernigan A.D., Hatch R.C., Wilson R.C., et al. Pharmacokinetics of gentamicin in cats given Escherichia coli endotoxin. Am J Vet Res. 1988;49(5):603-607.
115. Jernigan A.D., Hatch R.C., Wilson R.C., et al. Pathologic changes and tissue gentamicin concentrations after intravenous gentamicin administration in clinically normal and endotoxemic cats. Am J Vet Res. 1988;49(5):613-617.
116. Kim H.-S., Sohn I.-J., Min D.I. Pharmacokinetics of amikacin and effect of ascites in Korean patients. Am J Health-Syst Pharm. 2002;59:1855-1857.
117. Kim M.-J., Bertino J.S.Jr., Erb T.A., et al. Application of bayes theorem to aminoglycoside-associated nephrotoxicity: comparison of extended-interval dosing, individualized pharmacokinetic monitoring, and multiple-daily dosing. J Clin Pharmacol. 2004;44:696-707.
118. Shy-Modjeska J.S., Riviere J.E., Rawlings J.O. Application of biplot methods to the multivariate analysis of toxicological and pharmacokinetic data. Toxicol Appl Pharmacol. 1984;72(1):91-101.
119. Riviere J.E., Hinsman E.J., Coppoc G.L., et al. Morphological and functional aspects of experimental gentamicin nephrotoxicity in young beagles and foals. Vet Res Commun. 1983;7(1):211-213.
120. Isoherranen N., Lavy E., Soback S. Pharmacokinetics of gentamicin C1, C1a, and C2 in beagles after a single intravenous dose. Antimicrob Agents Chemother. 2000;44(6):1443-1447.
121. Jernigan A.D., Hatch R.C., Brown J., et al. Pharmacokinetic and pathological evaluation of gentamicin in cats given a small intravenous dose repeatedly for five days. Can J Vet Res. 1988;52(2):177-180.
122. Jernigan A.D., Wilson R.C., Hatch R.C., et al. Pharmacokinetics of gentamicin after intravenous, intramuscular, and subcutaneous administration in cats. Am J Vet Res Jan:. 1988;49(1):32-35.
123. Grauer G.F., Greco D.S., Behrend E.N., et al. Estimation of quantitative enzymuria in dogs with gentamicin induced nephrotoxicosis using urine enzyme/creatinine ratios from spot urine samples. J Vet Intern Med. 1995;9(5):324-327.
124. Brown S.A., Garry F.B. Comparison of serum and renal gentamicin concentrations with fractional urinary excretion tests as indicators of nephrotoxicity. J Vet Pharmacol Ther. 1988;11:330-337.
125. Frazier D.L., Aucoin D.P., Riviere J.E. Gentamicin pharmacokinetics and nephrotoxicity in naturally acquired and experimentally induced disease in dogs. J Am Vet Med Assoc. 1988;192:57-63.
126. Boothe D.M. Adverse renal effects of selected drugs, Veterinary previews, Purina Publication for Veterinarians. Veterinary Learning Systems. 1995;2:10-13.
127. Hsu C.H., Kurtz T.W., Easterling R.E., et al. Potentiation of gentamicin nephrotoxicity by metabolic acidosis. Proc Soc Exp Biol Med. 1974;146:894-897.
128. Julien N., Karzazi M., Labrecque G., et al. Temporal modulation of nephrotoxicity, feeding, and drinking in gentamicin-treated rats. Physiol Behav. 2000;68(4):533-541.
129. Prins J.M., Weverling G.J., van Ketel R.J., et al. Circadian variations in serum levels and the renal toxicity of aminoglycosides in patients. Clin Pharmacol Ther. 1997;62:106-111.
130. Cowan R.H., Jukkola A.F., Arant B.S. Pathophysiologic evidence of gentamicin nephrotoxicity in neonatal puppies. Pediatr Res. 1980;14:1204-1211.
131. Brown S.A., Nelson R.W., Moncrieff C.S. Gentamicin pharmacokinetics in diabetic dogs. J Vet Pharmacol Ther. 1991;14:90-95.
132. Chambers H.F. Aminoglycosides. In Brunton L.L., Lazo J.S., Parker K.L., editors: Goodman & Gilman’s the pharmacological basis of therapeutics, ed 11, New York: McGraw Hill, 2006.
133. Kes P., Reiner Z. Symptomatic hypomagnesemia associated with gentamicin therapy. Magnes Trace Elem. 1990;9(1):54-60.
134. Ozbek E., Turkoz Y., Sahna E., et al. Melatonin administration prevents the nephrotoxicity induced by gentamicin. Br Med J (Intl Ed). 2000;85(6):742-746.
135. Kopple J.D., Ding H., Letoha A., et al. L-carnitine ameliorates gentamicin-induced renal injury in rats. Nephrol Dial Transplant. 2002;17:2122-2131.
136. Mazzon E., Britti D., de Sarro A., et al. Effect of N-acetylcysteine on gentamicin-mediated nephropathy in rats. Eur J Pharmacol. 2001;424(1):75-83.
137. Feldman L., Efrati S., Eviatar E., et al. Gentamicin-induced ototoxicity in hemodialysis patients is ameliorated by N-acetylcysteine. Kidney Int. 2007;72(3):359-363.
138. Konishi H., Goto M., Nakamoto Y., et al. Tobramycin inactivation by carbenicillin, ticarcillin and piperacillin. Antimicrob Agents Chemother. 1983;23:654-657.
139. Uber W.E., Brundage R.C., White R.L., et al. In vivo inactivation of tobramycin by piperacillin. Ann Pharmacother. 1991;25:357-359.
140. Ariano R.E., Kassume D.A., Meatherall R.C., et al. Lack of in vitro inactivation of tobramycin by imipenem/cilastin. Ann Pharmacother. 1992;26:1075-1077.
140a. Atilla A., Boothe H.W., Tollett M., Duran S., Campos Diaz H., Boothe D.M. In vitro elution of amikacin and vancomycin from impregnated plaster of Paris beads. Accepted for publication. Vet Surg 39: 715–721. 2010.
141. Riviere J.E., Carver M.P., Coppoc G.L., et al. Pharmacokinetics and comparative nephrotoxicity of fixed-dose versus fixed-interval reduction of gentamicin dosage in subtotal nephrectomized dogs. Toxicol Appl Pharmacol. 1984;75(3):496-509.
142. Barza M., Loannidis J.P.A., Cappelleri J.C., et al. Single or multiple daily doses of aminoglycosides: a meta-analysis. Br Med J. 1996;312:338-345.
143. Bailey T.C., Little J.R., Littenberg B., et al. A meta-analysis of extended-interval dosing versus multiple daily dosing of aminoglycosides. Clin Infect Dis. 1997;24(5):786-795.
144. Ali M.Z., Goetz M.B. A meta-analysis of the relative efficacy and toxicity of single daily dosing versus multiple daily dosing of aminoglycosides. Clin Infect Dis. 1997;24(5):796-809.
145. Gilbert D.N., Lee B.L., Dworkin R.J., et al. A randomized comparison of the safety and efficacy of once-daily gentamicin or thrice-daily gentamicin in combination with ticarcillin-clavulanate. Am J Med. 1998;105(3):182-191.
146. Wallace A.W., Jones M., Bertino J.S. Evaluation of four once-daily aminoglycoside dosing nomograms. Pharmacotherapy. 2002;22(9):1077-1083.
147. Woeltje K.F., Ritchie D.J. Antimicrobials. In: Carey C.F., Lee H.H., Woeltje K.F., editors. The Washington manual of medical therapeutics. ed 29. Philadelphia: Lippincott-Raven; 1998:250-251.
148. Rougier F., Claude D., Maurin M., et al. Aminoglycoside nephrotoxicity. Curr Drug Targets Infec Disord. 2004;4:153-162.
149. Kingsley P, Coulthard D G, Peckham SP, Conway et al: Therapeutic drug monitoring of once daily tobramycin in cystic fibrosis—caution with trough concentrations. Accessed April 2007, at http://www.cysticfibrosismedicine.com 6(2):125–130, 2001.
150. Neu H.C. The quinolones. Infect Dis Clin North Am. 1989;3:625-640.
151. Schmitz F.J., Higgins P.G., Mayer S. Activity of quinolones against gram-positive cocci: mechanisms of drug action and bacterial resistance. Eur J Clin Microbiol Infect Dis. 2002;21:647-659.
152. Petri W.A.Jr. Chemotherapy of tuberculosis, Mycobacterium avium complex disease, and leprosy. In Brunton L.L., Lazo J.S., Parker K.L., editors: Goodman & Gilman’s the pharmacological basis of therapeutics, ed 11, New York: McGraw-Hill, 2006.
153. Ng E.Y., Truckis M., Hooper D.C. Quinolone resistance mutations in topoisomerase IV: Relationship to target of fluoroquinolones in Staphylococcus aureus. Antimicrob Agents Chemother. 1996;40:1881-1888.
154. Ginsburg A.S., Grosset J.H., Bishai W.R. Fluoroquinolones, tuberculosis and resistance. The Lancet Infect Dis. 2003;3:432-442.
155. Power E.G.M., Bellido J.L.M., Phillips I. Detection of ciprofloxacin resistance in gram-negative bacteria due to alterations in gyrA. J Antimicrob Chemother. 1992;29:9-17.
156. Prescott J.F., Yielding K.M. In vitro susceptibility of selected veterinary bacterial pathogens to ciprofloxacin, enrofloxacin and norfloxacin. Can J Vet Res. 1990;54:195-197.
157. Witte W., Grimm H. Occurrence of quinolone resistance in Staphylococcus aureus from nosocomial infection. Epidemiol Infect. 1992;109:413-421.
158. Wetzstein HG, Schmeer N: Bactericidal activity of enrofloxacin against Escherichia coli growing under strictly anaerobic conditions, Proceedings of the 95th General Meeting, American Society of Microbiologists, Washington, DC, A-37, 1995.
159. van de Hoven R., Wagenaar J.A., Walker R.D. In vitro activity of difloxacin against canine bacterial isolates. J Vet Diagn Invest. 2000;12:218-233.
160. Wetzstein H.G. The in vitro postantibiotic effect of enrofloxacin, Proc 18th World Buiatrics Congress, Bologna. Italy. 1994;18:615-618.
161. Walker R.D., Stein G.E., Hauptman J.G., et al. Pharmacokinetic evaluation of enrofloxacin administered orally to healthy dogs. Am J Vet Res. 1992;53:2315-2319.
162. McKinnon P.S., Davis S.L. Pharmacokinetic and pharmacodynamic issues in the treatment of bacterial infectious diseases. Eur J Clin Microbiol Infect Dis. 2004;23:271-288.
163. Schentag J.J., Meagher A.K., Forrest A. Fluoroquinolone AUIC break points and the link to bacterial killing rates. Part 1: In vitro and animal models. Ann Pharmacother. 2003;37(9):1287-1298.
164. Boothe DM, Boeckh A, Slimpson RB, et al: Comparison of pharmacodynamic and pharmacokinetic indices of efficacy for 5 fluoroquinolones toward pathogens of dogs and cats, J Vet Intern Med 20(6):1297–13306, 2006.
165a. Shaheen B.S., Nayak R., Boothe D.M. Identification of novel mutations and high incidence of plasmid mediated quinolone resistance determinants among extended-spectrum cephalosporins in Escherichia coli isolates from companion animals in the United States. Toronto: Presented at the American Society of Microbiology Conference Antimicrobial Resistance in Zoonotic Bacteria and Foodborne Pathogens; June 8-11, 2010.
165. Hopkins K.L., Davies R.H., Threlfall E.J. Mechanisms of quinolone resistance in Escherichia coli and Salmonella: recent developments. Int J Antimicrob Agents. 2005;25:358-373.
166. Riddle C., Lemons C.L., Papich M.G., et al. Evaluation of ciprofloaxcin as a representative veterinary fluoroquinolone in susceptibility testing. J Clin Microbiol. 2000;38(4):1636-1637.
167. Pfaller M.A., Jones R.N. Trends in ciprofloxacin nonsusceptibility and levofloxacin resistance among Streptococcus pneumoniae isolates in North America. J Clin Microbiol. 2001;39(7):2748-2750.
168. Breitschwerdt E.B., Papich M.G., Hegarty B.C., et al. Efficacy of doxycycline, azithromycin, or trovafloxacin for treatment of experimental rocky mountain spotted fever in dogs. Antimicrob Agents Chemother. 1999;43(4):813-821.
169. Kang S.L., Rybak M.J., McGrath B.J., et al. Pharmacodynamics of levofloxacin, ofloxacin, and ciprofloxacin, alone and in combination with rifampin, against methicillin-susceptible and –resistant Staphylococcus aureus in an in vitro infection model. Antimicrob Agents Chemother. 1994;38(12):2702-2709.
170. Fritsche T.R., Sader H.S., Jones R.N. Epidemiology of antimicrobial resistance: species prevalence, susceptiblity profiles and resistance trends. In: Lorian V., editor. Antibiotics in laboratory medicine. Baltimore: Williams & Wilkins; 2005:815-850.
171. Hecht D.W., Wexler H.M. In vitro susceptibility of anaerobes to quinolones in the United States. Clin Infect Dis. 1996;23:S2-S8.
172. Drlica K., Zhao X., Blondeau J.M., et al. Low correlation between MIC and mutant prevention concentration. Antimicrob Agents Chemother. 2006;50(1):403-404.
173. Sánchez Navarro M.D., Sayalero Marinero M.L. Sánchez Navarro A: Pharmacokinetic/pharmacodynamic modelling of ciprofloxacin 250 mg/12 h versus 500 mg/24 h for urinary infections. J Antimicrob Chemother. 2002;50:67-72.
174. Marchbanks C.R., McKiel J.R., Gilbert D.H., et al. Dose ranging and fractionation of intravenous ciprofloxacin against Pseudomonas aeruginosa and Staphylococcus aureus in an in vitro model of infection. Antimicrob Agents Chemother. 1993;37:1756-1763.
175. Cole L.K., Kwochka K., Kowalski J., et al. Microbial flora and antimicrobial susceptibility patterns of isolated pathogens from the horizontal ear canal and middle ear in dogs with otitis media. J Amer Anim Hosp Assoc. 1998;212:534-538.
176. Boothe D.M., Smaha T., Carpenter M., et al. Emerging resistance in canine and feline Escherchia coli pathogens: a pilot surveillance study. Submitted to J Vet Int Med. March 2009.
177. Hooper D.C. Emerging mechanisms of fluoroquinolone resistance. Emerg Infect Dis. 7(2), 2001. Accessed November 12, 2009 at www.cdc.gov/ncidod/eid/vol7no2/hooper.htm
178. Debavalya N., Boothe D.M., Hathcock T. Multi-drug resistance in fecal Escherichia coli following routine enrofloxacin but not amoxicillin therapy in dogs. Am Coll Vet Int Med (Proceedings). 2008.
179. Shaheen B.S., Boothe D.M., Oyarzabal O., et al. The contribution of gyrA mutation and efflux pumps to fluoroquinolone and multi-drug resistance in canine and feline pathogenic Escherichia coli isolates from the US. In print. Am J Vet Res. 2010.
179a. Shaheen B.W., Boothe D.M., Oyarzabal O.A., et al. Antimicrobial resistance profiles and clonal relatedness of canine and feline Escherichia coli pathogens expressing multidrug resistance in the United States. J Vet Intern Med Mar-Apr:. 2010;24(2):323-330.
180. Wetzstein H.G. Comparative mutant prevention concentrations of pradofloxacin and other veterinary fluoroquinolones indicate differing potentials in preventing selection of resistance. Antimicrob Agents Chemother. 2005;49(10):4166-4173.
181. Pasquali F., Manfreda G. Mutant prevention concentration of ciprofloxacin and enrofloxacin against Echerichia coli, Salmonella Typhimurium and. Pseudomonas aeruginosa, Vet Microbiol. 2007;119:304-310.
182. Schwaber M., Cosgrove S.E., Gold H. Fluoroquinolones protective against cephalosporin resistance in gram negative nosocomial pathogens. Emerging Infectious Diseases. 2004;10(1):94-99.
183. Karlowsky J.A. Susceptibilities to levofloxacin in Streptococcus pneumoniae, Haemophilus influenzae, and Moraxella catarrhalis clinical isolates from children: results from 2000-2001 and 2001-2002 TRUST studies in the United States. Antimicrob Agents Chemother. 2003;47(6):1790-1797.
184. Seral C., Barcia-Macay M., Mingeot-Leclercq P., et al. Comparative activity of quinolones (ciprofloxacin, levofloxacin, moxifloxacin and garenoxacin) against extracellular and intracellular infection by Listeria monocytogenes and Staphylococcus aureus in J774 macrophages. J Antimicrob Chemother. 2005;55:511-517.
185. Seguin A., Papich M.G., Siegle K.J., et al. Pharmacokientics of enrofloxacin in neonatal kittens. Am J Vet Res. 2004;65:350-356.
186. Bidgood T.L., Papich M.G. Plasma and interstitial fluid pharmacokinetics of enrofloxacin, its metabolite ciprofloxacin, and marbofloxacin after oral administration and a constant rate intravenous infusion in dogs. J Vet Pharmacol Therap. 2005;28:329-341.
187. Isaccs A, Boothe DM, Axlund T: Comparative distribution of fluorquinolons in the brain and cerebral spinal fluid of dogs, 2010 (In preparation)
188. Boothe D.M., Boeckh A., Boothe H.W., et al. Tissue concentrations of enrofloxacin and ciprofloxacin in anesthetized dogs following single intravenous administration. Vet Ther. 2001;2:120-128.
189. Frazier D.L., Thompson L., Trettien A., et al. Comparison of fluoroquinolone pharmacokinetic parameters after treatment with marbofloxacin, enrofloxacin, and difloxacin in dogs. J Vet Pharmacol Therap. 2000;23:293-302.
190. Boothe D.M., Boothe H.W., Doornink M. Pharmacokinetic and pharmacodynamic indices of pradofloxacin efficacy in canine serum, and subcutaneous interstitial fluid. Berlin, Germany: Presented as a final report to Bayer Animal Health; 2006.
191. Regnier A., Concordet D., Schneider M., et al. Population pharmacokientics of marbofloxacin in aqueous humor after intravenous administration in dogs. Am J Vet Res. 2003;64:899-993.
192. Boothe D.M., Boeckh A., Boothe H.W., et al. Tissue concentrations of enrofloxacin and ciprofloxacin in anesthetized dogs following single intravenous administration. Vet Ther. 2001;2:120-128.
193. Boeckh A., Boothe D.M., Wilkie S., et al. Time course of enrofloxacin and its active metabolite in peripheral leukocytes of dogs. Vet Ther. 2001;2:334-344.
194. Hawkins E.C., Boothe D.M., Guinn A., et al. Concentration of enrofloxacin and its active metabolite in alveolar macrophages and pulmonary epithelial lining fluid of dogs. J Vet Pharmacol Ther: Feb:. 1998;21(1):18-23.
195. Boothe H.W., Jones S.A., Wilkie W.S., et al. Evaluation of the concentration of marbofloxacin in alveolar macrophages and pulmonary epithelial lining fluid after administration in dogs. Am J Vet Res. 2005;66:1770-1774.
196. Boothe D.M., Boeckh A., Boothe H.W. Evaluation of the distribution of enrofloxacin by circulating leukocytes to sites of inflammation in dogs. Am J Vet Res Jan:. 2009;70(1):16-22.
197. Carbon C. Clinical relevance of intracellular and extracellular concentrations of macrolides. Infection. 1995;23:S10-S14.
198. Lefebvre H.P., Schneider M., Dupouy V., et al. Effects of experimental renal impairment on disposition of marbofloxacin and its metabolites in the dog. J Vet Pharmcol Ther. 1998;21:453-461.
199. Boothe D.M., Boeckh A., Boothe H.W., et al. Plasma concentrations of enrofloxacin and its active metabolite ciprofloxacin in dogs following single oral administration of enrofloxacin at 7.5, 10, or 20 mg/kg. Vet Ther. 2002;3(4):409-419.
200. Heinen E. Comparative serum pharmacokinetics of the fluoroquinolones enrofloxacin, difloxacin, marbofloxacin, and orbifloxacin in dogs after single oral administration. J Vet Pharmacol Therap. 2002;25:1-5.
201. Abadıá A.R., Aramayona J.J., Munõz M.J., et al. Disposition of ciprofloxacin following intravenous administration in dogs. J Vet Pharmacol The. 1994;17:384-388.
202. Abadıá A.R., Aramayona J.J., Munõz M.J., et al. Ciprofloxacin pharmacokinetics in dogs following oral administration. J Vet Med. 1995;42:505-511.
203. Dalhoff A., Bergan T. Pharmacokinetics of fluoroquinolones in experimental animals. In: Kuhlman J., Dalhoff A., Zeiler H.J., editors. Quinolone antibacterials. Berlin: Springer Verlag; 1998:188-189.
204. Albarellos G., Montoya L., Ambros L., et al. Multiple once-daily dose pharmacokinetics and renal safety of gentamicin in dogs. J Vet Pharmacol Therap. 2004;27:21-25.
205. Albarellos G.A., Kreil V.E., Landoni M.F. Pharmacokinetics of ciprofloxacin after single intravenous and repeat oral administration to cats. J Vet Pharmacol Therap. 2004;27:155-162.
206. Miyamoto K. Use of plasma clearance of iohexol for estimating glomerular filtration rate in cats. Am J Vet Res. 2001;62(4):572-575.
207. Marchetti F., Viale P. Current and future perspectives for levofloxacin in severe Pseudomonas aeruginosa infections. J Chemother. 2003;15(4):315-322.
208. Fish D.N., Chow A.T. The clinical pharmacokinetics of levofloxacin. Clin Pharmacokinet. 1997;32(2):101-119.
209. Yoshida K., Yabe K., Nishida S., et al. Pharmacokinetic disposition and arthropathic potential of oral ofloxacin in dogs. J Vet Pharmacol Therap. 1998;21:128-132.
210. Albarellos G.A., Ambros L.A., Landoni M.F. Pharmacokinetics of levofloxacin after single intravenous and repeat oral administration to cats. J Vet Pharmacol Therap. 2005;28:363-369.
211. Intorre L., Mengozzi G., Maccheroni M., et al. Enrofloxacin-theophylline interaction: influence of enrofloxacin on theophylline steady state pharmacokinetics in the beagle dog. J Vet Pharmacol Ther. 1995;18:352-356.
212. Hirt R.A., Teinfalt M., Dederichs D. The effect of orally administered marbofloxacin on the pharmacokinetics of theophylline. J Vet Med Assoc. 2003;50:246-250.
213. Landor M., Iashinsky A., Waxman J. Quinolone allergy? Ann Allergy Asthma Immunol. 1996;77:273-276.
214. Davenport C.M., Boston R.C., Richards D.W. Enrofloxacin and magnesium deficiency on matrix metabolism in equie articular cartilage. Am M Vet Res. 2001;62:160-166.
215. Ergerbacher M., Edinger J., Tschulenk W. Effects of enrofloxcin and ciprofloxacin hydrochloride on canine and equine chondrocytes in culture. Am J Vet Res. 2001;63:704-708.
216. Stahlmann R., Forster C., Shakiboei M., et al. Magnesium deficiency induces joint cartilage lesions in juvenile rats which are identical to quinolone-induced arthopathy. Antimicrob Agents Chemother. 1995;39:2013-2018.
217. Ergerbacher M., Wolfesberger B., Gabler C. In vitro evidence for effects of magnesium supplementation on quinolone-treated horse and dog chondrocytes. Vet Pathol. 2001;38(2):143-148.
218. Huddleston P.M., Hanssen A.D., Rouse M.S., et al. Ciprofloxacin inhibition of experimental fracture-healing. The Fluoroquinolone Toxicity Research Foundation; 2003.
219. Shakibaei M., de Souza P., van Sickle D. Biochemical changes in achilles tendon from juvenile dogs after treatment with ciprofloxacin or feeding a magnesium-deficient diet. Arch Toxicol. 2001;75(6):369-374.
220. Halliwell R.F., Davey P.G., Lambert J.J. The effects of quinolones and NSAIDS upon GABA-evoked currents recorded from rat dorsal root ganglion neurons. J Antimicrob Chemother. 1991;27:209-218.
221. De Sarro A., Cecchetti V., Fravolini V., et al. Effects of novel 6-desfluoroquinolones and classic quinolones on Pentylenetetrazole-induced seizures in mice. Antimicrob Agents Chemother. 1999;43(7):1729-1736.
222. Lode H. Potential interactions of the extended-spectrum fluoroquinolones with the CNS. Drug Safety. 1999;21:123-135.
223. Cohn J.S. Peripheral neuropathy associated with fluoroquinolones. Ann Pharmacother. 34(1), 2001.
224. Gelatt K.N., Van der Woerdt A., Ketring K.L., et al. Enrofloxacin associated retinal degeneration in cats. Vet Ophthalmol. 2001;4:99-106.
225. Wiebe V., Hamilton P. Fluoroqinolone-induced retinal degeneration in cats. Am Vet Med Assoc. 2002;221:1508-1571.
226. Marutani K., Matsumoto M., Otabe Y., et al. Reduced phototoxicity of a fluoroquinolone antibacterial agen with a methoxy group at the 8 position in mice irradiated with long-wave length UV light. Antimicrob Agents Chemother. 1993;37:2217-2222.
227. Miller C.W., Prescott J.R., Mathews K.A., et al. Streptococcal toxic shock syndrome in dogs. J Am Vet Med Assoc. 1996;209:1421-1426.
228. Ingrey K.T., Ren J., Prescott J.F. A fluoroquinolone induces a novel mitogen-encoding bacteriophage in. Streptococcus canis, Infect Immun. 2003;71(6):3028-3033.
229. Baciewicz A.M., Chrisman C.R., Finch C.K., et al. Update on rifampin and rifabutin drug interactions. Am J Med Sci. 2008;335(2):126-136.
230. Ziglam H.M., Daniels I., Finch R.G. Immunomodulating activity of rifampicin. J Chemother. 2004;16(4):357-361.
231. Adachi J.A., DuPont H.L. Rifaximin: a novel nonabsorbed rifamycin for gastrointestinal disorders. Clin Infect Dis. 2006;42:541-547.
232. Phillips M.A., Stanley S.L.Jr. Chemotherapy of protozoal infections: amebiasis, giardiasis, trichomoniasis, trypanosomiasis, leishmaniasis, and other protozoal infections. In Brunton L.L., Lazo J.S., Parker K.L., editors: Goodman & Gilman’s the pharmacological basis of therapeutics, ed 11, New York: McGraw-Hill, 2006.
233. Muller M. Mode of action of metronidazole on anaerobic bacteria and protozoa. Surgery. 1983;93:165-171.
234. Levett P.N. Time-dependent killing effect of Clostridium difficile by metronidazole and vancomycin. J Antimicrob Chemother. 1991;27:55-62.
235. Karjagin J., Pähkla R., Karki T., et al. Distribution of metronidazole in muscle tissue of patients with septic shock and its efficacy against. Bacteroides fragilis in vitro, J Antimicrob Chemother. 2005;55:341-346.
236. Nix D.E., Tyrrell R., Muller M. Pharmacodynamics of metronidazole determined by a time-kill assay for Trichomonas vaginalis. Antimicrob Agents Chemother. 1995;39(8):1848-1852.
237. Neff-Davis C.A., Davis L.E., Gillette E.L. Metronidazole: a method for its determination in biological fluids and its disposition kinetics in the dog. J Vet Pharmacol Ther. 1981;4(2):121-127.
238. Sekis I., Ramstead K., Rishniw M., et al. Single-dose pharmacokinetics and genotoxicity of metronidazole in cats. J Feline Med Surg. 2009;11:60-68.
239. Fitch R., Moore M., Roen D. A warning to clinicians: metronidazole neurotoxicity in a dog. Probl Vet Neurol. 1991;2:307-309.
240. Heaney C.J., Campeau N.G., Lindell E.P. MR imaging and diffusion-weighted imaging changes in metronidazole (Flagyl)-induced cerebellar toxicity. Am J Neuroradiol. 2003;24:1615-1617.
241. Evans J., Levesque D., Knowles K. Diazepam as a treatment for metronidazole toxicosis: a retrospective study of 21 dogs. J Vet Intern Med. 2003;17:304-310.
242. Caylor K.B., Cassimatis M.K. Metronidazole neurotoxicosis in two cats. J Am Anim Hosp Assoc. 2001;37(3):258-262.
243. Olson E.J., Morales S.C., McVey A.S., et al. Putative metronidazole neurotoxicosis in a cat. Vet Pathol. 2005;42:665-669.
244. Davidson G. To benzoate or not to benzoate: cats are the question. Int J Pharm Compound. 2001;5:89-90.
245. Wu Y., Fassihi R. Stability of metronidazole, tetracycline HCl and famotidine alone and in combination. Int J Pharm. 2005;290:1-13.
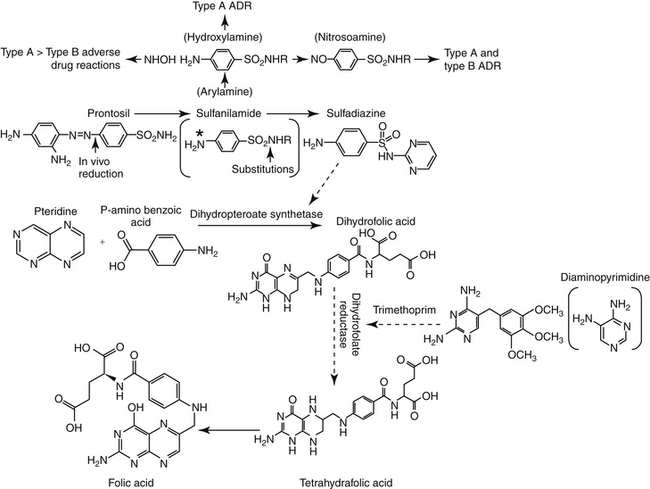
246. Petri W.A.Jr. : Sulfonamides, trimethoprim-sulfamethoxazole, quinolones, and agents for urinary tract infections. In Brunton L.L., Lazo J.S., Parker K.L., editors: Goodman & Gilman’s the pharmacological basis of therapeutics, ed 11, New York: McGraw-Hill, 2006.
247. Hirsch D.C., Biberstein E.L., Jang S.S. Obligate anaerobes in clinical veterinary practice. J Clin Microbiol. 1979;10:188-191.
248. Hirsch D.C., Indiveri M.C., Jang S.S., et al. Changes in prevalence and susceptibility of obligate anaerobes in clinical veterinary practice. J Am Vet Med Assoc. 1985;186(10):1086-1089.
249. Indiveri M.C., Hirsch D.W. Susceptibility of obligate anaerobes to trimethoprim-sulfamethoxazole. J Am Vet Med Assoc. 1986;188:46-48.
249a. Kuo C.C., Wang S., Grayston J.T. Antimicrobial activity of several antibiotics and a sulfonamide against Chlamydia trachomatis organisms in cell culture. Antimicrob Agents Chemother. 1977;12(1):80-83.
250. Sharer W.C., Fair W.R. The pharmacokinetics of antibiotic diffusion in chronic bacterial prostatitis. Prostate. 1982;3(2):139-148.
251. Trepanier L.A., Ray K., Winand N.J., et al. Cytosolic arylamine N-acetyltransferase (NAT) deficiency in the dog and other canids due to an absence of NAT genes. Biochem Pharmacol. 1997;54(1):73-80.
252. Trepanier L.A. Idiosyncratic toxicity associated with potential sulfonamides in the dog. J Vet Pharmacol Therap. 2004;27:129-138.
253. Hall I.A., Campbell K., Chambers M.D., et al. Effect of trimethoprim-sulfamethoxazole on thyroid function in dogs with pyoderma. J Am Vet Med Assoc. 1993;202:1959-1962.
254. Trepanier L.A., Danhof R., Toll J., et al. Clinical findings in 40 dogs with hypersensitivity associated with administration of potentiated sulfonamides. J Vet Intern Med. 2003;17:647-652.
255. Chopra I. New developments in tetracycline antibiotics: glycylcyclines and tetracycline efflux pump inhibitors. Drug Resist Updat. 2002;5:119-125.
256. Westfall D.S., Twedt D.C., Steyn P.F., et al. Evaluation of esophageal transit of tablets and capsules in 30 cats. J Vet Intern Med. 2008;15(5):467-470.
257. Carlborg B., Densert O. Esophageal lesions caused by orally administered drugs. An experimental study in the cat. Eur Surg Res. 1980;12(4):270-282.
258. Apaydin B.B., Paksoy M., Art T., et al. Influence of pentoxifylline and interferon-alpha on prevention of stricture due to corrosive esophagitis. Eur Surg Res. 2001;33:225-231.
259. Saiman L., Liu Z., Chen Y. Synergistic activity of macrolide antibioitics paired with conventional antimicrobial agents against multiply antibiotic resistant P aeruginosa isolated from CF patients. Antimicrob Agents Chemother. 2002;46(4):1105-1107.
260. Park B.-K., Lim J.-H., Kim M.-S., et al. Pharmacokinetics of flor-fenicol and its metabolite, florfenicol amine, in dogs. Res Vet Sci. 2008;84:85-89.
261. Papich M.G., Riviere J. Chloramphenicol. In: Adams R., editor. Veterinary pharmacology and therapeutics. ed 8. Ames, Iowa: Iowa State University Press; 2001:868-897.
262. Watson A.D.J. Chloramphenicol in the dog: observations of plasma levels following oral administration. Res Vet Sci. 1974;16:147-151.
263. Glazko A.J., Wolf L.M., Dill W.A., et al. Biochemical studies on chloramphenicol (chloromycetin). J Pharm Exp Ther. 1949;96:445-449.
264. Watson A.D. Chloramphenicol 2. Clinical pharmacology in dogs and cats. Aust Vet J. 1991;68(1):2-5.
265. Watson A.D.J. Plasma chloramphenicol concentrations in cats after parenteral administration of chloramphenicol sodium succinate. J Vet Pharamcol Therap. 1979;2:123-127.
266. Watson A.D.J. Effect of ingesta on systemic availability of chloramphenicol from two oral preparations in cats. J Vet Pharmacol Therap. 1979;2:117-121.
267. Papich M.G. Florfenicol pharmacokinetics in dogs and cats (Abstract No. 235). Chicago, IL: 17th Annual Veterinary Medical Forum, American College of Veterinary Internal Medicine; June 10-13, 1999.
267a. Michel J., Bornstein H., Luboshitzky R., et al. Mechanisms of chlorampenicol-cephalordine synergism on Enterobacteiaeae. Antimicrob Agents Chemother. 1975;7(6):845-849.
268. Adams H.R., Dixit B.N. Prolongation of pentobarbital by chloramphenicol in dogs and cats. J Am Vet Med Assoc. 1970;156(7):902-905.
269. Sanders J.E., Yeary R.A., Fenner W.R., et al. Interaction of phenytoin with chloramphenicol or pentobarbital in the dog. J Am Vet Med Assoc. 1979;175(2):177-180.
270. Turco J.D. Pharmacokinetics and interactions of digoxin with phenobarbital in dogs. Am J Vet Res. 1987;48(8):1244-1249.
271. Boothe D.M., Brown S.A., Fate G.D., et al. Plasma disposition of clindamycin microbiologic activity in cats after single oral doses of clindamycin hydrochloride as either capsules or aqueous solution. J Vet Pharmacol Ther. 1996;19:491-494.
272. Lavy E., Ziv G., Shem-Tove M., et al. Pharmacokinetics of clindamycin HCl administered intravenously, intramuscularly, and subcutaneously to dogs. J Vet Pharmacol Therap. 1999;22:261-265.
273. Yamasaki T., Ichimiya T., Hirai K., et al. Effect of antimicrobial agents on the piliation of Pseudomonas aeruginosa and adherence to mouse tracheal epithelium. J Chemother. 1997;9:32-37.
274. Asaka T., Manaka A., Sugiyama H. Recent developments in macrolide antimicrobial research. Curr Top Med Chem. 2003;3:961-989.
275. Schlunzen F., Harms J.M. Structural basis for the antibiotic activity of ketolides and azalides. Structure. 2003;11:329-338.
276. Dorfman M.S., Wagner R.S., Jamison T., et al. The pharmacodynamic properties of azithromycin in a kinetics-of-kill model and implications for bacterial conjunctivitis treatment. Adv Ther. 2008;25(3):208-217.
277. Albarellos G.A., Kreil V.E., Ambros L.A., et al. Pharmacokinetics of erythromycin after the administration of intravenous and various oral dosage forms to dogs. J Vet Pharmacol Ther. 2008;31(6):496-500.
278. Garver E., Hugger E.D., Shearn S.P., et al. Involvement of intestinal uptake transporters in the absorption of azithromycin and clarithromycin in the rat. Drug Metab Dispos. 2008;36:2492-2498.
279. Shepard R.M., Falkner F.C. Pharmacokinetics of azithromycin in rats and dogs. J Antimicrob Chemother. 1990;25(Suppl A):49-60.
280. Hunter R.P., Lynch M.J., Ericson J.F. Pharmacokinetics, oral bioavailability and tissue distribution of azithromycin in cats. J Vet Pharmacol Ther. 1995;18(1):38-46.
280a. Haddad A., Davis M., Lagman R. The pharmacological importance of cytochrome CYP3A4 in the palliation of symptoms: review and recommendations for avoiding adverse drug interactions. Support Care Cancer. 2007;15(3):251-257.
281. Bizjak E.D., Mauro V.F. Digoxin-macrolide drug interaction. Ann Pharmacother. 1997;31(9):1077-1079.
282. Sugie M., Asakura E., Zhao Y.L., et al. Possible involvement of the drug transporters P glycoprotein and multidrug resistance-associated protein Mrp2 in disposition of azithromycin. Antimicrob Agents Chemother. 2004;48(3):809-814.
283. Carfartan G., Gerardin P., Turck D., et al. Effect of subinhibitory concentrations of azithromycin on adherence of Pseudomonas aeruginosa to bronchial mucins collected from cystic fibrosis patients. J Antimicrob Chemother. 2004;53:686-688.
284. Gillis R.J., Iglewski B.H. Azithromycin retards Pseudomonas aeruginosa biofilm formation. J Clin Microbiol. 2004;42(12):5842-5845.
285. Kourlas H. Anti-inflammatory properties of macrolide antibiotics. J Pharm Pract. 2006;19(5):326-329.
286. Amsden G.W. Anti-inflammatory effects of macrolides—an underappreciated benefit in the treatment of community-acquired respiratory tract infections and chronic inflammatory pulmonary conditions? J Antimicrob Chemother. 2005;55:10-21.
287. Lorenz J. Telithromycin: the first ketolide antibacterial for the treatment of community acquired respiratory infections. Int J Clin Pract. 2003;57:519-529.
288. Bozdogan B., Applebaum P.C. Oxazolidinones: activity, mode of action, and mechanism of resistance. Int J Antimicrob Agents. 2004;23:113-119.
289. Yagi B.H., Zurenko G.E. An in vitro time-kill assessment of linezolid and anaerobic bacteria. Anaerobe. 2003;9(1):1-3.
290. Ntziora F, Falagas ME: Linezolid for the treatment of patients with mycobacterial infections: a systematic review. Int J Tuberc Lung Dis. 2007;11(6):606-611.
291. Brown-Elliott B.A., Ward S.C., et al. In vitro activities of linezolid against multiple Nocardia species. Antimicrob Agents Chemother. 2001;45(4):1295-1297.
292. Smith A.J., Hall V., Thakker B., et al. Antimicrobial susceptibility testing of Actinomyces species with 12 antimicrobial agents. J Antimicrob Chemother. 2005;56(2):407-409.
293. Slatter J.G., Adams L.A., Bush E.C., et al. Pharmacokinetics, toxicokinetics, distribution, metabolism and excretion of linezolid in mouse, rat and dog. Xenobiotica. 2002;32(10):907-924.
294. Garrabou G., Soriano A., Lopez S., et al. Reversible inhibition of mitochondrial protein synthesis during linezolid-related hyperlactatemia. Antimicrob Agents Chemother. 2007;51(3):962-967.
295. Oleson F.B.Jr., Berman C.L., Kirkpatrick J.B., et al. Once-daily dosing in dogs optimizes daptomycin safety. Antimicrob Agents Chemother. 2000;44(11):2948-2953.
296. Rybníček J., Hill P.B. Suspected polymyxin B-induced pemphigus vulgaris in a dog. Vet Dermatol. 2007;18(3):165-170.
297. Spann C.T., Turtrone W.D., Weinberg J.M. Topical antibacterial agents for wound care: a primer. Dermatol Surg. 2003;29:620-626.