CHAPTER 19 Clinical Manifestations of Lower Respiratory Tract Disorders
CLINICAL SIGNS
In this discussion, the term lower respiratory tract disorders refers to diseases of the trachea, bronchi, bronchioles, alveoli, interstitium, and vasculature of the lung (Box 19-1). Dogs and cats with diseases of the lower respiratory tract are commonly seen for evaluation of cough. Lower respiratory tract diseases that interfere with the oxygenation of blood can result in respiratory distress, exercise intolerance, weakness, cyanosis, or syncope. Nonlocalizing signs such as fever, anorexia, weight loss, and depression also occur and are the only presenting sign in some animals. In rare instances, potentially misleading signs, such as vomiting, can occur in animals with lower respiratory tract disease. Auscultation and thoracic radiography help localize the disease to the lower respiratory tract in these animals. The two major presenting signs in animals with lower respiratory tract disease, cough and respiratory distress, can be further characterized by a careful history and physical examination.
 BOX 19-1 Differential Diagnoses for Lower Respiratory Tract Disease in Dogs and Cats
BOX 19-1 Differential Diagnoses for Lower Respiratory Tract Disease in Dogs and Cats
COUGH
A cough is an explosive release of air from the lungs through the mouth. It is generally a protective reflex to expel material from the airways, although inflammation or compression of the airways can also stimulate cough. Cough is sometimes caused by disease outside of the lower respiratory tract. Chylothorax can cause cough. Although not well documented in dogs or cats, gastroesophageal reflux and postnasal drip are common causes of cough in people.
Classically, differential diagnoses for cough are divided into those that cause productive cough and those that cause nonproductive cough. A productive cough results in the delivery of mucus, exudate, edema fluid, or blood from the airways into the oral cavity. A moist sound can often be heard during the cough. Animals rarely expectorate the fluid, but swallowing can be seen after a coughing episode. If expectoration occurs, clients may confuse the cough with vomiting. In human medicine, categorizing cough as productive or nonproductive is rarely difficult because the patient can report the coughing up of secretions. In veterinary medicine, recognition of a productive cough is more difficult. If the owner or veterinarian has heard or seen evidence that the cough is productive, it usually is. However, not hearing or seeing evidence of productivity does not rule out the possibility of its presence. Productive coughs are most commonly caused by inflammatory or infectious diseases of the airways or alveoli and by heart failure (Box 19-2).
 BOX 19-2 Differential Diagnoses for Productive Cough* in Dogs and Cats
BOX 19-2 Differential Diagnoses for Productive Cough* in Dogs and Cats
* Because it can be difficult to determine the productive nature of a cough in veterinary medicine, these differential diagnoses should also be considered in patients with nonproductive cough.
† Diseases of the lower respiratory tract disease most often associated with cough in cats. Cough in cats is rarely identified as productive.
Hemoptysis is the coughing up of blood. Blood-tinged saliva may be observed within the oral cavity or dripping from the commissures of the mouth after a cough. Hemoptysis is an unusual clinical sign that most commonly occurs in animals with heartworm disease or pulmonary neoplasia. Less common causes of hemoptysis are mycotic infections, foreign bodies, severe congestive heart failure, thromboembolic disease, lung lobe torsion, and some systemic bleeding disorders such as disseminated intravascular coagulation (see Box 19-2).
Intensity of cough is useful in prioritizing the differential diagnoses. Cough associated with airway inflammation (i.e., bronchitis) or large airway collapse is often loud, harsh, and paroxysmal. The cough associated with tracheal collapse is often described as a “goose-honk.” Cough resulting from tracheal disease can usually be induced by palpation of the trachea, although the concurrent involvement of deeper airways is possible. Cough associated with pneumonias and pulmonary edema is usually soft.
The association of coughing with temporal events can be helpful. Cough resulting from tracheal disease is exacerbated by pressure on the neck, such as pulling on the animal’s collar. Cough caused by heart failure tends to occur more frequently at night, whereas cough caused by airway inflammation (bronchitis) tends to occur more frequently upon rising from sleep or during and after exercise or exposure to cold air. The client’s perception of frequency may be biased by the times of day during which they have the most contact with their pets, often in the evenings and during exercise.
Surprisingly, cats with many of the disorders listed in Box 19-2 do not cough. In cats that cough, the index of suspicion for bronchitis, lung parasites, and heartworm disease is high.
EXERCISE INTOLERANCE AND RESPIRATORY DISTRESS
Diseases of the lower respiratory tract can compromise the lung’s function of oxygenating the blood through a variety of mechanisms (see the section on blood gas analysis in Chapter 20). Clinical signs of such compromise begin as mildly increased respirations and subtly decreased activity and progress through exercise intolerance (manifested as reluctance to exercise or respiratory distress with exertion) to overt respiratory distress at rest. Because of compensatory mechanisms, the ability of most pets to self-regulate their activity, and the inability of pets to communicate, many veterinary patients with compromised lung function arrive in overt respiratory distress. Dogs in overt distress will often stand with their neck extended and elbows abducted. Movements of the abdominal muscles may be exaggerated. Healthy cats have minimally visible respiratory efforts. Cats that show noticeable chest excursions or open-mouth breathing are severely compromised. Patients in overt distress require rapid physical assessment and immediate stabilization before further diagnostic testing, as discussed in Chapter 26.
Resting Respiratory Rate
Resting respiratory rate can be used as an indicator of pulmonary function in patients that are not yet in respiratory distress. The measurement is ideally made at home by the owner, which spares the patient the stress of the veterinary hospital. The normal respiratory rate of a dog or cat without stress, at rest, is less than 20 respirations per minute. A rate of up to 30 respirations per minute is generally considered normal during a routine physical examination.
Mucous Membrane Color
Cyanosis, in which normally pink mucous membranes are bluish, is a sign of severe hypoxemia and indicates that the increased respiratory effort is not sufficiently compensating for the degree of respiratory dysfunction. Pallor of mucous membranes is a more common sign of acute hypoxemia resulting from respiratory disease.
Breathing Pattern
Patients in respiratory distress resulting from diseases of the lower respiratory tract, excluding the large airways, typically have rapid and often shallow respirations; increased expiratory or inspiratory efforts, or both; and abnormal lung sounds on auscultation. Patients with intrathoracic large airway obstruction (intrathoracic trachea and/or large bronchi) generally have normal to slightly increased respiratory rate; prolonged, labored expiration; and audible or auscultable expiratory sounds (see Chapter 26).
DIAGNOSTIC APPROACH TO DOGS AND CATS WITH LOWER RESPIRATORY TRACT DISEASE
INITIAL DIAGNOSTIC EVALUATION
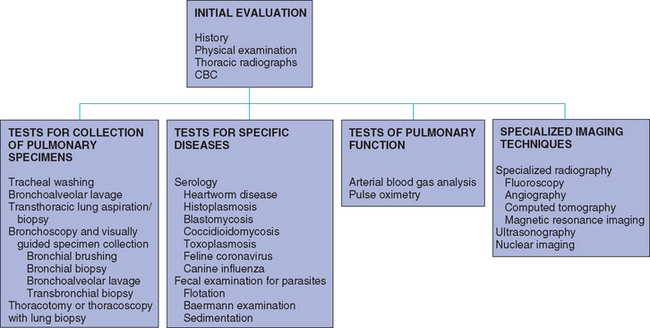
The initial diagnostic evaluation of dogs or cats with signs of lower respiratory tract disease includes a complete history, physical examination, thoracic radiographs, and complete blood count (CBC). Further diagnostic tests are selected on the basis of information obtained from these procedures; these include the evaluation of specimens collected from the lower respiratory tract, tests for specific diseases, and arterial blood gas analysis. Historical information was discussed in previous paragraphs.
Physical Examination
Measurement of respiratory rate, assessment of mucous membrane color, and observation of the breathing pattern were described in the previous sections. A complete physical examination, including a fundic examination, is warranted to identify signs of disease that may be concurrently or secondarily affecting the lungs (e.g., systemic mycoses, metastatic neoplasia, megaesophagus). The cardiovascular system should be carefully evaluated. Mitral insufficiency murmurs are frequently auscultated in older small-breed dogs brought to the clinician with the primary complaint of cough. Mitral insufficiency is often an incidental finding, but the clinician must consider both cardiac and respiratory tract diseases as differential diagnoses in these animals. Mitral insufficiency can lead to left atrial enlargement with compression of the mainstem bronchi, causing cough, or to congestive heart failure. Dogs in congestive heart failure are nearly always tachycardic, and any cough is usually soft. Other signs of heart disease include prolonged capillary refill time, weak or irregular pulses, abnormal jugular pulses, ascites or subcutaneous edema, gallop rhythms, and pulse deficits. Thoracic radiographs and occasionally echocardiography may be needed before cardiac problems can be comfortably ruled out as a cause of lower respiratory tract signs.
Thoracic auscultation.
Careful auscultation of the upper airways and lungs is a critical component of the physical examination in dogs and cats with respiratory tract signs. Auscultation should be performed in a quiet location with the animal calm. Panting and purring do not result in deep inspiration, precluding evaluation of lung sounds. The heart and upper airways should be auscultated first. The clinician can then mentally subtract the contribution of these sounds from the sounds auscultated over the lung fields.
Initially, the stethoscope is placed over the trachea near the larynx (Fig. 19-1). Discontinuous snoring or snorting sounds can be referred from the nasal cavity and pharynx as a result of obstructions stemming from structural abnormalities, such as an elongated soft palate or mass lesions, and excessive mucus or exudate. Wheezes, which are continuous high-pitched sounds, occur in animals with obstructive laryngeal conditions, such as laryngeal paralysis, neoplasia, inflammation, and foreign bodies. Discontinuous snoring sounds and wheezes are known as stertor and stridor, respectively, when they can be heard without a stethoscope. The entire cervical trachea is then auscultated for areas of high-pitched sounds caused by localized airway narrowing. Several breaths are auscultated with the stethoscope in each position, and the phase of respiration in which abnormal sounds occur is noted. Abnormal sounds resulting from extrathoracic disease are generally loudest during inspiration.
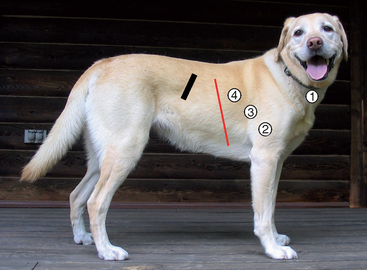
FIG 19-1 Auscultation of the respiratory tract begins with the stethoscope positioned over the trachea (stethoscope position 1). After assessing upper airway sounds, the stethoscope is positioned to evaluate the cranioventral, central, and dorsal lung fields on both sides of the chest (stethoscope positions 2, 3, and 4). Note that the lung fields extend from the thoracic inlet to approximately the seventh rib along the sternum and to approximately the ninth intercostal space along the spine (thin red line). Common mistakes are to neglect the cranioventral lung fields, reached by placing the stethoscope between the forelimb and the chest, and to position the stethoscope too far caudally, beyond the lung fields and over the liver. (Thick black line indicates position of the thirteenth rib.)
The lungs are auscultated next. Normally, the lungs extend cranially to the thoracic inlet and caudally to about the seventh rib ventrally along the sternum and to approximately the ninth intercostal space dorsally along the spine (see Fig. 19-1). The cranioventral, central, and dorsal lung fields on both the left and right sides are auscultated systematically. Any asymmetry in the sounds between the left and right sides is abnormal.
Normal lung sounds have been described historically as a mixture of “bronchial” and “vesicular” sounds, although all sounds originate from the large airways. The bronchial sounds are most prominent in the central regions of the lungs. They are tubular sounds similar in character to those heard over the trachea, but they are quieter. Vesicular sounds are most prominent in the peripheral lung fields. They are soft and have been likened to a breeze blowing through leaves. These normal sounds are best described as “normal breath sounds.”
Decreased lung sounds over one or both sides of the thorax occur in dogs and cats with pleural effusion, pneumothorax, diaphragmatic hernia, or mass lesions. Surprisingly, consolidated lung lobes and mass lesions can result in enhanced lung sounds because of the improved transmission of airway sounds from adjacent lobes. Abnormal lungs sounds are described as increased breath sounds (alternatively, harsh lung sounds), crackles, or wheezes. Increased breath sounds are a nonspecific finding but are common in patients with pulmonary edema or pneumonia. Crackles are nonmusical, discontinuous noises that sound like paper being crumpled or bubbles popping. Diseases resulting in the formation of edema or an exudate within the airways (e.g., pulmonary edema, infectious or aspiration pneumonia, bronchitis) and some interstitial pneumonias, particularly interstitial fibrosis, can result in crackles. Wheezes are musical, continuous sounds that indicate the presence of airway narrowing. Narrowing can occur as a result of bronchoconstriction, bronchial wall thickening, exudate or fluid within the bronchial lumen, intraluminal masses, or external airway compression. They are most commonly heard in cats with bronchitis. Wheezes caused by an intrathoracic airway obstruction are loudest during early expiration. Sudden snapping at the end of expiration can be heard in some dogs with intrathoracic tracheal collapse.
Radiography
Thoracic radiographs are indicated in dogs and cats with lower respiratory tract signs. Neck radiographs should also be obtained in animals with suspected tracheal disease. Radiography is perhaps the single most helpful diagnostic tool in the evaluation of dogs and cats with intrathoracic disease. It helps in localizing the problem to an organ system (i.e., cardiac, pulmonary, mediastinal, pleural), identifying the area of involvement within the lower respiratory tract (i.e., vascular, bronchial, alveolar, interstitial), and narrowing the list of potential differential diagnoses. It also helps in the formulation of a diagnostic plan (see Chapter 20). Additional diagnostic tests are necessary in most animals to establish a definitive diagnosis.
Complete Blood Count
The CBC of patients with lower respiratory tract disease may show the anemia of inflammatory disease, polycythemia secondary to chronic hypoxia, or a white blood cell response characteristic of an inflammatory process of the lungs. The hematologic changes are insensitive, however, and an absence of abnormalities cannot be used as the basis for ruling out inflammatory lung diseases. For instance, only half of dogs with bacterial pneumonia have a neutrophilic leukocytosis and left shift. Abnormalities are also not specific. For instance, eosinophilia is commonly encountered as a result of hypersensitivity or parasitic disease involving organs other than the lung.
PULMONARY SPECIMENS AND SPECIFIC DISEASE TESTING
Based on results of the history, physical examination, thoracic radiographs, and CBC, a prioritized list of differential diagnoses is developed. Additional diagnostic tests (Fig. 19-2) are nearly always required to achieve a definitive diagnosis, which is necessary for optimal therapy and outcome. Selection of appropriate tests is based on the most likely differential diagnoses, the localization of disease within the lower respiratory tract (e.g., diffuse bronchial disease, single mass lesion), the degree of respiratory compromise of the patient, and the client’s motivation for optimal care.
Invasive and noninvasive tests are available. Noninvasive tests have the obvious advantage of being nearly risk free but are usually aimed at confirming a specific diagnosis. Most patients with lower respiratory tract disease require collec tion of a pulmonary specimen for microscopic and microbiologic analysis to further narrow the list of differential diagnoses or make a definitive diagnosis. Although the procedures for specimen collection from the lung are considered invasive, they carry varying degrees of risk, depending on the procedure used and the degree of respiratory compromise of the patient. The risk is minimal in many instances.
Noninvasive tests include serology for pulmonary pathogens, fecal examinations for parasites, and specialized imaging techniques such as fluoroscopy, angiography, computed tomography (CT), ultrasonography, magnetic resonance imaging (MRI), and nuclear imaging. Techniques for collection of pulmonary specimens that can be performed without specialized equipment include tracheal wash, bronchoalveolar lavage, and transthoracic lung aspiration. Visually guided specimens can be collected during bronchoscopy. Bronchoscopy has the additional benefit of allowing visual assessment of the airways. If analysis of lung specimens and results of reasonable noninvasive tests do not provide a diagnosis in a patient with progressive disease, thoracoscopy or thoracotomy with lung biopsy is indicated.
Valuable information about patients with lower respiratory tract disease can also be obtained by assessing lung function through arterial blood gas analysis. Results are rarely helpful in making a final diagnosis, but they are useful in determining degree of compromise and in monitoring response to therapy. Pulse oximetry, a noninvasive technique to measure oxygen saturation of the blood, is particularly valuable in monitoring patients with respiratory compromise during anesthetic procedures or respiratory crises.