chapter 19 Treatment of cognitive-perceptual deficits: a function-based approach
After completing this chapter, the reader will be able to accomplish the following:
1. Understand the different approaches to treatment of cognitive and perceptual impairments and be aware of research conducted on each approach.
2. Integrate performance-based assessments to guide intervention planning.
3. Discuss different treatment approaches to individual neurobehavioral impairments.
4. Realize the relevance and importance of occupation-based activities in the treatment of cognitive and perceptual impairments.
Few things are more interesting or frustrating to a therapist than observing a stroke survivor with severe neglect or apraxia attempting unsuccessfully to perform an activity. Cognitive and perceptual (processing) impairments can severely impair a person’s ability to participate in everyday activities. Frequently, the priority for occupational therapists is to determine what can be done to improve the performance in activities for stroke patients with processing impairments.
This chapter focuses on assessment and interventions for those living with functional deficits secondary to cognitive/perceptual impairments. It reviews studies and other literature on treatment approaches and discusses suggestions for treating processing impairments that frequently are found in persons who have sustained a stroke. The reader should review Chapters 17 and 18 for a full overview of this topic.
Neurobehavior
Neurobehavior has been defined as any behavioral response resulting from central nervous system processing. Neurobehavior is considered the basis of performance in activities of daily living (ADL).6 In this chapter, neurobehavior refers to cognitive and perceptual components of behavior, including praxis, attention, memory, spatial relations, sequencing, and problem-solving.
Treatment approaches
Approaches to stroke rehabilitation can be directed at the level of impairment, activity limitations, or participation restrictions. Impairment refers to body dysfunction; activity limitation, to task performance dysfunction; and participation restriction, to problems in life situations. Approaches aimed at the level of participation restrictions have the greatest impact on the stroke survivor’s quality of life.62 Unfortunately, many times in current practice, participation restrictions are deemphasized, whereas impairment or activity limitation is stressed. Therapists must strive to provide service in all three areas of need while promoting issues relevant to the patient’s quality of life. See Chapter 3.
Treatment approaches to perceptual or cognitive impairments generally are classified in one of two categories: (1) the functional or adaptive approach or (2) the remediation or restoration approach.34 The functional or adaptive approach underscores techniques to assist the patient in adapting to deficits, changing the environmental parameters of a task to facilitate function, and using a person’s strengths to compensate for loss of function. Remediation, or restoration, highlights the use of techniques to facilitate recovery of the actual cognitive or perceptual skills affected by the stroke. Each approach has strengths and limitations, and therapists often use both approaches during stroke rehabilitation (Table 19-1).
Table 19-1 Traditional Classifications of Interventions
| REMEDIATION | ADAPTATION |
|---|---|
| Also known as a restorative or transfer of training approach | Also known as a functional approach |
| Focused on the decreasing impairment(s) | Focused on decreasing activity limitations and participation restrictions |
| Focused on the cause of the functional limitation. Assumes cortical reorganization takes place | Focused on the symptoms of the problem |
| Typically uses deficit-specific cognitive and perceptual retraining activities chosen based on the pattern of impairment | Typically uses practice of functional activities chosen based on what the person receiving services wants to do, needs to do, or has to do in his or her own environment |
| Examples of interventions: cognitive and perceptual table-top “exercises,” parquetry blocks, specialized computer software programs, cancellation tasks, block designs, pegboard design copying, puzzles, sequencing cards, gesture imitation, picture matching, design copying | Examples of interventions: meal preparation, dressing, generating a shopping list, balancing a checkbook, finding a number in the phonebook, environmental adaptations (i.e., placing all necessary grooming items on the right side of the sink for a person with neglect), compensatory strategy training approaches (i.e., using a scanning strategy such as the “Lighthouse Strategy” to improve attention to the left side of the environment for those living with; an alarm watch to remember to take a medication for those with memory impairment) |
| Requires the ability to learn and generalize the intervention strategies to a real world situation | Using a compensatory strategy requires insight to the functional deficits and accepting that the impairment is relatively permanent. Environmental modifications do not require insight or learning on the part of the person receiving services. |
| Assumes that improvement in a particular cognitive-perceptual activity will “carryover” to functional activities | Does not assume that the underlying impairment is even affected by the intervention |
From Gillen, G. Cognitive and perceptual rehabilitation: optimizing function, St. Louis, 2009, Mosby/Elsevier.
Functional/adaptation approach
The functional approach uses repetitive practice in particular activities, usually daily living tasks, to help the patient become more independent. This approach is designed to treat symptoms rather than the cause of the dysfunction.33 Some occupational therapists believe their role in cognitive and perceptual rehabilitation lies solely in the realm of a functional approach, involving training in compensatory techniques and only with tasks directly related to functional performance.76 This approach appears most compatible with research indicating that family members and financial providers rank independence in ADL as the highest priority for rehabilitation.29,72
Therapists use the functional approach to train patients to function by compensating. An example of compensation is the use of an alarm watch to remind someone with poor memory to take medication. Compensation circumvents the problem. Some therapists believe the use of compensation should be limited to patients who have accepted the permanence of the perceptual or cognitive deficit.77 Only persons who can benefit from compensation should be taught these strategies; they must have a basic understanding of their skills and the permanence of their limitations because the use of compensation for disability requires that the individual recognize the need to compensate. The patient must be a self-starter, must be goal directed, have insight/awareness of the functional consequences of his or her impairments, and must want to learn new strategies. Successful compensation requires practice, repetition, and overlearning of the strategies.116
Environmental adaptation is more appropriate for those who cannot use compensatory strategies because of poor insight of disability. Adaptation involves changing the characteristics of the task or environment. This technique is used in patients with poor learning potential. An example of adaptation is the use of contrasting colors for a plate and placemat for someone with figure-ground difficulties. Establishing a routine and constant environment with repeated participation in familiar activities is often the most successful strategy for these individuals. The adaptive approach relies on caregivers to implement treatment strategies.116
A significant limitation of the functional approach is the task specificity of the strategies and lack of generalizability to other tasks.25 For example, the use of an alarm timer to take medications on time does not help the patient remember a repertoire of other activities, such as to take a shower, start meal preparation, or get to a doctor’s appointment, unless the patient specifically has been trained to do so.
Remedial approach
Remediation (or restoration or transfer of training) emphasizes restoration of the function or skill lost due to the stroke. Remedial treatment relies on several assumptions: the cerebral cortex is malleable and can adapt, and the brain can repair and reorganize itself after injury. Practice and repetition are assumed to result in learning. In turn, learning results in a more organized, functional system. Another assumption is that table-top activities, such as pegboard tasks or computer activities, directly affect the underlying processing skills required for the patient to perform those activities. The most important assumption is that improved task performance of table-top activities will be carried over to improved performance in functional activities.25,33,67
Although this approach has been successful when used in the initial stages of treatment,33 most studies show only short-term results, generalization only to similar tasks,104 or little effectiveness from remedial training for neurobehavioral impairments.33,44 For this approach to be successful, treatment sessions must be frequent and lengthy.
Neistadt67 believes that only those patients who show transfer of learning to tasks that are different in multiple characteristics are appropriate candidates for the remedial approach to processing impairments. Therapists widely agree that practice of a subcomponent skill, such as problem-solving or attention to task, must occur in multiple contexts for successful transfer of learning.116 According to Neistadt,68 therapists always should train for transfer of skills because the patient’s home environment is always different from the clinical setting. Those who can transfer learning only to similar tasks should be restricted to a functional/adaptive approach to maximize their training potential.66
Recommended approach
Determination of the appropriate treatment approach for the stroke patient with processing impairments relies on the results of the assessment. Important questions include the following:
 Does the patient have the potential to learn?
Does the patient have the potential to learn?
 Is the patient aware of errors during task performance; and if so, does the patient have the potential to seek solutions to those errors?
Is the patient aware of errors during task performance; and if so, does the patient have the potential to seek solutions to those errors?
If the patient has poor learning potential or poor awareness and is unlikely to benefit from the use of cues or task modification, a strictly functional approach involving domain-specific training would be recommended.101 Domain-specific training requires little or no transfer of learning (generalizability) and involves repetitive performance of a specific functional task using a system of vanishing cues. (Vanishing cues are cues that are provided at every step of task performance but then gradually are removed. The goal is to establish a program in which the patient can successfully perform the task with a minimum number of cues.) This type of training is hyperspecific, and the learning associated with it persists only if the task and environmental characteristics remain unchanged.
Traditionally the therapist has used a restorative or functional approach; however, Abreu and colleagues1 have proposed an integrated functional approach to treatment using principles from both approaches simultaneously. In this approach, areas of occupation and context are used to challenge processing skills. Because individuals engage in occupations as integrated wholes—not as separate attention machines, categorizers, or memory coders—treatments that are not aimed at real life contexts are irrelevant to real life. With this integrated functional approach, treatment may be focused on a subcomponent skill such as sustained attention, but daily occupations are used as the modality. For example, a self-feeding task can be used to improve sustained attention to task. Mealtime is often distracting. Eating can be a difficult task if attention deficits are present. A system of vanishing cues and a gradual increase in the amount of environmental distraction can be used to address inattention to task and activity participation.
The use of a functional approach is supported by today’s health care industry, which seeks documentation of patient’s functional competence in ADL. Only cost-effective interventions that directly affect functional status are embraced in today’s health care environment.
Any functional task can be used to address a myriad of neurobehavioral impairments. For occupational therapists to use their skills in activity analysis to evaluate an activity for its effectiveness in addressing particular cognitive or perceptual deficits is imperative. Box 19-1 contains an example of using everyday function to address neurobehavioral performance skills.
Assessment decisions
The assessment of the impact of cognitive and perceptual deficits on daily function is a complex process (see Chapter 18). To increase the efficiency and use of this process, the following recommendations are made:
 As opposed to pen and paper/table-top measures, performance-based assessments are recommended. See Table 19-2 and other samples within this chapter for examples. Pen and paper or “table-top” assessments typically include items that attempt to detect the presence of a particular impairment (i.e., deficit-specific). Test items are usually contrived and are usually nonfunctional tasks such as copying geometrical forms, pegboard constructions, constructing block designs, matching picture halves, drawing tasks, sequencing pictures, remembering number strings, cancellation tasks, identifying overlapping figures, completing body puzzles, etc. It may be argued that this type of test has low ecological validity. Does the ability to sequence a series of picture cards predict the ability to plan, cook, and clean up a family meal? Does failure to accurately create a three-dimensional block design from a two-dimensional cue card mean that an individual will not be able to dress or bathe independently? The use of this type of assessment procedure as the basis for clinical assessment needs to be questioned if the goal of the cognitive and perceptual assessment is to determine if/how impairment(s) will affect functioning in the real world. In contrast, a performance-based test uses functional activities commonly engaged in during daily life as the method of assessment. The use of structured observations to detect underlying impairments is a not only clinically valid 6,84,93,107 but provides the clinician with detailed information regarding how the underlying impairments directly impacts task performance.
As opposed to pen and paper/table-top measures, performance-based assessments are recommended. See Table 19-2 and other samples within this chapter for examples. Pen and paper or “table-top” assessments typically include items that attempt to detect the presence of a particular impairment (i.e., deficit-specific). Test items are usually contrived and are usually nonfunctional tasks such as copying geometrical forms, pegboard constructions, constructing block designs, matching picture halves, drawing tasks, sequencing pictures, remembering number strings, cancellation tasks, identifying overlapping figures, completing body puzzles, etc. It may be argued that this type of test has low ecological validity. Does the ability to sequence a series of picture cards predict the ability to plan, cook, and clean up a family meal? Does failure to accurately create a three-dimensional block design from a two-dimensional cue card mean that an individual will not be able to dress or bathe independently? The use of this type of assessment procedure as the basis for clinical assessment needs to be questioned if the goal of the cognitive and perceptual assessment is to determine if/how impairment(s) will affect functioning in the real world. In contrast, a performance-based test uses functional activities commonly engaged in during daily life as the method of assessment. The use of structured observations to detect underlying impairments is a not only clinically valid 6,84,93,107 but provides the clinician with detailed information regarding how the underlying impairments directly impacts task performance.
The environment chosen to conduct the assessment must be carefully considered. Typically these assessments are conducted in a quiet room, free of distractions. This may be an appropriate starting point, but the findings might underestimate the impairment. Sbordone82 emphasized that the typical assessment environment (a quiet room without environmental distracters) is not the real world. Specific concerns with a typical testing environment include:
 Problems with task initiation, organization, and follow-through are minimized as the clinician provides multiple cues for task progression, and the tests tend to include discrete items that are performed one at a time as opposed to a sequence of events.17
Problems with task initiation, organization, and follow-through are minimized as the clinician provides multiple cues for task progression, and the tests tend to include discrete items that are performed one at a time as opposed to a sequence of events.17Table 19-2 Selected Performance-Based and Self-Report Assessments for Use with Those Experiencing Limitations in Daily Function Secondary to Cognitive and Perceptual Impairments
| INSTRUMENT | INSTRUMENT DESCRIPTION |
|---|---|
| Comprehensive assessments | |
| Árnadóttir Occupational Therapy-ADL Neurobehavioral Evaluation (A-ONE)6,7 See Chapter 18. |
Structured observation of basic ADL including feeding, grooming and hygiene, dressing, transfers, and mobility to detect the impact of multiple underlying impairments Provides information related to how neurobehavioral deficits affect everyday living Includes items related to ideational apraxia, motor apraxia, unilateral body neglect, somatoagnosia, spatial relations dysfunction, unilateral spatial neglect, perseveration, organization and sequencing dysfunction, topographical disorientation, motor control impairments, agnosias (visual object, associative visual object, visual spatial), anosognosia, body scheme disturbances, emotional/affective disturbances, impaired attention and alertness, memory loss, etc. Requires training |
| Assessment of Motor and Process Skills (AMPS)36,37 See Chapter 21. |
An observational assessment used to measure the quality of a person’s ADL assessed by rating the effort, efficiency, safety, and independence of 16 motor and 20 process skill items Includes choices from 85 tasks Provides information related to everyday function Requires training |
| Brief measure of cognitive functional performance | |
| Kettle Test46 | Provides a brief performance-based assessment of an instrumental ADL task designed to tap into a broad range of cognitive skills. The task consists of making two hot beverages that differ in two ingredients (one for the client and one for the therapist). The electric kettle is emptied and disassembled to challenge problem-solving skills and safety judgment, and additional kitchen utensils and ingredients are placed as distracters to increase attention demands. |
| Assessing apraxia | |
| ADL Observations to measure disabilities in those with apraxia106,107 | Structured observation of four activities: washing face and upper body, putting on a shirt or blouse, preparing food, an individualized task chosen by the occupational therapist Scored based on initiation, execution, and control |
| The ADL Test for those with apraxia41 | Observation of spreading margarine on bread, putting on a T-shirt, brushing teeth, or putting cream on hands Scores based on reparable or fatal errors relate to selection of objects, movements, or sequencing |
| Assessing unilateral neglect | |
| Catherine Bergego Scale (CBS)9,18 | Examines the presence of neglect related to direct observation of functional activities such as grooming, dressing, feeding, walking, wheelchair navigation, finding belongings, positioning self in a chair. Has been used as a self-assessment with results compared with therapist’s ratings to objectify anosognosia (awareness) Measures personal and extrapersonal neglect |
| Behavioral Inattention Test (BIT)45,113 | Assessment for unilateral neglect using 6 pen-and-paper tests and 9 behavioral tests. Behavioral tests consist of simulated tasks. |
| Comb and razor/compact test19,64 | Analyzes attention to both sides of the body during hair combing followed by simulating shaving or applying makeup Each task is 30 seconds. |
| Wheelchair collision test75 | The person is asked to propel a wheelchair to pass four chairs arranged in two rows. Screening tool only |
| Baking Tray Task5,99 | Clients are asked to spread out 16 cubes on a 75 × 50 cm board or A4 paper (8.27 × 11.69 inches) “as if they were buns on a baking tray.” Simulated task |
| Fluff test28 | 24 white cardboard circles are adhered to various areas on a person’s clothing (15 on the left side of the body and 9 on the right). The person must find and remove the targets from the clothing. |
| Assessing impairments of attention | |
| Test of Everyday Attention80 | Considered an ecologically valid test of various types of everyday attention such as sustained attention, selective attention, attentional switching, and divided attention Includes several subtests. It is one of the few tests of attention that simulates everyday life tasks. The test is based on the imagined scenario of a vacation trip to the Philadelphia area of the United States. |
| Cognitive Failures Questionnaire21 | Self-report measure of the frequency of lapses of attention and cognition in daily life. Includes items related to memory, attention, and executive dysfunction. |
| Assessing executive function imapirments | |
| Executive Function Performance Test (EFPT)12 | Assesses executive function deficits during the performance of real world tasks (cooking oatmeal, making a phone call, managing medications, and paying a bill). The test uses a structured cueing and scoring system to assess initiation, organization, safety, and task completion and to develop cuing strategies. |
| Multiple Errands Test2,30,58,85 | Tasks include purchasing 3 items, picking up an envelope from reception, using telephone, posting the envelope, writing down four items (i.e., price of a candy bar), meeting assessor, and informing assessor that the test was completed. |
| Behavioural Assessment of Dysexecutive Syndrome (BADS)111,114 | Includes items that are sensitive to those skills involved in problem solving, planning, and organizing behavior over an extended preiod of time. The battery is designed to access capacities that are typically required in everyday living using simulated tasks. It includes the six subtests that represent different executive abilties such as cognitive flexibility, novel problem solving, planning, judgment and estimation, and behavioral regulation. |
| Assessing memory loss | |
| Rivermead Behavioral Memory Test112 | Ecologically valid test of everyday memory. Uses simulations of everyday memory tasks. The original version is used for those with moderate to severe impairments while an extended version is available for those with subtle memory loss. Modifications are available for those with perceptual, language, and mobility impairments. |
| Everyday Memory Questionnaire81,93,95 | Subjective report of everyday memory. A metamemory questionnaire. Self-report or via proxy. |
| Prospective and Retrospective Memory Questionnaire55,88 | Measure of prospective and retrospective failures in everyday life. Self-rated or proxy-rated. Norms are published. |
Treatment considerations
Therapists must consider many factors while preparing a treatment plan. A stroke survivor may not have the same needs as a person with a closed-head injury, encephalitis, or a gunshot wound to the head. All have brain injury, but they have different patterns of behavior and recovery. Likewise, one must remember that no two stroke survivors are alike. Each person with a stroke is a unique individual with special needs, goals, and problems.
Environment
The importance of the environment or setting in which treatment takes place cannot be underestimated. Patients plan and perform ADL differently73 at home than in the clinical setting.69 Exposure to different environments and contexts requires patients to adapt strategies and solve problems,51 leading to greater independence in a variety of situations.
The adaptation of purposeful activities to ensure success is important in occupational therapy (OT). Success depends on the therapist’s ability to analyze the activities and the patients’ strengths, weaknesses, and needs to present the most relevant and challenging activity.
Generalization
One of the biggest challenges to providing interventions to this population is the issue of generalizing or transfer of what is learned in therapy sessions to other real world situations. Examples include generalizing the use of the skills learned on an inpatient rehabilitation related to meal preparation to making a meal at home on discharge, use of a scanning strategy used to read a newspaper article or to locate an item of clothing in a closet, or use of tactile feedback to identify objects on a meal tray or when shopping for grooming items. The consistent perspective on the idea of generalization is that it will not occur spontaneously but will instead need to be addressed explicitly in an intervention plan.66,90,101,102,103
Suggestions have been made in the literature to enhance generalization of cognitive and perceptual rehabilitation techniques:
 Avoid repetitively teaching the same activity in the same environment.101,102,103 Consistently practicing bed mobility and wheelchair transfers in a person’s hospital room does not guarantee that the skill will generalize to the ability to transfer to a toilet in a shopping mall.
Avoid repetitively teaching the same activity in the same environment.101,102,103 Consistently practicing bed mobility and wheelchair transfers in a person’s hospital room does not guarantee that the skill will generalize to the ability to transfer to a toilet in a shopping mall.
 Practice the same strategy across multiple tasks (see Chapter 5). For example, if the “lighthouse strategy” (see later in this chapter) is successfully used during the treatment of an individual with spatial neglect to accurately read an 8½ by 11 inch menu, the same strategy should be consistently and progressively practiced to read a newspaper, followed by reading the labels on spices in a spice rack, followed by a street sign, etc.
Practice the same strategy across multiple tasks (see Chapter 5). For example, if the “lighthouse strategy” (see later in this chapter) is successfully used during the treatment of an individual with spatial neglect to accurately read an 8½ by 11 inch menu, the same strategy should be consistently and progressively practiced to read a newspaper, followed by reading the labels on spices in a spice rack, followed by a street sign, etc.
 Practice the same task and strategies in multiple natural environments.101,102,103 Practice of organized visual scanning for an inpatient should be done in the therapy clinic, in the person’s hospital room, in the facility’s lobby and gift shop, in the therapist’s office, etc.
Practice the same task and strategies in multiple natural environments.101,102,103 Practice of organized visual scanning for an inpatient should be done in the therapy clinic, in the person’s hospital room, in the facility’s lobby and gift shop, in the therapist’s office, etc.
 Include metacognitive training in the intervention plan to improve awareness.
Include metacognitive training in the intervention plan to improve awareness.
Toglia101,102,103 identified a continuum related to the transfer of learning and emphasized that generalization is not an all or none phenomenon. She discussed grading tasks to promote generalization of learning from those that are very similar to those that are very different. Toglia’s101,103 criteria for transfer included:
 Near transfer. Only one to two of the characteristics are changed from the originally practiced task. The tasks are similar, such as making coffee as compared to making hot chocolate or lemonade.103
Near transfer. Only one to two of the characteristics are changed from the originally practiced task. The tasks are similar, such as making coffee as compared to making hot chocolate or lemonade.103
 Intermediate transfer. Three to six characteristics are changed from the original task. The tasks are somewhat similar, such as making coffee as compared to making oatmeal.
Intermediate transfer. Three to six characteristics are changed from the original task. The tasks are somewhat similar, such as making coffee as compared to making oatmeal.
 Far transfer. The tasks are conceptually similar but share only one similarity. The tasks are different, such as making coffee as compared to making a sandwich.
Far transfer. The tasks are conceptually similar but share only one similarity. The tasks are different, such as making coffee as compared to making a sandwich.
 Very far transfer. The tasks are very different, such as making coffee as compared to setting a table.
Very far transfer. The tasks are very different, such as making coffee as compared to setting a table.
Based on her research and review of the literature, Neistadt67 suggested that only those individuals who have the ability to perform far and very far transfers of learning are candidates for the remedial approach to cognitive and perceptual rehabilitation. She suggested that, on the other hand, those who are only capable of near and intermediate transfers of learning are candidates for the adaptive approach, as described earlier. Similarly, near transfers seem to be possible for all individuals regardless of severity of brain damage, while intermediate, far, and very far transfers may be possible only for those with localized brain lesions and preserved abstract thinking, and with those who have been explicitly taught to generalize.67 While these statements should continue to be tested empirically, they give clinicians guidelines related to intervention planning.
Neurobehavioral impairments in the stroke population
Processing impairments in the stroke population are part of an interactive process involving the patient, the activity at hand, and the context in which the task is being performed.103 Cognition and perception are a dynamical process, constantly changing and reacting to internal and external stimuli. Therapists must address neurobehavioral impairments in the context of the situation and according to the person’s needs and goals. This is why a generic, general approach does not work for the patients included in this population.
Neurobehavioral impairments often are noted in stroke survivors. Lesions from a stroke may cause localized loss of function such as language comprehension. More often, strokes cause a variety of neurobehavioral impairments associated with the severity of the infarct. General treatment strategies for persons with cognitive and perceptual impairments after stroke are addressed next. Commonly noted neurobehavioral impairments are discussed individually later in the chapter.
Intervention strategies
Activity processing
Activity processing is especially helpful in cognitive rehabilitation because the therapist discusses the purpose and results of the activity with the patient. The therapists can discern awareness by the patient from feedback provided during and after activity participation. Activity processing enhances the patient’s metacognition (knowledge of one’s own cognitive ability and ability to monitor one’s own performance) and general knowledge. Activity processing emphasizes the purpose of the activity in the rehabilitation process.23 For example, when practicing spatial positioning during a dressing task, the therapists should instruct the patient on the spatial requirements for each step of the activity and the purpose of using the dressing task to improve spatial skills. As the patient performs the task, the patient and the therapist should discuss performance and strategies to perform the activity.
Behavior modification
Use of behavior modification techniques such as prompting, shaping (reinforcing responses that increasingly resemble the sought-after behavior), and contingent reinforcement (reward contingent on an appropriate response) are common in the stroke and/or brain injury population. Behavior modification techniques with intermittent praise and reinforcement to improve independence in daily activity have been successful.43,53
Group treatment
Group treatment in the stroke population is often effective. It can yield situations more like real life, because they are less structured and can generate unpredictable events and provide distractions. In a group, patients can get feedback from their peers (which is often more meaningful), share similar experiences, and exchange problem-solving and coping strategies. Group treatment allows patients to learn from others’ mistakes, practice monitoring their own behavior, and see that their problems are not unique.
Treatment approaches for specific neurobehavioral impairments
Therapists rarely observe perceptual or cognitive deficits in isolation. Usually these deficits overlap and are difficult to interpret because of their complexity. Little research has been conducted or published on outcomes of specific treatment approaches for isolated perceptual and cognitive deficits, with the possible exceptions of memory impairments and unilateral neglect. However, therapists continue to assess these impairments individually, and using a combination of general and specific treatment approaches to neurobehavioral impairments does help sometimes. With this thought in mind, information on distinct treatment approaches related to specific impairments follows.
Decreased awareness
Most authors recommend that self-awareness should be evaluated before initiating an intervention program focused on retraining living skills. Findings from standardized evaluations of self-awareness will clearly guide intervention choices. For example, a person who exhibits insight into an everyday memory deficit may be a candidate for teaching compensatory strategies such as using a diary or notebook However, a person who does not realize he or she is presenting with a severe unilateral neglect may not be able to learn compensatory strategies but may require environmental modifications (e.g., all clothing hung on the right side of the closet) to improve everyday function. In addition, ascertaining the level of insight to a disability is one factor that may determine how motivated one is to participate in the rehabilitation process. In the most simplistic interpretation, one must be aware and concerned about a deficit in everyday function to be motivated to participate in what may be a long and difficult rehabilitation process.
A variety of assessment measures are typically recommended to ascertain a person’s level of self-awareness, including questionnaires (self or clinician rated); interviews; rating scales; functional observations; comparisons of self-ratings and ratings made by others such as significant others, caretakers, or rehabilitation staff; and comparisons of self-ratings and ratings based on objective measures of function or cognitive constructs. In addition, naturalistic observations can provide further information related to how decreased awareness interferes with performance of everyday tasks.
Simmond and Fleming86,87summarized that a comprehensive and clinically relevant assessment should:
 Be preceded by an assessment of intellectual awareness (e.g., the Self-Awareness of Deficits Interview) as intellectual awareness seems to be a prerequisite to online awareness.
Be preceded by an assessment of intellectual awareness (e.g., the Self-Awareness of Deficits Interview) as intellectual awareness seems to be a prerequisite to online awareness.
 Allow a client to rate his or her own performance before, during, and after the assessment.
Allow a client to rate his or her own performance before, during, and after the assessment.
 Use activities that allow enough flexibility to challenge clients.
Use activities that allow enough flexibility to challenge clients.
 Be goal focused. The assessment findings should be used to work toward acceptance of a disability followed by interventions to improve function.
Be goal focused. The assessment findings should be used to work toward acceptance of a disability followed by interventions to improve function.
Sohlberg89 further suggested that five assessment questions should be answered to comprehensively manage a lack of awareness. Sohlberg’s suggestions for resources to answer each question follow as well:
1. What is an individual’s knowledge or understanding of strengths and deficits? Sohlberg suggested gleaning information from standardized questionnaires and rating scales, and interviews with the client and significant others.
2. How much of the problem is denial versus organically-based unawareness? This complicated question may be answered via a review of medical history, cognitive assessment, standardized questionnaires and rating scales, interviews with the client and significant others, observations (strategy use, use of prediction, self-evaluation, and error response), and response to feedback.
3. Is unawareness generalized or modality specific and does it accompany other cognitive impairments? Similar to the previous question, Sohlberg recommended collecting data from multiple sources including a review of medical history, cognitive assessment, standardized questionnaires and rating scales, interviews with the client and significant others, and observations (strategy use, use of prediction, self-evaluation, error response, and response to feedback).
4. Does the individual consciously or unconsciously accommodate changes in functioning? This question may be answered via interviews with the client and significant others, and through observations (strategy use, use of prediction, self-evaluation, error response, and response to feedback).
5. What are the consequences of awareness? Similar to question 4, this may be answered via interviews with the client and significant others, and through observations (strategy use, use of prediction, self-evaluation, error response, and response to feedback).
See Table 19-3 for a summary of assessments used to ascertain level of awareness.
Table 19-3 Recommended Measures of Awareness
| INSTRUMENT AND AUTHOR | VALIDITY | COMMENTS |
|---|---|---|
| Self-Awareness of Deficits Interview38 | Correlated with the Self-Regulation Skills Interview and the Awareness Questionnaire Correlated with work status Discriminates between those with brain injury and spinal injury |
Measures intellectual awareness via a rating scale Rated by clinicians |
| Self-Regulation Skills Interview71 | Discriminates between brain injured and non-brain injured subjects for awareness Correlated with the Self-Awareness of Deficits Interview and Health and Safety Scale Correlated with work status |
Rated by clinicians As area of difficulty is determined by the client, it requires a level of intellectual awareness and includes items related to emergent and anticipatory awareness. |
| Awareness Interview4 | Correlated in the expected direction with the Wechsler Adult Intelligence Scale and measures of temporal disorientation | Measures intellectual awareness via a discrepancy score compared with performance on standardized neurological tests |
| Assessment of Awareness of Disability97,98 | A Rasch analysis suggested acceptable scale validity, construct validity, and person response validity | Used in conjunction with the Assessment of Motor and Process Skills (AMPS) |
Use of prompts and cues is key to successful cognitive and perceptual rehabilitation. Cues can be faded by reducing the number, frequency, or specificity of the prompts.117 For example, a therapist initially may provide detailed cues at every step of task performance, such as “Look to the left to find the soap.” Cues should be tapered and should become less detailed as the patient progresses (e.g., “Have you remembered all the steps?”). Therapists should provide prompts and cues in a calculated and graded fashion. The use of cues and prompts is part of cognitive and perceptual rehabilitation and is an essential way of facilitating patient insight, error detection, and strategy development (Table 19-4). See Box 19-2 for awareness training interventions.
Table 19-4 Prompting Procedures
| PROMPTS | RATIONALE |
|---|---|
| “How do you know this is the right answer/procedure?” or “Tell me why you chose this answer/procedure.” | Refocuses patient’s attention to task performance and error detection. Can patient self-correct with a general cue? |
| “That is not correct. Can you see why?” | Provides general feedback about error but is not specific Can patient find error and initiate correction? |
| “It is not correct because . . .” | Provides specific feedback about error Can patient correct error when it is pointed out? |
| “Try this [strategy]” (e.g., going slower, saying each step out loud, verbalizing a plan before starting, or using a checklist) | Provides patient with a specific, alternate approach Can patient use strategy given? |
| Task is altered. “Try it another way.” | Modifies task by one parameter. Can patient perform task? Begin again with grading of prompting described previously. |
Adapted from Toglia JP: Attention and memory. In Royen CB, editor: AOTA self-study series: cognitive rehabilitation, Rockville, Md, 1993, American Occupational Therapy Association; and Toglia JP: Generalization of treatment: a multicontext approach to cognitive perceptual impairment in adults with brain injury. Am J Occup Ther 45(6):505, 1991.
Box 19-2 Suggestions for Improving Awareness
Have clients perform tasks of interest and then provide them with feedback about their performance. The goal is to have clients monitor and observe their behavior more accurately so that they can make more realistic predictions about future performance and gain insight into their strengths and weaknesses.
Encourage self-questioning during a task and self-evaluation after a task (e.g., “Have I completed all of the steps needed?”).
Provide methods of comparing functioning pre- and postinjury to improve awareness.
Use prediction methods. Have the client estimate various task parameters such as difficulty, time needed for completion, number of errors, and/or amount assistance needed before, during, or after a task and compare with actual results.
Help clients develop and appropriately set their personal goals.
Allow clients to observe their own performance during specific tasks (i.e., via videotape) and compare actual performance to what they state they can do.
Group treatments and peer feedback may be used because one person can receive feedback on performance from multiple individuals.
Use role reversals. Have the therapist perform the task, make errors, and have the client detect the errors.
The development of a strong therapeutic alliance is critical in managing both denial and lack of self-awareness. This alliance should be open and based on trust. Coaching clients to make better choices and understand how defensive strategies affect daily function.
Use familiar tasks that are graded to match the person’s cognitive level (“just the right challenge”) to develop self-monitoring skills and error recognition.
Provide education related to deficit areas for clients and families.
Integrate experiential feedback experiences. This method has been called “supported risk taking” and “planned failures” and is used during daily activities to gently demonstrate impairments. High levels of therapist supported are mandatory during this intervention.
Monitor for increased signs of depression and anxiety as awareness increases.
Increase mastery and control during performance of daily tasks to increase awareness.
Use emotionally neutral tasks to increase error recognition.
Use tasks that offer “just the right challenge” to increase error recognition/correction.
Provide feedback in a sandwich format (negative comments are preceded and followed by positive feedback).
Data from Fleming JM, Strong J, Ashton R: Cluster analysis of self-awareness levels in adults with traumatic brain injury and relationship to outcome. J Head Trauma Rehabil 13(5):39-51, 1998; Klonoff PS, O’Brien KP, Prigatano GP, et al: Cognitive retraining after traumatic brain injury and its role in facilitating awareness. J Head Trauma Rehabil 4(3):37-45, 1989; Lucas SE, Fleming JM: Interventions for improving self-awareness following acquired brain injury. Austr Occup Ther J 52(2):160-170, 2005; Prigatano GP: Disturbances of self-awareness and rehabilitation of patients with traumatic brain injury: a 20-year perspective. J Head Trauma Rehabil 20(1):19-29, 2005; Sherer M, Oden K, Bergloff P, et al: Assessment and treatment of impaired awareness after brain injury: implications for community re-integration. NeuroRehabilitation 10:25-37, 1998; Tham K, Tegner R: Video feedback in the rehabilitation of patients with unilateral neglect. Arch Phys Med Rehabil 78(4):410-413, 1997; Toglia J: A dynamic interactional approach to cognitive rehabilitation. In Katz N, editor: Cognition and occupation across the life span, Bethesda, Md, 2005, AOTA Press; Toglia JP: Generalization of treatment: a multicontext approach to cognitive perceptual impairment in adults with brain injury. Am J Occup Ther 45(6):505-516, 1991; and Toglia J, Kirk U: Understanding awareness deficits following brain injury. NeuroRehabilitation 15(1):57-70, 2000.
Apraxia
According to Ayres,8 praxis is one of the most important connections between brain and behavior; it is what allows persons to interact with the physical world. Apraxia is a dysfunction of purposeful movement that does not result primarily from motor, sensory, or comprehension impairments.6 Although many different types of apraxia have been named and defined, the labels used to classify them are not universally accepted.11 For relevance in this chapter, however, they fit into two general categories: motor and ideational apraxia. See Chapter 18 for examples of how the various types of apraxia affect daily living skills.
Patients with apraxia are often unaware of their deficits,96 creating a dilemma for planning therapeutic interventions. However, one study concluded that patients with more severe cognitive (and motor) impairments showed the most significant improvement in ADL.108 The study demonstrated the obvious potential for improvement with severely apraxic patients using compensatory strategy training for ADL skills and therefore negates the idea that severely apraxic patients have poor potential for improvement. Box 19-3 lists general treatment guidelines for patients with apraxia. See Box 19-4 for a specific example of a performance-based assessment.
Box 19-3 Potential Interventions for Those Living with Functional Limitations Secondary to Apraxia
Use functional tasks (previously learned and new tasks that are necessary to perform secondary to neurological impairments) for the interventions, i.e., an individualized task-specific approach.
“Tap into” an individual’s routines and habits.
Collaborate with the client and his or her significant others/caregivers in order to choose the tasks to focus on and become the goals of therapy, i.e., a client-centered approach.
Practice these activities in the appropriate environments and at the appropriate time of day, i.e., context-specific with full contextual cues.
Use strategy training interventions to develop internal or external compensations during the performance of functional activities.
Focus interventions based on the errors made during the task: initiation, execution, and or control, i.e., error-specific interventions.
Practice functional activities with vanishing cues.
Provide graded assistance via providing graded instructions, assistance, or feedback during task performance.
Practice functional activities using errorless learning (preempting the error via assistance) approaches.
Box 19-4 Assessment of Disabilities in Stroke Patients with Apraxia
Observation and scoring of activities of daily living
Method:
The therapist observes the following activities and scores the findings for each activity and each aspect.
I. score of independence
0—The patient is totally independent, can function without any help in any situation.
1—The patient is able to perform the activity but needs some supervision.
—The patient needs minimal verbal assistance to perform adequately.
—The patient needs maximal verbal assistance to perform adequately.
2—The patient needs minimal physical assistance to perform adequately.
—The patient needs maximal physical assistance to perform adequately.
3—The patient cannot perform the task despite full assistance.
Ii. the course of an activity
In every aspect, the patient can encounter problems; however, for each aspect only one score can be entered.
0—There are no observable problems: the patient understands the instruction and initiates the activity.
1—The verbal instruction has to be adapted or extended.
—The therapist has to demonstrate the activity.
—It is necessary to show pictures or write down the instructions.
—The objects needed to perform the task have to be given to the patient.
2—The therapist has to initiate the activity together with the patient.
—The activity has to be modified in order to be performed adequately.
3—The therapist has to take over.
0—There are no observable problems; the activity is performed correctly.
1—The patient needs verbal guidance.
—Verbal guidance has to be combined with gestures, pantomime, and intonation.
—Pictures of the proper sequence of action have to be shown.
2—The patient needs physical guidance.
3—The therapist has to take over.
0—There are no observable problems; the patient does not need feedback.
1—The patient needs verbal feedback about the result of the performance.
—The patient needs physical feedback about the result of the performance.
2—The patient needs verbal feedback about the execution.
—The patient needs physical feedback about the execution.
From van Heugten C, Dekker J, Deelman B et al: Assessment of disabilities in stroke patients with apraxia: internal consistency and inter-observer reliability. Occup Ther J Res 19(1):55-73, 1999.
If physical guiding of the limbs is used during a task, incorporate the suggested principles of guiding,22 including:
 Place their hands over the patient’s whole hand, down to the fingertips.
Place their hands over the patient’s whole hand, down to the fingertips.
 Guide both sides of the body when possible.
Guide both sides of the body when possible.
 Move along a supported surface to give the patient maximal tactile feedback.
Move along a supported surface to give the patient maximal tactile feedback.
 Involve the whole body in the task to challenge posture.
Involve the whole body in the task to challenge posture.
 Provide changes in resistance during the activity.
Provide changes in resistance during the activity.
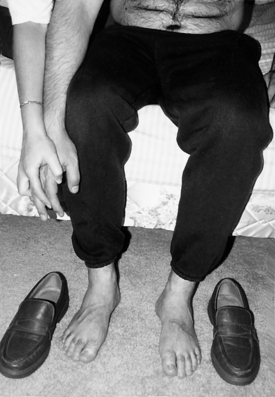
 Allow the patient to make mistakes to give opportunities to solve problems (Figs. 19-1 and 19-2).
Allow the patient to make mistakes to give opportunities to solve problems (Figs. 19-1 and 19-2).
Encourage tactile exploration of functional objects and tools to enhance performance as somatosensory feedback from the tool may play a role in organizing movements.42 Related to the above, object affordances (the functional use of particular objects within a context) positively affects motor performance.42 Using meaningful objects and tasks will yield better results than movements performed in isolation.61 As those with apraxia have compromised learning of old and new tasks, increased repetitions and practice will be necessary. Goals should be scaled accordingly. Encourage practice of learned skills outside of therapy and throughout the day. For those with ideomotor apraxia, experiment with decreasing the degrees of freedom (i.e., number of joints) used to perform the task (i.e., encourage a woman who is attempting to apply makeup to keep her elbow on the table). Grade the number of tools and distracters used in a task (i.e., finger feeding [no tools], followed by eating applesauce with only a spoon available, followed by eating applesauce with the choice of one to three utensils, followed by eating a meal requiring the choice of various tools for different aspects of the task [spoon to stir coffee, knife to cut and spread butter, etc.], followed by a meal with the necessary and usual utensils and distracter tools such as comb and toothbrush).40
 Grade the number of steps of an activity via chaining procedures. The whole task should be completed for each trial.
Grade the number of steps of an activity via chaining procedures. The whole task should be completed for each trial.
 Grade the number of tasks that will be performed in succession such as during a morning routine.
Grade the number of tasks that will be performed in succession such as during a morning routine.
 Use clear and short directions.
Use clear and short directions.
 Use multiple cues to elicit functions: visual demonstration, verbal explanation, tactile guiding.
Use multiple cues to elicit functions: visual demonstration, verbal explanation, tactile guiding.
 Demonstrate the task while sitting parallel to the person with apraxia to help develop a visual model of the task.
Demonstrate the task while sitting parallel to the person with apraxia to help develop a visual model of the task.
Further interventions for apraxia
The following paragraphs summarize evidenced-based interventions for those living with functional limitations secondary to apraxia.
Strategy training.
van Heugten and colleagues105 described an intervention study designed for use by occupational therapists and based on teaching patients strategies to compensate for the presence of apraxia. In addition to interest checklists, the decision as to which activities to focus on was a joint decision between the therapist and patient. The focus of the intervention was determined by the specific problems observed during standardized ADL observations (see Box 19-4). Specifically, interventions focused on errors related to:
 Initiation: inclusive of developing a plan of action and selection of necessary and correct objects
Initiation: inclusive of developing a plan of action and selection of necessary and correct objects
 Execution: performance of the plan
Execution: performance of the plan
 Control: inclusive of controlling and correcting the activity to ensure an adequate result
Control: inclusive of controlling and correcting the activity to ensure an adequate result
Difficulties related to initiation were treated via specific instructions. Instructions were hierarchical in nature and could include verbal instructions, alerting the patient with tactile or auditory cues, gesturing, pointing, handing objects starting the activity together, etc. Assistance was the intervention provided when problems related to execution of the activity occurred. Also hierarchical, assistance could range from various types of verbal assist, stimulating verbalization of steps, naming the steps of the activity, to physical assistance such as guiding movements (see Figs. 19-1 and 19-2). Feedback is provided when patients have difficulty with control (i.e., patients do not detect or correct the errors they make during the activity) and can be verbal feedback related to the results of performance, verbal feedback focused on having the patient use a variety of senses to evaluate the results, or physical feedback focused on knowledge of results. The specific strategy training intervention protocol is included in Box 19-5. The strategy training approach for apraxia has been tested with promising results.32
Box 19-5 Protocol for Strategy Training for Those Living with Functional Deficits Secondary to Apraxia
The specific interventions are built up in a hierarchical order, depending on the patient’s level of functioning. The therapist can use instructions, assistance, and feedback.
Instructions
The occupational therapist can give the following instructions:
 Start with a verbal instruction.
Start with a verbal instruction.
 Shift to a relevant environment for the task at hand.
Shift to a relevant environment for the task at hand.
 Use gestures, point to the objects.
Use gestures, point to the objects.
 Demonstrate (part of) the task.
Demonstrate (part of) the task.
 Show pictures of the activity.
Show pictures of the activity.
 Place the objects near the patient, point to the objects, put the objects in the proper sequence.
Place the objects near the patient, point to the objects, put the objects in the proper sequence.
 Hand the objects one at a time to the patient.
Hand the objects one at a time to the patient.
 Start the activity together with the patient one or more times.
Start the activity together with the patient one or more times.
 Adjust the task to make it easier for the patient.
Adjust the task to make it easier for the patient.
 Finally, take over the task because all efforts did not lead to the desired result.
Finally, take over the task because all efforts did not lead to the desired result.
Assistance
The following forms of assistance can be given by the therapist:
Feedback
Feedback can be offered in the following ways:
 No feedback is necessary because the result is adequate.
No feedback is necessary because the result is adequate.
 Verbal feedback is needed in terms of the result (knowledge of results).
Verbal feedback is needed in terms of the result (knowledge of results).
 Verbal feedback by telling the patient to consciously use the senses to evaluate the result (tell the patient see, hear, feel, smell, or taste).
Verbal feedback by telling the patient to consciously use the senses to evaluate the result (tell the patient see, hear, feel, smell, or taste).
 Physical feedback is needed in terms of the result (knowledge of results):
Physical feedback is needed in terms of the result (knowledge of results):
 Physical feedback is given by pointing or handing the objects to the patient.
Physical feedback is given by pointing or handing the objects to the patient.
 Verbal feedback is needed in terms of performance (knowledge of performance).
Verbal feedback is needed in terms of performance (knowledge of performance).
 Physical feedback is needed in terms of performance (knowledge of performance).
Physical feedback is needed in terms of performance (knowledge of performance).
 Place the patient in front of a mirror.
Place the patient in front of a mirror.
 Make video recordings of the patient’s performance and show the recordings.
Make video recordings of the patient’s performance and show the recordings.
 Take over the control of the task and correct possible errors.
Take over the control of the task and correct possible errors.
From van Heugten C, Dekker J, Deelman B, et al: Outcome of strategy training in stroke patients with apraxia: a phase II study. Clin Rehabil 12(4):294-303, 1998.
A pretest/posttest study design105 demonstrated significant improvements and large effects for three different ADL measures (Barthel Index; a standardized evaluation of personal hygiene, dressing, preparing food, and a patient chosen activity; and an ADL questionnaire that was filled out by both therapists and patients). In addition, significant improvements were documented on tests of apraxia (small to medium effects) and motor function (small effects). Improved ADL function was still significant after correcting for the improvement on the apraxia measures, motor measure, and time poststroke. Of the patients in this study, 84% perceived complete recovery or substantial improvement because of the intervention. While the intervention did not explicitly focus on decreasing the apraxic impairment, the strategy training approach during participation in functional activities decreased both activity limitations and severity of impairment.
Donkervoort and colleagues32 also tested this intervention via a large randomized clinical trial comparing usual OT to strategy training integrated into usual OT. After intervention, those receiving strategy training improved significantly on ADL observations (small to medium effect size) and the Barthel Index (medium effect size) as compared to those who received usual care.
A posthoc analysis of Donkervoort and colleagues data performed by Geusgens and colleagues39 focused on whether or not the strategy training approach resulted in transfer of training to untrained tasks. The analyses revealed that both intervention groups (traditional OT and traditional OT combined with strategy training) demonstrated significantly improved scores on nontrained tasks. Change scores of the nontrained activities were significantly larger in the strategy training group as compared to usual OT.
Errorless completion and training of details.
Goldenberg and Hagman42 tested a method of specifically training ADL for those living with apraxia. They specifically examined spreading margarine on a slice of bread, putting on a T-shirt, and brushing teeth or applying hand cream. When an activity was being trained, the focus was on errorless completion of the whole activity. As opposed to trial and error learning, errorless learning or completion is a technique in which the person learns the activity by doing it. The therapist intervenes to prevent errors from occurring during the learning process. Specific interventions included:
 Guiding the hand through a difficult aspect of the activity (see Figs. 19-1 and 19-2)
Guiding the hand through a difficult aspect of the activity (see Figs. 19-1 and 19-2)
 Sitting beside the patient (parallel position) and doing the same action simultaneously with the patient
Sitting beside the patient (parallel position) and doing the same action simultaneously with the patient
 Demonstrating the required action and asking the patient to copy it afterwards
Demonstrating the required action and asking the patient to copy it afterwards
In addition, the intervention focused on training of details. This was aimed at directing the patient’s attention to “the functional significance of single perceptual details and to critical features of the actions associated with them” (p.133).42 Specific difficult steps of the activity were trained using this approach. To promote knowledge of object use, key details of ADL objects, such as the bristles on a toothbrush and the teeth on a comb, were explored and examined. Actions connected to the details were then practiced (i.e., searching for and positioning a shirt sleeve for a person with dressing difficulties) outside of therapy. Specific necessary motor actions were also practiced in other activities and contexts (i.e., squeezing paint from tubes as a similar action as squeezing toothpaste).
Goldenberg and Hagman42 tested this intervention by examining 15 patients with apraxia with repeated measures of ADL function. Success of therapy was based on the reduction of errors of specific tasks. The authors differentiated between reparable errors (the patients succeeds in continuing the task) or fatal errors (the patient is unable to proceed without help, or the task is completed but did not fulfill its purpose). Across the whole group, the number of fatal errors decreased significantly while the number of reparable errors did not significantly change.
Direct training of the whole activity versus exploration training.
Goldenberg and colleagues41 developed and compared two therapy interventions aimed at restoring the ability to engage in complex ADL for those living with apraxia. Exploration training focused on having patients infer function from structure and solve mechanical problems embedded in tasks. During treatment, the therapist directed the patient’s attention to functionally significant details of the object (i.e., prongs on a fork, serrations on a butter knife, bristles on a toothbrush). The therapist explained the functional significance via verbal, gestural, and pointing cues. The patients did not practice use of the tools. Specific interventions related to exploration training included explanation, touching, and comparing objects with photographs.
The direct training focused on the patient carrying out the whole activity with a minimum of errors. The technique is similar to errorless completion as reviewed previously and includes guided movements, with the therapist sitting beside the patient to perform the task simultaneously. During the training, particularly difficult components of the activity were practiced, but the whole activity was always completed. Specific interventions for direct training included guided performance of the whole activity, passive guidance, guidance by example, and rehearsal of steps.
Goldenberg and colleagues41 tested these interventions related to the training of four complex ADL. The authors found that exploration training had no effect on performance, while direct training resulted in a significant reduction of errors and the amount of assist required to complete the task. Follow-up three months later revealed that gains were maintained.
Task-specific training.
Poole74 examined the ability of those living with apraxia to master the technique of one-handed shoe tying (commonly a necessary skill to be mastered after brain injury). She compared those living with a stroke without apraxia, those living with stroke with apraxia, and healthy adults. The task was taught using published standardized procedures via demonstration and simultaneously verbalizing instructions. Repetition was used until the task was achieved. The mean number of trials to learn the task was higher for those with apraxia (M =6.4) as compared to those stroke survivors without apraxia (M =3.2) versus healthy controls (M =1.2).While the number of trial required to learn the task was greater, the majority of those with apraxia were able to retain the task.
Wilson110 documented a task-specific training program for a young woman status post an anoxic brain injury. The program focused on two tasks: drinking from a cup and sitting on a chair followed by positioning it correctly at the table. Functional performance was improved for this woman via the techniques of breaking down the steps of the tasks followed by practice of the steps, chaining procedures, and verbal mediation. The author noted that generalization to untrained tasks was not evident.
Perseveration
Perseveration is demonstrated by the inability to shift from one concept to another or to change or cease a behavior pattern once having started it. Perseveration also refers to the inability to translate knowledge into action (initiation of a task). The person is “stuck in set”—unable to discard the previous set of behaviors—or is unable to “activate” for a new situation. The person stuck in set attempts to solve another problem with information relevant to a previous problem.
Bringing perseveration to a conscious level and training the patient to inhibit the perseverative behavior has been successful.48 Other strategies include redirecting attention, assisting the patient in initiating a new movement or task, and engaging the patient in tasks that involve repetitive action (e.g., washing the face or body, stirring food, or sanding wood) to promote successful task participation.
Unilateral neglect
Unilateral neglect has been defined as “the failure to report, respond, or orient to novel or meaningful stimuli presented to the side opposite a brain lesion, when this failure cannot be attributed to either sensory or motor defects.”47 Unilateral neglect is most often seen when right-side brain damage occurs; therefore, the most frequent clinical presentation is that of left unilateral neglect. Although the mechanisms underlying neglect are still debated, a common hypothesis is that neglect is related to attention-based impairments and has been described as a lateralized attention deficit. Behaviors observed during everyday activities lend support to the attentional hypothesis, including the following:
 Not being aware of incoming stimuli on the side opposite the brain lesion (e.g., hypoattentive to the left side)
Not being aware of incoming stimuli on the side opposite the brain lesion (e.g., hypoattentive to the left side)
 A bias in attention to information presented on same side of the lesion (e.g., hyperattentive to the right side)
A bias in attention to information presented on same side of the lesion (e.g., hyperattentive to the right side)
The fact that those living with neglect most often present with left neglect also supports the attentional hypothesis because the right hemisphere is thought to be dominant for attention. That being said, right unilateral neglect is possible.92 Beis and associates15 documented right neglect in 10% to 13.2% of those they examined. They concluded that right neglect caused by left hemispheric involvement is an elusive phenomenon and is less consistent than right hemispheric neglect. In addition, the frequency of occurrence of right neglect was, as expected, much lower than that reported in a study using the same assessment battery in right brain damage stroke clients.
Unilateral neglect can present with or without a concurrent visual field cut (see Chapter 16 and Table 19-5). In addition, neglect can interfere with attending to personal space (body neglect), near space, and/or far space (Table 19-6). Therefore, the recommended assessment method is a performance-based approach to give the therapist multiple opportunities to evaluate the impact of neglect on tasks that occur in the various aspects of space. Examples include the A-ONE (see Chapter 18) and the Catherine Bergego Scale (Fig. 19-3). Evidenced interventions to decrease the functional impact of neglect include the following.
Table 19-5 Suggestions to Differentiate between Neglect and Visual Field Loss Based on Analysis of Behaviors
| VISUAL FIELD LOSS | NEGLECT |
|---|---|
| Objectively tested via confrontation testing (screening) or via formalized perimetry testing (see Chapter 16) | Objectively tested using a battery of assessments to identify body/personal, extrapersonal (near and far), and motor neglect |
| Awareness of deficits emerge early in the recovery process. | Lack of awareness is more severe and persistent. |
| Compensatory strategies such as head turning are observed early and relatively easily taught. | Compensatory interventions are difficult, may require multiple sessions, or may not be effective. |
| Postural alignment is usually not affected. | Postural alignment of the head, neck, and trunk may bias toward the right side. |
| Sensory-based deficit | Attention-based deficit |
| Visual deficit only | Multiple sensory systems may be involved (visual, auditory, tactile). |
| Effective compensatory strategies result in positive functional outcomes. | Functional outcomes tend to be poor as compared to those without neglect. |
| Cortical representation of the “whole real world” is intact. | Decreased representation of the left side of space while describing a room from memory |
| Movement into both hemifields is not affected. | Resistance to moving actively (akinesia) or passively into the left field Long delays related to moving into the affected field (hypokinesia) |
| Extinction is not present. | Extinction may be present. |
| Early leftward eye movements noted | Rightward-biased eye movements |
| Not fully effective but consistent scanning patterns | Haphazard scanning patterns biased to the right |
| Comparatively, not as severe a deficit | A severe deficit related to functional outcome, rehabilitation needs, and caregiver burden |
Table 19-6 Spatial Aspects of Neglect during Functional Activities*
| TYPE OF NEGLECT | FUNCTIONAL ACTIVITY DIFFICULTIES |
|---|---|
| Personal or body neglect | Does not shave left side of face Does not comb left side of head Does not apply makeup to left side of face Does not wash or dry left side of body Does not integrate left side of body during bed mobility and transfers Does not use left side of body |
| Near extrapersonal (peripersonal [within arms’ reach]) neglect | Cannot find objects on left side of sink Cannot find objects on left side of desk Inability to read Inability to locate numbers on the left side of the phone Does not eat food on left side of the plate Cannot find wheelchair brakes on left side of the chair |
| Far extrapersonal neglect | Cannot locate clock on left side of wall Gets lost easily during ambulation or wheelchair mobility Cannot navigate doorways Difficulty watching TV Cannot locate source of voices |
* Spatial neglect includes both near and far extrapersonal space.
From Gillen G: Cognitive and perceptual rehabilitation: optimizing function, St. Louis, 2009, Mosby/Elsevier.
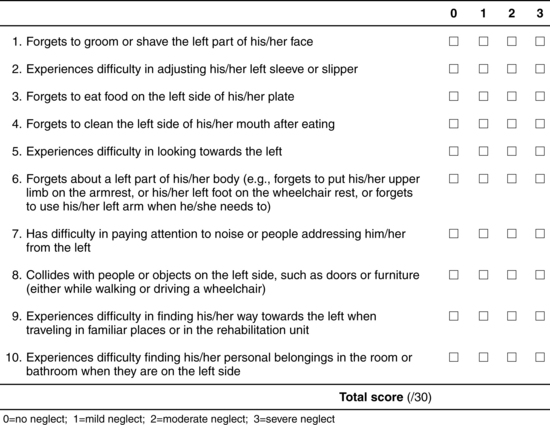
Figure 19-3 Catherine Bergego Scale. A test of functional neglect including personal, peripersonal, and extrapersonal aspects of neglect. Score of 0 is given if no spatial bias is noted. Score of 1 is given when the patient always first explores the right hemispace before going slowly and hesitatingly toward the left space and shows occasional left sided omissions. Score of 2 is given if the patient shows clear and constant left-sided omissions and collisions. Score of 3 is given when the patient is totally unable to explore the left hemispace.
(From Bergego C, Azouvi P, Samuel C, et al: Validation d’une échelle d’évaluation fonctionnelle de l’héminégligence dans la vie quotidienne: l’échelle CB. Ann Readapt Med Phys 38:183-189, 1995.)
Awareness training
Tham and coworkers98 developed an intervention to improve awareness related to the effect of neglect on functional performance. Purposeful and meaningful (for the participant) daily occupations were used as therapeutic change agents to improve awareness of disabilities. Specific interventions include the following:
 Encourage the participants to choose motivating tasks as the modality of intervention.
Encourage the participants to choose motivating tasks as the modality of intervention.
 Discuss task performance. Examples include encouraging the participants to describe their anticipated difficulties, to link their earlier experiences of disability to new tasks, and to plan how they would handle new situations; and asking the participants to evaluate and describe their performance and to think about whether they could improve performance by doing the task in another way.
Discuss task performance. Examples include encouraging the participants to describe their anticipated difficulties, to link their earlier experiences of disability to new tasks, and to plan how they would handle new situations; and asking the participants to evaluate and describe their performance and to think about whether they could improve performance by doing the task in another way.
 Provide feedback about the observed difficulties including verbal feedback (describe to the participant difficulties with reading and understanding the text in the left half of the page of the newspaper), visual feedback (give visual guidance to show the “neglected” text in the left half of the page), and physical guidance.
Provide feedback about the observed difficulties including verbal feedback (describe to the participant difficulties with reading and understanding the text in the left half of the page of the newspaper), visual feedback (give visual guidance to show the “neglected” text in the left half of the page), and physical guidance.
 When participants could describe their difficulties, the therapists and participants discussed compensatory techniques that could improve task performance.
When participants could describe their difficulties, the therapists and participants discussed compensatory techniques that could improve task performance.
 The participant performed the task again, using the newly learned compensatory techniques.
The participant performed the task again, using the newly learned compensatory techniques.
 The home environment was used to confront difficulties in familiar settings.
The home environment was used to confront difficulties in familiar settings.
Scanning training
Scanning training has long been considered a critical aspect of intervention programs for those with neglect. Scanning training has been documented to include the following:
Lighthouse strategy (lhs)
The specific intervention is outlined as follows:65
 A cancellation test is administered during the initial evaluation.
A cancellation test is administered during the initial evaluation.
 The test is scored, and the person is shown the letters missed on the test.
The test is scored, and the person is shown the letters missed on the test.
 The therapist makes introductory statements such as, “I teach a strategy to help people pay better attention to their left [or right]. See how you missed these on this side? I can help you fix this problem.”
The therapist makes introductory statements such as, “I teach a strategy to help people pay better attention to their left [or right]. See how you missed these on this side? I can help you fix this problem.”
 The LHS is introduced as a strategy for helping people pay better attention to their left and right and is explained fully. The person is shown a simple line drawing of the Cape Hatteras lighthouse, with the light beams and top lights highlighted with a yellow marker. The person is told to imagine that his or her eyes and head were like the light inside the top of the lighthouse, sweeping to the left and to the right of the horizon to guide ships to safety. The person is then asked to think about what would happen if the lighthouse only provided light to the right (or left) side of the ocean and horizon. The therapist probes for consequences of the lighthouse illuminating only one side.
The LHS is introduced as a strategy for helping people pay better attention to their left and right and is explained fully. The person is shown a simple line drawing of the Cape Hatteras lighthouse, with the light beams and top lights highlighted with a yellow marker. The person is told to imagine that his or her eyes and head were like the light inside the top of the lighthouse, sweeping to the left and to the right of the horizon to guide ships to safety. The person is then asked to think about what would happen if the lighthouse only provided light to the right (or left) side of the ocean and horizon. The therapist probes for consequences of the lighthouse illuminating only one side.
 The picture of the lighthouse is placed on the table to the right and in front of the person.
The picture of the lighthouse is placed on the table to the right and in front of the person.
 The therapist then introduces a task requiring full scanning of the left and right fields. The person is asked to close the eyes while the therapist sets up objects across the table in front of the person. The person is asked to find these objects.
The therapist then introduces a task requiring full scanning of the left and right fields. The person is asked to close the eyes while the therapist sets up objects across the table in front of the person. The person is asked to find these objects.
 Each time an object is missed, the person is asked to turn the head “like a lighthouse, left and right, like this” while the therapist demonstrates the proper degree and pace of head turning. The person is shown how to line the tip of the chin first with the top of the right and then the top of the left shoulder.
Each time an object is missed, the person is asked to turn the head “like a lighthouse, left and right, like this” while the therapist demonstrates the proper degree and pace of head turning. The person is shown how to line the tip of the chin first with the top of the right and then the top of the left shoulder.
 The person is then asked to find the objects again, this time using the LHS.
The person is then asked to find the objects again, this time using the LHS.
 A tactile cue such as a light tap on the left shoulder may be given in addition to the verbal cue.
A tactile cue such as a light tap on the left shoulder may be given in addition to the verbal cue.
 The person is asked to notice how many more objects can be seen when the LHS is used.
The person is asked to notice how many more objects can be seen when the LHS is used.
 A copy of the lighthouse poster is placed on the wall of the person’s room, to the right of the bed.
A copy of the lighthouse poster is placed on the wall of the person’s room, to the right of the bed.
 All therapists are given copies of the poster and asked to use it to cue the person when task performance requires attention to both the right and left fields (i.e., grooming, feeding, mobility.).
All therapists are given copies of the poster and asked to use it to cue the person when task performance requires attention to both the right and left fields (i.e., grooming, feeding, mobility.).
Limb activation
Limb activation is based on the idea that any movement of the contralesional side may function as a motor stimulus, activating the right hemisphere and improving neglect. It has been shown across a series of studies that unilateral neglect can be improved by encouraging clients to make even small movements with some part of the left side of their body if these movements are performed in the left hemispace. In general, the principle behind this approach is to “find” the affected limb and encourage movements of the affected limb in the neglected hemispace (i.e., spatiomotor cueing). It is hypothesized that these movements lead to summation of activation of affected receptive fields of two distinct but linked spatial systems for personal and extrapersonal space, resulting in improvements in attentional skills and appreciation of spatial relationships on the affected side.52,79 A counter hypothesis is that the movements in the left hemispace serve as perceptual cues such as an anchor. Studies have demonstrated a reduction in the severity of neglect when subjects actively engage their left hand in a task.
Partial visual occlusion
In a randomized study, Beis and colleagues14 examined 22 subjects with left unilateral neglect. Interventions included the use of right half-field patches (n = 7), a right monocular patch (n = 7), and a control group (n = 8). Patches were worn throughout the day during inpatient rehabilitation. Results of paired comparison tests showed significant differences between the control group and the group with the half-eye patches for the total Functional Independence Measure score and objective measures of displacements of the right eye in the left field. No significant differences were found between the control group and the group with the right monocular patch.
Videotaped feedback of task performance
Using videotaped feedback of task performance has been suggested as a strategy to decrease the effects of unilateral neglect. When viewing one’s own performance on a TV screen during video playback, one can see and attend to the neglected left side on the right side of the TV monitor (i.e., neglect behaviors can be observed in the non-neglected space). This may be a key therapeutic factor. In usual care, the therapist describes the neglect behavior, but the person with neglect may not be able to “see” his or her mistakes. Visualizing the mistakes, followed by processing them with the therapist, may help insight building and subsequent strategy formation.
Environmental adaptation
Some people will not recover spontaneously or respond to “active” interventions such as teaching a new strategy to perform a task. Similarly, those who have poor awareness and insight and who don’t respond to awareness training may not respond to interventions that require self-generated compensatory strategies. In these cases, a person’s functional performance may be enhanced by implementing and teaching caregivers or family members environmental strategies (Table 19-7).
Table 19-7 Sample Environmental Strategies to Improve Function in Those with Neglect
| FUNCTION | STRATEGIES |
|---|---|
| Feeding | Place food, utensils, napkin, etc., on the right side of plate and placemat. Note: This intervention may be combined with the use of cue on the left side of the placemat such as a colored anchor (strip of tape or nonslip material) and/or the person’s left arm on the table to be used as a spatiomotor cue. Situate person at the table so that other diners are biased to the right to enhance socialization. |
| Table games | Rotate the person’s chair 45 degrees to the left to place key game items in the intact field. Situate person at the table so that other players are biased to the right. |
| Home management | Organize closets, drawers, refrigerator, etc. so that the person’s necessary items are on the right. |
| Bed side care | Call bell always placed on right. Orient bed so that incoming stimuli (doorway, television, seating) are in the right field.* |
| Mobility | Colored markers on furniture that be an obstacle; signs posted on right side of hall, i.e., “Turn left here” |
* In the acute stages, this may be controversial because the therapist may want to “force” the person to respond to the left side of the environment.
From Gillen G: Cognitive and perceptual rehabilitation: optimizing function, St. Louis, 2009, Mosby/Elsevier.
Organization/sequencing deficits
The ability to organize thoughts requires the integration of multiple skills, including praxis, sequencing, and problem-solving. Sequencing refers to the ability to plan and carry out events in proper order, progression, and time.6 Sequencing and organization deficits represent the breakdown of a complex integration of skills, including use of sensory feedback and organization. Patients with sequencing and organization deficits can be trained to use a daily planner, tape recordings, or cue cards (depending on whether they perform better with auditory or visual cues) to help sequence the steps of daily tasks. Gradually increasing the number of steps in a task can increase a patient’s tolerance and ability to perform more complex tasks (Box 19-6). Note those living with ideational apraxia will also present with organization and sequencing deficits.
Box 19-6 SEQUENCING DEFICITS: TIPS FOR FAMILY MEMBERS
 Frustration and error can be lessened by step-by-step directions written in a simple format (e.g., a checklist).
Frustration and error can be lessened by step-by-step directions written in a simple format (e.g., a checklist).
 Maps and diagrams may be useful.
Maps and diagrams may be useful.
 Visual aids often prove helpful, especially when combined with verbal instructions or physical guiding.
Visual aids often prove helpful, especially when combined with verbal instructions or physical guiding.
 Frequent, routine practice should help reinforce the sequencing of daily activities.
Frequent, routine practice should help reinforce the sequencing of daily activities.
Spatial relations syndrome
Spatial relations syndrome is the label given to disorders with impairment in the perception of spatial relationship of objects. These disorders include impairments with figure-ground, position in space, spatial relations, and form and space constancy skills. Topographical disorientation also is classified sometimes as part of spatial relations syndrome. Recommendations for spatial impairments include training patients to move slowly through their environments, encouraging patients to touch objects in the environment frequently, teaching patients to handle objects by the base, and using verbal cues or feedback instead of gestures.70 Perceptual impairments are often difficult for families to understand. Educating the caregivers about these disorders and instructing them on how they can help their loved ones (Box 19-7) is especially important. See Chapter 16.
Box 19-7 PERCEPTUAL PROBLEMS: TIPS FOR FAMILY MEMBERS
 Overstimulation from visual information may increase the problem.
Overstimulation from visual information may increase the problem.
 Getting rid of unnecessary objects and equipment lessens the demands on the patient and simplifies the task. For example, the table-top should be cleared of objects that look alike so that the patient does not confuse them.
Getting rid of unnecessary objects and equipment lessens the demands on the patient and simplifies the task. For example, the table-top should be cleared of objects that look alike so that the patient does not confuse them.
 Slowing down while reaching for an object or walking into a new area is usually helpful.
Slowing down while reaching for an object or walking into a new area is usually helpful.
Spatial relation dysfunction
Spatial relation dysfunction is an impairment in relating objects to one another or to the self. Some examples of functional activities for patients with spatial deficits include identification and orientation of clothing during a dressing activity. This includes matching buttons and buttonholes together on a shirt or working on the ability to orient shoelaces during a one-handed tie. Wheelchair transfers require the ability to position the body in relation to a bed or other object and spatial orientation to maneuver wheelchair brakes and armrests in the correct direction. Simple meal preparation is another activity that requires spatial orientation and positioning because of tasks as locating and selecting needed items, stirring food, and setting the table.50
The use of the computer for visuospatial retraining has little or no effect on visuospatial skills and no carryover to functional activities.44 Thus the use of computer programs aimed solely at addressing visuospatial skill retraining appears to be an ineffective remediation technique. A computer screen provides information as a two-dimensional image. Spatial relation impairment is a three-dimensional problem. For persons who use the computer for work or leisure, however, the use of the keyboard or mouse while working on the computer can be an effective, challenging, and meaningful modality.
Spatial positioning impairment
The concept of spatial positioning involves accurate placement or positioning of objects, including body parts. That impairment may be associated with impaired proprioception, however. This disorder is linked with language comprehension. Concepts such as above, in, and under are interpreted according to position in space and language skills.
Treatment for spatial positioning impairment should include increasing the patient’s awareness of the impairment and teaching compensatory strategies. Matching colored markers for correct placement of objects can be helpful. Treatment ideas include having the patient practice placing a glass on top, in front, to the right, and to the left of a plate on command, placing certain objects (cups or utensils) in a row and having the patient identify which object is in a position different from those of the others. If language skills are impaired, the patient can be asked to create a place setting from a model. Repetition of specific spatial concepts, with emphasis on attention to detail and compensatory strategies (e.g., Velcro shoe strap goes toward the colored marker), may be helpful.
Treatment techniques for right-left discrimination problems include providing activities that stress right and left differences, such as dressing and grooming. In addition, therapists may use color or other markers to distinguish the right from the left side of items such as clothing and shoes.
Figure-ground impairment
Figure-ground deficits involve the inability to distinguish the foreground from the background. Treatment strategies for figure-ground deficits should include teaching the patient to be cognitively aware of the deficit and to slow down enough during task performance to identify all the relevant objects or stimuli before handling or manipulating them. The environment can be adapted to make it simple and uncluttered (e.g., organizing drawers or shelves). The use of stark contrast between objects (e.g., the plate and table during mealtime) is helpful for patients with this disorder. Sorting objects such as utensils from a kitchen drawer or nuts and bolts from a toolkit can be a good therapeutic activity; the sorting can be made more difficult with the addition of smaller and larger objects, thereby adding the element of size discrimination. The sorting should have a purpose, such as using the utensils for a cooking task.
Topographical disorientation
Topographical disorientation is difficulty finding direction in space.6 The use of compensatory techniques and environmental adaptation, progressively reduced as the patient demonstrates learning, is often successful in the treatment of this disorder. Therapists can use markers such as colored dots to identify a route the patient must travel every day. The therapist gradually removes cues as the patient memorizes the route. One successful treatment program described by Borst and Peterson20 used the patient’s intact skills of right-left discrimination and language to assist with functional mobility. In this treatment program, the patient practiced following directional instructions (e.g., “Go left at the next door.”). The patient then was asked to draw the path from room to room on a map of the clinical area. Such an exercise would be especially helpful in the home setting. At first the therapist may need to assist the patient with correctly orientating the map with each turn. The therapist should withdraw verbal cues slowly. Next, the patient should attempt to go from room to room with only brief glances at the map. The last step is to withdraw the use of the map altogether. Generalization of this type of treatment is unlikely; therefore, treatment should take place only in the most meaningful environment.
Agnosia
Agnosia typically is defined as the inability to recognize sensory stimuli. Agnosia presents as a defect of one particular sensory channel, such as visual, auditory, or tactile. Examples include finger agnosia, visual agnosia, somatoagnosia, simultanagnosia, and tactile agnosia. These disorders are rarely seen in isolation, and little data have been published regarding treatment techniques for agnosia. However, because the defining principle of agnosia is impairment of one specific sensory modality, treatment usually focuses on teaching the patient to use the intact sensory modalities. For example, in tactile agnosia—the inability to recognize objects by handling them—the patient is taught to use visual, olfactory, and auditory senses to recognize objects (Box 19-8 and Box 19-9).
Box 19-8 Difficulties during Everyday Function and Agnosia
Visual (object) agnosia
Inability to find the razor on the sink despite adequate scanning abilities. The razor can only be located by touch.
Visuospatial agnosia
Misjudging the distance while reaching for a cup resulting in an inappropriate endpoint (i.e., the hand end up several inches from the cup)
Difficulties orienting a shirt to one’s body. See Chapter 16.
Tactile agnosia
Difficulty with clothing fasteners despite intact motor function
Inability to recognize objects that are in one’s pockets unless vision is also used
Data from Árnadóttir G: The brain and behavior: assessing cortical dysfunction through activities of daily living, St Louis, 1990, Mosby.
Box 19-9 More Interventions for Agnosia, Based on the Literature
Visual agnosia
Teach compensation via the use of other senses such as tactile information.
Teach awareness of deficits focusing on consequences of the impairments because those with visual agnosia may underestimate the consequences of the deficit.83
Teach recognition of figures and shapes by kinesthetic sense combined with visual information.96
Teach tracing with eyes and fingers such as tracing letters to improve recognition.96
Moving an object or moving the head relative to an unrecognizable object and tracing the outline may facilitate recognition.54 Encourage head movements when examining objects and encourage observing items related to depth cues.27,100
Teach the use of spatial and location cues to recognize objects, people, etc. Examples include organizing a bedroom or classroom so that needed objects are assigned to specific spatial locations such as school clothes on the right side of the dresser and casual clothes on the left.83 Teach the use of unique identifying features and idiosyncratic cues to assist recognition (e.g., color or shape).83 Use knowledge of relevant and critical features to identify objects. For example, when looking for Swiss cheese in the refrigerator, focus on color (white) and shape (cube shaped) to narrow down the number of objects that must be examined.
Teach a piecemeal reconstruction approach using feature-by-feature analysis.83
Teach reliance on verbal memory skills and verbal reasoning to interpret the piecemeal visual information into a whole (e.g., “it’s a person, no it’s a dress, it’s short, it must be a shirt”).83
Use color cues, labels, or textures on objects or environments (e.g., Velcro on the phone receiver or red tape on doorknobs).24,60
Encourage overt verbalization of the visual characteristics of objects before producing a name.26
Practice identification of real objects vs. line drawings. Real objects are more easily recognized than drawings or pictures. Focus attention to depth cues, surface texture, and colors.100 Real objects provide cues based on surface detail (different luminance and textures), color shades, and provide depth information.27
Use landmarks such as a sofa to route find.60
Use cues from other people to help generate a strategy. For example, if during a meal one cannot find utensils, watching others during the meal may help locate these items.60
Alexia
Read via letter tracing.24
Trace letters on the palm of the hand.
Text to speech software programs such as Kurzweil 1000 or RealSpeak.
Prosopagnosia
Use gait clues to identify people (e.g., speed, sound of shoes).83
Using clothing sounds or clues to recognize.13 Use localization clues (e.g., Ann sits behind me in the classroom, and John is to my right).83
Highlight distinguishing features such as eye color, a scar, or mustache.24
Topographical disorientation secondary to agnosia and related disorders
Teach navigation in home environments by always starting at the same point such as the front door.24
Focus on past memories of the home to assist in navigation or relearning directions using kinesthetic and vestibular cues.
Use color markers on key rooms (e.g., a blue circle is my room).
Teach the use of kinesthetic memory for route finding such as the number of turns or steps.83
Tactile agnosia and/or astereognosis
Begin practicing with identifying simple shapes via tactile information. Practice recognition of two-dimensional and three-dimensional objects because recognition may not be consistent.78
From Gillen G: Cognitive and perceptual rehabilitation: optimizing function, St. Louis, 2009, Mosby/Elsevier.
Memory impairments
Although memory impairments are not as common in persons who have sustained strokes as they are in those with closed-head injuries, dementia, or encephalitis, difficulty retaining information is nonetheless common in the stroke population.
Human memory is composed of multiple and distinct systems10,90 that are required to support daily activities and participate in the community. Examples include remembering your significant other’s birthday, remembering to take your medications, remembering to feed the dog, remembering how to type, remembering events that occurred during a vacation, and so on. Even this “simple” list of memory tasks requires intact functioning of multiple memory systems and includes knowledge of facts and events, procedures, and remembering future intentions. Clearly, memory serves as a key cognitive support to facilitate independent living.
The steps or stages of memory have been well-documented.10,90 The flow of these stages follows (Table 19-8):
| STAGE OF MEMORY | DESCRIPTION | NEUROANATOMICAL AREA OF FUNCTION |
|---|---|---|
| Attention | The processes that allow a person to gain access to and use incoming information. Inclusive of alertness, arousal, and various attention processes such as selective attention. | Brainstem Thalamic structures Frontal lobes |
| Encoding | How memories are formed. An initial stage of memory that analyzes the material to be remembered (visual vs. verbal characteristics of information). Correct analysis of information is required for proper storage of the information. | Dorsomedial thalamus Frontal lobes Language system (e.g., Wernicke area) Visual system (e.g., visual association areas) |
| Storage | How memories are retained Transfer of a transient memory to a form or location in the brain for permanent retention/access |
Hippocampus Bilateral medial temporal lobes |
| Retrieval | How memories are recalled Searching for or activating existing memory traces | Frontal lobe |
Data from Sohlberg MM, Mateer CA: Memory theory applied to intervention. In Sohlberg MM, Mateer CA, editors: Cognitive rehabilitation: an integrative neuropsychological approach, New York, 2001, Guilford Press.
A variety of memory impairments have been documented and each impact daily function differently (Table 19-9).
Table 19-9 Terminology Related to Memory Impairments
| TERM | DEFINITION | EXAMPLES OF EVERYDAY BEHAVIORS |
|---|---|---|
| Anterograde amnesia | A deficit in new learning. An inability to recall information learned after acquired brain damage. An inability to form new memories after brain damage occurs | Not able to recall staff names, easily gets lost secondary to topographical disorientation, not able to recall what occurred in therapy this morning, difficulty learning adaptive strategies to compensate for memory loss |
| Retrograde amnesia | Difficulty recalling memories formed and stored prior to the disease onset. May be worse for recent events as opposed to substantially older memories | Inability to remember autobiographical information (address, social security number, birth order), not able to remember historical events (war, presidential elections, scientific breakthroughs), and/or personally experienced events (weddings, vacations) |
| Short-term memory | Storage of limited information for a limited amount of time | Difficulty remembering instructions related to the use of adaptive equipment, not able to remember the names of someone just introduced at a dinner party, not able to remember “today’s specials” in a restaurant |
| Working memory | Related to short-term memory and refers to actively manipulating information in short-term storage via rehearsals | Unable to remember and use the rules of the game while playing a board game, not able to perform calculations mentally while balancing the checkbook, difficulty remembering and adapting a recipe. |
| Long-term memory (LTM) | Relatively permanent storing of information with unlimited capacity | May affect declarative memory of knowledge, episodes, and facts or nondeclarative memories such as those related to skills and habits |
| Nondeclarative/implicit or procedural memory | Knowing how to perform a skill, retaining previously learned skills and learning new skills. Form of LTM | Driving, playing sports, hand crafts, learning to use adaptive ADL equipment or a wheelchair. |
| Declarative/explicit memory | Knowing that something was learned, verbal retrieval of a knowledge base such as facts, and remembering everyday events. Includes episodic and semantic information. Form of LTM (see following) | See episodic and semantic memory. |
| Episodic memory | Autobiographical memory for contextually specific events. Personally experienced events. Form of declarative LTM | Remembering the day’s events, what one had for breakfast, occurrences on the job, the content of therapy sessions |
| Semantic memory | Knowledge of the general world, facts, linguistic skill, and vocabulary. (Note: may be spared after injury.) Form of declarative LTM | Remembering the dates of holidays, the name of the president, dates of world events |
| Explicit memory | Explicit memories consist of memories from events that have occurred in the external world. Information stored in explicit memory is about a specific event that happened at a specific time and place. | Remembering places and names, and various words. See declarative memory. |
| Implicit memory | Does not require conscious retrieval of the past. Knowledge is expressed in performance without the person being aware of possessing this knowledge. Consists of memories necessary to perform events and tasks, or to produce a specific type of response. | Memory of skills, habits, and subconscious processes. See nondeclarative memory. |
| Prospective memory | Remembering to carry out future intentions | Remembering to take medications, return phone calls, buy food, pick up children from school, mail the bills. A critical aspect of memory to support everyday living |
| Metamemory | Awareness of your own memory abilities | Knowing when you need to compensate for memory capacity (making a list of errands, shopping list, writing down a new phone number or driving directions), recognizing errors in memory |
Data from Baddeley AD: The psychology of memory. In Baddeley AD, Kopelman MD, Wilson BA, editors: The essential handbook of memory disorders for clinicians, Hoboken, NJ, 2004, John Wiley; Bauer RM, Grande L, Valenstein E: Amnesic disorders. In Heilman KM, Valenstein E, editors: Clinical neuropsychology, ed 4, New York, 2003, Oxford University Press; Markowitsch HJ: Cognitive neuroscience of memory. Neurocase 4(6):429-435, 1998; and Sohlberg MM, Mateer CA: Memory theory applied to intervention. In Sohlberg MM, Mateer CA, editors: Cognitive rehabilitation: an integrative neuropsychological approach, New York, 2001, Guilford Press.
Interventions focused on those with memory deficits can be categorized as restorative approaches to improve underlying memory deficits, strategy training, use of nonelectronic memory aids, and electronic memory aids or assistive technology. Techniques aimed at improving the underlying memory impairment such as memory drills have been unsuccessful in terms of generalizing to meaningful activities. An improvement may be detected on a laboratory-based measure of memory without a corresponding change in daily function or subjective memory reports.
As will be discussed later, the most promising interventions to improve function in those living with memory deficits rely at least partially on compensatory techniques. When using a compensatory approach, choosing the correct system of compensation is critical. Kime57 suggested a comprehensive evaluation that includes the following:
 Presence of comorbidities including physical impairments, language deficits, and other cognitive deficits
Presence of comorbidities including physical impairments, language deficits, and other cognitive deficits
 Client needs (e.g., will the system be used for work, home management)
Client needs (e.g., will the system be used for work, home management)
Memory notebooks and diaries
Sohlberg and Mateer90 published a systematic, structured training sequence for teaching individuals with severe memory impairments to independently use a compensatory memory book. The training sequence they proposed incorporates principles of learning theory and procedural memory skills, which may be preserved in many clients with even severe memory impairments. Their paper described the components of a functional memory book. In addition, they explained a three-stage approach to using the notebook.
 Application or where and when to use it
Application or where and when to use it
 Adaptation or how to update it and use it in novel situations
Adaptation or how to update it and use it in novel situations
Sohlberg and Mateer90 highlighted that successful memory book training takes time, requires that all staff and family need to be trained in its use, that the person carry the book at all times, and that its use is individualized and function-based. They documented the effectiveness of this approach to memory book training via a case study in which the intervention was successfully used to support daily living and employment, despite persistent memory deficits.
Donaghy and Williams31 suggested that the diary or notebook include a pair of pages for each day of the week. The notebook is set up to aid scheduling things to do in the future and record activities done in the past. Within each pair of pages, the left-hand page contains two columns: one with a timetable for the day, and the other with the to-do items. The right-hand page contains the memory log. A “Last Week” section at the back stores previous memory log entries. A full year calendar allows for appointments to be recorded. Donaghy and Williams31 published their training protocol and two case studies to support use of the notebook.
Errorless learning
Errorless learning is a learning strategy that is in contrast to trial and error learning or errorful learning. Interventions using an errorless learning approach are based on differences in learning abilities. People with memory impairments typically remember their own mistakes as results of their own action more successfully than they remember the corrections to their mistakes occurring via explicit means (e.g., a therapist’s cue). People may remember their mistakes but not the correction. With errorless learning, a person learns something by saying or doing it, rather than being told or shown by someone. In addition, the person is not given the opportunity to make a mistake (i.e., there are no mistakes to be remembered). The hypothesis is that reduction or prevention of incorrect or inappropriate responses facilitates memory performance. The technique is straightforward and involves preventing clients from making any errors during learning via physical and verbal support or cues from the therapist, reducing the use of trial and error and avoiding mistakes.
Evans and colleagues35 presented nine experiments, in three study phases, which tested the hypothesis that learning methods that prevent the making of errors (errorless learning) will lead to greater learning than trial and error learning methods among those who are memory impaired because of acquired brain injury. Errorless learning techniques include the following:
 Providing the correct answer immediately: For example, when showing a picture of unfamiliar face, the therapist would ask, “What is this person’s name? His name begins with M; his name is Michael.” The authors found that this technique was beneficial for remembering names by first letter–cued recall as compared to learning names by trial and error.
Providing the correct answer immediately: For example, when showing a picture of unfamiliar face, the therapist would ask, “What is this person’s name? His name begins with M; his name is Michael.” The authors found that this technique was beneficial for remembering names by first letter–cued recall as compared to learning names by trial and error.
 Backward chaining: Used to teach multistep tasks. In this approach the therapist shows or prompts all of the steps of the task. On the next trial, all of the steps except for the last one are demonstrated or prompted and the person being taught the skill must demonstrate it. After each trial, prompts are withdrawn and the technique progresses until all of the steps are learned. The authors found that this technique was beneficial for learning names by first letter–cued recall as compared to trail and error.
Backward chaining: Used to teach multistep tasks. In this approach the therapist shows or prompts all of the steps of the task. On the next trial, all of the steps except for the last one are demonstrated or prompted and the person being taught the skill must demonstrate it. After each trial, prompts are withdrawn and the technique progresses until all of the steps are learned. The authors found that this technique was beneficial for learning names by first letter–cued recall as compared to trail and error.
 Forward chaining: Also used to teach multiple step tasks. The therapist prompts or demonstrates the first step on the first trial, the first two steps on the second trial, and continues until the whole sequence is remembered.
Forward chaining: Also used to teach multiple step tasks. The therapist prompts or demonstrates the first step on the first trial, the first two steps on the second trial, and continues until the whole sequence is remembered.
 Combined imagery with errorless learning: Associations between faces and names were taught by having the subject create a mental image based on facial features; for example, the wave in the person’s hair looks like a W; his name is Walter. The authors documented improved free recall of names using this technique.
Combined imagery with errorless learning: Associations between faces and names were taught by having the subject create a mental image based on facial features; for example, the wave in the person’s hair looks like a W; his name is Walter. The authors documented improved free recall of names using this technique.
The authors’ results suggest that tasks and situations that facilitate retrieval of implicit memory for the learned material (e.g., learning names with a first letter cue) will benefit from errorless learning methods, whereas those that require the explicit recall of novel associations (such as learning routes or programming an electronic organizer) will not benefit from errorless learning. The more severely memory-impaired clients benefited to a greater extent from errorless learning methods than those who were less severely memory impaired, but the authors cautioned that this may apply only when the interval between learning and recall is relatively short.
Assistive technology
Several studies have documented the success of using simple assistive technology to compensate for memory loss and improve daily function (Box 19-10). Interventions for those with memory impairments must consider social networks as well. Including significant others in all interventions may be the key factor to ensure success (Box 19-11).
Box 19-10 Assistive Technology for Those with Memory Loss
Adaptive stove controls to turn off an electric stove after a certain period of time or when heat becomes excessive
A phone with programmable memory buttons (affix pictures to the buttons)
A phone with buttons programmed to speak the name of the person being called
Tape recorders used to cue a behavioral sequence such as morning care
From Gillen G: Cognitive and perceptual rehabilitation: optimizing function, St. Louis, 2009, Mosby/Elsevier.
Box 19-11 Strategies for Significant Others Living with Those Living with Memory Impairment after Stroke
Understand that in many cases this impairment may not be reversible.
Become very familiar with the specific type of compensatory memory strategies that have been prescribed.
Keep daily schedules as consistent as able. Stick with habits and routines.
Simplify the environment by decreasing clutter and keeping the living areas organized.
Decrease excessive environmental stimuli.
Help by organizing calendars, clocks, and reminders posted around the house.
Be proactive in identifying potential safety issues.
Use short and direct sentences.
Make sure that the most important information comes at the beginning the sentence.
Highlight, cue, and emphasize key aspects of communication (i.e., repeat, point.)
Avoid conversations that rely on memory (i.e., keep conversations in the present).
Repetition of sentences may be inevitable.
Remember that in many cases, intelligence may remain intact.
Keep “a place for everything and everything in its place.”
Use photographs, souvenirs, and other appropriate items to help access memories.
Understand that fatigue, stress, sleep disorders, and depression can exacerbate memory loss.
Keep back-up items (glasses, spare keys, etc.).
Help create to-do lists. Remind loved ones to check it off or highlight the item when the task is completed.
Attention deficits
Attention is an essential element in successful task performance. Poor ability to attend to a task often is misinterpreted as a lack of motivation or neglect. Accurate assessment of an attention impairment is important to implementing appropriate treatment techniques. One method that may be helpful in managing attention problems is changing the way occupational therapists speak to patients. The goal is to couple the patient’s attention with the intended action; instructions should be in the logical sequence of the action. Instead of instructing a patient to “Scoot forward,” the therapist would say, “Your bottom [pause]. Move it forward to the edge of the chair.” The wording should correspond with the order in which the steps are to be executed and should allow the patient to attend to each step. The pause is important to allow the patient enough time to shift focus and process the information.25
Use of systematic training incorporating a series of tasks with progressively increasing attentional demands has resulted in improvements in memory and attention to task,16 although other studies have failed to demonstrate support for remedial training in attention.102
Family members often are frustrated when their loved ones are distracted easily or are unable to focus on a task. Family members must be informed that stroke survivors do not behave erratically on purpose. Teaching the family the way to create a supportive environment is important (Box 19-12).
Box 19-12 Attention Deficits: Strategies for Clinicians and Caretakers
Avoid overstimulating/distracting environments.
Face away from visual distracters during tasks.
Shop or go to restaurants at off-peak times.
Use filing systems to enhance organization.
Reduce clutter and visual distracters.
Use self-instruction strategies.
Use time pressure management strategies.
Control the rate of incoming information.
Self-manage effort and emotional responses during tasks.
Teach monitoring or shared attentional resources when multitasking.
Manage the home environment to decrease auditory and visual stimuli. Keep radios and phones turned off. Close doors and curtains. Keep surfaces, cabinets, closets, and refrigerators organized and uncluttered.
Use daily checklists for work, self-care, and instrumental activities of daily living.
Data from Cicerone KD: Remediation of “working attention” in mild traumatic brain injury. Brain Inj 16(3):185-195, 2002; Fasotti L, Kovacs F, Eling Paul ATM et al: Time pressure management as a compensatory strategy training after closed head injury. Neuropsychol Rehabil 10(1)47:-65, 2000; Michel JA, Mateer CA: Attention rehabilitation following stroke and traumatic brain injury, a review. Eura Medicophys 42(1):59-67, 2006; and Webster JS, Scott RR: The effects of self-instructional training on attentional deficits following head injury. Clin Neuropsychol 5(2):69-74, 1983.
Attention has been described as having four distinct domains: alertness, selective attention, sustained attention, and divided or alternating attention. Therapists must train patients in each domain skill individually, and generalization from one domain to another should not be expected after training.63
Selective attention impairment
The ability to focus on relevant stimuli while screening out irrelevant stimuli is referred to as selective attention. Training patients to react to certain environmental cues and ignore distractions may improve selective attention. For example, the therapist can ask a patient to follow audio-recorded instructions for a hygiene task (or meal preparation, if a more complex task is desired). After the patient is able to complete the task successfully, the therapist can add elements of distraction, such as a radio or television, one by one.
Sustained attention impairment
Sustained attention is the ability to maintain attention over a period. Focusing and sustaining attention is improved by gradually increasing the attentional demands of activities, through choosing activities with longer duration and additional distractions. For example, a task such as combing hair in a quiet bathroom without a mirror initially may require less than 30 seconds of focused attention to complete (and have few inherent distractions). As the patient successfully completes these types of tasks, the therapist should choose activities that require focused attention to detail and have more distractions (e.g., straight razor shaving task with the radio playing in the background). Some support exists for providing specific training for attention to improve alertness and sustained attention, but no evidence exists that attention training affects functional abilities.63
Alternating attention impairment
Alternating attention is shifting focus from one stimulus to another. For the brain-injured population, the therapist should plan graded activities from simple to complex that initially require the patient to shift attention from one stimulus to another. For example, a simple activity may consist of participating in a ceramics painting project (in which the patient alternates attention from the paint to ceramic vase); a more complex task would be to have the patient perform a dressing task while watching the news on television and having the patient repeat important daily events after completing the task. Initially, tasks should require only attention shifts between two focal points. As the patient successfully completes these tasks, the therapist should use activities incorporating more focal points (e.g., a meal preparation task in which focus must alternate among planning, following directions, searching for supplies, monitoring other foods, timing, and place setting).
Concrete thinking
Inflexible thought processes characterize persons who use concrete thinking. They have difficulty generalizing information from one situation to another and rely heavily on available sensory information.
Persons with impaired abstraction skills usually have poor ability to recognize and learn the cognitive and perceptual skills needed for a specific task. Therefore, they may benefit only from learning splinter (nongeneralizable) skills in treatment and may demonstrate training only in those tasks that are similar to those learned.67 Box 19-13 reviews suggestions for family members to facilitate communication and task performance with this population.
Box 19-13 COGNITIVE INFLEXIBILITY: TIPS FOR FAMILY MEMBERS
 Make statements and questions as simple and uncomplicated as possible.
Make statements and questions as simple and uncomplicated as possible.
 Explain the reasons for certain procedures. The person may have difficulty understanding the long-term effects of therapy or medical procedures. Explain these with smaller goals that are easier to accomplish.
Explain the reasons for certain procedures. The person may have difficulty understanding the long-term effects of therapy or medical procedures. Explain these with smaller goals that are easier to accomplish.
 If possible, structure tasks so they consist of a series of related tasks rather than many unrelated tasks.
If possible, structure tasks so they consist of a series of related tasks rather than many unrelated tasks.
Executive function impairments
Executive functions is an umbrella term that refers to complex cognitive processing requiring the coordination of several subprocesses to achieve a particular goal.34a This term has been defined as “a product of the coordinated operation of various processes to accomplish a particular goal in a flexible manner”38a or “those functions that enable a person to engage successfully in independent, purposive, self-serving behavior.”60a These higher-order mental capacities allow one to adapt to new situations and achieve goals. They include multiple specific functions such as decision-making, problem-solving, planning, task switching, modifying behavior in the light of new information, self-correction, generating strategies, formulating goals, and sequencing complex actions.12,60a Clearly these executive functions support engagement in daily life activities and participation in the community, most important during new, nonroutine, complex, and unstructured situations.60a (Table 19-10). Intervention approaches for these problems are somewhat lacking in the stroke survivor population. Available information is summarized in Boxes 19-14 and 19-15.
Table 19-10 Examples of Executive Functions Related to Everyday Living: Preparing a Salad
| EXECUTIVE FUNCTION | ASSOCIATED TASKS |
|---|---|
| Initiation | Starting the task at the appropriate time without overreliance on prompts |
| Organization | Organizing the work space and performing the task efficiently (e.g., gathering necessary vegetables at the same time from the refrigerator) |
| Sequencing | Sequencing the steps of the task appropriately (e.g., gather tools and vegetables, wash vegetables, chop and slice vegetables, mix in bowl, add dressing) |
| Problem-solving | Solving the problem of using a knife that is too dull to slice |
Box 19-14 Categories of Interventions for Those Living with Impairments of the Executive Functions
Environmental modifications: Examples include using antecedent control, manipulating the amount of distractions and structure in the environment, organizing work and living spaces, and ensuring balance of work, play, and rest.
Compensatory strategies: Examples include the use of external cueing devices such as checklists, electronic pagers, use of reminder systems, organizers.
Task-specific training: Training of specific functional skills and routines including task modifications.
Training in metacognitive strategies to promote a functional change by increasing self-awareness and control over regulatory processes: These include self-instruction strategies, teaching problem-solving, and goal management training.
Data from Cicerone KD, Giacino JT: Remediation of executive function deficits after traumatic brain injury. NeuroRehabilitation 2(3):12-22, 1992; Sohlberg MM, Mateer CA: Management of dysexecutive symptoms. In Sohlberg MM, Mateer CA, editors: Cognitive rehabilitation: an integrative neuropsychological approach, New York, 2001, Guilford Press; and Worthington A: Rehabilitation of executive deficits: the effect on disability. In Halligan PW, Wade, DT, editors: Effectiveness of rehabilitation for cognitive deficits, Oxford, 2005, Oxford University Press.
Box 19-15 Further Strategies to Manage Functional Deficits Secondary to Dysexecutive Symptoms*
1. Organize living and work spaces such as:
 Organizing shelves in kitchen cabinets and the refrigerator based on categories (e.g., by meal, food category, products used together).
Organizing shelves in kitchen cabinets and the refrigerator based on categories (e.g., by meal, food category, products used together). Color code or use in/out tray systems for work and home tasks (e.g., blue dots indicate priority work such as bills to be paid, or files in the bottom tray can be reviewed next week).
Color code or use in/out tray systems for work and home tasks (e.g., blue dots indicate priority work such as bills to be paid, or files in the bottom tray can be reviewed next week). Use organizing technology such as personal data assistants, alarm watches, handheld organizers, and personal information manager software (these may include e-mail applications, a calendar, task and contact management, note taking, and a journal).
Use organizing technology such as personal data assistants, alarm watches, handheld organizers, and personal information manager software (these may include e-mail applications, a calendar, task and contact management, note taking, and a journal). Post lists of usual and typical sequenced tasks in appropriate locations (e.g., a morning ADL routine posted on the bathroom mirror, night tasks such as lock the door and make lunch posted on the nightstand, arrive-at-work tasks such as check e-mail and phone messages posted on the computer screen).
Post lists of usual and typical sequenced tasks in appropriate locations (e.g., a morning ADL routine posted on the bathroom mirror, night tasks such as lock the door and make lunch posted on the nightstand, arrive-at-work tasks such as check e-mail and phone messages posted on the computer screen).Data from Cicerone KD, Giacino JT: Remediation of executive function deficits after traumatic brain injury. NeuroRehabilitation 2(3):12-22, 1992; Sohlberg MM, Mateer CA: Management of dysexecutive symptoms. In Sohlberg MM, Mateer CA, editors: Cognitive rehabilitation: an integrative neuropsychological approach, New York, 2001, Guilford Press; and Worthington A: Rehabilitation of executive deficits: the effect on disability. In Halligan PW, Wade, DT, editors: Effectiveness of rehabilitation for cognitive deficits, Oxford, 2005, Oxford University Press.
Goals
The ability to document OT evaluation and treatment information appropriately is more important than ever. The insurance industry reimburses for OT services according to information provided to them through documentation; the goals set for a patient are critical to the support of the plan of care by the insurance company. Functional outcomes have gained increasing support and, in many cases, are required by insurance companies for reimbursement. Therefore, goals should be meaningful and sustainable; they must be valued and carried out by the patient outside the clinical environment. Examples include:
 Patient will properly sequence dressing tasks involving the legs with fewer than two verbal cues in three out of three trials.
Patient will properly sequence dressing tasks involving the legs with fewer than two verbal cues in three out of three trials.
 Patient will use grab bars or other objects for stability and safety during dressing task with close supervision in three out of three trials.
Patient will use grab bars or other objects for stability and safety during dressing task with close supervision in three out of three trials.
 Patient will demonstrate appropriate and independent use of pillbox for medication schedule in three out of three trials.
Patient will demonstrate appropriate and independent use of pillbox for medication schedule in three out of three trials.
 Patient will prepare a shopping list from a recipe with all needed ingredients with minimal assist in two out of three trials.
Patient will prepare a shopping list from a recipe with all needed ingredients with minimal assist in two out of three trials.
 Patient will independently use 75% of objects and eat 75% of food placed on left side of midline, without verbal cues, in three out of three trials.
Patient will independently use 75% of objects and eat 75% of food placed on left side of midline, without verbal cues, in three out of three trials.
 Patient will prepare a simple, familiar meal with 80% recognition of errors in three out of five trials with close supervision.
Patient will prepare a simple, familiar meal with 80% recognition of errors in three out of five trials with close supervision.
 Patient will use objects appropriately in hygiene tasks without assistance in two out of three trials.
Patient will use objects appropriately in hygiene tasks without assistance in two out of three trials.
 Patient will attend to and perform all steps of audio-cued grooming task in three out of three trials with distant supervision.
Patient will attend to and perform all steps of audio-cued grooming task in three out of three trials with distant supervision.
 Patient will plan and participate in community activities once a week in three out of five trials with supervision.
Patient will plan and participate in community activities once a week in three out of five trials with supervision.
CASE STUDY 1 Neurobehavioral Deficits after Stroke
G.W., a 49-year-old man, was working as a security guard at a prison when he sustained a massive right middle cerebral artery stroke. He was hospitalized for seven days and subsequently received OT on an outpatient basis. G.W.’s neurobehavioral deficits initially included severe left-side spatial and body neglect, anosognosia, and difficulty with spatial relationships, along with hemiparesis, resulting in total dependence in mobility and all ADL except eating (for which he needed moderate assistance).
Initial treatment plans focused on setting up functional activities such as eating, grooming, hygiene, and dressing. G.W. was required visually to scan the left side of space to find needed objects or use both arms to practice use of the left side of the body. (This was achieved through use of guiding techniques because no independent movement of left arm was present.) Diminishing verbal cues were used for G.W. to learn to attend to the left side of his body and left side of space during functional task performance. G.W.’s greatest initial impediment was his steadfast denial that his left arm and leg belonged to him (known as anosognosia). Fortunately, this denial diminished and was no longer present four weeks after the stroke.
Techniques such as matching color markers were minimally successful in treating spatial deficits. However, adaptive devices, such as elastic shoelaces (to prevent the need spatially to execute one-handed shoelace tying), and compensatory strategies, such as slowing down movements and keeping hands on supported surfaces while reaching, were highly successful in increasing G.W.’s independence in daily task performance.
As G.W.’s awareness of his disability improved, use of awareness questioning was emphasized. G.W. initially was questioned after (and then before) each task; he later learned to ask himself questions such as, “What do I do before I start?” “Do I see everything I need?” “Is there anything I forgot?” and “Did I pay attention to my left side?” Awareness questioning was the most successful technique for improving G.W.’s ability to achieve independent performance of basic self-care and eventually perform instrumental ADL without assistance. Initially he lived with his mother and brother after the stroke, but he returned to independent living in his apartment and at the time of discharge was working with vocational rehabilitation services to explore employment options.
CASE STUDY 2 Role of Family in Overcoming Neurobehavioral Deficits after Stroke
M.A., an 82-year-old man, sustained a stroke in the left hemisphere at the age of 80 and subsequently underwent above-the-knee amputation of his right leg due to peripheral vascular disease. M.A. was placed in a skilled nursing facility, and soon thereafter OT services were initiated. Neurobehavioral impairments noted at the time of evaluation included global aphasia, motor and ideational apraxia, and severe attention deficits. M.A. depended on others for all mobility and ADL skills, including eating. M.A.’s family was supportive and visited him daily at lunch and dinnertime. Much of the OT was focused on patient, family, and staff education. The family was taught to use guiding techniques, which they implemented at mealtime and for grooming and hygiene tasks. The family and staff were taught ways to facilitate communication through tactile and visual cues and guiding techniques, ways to decrease environmental stimulation and distractions, and ways to approach M.A. to help him attend to tasks. M.A. responded well to guiding techniques, requiring only occasional tactile cues after initiating the task (through guiding) to eat, comb his hair, and wash his face in a low-stimulus environment. OT continued for seven weeks (because M.A. also was seen for contracture management), and eventually M.A. was discharged from the skilled nursing facility to his family’s care.
Review questions
1. How is the integrated functional approach different from traditional functional approaches, and why is it the recommended approach for cognitive and perceptual impairments?
2. What neurobehavioral components are required to perform a hair grooming task? How can this task be used in the treatment of motor apraxia?
3. How can caregivers adapt environments to assist loved ones with cognitive or perceptual impairments?
4. What are two interventions that can be used to increase function in those living with unilateral neglect? Apraxia? Memory loss?
1. Abreu B, Duval M, Gerber D, et al. Occupational performance and the functional approach. In: Royeen CB, editor. AOTA self-study series: cognitive rehabilitation. Rockville, MD: American Occupational Therapy Association, 1994.
2. Alderman N, Burgess PW, Knight C, et al. Ecological validity of a simplified version of the Multiple Errands Shopping Test. J Clin Exp Neuropsychol. 2003;9(1):31-44.
4. Anderson SW, Tranel D. Awareness of disease states following cerebral infarction, dementia, and head trauma. standardized assessment. Clin Neuropsychol. 1989;3:327-339.
5. Appelros P, Karlsson GM, Thorwalls A, et al. Unilateral neglect. further validation of the baking tray task. J Rehabil Med. 2004:36;6:258-261.
6. Árnadóttir G. The brain and behavior. assessing cortical dysfunction through activities of daily living. St Louis: Mosby. 1990.
7. Árnadóttir G. Evaluation and intervention with complex perceptual impairment. In: Unsworth C, editor. Cognitive and perceptual dysfunction: a clinical-reasoning approach to evaluation and intervention. Philadelphia: FA Davis, 1999.
8. Ayres AJ. Development dyspraxia and adult onset apraxia. Torrance, CA: Sensory Integration International; 1985.
9. Azouvi P, Olivier S, de Montety G, et al. Behavioral assessment of unilateral neglect. study of the psychometric properties of the Catherine Bergego Scale. Arch Phys Med Rehabil. 2003:84;1:51-57.
10. Baddeley AD. The psychology of memory. In: Baddeley AD, Kopelman MD, Wilson BA, editors. The essential handbook of memory disorders for clinicians. Hoboken, NJ: John Wiley, 2004.
11. Baggerly J. Sensory perceptual problems following stroke. Nurs Clin North Am. 1991;26(4):997-1005.
12. Baum CM, Edwards DF, Morrison T, et al. The reliability, validity, and clinical utility of the Executive Function Performance Test. a measure of executive function in a sample of persons with stroke. Am J Occup Ther. 2008:62;4:446-455.
13. Behrmann M, Marotta J, Gauthier I, et al. Behavioral change and its neural correlates in visual agnosia after expertise training. J Cogn Neurosci. 2005;17(4):554-568.
14. Beis JM, Andre JM, Baumgarten A, et al. Eye patching in unilateral spatial neglect. efficacy of two methods. Arch Phys Med Rehabil. 1999:80;1:71-76.
15. Beis JM, Keller C, Morin N, et al. French collaborative study group on assessment of unilateral neglect (GEREN/GRECO). Right spatial neglect after left hemisphere stroke. qualitative and quantitative study. Neurology. 2004:63;9:1600-1605.
16. Ben-Yishay Y, Piasetsky EB, Rattok J. A systematic method for ameliorating disorders in basic attention. New York: Guilford Pres; 1987.
17. Bennett TL. Neuropsychological evaluation in rehabilitation planning and evaluation of functional skills. Arch Clin Neuropsychol. 2001;16(3):237-253.
18. Bergego C, Azouvi P, Samuel C, et al. Validation d’une échelle d’évaluation fonctionnelle de l’héminégligence dans la vie quotidienne. l’échelle CB. Ann Readapt Med Phys. 1995;38:183-189.
19. Beschin N, Robertson IH. Personal versus extrapersonal neglect. a group study of their dissociation using a reliable clinical test. Cortex. 1997:33;2:379-384.
20. Borst MJ, Peterson CQ. Overcoming topographical orientation deficits in an elderly women with a right cerebrovascular accident. Am J Occup Ther. 1993;47(6):551.
21. Broadbent DE, Cooper PF, FitzGerald P, et al. The Cognitive Failures Questionnaire (CFQ) and its correlates. Bri J Clin Psychol. 1982;21(Pt 1):1-16.
22. Brockmann-Rubio K, Gillen G. Treatment of cognitive-perceptual impairments. A function-based approach. Gillen G, Burkhardt A, editors. Stroke rehabilitation: a function-based approach, ed 2, St Louis: Elsevier Science/Mosby, 2004.
23. Bruce MA. Cognitive rehabilitation. intelligence, insight, and knowledge. Royeen CB, editor. AOTA self-study series: cognitive rehabilitation. Rockville, MD: American Occupational Therapy Association, 1994.
24. Burns MS. Clinical management of agnosia. Top Stroke Rehabil. 2004;11(1):1-9.
25. Calvanio R, Levine D, Petrone P. Elements of cognitive rehabilitation after right hemisphere stroke. Behav Neurol. 1993;11(1):25-57.
26. Carlesimo GA, Casadio P, Sabbadini M, et al. Associated visual agnosia resulting from a disconnection between intact visual memory and semantic systems. Cortex. 1998;34(4):563-576.
27. Chainay H, Humphreys GW. The real-object advantage in agnosia. evidence for a role of surface and depth information in object recognition. Cogn Neuropsychol. 2001:18;2:175-191.
28. Cocchini G, Beschin N, Jehkonen M. The fluff test. a simple task to assess body representation neglect. Neuropsychol Rehabil. 2001:11;1:17-31.
29. Condeluci A, Ferris LL, Bogdan A. Outcome and value. the survivor perspective. J Head Trauma Rehabil. 1992:7;4:37.
30. Dawson DR, Anderson ND, Burgess P, et al. Further development of the Multiple Errands Test. standardized scoring, reliability, and ecological validity for the Baycrest version. Arch Phys Med Rehabil. 2009:90;11 Suppl:S41-51.
31. Donaghy S, Williams W. A new protocol for training severely impaired patients in the usage of memory journals. Brain Inj. 1998;12(12):1061-1076.
32. Donkervoort M, Dekker J, Stehmann-Saris FC, et al. Efficacy of strategy training in left hemisphere stroke patients with apraxia. A randomized clinical trial. Neuropsychol Rehabil. 2001:11;5:549-566.
33. Edmans JA, Lincoln NB. Treatment of visual perceptual deficits after stroke. Int Disabil Stud. 1989;11(1):25-33.
34. Edmans JA, Webster J, Lincoln NB. A comparison of two approaches in the treatment of perceptual problems after stroke. Clin Rehabil. 2000;14(3):230-243.
34a. Elliott R. Executive functions and their disorders. Br Med Bull. 2003;65(1):49-59.
35. Evans JJ, Wilson BA, Schuri U, et al. A comparison of “errorless” and “trial-and-error” learning methods for teaching individuals with acquired memory deficits. Neuropsychol Rehabil. 2000;10(1):67-101.
36. Fisher AG. Assessment of motor and process skills. vol. 1. development, standardization, and administration manual, ed 5. Fort Collins, CO: Three Star Press. 2003.
37. Fisher AG. Assessment of motor and process skills. vol. 2. user manual, ed 5. Fort Collins, CO: Three Star Press. 2003.
38. Fleming JM, Strong J, Ashton R. Self-awareness of deficits in adults with traumatic brain injury. how best to measure. Brain Inj. 1996:10;1:1-15.
38a. Funahashi S. Neuronal mechanisms of executive control by the perfrontal cortex. Neurosci Res. 2001;39(2):147-165.
39. Geusgens C, van Heugten C, Donkervoort M, et al. Transfer of training effects in stroke patients with apraxia. An exploratory study. Neuropsychol Rehabil. 2006:16;2:29-213.
40. Gillen G. Cognitive and perceptual rehabilitation. optimizing function. St. Louis: Mosby/Elsevier. 2009.
41. Goldenberg G, Daumuller, Hagmann S. Assessment and therapy of complex activities of daily living in apraxia. Neuropsychol Rehabil. 2001;11(2):147-169.
42. Goldenberg G, Hagmann S. Therapy of activities of daily living in patients with apraxia. Neuropsychol Rehabil. 1998;8(2):123-141.
43. Guiles GM, Clark-Wilson J. use of behavioral techniques in functional skills training after severe brain injury. Am J Occup Ther. 1988;42;10:658-665.
44. Hajek VE. The effect of visuo-spatial training in patients with right hemisphere stroke. Can J Rehabil. 1993;6(3):175.
45. Halligan PW, Cockburn J, Wilson BA. The behavioural assessment of visual neglect. Neuropsychol Rehabil. 1991;1(1):5-32.
46. Hartman-Maeir A, Harel H, Katz N. The Kettle Test—a brief measure of cognitive functional performance. reliability and validity in stroke rehabilitation. Am J Occup Ther. 2009:63;5:592-599.
47. Heilman KM, Watson RT, Valenstein E. Neglect and related disorders. In Hilman KM, Valenstein E, editors: Clinical neuropsychology, ed 4, New York: Oxford, 2003.
48. Helm-Estabrooks N, Emory P, Albert ML. Treatment of aphasic perseveration. Arch Neurol. 1987;44(12):1253-1255.
50. Jabri J. Providing visuoperceptual remediation treatment for stroke patients in the home setting. J Home Health Care Pract. 1992;4(4):36.
51. Jarus T. Motor learning and occupational therapy. the organization of practice. Am J Occup Ther. 1994:48;9:810-816.
52. Kalra L, Perez I, Gupta S, et al. The influence of visual neglect on stroke rehabilitation. Stroke. 1997;28(7):1386-1391.
53. Katzmann S, Mix C. improving functional independence in a patient with encephalitis through behavior modification shaping techniques. Am J Occup Ther. 1994;48(3):259-262.
54. Kertesz A. Visual agnosia. the dual deficit of perception and recognition. Cortex. 1979:15;3:403-419.
55. Kim HJ, Craik FI, Luo L, Ween JE. Impairments in prospective and retrospective memory following stroke. Neurocase. 2009;15(2):56-145.
57. Kime SK. Compensating for memory deficits using a systematic approach. Bethesda, MD: AOTA Press; 2006.
58. Knight C, Alderman N, Burgess PW. Development of a simplified version of the multiple errands test for use in hospital settings. Neuropsychol Rehabil. 2002;12(3):231-256.
59. Kottorp A, Tham K. Assessment of Awareness of Disability (AAD), manual for administration, scoring, and interpretation. Stockholm, Sweden: Karolinska Institutet, NEUROTEC Department, Division of Occupational Therapy; 2005.
60. Lampinen J, Tham K. Interaction with the physical environment in everyday occupation after stroke. a phenomenological study of persons with visuospatial agnosia. Scand J Occup Ther. 2003:10;4:56-147.
60a. Lezak MD. Executive function and motor performance. In: Lezak MD, Howieson DB, Loring DW, editors. Neurological assessment. New York: Oxford University Press, 2004.
61. Lin K, Wu C, Tickle-Degnen L, Coster W. Enhancing occupational performance through occupational embedded exercise. A meta-analytic review. Occup Ther J Res. 1997:17;1:25-47.
62. Lincoln N. Stroke rehabilitation. Curr Opin Neurol Neurosurg. 1992;5(5):677-681.
63. Lincoln NB, Majid MJ, Weyman N. Cognitive rehabilitation for attention deficits following stroke. Cochrane Database Syst Rev. (4):2000. CD002842
64. McIntosh RD, Brodie EE, Beschin N, et al. Improving the clinical diagnosis of personal neglect. a reformulated comb and razor test. Cortex. 2000:36;2:289-292.
65. Niemeier JP. Visual imagery training for patients with visual perceptual deficits following right hemisphere cerebrovascular accidents. a case study presenting the Lighthouse Strategy. Rehabil Psychol. 2002:47;4:426-437.
66. Neistadt ME. A meal preparation treatment protocol for adults with brain injury. Am J Occup Ther. 1994;48(5):431-438.
67. Neistadt ME. The neurobiology of learning. implications for treatment of adults with brain injury. Am J Occup Ther. 1994:48;5:421-430.
68. Neistadt ME. Perceptual retraining for adults with diffuse brain injury. Am J Occup Ther. 1994;48(3):225-233.
69. Nygard L, Bernspang B, Fisher AG, et al. Comparing motor and process ability of persons with suspected dementia in home and clinic settings. Am J Occup Ther. 1994;48(8):689-696.
70. Olson E. Perceptual deficits affecting the stroke patient. Rehabil Nurs. 1991;16(4):212-213.
71. Ownsworth TL, McFarland KM, Young RM. Development and standardization of the Self-regulation Skills Interview (SRSI). a new clinical assessment tool for acquired brain injury. Clin Neuropsychol. 2000:14;1:76-92.
72. Papstrat LA. Outcome and value following brain injury. a financial provider’s perspective. J Head Trauma Rehabil. 1992:7;4:11.
73. Park S, Fisher AG, Velonzo C. Using the assessment of motor and process skills to compare occupational performance between home and clinic settings. Am J Occup Ther. 1994;48(8):697-709.
74. Poole JL. Effect of apraxia on the ability to learn one-handed shoe tying. Occup Ther J Res. 1998;18(3):99-104.
75. Qiang W, Sonoda S, Suzuki M, et al. Reliability and validity of a wheelchair collision test for screening behavioral assessment of unilateral neglect after stroke. Am J Phys Med Rehabil. 2005;84(3):161-166.
76. Radomski MV. Cognitive rehabilitation. advancing the stature of occupational therapy. Am J Occup Ther. 1994:48;3:271-273.
77. Radomski MV, Dougherty PM, Fine S, et al. Case studies in cognitive rehabilitation. In: Royeen CB, editor. AOTA self-study series: cognitive rehabilitation. Rockville, MD: American Occupational Therapy Association, 1994.
78. Reed CL, Caselli RJ, Farah MJ. Tactile agnosia. underlying impairment and implications for normal tactile object recognition. Brain. 1996:119;Pt 3:875-888.
79. Robertson IH, North N. Spatio-motor cueing in unilateral left neglect. the role of hemispace, hand and motor activation. Neuropsychologia. 1992:30;6:553-563.
80. Robertson IH, Ward T, Ridgeway V, Nimmo-Smith I. The structure of normal human attention. the Test of Everyday Attention. J Clin Exp Neuropsychol. 1996:2;6:525-534.
81. Royle J, Lincoln NB. The Everyday Memory Questionnaire-revised. development of a 13–item scale. Disabil Rehabil. 2008:30;2:21-114.
82. Sbordone RJ. Limitations of neuropsychological testing to predict the cognitive and behavioral functioning of persons with brain injury in real world settings. Neurorehabilitation. 2002;16(4):199-201.
83. Schiavetto A, Decaile J, Flessas J, et al. Childhood visual agnosia. a seven-year follow-up. Neurocase. 1997:3;1:1-17.
84. Schwartz MF, Segal M, Veramonti T, et al. The Naturalistic Action Test. A standardised assessment for everyday action impairment. Neuropsychol Rehabil. 2002:12;4:311-339.
85. Shallice T, Burgess PW. Deficits in strategy application following frontal lobe damage in man. Brain. 1991;114(Pt 2):727-741.
86. Simmond M, Fleming JM. Occupational therapy assessment of self-awareness following traumatic brain injury. Br J Occup Ther. 2003;66(10):447-453.
87. Simmond M, Fleming J. Reliability of the self-awareness of deficits interview for adults with traumatic brain injury. Brain Inj. 2003;17(4):325-337.
88. Smith G, Della Sala S, Logie RH, Maylor EA. Prospective and retrospective memory in normal ageing and dementia. a questionnaire study. Memory. 2000:8;5:311-321.
89. Sohlberg MM. Assessing and managing unawareness of self. Semin Speech Lang. 2000;21(2):135-151.
90. Sohlberg MM, Mateer CA. Training use of compensatory memory books. a three stage behavioral approach. J Clin Exper Neuropsychol. 1989:11;6:871-891.
91. Sohlberg MM, Mateer CA. Memory theory applied to intervention. In: Sohlberg MM, Mateer CA, editors. Cognitive rehabilitation: an integrative neuropsychological approach. New York: Guilford Press, 2001.
92. Stone SP, Patel P, Greenwood RJ, et al. Measuring visual neglect in acute stroke and predicting its recovery. the visual neglect recovery index. J neurol Neurosurg Psych. 1992:55;6:431-436.
93. Sunderland A, Harris JE, Baddeley AD. Do laboratory tests predict everyday memory? a neuropsychological study. J Verbal Learn Verbal Behav. 1983;22(3):341-357.
94. Sunderland A, Harris JE, Baddeley AD. Assessing everyday memory after severe head injury. In: Harris JE, Morris PE, editors. Everyday memory, actions, and absent-mindedness. London: Academic Press, 1984.
95. Sunderland A, Walker CM, Walker MF. Action errors and dressing disability after stroke. an ecological approach to neuropsychological assessment and intervention. Neuropsychol Rehabil. 2006:16;6:83-666.
96. Tanemura R. Awareness in apraxia and agnosia. Top Stroke Rehabil. 1999;6(1):33-42.
97. Tham K, Bernsprang B, Fisher AG. Development of the assessment of awareness of disability. Top Stroke Rehabil. 1999;6:184-190.
98. Tham K, Ginsburg E, Fisher A, et al. Training to improve awareness of disabilities in clients with unilateral neglect. Am J Occup Ther. 2001;55(1):46-54.
99. Tham K, Tegner R. The baking tray task. a test of spatial neglect. Neuropsychol Rehabil. 1996:6;1:19-25.
100. Thomas RM, Forde EM, Humphreys GW, et al. A longitudinal study of category-specific agnosia. Neurocase. 2002;8(6):466-479.
101. Toglia JP. Generalization of treatment. a multicontext approach to cognitive perceptual impairment in adults with brain injury. Am J Occup Ther. 1991:45;6:505-516.
102. Toglia JP. Attention and memory. In: Royeen CB, editor. AOTA self-studies series: cognitive rehabilitation. Rockville, MD: American Occupational Therapy Association, 1993.
103. Toglia JP. A dynamic interactional approach to cognitive rehabilitation. In: Katz N, editor. Cognitive and occupation throughout the lifespan. Bethesda, MD: AOTA, 2005.
104. Trombly C. Clinical practice guidelines for post-stroke rehabilitation and occupational therapy practice. Am J Occup Ther. 1995;49(7):711-714.
105. van Heugten C, Dekker J, Deelman B, et al. Outcome of strategy training in stroke patients with apraxia. A phase II study. Clin Rehabil. 1998:12;4:294-303.
106. van Heugten C, Dekker J, Deelman B, et al. Assessment of disabilities in stroke patients with apraxia. internal consistency and inter-observer reliability. Occup Ther J Res. 1999:19;1:55-73.
107. van Heugten C, Dekker J, Deelman B, et al. Measuring disabilities in stroke patients with apraxia. a validity study of an observational method. Neuropsychol Rehabil. 2000:10;4:401-414.
108. van Heugten CM, Dekker J, Deelman BG, et al. Rehabilitation of stroke patients with apraxia. the role of additional cognitive and motor impairments. Disabil Rehabil. 2000:22;12:547-554.
110. Wilson BA. Remediation of apraxia following an anaesthetic accident. In: West J, Spinks P, editors. Case Studies in Clinical Psychology. Bristol UK: John Wright, 1988.
111. Wilson BA, Alderman N, Burgess PW, et al. Behavioural assessment of the dysexecutive syndrome. Edmunds, UK: Thames Valley Test Company; 1996.
112. Wilson B, Cockburn J, Baddeley AD, Hiorns R. The development and validation of a test battery for detecting and monitoring everyday memory problems. J Clin Exp Neuropsychol. 1989;11(6):855-870.
113. Wilson B, Cockburn J, Halligan P. Development of a behavioral test of visuospatial neglect. Arch Phys Med Rehabil. 1987;68(2):98-102.
114. Wilson BA, Evans JJ, Emslie H, et al. The development of an ecologically valid test for assessing patients with dysexecutive syndrome. Neuropsychol Rehabil. 1998;8(3):213-228.
115. Wu C, Trombly C, Tickle-Degnen L. Effects of object affordances on movement performances. A meta-analysis. Scand J Occup Ther. 1998:5;2:83-92.
116. Yuen HK. Increasing medication compliance in a woman with anoxic brain damage and partial epilepsy. Am J Occup Ther. 1993;47(1):30-33.
117. Zemke R. Task skills, problem solving, and social interaction. In: Royeen CB, editor. AOTA self-study series: cognitive rehabilitation. Rockville, MD: American Occupational Therapy Association, 1994.