chapter 26 Seating and wheeled mobility prescription
After completing this chapter, the reader will be able to accomplish the following:
1. Understand the seating system and mobility system evaluation process.
2. Appreciate the difference between seating for rest and seating for activity performance.
3. Implement a treatment plan and identify the goals of the mobility device and seating and positioning system.
4. Appreciate the pros and cons of different mobility bases and seating system components.
5. Understand the influence of the seating system on carryover of treatment goals.
6. Appreciate the importance of the team process throughout the evaluation and fitting/delivery process.
7. Understand the importance of fitting and training with the recommended seating system and mobility device.
The statistics from the National Stroke Association indicate that stroke is the leading cause of serious adult disability in the United States.12 Despite advances in rehabilitation and treatment approaches, many individuals have difficulty with mobility and performance of activities of daily living (ADL). An appropriate seating system and mobility base is essential to maximize each client’s potential to achieve the upmost independence and safety with ADL. Consequently, it is important for a therapist to develop a working knowledge of assistive technology. Assistive technology is an umbrella term that includes seating and wheeled mobility, including manual and power wheelchairs, electronic aids to daily living (formerly known as environmental control units), computer access including workstation setup, and augmentative and alternative communication devices.
This chapter provides a general introduction and then focuses on the basic principles of seating and positioning, the evaluation process, the fitting/delivery and training process, and the features of various seating system products and mobility devices. Although the emphasis is on the seating and wheeled mobility process specific to persons with a stroke, many of these principles are appropriate for use with all individuals with disabilities who have impaired functioning and disability.
The terms client and individual with disability are used interchangeably throughout the chapter for appropriate semantics. These terms consistently refer to the same person.
The wheelchair and seating system provision process is a collaborative process that begins with a client interview and ends with fitting, training, and follow-up with the recommended wheelchair and seating system. A team approach throughout this process is essential to ensure achievement of safety and the client’s goals. The ideal wheelchair and seating system team consists of the client; health care practitioners such as a medical doctor, an occupational and/or physical therapist, and a speech pathologist (as needed); the caregiver and/or significant other; and an assistive technology supplier. The client is the central person in the wheelchair and seating system process, and the client’s goals are given the highest priority.
If a client can communicate his or her needs and has the cognitive functioning to participate in decision-making, then the therapist’s role is to empower him or her, through education, to be more active in the decision-making process. If a client has cognitive changes that limit his or her ability to function and be involved in the decision-making process, then he or she is still central; however, increased attention may be given to the caregiver’s needs and goals.
In the past 35 years, numerous changes have occurred in the health care industry. These changes were primarily at the environment level and include societal attitudes and expectations of persons with disabilities, rehabilitation service provision, manufacturer production of durable medical equipment, reimbursement policies, and system changes that include the development of authorities and organizations to organize, control, and monitor assistive technology services. Due to these changes in the wheelchair industry, increased emphasis is on the client taking a more active role in medical care, increased expectations of returning to a previous level of activity and function, minimization of deformities and secondary complications, actual evaluation of trial equipment, and the certification of a group of therapists and suppliers with a basic wide-range knowledge base of seating system and mobility device evaluation and provision.
Societal attitudes and expectations of persons with disabilities
For the past 35 years, individuals with disabilities have been lobbying for their needs and rights and have been relatively successful with the passage of several laws. The Americans with Disabilities Act has played a major role at the International Classification of Functioning, Disability and Health (ICF)6 activities and participation level to increase access to transportation and public places. This increase in environmental accessibility has enabled many individuals with disabilities to pursue their education, employment, and leisure interests to become more active, productive members of society. These changes have fueled the wheelchair manufacturing industry to develop and provide appropriate equipment to meet these more active lifestyles.
Rehabilitation services
The provision of rehabilitation services has changed drastically regarding length of stay on rehabilitation units and knowledge required to appreciate the variety of wheelchair and seating system options. Initially, clients had sufficient time in rehabilitation programs to adjust to the changes in their bodies and reach their full potential before they received a wheelchair and integrated into their discharge environment, preferably home. Today, because of the influence of traditional insurance funding limitations, clients are discharged from rehabilitation units once they are medically stable, have demonstrated restoration gains, and have a support system in place to enable them to be relatively safe with their basic ADL. As a result, therapists are forced to look at a permanent seating system early to ensure that it will facilitate functional restoration and minimize the risk for increased deformity and secondary complications.
Years ago an overall one-size-fits-all philosophy prevailed and a limited number of wheelchair and seating system options were available for individuals with disabilities. Because of changes in the manufacturing industry, a multitude of product options now are available to facilitate optimal positioning for individuals with a wide variety of needs. The knowledge base of therapists and the increased number of seating systems and accessories now available can help decrease the progression of deformities, pain, and other secondary problems. An individual who is seated appropriately can access available motor function, perform ADL with increased sense of security, and can lead a healthier, more enriching life. Specific product options are addressed later in this chapter.
Manufacturer production of durable medical equipment
The durable medical equipment industry has grown tremendously in the past 35 years to meet the increasing population of persons with disabilities and the increasing demand for more versatile, lighter-weight products. The increase in product options and advancement to lighter-weight materials such as aluminum and titanium has resulted in a vast selection of off-the-shelf products that have the potential to meet a wide array of needs. Manufacturers understand the need for persons with disabilities to try specific products to ensure they will meet their needs. Accordingly, they often provide evaluation equipment for clients to try.
Reimbursement policies
Insurance companies are the funding source for the majority of durable medical equipment provided for individuals with disabilities. Unfortunately, as a result, the funding source often influences the decision-making process. This discussion will focus primarily on Medicare guidelines because many private insurance companies follow these guidelines, and Medicare is the primary funding source for individuals who are older than 65-years-old and have had a stroke. Medicare has specific codes and reimbursement guidelines for durable medical equipment. It is concerned primarily about mobility within the home and will consider payment for a device only after an individual has received it. As a result, durable medical equipment suppliers have to take the risk and supply equipment without receiving any guarantee of payment from Medicare. Consequently, differences exist between individual supplier policies and what wheelchair and seating system products suppliers are willing to provide. As one can imagine, some suppliers hesitate to provide more complex, expensive equipment for individuals with more involved needs. It is essential for the team to work together to ensure that each individual has access to the best product to meet his or her needs. If this is not possible under Medicare guidelines, the client should notify the local congressional representative, and the team should consider other funding sources.
System and policy changes: development of standards and organizations to monitor assistive technology services
System changes have evolved over the past three decades and include the development of authorities and organizations to organize, control, and monitor assistive technology services. The Rehabilitation Engineers Society of North America (RESNA), the National Registry of Rehabilitation Technology Suppliers (NRRTS), the American Academy of Physical Medicine and Rehabilitation, and the Foundation for Physical Medicine and Rehabilitation have been created to develop or have been active in developing standards to ensure a higher standard of practice with wheelchair service provision. A monumental accomplishment was the American National Standards Institute/RESNA Wheelchair Standards. These standards provided the industry with increased consistency for wheelchair performance characteristics and measurements that are widely used by manufacturers to categorize and test wheelchairs. Consequently, these standards provide the wheelchair team with the ability to compare similar products from different manufacturers.
Another major accomplishment has been the development of credentialing programs. The RESNA awards therapists and suppliers credentials for an assistive technology professional and a seating and mobility specialist. The NRRTS awards a certified rehabilitation technology supplier credential. These credentials increase the likelihood that the professional members of the treatment team have a certain knowledge base of client’s needs and assistive technology products.
Numerous outcome studies have been performed and are being performed at a multitude of levels to determine the efficacy of wheelchairs, seating system products, and wheelchair service provisions. Specific topics studied include long-term wheelchair use, wheelchair design, repetitive stress injuries, propulsion methods, pressure relief techniques, and community integration. Many of these studies have focused on the individuals with spinal cord injury; however, the results are meaningful for all individuals who use wheelchairs as their primary means of mobility. The results from these studies have influenced manufacturing focuses and current practice with wheelchair prescription trends. This has translated into higher-quality products that minimize an individual’s risk of injury and increase their efficiency with mobility for increased integration into society. Continued involvement of health care practitioners in education, research, and product development is essential to ensure that all individuals with disabilities receive the best possible equipment to minimize their risk for secondary complications and maximize their ability to function indoors and outdoors.
Biomechanics of sitting
To appreciate and evaluate postural alignment, it is important to have an understanding of biomechanics. A therapist should understand basic anatomy of skeletal structures and their relationship to one another. The pelvis is the foundation for sitting; consequently, knowledge of the anatomy and biomechanical features of the pelvis and its relationship with the musculature and fascia of the spine and lower extremities is essential to understand how changes in lower-extremity positioning influence the pelvis and subsequently the spine.
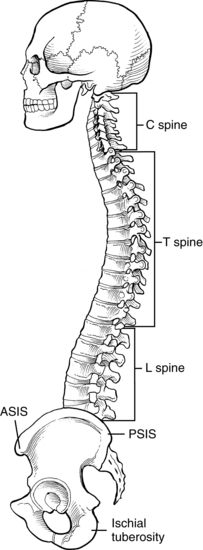
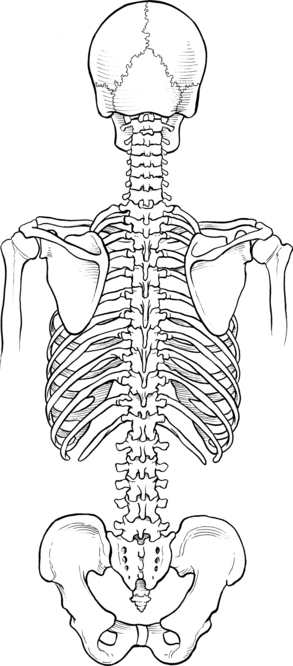
The pelvis moves anteriorly and posteriorly in the sagittal plane around a coronal axis, laterally tilting in a frontal plane around an anteroposterior axis and rotationally in a transverse plane around a vertical axis. A stable neutral position of the pelvis must be attained to provide the optimal postural alignment of the spine (Fig. 26-1). In a neutral pelvic position, the anterior superior iliac spine (ASIS) is level in a frontal plane and level with or slightly lower than the posterior superior iliac spine (PSIS) in the sagittal plane. A pelvis is also positioned in neutral when both ischial tuberosities bear weight equally (Fig. 26-2). Palpating the ASIS and PSIS and then both right and left anterior superior iliac spine can help the therapist to determine the position of the pelvis. Fig. 26-3 shows optimal sitting posture with a stable neutral pelvic position and symmetrical positioning of the lower extremities and trunk.
Assymmetrical pelvic positions, concerns, and common causes
Fig. 26-4, A, B, and C, shows changes in pelvic alignment. Part A demonstrates lateral tilting of the pelvis, in which one ASIS is higher than the other is. This pelvic obliquity results in unequal weight distribution through the ischial tuberosities and a C- or an S-shaped spinal curve. This posture places an individual at a high risk for developing a pressure sore under the lower, weight-bearing ischial tuberosity and secondary shoulder and neck discomfort. This problem is seen commonly in individuals with asymmetrical muscular strength, asymmetrical muscle tone, limited hip joint mobility, lower extremity hip flexion or internal/external rotation range of motion limitations, asymmetrical lower extremity muscle strength, and midline orientation deficits.
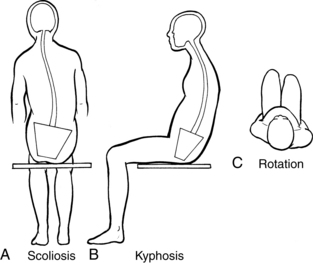
Figure 26-4 Common posturing following a stroke. A, Lateral tilting of the pelvis in a client with right-sided weakness. B, Posterior pelvic tilt with kyphosis. C, Trunk and pelvic rotation (superior view).
Fig. 26-4, B demonstrates a posterior pelvic tilt. A posterior pelvic tilt occurs when the ASIS is higher than the PSIS. This abnormal pelvic position results in a kyphotic spinal posture. A posterior pelvis with lumbar and thoracic spinal kyphosis results in changed weight distribution, with increased pressures on the sacrum and coccyx, and a compensatory cervical hyperextension. This posture can lead to pressure sores on the sacrum and coccyx, neck and back pain, limited neck range of motion, and a decreased visual field. Posterior pelvic tilt is commonly seen in individuals with trunk weakness, muscle imbalance, limited pelvic mobility, limited hip joint mobility, limited lower extremity hip flexion, and/or limited hamstring muscle length.
With anterior pelvic tilt, the ASIS is lower than the PSIS. This pelvic position usually results in a more pronounced lordotic curve in the spine. This posture is typically seen in individuals with decreased muscle recruitment and overall muscle weakness.
A pelvic rotation is present when one ASIS is farther forward than the other (see Fig. 26-4, C). The posture can present as unequal leg length posturing when an individual is seated. This abnormal pelvic rotation influences the spine to move into a rotated position and predisposes an individual to a scoliotic curvature of the spine. Pelvic rotation can create unequal weight distribution between the ischial tuberosities, which can lead to pressure sores. This posture is commonly seen in individuals with asymmetrical muscle strength, asymmetrical muscle tone, limited hip joint mobility, lower extremity abduction, or adduction limitations.
Wheelchair and seating system assessment
Basic principles
Although accessibility and wheelchair technology have changed drastically over the past 30 years, Judai’s study7 is a reminder that the process still is evolving. Judai used the Psychosocial Impact of Assist Device Scale to assess the psychosocial impact of assistive devices on individuals one and three months following the stroke. His findings for individuals who used wheelchairs indicated that some individuals reported a negative effect on their self-esteem, competence, and adaptability. This is a reminder to be attentive to the social and attitudinal environment that includes the stigma associated with using a wheelchair. Approaching each treatment session with a positive tone and educating individuals about the benefits of increased comfort and the potential ability to function independently indoors and outdoors are important.7 It is also helpful if the team has a working knowledge of community resources (i.e., support groups, transportation, and general accessibility) by which to educate the client about strategies for increased integration in the community.
Unfortunately, no specific formula exists to choosing the “right” seating system and mobility base. However, the set of guidelines discussed next can help the team achieve the best combination of mobility base and seating system with each client. The wheelchair and seating system decision is the result of an intricate interplay among an individual’s postural seated needs, personal preferences and goals, home and community environment, financial situation, and method of transportation. It is important to remember that the one-size-fits-all philosophy has no place in seating system and mobility device prescription.
The wheelchair and seating system assessment is specific to each individual’s needs. After obtaining demographic data, the assessment process generally begins at the ICF activities and participation level and progresses to the body functions and structures level. Initially, an in-depth comprehensive interview with the wheelchair team takes place to develop an understanding of an individual’s functional goals, environments he needs to function in, ability to participate in ADL, and knowledge base of wheelchair and seating system needs. The assessment then continues to screen numerous body functions such as muscle strength, balance, and cognition. This includes a mat evaluation, client education regarding postural needs and pros/cons of various seating and mobility base options, seating product and mobility product trial, and specifications of the wheelchair and seating system products. It is extremely important to take the time to perform a thorough assessment to avoid compromising the result and to minimize time spent fixing mistakes.2
Step 1: conduct a comprehensive interview
The therapist should lead the team and conduct a comprehensive interview that includes the client’s diagnosis; medical and surgical history; skin history; future medical and surgical considerations; allergies; precautions; pain; funding sources; social support network; use of splints or orthotics; previous and current level of functioning; likes and dislikes with current equipment; equipment fit in home environment, work environment, and community; transportation method(s) (car, van, taxi, or bus); and the client’s goals for the new or modified equipment. The interview should include psychosocial issues with respect to roles and lifestyle preferences; basic and instrumental ADL performance, including indoor and outdoor mobility; and transfer status. A physical status screening should take place to ascertain passive and active range of motion, available movement patterns, muscle strength, sensation, endurance, balance, visual-perception, and cognition. If the client has moderate to severe oral-motor control issues, a speech pathologist should be a member of the treatment team to ensure that the client’s communication and/or augmentative communication needs are addressed thoroughly. See Chapter 20.
If this is a client’s first wheelchair, a home evaluation form is generally provided and additional education is necessary to ensure that the client and significant others understand the environments that wheelchair maneuverability will have impact on.
Step 2: perform a supine and seated mat assessment
A mat assessment is an intimate evaluation that can be intimidating and confusing to the client and significant others. The assessment involves therapeutic handling, palpation, and range of motion. The results of the mat assessment are essential to determine the amount of support an individual requires for upright sitting, the goals and overall setup of the seating system, and the mobility base options needed to accommodate the recommended seating system. The therapist must take the time to articulate the purpose and importance of the mat evaluation to ensure that everyone “understands what you are looking for, how you will be going about it, and why this information is important to reach a good end result.”2
Before beginning a mat assessment, it is important for the therapist to understand some basic biomechanical and seating principles. One of the main concepts is the distinction between flexible, difficult to correct, and fixed postural deformities. These concepts clarify skeletal positions in the supine and seated mat assessment.
The initial focus with a mat evaluation is to determine whether neutral pelvic and trunk alignment can be achieved. If the pelvis is in an oblique position and lower extremity influence has been accommodated for or ruled out, the therapist should attempt to correct the pelvis manually.
If the pelvis stays in the corrected position, without handling, the deformity is considered flexible.19 If the pelvis goes back into the oblique position but is repositioned easily to neutral and requires gentle therapeutic handling to stay in neutral, the deformity is considered difficult to correct.19 If the pelvis cannot be repositioned manually into a neutral position, the deformity is considered fixed.19 A pelvic obliquity is measured by the height difference between each ASIS and is named for the side that is lower.19 A subsequent section discusses seating considerations for flexible, difficult to correct, and fixed body structures.
A thorough mat assessment can require two to four persons and consists of four major components:
1. Observation of the client in the clinic with the current or loaned equipment; the therapist assesses postural positioning in the wheelchair and screens muscle tone and strength. The specific focus should include the influence of tone on movement, influence of movement on tone, and influence of tone on postural control.
2. For a supine mat assessment, the client is positioned on a mat. This is essential to determine the bony structure, muscle flexibility (including muscle tone), and range of motion of the client to achieve optimal spinal-pelvic alignment. The assessment provides the therapist with a “true” picture of each individual’s potential to be seated with optimal spinal-pelvic alignment. The results from the supine assessment are essential to guide how an individual is positioned or supported for the seated mat evaluation
3. A seated mat assessment is essential to determine the influence of gravity on the individual’s ability to sit upright. The therapist can usually perform the seated assessment with the client seated on the edge of the mat with therapeutic handling by the therapist and other members of the treatment team. At this time, muscle tone may be increased as the individual attempts to hold his or her body up against gravity. If a client has moderate to significant postural needs, a positioning simulator can be helpful to support the client in the upright position. A more detailed description follows.
4. Once an individual is positioned with maximum aligned posture on the mat or in the simulator, the time and location are ideal to take accurate measurements of the client’s body. The five basic measurements for an active individual are seat width, seat depth, knee to heel (with shoe), elbow height, and distance from the seating surface to inferior angle of the scapula. All measurements can be documented in half-inch or one inch increments (e.g., 17.5-inch seat width). Chest width, axilla, top of shoulder, and occiput measurements are important to obtain if an individual requires more aggressive support (Fig. 26-5).
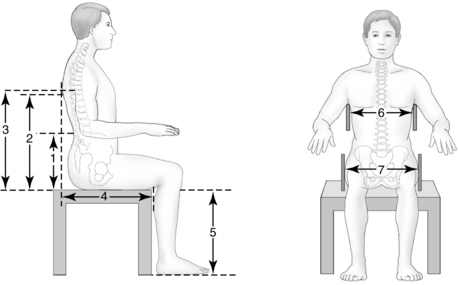
Figure 26-5 Measurements during the mat assessment. 1, Elbow height; 2, seat to inferior angle of scapula; 3, axilla; 4, seat depth; 5, knee to heel; 6, chest width; 7, hip width.
A simulator is a tool that permits the team to evaluate a sitting client more easily with various angles and amounts of support. This simulator is composed of planar surfaces that can be adjusted to different depths, and recline, and tilt to provide appropriate support. In addition, it consists of easily adjusted components (headrest, lateral support, hip support, armrest, and footrest) that can be placed in numerous positions and are adjustable through knobs. The simulator permits therapists to evaluate the seated position with an individual, evaluate the level of function with different positions, educate the client on the potential to achieve the best possible resting posture, take more accurate measurements, visually document potential for increased alignment via pictures to funding sources, and save an enormous amount of time with evaluating different products. The simulator can help narrow the product options necessary for evaluation to provide optimal support (Fig. 26-6).
Step 3: provide client and team education
Educating the client about the mat evaluation findings and their effect on postural alignment in a seated position is important. At that time, the therapist can review a client’s goals, and each team member should articulate their goals to ensure that all are headed in the same direction. Education is essential to enable an individual to participate actively in the wheelchair and seating system trial and decide what compromises he or she is willing to make to maximize the ability to function in a wheelchair. Although the client is the primary decision-maker, the therapist and assistive technology supplier should freely discuss their professional opinions. Part of the educational process is to help a client prioritize what is most important, especially when future health, skin integrity, and secondary complications are a concern. There is no one wheelchair and seating system that is perfect for individuals with stroke; the solution is perfect only when a client makes informed decisions about what various components will work best for his or her lifestyle.
It is helpful to discuss wheelchair and seating system needs in a general way and then to select products so that a client can choose from two or three options. Using the mat evaluation results and understanding product features and benefits is essential and described in detail later in this chapter. The therapist and assistive technology supplier have the responsibility to clearly articulate the features, benefits, and pros and cons of various options to empower the clients to select products to best meet their needs. Providing this information empowers the client and significant others to be educated, reinforces their confidence in the decision of the team, and increases their satisfaction with the final product.
Step 4: equipment trial
Actual trial of seating system and wheelchair options is the best case scenario; however, this is not always possible. If a manufacturer is unable to provide the team members with the equipment they are considering, simulating the type of seating design and components is important for the team to ensure that the product is accomplishing what they had hoped to achieve.
Actual trial of more complex, expensive equipment is highly recommended to minimize unseen compatibility and fit problems and ensure that the full system can meet the client’s needs and goals.
Once the ideal wheelchair and seating system is decided upon, the team gathers around the client in the “evaluation” wheelchair and seating system. At this point, the team decides the measurements of the product, specifies wheelchair and seating system features with order forms, and provides additional education about the pros and cons of specific features (such as pneumatic versus solid tires). In an ideal situation, this is truly a collaborative team process.
Step 5: documentation
At this point, the therapist has gathered all the information needed to write a letter of medical necessity. This letter is a concise summary of the client’s activities and participation status, mat evaluation findings, problems with existing equipment, wheelchair and seating needs to maximize activity and participation, and medical and functional justification for the wheelchair, wheelchair features, and seating system recommendations. This is the letter that the medical doctor reviews and signs once the final additions are completed.
As the medical professionals are generating the letter of medical necessity and organizing the medical chart notes and prescriptions, the assistive technology supplier contacts each of the manufacturers for price quotes and generates a product description form. The doctor reviews and signs this form. It is sent with the letter of medical necessity and other insurance documentation to the assistive technology supplier for funding approval.
Step 6: fitting, training, and delivery
After the team has recommended and documented the person’s equipment needs, the job is only half over. It is common for funding sources to question the team’s recommendation. It is important to respond as promptly as possible to these inquiries and clearly communicate the team’s goals.
Once the assistive technology supplier feels secure that the equipment will be funded and in some cases “approved” by the funding source, the equipment is ordered. All team members who were involved in steps 1 to 5 should be available for steps 6 and 7. During fitting, training, and delivery, the wheelchair and seating system is set up and adjusted to specifically meet each client’s needs. At this time, the therapist and assistive technology supplier educate the client and significant others regarding wheelchair and seating system parts management, care, and general maintenance, including whom to contact if problems arise. For example, if a client needs replacement parts, he or she is advised to contact the assistive technology supplier; if a client experiences physical changes and is no longer comfortable, he or she is advised to contact the medical doctor and the therapist.
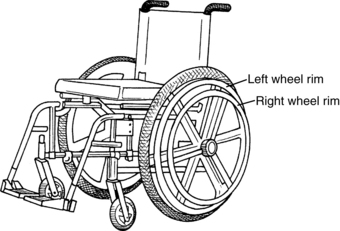
Mobility skills training is essential to provide clients with strategies and techniques for maximum safety and independence with mobility. This includes training for manual wheelchair operation using the traditional ipsilateral arm-foot propulsion technique,3 a one-arm drive wheelchair, or a power mobility product. Rudman and colleagues16 concluded that training was needed beyond the prescription of the wheelchair. This training is essential to provide clients with the ability to reach their full functional potential with activities and participation.
This fitting and delivery step is essential to ensure that the end product accomplishes the team’s goals and minimizes an individual’s risk for deformity and secondary problems. Another benefit to this step is that it significantly reduces the potential for product abandonment.
Step 7: functional outcome measurement and follow-up
The ideal situation would be for an individual to attend a follow-up treatment session three months after the fitting and delivery or at least to participate in a phone interview with the therapist to determine the success of the wheelchair and seating system intervention. This step is a true test to ensure achievement of the team’s goals. Follow-up should focus on issues such as whether the equipment is holding up to the individual’s specific needs and has made a difference on pain, quality of life, and independent functioning.
Barker and colleagues1 reported that wheelchairs were an enabler of community participation. Pettersson and colleagues13 used the Psychosocial Impact of Assistive Devices Scale and found that wheelchairs increased quality of life for individuals after stroke.
Matching equipment to client function: seating system principles
Translating the mat evaluation into the seating system
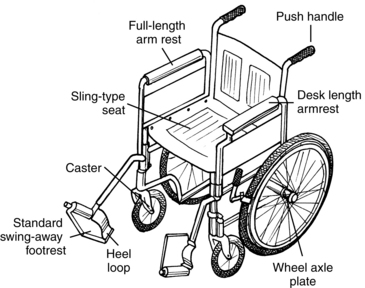
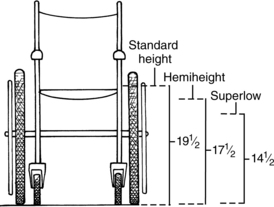
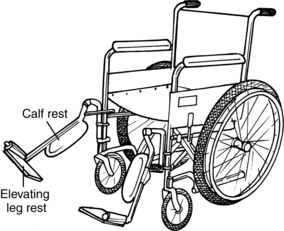
Once the mat assessment is completed, the therapist must translate the measurements and ranges into the set-up of the seating system and wheelchair. For example, if Mr. S. has only 80 degrees of hip flexion range, the seat-to-back angle must be set up to accommodate this 10-degree limitation. Most back canes have an 8-degree bend rearward, and therefore a back support with some adjustability is provided with an additional 2 to 7 degrees of open seat-to-back angle. The extra 5 degrees is necessary to allow for some adjustment for comfort. It is important not to position an individual at the maximum range available. Likewise, if Mr. S. has hamstring tightness (−70 degrees of knee extension with his hip at 80 degrees of flexion), the therapist must be cautious about using an elevating leg rest, because it generally positions the lower extremity in −65 degrees of knee extension and would overstretch his tight hamstring musculature. Because Mr. S.’s hamstring muscle cannot sufficiently elongate to tolerate this open knee angle, his body will automatically compensate for this, which would result in Mr. S sitting with a posterior pelvic tilt. In this situation the team can order a 70-degree standard footrest and use a longer heel loop for foot position rearward for a −70- to −75-degree knee angle, being mindful of caster (front wheel) clearance. This is essential to adequately accommodate his hamstring muscle tightness and allow for optimal pelvic and spine positioning.
Flexible, difficult to correct, and fixed deformities
Once a therapist establishes what type of deformity is present, he or she must figure out how to support the client to minimize his or her risk for increased deformity. If an individual has a flexible or difficult to correct deformity, the seating system should be set up to imitate the therapeutic handling to “correct” the deformity. At this time, client education regarding repositioning strategies is helpful to ensure the client is aligned properly and to facilitate neuromuscular reeducation. It is important to carefully monitor each client’s tolerance for correction and adjust the seating system accordingly to maximize success. The process may require incremental steps to achieve increased alignment or may involve backing down from an aggressive start. If a deformity is fixed, as much aggressive support as possible is important to assist the client around his deformity to decrease progression and to minimize his or her risk for increased deformity.
With more aggressive seating systems, a mobile person can be “locked” up by the aggressive supports used to achieve optimal spinal-pelvic alignment. Unfortunately, this often limits an individual’s ability to function. With positioning for function, a compromise occurs to provide as much support as possible for the resting body position without affecting or limiting an individual’s ability to function. Consequently, wheelchair seating is a continuum with safety and maximum postural support on one end and mobility for activity and participation on the other end. An ideal seating system should have some flexibility to provide optimal spinal-pelvic alignment and facilitate function. It is important to maximize the potential movement options of individuals who use wheelchairs as their primary means of mobility. Individuals with good motor control may choose to sit on a chair or stool for more active functioning. For individuals who do not have as many mobility options available, the wheelchair must have the ability to accommodate both active and resting seated postures.
Although online resources for wheelchair and seating system products are an excellent source of information and education, online purchase of these products is not recommended because a client does not receive any of the benefits that an assistive technology supplier provides (i.e., assistance with set-up and assembly, on-site adjustments, and personalized modifications).9 In addition, an individual purchasing equipment online misses the opportunity for the team evaluation and product trial and may not be in-tune to mild physical changes that have occurred since last receiving a wheelchair and seating system.
General seating system principles for individuals with stroke
Therapeutic intervention for individuals with brain damage caused by a stroke depends on the severity of the infarct and the amount of functional change that has occurred, including physical, visual-perceptual, and cognitive changes. Accordingly, wheelchair and seating system intervention also depends on the level of functional changes and confounding variables, including the environment in which the individual is functioning and the presence of other diagnoses such as diabetes, hypertension, and coronary artery disease. Seating systems for individuals with more involved needs may be more supportive because of decreased plasticity in the central nervous system and permanent brain damage.5
Individuals with hemiplegia resulting from stroke often have difficulty controlling posture, balance reactions, and smooth movement patterns that enable the performance of functional tasks. Davies5 described the typical patterns of adult hemiplegia (Table 26-1).
Table 26-1 Typical Patterns of Adult Hemiplegia
| BODY PART | COMMON POSTURE |
|---|---|
| Head | Flexion toward hemiplegic side, neck rotation toward unaffected side |
| Upper extremity (flexion pattern) | Scapula retraction, shoulder girdle depression, humeral adduction and internal rotation Elbow flexion, forearm primarily in pronation; occasionally supination dominates Wrist flexion and ulnar deviation Thumb and finger flexion and adduction |
| Trunk | Trunk rotation backward on hemiplegic side with lateral trunk flexion |
| Pelvis | Posterior tilt with obliquity (lower on unaffected side) |
| Lower extremity | Hip extension, adduction, and internal rotation Knee extension Foot plantar flexion and inversion Toe flexion and adduction |
For individuals who use a wheelchair as their primary means of mobility, seating and mobility recommendations should address these typical patterns of adult hemiplegia. The following are typical seating system goals and seating principles specific to individuals with stroke.
Goals of the seating system
The primary goals of seating and positioning at the ICF body functions and structures level are as follows:
Provide adequate postural support
 To prevent deformity or minimize the risk of increased deformity
To prevent deformity or minimize the risk of increased deformity
 To balance skeletal muscle activity
To balance skeletal muscle activity
 To minimize compensatory postures
To minimize compensatory postures
 To maximize pressure distribution and minimize the risk of pressure ulcers
To maximize pressure distribution and minimize the risk of pressure ulcers
 To enhance distal extremity control
To enhance distal extremity control
The primary goals of seating and positioning at the ICF6 activities and participation level are as follows:
Provide adequate postural support
 To maximize ability to perform functional activities
To maximize ability to perform functional activities
 Aesthetically to enhance dignity and self-esteem and quality of life
Aesthetically to enhance dignity and self-esteem and quality of life
 To increase comfort for increased social interaction and participation in community activities
To increase comfort for increased social interaction and participation in community activities
Postural stability and control.
Abnormal skeletal muscle activity and pathological reflexes often influence the postural alignment of an individual with neurological insult. A seating system should provide a stable foundation for maximum postural alignment to reestablish the length tension relationship of the muscles, balance muscle activity, normalize muscle tone, and decrease compensatory posturing. Improved postural stability provides individuals with the freedom to interact, move their extremities, and hold their heads in the midline position.2 Secondary benefits of improved stability and control are increased ability to attend to what is happening in the environment, increased interaction with the environment, improved ability to assist in or perform ADL, and increased independence with mobility.
Proximal muscle stability to enhance distal muscular control.
A stable base of support for the pelvis provides individuals with the opportunity to develop control and balance of their trunk musculature. When the pelvis is stable, an individual’s center of gravity passes through the base of support, which helps promote stability. This central stability allows for distal extremity control. The client is better able to access muscles for arm or leg movement, head control, or oral motor control to perform functional tasks (i.e., hand function for dressing, leg movement for wheelchair propulsion, midline head orientation for improved visual tracking of objects, and oral motor control for speech articulation or swallowing).
Decrease development of muscle contracture and skeletal deformity.
Decreased pelvic control, muscle weakness, and muscle imbalance contribute to asymmetrical posturing. Asymmetrical postures can result in shortening or tightening of muscle groups, which can lead to a decreased range of motion in joints, increased tone, muscle contractures, and skeletal deformity. Asymmetrical posture must be corrected in a resting seated position to minimize an individual’s risk for development of a fixed deformity. If soft tissue and skeletal flexibility is preserved, an individual can be encouraged successfully to sit with improved spinal-pelvic alignment through seating and seating system accessories. This positioning serves as a guide that eventually can promote the development of more balanced muscle control in that desired position. If muscle control cannot be improved, good positioning provides adequate support.
Enhance comfort and appearance.
With optimal postural support in the seated position, individuals feel and look better. However, the process is not always a one-time event; seating system modifications can be introduced gradually to facilitate neuromuscular reeducation. Once an individual can tolerate increased postural alignment, the benefits are tenfold. Individuals who feel comfortable and feel good about themselves are much more productive and functional. This can lead to increased social interaction, communication, and an improved quality of life.
Minimize development of pressure ulcers.
When impaired sensation, motor control, or judgment affect an individual’s ability to shift body weight, the client is usually at risk for developing pressure ulcers. Essential aspects of seating are to focus on pressure-redistributing cushions to maximize seating surface pressure dissemination and to consider a method of pressure relief (power tilt or recline) that the client can operate independently or a tilt-in space or recliner wheelchair in which a caregiver can perform the pressure-relief technique. Performance of regular (i.e., every half hour) pressure relief technique is essential to minimize risk of pressure ulcers.
Improve function of the autonomic nervous system.
Abnormal posturing, muscle shortening, and the inability to shift weight can increase pressure on internal organs and other structures. When an individual is leaning forward or to the side because of poor pelvic or spinal muscle control, a strain on circulation, digestion, and cardiopulmonary function can result. Postural supports can facilitate optimal pelvic, spinal, and trunk alignment, which in turn can provide improved physiological functioning of the autonomic nervous system. Sufficient head and neck support can decrease the potential for aspiration when swallowing problems exist.2
Increase sitting tolerance and energy level.
If an individual is well-supported and can function from the wheelchair, sitting tolerance increases along with the ability to participate in therapy programs and functional activities. Individuals who receive adequate postural support experience less fatigue and pain than those who fix and stabilize continually with a higher level of abnormal muscle activity and reflexes to support the body upright against gravity. The increased energy level associated with a more symmetrical posture increases sitting tolerance and an individual’s ability to participate in functional activities within the home and the community.
Functional positioning: an active seating system.
Although the primary focus for seating intervention thus far has been on symmetry and alignment, a therapist must remember that functional movement is asymmetrical and dynamic. As a result, it is essential to consider seating systems that allow for function and activity performance and yet provide individuals with as much postural support as necessary to minimize their risk for increased deformity. It is important to remember that “body control is interpreted and performed when the body understands its relationship to gravity, primarily through activation of the vestibular system.”8
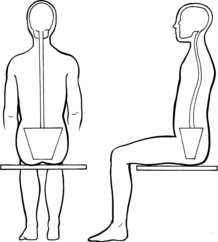
The pelvis is the foundation for seated posture. With this in mind, it is important to consider Kangas’ perspective on pelvic stability. Kangas8 stated, “pelvic stability is not simply a musculoskeletal posture but rather is a movement of the body that includes an ongoing interaction of numerous systems, including the musculoskeletal, neuromuscular, circulatory, respiratory, gastrointestinal, and endocrinological systems.” Pelvic stability is “not simply a musculoskeletal posture.” It involves a position of actively holding still rather than being passively restricted. For individuals with a stroke, an active seating system generally provides as much seating surface as possible, a slightly anterior tilted seat, mild contour for upper leg positioning, and weight-bearing of the feet on the floor to enable the individual to position them as he or she chooses. This base of support can provide the body with sufficient pelvic stability, and this position of active weight-bearing allows an individual to assume an active task performance position for eating, writing a check, or working at a computer.8
An active seating system can be attained easily with minor adjustments to the wheelchair and seating system that is set-up slightly higher on the continuum for increased safety and adequate support. This is beneficial for times when an individual is more active (i.e., meal preparation in the kitchen). A seat wedge can be placed under the cushion and the footrests and positioning straps removed to allow an individual to achieve a more active position. As with all intervention recommendations, the therapist and client should evaluate this intervention together to ensure that it provides adequate stability for maximum safety with functioning. The art with mobility and seating system prescription is to achieve a balance between positioning for functional activity performance and symmetrical postural alignment for more sedentary activities (i.e., watching television) and to minimize an individual’s risk for increased deformity and secondary complications.
Matching equipment to client function: seating systems
Seating and positioning is a continuum that encompasses all of the foregoing goals and principles. It is important for clients to understand that the wheelchair is not uncomfortable; usually the seating system is. The seating system is the primary unit that influences body posture because it is the direct interface between the client and the wheelchair and provides the client with the foundation for adequate postural support to rest and function. The mobility base is a frame that has some seating components such as footrests and armrests; however, its primary focus is mobility indoors and outdoors. It is essential to have a seating system that provides sufficient postural support interfaced with a wheelchair frame set at the appropriate angles to facilitate optimal spinal-pelvic alignment. Without appropriate postural support, an individual may be able to move about the environment; however, the risk for further deformity and pain is a major concern. A good rule of thumb for optimal positioning is to start with the pelvis and then proceed to the trunk and extremities. This approach follows the “support proximal to distal philosophy” inherent in numerous treatment approaches for individuals with neurological dysfunction.
The importance of seating, goals, and assessment of biomechanics and posture were reviewed previously. This section describes the types of seating systems available and their various features. Three basic styles of seating exist: linear, contoured, and custom contoured. Each of these provides different levels of support to promote postural alignment and pressure distribution. The definition of each with their respective benefits and concerns follows.
Linear seating systems
Linear seating systems (Table 26-2) are flat, noncontoured planes of support. Linear seat cushions or backs can be custom-made or ordered from the factory in various sizes, densities, and with different fabric covers.
| SEATING COMPONENT | INDICATIONS FOR USE | POSTURAL AND FUNCTIONAL CONSIDERATIONS |
| Solid insert |
Insert can provide a level base of support on the sling wheelchair seat. Slide insert inside the cover, under the cushion, and secure to cushion base with Velcro. The cushion cover usually has Velcro to attach the cushion securely to sling upholstery of the wheelchair. | A sling wheelchair seat encourages a posterior pelvic tilt with hip adduction and internal rotation. This sets an individual up for a “slumped” posture. A solid insert is necessary to provide a firm and level base of support on the sling wheelchair seat. This facilitates more neutral pelvic positioning for upright posture and upper body movement for functional activities. |
| 1.5–inch seat wedge | Wedge slides inside the cushion cover, under the cushion. Wedge can provide an anterior or posterior seat tilt. | Wedge is a lightweight, easy to remove component to use for an anterior-sloped seat or a posterior-sloped seat. An anterior tilt would facilitate upright positioning for an individual who is working at a workstation or propelling with one arm and one foot. A posterior tilt can assist with decreasing extensor spasticity or creating a set, slight tilt for increased postural support in a standard wheelchair. |
| Solid seat |
Remove wheelchair upholstery to install. To mount, solid seat hooks lock down on seat rails of wheelchair. The adjustable hooks on the solid seat can be positioned to provide an anterior or posterior tilt of solid seat and subsequently the cushion on the wheelchair frame. | Seat also encourages neutral pelvic alignment and lower extremity alignment. One concern is that it adds a significant amount of weight to the wheelchair. Unless necessary to achieve a low seat-to-floor height that cannot be achieved with a super low wheelchair, the weight disadvantage outweighs the positioning advantages. |
| Foam cushion |
Foam linear cushions provide a stable base of support for individuals with mild postural support needs. The foam comes in varying densities and can be layered in different densities to provide support, comfort, and some pressure relief. | Cushions can enhance sitting posture, pressure distribution, and increase comfort. |
| Contoured foam cushion |
Contoured foam cushion provides an increased surface area of support and pressure relief for individuals with mild to moderate support and pressure distribution needs. A variety of foam densities are available. | The combination of stability and pressure relief is a major advantage to this cushion. The weight is a consideration; however, the advantage of a stable and pressure-distributing base of support minimizes the need for external supports. |
| “Pressure-relieving” cushion (fluid medium) |
A firm, contoured cushion base with pressure-distributing gel fluid pad on top provides stability and a high level of pressure relief appropriate for all individuals who need moderate to significant postural support and pressure distribution. The gel bladder allows the pelvis to sink into it for full contact support for adequate pressure distribution to minimize the risk of pressure sores. | These off-the-shelf cushions provide a superior level of pressure distribution and good pelvic stability. This stability is important for improved balance and for adequate support. It can improve function at a wheelchair level and minimize compensatory posturing. |
| “Pressure-relieving” cushion (air medium) |
The air medium allows the seated individual to sink into this cushion for contoured support and a high degree of pressure distribution to minimize the risk of pressure ulcers. | The pressure distribution and lightweight qualities of this cushion are unsurpassed. However, this cushion does not provide any stability, and additional postural supports such as hip guides and adductors are essential for optimal alignment. These supports increase weight of the whole wheelchair system. Another concern is the continual air maintenance required with this cushion. |
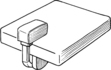
| Lumbar-sacral back support |
This component can provide support to the lumbar-sacral region to support the pelvis in neutral pelvic alignment. A more secure attachment method is recommended to keep it in position. | This support is a low-cost method to provide minimal postural support for increased spinal-pelvic alignment. The support is easy to remove, which is an advantage for car transport but a disadvantage because the support is not stable and can shift out of place easily. |
| Solid back support |
The solid back insert provides firm support to facilitate improved postural alignment for individuals with good pelvic and trunk control. The support is easy to remove for transportability of the wheelchair and usually is attached to the wheelchair back canes with Velcro straps. | This support is a low-cost method to provide minimal postural support for increased spinal-pelvic alignment. The support is easy to remove, which is an advantage for car transport but a disadvantage because the support is not stable and can shift out of place easily. |
| Pita back |
This solid back insert provides a firm support to facilitate improved postural alignment for individuals with good pelvic and trunk control. The support is easy to remove for transportability of the wheelchair and slides into and out of a pocket in the back support upholstery. | This simple, low-cost back support can provide minimal postural support for increased spinal-pelvic alignment. The lack of foam makes the support easy to use; however, lack of sufficient padding is a concern for individuals using the wheelchair as a primary means of mobility. |
| Linear back support |
This solid back insert provides a more durable back support for increased spinal-pelvic alignment. It is beneficial for individuals with good postural control, is attached to the wheelchair frame with quick-release hardware, and usually is linear with a solid posterior base with foam in front. The support may be covered in vinyl or other materials. | This is a planar back support to enhance upright sitting. The adjustable mounting brackets makes it possible to open up seat-to-back angle to accommodate a hip range of motion limitation or for increased postural support and balance via gravity. This hardware is durable. One concern is the weight added to the wheelchair. |
| Adjustable-angle off-the-shelf back support |
This back support can be attached to the wheelchair with quick-release hardware. The support has generic, gentle contours that provide a guide for increased postural alignment for individuals with mild to moderate positioning needs and can be used in its original configuration or can accommodate a contoured foam in-place back support. | This back support provides mild contour to facilitate neutral trunk posturing and increased spinal-pelvic alignment. The angle can be adjusted to open up seat-to-back angle to accommodate a hip range of motion limitation or for increased postural support and balance via gravity. This support is a lightweight option that provides good support. One concern is that more durable hardware may be necessary for individuals with significant spasticity. |
| Adjustable-angle custom back support | This rigid back support can be attached to the wheelchair with quick-release or stationary hardware. The support often is positioned at an angle with a custom-contoured amount of support. The shell can be reused if the foam insert needs to be modified. This support benefits individuals with moderate to significant trunk weaknesses and/or flexible or fixed postural deformities. | This back support can provide moderate to significant support for individuals with flexible and fixed deformities. The hardware can open up the seat-to-back angle for the foregoing reasons. The contoured support provides maximum surface area contact to maximize alignment, accommodate deformities, and maximize pressure distribution to minimize the risk for increased deformities and pressure sores. |
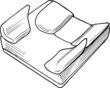
| Pelvic positioning belt |
Pelvic belts are designed to maintain optimal pelvic alignment and minimize an individual’s risk for sliding out of the wheelchair. They are mounted to the seat frame via screws or straps and are available with various angles of pull and various buckles such as auto and airline style. | This support can be positioned at various angles depending on the individual’s needs and functional level. A pelvic belt at the traditional 45 degrees can limit pelvic mobility for an anterior weight shift for forward reach and functioning at a table. Padded belts are available to minimize pressure concerns, and various buckles are available for maximum independence with opening/closing. |
| Leg adductors |
A leg adductor can be attached to the wheelchair cushion base, under the seat, or on the footrest hanger and is designed to maximize lower extremity alignment and prevent the legs from rolling into abduction or external hip rotation. This is an example of an adductor added to the front of the cushion. | Adductors can facilitate increased lower extremity alignment to minimize an individual’s risk of increased deformity and pain. The height of the adductor can limit side-to-side transfers; a removable one can provide adequate support and increased safety with side transfers. |
| Hip guides |
Hip guides provide support to maximize pelvic alignment, can be contoured or linear, and usually are made of different density foams with a solid back. Hip guides can be mounted onto the wheelchair armrests, seat pan, or back canes. The hardware can be fixed or removable. This is an example of hip guides that are attached to the rear of the cushion. | In addition to the lateral supports, hip guides can provide a third point of control for individuals with fixed or flexible spinal curves or individuals who have a pelvic obliquity. Removable hardware is often necessary for individuals who perform side-to-side transfers. |
| Medial knee block (pommel) with flip-down hardware |
Medial knee blocks or pommels can maximize lower extremity alignment. They are designed to minimize leg adduction and internal hip rotation. For optimal support the medial knee blocks are custom-made in a variety of shapes and sizes. This contour is essential for adequate contour and fit for increased pelvic and lower extremity alignment. The knee blocks and pommels typically are constructed of a variety of foams with a solid inner component and are attached to the wheelchair with various types of hardware. | Medial knee blocks are often necessary for individuals with severe adductor spasticity. They are most successful when used with the other postural supports to maximize overall postural alignment. They can promote increased lower extremity alignment. Small medial knee blocks are helpful as a guide for more neutral lower extremity posturing. |
| Pelvic obliquity build-up |
This component is usually mounted under the gel pad or created with foam; it can be a gel or foam medium and can provide increased support under the lower ischium to “correct” a deformity, under the weaker side to accommodate for muscle atrophy, or under the higher ischium to accommodate a deformity. This component may be used with hip guides to minimize lateral tilting of the pelvis for increased spinal-pelvic alignment. |
Foam or gel inserts are helpful for individuals with asymmetrical muscle strength. They can compensate for the decreased muscle bulk to facilitate a more level pelvic position. When used with hip guides, inserts can support optimal pelvic alignment in individuals who have a flexible pelvis. One concern is the amount of pressure the inserts place on the ipsilateral ischial tuberosity.17 Monitoring of pressure with this treatment approach is important. If a pelvic obliquity is fixed, positioning an insert under the higher side is necessary. This will accommodate and support the fixed pelvic obliquity, increase pressure distribution, and minimize the risk of increased deformity. |
| Lateral trunk supports, straight and curved |
These supports usually are mounted off the back support or back canes and are available in various sizes in planar or contoured levels of support. They are beneficial for individuals with trunk weakness or a tendency to lean to one side. Another point of control, usually via hip guides, is necessary for adequate trunk support to correct a flexible deformity or accommodate a fixed deformity. The hardware to mount to the wheelchair can be stationary or quick release. |
Individuals who have decreased trunk support often hold themselves upright with their upper extremities. Lateral supports can provide increased trunk support to these individuals so that they can use their extremities for bilateral upper extremity tasks. Lateral supports also can provide the upper two points of control to correct or accommodate a lateral spinal curve for increased midline positioning of the torso in the wheelchair. The swing-away hardware is helpful to position the lateral support out of the way for transfers, dressing, and initial positioning in the wheelchair. Lateral support hardware that aggressively contours to the back support contour is necessary to keep the hardware profile minimal to allow for adequate upper extremity mobility. Curved lateral support pads provide improved contour and support over planar lateral support pads. |
| Harness/anterior chest support |
Anterior chest supports are mounted to the wheelchair via four points of attachment, usually to each side of the back support and the seat rails. They are available in a variety of styles and are beneficial for individuals with severe trunk weakness. These supports often are used with a tilt or recline seating system to maximize postural support when an individual is more upright against gravity. | This component can provide anterior trunk support to allow an individual with poor trunk control to be more upright against gravity. This is helpful for more dynamic, engaging activities (i.e., working at a desk). Therapists should consider this component after evaluating a recline or tilt-in-space seating system for increased postural support in a more sedentary, posterior position. The component can be helpful for maximum trunk support for increased safety and stability when negotiating varying terrain (i.e., ramps and door saddles). |
| Head/neck support |
Head/neck supports can be mounted to the back support via quick-release or flip down hardware. A headrest and/or neck support is essential to provide adequate head support for individuals with poor head or neck control. The quick release and flip down hardware is necessary to maneuver the headrest out of the way for positioning the client in the wheelchair, hair washing, etc. |
This component is necessary for individuals with fair head control and for head and neck support when an individual tilts back for pressure relief or improved postural support. Additional pads and head bands are available for individuals with significant head positioning needs. The head and neck supports should be adjusted to support the head in as neutral alignment as possible for optimal functioning (i.e., respiration and feeding) and speech. |
| Wheel lock extension |
Wheel lock extensions can be mounted over the existing wheel lock handle. They are available in various sizes. Wheel lock extensions provide a longer lever arm to make it possible to access and lock/unlock the wheel locks if an individual cannot negotiate the standard wheel lock. | Extensions are important for maximum independence and to stabilize the wheelchair for functioning and safety with transfers to and from the wheelchair. For individuals with stroke, a wheel lock extension on the wheel on the client’s weaker side is often very helpful for independent use with either the weaker or the stronger upper extremity. |
| Upper extremity support, full and half lap trays |
Lap trays can be mounted over the armpad with “slide” hardware with an additional strap for stability, if necessary. They come in full or half tray models in various sizes. They can provide individuals with a support surface for their paretic upper extremity. | Adequate upper extremity support is essential to minimize an individual’s risk for increased shoulder pain and deformity. A lap tray can provide a work surface for functional activities such as writing and feeding. The clear version can also provide an individual with a clear view of the feet for maximum safety with wheelchair propulsion. Upper extremity edema is often present in individuals who are unable to move their upper extremity functionally. A lap tray can facilitate increased awareness of this extremity for edema management, weight-bearing, and positioning to minimize upper extremity edema. |
| Arm trough | An arm trough can be mounted on the standard armrest in place of the armpad. The trough can provide more aggressive support for adequate upper extremity joint protection. Full length armrests are often necessary to provide sufficient stability for an arm trough. |
An arm trough provides optimal support for individuals with absent to poor upper extremity control. Support is important to minimize the risk for pain, subluxation, and edema. An arm trough can provide an individual with a surface for upper extremity weight-bearing for functional reaching activities or for repositioning his/her body in the wheelchair. |
Linear seating provides a firm, rigid seating base that can be beneficial for active individuals. Individuals with minimal musculoskeletal involvement typically benefit the most from linear seating. This seating is generally a lower cost option, and because of the flat surface, independent transfers are easy to achieve. Linear seating systems provide the least amount of postural support; however, because the human body is contoured, lack of support can result in higher peak pressures and pressure ulcers for individuals with prominent bony structures.
Contoured seating options
Contoured seating system options (see Table 26-2) are designed to support the body ergonomically. They are generally available in predetermined shapes of varying contours in a wide range of sizes.
Contoured seating options provide a range of contours from mild to aggressive. This type of seating system provides an excellent surface area for support that can enhance postural alignment and pressure relief. Individuals with minimal neuromuscular or central nervous system insults can benefit from the gentle cues that the slight contours of this seating system provide. Individuals can also achieve independent transfers with the mild contour options.
Individuals with moderate impairments benefit more from moderately contoured seating systems. These individuals are less likely to perform independent transfers, and the increased contours can meet their more involved postural support and pressure distribution needs. An advantage to an off-the-shelf contoured seating system is that it can be modified as an individual’s needs change. It is important to remember that more aggressive contoured supports really hold and support an individual, which is ideal for postural alignment but can make transfers more difficult.
Custom seating options
Custom seat cushions and backs provide adapted support to meet an individual’s specific needs. Customized seating systems are essential to provide maximum support, accommodation, and comfort for individuals with moderate to severe deformities. The concerns with custom-molded seating systems is the lack of flexibility for changing postural support needs, the high cost, and the amount of labor to create a customized seating system. An experienced therapist and assistive technology supplier is essential to achieve a successful end product with this level of seating system.
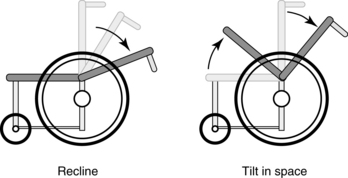
In addition to the primary support surface contours, the angles and degree of postural support from gravity are major considerations. Two dynamic seating system options available are recline and tilt-in-space seating systems. Both of these systems can position a person posterior from the upright, 90-degree sitting for postural support from gravity. A recline seating system is one in which the back support can be shifted backward or forward for varying levels of support and upright posture (Fig. 26-7). A tilt-in-space seating system is one in which the whole seating system (cushion and back support) tilts backward for increased postural support from gravity. Both of these systems can provide individuals with increased postural support and a method of pressure distribution through movement of the seating system. A recliner or a tilt-in-space wheelchair is often beneficial for individuals who need moderate to maximal support for upright sitting. These seating system options are available in both manual and power wheelchairs. With a manual seating system, a caregiver is essential to perform the movement. A power-operated seating system can provide an individual in the wheelchair with the ability to shift position independently for pressure distribution, increase postural support due to fatigue, decrease postural support for more upright seated functioning (i.e., feeding), or meet varying environmental demands (i.e., increased recline for improved support when descending a ramp).
The concept of reclining the back of the seating system or slightly tilting the seating system can be performed in 5- to 15-degree ranges in a standard wheelchair through add-on back supports and/or seat wedges. This is often necessary to accommodate hip range limitations or provide an individual with improved postural support and balance to function upright against gravity. One consideration is that this is a fixed, stationary position in a standard wheelchair. The stability of a recliner or tilt-in-space wheelchair that is specifically designed for tilt or recline is essential for this position to be a dynamic seating function.
Table 26-2 describes a variety of seating system products and secondary support products for seating systems and depicts the seating component, its indications for use, considerations for use, and the functional benefit.
Fitting the person based on functional status
The following list addresses body structures and the seating components that can be used for individuals with hemiplegia and flexible deformities. This list encompasses individuals who have a wide range of functional abilities. One concept that is present throughout neurological rehabilitation and seating and positioning is to always provide proximal support first and then support distally. An example of this concept with an upper extremity support is to provide sufficient trunk support first, before supporting the upper extremity on a half-lap tray. This is essential to minimize the risk of injury to the shoulder girdle.
 Pelvic positioning: Wheelchair upholstery stretches over time; consequently, the sling facilitates poor postural alignment with a posterior pelvic tilt, a pelvic obliquity, and lower extremity adduction and internal rotation. A cushion with a solid base of support (such as a wood insert) is highly recommended to provide a firm and level base of support for the pelvis on the sling wheelchair seat. This is essential for all individuals at various stages of the rehabilitation process. Initially, the support can facilitate carryover of rehabilitation restoration goals and later can provide a seating surface for upright functioning at a wheelchair level.
Pelvic positioning: Wheelchair upholstery stretches over time; consequently, the sling facilitates poor postural alignment with a posterior pelvic tilt, a pelvic obliquity, and lower extremity adduction and internal rotation. A cushion with a solid base of support (such as a wood insert) is highly recommended to provide a firm and level base of support for the pelvis on the sling wheelchair seat. This is essential for all individuals at various stages of the rehabilitation process. Initially, the support can facilitate carryover of rehabilitation restoration goals and later can provide a seating surface for upright functioning at a wheelchair level.
 Lower extremity positioning: The affected side is typically postured in a position of hip adduction and internal rotation.2 This posture can be decreased significantly with a mild contoured cushion and a solid insert. For individuals with more significant spasticity and lower extremity adduction, postural support via gravity through tilt, a padded pelvic belt, hip guides, and a medial knee support should be considered. For individuals with severe adduction and internal rotation, medial knee blocks are necessary to minimize the risk for hip dislocation.
Lower extremity positioning: The affected side is typically postured in a position of hip adduction and internal rotation.2 This posture can be decreased significantly with a mild contoured cushion and a solid insert. For individuals with more significant spasticity and lower extremity adduction, postural support via gravity through tilt, a padded pelvic belt, hip guides, and a medial knee support should be considered. For individuals with severe adduction and internal rotation, medial knee blocks are necessary to minimize the risk for hip dislocation.
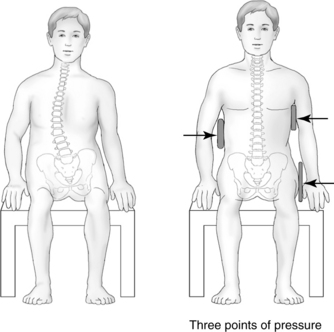
 Trunk: The affected hemiplegic side typically postures with lateral trunk flexion.5 The lateral trunk flexion is often a consequence of decreased pelvic alignment. Optimal pelvic positioning with a good cushion and sacral support with a mild contoured back support can significantly decrease or fully correct the lateral trunk flexion. For individuals with severe weakness, hip guides and a build-up in the cushion can compensate for asymmetrical muscle loss and provide optimal pelvic alignment. In addition, lateral trunk supports can be added as needed to support the body in alignment. Three points of control are essential for optimal trunk support. Fig. 26-8 shows placement of these supports. It is important to remember that a fixed deformity is supported to minimize the risk of increased deformity. A flexible deformity can be “corrected”; however; the therapist should monitor an individual’s tolerance of this correction.
Trunk: The affected hemiplegic side typically postures with lateral trunk flexion.5 The lateral trunk flexion is often a consequence of decreased pelvic alignment. Optimal pelvic positioning with a good cushion and sacral support with a mild contoured back support can significantly decrease or fully correct the lateral trunk flexion. For individuals with severe weakness, hip guides and a build-up in the cushion can compensate for asymmetrical muscle loss and provide optimal pelvic alignment. In addition, lateral trunk supports can be added as needed to support the body in alignment. Three points of control are essential for optimal trunk support. Fig. 26-8 shows placement of these supports. It is important to remember that a fixed deformity is supported to minimize the risk of increased deformity. A flexible deformity can be “corrected”; however; the therapist should monitor an individual’s tolerance of this correction.
 Upper extremity: If a client has mild limitations, active use is encouraged. If an individual has significant weakness, the affected upper extremity requires adequate scapula and glenohumeral support and thus stability from a lap tray or arm trough to minimize the risk for increased pain and subluxation. Appropriate positioning is essential to facilitate optimal upper extremity alignment and motor return, and to maximize function. For a paretic upper extremity, optimal upper extremity alignment is with the shoulder in 5 degrees of abduction and flexion with neutral rotation, the elbow in 90 degrees of flexion and positioned slightly forward of the shoulder joint, the forearm in a neutral or pronated position, and the hand in a functional resting position. Functional hand splints are often integrated into the seating system for optimal wrist and hand support with the forearm supported on a lap tray. More aggressive supports and straps may be used for individuals with more severe spasticity.
Upper extremity: If a client has mild limitations, active use is encouraged. If an individual has significant weakness, the affected upper extremity requires adequate scapula and glenohumeral support and thus stability from a lap tray or arm trough to minimize the risk for increased pain and subluxation. Appropriate positioning is essential to facilitate optimal upper extremity alignment and motor return, and to maximize function. For a paretic upper extremity, optimal upper extremity alignment is with the shoulder in 5 degrees of abduction and flexion with neutral rotation, the elbow in 90 degrees of flexion and positioned slightly forward of the shoulder joint, the forearm in a neutral or pronated position, and the hand in a functional resting position. Functional hand splints are often integrated into the seating system for optimal wrist and hand support with the forearm supported on a lap tray. More aggressive supports and straps may be used for individuals with more severe spasticity.
 Head/neck: Typically, if an individual is seated with a stable base of support at the pelvis and lower extremities and has adequate trunk control or support, the asymmetrical neck posture decreases or disappears. For individuals with moderate to severe involvement who require hip guides and lateral supports, a headrest can be placed on the chair to ensure proper support of the cervical spine and head. After stroke, head support is generally recommended for clients with head/neck weakness, reflex activity, and/or to optimize head positioning to address visual field neglect or other visual-perceptual challenges.
Head/neck: Typically, if an individual is seated with a stable base of support at the pelvis and lower extremities and has adequate trunk control or support, the asymmetrical neck posture decreases or disappears. For individuals with moderate to severe involvement who require hip guides and lateral supports, a headrest can be placed on the chair to ensure proper support of the cervical spine and head. After stroke, head support is generally recommended for clients with head/neck weakness, reflex activity, and/or to optimize head positioning to address visual field neglect or other visual-perceptual challenges.
 Feet: Foot support typically is determined by the person’s functional level. Most individuals with hemiplegia who propel wheelchairs have the best success with propulsion using the unaffected arm and leg. Consequently, the top of the cushion to floor (seat-to-floor height) is a crucial measurement. The seat-to-floor height must allow the person’s heel to access the ground for a successful heel strike to propel the wheelchair effectively. It is also important to consider the depth of the seat cushion. This should be slightly shorter than a client’s seat depth or have an undercut/beveled base of the cushion for adequate freedom of movement. A leg rest or footrest should support the affected lower extremity. In general, individuals with stroke do not benefit from elevating leg rests. Elevating leg rests tend to cause overstretching of the hamstring muscles and facilitate posturing with a posterior pelvic tilt when muscle imbalance or spasticity is present.
Feet: Foot support typically is determined by the person’s functional level. Most individuals with hemiplegia who propel wheelchairs have the best success with propulsion using the unaffected arm and leg. Consequently, the top of the cushion to floor (seat-to-floor height) is a crucial measurement. The seat-to-floor height must allow the person’s heel to access the ground for a successful heel strike to propel the wheelchair effectively. It is also important to consider the depth of the seat cushion. This should be slightly shorter than a client’s seat depth or have an undercut/beveled base of the cushion for adequate freedom of movement. A leg rest or footrest should support the affected lower extremity. In general, individuals with stroke do not benefit from elevating leg rests. Elevating leg rests tend to cause overstretching of the hamstring muscles and facilitate posturing with a posterior pelvic tilt when muscle imbalance or spasticity is present.
Mobility base considerations
The primary goals are to increase safety and independence with mobility and to provide an efficient method of mobility. The primary goal of the mobility base at the ICF6 activities and participation level is to maximize an individual’s ability to function and interact with the environment. An example of this would be the ability to access a closet for clothing to dress.
Unilateral neglect
Depending on the stroke, some clients present with unilateral neglect at the body structures and function level. This leads to significant challenges with activities and participation. Several studies investigated unilateral neglect and mobility including wheelchair mobility. Qiang and colleagues15 used a wheelchair collision test to assess behavioral unilateral neglect. Their investigation found high test-retest reliability with this as a simple screening test for unilateral neglect.
In addition to the test, several studies investigated the effect of unilateral neglect on mobility. Turton and colleagues18 found that differences in environmental navigation were dependant on their mobility product use. They found that subjects with left side neglect tended to drift to the left with wheelchair use. However, two of the same clients consistently drifted to the opposite side, the right side, when they ambulated. Punt and colleagues14 found that differences in subject’s mobility tendencies with drifting to the ipsilesional versus contralesional side were dependant on the environment. In open spaces, the clients with neglect tended to drift toward the ipsilesional side, and in tighter spaces. clients with neglect tended to drift toward the contralesional side. Both of these studies14,18 have implications in training individuals with neglect for safe mobility using both manual and power wheelchairs. See Chapters 18 and 19.
Manual wheelchair frame styles
Two basic types of manual wheelchair frame styles are available: rigid and folding. Rigid wheelchairs tend to be lighter weight and more maneuverable than their folding counterparts. This is because of fewer moving parts and a shorter base length resulting from the integrated footrest design. Folding wheelchairs are designed with a cross brace that allows the chair to fold in half for transport and storage. The wheelchair style commonly recommended for individuals with stroke is the folding style, which is because the style is traditional and most familiar to medical professionals, can be folded up to store in the corner, fits into certain reimbursement codes, and is recognized easily by the general public.
An individual’s medical condition, functional status, seating system support needs, home environment, method of community mobility, and funding source are important variables that influence the style of wheelchair frame recommended. Wheelchair frames are made of different materials to meet various chair weight requirements. The weight of the wheelchair is important if the person’s strength, endurance, and propulsion abilities are in question. A basic wheelchair is constructed of aluminum, is relatively heavy, and is appropriate for persons who are not active and do not use a wheelchair as their primary means of mobility. These wheelchairs are durable enough for light everyday use and are reasonably priced. Ultra-lightweight wheelchair frames typically are constructed with aircraft aluminum or titanium and are durable but more costly than standard wheelchairs. In general, these wheelchairs are not typically recommended for individuals with stroke, even for individuals who will use a wheelchair for their primary means of mobility. There are many thoughts on why this better quality wheelchair is not recommended, which include the wheelchair code that the principal funding source Medicare has for this level wheelchair and the documentation necessary for this level of wheelchair.
Because of the increased incidence of repetitive stress injuries in individuals who use wheelchairs as their primary method of mobility, a strong case can be made for justification of an ultra-lightweight wheelchair for individuals who have sustained a stroke. For individuals with hemiplegia, trunk weakness and use of one upper extremity for all mobility, transfers, and ADL performance is of great concern. A study by Cowan and colleagues4 focused on novice older adults and found that a more anterior axle position decreased the forces necessary to propel the wheelchair, especially on everyday surfaces such as carpets and ramps. This author feels these results support the use of an ultra-lightweight wheelchair for mobility. Ultra-lightweight wheelchairs typically have an adjustable axle that can be adjusted lower for increased trunk balance and slightly forward for a different center of gravity and an optimal hand-to-wheel relationship. This adjustment can decrease the mechanical forces required for wheelchair propulsion and is essential for energy conservation and adequate joint protection of the upper extremity. For the same reasons, power mobility can be considered as a viable option to preserve upper extremity function and maximize overall functioning and community mobility for individuals who have sustained a stroke.
Fig. 26-9 shows the basic wheelchair frame style. Consideration of frame style, wheelchair accessories, and the seating system is crucial to ensure adequate postural support and maximum function at a wheelchair level.
The following are wheelchair and wheelchair frame features that are important to consider when recommending a folding manual wheelchair.
Wheelchair frame seat-to-floor height
Three common seat-to-floor heights are these (Fig. 26-10):
The seat-to-floor height is the height from the floor to the sling seat of the wheelchair. It is important to remember that the height of the cushion chosen also influences the seat-to-floor height. The wheelchair frame height decision is based on the individual’s lower extremity knee-to-heel measurement and what type of wheelchair propulsion the client uses.
If an individual pushes the wheelchair with both arms or is not independently propelling the wheelchair, the footrest clearance is a major concern. After the client is positioned with good femoral support on the wheelchair cushion, approximately 3 inches of clearance should be between the footplate and the ground. This is essential so that the client can negotiate ramps and uneven surfaces without scraping the footplates on the ground. This seat-to-floor height is often compromised to 2 inches of clearance to allow for improved table and desk access.
If an individual is negotiating the wheelchair with one arm and one foot, then the seat-to-floor height is crucial for comfort of the hemiparetic lower extremity on the foot rest and adequate heel access for propulsion of the wheelchair with one or both lower extremities.3 The individual’s knee-to-heel measurement (taken with shoe on) is generally the exact measurement from the top of the wheelchair cushion to the floor. The wheelchair should not be too high because the client will slide into a posterior pelvic tilt to obtain improved heel contact for efficient mobility.3
Wheel style.
Several styles of inner wheel support structure are available. For the purpose of this chapter, discussion is limited to mag wheels and spoke wheels. Wheel style is chosen based on an individual’s ability to care for and maintain the wheelchair.
The team should consider the following:
 The advantage of mag wheels is that they do not require maintenance. However, they do not have as much shock absorption as spoke wheels and can be slightly heavier.
The advantage of mag wheels is that they do not require maintenance. However, they do not have as much shock absorption as spoke wheels and can be slightly heavier.
 Spoke wheels are lighter than mag wheels; however, they require periodic tightening of the individual spokes. A local bicycle shop can perform this adjustment.
Spoke wheels are lighter than mag wheels; however, they require periodic tightening of the individual spokes. A local bicycle shop can perform this adjustment.
Rear wheel size.
Wheelchair wheels are measured from the ground to the top of the wheel. They are available in 12-, 20-, 22-, 24-, 25-, and 26-inch diameters. For individuals with stroke, the seat-to-floor height needs of the individual primarily determines the size of the rear wheel.
Tire style.
Numerous tire options are available; however, for simplicity this section focuses on the types of tires available for standard, folding wheelchairs: pneumatic, pneumatic with flat-free inserts, and polyurethane.
The team should consider the following options:
 Pneumatic tires provide a smoother ride because of good shock absorption ability. The traction of the tires provides good wheelchair stabilization for safety with transfers, and the tires handle varying terrain better than the other two options. The disadvantages are maintenance of air pressure and the risk of a flat tire.
Pneumatic tires provide a smoother ride because of good shock absorption ability. The traction of the tires provides good wheelchair stabilization for safety with transfers, and the tires handle varying terrain better than the other two options. The disadvantages are maintenance of air pressure and the risk of a flat tire.
 Pneumatic tires with flat-free inserts are pneumatic tires with an insert to replace the air. This eliminates the need for air pressure maintenance and the possibility of flats. The benefit of this combination is the traction of the tire that results in increased stability of the wheelchair for safe transfers. Unfortunately, the flat-free inserts decrease the shock absorption potential and add weight to the tire.
Pneumatic tires with flat-free inserts are pneumatic tires with an insert to replace the air. This eliminates the need for air pressure maintenance and the possibility of flats. The benefit of this combination is the traction of the tire that results in increased stability of the wheelchair for safe transfers. Unfortunately, the flat-free inserts decrease the shock absorption potential and add weight to the tire.
 Polyurethane tires are the least expensive and are durable; however, they are heavier than pneumatic tires, provide no shock absorption, and handle varying terrain poorly. In addition, the smoothness of the tire does not provide any traction of the wheelchair wheel on smooth flooring. Often these tires are the reason wheelchairs slide when persons transfer to and from them.
Polyurethane tires are the least expensive and are durable; however, they are heavier than pneumatic tires, provide no shock absorption, and handle varying terrain poorly. In addition, the smoothness of the tire does not provide any traction of the wheelchair wheel on smooth flooring. Often these tires are the reason wheelchairs slide when persons transfer to and from them.
Wheel handrims and one-arm drive wheelchairs.
Handrims are the circumferential rim on the outside of the tire to allow stroking and propulsion of the wheel. Hand rims are available in aluminum, plastic-coated, or projection styles. One-arm drive wheelchairs have two hand rims on one wheel only (Fig. 26-11).
The team should consider the following options:
 Aluminum or composite hand rims are standard on most wheelchairs. Aluminum hand rims can become slippery or cold in different weather conditions. As a result, most active wheelchair users wear specific gloves to compensate for this.
Aluminum or composite hand rims are standard on most wheelchairs. Aluminum hand rims can become slippery or cold in different weather conditions. As a result, most active wheelchair users wear specific gloves to compensate for this.
 Plastic-coated hand rims are beneficial for individuals with decreased grasp. The plastic coating provides traction against an individual’s hand or a Dycem glove. The one disadvantage is that individuals cannot let the rim run through their hands as they descend hills and ramps because the friction will burn the skin on their hands.
Plastic-coated hand rims are beneficial for individuals with decreased grasp. The plastic coating provides traction against an individual’s hand or a Dycem glove. The one disadvantage is that individuals cannot let the rim run through their hands as they descend hills and ramps because the friction will burn the skin on their hands.
 Projection handrims are occasionally used for individuals with decreased grasp. The disadvantages are that they can increase the overall width of the wheelchair if they are not vertical and the propulsion method is more labor intensive because one has to look continually at the handrim to hit the projection.
Projection handrims are occasionally used for individuals with decreased grasp. The disadvantages are that they can increase the overall width of the wheelchair if they are not vertical and the propulsion method is more labor intensive because one has to look continually at the handrim to hit the projection.
One-arm drive wheelchairs have right- and left-hand rims on the same side. This wheelchair was designed for individuals with only one functional upper extremity (see Fig. 26-11). The double hand rim allows one upper extremity to control the wheelchair in all directions. Use of these wheelchairs takes much strength and a high degree of coordination to move straight. In addition, this propulsion method has a longer learning curve because the concept is difficult to master. Mandy and colleagues11 documented the inefficiency of mobility using a one-arm drive wheelchair and investigated an ankle controlled prototype product to increased efficiency with manual wheelchair use. This product demonstrated promising potential for increased efficiency with mobility in a manual wheelchair. However, it is still in the prototype phase and not readily available for purchase at this time. Unfortunately, unilateral hand-foot propulsion or a one-arm drive propulsion style are the only options available for individuals with hemiplegia at this time. Asking an individual to use his or her one functional upper extremity for wheelchair propulsion is an excessive request if one considers that the client also uses this one extremity for all other ADL. The study by Barker colleagues1 study supports this and found the effort to mobilize a manual wheelchair was a contextual barrier for activities and participation. This study supports the concept that a power wheelchair should be strongly considered for independent mobility along with adequate upper extremity joint protection and energy conservation. The increased community participation with power mobility is supported in studies performed by Barker and colleagues1 and Pettersson and colleagues.13
Wheel axle positioning.
Standard wheelchairs allow minimal or no axle adjustment. If a standard wheelchair allows for axle positioning, it only allows the wheel to go up and down in proportion to the front caster to create a hemi- or standard-height wheelchair. On ultra-lightweight wheelchairs, an adjustable wheel axle plate allows for wheel positioning up and down and back and forth.
An adjustable axle position allows the chair to be fine-tuned by adjustment of the wheel to the best position for propulsion. This is essential for optimal wheel set-up for an energy-efficient propulsion stroke4 and for minimizing an individual’s risk for upper extremity repetitive strain injuries. As the wheel is shifted slightly into a forward position, wheel access is improved and propulsion is easier for an individual. This adjustment should be performed with caution as it affects the balance of the wheelchair. One concern is for individuals who have had a lower extremity amputation (because of a compounding diagnosis such as diabetes); the axle is better placed in a rear position to stabilize the wheelchair adequately.
Casters.
Casters are the front wheels of the wheelchair (see Fig. 26-9). They are available in several diameters (3, 4, 5, 6, and 8 inches) and two thicknesses (1 and 1.5 inches).
The team should consider the following:
 Large casters handle uneven terrain and door saddles well; however, they increase the turning radius of the wheelchair and provide higher rolling resistance to the user.
Large casters handle uneven terrain and door saddles well; however, they increase the turning radius of the wheelchair and provide higher rolling resistance to the user.
 Small casters are typical in super low and ultra-lightweight, rigid wheelchairs. They provide the client with a lower front seat-to-floor height and improved maneuverability in small areas. The disadvantage of small casters is that they become stuck in cracks and bumps on sidewalks and streets.
Small casters are typical in super low and ultra-lightweight, rigid wheelchairs. They provide the client with a lower front seat-to-floor height and improved maneuverability in small areas. The disadvantage of small casters is that they become stuck in cracks and bumps on sidewalks and streets.
 Narrow-width casters handle smooth surfaces well but can become stuck easily in uneven terrain.
Narrow-width casters handle smooth surfaces well but can become stuck easily in uneven terrain.
 The 1.5-inch width is available on the 5- and 6-inch diameter casters. This option balances maneuverability and performance over uneven surfaces; the smaller diameter provides improved maneuverability in tight areas and the increased width facilitates transitioning over different surfaces such as door saddles and prevents the casters from getting stuck in sidewalk cracks.
The 1.5-inch width is available on the 5- and 6-inch diameter casters. This option balances maneuverability and performance over uneven surfaces; the smaller diameter provides improved maneuverability in tight areas and the increased width facilitates transitioning over different surfaces such as door saddles and prevents the casters from getting stuck in sidewalk cracks.
Elevating leg rests and footrests.
Elevating leg rests can raise or lower the lower extremities if an individual requires this because of a medical condition (Fig. 26-12). Footrests have a fixed knee angle and support the lower extremity in sitting.
The team should consider the following:
 Elevating leg rests typically are recommended for individuals with limited knee angles (because of arthritis or other orthopedic diagnosis), poor circulation in the lower extremities, or edema. These leg rests typically are overprescribed and should be considered carefully. An elevating leg rest usually protrudes out farther than a footrest. This increases the overall length of the wheelchair and compromises maneuverability. If an individual does not have adequate hamstring muscle elongation to tolerate this large knee angle change, he or she will sit with a posterior pelvic tilt to compensate for the lack of muscle flexibility (Fig. 26-13).9
Elevating leg rests typically are recommended for individuals with limited knee angles (because of arthritis or other orthopedic diagnosis), poor circulation in the lower extremities, or edema. These leg rests typically are overprescribed and should be considered carefully. An elevating leg rest usually protrudes out farther than a footrest. This increases the overall length of the wheelchair and compromises maneuverability. If an individual does not have adequate hamstring muscle elongation to tolerate this large knee angle change, he or she will sit with a posterior pelvic tilt to compensate for the lack of muscle flexibility (Fig. 26-13).9
 The circulation benefits of these leg rests are questionable, since they do not raise the lower extremity above the heart in a standard wheelchair.
The circulation benefits of these leg rests are questionable, since they do not raise the lower extremity above the heart in a standard wheelchair.
 A major disadvantage to elevating leg rests is the significant amount of weight they add to the wheelchair.
A major disadvantage to elevating leg rests is the significant amount of weight they add to the wheelchair.
 Footrests are available in different knee angles, typically 60, 70, and 75 degrees. The angle recommended should be based on the individual’s knee range and hamstring range from the mat evaluation. Proper adjustment of the footrest length is important to ensure lower extremity stability and support in sitting. Swing-away removable footrests enable the footrests to be shifted out of the way for increased safety with transfers and improved table accessibility.
Footrests are available in different knee angles, typically 60, 70, and 75 degrees. The angle recommended should be based on the individual’s knee range and hamstring range from the mat evaluation. Proper adjustment of the footrest length is important to ensure lower extremity stability and support in sitting. Swing-away removable footrests enable the footrests to be shifted out of the way for increased safety with transfers and improved table accessibility.
 A 70-degree angle is usually a standard option and provides a shorter turning radius than a wheelchair with the 60-degree angle footrest.
A 70-degree angle is usually a standard option and provides a shorter turning radius than a wheelchair with the 60-degree angle footrest.
Footplates.
Footplates are available in different materials such as composite and aluminum and are available in different sizes with different angle options: angle adjustable or standard.
Armrests.
Depending on the level of wheelchair, armrests (see Fig. 26-9) are available in different styles: (1) fixed or removable with different height options: fixed and adjustable height, and (2) with two different length options: full and desk length.
The team should consider the following:
 Fixed armrests are welded to the frame and set at a standard height; they cannot be adjusted. This is good for an individual who stands from the wheelchair; however, this design does not work for an individual who needs to transfer sideways to and from the wheelchair.
Fixed armrests are welded to the frame and set at a standard height; they cannot be adjusted. This is good for an individual who stands from the wheelchair; however, this design does not work for an individual who needs to transfer sideways to and from the wheelchair.
 Removable armrests can be positioned out of the way to allow an individual to transfer sideways into and out of the wheelchair. The armrests also can be removed from the wheelchair frame for more compact storage locations such as the trunk of a car.
Removable armrests can be positioned out of the way to allow an individual to transfer sideways into and out of the wheelchair. The armrests also can be removed from the wheelchair frame for more compact storage locations such as the trunk of a car.
 Adjustable-height armrests allow for height adjustment to provide sufficient glenohumeral support. This is important for individuals with hemiparesis and shoulder subluxation.
Adjustable-height armrests allow for height adjustment to provide sufficient glenohumeral support. This is important for individuals with hemiparesis and shoulder subluxation.
 Full-length arms provide full arm support at rest and upper extremity support during sit to stand and stand-pivot transfers.
Full-length arms provide full arm support at rest and upper extremity support during sit to stand and stand-pivot transfers.
 Desk-length armrests are shorter. This can provide an individual with the ability to maneuver close to desks and tables for functional activities such as feeding or writing.
Desk-length armrests are shorter. This can provide an individual with the ability to maneuver close to desks and tables for functional activities such as feeding or writing.
Power mobility products
Barker and colleagues1 studied stroke survivors and wheelchair use. They found that a manual wheelchair was actually a contextual barrier for individuals with stroke and power wheelchair use enabled community participation. Studies by Makino and colleagues10 and Mandy and colleagues11 also documented the inefficiency of mobility using current techniques and products (a one-arm drive wheelchair and ipsilateral hand/foot propulsion technique) and investigated different prototype products to increased efficiency with manual wheelchair use. There have been several products developed that show promising potential for increased efficiency with mobility in a manual wheelchair.10,11 However, these products are in the prototype phase, are not necessarily practical for daily use, and are not readily available for purchase at this time. As a result, power mobility appears to be an enabling option for individuals with denser hemiplegia.
Power mobility products frequently are recommended for individuals who do not have the strength, endurance, or coordination to negotiate a wheelchair manually. Power mobility can provide individuals with increased independent and safe mobility within the home and the community. This mobility is essential to provide individuals with increased ability to perform ADL and to perform their life roles. At this time, it is important to note that clients need to present with a basic level of visual-perceptual and cognitive functioning and be available for power wheelchair mobility skills training for a power wheelchair to be a safe method of mobility. The wheelchair industry has progressed significantly in the past 20 years; consequently, a wide array of products now exist to meet the most challenging physical needs. This section gives an overview of power mobility products with a general list of considerations for each option.
Power scooters
Scooters provide individuals who have good balance and upper extremity control with a means of power mobility. They are available in three- or four-wheel bases (Fig. 26-14). Scooters have a long and narrow base, and as a result, they are great for open areas and general outdoor community mobility. They can be disassembled for car transport; however, this is an awkward task to perform and may present an injury risk for the caregiver.
Figure 26-14 Clients are appropriate for power scooters if they have good functional control of their upper extremities, trunk control, and appropriate visual, perceptual, and cognitive skills.
The team should consider the following:
 Scooters generally have mildly contoured seating systems. They are similar to car seats, with a limited number of options. As a result, they cannot provide sufficient postural support for individuals who need a moderate level of trunk support.
Scooters generally have mildly contoured seating systems. They are similar to car seats, with a limited number of options. As a result, they cannot provide sufficient postural support for individuals who need a moderate level of trunk support.
 In general, scooters are long and narrow. As a result, they have a large turning radius and often do not fit and maneuver in well in most apartments and homes.
In general, scooters are long and narrow. As a result, they have a large turning radius and often do not fit and maneuver in well in most apartments and homes.
 Four-wheeled scooters handle outdoor terrain better but are less maneuverable in smaller areas. In addition, they are heavier and therefore are more difficult for a caregiver to break down for car transport.
Four-wheeled scooters handle outdoor terrain better but are less maneuverable in smaller areas. In addition, they are heavier and therefore are more difficult for a caregiver to break down for car transport.
Power wheelchairs
Power wheelchairs are available with a folding frame or a power-base frame with the drive wheel in the front, middle, or rear position. For ease of discussion, power wheelchairs are divided into the front-, center-, and rear-wheel drive bases with the understanding that each of these models can be classified further into a basic-level wheelchair and a power-base wheelchair.
After the therapist determines that an individual has the range of motion to sit in most wheelchair styles and the sufficient visual-perceptual and cognitive level abilities to move safely, the next important consideration is fit of the wheelchair into and within an individual’s home environment. This fit is critical and often influences the type of drive-wheel base selected.
Front-wheel drive wheelchairs.
A front-wheel drive wheelchair is a base with the large drive wheel in the front. This style of wheelchair is a very stable base and is beneficial for individuals with significant hamstring muscle limitations. Accommodation of hamstring tightness in a rear-wheel drive base either places excessive weight on the casters and compromises driving or an individual often has to be positioned high up to keep his feet above the caster wheels. A front wheel drive base is the only base that can accommodate positioning the feet as far back as possible without compromising the seat height and interfering with casters or motors. The team should consider the following:
 A front-wheel drive wheelchair is an excellent option for individuals who have certain environmental limitations. This style of wheelchair is excellent for tight turns into doorways at the end of a hall and maneuvering at a desk, counter, or table.
A front-wheel drive wheelchair is an excellent option for individuals who have certain environmental limitations. This style of wheelchair is excellent for tight turns into doorways at the end of a hall and maneuvering at a desk, counter, or table.
 A portable ramp is necessary for individuals to negotiate curbs or one-step entrances more than 3 inches high.
A portable ramp is necessary for individuals to negotiate curbs or one-step entrances more than 3 inches high.
 Because of the design of this base, turning occurs in the rear, outside of the driver’s visual field. Consequently, an individual requires excellent proprioception to know where the wheelchair is for safe mobility. This wheelchair base generally is not recommended if an individual has visual or cognitive limitations.
Because of the design of this base, turning occurs in the rear, outside of the driver’s visual field. Consequently, an individual requires excellent proprioception to know where the wheelchair is for safe mobility. This wheelchair base generally is not recommended if an individual has visual or cognitive limitations.
Mid-wheel drive wheelchairs.
For the purpose of this chapter, the term mid-wheel drive wheelchair includes center-wheel drive wheelchairs. A mid-wheel drive wheelchair is a wheelchair base that has the drive wheel in the center of the wheelchair with smaller wheels in the front and the rear. This base requires wheels in the front and the back for maximum stability of the wheelchair base. Because the drive wheel is in the middle, this wheelchair usually has the smallest turning radius and is the most maneuverable in tight areas.
The team should consider the following:
 Because of the design of this base, turning occurs at the center, which is the same axis on which the body turns. As a result, some individuals feel that this is an easier drive method to learn; however, one concern is that some of the turning occurs in the rear, outside of the driver’s visual field. Consequently, an individual requires good proprioception to know where the wheelchair is for safe mobility. This wheelchair base generally is not recommended if an individual has more involved visual or cognitive limitations.
Because of the design of this base, turning occurs at the center, which is the same axis on which the body turns. As a result, some individuals feel that this is an easier drive method to learn; however, one concern is that some of the turning occurs in the rear, outside of the driver’s visual field. Consequently, an individual requires good proprioception to know where the wheelchair is for safe mobility. This wheelchair base generally is not recommended if an individual has more involved visual or cognitive limitations.
 A portable ramp is necessary for individuals to negotiate curbs or one-step entrances more than 3 inches high.
A portable ramp is necessary for individuals to negotiate curbs or one-step entrances more than 3 inches high.
Rear-wheel drive wheelchairs.
A rear-wheel drive wheelchair is the original style of power wheelchair in the United States. Because the drive wheel is in the rear position, most of the weight of the wheelchair is in the rear. As a result, this style of wheelchair has small “anti-tipper” wheels in the back for maximum safety ascending inclines.
The team should consider the following:
 This wheelchair base maneuvers similar to a car, and consequently, many individuals find the drive familiar and, as a result, the wheelchair easy to operate.
This wheelchair base maneuvers similar to a car, and consequently, many individuals find the drive familiar and, as a result, the wheelchair easy to operate.
 This wheelchair base is easier to control at higher speeds than the comparable front-wheel drive and mid-wheel drive models.
This wheelchair base is easier to control at higher speeds than the comparable front-wheel drive and mid-wheel drive models.
 Because of the design of this wheelchair base, the turning wheels are in front of the driver. As a result, all turns happen within the driver’s visual field. This is the optimal situation for individuals with sensory (auditory), visual, or cognitive limitations because this base provides the driver with the maximum amount of visual input about the environment they are negotiating.
Because of the design of this wheelchair base, the turning wheels are in front of the driver. As a result, all turns happen within the driver’s visual field. This is the optimal situation for individuals with sensory (auditory), visual, or cognitive limitations because this base provides the driver with the maximum amount of visual input about the environment they are negotiating.
 Because of the design of this wheelchair base, the footrests have to be positioned in front to allow the casters to turn. This increases the overall length of the wheelchair and results in a larger turning radius. Consequently, a rear-wheel drive base is not as maneuverable in tight areas as a mid-wheel drive base.
Because of the design of this wheelchair base, the footrests have to be positioned in front to allow the casters to turn. This increases the overall length of the wheelchair and results in a larger turning radius. Consequently, a rear-wheel drive base is not as maneuverable in tight areas as a mid-wheel drive base.
 This wheelchair base can be assisted up an 8-inch step and curbs, if necessary. If a rear-wheel drive wheelchair is tipped back onto the tippers, the amount of caster clearance determines the actual height one can negotiate with assistance of another person. This is important for one-step entrances and curbs that are 6 to 8 inches in height. This feature is not a luxury but a necessity for individuals to access their favorite restaurants and stores without a ramp. This is an advanced skill and should only be performed with a skilled therapist or supplier.
This wheelchair base can be assisted up an 8-inch step and curbs, if necessary. If a rear-wheel drive wheelchair is tipped back onto the tippers, the amount of caster clearance determines the actual height one can negotiate with assistance of another person. This is important for one-step entrances and curbs that are 6 to 8 inches in height. This feature is not a luxury but a necessity for individuals to access their favorite restaurants and stores without a ramp. This is an advanced skill and should only be performed with a skilled therapist or supplier.
Basic power wheelchair
A basic power wheelchair is durable and can handle relatively level terrain. Most basic power wheelchairs operate by joystick. The joystick controls the speed and direction of the wheelchair. Some basic power wheelchairs can even be folded for car transport.
The team should consider the following:
 Basic power wheelchairs have basic electronics with little programmability. Consequently, if an individual requires a higher degree of electronics adjustments because of tremors, spasticity, or ataxia, a power base with more flexible electronics may be indicated.
Basic power wheelchairs have basic electronics with little programmability. Consequently, if an individual requires a higher degree of electronics adjustments because of tremors, spasticity, or ataxia, a power base with more flexible electronics may be indicated.
 If an individual requires a moderate or aggressive level of postural support, including a tilt or recline seating system, this wheelchair base would not meet that person’s needs.
If an individual requires a moderate or aggressive level of postural support, including a tilt or recline seating system, this wheelchair base would not meet that person’s needs.
 Because of its folding crossbar and flexible frame, a power folding frame does not handle terrain as well as a power base. However, for basic power mobility, the model is an efficient and reasonably priced alternative.
Because of its folding crossbar and flexible frame, a power folding frame does not handle terrain as well as a power base. However, for basic power mobility, the model is an efficient and reasonably priced alternative.
 Power folding frames are practical in theory but not in reality. Although the frame can be folded by pulling out the batteries and battery tray, the wheelchair components are still heavy and awkward. Two strong adults can lift the folded power frame in and out of a van or car; however, daily use with one person assisting the individual with a stroke is difficult and unrealistic.
Power folding frames are practical in theory but not in reality. Although the frame can be folded by pulling out the batteries and battery tray, the wheelchair components are still heavy and awkward. Two strong adults can lift the folded power frame in and out of a van or car; however, daily use with one person assisting the individual with a stroke is difficult and unrealistic.
Power wheelchair bases.
Power wheelchair bases are much more durable than basic power wheelchair frames. The frame style is more rigid, which translates into increased durability, increased ability to handle uneven terrain, and a smoother ride. In addition, the base style wheelchairs are often available with the option for more advanced, higher-level electronics and the option for a more supportive seating system such as a tilt or recline seating system.
The team must consider that power bases cannot be disassembled for car transport. As a result, these individuals would need access to transportation by a bus, ambulette, or accessible van.
Power wheelchair options.
For most power wheelchairs, a wide array of joystick handle and joystick mounting options are available to position the joystick in the best location for an individual with a stroke. These include larger ball joystick handles, built-up cylindrical-type joystick handles, swing-away joystick mounts, and midline joystick mounting brackets.
On power wheelchairs with more advanced electronics, alternative drive methods such as a single-switch scanner, a head array, or a pneumatic controller can be easily set up. These options can enable individuals who do not have the upper extremity control to operate a joystick or modified joystick to maneuver the wheelchair safely and independently.
Review questions
1. What are the most important considerations when recommending a wheelchair and seating system?
2. Why is a mat evaluation an important first step before considering a wheelchair and seating system?
3. What is the treatment approach difference for a fixed versus a flexible deformity?
4. What is a wheelchair contributing factor to sitting with a posterior pelvic tilt?
5. What are the basic differences between a rigid and a folding wheelchair?
6. In addition to the mat evaluation, what are important areas to screen when considering power mobility?
7. What are the differences between a front-wheel drive, mid-wheel drive, and rear-wheel drive power wheelchair?
1. Barker DJ, Reid D, Cott C. The experience of senior stroke survivors. factors in community participation among wheelchair users. Can J Occup Ther. 2006:73;1:18-25.
2. Bergen A. Assessment for seating and wheeled mobility systems. Team Rehab Rep; April 1998, 16.
3. Buck S. Wheelchair propulsion by foot. assessment considerations. Top Stroke Rehabil. 2004:11;4:68-71.
4. Cowan RE, Nash MS, Collinger JL, et al. Impact of surface type, wheelchair weight, and axle position on wheelchair propulsion by novice older adults. Arch Phys Med Rehabil. 2009;90(7):1076-1083.
5. Davies PM. Steps to follow. a guide to the treatment of adult hemiplegia. Heidelberg, Germany: Springer-Verlag. 1985.
6. International classification of functioning, disability and health. ICF short version. Geneva: World Health Organization; 2001.
7. Judai JW. Psychosocial impact of assistive devices in stroke. Atlanta: Proceedings of the twenty-sixth International RESNA Conference on Technology and Disability: Research, Design, Practice, and Policy; June 2003.
8. Kangas KM. The task performance position. providing seating for accurate access to assistive technology. Physical Disabilities Special Interest Section Quarterly. 2000;23;3.
9. Lipka DD. BuyerBeware.com. Physical Disabilities Special Interest Section Quarterly. 2000;23(3):3.
10. Makino K, Wada F, Hachisuka K, et al. Speed and physiological cost index of hemiplegic patients pedaling a wheelchair with both legs. J Rehabil Med. 2005;37(2):83-86.
11. Mandy A, Lesley S. Measures of energy expenditure and comfort in an ESP wheelchair. a controlled trial using hemiplegic users. Disabil Rehabil Assist Technol. 2009:4;3:137-142.
12. National Stroke Association. What is stroke. (website) www.stroke.org/site/DocServer/STROKE_101_Fact_Sheet.pdf?docID=4541, April 11, 2009. Accessed
13. Pettersson I, Ahlstrom G, Tornquiat K. The value of an outdoor powered wheelchair with regard to the quality of life of persons with stroke. a follow up study. Asst Technol. 2007:19;3:143-153.
14. Punt TD, Kitadono K, Hulleman J, et al. From both sides now. crossover effects influence navigation in patients with unilateral neglect. J. 2008:79;4:464-466.
15. Qiang W, Sonoda S, Suzuki M, et al. Reliability and validity of a wheelchair collision test for screening behavior assessment of unilateral neglect after stroke. Am J Phys Med Rehabil. 2005;84(3):161-166.
16. Rudman DL, Heber D, Reid D. Living in a restricted occupational world. The occupational experiences of stroke survivors who are wheelchair users and their caregivers. CJOT. 2006:73;3:141-152.
17. Shea M. A wheelchair cushion insert and its effect on pelvic pressure distribution. Orlando, FL: Proceedings of the twenty-third International RESNA Conference: Technology for the New Millennium; June 2000.
18. Turton AJ, Dewar SJ, Lievesley A, et al. Walking and wheelchair navigation in patients with left visual neglect. Neuropsych Rehabil. 2009;19(2):274-290.
19. Zollars JA. Special seating. an illustrated guide, Minneapolis, MN. Minneapolis, MN: Otto Back Orthopedic Industry. 1996.
Angelo J. Assistive technology for rehabilitation therapists. Philadelphia: FA Davis, 1997.
Axleton P, Chesney D, Minkel, J, et al. The manual wheelchair training guide. Santa Cruz, CA: Pax Press, 1998.
Axleton P, Minkel J, Chesney D. A guide to wheelchair selection. how to use the ANSI/RESNA wheelchair standards to buy a wheelchair. Washington, DC: Paralyzed Veterans of America. 1994.
Bergen AF. Positioning for function. Valhalla, NY: Valhalla -Rehabilitation, 1990.
Carr EK. Positioning of the stroke person. a review of the literature. Int J Nurs Stud. 1992:29;4:355.
Ferido T. Spasticity in head trauma and CVA persons. etiology and management. J Neurosci Nurs. 1988:20;1:17.
Lange ML. Positioning the upper extremities. OT Practice, May 1999.
Lange ML. Power wheelchair access methods. OT Practice. 1999. July/Aug
Lange ML. Tilt in space versus recline. new trends in an old debate. Tech Spec Interest Section Q. 2000:10;2:1-3.
Minkel JL. Sitting solutions. principles of wheelchair positioning and mobility devices. New Windsor, NY: Minkel Consulting. 1996.
Ramsey C. Power mobility access methods. Tech Spec Interest Section Q. 1999;9(3):1-3.
Sparacio J. The effects of seating on upper-extremity function. Tech Spec Interest Section Q. 1999;9(2):1-2.
Sweet-Michaels B. Alternative methods for power wheelchair control. then and now. Tech Spec Interest Section Q. 1999:9;3:1-4.
Taylor SJ. The head control dilemma. Tech Spec Interest Section Q. 1999;9(2):1-3.
Trefler E. Then and now. simulators have evolved from simple positioning chairs into devices with multiple uses and benefits. Is it time your facility purchased one?. Team Rehab Rep, Feb:32, 1999.
US Department of Health and Human Services. In Pressure ulcers in adults. prediction and prevention. Rockville MD: US Department of Health and Human Services. 1992. AHCPR Pub No 92-0050
Vogel B. Maintaining your chair. New Mobility. June:25, 2003.