Viscera of the Abdomen
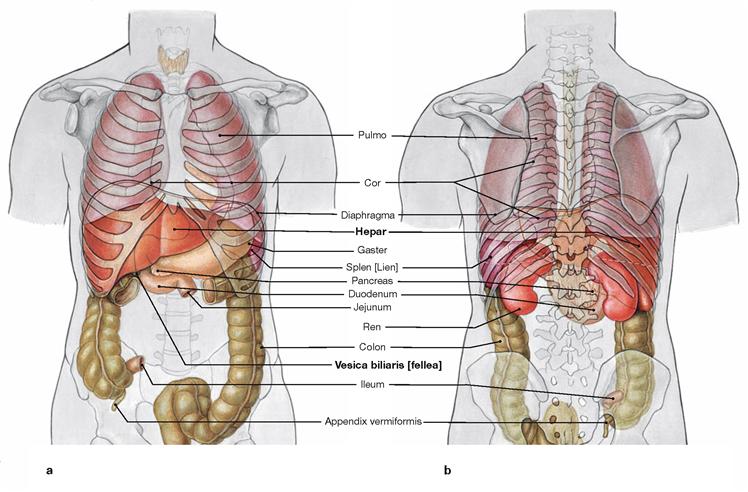
The Abdomen –Concealed Organs
The origin of the terms abdomen and abdominal for the organs that lie in its cavity (Cavitas abdominalis), are derived from the Latin verb “abdo” – “I hide”. In fact, the abdomen does not only hide many organs, but even more causes for diseases.
At a First Glance
Once opened, one looks into an abdominal cavity which is tightly filled with soft and solid organs (Viscera). This is called the situs, “the positioning” of the organs in relation to one another. The inside of the abdominal wall as well as the surfaces of the abdominal organs are covered with soft, moist, and shiny linings, known as the Peritoneum. The wall-covering Peritoneum is the parietal layer; the organ-covering Peritoneum is the visceral layer. The smooth peritoneum enables for example the peristaltic movements of stomach and intestines, allowing intestinal loops to slide against each other.
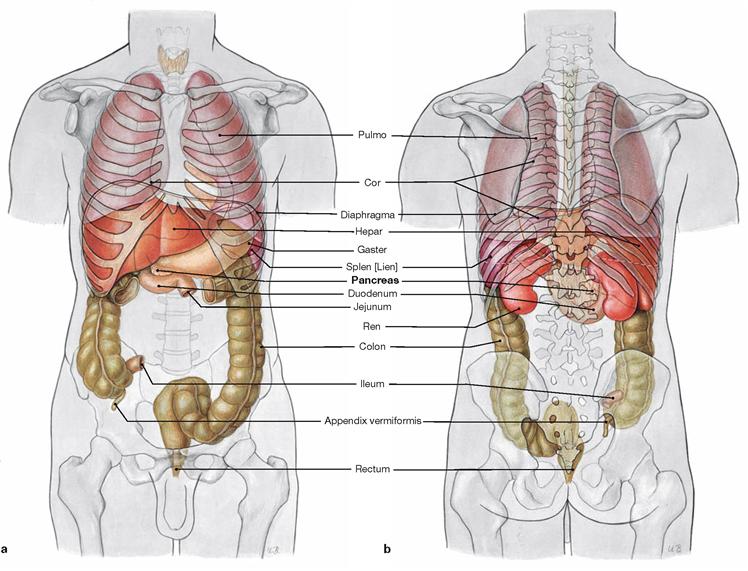
Upper Abdominal Situs
The organs of the upper abdomen lie beneath and between the arches of the rib cage, beneath the dome of the diaphragm, in the Regiones hypochondriacae and the Regio epigastrica. This region contains the liver (Hepar) and the Pancreas, the largest glands in the human body. The liver occupies the entire Regio hypochondriaca dextra and parts of the Regio epigastrica, where its surface clings closely to the diaphragm. At its inferior surface it bears the reservoir for its secretion, the gallbladder (Vesica biliaris). The stomach (Gaster) is just below the ribs of the Regio hypochondriaca sinistra. At the right Regio epigastrica, the stomach transitions into the Duodenum (the first part of the small intestine) at the Pylorus (M. sphincter pyloricus). Between the Duodenum and stomach on one side and the inferior surface of the liver on the other spans a peritoneal duplication, called the Omentum minus. The Pancreas and a greater part of the Duodenum are located dorsal and slightly caudal to the stomach at the dorsal wall of the abdominal cavity. Lateral and posterior to the stomach, in the “outer left corner” of the Regio hypochondriaca sinistra, the spleen (Splen) is located in its “niche”. It is also not visible at first, but easily palpable when one glides the hand over the stomach towards the spleen.
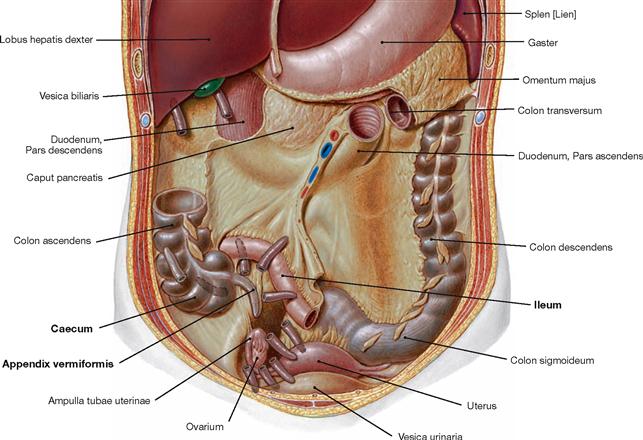
Lower Abdominal Situs
In the remaining larger part of the abdomen, in the Regiones abdominales laterales, inguinales, umbilicalis, and pubica, the intestines (Intestinum) are located – hardly visible at first. Hanging down from the lower margin of the stomach, the Omentum majus resembles an apron containing adipose tissue. Lifting it, one observes the convolution of the intestines. The lower segments of the small intestine (Intestinum tenue), Jejunum and Ileum, are strongly wound and several meters long. If the small intestines are slightly moved back and forth, one notices that they are framed by the Colon (Intestinum crassum) like an inverted “U”: the Colon ascendens on the right hand side, the Colon transversum (where the Omentum majus is attached to in a similar way as to the stomach) marks the border to the Epigastrium, and the Colon descendens on the left hand side. Then, with an elegant swing, the Colon sigmoideum disappears in the lower pelvis where it transitions into the Rectum.
“Mesos” and Peritoneal Relationships
Some of the organs of the Situs viscerum (e.g. Intestinum tenue) are attached to planar, adipose-rich duplications of the Peritoneum (“Mesos”) which project into the lumen of the body cavity. The Mesos carry blood vessels and nerves for the particular Viscera. Depending on the organ associated with the Meso, it is referred to as the Mesocolon (of the Colon transversum), the mesentery (of the small intestine) or the Mesogastrium (of the stomach). The “Mesos” can be pictured as so-called “planar stems” that serve to suspend the respective organs from the abdominal wall. As a result, the entire organs are covered by Peritoneum, except on the “seam-line” to the Meso. They are therefore called intraperitoneal.
Other organs (such as the Colon ascendens, the Colon descendens or the Pancreas) are located at the dorsal wall of the abdomen and fixed in place by connective tissue; hence they have no “stalks”. Therefore these organs are less mobile, they are covered by Peritoneum only on their ventral surfaces facing the abdominal cavity, and are referred to as retroperitoneal. In contrast to the organs of the retroperitoneal situs (see below), these organs shifted to the dorsal body wall during development and are, therefore, called secondary retroperitoneal.
The position of these two groups of organs is not only of academic interest, but essential for all surgical disciplines: in contrast to the organs of the retroperitoneal situs, intraperitoneal organs can only be reached once the abdominal cavity is opened and this increases the risk of infection and complications.
Retroperitoneal Situs
If the space occupied by the gastro-intestinal tract, including its accessory glands, were “cleared”, the organs behind the Peritoneum parietale would become visible on the dorsal wall of the Cavitas abdominalis, which resembles the retroperitoneal space (→ p. 158). The kidneys (Renes) are located ventral to the lowest ribs. The V. cava inferior ascends just to the right side of the vertebral column. It arises at the level of the lowest lumbar vertebra from the confluence of the two Vv. iliacae communes. Nota bene, the V. cava inferior receives no direct venous inflow from the abdominal viscera. Instead their venous blood is collected in the hepatic portal vein, the V. portae hepatis, and flows through the capillary bed of the liver before it enters the V. cava inferior. The Aorta abdominalis descends in the median plane along the vertebral bodies, and divides into the Aa. iliacae communes ventral to the fourth lumbar vertebra. Three large, unpaired arterial trunks, which leave the Aorta ventrally, supply the organs of the upper abdomen (Truncus coeliacus) and the intestines (Aa. mesentericae superior and inferior).
Abdominal Pain
Abdominal pain has several causes which range from innocuous situations to imminent disasters. The abdominal wall can be soft and hardly tender to palpation, but also show board-like rigidity and rebound tenderness. It takes a skilled internist or surgeon to accurately diagnose the causal pathology of an “acute abdomen”, which per se is only a symptom, to provide appropriate therapeutic options. This will only be successful, if one has a clear picture of the composition of the abdomen.
→ Dissection Link
After opening the abdominal cavity, initially the undissected situs with the Bursa omentalis and the Omenta majus and minus should be demonstrated, as dissection significantly changes the relative positions of the structures. Alternatively, only the organs of the lower abdomen or all organs of the peritoneal cavity as a block should be removed to dissect the retroperitoneum and pelvic situs. Prior to resection, the three unpaired blood vessels of the abdominal aorta (Truncus coeliacus, Aa. mesentericae superior and inferior) must first be identified and cut, if needed. After transection and ligation of the Oesophagus or Duodenum proximally, and of the terminal ileum and the Rectum distally, the intraperitoneal and secondary retroperitoneal organs are mobilised bluntly. In addition, the liver should be separated from the V. cava inferior. Afterwards, neurovascular structures of the organs remaining in situ and the removed organs must be traced. At stomach, spleen, and intestines, primarily the blood vessels are to be dissected and displayed. The extrahepatic bile ducts are dissected in the region of the hilum of the liver and the gallbladder.
Development
Development of the upper abdominal situs
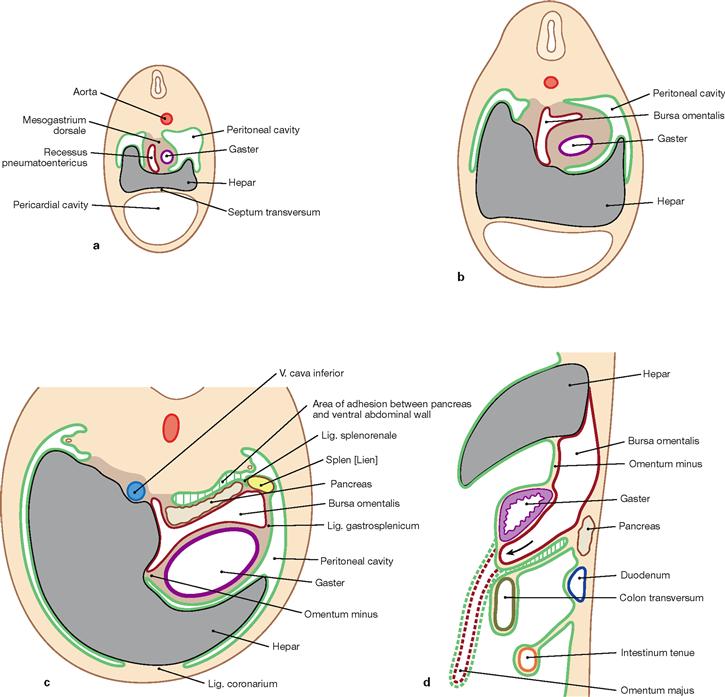
Figs. 6.1a to d Development of the upper abdominal situs at the end of week 4 (a), at the beginning of week 5 (b), and at the beginning of week 7 (c); transverse sections (a to c) and paramedian section (d) of the upper abdomen. Peritoneum (green); Peritoneum of the Recessus pneumatoentericus and the Bursa omentalis (dark red), respectively. (according to [1])
The primordial gut predominantly derives from the endoderm and parts of the yolk sac. In the surrounding mesoderm, developing gaps fuse to form the body cavity. The mesoderm covering the primordial gut later forms the Peritoneum viscerale and, as Peritoneum parietale, lines the abdominal cavity. The Peritoneum viscerale also forms the mesenteries which contain the supplying neurovascular structures and serve as attachments. The dorsal mesentery connects the primordial gut with the dorsal wall of the trunk. The upper abdomen also contains a ventral mesentery.
At the beginning of week 4, an endodermal outgrowth develops ventral to the primordial gut at the level of the later Duodenum and gives rise to the epithelial tissues of liver, gallbladder, bile ducts and Pancreas. Subsequently, the following restructuring occurs:
1. The liver expands into the Mesogastrium ventrale and, thus, creates a division into the Mesohepaticum ventrale (between ventral wall of the trunk and liver) and the Mesohepaticum dorsale (between liver and stomach) (a and b). The Mesohepaticum ventrale later forms the Lig. coronarium cranially and the Lig. falciforme hepatis caudally. The Lig. teres hepatis at the caudal margin is a remnant of the umbilical vein. The Mesohepaticum dorsale becomes the Omentum minus.
2. In the Mesogastrium dorsale a gap appears at the right side (Recessus pneumatoentericus) which later forms the Bursa omentalis (a and b).
3. The stomach rotates 90° in a clockwise direction (cranial view) and thus is located in a frontal position at the left side of the body (c). The Omentum minus connects the liver and lesser curvature of the stomach also in a frontal plane and forms the ventral border of the Bursa omentalis which has reached a position on the left side behind the stomach.
4. In the Mesogastrium dorsale, the Pancreas and the spleen develop. The Pancreas subsequently acquires a retroperitoneal position, and the spleen remains intraperitoneal.
5. The Mesogastrium dorsale eventually separates into the Lig. gastrosplenicum (from the greater curvature of the stomach to the spleen) and the Lig. splenorenale (from the splenic hilum to the dorsal abdominal wall) and forms the other portions of the Omentum majus (apron-like at the greater curvature of the stomach; d). Therefore, due to its development and the neurovascular supply, the Omentum majus is associated with the upper abdominal situs.
Development of the lower abdominal situs
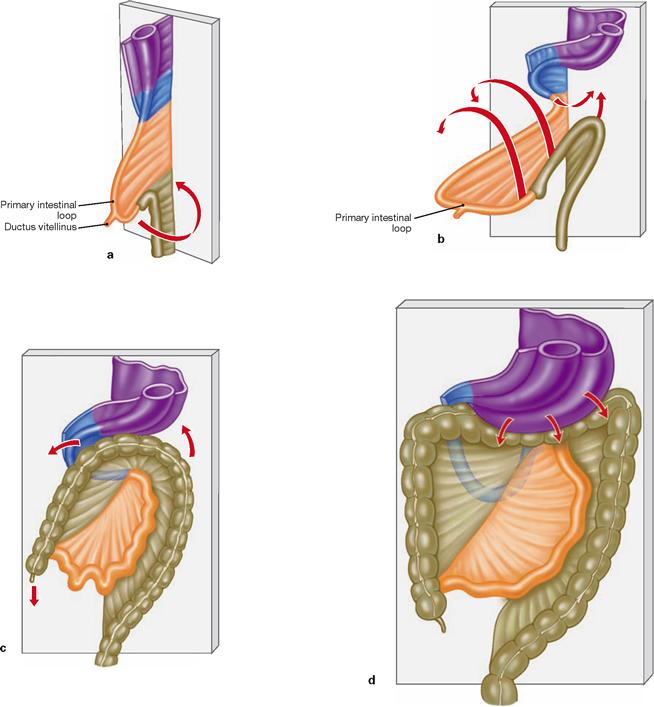
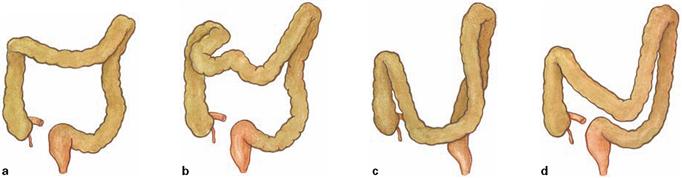
Figs. 6.2a to d Schematic illustrations of the intestinal rotation.
Intestinal segments and their mesenteries are highlighted in different colours: Gaster and Mesogastrium (purple), Duodenum and Mesoduodenum (blue), Jejunum and Ileum with associated mesenteries (orange), Colon and Mesocolon (ochre). (according to [1])
1. Caused by the longitudinal growth of the primordial gut, a ventrally oriented loop forms (primary intestinal loop). The proximal (upper) limb of this loop develops into the major part of the small intestine, the distal (lower) limb develops into the colon including the Colon transversum. The distal large intestine develops from the hindgut and, thus, differs in its neurovascular supply.
2. Due to a lack of space, the primary intestinal loop is temporarily located outside of the embryo in the umbilical cord (physiological umbilical hernia) and remains connected to the yolk sac via the Ductus vitellinus. If the intestines fail to relocate entirely into the embryo, a congenital umbilical hernia (omphalocele) remains which contains portions of the intestinal segments and their mesenteries. Because this congenital hernia traverses through the later umbilical ring, it is covered by amnion only but not by muscles of the abdominal wall.
3. Remnants of the Ductus vitellinus may remain as MECKEL’s diverticulum located at the small intestine.
4. The elongation of the intestines initiates a 270° counter-clockwise rotation, resulting in the colon to surround the small intestine like a frame.
5. Colon ascendens and Colon descendens are secondarily relocated in a retroperitoneal position.
Stomach
Projection of the stomach
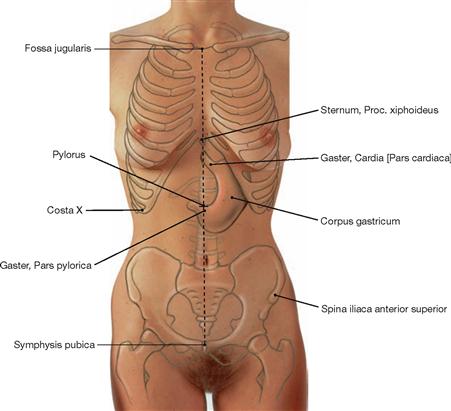
Fig. 6.3 Projection of the stomach, Gaster, onto the ventral wall of the trunk.
The cardiac orifice (Cardia) projects onto the level of the 10th thoracic vertebra, thus, ventrally below the Proc. xiphoideus of the sternum. The position of the caudal part of the stomach is relatively variable at the level of the 2nd to 3rd lumbar vertebra. The Pylorus, on the other hand, regularly locates halfway along a virtual line connecting the pubic symphysis (Symphysis pubica) and the jugular fossa (Fossa jugularis), projecting onto the 1st lumbar vertebra.
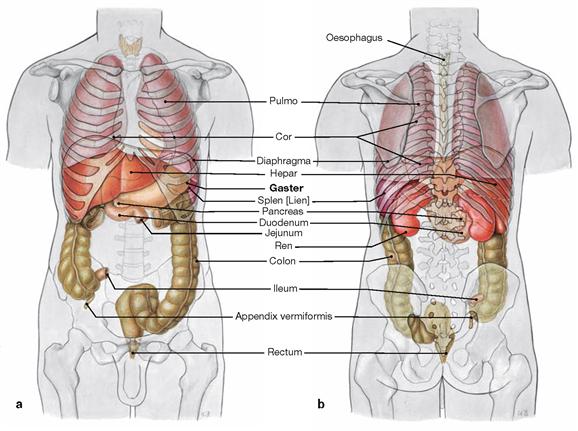
Figs. 6.4a and b Projection of the internal organs onto the body surface; ventral (a) and dorsal (b) views.
The stomach is positioned intraperitoneally in the left Epigastrium between the left lobe of the liver and the spleen. The stomach is mostly covered by the left costal arch but a small area is directly adjacent to the ventral abdominal wall. This area is clinically relevant since PEG-tubes (percutaneous endoscopic gastrostomy) can be placed here for parenteral nutrition.
Divisions of the stomach
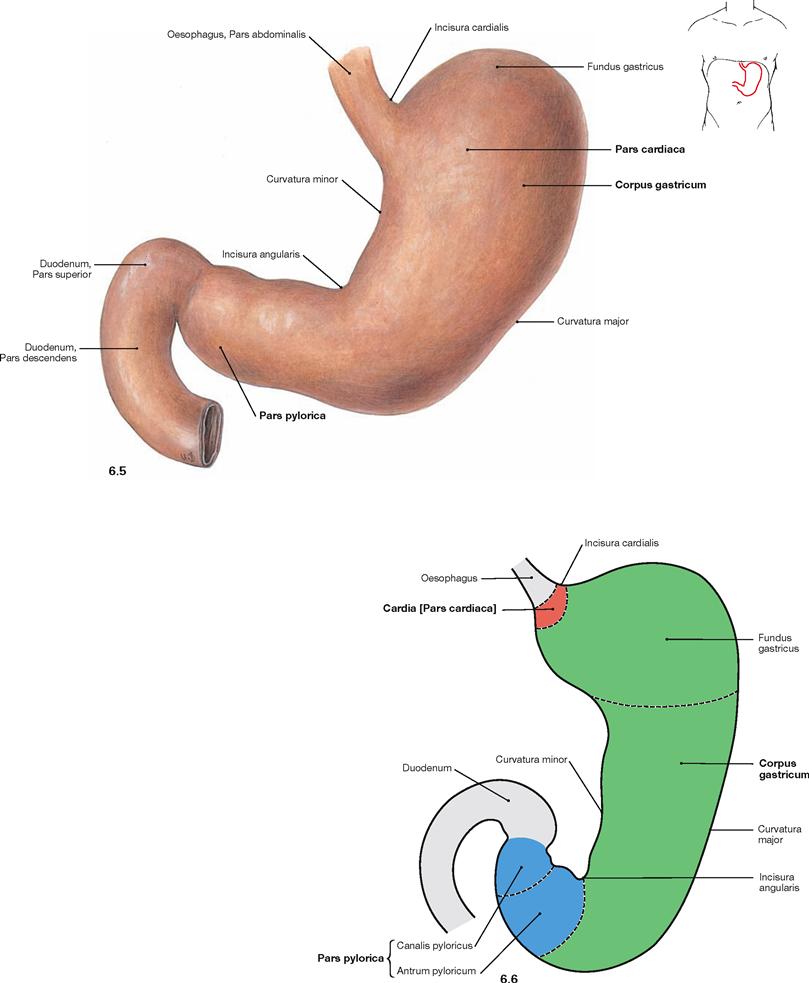
Fig. 6.5 and Fig. 6.6 Stomach, Gaster; ventral view (→ Fig. 6.5) and schematic illustration (→ Fig. 6.6). (Fig. 6.6 according to [1])
The stomach has three parts:
• Pars cardiaca: entrance to the stomach
• Corpus gastricum: main part with superior Fundus gastricus
• Pars pylorica: exit of the stomach which continues as Antrum pyloricum and Canalis pyloricus, the latter being surrounded by the sphincter muscle (M. sphincter pyloricus).
The stomach has an anterior and posterior wall (Paries anterior and posterior). The lesser curvature (Curvatura minor) is directed to the right side, the greater curvature (Curvatura major) to the left side. The kink in the lesser curvature (Incisura angularis) marks the beginning of the Pars pylorica. The greater curvature also begins with an indentation (Incisura cardialis) which marks the angle of HIS between the Oesophagus and the stomach (cardiac notch). At the inside of the stomach, this transition between both organs is marked by a mucosal fold which, together with the angiomuscular gastro-oesophageal valve, contributes to the closure of the stomach.
Muscles of the stomach
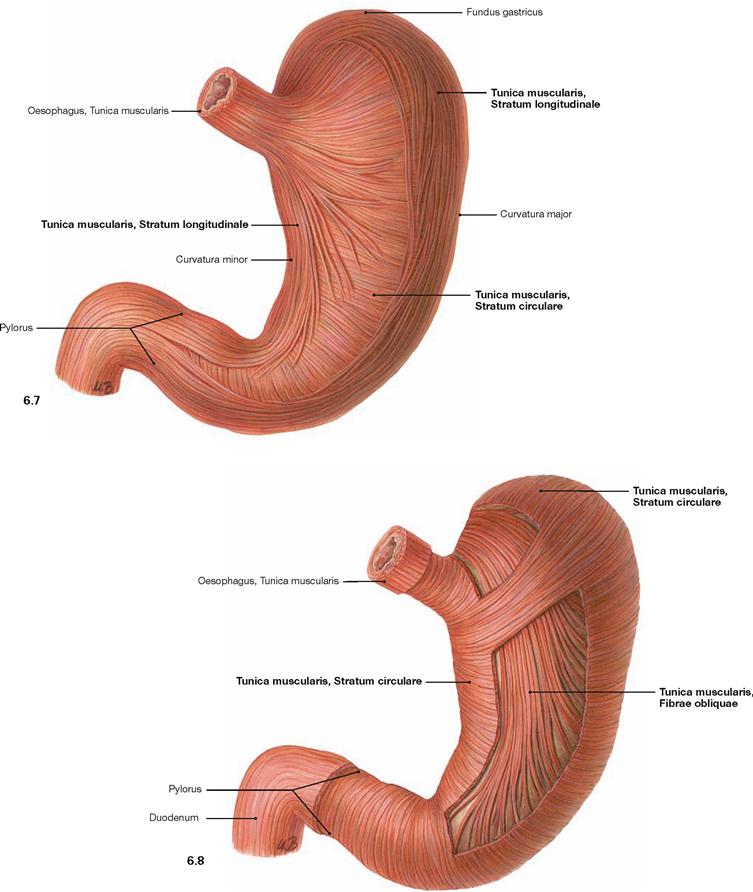
Fig. 6.7 and Fig. 6.8 Outer (→ Fig. 6.7) and inner (→ Fig. 6.8) muscular layers of the stomach, Gaster; ventral view.
The wall of the stomach comprises three muscular layers (Tunica muscularis) not consistently found in all regions of the stomach. The external longitudinal layer (Stratum longitudinale) is adjacent to the circular layer (Stratum circulare). The innermost layer consists of the oblique muscle fibres (Fibrae obliquae) which are missing at the lesser curvature.
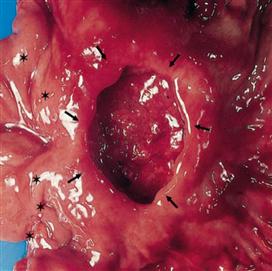
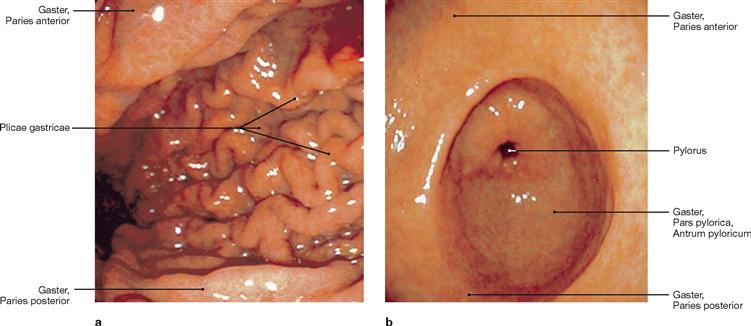
Inner relief of the stomach
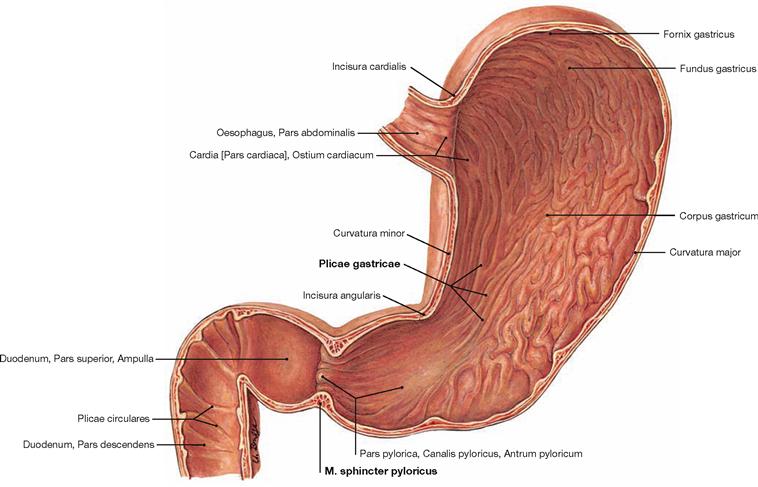
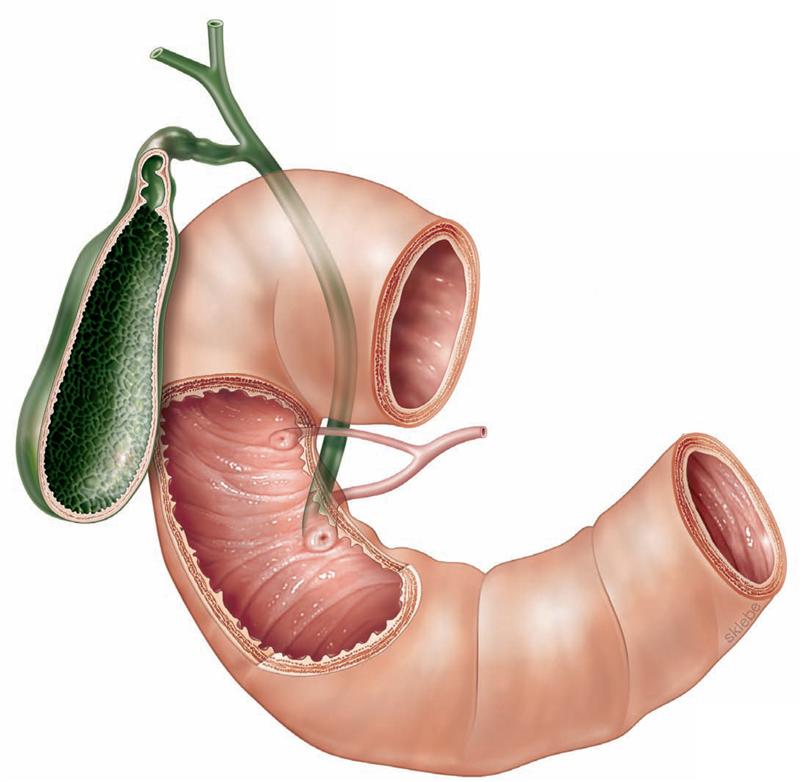
Fig. 6.9 Stomach, Gaster, and duodenum, Duodenum; ventral view.
The gastric mucosa has a characteristic relief serving the enlargement of the inner surface. The macroscopically recognisable gastric folds (Plicae gastricae) are longitudinally oriented and form the functional canal along the lesser curvature (gastric canal). The mucosal folds reveal small microscopic areas (Areae gastricae; → Fig. 6.10). At the exit of the stomach (Pylorus), the circular muscle layer is thickened to form the pyloric sphincter muscle (M. sphincter pyloricus).
Structure of the wall of the stomach
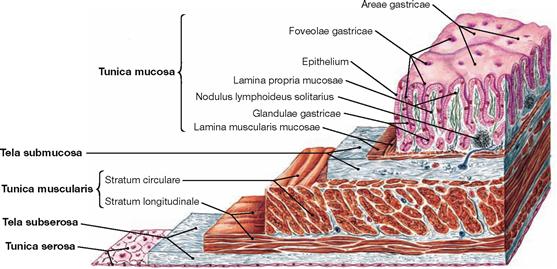
Fig. 6.10 Wall of the stomach, Gaster; microscopic view.
Similar to the whole intestines, the wall of the stomach comprises an inner mucosal layer (Tunica mucosa) which is separated from the muscular layer (Tunica muscularis, → Figs. 6.7 and 6.8) by a layer of loose connective tissue (Tela submucosa). As an intraperitoneal organ the outer surface of the stomach is covered by visceral peritoneum (Peritoneum viscerale) which forms the Tunica serosa.
Topographical relations of the stomach
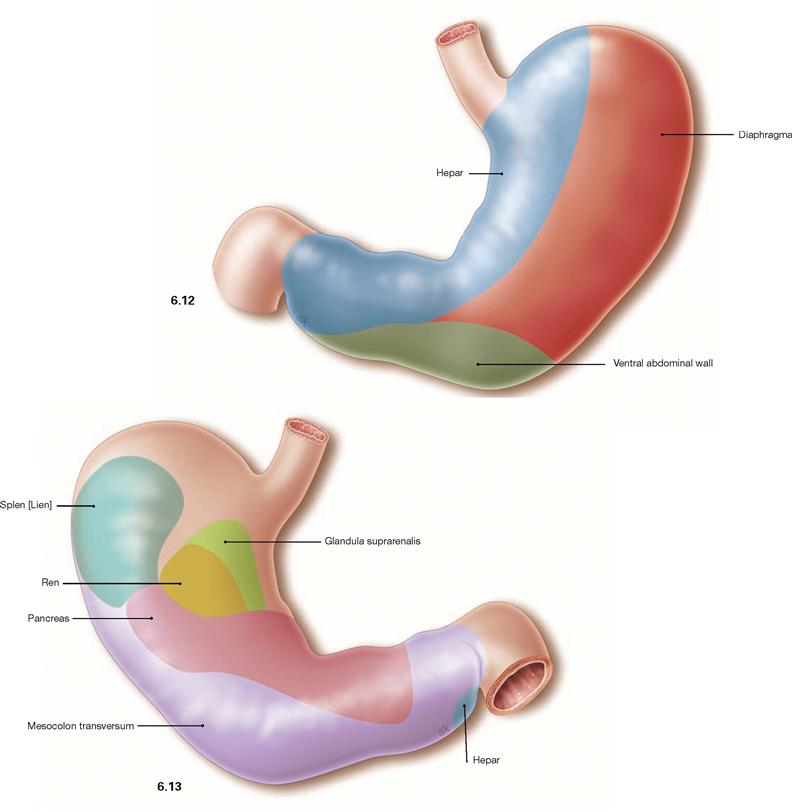
Fig. 6.12 and Fig. 6.13 Contact areas, Facies, of the anterior wall (→ Fig. 6.12) and the posterior wall (→ Fig. 6.13) of the stomach with adjacent organs:
• ventral: liver, diaphragm, abdominal wall
• dorsal: spleen, kidney, adrenal gland, Pancreas, Mesocolon transversum
The stomach is mobile and, depending on the filling state, has different contact areas with its adjacent organs.
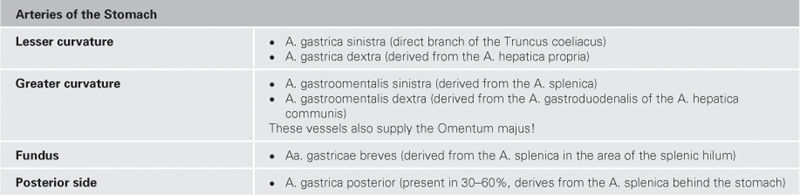
Arteries of the stomach
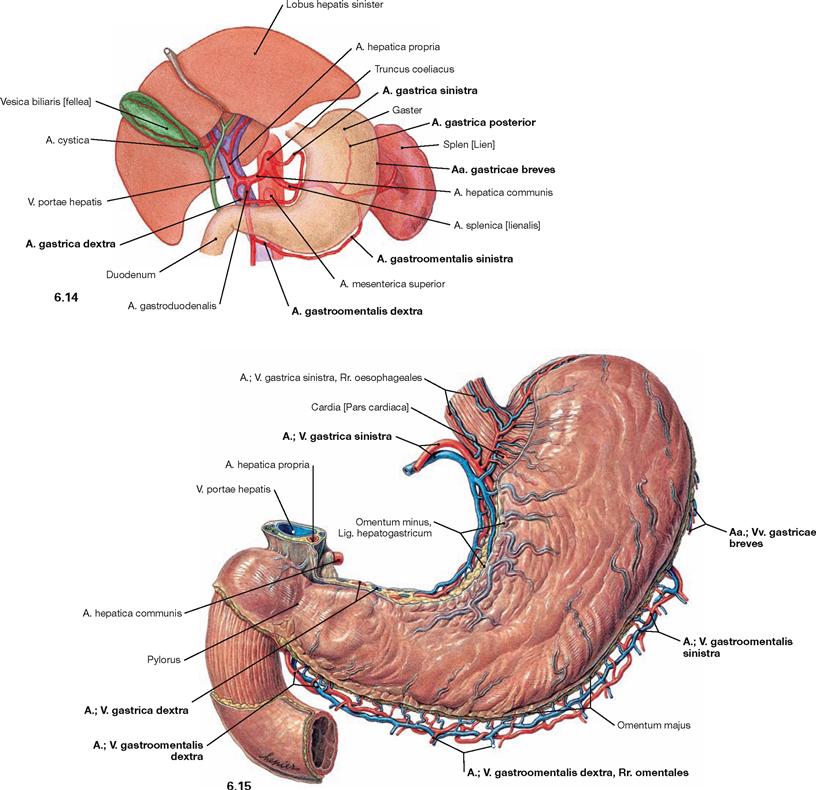
Fig. 6.14 and Fig. 6.15 Arteries of the stomach, Gaster, as schematic illustration (→ Fig. 6.14) and their course along the curvatures of the stomach (→ Fig. 6.15); ventral view.
The three main branches of the Truncus coeliacus (A. gastrica sinistra, A. hepatica communis, A. splenica) collectively give rise to six gastric arteries (→ Table).
Veins of the stomach
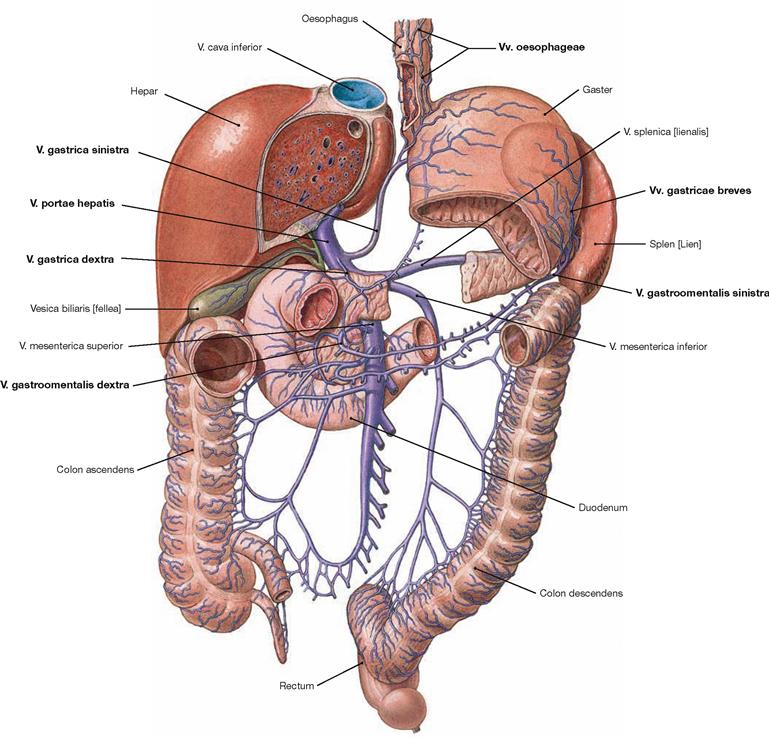
Fig. 6.16 Veins of the stomach, Gaster, in relation to the portal vein, V. portae hepatis; ventral view.
The veins are corresponding to the arteries, but the veins at the lesser curvature directly enter the portal vein, whereas the veins at the greater curvature drain into the larger branches of the portal vein.
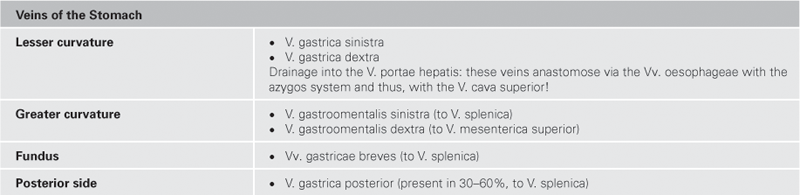
Lymph vessels of the stomach
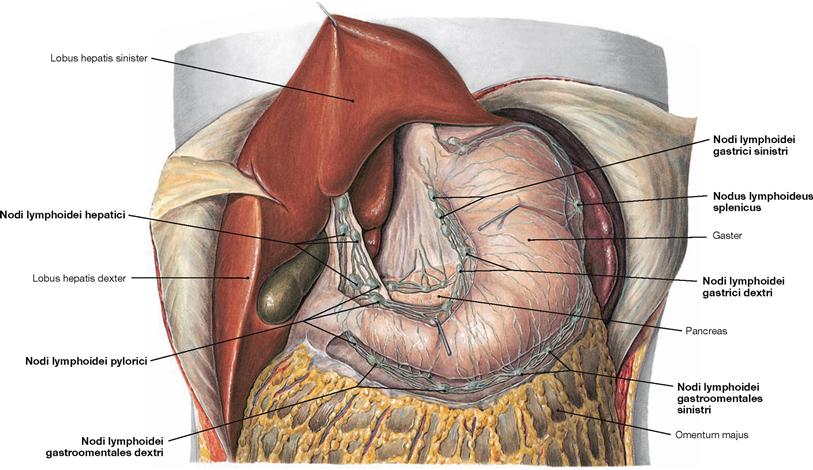
Fig. 6.17 Lymph vessels and lymph nodes of the stomach, Gaster, and the liver, Hepar; ventral view.
The lymph vessels and lymph nodes of the stomach are located alongside both curvatures and around the Pylorus: the lesser curvature shows the Nodi lymphoidei gastrici, the greater curvature harbours the Nodi lymphoidei splenici and caudal thereof the Nodi lymphoidei gastroomentales. The Nodi lymphoidei pylorici in the region of the Pylorus connect to the Nodi lymphoidei hepatici at the hilum of the liver. Three major lymphatic drainage pathways with three subsequent lymph node stations are distinguished (→ Fig. 6.18).
Lymph vessels of the stomach
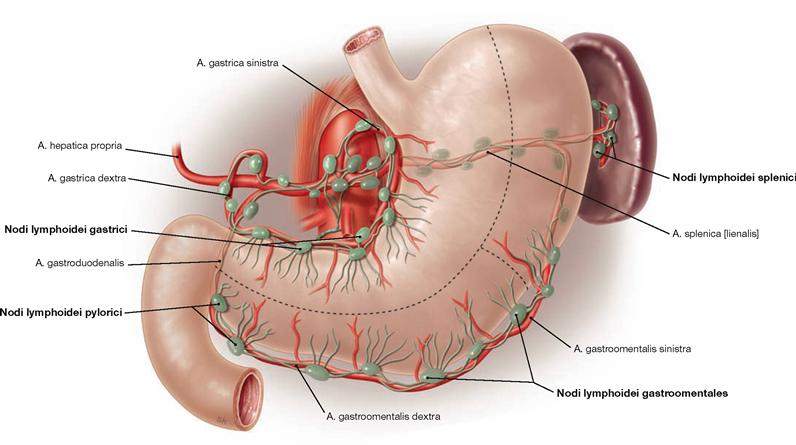
Fig. 6.18 Lymphatic drainage and regional lymph nodes of the stomach, Gaster; ventral view. (according to [1])
The three principle lymphatic drainage pathways which exist for the stomach are marked by dashed lines in this illustration:
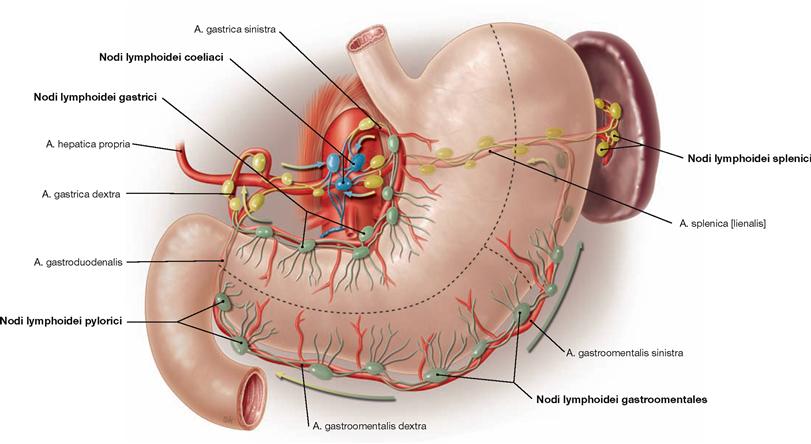
Fig. 6.19 Lymphatic drainage stations of the stomach; ventral view. (according to [1])
Within the three principle lymphatic drainage pathways there are three subsequent stations:
• first station (green): lymph nodes along the curvatures (→ Fig. 6.18)
• second station (yellow): lymph nodes along the branches of the Truncus coeliacus
• third station (blue): lymph nodes at the origin of the Truncus coeliacus [Nodi lymphoidei coeliaci]; from here the lymph is drained via the Truncus intestinalis into the Ductus thoracicus.
Autonomic innervation of the stomach
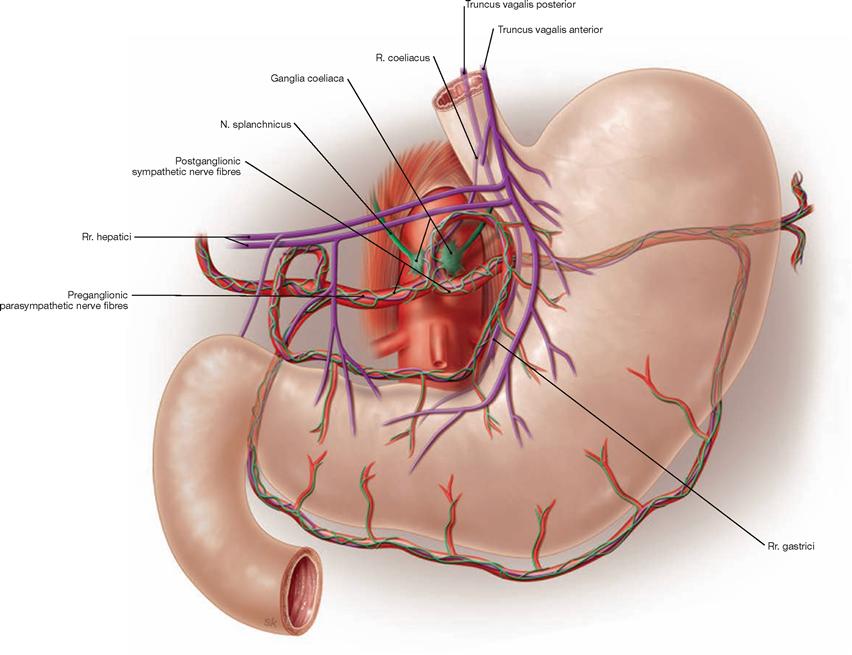
Fig. 6.20 Autonomic innervation of the stomach, Gaster; semischematic illustration. Sympathetic innervation (green), parasympathetic innervation (purple). (according to [1])
Preganglionic parasympathetic fibres (Rr. gastrici) reach the stomach as Trunci vagales anterior and posterior descending along the Oesophagus and course along the lesser curvature. As a result of the gastric rotation during development, the anterior Truncus vagalis is predominantly derived from the left, the posterior Truncus vagalis from the right N. vagus [X]. The Pars pylorica is innervated by separate branches (Rr. hepatici) of the Trunci vagales. The postganglionic neurons are located within the muscular layers of the stomach. The parasympathetic innervation stimulates the production of gastric acids and promotes the gastric peristalsis.
Preganglionic sympathetic fibres traverse the diaphragm on both sides as Nn. splanchnici major and minor and are synapsed to the postganglionic sympathetic neurons in the Ganglia coeliaca located at the origin of the Truncus coeliacus. These postganglionic sympathetic fibres reach the stomach as peri-arterial nerve plexus. The sympathetic innervation counterbalances the parasympathetic influence by reducing gastric acid production, peristalsis, and perfusion.
Stomach, gastroscopy
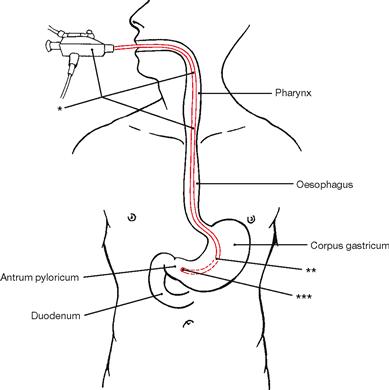
Fig. 6.21 Technique for oesophagoscopy and gastroscopy.
** gastroscope, tip in the Corpus gastricum (→ Fig. 6.22a)
*** gastroscope, tip in the Antrum pyloricum (→ Fig. 6.22b)
Projection of the small intestine
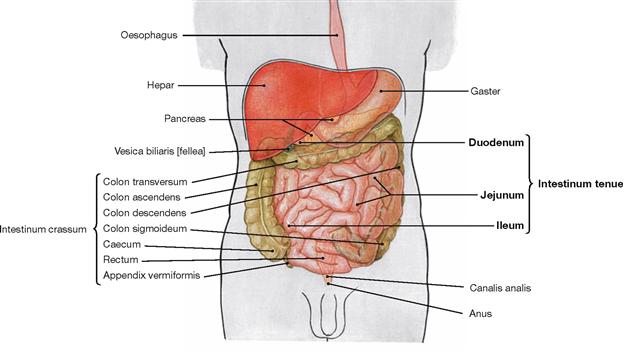
Fig. 6.23 Projection of the abdominal viscera onto the body surface; ventral view.
The small intestine (4–6 m) has three parts:
The Duodenum starts at the Pylorus of the stomach and ends at the Flexura duodenojejunalis. Except for its first part (Pars superior), the Duodenum is fixed in its retroperitoneal position and well separated from the other parts of the small intestine. In contrast, the intraperitoneal convoluted parts of the Jejunum and Ileum are not separable macroscopically and reach distally to the Valva iliocaecalis (BAUHIN’s valve) at the transition to the large intestine.
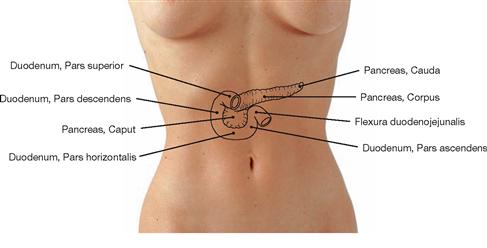
Fig. 6.24 Projection of the duodenum, Duodenum, and pancreas, Pancreas, onto the ventral abdominal wall.
The intraperitoneal Pars superior of the Duodenum projects onto the level of the 1st lumbar vertebra. All other parts are located secondary retroperitoneally and encompass the head of the Pancreas in a C-shaped manner. The head of the Pancreas is adjacent to the Pars descendens of the Duodenum. The Pars horizontalis lies at the level of the 3rd lumbar vertebra and continues as Pars ascendens to the Flexura duodenojejunalis at the level of the 2nd lumbar vertebra. This flexure marks the transition to the intraperitoneal Jejunum.
Structure of the wall of the small intestine
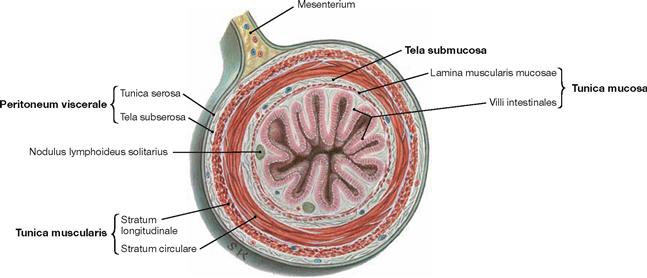
Fig. 6.25 Small intestine, Intestinum tenue; cross-section.
The layers are described in → Figure 6.26.
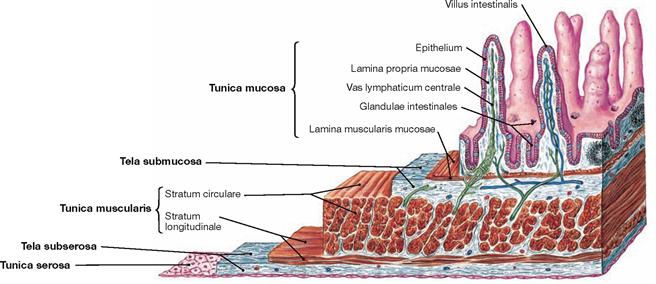
Fig. 6.26 Wall structure of the small intestine, Intestinum tenue; microscopic view.
Similar to other parts of the intestines, the wall of the small intestine consists of the innermost mucosal layer (Tunica mucosa) with intestinal villi (Villi intestinales) for surface enlargement. Separated by a loose connective tissue layer (Tela submucosa), the muscular layer (Tunica muscularis) consists of the inner circular layer (Stratum circulare) and the outer longitudinal layer (Stratum longitudinale). The intraperitoneal parts (Pars superior of the Duodenum, Jejunum and Ileum) are covered on their outer surface with peritoneum (Peritoneum viscerale) which forms the Tunica serosa. Retroperitoneal parts of the Duodenum are anchored by a Tunica adventitia within the connective tissue of the retroperitoneal space.
Intestines
Divisions of the duodenum
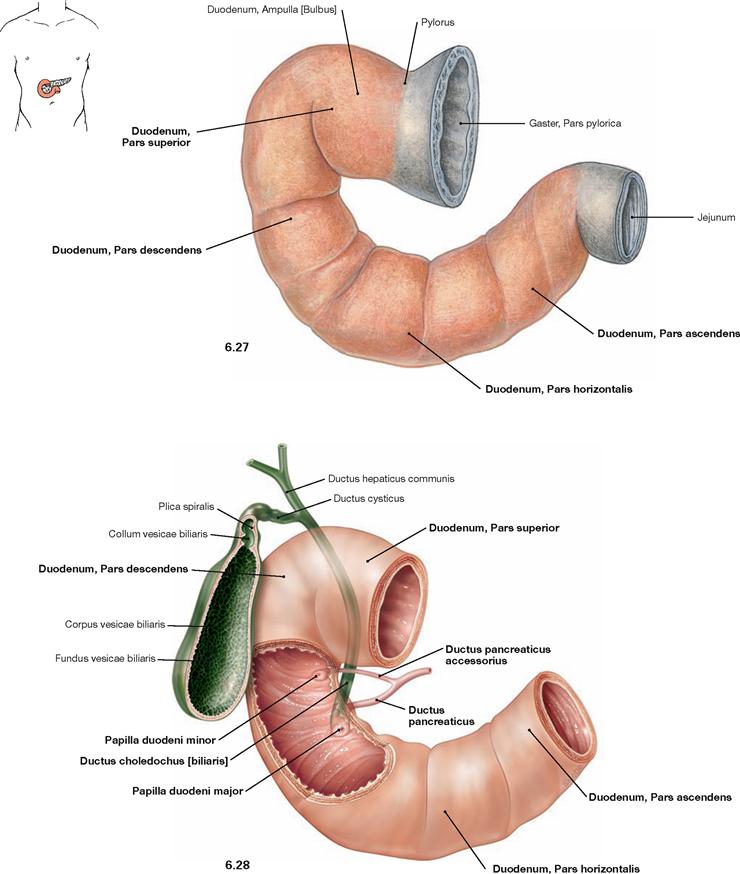
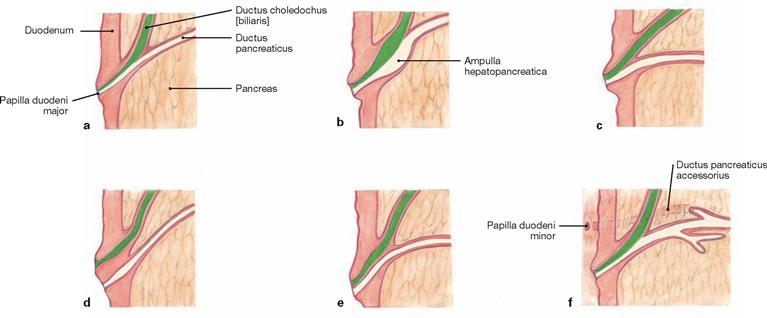
Fig. 6.27 and Fig. 6.28 Divisions of the duodenum, Duodenum, isolated (→ Fig. 6.27) and together with the extrahepatic bile ducts (→ Fig. 6.28); ventral view.
The Duodenum has four parts:
The Pars superior is the only intraperitoneal part and its wider proximal lumen is referred to as Ampulla (Bulbus) duodeni.
The excretory duct of the Pancreas (Ductus pancreaticus, duct of WIRSUNG) enters the Pars descendens of the Duodenum frequently together with the common bile duct (Ductus choledochus) on a mucosal papilla (Papilla duodeni major, ampulla of VATER) which is found 8–10 cm distal to the Pylorus. Often, 2 cm proximal to the latter, a smaller Papilla duodeni minor is found into which the Ductus pancreaticus accessorius (SANTORINI’s duct) empties its secretion.
The Pars horizontalis crosses the vertebral column and continues as Pars ascendens.
Structure of the duodenum
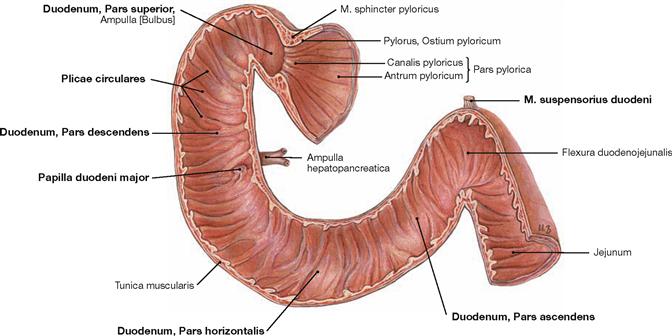
Fig. 6.29 Inner relief of the duodenum, Duodenum; frontal section; ventral view.
The Duodenum has the following four parts: 1. Pars superior, 2. Pars descendens, 3. Pars horizontalis, and 4. Pars ascendens. To increase the absorptive surface, the inner relief of the Duodenum shows circular mucosal folds (Plicae circulares, KERCKRING’s folds) similar to other parts of the small intestine. The Pars descendens contains the Papilla duodeni major (ampulla of VATER) at the entrance of the Ductus pancreaticus (duct of WIRSUNG) and the common bile duct (Ductus choledochus), both of which usually merge to form the Ampulla hepatopancreatica. The Pars ascendens is attached to the aorta near the origin of the A. mesenterica superior by smooth muscle fibres (M. suspensorius duodeni, muscle of TREITZ) and dense connective tissue (Lig. suspensorium duodeni), just before the Duodenum transitions into the intraperitoneal Jejunum at the Flexura duodenojejunalis.
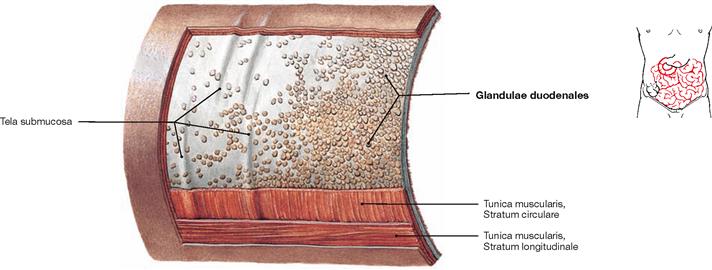
Fig. 6.30 Wall structure of the duodenum, Duodenum, with Glandulae duodenales; view from outside.
The mucous-producing Glandulae duodenales (BRUNNER‘s glands) are located in the Tela submucosa and allow the identification of the Duodenum in histological sections.
Duodenum, imaging
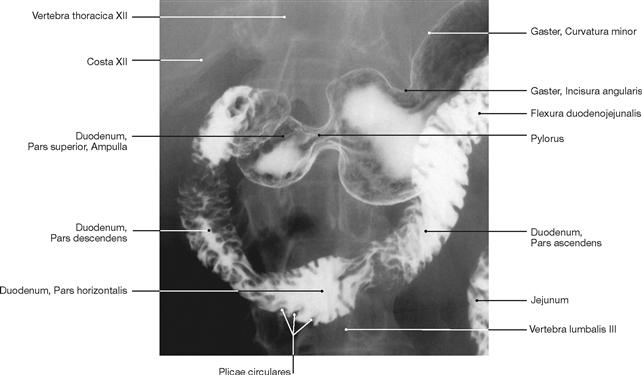
Fig. 6.31 Duodenum, Duodenum; radiograph in anteroposterior (AP) beam projection after oral application of a contrast material; patient in upright position; ventral view.

Fig. 6.32 Duodenum, Duodenum; endoscopic image.
The circular mucosal folds (Plicae circulares, KERCKRING’s folds) are clearly visible.
Structure of the wall of jejunum and ileum
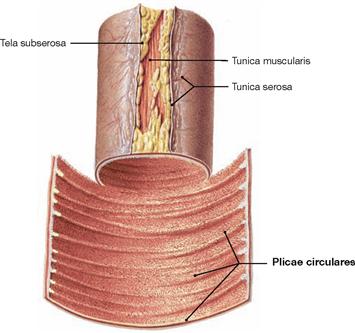
Fig. 6.33 Detail of the jejunum, Jejunum.
The structure of the Jejunum is very similar to the Duodenum but does not contain the Glandulae duodenales (BRUNNER’s glands).
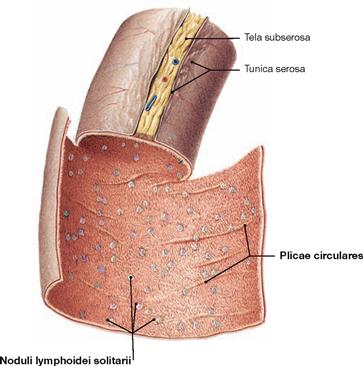
Fig. 6.34 Detail of the proximal ileum, Ileum.
The Plicae circulares (KERCKRING’s folds) are much less frequent in the Ileum when compared to the upper small intestine.
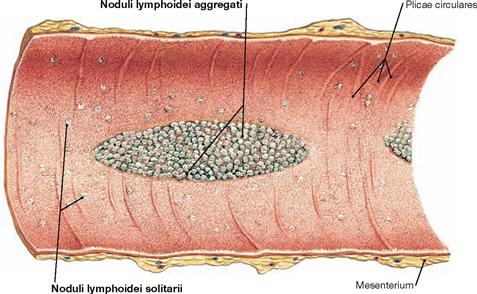
Fig. 6.35 Detail of the distal ileum, Ileum.
The large assemblies of lymph follicles are characteristic for the terminal Ileum. They are a part of the mucosa-associated lymphoid tissue (MALT). The lymph nodes are either located individually (Nodi lymphoidei solitarii; → Fig. 6.34) in the Tela submucosa or are assembled in groups (Noduli lymphoidei aggregati; PEYER’s plaques) underneath the elevated mucosa.
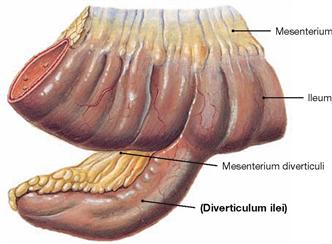
Fig. 6.36 MECKEL’s diverticulum, Diverticulum ilei.
Up to 3% of people have been diagnosed with a diverticulum, which exists as a remnant of the embryological Ductus vitellinus (→ Fig. 6.2). It is usually located in the Ileum about 100 cm proximal to the ileocaecal valve at the opposite side of the mesentery.
MECKEL’s diverticula may contain disseminated gastric mucosa and, when inflamed or bleeding, can mimic the symptoms of an appendicitis.
Projection of the large intestine
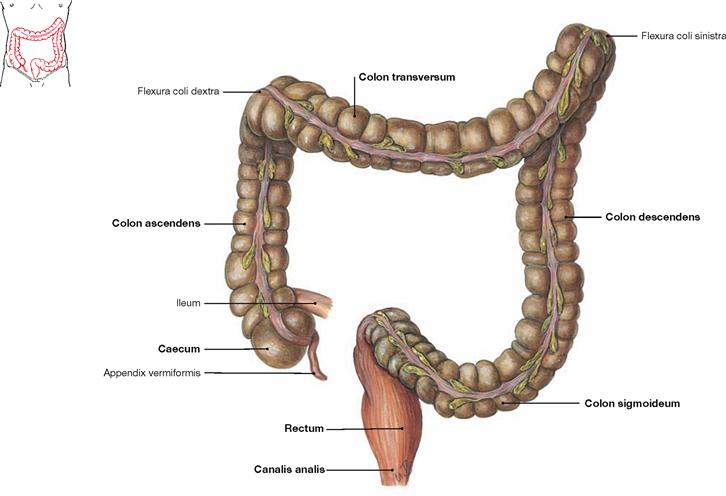
Fig. 6.37 Divisions of the large intestine, Intestinum crassum; ventral view.
The large intestine is about 1.5 m long and consists of four parts:
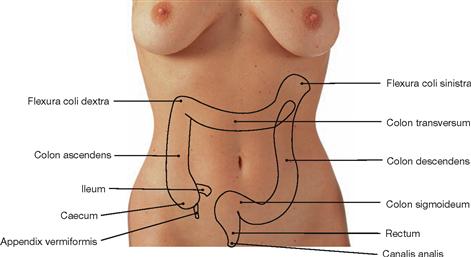
Fig. 6.38 Projection of the large intestine, Intestinum crassum, onto the ventral abdominal wall.
Caecum with Appendix vermiformis, Colon transversum, and Colon sigmoideum are positioned intraperitoneally and have individual mesenteries. Caecum and Appendix vermiformis may also be located retroritoneally (Caecum fixum); in this case they do not have a mesentery. Colon ascendens, Colon descendens, and the major part of the Rectum are usually secondarily retroperitoneal organs, the distal Rectum and the anal canal are subperitoneal. The projections and the length of the individual segments of the large intestine are highly variable and the retroperitoneal segments are usually inconsistently fused with the posterior abdominal wall. Due to the position of the liver on the right side, the left colic flexure (Flexura coli sinistra) is positioned farther cranial than the right colic flexure (Flexura coli dextra; → Fig. 6.53).
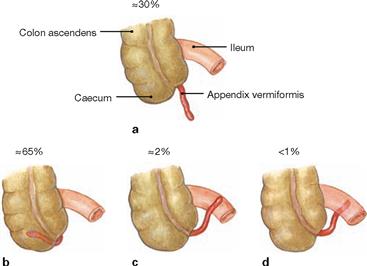
Projection and positional variations of the Appendix vermiformis
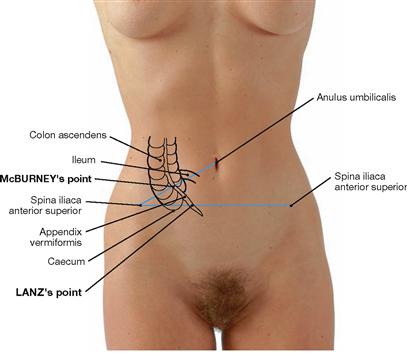
Fig. 6.39 Projection of the caecum, Caecum, and Appendix vermiformis onto the ventral abdominal wall.
The base of the Appendix vermiformis projects onto the McBURNEY’s point (the transition between the lateral third and the medial two-thirds on a line connecting the umbilicus with the Spina iliaca anterior superior). The location of the tip of the appendix is more variable and projects onto the LANZ’s point (the transition between the right third and the left two-thirds on a line connecting both Spinae iliacae anteriores superiores; 30%; → Figs. 6.40 and 6.41).
Structure of the large intestine
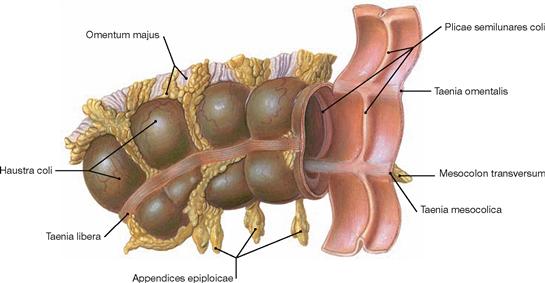
Fig. 6.42 Structural characteristics of the large intestine, Intestinum crassum, the transverse colon taken as an example; ventral caudal view.
The large intestine has four characteristic differences to the small intestine:
• larger diameter (“thick” rather than “thin”)
• Taenia: the longitudinal muscle layer is reduced to three bands. Of these, the Taenia libera is visible, whereas the Taenia mesocolica attaches to the Mesocolon transversum and the Taenia omentalis connects to the greater omentum (Omentum majus).
• Haustra and Plicae semilunares: the haustra (Haustra coli) are sacculations of the intestinal wall which correspond to crescent-shaped mucosal folds (Plicae semilunares) at the inner surface.
• Appendices epiploicae: fatty projections from the adipose tissue of the Tela subserosa.
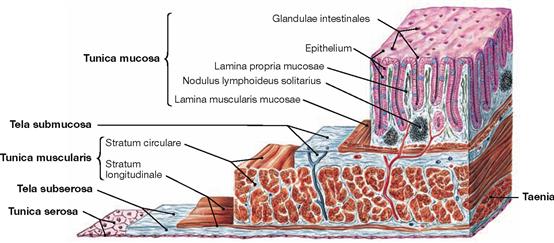
Fig. 6.43 Structure of the wall of the large intestine, Intestinum crassum; microscopic view.
Similar to the other parts of the intestines, the wall of the large intestine consists of an inner mucosal layer (Tunica mucosa) which, in contrast to the Duodenum, has no mucosal villi. Separated from the Tunica mucosa by a connective tissue layer (Tela submucosa) is the muscular layer (Tunica muscularis). It consists of an inner circular layer (Stratum circulare) and an outer longitudinal layer (Stratum longitudinale). However, the longitudinal layer is not continuous but is reduced to three bands (Taenia). At the outside, the intraperitoneal parts (Caecum with Appendix vermiformis, Colon transversum, and Colon sigmoideum) are covered by peritoneum (Peritoneum viscerale) forming the Tunica serosa. In contrast, the retroperitoneal parts (Colon ascendens, Colon descendens, and upper rectum) are anchored by the Tunica adventitia in the connective tissue of the retroperitoneal space.
Caecum and Appendix vermiformis
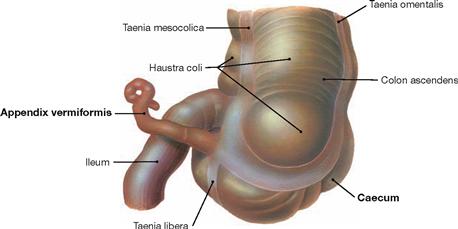
Fig. 6.44 Caecum with Appendix vermiformis, and terminal ileum, Pars terminalis ilei; dorsal view.
The Caecum is approximately 7 cm long. The 8–9 cm long Appendix vermiformis is attached to the Caecum and has its own mesentery (not shown here) with supplying neurovascular structures. The taenia of the Colon converge at the appendix to form a continuous longitudinal muscular layer.
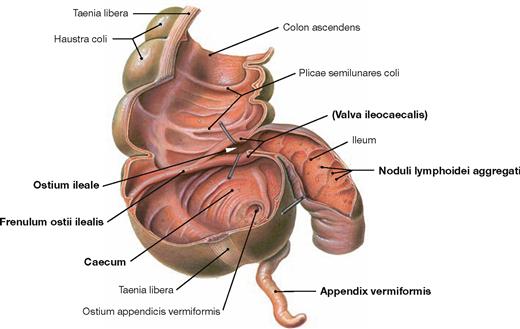
Fig. 6.45 Caecum with Appendix vermiformis, and terminal ileum, Pars terminalis ilei; ventral view; after removal of the anterior parts of the wall.
The Caecum is separated from the terminal ileum by the ileocaecal valve (Valva ileocaecalis, BAUHIN’s valve). Internally, the two lips of the valve form the Papilla ilealis and border the ileal orifice (Ostium ileale). Laterally, the lips continue in the Frenulum ostii ilealis. The terminal ileum contains aggregations of lymph follicles (Nodi lymphoidei aggregati), referred to as PEYER’s plaques, which are part of the mucosa-associated lymphoid tissue (MALT). Similarly, the Appendix vermiformis contains large aggregations of lymph follicles and serves the immune defence.
Arteries of the small intestine

Fig. 6.46 Arteries of the duodenum, Duodenum; ventral view. (according to [1])
The blood supply of the Duodenum is accomplished by a ventral and dorsal double arterial arch. This arch is supplied cranially by the Aa. pancreaticoduodenales superiores anterior and posterior which branch off the Truncus coeliacus. Caudally, the arches are supplied by the A. pancreaticoduodenalis inferior (R. anterior and R. posterior) of the A. mesenterica superior.
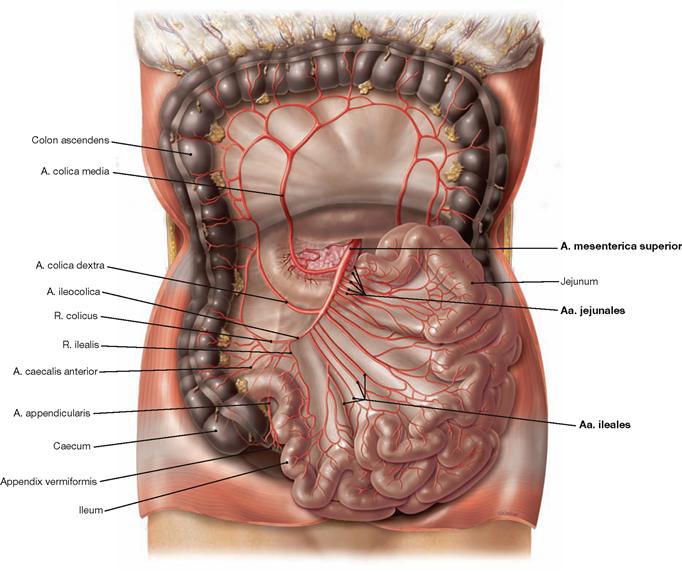
Fig. 6.47 Arteries of the jejunum, Jejunum, and ileum, Ileum; ventral view; Colon transversum reflected superiorly. (according to [1])
The intraperitoneal convolute of the Jejunum and Ileum is supplied by the A. mesenterica superior which distributes its branches (usually four to five Aa. jejunales and twelve Aa. ileales) within the mesentery of the small intestine (→ Fig. 6.115).
Arteries of the large intestine
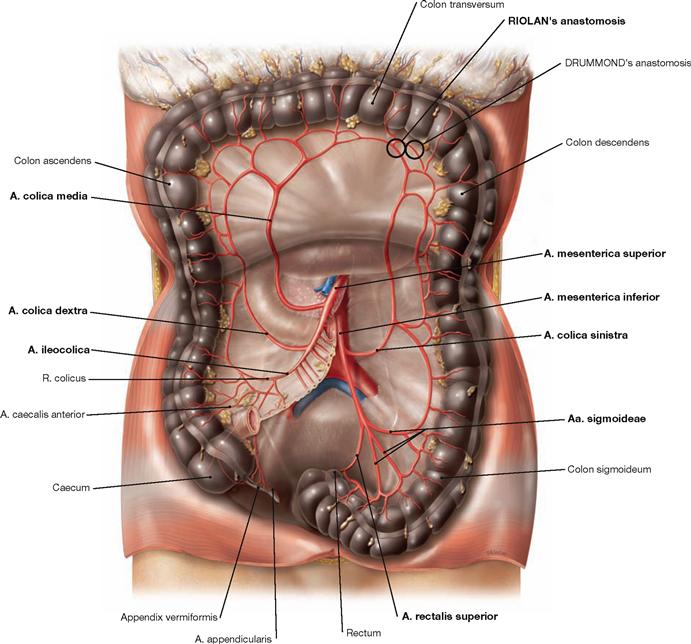
Fig. 6.48 Arteries of the large intestine, Intestinum crassum; ventral view; Colon transversum reflected superiorly. (according to [1])
• Caecum and Appendix vermiformis: A. ileocolica with a R. ilealis to the terminal ileum (anastomoses with the last A. ilealis) and with a R. colicus (anastomoses with the A. colica dextra). The artery then divides into the A. caecalis anterior and the A. caecalis posterior on both sides of the Caecum and into the A. appendicularis which courses in the meso-appendix to supply the Appendix vermiformis.
• Colon ascendens and Colon transversum: A. colica dextra and A. colica media (from the A. mesenterica superior) anastomose with each other. The A. colica media connects to the A. colica sinistra (RIOLAN’s anastomosis). An occasionally existing anastomosis with one of the arcades at the left colic flexure is referred to as DRUMMOND’s anastomosis.
• Colon descendens and Colon sigmoideum: A. colica sinistra and Aa. sigmoideae from the A. mesenterica inferior. The A. rectalis superior also derives from the A. mesenterica inferior and supplies the upper rectum.
For developmental reasons, the left colic flexure is the watershed for the neurovascular supply. With respect to the arteries: the supply by the A. mesenterica superior for the Colon ascendens and Colon transversum shifts to the supply by the A. mesenterica inferior for the Colon descendens and upper Rectum.
Veins of the small and large intestine
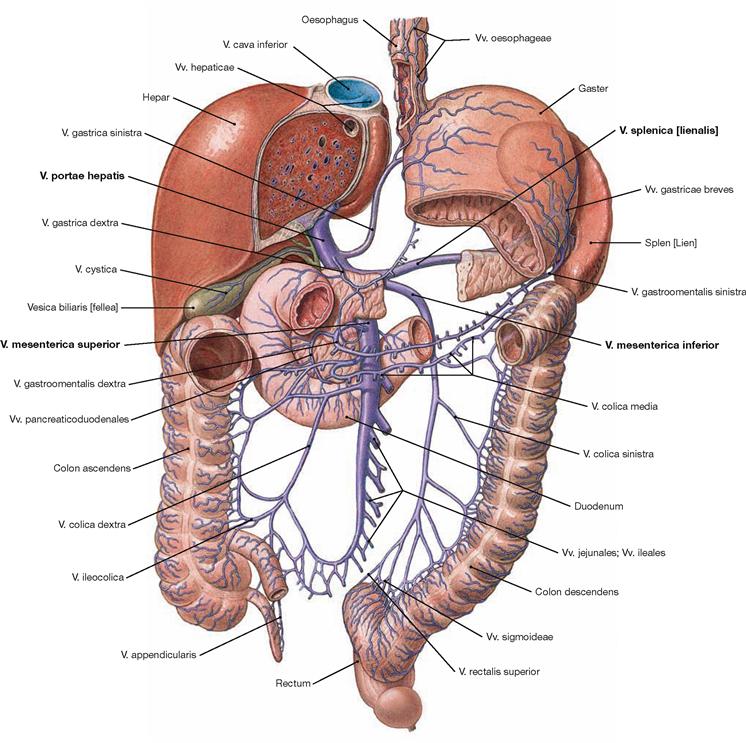
Fig. 6.49 Veins of the small intestine, Intestinum tenue, and the large intestine, Intestinum crassum; ventral view.
Name and course of the intestinal veins are similar to those of the arteries. The veins enter one of the three main tributaries of the portal vein (V. portae hepatis): the V. mesenterica superior merges with the V. splenica behind the pancreatic head to form the V. portae hepatis. The V. mesenterica inferior drains into the V. splenica (70 % of all cases) or into the V. mesenterica superior (30%).
Developmentally, the left colic flexure is the watershed for the neurovascular supply. With respect to the veins: from the Colon ascendens and Colon transversum venous blood drains into the V. mesenterica superior and from the Colon descendens and the upper Rectum the venous blood drains into the V. mesenterica inferior.
Branches of the V. mesenterica superior:
Lymph vessels of the intestines
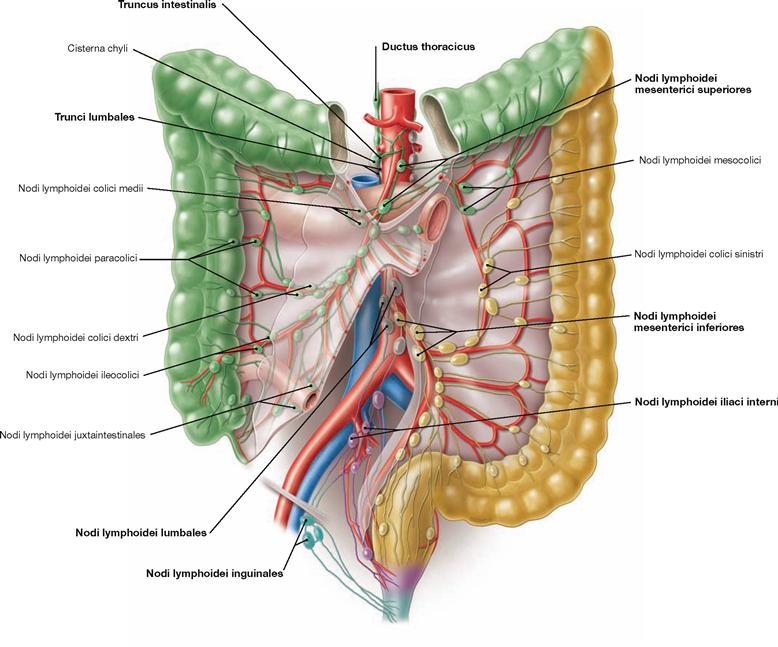
Fig. 6.50 Lymph vessels and regional lymph nodes of the small intestine, Intestinum tenue, and the large intestine, Intestinum crassum.
The respective groups of lymph nodes (a total of 100 to 200 lymph nodes) are coloured differently according to their drainage areas. (according to [1])
Located directly adjacent to the small intestine are the Nodi lymphoidei juxtaintestinales, adjacent to the large intestine the Nodi lymphoidei paracolici. After filtration in several successive lymph stations along the vascular arcades (e.g. Nodi lymphoidei colici dextri, colici medii, colici sinistri, ileocolici, mesocolici), the lymph enters into two major drainage systems:
• From the entire small intestine as well as Caecum, Colon ascendens, and Colon transversum, the lymph drains into the Nodi lymphoidei mesenterici superiores at the origin of the A. mesenterica superior and further via the Truncus intestinalis into the Ductus thoracicus (green).
• From the Colon descendens, Colon sigmoideum, and proximal rectum, the lymph reaches the Nodi lymphoidei mesenterici inferiores at the origin of the A. mesenterica inferior (yellow) and further via the retroperitoneal para-aortal lymph nodes (Nodi lymphoidei lumbales, grey) into the Trunci lumbales (grey).
The distal rectum and the anal canal also drain into the Trunci lumbales. The first lymph node stations, however, are the Nodi lymphoidei iliaci interni, and the Nodi lymphoidei inguinales (pink, turquoise) for the terminal segment of the anal canal, respectively.
Developmentally, the left colic flexure is the watershed for the neurovascular supply. With respect to the lymphatic drainage: the Nodi lymphoidei mesenterici superiores are the regional lymph nodes for the Colon ascendens and Colon transversum, whereas the Nodi lymphoidei mesenterici inferiores drain the Colon descendens.
Innervation of the intestines
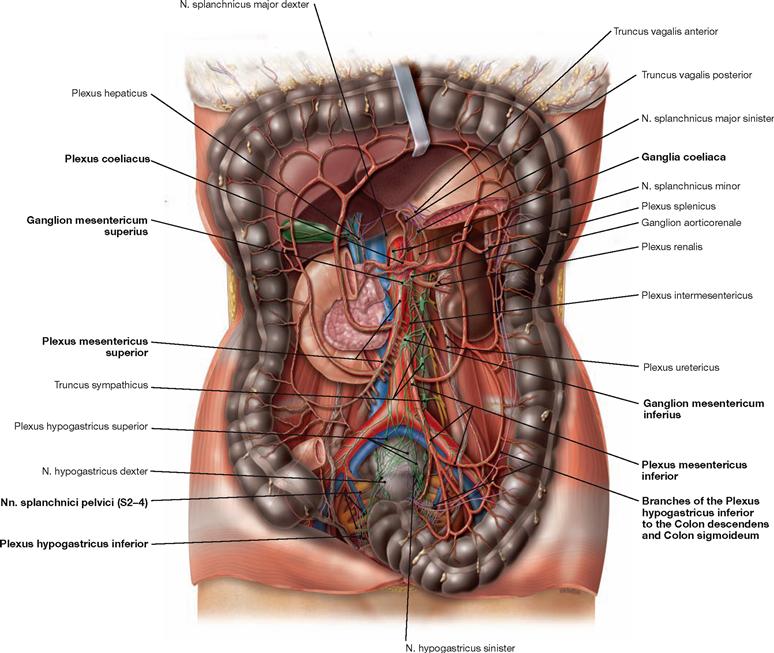
Fig. 6.51 Autonomic innervation of the small intestine, Intestinum tenue, and large intestine, Intestinum crassum; ventral view. (according to [1])
The autonomic nerves of the sympathetic (green) and parasympathetic (purple) nervous system generate a plexus at the anterior side of the Aorta (Plexus aorticus abdominalis). These nerve fibres continue along the major branches of the Aorta to reach the target organs. Small and large intestines are innervated by fibres derived from the plexus around the three major visceral branches of the Aorta (Plexus coeliacus, Plexus mesentericus superior and Plexus mesentericus inferior).
The perikarya of the preganglionic sympathetic neurons are located in the intermediolateral cell column of the spinal cord. Their axons reach the sympathetic trunk (Truncus sympathicus) and course without synapsing in the Nn. splanchnici major and minor to the plexus around the Aorta, where they finally synapse in the respective ganglia (Ganglion coeliacum, Ganglia mesenterica superius and inferius) to postganglionic neurons. Axons of the postganglionic neurons travel along the arteries to reach the intestines.
Preganglionic parasympathetic neurons of the Nn. vagi [X] course along the Oesophagus as Trunci vagales anterior and posterior, pass through the diaphragm and reach the visceral nerve plexus of the Aorta abdominalis. They pass through the ganglia without synapsing to reach the postganglionic neurons within the wall or in the vicinity of the target organs. The innervation area of the Nn. vagi [X] ends in the Plexus mesentericus superior and, thus, in the area of the left colic flexure.
The Colon descendens is innervated by the sacral division of the parasympathetic nervous system. The preganglionic parasympathetic neurons are localised at the S2–S4 spinal cord level and the nerve fibres leave the spinal nerves as Nn. splanchnici pelvici. They are synapsed in the ganglia of the Plexus hypogastricus inferior in the vicinity of the Rectum. The postganglionic nerve fibres either ascend to the Plexus mesentericus inferior (not shown) or directly reach the Colon descendens.
The parasympathetic innervation stimulates, and the sympathetic innervation inhibits peristalsis and perfusion of the intestines.
For developmental reasons, the left colic flexure is the watershed for the neurovascular supply. With respect to the autonomic innervation: Colon ascendens and Colon transversum are innervated from the Plexus mesentericus superior, whereas the Colon descendens is innervated by the Plexus mesentericus inferior (cranial/sacral division of the parasympathetic system).
Large intestine, imaging

Fig. 6.52 Large intestine, Intestinum crassum; radiograph in anteroposterior (AP) beam projection after application of contrast medium and air (double contrast barium enema). Positional variations of the Colon transversum can be detected (→ Fig. 6.53).
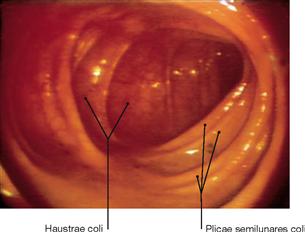
Fig. 6.54 Ascending colon, Colon ascendens; endoscopy of the colon (coloscopy).
In contrast to the circular mucosal folds of the small intestine, the mucosal folds of the large intestine are crescent-shaped (Plicae semilunares).
Projection of liver and gallbladder
Figs. 6.55a and b Projection of the viscera onto the body surface; ventral (a) and dorsal (b) views.
The liver and gallbladder are located intraperitoneally in the right epigastrium. The fundus of the gallbladder projects onto the right midclavicular line at the level of rib IX. The left lobe of the liver is located in the left Epigastrium (up to the left midclavicular line) anterior to the stomach. The position of the liver varies with respiration (lower with inspiration, higher with expiration) because its Area nuda is attached to the diaphragm. Therefore, its position is also dependent on the size of the lung. Because of the dome-shaped diaphragm, the anterior and posterior side of the liver is covered in part by the pleural cavity (→ Fig. 6.124). Up to the midclavicular line, the inferior margin of the liver usually co-locates with the right inferior costal margin and, thus, the liver is not palpable. With an enlarged lung, such as with pulmonary emphysema in a smoker, the liver may be palpable without being enlarged. The topography of the liver is also important for diagnostic procedures such as liver biopsies (→ Fig. 6.75).
Development of the liver and gallbladder
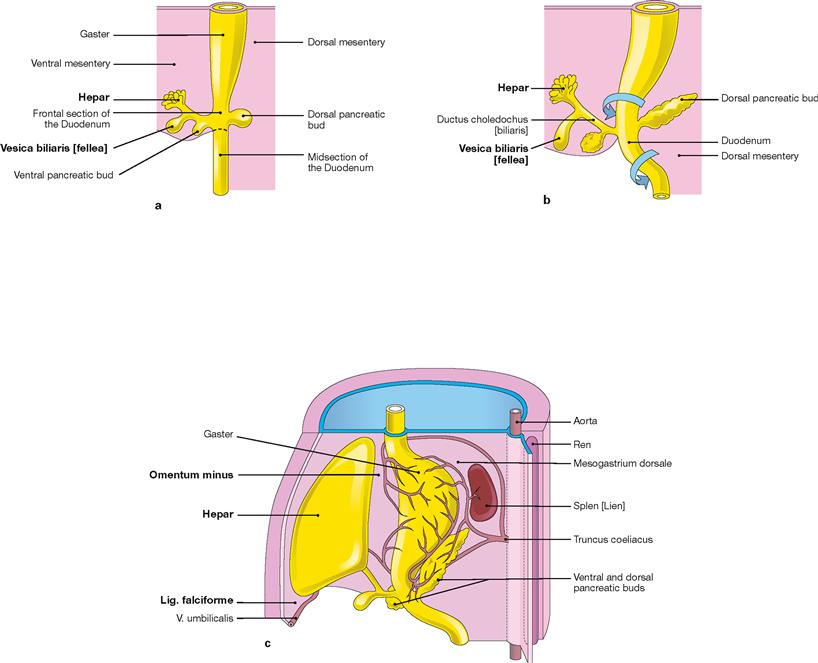
Figs. 6.56a to c Developmental stages of the liver, Hepar, and the gallbladder, Vesica biliaris, in weeks 4 to 5. [20]
The epithelial tissues of liver and gallbladder derive from the endoderm of the primordial gut at the level of the future Duodenum. In week 4 (from day 22 on) the endoderm forms a thickening (hepatic diverticulum) which divides into a superior liver primordium and an inferior primordium for the bile system (a and b). The epithelium of the liver primordium grows into the connective tissue of the Septum transversum in which islets of haematopoiesis develop. This way, the connective tissue components and the intrahepatic blood vessels (sinusoids) intermingle with the liver primordium. The liver then grows into the Mesogastrium ventrale (c) and, thus, splits it into a Mesohepaticum ventrale and a Mesohepaticum dorsale (→ Fig. 6.1). The Mesohepaticum ventrale develops into the Lig. falciforme hepatis and connects to the ventral body wall. The Mesohepaticum dorsale becomes the Omentum minus connecting the liver with the stomach and the Duodenum.
Liver and gallbladder
Liver, overview
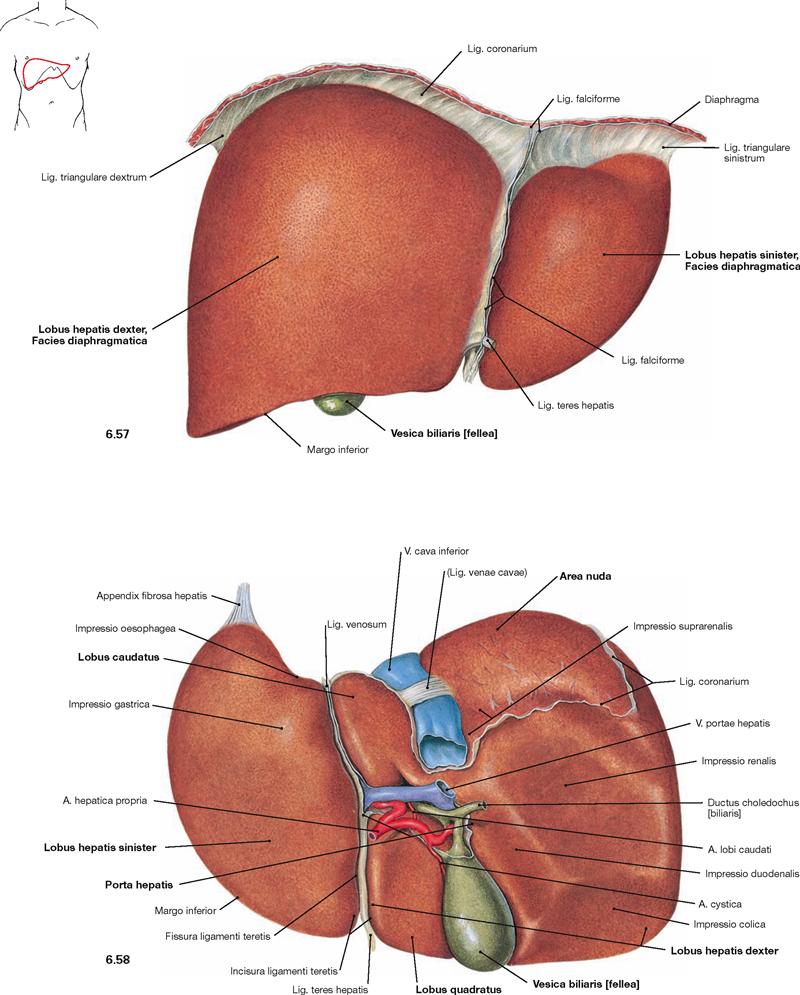
Fig. 6.57 and Fig. 6.58 Liver, Hepar; ventral (→ Fig. 6.57) and dorsal caudal (→ Fig. 6.58) views. For explanations → Figure 6.59.
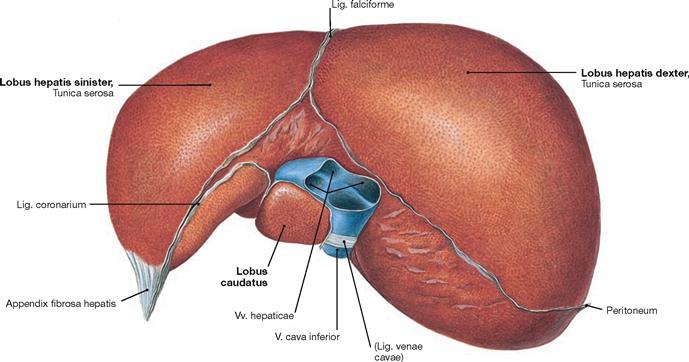
Fig. 6.59 Liver, Hepar; cranial view.
The liver is the largest gland (1200–1800 g) and the main metabolic organ of the body. The Facies diaphragmatica is adjacent to the diaphragm and the Facies visceralis with the anterior lower margin (Margo inferior) points towards the abdominal viscera (→ Figs. 6.57 and 6.58).
The Facies diaphragmatica is partly adherent to the diaphragm and lacks the peritoneal lining in this area (Area nuda). The liver is divided in a larger right and a smaller left lobe (Lobus dexter and Lobus sinister) which are separated ventrally by the Lig. falciforme. The latter continues as Lig. coronarium which then becomes the right and left Lig. triangulare connecting to the diaphragm. The Lig. triangulare sinistrum continues into the fibrous Appendix fibrosa hepatis. The free margin of the Lig. falciforme contains the Lig. teres hepatis (remnant of the prenatal V. umbilicalis). Both ligaments connect to the ventral abdominal wall.
At the Facies visceralis the Fissura ligamenti teretis hepatis continues to the Porta hepatis which harbours the vascular structures to and from the liver (V. portae hepatis, A. hepatica propria, Ductus hepaticus communis). Cranially, the Lig. venosum (remnant of the prenatal Ductus venosus) is shown. On the right side of the Porta hepatis (hilum of the liver), the V. cava inferior is located in a superior groove and the gallbladder (Vesica biliaris) is embedded in the inferior Fossa vesicae biliaris. The Lig. teres hepatis, Lig. venosum, V. cava inferior, and gallbladder delineate two rectangular areas on both sides of the Porta hepatis at the inferior side of the right hepatic lobe, the ventral Lobus quadratus and the dorsal Lobus caudatus. The liver is not covered by peritoneum in four larger areas: Area nuda, Porta hepatis, bed of the gallbladder, and groove of the V. cava inferior.
In vivo, the liver is deformable and adjusts to the shape of the surrounding organs. In fixed condition, adjacent organs cause impressions which are fixation artifacts without further relevance, although they provide positional information about the liver.
Structure of the liver
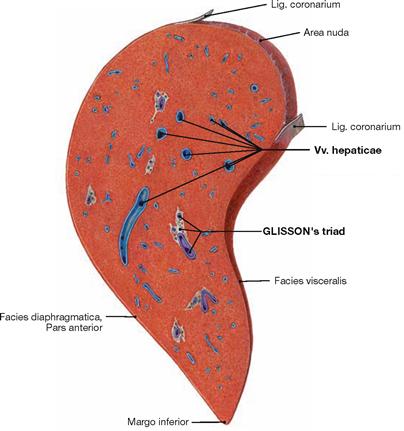
Fig. 6.60 Liver, Hepar; sagittal section through the right lobe of the liver.
The vascular and bile duct structures entering the liver at the hilum (V. portae hepatis, A. hepatica propria, Ductus hepaticus communis) are surrounded by connective tissue. They branch within the parenchyma of the liver, and create the GLISSON’s triad (portal triad) in the portal tracts (portal canals) (→ Fig. 6.61).
The liver veins (Vv. hepaticae) and their tributaries which drain the blood from the liver into the V. cava inferior course separately from the vessels of the GLISSON’s triad.
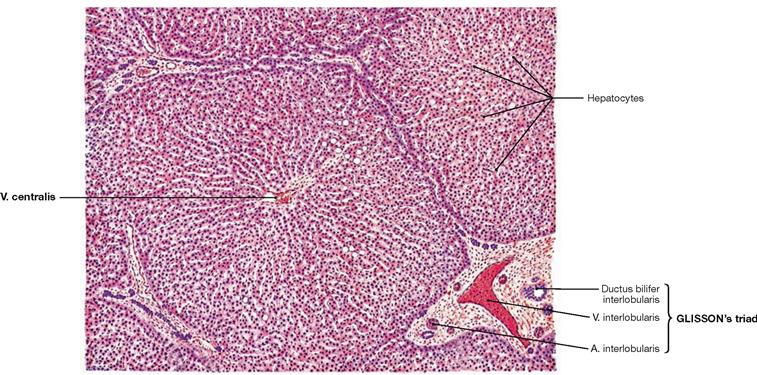
Fig. 6.61 Structure of the liver, Hepar; microscopic view. [24]
The structural unit of the liver parenchyma is the hepatic lobule which consists of radially oriented trabeculae of hepatocytes. The classical almost hexagonal hepatic lobule is surrounded by portal tracts at three to six corners. Three structures referred to collectively as GLISSON’s triad (portal triad) are always found in the portal tract, embedded in connective tissue (A. and V. interlobularis, Ductus bilifer interlobularis). The centrilobular venule (V. centralis) is located in the centre of the hepatic lobule and collects the blood from the liver sinusoids which originally derives the arteries and veins at the periphery of the lobule. The centrilobular venule then drains into the Vv. sublobulares, which are branches of the Vv. hepaticae. The slow radial blood flow in the sinusoids enables hepatocytes to absorb nutrients and metabolites and to secrete synthesised proteins as for example plasma proteins.
Segments of the liver
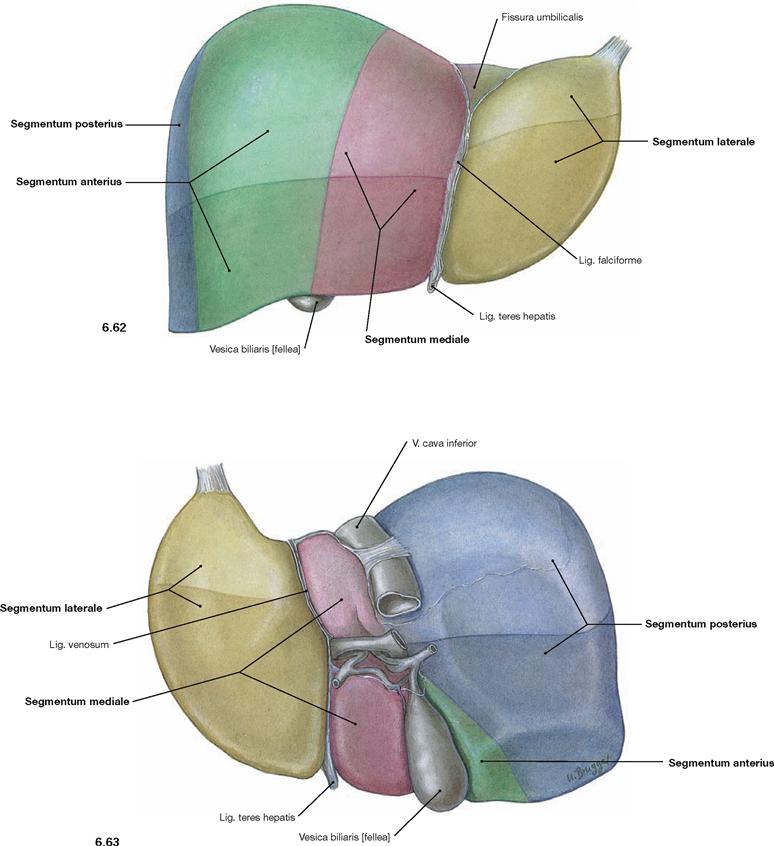
Fig. 6.62 and Fig. 6.63 Segments of the liver, Hepar; ventral (→ Fig. 6.62) and dorsal (→ Fig. 6.63) views. Individual liver segments are coloured differently.
The three almost vertically oriented liver veins (Vv. hepaticae, → Fig. 6.64) divide the liver into four adjacent segments. The Segmentum laterale corresponds to the anatomical left lobe of the liver and is bordered by the Lig. falciforme hepatis, which is adjacent to the left liver vein. The Segmentum mediale is located between the Lig. falciforme and the gallbladder at the level of the middle liver vein. To the right side, the Segmentum anterius and the Segmentum posterius follow and are separated by the right liver vein, which is not visible on the liver surface. The structures of the portal triad organise these liver segments into eight functional and clinically important liver segments (→ Fig. 6.64) which are indicated here by different colourations.
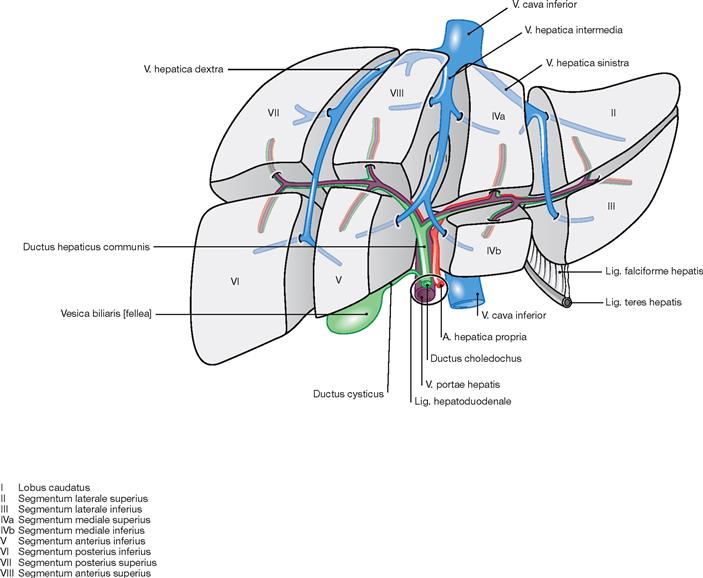
Fig. 6.64 Schematic illustration of the liver segments and their relations to the intrahepatic blood vessels and the bile ducts; ventral view. (according to [1])
The liver is divided into eight functional segments which are supplied by one branch of the portal triad (V. portae hepatis, A. hepatica propria, Ductus hepaticus communis) each and therefore are functionally independent. Two segments each are combined by the vertically oriented three liver veins to four adjacent liver segments (→ Figs. 6.62 and 6.63). It is of functional importance that segments I to IV are supplied by branches of the left portal triad and can be combined to a functional left liver lobe. The segments V to VIII are supplied by branches of the right portal triad and represent the functional right liver lobe. As a result, the border between the functional right and left liver lobes is located in the sagittal plane between the V. cava inferior and gallbladder and not at the level of the Lig. falciforme hepatis.
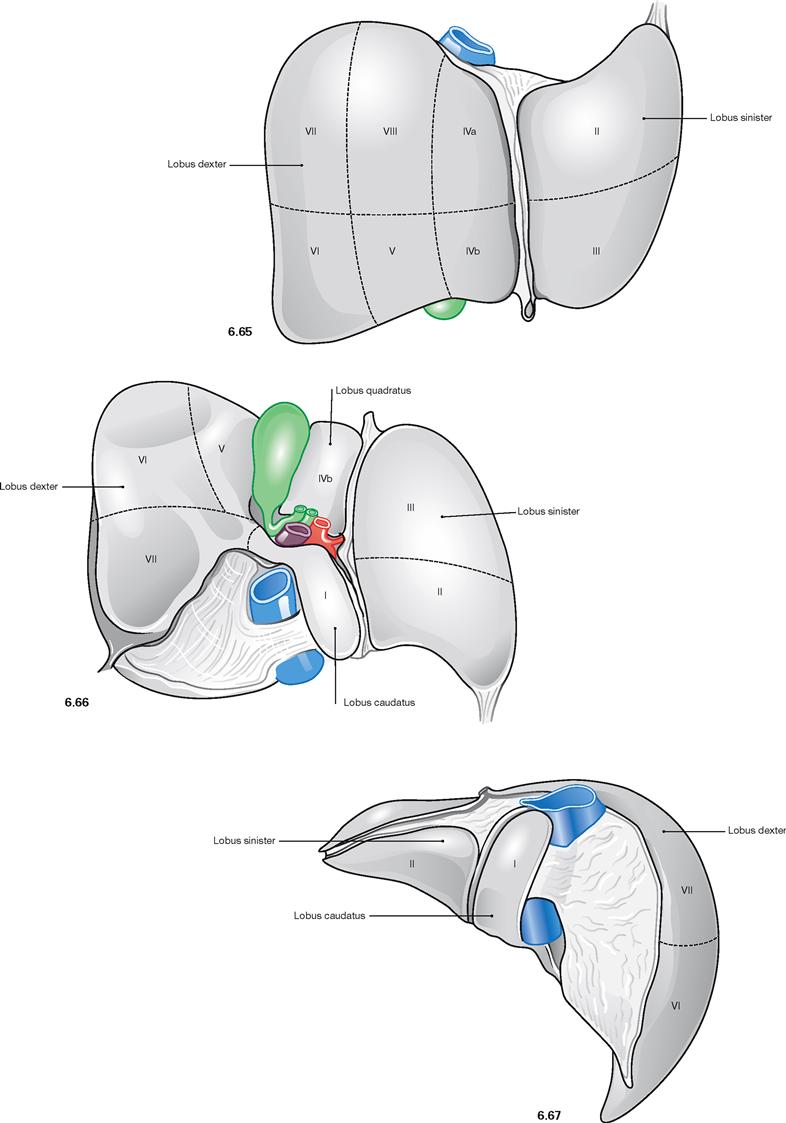
Fig. 6.65 to Fig. 6.67 Segments of the liver, Hepar; ventral (→ Fig. 6.65), dorsocaudal (→ Fig. 6.66), and dorsocranial (→ Fig. 6.67) view. (according to [1])
Because of their clinical relevance for visceral surgery, the liver segments are marked in this figure with Roman numerals (→ Fig. 6.64) on the liver surface. The Lobus caudatus represents segment I at the underside of the anatomical right lobe of the liver. However, this segment functionally belongs to the left lobe of the liver.
Arteries of the liver and gallbladder
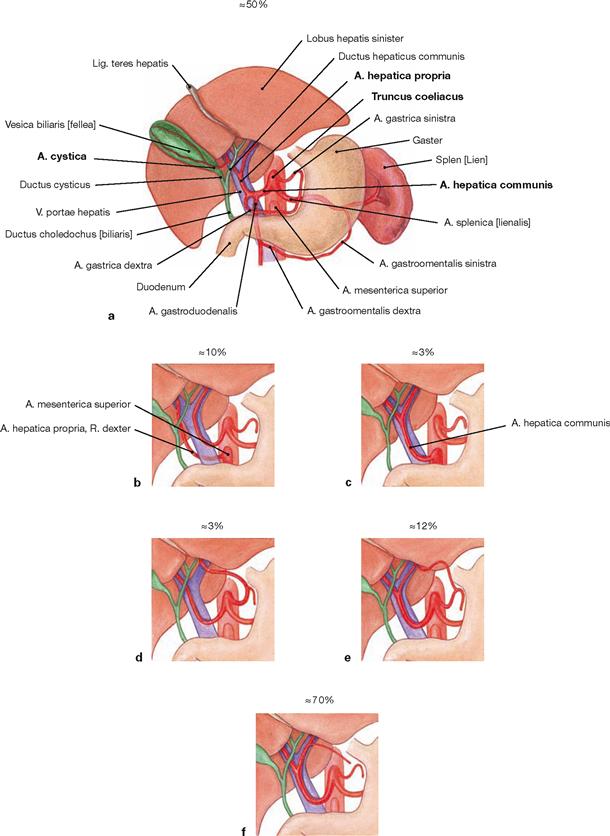
Figs. 6.68a to f Arteries of the liver, Hepar, and the gallbladder, Vesica biliaris.
The liver is supplied by the A. hepatica propria derived from the A. hepatica communis, a direct arterial branch of the Truncus coeliacus. After giving off the A. gastrica dextra, the A. hepatica propria courses within the Lig. hepatoduodenale together with the V. portae hepatis and the common bile duct (Ductus choledochus) to the hilum of the liver. Here, this artery divides into the R. dexter and the R. sinister to the liver lobes. The R. dexter gives rise to the A. cystica to the gallbladder. In 10–20% of all cases, the A. mesenterica superior contributes to the blood supply of the right liver lobe, and the A. gastrica sinistra contributes to the supply of the left liver lobe.
Variations of the blood supply of the liver:
b. contribution of the A. mesenterica superior to the blood supply of the right liver lobe
c. origin of the A. hepatica communis by the A. mesenterica superior
d. blood supply of the left liver lobe by the A. gastrica sinistra
e. contribution of a branch of the A. gastrica sinistra to the blood supply of the left liver lobe in addition to the R. sinister of the A. hepatica propria
f. blood supply of the lesser curvature of the stomach by an accessory branch of the A. hepatica propria
Veins of the liver and gallbladder
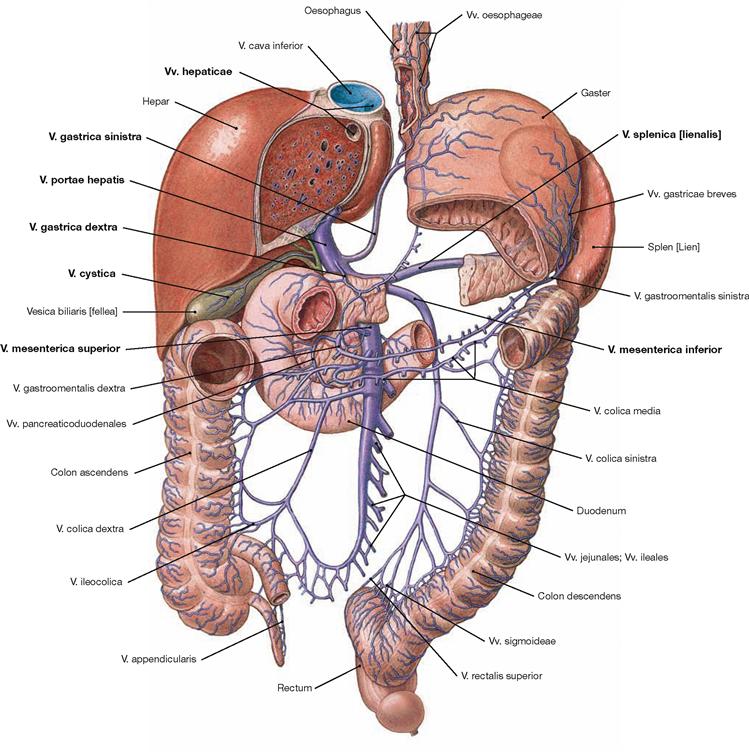
Fig. 6.69 Veins of the liver, Hepar, and the gallbladder, Vesica biliaris; ventral view.
The liver has an incoming and an outgoing venous system. The portal vein (V. portae hepatis) collects the nutrient-rich blood from the unpaired abdominal organs (stomach, intestines, Pancreas, spleen) and feeds this blood, together with the arterial blood from the A. hepatica communis, into the sinusoids of the liver lobules. Three liver veins (Vv. hepaticae, → Fig. 6.60) transport the blood from the liver to the V. cava inferior.
The portal vein has three main tributaries: Behind the head of the Pancreas, the V. mesenterica superior merges with the V. splenica to form the V. portae hepatis. In most cases (70 %), the V. mesenterica inferior drains into the V. splenica; in the remaining cases (30%) it drains into the V. mesenterica superior.
Branches of the V. splenica (collecting blood from the spleen and from parts of the stomach and Pancreas):
Branches of the V. mesenterica superior (collecting blood from parts of the stomach and Pancreas, from the entire small intestine, the Colon ascendens, and Colon transversum):
• V. gastroomentalis dextra with Vv. pancreaticoduodenales
Branches of the V. mesenterica inferior (collecting blood from the Colon descendens, and the upper Rectum):
• V. rectalis superior: the vein anastomoses with the V. rectalis media and the V. rectalis inferior, which drain into the V. cava inferior.
In addition, there are veins which drain directly into the portal vein once the main venous branches have merged:
Portocaval anastomoses
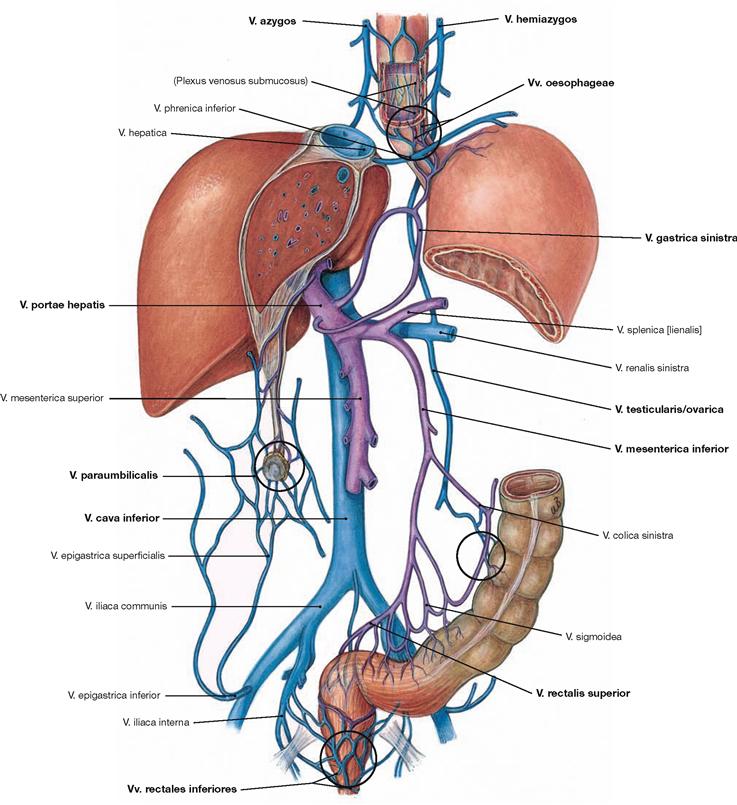
Fig. 6.70 Portocaval anastomoses (connections between the portal vein and the V. cava superior/inferior). Tributaries to the V. cava superior/inferior (blue), tributaries to the V. portae hepatis (purple).
There are four possible collateral circulations via portocaval anastomoses (marked by black circles):
• Vv. gastricae dextrae and sinistrae via oesophageal veins and veins of the azygos system to the V. cava superior. This may result in the dilation of submucosal veins of the Oesophagus (oesophageal varices).
• Vv. paraumbilicales via veins of the ventral abdominal wall (deep: Vv. epigastricae superior and inferior; superficial: V. thoracoepigastrica and V. epigastrica superficialis) to the V. cava superior and inferior. Dilation of the superficial veins may appear as Caput medusae.
• V. rectalis superior via veins of the distal rectum and anal canal and via the V. iliaca interna to the V. cava inferior
• retroperitoneal anastomoses via the V. mesenterica inferior to the V. testicularis/ovarica with connection to the V. cava inferior
Lymph vessels of the liver and gallbladder
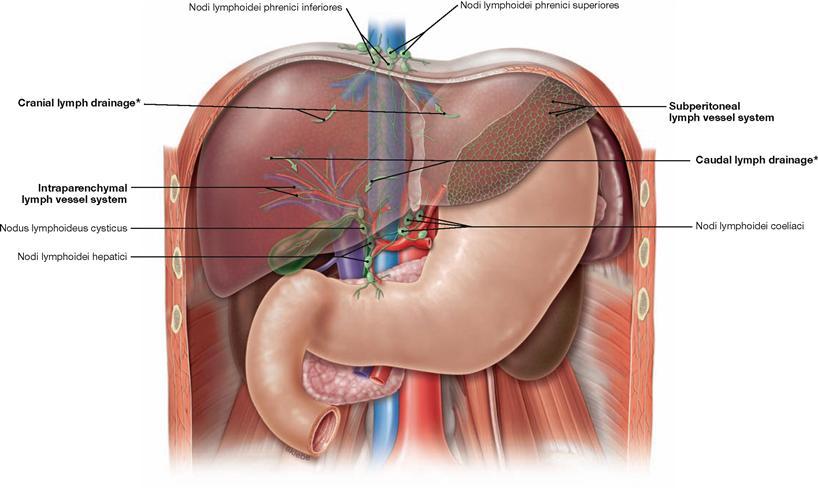
Fig. 6.71 Lymph vessels and lymph nodes of the liver and bile duct system.
The liver has two lymph vessel systems:
• the subperitoneal system at the surface of the liver
• the intraparenchymal system alongside the structures in the portal triad to the hilum of the liver
With respect to the regional lymph nodes, there are two major lymph drainage routes:
• in caudal direction to the hilum of the liver (most important) via the Nodi lymphoidei hepatici at the hilum of the liver (→ Fig. 6.17) and from there via the Nodi lymphoidei coeliaci to the Truncus intestinalis
• in cranial direction passing the diaphragm via the Nodi lymphoidei phrenici inferiores and superiores into the Nodi lymphoidei mediastinales anteriores and posteriores which drain into the Trunci bronchomediastinales; using this drainage pathway, carcinomas of the liver may also metastasise into thoracic lymph nodes.
There are two minor lymph drainage route:
• to the anterior abdominal wall via the lymph vessels in the Lig. teres hepatis to the inguinal and axillary lymph nodes
• to the stomach and Pancreas from the left lobe of the liver
The gallbladder usually has its own Nodus lymphoideus cysticus in the area of the neck, which drains into the lymph nodes at the hilum of the liver (in the caudal direction).
* The arrows depict the direction of lymph drainage from the parenchyma via the cranial or caudal route.
Liver, imaging
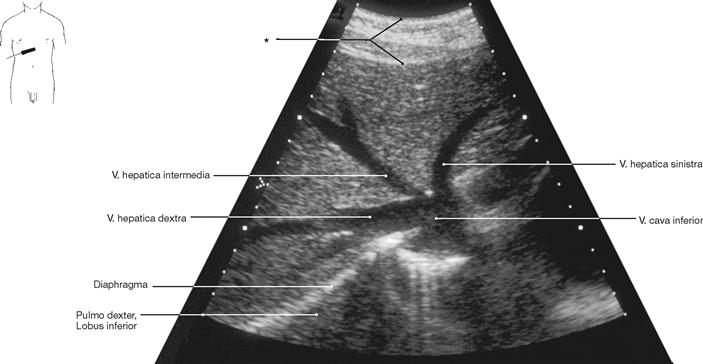
Fig. 6.72 Confluence of the liver veins, Vv. hepaticae, with the V. cava inferior; ultrasound image; caudal view.
* abdominal wall
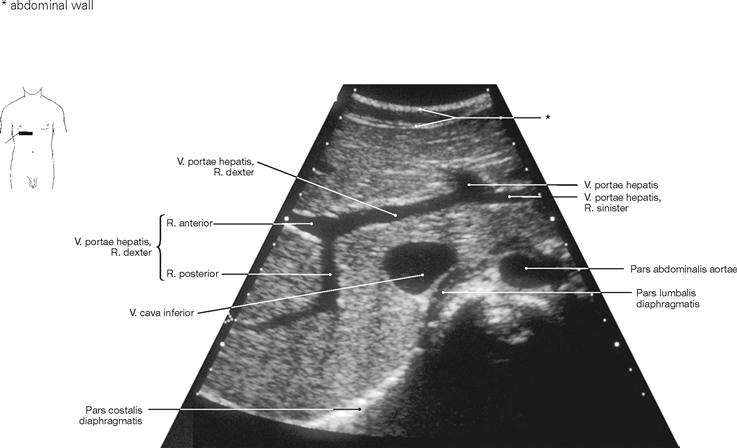
Fig. 6.73 Liver, Hepar, V. portae hepatis; demonstration of the branching of the portal vein; ultrasound image; caudal view.
* abdominal wall
Liver biopsy
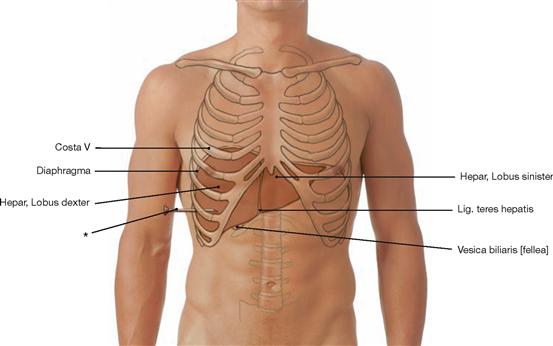
Fig. 6.74 Projection of the liver, Hepar, and the gallbladder, Vesica biliaris, onto the ventral abdominal wall in mid-respiration position.
* position of the needle during liver puncture
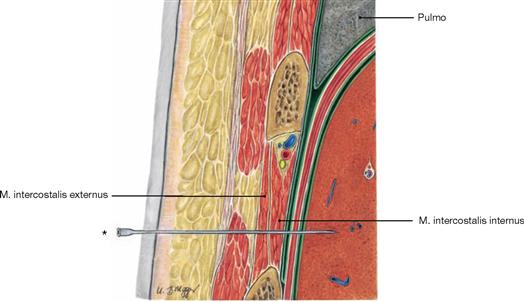
Fig. 6.75 Layers of the chest wall and the liver, Hepar; frontal section; liver puncture biopsy.
The ultrasound-guided puncture is performed in expiration through one of the lower intercostal spaces. Since the liver is partly covered by the pleural cavity this access reduces the risk of a pneumothorax. To spare the intercostal neurovascular structures, the puncture is always performed at the superior costal margin. The peritoneal lining covering the liver capsule receives sensory innervation by the N. phrenicus (C3–C5) from the Plexus cervicalis. This explains why patients often experience referred pain in the area of the right shoulder.
* position of the needle during liver puncture
Liver and gallbladder, imaging
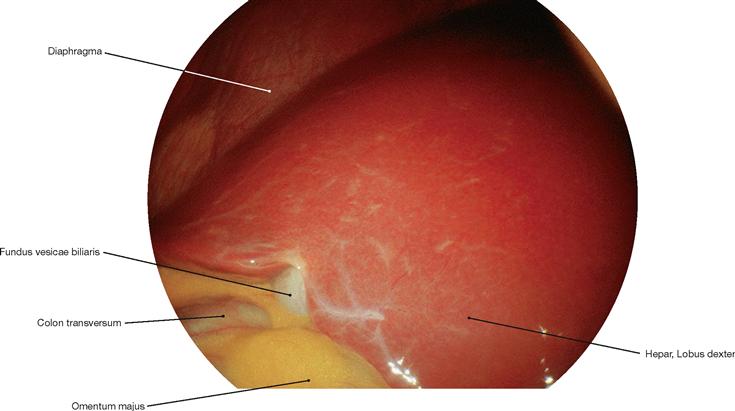
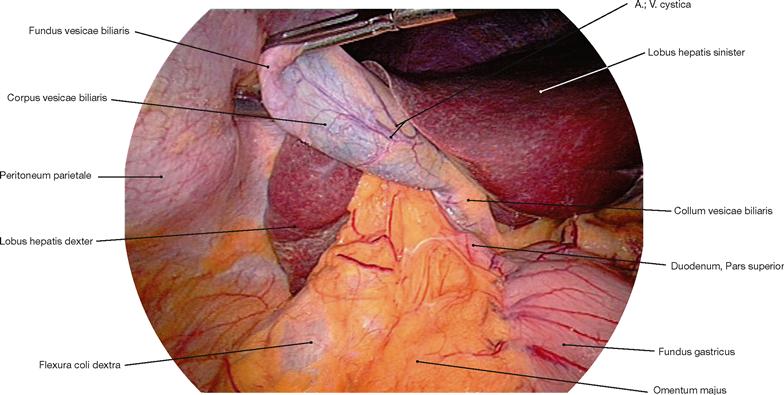
Fig. 6.76 Liver, Hepar, and gallbladder, Vesica biliaris; laparoscopic image; oblique caudal view from the left side.
Structure of the gallbladder and extrahepatic bile ducts
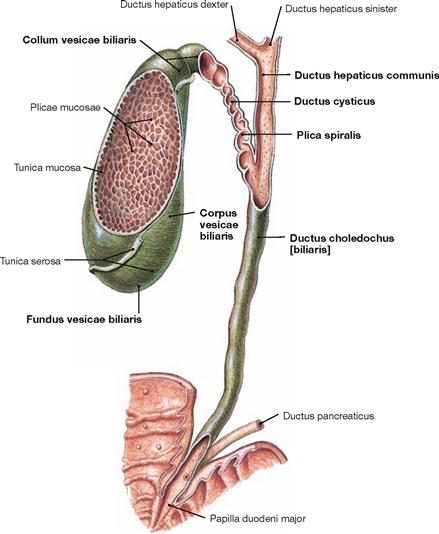
Fig. 6.78 Gallbladder, Vesica biliaris, and extrahepatic bile ducts; ventral view.
The gallbladder usually holds approximately 40–70 ml of bile. It consists of a body (Corpus vesicae biliaris) with a fundus and a neck part (Collum vesicae biliaris). A spiral fold (Plica spiralis HEISTER) at the terminal end of the neck closes the opening of the excretory cystic duct (Ductus cysticus), which then fuses with the common hepatic duct (Ductus hepaticus communis) to form the common bile duct (Ductus choledochus).
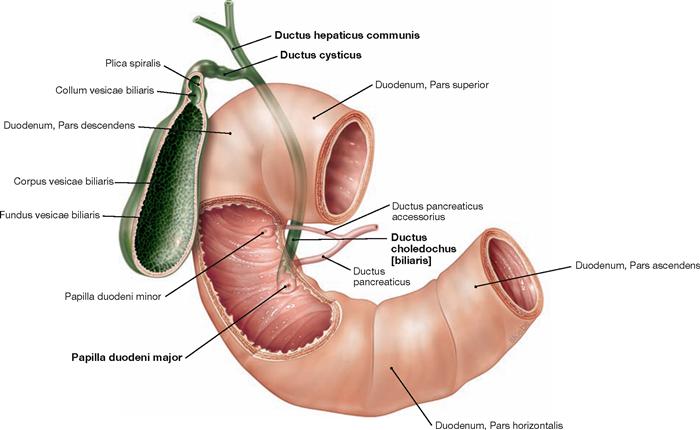
Fig. 6.79 Gallbladder, Vesica biliaris, extrahepatic bile ducts and duodenum, Duodenum; ventral view.
The common bile duct (Ductus choledochus) is usually 6 cm long and 0.4–0.9 cm in diameter. It courses within the Lig. hepatoduodenale ventral to the portal vein, then runs behind the Pars superior of the Duodenum to traverse the head of the Pancreas and reach the descending part of the Duodenum. In 60% of all cases, the common bile duct fuses with the Ductus pancreaticus to form the Ampulla hepatopancreatica, which enters the Duodenum at the Papilla duodeni major (Papilla VATERI). At its distal end, smooth muscles of the common bile duct (Ductus choledochus) create the M. sphincter ductus choledochi. The inferior part thereof, also referred to as M. sphincter ampullae (ODDI), encompasses the ampulla and the entrance of the Duodenum.
Liver and gallbladder
CALOT‘s triangle
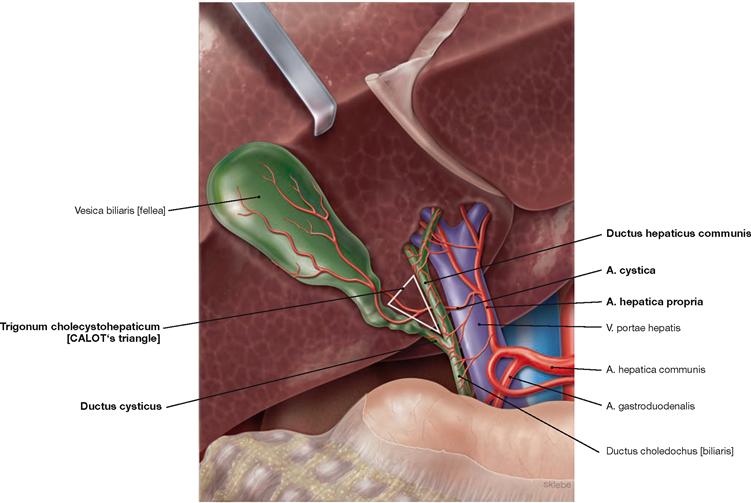
Fig. 6.80 CALOT’s triangle, Trigonum cholecystohepaticum; caudal view. (according to [1])
The Ductus cysticus, the Ductus hepaticus communis and the inferior area of the liver together form the Trigonum cholecystohepaticum, also referred to as CALOT’s triangle. In 75% of all cases, the A. cystica originates in this triangle from the R. dexter of the A. hepatica propria and courses posteriorly through this triangle to reach the Ductus cysticus and the neck of the gallbladder.
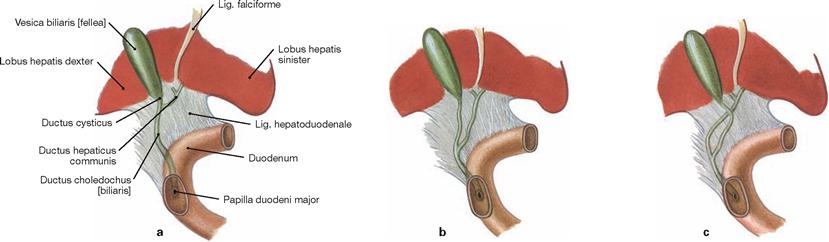
Figs. 6.81a to c Variations of the bile ducts regarding the confluence of the Ductus hepaticus communis and Ductus cysticus.
Gallbladder and extrahepatic bile ducts, imaging
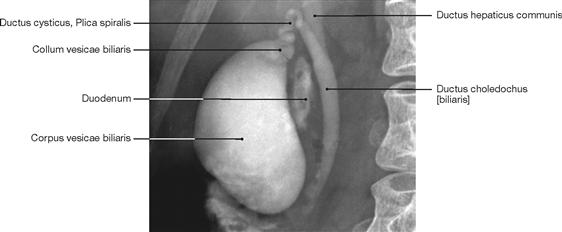
Fig. 6.82 Gallbladder, Vesica biliaris, extrahepatic bile ducts; radiograph in anteroposterior (AP) beam projection after application of contrast medium; patient in upright position; ventral view.
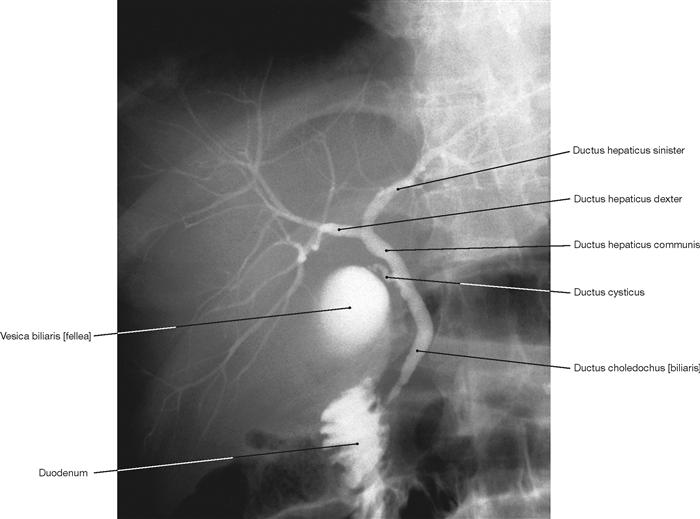
Fig. 6.83 Gallbladder, Vesica biliaris, as well as intra- and extrahepatic bile ducts; radiograph in anteroposterior (AP) beam projection after application of contrast medium; patient in upright position; ventral view.
Projection of the pancreas
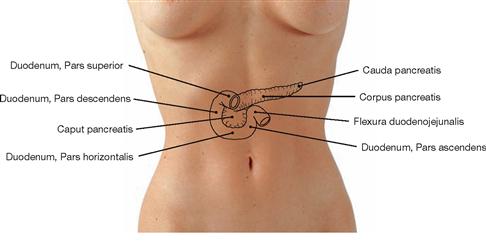
Fig. 6.84 Projection of the pancreas, Pancreas, and the duodenum, Duodenum, on the ventral abdominal wall.
The Pancreas is in a secondary retroperitoneal position and projects roughly onto the 1st or 2nd lumbar vertebra. The head (Caput pancreatis) is adjacent to the Pars descendens of the Duodenum and continues as pancreatic body (Corpus pancreatis) which crosses the vertebral column to continue as pancreatic tail (Cauda panceatis) to the hilum of the spleen.
Figs. 6.85a and b Projection of the viscera onto the body surface; ventral (a) and dorsal (b) views.
Development of the pancreas
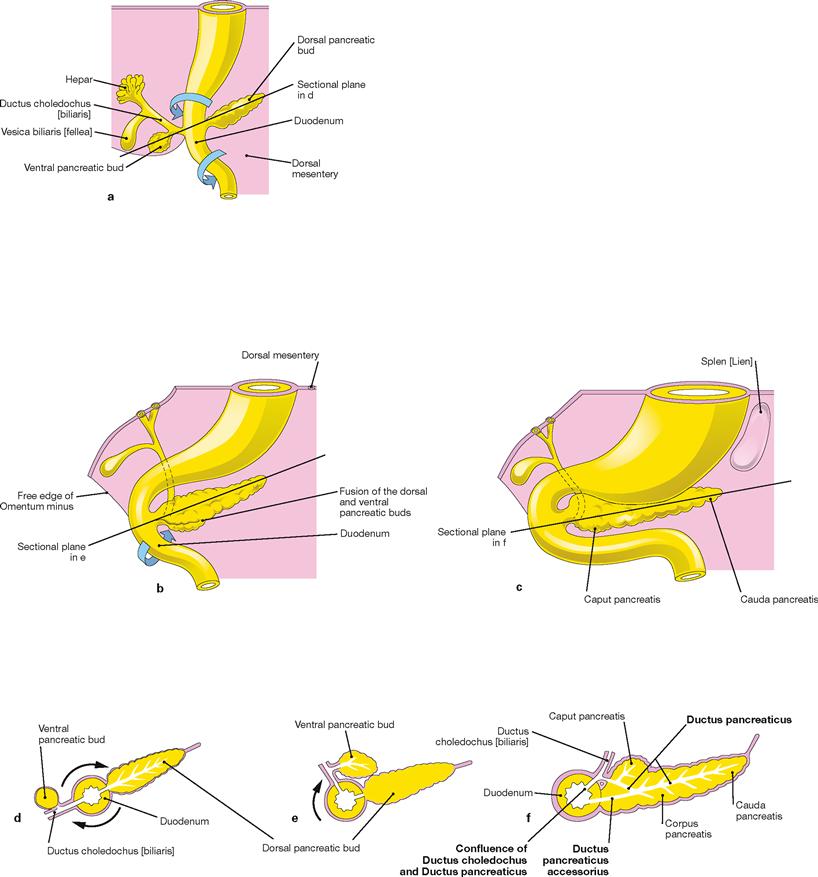
Figs. 6.86a to f Development of the pancreas, Pancreas, in weeks 5 to 8. [20]
d. to f schematic cross-sections through to Duodenum and Pancreas primordium; rotations marked by arrows
On day 28, a ventral and a dorsal pancreatic bud emerge from the endoderm of the primordial gut (a, d) inferior to the primordium of liver and gallbladder at the level of the future Duodenum. The ventral pancreatic bud moves dorsally (b, e) and, in weeks 6 to 7, fuses with the dorsal pancreatic bud, including their respective excretory ducts (d, f).
The excretory pancreatic duct is formed by the union of the distal dorsal pancreatic duct and the ventral pancreatic duct and enters the Papilla duodeni major. The proximal portion of the dorsal pancreatic duct develops (65% of all cases) into the accessory pancreatic duct which joins the Duodenum at the Papilla duodeni minor.
Structure and topographical relationships of the pancreas
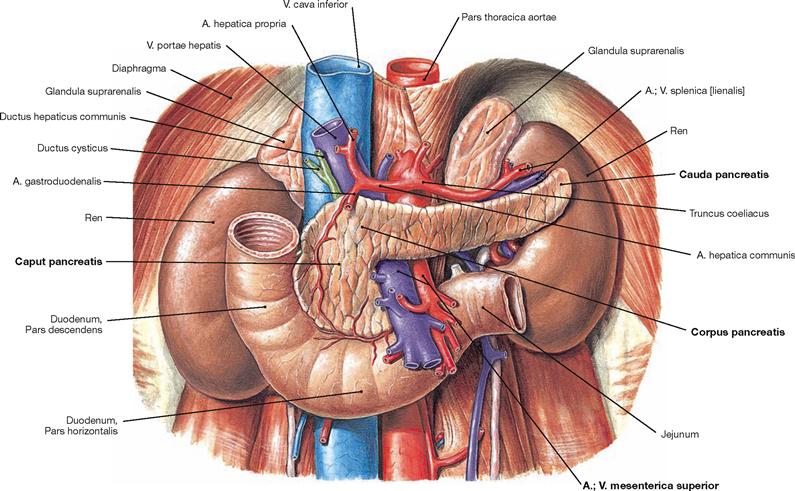
Fig. 6.87 Retroperitoneal organs of the epigastrium: pancreas, Pancreas, duodenum, Duodenum, and on both sides kidney, Ren, and adrenal gland, Glandula suprarenalis; ventral view.
The Pancreas is in a secondary retroperitoneal position. The head (Caput pancreatis) is adjacent to the Pars descendens of the Duodenum and has a dorsal uncinate process (Proc. uncinatus) which embraces the A. and V. mesenterica superior. Caudally, the Pars horizontalis of the Duodenum is adjacent.
To the left side, the pancreatic head continues as the pancreatic body (Corpus pancreatis) which traverses the vertebral column. The subsequent pancreatic tail (Cauda pancreatis) passes over the left kidney to reach the hilum of the spleen.
The Pancreas has an anterior and a posterior surface (Facies anterior and Facies posterior) which are separated by the dull upper and lower border (Margo superior and Margo inferior). The anterior aspect of the Pancreas is covered by parietal peritoneum and forms the posterior wall of the Bursa omentalis. The posterior aspect of the Pancreas is fused to the original parietal peritoneum of the posterior abdominal wall because the Pancreas was repositioned into the retroperitoneal space during its development. The fused area appears as a fascia during dissection.
Structure of the pancreas
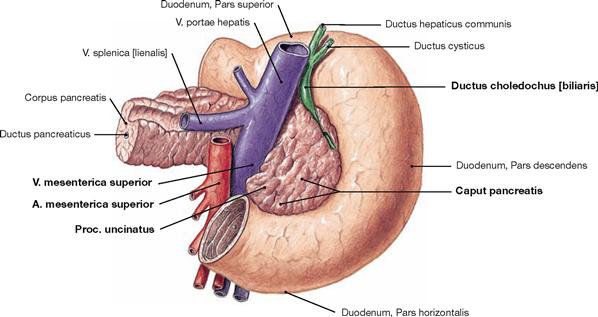
Fig. 6.88 Pancreas, Pancreas, and duodenum, Duodenum; dorsal view.
The figure illustrates the pancreatic head (Caput pancreatis) located in the C-shaped Pars descendens of the duodenum where it is obliquely pierced by the common bile duct (Ductus choledochus) in its course to the Papilla duodeni major. Dorsally, the uncinate process (Proc. uncinatus) of the pancreatic head embraces the A. and V. mesenterica superior.
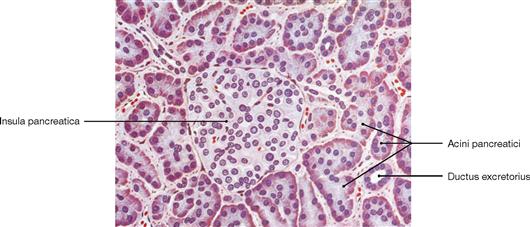
Fig. 6.89 Structure of the pancreas, Pancreas; microscopic view. [26]
The pancreas is a mixed exocrine and endocrine gland. In the acini, the exocrine part produces digestive enzymes which are delivered as inactive precursors via the duct system to reach the lumen of the intestine. The endocrine part consists of the islets of LANGERHANS (Insulae pancreaticae) and is embedded within the parenchyma of the exocrine gland, particularly in the pancreatic tail. Besides other hormones, the islets produce insulin and glucagon which are secreted into the blood and serve the regulation of the blood glucose level.
Excretory ducts of the pancreas
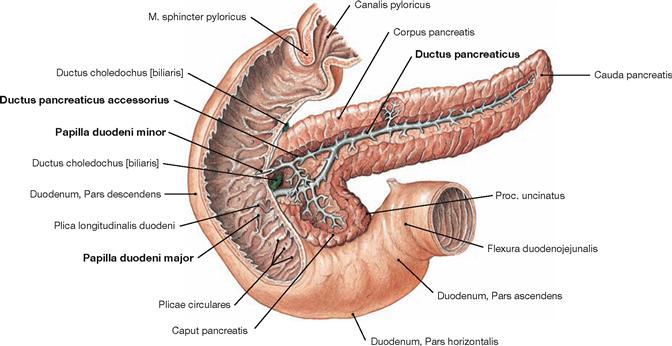
Fig. 6.90 Excretory duct system of the pancreas, Pancreas; ventral view; Ductus pancreaticus after partial resection of the Duodenum and the ventral Pancreas.
The main excretory duct (Ductus pancreaticus [duct of WIRSUNG]) fuses with the terminal segment of the common bile duct (Ductus choledochus) in 60% of all cases to form the Ampulla hepatopancreatica. The latter enters the Pars descendens of the Duodenum at the Papilla duodeni major (papilla of VATER). Developmentally (→ Fig. 6.86), an accessory duct (Ductus pancreaticus accessorius [SANTORINI’s duct]) exists in 65% of all cases which opens into the Duodenum 2 cm proximal to the Papilla duodeni minor.
Arteries of the pancreas
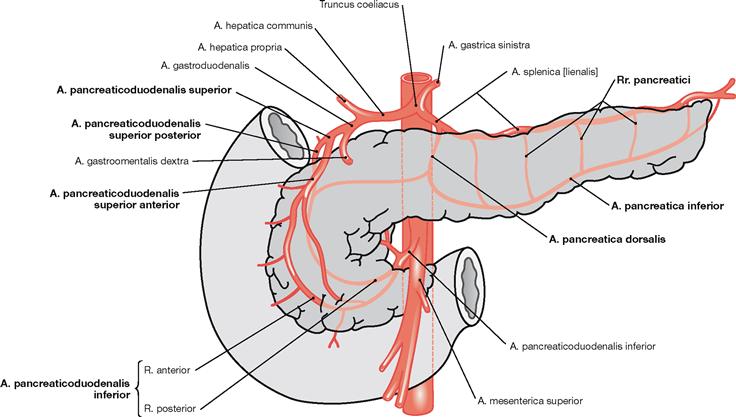
Fig. 6.92 Arteries of the pancreas, Pancreas; schematic illustration. (according to [1])
The Pancreas is supplied by two separate arterial systems for the pancreatic head, and the pancreatic body and tail, respectively.
• head: double arterial arches from the Aa. pancreaticoduodenales superiores anterior and posterior (from the A. gastroduodenalis) and from the A. pancreaticoduodenalis inferior with a R. anterior and a R. posterior (from the A. mesenterica superior).
• body and tail: Rr. pancreatici from the A. splenica which give rise to an A. pancreatica dorsalis behind the Pancreas and an A. pancreatica inferior at the inferior border of the gland.
This extensive perfusion of the gland may explain why infarction of the Pancreas is rare.
The veins of the Pancreas correspond to the arteries and drain via the V. mesenterica superior and the V. splenica into the portal vein (→ Fig. 6.69).
Lymph vessels of the pancreas
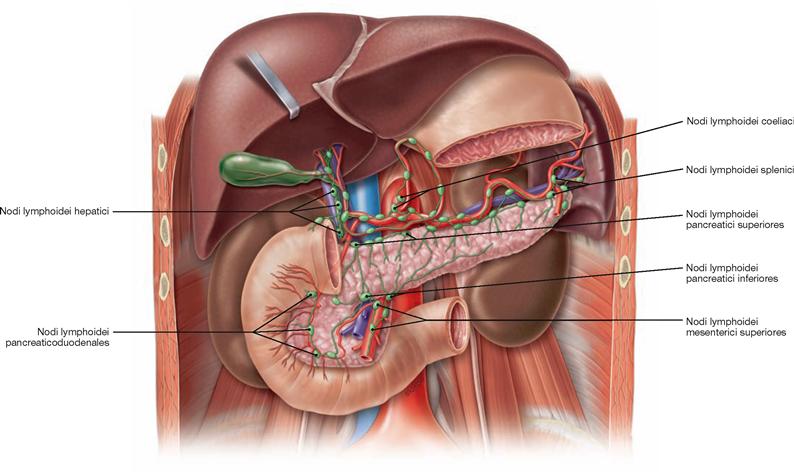
Fig. 6.93 Lymphatic drainage pathways of the pancreas, Pancreas; ventral view.
The distinct parts of the pancreas have separate regional lymph nodes.
• head: Nodi lymphoidei pancreaticoduodenales anteriores and posteriores along the identically named arteries (Aa. pancreaticoduodenales superiores anterior and posterior), then via Nodi lymphoidei hepatici to the Nodi lymphoidei coeliaci or directly to the Nodi lymphoidei mesenterici superiores and finally to the Truncus intestinalis
• body: Nodi lymphoidei pancreatici superiores and inferiores along the A. and V. splenica; from there to the Nodi lymphoidei coeliaci and to the Nodi lymphoidei mesenterici superiores. There are also connections to the retroperitoneal Nodi lymphoidei lumbales.
Pancreas, imaging
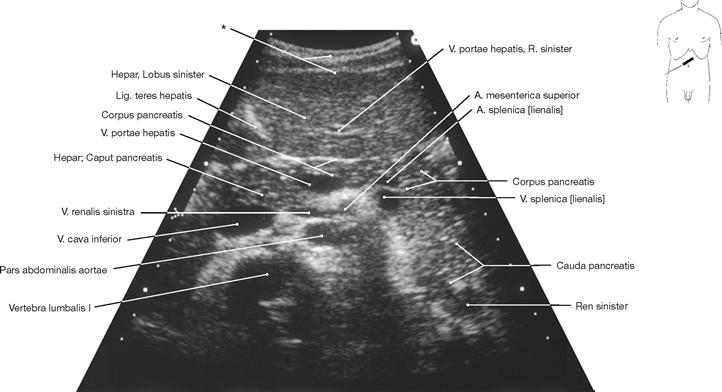
Fig. 6.94 Pancreas, Pancreas; ultrasound image; oblique caudal view in deep inspiration.
The ultrasonic examination of the Pancreas frequently is unsatisfactory as the retroperitoneal Pancreas is usually obscured by air-filled bowels
* abdominal wall
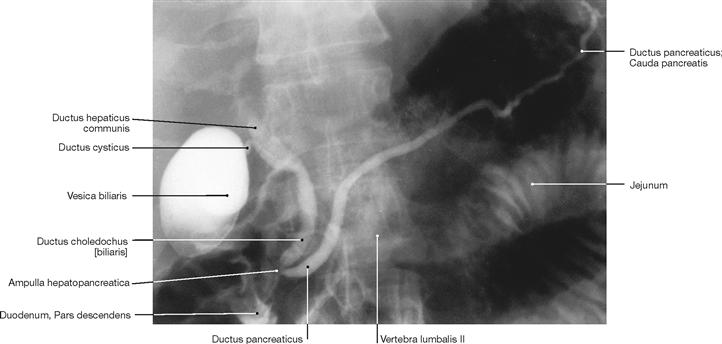
Fig. 6.95 Pancreas, Pancreas, and bile ducts; endoscopic retrograde cholangiopancreatography (ERCP); ventral view.
To visualise the duct systems in the radiograph, the excretory duct of
the Pancreas and the Ductus choledochus were filled with contrast medium from the Papilla duodeni major via an endoscope.
Projection of the spleen
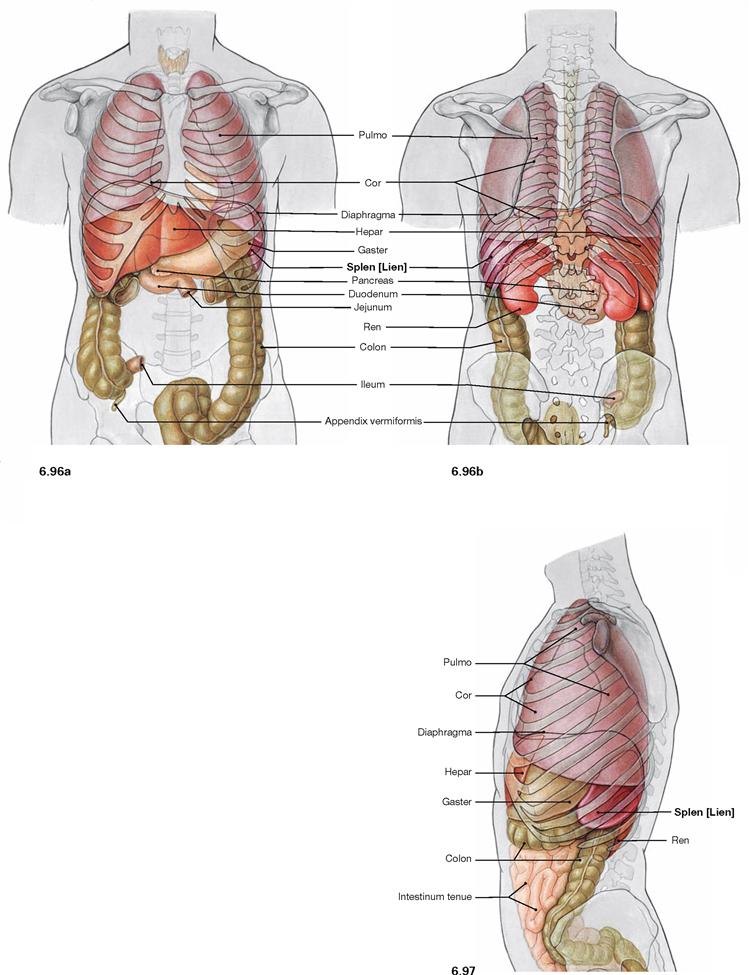
Fig. 6.96 and Fig. 6.97 Projection of the viscera onto the body surface; ventral (→ Fig. 6.96a) and dorsal (→ Fig. 6.96b) views, and view from the left side (→ Fig. 6.97).
The spleen is located intraperitoneally in the left epigastrium. Its longitudinal axis projects onto rib X. A normal-sized spleen is not palpable beyond the costal margin. Due to its large contact area with the diaphragm, the position of the spleen is dependent on respiration. The spleen lies in the so-called splenic niche which is confined inferiorly by the Lig. phrenicocolicum between the left colic flexure and diaphragm (→ Fig. 6.102).
Spleen
Structure of the spleen
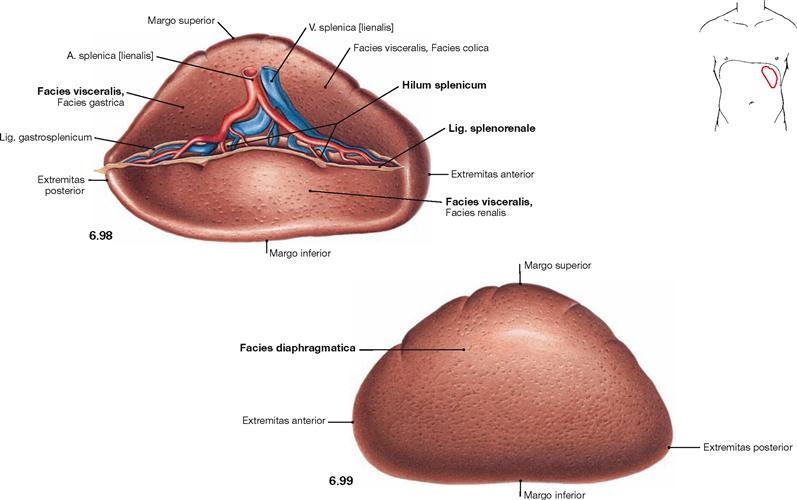
Fig. 6.98 and Fig. 6.99 Spleen, Splen [Lien]; medial ventral (→ Fig. 6.98) and lateral cranial (→ Fig. 6.99) views.
The spleen is a secondary lymphatic organ and plays a role in the immune system as well as in filtering of the blood. The spleen weighs 150 g, is 11 cm long, 7 cm wide and 4 cm high. Its convex side, Facies diaphragmatica, is adjacent to the diaphragm, its concave side, Facies visceralis, is facing the abdominal viscera, especially the left kidney, the left colic flexure, and the stomach. The superior border (Margo superior) shows indentations, whereas the inferior border (Margo inferior) is rather smooth. The blood vessels enter and exit at the splenic hilum (Hilum splenicum). The branching pattern of the blood vessels reflects the segmentation of the spleen, although the segments can not be identified at the surface. The spleen is anchored to the surroundings by two peritoneal duplicatures, both of which insert at the splenic hilum. The Lig. gastrosplenicum connects the spleen to the stomach and continues as Lig. splenorenale to the posterior wall of the trunk.
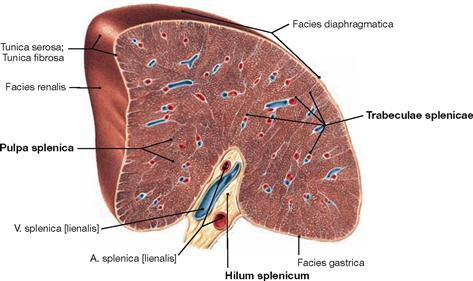
Fig. 6.100 Spleen, Splen [Lien]; cross-section through the hilum; medial cranial view.
The spleen is covered by a firm capsule which projects trabeculations of connective tissue towards the centre of the parenchyma (Pulpa splenica). Embedded within these trabeculae are the larger branches of the A. and V. splenica. The splenic pulp consists of the blood-filled red pulp and disseminated “white” nodules which are collectively referred to as white pulp. The white pulp contains lymphatic tissue.
Greater omentum
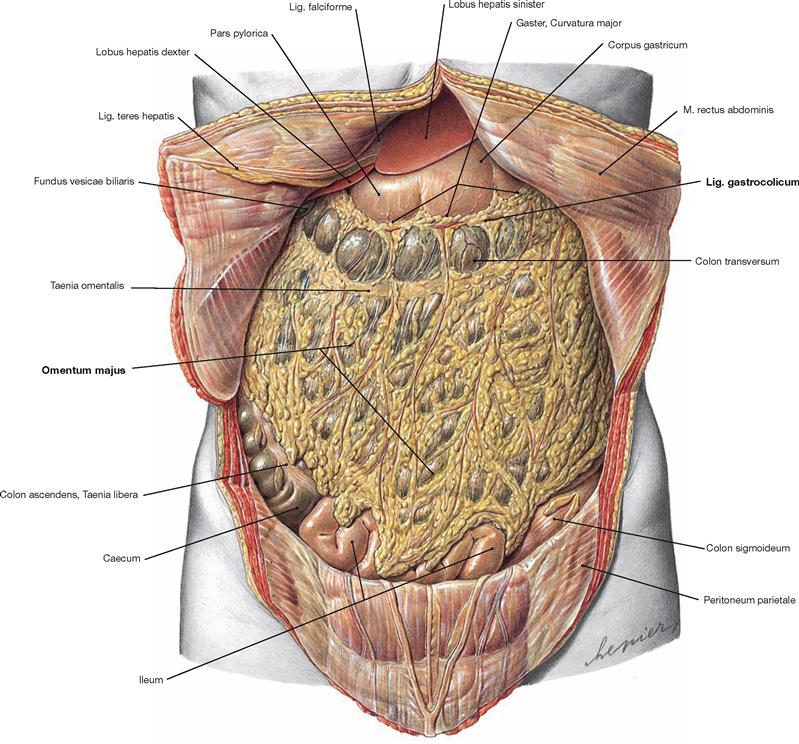
Fig. 6.101 Position of the viscera, Situs viscerum, in the Epigastrium and the greater omentum, Omentum majus; ventral view.
The abdominal cavity is opened and the Umbilicus was cut from the left side to preserve the Lig. teres hepatis between the liver and the ventral abdominal wall. The horizontal Colon transversum divides the abdomen in epigastrium and hypogastrium. The viscera of the lower abdomen are almost completely covered by the greater omentum which is attached to the greater curvature of the stomach. The Omentum is associated with the Epigastrium because its blood supply is derived from the vessels of the greater curvature of the stomach (Rr. omentales of the Aa. gastroomentales; → Fig. 6.116). The Omentum majus is a peritoneal duplicature composed of the Lig. gas-trocolicum, the Lig. gastrosplenicum and a free apron-like portion. The greater omentum plays a role not only in the mechanical protection and thermal insulation but also in the secretion and absorption of peritoneal fluids. It also contains lymphatic tissue and has immunological functions.
Topography
Epigastrium
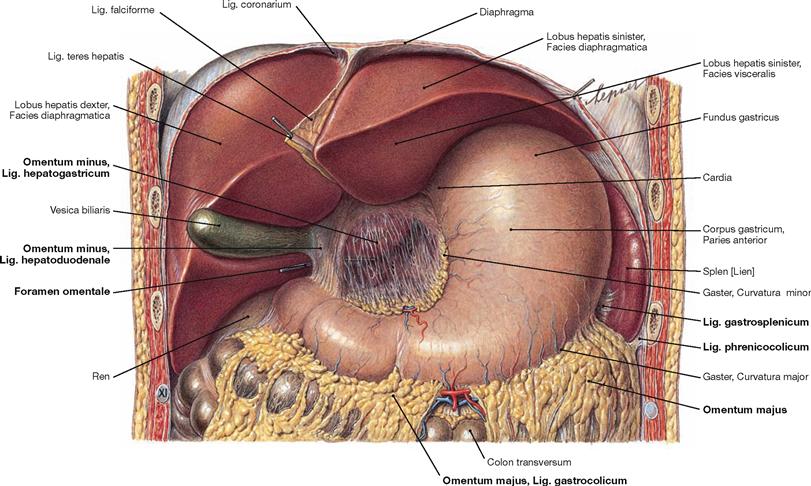
Fig. 6.102 Position of the viscera, Situs viscerum, in the Epigastrium; ventral view.
The liver was reflected cranially to visualise the lesser omentum (Omentum minus). It spans between the liver and the lesser curvature of the stomach and the Pars superior of the Duodenum. The Omentum minus consists of the Lig. hepatogastricum and the Lig. hepatoduodenale. The latter guides the common bile duct (Ductus choledochus), the portal vein (V. portae hepatis), and the A. hepatica propria to the Porta hepatis (the hilum of the liver). Behind the Lig. hepatoduodenale is the entrance to the Bursa omentalis (Foramen omentale, marked here by a probe), a sliding space between stomach and pancreas anteriorly confined by the Omentum minus.
The Omentum majus is attached to the greater curvature of the stomach and to the Taenia omentalis of the transverse colon. It is subdivided into the Lig. gastrocolicum (to the Colon transversum) and the Lig. gastrosplenicum (to the spleen). The spleen resides in the splenic niche and rests on the Lig. phrenicocolicum between the left colic flexure and diaphragm.
Epigastrium with Bursa omentalis
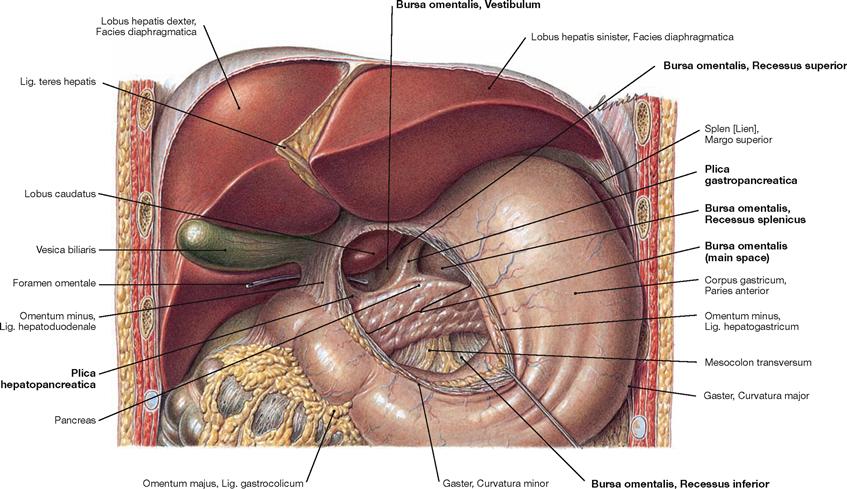
Fig. 6.103 Position of the viscera, Situs viscerum, in the Epigastrium; ventral view.
The lesser omentum (Omentum minus) between the liver and the lesser curvature of the stomach was separated to show the Bursa omentalis.
The Bursa omentalis is a sliding space between stomach and Pancreas and exclusively communicates with the abdominal cavity through the Foramen omentale behind the Lig. hepatoduodenale. Due to its confined position, the Bursa omentalis is also referred to as the “lesser sac of the peritoneal cavity”.
The Bursa omentalis is subdivided into four parts:
• Foramen omentale: The entrance to the Bursa omentalis is confined anteriorly by the Lig. hepatoduodenale, cranially by the Lobus caudatus, caudally by the Bulbus duodeni, and posteriorly by the V. cava inferior.
• Vestibulum: The vestibule is confined by the Omentum minus ventrally and its Recessus superior extends behind the liver.
• Isthmus: The narrowing between vestibule and main space is confined by two peritoneal folds: on the right side by the Plica hepatopancreatica which is created by the A. hepatica communis, and on the left side by the Plica gastropancreatica which marks the course of the A. gastrica sinistra.
• Main space: This space is located between the stomach (anterior) and the Pancreas and the Mesocolon transversum (posterior), respectively. On the left side, the Recessus splenicus extends to the hilum of the spleen; the Recessus inferior lies behind the Lig. gastrocolicum and extends to the origin of the Mesocolon at the Colon transversum.
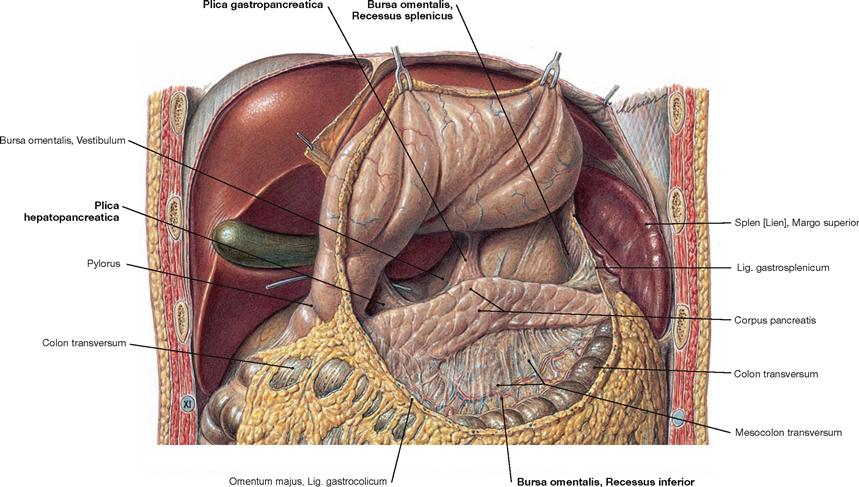
Fig. 6.104 Position of the viscera, Situs viscerum, in the Epigastrium; ventral view.
The Lig. gastrocolicum was sectioned and the stomach reflected cranially to show the main space of the Bursa omentalis. The posterior wall of the bursa is created by the Pancreas and the Mesocolon transversum. On the left side, it extends to the hilum of the spleen (Recessus splenicus), inferiorly to the origin of the Mesocolon at the Colon transversum (Recessus inferior).
Viscera of the Abdomen
Hypogastricum
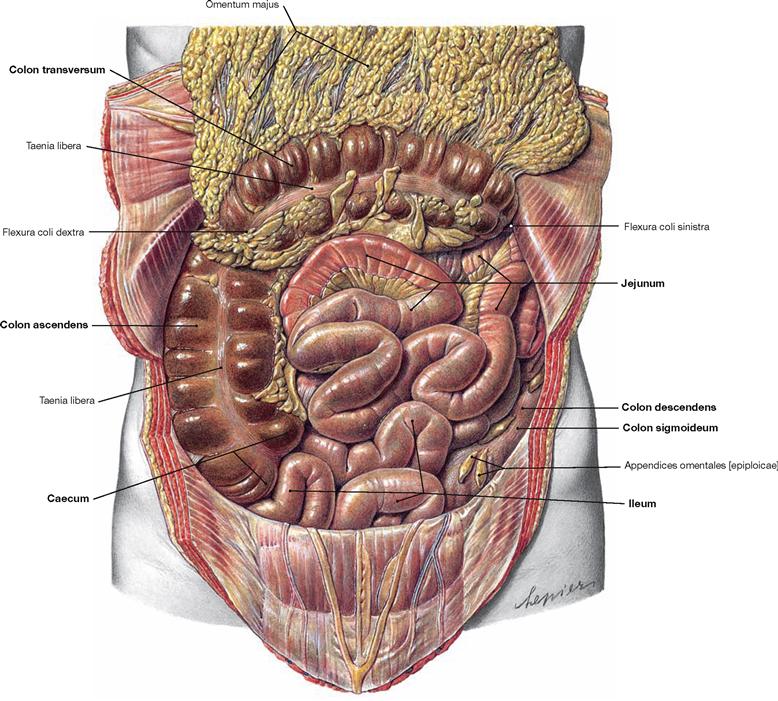
Fig. 6.105 Position of the viscera, Situs viscerum, in the Hypogastrium; ventral view.
The Omentum majus was reflected cranially to visualise the small and large intestines in the Hypogastrium. Thus, the intraperitoneal segments are visible: Jejunum and Ileum of the small intestine, Caecum, Colon transversum, and Colon sigmoideum of the large intestine. This figure also shows that the retroperitoneal segments of the colon are relocated to the posterior wall of the abdomen to a variable extent. In this case, the Colon ascendens is clearly visible, but the Colon descendens is shifted further dorsally and is partially covered by the small intestine. The large intestine frames the convolute of Jejunum and Ileum.
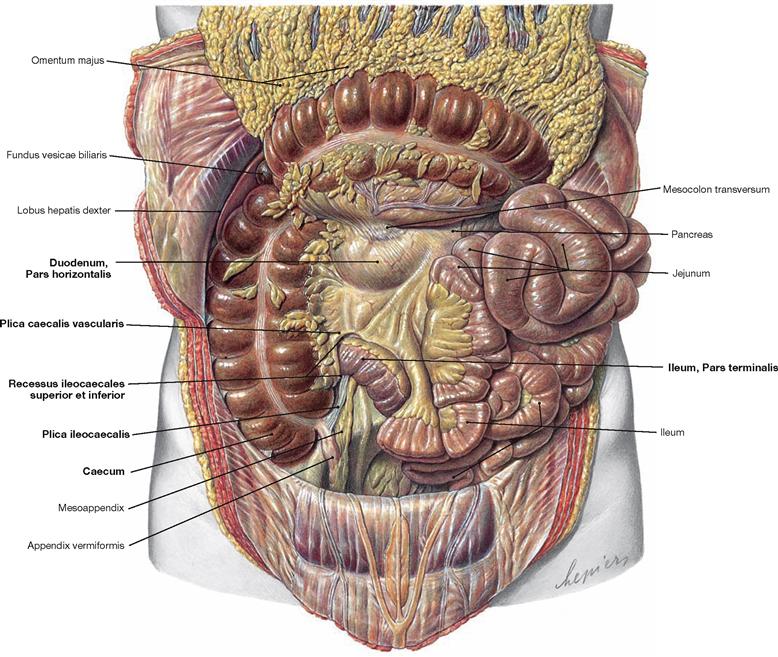
Fig. 6.106 Position of the viscera, Situs viscerum, in the Hypogastrium; ventral view.
The Omentum majus was reflected cranially and the loops of the small intestine were reflected to the left side to visualise the secondary retroperitoneal Pars horizontalis of the Duodenum. At the transition between the Ileum and the Caecum there are two spaces: the Recessus ileocaecalis superior is covered by the Plica caecalis vascularis (contains a branch of the A. ileocolica), the Recessus ileocaecalis inferior is covered by the Plica ileocaecalis between the Ileum and the Appendix vermiformis. Similar to the Bursa omentalis and other abdominal recessus, small intestinal loops may be trapped here (internal hernias).
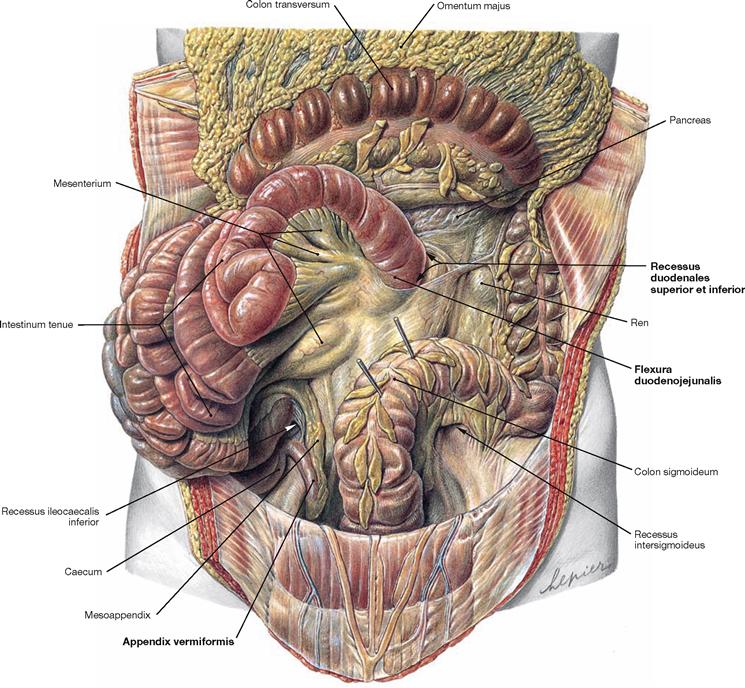
Fig. 6.107 Position of the viscera, Situs viscerum, in the Hypogastrium; ventral view.
The Omentum majus was reflected cranially and the loops of the small intestine were reflected to the right side to demonstrate the Flexura duodenojejunalis which marks the transition of the retroperitoneal Duodenum into the intraperitoneal Jejunum. This area also contains two recesses: Recessus duodenales superior and inferior. In the right Hypogastrium, the Appendix vermiformis is visible, the tip of which descends into the small pelvis (descending type).
Mesenteries
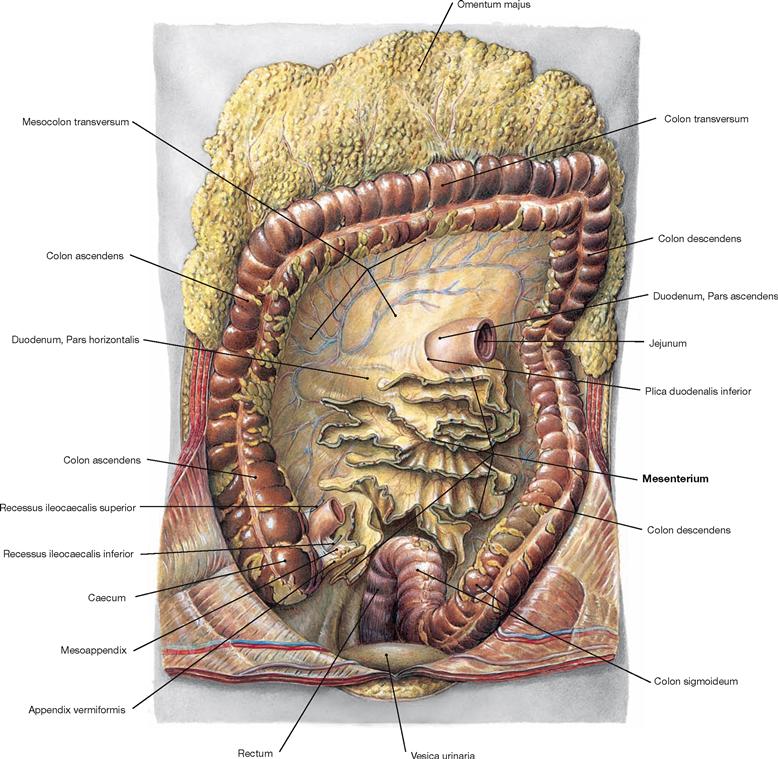
Fig. 6.108 Mesenteries of the small intestine, Mesenterium, and large intestine, Intestinum crassum; ventral view.
The Omentum majus and the Colon transversum were reflected cranially. The intraperitoneal small intestinal convolute of Jejunum and Ileum was resected at the mesentery. The mesentery consists of a duplicature of the peritoneal membranes, contains the neurovascular structures to supply the small intestine, and serves as mobile attachment of the small intestine to the posterior abdominal wall.
Secondary retroperitoneal organs
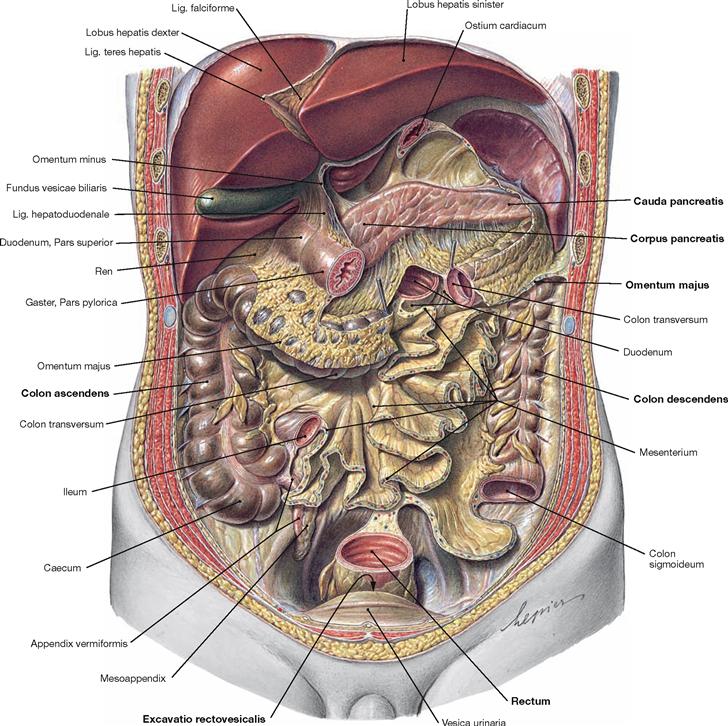
Fig. 6.109 Position of the secondary retroperitoneal organs; ventral view.
The stomach was removed, Jejunum and Ileum were resected at the mesentery, and Colon transversum and Colon sigmoideum were sectioned. Most of the secondary retroperitoneal organs are now visible. These include the Duodenum (except for the Pars superior), the Pancreas, the Colon ascendens, and the Colon descendens, and the Rectum to the Flexura sacralis. Anterior to the Rectum, the opening of the Excavatio rectovesicalis can be seen. This peritoneal pouch is the most inferior part of the peritoneal cavity in men.
Posterior wall of the peritoneal cavity
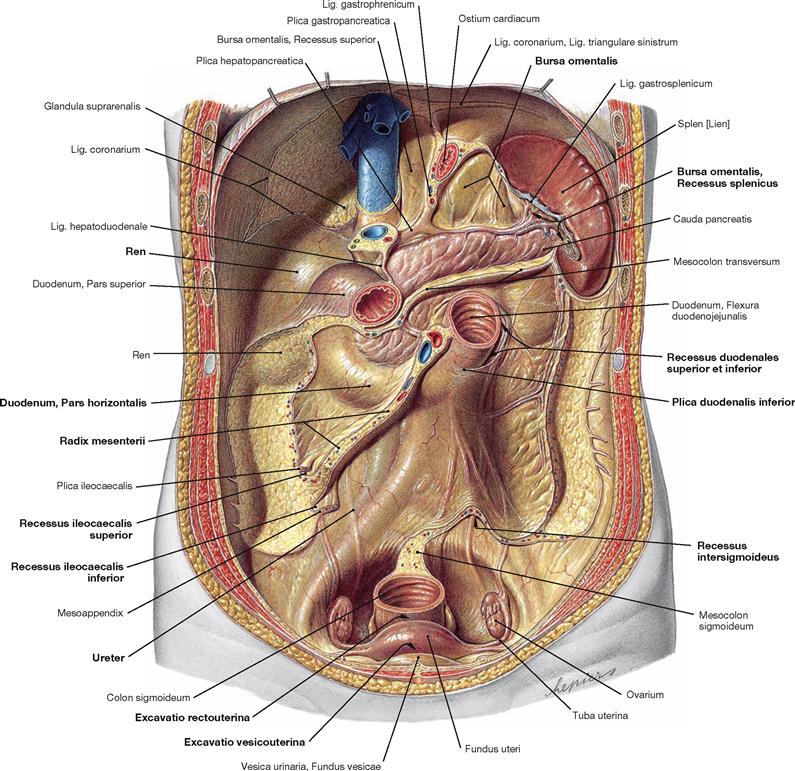
Fig. 6.110 Dorsal wall of the peritoneal cavity, Cavitas peritonealis, with recesses, Recessus, and spleen, Splen [Lien]; ventral view.
Liver, small and large intestines were removed except for the Duodenum to expose the dorsal wall of the peritoneal cavity. The peritoneal lining over the right kidney and the Pars descendens of the Duodenum is clearly visible due to its shiny surface. The attachment areas of the secondary retroperitoneal Colon ascendens and Colon descendens are lacking this peritoneal lining.
The peritoneal duplicatures form the relief of the dorsal wall of the peritoneal cavity as folds (Plicae) and ligaments and create diverse recesses (Recessus). The largest of them is the Bursa omentalis (→ Fig. 6.103), the portions and extensions thereof are visible here. At the area of the Flexura duodenojejunalis, the Plicae duodenales superior and inferior form two recesses (Recessus duodenales superior and inferior). Further recesses (peritoneal gutters) are located at the entrance of the terminal ileum into the Caecum (Recessus iliocaecales superior and inferior) and occasionally another recess is located inferior to the Mesocolon sigmoideum (Recessus intersigmoideus).
Anterior to the rectum, a deep peritoneal space exists which is confined by the uterus and the broad ligament at the ventral side. This Excavatio rectouterina (pouch of DOUGLAS) is the most caudal recess of the peritoneal cavity in women. The ventrally positioned Excavatio vesicouterina between urinary bladder and Uterus does not extend downwards as deeply as the Excavatio rectouterina. Between the Flexura duodenojejunalis and the right Fossa iliaca, the 12–16 cm long root of the mesentery (Radix mesenterii) is attached. It contains the blood vessels supplying the small intestine (A./V. mesenterica superior). The root of the mesentery traverses the Pars horizontalis of the Duodenum and the right Ureter.
Arteries of the abdomen
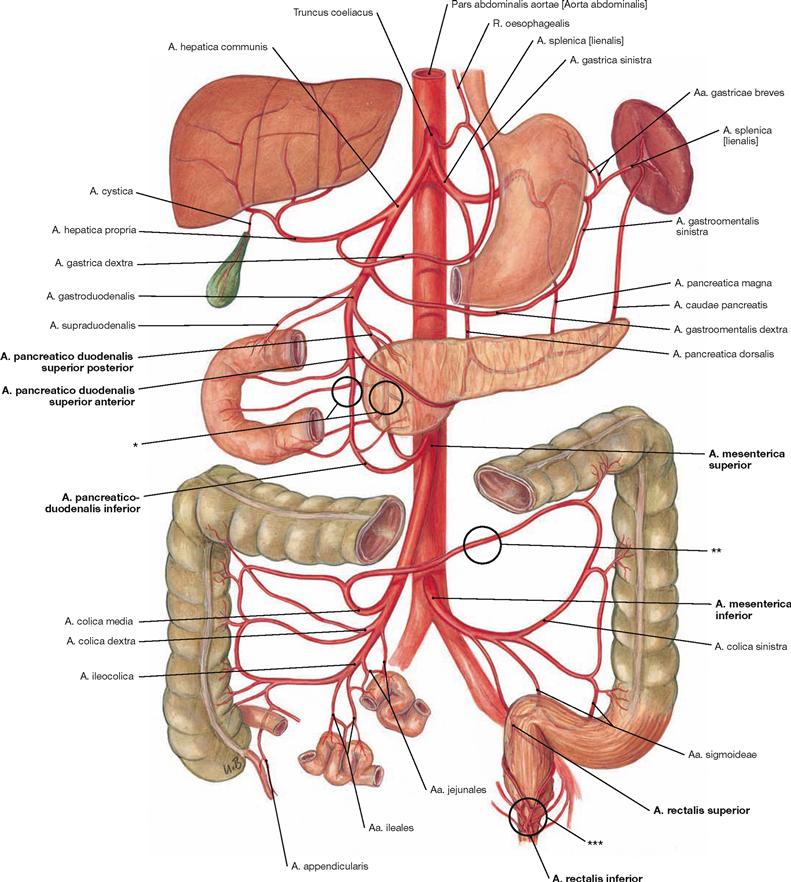
Fig. 6.111 Arteries of the abdominal viscera; semischematic illustration; ventral view.
The most important anastomoses are marked by black circles. The three unpaired arteries to the abdominal viscera derived from the Aorta abdominalis are the Truncus coeliacus, the A. mesenterica superior, and the A. mesenterica inferior. The A. mesenterica superior has its origin directly below the Truncus coeliacus (here not shown due to semischematic presentation). Its respective branches are described on the following pages. All three arteries anastomose with each other and with branches of the A. iliaca interna. This may prevent ischemic infarction in cases of an occlusion of one of these vessels.
The anastomoses are:
• connections between the Truncus coeliacus and the A. mesenterica superior via Aa. pancreaticoduodenales (*).
• connections between the Aa. mesentericae superior and inferior: RIOLAN’s anastomosis between the A. colica media and A. colica sinistra (**).
• Plexus of rectal arteries: here the A. rectalis superior from the A. mesenterica inferior connects to the Aa. rectales media and inferior from the A. iliaca interna (***).
Veins of the abdomen
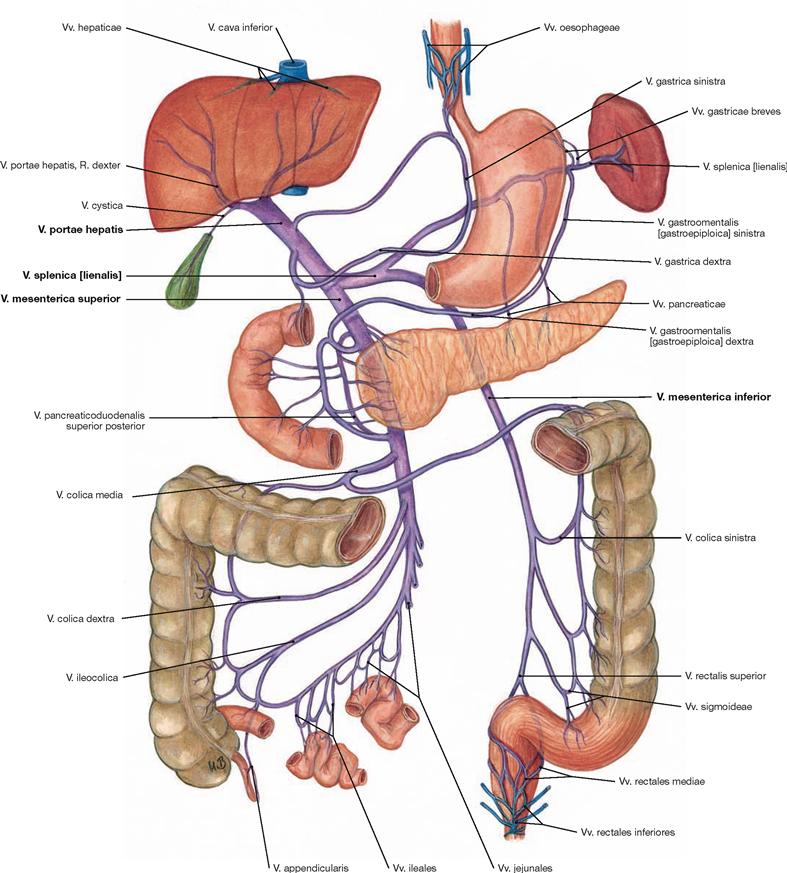
Fig. 6.112 Portal vein, V. portae hepatis, with tributaries; semischematic illustration; ventral view.
The tributaries of the portal vein are described in detail in → Figure 6.69.
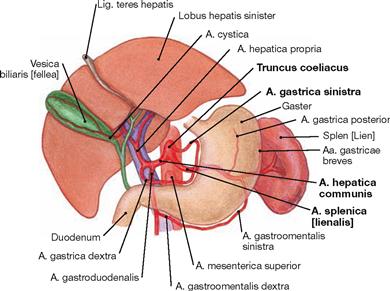
Truncus coeliacus
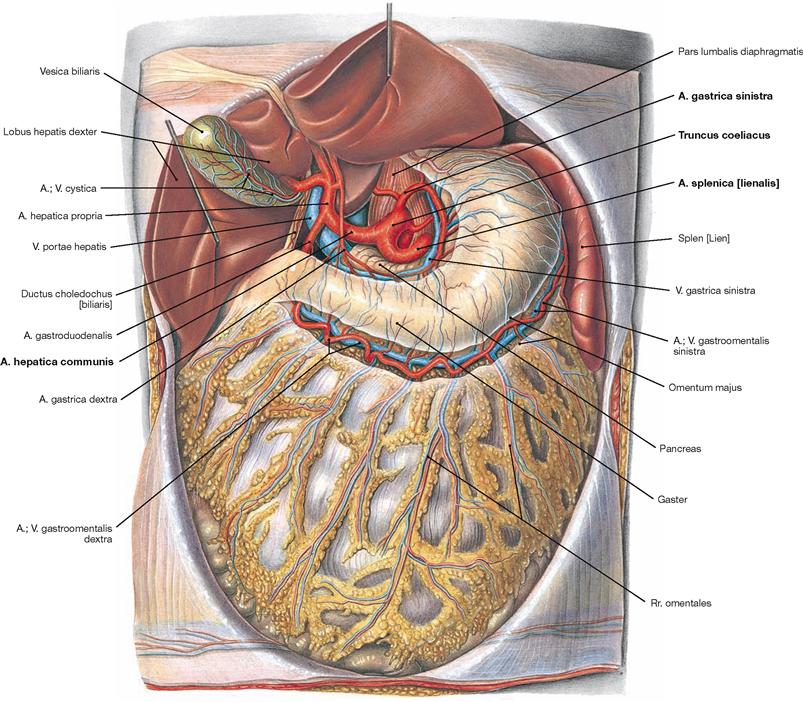
Fig. 6.113 Truncus coeliacus; ventral view; after removal of the Omentum minus.
The Truncus coeliacus derives as first unpaired branch from the Aorta abdominalis. In the retroperitoneal space behind the Bursa omentalis its short (mostly 2–3 cm) trunk divides into the three major arteries which supply the viscera of the Epigastrium (Gaster, Duodenum, Hepar, Vesica biliaris, Pancreas and Splen):
• A. gastrica sinistra: branches off to the left and superior side. It anastomoses with the A. gastrica dextra at the lesser curvature of the stomach and is usually the stronger vessel.
• A. hepatica communis: turns to the right side and divides into:
– A. hepatica propria: releases the A. gastrica dextra and supplies liver and gallbladder (A. cystica)
– A. gastroduodenalis: descends behind the Pylorus or Duodenum, divides into the A. gastroomentalis dextra to the greater curvature of the stomach and the Aa. pancreaticoduodenales superiores anterior and posterior which anastomose with the A. pancreaticoduodenalis inferior from the A. mesenterica superior to supply the head of the Pancreas and the Duodenum.
• A. splenica: courses to the inferior left side at the superior border of the Pancreas and releases the following branches during its course to the spleen:
– Rr. pancreatici for the Pancreas
– A. gastrica posterior to the stomach (30–60% of all cases)
– A. gastroomentalis sinistra: courses from the left side to the greater curvature of the stomach and anastomoses with the A. gastroomentalis dextra
– Aa. gastrici breves: short branches to the fundus of the stomach
A. mesenterica superior
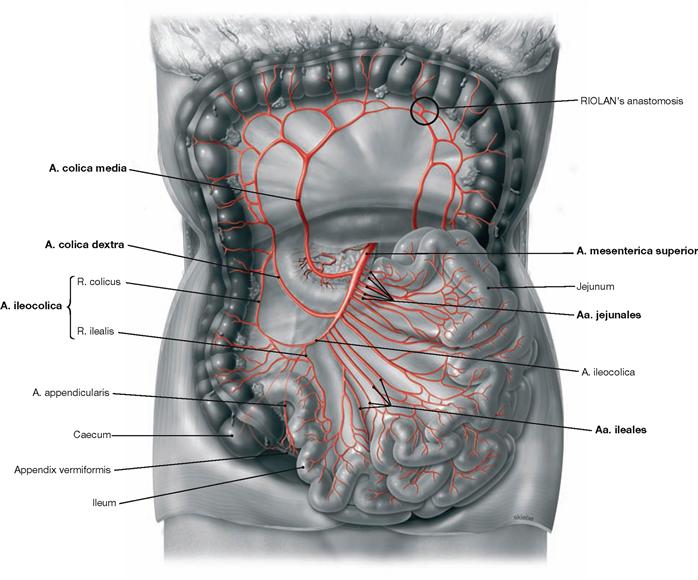
Fig. 6.115 A. mesenterica superior; ventral view; Colon transversum reflected cranially. (according to [1])
The unpaired A. mesenterica superior branches off the Aorta abdominalis directly below the Truncus coeliacus, courses retroperitoneally behind the Pancreas and then enters the mesentery. Its branches can be displayed if the mesentery is opened and the adipose tissue between the vascular arcades is removed. It supplies parts of the Pancreas and Duodenum, the entire small intestine, and the large intestine up to the left colic flexure.
Branches of the A. mesenterica superior:
• A. pancreaticoduodenalis inferior: branches off to the superior right side; R. anterior and R. posterior anastomose with the Aa. pancreaticoduodenales superiores anterior and posterior (→ Fig. 6.116).
• Aa. jejunales (4–5) and Aa. ileales (12): directed to the left side
• A. colica media: originates on the right side and anastomoses with the A. colica dextra and with the A. colica sinistra (RIOLAN’s anastomosis)
• A. colica dextra: courses to the Colon ascendens
• A. ileocolica: supplies the distal Ileum, Caecum and Appendix vermiformis (A. appendicularis)
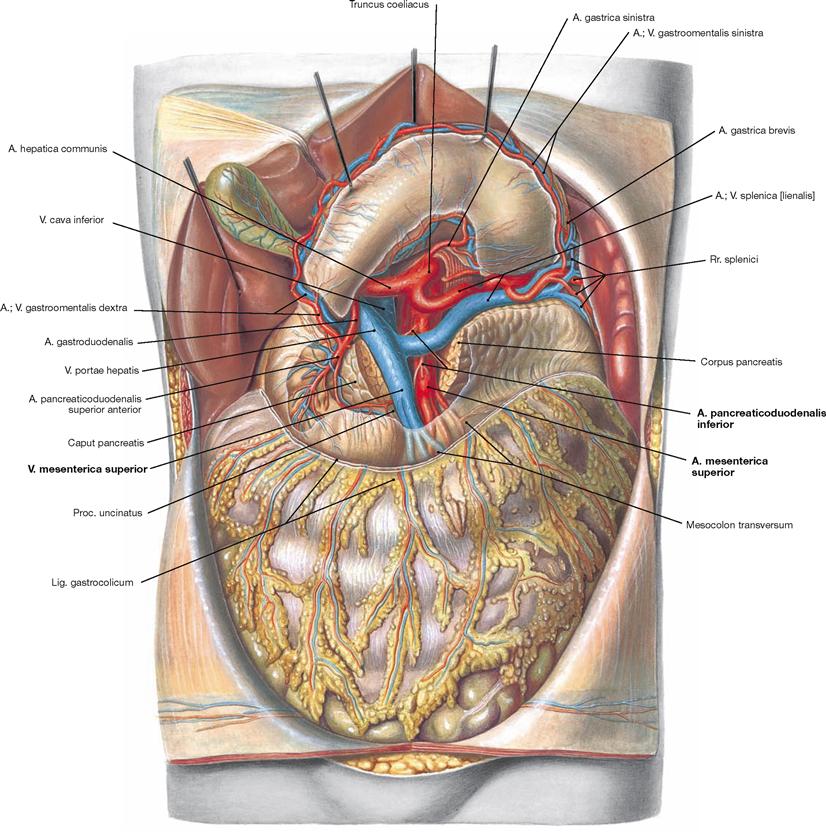
Fig. 6.116 Origins of the A. mesenterica superior and Truncus coeliacus; ventral view; after reflecting the stomach cranially and dissecting the Pancreas.
Following its origin from the Aorta abdominalis inferior to the Truncus coeliacus, the A. mesenterica superior descends behind the Pancreas and enters the mesentery anterior to the Duodenum. The Pancreas was sectioned to show the A. and V. mesenterica superior ventral to the Proc. uncinatus of the Pancreas. The A. mesenterica superior supplies the A. pancreaticoduodenalis inferior as its first branch to the right side.
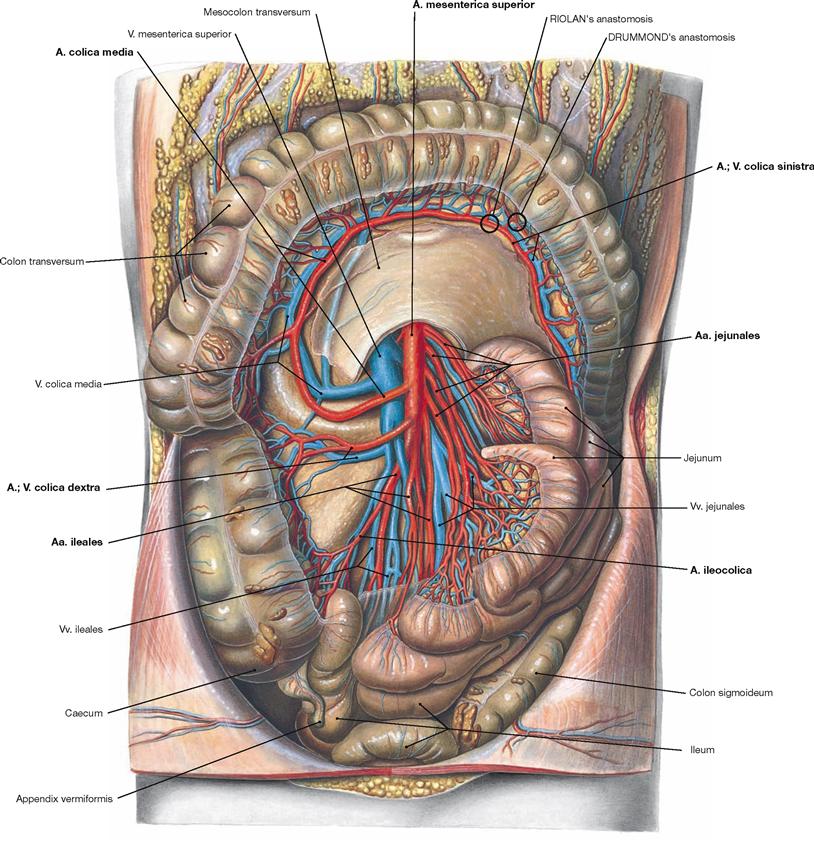
Fig. 6.117 Course of the A. and V. mesenterica superior; ventral view; after opening of the mesentery with the Colon transversum reflected cranially.
Within the mesentery, the A. mesenterica superior gives rise to the following branches: Aa. jejunales and Aa. ileales to the left side, A. colica media, A. colica dextra, and A. ileocolica to the right side. All arteries form arcades at different levels of their divisions. This allows the mobility of the intestinal loops. At the left colic flexure, the A. colica media forms a functionally important anastomosis (RIOLAN’s anastomosis) with the A. colica sinistra from the A. mesenterica inferior. This facilitates the formation of collateral circulations in the case of occlusion of one of the arteries. The anastomosis between the two arteries in one of the arcades close to the intestines is occasionally referred to as DRUMMOND’s anastomosis. In the clinical jargon, all anastomoses in the area of the left colic flexure are summarised as RIOLAN’s anastomosis.
The venous branches correspond to the arteries.
A. mesenterica inferior
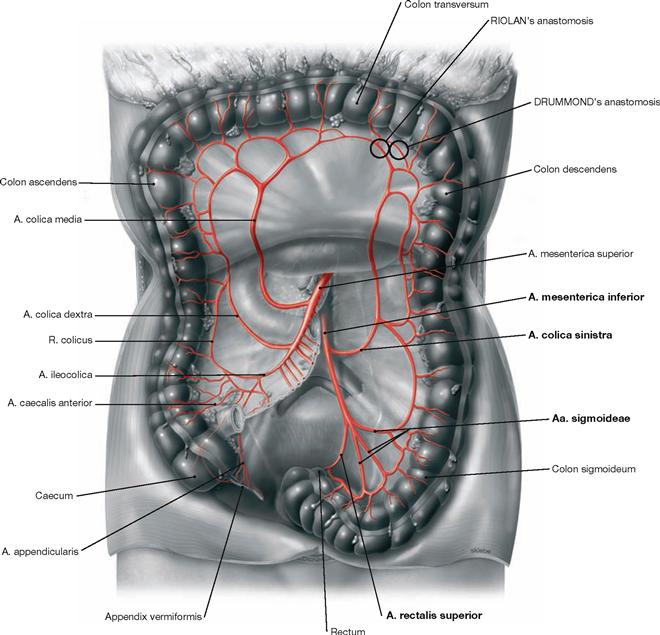
Fig. 6.118 A. mesenterica inferior; ventral view; Colon transversum reflected cranially. (according to [1])
The unpaired A. mesenterica inferior branches off the abdominal aorta approximately 5 cm above its bifurcation and turns to the left side. With the exception of a short terminal section, the A. mesenterica inferior descends into the retroperitoneal space to supply the Colon descendens and the upper Rectum.
Branches of the A. mesenterica inferior:
• A. colica sinistra: ascends along the Colon descendens and anastomoses via the A. colica sinistra with the A. colica media from the A. mesenterica superior (RIOLAN’s anastomosis)
• Aa. sigmoideae: several branches to the Colon sigmoideum
• A. rectalis superior: descends to the upper Rectum and supplies the rectal cavernous bodies in the submucosa (Corpus cavernosum recti) which are a part of the continence mechanism.
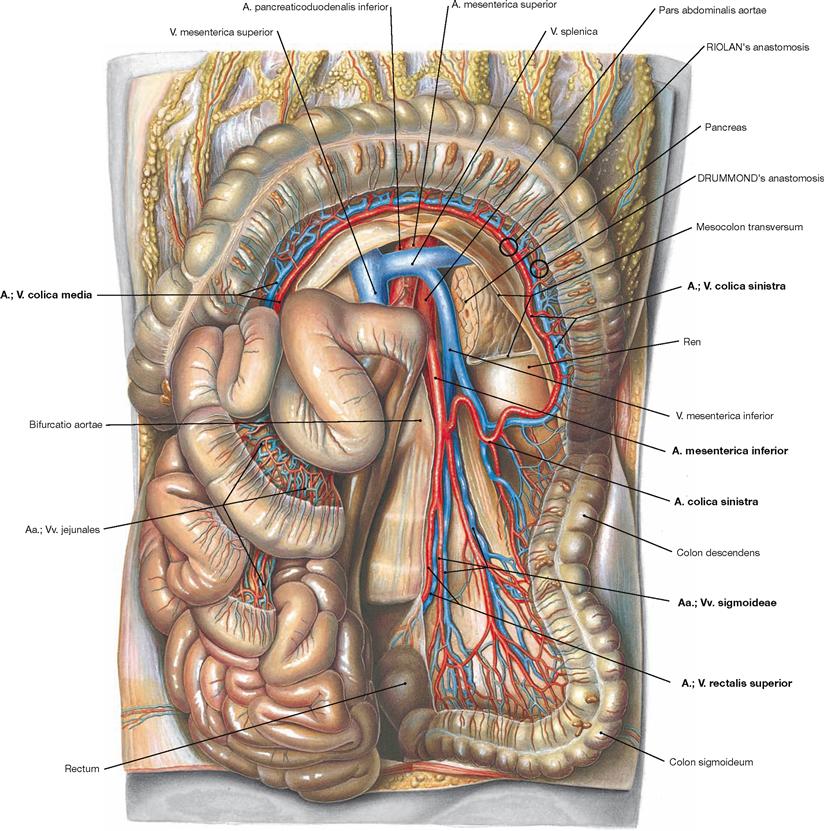
Fig. 6.119 Course of the A. and V. mesenterica inferior in the retroperitoneal space; ventral view; Colon transversum reflected cranially and small intestinal loops to the right side.
Following its origin above the aortic bifurcation, the A. mesenterica inferior descends in the retroperitoneal space and releases first the A. colica sinistra to the left side, then several Aa. sigmoideae and finally the unpaired A. rectalis superior.
The A. colica sinistra ascends along the Colon descendens, forms arcades and anastomoses with the A. colica media derived from the A. mesenterica superior (RIOLAN’s anastomosis). The anastomosis between the two arteries in one of the arcades close to the intestines is occasionally referred to as DRUMMOND’s anastomosis.
Abdomen and pelvis, median section
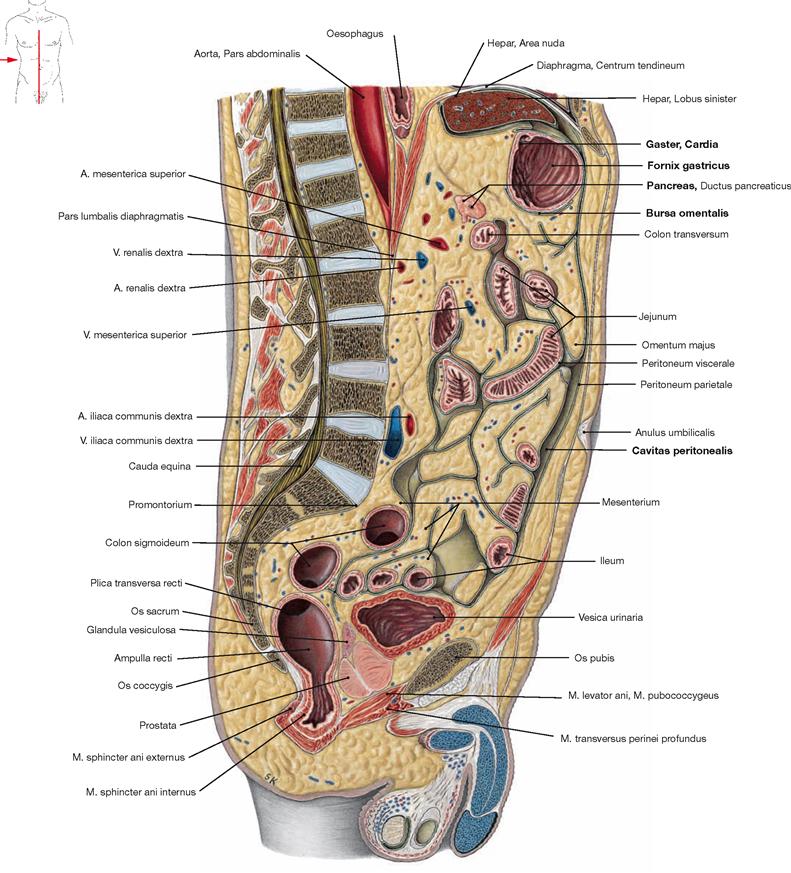
Fig. 6.120 Abdomen, Abdomen, and pelvis, Pelvis, of a man; median section; view from the right side.
This illustration shows clearly that the peritoneal cavity (Cavitas peritonealis) is not a wide empty space, but rather consists of small recesses between the intraperitoneal viscera. Also the Bursa omentalis between the stomach and the Pancreas is only a narrow space with peritoneal lining. A large portion of the abdominal cavity is occupied by the mesentery which may accumulate plenty of adipose tissue.
Abdomen and pelvis, sagittal section
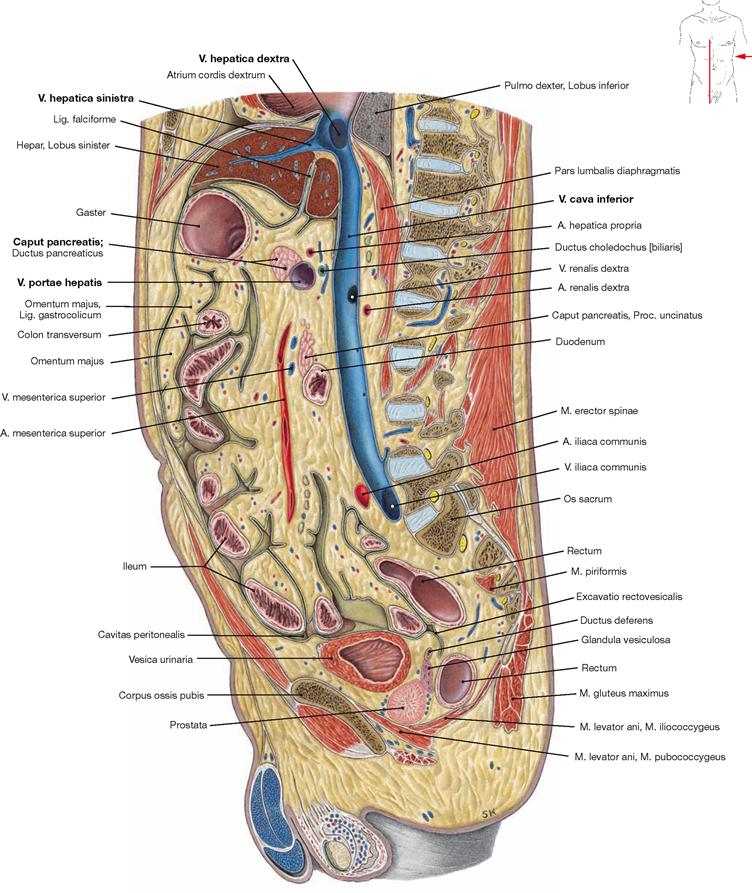
Fig. 6.121 Abdomen, Abdomen, and pelvis, Pelvis, of a man; sagittal section; view from the left side.
This is a right paramedian section at the level of the V. cava inferior. Thus, the confluence of the liver veins (Vv. hepaticae), which drain the venous blood from the liver, is clearly visible. The portal vein (V. portae hepatis), which brings the nutrient-rich blood from the unpaired viscera to the liver, arises from the confluence of the two main tributaries behind the pancreatic head.
Abdomen and pelvis, frontal section
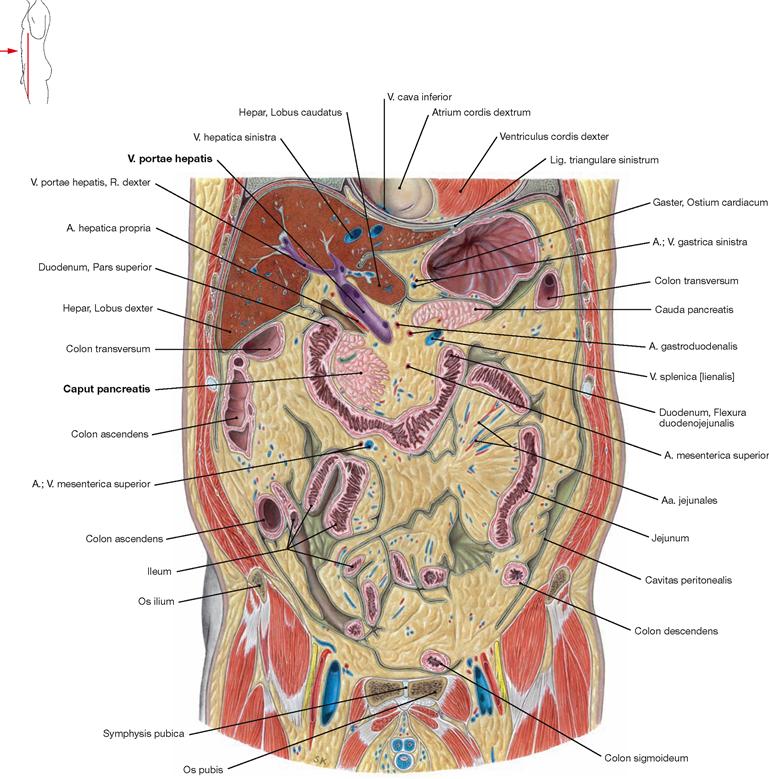
Fig. 6.122 Abdomen, Abdomen, and pelvis, Pelvis, of a man; frontal section through the anterior part; ventral view.
This is a frontal section through the portal vein (V. portae hepatis) which courses above the pancreatic head (Caput pancreatis) to the hilum of the liver and divides into a right and a left branch.
Sections
Epigastrium, frontal section
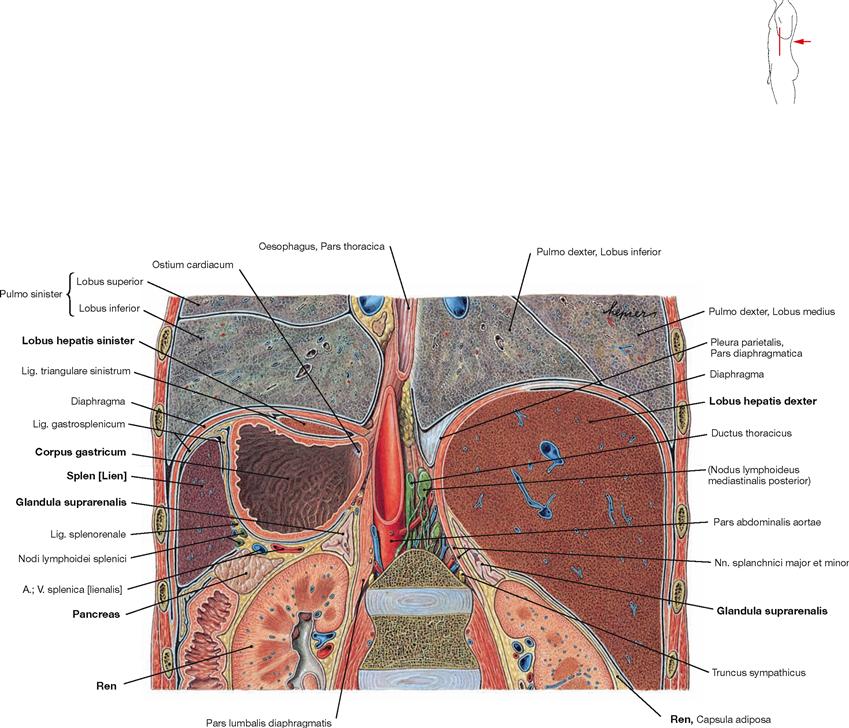
Fig. 6.123 Abdominal cavity, Cavitas abdominalis, and inferior thorax, Cavitas thoracis; frontal section at the level of the kidneys; dorsal view.
The section shows the topographical relationships of the epigastric viscera. The right Epigastrium is entirely occupied by the right lobe of the liver (Lobus hepatis dexter) which contacts the right kidney (Ren) and the right adrenal gland (Glandula suprarenalis) at its caudal aspect. On the left side, the cranial part of the left hepatic lobe covers the stomach (Gaster) which, in turn, contacts the spleen and caudally the left kidney, the left adrenal gland and the Pancreas. The pancreatic tail extends towards the spleen.
Epigastrium, sagittal section
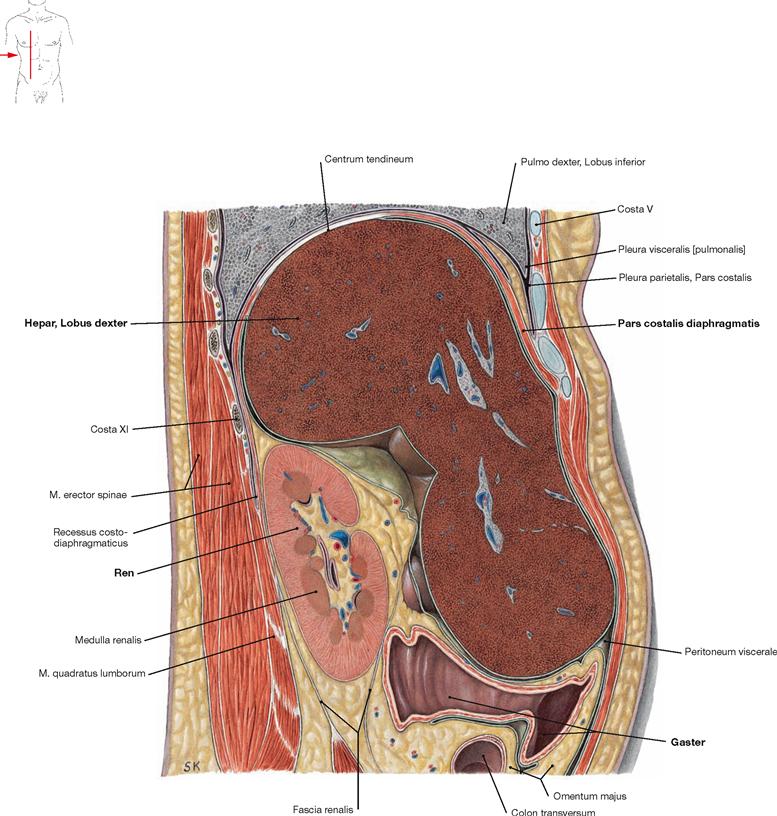
Fig. 6.124 Abdomen, Abdomen; sagittal section through the right epigastrium at the level of the kidney; view from the right side.
The right epigastrium contains the right lobe of the liver (Hepar, Lobus dexter) which has extensive contacts with the inferior aspect of the diaphragm. Dorsal and inferior to the liver, the kidney (Ren) is located in the retroperitoneal space; ventral thereof the Pass pylorica of the stomach (Gaster) is located in the intraperitoneal cavity.
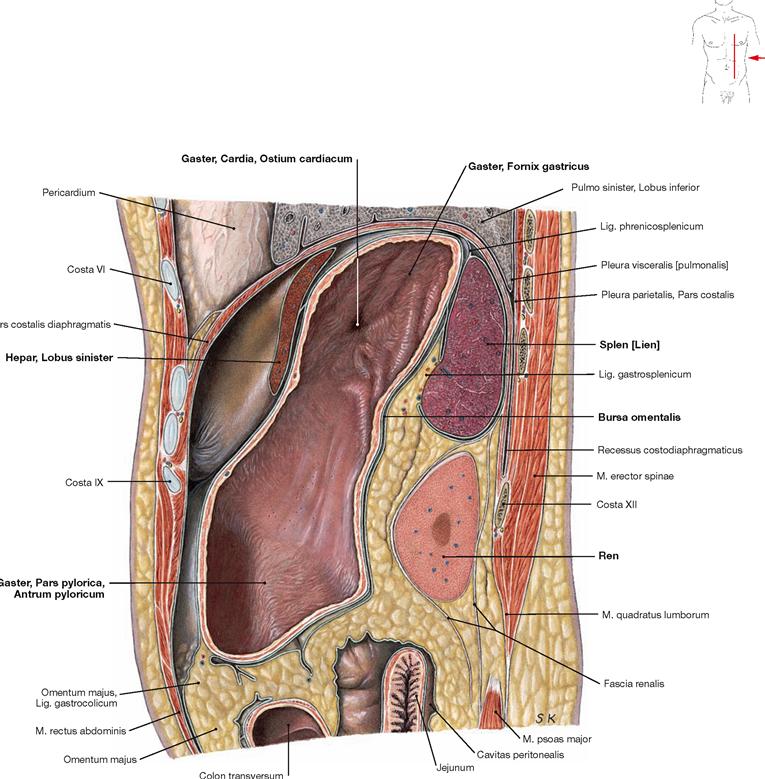
Fig. 6.125 Abdomen, Abdomen; sagittal section through the left epigastrium at the level of the spleen; view from the left side.
The stomach (Gaster) occupies the major part of the left Epigastrium. It is covered ventrally by the left lobe of the liver (Hepar, Lobus sinister) and contacts the spleen and the left kidney (Ren) at its dorsal side; the left kidney is located in the retroperitoneal space. Lined by peritoneum, the Bursa omentalis forms a small recess behind the stomach.
Epigastrium, transverse sections
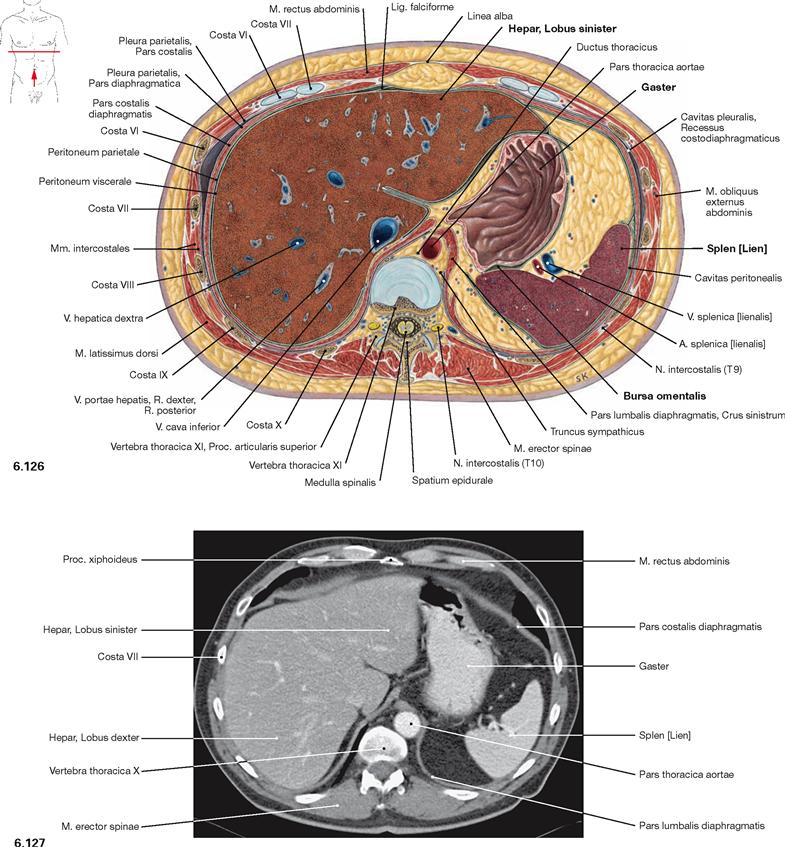
Fig. 6.126 and Fig. 6.127 Abdominal cavity, Cavitas abdominalis; transverse section at the level of the 11th thoracic vertebra (→ Fig. 6.126) and corresponding computed tomographic section (CT; → Fig. 6.127); caudal view.
The liver occupies the entire right epigastrium and with its left lobe extends to the left anterior side of the stomach (Gaster). Posterior to the stomach and lined by peritoneum is the Bursa omentalis. The spleen is cut in the left Epigastrium.
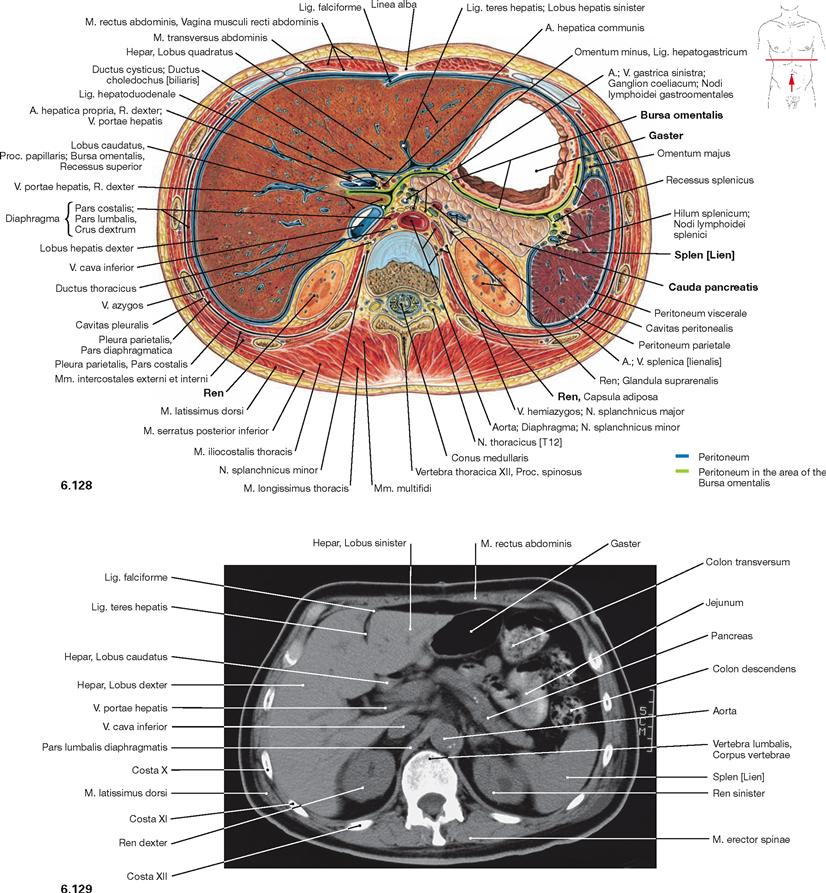
Fig. 6.128 and Fig. 6.129 Abdominal cavity, Cavitas abdominalis; transverse section at the level of the 1st lumbar vertebra (→ Fig. 6.128) and corresponding computed tomographic section (CT; → Fig. 6.129); caudal view.
At the level of the 1st lumbar vertebra, additional viscera are visible, such as the superior poles of the kidneys (Ren) and the Pancreas. The Pancreas is located posterior to the stomach, separated by the Bursa omentalis, and extends to the left side until it reaches the hilum of the spleen.
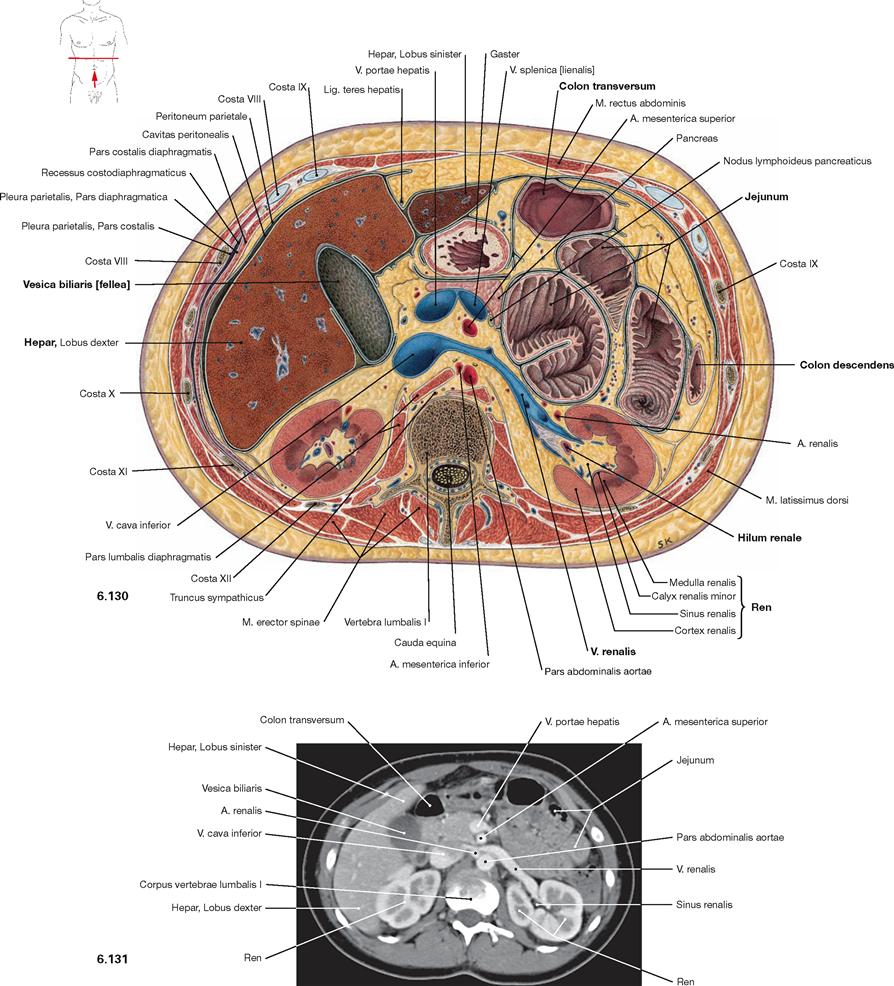
Fig. 6.130 and Fig. 6.131 Abdominal cavity, Cavitas abdominalis; transverse section at the level of the 1st lumbar vertebra (→ Fig. 6.130) and corresponding computed tomographic section (CT; → Fig. 6.131); caudal view.
Typically, the hilum of the kidney (Ren) is located at the level of the first two lumbar vertebrae (recognised by the confluence of the left V. renalis). The gallbladder (Vesica biliaris) is sectioned at the inferior border of the liver (Hepar). In the left Epigastrium, portions of the small intestinal Loops (Jejunum) and portions of the large intestine (Colon transversum and Colon descendens) are visible.