chapter 10 Upper extremity function and management
After completing this chapter, the reader will be able to accomplish the following:
1. Develop evidence-based treatment plans to regain upper extremity function with functional task-related training.
2. Understand the application of adjunct treatments for the upper extremity after stroke, including treatments such as positioning, shoulder supports, electrical stimulation, biofeedback, and stretching programs.
3. Choose functional treatment activities appropriate to the level of available motor control.
4. Understand evaluation and treatment procedures for patients with symptoms of pain syndromes and implement pain prevention protocols into current treatment plans.
5. Identify the common biomechanical malalignments of the upper extremity and trunk after stroke and recognize their effect on function.
6. Prevent secondary complications such as pain, contracture, and learned nonuse.
Impaired upper extremity function is one of the most common and challenging sequelae of a stroke. The Copenhagen stroke study included 515 stroke patients, 71% of whom received occupational and physical therapy and 69% of whom had mild to severe upper extremity dysfunction on admission; all treatment plans included a focus on upper extremity function.132 Obviously, numerous hours of therapy are spent on this area, as are numerous dollars. This chapter highlights problems associated with upper extremity function after a stroke, research that has been published on upper extremity function/dysfunction after stroke, and suggested evaluation and treatment techniques that focus on acquiring functional use of the extremity and preventing pain syndromes and deformities. Readers should review the concepts in Chapters 4 to 9 and Chapters 11 and 12 for a complete overview of topics related to upper extremity function and motor control.
Overview of occupational therapy perspective
“I want to use my arm again” is a goal that occupational therapists hear from stroke survivors during almost every evaluation. For therapists to assist patients with meeting this goal, a thorough understanding of the various problems associated with upper extremity dysfunction after stroke is required. The therapist has the responsibility to stay informed of (and contribute to) the new developments in and information about upper extremity function.
Current models of motor control encompass a variety of neuromotor, biomechanical, behavioral, cognitive, environmental, and learning processes. Mathiowetz and Bass-Haugen121 have compared and contrasted the various models of motor control therapy in the past and present. Research comparing the effectiveness of various approaches is lacking. However, clearly the current motor behavior research supports a treatment technique well known to occupational therapists: the use of function-based tasks and/or task-specific or task-related training. See Chapters 4, 5, and 6.
The use of functional activities has formed the basis of occupational therapy since its inception.125 However, the complex problems that interfere with upper extremity function may require an integrated treatment approach that uses functional tasks as the intervention foundation and hands-on approaches/modalities (e.g., mobilization, soft-tissue elongation, and biofeedback) as adjuncts to intervention.
As the body of knowledge concerning motor behavior continues to grow, therapists must analyze research findings their own clinical practices critically. Burgess38 reminds “A danger in times of transition and rapid change is a distraction from basic principles. When faced with a choice between conventional and new approaches, the occupational therapist should consider the following questions: Is this treatment effective? How does it work and on what principles is it based? Is it accomplishing what is needed for this patient? Are some of the older treatment methods more solidly based, more effective, or cheaper? Are there other better ways to meet this patient’s needs?” This holds true today as new technologies are being developed in an effort to improve upper extremity outcomes after stroke. See Chapter 11.
Definitions and classifications
A review of the literature on upper extremity function reveals a consistent problem: the lack of a definition for the word function. This may be attributed to the fact that a variety of disciplines are contributing information. From an occupational therapy perspective, function refers to using the upper extremity to support engagement in meaningful occupations. The International Classification of Function of the World Health Organization is a helpful classification system that includes the following categories:
 Impairment of body systems and body structure: examples include paresis, spasticity, sensory loss, and decreased postural control
Impairment of body systems and body structure: examples include paresis, spasticity, sensory loss, and decreased postural control
 Activity limitations: dysfunction in task performance such as activities of daily living (ADL) and leisure tasks
Activity limitations: dysfunction in task performance such as activities of daily living (ADL) and leisure tasks
 Participation restrictions: factor that limits or prevents fulfillment of a role (e.g., parent or worker)195
Participation restrictions: factor that limits or prevents fulfillment of a role (e.g., parent or worker)195
Hughlings Jackson’s classification of observed symptoms after a central nervous system lesion is another system helpful for evaluating and treating the upper extremity after stroke. Jackson, a nineteenth-century neurologist, classified symptoms as positive or negative.
Positive symptoms are spontaneous, exaggerated disturbances of normal function and react to specific external stimuli. They include spasticity, increased deep tendon reflexes, and hyperactive flexion reflexes. In contrast, the negative symptoms are deficits of normal behavior or performance. Negative symptoms include loss of dexterity, loss of strength, and restricted ability to move.107,108
In the past, the major focus of therapeutic interventions was to decrease the positive symptoms associated with brain lesions. Therapists worked under the assumption that a cause-and-effect relationship existed between the two groups of symptoms. It has become clear that the alleviation of positive symptoms (e.g., spasticity) does not automatically result in an increased ability to move. Therapists therefore must take a broader view when identifying and treating upper extremity problems. A focus on only the positive symptoms (e.g., normalizing tone) does not result directly in increased function. See Chapter 6.
Activity analysis of select upper extremity tasks
The following examples illustrate the complexity of upper extremity function and should assist in the evaluation process.
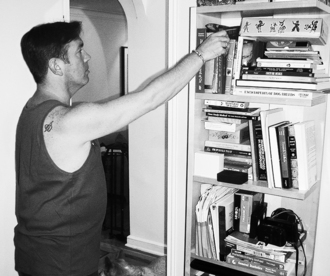
Reaching task/open chain activity
The reaching task described requires the patient to reach for a book on a shelf that is at forehead level. First, initiation of any movement pattern requires a motivational drive to perform; therefore, the activity must have an inherent purpose. The motivation behind and purpose of this activity may be to further knowledge, enhance leisure time, or pass a midterm examination. To complete this activity successfully, the patient must process appropriately the visual/perceptual information collected during the scanning process before initiating the reach pattern. Because the item is above eye level, neck extension with concurrent right and left lateral head and neck rotation and sufficient ocular range of motion (ROM) are required. A person collects a variety of visual information during visual scanning that helps identify particular characteristics of the book (e.g., call number, title, color, and size). This information is interpreted by several visual/perceptual processes (e.g., figure ground, color discrimination, and depth perception). See Chapters 16 and 18.
Before initiation of the reach pattern the lower extremities and trunk undergo several postural adjustments to provide stabilization (anticipatory reactions). The antigravity shoulder muscles prepare to bring the arm to shelf level, and the hand is prepositioned and oriented to prepare for grasping. While the reach pattern is being performed, the scapula protracts and rotates upward by the combination actions of the serratus anterior and upper and lower trapezius muscles. The rotator cuff keeps the humerus in a position biased toward external rotation and seats the head of the humerus in the glenoid fossa. The lower extremities and trunk stay active and stable during the performance of the pattern and may assist with a weight shift toward the shelves depending on the body position.
When the hand makes contact with the book, it is molded to the spine of the book, and the pattern of function is reversed (eccentrically) to return the book to the side of the body. After the person removes the book from the shelf, the grasp and pattern of skeletal muscle recruitment may be adjusted depending on the weight of the book. Although this activity pattern is preplanned based on prior experience, the book may be lighter or heavier than anticipated, so adjustments must be made in response to the feedback. (For example, attempting to pick up a supposedly full suitcase that is actually empty results in an exaggerated lifting motion that may cause a loss of balance.) While the book is being returned to the side, a variety of adjustments may have to be made to allow visualization of the cover of the book or call number (Fig. 10-1).
Weight-bearing task/closed chain activity
The weight-bearing task described requires the patient to use one arm as a postural support (i.e., extended-arm weight-bearing to support function) on a kitchen table while the other arm and hand wipe the table. As mentioned previously, motivation and purpose are required. The motivation may be hunger (so the table must be cleaned in preparation for a meal), extrinsic (e.g., visitors), or work-related (e.g., table space needed to balance the checkbook or prepare a lecture). Because the weight-bearing arm is being used as a postural support, a variety of postural adjustments occur in the arm. The weight-bearing arm is active during the task; the active skeletal muscles include (but are not limited to) the scapula muscles biased toward protraction and stabilizing, the elbow extensors, the lower extremities, and the trunk muscles. The amount of skeletal muscle activity in the arm may decrease because of fatigue, resulting in a “locked” elbow, an inactive scapula biased toward an elevated position and retraction, and the trunk inactive and “hanging” on the arm.
The arm wiping the table must stay active (closed chain with superimposed movement) and endure the entire activity if the task is going to be successful. The shoulder complex of this arm glides the hand and sponge along the table surface, so the upper extremity is supported by the environment and is moving simultaneously. The amount of force and pressure exerted on the hand depends on the demands of the task (e.g., wiping crumbs or cleaning off dried syrup). A variety of weight shifts occur during this activity, and they are affected by the size of the table and amount of pressure needed by the wiping hand to accomplish the task. The degree and variety of motor output is specific to the demands of the task.
As with all upper extremity tasks, multiple visual/perceptual processes are required for successful completion of this task. These processes are used to locate the crumbs on the table, clean both sides of the table, and determine when the task is complete (i.e., when the table is clean) (Fig. 10-2).

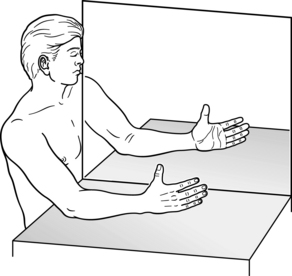
Figure 10-2 A, Using the right upper extremity as a postural support while the left upper extremity is supported by the table but moving. Intervention for the involved upper extremities should include engaging the patient in activities that use the upper extremities to support task performance. B, An alignment that fosters minimal upper extremity activity. Compare with A.
Selected evaluation tools
Evaluation tools that are standardized, reliable, and valid can be overlooked no longer. Many therapists continue to use piecemeal evaluations that do not incorporate the use of functional tasks and rely too heavily on evaluation of impairments.
Beyond validity and reliability, when choosing assessments, clinicians must consider time factors, level of motor function, the purpose of the evaluation (clinical, research, or both), and the environment in which the assessment will take place. Many available assessments such as the Fugl-Meyer Assessment only evaluate the impairment level and do not include information regarding how the upper extremity is used during daily occupations. Many use contrived or simulated functional tasks.
Motor activity log (self-report)
The Motor Activity Log is a self-report questionnaire (report by patient or family) related to actual use of the involved upper extremity outside of structured therapy time. It uses a semistructured interview format. Quality of movement (“How well” scale) and amount of use (“How much” scale) are graded on a 6-point scale. At present, there are 14, 28, and 30 item versions of the tool. Sample items include hold book, use a towel, pick up a glass, write/type, and steady myself, etc.179-181
Manual ability measure (mam-36) (self-report)
The 36-item Manual Ability Measure (MAM-36) is a new Rasch-developed, self-report disability outcome measure. It contains 36 gender neutral, common performed everyday hand tasks. The patient is asked to report the ease or difficulty of performing such items. It used a 4-point rating scale, with 1 indicating “Unable” (I am unable to do the task all by myself), 2 indicating “Very hard” (It is very hard for me to do the task and I usually ask others to do it for me unless no one is around), 3 indicating “A little hard” (I usually do the task myself, although it takes longer or more effort now than before), and 4 indicating “Easy” (I can do the task without any problem). The MAM-36 can be accessed.49 A look-up table from raw scores to converted 0-100 Rasch measures is available.48
Abilhand questionnaire (self-report)
The ABILHAND questionnaire asks clients to use a 3-point scale (0 = impossible, 2 = easy) to rate how difficult it would be to complete 23 bimanual tasks (e.g., hammering a nail, wrapping a gift, thread a needle, file nails, cut meat, peel onions, open jar, etc.). Grip strength, motricity, dexterity, and depression are significantly correlated with the ABILHAND measures.144
Assessment of motor and process skills
The therapists evaluate motor and process skills68,69 within the context of basic ADL and instrumental activities of daily living (IADL). The quality of the person’s ADL performance is assessed by rating the effort, efficiency, safety, and independence of 16 ADL motor and 20 ADL process skill items, while the person is doing chosen, familiar, and life-relevant ADL tasks. There are more than 100 tasks to choose from, thus promoting a client-centered approach to assessment. Examples of evaluated motor skills include posture, mobility, coordination, strength, reach, manipulation, grip, lifting, effort, and energy expenditure. See Chapter 21.
Arm motor ability test
The Arm Motor Ability Test (AMAT) has been used to determine the effectiveness of constraint-induced movement therapy (CIMT) and includes 13 unilateral and bilateral tasks. Sample items include tying a shoe, opening a jar, wiping up spilled water, using a light switch, using utensils, and drinking. The therapist times task performance and rates movement quality on a 6-point scale. The test is appropriate for evaluating motor skills in high-level clients with active wrist and finger extension. However, most of the AMAT activities are too difficult and frustrating for persons with little motor recovery.102,146
Wolf motor function test
The Wolf Motor Function Test has been used to document the outcomes related to CIMT and includes a variety of tasks such basic reaching tasks (e.g., lifting arm from lap to table, extending elbow with and without a weight attached) and more functional activities that involve fine motor control (e.g., picking up a pencil, turning a key in a lock). All tasks but one are unilateral and appropriate for both the dominant and nondominant arm. As many tasks do not require distal control, it is appropriate for people with a more involved upper extremity. The therapist times task performance and qualitatively grades movement.191
Chedoke arm and hand activity inventory
Chedoke Arm and Hand Activity Inventory is a functional measure with 13 items that are assessed using a 7-point quantitative scale, similar to that of the FIM instrument (e.g., 1 = total assist and 7 = independent). It yields a total raw sum of 91 (minimum score = 13) that can be converted to a percentage. Sample items include opening a jar of coffee, dialing 911, zipping a zipper, carrying a bag up the stairs, and drying back with towel.12,13
Jebsen test of hand function
The Jebsen Test of Hand Function97 includes the performance of seven test activities: writing a short sentence, turning over index cards, picking up small objects and placing them in a container, stacking checkers, simulating eating, moving empty large cans, and moving weighted large cans during timed trials. The original paper is based on data collected from 360 normal subjects and patients, including patients with hemiparesis resulting from a stroke. The mean times and standard deviations for normal subjects (with their dominant and nondominant hand) are published in the paper. The test is standardized and reliable and does not have a practice effect. Therapists must be aware that some of the tasks are simulated activities, and some tasks cannot be considered ADL tasks.
Action research arm test
The Action Research Arm Test consists of 19 items in four categories: pinch, grasp, grip, and gross movement. The test is short (approximately 10 minutes). Items are graded on a 4-point scale. Scores for each subtest range from 0 (unable to perform any task) to 6 (able to perform all six tasks). Performance is rated on a 4-point scale ranging from 0 (unable to perform) to 3 (performs normally). The test is most useful for patients with some distal function. The tasks included are contrived.117
Motor assessment scale
Developed by Carr and Shepherd, the Motor Assessment Scale44 has been found to be highly reliable, with an average interrater correlation of 0.95 and a 0.98 average test/retest correlation. This evaluation includes sections on upper arm function, hand movements, and advanced hand activities. The upper arm function section includes movement patterns without tasks; the hand sections incorporate the use of objects. Each item is scored on a 7-point scale.
Box and block test
The number of wooden blocks (2.5×2.5×2.5 cm) that can be transported from compartment of box to another in one minute is counted.120,145
Nine-hole peg test
A measure of dexterity, the Nine Hole Peg Test consists of a plastic console with a shallow round dish to contain the pegs on one end of the console and the nine-hole peg-board on the opposite end. Time taken to complete the test is measured as the patient grasps nine pegs and places them in and removes them from the holes on the console.136
Functional test for the hemiplegic/paretic upper extremity
Although this evaluation188 is based on Brunnstrom’s view that motor recovery takes place in a specific sequence, it does involve functional tasks associated with daily living. This test has been found to be highly correlated with scores on the Fugl-Meyer Assessment and requires approximately 30 minutes to administer. It consists of 17 test items arranged in seven levels according to difficulty. Examples of tasks evaluated include folding a sheet, stabilizing a jar, hooking and zipping a zipper, screwing in a light bulb, and placing a box on a shelf.
Upper extremity performance test for the elderly/test d’evaluation des membres supérieurs de personnes agées (tempa)
This test consists of four unilateral (pick up and move a jar, pick up a pitcher and pour water into a glass, handle coins, and move small objects) and five bilateral (open a jar and take a spoonful of coffee, unlock a lock and open a pill container, write on an envelope and place a stamp on it, tie a scarf around your neck, and shuffle and deal playing cards) functional tasks. It includes speed of execution and functional ratings. The functional rating is related to level of independence and uses a 4-point scale.60
Frenchay arm test
This quick test includes five items, such as hair combing with the weak arm and drinking water. Items are graded as successful or unsuccessful.87
Motricity index
This test includes a brief impairment measure of upper extremity function after stroke. Items include pinch strength, elbow flexion, and abduction.51
Rivermead motor assessment (arm section)
This text is part of a comprehensive battery and contains 15 items related to motor recovery of the arm. Sample items include protracting a shoulder girdle while supine, picking up a piece of paper from the table in front and releasing five times, cutting putty on a plate with a knife and fork, and placing string around the head and tying a bow in the back. The scores are dichotomous: success (1) or failure (0).115
Fugl-meyer assessment (upper extremity motor function)
Familiarity with this impairment-based test is helpful because the test is used in many research papers to document improvement in function. The assessment is based on the motor recovery model developed by Twitchell and on Brunnstrom’s idea that motor recovery occurs in a specific sequence of steps. Improved motor function is considered a deviation from stereotypical synergies defined by Brunnstrom in this test. The test does not involve the use of functional tasks. Sections include ROM, sensation, balance, upper extremity, and lower extremity. Items are graded on a 3-point scale.72
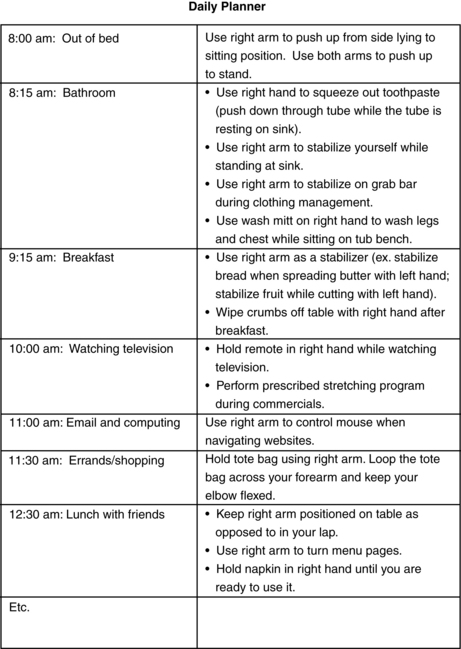
Use of the involved upper extremity to support task performance: suggestions for intervention
The foundation of occupational therapy is built on patients taking an active role in their own recovery by participating in functional activities. In the past, many therapists, while attempting to apply neurophysiological principles to treatment, have limited their use of this modality in favor of more passive techniques that are applied to the patient (e.g., brushing, icing, and neurodevelopmental treatment–based handling techniques performed separately from functional tasks). Occupational therapy now has come full circle, with the most current research on motor control supporting the use of tasks performed in context-specific situations (see Chapters 4 through 6.) Functional tasks in therapy include occupations that require upper extremity weight-bearing for postural support, reaching, carrying, lifting, grasping, and manipulating of common objects. These types of activities clearly carry over into daily life tasks and are comprehensive enough to treat a variety of problem areas. The importance of using occupation-embedded interventions as opposed to rote exercise has been established.111,198 Indeed descriptions of the most effective interventions after stroke include task specific, repetitive, intense, active, evidence-based, and function-based. Further task-specific training should be relevant to the patient and context, be randomly ordered from a practice perspective, be repetitive and involve massed practice, focus on whole task practice, and be positively reinforced (Fig. 10-3 and Table 10-1).89
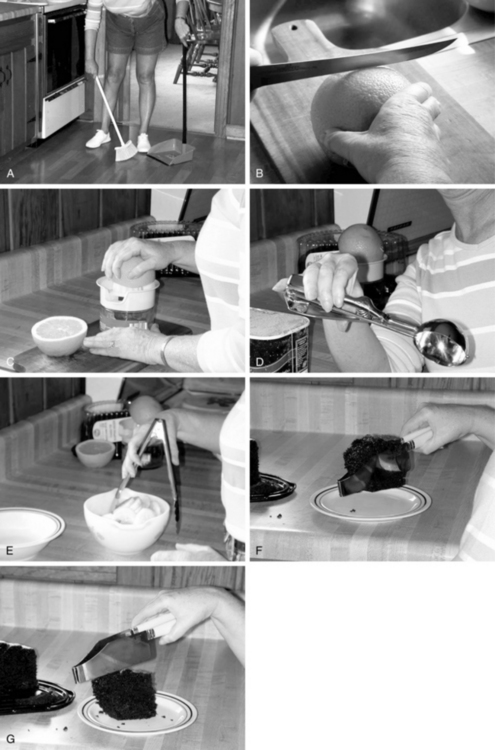
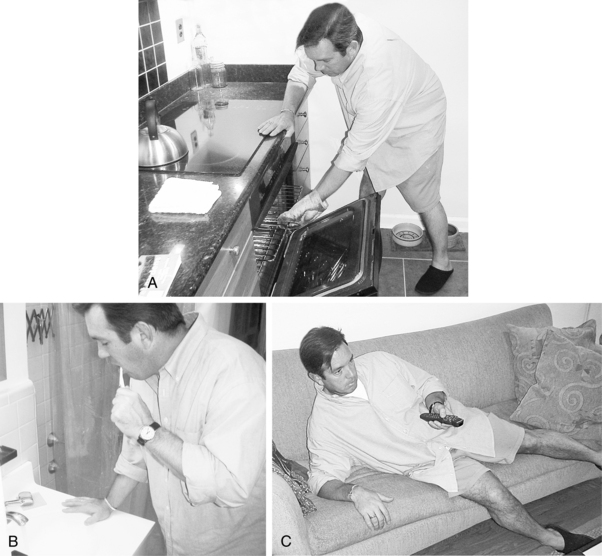
Figure 10-3 A to G, Task-oriented interventions: using the impaired upper extremity to support participation after stroke. (Courtesy of Yvette Hachtel, JD, MEd, OTR/L)
Table 10-1 Managing the Poststroke Upper Extremity Using Evidence from Systematic Reviews, Meta-analyses, and Randomized Controlled Trials
| INTERVENTION | DESIGN/SUBJECTS | CONCLUSIONS |
|---|---|---|
| Task-related/specific practice | A randomized controlled trial comparing standard care (SC), functional task practice (FTP), and strength training (ST).189 | Compared with SC participants, those in the FTP and ST groups had significantly greater increases in upper extremity function and strength, and decreased upper extremity impairment in the short-term. In the long-term, those in the FTP group benefited the most. |
| A prospective, randomized, single blind clinical trial recruited 30 stroke subjects into either an upper limb or a mobility group. All subjects received their usual rehabilitation and an additional session of task-oriented practice using a circuit class format.17 | Both groups improved significantly between pre- and posttests on all of the mobility measures, while only the upper limb group made a significant improvement on the Jebsen Test of Hand Function and Motor Assessment Scale upper arm items. | |
| A systematic review of task-oriented training after stroke.151 | “Studies of task-related training showed benefits for functional outcome compared with traditional therapies. Active use of task-oriented training with stroke survivors will lead to improvements in functional outcomes and overall health-related quality of life.” The authors recommended “creating opportunities to practise meaningful functional tasks outside of regular therapy sessions.” | |
| Double-blind randomized control trial. Intervention group (TR group) received progressive object-related reach-to-grasp training with prevention of trunk movements. Control group (C) practiced tasks without trunk restraint.126 | “TR training led to greater improvements in impairment and function compared with C. Improvements were accompanied by increased active joint range and were greater in initially more severe patients. In these patients, TR decreased trunk movement and increased elbow extension, whereas C had opposite effects (increased compensatory movements). In TR, changes in arm function were correlated with changes in arm and trunk kinematics.” | |
| An investigation of the effects of different intensities of arm and leg rehabilitation training on the functional recovery of activities of daily living (ADL), walking ability, and dexterity of the paretic arm, in a single-blind randomized controlled trial.105 | Greater intensity of leg rehabilitation improved functional recovery and health-related functional status, and greater intensity of arm rehabilitation resulted in improvements in dexterity. | |
| Constraint induced movement therapy (CIMT) | A systematic review that found 13 randomized controlled trials, 4 of which were excluded because they aimed at comparing different intensity of CIMT.26 | Findings were positive in all studies, but the minimal clinically important difference, defined as a change of at least 10% of the maximum score of the scale used, was reached only in smaller ones, which may have been influenced by patients’ characteristics. |
| A placebo-controlled trial of CIMT in patients with mild to moderate chronic motor deficit after stroke. The study compared CIMT to a placebo group that received a program of physical fitness, cognitive, and relaxation exercises for the same length of time and with the same amount of therapist interaction as the experimental group.172 | After CIMT, patients showed large to very large improvements in the functional use of their more affected arm in their daily lives. The changes persisted over the 2 years tested. Placebo subjects showed no significant changes. | |
| A prospective, single-blind, randomized, multisite clinical trial conducted at 7 U.S. academic institutions.193 | Among patients who had a stroke within the previous 3 to 9 months, CIMT produced statistically significant and clinically relevant improvements in arm motor function that persisted for at least 1 year. | |
| Modified constraint induced movement therapy (mCIMT)* | Thirty-two patients were randomized to receive mCIMT or traditional rehabilitation for three weeks.112 | In addition to improving functional use of the affected arm and daily functioning, mCIMT improved motor control strategy during goal-directed reaching. |
| This study compared a mCIMT intervention with a dose-matched control intervention that included restraint of the less affected hand and assessed for differences in motor and functional performance and health-related quality of life. N = 32.113 | Compared with the control group, the mCIMT group exhibited significantly better performance in motor function, level of functional independence, mobility of extended ADL, and health-related quality of life after treatment. | |
| A single-blinded randomized controlled trial compared mCIMT to a time-matched exercise program for the more affected arm or a no-treatment control regimen.137 | After intervention, significant differences were observed on the Action Research Arm Test and Motor Activity Log Amount of Use and Quality of Movement scales, all in favor of the mCIMT group. | |
| Twenty-six patients received either mCIMT or traditional rehabilitation for a period of 3 weeks.196 | The mCIMT group exhibited significantly greater improvements in motor function, daily function, and health-related quality of life than the traditional rehabilitation group. In addition, those in the mCIMT group perceived significantly greater percent of recovery after treatment than patients in the traditional rehabilitation group. | |
| Thirty stroke patients were randomly assigned to either an mCIMT or a control group.201 | Significant differences in favor of mCIMT were found in 6 elements of the Wolf Motor Function Test. | |
| Mental practice | A systematic review of 15 studies of mental practice focused on decreasing impairment and improving function in the poststroke upper extremity.135 | The results of the majority of the studies suggest mental practice has a positive effect on upper limb recovery at both the impairment and functional levels. However, it is unclear whether the improvements seen are retained over time, or how broad the effects are in terms of improving perceived occupational performance. |
| A randomized placebo controlled trial of mental practice of specific arm movements.139 | Those receiving mental practice showed significant reductions in affected arm impairment and significant increases in daily arm function. Those in the group receiving mental practice exhibited new ability to perform valued activities. | |
| Combined mCIMT and mental practice | A randomized trial comparing mCIMT versus mCIMT plus mental practice.138 | All subjects exhibited reductions in affected arm impairment and functional limitation. Those in the mCIMT plus mental practice group exhibited significantly larger changes on both movement measures after intervention. |
| Electromyographic (EMG) biofeedback | Subjects were randomly assigned to EMG biofeedback or placebo EMG biofeedback groups. Both treatments were applied 5 times a week for a period of 20 days. In addition, the patients in both groups received an exercise program.7 | “The results showed that there were statistically significant improvements in all variables in both groups, but the improvements in active range of motion and surface EMG potentials were significantly greater in the EMG biofeedback group at the end of the treatment.” |
| The purpose of this study was to assess electromyographic biofeedback efficacy through metaanalysis. Eight studies met the inclusion criteria (N = 192). Their average effect size was 0.81. The 95% confidence interval for the effect size was 0.5 to 1.12.161 | “The results indicate that electromyographic biofeedback is an effective tool for neuromuscular reeducation in the hemiplegic stroke patient.” | |
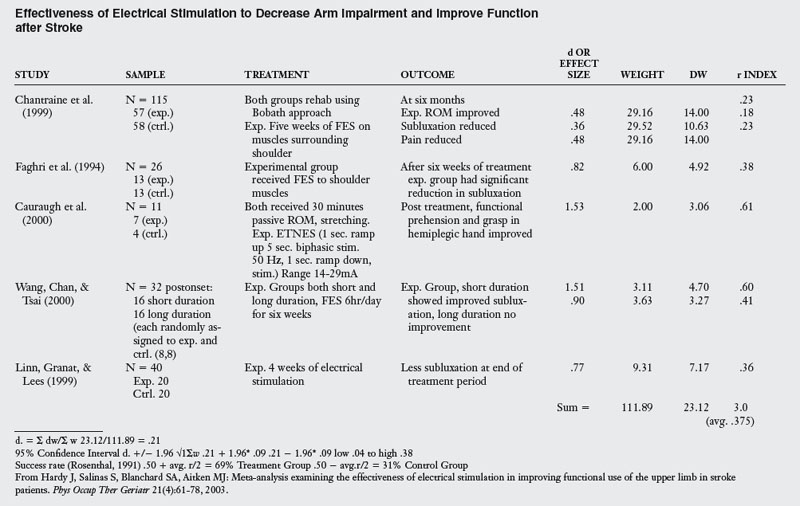
| Electrical stimulation | The meta-analysis examined the efficacy of surface electrical stimulation for the prevention or reduction of shoulder subluxation after stroke. Seven (four early and three late) trials met the inclusion criteria.3 | “Analysis found that, when added to conventional therapy, electrical stimulation prevented on average 6.5 mm of shoulder subluxation (weighted mean difference, 95% CI 4.4 to 8.6) but only reduced it by 1.9 mm (weighted mean difference, 95% CI −2.3 to 6.1) compared with conventional therapy alone. Therefore, evidence supports the use of electrical stimulation early after stroke for the prevention of, but not late after stroke for the reduction of, shoulder subluxation.” |
| A randomized trial (N= 46). The treatment group received surface neuromuscular stimulation to produce wrist and finger extension exercises. The control group received placebo stimulation over the paretic forearm.47 | “Data suggest that neuromuscular stimulation enhances the upper extremity motor recovery of acute stroke survivors. However, the sample size in this study was too small to detect any significant effect of neuromuscular stimulation on self-care function.” | |
| This meta-analysis examined the effectiveness of electrical stimulation of subluxation, shoulder pain, range of motion and functional use. The study included 5 papers with 8 data points.84 | This analysis suggests that electrical stimulation produces positive results including improving subluxation, pain, range of motion, and functional use. | |
| A systematic review of randomized trials related to poststroke shoulder pain. Four trials (a total of 170 subjects) fitted the inclusion criteria.150 | The review found no significant change in pain incidence or change in pain intensity after electrical stimulation treatment compared with control. There was a significant treatment effect in favor of electrical stimulation for improvement in pain-free range of passive humeral lateral rotation. In these studies, electrical stimulation reduced the severity of glenohumeral subluxation, but there was no significant effect on upper limb motor recovery or upper limb spasticity The authors noted that there does not appear to be any negative effects of electrical stimulation at the shoulder. | |
| EMG-triggered neuromuscular stimulation | This systematic literature search was performed to identify clinical trials evaluating the effect of electrical stimulation. The authors specifically examined the relationship between outcomes and characteristics of the stimulation. 19 clinical trials were included, and the results of 22 patient groups were evaluated.59 | “A positive effect of electrical stimulation was reported for 13 patient groups. Positive results were more common when electrical stimulation was triggered by voluntary movement rather than when non-triggered electrical stimulation was used.” The authors concluded that “triggered electrical stimulation may be more effective than non-triggered electrical stimulation in facilitating upper extremity motor recovery following stroke.” |
| This meta-analysis assessed the effect of EMG-triggered neuromuscular stimulation on arm and hand functions, specifically the focus was on wrist extension.25 | The meta-analysis revealed a significant overall mean effect size (delta=0.82, S.D.=0.59). These improved wrist extension motor capabilities findings support EMG-triggered neuromuscular stimulation as an effective poststroke protocol. | |
| A randomized trial to assess the efficacy of EMG-triggered neuromuscular stimulation (EMG-stim) in enhancing upper extremity motor and functional recovery of acute stroke survivors.71 | “Subjects treated with EMG-stim exhibited significantly greater gains in Fugl-Meyer (27.0 vs 10.4; p = .05), and FIM (6.0 vs 3.4; p = .02) scores compared with controls.” Data suggest that EMG-stim enhances the arm function of acute stroke survivors.” | |
| Bilateral upper extremity training | A systematic review and meta-analysis of 11 studies of bilateral arm training after stroke.168 | “These findings indicate that bilateral movement training was beneficial for improving motor recovery post-stroke.” “These meta-analysis findings indicate that bilateral movements alone or in combination with auxiliary sensory feedback are effective stroke rehabilitation protocols during the sub-acute and chronic phases of recovery.” |
| A randomized, single-blind training study comparing bilateral (practice of bilateral symmetrical activities) to unilateral training (performed the same activity with the affected arm only). The activities consisted of reaching-based tasks that were both rhythmic and discrete.170 | Both groups had significant improvements on the Motor Status Scale and measures of strength. The bilateral group had significantly greater improvement on the Upper Arm Function scale. Both bilateral and unilateral training are efficacious for moderately impaired chronic stroke survivors. Bilateral training may be more advantageous for proximal arm function. | |
| A randomized controlled trial. Subjects randomized to distributed CIMT, bilateral arm training (BAT), or a control intervention of less specific but active therapy.114 | BAT may uniquely improve proximal upper limb motor impairment. In contrast, distributed CIMT may produce greater functional gains for the affected upper limb in subjects with mild to moderate chronic hemiparesis. | |
| Mirror therapy | A randomized trial to evaluate the effects of mirror therapy on upper extremity motor recovery, spasticity, and hand-related functioning of inpatients with subacute stroke.199 | In our group of subacute stroke patients, hand functioning improved more after mirror therapy, in addition to a conventional rehabilitation program, compared with a control treatment immediately after 4 weeks of treatment and at the 6-month follow-up, whereas mirror therapy did not affect spasticity. |
| A randomized trial to evaluate the effect of a therapy that includes use of a mirror (MT) to simulate the affected upper extremity with the unaffected upper extremity early after stroke compared to a control (CT).62 | “In the subgroup of 25 patients with distal plegia at the beginning of the therapy, MT patients regained more distal function than CT patients. Furthermore, across all patients, MT improved recovery of surface sensibility. Neither of these effects depended on the side of the lesioned hemisphere. MT stimulated recovery from hemineglect.” | |
| Strengthening interventions for weakness | Systematic review with meta-analysis of randomized trials. 21 trials were identified and 15 had data that could be included in the meta-analysis.2 | Strengthening interventions increase strength, improve activity, and do not increase spasticity. These findings suggest that strengthening programs should be part of rehabilitation after stroke. |
| A review of poststroke strengthening trials.141 | “While the number of studies is limited, emerging evidence suggests that persons with poststroke weakness can improve strength through resistance exercise in the absence of negative side effects, including exacerbation of hypertonia. Moreover, these improvements in strength appear to transfer to functional improvements. Still, many unresolved issues remain. The potential for strength training to improve the overall outcomes of rehabilitation for persons with poststroke hemiplegia warrants further investigation.” | |
| Positioning | A randomized trial to determine the efficacy of positioning the affected shoulder in flexion and external rotation to prevent contracture shortly after stroke.5 | At least 30 minutes a day of positioning the affected shoulder in external rotation should be started as soon as possible for stroke patients who have little activity in the upper arm. |
* Treatment protocols vary greatly and are discussed in Table 10-3.
Task-oriented reaching and manipulation
The events leading up to a simple voluntary movement such as reaching for a glass of water involve multiple complex processes. Ghez74 classifies these processes as follows. First, the person needs to identify the glass and its position in space. This first step encompasses a variety of visual and perceptual processes. Second, the person needs to select a plan of action to bring the glass to the mouth. Ghez points out that this step involves specifying which body parts are needed and in which direction they should move. To do this, the person must evaluate the location of the glass in relation to the position of the hand and body. The information collected allows the motor system to determine the appropriate trajectory of the hand. The last step is the execution of the response. Multiple commands are sent to the motor neurons specifying the temporal sequence of muscle activation, the forces to be developed, the changes in joint angles, the orientation of the hand to fit the glass, and the coordination of the shoulder with the distal arm to ensure that the glass will be grasped on contact and immediately. Multiple problems can interfere with these three steps, including the issues discussed in the previous section, visual dysfunction, and praxis deficits.
Two components of upper extremity function have been described by Jeannerod95,96: the transportation component, which includes the trajectory of the arm between the starting position and the object, and the manipulation component, which is the formation of grip by combined movements of the thumb and the index finger during arm movement.
In her study of reaching deficits in subjects with left hemiparesis, Trombly177 used kinematic analysis and electromyography to document impairments in voluntary arm movements. Her analysis demonstrated that the ability to reach smoothly and with coordination was significantly less in the impaired arms than in the unimpaired arms. The continuous movement strategy used during reaching activities was lost, movement time was longer, peak velocity occurred earlier, and indications of weakness were present.
In a follow-up study, Trombly176 documented the observed improvements in her subjects’ reaching abilities. Her findings indicated that the amplitude of peak velocity improved over time. The level of muscular activity did not improve, but the discontinuity of movements decreased. From her findings, Trombly hypothesized that therapy that allows relearning of sensorimotor relationships is warranted for some patients. She stated that the “level and pattern of muscle activity of these subjects depended on the biomechanical demands of the task rather than any stereotypical neurological linkages between muscles.”
From a treatment perspective, research by Trombly and Wu178 concluded that “Goal-directed reach enabled persons with stroke to display characteristics typical of reach to a target by persons who have not had a stroke better than reaching out in space. These findings support the occupational therapy practice of using objects in a functional context to improve coordinated movement. However, the nature of the objects to be used requires further study.”
Van Vliet and colleagues185 studied subjects in the early months after a stroke. The subjects were able to improve their reaching kinematics during a three- to four-week period; they progressed toward normal performance. Providing the subjects with a meaningful task (e.g., drinking from a cup) helped them perform the reach-to-grasp movement.
Jeannerod96 stated that “Formation of the finger grip during the action of grasping a visual object involves two main functional requirements, the fulfillment of which will determine the quality of the grasp. First, the grip must be adapted to the size, shape, and use of the object to be grasped. Second, the relative timing of the finger movements must be coordinated with that of the other component of prehension by which the hand is transported to the spatial location of the object.” Jeannerod observed that finger posturing anticipates the real grasp and occurs during transportation of the hand. This shaping of the hand is a mechanism independent of the manipulation itself. If treatment programs focused on improved function of the upper extremity are to be designed, then they must include a variety of common objects with different shapes, sizes, and textures to affect this reaching component.
Exner,66 who defined in-hand manipulation as the process of adjusting objects being grasped in the hand, developed a classification system to assist the therapist in activity choice, despite the system not being standardized on stroke survivors (Box 10-1 outlines Exner classification system).
Box 10-1 Exner Classification of Manipulation Tasks
Shift
Movement occurs at the finger and thumb pads by alternating thumb and radial finger movements (e.g., moving a coin near the distal interphalangeal joints farther out to the pads of the fingers).
Wu, Trombly, and Lin198 demonstrated that using material-based occupation (e.g., picking up a pen and preparing to write one’s name) enhanced quality of movement performance more than imagery-based occupation (e.g., pretending to pick up a pen and preparing to sign one’s name) and exercise (e.g., moving the arm forward). Their data suggested that material-based occupation resulted in decreased reaction time, movement time, and movement units. Although this study was performed on normal subjects, they inferred that material-based occupation may be used to elicit efficient and economical preprogrammed movement for performing tasks.
In a study of fine motor coordination training, Neistadt133 examined the effects of constructing puzzles and performing kitchen activities on fine motor coordination in a group of brain-injured men. Her results demonstrated that the subjects in the functional meal preparation group showed significantly greater improvements in dominant hand dexterity, which is used for picking up small objects, than the subjects in the tabletop puzzle activity group. Her findings suggested that functional activities are more effective (not to mention more meaningful) than tabletop activities for fine motor coordination training in the brain-injured population.
Sietsema and colleagues163 studied brain-injured patients engaged in rote exercise tasks and occupationally embedded tasks (e.g., reaching out to control a computer game). Their subjects had “mild to moderate spasticity” on evaluation. Their results indicated that the game elicited significantly more ROM during the reach pattern performance than the rote exercise. Their study supported the hypothesis that occupationally embedded interventions promote increased performance. The authors hypothesized that the game provided motivating feedback that enhanced performance.
At this point, research has confirmed that the demands and goals of the task influence motor output.198 For example, the characteristics of an item being carried across a kitchen influence factors such as how fast a person moves, whether one or two hands are used to grip the object, how close to the body the item is carried, and how stable the arms are held. In daily life, there are many examples of the ways in which movement in daily activities is influenced by the environment (e.g., carrying empty ice trays or full trays, a half-glass of wine or a full cup of coffee, one paper plate or a stack of china plates).
Rosenbaum and Jorgensen153 have demonstrated that the goal of the task influences motor output. Their subjects were asked to reach for a cylinder and stand it on one end or the other. Depending on the goal of the task (e.g., which side they were to stand the cylinder on), subjects reached with a pronated or supinated grasp pattern. Box 10-2 provides sample activities used to retrain reach patterns. See Chapters 4 and 5.
Box 10-2 Activities to Retrain Reach Patterns
 With the patient positioned in a supine posture, the therapist supports the weight of the distal extremity with a handhold position. The patient attempts to hold various positions and/or to follow the movements of the therapist’s hand. This activity is appropriate for the early motor recovery stage. The degrees of freedom are minimized (with trunk and scapula being supported by the supine posture), and the therapist eliminates the weight of the patient’s extremity, maximizing the potential for skeletal muscle recruitment. This activity is easily taught to family members.
With the patient positioned in a supine posture, the therapist supports the weight of the distal extremity with a handhold position. The patient attempts to hold various positions and/or to follow the movements of the therapist’s hand. This activity is appropriate for the early motor recovery stage. The degrees of freedom are minimized (with trunk and scapula being supported by the supine posture), and the therapist eliminates the weight of the patient’s extremity, maximizing the potential for skeletal muscle recruitment. This activity is easily taught to family members.
 Position the patient in side lying with the patient’s arm supported on a table. Practice reaching in multiple directions for various objects or towards various targets while the weight of the limb is supported on the table.
Position the patient in side lying with the patient’s arm supported on a table. Practice reaching in multiple directions for various objects or towards various targets while the weight of the limb is supported on the table.
 The patient stands or sits in front of a table with a hand resting on a dust cloth on top of the table. The patient focuses on gliding the hand across the table. The critical pattern consists of humeral flexion, scapula protraction, and elbow extension. The cloth reduces friction, and the weight of the arm is supported on the table (e.g., reach with support).
The patient stands or sits in front of a table with a hand resting on a dust cloth on top of the table. The patient focuses on gliding the hand across the table. The critical pattern consists of humeral flexion, scapula protraction, and elbow extension. The cloth reduces friction, and the weight of the arm is supported on the table (e.g., reach with support).
 The patient is seated, and objects are positioned on the floor in front of patient. The patient reaches for objects on the floor. This downward reach pattern enhances scapula protraction, humeral flexion, and elbow extension by nature of the position of the objects. As the patient gains more control, the objects are raised up to the midshank level, then the knee level, and then the waist level, systematically increasing the motor demands of the task.
The patient is seated, and objects are positioned on the floor in front of patient. The patient reaches for objects on the floor. This downward reach pattern enhances scapula protraction, humeral flexion, and elbow extension by nature of the position of the objects. As the patient gains more control, the objects are raised up to the midshank level, then the knee level, and then the waist level, systematically increasing the motor demands of the task.
 The patient is engaged in the foregoing reach patterns while therapist provides resistance to the functional pattern by tying an elastic band around the palm. The therapist is behind the patient holding the opposite end of the band and is able to grade the level of resistance.
The patient is engaged in the foregoing reach patterns while therapist provides resistance to the functional pattern by tying an elastic band around the palm. The therapist is behind the patient holding the opposite end of the band and is able to grade the level of resistance.
 During the reach activities, the demands of the distal components of movement are systematically increased (e.g., increasing manipulation requirements). Examples include pouring water and opening jars.
During the reach activities, the demands of the distal components of movement are systematically increased (e.g., increasing manipulation requirements). Examples include pouring water and opening jars.
Weight-bearing to support function
The use of weight-bearing tasks has long been advocated in patients after stroke. Upper extremity weight-bearing has been suggested anecdotally for achieving a variety of therapeutic goals, including inhibiting hypertonus by moving the body proximally against the distal upper extremity55 and stimulating upper extremity extension during protective responses.19 Brouwer and Ambury37 concluded that upper extremity weight-bearing normalizes corticospinal facilitation of motor units in stroke patients. They hypothesized that the mechanism responsible for their results was a sustained increase in motor cortical excitability through augmented afferent input.
McIllroy and Maki122 and Marsden, Merton, and Morton118 documented that if the upper extremity is used as a postural support (e.g., during weight-bearing), postural responses to the movements of the opposite arm occur throughout the weight-bearing upper extremity and to other perturbations of posture. Their paper also demonstrated that postural responses from the triceps only occurred when the hand was in contact with a firm object.
Although from a neurophysiological perspective, the effect of weight bearing on upper extremity control (e.g. the “normalization of tone” and “inhibition of spasticity”) remains controversial and unproven, the use of weight-bearing patterns is still necessary for treating the upper extremity after a stroke if the goal of treatment is to improve functional performance. Examples include using the more affected upper extremity in a weight-bearing pattern and as a postural support while manipulating clothing during toileting activities or to enhance participation in IADL (e.g., using the more affected extremity as a postural support during activities requiring standing such as doing the laundry or preparing a meal).
Therapists also can use weight-bearing activities to address impairments that interfere with function. The problem of soft-tissue shortening in the long flexors can be prevented or reversed by bearing weight on extended wrists with extended digits to maintain or increase tissue length. If evaluation reveals that weakness in the extremity is having a limiting effect on function, the therapist can use extended-arm weight-bearing activities to strengthen the triceps and scapula musculature if the weight-bearing activities are performed in appropriate alignment and the weight-bearing pattern remains active during the activity.
To ensure appropriate alignment, the therapists should avoid severe internal rotation, forced elbow extension, and an inactive trunk in patients.156 During weight-bearing activities, maintenance of palmar hand arches is important for maintaining biomechanical alignment and enhancing active patterns. The points of contact between the weight-bearing surface and the hand include the thenar eminence, hypothenar eminence, metacarpal heads, and palmar surfaces of the phalanges.100 The arch should be maintained so that therapists can insert a finger between the web space and the first metacarpal head and slide it under the hand until they make contact with the hypothenar eminence.
Although the more affected arm is in a weight-bearing position, the less involved extremity should be engaged in activities that promote weight shifting in all directions (Fig. 10-4). Weight-bearing activities can be performed by the forearm or an extended arm, depending on the demands of the task and the level of available motor control. See Table 10-1 for a review of evidence related to task related training.
Goals, task choices, and interventions to promote function
The following goals are examples of treatment activities for different levels and combinations of functional recovery. Using goals and treatments interchangeably ensures a task-specific approach to intervention. These examples should not be interpreted as progression in recovery. Although previous assumptions were that proximal recovery of abilities precedes distal recovery of abilities, this is not always the case. The following activities are graded by increasing the degrees of freedom (e.g., increasing the number of planes of movement that are controlled and integrating hand use), the level of antigravity control, and the objects used in the task. An important note is that the cognitive demands of the task have a substantial effect on the level of upper extremity function. Readers should not consider this list hierarchical. For example, weight-bearing is not a prerequisite to reaching, because the neurological and biomechanical demands are different. Patients need to be engaged in a variety of tasks that require the use of the upper extremity in a variety ways and engaged in task-specific training.
Focused attention on the more affected upper extremity (no active movement)
 Patient washes upper extremity during upper body bathing activities.
Patient washes upper extremity during upper body bathing activities.
 Patient attends to upper extremity while rolling by passively guiding upper extremity across trunk when preparing to roll.
Patient attends to upper extremity while rolling by passively guiding upper extremity across trunk when preparing to roll.
 Patient stretches arm correctly by reaching to floor and maintaining this position after difficult tasks result in arm posturing.
Patient stretches arm correctly by reaching to floor and maintaining this position after difficult tasks result in arm posturing.
 Patient’s family demonstrates proper guarding techniques for a mobile patient.
Patient’s family demonstrates proper guarding techniques for a mobile patient.
 Patient’s caretaker demonstrates proper positioning of patient in bed.
Patient’s caretaker demonstrates proper positioning of patient in bed.
 Patient’s caretaker demonstrates proper technique to transfer patient from one surface to another (e.g., not by lifting under the axillas).
Patient’s caretaker demonstrates proper technique to transfer patient from one surface to another (e.g., not by lifting under the axillas).
Forearm weight-bearing as a stabilizer
 Patient stabilizes checkbook with upper extremity while writing checks.
Patient stabilizes checkbook with upper extremity while writing checks.
 Patient stabilizes cutting board with upper extremity during meal preparation.
Patient stabilizes cutting board with upper extremity during meal preparation.
 Patient holds magazine open with upper extremity while doing crossword puzzle.
Patient holds magazine open with upper extremity while doing crossword puzzle.
Using upper extremity for assistance during transitions
 Patient uses upper extremity for assistance with assuming sitting position from side-lying position.
Patient uses upper extremity for assistance with assuming sitting position from side-lying position.
 Patient uses upper extremity to push up into standing position.
Patient uses upper extremity to push up into standing position.
 Patient uses upper extremity to reach back before sitting.
Patient uses upper extremity to reach back before sitting.
 Patient uses upper extremity to lower trunk to mat when assuming supine posture from sitting posture.
Patient uses upper extremity to lower trunk to mat when assuming supine posture from sitting posture.
Incorporating upper extremity as a postural support when sitting and standing (extended-arm weight-bearing with stabilized hands-on support surface)
 Patient uses upper extremity to assist with lateral shifting while relieving pressure.
Patient uses upper extremity to assist with lateral shifting while relieving pressure.
 Patient stabilizes upper body with affected upper extremity while wiping and dusting table or ironing with less affected upper extremity.
Patient stabilizes upper body with affected upper extremity while wiping and dusting table or ironing with less affected upper extremity.
 Patient uses more affected upper extremity as a stabilizer on a grab bar while manipulating clothing with less affected upper extremity during toileting.
Patient uses more affected upper extremity as a stabilizer on a grab bar while manipulating clothing with less affected upper extremity during toileting.
 Patient stabilizes upper body with upper extremity while grooming at sink.
Patient stabilizes upper body with upper extremity while grooming at sink.
Weight-bearing with superimposed motion (e.g., hand does not leave support surface but slides and pulls objects)
 Patient irons and/or dusts with more affected upper extremity while stabilizing upper body with less affected upper extremity.
Patient irons and/or dusts with more affected upper extremity while stabilizing upper body with less affected upper extremity.
 Patient uses affected upper extremity to lock wheelchair brakes with brake extensions.
Patient uses affected upper extremity to lock wheelchair brakes with brake extensions.
 Patient uses more affected upper extremity to smooth out laundry.
Patient uses more affected upper extremity to smooth out laundry.
 Patient uses more affected upper extremity to wax and buff car.
Patient uses more affected upper extremity to wax and buff car.
 Patient uses more affected upper extremity to push shopping cart or rolling walker.
Patient uses more affected upper extremity to push shopping cart or rolling walker.
 Patient uses affected upper extremity to apply body lotion.
Patient uses affected upper extremity to apply body lotion.
 Patient uses affected upper extremity to wash a mirror or window.
Patient uses affected upper extremity to wash a mirror or window.
Antigravity shoulder movements without hand function
 Patient initiates roll with more affected upper extremity.
Patient initiates roll with more affected upper extremity.
 Patient lifts more affected upper extremity into shirt sleeve.
Patient lifts more affected upper extremity into shirt sleeve.
 Patient lifts more affected upper extremity to countertop.
Patient lifts more affected upper extremity to countertop.
 Patient pushes drawer closed with back of more affected hand.
Patient pushes drawer closed with back of more affected hand.
 Patient turns off light switch with side of more affected hand.
Patient turns off light switch with side of more affected hand.
Initial hand movement (static grasp) with limited shoulder movement (in lap or on work-surface activities)
 Patient adjusts shirt cuff with more affected upper extremity.
Patient adjusts shirt cuff with more affected upper extremity.
 Patient holds book in lap with both hands while reading.
Patient holds book in lap with both hands while reading.
 Patient stabilizes fruits or vegetables with affected hand while cutting with less affected hand.
Patient stabilizes fruits or vegetables with affected hand while cutting with less affected hand.
 Patient holds shopping bag with more affected upper extremity during ambulation.
Patient holds shopping bag with more affected upper extremity during ambulation.
 Patient holds washcloth with more affected upper extremity and washes mid to lower body.
Patient holds washcloth with more affected upper extremity and washes mid to lower body.
Reach patterns with hand activity
 Patient picks up sock from floor with more affected upper extremity.
Patient picks up sock from floor with more affected upper extremity.
 Patient retrieves item from under sink cabinet with more affected upper extremity.
Patient retrieves item from under sink cabinet with more affected upper extremity.
 Patient opens medicine cabinet with more affected upper extremity.
Patient opens medicine cabinet with more affected upper extremity.
 Patient retrieves item from top shelf of medicine cabinet with more affected upper extremity.
Patient retrieves item from top shelf of medicine cabinet with more affected upper extremity.
 Patient drinks out of a cup with more affected upper extremity.
Patient drinks out of a cup with more affected upper extremity.
 Patient holds coins in affected palm and slides them to finger tips.
Patient holds coins in affected palm and slides them to finger tips.
 Patient types 15 words per minute with both upper extremities.
Patient types 15 words per minute with both upper extremities.
 Patient signs check with more affected upper extremity.
Patient signs check with more affected upper extremity.
 Patient picks up and reorients paperclip with affected upper extremity.
Patient picks up and reorients paperclip with affected upper extremity.
A benchmarking outcomes system is suggested to track and communicate progress (Box 10-3). Table 10-2 provides further suggestions for choosing tasks for a variety of levels of function.
Box 10-3 The Australian Therapy Outcome Measures (AusTOMs) for Occupational Therapy: Upper Limb Use
The ability to use one or both upper limbs during activities of daily living include gross and fine manipulative skills and hand and arm use. This may comprise lifting and moving a heavy object while walking; picking up and using a pencil; grasping, using, and releasing objects such as keys, buttons, or taps; throwing and catching an object; and pushing, pulling, twisting, and turning objects.
Scoring: You are able to use half-points.
Impairment of either structure or function (as appropriate to age)
Impairments are problems in body structure (anatomical) or function (physiological or psychological) as a significant deviation or loss. Impairments may be mental (cognitive/perceptual), sensory, cardiovascular/respiratory, digestive/metabolic/endocrine systems, neurological movement, or musculoskeletal. A variety of impairments may affect ability to use upper limbs (if only one upper limb is affected, then rate the severity of impairments affecting this limb; if both are affected, then rate both). Considering all the impairments an individual may have that affect upper limb use, assess the level of severity of these. Base your assessment on typical presentation of the individual’s impairment(s) in an appropriate environment.
0 The most severe presentation of impairment/s., e.g., very dense hemiplegia, severe fixed contractures, unbearable pain, or most severe presentation of cognitive impairment
1 Severe presentation of impairment/s, e.g., dense hemiplegia, severely restricted range of movement, severe pain, or severe cognitive impairment
2 Moderate/severe presentation of impairment/s, e.g., moderate to severe hemiplegia, moderate to severely restricted range of movement, moderate to severe pain, or moderate to severe cognitive impairment
3 Moderate presentation of impairment/s, e.g., moderate hemiplegia, moderately restricted range of movement, moderate pain, or moderate cognitive impairment
4 Mild presentation of impairment/s, e.g., mild hemiplegia, mildly restricted range of movement (e.g., morning stiffness), mild pain, or mild cognitive impairment
5 No impairment/s of structure or function. All structures and functions intact. No pain. Affected arm equal to unaffected arm or norms.
Activity limitation (as appropriate to age)
Activity limitation results from difficulty in the performance of an activity. Activity is the execution of a task by an individual. Assess the individual’s ability to use both upper limb/s for tasks and what the client can actually do, e.g., if the client can do all tasks independently with one arm, then score as 5.
0 Does not use upper limb/s. Unable to lift, move, manipulate, use upper limb/s. Full assistance required.
1 Severe limitation in using upper limb/s. Maximum assistance required. Enough function to prevent further injury or to minimize functional restrictions, e.g., shoulder can be slightly abducted to enable clothes to be put on. Client completes some of the movement required for activity.
2 Moderate/severe limitation in using upper limb/s. Needs a person to give some hands on assistance, or requires constant verbal prompting. Can initiate gross motor movements, but difficulty with end of range movements and fine motor control, e.g., consistently spills contents of cup; functional pencil grip but unable to write or form legible letters, can draw. Able to use upper limb for gross function only, such as stabilizing/or able to perform fine grasp but cannot manage gross movements.
3 Moderate limitation in using upper limb/s. Requires verbal cueing, supervision or set-up. Generally, gross movements intact, poor fine motor/dexterity, e.g., reaching for clothesline independently, requiring assistance to manipulate peg on line. Inconsistent completion, e.g., picks up half-full lightweight cup with handles with occasional spills; illegible writing.
4 Mild limitation in using upper limb/s. Able to do but lacking in quality, or extra time required, e.g., clumsy, unreliable grasp/release, reduced carrying capacity, weaker grasp, mildly reduced coordination and dexterity, reduced reach, decreased efficiency and fluency of movement, e.g., holds and raises standard full cup with external support (table, other arm); completes legible writing although may display decreased quality/slow speed/reduced fluency.
5 No limitation in using upper limb/s. Able to lift, move, manipulate, use hand and arm to complete functional tasks bilaterally or unilaterally. May or may not use aids or adaptive equipment such as prosthesis/orthosis, or enlarged/lightweight handle. Completes upper limb activities in reasonable time.
You must also make a rating of the client’s participation Restriction and Distress/Wellbeing.
From Unsworth CA, Duncombe D: AusTOMs for occupational therapy, ed 2, Melbourne, 2007, La Trobe University. Copyright © 2007 by La Trobe University. www.latrobe.edu.au/austoms
Table 10-2 Suggestions for Categorizing Upper Extremity Tasks
| CATEGORY | TASKS |
|---|---|
| No functional use | Teach shoulder protection |
| Self range of motion | |
| Positioning | |
| Postural support/weight-bearing (forearm or extended arm) | Bed mobility assist |
| Support upright function (work, leisure, activities of daily living) | |
| Support during reach with opposite hand | |
| Stabilize objects | |
| Supported reach (hand on work surface) | Wiping a table |
| Ironing | |
| Polishing | |
| Sanding | |
| Smoothing out laundry | |
| Applying body lotion | |
| Washing body parts | |
| Vacuuming | |
| Locking wheelchair brakes | |
| Reach | Multiple possibilities to engage upper extremity into activities of daily living, leisure, and mobility; grade tasks by height/distance reached, weight of object, speed, and accuracy |
Constraint-induced movement therapy (traditional and modified protocols)
The term learned nonuse was coined by Taub.171 The learned nonuse phenomenon originally was identified in primate studies and later was applied to chronic stroke patients. With deafferentation of a single forelimb of a monkey, the animal would not use that limb in an unrestricted (free) environment. The monkey’s initial attempts to use the limb resulted in failures (e.g., dropping food, losing balance, and falling). The monkeys in this study soon found that they could function in their environment with three limbs instead of four. Continued attempts to use the affected limb led to repeated failures at attempted tasks; the effect was suppression of any desire to use that limb. The monkeys learned not to use the limb to avoid failure, which masked any future recovery of limb function. Taub and colleagues171 pointed out that in a free situation, the monkeys did not learn that they could regain use of the forelimb as they recovered function. When the intact forelimb was restrained, the monkeys were forced to use the affected side. This technique converted a useless limb into one capable of function.
Taub171 hypothesized that the nonuse or limited use of an affected upper extremity in human beings after stroke could in some cases result from a similar phenomenon of learned suppression. To test this hypothesis, Taub171 studied nine patients with chronic (i.e., greater than one year after stroke) hemiplegia. To be included in this study, patients had to demonstrate the ability to extend the metacarpophalangeal and interphalangeal joints at least 10 degrees, extend the wrist 20 degrees, and walk without an assistive device. They had to have grossly intact cognitive function, no excess spasticity, be right-arm dominant, and be less than 75-years-old.
Patients were assigned to a control or an experimental group. The experimental group underwent forced-use/CIMT in which the intact limb was placed in a sling and resting-hand splint. The restraint was worn at all times during waking hours except when toileting, when napping, and at times when balance might be compromised. The restraint was worn for 14 days. Each weekday, patients received therapy and were given a variety of tasks—such as eating with utensils, playing ball, playing Chinese checkers and dominoes, writing, and sweeping—to perform with the paretic limb for six hours throughout the day.
The treatment of the control group focused on increasing attention to the paretic limb. This group was told that they had more potential in their extremities than they were using. Therapists performed passive ROM activities, and patients performed ROM activities daily for 15 minutes. The affected limb was not given any training for active movement.
Each group was evaluated before and after intervention with a variety of arm function evaluations and a self-reported Motor Activity Log. The experimental group had significantly faster mean performance speeds from the evaluations, increased quality of movement, and an increased ability to use the extremity in ADL. These improvements were reevaluated two years later; they were at least maintained if not increased. Although the comparison group made subtle gains after intervention, the gains were not retained for the follow-up evaluation. Taub and colleagues171 concluded that the motor ability of stroke patients who met their inclusion criteria could be increased significantly by the interventions effective for overcoming learned nonuse.
Wolf and colleagues192 researched forced-use treatment in 25 chronic hemiplegic and stroke patients with minimal to moderate extensor muscle function. The CIMT program lasted for two weeks, with the intact limb being restrained during waking hours. The authors noted significant changes in performance of 19 of the 21 tasks that were evaluated, with most changes persisting for one year after the study. The authors concluded that learned nonuse does occur in select patients with neurological deficits and that this behavior can be reversed through application of a CIMT paradigm.
Van der Lee and colleagues182 completed an observer-blinded randomized clinical trial with 66 chronic stroke patients who were randomized to two weeks of CIMT or a comparison of equally intensive bimanual training based on two weeks of neurodevelopmental therapy. One week after the last treatment session, the authors found a significant difference in effectiveness in favor of CIMT group compared with the neurodevelopmental therapy group, after correction for baseline differences, on the Action Research Arm Test and the Motor Activity Log amount of use score. One-year follow-up effects were observed only for the Action Research Arm Test. The authors also found that the differences in treatment effect for the Action Research Arm Test and the Motor Activity Log amount of use scores were clinically relevant for patients with sensory disorders and hemineglect, respectively.
The EXCITE trial193 was a prospective, single-blind, randomized, multisite study and included 222 patients with stroke. Subjects were randomized to either customary care or constraint-induced therapy. Constraint-induced therapy consisted of two components applied over a two-week period; subjects performed intense practice of functional tasks using the affected hand for six hours per day plus subjects reduced use of the unaffected hand by covering it with a mitt for at least 90% of waking hours. The trial found significantly positive results that were maintained in the long term. Outcome measures included:
 The Wolf Motor Function Test, which showed a 52% reduction in time to complete its tasks, significantly better than the 26% reduction found in those in the customary care group.
The Wolf Motor Function Test, which showed a 52% reduction in time to complete its tasks, significantly better than the 26% reduction found in those in the customary care group.
 The Motor Activity Log, which showed a 76% increase in quantity and a 77% increase in quality of arm use, each significantly better than the 43% and 41% respective increases found in the customary care group.
The Motor Activity Log, which showed a 76% increase in quantity and a 77% increase in quality of arm use, each significantly better than the 43% and 41% respective increases found in the customary care group.
Dromerick, Edwards, and Hahn63 questioned whether a CIMT program could be implemented in the acute stroke population (two weeks after stroke) and whether this intervention was more effective than traditional upper extremity interventions (control group) during the acute period. The research team enrolled 23 subjects in a pilot randomized, controlled trial that compared CIMT with traditional therapies. Treatment plans were designed to make sure that patients in both groups received equivalent time and intensity of treatment directly, and an occupational therapist supervised the program. The subjects received routine interdisciplinary stroke rehabilitation, except for the CIMT that occurred during the regularly scheduled occupational therapy sessions. Individualized and circuit-training techniques were used in both groups. All subjects received study treatment for two hours per day, five days per week, for two consecutive weeks. Twenty subjects completed the trial. The CIMT group had significantly higher scores on the Action Research Arm Test and pinch subscale scores. Differences in the mean grip, grasp, and gross movement subscale scores of the Action Research Arm Test did not reach statistical significance. ADL performance was not significantly different between groups. No subject withdrew because of pain or frustration. The authors concluded that CIMT during acute rehabilitation is feasible. Furthermore, CIMT was associated with less arm impairment at the end of the trial.
Page and colleagues140 examined the feasibility and efficacy of a modified CIMT protocol administered on an outpatient basis. Their protocol was developed to be more consistent with therapy scheduling and reimbursement patterns, in other words, more user friendly and feasible from the therapist’s perspective. They examined six patients who were in a subacute stage of stroke recovery and who exhibited learned nonuse. The patients were assigned to one of three groups; two patients received half-hour physical and occupational therapy sessions three times a week for 10 weeks while they simultaneously had their unaffected arms and hands restrained five days per week during five hours identified as times of frequent use; two patients received regular therapy, and two control patients received no therapy. Outcomes were measured by the Fugl-Meyer Assessment of motor recovery, the Action Research Arm Test, the Wolf Motor Function Test, and the Motor Activity Log. Patients receiving modified CIMT exhibited substantial improvements on the Fugl-Meyer Assessment, Action Research Arm Test, the Wolf Motor Function Test and reported increases in amount and quality of use of the limb based on the Motor Activity Log. Patients receiving traditional or no therapy exhibited no improvements. The author concluded that modified CIMT may be an efficacious method of improving function and use of the affected arms of patients exhibiting learned nonuse. See Table 10-3 for CIMT protocols.
Table 10-3 Tested Constraint-Induced Movement Therapy Protocols
| TRADITIONAL PROTOCOL | MODIFIED PROTOCOLS |
|---|---|
| The EXCITE trial defined the intervention as: “Participants in the intervention group were taught to apply an instrumented protective safety mitt and encouraged to wear it on their less-impaired upper extremity for a goal of 90% of their waking hours over a 2-week period, including 2 weekends, for a total of 14 days. On each weekday, participants received shaping (adaptive task practice) and standard task training of the paretic limb for up to 6 hours per day. The former is based on the principles of behavioral training that can also be described in terms of motor learning derived from adaptive or part-task practice. Standard task practice is less structured (i.e., repetition of tasks is not conducted as individual trials of discrete movements); it involves functional activities performed continuously for a period of 15 to 20 minutes (e.g., eating, writing).” 193 | Page and colleagues137 described the following protocol consisting of 2 components. “The first component consisted of half-hour, one-on-one sessions of more affected arm therapy occurring 3 days per week during a 10-week period. This component included shaping in which operant conditioning was applied in such a way that subjects received positive verbal encouragement to more fully perform selected motor skills with their more affected arm. Shaping was applied with 2 or 3 upper-limb activities (e.g., writing, using a fork) chosen by the subjects with help from their therapist. In the second component of the mCIT intervention, during the same 10-week period, subjects’ less affected arms were restrained every weekday for 5 hours identified as a time of frequent arm use, as identified by the subjects with assistance from the therapist. Their arms were restrained using a cotton hemi-sling, while their hands were placed in mesh, polystyrene-filled mitts with Velcro straps around the wrist.” Lin and colleagues112 defined their protocol as “restraint of the less affected limb combined with intensive training of the affected limb for 2 hours daily 5 days per week for 3 weeks and restraint of the less affected hand for 5 hours outside of the rehabilitation training.” |
| Sterr and colleagues167 defined their protocol as 14 consecutive days; constraint of unaffected hand for a target of 90% of waking hours with 3 hours of shaping training with the affected hand per day. To note they concluded that: “The 3-hour CIMT training schedule significantly improved motor function in chronic hemiparesis, but it was less effective than the 6-hour training schedule.” |
In addition to the apparent functional improvements in the select group of patients who are appropriate for a trial of CIMT, researchers have demonstrated that CIMT produces long-term alteration in brain function. This is the first documented cortical-level change associated with a therapy-induced improvement in the rehabilitation of movement after neurological injury. Liepert and colleagues110 investigated whether CIMT could produce treatment-induced plastic changes/reorganization of the motor cortex in the human brain. Using focal transcranial magnetic stimulation, the authors mapped cortical motor output area of a hand muscle on both sides in 13 stroke patients in the chronic stage of their illness before and after a 12-day-period of CIMT. The authors found the following:
 Before treatment, the cortical representation area of the affected hand muscle was significantly smaller than the contralateral side.
Before treatment, the cortical representation area of the affected hand muscle was significantly smaller than the contralateral side.
 After treatment, the muscle output area in the affected hemisphere was significantly enlarged, corresponding to a greatly improved motor performance of the paretic limb.
After treatment, the muscle output area in the affected hemisphere was significantly enlarged, corresponding to a greatly improved motor performance of the paretic limb.
 Shifts of the center of the output map in the affected hemisphere suggested the recruitment of adjacent brain areas.
Shifts of the center of the output map in the affected hemisphere suggested the recruitment of adjacent brain areas.
 In follow-up examinations up to six months after treatment, motor performance remained at a high level.
In follow-up examinations up to six months after treatment, motor performance remained at a high level.
 At follow-up, the cortical area sizes in the two hemispheres became almost identical, representing a return of the balance of excitability between the two hemispheres toward a normal condition.
At follow-up, the cortical area sizes in the two hemispheres became almost identical, representing a return of the balance of excitability between the two hemispheres toward a normal condition.
Taub and colleagues171 summarized by stating that if the “neural substrate for a movement is destroyed by CNS injury, no amount of intervention designed to overcome learned nonuse can be successful in helping recover lost function. However, many stroke patients . . . have considerably more motor ability available than they utilize. The suppression of this additional motor capacity is set up by unsuccessful attempts at movement in the acute poststroke phase . . . increased motor activity should then become increasingly possible, but the suppression of movement remains unabated and inhibits use of the limb. However, if individuals are correctly motivated to use this unexpressed ability, they will be able to do so.” See Table 10-1 for a review of evidence related to constraint induced movement therapy (Box 10-4). See Chapter 6.
Box 10-4 Summary of Constraint-Induced Movement Therapy
 Use to counteract learned nonuse. Hypothesized causes of learned nonuse include therapeutic interventions implemented during the acute period of neurological suppression after stroke, an early focus on adaptations to meet functional goals, negative reinforcement experienced by the patients as they unsuccessfully attempt to use the affected limb, and positive reinforcement experienced by using the less involved hand and/or use of successful adaptations.
Use to counteract learned nonuse. Hypothesized causes of learned nonuse include therapeutic interventions implemented during the acute period of neurological suppression after stroke, an early focus on adaptations to meet functional goals, negative reinforcement experienced by the patients as they unsuccessfully attempt to use the affected limb, and positive reinforcement experienced by using the less involved hand and/or use of successful adaptations.
 Motor inclusion criteria. Control of the wrist and digits is necessary to engage in this type of intervention. Current and past protocols have used the following inclusion criteria: 20 degrees of extension of the wrist and 10 degrees of extension of each finger; or 10 degrees extension of the wrist, 10 degrees abduction of the thumb, and 10 degrees extension of any two other digits; or able to lift a wash rag off a table using any type of prehension and then release it. It is clear that distal function (particularly wrist and digit extension) is a critical factor in being a candidate for the intervention. Therapists should focus on these movements early and intensely. Potential interventions to regain this motor control included electrical stimulation, mental practice, and activities that require distal extension such as reaching for large objects.
Motor inclusion criteria. Control of the wrist and digits is necessary to engage in this type of intervention. Current and past protocols have used the following inclusion criteria: 20 degrees of extension of the wrist and 10 degrees of extension of each finger; or 10 degrees extension of the wrist, 10 degrees abduction of the thumb, and 10 degrees extension of any two other digits; or able to lift a wash rag off a table using any type of prehension and then release it. It is clear that distal function (particularly wrist and digit extension) is a critical factor in being a candidate for the intervention. Therapists should focus on these movements early and intensely. Potential interventions to regain this motor control included electrical stimulation, mental practice, and activities that require distal extension such as reaching for large objects.
 Main therapeutic factor. Massed practice and shaping of the affected limb during repetitive functional activities appears to be the therapeutic change agent. “There is thus nothing talismanic about use of a sling or other constraining device on the less-affected limb.”173
Main therapeutic factor. Massed practice and shaping of the affected limb during repetitive functional activities appears to be the therapeutic change agent. “There is thus nothing talismanic about use of a sling or other constraining device on the less-affected limb.”173
 Activity choices and therapist’s interventions. Select tasks that address the motor deficits of the individual patient, assist the patient to carry out parts of a movement sequence if the patient incapable of completing the movement on is his or her own at first, providing explicit verbal feedback and verbal reward for small improvements in task performance, use modeling and prompting of task performance, use tasks that are of interest and motivating to the patient, ignore regression of function, and use tasks that can be quantified related to improvements.
Activity choices and therapist’s interventions. Select tasks that address the motor deficits of the individual patient, assist the patient to carry out parts of a movement sequence if the patient incapable of completing the movement on is his or her own at first, providing explicit verbal feedback and verbal reward for small improvements in task performance, use modeling and prompting of task performance, use tasks that are of interest and motivating to the patient, ignore regression of function, and use tasks that can be quantified related to improvements.
 Outcome measures. The Motor Activity Log (actual use outside of structured therapy or “real-world use”), Arm Motor Ability Test, Wolf Motor Function Test, and the Action Research Arm Test have been used to document outcomes.
Outcome measures. The Motor Activity Log (actual use outside of structured therapy or “real-world use”), Arm Motor Ability Test, Wolf Motor Function Test, and the Action Research Arm Test have been used to document outcomes.
 Cortical reorganization. Constraint-induced movement therapy is the first rehabilitation intervention demonstrated to induce changes in the cortical representation of the affected upper limb.
Cortical reorganization. Constraint-induced movement therapy is the first rehabilitation intervention demonstrated to induce changes in the cortical representation of the affected upper limb.
 The continued rigorous research that has been and continues to be carried out to demonstrate the effectiveness/efficacy of constraint-induced movement therapy should be used as a gold standard for other rehabilitation interventions that are used traditionally (e.g., neurodevelopmental therapy) but have little or no research support.
The continued rigorous research that has been and continues to be carried out to demonstrate the effectiveness/efficacy of constraint-induced movement therapy should be used as a gold standard for other rehabilitation interventions that are used traditionally (e.g., neurodevelopmental therapy) but have little or no research support.
 Based on available evidence, constraint-induced movement therapy appears to be an effective intervention for stroke survivors who have learned nonuse and who fit the motor inclusion criteria.
Based on available evidence, constraint-induced movement therapy appears to be an effective intervention for stroke survivors who have learned nonuse and who fit the motor inclusion criteria.
Managing inefficient and ineffective movement patterns
Being unable to move effectively and therefore unable to interact with the environment is one of the most devastating sequelae of stroke. The loss of the ability to move effectively is a negative stroke symptom.
The movement patterns of stroke survivors have long been discussed in the literature. Controversy continues over the nature of these patterns. These movement patterns have been described as reflex based, a release of abnormal synergies, the result of reversed inhibition or the release of lower patterns of activity from higher inhibitory control, and as learned patterns of movement. Mathiowetz and Bass-Haugen121 point out that more contemporary models of motor control describe patterns developing after central nervous system damage as results of attempts to use remaining resources to achieve occupational performance. They give the example of a typical flexor pattern (scapula retraction, internal rotation, elbow/wrist/digit flexion) in the upper extremity; the pattern can stem from factors other than spasticity, such as the inability to recruit appropriate muscles, weakness, soft-tissue tightness, and perceptual deficits.
Carr and Shepherd42 state that “muscles that are held persistently in a shortened position not only develop contracture but also appear ‘easier’ for the patients to activate. . . . In the stroke patient such activity appears to become habitual, certain muscle groups, apparently those whose mechanical advantages are greatest (because of their shortened length), contracting persistently to the disadvantage of others.” The therapist can observe this phenomenon if a patient is reaching out to a target. Many patients have difficulty with the protraction, elbow extension, and wrist and digit extension patterns of this task. If the therapist observes the patients who have been in a resting posture (e.g., seated in a wheelchair) for a prolonged time, the shortened muscles include the retractors, elbow flexors, and wrist and digit flexors.
Ada and colleagues1 hypothesize that muscle weakness or paralysis effectively immobilize the upper limb, which results in soft-tissue contracture. The immobility causes length-associated changes in muscles, and persistent positioning results in contracture. These changes in the upper limb result in compensatory movements that generate strong neural connections after frequent repetition, ensuring that the compensatory or adaptive movement patterns become learned rather than more effective and efficient.
A Russian neurologist, Nicoli Bernstein, emphasized a early task-oriented view of motor performance and introduced the concept that purposeful movement is organized to solve motor problems and the concept of degrees of freedom.158 He hypothesized that the principal problem faced by the central nervous system was the large number of joints and muscles in the human body and the infinite combinations of muscle action. For example, the upper extremity has multiple degrees of freedom if the number of planes through which each joint moves are combined. When contemplating the combinations of degrees of freedom in the trunk, scapula, and shoulder to the hand, it becomes evident that task of controlling them is phenomenal. Bernstein states that “The coordination of a movement is the process of mastering redundant degrees of freedom of the moving organ, that is, its conversion to a controllable system.”158 Bernstein views motor control as a person’s ability to coordinate kinematic linkages that limit degrees of freedom. See Chapter 5.
Flinn70 uses the example of gymnasts learning a new maneuver to apply the concept of degrees of freedom to a task. Gymnasts limit the degrees of freedom in the task by holding some joints rigid while focusing on one specific body part (e.g., foot placement). Although the gymnasts initially may appear stiff, as they become able to control more degrees of freedom, the stiffness disappears and movement relaxes. This example can be applied to learning how to roller-blade, ice-skate, or perform a new swimming stroke. Sabari158 discusses a patient with hemiplegia who does not dissociate the pelvis from the lumbar spine or scapula from the thorax, which may be an effort to decrease the degrees of freedom.
With this concept in mind, many of the ineffective movement patterns observed in patients can be attributed to attempts to control the degrees of freedom. Therapists need to consider this during treatment planning when choosing activities. The degrees of freedom must be controlled carefully by stabilizing or eliminating use of some of the joints and therefore decreasing the number of joints involved (e.g., supporting the distal extremity on a table or substituting flat-hand stabilization for a hand grasp).70 Gillen76,77 has demonstrated a variety of methods to improve task performance in clients with central nervous system dysfunction by manipulating the degrees of freedom via positioning, splinting, movement retraining, and equipment. Further research is required with the stroke population.
Many of the inefficient movement patterns in stroke survivors may result from attempting tasks beyond their level of motor control (Fig. 10-5). Many therapists have watched patients with newly developed motor control proudly show how they can “lift their arm.” Of course, the resulting movement is a stereotypical pattern used by stroke survivors. Mathiowetz and Bass-Haugen121 suggest that the use of these movement patterns is evidence of attempts to use remaining systems to complete tasks. They give the example of a patient with weak shoulder flexors trying to lift an arm. The patient flexes the elbow when trying to raise the arm because this movement strategy shortens the lever arm and makes shoulder flexion easier. This phenomenon can be observed in those with other diagnoses that result in proximal weakness (Fig. 10-6).
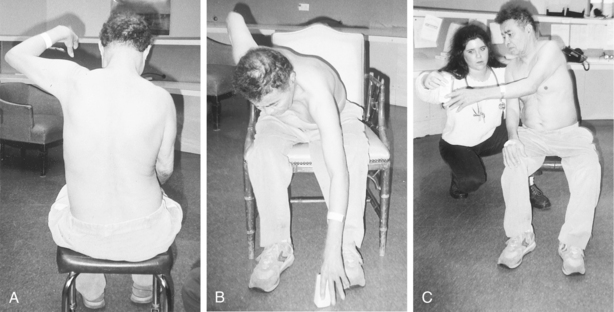
Figure 10-5 A, When asked to reach, this patient uses a stereotypical flexor pattern. Note trunk lateral flexion, scapula adduction, humeral abduction, and distal flexion. B, When the position of the activity is changed to correspond with the available motor control, and the patient is given a goal (e.g., “Pick up the bottle”), movement pattern is more effective and efficient. C, Another position change of same activity results in forward reach with less impact of compensations seen in A. The patient reaches with wrist extension, and his hand is prepositioned for successful task completion. The purpose of the activity drives motor output.
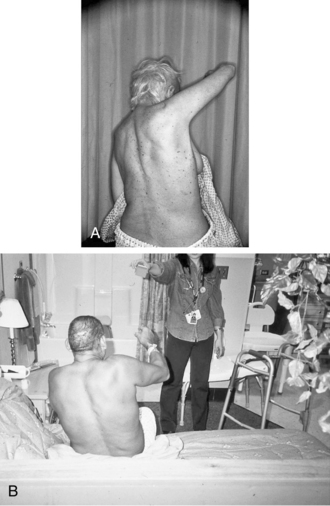
Figure 10-6 Compensatory movements from proximal weakness. A, This person’s is status post left brain damage resulting in right sided weakness including right scapula instability. Compensatory strategies used to lift her arm include lateral trunk flexion, trunk rotation, scapula adduction and elevation, and elbow flexion. These compensatory movement strategies act to decrease the degrees of freedom, provide proximal stability, and shorten the lever arm of the upper extremity. This person has relatively preserved elbow extension strength, which she cannot use during this movement as it will create a longer lever arm and a loss of control. In the recent past, this movement pattern was attributed to abnormal flexor tone placing the treatment focus on decreasing tone in the antagonistic muscle groups (i.e., elbow flexors). A more current treatment approach includes interventions related to proximal strengthening and practice of graded reach patterns ( i.e., a focus on the weak agonists). B, This man is using very similar compensatory movements as the woman in A, although his diagnosis is a right rotator cuff tear. The inefficient and ineffective movement patterns and the compensatory movements are secondary to proximal weakness.
Based on these concepts, the roles of the occupational therapist in treating inefficient and ineffective upper extremity patterns are the following:
 To use skills of activity analysis to guide patients’ participation in functional upper extremity tasks that correspond to their level of motor control
To use skills of activity analysis to guide patients’ participation in functional upper extremity tasks that correspond to their level of motor control
 Through this process, to enable patients to interact with the environment using their more affected upper extremity
Through this process, to enable patients to interact with the environment using their more affected upper extremity
 To use evaluation skills to determine which impairments (e.g., loss of postural control, weakness, pain, or a combination of components) related to upper extremity function are blocking improvements in occupational performance (e.g., ADL, IADL, work, and leisure)
To use evaluation skills to determine which impairments (e.g., loss of postural control, weakness, pain, or a combination of components) related to upper extremity function are blocking improvements in occupational performance (e.g., ADL, IADL, work, and leisure)
 To provide function-based activities that focus on improving the identified problem area in an effort to improve task performance
To provide function-based activities that focus on improving the identified problem area in an effort to improve task performance
 To provide opportunities to use available motor control throughout the day. Strategies include using devices that unweight the weak upper extremity so that movement can be accessed (Fig. 10-7), providing bedside and home-based activity programs as opposed to only exercise programs, and explicitly teaching stroke survivors how the upper extremity should be used throughout the course of the day to support participation (Fig. 10-8).
To provide opportunities to use available motor control throughout the day. Strategies include using devices that unweight the weak upper extremity so that movement can be accessed (Fig. 10-7), providing bedside and home-based activity programs as opposed to only exercise programs, and explicitly teaching stroke survivors how the upper extremity should be used throughout the course of the day to support participation (Fig. 10-8).

Figure 10-7 Suspension arm sling. Unweighting the upper extremity may promote increased use during the day. The therapist must consider ways in which the patient can move and use the upper extremity outside of therapy. Caution: When evaluating patients using this device, the therapist must make sure that the movement is being generated by the upper extremity as opposed to swinging the arm by moving the trunk.
In terms of treatment, Mathiowetz and Bass-Haugen121 suggest that therapists help the patients “find the optimal strategy for achieving functional goals.” Goals can be achieved by altering the task requirements, altering the environmental context, and by guiding remediation of the component deficits that interfere with functional performance. The most powerful tools occupational therapists have for intervention are functional activities. Although functional activities have formed the basis of treatment since the profession was developed, only recently has the true impact of functional tasks been evaluated in this area of intervention (Fig. 10-9). See Chapter 4.
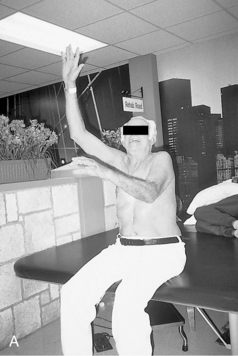



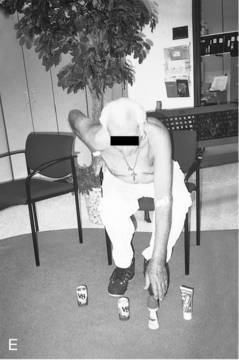

Figure 10-9 Reaching activities used to challenge available motor control appropriately. A, When attempting to lift both arms, this man uses an ineffective and inefficient movement pattern. He recruits his available scapula elevators, elbow flexors, trunk extensors, and head/neck extensors. Although it may appear that he lacks elbow extension or that his elbow flexors are “spastic” or “overactive,” muscle testing in supine yields a grade of 4 out of 5 for all elbow musculature. His lack of ability to use elbow extension in this movement may indicate an attempt to shorten the lever arm and control the degrees of freedom. B and C, Using leisure and work tasks that are more appropriate to this man’s level of motor control. Both activities are considered supported reach because the hand is in contact with the work surface. Note that the upper extremity patterns are more effective and efficient. D, The therapist provides graded physical assist to complete the task as increased biomechanical demands are made using the incline of the car. E and F, Grading the reaching in space activity using gravity to make the task progressively more difficult.
Selected adjunct interventions used with a task-oriented approach
Mental practice/imagery
The use of imagery in treatment has received an increasing amount of support in the literature. Using imagery and mental practice has been shown to do the following:
 Activate the cortical representation and musculature the correlates with the imagined movements
Activate the cortical representation and musculature the correlates with the imagined movements
Yue and Cole202 proposed a method for increasing skeletal muscle strength. Healthy subjects were separated into three groups: those receiving imagining training (i.e., training in which the person imagines a muscle is contracting but is not activating the muscle), those receiving contraction training, and a control group. Training resulted in a maximum voluntary contraction force increase of 22% in the imagining group, 30% in the contraction group, and 3.7% in the control group. This study demonstrated that strength increases can be achieved without muscle activation. Early strength increases appear to result from practice efforts on central motor programming. This study adds to the increasing evidence that the neural origin of strength increases before muscle hypertrophy.
In an early study focused on improving upper extremity function after stroke, Page139 hypothesized that imagery use combined with traditional occupational therapy could enhance motor recovery in patients with upper extremity hemiparesis. He provided eight chronic stroke patients with a four-week course of occupational therapy and imagery (a 20-minute audio tape that consisted of relaxation followed by cognitive visual images related to the upper extremity being used in weight-bearing tasks and functional tasks that were practiced in occupational therapy). This group was compared with eight controls that received only occupational therapy. He concluded that the patients who received occupational therapy and imagery had significantly more improved function as measured by the upper extremity section of the Fugl-Meyer Assessment. Since then, multiple studies have documented the effectiveness of this adjunctive intervention. See Table 10-1 for a review of evidence related to mental practice (Box 10-5).
Box 10-5 Summary: Using Mental Practice to Improve Upper Extremity Function after Stroke
 During mental practice, an internal representation of the movement is activated and the execution of the movement repeatedly mentally simulated, without physical activity, within a chosen context. It is used for the goal-oriented improvement or stabilization of a given movement.33 It is cognitive rehearsal of a motor act or task.94
During mental practice, an internal representation of the movement is activated and the execution of the movement repeatedly mentally simulated, without physical activity, within a chosen context. It is used for the goal-oriented improvement or stabilization of a given movement.33 It is cognitive rehearsal of a motor act or task.94
 Provides opportunity to promote repetitive task practice
Provides opportunity to promote repetitive task practice
 Most commonly, the mental practice intervention is administered via audiotape. The audiotapes consist of a few minutes of relaxation and focusing followed by several minutes of mental practice of tasks such as turning pages in a book, drinking from a cup, writing, etc. The length of the audiotapes have varied from approximately 10 to 20 minutes.
Most commonly, the mental practice intervention is administered via audiotape. The audiotapes consist of a few minutes of relaxation and focusing followed by several minutes of mental practice of tasks such as turning pages in a book, drinking from a cup, writing, etc. The length of the audiotapes have varied from approximately 10 to 20 minutes.
 Consistent and positive outcomes have been documented, including decreased upper extremity impairment, increased upper extremity function, and increase in everyday use of the limb outside of structured therapy.135
Consistent and positive outcomes have been documented, including decreased upper extremity impairment, increased upper extremity function, and increase in everyday use of the limb outside of structured therapy.135
 Data from psychophysical, neurophysiological, and brain imaging studies support the existence of a similarity between executed and imagined actions.94
Data from psychophysical, neurophysiological, and brain imaging studies support the existence of a similarity between executed and imagined actions.94
Electromyographic biofeedback
Electromyographic (EMG) biofeedback shows promise and should be studied further for its potential use in treating upper extremity dysfunction after stroke. Biofeedback is provided by electronic instruments that measure and give information about neuromuscular or autonomic activity in the form of auditory or visual feedback signals.
Tries’ review175 of the literature included a variety of rationales for integrating this noninvasive modality, including training voluntary inhibition of spastic muscles and restoring muscle balance, into an upper extremity program. Tries175 outlined specific techniques for scapula mobility and stability, humeral rotation, integrating scapular and humeral rotation with a forward reach pattern, and reinforcement of functional patterns in the elbow, forearm, and hand.
Tries175 presented a case study outlining the applications of biofeedback for a left-sided hemiplegic patient. Her case study illustrated that despite sensory, cognitive, and perceptual impairments, this patient had significant clinical upper limb functional improvements when combining EMG biofeedback and traditional occupational therapy.
Greenberg and Fowler80 compared kinesthetic biofeedback (feedback information pertaining to actual movement of a body part rather than the activity of muscle fibers) to conventional occupational therapy. Their results indicated that kinesthetic biofeedback was equally as therapeutic as but no more effective than conventional occupational therapy for increasing elbow extension in hemiplegic subjects.
Crow and colleagues53 studied two groups (a group receiving biofeedback and a control group) of 20 patients. The patients were studied before and after six weeks of treatment and during a follow-up visit six weeks later. Although the groups did not differ significantly before treatment, the biofeedback group improved significantly on arm-function evaluations. At the six-week follow-up, the beneficial effects were discovered not to have persisted in the experimental group.
Schleenbaker and Mainous161 concluded from their meta-analysis that biofeedback is an effective tool in neuromuscular reeducation for executing ADL. The use of EMG biofeedback warrants further investigation into its use as an adjunct tool to enhance upper extremity function in select patients with hemiparesis. See Table 10-1 for a review of evidence related to EMG biofeedback.
Electrical stimulation
Electrical stimulation has been used in poststroke upper extremity rehabilitation for many years. Potential uses have included reduction of shoulder subluxation, reduction of pain, improved motor control, and increasing use of the involved extremity. In general, the effects of electrical stimulation have been the most consistent at improving limb impairments such as ROM and reducing pain. The effects on function and ADL have received less attention and have been inconsistent. See Table 10-1 and Table 10-4 for an evidenced-based review of electrical stimulation.
Electromyographic-triggered electrical stimulation
Electrical stimulation can be triggered by voluntary movement or nontriggered. EMG-triggered stimulation detects underlying muscle activity when it reaches a threshold level prior to providing the stimulation. The stroke survivor must voluntarily activate the correct muscles prior to the stimulation facilitating the motor response. This type of stimulation assures that the intervention is not passive in nature. Triggered electrical stimulation may be more effective than nontriggered electrical stimulation in facilitating upper extremity motor recovery following stroke.59 This intervention has been shown to be effective at improving wrist extension, a key movement to be considered a candidate for some task oriented approaches such as CIMT. See Table 10-1 for an evidence-based review of EMG-triggered electrical stimulation.
Bilateral training
Recently, bilateral training (i.e., patients practice identical activities with both upper limbs simultaneously) has been proposed as a strategy to improve upper limb control and function post stroke.130a The theory and rationale as to why the intervention may be effective has been described as follows: “Control of bilaterally identical synchronous movement appears to occur centrally through bilaterally distributed neural networks linked via the corpus callosum and involving cortical and subcortical areas. These networks indicate a common facilitatory drive to both motor cortices thought to lead to tight temporal and spatial coupling of limb movement observed during bilaterally identical synchronous voluntary movement. Beneficial effects of bilateral training in stroke are assumed to arise from this coupling effect in which the nonparetic limb provides a template for the paretic limb in terms of movement characteristics, facilitating restoration of movement.”129 Stoykov and Corcos169 further reviewed neural mechanisms mediating bilateral training including recruitment of the ipsilateral corticospinal track, increased control from the contralesional hemisphere, and a normalization of inhibitory mechanism.
Although some findings have been inconsistent, a recent meta-analysis and randomized controlled trials have demonstrated improvement. Protocols vary but typically use either functional tasks or repetitive arm movements. This technique has been combined with auditory rhythmic cuing and neuromuscular stimulation. Some research has concluded that the technique may be more beneficial for those with proximal limb involvement. See Tables 10-1 and 10-5 for an evidence-based review of bilateral training. See Box 10-6 for a sample protocol.
Table 10-5 Characteristics of Each Study Used in the Meta-Analysis by Stewart and Colleagues168
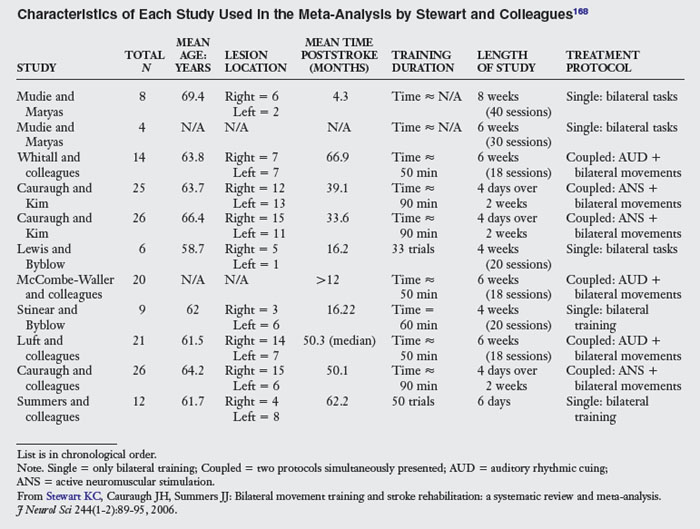
Box 10-6 Example of Bilateral Training Protocol
| TASK PROTOCOL | |
|---|---|
| UNILATERAL TREATMENT ACTIVITIES | BILATERAL TREATMENT ACTIVITIES |
From Stoykov ME, Lewis GN, Corcos DM: Comparison of bilateral and unilateral training for upper extremity hemiparesis in stroke, Neurorehabil Repair 23(9):945-953, 2009.
Mirror therapy
A relatively new intervention, this intervention appears to be cost-efficient and is able to be done independently. Yavuzer and colleagues199 describe the intervention as “During the mirror practices, patients were seated close to a table on which a mirror (35×35 cm) was placed vertically. The involved hand was placed behind the mirror and the noninvolved hand in front of the mirror. The practice consisted of nonparetic-side wrist and finger flexion and extension movements while patients looked into the mirror, watching the image of their noninvolved hand, thus seeing the reflection of the hand movement projected over the involved hand. Patients could see only the noninvolved hand in the mirror; otherwise, the noninvolved hand was hidden from sight. During the session patients were asked to try to do the same movements with the paretic hand while they were moving the nonparetic hand” (Fig. 10-11). See Table 10-1 for an evidence-based review of mirror training.