chapter 13 Splinting applications
After completing this chapter, the reader will be able to accomplish the following:
1. Identify a variety of splinting options.
2. Review positive and negative aspects of commonly used splints.
3. Summarize the published research for splinting and persons who have had strokes.
4. Present rationales for splinting that consider current concepts of motor control, including biomechanical principles.
5. Critically analyze and reconsider the present approach to splinting, evaluating, and developing interventions for each extremity based on individual findings.
Any discussion of splinting of the upper extremity after stroke produces debate among occupational therapists. The use of splints after stroke can be traced as far back as 1911.37 Since then the debate about whether to splint and about the rationales for splinting has continued.
The following principles guide splinting decisions for patients after stroke:
 Splints are used to maintain or increase the length of soft tissues (e.g., muscles, tendons, and ligaments) by preventing or lengthening shortened tissues and preventing overstretching of antagonist soft tissue.
Splints are used to maintain or increase the length of soft tissues (e.g., muscles, tendons, and ligaments) by preventing or lengthening shortened tissues and preventing overstretching of antagonist soft tissue.
 Splints are used to correct biomechanical malalignment, restoring muscles to normal resting length and protecting joint integrity. This biomechanical correction may result in a decrease in excessive skeletal muscle activity.
Splints are used to correct biomechanical malalignment, restoring muscles to normal resting length and protecting joint integrity. This biomechanical correction may result in a decrease in excessive skeletal muscle activity.
 Splints are used to position the hand to assist in functional activities.
Splints are used to position the hand to assist in functional activities.
 Splints may be used to promote independence in specific areas of occupation.
Splints may be used to promote independence in specific areas of occupation.
 Splints compensate for weakness by providing external support, blocking the pull of muscle groups that have lost a balanced agonist-antagonist relationship, and altering the resting alignment of the joints to enhance functional postures.
Splints compensate for weakness by providing external support, blocking the pull of muscle groups that have lost a balanced agonist-antagonist relationship, and altering the resting alignment of the joints to enhance functional postures.
The use of one splinting rationale (i.e., never splinting, always splinting, only using resting splints, etc.) for those after stroke is not effective because of the variety of patterns of impairments that occur after stroke. Each individual must be evaluated separately to determine if there are splinting needs. The sequelae of stroke are multilayered, encompassing a variety of symptoms and problem areas. The complexity of these problems has served as fuel for the splinting debate and the controversies surrounding splinting.
Historical perspective
Neuhaus and colleagues37 have published a review of the splinting literature covering a 100-year period. Their review has documented two different approaches to splinting: the biomechanical approach and the neurophysiological approach.
The biomechanical perspective considers issues such as soft-tissue lengthening, prevention of contracture and deformity, maintenance of biomechanical alignment, and effects on the nonneural components of spasticity. In contrast, the neurophysiological perspective considers reflex inhibition, effects on the neural basis of spasticity, facilitation through sensory input, and inhibition through positioning and sensory input.
Earlier publications (from the early 1900s to the 1950s) emphasized a biomechanical approach, whereas literature after World War II emphasized a shift toward the neurophysiological frame of reference. During this time, therapists (Rood, Bobath, Knott, and Voss) developed theories based on neurophysiological principles. Many of the neurophysiological theorists clearly were opposed to splinting; others did not mention splinting at all as part of their treatment regimens. Rood (as cited by Stockmeyer46) stated that spasticity may be increased “by activating sensory stimuli of touch, pressure, and stretch, which result in undesirable contraction of muscle.”
The neurophysiological perspective is currently being seriously questioned because of a lack of research support, and a shift is occurring toward a more comprehensive and current understanding of motor behavior. Nevertheless, many styles of splints and rationales are still based on neurophysiological principles.
To date, research does not support one style of splint as superior to another. Many of the statements and principles documented by the originators of the neurophysiological theories have been accepted as fact. In light of current understanding of motor control, these statements need to be analyzed and researched critically before further splinting interventions are based on these concepts. See Chapter 6 for a comprehensive review of these issues.
In general, a current review of the empirical literature related to stroke cannot support or refute the use of splints. There are few well-designed studies, and most have methodological flaws. Nonetheless, conclusions from current reviews include:
 Steultjens and colleagues43 systematically reviewed five studies (two randomized controlled trials, two case control trials, and one crossover trial) that evaluated the effect of splinting on muscle tone. They found that all studies were of low methodological quality and that none of the studies presented significant results of the measures used. They concluded that there is insufficient evidence that splinting is effective for decreasing muscle tone.
Steultjens and colleagues43 systematically reviewed five studies (two randomized controlled trials, two case control trials, and one crossover trial) that evaluated the effect of splinting on muscle tone. They found that all studies were of low methodological quality and that none of the studies presented significant results of the measures used. They concluded that there is insufficient evidence that splinting is effective for decreasing muscle tone.
 In their review of studies aimed at testing the effects of splinting on reducing tone, Ma and Trombly27 concluded that “In summary, based on study of a total of only 35 participants with stroke, we can make no conclusive statement about splinting and its effect on spasticity. However, it appears that splinting for less time is the most beneficial. Research using much larger samples is needed.” They also stated that “best evidence” indicates that, although commonly used, treatments using splints to decrease spasticity may be ineffective, and recommend that the treatment not be used.
In their review of studies aimed at testing the effects of splinting on reducing tone, Ma and Trombly27 concluded that “In summary, based on study of a total of only 35 participants with stroke, we can make no conclusive statement about splinting and its effect on spasticity. However, it appears that splinting for less time is the most beneficial. Research using much larger samples is needed.” They also stated that “best evidence” indicates that, although commonly used, treatments using splints to decrease spasticity may be ineffective, and recommend that the treatment not be used.
 Based on a review of three studies, Tyson and Kent49 concluded that “An upper limb orthosis does not affect on upper limb function, range of movement at the wrist, fingers or thumb, nor pain.” It should be noted that these three studies involved a mixed group of participants, and none of the studies recruited participants who had functioning upper limbs.
Based on a review of three studies, Tyson and Kent49 concluded that “An upper limb orthosis does not affect on upper limb function, range of movement at the wrist, fingers or thumb, nor pain.” It should be noted that these three studies involved a mixed group of participants, and none of the studies recruited participants who had functioning upper limbs.
 Lannin and Herbert23 assessed the effectiveness of hand splinting on the hemiplegic upper extremity following stroke via a systematic review. They appraised 19 studies for content. Sixty-three percent were reports of case series, and 21% were randomized controlled trials. They concluded that there is insufficient evidence to either support or refute the effectiveness of hand splinting for adults following stroke. They also stated that the “limited research and a lack of a no-splint control group in all trials to date limit the usefulness of these results.”
Lannin and Herbert23 assessed the effectiveness of hand splinting on the hemiplegic upper extremity following stroke via a systematic review. They appraised 19 studies for content. Sixty-three percent were reports of case series, and 21% were randomized controlled trials. They concluded that there is insufficient evidence to either support or refute the effectiveness of hand splinting for adults following stroke. They also stated that the “limited research and a lack of a no-splint control group in all trials to date limit the usefulness of these results.”
Clearly well-designed studies are critical to help therapists make informed decisions about this intervention. At this point, each patient/client must be evaluated individually based on their clinical presentation. Clinical reasoning suggestions follow.
Dorsal versus volar splinting
Splint fabrication and points of contact are areas of continuing debate. The following studies have investigated this controversy.
Zislis53 compared the effects of two different wrist-hand splints on a patient with spastic hemiplegia. The author used simultaneous electromyographic (EMG) recordings of the flexors and extensors in the forearm to provide an objective measure of muscle activity. EMG readings were taken with no splint, with a dorsal-based splint (which kept the wrist neutral, fingers adducted and extended, and thumb free) used in hopes of facilitating the extensors, and with a volar-based splint (which kept the wrist neutral, fingers extended and abducted, and thumb free).
Zislis’ results53 indicated that extensor muscle activity was not altered in any of the three situations, although flexor activity was varied. With no splint, flexor activity was exaggerated compared with extensor activity. The dorsal splint greatly increased the flexor activity, even more so than when no splint was worn. Finally, the volar-based splint diminished flexor activity and achieved a state of “balanced physiological activity between flexor and extensor muscle groups.”
Zislis53 drew the following conclusions from the patient he studied:
 Dorsal facilitation of the extensor was not evident, although dorsal facilitation of the flexors did occur.
Dorsal facilitation of the extensor was not evident, although dorsal facilitation of the flexors did occur.
 Flexor inhibition from volar cutaneous receptors may occur.
Flexor inhibition from volar cutaneous receptors may occur.
 Abduction and extension of the fingers may produce flexor inhibition.
Abduction and extension of the fingers may produce flexor inhibition.
Therefore, Zislis53 recommended the use of volar-based splints with extension and abduction of the fingers.
Charait7 observed 20 patients in her study of dorsal versus volar “functional position splints.” In the splinted position, the wrist varied from less than neutral to 30 degrees, the thumb was abducted and opposed, and the fingers were positioned at 45 degrees of finger flexion at the metacarpophalangeal (MCP) and proximal interphalangeal (PIP) joints.
Charait7 observed the amount of spasticity and voluntary movement in both groups. In the group wearing volar splints, four patients showed no change in spasticity or voluntary motion, and six experienced increased spasticity. In the group wearing dorsal splints, one patient showed no change, one experienced a considerable increase in spasticity, and eight had decreased spasticity (four of these also exhibited increased active finger and wrist extension). The author drew the following conclusions from her observations:
 Volar pressure facilitates flexor muscles.
Volar pressure facilitates flexor muscles.
 Dorsal pressure with decreased volar contact facilitates the extensors.
Dorsal pressure with decreased volar contact facilitates the extensors.
Charait7 recommended splinting using dorsal-based appliances.
McPherson and colleagues32 compared dorsal and volar resting splints for the reduction of hypertonus. They assigned 10 subjects with hypertonic wrist flexors to the dorsal or volar group. For the purposes of the study, the authors defined hypertonus as “the plastic, viscous, and elastic properties of the muscle resistant to stretch and with a tendency to return a limb to a particular abnormal resting posture.” They used a spring-weighted scale to take measurements to assess the effectiveness of the splints in reducing hypertonicity. The results indicated no significant difference between the volar and dorsal splints in the reduction of hypertonus. As an aside, the authors found a correlation between age and reduction in hypertonus. The older subjects in the study demonstrated gradual but not statistically significant decline in hypertonus, whereas the younger adults demonstrated significant decline in hypertonus over 6 weeks.
Other studies have not compared dorsal and volar splinting specifically but instead have evaluated the effects of one or the other. Kaplan21 evaluated 10 patients who wore dorsal wrist splints. His study set out to “determine whether prolonged therapy with a dorsal splint will inhibit or diminish hyperreflexia or stretch reflex and at the same time increase muscular power by sensorimotor stimulation.” The splint used in this study positioned the wrist and fingers in extension and supported the thumb in abduction. Most of the subjects wore the splints at least eight hours per day, and Kaplan noted that many patients required several serial splints to increase the stretch on the flexors gradually. Patients were evaluated with EMG, strength testing, and hand function evaluation before and after splint application. The subjects in this study demonstrated “improvement in strength and function of muscle, with a decrease in the stretch reflex and spasticity . . . when a dorsal splint was properly applied in treatment of hemiplegia involving an upper extremity.”
Brennan5 studied the effects of volar-based splints on his subjects. At the end of his study the patients who wore the volar-based wrist and hand splints demonstrated increased range of passive movement in which no resistance to stretch could be felt.
In their study of positioning devices on normal and spastic hands, Mathiowetz, Bolding, and Trombly30 demonstrated that a volar-based resting splint increased EMG activity as the subjects performed a grasping activity on the contralateral side. They noted that the volar splint “is the least desirable positioning device while the hemiplegic subject is doing any activity that requires a comparable effort to squeezing 50% maximal voluntary contraction of grip.”
The variability in the aforementioned studies makes decisions regarding dorsal-versus volar-based treatment difficult to reach based on available research. Therapists must still evaluate each patient individually to determine the effect of variables on splinting outcomes. Moreover, the studies discussed in this chapter used a variety of outcome measures, varied in their methodologies, and implemented variable definitions and styles of splints.
Review of splints commonly used for patients after stroke
This section reviews positive and negative aspects of splints frequently used by occupational therapists; available research is discussed. Several of the following splints were developed based on a now outdated understanding of motor function. Some of the splints still may be useful and effective, although the rationale for their use may no longer be based on the original purpose of the splint.
Finger spreader (finger abduction splint)
The finger spreader (finger abduction splint) is fabricated of foam rubber and positions the fingers and thumb in abduction. According to Bobath,3 the purpose of the splint is to “obtain extension of wrist and fingers. . . . Abduction not only facilitates extension of the fingers, but also reduces flexor spasticity throughout the whole arm. . . . It has a better and more dynamic effect than the use of a (standard) splint and reduces the possibility of edema.” One should note that Bobath’s rationale is not consistent with the current understanding of motor control and related neurological principles.
A sturdier version of this splint (fabricated of low-temperature plastic) was proposed by Doubilet and Polkow.9 They recommended wearing the splint only during the day. Their paper includes anecdotal evidence of the effectiveness of the splint.
The finger abduction splint was worn by fifteen patients who were two to six months post stroke, these patients exhibited moderate to severe spasticity of the fingers and wrist, decreased range of motion, and edema in the wrist and hand. After one week of using the splint plus standard treatment in the therapy sessions a moderate reduction of spasticity was seen in these patients.
Doubilet and Polkow9 concluded that the splint results are promising and warrant continued trial and experimentation.
Mathiowetz, Bolding, and Trombly30 objectively evaluated the finger abduction splint in a study investigating the effects of a variety of splints on the distal muscle activity of normal and hemiplegic subjects. Subjects wore the splints while performing resistive activities with the opposite hand. The results indicated “significantly greater EMG activity for the finger spreader compared to no device in the flexor carpi radialis of normal subjects during grasping” with the contralateral hand. In hemiplegic subjects, the finger spreader did not evoke less EMG activity than no device. According to the authors, the belief that this splint decreases spasticity shortly after application needs to be questioned seriously.
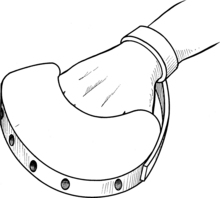
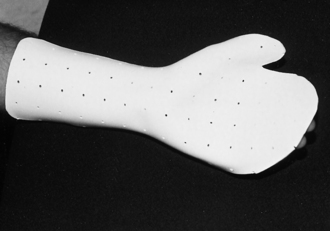
The finger spreader may be useful in maintaining the length of the flexors; however, wrist position is not considered with this splint, and the therapist must be aware of the wrist position. To control this problem, the therapist may combine the finger spreader with a standard wrist extension splint. Because the splint is subtle in terms of corrective forces, it may be indicated for patients with low tolerance for other, more cumbersome devices and for patients with low pain thresholds. Donning and doffing procedures are straightforward for the confused patient (Fig. 13-1).
Firm cone
The firm cone can be fabricated of low-temperature plastic or purchased commercially; it is based on the traditional theories of Rood. Rood’s theory (as interpreted by Stockmeyer46) states that firm and prolonged pressure over the flexor surface of the palm and fingers results in an inhibition of the long flexors. A more current understanding of the mechanism of this splint from a biomechanical and functional perspective is that the cone is positioned to place stretch on the shortened long flexors and is graded progressively to increase stress to the soft tissues to promote a more normal resting length. The cone initially is positioned with the narrow end of the cone toward the radial side of the hand in the web space if the hand is excessively tight. As the hand begins to relax from the directed stress, the ideal biomechanical position is for the cone to be positioned opposite to the initial position; that is, the wide end of the cone is placed in the radial side of the hand in the web space, and the narrow end is placed in the ulnar side of the hand (Fig. 13-2). The therapist can use strapping material to hold the cone in place. This device was included in the study by Mathiowetz, Bolding, and Trombly;30 the researchers found that the cone did not evoke significantly less EMG activity during contralateral resisted function.
Neurophysiological principles aside, the cone may be an effective positioning device for patients who have developed contracture in the long flexors. Combined applications of the cone with a standard wrist-extension splint, controlling the stretch on the wrist and digit flexors separately, are feasible. The size of the cone and the angle of wrist extension can be graded as the patient’s status improves.
Another practical use of the cone is in the prevention of maceration of tissue in patients with moderate to severe flexion of the digits. The maintenance of flexor length is required for hygiene and cosmesis. Similar to the use of the finger abduction splint, the use of the cone in isolation does not provide wrist support, thus predisposing the wrist to a flexed posture. Donning and doffing procedures are straightforward.
Orthokinetic orthotics
According to Neeman and Neeman,34 the term orthokinetic orthosis “describes a cuff-shaped dynamic orthopaedic appliance which does not include rigid polymer or metal components. It does not apply any extraneous modulating force or constraint, in contrast to the typical splint.” The orthokinetic cuffs designed by Blashy and Fuchs-Neeman1 have been used for almost 40 years for patients with muscle weakness, muscle paresis, and resulting agonist-antagonist imbalance. The action of these orthoses is “exerted through internal restoration of neuromuscular balance between agonist and antagonist musculatures, by input of mild neural stimuli to mechanoreceptors in specifically targeted skin areas.”1 The designers state that the neurophysiological mechanism involves activation of paretic agonist muscles and reciprocal inhibition of antagonist musculature.
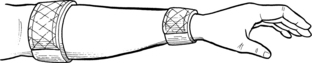
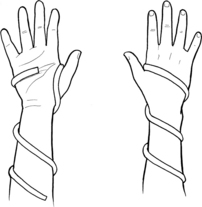
The orthokinetic cuffs are fabricated of ribbed elastic bandage material applied circumferentially around various aspects of the patient’s upper extremity and are held on the arm by fasteners. Half of the cuff is designed to be elastic (the active field), and the other half of the cuff is sewn to reduce the stretch (the inactive field). The active field is worn over the muscle belly to be activated, and the inactive field is placed over the antagonist.
Neeman and Neeman have published several studies33-36 on the effectiveness of these cuffs in the rehabilitation of the upper extremity after stroke. They concluded that use of the cuffs results in pronounced restoration of agonist-antagonist muscle balance, increased active range of motion (ROM) throughout the extremity, and increased ability to participate in functional tasks.
The orthokinetic cuffs have been subjected to the greatest number of efficacy studies, all showing positive results. Fabrication guidelines are stated clearly in the cited studies, and the cuffs are applied easily and are comfortable.
The neurophysiological rationale for the orthokinetic cuff has not been established fully. The active field may produce cutaneous stimulation and activate the exteroceptors of the skin and Ia afferent neurons of the muscle spindle. The inactive field seems to provide sustained deep pressure, which may produce an inhibitory response (Fig. 13-3).
Orthokinetic wrist splint
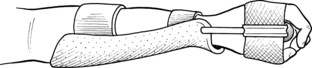
The dynamic design of the orthokinetic wrist splint is based on the concepts of Rood (as cited in Stockmeyer46). Components of the splint include a firm cone in the palm of the hand, a volar-based forearm support, elastic straps to secure the forearm support by acting as orthokinetic cuffs, and a wrist hinge.22 This splint has been recommended for patients with flexor hypertonicity who have at least minimal voluntary extensor activity. However, no data support the effectiveness of this splint (Fig. 13-4).
Spasticity reduction splint
The spasticity reduction splint was developed by Snook44 and is based on the Bobath3 principle of reflex-inhibiting patterns that has not been supported by current research. The splint is fabricated of low-temperature plastic. The forearm support is dorsal based and continues into a volar-based finger support. The wrist is positioned in 30 degrees of wrist extension; the MCP joints are at 45 degrees of flexion. The interphalangeal (IP) joints are extended fully, the fingers are abducted with separators, and the thumb is positioned in abduction and extension. Snook44 notes that if a flexion contracture is present, the wrist may be positioned at neutral or slightly less than neutral without producing a significant effect on the effectiveness of the splint.
Snook44 recommended an intermittent wearing schedule, observing that “a decrease in tone is usually seen almost immediately upon splint application; however, after an extended period of wearing time, tone tends to gradually increase.”
Snook’s original article described fabrication and provided clinical observations and case studies. Research was not included in this article. Snook44 concluded that based on preliminary findings, the spasticity reduction splint has an effect “on the reduction and normalization of tone” and should be considered as a therapeutic tool when the therapist is dealing with a spastic hand.
McPherson31 evaluated the effect of this splint on five severely and profoundly handicapped subjects (no patients who had strokes were included in this study). His results demonstrated a significant reduction in hypertonicity after four weeks of splint use. He further stated that the effects of the splint were not permanent; after the splints were removed, hypertonicity increased. The author measured “the force of spastic wrist flexors in pounds of pull on a spring weighted scale.”
The fabrication guidelines for this splint are outlined in Snook’s article.44 Compliance in wearing schedules may be problematic because the splint is bulky and the wrist and hand are held in an extreme range. Many patients require assistance donning the splint, depending on the level of flexion posturing in their hands.
Although the principles that this splint was based on originally are out of date, this splint maintains a stretch to the musculature that traditionally becomes shortened in patients after stroke. It may be useful as an adjunct to treatment focusing on the maintenance of soft-tissue length. Further research is required on patients after cerebrovascular accident (CVA) to document this splint’s effectiveness (Fig. 13-5).
Pressure splints (air splints)
The use of inflatable pressure splints as adjuncts to therapy was first advocated by Johnstone.19 These splints are commercially available and exert continuous or intermittent pressure to the area to which they are applied. The pressure of the splints should not exceed 40 mm Hg.42 According to Poole and colleagues,42 “inflatable splints have been used with patients who have had a stroke to reduce tone, facilitate muscle activity around a joint, facilitate sensory input, control edema, and reduce pain.” Their article includes a review of the neurophysiological rationales for the use of inflatable splints.
Three studies have been published of investigations of the effectiveness of inflatable splints on patients who have had strokes. The earliest was a case study by Bloch and Evans;2 its results indicated a reduction in spasticity and an increase in hand ROM.
Nicholson38 (as cited by Poole and Whitney41) treated patients for one week with inflatable splints along with weight-bearing patterns. At the end of the treatment protocol, no improvements had occurred in sensation, strength, and ROM.
Likewise, Poole and colleagues42 treated 18 persons and assigned them to splint or nonsplint treatment protocols. The splinted group wore the splint for 30 minutes five days a week for three weeks. The splinted patients did not perform activities with the splinted extremity. The authors’ results indicated no statistically significant differences in mean change in upper extremity sensation, pain, and motor function between the splinted and nonsplinted groups.
Although inflatable pressure splints do not seem to elicit the effects originally proposed, some therapists may consider using this style of splint to enhance functional performance during weight-bearing activities (Fig. 13-6). In essence, this splint can be used to control the degrees of freedom in the upper extremity, thereby promoting functional use during daily activities.
Wrist extension splints
Wrist splints are commonly used in stroke populations to prevent wrist contracture and to stabilize the wrist to provide the fingers a steady base from which they can function. Lannin and colleagues25 aimed to determine whether wearing a hand splint, which positions the wrist in either a neutral or an extended position, reduces wrist contracture in adults with hemiplegia after stroke (N=63). The subjects were randomized to either a control group (routine therapy) or one of two intervention groups (routine therapy and splint in either a neutral or an extended wrist position). Participants in the neutral splint group wore a hand splint, which positioned the wrist in zero degrees to 10 degrees extension, and those in the extension splint group wore a hand splint, which positioned the wrist in a comfortable end-of-range position (greater than 45 degrees wrist extension) with the MCP and IP joints extended. The splints were worn overnight for, on average, between nine and 12 hours, for four weeks. The outcome was extensibility of the wrist and long finger flexor muscles (angle of wrist extension at a standardized torque). The authors concluded that splinting the wrist in either the neutral or extended wrist position for four weeks did not reduce wrist contracture after stroke.
Resting splints
The resting splint can be dorsal or volar based. The suggested position is 20 to 30 degrees of wrist extension, MCP joints at 40 to 45 degrees of flexion, IP joints in 10 to 20 degrees of flexion, and thumb in opposition to the index finger.29
One of the most important aspects of clinical reasoning is that each patient must be evaluated and treated individually, and these goniometrics should be used as a guideline only. The goal is to adjust the splint to promote a low-load prolonged stress (LLPS) to achieve a more advantageous biomechanical position as necessary.
Lannin and colleagues24 evaluated the effects of four weeks of hand splinting on the length of finger and wrist flexor muscles, hand function, and pain in people with acquired brain damage via randomized, assessor-blinded trial. They examined 28 adults, all within six months of injury. Subjects in both experimental (n=17) and control (n=11) groups participated in routine therapy-motor training for upper limb use and upper limb stretches five days a week. The experimental group also wore an immobilizing hand splint in the functional position (10 to 30 degrees wrist extension) for a maximum of 12 hours each night for the duration of the four-week intervention period. Outcomes included length of the wrist and extrinsic finger flexor muscles measured via torque-controlled range of wrist extension with the fingers extended, the Motor Assessment Scale, and pain via a visual analog scale. The authors found that the effects of splinting were statistically nonsignificant and clinically unimportant, and they concluded that “an overnight splint-wearing regimen with the affected hand in the functional position does not produce clinically beneficial effects in adults with acquired brain impairment.”
The resting splint is used commonly in clinics. Although the splint may be effective in the long-term for patients after stroke, therapists must analyze critically the effects of this splint on the patient with acute and subacute impairments. This splint blocks any automatic and voluntary attempts at movement, thereby promoting learned nonuse. It completely covers the surface of the hand (thus preventing sensory input) and gives full passive support to the wrist and digits, which may be contrary to treatment programs attempting to train patients to be responsible for the positioning and ranging of their hands. Therapists need to consider alternatives to this splint.
Mathiowetz, Bolding, and Trombly30 demonstrated that the use of a volar-based resting splint increased EMG activity in hemiplegic subjects who were performing grasping tasks with the opposite extremity. They concluded that this type of volar splint “is the least desirable positioning device while the hemiplegic subject is doing any activity that requires a comparable effort to squeezing fifty percent maximal voluntary contraction of grip.”
Resting splints can be custom fabricated; they also are available commercially. The therapist may consider nighttime use of the resting splint for prevention of soft-tissue contracture, but this style of splint should not be worn during daytime because it completely blocks spontaneous function, sensory input, and self-management of the hand and may promote learned nonuse (Fig. 13-7).
Tone and positioning splint
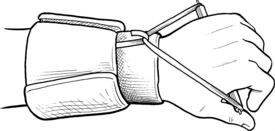
The tone and positioning splint is semidynamic and is commercially available from Smith & Nephew Rolyan. The splint supports the thumb in abduction and extension with a neoprene glove. The tone and positioning splint includes an elastic strap that is wrapped spirally up the forearm, providing a dynamic assist into pronation and supination. Data supporting the effectiveness of this splint are not available.
Casey and Kratz6 have published a paper on the thumb abduction supinator splint. This splint is similar in design to the commercially available tone and positioning splint. Their paper included fabrication guidelines and recommended a wearing schedule of three to four hours on, and then 30 minutes to one hour off to allow the skin to be exposed to the air. They recommended using the splints on patients with mild to moderate spasticity without severe contractures: those who posture in a pattern of forearm pronation, with a fisted hand, and with the thumb in the palm.
The tone and positioning splint and thumb abduction supinator splint may present difficulties to patients learning to don and doff splints independently. These splints are designed to be used to enhance positioning and to be worn during functional activities. They may be particularly effective if worn during activities that result in stereotypical posturing of the limb (e.g., gait and transfers). They also may be effective during upper extremity activities because the digits are free to move (Fig. 13-8).
Thumb loop and thumb abduction splint
Variations of the thumb abduction splint have been proposed by several authors.8,16,45 The papers cited in the references include fabrication guidelines; the splint is commercially available. The thumb abduction splint is considered a semidynamic splint, and the focus of positioning is on thumb and wrist alignment. The strapping material used in the fabrication of this splint positions the thumb in abduction and aligns the wrist in a position of slight radial wrist extension. The hand is placed in a position that enhances prehension, manipulation, and release of objects, and provides the freedom of movement needed for bilateral coordination.16
Stern45 stated that another indication for use is during any activity involving effort, particularly when performing fine activities with the unaffected limb results in increased thumb adduction on the affected side. Therefore, this splint has been suggested for positioning and enhancement of functional performance.
Stern45 cautioned that, “For this splint to be of any value, the patients must be able to use the affected hand for grasp and release, their main problem being adduction of the thumb, which prevents sufficient opening of the hand to allow for palmar grasp.” Patients with fixed adductor contracture are less likely to benefit.
Research evaluating the effectiveness of this splint in the adult population is lacking. Currie and Mendiola8 evaluated the effectiveness of a variation of this type of splint on five children with “mild to moderate spastic hemiplegic cerebral palsy.” These children exhibited a cortical thumb (adducted thumb) at rest, and their hand functions were limited to a “raking” ulnar type of prehension pattern.
With the use of this splint, all five children’s resting thumb patterns were enhanced, and their prehension patterns improved to a radial grasp, usually in a three jaw chuck or large cylindrical prehension pattern, depending on the size of the object being manipulated (Fig. 13-9).
Hand-based thumb abduction splint
If the patient has controlled wrist movement in flexion and extension (not necessarily full wrist ROM, but some isolated control) but continues to have flexor activity influencing the digits, a hand-based thumb abduction C-spacer splint may be useful during functional activities. The splint is custom fabricated from thermoplastic material. The thumb abduction splint positions the thumb in an enhanced prehension pattern for manipulation of objects during grasp and release activities (Fig. 13-10).
Mackinnon splint
Although the MacKinnon splint was developed for the pediatric population, it may be indicated at times for the adult population. The splint includes a dorsal-based forearm support that wraps three fourths of the distal half of the forearm, a dowel placed in the palm of the hand to provide pressure on the MCP heads, and rubber tubing attaching the dowel to the dorsal forearm support; the fingers are left free to assume functional patterns.
The goal of this splint is to release the overactive finger flexors and adductor pollicis to gain balanced muscle action of the wrist. The paper by MacKinnon, Sanderson, and Buchanan28 included fabrication guidelines and observations of approximately 30 children who used the splint and gained improved hand awareness, increased use, and decreased spasticity when the splint was removed. Research regarding the effectiveness of this splint is not available, and it has not been documented for use with the adult patient recovering from CVA (Fig. 13-11).
Submaximal range splint
The submaximal range splint was described by Peterson;40 its design is based on the clinical observation that muscles splinted on full stretch or maximal ROM increased in tightness.
The splint is fabricated in the fashion of a resting hand splint. The splint should position the distal extremity with the thumb in partial opposition to the index finger, the MCP and PIP joints in 45 degrees of flexion, with distal interphalangeal (DIP) joint extension, and the wrist in 10 to 20 degrees of extension; the splint should provide pressure to the palmar arch. If the patient cannot achieve this ideal range, each joint should be positioned in five to 10 degrees less than the available range.10 Fabrication guidelines are the same as those for a resting hand splint.
No research is available that evaluates the effectiveness of this splint, but the precautionary statements about the resting hand splint are similar to those for this splint design (see Fig. 13-7).
Serpentine splint
The serpentine splint must be custom fabricated from thermoplastic materials. The splint was originally designed for use with pediatric patients with cerebral palsy who had difficulty grasping objects. The splint is adapted easily to the adult with neurological impairments. The serpentine splint provides sufficient thumb abduction support, positions the hand and wrist in a more optimal position for function, and allows “active wrist function in the child with moderately increased tone.”47 The designers of the splint feel that the serpentine splint inhibits the thumb-in-palm reflex by using the thumb abduction position.
The authors have used an adaptation of the serpentine splint with several patients after CVA, with positive outcomes. The serpentine splint can be used for patients with mild to moderate increased skeletal muscle activity (it is not recommended for the flaccid hand). This splint is never recommended for hands that exhibit severe increases in skeletal muscle activity for the reasons outlined previously in this chapter.
The wrist is positioned in 20 to 30 degrees of extension, the thumb is positioned in 30 to 40 degrees of abduction, and the material continues two thirds of the length proximally up the forearm. The splint positions the hand in a more functional position for grasping exercises and activities.47 The splint is worn during the day for activities and wrist support and is removed at night. The serpentine splint requires maximal assistance for application and moderate assistance for removal and is a practical alternative to more conventional static splints. Because the splint is an open splint, it is less confining; it also is lightweight and allows for air circulation, which results in decreased perspiration, decreased skin maceration, and reduced potential for skin breakdown. When fabricating this splint, the therapist places the roll in the palm, then wraps it around the ulnar aspect of the hand, forms it over the dorsum of the hand through the web space, brings the roll over the thenar eminence and under the base of the thumb, and continues wrapping the material two thirds of the way up the forearm. The seam made by rolling the splint material should face away from the skin to prevent skin irritation and breakdown (Fig. 13-12).
Drop-out splint
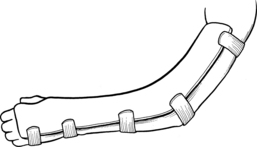
The drop-out splint is a custom-fabricated splint designed to decrease elbow contractures that may be common in the patient after stroke. The splint is designed from thermoplastic material positioned volarly on the humerus, distal to the axilla; it extends into the palm of the hand proximal to the distal palmar crease. The splint is fabricated with the shoulder and humerus externally rotated and the forearm in as much supination as possible. It is customized with a gentle stretch to the contracted elbow joint (not to the point of discomfort) using the LLPS principles in the section Treatment of Joint Contractures with Low-Load Prolonged Stress. The splint is used during rest periods to maximize the low-load prolonged stretch to the elbow. The elbow contracture is measured with a goniometer before application of the splint and checked weekly to allow appropriate adjustments of the splint for increased extension as needed. As with all splints used in the patient who has had a stroke, but especially for splints using the low-load prolonged stretching principles, the therapist must monitor the upper extremity frequently for skin maceration and breakdown (Fig. 13-13).
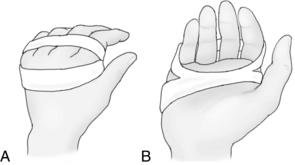
Belly gutter splint for proximal interphalangeal joint flexion contractures
The belly gutter splint is a static PIP extension splint custom fabricated from thermoplastic material. Many PIP extension splints are commercially available. Joint Jack, LMB Wire-foam, and safety-pin splints, which apply two points of volar pressure to make a perpendicular pull on the involved segments, are a few. If the flexion contracture is greater than 35 degrees, these splints are not effective. Dynamic extension splints and the belly gutter splint provide traction tension at a 90-degree angle to the phalanx. The belly gutter splint provides the 90-degree angle pull by incorporating a convex belly in the middle of the gutter.52 When fabricating and applying this splint, the therapist must place the Velcro strap directly over the PIP joint; the belly of the splint must be directly under the PIP joint axis for the splint to be effective. The authors have found this splint to be effective for flexion contractures of the PIP joint from approximately 15 degrees of contracture to 35 degrees of contracture. A PIP joint contracture of more than 35 degrees requires dynamic splinting.11 The belly gutter splint is used at the beginning of treatment for one hour on and one hour off. Gradually, as the contracture decreases, the time may be extended to as much as four hours, but as always, close monitoring of the splint is mandatory (Fig. 13-14).
Inflatable hand splint
The inflatable hand splint, which is commercially available, is marketed for contracture management of the population in the chronic stages of stroke rehabilitation. The splint consists of an adjustable volar-based wrist support that is easily adjusted to achieve the desired range of extension. The palmar aspect of the splint is an air bladder that can be inflated or deflated easily, depending on the desired stretch and level of contracture. The splint is easily donned and is comfortable (Fig. 13-15).

Figure 13-15 DeRoyal’s Pucci Air-T Inflatable Hand Orthosis.
(Manufactured and distributed by DeRoyal.)
The therapist must consider many issues when prescribing or designing a splint for use on persons after stroke. The following section exposes therapists to the complexity of issues to be considered during the splinting evaluation.
Considerations in prescribing and designing a splint for the distal extremity after stroke
Spasticity
Many commonly used splints are applied in the hope that they will inhibit spasticity with a result of improved function. As outlined in Chapter 10, the cause-and-effect relationship between spasticity and function has not been supported in available research.
The link between spasticity and contracture has been well-documented; see Chapter 10. Therefore, splinting of patients who are experiencing distal spasticity may be indicated to prevent painful contractures and loss of tissue length. This differentiation is important if therapists are to analyze objectively the effectiveness of the splints provided.
Hummelsheim and colleagues17 have demonstrated that prolonged stretch resulted in “a significant reduction in the spastic hypertonus in elbow, hand and finger flexors” of the 15 patients they studied. Spasticity was measured by the Ashworth Scale. The EMG recordings included in their study objectively demonstrated that late EMG potentials are reduced or disappear after sustained muscle stretch. The authors hypothesized that “the beneficial effect resulting from sustained muscle stretch is due to stretch receptor fatigue or adaptation to the new extended position.”
Although this study was based on manual stretching techniques, the same principles may be applied to splinting. Therefore, splinting may be used as an adjunct to interventions aimed at relaxing the distal extremity.
Feldman10 recommended early splinting interventions for patients with spasticity; treatment should begin before the spasticity becomes severe. She stated that “the longer tonal influences are left to bear on the joints, the greater the risk for contractures and other complications.” Feldman also warned that patients with severe spasticity should not be considered for splinting programs. These patients are at risk for skin breakdown, edema, and circulatory impairment. Instead, Feldman recommended interventions with spasticity medication and nerve blocks for these patients (see Chapter 10).
Soft-tissue shortening
Many of the wrists and hands that therapists evaluate are immobilized. This immobilization may be because of weakness, static splinting for prolonged periods, excessive skeletal muscle activity, or contracture. The deleterious effects of immobilization begin to occur soon after immobilization begins.
Consequences of prolonged positioning following immobilization include anatomical, biochemical, and physiological changes. Specific changes include the number of sarcomeres, protein content, loss of muscle weight, the amount of passive and active soft-tissue tension, decreased aerobic function, and type I and II fiber atrophy.14
From their review of the literature, Gossman, Sahrman, and Rose14 concluded that “evidence from experimental studies and clinical observations clearly indicates that muscle is an extremely mutable (prone to change) tissue. Change is more pronounced when a muscle is shortened than when it is lengthened. The changes can be deleterious, but they are reversible, a condition that can be used in correcting movement dysfunction.”
Halar and Bell15 stated that if mild contractures have formed, prolonged stretches for 30 minutes are effective. More severe contractures may require longer sustained stretch through splinting. They recommended application of heat before splinting to decrease the viscous properties of connective tissue and maximize the effects of stretching.
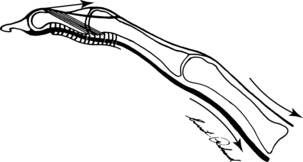
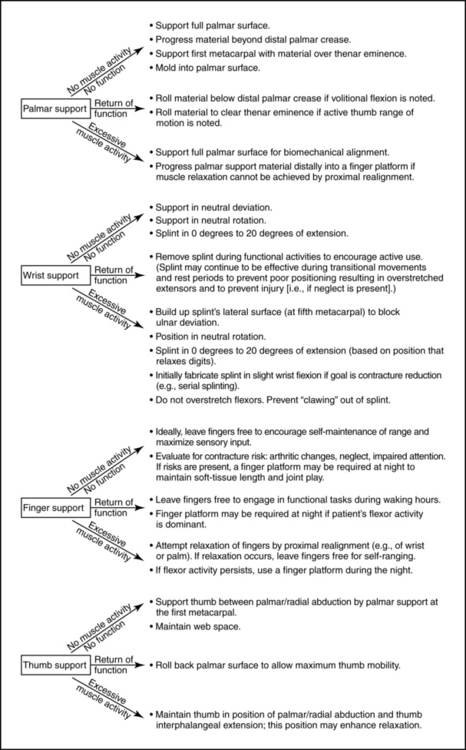
During the splinting evaluation, the therapist must assess the differences between extrinsic and intrinsic tightness and joint contractures. Therapists must understand the biomechanical mechanism of the extrinsic flexors and extensors. To review, when the wrist and digits are in composite flexion (i.e., all joints are flexed), the extensors are stretched fully and the flexors are slack. In contrast, when the wrist and digits are in composite extension (i.e., all joints are extended), the flexors are stretched fully and the extensors are slack (Fig. 13-16).

Figure 13-16 Normal excursion of the flexor and extensor muscles acting on the wrist and hand. A, Wrist and digits flexed: extensors are fully stretched (elongated) and the flexors are slack (shortened). B, Wrist and digits extended: flexors are fully stretched (elongated) and extensors are slack (shortened).
Fess and Philips11 suggested altering wrist posture to detect extrinsic soft-tissue involvement. If extrinsic tightness is evident, changing the wrist posture from slight extension to flexion results in an increase in the ROM of the digits (the tenodesis effect). In contrast, if ROM limitations are caused by a pathological condition of the joint, an altered wrist position does not affect the ROM. Evaluation procedures for assessing extrinsic tightness are as follows: (1) extend the wrist with the digits flexed, and (2) maintain the wrist in extension and attempt to extend the digits. If composite extension can be achieved, then the extrinsic flexors have full excursion. If the digits cannot be extended while the wrist is in extension, the evaluation must continue to determine whether the limitation is related to a pathological joint condition or extrinsic flexor tightness. The evaluation continues as follows: (3) flex the wrist and determine if the excursion of the digits toward extension (tenodesis) is increased. If so, the limitation is due to extrinsic flexor tightness. If no change in available digit extension occurs, the pathological condition of the joint is the limiting factor48 (Fig. 13-17).
Figure 13-17 Testing for extrinsic shortening. A, The therapist extends the wrist with the digits flexed. This position partially elongates the long flexors. B, The therapist maintains the wrist in extension and extends the digits. If composite extension can be achieved, the extrinsic flexors have full excursion and the evaluation is complete. C, If the therapist cannot extend the wrist and digits fully simultaneously, the evaluation must continue to determine whether the limitation is related to a pathological joint condition or extrinsic flexor tightness. D, The therapist flexes the wrist to determine if excursion of the digits toward extension (tenodesis) is increased. If so, the limitation is due to extrinsic flexor tightness. E, If no change in available digit extension occurs while the wrist is flexed, the pathological joint condition (i.e., bony contracture) is the limiting factor.
In terms of the biomechanics of the intrinsic mechanism, when the MCP joints are flexed and the IP joints are extended (intrinsic plus), the intrinsic muscles are shortened. In contrast, when the MCP joints are extended and IP joints are flexed, the intrinsic muscles are fully stretched (Fig.13-18).
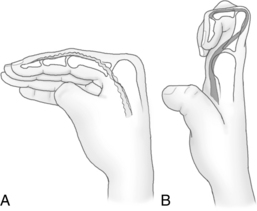
Figure 13-18 Normal excursion of the intrinsic muscles (lumbricales). A, When the metacarpophalangeal joints are flexed and the interphalangeal joints are extended (“intrinsic plus”), the intrinsic muscles are in a shortened position. B, When the metacarpophalangeal joints are extended and the interphalangeal joints are flexed (“intrinsic minus”), the intrinsic muscles are elongated.
Fess and Philips11 suggested evaluating intrinsic tightness by holding the MCP joint in extension and attempting to flex the PIP joint; full passive flexion of the PIP joint is absent if the intrinsic muscles have become tight. With intrinsic tightness, however, one may possibly attain full passive PIP joint flexion with the MCP joint in flexion (Fig. 13-19).
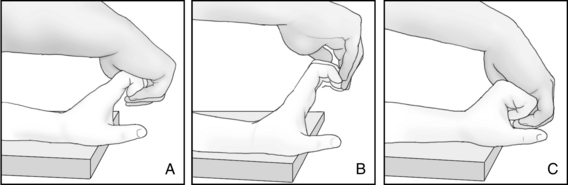
Figure 13-19 Testing for intrinsic shortening. A, The therapist holds the metacarpophalangeal joints in extension and attempts to flex the proximal interphalangeal joints. If the therapist can achieve this position, then full excursion of the intrinsic muscles is present. The evaluation is complete. B, If therapist cannot achieve full passive flexion of the proximal interphalangeal joint while the metacarpophalangeal joints are extended, the intrinsic muscles have become tight. C, With intrinsic tightness, however, the therapist possibly may attain full passive proximal interphalangeal flexion with the metacarpophalangeal joint in flexion.
Many patients also develop contracture of the extensor tendons. Therapists must determine whether the alteration of the position of the MCP joint affects the amount of flexion obtained at the PIP joint. If shortening or adhesion of the extensor has occurred, the therapist is able to flex the PIP joint further with the MCP joint extended than with it flexed.48 This phenomenon occurs because extension relaxes the extensor system, whereas flexion builds up the passive tension.
Collateral ligament tightness of the PIP joint limits PIP joint motion regardless of the position of the MCP joint.18 The testing is performed by flexing the PIP joint with the MCP joint extended and again with it flexed; if PIP joint motion is limited in both testing positions, the collateral ligaments of the PIP joint have shortened (Fig. 13-20) and splinting of the PIP joint is indicated. A dynamic PIP extension splint is used if the contracture is greater than 35 degrees; a static PIP extension splint is used if the contracture is less than 35 degrees.11 A combination of both splints sometimes is used; the dynamic splint is applied for the more severe contracture, and a static extension splint is worn after the contracture is reduced to less than 35 degrees.

Figure 13-20 Proximal interphalangeal joint contracture. Collateral ligament tightness limits proximal phalangeal joint motion, regardless of the position of the metacarpophalangeal joint.
(From Hunter JM, Mackin E, Callahan A: Rehabilitation of the hand: surgery and therapy, ed 4, St Louis, 1995, Mosby.)
Loss of active flexion of the DIP joint may be caused by joint contracture or contracture of the oblique retinacular ligament. The therapist performs the oblique retinacular ligament tightness test by passively flexing the DIP joint with the PIP joint in extension and then repeating the test with the PIP joint in flexion. If more motion occurs when the PIP joint is flexed than when it is extended, a shortening or contracture of this ligament has occurred (Fig. 13-21). If equal loss of flexion occurs with the PIP joint flexed or extended, a joint contracture is evident.18 Contracture of the DIP joint with decreased DIP flexion can be treated with the use of a flexion strap with the MCP, PIP, and DIP joints in as much flexion as possible. This strap can be fabricated from Velcro strapping and is commercially available (Fig. 13-22). The patient can use the strap intermittently during the day for one hour on and one hour off.
Treatment of joint contractures with low-load prolonged stress
Neuromuscular dysfunction is a common cause of physiological joint restriction and contractures.26 Splints are used to maintain or lengthen soft tissues and maintain joint integrity. If a joint has become contracted, the joint capsule becomes stiff, the synovial fluid becomes thickened from nonmovement, and the ligaments around one side of the joint become shortened, whereas the ligaments on the other side become lax. Soft-tissue involvement in contractures includes shortened tendons and skeletal muscle. High-load brief stretch manual therapy alone does not achieve plastic elongation of tissues over time.12 LLPS involves holding the tissues in a low-lengthened position for a total end range time. A low-lengthened position is a passive position with a low-load stress (in which the patient feels a slight stress but one that he or she can tolerate for a significant amount of time, i.e., three to four hours total end range time). The total end range time increases over time to an ideal of six to eight hours. The soft tissue grows, not stretches, to the new lengthened position.26
Current literature supports LLPS as the preferred method of lengthening shortened tissues. The common clinical practice of stretching contractures manually with high brief-load periods for one to two minutes is contraindicated in the literature.26 The elongation accomplished by manual stretch alone shortens when the force is relaxed. Manual therapy prepares tissues but must be followed with splinting and activities to affect permanent changes.12
A study by Light and colleagues26 tested knee contractures using high-load brief stretch or LLPS on 11 geriatric patients. All subjects had bilateral knee contractures; high-load brief stretch was the treatment for one knee, and LLPS was the treatment for the other. The LLPS in this study was accomplished by traction. LLPS produced a greater overall increase in passive ROM than did the high-load brief stretch.
Splinting to provide an LLPS is a noninvasive, nonstressful, and ideally painless treatment.26 The treatment for joint stiffness and contracture is stress, which involves intensity (amount of effort), duration (amount of time), and frequency (amount of repetition).12 Although all these stress factors are important, duration is the most important for LLPS, the optimal time being six to eight hours. This optimal duration usually must be built up slowly, beginning with one to two hours. As the joint contracture decreases, the splint must be readjusted regularly (usually weekly) to increase prolonged stress. LLPS is the principle used in some of the splints mentioned previously in this chapter, including the elbow drop-out splint, the belly gutter splint, and any dynamic splinting. As with all splinting, but especially in using LLPS splinting for patients with sensory impairments, therapists must monitor patients using these splints for skin breakdown.
Injury to the extremity
Because of decreased motor control and perceptual dysfunction (e.g., body neglect and somatoagnosia), many patients are at risk for injuries to the already compromised extremity. Many times these patients assume malaligned upper extremity patterns for prolonged periods. A common example may be observed during bed mobility training. Patients assume sitting postures from side lying and end up bearing their weight through the dorsum of their hands with the wrist flexed. This posture puts patients at risk of developing traumatic synovitis, increased edema, and pain. The patient, depending on the level of awareness, may maintain this maladaptive posture during the next task (e.g., dressing) before noticing the problem, resulting in the potential for tissue damage.
Another common alignment problem that puts patients at risk for injury occurs if upper extremity positioning devices are ineffective. Many patients are prescribed half or full lap trays to provide upper extremity support while they are seated in their wheelchairs. In many cases, the supported extremity slides between the lapboard and the patient’s trunk, pinning the wrist in extreme flexion. Depending on patient and staff awareness, this position unfortunately may be maintained for prolonged periods. Injury also can lead to pain and swelling, which in turn may trigger the initial symptoms of shoulder-hand syndrome.
Biomechanical alignment
The position a hand assumes at rest (the resting posture) has been documented by several authors. A summary of this posture is as follows:
 Forearm midway between pronation and supination29
Forearm midway between pronation and supination29
 Wrist at 10 to 15 degrees of extension11
Wrist at 10 to 15 degrees of extension11
 Thumb in slight extension and abduction with the MCP and IP joints flexed approximately 15 to 20 degrees
Thumb in slight extension and abduction with the MCP and IP joints flexed approximately 15 to 20 degrees
 Digits posture toward flexion, exhibiting greater composite flexion toward the ulnar side of the hand
Digits posture toward flexion, exhibiting greater composite flexion toward the ulnar side of the hand
 Second metacarpal aligned with the radius
Second metacarpal aligned with the radius
The therapist must consider the concept of dual obliquity when evaluating the alignment of the hand. Because of a successive decrease in the length of the metacarpals from the radial to the ulnar side, objects held in the hand assume two oblique angles.39 For example, if a pencil is held in the palm across the metacarpal heads (eraser toward the ulnar side) and the forearm is held in pronation resting on the table, the examiner can identify two oblique angles. The first angle is observed with the pencil point angled upward in relation to the wrist joint axis. The second oblique angle is observed on examination of height of each end of the pencil. The radial side is held higher than the ulnar side, that is, the pencil is not parallel to the table (Fig. 13-23).
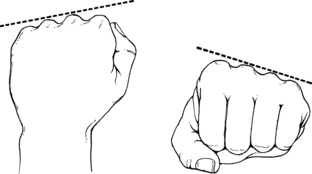
Figure 13-23 Dorsally, the consecutive metacarpal heads create an oblique angle to the longitudinal axis of the forearm. Distally, the fisted hand exhibits an ulnar metacarpal descent that creates an oblique angle in the transverse plane of the forearm.
(From Fess EE, Philips CA: Hand splinting: principles and methods, ed 2, St Louis, 1987, Mosby.)
The obliquity of the palmar transverse arch follows a line from “the second to the fifth metacarpal head and forms an angle of seventy-five degrees with the axis of the third ray.”48 Therefore, from a biomechanical perspective, the firm cone splint discussed earlier for a moderately relaxed hand should be placed with the narrow end in the ulnar side and the wide end on the radial side, following the normal obliquity.
The therapist must note deviations from the resting posture; they assist in the design of the splint. Therapists must consider that patients may differ slightly from the normal resting posture because of heredity, habits, and job descriptions; examining the opposite hand is helpful in determining the “normal” resting posture for each patient.22
The distal extremity assumes several typical alignment deviations after stroke. These deviations and their consequences include the following:
1. Wrist flexion following decreased skeletal muscle activity. This common posture (most often observed in the flaccid stage) produces a variety of pathological processes. A hand positioned in wrist flexion results in the following: flattening of the palmar arches, passive extension of the fingers due to tenodesis action, shortened collateral ligaments because of the extended digits, narrowing of the web space,11 inability to perform the grasping function (flexor action of the thumb and digits reinforced by extension of the wrist),48 blockage of ulnar and radial deviation of the wrist when it is in flexion,20 overstretching of the wrist extensors and dorsal ligaments,48 shortening of the long flexors, and a tendency to develop an edema syndrome.
2. Extreme ulnar deviation. The posture of ulnar deviation results in a variety of compounded problems. A wrist positioned in extreme ulnar deviation produces the following: effective blockage of wrist extension,20 shortening of the ulnar deviators and overstretching of the radial deviators, and shifting of the proximal and distal rows of carpal bones.48
3. Wrist and digit flexion. This posture may occur following excessive skeletal muscle activity and soft-tissue shortening. This posture results in the following: loss of normal tenodesis function (wrist extension with digit flexion and adduction, wrist flexion with digit extension and abduction), shortening of the extrinsic flexors with resultant overstretching of the extensors, potential for skin maceration, and painful contracture and deformity.
Loss of palmar arches
A familiar alignment problem in patients after stroke is the loss of palmar arches, or the development of a “flattened hand.” The maintenance of the palmar arches is crucial for hand function.4 Kapandji20 outlines the arches of the hand as follows (Fig. 13-24):
 Transverse arch: This structure consists of two arches and includes the carpal arch, which corresponds to the concavity of the wrist and is continuous with the distal metacarpal arch formed by the metacarpal heads. The carpal arch is rigid, whereas the metacarpal arch is mobile and adaptable. The long axis of the transverse arch crosses the lunate, capitate (the “keystone” of the carpal arch11), and the third metacarpal bones. Boehme4 states that the functional significance of this arch stems from its forming the hand into a gutter, bringing together the radial and ulnar borders of the hand. This arch can widen or narrow the surface area of the hand.
Transverse arch: This structure consists of two arches and includes the carpal arch, which corresponds to the concavity of the wrist and is continuous with the distal metacarpal arch formed by the metacarpal heads. The carpal arch is rigid, whereas the metacarpal arch is mobile and adaptable. The long axis of the transverse arch crosses the lunate, capitate (the “keystone” of the carpal arch11), and the third metacarpal bones. Boehme4 states that the functional significance of this arch stems from its forming the hand into a gutter, bringing together the radial and ulnar borders of the hand. This arch can widen or narrow the surface area of the hand.
 Longitudinal arch: This arch includes the carpometacarpophalangeal arches. These arches are formed for each finger by the corresponding metacarpal bones and phalanges. Kapandji20 notes that the arches are concave on the palmar surface; the “keystone” of each arch lies at the level of the MCP joint. According to Boehme,4 in its simplest form, this arch supports a basic cylindrical grasp. If the arches are expanded, the hand is longer. This arch allows the palm to flatten and cup itself around objects.11
Longitudinal arch: This arch includes the carpometacarpophalangeal arches. These arches are formed for each finger by the corresponding metacarpal bones and phalanges. Kapandji20 notes that the arches are concave on the palmar surface; the “keystone” of each arch lies at the level of the MCP joint. According to Boehme,4 in its simplest form, this arch supports a basic cylindrical grasp. If the arches are expanded, the hand is longer. This arch allows the palm to flatten and cup itself around objects.11
 Oblique arches: These arches are formed by the thumb during opposition with the other fingers. Kapandji20 states that the most important of these arches is the one linking the thumb and index finger; the most extreme is the one linking the thumb and the little finger. These arches are obviously crucial in the opposition of the digits.
Oblique arches: These arches are formed by the thumb during opposition with the other fingers. Kapandji20 states that the most important of these arches is the one linking the thumb and index finger; the most extreme is the one linking the thumb and the little finger. These arches are obviously crucial in the opposition of the digits.
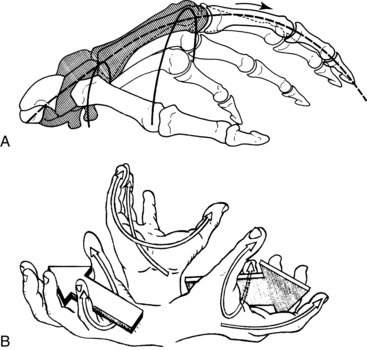
Figure 13-24 A, Side view of the longitudinal and transverse arches of the hand. The shaded areas show the fixed part of the skeleton. B, The thumb forms, along with the other digits, four oblique arches of opposition. The most useful and functionally important arch is between the thumb and index finger, used for precision grip. The farthest arch, between the thumb and little finger, ensures a locking mechanism on the ulnar side of the hand in power grips.
(From Tubiana R, Thomine JM, Mackin E: Examination of the hand and wrist, St Louis, 1996, Mosby.)
Patients lose their arches after stroke for a variety of reasons, including edema in the dorsum of the hand that biomechanically forces the metacarpals inferiorly, inactivity of the wrist and hand, prolonged and extreme wrist flexion (resulting in a flattening of the arches), and inappropriate support of the hand during weight-bearing activities.4
During evaluation of splinting, therapists should examine the arches of the hand and compare them with those of the unaffected hand. In the dorsal surface of a normal hand at rest, the MCP joints form an arch with the apex at the third metacarpal (i.e., the third metacarpal head is higher than the others are) (see Fig. 13-24). Many patients have a flattened arch (i.e., the MCP joints lose their arches), and in response the proximal phalanges hyperextend. This posture puts the patient at risk for developing a permanent claw-hand deformity and effectively blocks opposition of the thumb (Fig. 13-25).

Figure 13-25 Flattening of the palmar arches resulting from hand paralysis. Hyperextension of the metacarpophalangeal joints and flexion of the proximal and distal interphalangeal joints occur because of an imbalance of the extrinsic flexor and extensor systems.
(From Hunter JM, Mackin E, Callahan A: Rehabilitation of the hand: surgery and therapy, ed 4, St Louis, 1995, Mosby.)
In these cases, splinting may be indicated to give outside support to the arches through upward pressure on the palmar surface of the hand. To be effective and give full support to the metacarpals, the splint must conform to the arches and be contoured to the individual’s hand. Commercially available splints are not effective for this type of intervention because they do not take into account the variability of arches.
For patients with hyperextended MCPs and flexed PIP joints (i.e., claw-hand deformity), a dorsal MCP extension restriction splint can be fabricated in thermoplastic material to eliminate deformity and increase function (Fig. 13-26).
Learned nonuse
Current research (see Chapter 10) has demonstrated the existence of a component of upper extremity dysfunction resulting from a learned phenomenon of nonintegration of the hand into functional tasks. This process likely begins in the early stages after stroke, before any functional recovery has commenced. Patients learn to compensate with their unaffected sides, thereby repressing any return of function on the hemiplegic side.
Many CVA protocols call for splinting immediately after stroke. Some facilities have standing orders for splinting in their acute services. Current research indicates that early splinting in the early poststroke phase may be detrimental. The splint gives a message that an outside device is responsible for the maintenance and improvement of the affected hand. Because the hand is supported and aligned through outside means, the patient does not attend to the hand, stretch the wrist and hand, or attempt to integrate it into functional tasks. Early splinting may predispose patients to a learned nonuse phenomenon. A sign that a patient is predisposed to learned nonuse is the observation that a patient, after cueing, can integrate functional return during a therapy session but does not integrate this new function outside the sessions. The therapist must balance interventions for contracture prevention with activities that encourage functional use of the hand, thereby negating the effects of learned nonuse. Splinting for contractures can be used at night instead of during the day to prevent learned nonuse behavior patterns.
Decision-making process
The therapist must evaluate all of the following areas when deciding whether to splint and choosing the type of splint to fabricate. This section is designed to help guide the therapist’s clinical reasoning in making splinting decisions.
1. Evaluate cognitive and perceptual status: Does the patient attend to the extremity during the day (attending includes self-ranging, rubbing, positioning, and protecting)? Is the patient alert for the greater portion of the day?
 If the answer is yes, the patient may be able to maintain ROM and alignment in the extremity without the use of splints; the therapist should consider not splinting.
If the answer is yes, the patient may be able to maintain ROM and alignment in the extremity without the use of splints; the therapist should consider not splinting. If the answer is no, neglect, decreased attention, somatoagnosia, and decreased alertness and arousal may place the patient at risk for contracture and malalignment; splinting therefore may be indicated.
If the answer is no, neglect, decreased attention, somatoagnosia, and decreased alertness and arousal may place the patient at risk for contracture and malalignment; splinting therefore may be indicated.2. Evaluate soft tissue tightness: Does the patient have full composite flexion and extension? Can the patient be ranged into a full intrinsic minus/intrinsic plus position? Does the patient have full and pain-free range of wrist motion, especially extension and radial deviation?
 If the answer is yes, the therapist should consider not splinting. Treatment should focus on teaching the patient and family techniques to maintain this range and prevent pain and contracture.
If the answer is yes, the therapist should consider not splinting. Treatment should focus on teaching the patient and family techniques to maintain this range and prevent pain and contracture. If the answer is no, splinting may be indicated to improve or at least maintain soft-tissue length. The splint should be designed to place the shortened soft tissues on prolonged stretch.
If the answer is no, splinting may be indicated to improve or at least maintain soft-tissue length. The splint should be designed to place the shortened soft tissues on prolonged stretch.3. Evaluate joint contracture: Splinting is necessary to ameliorate joint contracture and prevent further deformity.
4. Evaluate learned nonuse: Does the patient integrate the extremity into functional tasks in the clinic without carryover into nontherapy hours?
 If the answer is yes, the therapist should consider not splinting. In this situation, the patient does have distal function; this function should not be impeded by splinting. The splint may in fact feed into the learned nonuse cycle.
If the answer is yes, the therapist should consider not splinting. In this situation, the patient does have distal function; this function should not be impeded by splinting. The splint may in fact feed into the learned nonuse cycle.5. Evaluate function: Does the patient exhibit distal motor control (including gross patterns) that can be integrated into activities of daily living and instrumental activities of daily living?
 If the answer is yes, the therapist should consider not splinting or should choose a splint that enhances the functional return (e.g., a basic wrist extension splint to provide a stable proximal segment for the digits to work from or a simple opponens splint to improve fine motor control).
If the answer is yes, the therapist should consider not splinting or should choose a splint that enhances the functional return (e.g., a basic wrist extension splint to provide a stable proximal segment for the digits to work from or a simple opponens splint to improve fine motor control). If the answer is no, splinting may be indicated, although the therapist must consider that splinting a hand without functional recovery may block the initial motor return (sometimes automatic reactions and protective responses) or the patient’s initial attempts at function.
If the answer is no, splinting may be indicated, although the therapist must consider that splinting a hand without functional recovery may block the initial motor return (sometimes automatic reactions and protective responses) or the patient’s initial attempts at function.6. Evaluate potential for soft-tissue injury: Is evidence of skin maceration and laceration in the palm of the hand and lateral aspect of the thumb from extreme flexion apparent?
 If the answer is yes, the therapist seriously must consider splinting to prevent further damage and enhance the healing process; wrist extension splints with distal cones or palm guards are recommended.
If the answer is yes, the therapist seriously must consider splinting to prevent further damage and enhance the healing process; wrist extension splints with distal cones or palm guards are recommended.7. Evaluate biomechanical alignment: Are deviations from the standard resting position of the hand evident? Does realigning the hand result in increased relaxation?
 If the answer is yes, the therapist should consider splinting to improve resting alignment of the extremity to prevent shortening and overstretching of soft tissue.
If the answer is yes, the therapist should consider splinting to improve resting alignment of the extremity to prevent shortening and overstretching of soft tissue.8. Evaluate sensation: Does the patient have sensory impairments?
 If the answer is yes, the therapist should consider the amount of cutaneous surface area that is covered by splinting. The splint may end up blocking the little sensory input the hand is receiving. A general goal for the involved extremity is to maximize sensory input. If sensation is impaired, extra precautions are necessary for careful, custom splint fabrication and diligent, ongoing monitoring of the skin condition by the therapist, patient, and family for any breakdown or maceration, which the patient may not detect. This is especially important if cognitive deficits are present.
If the answer is yes, the therapist should consider the amount of cutaneous surface area that is covered by splinting. The splint may end up blocking the little sensory input the hand is receiving. A general goal for the involved extremity is to maximize sensory input. If sensation is impaired, extra precautions are necessary for careful, custom splint fabrication and diligent, ongoing monitoring of the skin condition by the therapist, patient, and family for any breakdown or maceration, which the patient may not detect. This is especially important if cognitive deficits are present.9. Evaluate edema: Does the patient have distal edema?
 If the answer is yes, the therapist should consider whether a splint will support a flexed wrist with the goal of counteracting the dependent positioning of the hand, thereby decreasing or preventing further edema. Will the immobilization of the splint increase the edema by blocking the “pumping action” of muscles generated by active ROM? Patients with edema tend to lose digit flexion, thereby keeping the collateral ligaments in a shortened position. Will the splint block digit flexion, thereby exacerbating this problem? Will the splint impinge on neuromuscular structures and further limit hemodynamic function?
If the answer is yes, the therapist should consider whether a splint will support a flexed wrist with the goal of counteracting the dependent positioning of the hand, thereby decreasing or preventing further edema. Will the immobilization of the splint increase the edema by blocking the “pumping action” of muscles generated by active ROM? Patients with edema tend to lose digit flexion, thereby keeping the collateral ligaments in a shortened position. Will the splint block digit flexion, thereby exacerbating this problem? Will the splint impinge on neuromuscular structures and further limit hemodynamic function?10. Evaluate posturing: Does the patient posture in persistent flexion?
General splinting guidelines
Therapists should consider the following guidelines regarding splinting:
1. Check for abnormal pressure points, especially over bony prominences (e.g., ulnar head).
2. Decide during which activities and periods the patient will wear the splint. The splint must be evaluated or fabricated while the patient is in the most difficult posture and performing the most stressful activities if the effectiveness of the splint is to be evaluated. For example, fabricating a splint while the patient is seated and relaxed may result in a good fit with a relaxed hand. However, if the patient then leaves therapy to prepare a meal at home, the therapist may find the patient’s hand “clawing” and flexing out of the splint. If the splint was fabricated with the patient standing and with the appropriate level of stretch, this phenomenon may not be a problem.
3. Splint for comfort. Pain and pressure responses may increase the patient’s bias toward stereotypical posturing.
4. Patients need to experience full ROM. Use positioning splints only as adjuncts to a comprehensive upper extremity program.
5. Monitor full ROM. Many patients have been provided with resting hand splints to prevent flexion contractures only to end up with extension contractures, or “intrinsic lock.”
6. Make wearing schedules practical to ensure patient compliance.
7. Therapists must have reasonable expectations for splints. An extremely tight hand may require several serial splints to achieve a desired position. Splints designed to provide correction at more than one joint can lead to added deformity if excessive skeletal muscle activity is present. For example, attempting to position the wrist and digits into extension may create a clawing effect in the digits as a result of the amount of stretch at the wrist and digits.50 A severely malaligned hand may respond best if the therapist only focuses on one particular aspect of the malalignment (proximal first). For example, counteracting the extreme ulnar deviation in this type of extremity may be the goal of the first splint, followed by neutral deviation with slight wrist extension for the next splint. The therapist must remember that with an extremely tight or contracted hand, all deformities cannot be addressed simultaneously; if simultaneous correction is attempted, compliance with splinting may be jeopardized because of the discomfort level and skin breakdown.
8. Educate patients about the realistic goals and expectations of the use of a splint. Many patients wear their splints for prolonged periods with the hope that the splint will “make their hand better.” Most patients interpret “better” as a return in function. However, this may not be the case for all patients; therefore, the patient should be aware of the reasons that the splint was prescribed. No splint should be worn continuously.
General fabrication guidelines
Many splinting materials are commercially available today. They are thermoplastic materials; some have more rubber content base than others do. The rubber content base materials tend to have increased conformability and drape compared with pure thermoplastic materials, but they may be more difficult to handle because of their draping quality.
Thermoplastic materials generally have a greater memory capacity than do the rubber-based thermoplastics. Memory indicates the capability of the material to return to its original shape after the reheating that occurs during fabrication of the splint. Some therapists prefer the thermoplastics because of the memory capacity. The thermoplastics are available in perforated and solid forms. Perforated materials are recommended to allow for breathability and decrease the possibility of skin maceration (especially with patients with sympathetic nerve changes and sensory impairments). The therapist must take care when using maxiperforated thermoplastics to eliminate sharp edges after cutting the material. The edges must be heated with a heat gun and turned down to smooth the edging; the edges may also be covered with 1/16-inch solid material cut into 1-inch wide but long pieces, heated in water, and then applied to the edging. The therapist also may use a thin layer of moleskin to smooth the edges of perforated material.
The thermoplastic materials and rubber-based thermoplastics are available in various thicknesses ranging from ⅛-inch, 3/32-inch, 1/12-inch, and 1-inch; the most common width is ⅛-inch. Some of the splinting materials are available in a wide range of colors; these may help draw attention to the involved limb and prevent the splint from being lost in hospital bedding. Color also may enhance compliance. Several vendors offer precut splint blanks and kits. These products can be cut to size for customization and to decrease the amount of splinting time required for fabrication. Prefabricated splints also are available for many splinting needs, but some may be difficult to customize. The authors do not recommend some of the commercially available spring wire splints for patients with sensory impairments because these splints may apply too much pressure that the patient will not be able to detect. Custom-fabricated splints are the splints of choice for patients with sensory impairments.
Velcro strapping materials are now available in multiple colors. Velfoam, a padded strapping material, is highly recommended for the patient with sensory impairments because it is a softer strapping material.
Splint padding does not compensate for a poorly fitted splint and increases the pressure within the splint. Splint padding is recommended to cushion fingers at the point of contact of the thermoplastic material in dynamic splints only. Splint padding is available under different trade names. Splint padding materials only increase the pressure of an ill-fitting splint, and when used in this way, may also be hot and uncomfortable for the patient and may increase the possibility of skin maceration because of the increased perspiration that the padding may cause in a patient.
Splinting the extremity of a patient with neurological involvement is sometimes difficult if severely increased skeletal muscle activity is evident in the upper extremity. Maintaining the desired alignment and molding the splinting material may be almost impossible. The assistance of another person for positioning usually is indicated for a proper fit. Pattern-making also may be difficult with this type of patient. The fabrication of a gross pattern on the unaffected hand and reversal of the pattern for transfer to the splinting material are helpful at times.
The therapist must make allowances for bony prominences by cutting around or flaring the splinting material over the prominence. A helpful hint for flaring out the material is to place a spot of dark lipstick over the bony prominence (on the patient’s skin); place the cooled, already formed splint on the patient; and remove the splint. The lipstick now will be on the splint in the exact spot at which the splint requires flaring.
During the use of thermoplastic materials in splinting, the placement of curve in the material increases the tensile strength of the material to approximately 20 times that of straight material. This is helpful to remember in the fabrication of dynamic outriggers from thermoplastic material or the creation of an additional roll in the material as a spine or support.
Specific fabrication guidelines
Forearm support
If the splint prescribed for a patient includes a forearm trough, basic splinting principles call for the trough to cover two thirds of the forearm. To compensate for the weight of the hand and the excess force created by increased distal flexor activity, the forearm trough should be two thirds of the length of the forearm to provide a sufficient lever.
Palmar support
Many patients with neurological involvement have flattened arches at the MCP joints, with resultant clawing of the digits. This malalignment usually occurs in patients with little or no skeletal muscle activity in the affected hand. In molding the splint into the palmar arch in these cases, the therapist can use the thumb to mold a letter T pattern over the palmar surface of the splint. The base of the T runs longitudinally through the center of the palm, whereas the top of the T runs across the metacarpal heads. The base of the T should connect to the top of the T at the third MCP head. The T shape is molded into the palm to enhance the arch. To ensure sturdy arch support, the splint must progress distal to the distal palmar crease and does not need to clear the thenar eminence in a hand without movement. The therapist should reevaluate the patient frequently for returning motor control and should adjust the splint as needed. If the patient exhibits controlled digit flexion, the distal end of the splint needs to be rolled back proximal to the distal palmar crease so that returning function is not blocked. If the patient begins to exhibit thumb function, the palmar support surface of the splint must again be rolled back to clear the thenar eminence and therefore not block active movement.
After splint fabrication, the therapist evaluates the palmar support section of the splint by checking that the dual obliquity of the hand is maintained, the third metacarpal head is the apex of the arch formed by the metacarpal heads, and the hand is not “flattened” in the splint (Figs. 13-27 and 13-28).

Figure 13-27 Variations on palmar support fabrication. A, Full palmar support (material progresses past the distal palmar crease and gives the thumb support over the first metacarpal). B, As function returns, the distal and thenar aspects of the splint are rolled back to allow for joint excursion during functional tasks. The T shape is molded into the palmar aspect of the splint.

Figure 13-28 Molding the T support into the splint. The base of the T runs longitudinally through the palm, whereas the top of the T supports the metacarpal arch. The base of the T intersects the top of the T at the third metacarpal head. Palmar support is accurate if the arches of the hand are maintained, and the third metacarpal head is superior to the metacarpal heads of digits two and four.
Wrist support
When molding and evaluating the wrist component of a splint for the patient after stroke, the therapist must consider alignment:
 The third metacarpal should lie midway between the radius and ulna in a neutral deviated hand. Many hands with neurological involvement have a tendency to assume a position of ulnar deviation. Splint modifications to the wrist component include raising the border of the splint that lies lateral to the fifth metacarpal. This modification effectively blocks the ulnar deviation (Fig. 13-29).
The third metacarpal should lie midway between the radius and ulna in a neutral deviated hand. Many hands with neurological involvement have a tendency to assume a position of ulnar deviation. Splint modifications to the wrist component include raising the border of the splint that lies lateral to the fifth metacarpal. This modification effectively blocks the ulnar deviation (Fig. 13-29).
 The wrist should be supported between zero and 20 degrees of extension. Gillen and colleagues13 examined the effect of various wrist positions on upper extremity function in adults wearing a wrist immobilizing splint. The Jebsen Taylor Test of Hand Function was administered to 20 adults without upper extremity impairment to determine the effects, if any. The test was administered three consecutive times. Each time the subject wore a commercially available wrist extension splint that positioned the wrist in zero degrees (neutral), 15 degrees, or 30 degrees of wrist extension. Wrist angles were confirmed via goniometry. The order in which the wrist angles were tested was randomized to control for fatigue and practice effects. The results of this study indicated that there was no significant difference between the tested wrist positions (0 degrees, 15 degrees, 30 degrees) when using the nondominant hand to perform activities while wearing a wrist splint. However, significant differences were found when wearing various angled wrist splints to perform functional activities with the dominant hand albeit only for select tasks (feeding and stacking checkers). During the feeding subtest, participants performed at a significantly faster rate when their dominant wrists were positioned in 15 degrees of extension as compared to performance with a neutral wrist. During the stacking checkers subtest, participants performed at a significantly faster rate when their wrists were positioned in neutral when compared with when they were positioned in 30 degrees of extension. Nonetheless, the final decision depends on which angle allows the maximal amount of function or (if the hand is not functional) which angle in this range decreases the usual abnormal flexor activity in the digits. (Many patients’ digits relax if they are realigned proximally.) In some cases, the splint may be fabricated in some degree of flexion. This may be required if contracture of the extrinsic flexors is evident and the goal is systematically to lengthen the flexors with serial splinting. In these cases, each subsequent splint should be molded with an increased stretch on the flexors. For example, the first splint may be molded in 20 degrees of wrist flexion; the next in 10 degrees of flexion, neutral wrist; and finally in some degree of extension. Therapists must remember that if the goal is to lengthen the extrinsic flexors, wrist and digit support is required.
The wrist should be supported between zero and 20 degrees of extension. Gillen and colleagues13 examined the effect of various wrist positions on upper extremity function in adults wearing a wrist immobilizing splint. The Jebsen Taylor Test of Hand Function was administered to 20 adults without upper extremity impairment to determine the effects, if any. The test was administered three consecutive times. Each time the subject wore a commercially available wrist extension splint that positioned the wrist in zero degrees (neutral), 15 degrees, or 30 degrees of wrist extension. Wrist angles were confirmed via goniometry. The order in which the wrist angles were tested was randomized to control for fatigue and practice effects. The results of this study indicated that there was no significant difference between the tested wrist positions (0 degrees, 15 degrees, 30 degrees) when using the nondominant hand to perform activities while wearing a wrist splint. However, significant differences were found when wearing various angled wrist splints to perform functional activities with the dominant hand albeit only for select tasks (feeding and stacking checkers). During the feeding subtest, participants performed at a significantly faster rate when their dominant wrists were positioned in 15 degrees of extension as compared to performance with a neutral wrist. During the stacking checkers subtest, participants performed at a significantly faster rate when their wrists were positioned in neutral when compared with when they were positioned in 30 degrees of extension. Nonetheless, the final decision depends on which angle allows the maximal amount of function or (if the hand is not functional) which angle in this range decreases the usual abnormal flexor activity in the digits. (Many patients’ digits relax if they are realigned proximally.) In some cases, the splint may be fabricated in some degree of flexion. This may be required if contracture of the extrinsic flexors is evident and the goal is systematically to lengthen the flexors with serial splinting. In these cases, each subsequent splint should be molded with an increased stretch on the flexors. For example, the first splint may be molded in 20 degrees of wrist flexion; the next in 10 degrees of flexion, neutral wrist; and finally in some degree of extension. Therapists must remember that if the goal is to lengthen the extrinsic flexors, wrist and digit support is required.
 After molding the splint, the therapist should check that the hand is not in a position of medial or lateral rotation (neutral) compared with the forearm. Many patients who exhibit excessive skeletal muscle activity develop a tendency for the hand to rotate medially or laterally in relation to the forearm. The hand should be positioned in the splint so that the fifth metacarpal is aligned with the ulna instead of lying inferior to the ulna (the hand is laterally rotated in relation to the forearm) or lying superior to the ulna (the hand is medially rotated in relation to the forearm).
After molding the splint, the therapist should check that the hand is not in a position of medial or lateral rotation (neutral) compared with the forearm. Many patients who exhibit excessive skeletal muscle activity develop a tendency for the hand to rotate medially or laterally in relation to the forearm. The hand should be positioned in the splint so that the fifth metacarpal is aligned with the ulna instead of lying inferior to the ulna (the hand is laterally rotated in relation to the forearm) or lying superior to the ulna (the hand is medially rotated in relation to the forearm).
Digit support
The therapist should use a digit support platform only as a last resort. The therapist must include a digit support platform in the splint if the patient exhibits excessive flexor activity in the digits that cannot be otherwise controlled and if the patient is being splinted for contracture management. If the splint includes a digit platform, daytime use of the splint is discouraged.
If a patient exhibits excessive flexor activity, the therapist first should try a forearm and wrist splint that enhances alignment. In many patients, a proximal realignment of the joints and a prolonged state of accommodation of muscles to their resting length relaxes the hand. Therapists can evaluate this phenomenon by manually realigning the joints with their hands and evaluating whether a relaxation response occurs.
If a digit support platform is necessary, the digits should not be overstretched to the point that a “clawing” of the hand or a “bottoming out” of the metacarpals occurs. The therapist must ensure that the palmar arch remains intact when the digits are stretched onto the platform (Fig. 13-30).
Thumb support
In the nonfunctional hand, the thumb should be supported in a position midway between palmar and radial abduction. This position can be maintained by the previously described palmar support, which also supports the first metacarpal; if the splint is rolled back to clear the thenar eminence, the thumb cannot be supported in this position (see Fig. 13-27).
If the thumb is functional, the splinted position is dictated by evaluation of the position of thumb that is the most effective at enhancing function with the thumb in opposition. Fig. 13-31 describes the clinical reasoning process followed for deciding on the type and style of splint to fabricate.
Prefabricated splints
In cases in which prefabricated splints are indicated, therapists must take great care to ensure proper fitting. Patients should not be encouraged to purchase splints “off the shelf” without a therapist’s input because of the potential complications. Examples of commonly used and useful prefabricated splints include air-assist splints for LLPS (see Fig. 13-15), a Multi Podus ankle/foot orthosis (Fig. 13-32), and elbow splints to provide stretch (Fig. 13-33).
Summary
When designing or fabricating a splint for a patient after stroke, the therapist must consider each patient individually; no set of rules applies to all patients with neurological impairments. No definitive answers or protocols are available. The reader is encouraged to consider the questions in the decision-making section of this chapter to guide clinical reasoning, because the therapist must consider so many factors in treatment.
Any hand with a malalignment or deformity results in an overstretching of the soft tissues (muscles, ligaments) on one side of the joint and shortening of the soft tissues on the opposite side. All treatment, including splinting, should be instituted after consideration of this phenomenon and should aim to preserve the length and balance of soft tissue on either side of the joint. This treatment prepares the hand for possible future integration into functional activities and prevents permanent deformity.
All splints applied to patients after stroke, especially patients with increased skeletal muscle activity and decreased sensation who are being treated with the principles of LLPS, must be monitored continually by therapists, nursing staff, and family members to assess for skin integrity. This concept is particularly crucial for patients with cognitive and perceptual deficits. Factors in the monitoring of skin integrity include signs of skin discoloration, maceration, edema, and breakdown.
Splinting for patients after stroke that combines the principles of biomechanical positioning and the neurophysiological concepts of facilitation and inhibition may lead to the most favorable components of function.51
Realistic outcomes must be the guiding forces in the decision-making process in the fabrication of splints for patients after stroke. Clinicians working with this population who use splinting as an adjunct treatment should strive to gain a solid understanding of anatomy, biomechanics, and motor control theories.
Finally, therapists have a responsibility not only to stay current on research regarding this area of intervention but also to add to the literature through research, from single-subject case studies to qualitative trend analyses to large subject-sample qualitative studies. Until more definitive and well-designed research studies are available concerning this treatment, the splinting controversy for patients after stroke will continue, and therapists may be providing patients with less than optimal care.
Review questions
1. What is the normal resting posture of the hand? What are the common malalignments observed after a stroke?
2. What precautions should be followed when splinting a patient after stroke?
3. What is the recommended rationale for splinting the patient after stroke?
4. How does the therapist differentiate among intrinsic tightness, extrinsic tightness, and joint contracture when evaluating for a splint?
5. What are the advantages of LLPS versus high-load brief stretch?
1. Blashy MRM, Fuchs-Neeman RL. Orthokinetics. a new receptor facilitation method. Am J Occup Ther. 1959:13;5:226-234.
2. Bloch R, Evans MG. An inflatable splint for the spastic hand. Arch Phys Med Rehabil. 1977;58(4):179-180.
3. Bobath B. Adult hemiplegia: evaluation and treatment, ed 3. Oxford: Butterworth-Heineman; 1990.
4. Boehme R. Improving upper body control. an approach to assessment and treatment of tonal dysfunction. Tucson, AZ: Therapy Skill Builders. 1988.
5. Brennan J. Response to stretch of hypertonic muscle groups in hemiplegia. Br Med J. 1959;1(5136):1504-1507.
6. Casey CA, Kratz EJ. Soft splinting with neoprene. the thumb abduction supinator splint. Am J Occup Ther. 1988:42;6:395-398.
7. Charait SE. A comparison of volar and dorsal splinting of the hemiplegic hand. Am J Occup Ther. 1968;22(4):319-321.
8. Currie DM, Mendiola A. Cortical thumb orthosis for children with spastic hemiplegic cerebral palsy. Arch Phys Med Rehabil. 1987;68(4):214-217.
9. Doubilet L, Polkow LS. Theory and design of a finger abduction splint for the spastic hand. Am J Occup Ther. 1977;21(5):320-322.
10. Feldman PA. Upper extremity casting and splinting. In: Glenn MB, Whyte J, editors. The practical management of spasticity in children and adults. Philadelphia: Lea & Febiger, 1990.
11. Fess EE, Philips CA. Hand splinting. principles and methods, ed 2. St Louis: Mosby. 1987.
12. Flowers K. Orthopaedic assessment and mobilization of the upper extremity, Scar Wars I & II. Seminar conducted in New York City; 1992.
13. Gillen G, Goldberg R, Muller S, Straus J. The effect of wrist position on upper extremity function while wearing a wrist immobilizing splint. J Prosthet Orthot. 2008;20(1):19-23.
14. Gossman MR, Sahrman SA, Rose SJ. Review of length associated changes in muscles. experimental evidence and clinical implications. Phys Ther. 1982:62;12:1799-1808.
15. Halar EM, Bell KR. Contracture and other deleterious effects on immobility. In Delisa JA, editor: Rehabilitation medicine: principles and practice, ed 2, Philadelphia: JB Lippincott, 1993.
16. Hill SG. Current trends in upper extremity splinting. In: Boehme R, editor. Improving upper body control: an approach to assessment and treatment of tonal dysfunction. Tucson, AZ: Therapy Skill Builders, 1988.
17. Hummelsheim H, Munch B, Butefisch C, et al. Influence of sustained stretch on late muscular responses to magnetic brain stimulation in patients with upper motor neuron lesions. Scand J Rehabil Med. 1994;26(1):3-9.
18. Hunter JM, Mackin E, Callahan A. Rehabilitation of the hand. surgery and upper extremity, ed 5. St Louis: Mosby. 2002.
19. Johnstone M. Restoration of motor function in the stroke patient. a physiotherapist’s approach. New York: Churchill Livingstone. 1983.
20. Kapandji IA. The physiology of the joints, ed 5. New York: Churchill Livingstone. 1982. Upper limb, vol 1
21. Kaplan N. Effect of splinting on reflex inhibition and sensorimotor stimulation in treatment of spasticity. Arch Phys Med Rehabil. 1962;43:65-569.
22. Kiel JH. Basic hand splinting. a pattern-designing approach. Boston: Little, Brown. 1983.
23. Lannin NA, Herbert RD. Is hand splinting effective for adults following stroke? A systematic review and methodologic critique of published research. Clinical Rehabilitation. 2003;17(8):16-807.
24. Lannin NA, Horsley SA, Herbert R, et al. Splinting the hand in the functional position after brain impairment. a randomized, controlled trial. Arch Phys Med Rehabil. 2003:84;2:297-302.
25. Lannin NA, Cusick A, McCluskey A, Herbert RD. Effects of splinting on wrist contracture after stroke. a randomized controlled trial. Stroke. 2007:38;1:6-111.
26. Light KE, Nuzik S, Personius W, et al. Low-load prolonged stretch vs high-load brief stretching in treating knee contractures. Phys Ther. 1984;64(3):330-333.
27. Ma HI, Trombly CA. A synthesis of the effects of occupational therapy for persons with stroke, part II. remediation of impairments. Am J Occup Ther. 2002:56;3:74-260.
28. MacKinnon J, Sanderson E, Buchanan J. The MacKinnon splint. a functional hand splint. Can J Occup Ther. 1975:42;4:157-158.
29. Malick MH. Manual on static hand splinting, ed 5. Pittsburgh: Harmarvile Rehabilitation Center; 1985.
30. Mathiowetz V, Bolding DJ, Trombly CA. Immediate effects of positioning devices on the normal and spastic hand measured by electromyography. Am J Occup Ther. 1983;37(4):247-254.
31. McPherson JJ. Objective evaluation of a splint designed to reduce hypertonicity. Am J Occup Ther. 1981;35(3):189-194.
32. McPherson JJ, Kreimeyer D, Aalderks M, et al. A comparison of dorsal and volar resting hand splints in the reduction of hypertonus. Am J Occup Ther. 1982;36(10):664-670.
33. Neeman RL, Liederhouse JJ, Neeman M. A multidisciplinary efficacy study on orthokinetics treatment of a patient with post-CVA hemiparesis and pain. Can J Rehabil. 1988;2(1):41-52.
34. Neeman RL, Neeman M. Efficacy of orthokinetic orthotics for post-stroke upper extremity hemiparetic motor dysfunction. Int J Rehabil Res. 1993;16(4):302-307.
35. Neeman RL, Neeman M. Orthokinetic orthoses. clinical efficacy study of orthokinetics treatment for a patient with upper extremity movement dysfunction in late post-acute CVA. J Rehabil Res Dev. 1992;29:41-53. (ann suppl)
36. Neeman RL, Neeman M. Rehabilitation of a post stroke patient with upper extremity hemiparetic movement dysfunction by orthokinetic orthoses. J Hand Ther. 1992;5:147-155.
37. Neuhaus BE, Ascher ER, Coullon BA, et al. A survey of rationales for and against hand splinting in hemiplegia. Am J Occup Ther. 1981;35(2):83-90.
38. Nicholson DE. The effects of pressure splint treatment on the motor function of the involved limb in patients with hemiplegia. master’s thesis, Chapel Hill: University of North Carolina; 1984.
39. Pedretti LW. Hand splinting. In Pedretti LW, Zoltan B, editors: Occupational therapy: practice skills for physical dysfunction, ed 3, St Louis: Mosby, 1990.
40. Peterson LT. Neurological consideration in splinting spastic extremities. 1980. unpublished paper
41. Poole JL, Whitney SL. Inflatable pressure splints (airsplints) as adjunct treatment for individual with strokes. Phys Occup Ther Geriatr. 1992;11(1):17-27.
42. Poole JL, Whitney SL, Hangeland N, et al. The effectiveness of inflatable pressure splints on motor function in stroke patients. Occup Ther J Res. 1990;10(6):360-366.
43. Steultjens EM, Dekker J, Bouter LM, et al. Occupational therapy for stroke patients. a systematic review. Stroke. 2003:34;3:87-676.
44. Snook JH. Spasticity reduction splint. Am J Occup Ther. 1979;33(10):648-651.
45. Stern GR. Thumb abduction splint. Physiotherapy. 1980;66(10):352.
46. Stockmeyer S. An interpretation of the approach of Rood to the treatment of neuromuscular dysfunction. Am J Phys Med. 1967;46(1):900-961.
47. Thompson-Rangel T. The mystery of the serpentine splints. Occup Ther Forum Sept. 1991;20:4-6.
48. Tubiana R, Thomine JM, Mackin E. Examination of the hand and wrist. St Louis: Mosby; 1996.
49. Tyson SF, Kent RM. Orthotic devices after stroke and other non-progressive brain lesions. Cochrane Database of Syst Rev. (1):2009. CD003694
50. Wilson D, Caldwell C. Central control insufficiencyIII. Disturbed motor control and sensation. a treatment approach emphasizing upper extremity orthoses. Phys Ther. 1978:58;3:313-320.
51. Woodson AM. Proposal for splinting the adult hemiplegic hand to promote function. In: Cromwell FS, editor. Hand rehabilitation in occupational therapy. Redding, CA: Hawthorne Press, 1988.
52. Wu SH. A belly gutter splint for proximal interphalangeal joint flexion contracture. Am J Occup Ther. 1991;45(9):839-843.
53. Zislis JM. Splinting of hand in a spastic hemiplegic patient. Arch Phys Med Rehabil. 1964;45:41-43.