Eye
The Eye – a Window to the World
When anatomists discuss the visual organ (Organum visus), firstly they mean the eyeball (Bulbus oculi) and, secondly, the auxiliary structures in its immediate surroundings (Structurae oculi accessoriae). Except for the eyelids (Palpebrae), all auxiliary structures – including the eyeball – are enclosed within the orbit (Orbita).
Orbit
“Orbita” is certainly one of the least appropriate anatomical terms. The word is derived from the word “orbis” (circle), but a quick look at the skull confirms immediately that the outer opening of the orbit (Aditus orbitalis) is not completely circular but its contour is rather oval to round. At the nasal margin of the Aditus orbitalis, the bony structures of the nasolacrimal canal (Canalis nasolacrimalis) open towards the orbit. The walls of the orbit form a steep pyramid towards the inside of the orbit, with its upper and lower wall perforated by two large fissures (Fissurae orbitales superior and inferior) to allow many nerves and vessels to pass through. The canal for the optic nerve (Canalis nervi optici) is located at the tip of this pyramid.
Eyeball
The Bulbus oculi (lat. “bulbus”: the onion) actually resembles an onion more than a ball. One can imagine a multilayered onion sprouting at one pole and rooting at the opposite pole. Similarly, the ocular bulbus is made up of multiple layers. The eyeball contains a watchglass-curved transparent cornea (Cornea) and the optic nerve (N. opticus [II]) at its anterior and posterior pole, respectively.
The outer (fibrous) layer of the eyeball (Tunica fibrosa bulbi) is composed of the sclera (Sclera) and cornea (Cornea) and consists of firm collagenous connective tissue. The extra-ocular muscles (see below) are anchored in what one perceives as “the white of the eye”, which is the Sclera. The Sclera turns into the avascular and transparent cornea (Cornea) which consists also mainly of collagen.
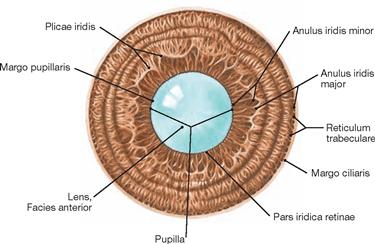
The middle (vascular) layer of the eyeball (Tunica vasculosa bulbi) consists of choroid (Choroidea), ciliary body (Corpus ciliare) and iris (Iris). It is very rich in vasculature (branches of Aa. ciliares) and strongly pigmented. This vascular layer of the eye also contains the intraocular muscles which are not subject to voluntary control. From the outside, the iris, the anterior portion of the Tunica vasculosa, along with the pupil (Pupilla) is visible. Muscles located within the iris can constrict or dilate the pupil (adaption). Along and behind the root (outer margin) of the iris, the Tunica vasculosa forms a circular bulge known as the ciliary body (Corpus ciliare). The M. ciliaris is anchored within the Corpus ciliare. The ciliary body received its name because of the radial zonular fibres (Fibrae zonulares) which radiate towards the middle to secure the lens (Lens) in its position immediately behind the pupil. Normally, the lens is transparent and elastic. The effect of the zonular fibres and the ciliary body on the shape of the lens changes the refractive power of the lens and leads to focussing of the eye (accommodation). The actual vascular layer separates the Sclera and Retina and covers the posterior half of the eyeball.
The inner layer of the eyeball (Tunica interna bulbi, syn. Retina) consists of a photoreceptor-free (i.e. nonvisual) (Pars caeca retinae) and a photoreceptor (i.e. visual) part (Pars optica retinae). The Pars caeca is a thin, heavily pigmented epithelium that covers the posterior part of the iris and the Corpus ciliare. Along the serrated edge (Ora serrata), just behind the ciliary body, it transforms into the much thicker Pars optica. However, this “seeing” Pars optica has a blind spot (Discus nervi op-tici), where the optic nerve leaves the Retina and the branches of the A. centralis retinae penetrate into the Retina.
All layers of the eyeball and their differentiations surround the gelatinous, totally transparent interior of the eye, the vitreous body (Corpus vitreum). It stabilizes the entire membranous structure of the eye by its swelling pressure (intra-ocular pressure) – similar to the air bubble inside a soccer ball stabilizing its leathery coat.
Auxiliary Structures
The auxiliary structures of the eye consist of the eyelids (Palpebrae), the conjunctiva (Tunica conjunctiva), the lacrimal apparatus (Apparatus lacrimalis), the six extra-ocular muscles and their three motor (cranial) nerves, numerous blood vessels, and a considerable orbital fat body (Corpus adiposum orbitae).
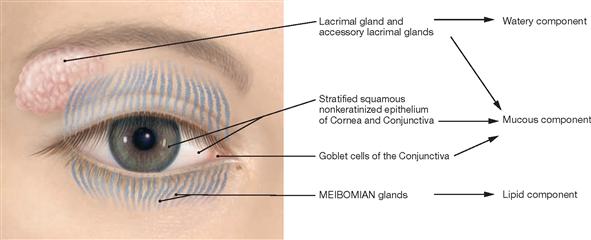
The eyelids (Palpebrae) are not only responsible for the protection of the eyeball but distribute the tear film across the surface of the eye while constantly blinking. This prevents the surface of the eye from drying out. Located in the eyelids, numerous specialized sebaceous glands (MEIBOMIAN glands; Glandulae tarsales) contribute a fatty se-cretion to the tear film.
The conjunctiva (Tunica conjunctiva) is a thin, transparent epithelial layer and covers the inner side of the Palpebrae and the visible part of the Sclera. Its mucous secretions are a component of the tear film. At the corneal limbus (Limbus corneae) the conjunctiva transitions into the corneal epithelium.
The lacrimal gland (Glandula lacrimalis), positioned at the upper outer (lateral) corner of the orbit, and numerous accessory glands (Glandulae lacrimales accessoriae) located in the eyelids, produce the watery constituent of the tears (Lacrimae). During eyelid closure the tear film is wiped towards the medial (nasal) canthus (nasal palpebral commissure) which contains the lacrimal caruncle (Caruncula lacrimalis), where the collected tears accumulate to create a lacrimal lake (Lacus lacrimalis). The lacrimal puncti (Puncta lacrimalia), one opening above and the other below the Caruncula, are connected to two lacrimal canaliculi (Canaliculi lacrimales). These canaliculi drain the tears into the lacrimal sac (Saccus lacrimalis), which opens into the nasolacrimal duct (Ductus nasolacrimalis) and empties the tears into the nasal cavity.
All six extra-ocular muscles insert at the Bulbus oculi and move it in different directions. Most of them arise from a common tendinous ring (Anulus tendineus communis) which surrounds the N. opticus [II] at its entry into the orbit. An exception is the inferior oblique eye muscle which lies on the floor of the orbit and originates directly lateral to the opening of the Canalis nasolacrimalis. The extra-ocular muscles form a muscle cone behind the eyeball with its tip pointing towards the Canalis nervi optici. Located in the centre of the Canalis nervi optici, the A. ophthalmica and the N. opticus [II] reach the posterior pole of the eyeball. The three nerves innervating the extra-ocular muscles, various branches of the N. ophthalmicus [V/1], as well as the branches of the V. ophthalmica are positioned within or adjacent to the cone. The remaining gaps between the structures are filled by adipose tissue, the Corpus adiposum orbitae.
→Dissection Link
For the dissection of the orbit, the Pars orbitalis of the M. orbicularis oculi together with the Partes palpebrales of the upper and the lower lid are removed from the underlying connective tissue and turned over medially. The structures should not be detached at the nasal canthus. Septum orbitale, Tarsus superior and inferior, and the Ligg. palpebralia mediale and laterale are presented. For cranial access to the orbit, skin and muscles covering the frontal bone and the Dura mater in the anterior cranial fossa are removed. The opening the orbital roof should be carried out carefully to avoid damage to the Periorbita and other structures passing through the Fissura orbitalis superior. Upon opening of the Periorbita, the M. levator palpebrae superioris with attached eyelid is dissected towards the Anulus tendineus (do not detach the N. trochlearis and R. superior of the N. oculomotorius). Next, all the structures of the orbit are dissected from top to bottom by removing the orbital fat body. Careful blunt removal of the orbital fat body should be performed to preserve the Ganglion ciliare.
Development
Development
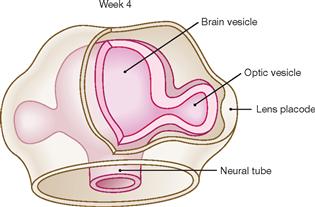
Fig. 9.1 Development of the eye, week 4. [21]
At week 4, the optic vesicle bulges out of the diencephalic area of the prosencephalon. As the optic vesicle grows, its distal part gets in contact with the surrounding surface ectoderm and induces the formation of the lens placode.
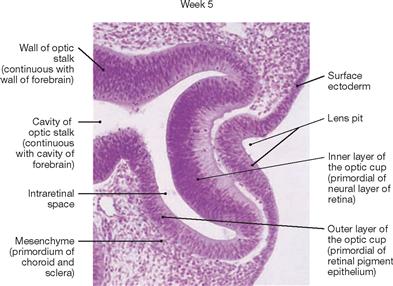
Fig. 9.2 Development of the eye, week 5; photomicrograph of a sagittal section. [20]
This image displays an invaginated double-walled optic vesicle with optic cup formation in close connection with the lens placode. Located between the two layers of the optic cup (primordium of the Retina) and in the optic stalk (primordium of the N. opticus [II]), the intraretinal space is still relatively wide.
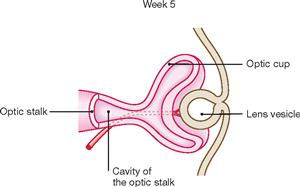
Fig. 9.3 Development of the eye, week 5. [21]
The spherical lens vesicle separates from the surface ectoderm and the rim of the optic cup infolds on the lens vesicle. The optic cup remains connected with the diencephalon by a small optic stalk, the former Sulcus opticus.
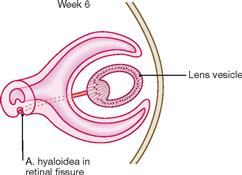
Fig. 9.4 Development of the eye, week 6. [21]
At the deepest point in the optic cup, a longitudinal groove, the optic fissure, becomes visible. This optic fissure contains blood vessels and the first nerve fibres of the later N. opticus [II]. The blood vessels supply as A. and V. hyaloidea the inside of the optic cup. At 7 months, distal parts of the hyaloid blood vessels degenerate, whereas the proximal parts persist as A. and V. centralis retinae in close connection with the N. opticus [II].
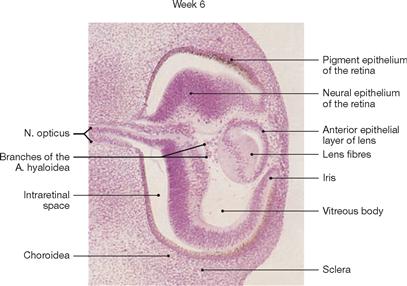
Fig. 9.5 Development of the eye, week 6; photomicrograph of a sagittal section. [20]
At week 7, lens fibres form as an elongation of epithelial cells at the posterior wall of the lens vesicle.
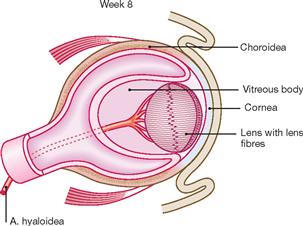
Fig. 9.6 Development of the eye, week 8. [21]
Mesenchymal cells migrate into the optic cup and form the vitreous body (Corpus vitreum) that is composed of vitreous humour, a gelatinous substance with tiny fibres embedded. The vitreous body gives the eye bulbus its firm shape.

Fig. 9.7 Male newborn with cyclopia. [20]
Cyclopia is an anomaly of the face and eye associated with a proboscis-shaped nasal appendage above a single medially located eye.
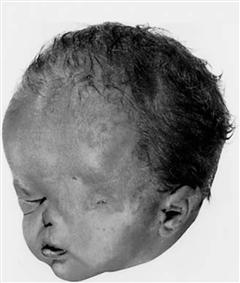
Fig. 9.8 Male newborn with anophthalmia. [20]
Congenital absence of all components of the eye and a single right nostril, with left nostril not formed. Although eyelids are formed, the upper and lower eyelids remain largely fused.
Skeleton
Bony orbit
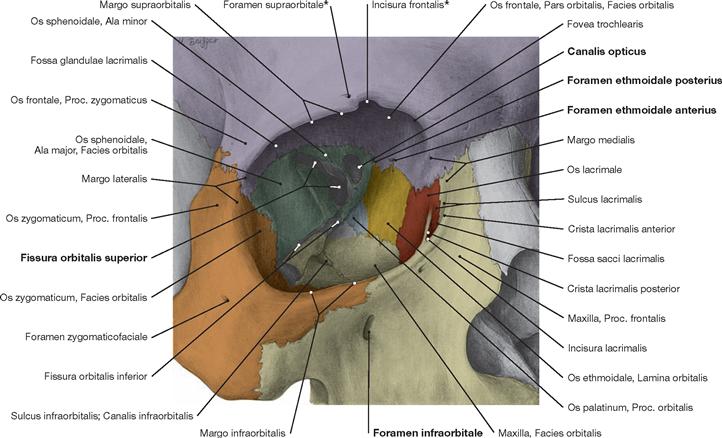
Fig. 9.9 Orbit, Orbita, right side; frontal view from an oblique angle; colour chart see inside of the back cover of this volume.
Seven bones form the walls of the orbit (Os frontale, Os ethmoidale, Os lacrimale, Os palatinum, Maxilla, Os sphenoidale, and Os zygomaticum). The Paries lateralis borders on the Fossa temporalis, the Paries medialis is located close to the ethmoidal cells and the nasal cavity. At its posterior aspect, the Orbita is in topographic proximity to the middle cranial fossa, the Canalis opticus, and the Fossa pterygopalatina.
* These structures can be present as Foramina or Incisurae.
* These structures can be present as Foramina or Incisurae.
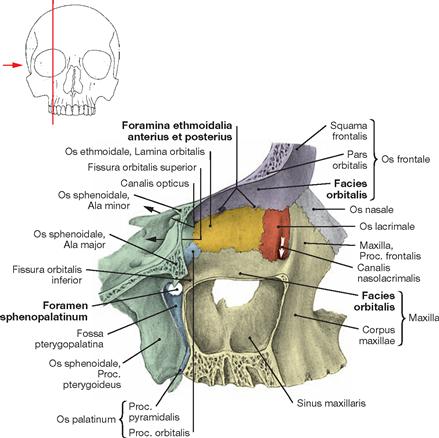
Fig. 9.10 Medial wall of the orbit, Paries medialis orbitae, right side; lateral view; colour chart see inside of the back cover of this volume.
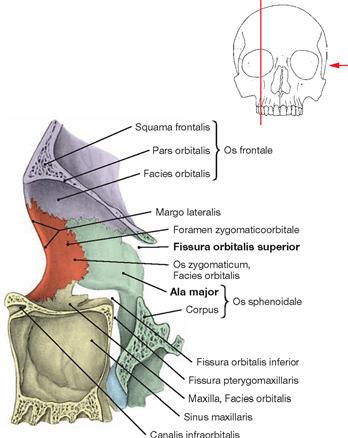
Fig. 9.11 Lateral wall of the orbit, Paries lateralis orbitae, right side; medial view; colour chart see inside of the back cover of this volume.
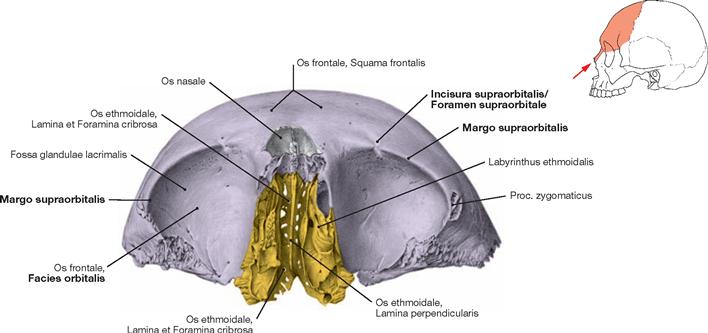
Fig. 9.12 Roof of the orbit, Paries superior orbitae; inferior view; colour chart see inside of the back cover of this volume.
The roof of the orbit is also the floor of the anterior cranial fossa and of parts of the Sinus frontalis. All bones of the Labyrinthus ethmoidalis are extremely thin and are easily fractured during surgical procedures.
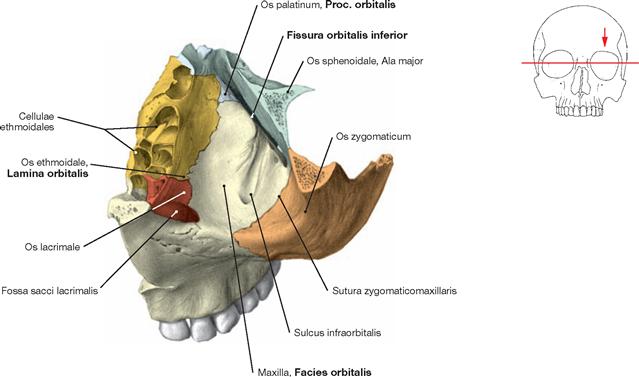
Fig. 9.13 Floor of the orbit, Paries inferior orbitae, left side; superior view; colour chart see inside of the back cover of this volume.
The floor of the orbit is also the roof of the Sinus maxillaris. The Sulcus infraorbitalis is located in the posterior aspect of the orbit and turns into a bony canal midway through the orbit. This Canalis infraorbitalis penetrates the Maxilla and terminates at the Foramen infraorbitale (not visible) located below the orbit.
Eyelids
Eyelids
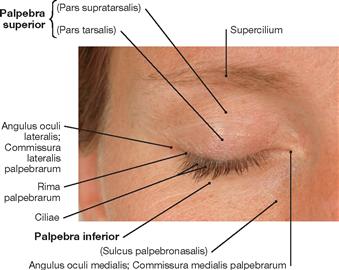
Fig. 9.14 Eye, Oculus, right side, with eyelids closed.
On average, a human eye blinks 20 to 30 times per minute. Each eyelid movement distributes a tear film across the surface of the eye. Blinking involves a consecutive contraction of the M. orbicularis oculi from temporal to nasal and results in a wiping motion in the direction of the nasal canthus. Mechanical irritations (e.g. sudden draft, dust particle, fly) activate the blink reflex (also known as corneal reflex) to protect the surface of the eye.
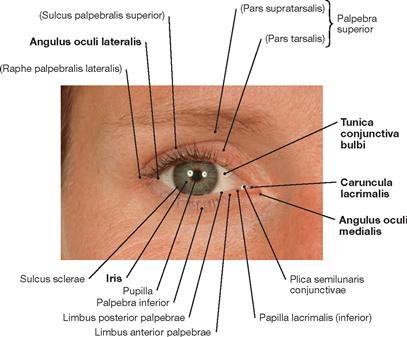
Fig. 9.15 Eye, Oculus, right side, with eyelids open.
In an adult with eyelids open, the width between the upper and lower eyelid ranges between 6–10 mm, and the distance between the temporal and nasal canthus is 28–30 mm.
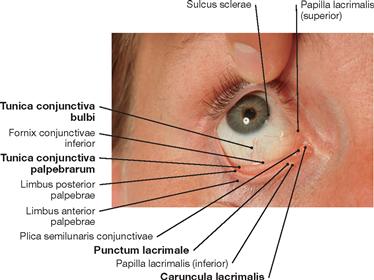
Fig. 9.16 Eye, Oculus, right side, with upper and lower eyelid everted.
With the exception of the cornea, the Conjunctiva, a translucent thin layer of mucosa with blood vessels, covers the part of the eyeball creating the eye surface, and the side of the eyelids in contact with the eye surface.
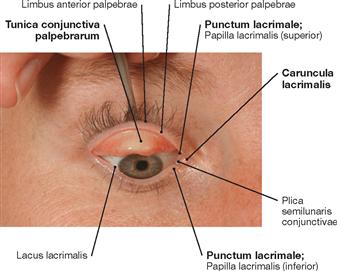
Fig. 9.17 Eye, Oculus, right side, with assisted ectropionised upper eyelid.
The Conjunctiva palpebrae and the Conjunctiva bulbi cover the rear side of the eyelid and the eyeball, respectively. Both conjunctival parts merge at the upper and lower Conjunctiva fornicis. The latter being the so-called conjunctival sac. Eyedrop medication is administered into the lower conjunctival sac.
Facial Muscles
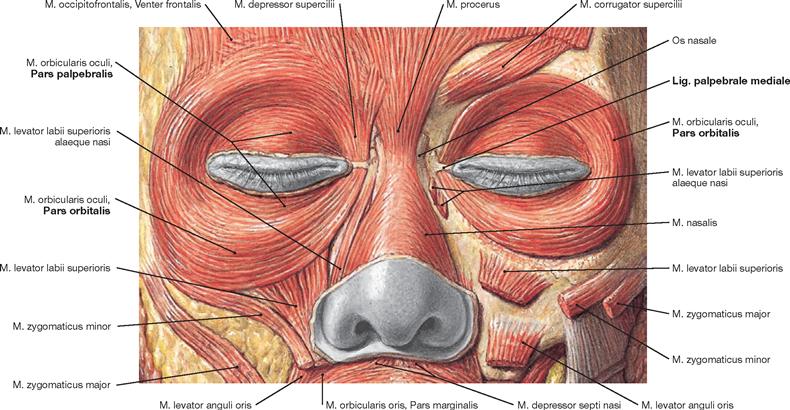
Fig. 9.18 Facial muscles, Mm. faciei, in the orbital region; frontal view.
The Pars orbitalis of the M. orbicularis oculi encircles the anterior opening of the orbit. The Pars palpebralis of this muscle continues into the eyelids.![]()
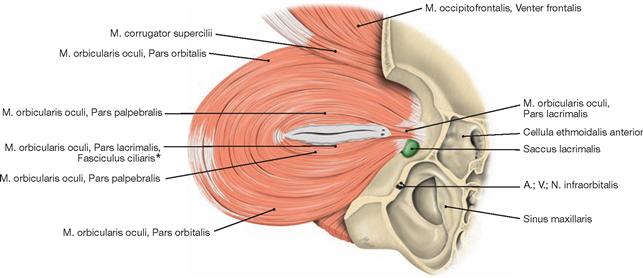
Fig. 9.19 M. orbicularis oculi, left side; posterior view.
At the nasal canthus the Pars lacrimalis of the muscle (HORNER‘s muscle), which assists in draining the tear fluid, is visible.
The M. orbicularis oculi consists of three parts. The Pars orbitalis is responsible for the voluntary firm occlusion of the eyelids. Contraction of the Pars palpebralis results in blinking of the eye, which can occur voluntarily but usually happens involuntarily. Placed around the lacrimal canaliculi, the Pars lacrimalis (HORNER‘s muscle) is essential for the drainage of the tear fluid. During blinking, the two lacrimal puncta (Puncta lacrimalia: Punctum lacrimale superius and Punctum lacrimale inferius) in the nasal third of the medial canthus dip into the lacrimal lake (Lacus lacrimalis). It is assumed is that the contraction of the Pars lacrimalis results in a suction effect (pressure-suction pump mechanism). Channeled via the lacrimal puncta, the tear fluid is sucked through the upper and lower lacrimal canaliculi (Canaliculus superior and inferior) into the lacrimal sac (Saccus lacrimalis). The lower lacrimal canaliculus transports most of the tear fluid.![]()
* muscle of RIOLAN
Eyelids, structure
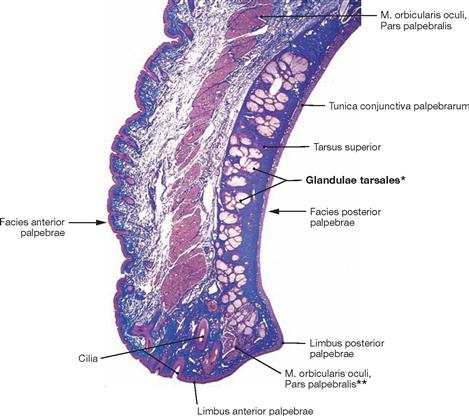
Fig. 9.20 Upper eyelid, Palpebra superior; photograph of a histological specimen; azan stain; sagittal section, magnified. [26]
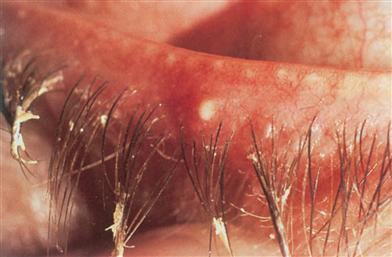
The eyelid can be divided into an outer and inner lamina. The outer lamina is composed of the striated M. orbicularis oculi with its Pars palpebralis. The inner lamina consists of the conjunctiva (Tunica conjunctiva palpebrarum), the tarsus (Tarsus) with integrated MEIBOMIAN glands (Glandulae tarsales, modified sebaceous glands) and, close to the rim of the eyelid, muscle fibres (muscle of RIOLAN, Fasciculi ciliares) derived from the Pars orbitalis of the M. orbitals oculi projecting into the tarsus.
* MEIBOMIAN glands
** muscle of RIOLAN
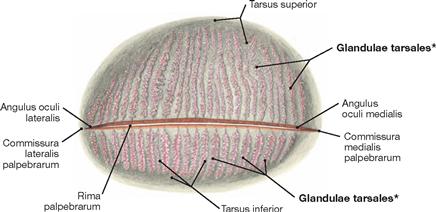
Fig. 9.21 Eyelids, Palpebrae, right side; posterior view; translucent specimen illustrating the excretory ductules of the tarsal glands.
Each eyelid contains approximately 25 to 30 individual glands with their excretory ductules opening into the rim of the eyelid (Rima palpebralis).
* MEIBOMIAN glands
Blood supply and innervation of the lacrimal gland and eyelids
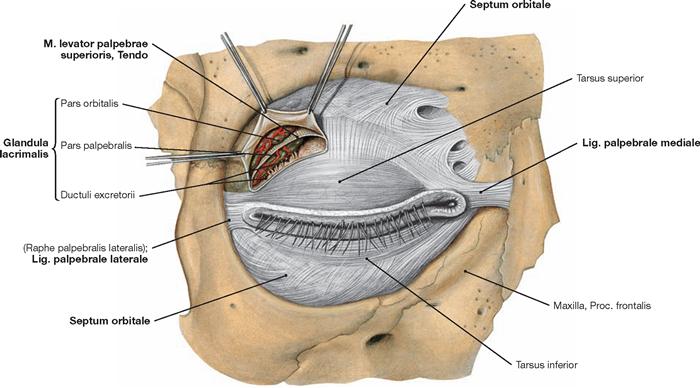
Fig. 9.23 Orbital opening, Aditus orbitalis, right side, with Septum orbitale, tarsal plates, and palpebral ligaments; frontal view.
Dissection of the Septum orbitale and of the inserting tendon of the M. levator palpebrae superioris displays the lacrimal gland. The tendon of the M. levator palpebrae superioris divides the lacrimal gland located in the temporal upper quadrant of the bulbus into a Pars orbitalis and a Pars palpebralis.
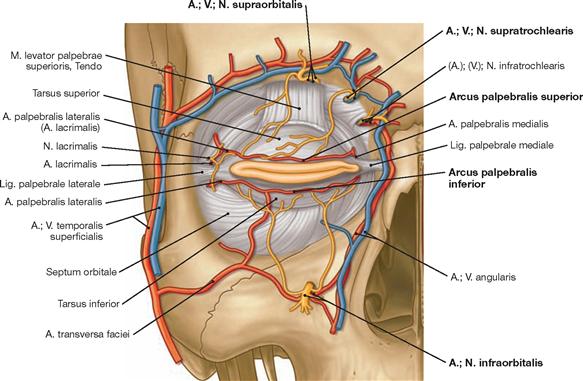
Fig. 9.24 Arteries, veins, and nerves at the orbital opening, Aditus orbitalis, and in the periorbital region, right side; frontal view. [10]
The superior and inferior Arcus palpebralis create an arterial circle located above the Septum orbitale and surrounding the orbit. This arterial circle is supplied by numerous arteries derived from the A. carotis interna (A. supraorbitalis, Aa. palpebrales laterales of the A. lacrimalis, Aa. palpebrales mediales) and the A. carotis externa (A. facialis, A. angularis, A. infraorbitalis, A. temporalis superficialis, A. zygomaticoorbitalis). The Nn. supraorbitalis and infraorbitalis are branches of the N. ophthalmicus [V/1] and N. maxillaris [V/2], respectively, and exit the orbit through the identically named Foramina (the N. supraorbitalis may exit the orbit through the Incisura supraorbitalis). The sensory perception of the N. ophthalmicus [V/1] and N. maxillaris [V/2] can be tested at both nerve exit points.
Lacrimal apparatus
Clinics
Fig. 9.26 Tear film of the eye, right side; frontal view; slit lamp examination with fluorescent dye in blue light. [15]
The spot represents a dry corneal area resulting from the disrupted tear film.

Fig. 9.27 SCHIRMER‘s test performed on a healthy person.
The two paper strips display a clear purple colouration of the yellow SCHIRMER‘s paper strip. Within 5 minutes, the paper strips are com-pletely purple.

Fig. 9.28 Reduced eyelid opening, right side; in the case of an acute dacryoadenitis (inflammation of the lacrimal gland). [15]
Lacrimal apparatus, innervation
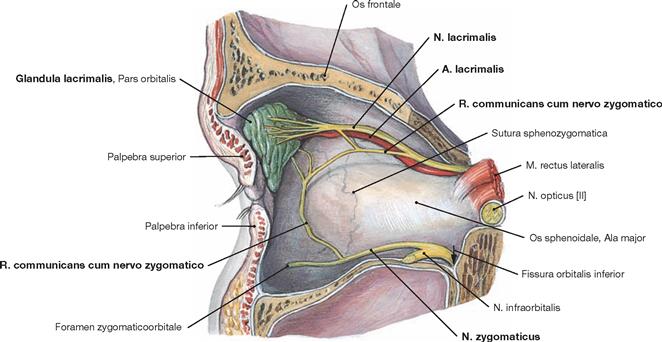
Fig. 9.29 Innervation of the lacrimal gland, Glandula lacrimalis, right side; medial view onto the lateral wall of the orbit.
Presentation of the lacrimal gland, the A. and N. lacrimalis and the connection between the N. zygomaticus and N. lacrimalis via the R. communicans cum nervo zygomatico.
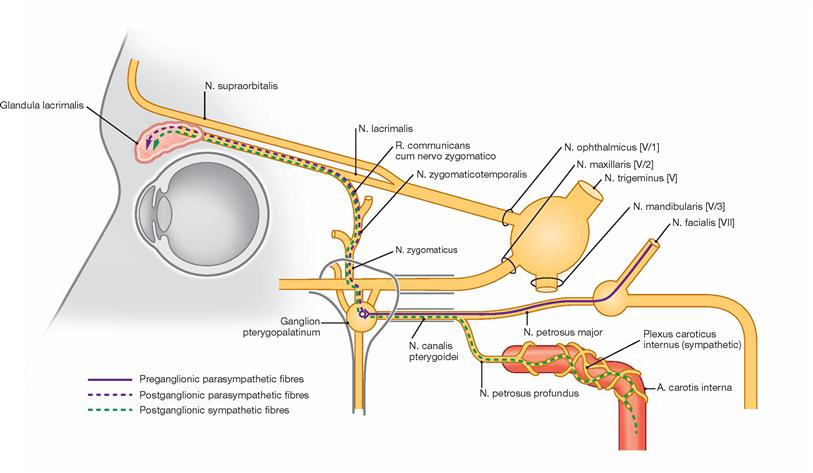
Fig. 9.30 Sympathetic and parasympathetic innervation of the lacrimal gland, Glandula lacrimalis; schematic drawing. [10]
Preganglionic sympathetic nerve fibres synapse in the Ganglion cervicale superius and postganglionic sympathetic fibres leave this ganglion to reach the lacrimal glands either by accompanying the Aa. carotis interna, ophthalmica, and lacrimalis, or by parting already from the A. carotis interna at the Foramen lacerum and joining the parasympathetic fibres on their way to the lacrimal gland. Preganglionic parasympathetic nerve fibres run with the intermedius portion of the N. facialis [VII], pass through the Ganglion geniculi without synapsing and reach the Ganglion pterygopalatinum via the N. petrosus major. Upon synapsing, postganglionic parasympathetic fibres associate with the N. zygomaticus and reach the N. lacrimalis and the lacrimal gland via the R. communicans cum nervo zygomatico.
Lacrimal apparatus
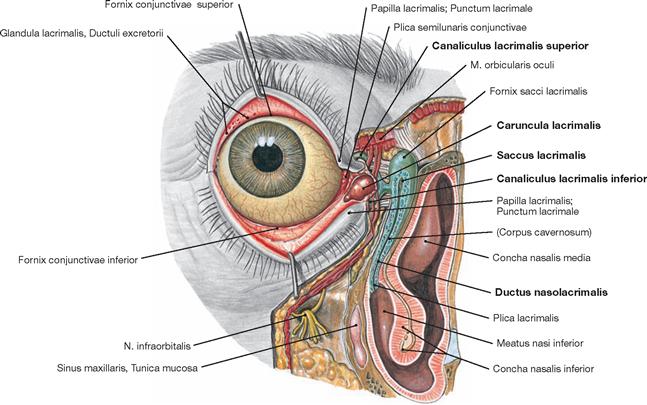
Fig. 9.31 Lacrimal apparatus, Apparatus lacrimalis, right side; frontal view; the eyelids have been pulled away from the eyeball providing a view into the upper and lower conjunctival sac; the nasolacrimal duct has been opened up to the Meatus nasi inferior.
The draining nasolacrimal duct is composed of the upper and lower lacrimal canaliculi (Canaliculi superior and inferior), the lacrimal sac (Saccus lacrimalis), and the nasolacrimal duct (Ductus nasolacrimalis). The Ductus nasolacrimalis exits into the inferior nasal meatus (Meatus nasi inferior) beneath the inferior nasal concha (Concha nasalis inferior).
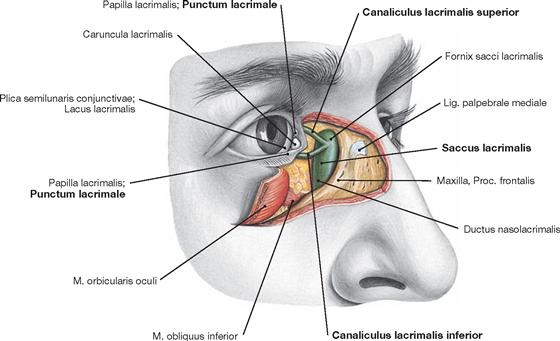
Fig. 9.32 Lacrimal apparatus, Apparatus lacrimalis, right side; frontolateral view; after removal of skin, muscles, and Septum orbitale in the nasal canthus.
The lacrimal sac (Saccus lacrimalis) is located in the Fossa sacci lacrimalis and continues caudally as Ductus nasolacrimalis in a bony enclosure formed by the Maxilla and the Os lacrimale in its anterior and posterior section, respectively. Each canaliculus originates as a 0.25 mm (upper) to 0.3 mm (lower) wide, round, oval or slit-shaped Punctum lacrimale which continues as an approximately 2 mm long vertical tube. Then, each canaliculus bends in an almost right angle and proceeds as an approximately 8 mm long horizontal segment. In the majority of cases (65–70%), both canaliculi merge to form a common tube approximately 1–2 mm long that opens into the lacrimal sac about 2–3 mm below the Fornix sacci lacrimalis.
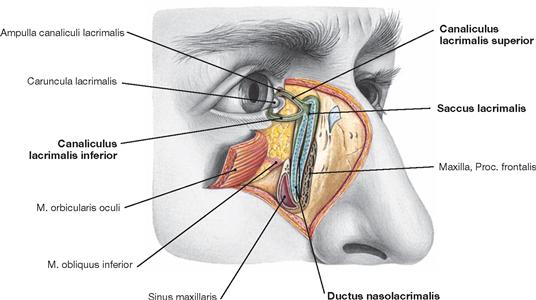
Fig. 9.33 Lacrimal apparatus, Apparatus lacrimalis, right side; horizontal section at the level of the lacrimal sac.
A cavernous body of tissue functionally supporting the transport of the tear fluid surrounds the lumen of the lacrimal sac. Swelling of this cavernous tissue reduces or blocks the transport of fluid and tears run down the cheek (crying). The blood vessels of the cavernous tissue dilate when a foreign particle enters the conjunctival sac or during strong emotions (e.g. intense happiness or sadness).
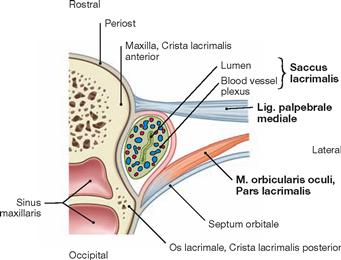
Fig. 9.34 Lacrimal apparatus, Apparatus lacrimalis, right side; horizontal section at the level of the lacrimal sac, Saccus lacrimalis. [8]
The vertical diameter of the lacrimal sac measures approximately 12 mm, the sagittal diameter 5–6 mm, and the transverse diameter 4–5 mm. The nasolacrimal duct of an adult is about 12.4 mm long. The surrounding bony canal is approximately 10 mm long and has a diameter of 4.6 mm. Notice the close topographic proximity to the Sinus maxillaris.
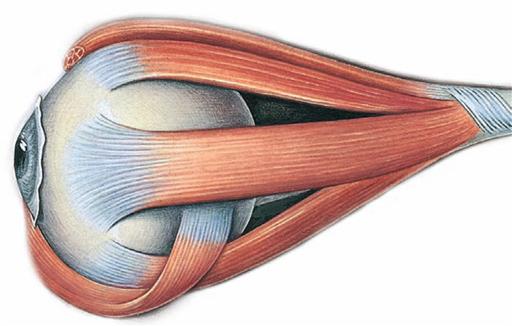
Extra-ocular muscles
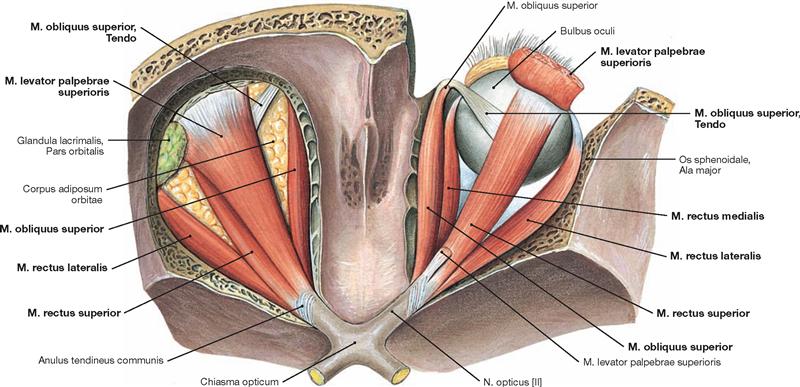
Fig. 9.35 Extra-ocular muscles, Mm. bulbi; superior view; upon removal of the roof of the orbit on both sides, and removal of the major part of the M. levator palpebrae superioris and of the orbital fat body on the right side.
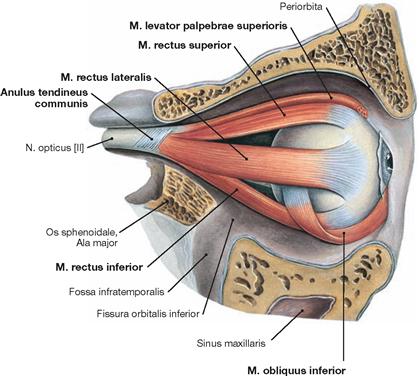
Fig. 9.36 Extra-ocular muscles, Mm. bulbi, right side; lateral view; upon removal of the lateral wall of the orbit.
The movement of the eyeball is controlled by six extra-ocular muscles in the orbit (four rectus muscles: Mm. recti superior, inferior, medialis, and lateralis; two oblique muscles: Mm. obliqui superior and inferior). With the exception of the M. obliquus inferior (origin at the Facies orbitalis of the Maxilla lateral of the Incisura lacrimalis maxillae in the anterior medial region of the orbit) and the M. obliquus superior (origin at the Corpus ossis sphenoidalis medial of the Anulus tendineus communis and the dural sheath of the N. opticus), all other extra-ocular muscles originate from the Anulus tendineus communis (tendinous anulus of ZINN).
All six muscles insert at the Sclera. All four extra-ocular rectus muscles insert anterior to the equator of the eyeball, whereas the oblique mus-cles of the orbit insert posterior to the equator. A tendinous pulley-like structure (Trochlea), which attaches to the anterior upper area of the Os frontale and acts as a hypomochlion for the M. obliquus superior, redirects this muscle backwards to its insertion area at the top of the eyeball posterior to its equator. The tendinous anulus of ZINN is also the origin of the M. levator palpebrae superioris which projects into the upper eyelid (Palpebra superior).
Muscles of the eye
Extra-ocular muscles
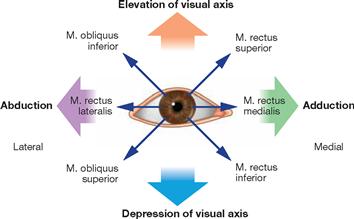
Fig. 9.37 Function of the extra-ocular muscles, Mm. bulbi. [8]
Testing the ability of the eyeball to move into the four main directions of the visual axis is part of a proper physical exam. Shown are the activated muscles during the movement of each eyeball into the four directions of the visual axis. The coordination of the synchronous movement of both eyeballs is very complex since the various extra-ocular muscles are innervated by different cranial nerves (Nn. oculomotorius, trochlearis, and abducens). The extra-ocular muscles receive very rich innervation and are distinct in fine structure from the normal striated muscles.
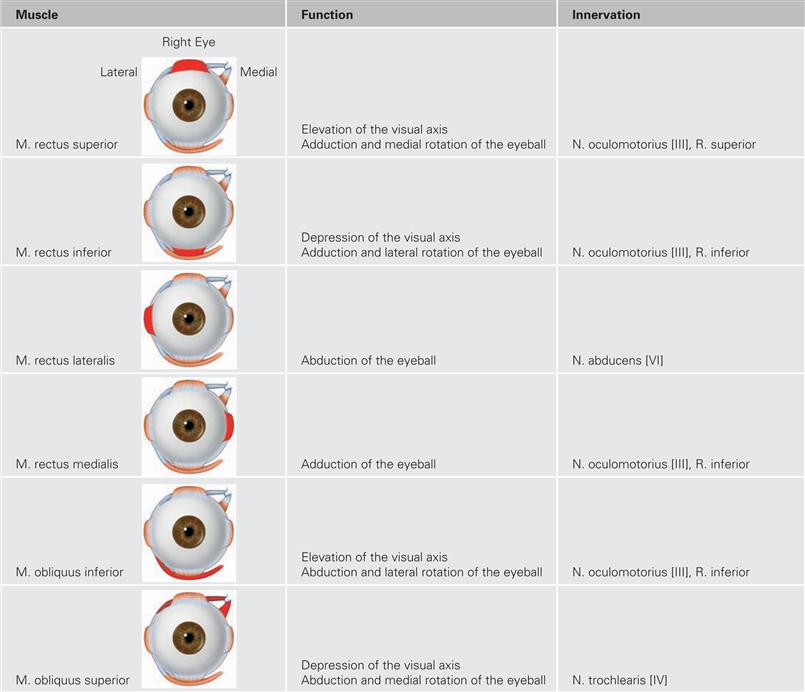
Fig. 9.38 Function and innervation of the extra-ocular muscles inserting at the Bulbus oculi. [10]
The respective muscle is coloured in dark red.
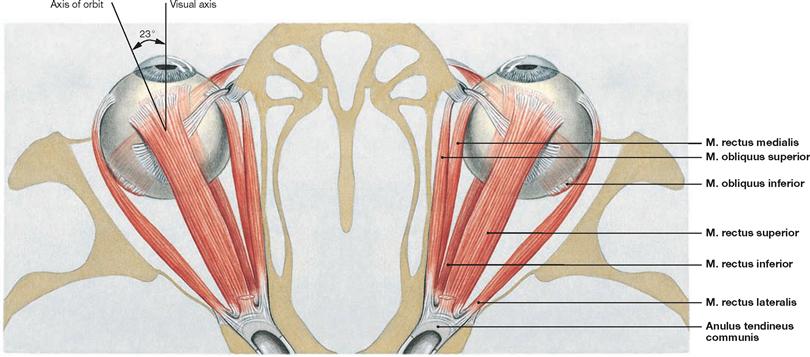
Fig. 9.39 Extra-ocular muscles, Mm. bulbi; superior view.
Shown are the Anulus tendineus communis (tendinous anulus of ZINN) and the insertion sites of the muscles at the eyeball.
The visual axis (imaginary line from the midpoint of the visual field to the Fovea centralis) and the axis of the orbit (imaginary line through the centre of the lens) differ by an angle of 23°. This is the reason why the Fovea centralis (retinal location of focused central vision) is located lateral to the Papilla nervi optici (blind spot).
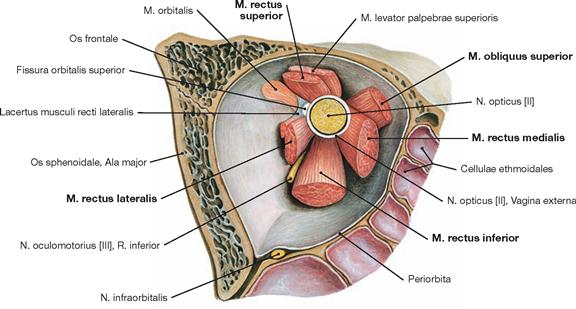
Fig. 9.40 Extra-ocular muscles, Mm. bulbi, right side; frontal view onto the posterior wall of the orbit. The periorbital space near the Fissura orbitalis superior contains muscle fibres with sympathetic nerve innervation; collectively, these form the M. orbitalis.
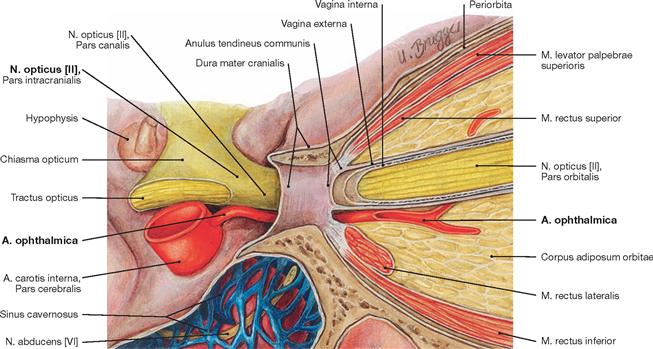
Fig. 9.41 Optic nerve, N. opticus [II]; right side; lateral view upon opening of the Canalis opticus.
Both, the N. opticus [II] and the A. ophthalmica (branch of the A. carotis interna) course through the Canalis opticus and the Anulus tendineus communis (tendinous anulus of ZINN) into the orbit.
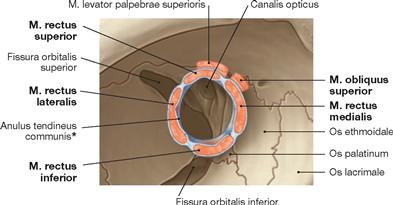
Fig. 9.42 Muscular origins at the Anulus tendineus communis (tendinous anulus of ZINN), right side; frontal view. [10]
The Anulus tendineus communis is the origin for the Mm. rectus superior, rectus medialis, rectus inferior, and rectus lateralis. A neurovascular bundle not depicted in this image passes through the Anulus (→ Fig. 9.43). Also shown is the M. levator palpebrae superioris which originates at the tip of the orbit from the Ala minor ossis sphenoidalis. The M. obliquus superior has its origin at the Corpus ossis sphenoidalis medial to the Anulus tendineus communis at the dural sheath.
* tendinous anulus of ZINN
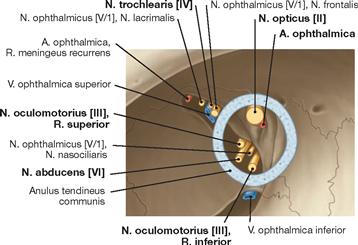
Fig. 9.43 Neurovascular structures passing through the Canalis opticus and the Fissura orbitalis superior, right side; frontal view. [10]
The N. oculomotorius [III], N. nasociliaris, N. abducens, and Radix sympathica ganglii ciliaris pass through the Fissura orbitalis superior and the Anulus tendineus communis (tendinous anulus of ZINN). The V. ophthalmica superior, N. lacrimalis, N. frontalis, and N. trochlearis [IV] also pass through the Fissura orbitalis superior into the orbit. However, these neurovascular structures run outside of the Anulus tendineus communis. Not shown are the V. ophthalmica inferior, A. infraorbitalis, N. infraorbitalis, and N. zygomaticus which enter the orbit through the Fissura orbitalis inferior. Centrally within the N. opticus [II] courses the A. centralis retinae as the first branch of the A. ophthalmica.
Blood vessels of the orbit
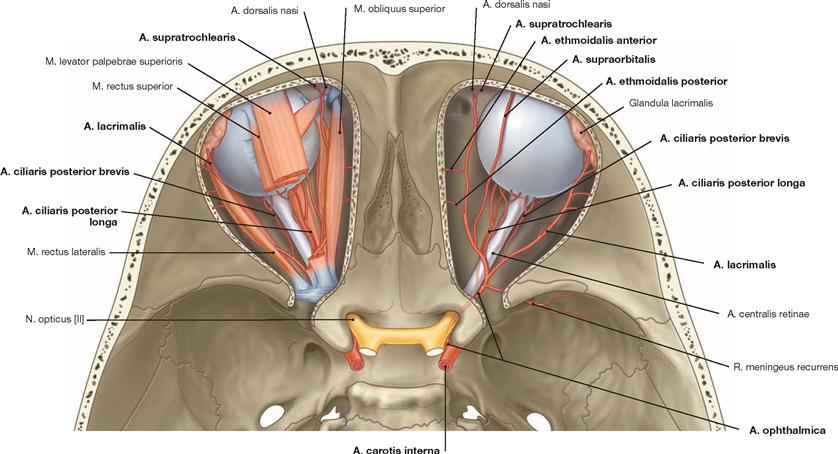
Fig. 9.44 Arteries of the eye, Oculus, and of the orbit, Orbita; superior view onto the openend Orbitae; left side: content of the orbit with extra-ocular muscles, right side: without extra-ocular muscles.[10]
The A. ophthalmica is the main artery of the orbit and branches off the Pars cerebralis of the A. carotis interna. The A. ophthalmica normally courses below the N. opticus [II] through the Canalis opticus into the orbit. Here, the artery divides into many branches which supply the eyeball and the structures of the orbit with blood. Anastomoses exist via a R. orbitalis to the A. meningea media, via the Aa. ethmoidales anterior and posterior to blood vessels in the nose, and via blood vessels penetrating the Septum orbitale or the bone to the facial arleries (Aa. supraorbitalis, supratrochlearis, palpebralis medialis and lateralis, dorsalis nasi).
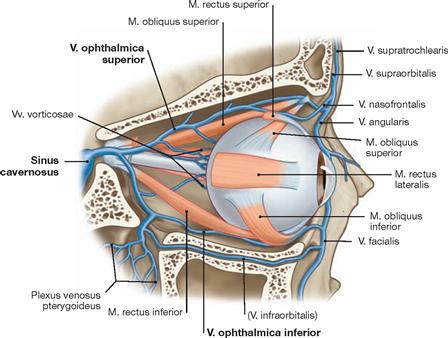
Fig. 9.45 Veins of the eye, Oculus, and of the orbit, Orbita; right side; lateral view into the Orbita; after removal of the lateral wall of the orbit. [10]
The Vv. ophthalmicae superior and inferior drain the venous blood. The latter is usually smaller than the A. ophthalmica superior. Venous anastomoses exist to the veins of the superficial and deep facial regions (Plexus pterygoideus) and the Sinus cavernosus.
Topography
Arteries and nerves of the orbit
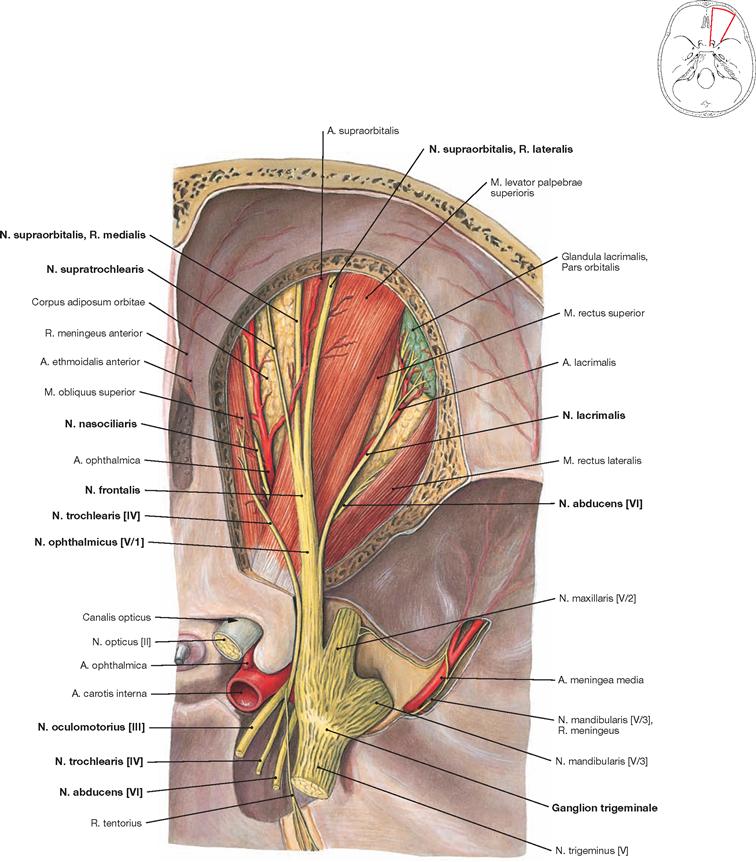
Fig. 9.46 Arteries and nerves of the orbit, Orbita, right side; superior view onto the openend orbit (upper level of the orbit);
Demonstration of the Ganglion trigeminale (Ganglion semilunare, Ganglion GASSERI); bony roof of the Orbita, Periorbita, and Corpus adiposum orbitae were partially removed.
Shown is the course of the N. ophthalmicus [V/1] through the opened Fissura orbitalis superior and its branching into Nn. lacrimalis and frontalis (incl. consecutive branching) and, running more deeply, the N. nasociliaris. In addition, the gracile N. trochlearis [IV] for the motor innervation of the M. obliquus superior and the more deeply located N. abducens [VI] for the innervation of the M. rectus lateralis are depicted.
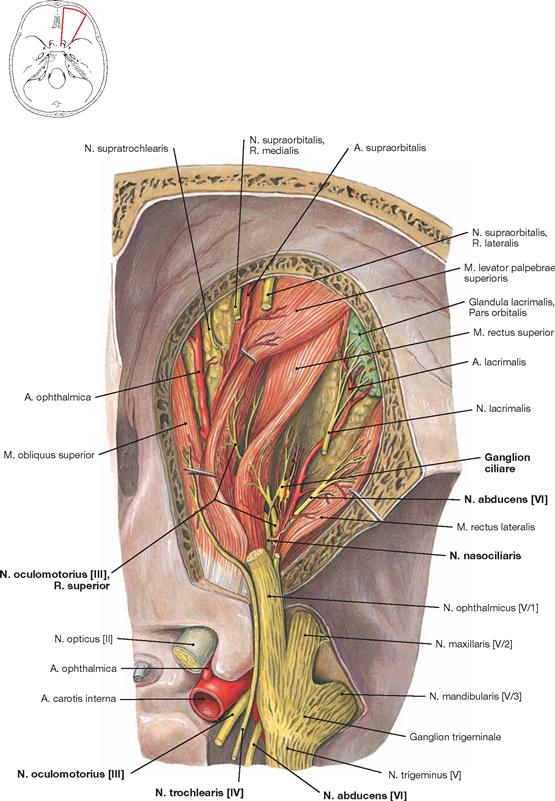
Fig. 9.47 Arteries and nerves of the orbit, Orbita, right side; superior view; after removal of the roof of the orbit; presentation of the Ganglion ciliare; the M. levator palpebrae superioris and M. rectus superior were folded back.
Shown are nerve branches of the N. oculomotorius [III] entering beneath the muscles. Upon removal of the orbital fat body beneath the muscles, the Ganglion ciliare, approximately 2 mm in size, becomes visible. Positioned approximately 2 cm lateral to the N. opticus [II] behind the Bulbus oculi, the Ganglion ciliare is embedded in the Corpus adiposum orbitae. The Ganglion ciliare contains perikarya of postganglionic parasympathetic neurons which synapse with the axons of preganglionic parasympathetic neurons located in the Nucleus oculomotorius accessorius (autonomicus, EDINGER-WESTPHAL nucleus). These parasympathetic fibres innervate the inner muscles of the eye (M. ciliaris und M. sphincter pupillae, → Fig. 8.163). Having switched earlier from preganglionic to postganglionic fibres in the Ganglion cervicale superius, postganglionic sympathetic fibres for the M. dilatator pupillae simply pass through the Ganglion ciliare.
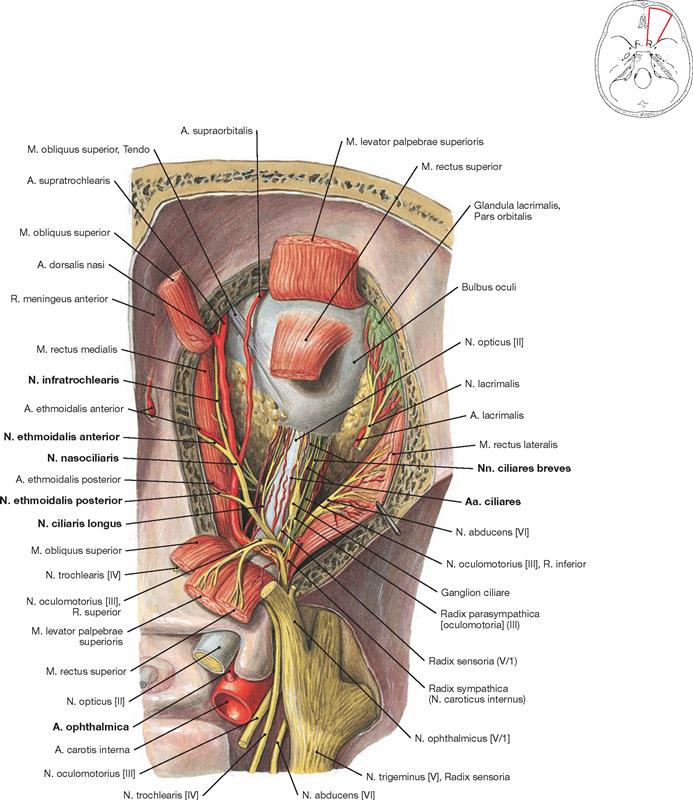
Fig. 9.48 Arteries and nerves of the orbit, Orbita, right side; superior view; upon partial removal of the Mm. levator palpebrae superioris, rectus superior, and obliquus superior.
The middle level of the orbit is depicted. Shown are the N. opticus [II] with supplying network of arteries (Aa. ciliares) branching off the A. ophthalmica, which is running through the orbit, as well as the Nn. ciliares longi and breves, the Ganglion ciliare, and the terminal branching of the N. nasociliaris.
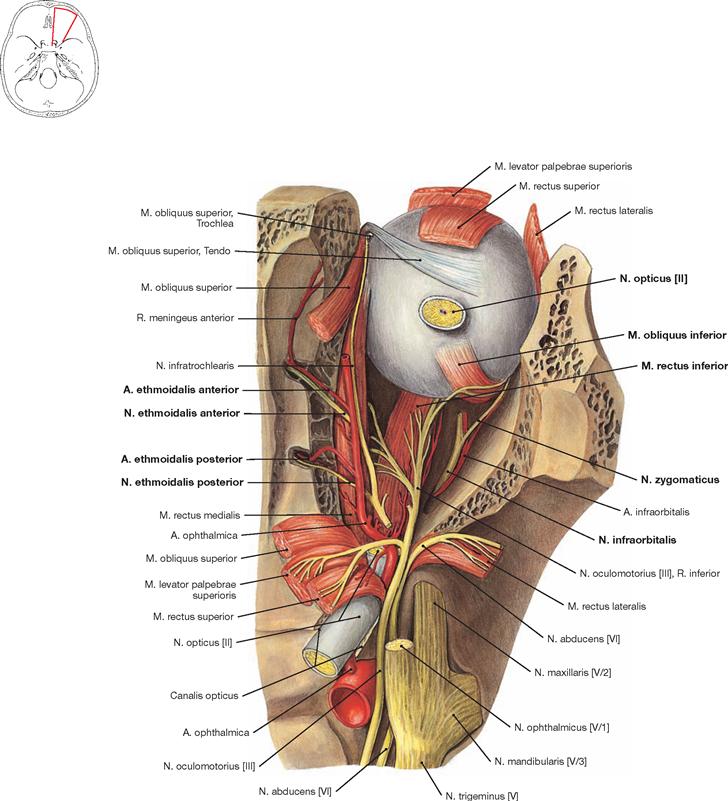
Fig. 9.49 Arteries and nerves of the orbit, Orbita, right side; superior view; the N. opticus [II] has been cut.
After dissecting additional structures and upon removal of the entire orbital fat body, the M. rectus inferior and the lower level of the orbit become visible. The bulbus is rotated in such a way that the insertion site of the M. obliquus inferior close to the entry site of the cut N. opticus [II] can be seen. The ethmoidal cells (Cellulae ethmoidales) at the medial side have been opened up to demonstrate the course of the Nn. ethmoidales anterior and posterior as well as the Aa. ethmoidales anterior and posterior from the orbit into the ethmoid bone. The A. and N. infraorbitalis are located in the lower level of the orbit. In addition to sensory fibres, the N. zygomaticus, a branch of the N. infraorbitalis, also contains postganglionic parasympathetic fibres for the autonomic innervation of the lacrimal gland.
Nerves of the orbit
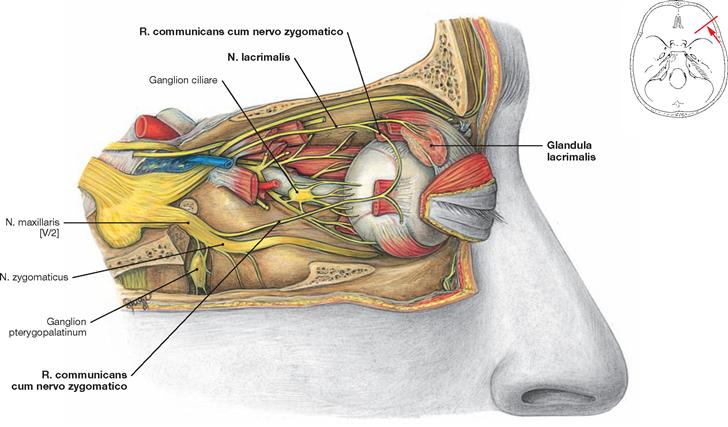
Fig. 9.50 Nerves of the orbit, Orbita, and the eye, Oculus, innervation of the lacrimal gland, Glandula lacrimalis, and demonstration of the Ganglion ciliare, right side; lateral view; after removal of the temporal wall and orbital fat body.
Sympathetic, parasympathetic, and sensory fibres innervate the lacrimal gland. Postganglionic parasympathetic fibres derive from the Ganglion pterygopalatinum to stimulate excretion by this gland. The fibres leave the Ganglion pterygopalatinum, associate with the N. zygomaticus (a branch of the N. maxillaris [V/2]), and separate as R. communicans cum nervo zygomatico (→ Figs. 8.163 and 9.30) to anastomose with the N. lacrimalis and reach the lacrimal gland. The N. lacrimalis (a branch of the N. ophthalmicus [V/1]) provides the sensory innervation of the lacrimal gland. The sympathetic fibres inhibit glandular secretion. Postganglionic sympathetic fibres derive from the Ganglion cervicale superius. Without synapsing, these fibres pass through the Ganglion pterygopalatinum and taking the same route as the parasympathetic fibres they reach the lacrimal gland (→ Fig. 9.30).
Orbit, topography
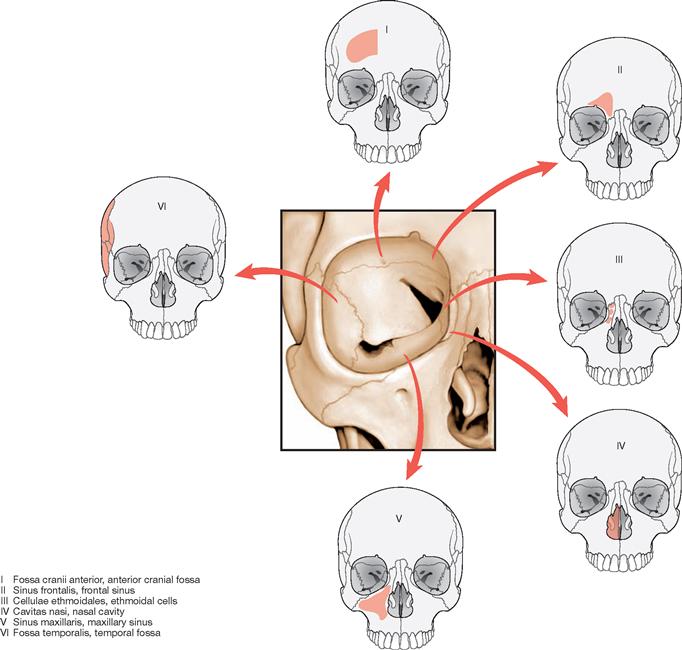
Fig. 9.52 Topographical relationships of the orbit, Orbita, and neighbouring regions, right side; frontal view.
The Orbita has a close topographical relationship with neighbouring regions. This includes the anterior cranial fossa (Fossa cranii anterior), the frontal sinus (Sinus frontalis), the ethmoidal cells (Cellulae ethmoidales), the nasal cavity (Cavitas nasi), the maxillary sinus (Sinus maxillaris), and the temporal fossa (Fossa temporalis).

Fig. 9.53 Patient suffering from endocrine orbitopathy. [18]
Shown is the pronounced exophthalmos as well as a scar in the neck region (condition after thyroidectomy).
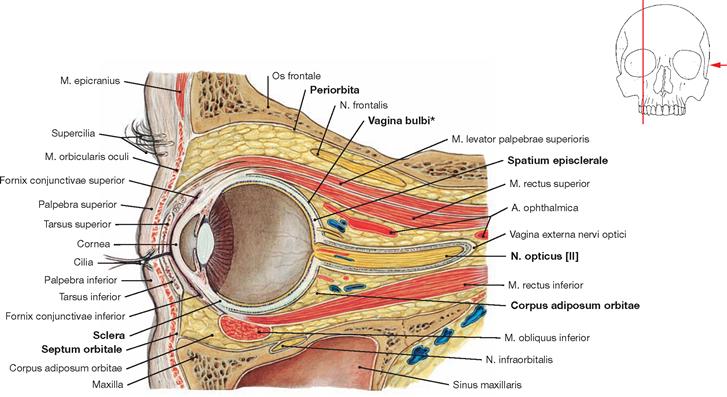
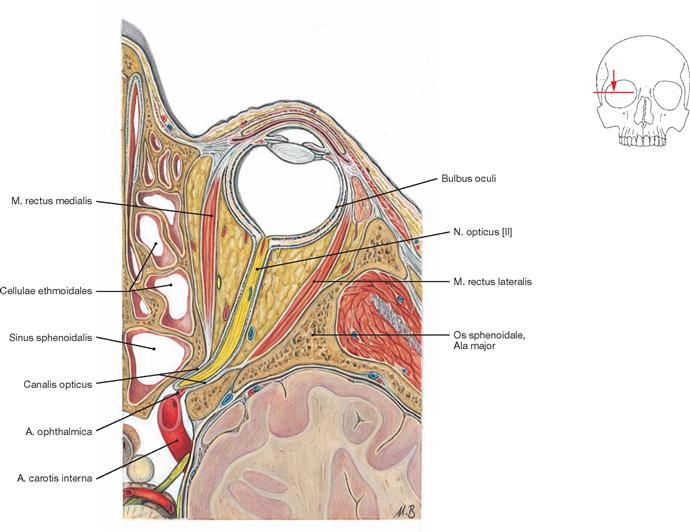
Fig. 9.54 Orbit, Orbita, right side; medial view; vertical midline section.
The Periorbita (periosteum) covers the inside of the orbit. All structures of the orbit are embedded in adipose tissue (Corpus adiposum orbitae). The Septum orbitale delineates the entrance to the orbit; a thin layer of connective tissue (Vagina bulbi, Fascia bulbi, or TENON’s capsule) surrounds the eyeball. A narrow gap (Spatium episclerale) separates the Vagina bulbi and the sclera of the eyeball.
* TENON’s capsule
Orbit, frontal sections
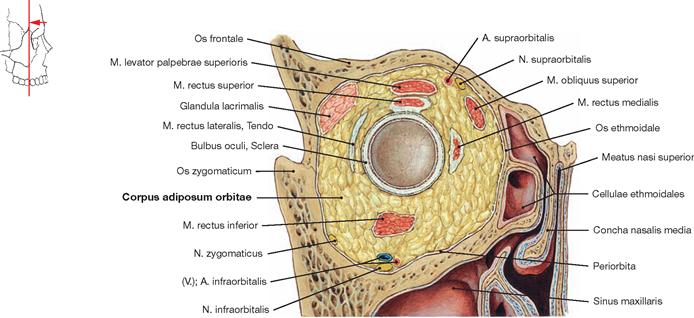
Fig. 9.55 Orbit, Orbita, right side; frontal section through the orbit at the level of the posterior aspect of the Bulbus oculi; frontal view.
The orbital fat body (Corpus adiposum orbitae) surrounds and buffers all structures within the orbit.
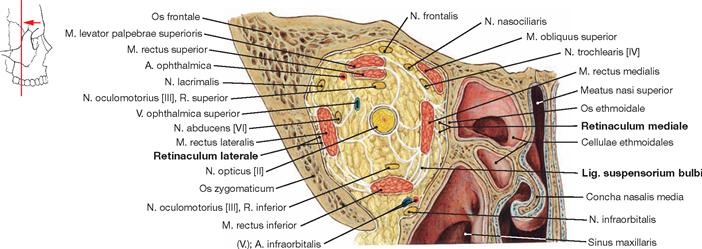
Fig. 9.56 Orbit, Orbita, right side; frontal section through the retrobulbar region of the orbit; frontal view.
The bulbus and the structures of the retrobulbar space connect to the Periorbita and among each other through thin ligaments. Stronger ligaments are the Retinaculum mediale (between the M. rectus medialis and the Periorbita), the Retinaculum laterale (between M. rectus lateralis and the Periorbita), and the Lig. suspensorium bulbi (LOCKWOOD’s ligament, between the M. rectus medialis, M. rectus inferior and the Periorbita).
Eyeball
Eyeball
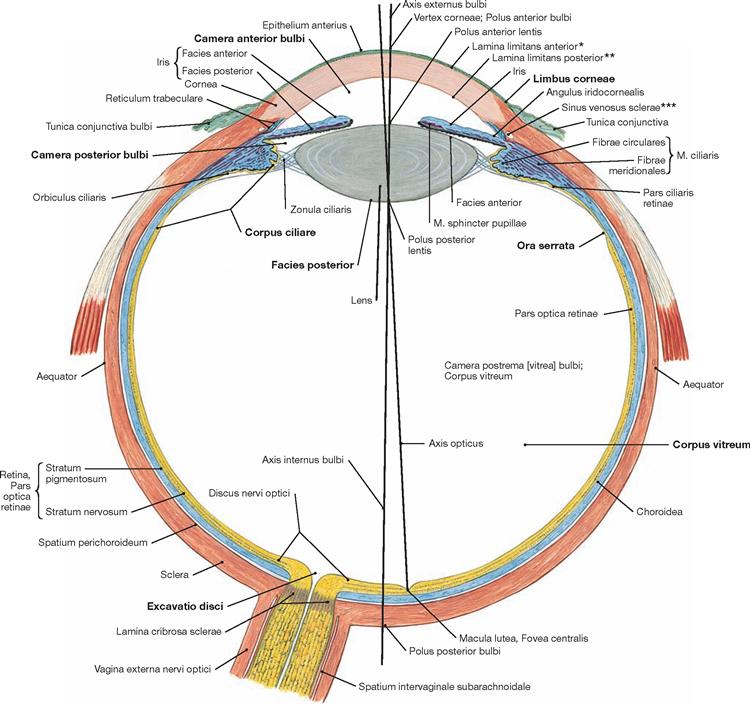
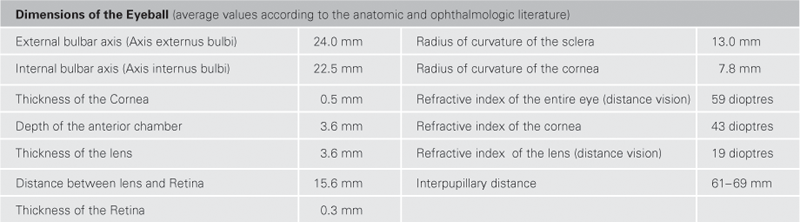
Fig. 9.57 Eyeball, Bulbus oculi, right side; schematic horizontal part at the level of the exit of the optic nerve.
In the anterior part of the eye, the Cornea forms the outer cover of the eyeball (Tunica fibrosa bulbi). Shaped like a convex disc, the Cornea bulges out from the rest of the bulbus. At the Limbus corneae, the Cornea merges into the less curved Sclera which forms the Tunica fibrosa bulbi in the posterior part of the eye. The extra-ocular muscles insert from outside at the Sclera. The Tunica vasculosa bulbi (vascular layer, Uvea) lies beneath the Sclera. Its anterior part consists of the Iris and the ciliary body (Corpus ciliare), while the choroid (Choroidea) forms the posterior part. At the Ora serrata, the ciliary body and the Choroidea meet. The Choroidea represents the most highly vascularized structure in the body. Its blood supply provides nutrients and oxygen to the adjacent retinal layer and is involved in thermoregulation of the eyeball. The Retina is the innermost layer of the eyeball (Tunica interna bulbi). It contains the neural layer (Stratum nervosum; photoreceptive cells) and the pigmented layer (Stratum pigmentosum; pigment cells), and in the anterior part the pigmented layer of the ciliary body and the epithelium of the Iris. The inner space of the eyeball consists of the vitreous body (Corpus vitreum).
* clinical term: BOWMAN’s membrane
** clinical term: DESCEMET’s membrane
*** clinical term: canal of SCHLEMM
Blood vessels of the eyeball
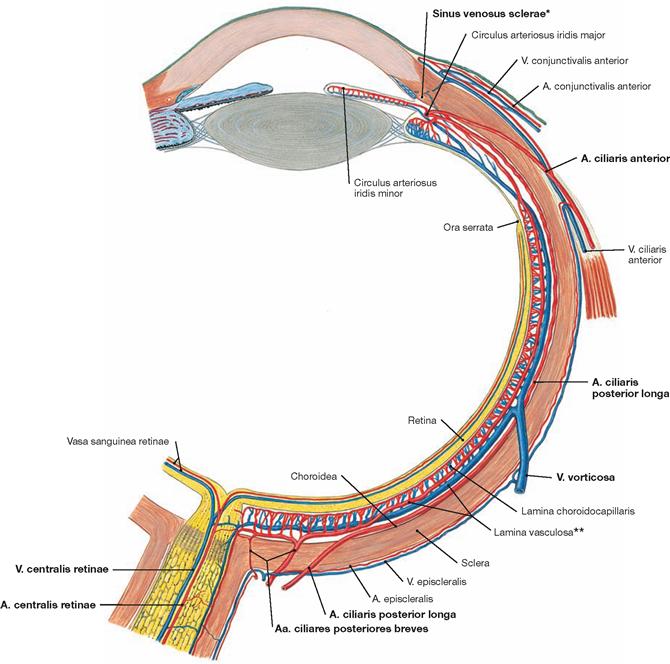
Fig. 9.58 Blood vessels of the eyeball, Bulbus oculi, right side; horizontal section at the level of the N. opticus [II]; superior view.
Arterial blood supply (→ Fig. 9.44). Venous drainage is through the V. centralis retinae and four to eight Vv. vorticosae (vorticose veins; → Fig. 9.45). The latter pierce the sclera posterior to the equator of the eyeball and join the Vv. ophthalmicae superior and inferior.
* clinical term: canal of SCHLEMM
** clinical term: Uvea
Iris and ciliary body
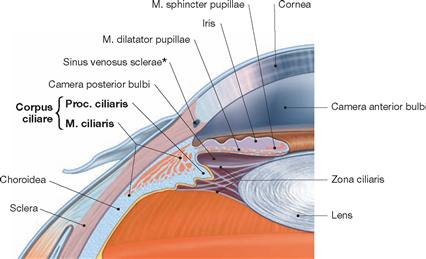
Fig. 9.59 Iridocorneal angle, Angulus iridocornealis, and adjacent structures. [8]
The Cornea, Iris, and Sclera provide the borders for the iridocorneal angle. The epithelial layer of the ciliary body produces the aqueous humour that flows from the posterior to the anterior chamber of the eye. When it reaches the trabecular meshwork at the iridocorneal angle, the fluid is collected in the canal of SCHLEMM (*) and drained into episcleral veins. The M. ciliaris is the major component of the ciliary body and important for accommodation. It consists of meridional (longitudinal, BRÜCKE’s muscle), radial, and circular (MÜLLER’s muscle) muscle cells.
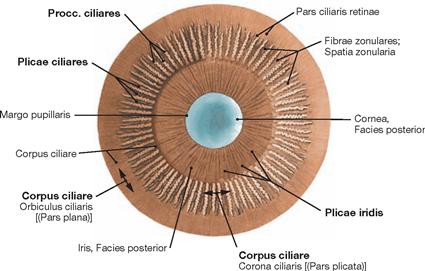
Fig. 9.61 Iris, Iris, and ciliary body, Corpus ciliare; posterior view; after removal of the lens.
The ciliary body is divided into a plane (Pars plana) and a raised part (Pars plicata). The latter serves as origin for approximately 70 ciliary processes (Procc. ciliares). The ciliary body is covered with ciliary epithelium, which, in the area of the Pars plicata, secretes the aqueous humour for the iridocorneal angle. Zonula fibres (suspensory ligaments of the lens, Zonulae ciliares) traverse the distance between the ciliary epithelium and the lens capsule.
Lens
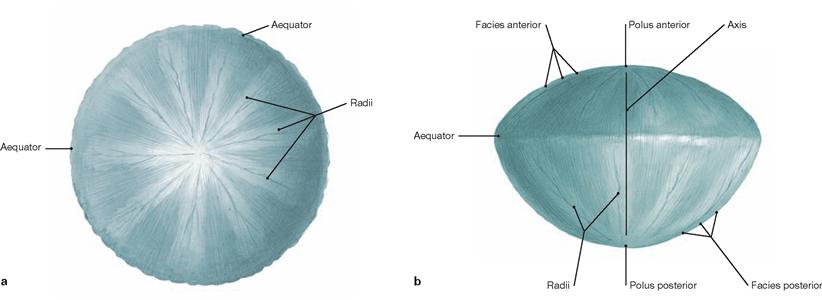
Depending on its particular level of accommodation, the refractive index of the lens varies between 10–20 dioptres (for comparison, the refractive index of the cornea is 43 dioptres but cannot be modified).
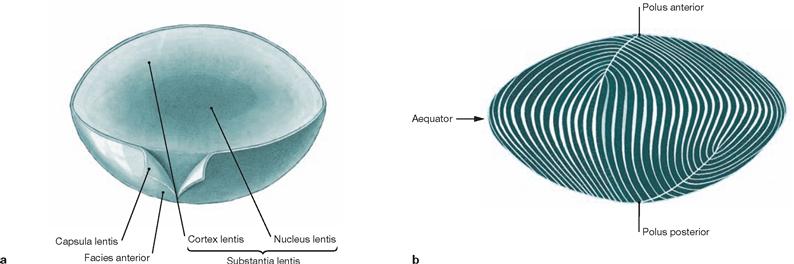
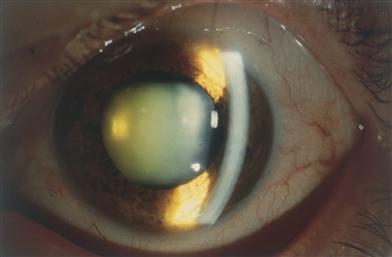
Fig. 9.64 Senile cataract (Cataracta senilis), right side; slit lamp examination.
Shown is a condition of progressive cataract with milky white opacity of the lens. The white curved bar on the right side of the image constitutes the reflection of the cornea.
Retina
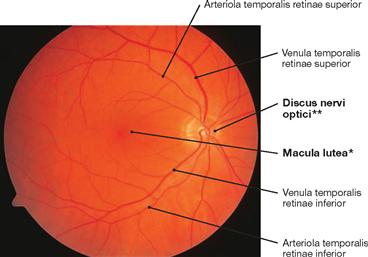
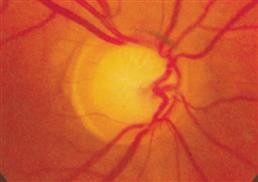
Fig. 9.65 Ocular fundus, Fundus oculi, right side; frontal view; ophthalmoscopic image of the central region.
The examination of the ocular fundus by direct ophthalmoscopy (funduscopy or fundoscopy) allows the clinical assessment of the condition of the Retina, its blood vessels (in particular the A. and V. centralis retinae), the optic disc (Discus nervi optici), as well as the Macula lutea and Fovea centralis (point of central vision). The blood vessels of the Retina (A. and V. centralis retinae and their branches) can be examined and distinguished according to their diameter (arteries – smaller diameter). Normally, the optic disc has a sharply delineated margin, a yellow to orange colour, and contains a central depression (Excavatio disci). At 3–4 mm to the temporal side of the optic disc lies the Macula lutea (contains the highest concentration of cone cells for colour vision). Numerous branches of the Vasa centralia retinae converge in a radial fashion onto the Macula, but fail to reach the centre (Fovea centralis). The latter is supplied by the Choroidea.
* clinical term: Macula lutea
** clinical term: optic disc or blind spot (discus = Papilla nervi optici)
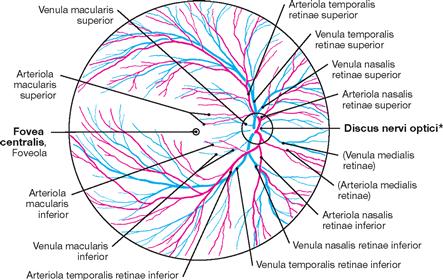
Fig. 9.66 Ocular fundus, Fundus oculi, and blood vessels of the retina, Vasa sanguinea retinae, right side; frontal view; schematic drawing of the course of the blood vessels.
* Papilla nervi optici
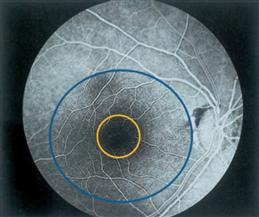
Fig. 9.67 Ocular fundus, Fundus oculi, right side; frontal view; fluorescence angiography during the arteriovenous phase with anatomic landmarks: Macula (blue circle); Fovea (yellow circle). [15]
Orbit, MRI
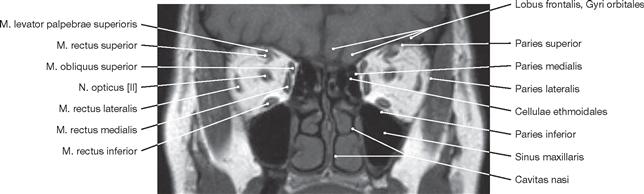
Fig. 9.69 Extra-ocular muscles, Mm. bulbi; magnetic resonance tomographic image (MRI), frontal section of a healthy individual at the level of the orbital centre; frontal view.
The close topographical relationships of the orbit with the Sinus maxillaris, Lobus frontalis, Cellulae ethmoidales, and M. temporalis (not indicated) are clearly visible.
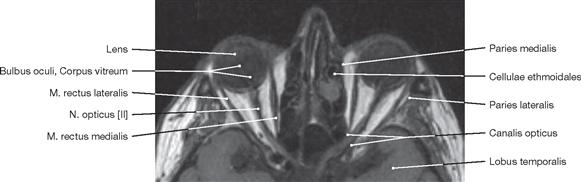
Fig. 9.70 Eyeball, Bulbus oculi, and extra-ocular muscles, Mm. bulbi; magnetic resonance tomographic image (MRI), transverse section of a healthy individual at the level of the N. opticus [II]; superior view. This sectional plane displays the slightly contorted course of the N. opticus [II]. The extra length of the nerve serves as reserve during the movements of the eyeball.
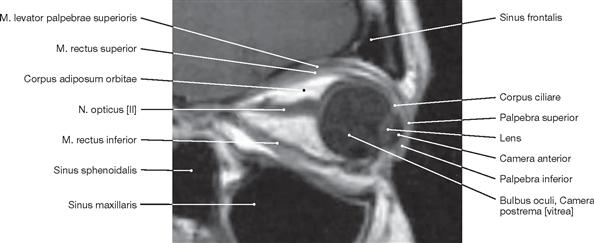
Fig. 9.71 Eyeball, Bulbus oculi, and extra-ocular muscles, Mm. bulbi; magnetic resonance tomographic image (MRI), sagittal section of a healthy individual at the level of the N. opticus [II]; lateral view.
MRI is an imaging technique ideally suited for the visualisation of the bulbar and retrobulbar space because the tissues of both regions provide distinctly different contrast ratios.
Visual pathway
Visual pathway and blood vessels
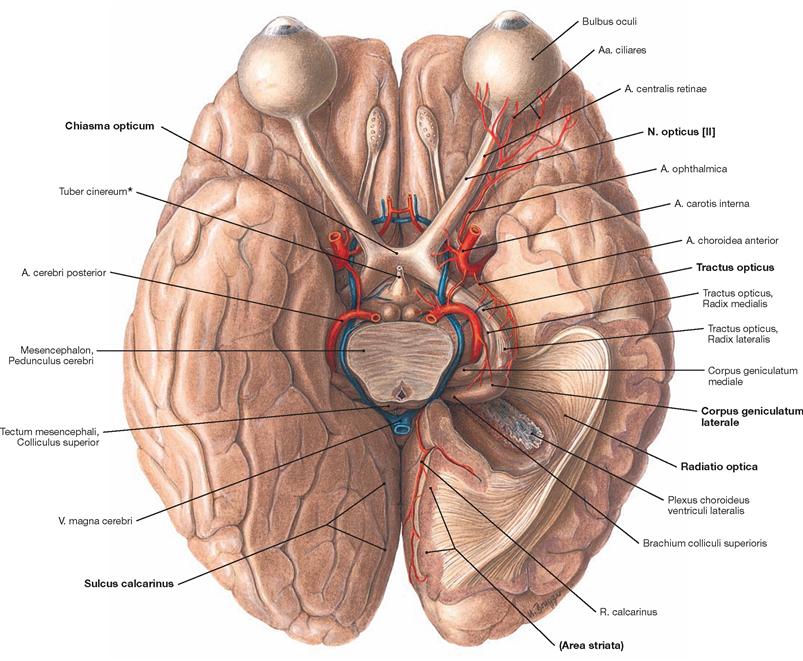
Fig. 9.72 Brain, Cerebrum, and blood supply of the visual pathway; inferior view. The pituitary gland has been removed at its infundibulum (*). The pituitary gland lies in close proximity to the Chiasma opticum.
The visual pathway originates within the retina and contains the first three neurons and interneurons (horizontal cells, amacrine cells). The different cell layers are (from outside to inside):
1st Neuron: photoreceptor cells of the retina (cone and rod cells)
2nd Neuron: bipolar ganglion cells of the retina (perikarya in the Ganglion retinae) which receive signals from the photoreceptor cells and transmit these signals to a multipolar ganglion cell (3rd Neuron)
3rd Neuron: multipolar ganglion cells of the retina (perikarya in the Ganglion opticum).
This principle network structure of three neurons forming an intraretinal chain only applies to the cone cells. Up to 40 rod cells converge their signals onto one bipolar cell and this cell will then transmit these signals indirectly, with the help of amacrine cells (20–50 different types of these cells are described in the literature), to one multipolar ganglion cell.
The axons of the Ganglion opticum extend primarily to the Corpus geniculatum laterale (Radix lateralis) although several fibres also extend into the Area pretectalis and into the Colliculus superior (Radix medialis) as well as to the Hypothalamus. The fibres run within the N. opticus [II] to the Chiasma opticum, where the fibres from the nasal part of the Retina cross to the opposite side. The fibres from the temporal part of the Retina do not cross. Each Tractus opticus contains fibres which transmit information from the contralateral half of the visual field.
4th Neuron: Its axons travel primarily from the Corpus geniculatum laterale to the areas 17 and 18 of the cerebral cortex (Area striata) in the region surrounding the Sulcus calcarinus.
Visual pathway
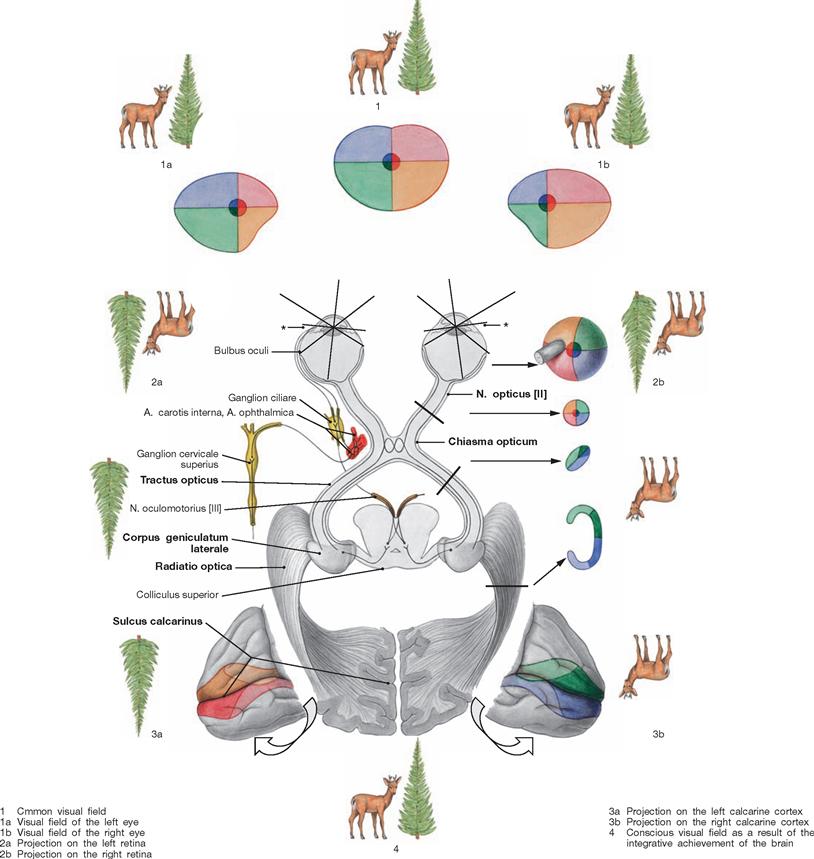
Fig. 9.73 Visual pathway; schematic overview; superior view.
The central vision field has a disproportionately large projection field.
The deer and the fir tree demonstrate how images are transmitted from one part of the visual pathway to the next. It is only at the level of the visual association cortices, that the image is perceived as it presents in front of our eyes. The different colouration of the visual quadrants serves to illustrate the way in which the informations of these visual areas are transmitted and presented in the visual pathway and on the visual cortex.
* plane of refraction of light