chapter 18 Impact of neurobehavioral deficits on activities of daily living
After completing this chapter, the reader will be able to accomplish the following:
1. Establish a relationship between neurobehavioral concepts and task performance.
2. Apply the theory on which the Árnadóttir OT-ADL Neurobehavioral Evaluation (A-ONE) is based as a structure for clinical observations of stroke patients.
3. Provide conceptual and operational definitions for neurobehavioral impairments and disability.
4. Apply clinical reasoning skills based on the A-ONE theory for hypothesis testing.
5. Relate the International Classification of Functioning, Disability and Health and the Occupational Therapy Practice Framework, 2nd Edition, to the concepts used in the A-ONE.
6. Provide examples of how strokes can cause different patterns of impairments affecting task performance.
Referrals to occupational therapy for patients who have had a stroke are usually made when the resulting impairments are suspected to affect activity performance. When neurobehavioral impairments result from a stroke, they can affect the performance of daily activities. This chapter contains discussions on the effect of neurobehavioral impairments on activity performance. Topics such as occupational performance, neurobehavior, function of the cerebral cortex, activity limitation, patterns of impairment resulting from different types of strokes, and application of clinical reasoning during assessment are discussed. However, before considering these issues, the following questions might be useful to consider: What are activities of daily living (ADL)? What is neurobehavior? What is neurobehavioral impairment? How is neurobehavior related to activity performance? How is the effect of neurobehavioral impairments on activity performance detected?
Activities of daily living
ADL are defined by the U.S. Department of Health and Human Services72 as basic daily activities such as eating, grooming, toileting, and dressing. The Center for Disease Control and Prevention refers to ADL as “bathing or showering, dressing, eating, getting in or out of bed or chairs, using the toilet, including getting to the toilet, and getting around inside the home.”25 The Occupational Therapy Practice Framework: Domain and Process, 2nd Edition (Framework-II),4 defines ADL as activities “that are oriented toward taking care of one’s own body.” These activities include, similarly to the definitions mentioned previously, bathing or showering, bowel and bladder management, dressing, eating, feeding, functional mobility, personal hygiene and grooming, and toilet hygiene. Thus all three definitions agree on characterizing ADL as self-care tasks and functional mobility. Additionally personal device care and sexual activity are included in the Framework’s definition of ADL. To locate ADL within the whole domain of occupational therapy, ADL are classified as one of eight areas of occupation, according to the Framework-II. The other seven areas of occupation are instrumental activities of daily living (IADL): rest and sleep, education, work, play, leisure, and social participation. In addition to areas of occupation, five other aspects of the domain of occupational therapy to which occupational therapists attend during the process of providing services are defined in the Framework-II. These are client factors, performance skills, performance patterns, contexts, environments, and activity demands.
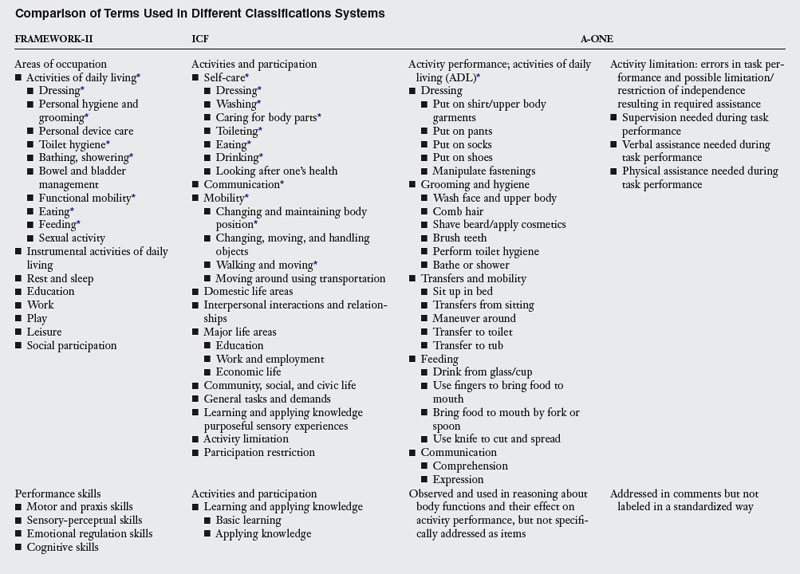
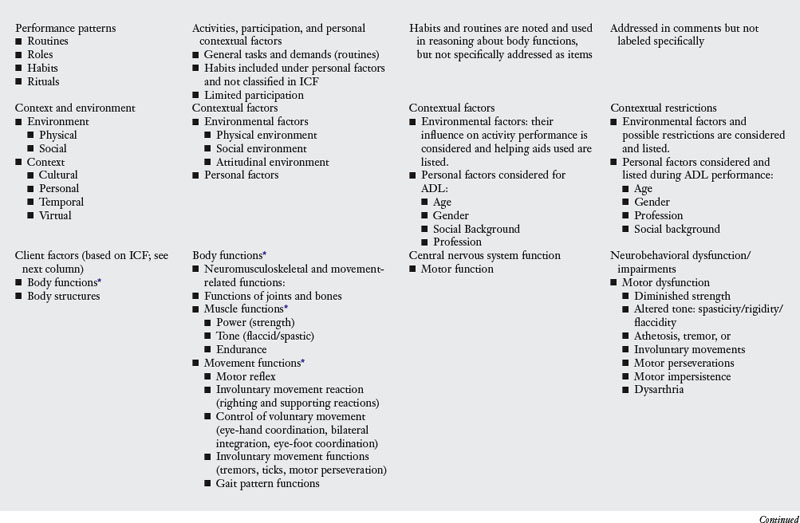
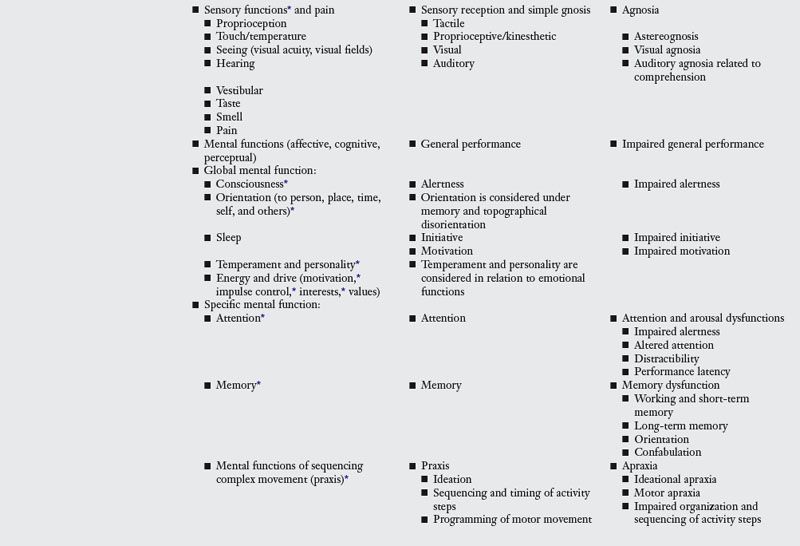
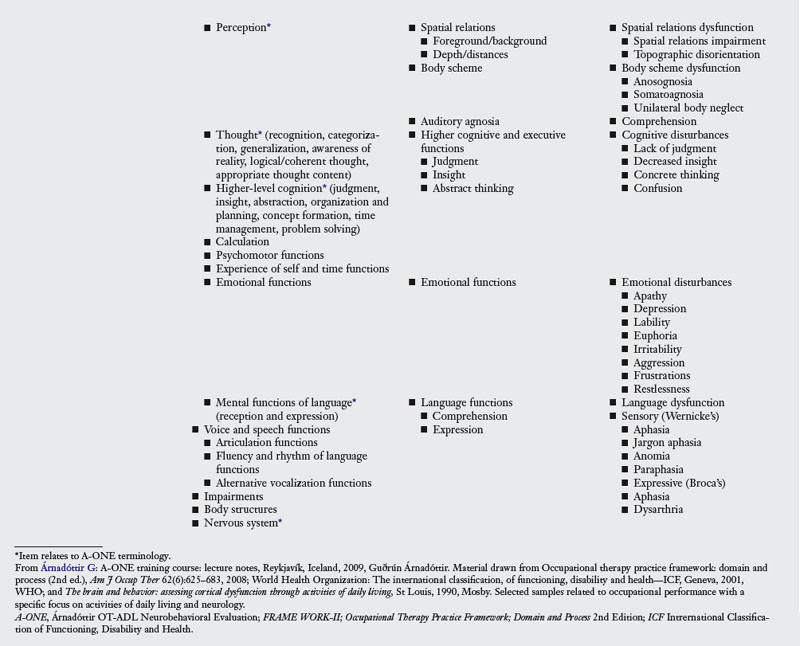
Client factors, including body functions and structures, values, beliefs and spirituality, are the foundation of human performance, according to the Framework-II. These fundamental factors residing from within the individual are required for successful performance of different tasks. The eight main groups of body functions in the Framework-II based on the International Classification of Functioning, Disability and Health (ICF),77 a document developed by the World Health Organization, include a group of mental functions (affect, cognition, perception) divided into global functions and specific functions; a group of sensory functions and pain; neuromusculoskeletal and movement-related functions; cardiovascular, hematological, immunological, and respiratory functions; voice and speech functions; digestive, metabolic, and endocrine functions; genitourinary and reproductive functions; and functions of skin and related structures. Each of these groups can be subdivided into smaller units or factors. Table 18-1 shows important aspects of the domain of occupation as presented in the Framework-II, in view of the main themes of this chapter—neurobehavior and ADL—and relates the Framework’s terminology to the classification systems of the ICF and items used in the Árnadóttir OT-ADL Neurobehavioral Evaluation (A-ONE).6 The A-ONE has more recently been referred to as the ADL-focused Occupation-based Neurobehavioral Evaluation.12,14
The ICF describes two parts: functioning and disability, and contextual factors. Each of these parts has two components. Functioning and disability includes the components of body structures and body functions referring to anatomical parts of the body and functioning of body structures that can become impaired; activities (referring to execution of task or activity by an individual) and participation (involvement in a live situation), thus referring to capacity and performance that can become limited or restricted; and environmental factors that can act as facilitators and barriers of performance.77 As can be seen in Table 18-1, the ICF does not differentiate between activity and participation, nor does it use the terms ADL and IADL tasks. Rather, what has been referred to as ADL earlier in this section spans several terms classified under activities and participation, i.e., self-care tasks, mobility, and communication.
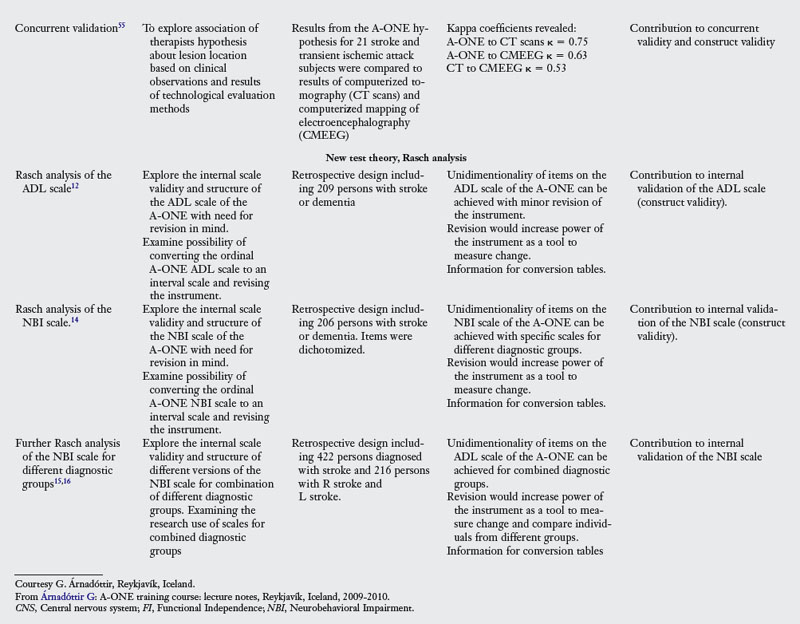
Neurobehavior: the process of linking occupation to neuronal activity
According to Árnadóttir,10,17 neurobehavior is defined as behavior based on neurological function. Neurobehavior can be linked to occupation (defined as a series of actions in which one is engaged)35 and occupational performance (defined as accomplishment of selected activity resulting from the dynamical transaction among the person, context, and activity in the Framework-II),4 as elements of neurobehavior include different types of sensory stimuli evoked by different tasks. These stimuli are processed by different mechanisms of the central nervous system (CNS) and result in different types of behavioral responses. Feedback from the responses affects new sensory stimuli.”6,9 Neurobehavior therefore includes the different types of pertinent neurological body functions necessary for performing different aspects of occupation. “All tasks provide sensory stimuli. Some functions relate to the reception of sensory stimuli, others to CNS processing of that information including for example different functions associated with perception, cognition, emotion, and praxis. Additional functions relate to different behavioral responses, such as affect and movement. The mechanism of nervous-system processing and neurobehavior leading to occupational performance is a complex interaction where different combinations of factors are involved depending on the task.”6,9,17 Fig. 18-1 illustrates the elements of neurobehavior. A neurobehavioral deficit has been defined by Árnadóttir6,17 as a functional impairment of an individual manifested as defective task performance resulting from a neurological processing dysfunction that influences body functions such as affect, body scheme, cognition, emotion, gnosis, language, memory, motor movement, perception, personality, praxis, sensory awareness, spatial relations, and visuospatial skills. Árnadóttir10,17 further defined occupational error as any deviations from flawless responses when performing occupation. Indications of neurobehavioral impairments that limit ADL task performance are based on detection of occupational errors through task analysis of the observed ADL performance. The observed errors are subsequently classified and scored by use of operational definitions of neurobehavioral impairments included in the A-ONE test manual.
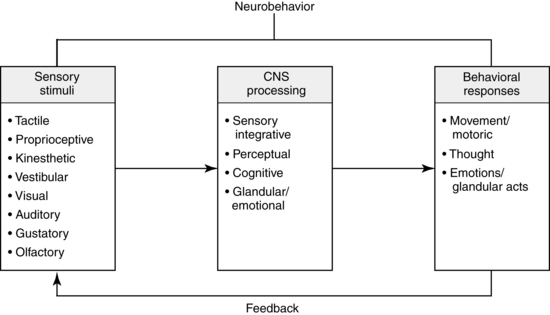
Figure 18-1 Elements of neurobehavior include different types of sensory stimuli. These stimuli are processed by different mechanisms in the central nervous system (CNS) and result in different types of behavioral responses. Feedback from the responses affects new sensory stimuli.
(Adapted from Llorens LA: Activity analysis: agreement among factors in a sensory processing model. Am J Occup Ther 40(2):103, 1986.)
Detecting the effect of neurobehavioral deficits on activity performance
The therapist can detect occupational errors through observation of occupational performance, with these errors indicating the effect of neurobehavioral deficits on task performance. Subsequently, the therapist can hypothesize about the impaired body functions that caused the error. As neurobehavioral deficits often interfere with independence, therapists can benefit from detecting errors in occupational performance while observing ADL and thereby gain an understanding of the impairments affecting the patient’s activity limitation.
Therapists can use the information based on observed task performance in a systematic way as a structure for clinical reasoning to help them assess functional independence related to the performance and to subsequently detect impaired neurological body functions. Such information can be important when intervention methods are aimed at addressing occupational errors6 during any of the following types of intervention programs classified by Fisher36 as adaptive, acquisitional, and restorative occupation, or occupation-based education programs, i.e., programs for families or caregivers of persons with neurological impairments. This method therefore allows the therapist to analyze the nature or cause of a functional problem that requires occupational therapy intervention, as recommended by Holm and Rogers,42,60 and so make the analysis from the view of occupations.
The use of different terms and definitions related to “analysis” in the field of occupational therapy is rather inconsistent and can lead to confusion. The following definitions were in mind when writing this chapter. Activity analysis has commonly been referred to as the process of examining activities in detail by breaking them into their components in order to understand and evaluate the activity. Therapists study body functions that are needed to perform specific tasks and the effects impaired body functions have on task performance.6,46 Activity analysis can be based on particular theories and conceptual frameworks or focused on specific body functions.27,70 Performance analysis is defined by Fisher36 as the “observational evaluation of the quality of a person’s occupational performance” taking into account how effectively the goal directed actions are performed. Task analysis, on the other hand, refers to interpretation of cause be it related to body functions, context, or environmental factors. Latham70 discussed performance focused activity analysis. The therapist in this analysis observes the person perform role related occupations. The role includes tasks that are divided into several activities that are subsequently separated into actions that are based on capacities. Performance focused activity analysis examines these from the top-down by observing the person perform.
When applying the A-ONE principles to evaluate occupational performance and subsequently dysfunctional body functions that limit the performance, the therapist applies different types of clinical reasoning, according to Árnadóttir.7,17 These are interactive reasoning, as interaction between the client and therapist takes place; and procedural reasoning,51 which is also termed diagnostic42,60 or scientific reasoning23 and refers to hypothesis formation following interpretation of cues about the nature of problems that interfere with occupational performance. When using the A-ONE, the therapist observes performance of an ADL task and while classifying level of assistance needed identifies observed errors in performance. The errors can subsequently be used in the clinical reasoning process required for analyzing the task, as they can contribute to hypotheses about different impairments and possible manifestations of CNS dysfunction. They are used to help identify the cause of the dysfunction. During the instrument development of the A-ONE, information based on neurologically focused activity analysis, used to determine which body functions are necessary for performance of the ADL tasks and task analysis based on behavioral observations of persons with neurological dysfunctions, were used to operationalize impairments. The analyses were performed to determine how dysfunction of specific neurological body functions is revealed by neurobehavioral responses and occupational errors during performance of activities. For clinical reasoning during the A-ONE focused task analysis, the therapist keeps in mind different possible neurological body functions and impairments and the theoretical definitions of functional and dysfunctional behavior. An example might explain this process better. A meaningful task, such as eating, calls for a goal directed, purposeful response. Various context and environmental factors are involved, such as food and cutlery, and body functions such as visuospatial relationships, muscle tone, and emotional state. Carrying out the behavior required to eat requires different body functions. When analyzed with the required factors in mind, the quality of the response reveals information not only about independence in ADL but also regarding neurobehavioral impairments—the problems that interfere with independence, such as misjudging distances when reaching out for a cup or not knowing how to use cutlery6 (Fig. 18-2).
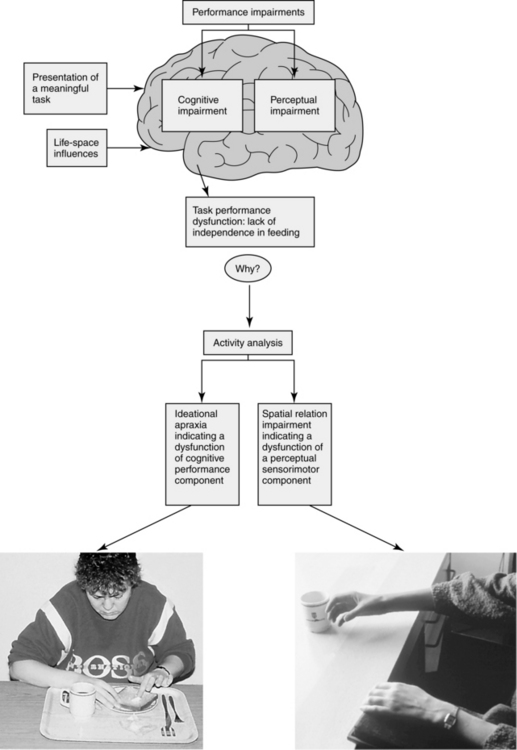
Figure 18-2 Cognitive and perceptual dysfunction leading to ideational apraxia and spatial relations impairment revealed by performance errors observed during feeding and detected by task analysis.
(Adapted from Árnadóttir G: The brain and behavior: assessing cortical dysfunction through activities of daily living, St Louis, 1990, Mosby.)
Function of the cerebral cortex: the foundation of task performance
Occupational therapists observe performance of daily activities regularly as they work with stroke survivors. With the use of clinical reasoning combined with task analysis, detection of impaired neurological body functions is possible. These functions are necessary for optimal task performance. Subsequently, therapists can detect the type and degree of severity of neurobehavioral impairments that interfere with activity performance. For forming hypotheses from ADL observation and errors affecting performance, the therapist commonly draws on his or her neurological knowledge and relates the body functions to functional areas of the brain responsible for different neuronal processing functions. Many body functions are based on neurological function, which takes place at different levels of the CNS. According to Árnadóttir,6 several CNS areas may contribute to a particular type of neuronal processing, resulting in simultaneous or parallel processing at different locations, which contributes to the development of the same body functions. During activity performance, different types of processing may take place simultaneously. Neuronal processing in the brain varies in complexity. It is common to view three levels of functional complexity in the cortex based on Luria’s theories,47,48 which are usually called primary, secondary, and tertiary cortical zones or projection areas.
Functional localization for neurological processing of body functions
During task analysis, the therapist draws on information about neurological functions in the clinical reasoning process when forming and testing hypotheses about impaired functions; a short summary of functional localization follows. Fig. 18-3 illustrates location of different cortical areas, the shades indicating primary, secondary, and tertiary projection areas. The frontal lobes are responsible for motor functions, including motor speech; motor praxis; emotions; intelligence; cognition including attention and working memory; and executive control functions such as ideation, intention, judgment, and motivation. This refers to neuromusculoskeletal and movement-related functions, including muscle and movement functions, according to the ICF terminology; voice and speech functions; and global and specific mental functions. The parietal lobes are concerned with the processing of somesthetic information—and more complex sensory input from different sources, which includes sensory reception of somesthetic information—and specific mental functions related to memory and sequencing of complex movement and to perception and emotional functions, according to the ICF. The occipital lobes process visual information (i.e., visual sensory functions and specific mental functions related to visual perception), and the temporal lobes process auditory information and long-term memory, emotion, and motivation. These functions are classified by the ICF as sensory functions of hearing, voice, and speech functions; global mental functions of temperament and personality; and specific mental functions of memory, perception of hearing, and emotional functions. Table 18-2 summarizes the functions of the different cortical lobes of the brain and relates them to primary, secondary, and tertiary functional areas in these lobes. As indicated in the table, several functional areas in different lobes may contribute to a particular neurological function. Therefore, different cortical areas may be responsible for processing particular neurological body functions. Although function can be related to different anatomical areas, one must remember that plasticity permits deviations from the usual localization sites under certain conditions such as injury or developmental abnormality.
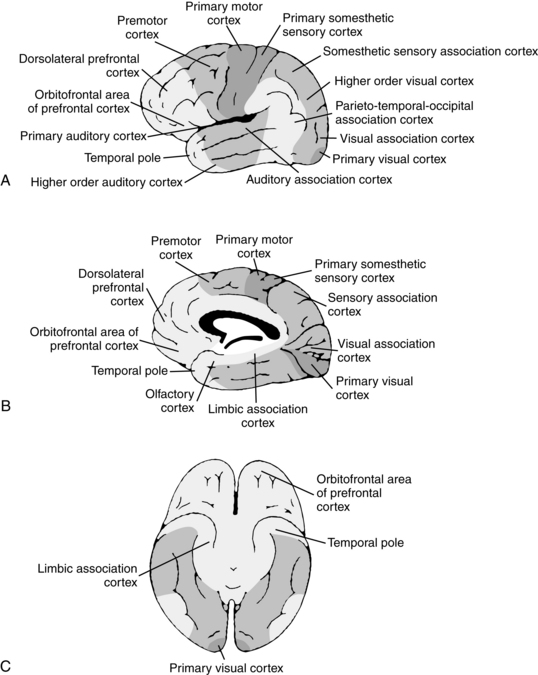
Figure 18-3 Functional organization of the cerebral cortex. A, Lateral surface. B, Medial surface. C, Inferior surface. The different shades refer to primary, secondary, and tertiary functional areas of the cortex. The darkest shades are primary areas, the medium shades are secondary areas, and the lightest shades are tertiary areas.
(From Árnadóttir G: The brain and behavior: assessing cortical dysfunction through activities of daily living, St Louis, 1990, Mosby.)
Table 18-2 Functions of the Cerebral Cortex
Adapted from Árnadóttir G: The brain and behavior: assessing cortical dysfunction through activities of daily living, St Louis, 1990, Mosby.
When considering CNS localization of body functions necessary for task performance, the therapist must keep in mind that the cortex does not function in isolation. The cortex communicates by various pathways with other CNS areas such as the thalamus, the basal ganglia, cerebellum, and brainstem that also contribute to neuronal processing.
Processing of praxis
Although certain neurological functions can be assigned to specific cortical or subcortical locations within lobes, several CNS areas help process particular neurological body functions. Árnadóttir6 summarized neurological information resulting in several processing models indicating processing sites of different functions in the cortex. One example is the processing model for praxis. Praxis takes place in two steps:18 ideation, referring to concept formation related to an activity and classified by the ICF as specific mental function related to thought and higher level cognition including sequencing of complex movement; and planning and programming of movement, which can be related to the neuromusculoskeletal and movement-related functions of the ICF. The result of praxis is motor execution. The ideation involved in praxis requires function of the frontal lobes (prefrontal and premotor areas) and of areas around the lateral fissure. The formulas for movement (praxicons) are stored in the left inferior part of the parietal lobe,40 the left hemisphere in general being superior in storing routinely used codes.39 Access to the left inferior parietal lobe is needed for either side of the body to move. Information flows from this area to the premotor area, which programs movement before the information is conveyed to the primary motor cortex in the left hemisphere (which controls execution of movements of the right side of the body). The premotor cortex on the left side connects with the premotor cortex of the right side by way of the anterior fibers of the corpus callosum and in turn relays the visuokinesthetic motor information to the right hemisphere. The right premotor cortex programs movements and instructs the adjacent primary motor cortex on the execution of movement of the left side of the body (Fig. 18-4).
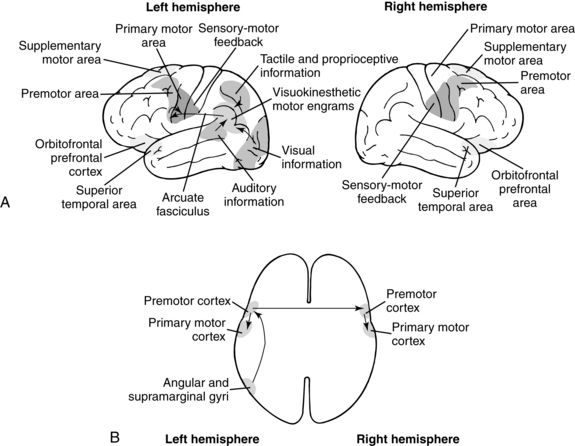
Figure 18-4 Processing of motor praxis. A, Active functional areas of the left and right hemispheres during praxis. B, Transverse view of the most commonly accepted sequential processing model of motor praxis.40
(From Árnadóttir G: The brain and behavior: assessing cortical dysfunction through activities of daily living, St Louis, 1990, Mosby.)
Processing during task performance
Motor praxis (as described previously) is only one type of neurological body function related to neurobehavior. The type of body function and the degree of involvement depend on the task performed. As mentioned, several processing mechanisms may be involved simultaneously in the performance of a particular activity. Árnadóttir has demonstrated this through analysis of task such as brushing hair.6 A person sitting in front of a mirror by a sink where the brush is located has at least three routes by which sensory information related to this particular task will reach the cortex. The person notes the brush visually, and this information travels through the visual pathway to the primary visual cortex where it is synthesized and further analyzed by the association areas. Memories and ideational processes are brought into play; as a result, the person gets the idea to want to brush the hair. Similarly, when the person is instructed verbally to brush the hair, this auditory input travels over the auditory pathway to the primary auditory area of the cortex in the temporal lobe where it is processed by the association areas. Subsequently, the input is compared with information in memory stores, yielding an idea based on the auditory information. The third pathway is somesthetic. A person who grasps or is handed a brush receives tactile and proprioceptive information, which (after it reaches the primary sensory cortex in the parietal lobe) is analyzed by the association areas and integrated with prior experiences.
Information from all three pathways travels from the pertinent primary receptive areas to secondary and tertiary areas where further processing takes place. Attention processes, memory processes, emotions, and higher-order thought are brought into play. The sensory information is integrated with previous experiences, and responses are planned. A response may be emotional or motoric, resulting in different processing mechanisms depending on the nature of the response. Simultaneous processing of information takes place as information from the different secondary association areas is fed into the limbic system, the tertiary association areas in the prefrontal lobe, and the temporal pole, where higher cognitive functions including emotion and memory take place. Different fiber connections in a hemisphere, between hemispheres, and between the cortex and other CNS structures play important roles in this processing.
During processing, ideation, intent to perform an action, and preparation of a sequenced plan of action occur; all result in flow of information to the primary motor cortex and ultimately in the functional response of picking up the brush. This process requires praxis. The intention to perform an action is relayed to the frontal lobes and supplementary motor areas. From the lower left parietal lobe (which houses movement formulas also called visuokinesthetic motor engrams or, more recently, praxicons), information travels to the left premotor cortex (which is responsible for planning and sequencing of movement) on its way to the middle part of the primary motor cortex of the frontal lobe in the left hemisphere (which is responsible for movement performed by the right hand). A series of feedback movement interactions and readjustments follow. This series is based on continuous sensory information from the activity. During the complex process of performing “simple” activity, other responses (e.g., emotional and verbal) may be elicited. Such responses require function of processing areas different from the ones mentioned previously. Fig. 18-5 illustrates some of the processing components that take place during the activity of brushing hair. Observation of task performance that results from this kind of neuronal processing and analysis of the errors detected by observation during the performance may reveal substantial information about function and subsequent dysfunction of the cerebral cortex. Therapists’ neurological knowledge is important and needs to be incorporated into their clinical reasoning when forming hypotheses about impairments and differentiating between hypotheses.
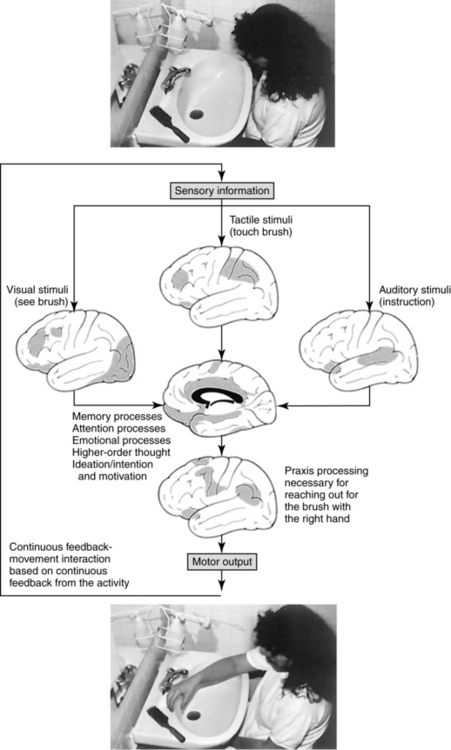
Figure 18-5 Different cortical areas involved in processing of various client factors during an activities of daily living task. A person sitting by a sink preparing for grooming is asked to brush her hair. Note that three types of sensory stimulation can lead to performance.
(From Árnadóttir G: The brain and behavior: assessing cortical dysfunction through activities of daily living, St Louis, 1990, Mosby.)
Dysfunction of the activities of daily living area of occupation due to stroke
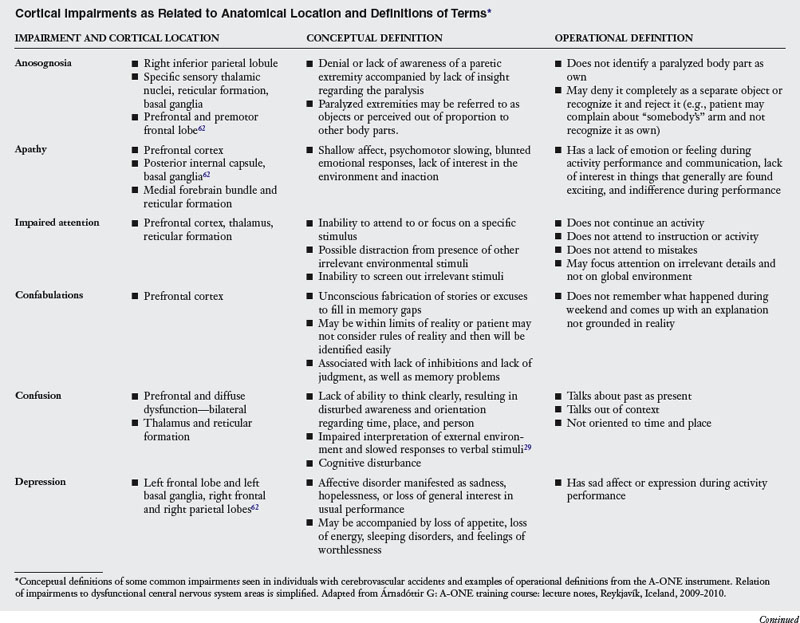
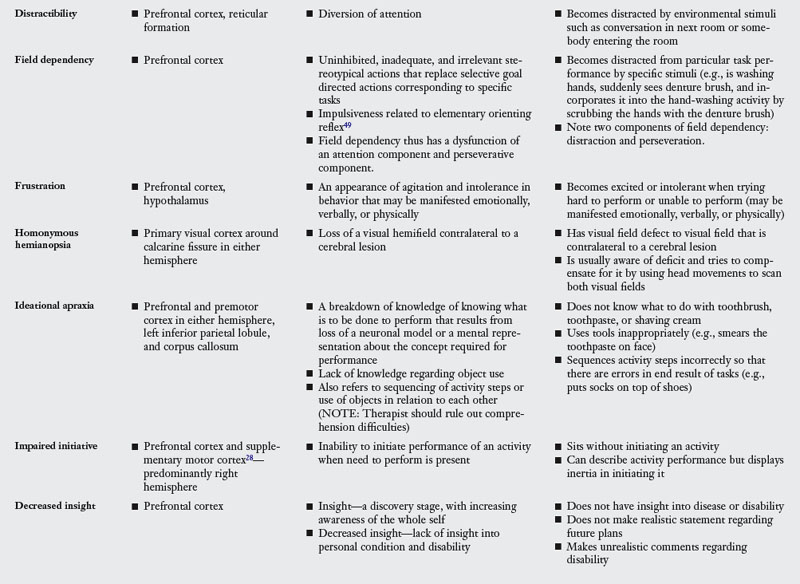
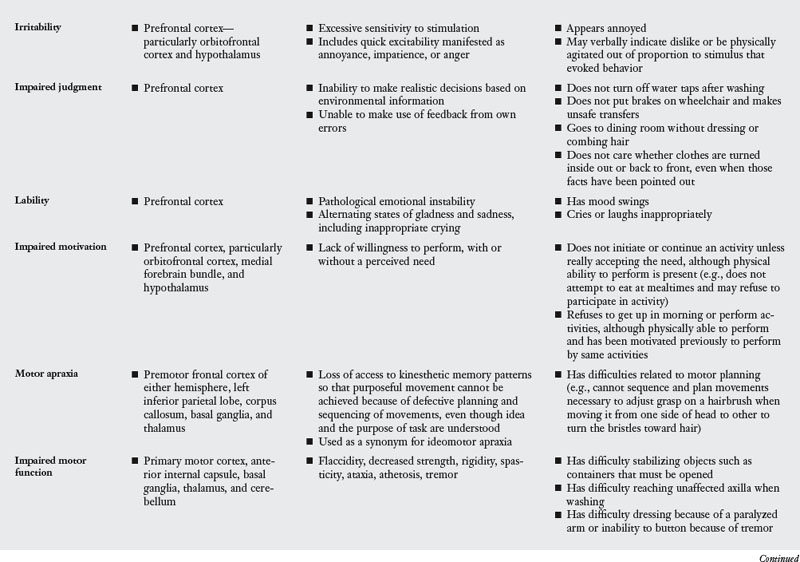
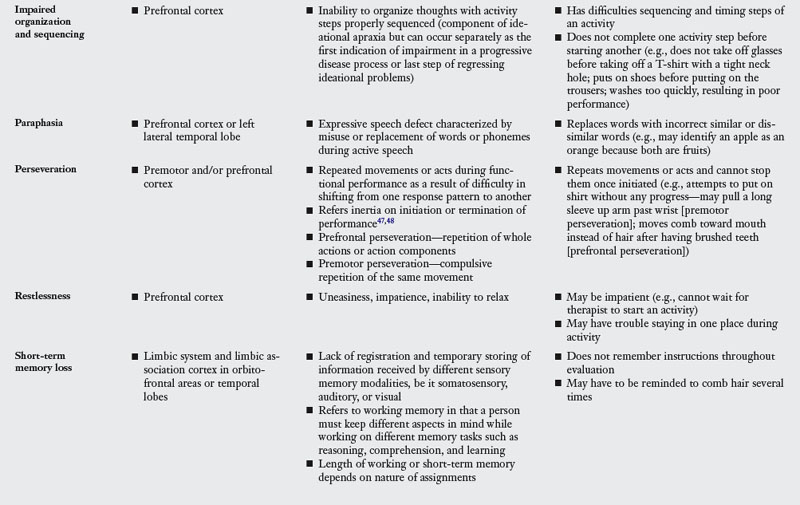
A stroke may affect neurological body functions. Dysfunction of these factors may interfere subsequently with primary ADL. Neurobehavioral impairments may be related to dysfunction of neurological body functions, which have been classified into four groups according to the ICF.77 These groups are (1) neuromuscular functions, (2) sensory functions and pain, (3) mental functions, and (4) voice and speech functions. These functions have been related previously to concepts used in the A-ONE theory in Table 18-2. Concepts may be defined in two ways. Conceptual definition is general and abstract, but an operational definition refers to how particular concepts are measured and observed (e.g., test items with which particular concepts can be measured). The content of the following sections are based on concepts from the A-ONE.
Conceptual definitions of terms
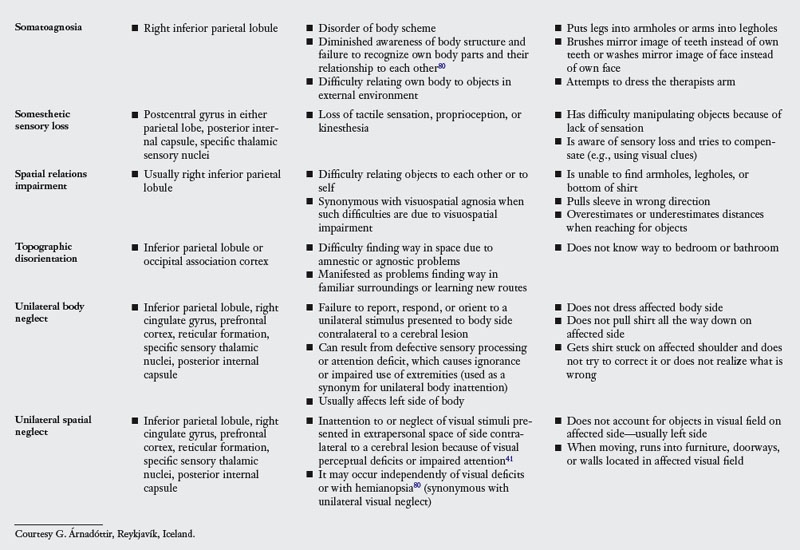
The frontal lobes process functions related to neuromusculoskeletal and movement-related body functions including muscle and movement functions, according to the ICF terminology; voice and speech functions; and global and specific mental functions.17 Dysfunction of the frontal lobes, for example, may affect neuromusculoskeletal body functions processed in the primary motor and premotor areas. Subsequently, the therapist may observe impairments including paralysis of the contralateral body side, muscle weakness, and spasticity. The distribution of impairments is related to lesion localization in the primary motor cortex. Table 18-3 includes definitions of impairments or dysfunction of neurological body functions and relates these to different cerebral lobes.6,17
The parietal lobes process somatosensory and complex sensory information from multimodal stimuli. When a dysfunction of the parietal lobes occurs, impairments related to different functional areas may develop, and these can be related to dysfunctions of body functions, in particular somesthetic sensory functions and specific mental functions.6 Dysfunction of the inferior parietal lobe, which processes information from the secondary association areas of all three posterior lobes, for example, may lead to impairments related to perceptual and motor processing of body functions, in particular specific mental functions related to sequencing of complex movement, memory, and perception. These impairments include bilateral motor- and ideational apraxia, if the left inferior parietal lobe is involved, because the movement formula or praxicons are stored in this area. Spatial relations disorders also may be present when the right hemisphere is involved. These disorders have been defined conceptually as difficulties in relating objects to each other or to the self. Such difficulties may include difficulties with foreground and background perception, depth and distance perception, perception of form constancy and perception of position in space. Further dysfunction of the right inferior parietal lobe may lead to body scheme disturbances including unilateral body neglect. Unilateral spatial neglect may also be present.6 See Table 18-3 for definitions of terms and different lesion sites.
The occipital lobe houses primary and secondary processing areas for visual information. The tertiary area for visual processing is located mainly in the inferior parietal lobe. If a dysfunction of the occipital lobe occurs, impairments are related to visual sensory functions and specific mental functions related to perception of visual information referring to the ICF.17 Lesions of the association area, for example, cause visual agnosia. Different types of visual agnosias exist, including visual object agnosia; visuospatial agnosia, which is a spatial relations disorder of visual origin; prosopagnosia; color agnosia; and associative visual agnosia.6 Visual object agnosia is defined conceptually as the inability of a patient to recognize, name, or demonstrate use of objects seen and results from distorted visual perception, regardless of visual acuity.65 The affected person can see and describe the components of the object but cannot recognize the object itself (see Table 18-3 for additional definitions of terms and lesion sites).6
The temporal lobes are involved with two types of processing—auditory and limbic—that can be related to sensory functions of hearing, voice and speech functions, global mental functions of temperament and personality, and specific mental functions of memory, perception of hearing, and emotional functions. The lateral sides of the hemispheres house primary and secondary processing sites for auditory stimuli and perceptual processing of such information. The tertiary processing area for these functions is located in the inferior part of the parietal lobe.17 A lesion of the auditory association cortex in the left hemisphere, for example, can cause anomia because the memory stores for nouns are located in this area. Anomia is loss of the ability to name objects or retrieve names of persons; the person does have fluent speech. As previously mentioned, Table 18-3 relates defined impairments to dysfunction of different cortical and subcortical areas.
Manifestation of neurobehavioral impairments during task performance: operational definitions of concepts
Operational definitions are how concepts are measured and observed. Following is a review based on Árnadóttir’s operational definitions of terms6 from the A-ONE regarding how one can detect neurobehavioral impairments during task performance in the areas of grooming and hygiene, dressing, functional mobility, and eating. Each of these performance areas comprises several tasks. For successful completion of each of the tasks, involvement of several neurological body functions is necessary. Dysfunction of body functions resulting in the previously defined impairments is manifested differently during performance. The following examples indicate the effect of different impairments on task performance manifested by occupational errors in the various performance areas. This review refers to the terms used in the classification systems of the Framework and the ICF (see Table 18-3 for conceptual and operational definitions of terms). Some impairments affect specific ADL areas. Other impairments are more pervasive and may appear in any ADL performance area or may need to be addressed specifically. One must keep in mind that behavior is flexible and neurobehavioral impairments are complex. The following behavioral examples are guidelines for detecting impairments. However, they cannot be taken for granted without knowledge of neurobehavior, cortical function, activity and task analysis, and clinical reasoning because similar behaviors may result from different impairments at times. Thus the behavior of not washing one arm during the task of washing the upper part of the body may be caused by unilateral body neglect when it occurs in an individual with right hemisphere dysfunction. However, an individual with left hemisphere dysfunction may need assistance to wash the affected arm, partly because of motor paralysis, and also may need guidance to wash the other arm and body parts because of ideation problems and difficulty in organizing and sequencing the activity steps of the task. The patient also may have comprehension difficulties, which complicates the situation. The behavior of not washing an arm therefore may result from unilateral body neglect or ideational apraxia, depending on the situation. Therefore the following examples are to be used only as guidelines. Clinical reasoning and knowledge of neurobehavioral impairments and how the impairments group together in different diagnostic categories are crucial for effective differentiation and classification of impairments.
Personal hygiene and grooming performance area.
Three activities listed in the Framework-II are included in the grooming and hygiene domain of the A-ONE: personal hygiene and grooming, toilet hygiene, and bathing or showering. The performance of grooming and hygiene activities comprises several tasks; for example, washing the face and body and bathing or showering; performing oral hygiene (including brushing teeth); combing hair; shaving; applying cosmetics, deodorants, or perfumes; and performing toilet hygiene. These tasks may be affected by dysfunction of different body functions, resulting in various behavioral outcomes. Dysfunction of neuromusculoskeletal and movement-related functions can result in paralysis, muscle weakness, and spasticity. Paralysis or muscle weakness may be manifested as difficulty in washing the affected arm or axilla (Fig. 18-6, A). The individual may need to learn to use one-handed techniques to overcome the impairment. Adapted equipment also may be needed for the individual to reach body parts such as the back or, if balance is poor, the feet. Stabilizing objects may be a problem; the individual may need a nonslip pad under the soap. While brushing teeth, the person may have problems opening the tube of toothpaste and may need to learn to compensate by stabilizing it between the knees or teeth. The same applies to other containers and the opening of lids. If the individual uses dentures, an adapted toothbrush or a suction brush for stabilization may be necessary (see Chapter 28).
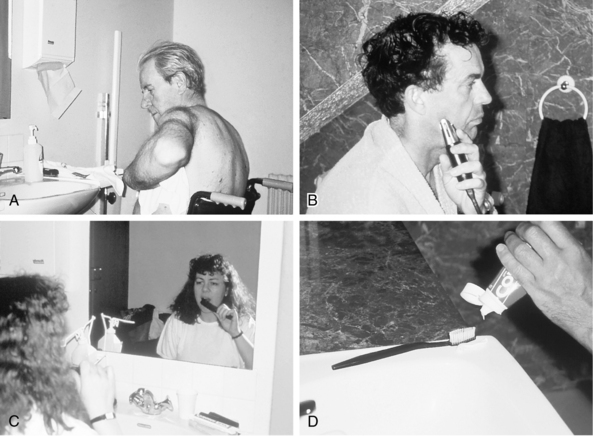

Figure 18-6 Dysfunction of neurological client factors manifested during grooming and hygiene tasks. A, Paralysis results in difficulty washing the affected axilla. B, Motor apraxia makes manipulation of razor difficult. C, Prefrontal perseveration, a part from the previous task of brushing the teeth, is perseverated during combing so that the comb is moved toward the mouth instead of the hair. D, Spatial relations impairment results in underestimation of distances when the individual attempts to place toothpaste on a toothbrush. E, Unilateral body inattention during shaving. Aftershave lotion spills from a bottle held in left hand while individual is reaching with right hand to face and looking into mirror. F, Somatoagnosia. Woman cannot differentiate between a mirror image and her own body when brushing her teeth. G, Ideational apraxia. Man does not know what to do with shaving cream. H, Lack of judgment. Water has been left running with the washcloth in the sink, producing a safety hazard.
Dysfunction of sensory functions can result in impaired tactile and proprioceptive sensation, astereognosis, or hemianopsia with a loss of a visual field, or a loss of part of a visual field may be present. Problems with tactile sensation, proprioception, or stereognosis affect object manipulation. An individual with such problems who does not suffer from inattention or neglect will be aware of the impairment and attempt to compensate for it (e.g., by using vision for sensory feedback). If a part of a visual field is defective or hemianopsia is present, an individual may have to compensate by turning the head. If an individual only has this impairment and not neglect, the individual will be aware of the problem and will be able to describe it, with insight into the dysfunction, and compensate for it.
Dysfunction of sequencing complex movement, classified as specific mental functions, can lead to motor apraxia and motor perseveration. Individuals with motor apraxia have difficulty with motor planning; they may have difficulty adjusting the grasp of a razor when moving from one side of the face to another or when moving the razor to the chin. This requires sequencing and planning of fine finger and wrist movements so that the razor is turned toward the face for effective use (see Fig. 18-6, B). Similarly, motor apraxia may influence the ability to comb or brush hair. The performance may be adequate on the side where the individual starts brushing but when moving the brush to the other side of the head or to the back, the individual has difficulty adjusting the hand movements required to turn the brush toward the hair. Manipulating a toothbrush and other items may be similarly difficult and manifested as “clumsiness.”
Premotor perseveration may be manifested as repetition of the movements of washing the face; the individual cannot stop the movements and take the washcloth to other body parts. Prefrontal perseveration is perseveration of whole acts. The affected individual, having completed one task such as brushing the teeth, begins another activity such as combing but perseverates a part of the previous action program. As a result, the individual approaches the mouth with the comb (see Fig. 18-6, C).
If a dysfunction of the perceptual processing aspect of the specific mental functions is present, a spatial relation disorder, difficulty with left-right discrimination, unilateral body inattention or neglect, unilateral visual inattention or neglect, anosognosia, or somatoagnosia may be expected. Spatial relation disorder may be manifested during hygiene and grooming tasks as difficulty in determining distances. An individual reaching for a toothbrush may overestimate or underestimate its distance. When the individual squeezes toothpaste onto the toothbrush, the paste may end up beside the brush (see Fig. 18-6, D). When trying to stabilize objects, the individual may reach next to the object, resulting in ineffective performance. For example, an individual may reach with the washcloth into the space next to the water faucet instead of under the faucet. When manipulating objects such as dentures, the individual may have problems determining the top from the bottom part of the dentures and the front from the back and left from right.
Impairments related to neglect or inattention can result from dysfunction of the specific mental function of perception or attention. In unilateral body neglect, or inattention, the individual does not use the affected limb according to available control. For example, the individual may not use the arm for stability while attempting to open a bottle. An individual with unilateral body neglect may not wash the affected side but washes other body parts systematically. The same may apply to other tasks as well, such as shaving and combing, in that the individual only attends to one side of the face or hair. A man holding an aftershave bottle in the left hand while looking at his own face in the mirror and reaching with the right hand to the face may tilt the bottle without noticing it and spill the liquid (see Fig. 18-6, E).
In unilateral spatial inattention or neglect, the individual randomly may locate all items in the affected visual field only when accidentally seeing them or may not notice an object at all in the affected visual field and does not systematically compensate for the impairment by rotating the head as required. An individual with somatoagnosia cannot differentiate between the mirror image and self. An individual thus affected may attempt to wash the mirror image of the face instead of the actual face (see Fig. 18-6, F). These individuals may not be able to differentiate between their own body parts and those of others. For example, an individual may grab another person’s arm and attempt to use it to hold onto objects. Somatoagnosia is defined in the A-ONE as a severe dysfunction that usually is accompanied by ideational apraxia and often by spatial relation disorders.
Dysfunctions of global and specific mental functions with an effect on grooming and hygiene tasks include ideational apraxia, organization and sequencing problems related to activity steps, impaired judgment, decreased level of arousal, lack of attention, distraction, field dependency, impaired memory, and impaired intention. Ideational apraxia may appear during grooming and hygiene activities; an individual may not know what to do with the toothbrush, toothpaste, or shaving cream or may use these items inappropriately (e.g., smear toothpaste over the face or spray the shaving cream over the sink; (see Figure 18-6, G). An individual with organization and sequencing difficulties only may have the general idea of how to perform but may have problems timing and sequencing activity steps. Such a patient may not complete one activity step before starting another or may perform activities too quickly due to problems in timing activity steps, resulting in a poor performance.
Lack of judgment may appear as an inability to make realistic decisions based on environmental information, providing that perception of those impulses is adequate. An individual so affected may leave the sink area without turning off the water taps or may leave the wash cloth in the sink, not noticing that the water level is increasing and threatening to overflow (see Fig. 18-6, H).
Field dependency has an attention component and a perseveration component. Individuals with this dysfunction may be distracted from performing a particular task by specific stimuli that they are compelled to act on or incorporate into the previous activity. For example, if an individual with field dependency sees a denture brush while washing the hands, then that person may incorporate the brush into the activity and scrub the hands with the denture brush.
An individual with short-term memory problems may not remember the sequence of activity steps or instructions throughout activity performance. The therapist may have to remind an individual several times to comb the hair, even though the individual does not have comprehension problems.
Lack of initiation may occur during performance of grooming and hygiene tasks; the individual may sit by the sink without performing, even after being asked to wash. With repeated instructions to begin, the individual may indicate that the activity is about to start, yet nothing happens. After several such incidents and if the therapist asks for a plan, the individual may state a detailed plan of action in which the water will be turned on, the washcloth will be picked up and put under the running water, soap will be put on the cloth, and washing will begin. The individual has a plan of action but cannot start the plan. This impairment may be associated with ideational problems as well.
Dressing performance area.
The dressing performance includes the tasks of dressing the upper part of the body, including putting on items such as underwear, T-shirts, pullovers, sweaters, shirts, bras, cardigans, or dresses; dressing the lower part, such as putting on pants, socks, pantyhose, and shoes; and manipulating fasteners, such as zippers, buckles, laces, or Velcro. Following are some examples of the effect of neurobehavioral impairments on task performance in this area. Dysfunction of neuromusculoskeletal and movement-related body function affecting this performance area can result in paralysis of a body side. Individuals with one-sided paralysis must learn one-handed dressing techniques (Fig. 18-7, A).

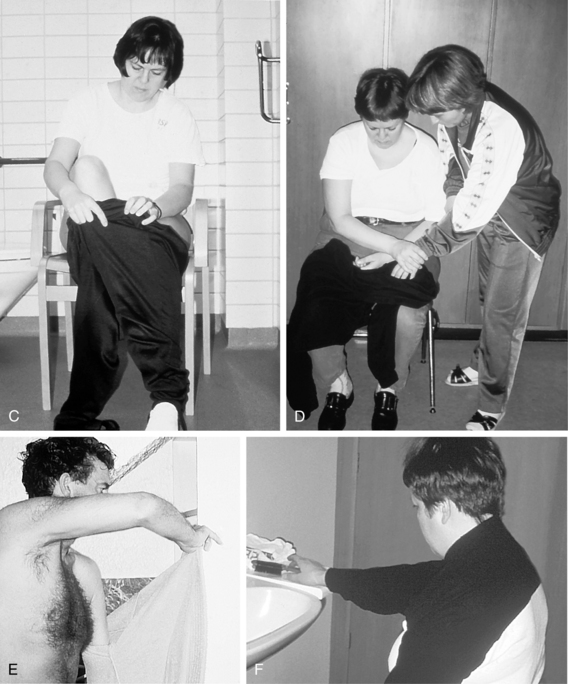
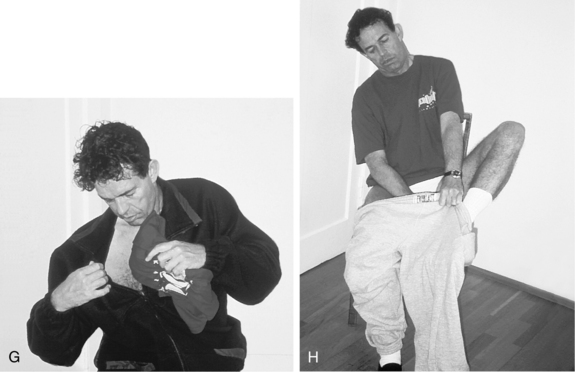
Figure 18-7 Dysfunction of neurological client factors manifested during dressing tasks. A, Paralysis requires use of one-handed dressing techniques. B, Premotor perseveration results in repetitions of movements so that the leghole may be pulled up to the knee; the patient pulls the sock repeatedly, although it is already in place. C, Spatial relations impairment, in which the patient places both legs in the same leghole. D, Somatoagnosia. Woman attempts to dress the therapist’s arm instead of her own. E, Unilateral body neglect. Man attempts to hang up his gown without having undressed his left arm. F, Field dependency. The sight of a comb distracts a woman in the middle of a dressing task. Woman discontinues dressing and begins combing. G, Ideational apraxia. Man knows that the T-shirt should go under the sweater but does not know how to accomplish the goal. H, Organization and sequencing impairment. Man puts on socks and shoes before trousers, resulting in difficulties donning trousers.
Dysfunction of the mental factor of sequencing complex movement can manifest as perseveration. Premotor perseveration may appear during dressing; the individual is unable to stop movements that have been initiated. For example, when the individual is placing an arm in a sleeve, the individual may keep pulling the arm into the sleeve until the end of the sleeve is up to the elbow or shoulder. Similarly the person may repeatedly pull up on a sock, even though it has already covered the foot (see Fig. 18-7, B).
Defective specific mental function factor of perception may result in spatial relation disorders such as difficulty figuring out the front and back, the inside and outside, and the top and bottom of an article of clothing. Although the individual knows that the shirt goes on the upper part of the body and tries to get the arm through the sleeve, the arm may go through the neckhole instead of the sleeve or in the right sleeve instead of the left. An individual may place both legs in the same leghole (see Fig. 18-7, C) or may not perceive that one of the legholes is turned inside out. Right-left disorientation can be related to visuospatial problems; for example, an individual may put the right shoe on the left foot. An individual with spatial relation disorder may pull the sleeve in the wrong direction when attempting to put on a shirt. The individual may be unable to tie shoelaces because of difficulty handling the spatial relations aspects of manipulating shoestrings. Velcro fastenings on shoes may be folded back on themselves instead of being passed through the D-loop before being folded backward. Somatoagnosia may manifest as a patient attempting to dress a therapist’s arm instead of his or her own (see Fig. 18-7, D) or when he or she attempts to place his or her legs into the armholes of a shirt. Thus, the individual has problems with differentiating his or her own body from the therapist’s body and relating objects to corresponding body parts. This is not only a spatial relation problem but also a defect in body image. An individual with only a visuospatial problem cannot find the correct armhole but realizes that a shirt is related to the upper body. This realization is not evident in individuals with somatoagnosia because of his or her body scheme dysfunction.
Unilateral body neglect may be severe, or less severe unilateral body inattention may be present. In severe cases an individual may not dress or undress the affected arm. The individual may even leave the arm in the armhole when undressing and attempt to hang the shirt on a clothes peg on the wall, not cognizant that the arm is still in the armhole (see Fig. 18-7, E). However, the problem is not always this severe or apparent. At times the shirt may get stuck on an affected shoulder without the individual noticing it, or the shirt may not be pulled properly down on the affected side. An individual with unilateral visual neglect or inattention may not put on clothes that are placed in the left visual field because they remain unnoticed.
Dysfunction of global and specific mental functions may be seen as field dependency, ideational problems, or impaired judgment. Field dependency is illustrated by an individual in the middle of the activity of putting on a sweater. Having placed both arms through the correct armholes and the neck through the neckhole, the patient is distracted by the sight of a comb. The activity of dressing subsequently is discontinued immediately as the individual grabs the comb and starts combing his or her hair. After combing, the individual may or may not go back to the task of putting on the shirt (see Fig. 18-7, F). A person might not know what to do with the clothes or how to put them on. A person with ideational apraxia may be able to perform certain activities automatically, such as putting on a sweater. Difficulty arises when the person realizes the T-shirt or undershirt has not been put on under the sweater. The individual may not be able to plan the necessary activity steps to correct the mistake. The T-shirt may be tucked down the neckhole instead of the sweater being removed and the activity started over (see Fig. 18-7, G). An individual with ideational apraxia also may attempt to put a sock on over a shoe. An individual who only has organization and sequencing problems might put shoes on before putting on trousers (see Fig. 18-7, H). However, the general ideas of how to put the clothes on and where they fit are intact. Organization and sequencing problems may appear when an individual dresses the unaffected arm before the affected one and then runs into difficulty dressing the affected arm. The therapist also may detect impaired judgment during dressing performance. An individual may be improperly dressed in the hallways or the dining area, indicating a lack of social judgment. Spatial relation disorder also may affect dressing performance. An affected individual may not be able to differentiate the front and the back of the clothes. Trousers may be put on with the front pockets and fastenings turned backward. Because these spatial relations deficits are of visual origin, the affected individual may not be able to identify the mistakes. However, when a therapist points out that the trousers are backwards, an individual with a lack of judgment might comment that it does not matter how the trousers are worn. A subject with intact judgment would attempt to make corrections, ask for assistance, or otherwise indicate a desire to have the performance corrected.
Functional mobility performance area.
The performance area of functional mobility includes the tasks of rolling over and sitting up in a bed, transferring to and from a bed, transferring to and from a chair, transferring to and from a toilet, transferring to and from a bathtub or a shower, and moving from one room to another. The previously defined impairments may interfere with the tasks of this performance area (see Chapter 14). Following are some examples of how these dysfunctions may be manifested.
If a dysfunction of the neuromusculoskeletal and movement-related functions, such as paralysis is present, it affects strength and control of one body side and thus affects mobility and balance. An individual therefore may need assistance with transfers, require a wheelchair or walking aids, or require supervision or personal assistance for mobility (Fig. 18-8, A).

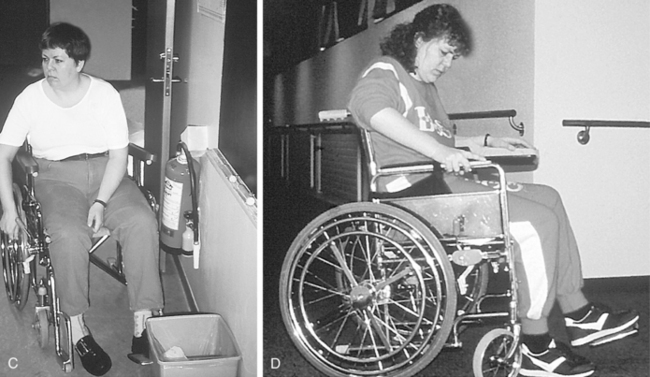
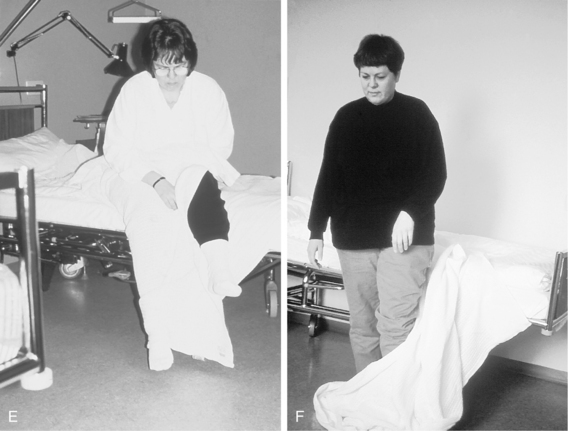
Figure 18-8 Dysfunction of neurological client factors manifested during functional mobility tasks. A, Paralysis affects strength and balance. Individuals require assistance when transferring from bed. A wheelchair is needed for mobility. B, Unilateral body neglect. Woman only moves intact body side over to wheelchair and leaves affected side in bed. C, Unilateral spatial neglect. Woman wheels into a garbage can in a neglected left visual field. D, Ideational apraxia. Woman does not know how to propel the wheelchair and pushes down on the armrest instead of the wheel. E, Organization and sequencing impairment. Woman does not lift off the blanket before sitting up in bed. F, Organization and sequencing impairment and ideational apraxia. Woman attempts to walk away from bed without having moved the blanket.
Dysfunction of the specific mental functions of sequencing complex movement may lead to perseveration and motor apraxia as previously mentioned. Individuals with premotor perseveration may not be able to stop the movements of wheeling a wheelchair; as a result, they continue wheeling and moving after reaching the desired destination.
Dysfunctions of the specific mental functions perceptual factor may result in spatial relation disorders in which the affected individual may misjudge distances. The individual may park a wheelchair too far from a bed or chair for a transfer. An individual with unilateral body neglect or inattention may not account for the affected body side when moving. Such an individual may hit furniture with the affected arm or walk into obstacles such as doorways. When transferring from the bed to a chair, an individual may only move the unaffected side to the chair, leaving the affected side in bed or off the chair (see Fig. 18-8, B). An individual with severe neglect also may have the impairment of anosognosia. These individuals may deny that they are paralyzed or that their affected arm or side is a part of themselves. The affected limb may be referred to as an object, or these individuals may claim that someone else’s arm is lying in bed with them. One man with anosognosia was heard to comment that he was going to occupational therapy and that he would “need to bring the arm along,” because the occupational therapist “always works on the arm.” Unilateral spatial neglect or inattention refers to the phenomenon in which the individual does not account for visual stimuli from the affected visual field. The individual may walk or wheel into obstacles such as garbage cans, furniture, doorways, or other individuals (see Fig. 18-8, C). Topographic disorientation, in which the person has visuospatial problems or memory problems regarding spatial locations also may be present. The individual does not know the way to different, familiar locations such as the bathroom, dining room, bedroom, or therapy department.
If a dysfunction of the global and specific mental factors is present, ideational apraxia or organization and sequencing problems may occur during transfers and mobility tasks. Individuals with ideational apraxia may not know how to get into bed. They literally may throw themselves into the bed. An individual may not know how to wheel a wheelchair and may push down repeatedly on the armrest (see Fig. 18-8, D). (However, the therapist should rule out attention problems.) An individual with organization and sequencing problems may sit up in bed without taking off the blanket but will remove the blanket before standing up (see Fig. 18-8, E). However, an individual with additional ideational apraxia may sit up without lifting the blanket off and then attempt to stand up and walk away without moving the blanket, thus producing a safety hazard (see Fig. 18-8, F). An individual with organization and sequencing problems only may not put on wheelchair brakes before transferring or take them off before moving. This particular performance difficulty might occur when memory problems are present as well. If memory problems without impaired judgment are present, the results of the unsafe transfers (e.g., instability) may remind these individuals to lock the brakes.
Eating performance area.
Neurobehavioral impairments or dysfunction of the previously mentioned body functions may affect dysfunction of eating performance, such as chewing and swallowing, drinking from a glass or a cup, eating without utensils (only using the fingers), eating with a fork or a spoon, and using a knife to cut or spread. Many of these tasks are accomplished earlier in the developmental sequence than some of the tasks mentioned previously.
A dysfunction of the neuromusculoskeletal and movement-related factors may result in paralysis of one side of the body, resulting in poor sitting balance and use of only one arm. Tactile and proprioceptive sensation in the affected hand and arm may be impaired because of defective sensory functions. All these impairments may affect eating tasks that require sitting balance and bilateral integration of the arms (e.g., stabilizing a slice of bread while buttering it or a slice of meat while cutting it, eating an egg, or peeling an orange). Because of the impairments, these eating tasks may require different performance techniques, helping aids, or personal assistance.
An individual with motor apraxia classified as dysfunction of the specific mental factor of sequencing complex movement according to the ICF classification system may spill soup when moving the spoon from the bowl to the mouth, a task that requires much significant adjustment of fine finger and wrist movements to keep the spoon level. Motor apraxia may result in “clumsy movements” when spreading butter, resulting in problems manipulating the knife (Fig. 18-9, A). Premotor perseveration is demonstrated when an individual cannot stop the movements of bringing the spoon to the mouth from the bowl after having finished the soup. Another example is the continuation of chewing movements after the food has dissolved in the mouth. Prefrontal perseveration, or perseveration of actions rather than movements (a cognitive factor), may manifest when an individual who has finished eating yogurt with a spoon reaches out for the spoon again to use it to get a sip of milk from a glass rather than drink directly from the glass (see Fig. 18-9, B).
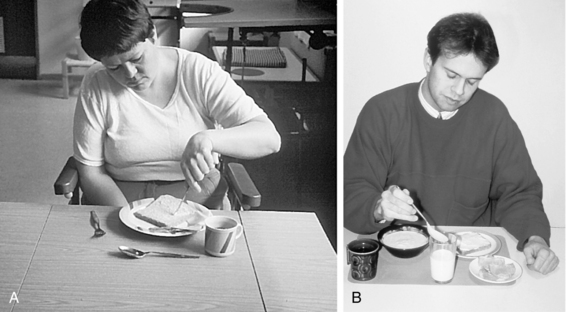
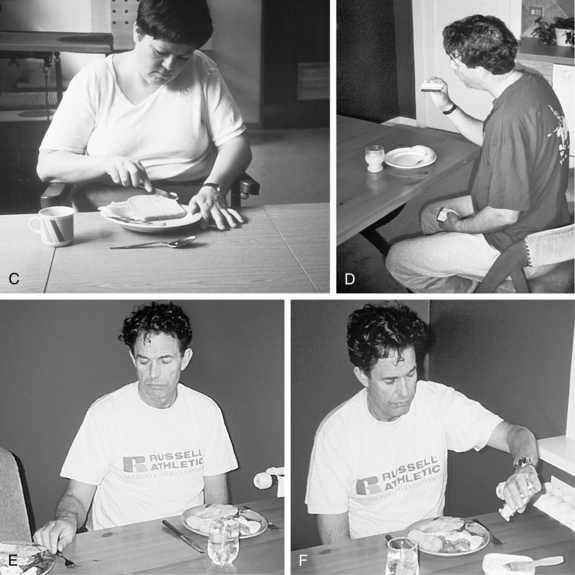
Figure 18-9 Dysfunction of neurological client factors manifested during feeding and eating tasks. A, Motor apraxia makes manipulation of a knife difficult when buttering bread. B, Prefrontal perseveration. Man continues to move the spoon toward the glass instead of drinking from it, after having used the spoon to eat yogurt. C, Spatial relations impairment. Woman attempts to stabilize a piece of bread but misjudges distances and grabs the side of the plate instead. D, Unilateral body neglect. Man does not attend to a piece of bread in left hand; hand slides unnoticed off the table, and man grabs another slice with right hand. E, Unilateral spatial neglect. Man does not notice fork in his left visual field but solves problem by borrowing a fork from the next plate in the right visual field. F, Ideational apraxia. Man does not know what salt is used for and shakes it over butter container.
Dysfunction of specific mental perceptual factors affecting eating behavior may result in spatial relation disorders; an individual trying to stabilize a slice of bread to butter it may misjudge distance and grab the plate instead of the bread (see Fig. 18-9, C). The individual may also overestimate or underestimate distances and reach beside the cup instead of grabbing the cup. Unilateral body neglect may occur during eating when the individual does not use the hand in a natural relation to its available function. Individuals may start eating bread using the left hand, “forget” that the bread is in the hand, and proceed to eat other items as the hand holding the bread slides off the table (see Fig. 18-9, D). Unilateral spatial neglect may manifest in that the individual may not attend to objects or food in the affected visual field. For example, an individual may not notice a fork in the left visual field and attempts to solve the problem by grabbing the next person’s fork located by a plate in the right visual field (see Fig. 18-9, E). Individuals may not eat food located in the affected visual field, although they enjoy that particular type of food.
Dysfunction of global and specific mental function factors may result in ideational apraxia in which the affected individual does not know which utensils to use or how to use them. The individual may simplify the activity by using the fingers to eat meat instead of a fork. The person also may misuse objects. An individual may attempt to eat the soup with a knife. Activity steps may be left out of the sequence, resulting in defective performance. An affected individual may not take the shell off an egg before attempting to eat it or may not peel an orange before biting it. An individual may have the proper object in hand but may not know how to use it for the situation at hand: the individual may open a teabag, remove the tea leaves, and place them in the cup instead of placing the bag in the cup. Individuals may misuse objects; for example, they may sprinkle salt on the butter container (see Fig. 18-9, F). Field dependency may be manifested during feeding activities. Individuals may start grabbing food items before having positioned themselves properly at the table. Individuals also may grab items as they are seen, although the items are inappropriate for the activity at hand.
Pervasive impairments.
According to the A-ONE classification,6,8,17 impairments can be classified as specific or pervasive in relation to activity performance. The impairments described in the previous sections and affecting specific tasks of an ADL domain are classified as specific because they are observed in relation to the particular task, whereas other impairments are not task-specific. Thus some impairments are not necessarily tied to a particular performance area but can occur in relation to any performance area. Emotional and affective disturbance classified by ICF as global mental functions, such as apathy, depression, frustration, irritability, aggression, and lack of motivation, are examples of this because they may affect task performance in different areas of occupation.
As stated earlier, different impairments have different effects on task performance. The behavioral examples described in this chapter are intended as guidelines to assist therapists in detecting impairments revealed by errors observed during task performance for assessment purposes. This information, used with the appropriate theoretical background and clinical reasoning, is important in determining intervention strategies. Occasionally, differentiation between impairments with similar behavioral manifestations may be difficult, particularly for less experienced therapists. Knowledge of neurological function and of how impairments are grouped in different diagnostic categories may be valuable for clinical reasoning in such instances.
Patterns of impairments resulting from strokes
In a preceding section, neurobehavioral impairments were defined and related to different cortical areas. Involvement of dysfunction affecting neurological body functions depends on various pathological conditions resulting in stroke and the different anatomical areas involved. The cerebral blood supply depends mainly on three arteries in each hemisphere: the middle and anterior cerebral arteries, which are branches of the internal carotid artery, and the posterior cerebral artery, which is a branch of the basilar artery, formed by the union of the vertebral arteries.45 Two major types of cerebrovascular dysfunction cause neurological lesions: (1) ischemia, or insufficient blood supply to the brain, which is responsible for 70% to 80% of all strokes, and (2) hemorrhage, or bleeding, caused by a ruptured blood vessel, which accounts for the remaining 15% to 20% of strokes.2,6,24,72 Hemorrhage results in swelling and compression of brain tissue. Different subtypes of strokes occur. Ischemia is subdivided into thrombosis, or blood flow obstruction caused by a local process in one or more blood vessels; embolism, in which blood flow obstruction is caused by materials from distant parts of the vascular system; and decreased systemic perfusion, or hypoperfusion, in which low systemic perfusion pressure results in reduced blood flow.6,24,72
Hemorrhage is subdivided into subarachnoid hemorrhage, which occurs at the surface of the brain and intracerebrally, and intraparenchymal hemorrhage, or bleeding in the cerebral tissue.2,6,24 Each type of stroke results in different patterns of impairment. The type of impairment and severity depend mainly on the anatomical location of the lesion.3,24 These further depend on the rate of arterial occlusion, adequacy of the collateral circulation, resistance of brain structures to ischemia,24 duration and severity of ischemia, hematoma size, and underlying mechanism of hypoperfusion79 and on edema.
Dysfunction of different arteries leads to different patterns of impairments. If the middle cerebral artery, for example, is occluded, affecting blood supply to the lateral aspect of the hemisphere, the impairments vary depending on which branches of the artery and which hemisphere is affected. If the insult affects the upper trunk of the middle cerebral artery, which supplies the lateral aspects of the frontal and parietal lobes, hemiplegia is expected on the contralateral body side, especially of the face and arm, along with hemisensory loss, including tactile and proprioceptive information. This type of insult also may cause impairment of a visual field to the opposite site of the lesion. If the right hemisphere is impaired, unilateral neglect of space and body may result, as well as attention deficits, including unilateral body inattention and unilateral spatial inattention, anosognosia, spatial relation dysfunction, unilateral motor apraxia of the left side (if not paralyzed), lack of judgment, lack of insight, field dependency, and organization of behavior and activity steps. Emotional disturbances such as apathy, lability, and depression also may be present. If the left hemisphere is involved, speech and language functions may be impaired, and bilateral motor apraxia may be observed. Ideational apraxia and perseverations and emotional disturbances such as depression and frustration may be a consequence. If the lower trunk of the middle cerebral artery is affected, visual field defect of the contralateral visual field, Wernicke’s aphasia caused by involvement of the left hemisphere, and emotional disturbances may be present.6,24 Table 18-4 indicates patterns of impairments as they relate to dysfunction of different cerebral arteries and systemic hypoperfusion, a diffuse cerebral dysfunction affecting the watershed regions or the border zones in the periphery of the major cerebral arteries, and different CNS areas, because of various vascular pathological conditions (see Chapter 1).
Table 18-4 Cerebral Artery Dysfunction: Cortical Involvement and Patterns of Impairment
| ARTERY | LOCATION | POSSIBLE IMPAIRMENTS |
|---|---|---|
| Middle cerebral artery: upper trunk | Lateral aspect of frontal and parietal lobe | |
| Middle cerebral artery: lower trunk | Lateral aspect of right temporal and occipital lobes | |
| Middle cerebral artery: both upper and lower trunks | Lateral aspect of the involved hemisphere | |
| Anterior cerebral artery | Medial and superior aspects of frontal and parietal lobes | |
| Internal carotid artery | Combination of middle cerebral artery distribution and anterior cerebral artery | |
| Anterior choroidal artery, a branch of the internal carotid artery | Globus pallidus, lateral geniculate body, posterior limb of the internal capsule, medial temporal lobe | |
| Posterior cerebral artery | Medial and inferior aspects of right temporal and occipital lobes, posterior corpus callosum and penetrating arteries to midbrain and thalamus |
|
| Basilar artery proximal | Pons |
|
| Basilar artery distal | Midbrain, thalamus, and caudate nucleus |
|
| Vertebral artery | Lateral medulla and cerebellum |
|
| Systemic hypoperfusion | Watershed region on lateral side of hemisphere, hippocampus and surrounding structures in medial temporal lobe |
|
Clinical reasoning involved in using the a-one
As mentioned in an earlier section of this chapter, the therapist applies different types of clinical reasoning when applying the A-ONE principles to evaluate task performance and dysfunctional body functions that limit the performance. Further exploration is necessary in relation to the reasoning that goes into the A-ONE. When observing dressing performance, the therapist may detect a critical cue such as not dressing one arm. The therapist interprets this cue, and other cues, by using previously described conceptual and operational definitions from the theory behind the A-ONE instrument and forms hypotheses. Possible hypotheses might be (1) lack of somesthetic sensory input from the arm, (2) unilateral body neglect—in which the person does not attend, usually to the left arm—that may or may not be paralyzed, (3) organization and sequencing problems in which the person is leaving an activity step out of the performance, or (4) ideational apraxia, in which the person does not have an idea of what to do with the shirt or how to put it on. In addition to considering definitions of terms when choosing the appropriate hypotheses, or determining which impairment is most likely to cause the particular activity limitation, the therapist keeps in mind indications of impairments during other activities because these might support a particular hypothesis. The neurological information on functional localization and patterns of impairments as related to different diagnoses or different cerebral arteries described in the previous section also would be included in the reasoning and hypothesis formation. Thus, if the patient (1) knows in general how to use objects, not to mention if the patient can state a plan of action for the activity performance, but does not use the left hand according to muscle strength, or (2) has other impairments that fit with the picture of right hemisphere dysfunction such as spatial relations impairment, one would probably suspect unilateral body neglect or inattention to body side as a result of right hemisphere dysfunction. The therapist would consider sensation in the arm because this may or may not be defective if neglect or inattention exists and could affect arm use. The therapist also would check insight into activity limitations and occupational errors by using operational definitions from the pervasive scale. If sensory loss exists, the patient is aware of the problem and how it affects performance. If neglect or inattention exists, the patient will not be aware consistently of the impairment and its effect on activity performance. If, however, cues indicate the patient is having difficulties with object use in other activities as well, cannot state a plan of action, or has language problems that might indicate a defect in inner language and problems forming a plan of action, one might conclude that the impairment of ideational apraxia limits the dressing performance. Thus, the therapist might hypothesize that ideational apraxia caused by left hemisphere dysfunction might be the nature of the problem that interferes with task performance.17 This information may be useful combined with other types of reasoning such as conditional reasoning51 (see Chapter 17) when making decisions regarding intervention methods, as discussed later.17
Assessment methods
Occupational therapists use basically two evaluation and intervention approaches when working with patients with neurological conditions: deficit-specific approach, also termed bottom-up, restorative, or remedial approach; and functional adaptation or compensation approach, also referred to as top-down, or adaptive approach. Evaluation tools used when applying the deficit-specific approach are aimed at the impaired body structures and functions, using the ICF terminology. The evaluation tools of the functional approach target the activity level or occupational performance. Today, different authors within occupational therapy emphasize the importance of focusing on task performance or occupational functioning in a top-down fashion when assessing patients rather than focusing on impairments.13,36,38,54 They also stress the importance of using standardized evaluation methods that relate occupational performance to body functions,13,36,38,42,50 or performance skills.21
The previous sections have described how the therapist can detect neurobehavioral impairments during observation of task performance by the use of task analysis based on the A-ONE theoretical framework. Functional assessments may include nonstandardized and standardized observations. According to Unsworth,71 a nonstandardized hypothesis testing approach for evaluation could be useful for therapists who have not had the chance to complete the required training for standardized assessments such as the A-ONE and the Assessment of Motor and Process Skills34 (see Chapter 21). Most authors agree that standardized assessments have established, during their developmental process, uniform standards regarding assessment conditions, materials, and instructions for collecting and analyzing information that must be followed precisely. Furthermore, particular assessments may require specific training programs.5,19,20,58,61 The development of conceptual and operational definitions can further be considered an important aspect of providing uniform standards.
Determining for which purpose information is needed is a crucial prerequisite for choosing an evaluation method. For gathering information for goal setting and choice of intervention, either standardized or nonstandardized evaluations may serve the desired purpose. However, if the purpose is to measure change in performance, standardized methods are not enough. Most instruments used in rehabilitation have ordinal scales. Such scales can be used as a base for descriptions of performance, but in order to measure performance interval scales are mandatory.22,52,78 Thus, in rehabilitation, increased emphasis is being placed on use of scales that have measurement properties67 both for clinical and research use. Such scales allow for measuring change over time and comparisons of different groups.
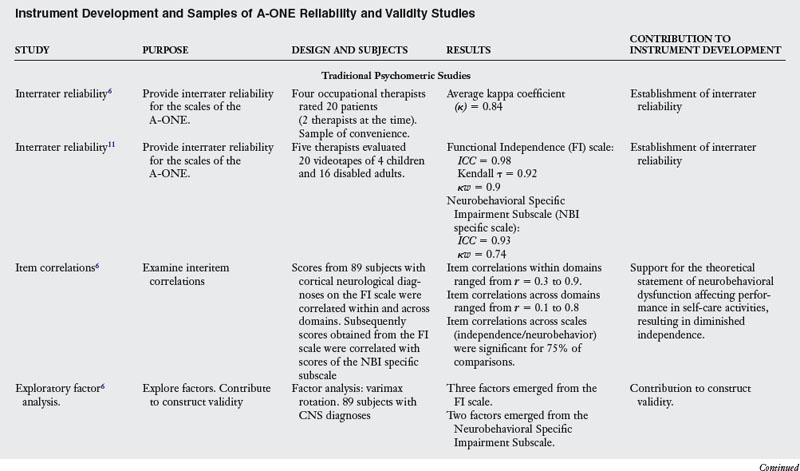
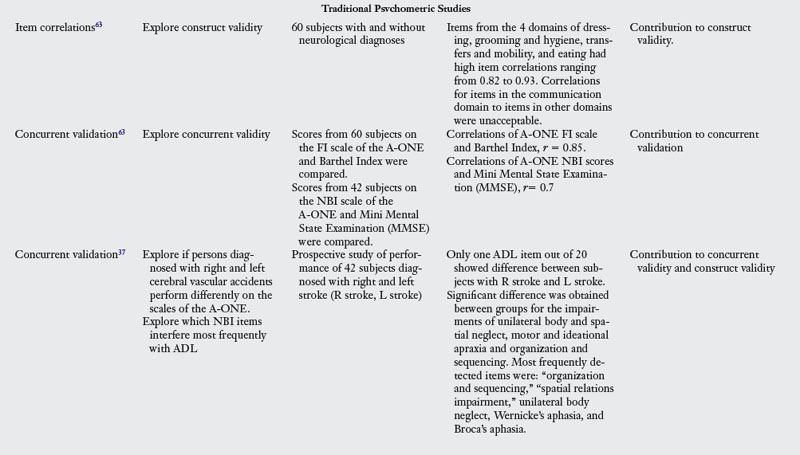
In contrast to the nonstandardized method reviewed earlier in this chapter and based on the A-ONE, the A-ONE instrument, a criterion based method, is standardized; that is, it includes detailed administration and scoring instructions. Several studies of validity and reliability have been conducted to ensure the A-ONE does what its developer claims it does and that it measures the traits consistently (Table 18-5). The instrument requires a training seminar for therapists to ensure reliability.17,63 The original development of the instrument was based on traditional psychometric methods and use of ordinal scales, as the purpose was to gather useful information for goal setting and intervention ideas, not to evaluate change. Increased demand for evidence-based practice and efficacy in rehabilitation services call for instruments with measurement potential. For this reason, the new test theory was used to revalidate the A-ONE and explore if the original ordinal scales could be converted to interval scales. The ADL scale of the A-ONE has successively been Rasch analyzed, and development of conversion tables to convert the ordinal scores recorded after observation of ADL performance to interval scores is taking place.12 Interval scales have also recently been constructed based on the ordinal neurobehavioral impairment scales of the A-ONE, by application of Rasch analysis.14 Thus, the revalidated A-ONE instrument permits comparison between patients in addition to monitoring of progress, regardless of which trained therapist administers and interprets the evaluation. The results provide useful information to guide the choice of intervention method based on strengths and weaknesses of the patient, from the perspective of task performance and body functions.
The way in which the A-ONE provides information on task performance dysfunction in different ADL domains and the neurobehavioral impairments that might affect ADL performance, becomes evident by exploring the case study that follows this review. The therapist first fills in scores for the level of assistance needed for task performance. Observations are written in the comments and reasoning sections about ineffective actions observed as errors in task performance. Subsequently the therapist reasons, based on the content of the observed errors, about the type of impairment responsible for the error. The neurobehavioral impairment is then scored based on whether the impairment is present or not and how much assistance is needed to complete the task.
The case study illustrated in Fig. 18-10 describes a patient who sustained a right hemispheric stroke. The A-ONE assessment was used to evaluate ADL performance and the type and severity of neurobehavioral impairments that interfered with task performance. The study demonstrates how neurobehavioral impairment interferes with ADL performance and how the two types of dysfunction—impaired neurological body functions and their effect on task performance—may be evaluated by different scales of the same assessment.
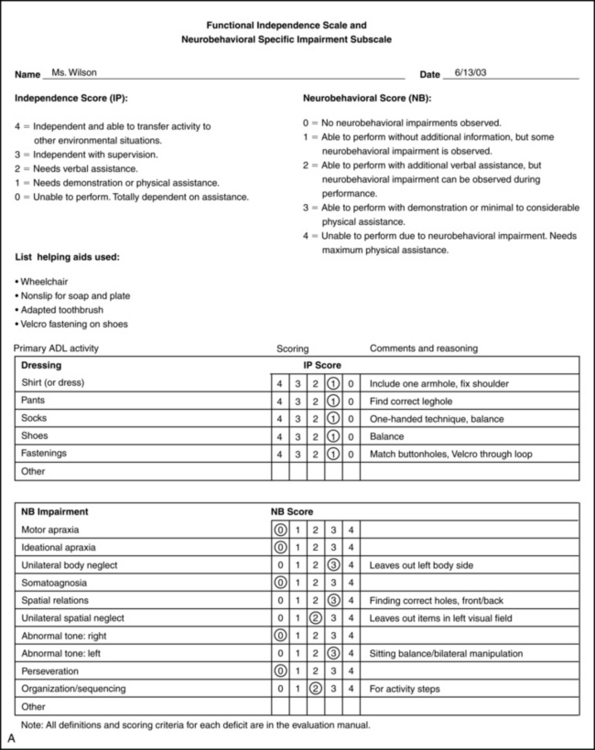
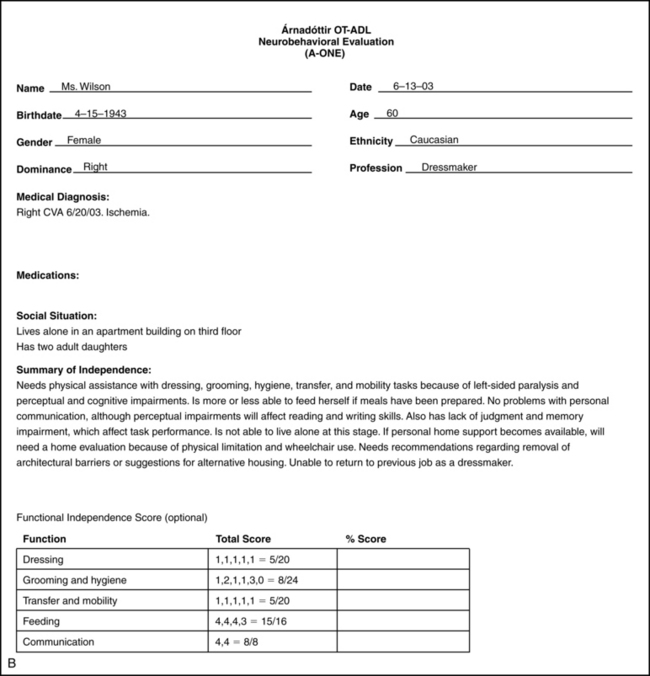
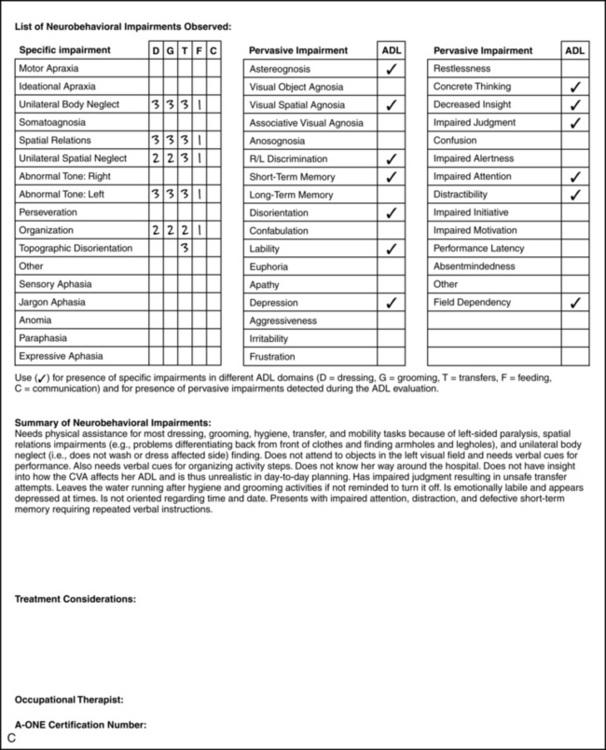
Figure 18-10 A, Árnadóttir OT-ADL Neurobehavioral Evaluation (A-ONE): sample from the dressing domain of the Functional Independence Scale and the Neurobehavioral Specific Impairment Subscale for Ms. Wilson. B, A-ONE ADL summary sheet. C, A-ONE neurobehavioral summary sheet.
(Courtesy G. Árnadóttir, Reykjavík, Iceland.)
The case study presents an individual who needs physical assistance with all items in the dressing domain of the Functional Independence Scale of the A-ONE (Fig. 18-10, A). The limitations in ADL task performance resulting in diminished independence are related to several neurobehavioral impairments including unilateral body neglect, spatial relations impairment, unilateral spatial neglect, organization and sequencing problems, and left hemiplegia (as indicated by scores on the Neurobehavioral Specific Impairment Subscale of the A-ONE). The dressing domain is one of five domains on the Functional Independence Scale of the A-ONE. Summary sheets from the A-ONE indicating scores in the other functional domains and different neurobehavioral impairments are also shown (see Fig. 18-10, B and C). A subsequent evaluation performed three months later indicated observed improvement in ADL performance. Measures of person ability were obtained by comparing the raw scores to conversion tables. Comparison of the ability measures from the initial evaluation (0.58 logits) to the follow-up evaluation (2.39 logits) revealed significant improvement (1.81 logits) in the magnitude of the measures.
Some authors have suggested use of deficit-specific tests as a follow-up of the functional evaluation under specific conditions. These conditions include circumstances in which the therapist has difficulties defining deficits, when a new therapist needs to refine observation skills,56,57 when therapists require an aid in quantification of the severity of the deficit,57 and/or when the therapist needs to report efficacy of treatment in research studies.50 A therapist interested in applying a deficit-specific approach to evaluate dysfunction of body functions (e.g., muscle strength and tone, motor apraxia, spatial relations, neglect, and memory) has a choice of applying test batteries or evaluations aimed at specific impairments. Examples of test batteries used by occupational therapists to evaluate a range of impairments in patients with stroke are the Lowenstein Occupational Therapy Cognitive Assessment (LOTCA)43 and the Rivermead Perceptual Assessment Battery (RPAB).73 Examples of standardized deficit-specific tests available for evaluating some of the impairments mentioned in the case presented in Fig. 18-10 are the Behavioral Inattention Test (BIT)76 for unilateral neglect or inattention; the Motor-Free Visual Perception Test—Vertical (MVPT—V),53 a deficit-specific evaluation that could be used to examine presence of spatial relations impairments; the Test of Every Day Attention (TEA)59 for attention deficits; the Behavioral Assessment of the Dysexecutive Syndrome (BADS)74 for evaluating prefrontal dysfunction; Rivermead Behavioral Memory Test (RBMT)75 for everyday memory functions; the Self-Reporting Awareness Test1 and the Assessment of Awareness of Disability68 for evaluating insight; a test for imitating gestures30 used to evaluate ideomotor apraxia; and a test for ideational apraxia.31 See Chapter 19.
Several studies have explored the relationship of scores from ADL instruments to scores from different cognitive, perceptual, and motor instruments for different reasons. These include examination of the associations between disability and impairment, search for prognostic factors useful for rehabilitation, and establishment of ecological validity for different scales. Sample size, type and number of items, scales, and psychometric methods used vary considerably in these studies. However, most of the obtained results support the notion that impairments and lowered ADL function are associated, although the reported strength of the association varies between studies. Correlations of scores from cognitive and perceptual scales to ADL scales most frequently range from small to moderate (r = 0.2 to 0.6).26,32,33,38,66 Correlations of motor functions to ADL scores sometimes reach higher values than cognitive and perceptual comparisons.45,66 Gillen38 pointed out in his consideration for evaluation of those with functional limitations secondary to neurological impairments that separate evaluations of cognitive and motor tasks reveal different results from using tasks that combine different body functions. Further, the performance of more than one task at the time, as is often the case in natural context as opposed to deficit-specific testing situations, may lead to worse performance. Thus, it is emphasized here that information from deficit-specific tests cannot replace information from observation in a natural context. Further, no other evaluation format can replace observation of task performance in natural settings.6,13,36
Summary
The information in this chapter has provided guidelines for the observation of stroke patients during task performance with the purpose of detecting impairments that interfere with independent performance. The conceptual and operational definitions provided in this text, based on the A-ONE, are important to ensure consistency of the method. The review allows therapists to interpret cues and to form hypotheses regarding impairments and activity limitation. However, this information has limitations and as presented in this text is not standardized. The standardized A-ONE instrument has recently been revalidated, adding measurement properties to previously established reliability and validity. The instrument aids therapists in understanding the reasons for the activity limitations. The instrument aids the therapist in analyzing the nature or cause of a functional problem requiring occupational therapy intervention. Subsequently, therapists can speculate about the best intervention for activity limitation and impaired body functions (see Chapter 19). Therapists can base the decision on information from the evaluation and the therapist’s knowledge of different intervention methods.Whether they are focused on the level of activity performance only or choosing to consider the CNS level of body functions as well either in influencing choice of tasks and environments or informing the patient’s support system about what to expect in terms of impairments and activity limitations in the persons performance. However, one must keep in mind that at present no functional assessment prescribes treatment, and therefore clinical reasoning is necessary to combine evaluation results with available treatment choices, and patient’s specific conditions such as conceptual factors. Furthermore, research studies are needed to test the efficacy of intervention and theories.49,64,69 For such testing, valid and reliable instruments are mandatory.
Review questions
1. Which kind of lesions may produce unilateral motor apraxia of the left side of the body and how might that impairment affect task performance of brushing teeth?
2. You observe a person placing both legs in the same leghole of a pair of pants. Which impairment(s) might cause such an error in performance and what is your reasoning for the decision(s) you made?
3. If an individual does not wash both sides of the body spontaneously, impairments such as unilateral body neglect, organizational and sequencing problems, or ideational apraxia might be suspected. How could you use clinical reasoning to differentiate among the different possible impairments?
4. What is the difference between expected impairments in the presence of a right middle cerebral artery dysfunction compared with expected impairments of a left middle cerebral artery dysfunction?
5. How might impairments of the left middle cerebral artery limit task performance in dressing?
1. Abreu BC. Evaluation and intervention with memory and learning impairments. In: Unsworth C, editor. Cognitive and perceptual dysfunction: a clinical reasoning approach to evaluation and intervention. Philadelphia: FA Davis, 1999.
2. American Heart Association. American Stroke Association. types of stroke, (website). www.strokeassociation.org/presenter.jhtml?identifier= 1014, August 20, 2009. Accessed
3. American Heart Association. American Stroke Association. effects of stroke, (website). www.strokeassociation.org/presenter.jhtml?identifier= 1052, August 20, 2009. Accessed
4. American Occupational Therapy Association. Occupational therapy practice framework. domain and process, ed. 2. Am J Occup Ther. 2008:62;6:625-683.
5. Anastasi A, Urbina S. Psychological testing, ed. 7. Upper Saddle River, NJ: Prentice Hall; 1997.
6. Árnadóttir G. The brain and behavior. assessing cortical dysfunction through activities of daily living. St Louis: Mosby. 1990.
7. Árnadóttir G. Impact of neurobehavioral deficits on ADL. Theoretical principles behind the Árnadóttir OT-ADL Neurobehavioral Evaluation (A-ONE) Poster presentation at the twelfth World Congress of Occupational Therapists. Montréal, Canada: World Federation of Occupational Therapists. 1998.
8. Árnadóttir G. Evaluation and intervention with complex perceptual impairment. In: Unsworth C, editor. Cognitive and perceptual dysfunction: a clinical reasoning approach to evaluation and intervention. Philadelphia: FA Davis, 1999.
9. Árnadóttir G. Neurobehavior. the key to occupation. Poster presentation at the thirteenth World Congress of Occupational Therapists. Stockholm, Sweden: World Federation of Occupational Therapists. 2002.
10. Árnadóttir G. Development versus dysfunction. Neurobehavioral perspective related to errors in occupational performance. Poster presentation at the seventh European Congress of Occupational Therapy. Athens, Greece: European Congress of Occupational Therapy. 2004.
11. Árnadóttir G. Arnadóttir OT-ADL Neurobehavioral Evaluation (A-ONE). interrater reliability. Poster presentation at the At Forum. Stockholm, Sweden: Förbundet Sveriges Arbetsterapeuter. 2005.
12. Árnadóttir G, Fisher AG. Rasch analysis of the ADL scale of the A-ONE. Am J Occup Ther. 2008;62(1):51-60.
13. Árnadóttir G. Árangur af iðjuþjálfun einstaklinga með taugaeinkenni. Hentug ADL matstæki. Iðjuþjálfinn. 2008:30;1:28-39.
14. Árnadóttir G, Fisher AG, Löfgren B. Dimensionality of nonmotor neurobehavioral impairments when observed in the natural contexts of ADL task performance. Neurorehabil Neural Repair. 2009;23(6):579-586.
15. Árnadóttir G, Löfgren B, Fisher AG. Neurobehavioral functions evaluated in naturalistic contexts. Rasch analysis of the A-ONE Neurobehavioral scale. Manuscript submitted for publication, 2009.
16. Árnadóttir G, Löfgren B, Fisher AG. The impact of neurobehavioral dysfunction on ADL performance in clients with right versus left hemispheric stroke. 2009. Unpublished manuscript
17. Árnadóttir G. A-ONE training course. lecture notes. Reykjavík, Iceland: Guðrún Árnadóttir. 2009–2010.
18. Ayres AJ. Developmental dyspraxia and adult onset apraxia. Torrance, CA: Sensory Integration International; 1985.
19. Bailay DM. Research for the health professional. a practical guide, ed. 2. Philadelphia: FA Davis. 1997.
20. Benson J, Schell BA. Measurement theory. application to occupational and physical therapy. Deusen JV, Brundt D, editors. Assessment in occupational therapy and physical therapy. Philadelphia: Saunders, 1997.
21. Bernspång B, Fisher AG. Differences between persons with right or left cerebral vascular accident on the assessment of motor and process skills. Arch Phys Med Rehabil. 1995;76(12):1144-1151.
22. Bond TG, Fox CM. Applying the Rasch model. fundamental measurement in the human sciences, ed. 2. Mahwah, NJ: Erlbaum. 2007.
23. Boyt Schell BA. Clinical reasoning. the basis of practice. Crepeau EB, Cohn ES, Boyt Schell BA, editors. Willard and Spackman’s occupational therapy, ed. 10, Philadelphia: Lippincott-Williams & Wilkins, 2003.
24. Caplan LR. Stroke. a clinical approach, ed. 2. Boston: Butterworth-Heinemann. 1993.
25. Center for Disease Control and Prevention. Health policy data requests—Limitations in ADL and IADL, (website). www.cdc.gov/nchs/health_ policy/ADL_tables.htm, July 2, 2009. Accessed
26. Cooke DM, McKenna K, Fleming J, Darnell R. Construct and ecological validity of the Occupational Therapy Adult Perceptual Screening Test (OT-APST). Scand J Occup Ther. 2006;13(1):49-61.
27. Crepeau EB, Boyt Schell BA. Analyzing occupations and activity. In: Crepeau EB, Boyt Schell BA, Cohn ES, editors. Willard and Spackman’s occupational therapy. Philadelphia: Lippincott-Williams & Wilkins, 2008.
28. Damasio AR, Anderson SW. The frontal lobes. Heilman KM, Valenstein E, editors. Clinical neuropsychology, ed. 3. New York: Oxford University Press. 1993.
29. Daube JR, Sandok BA. Medical neurosciences. an approach to anatomy, pathology and physiology by systems and levels. Boston: Little, Brown. 1978.
30. De Renzi E, Fabrizia M, Nichelli P. Imitating gestures. a quantitative approach to motor apraxia. Arch Neurol. 1980:37;1:6-10.
31. De Renzi E, Lucchelli F. Ideational apraxia. Brain. 1988;111(5):1173-1185.
32. Donkervoort M, Dekker J, Deelman BG. Sensitivity of different ADL measures to apraxia and motor impairments. Clin Rehabil. 2002;16(3):299-305.
33. Edmans JA, Lincoln NB. The relation between perceptual deficits after stroke and independence in activities of daily living. Br J Occup Ther. 1990;53(4):139-142.
34. Fisher AG. Assessment of motor and process skills. Development, standardization, and administration manual, vol 1, ed. 6. Fort Collins, CO: Three Star Press. 2006.
35. Fisher AG. Overview of performance skills and client factors. McHugh Pendleton H, Schultz-Krohn W, editors. Pedretti’s occupational therapy practice skills for physical dysfunction, ed. 6. St. Louis: Mosby. 2006.
36. Fisher AG. Occupational therapy intervention process model. A model for planning and implementing top-down, client-centered, and occupation-based interventions. Fort Collins, CO: Three Star Press. 2009.
37. Gardarsdóttir S, Kaplan S. Validity of the Árnadóttir OT-ADL neurobehavioral evaluation (A-ONE). performance in activities of daily living in persons with left and right hemisphere damage. Am J Occup Ther. 2002:56;5:499-508.
38. Gillen G. Cognitive and perceptual rehabilitation. Optimizing function. St Louis: Elsevier. 2009.
39. Goldberg E, Costa LD. Hemisphere differences in the acquisition and use of descriptive system. Brain Lang. 1981;14(1):144.
40. Heilman KM, Gonzalez Rothi LJ. Apraxia. In Heilman KM, Valenstein E, editors: Clinical neuropsychology, ed. 3, New York: Oxford University Press, 1993.
41. Heilman KM, Watson RT, Valenstein E. Neglect and related disorders. In Heilman KM, Valenstein E, editors: Clinical neuropsychology, ed. 3, New York: Oxford University Press, 1993.
42. Holm MB, Rogers JC. The therapists thinking behind functional assessment II. In: Royeen CB, editor. AOTA self study series: assessing function. Rockville, MD: American Occupational Therapy Association, 1989.
43. Itzkovich M, Elazar B, Averbuch S, et al. Lowenstein occupational therapy cognitive assessment. LOTCA™ Manual. Pequannock, NJ: Maddack. 1990.
44. Kiernan JA. Barr’s the human nervous system. an anatomical viewpoint, ed. 8. Philadelphia: Lippincott-Williams & Wilkins. 2005.
45. Korpelainen JT, Niilekselä E, Myllylä VV. The Sunnaas Index of Activities of Daily Living. Responsiveness and concurrent validity in stroke. Scand J Occup Ther. 1997:4;1:1-36.
46. Llorens LA. Activity analysis. agreement among factors in a sensory processing model. Am J Occup Ther. 1986:40;2:103-110.
47. Luria AR. The working brain. an introduction to neuropsychology. New York: Basic Books. 1973.
48. Luria AR. Higher cortical functions in man, ed. 2. New York: Basic Books; 1980.
49. Ma HI, Trombly CA. A synthesis of effects of occupational therapy for persons with stroke II. Remediation of impairments. Am J Occup Ther. 2002:56;3:260-274.
50. Mathiowetz V. Role of physical performance component evaluations in occupational therapy functional assessment. Am J Occup Ther. 1993;47(3):225-230.
51. Mattingly C, Fleming MH. Clinical reasoning. forms of enquiry in a therapeutic practice. Philadelphia: FA Davis. 1994.
52. Merbitz C, Morris J, Grip JC. Ordinal scales and foundations of misinference. Arch Phys Med Rehabil. 1989;70(4):308-312.
53. Mercier L, Hebert J, Colarusso RP, et al. MVPT-V Motor free visual perception test—vertical format—manual. Novato, CA: Academic Therapy Publications; 1997.
54. Neistadt ME. Occupational therapy evaluation for adults. a pocket guide. Baltimore: Lippincott Williams & Wilkins. 2000.
55. Nuwer MR, Árnadóttir G, Martin AA, et al. A comparison of quantitative electroencephalography, computed tomography, and behavioral evaluations to localize impairment in patients with stroke and transient ischemic attacks. J Neuroimaging. 1994;4(2):82-84.
56. Okkema K. Cognition and perception in the stroke patient. a guide to functional outcomes in occupational therapy. Gaithersburg, MD: Aspen. 1993.
57. Phillips ME, Wolters S. Assessment in practice. common tools and methods. Royeen CB, editor. AOTA self study series: stroke—strategies, treatment, rehabilitation, outcomes, knowledge and evaluation. Bethesda, MD: American Occupational Therapy Association, 1996.
58. Polgar JM. Critiquing assessments. In Crepeau EB, Cohn ES, Boyt Schell BA, editors: Willard & Spackman’s occupational therapy, ed. 9, Philadelphia: Lippincott-Raven, 1998.
59. Robertson I, Ward T, Ridgeway Y, et al. The test of everyday attention (TEA). Bury St Edmunds, England: Thames Valley Test Company; 1994.
60. Rogers JC, Holm MB. The therapists thinking behind functional assessment I. In: Royeen CB, editor. AOTA self study series: assessing function. Rockville, MD: American Occupational Therapy Association, 1989.
61. Royeen CB. A research primer in occupational and physical therapy. Bethesda, MD: American Occupational Therapy Association; 1997.
62. Starkstein SE, Robinson RG. Neuropsychiatric aspects of stroke. In: Coffey CE, Cummings JL, editors. Textbook of geriatric neuropsychiatry. Washington, DC: American Psychiatric Press, 1994.
63. Steultjens EM. A-ONE. De Nederlandse Versie. Ned Tidskrift Ergoterapie. 1998;26:100-104.
64. Steultjens EM, Dekker J, Bouter LM, et al. Occupational therapy for stroke patients. a systematic review. Stroke. 2003:34;3:676-687.
65. Strub RL, Black FW. The mental status examination in neurology, ed 2. Philadelphia: FA Davis; 1985.
66. Sveen U, Bautz-Holter E, Sødring KM, et al. Association between impairments, self-care ability and social activities 1 year after stroke. Disabil Rehabil. 1999;21(8):372-377.
67. Tesio L. Measuring behaviours and perceptions. Rasch analysis as a tool for rehabilitation research. J Rehab Med. 2003:35;3:105-115.
68. Tham K, Bernspång B, Fisher AG. Development of the assessment of awareness of disability. Scand J Occup Ther. 1999;6(4):184-190.
69. Trombly CA, MA HI. A synthesis of effects of occupational therapy for persons with stroke. I. Restoration of roles, tasks and activities. Am J Occup Ther. 2002;56(3):250-259.
70. Trombly Latham CA. Occupation as therapy. Selection, gradation, analysis and adaptation. Radomski MV, Trombly Latham CA, editors. Occupational therapy for physical dysfunction, ed. 6, Philadelphia: Lippincott Williams & Wilkins, 2008.
71. Unsworth C. Reflections on the process of therapy in cognitive and perceptual dysfunction. In: Unsworth C, editor. Cognitive and perceptual dysfunction: a clinical reasoning approach to evaluation and intervention. Philadelphia: FA Davis, 1999.
72. US Department of Health and Human Services. Clinical practice guideline number 16: post-stroke rehabilitation. Rockville, MD: US Department of Health and Human Services; 1995.
73. Whiting S, Lincoln N, Bhavnani G, et al. The Rivermead Perceptual Assessment Battery. Windsor: NFER-NELSON; 1985.
74. Wilson BA, Alderman P, Burgess H, et al. Behavioral assessment of the dysexecutive syndrome (BADS). Bury St Edmunds, England: Thames Valley Test Company; 1996.
75. Wilson BA, Cockburn J, Baddely A. The Rivermead behavioural memory test. Suffolk, England: Thames Valley Test Company; 1989.
76. Wilson BA, Cockburn J, Halligan P. Behavioral inattention test: manual. Suffolk, England: Thames Valley Test Company; 1987.
77. World Health Organization. The international classification of functioning, disability and health—ICF. Geneva, Switzerland: WHO; 2001.
78. Wright BD, Linacre JM. Observations are always ordinal; Measurements, however, must be interval. Arch Phys Med Rehabil. 1989;70(12):857-860.
79. Yatsu FM, Grotta JC, Pettigrew LC, et al. Stroke. 100 maxims. St Louis: Mosby. 1995.
80. Zoltan B. Vision, perception, and cognition. a manual for the evaluation and treatment of the neurologically impaired adult, ed. 3. Thorofare, NJ: Slack. 1996.