Concepts of Health, Illness, Stress, and Health Promotion
Upon completing this chapter, you should be able to:
1 Compare traditional and current views of the meanings of health and illness.
2 Describe what the word “health” means to you.
3 Define what “sickness” means to you.
4 Discuss why nurses need to be aware of any cultural, educational, and social differences that might exist between themselves and their patients.
5 Compare cultural/racial differences in disease predisposition and communication between the main cultures and different races.
6 List the components of holistic health care.
7 Identify the four areas of human needs and give an example within each level of need.
8 Identify ways in which the body adapts to maintain homeostasis.
9 Explain why a particular stressor may be experienced differently by two people.
10 List the common signs and symptoms of stress.
11 Identify four ways in which a nurse can help decrease stress and anxiety for patients.
1 Observe patients during the data-gathering process and interview process and determine their views on health and illness.
2 Recognize cultural differences in health care concepts and behaviors in the clinical setting and be able to share those observations with fellow students.
3 Determine a patient’s status on Maslow’s hierarchy during a clinical experience.
4 Describe alterations in homeostasis as observed in the clinical setting.
5 Document observations about stress-reduction techniques used by staff or patients during a clinical experience.
acute illness (p. 14)
adaptation (p. 14)
asymptomatic ( , p. 16)
, p. 16)
autonomic (p. 21)
chronic illness (p. 14)
convalescence ( , p. 14)
, p. 14)
coping (p. 16)
defense mechanisms (p. 25)
disease (p. 13)
etiology ( , p. 14)
, p. 14)
health (p. 13)
hierarchy ( , p. 18)
, p. 18)
holistic ( , p. 18)
, p. 18)
homeostasis ( , p. 21)
, p. 21)
idiopathic ( , p. 14)
, p. 14)
illness (p. 13)
maladaptation ( , p. 14)
, p. 14)
primary illness (p. 14)
secondary illness (p. 14)
self-actualization (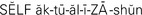 , p. 21)
, p. 21)
stress (p. 18)
stressor (p. 21)
terminal illness (p. 14)
wellness (p. 14)
HEALTH AND ILLNESS
The word “health” means many different things to people. For some health is the absence of disease (pathologic process that causes illness); for others it means optimum functioning on every level. “Health” comes from a word that means “wholeness.” According to the Miller-Keane dictionary, health is “a relative state in which one is able to function well physically, mentally, socially, and spiritually in order to express the full range of one’s unique potentialities within the environment in which one is living.”
It is important to define what you believe health and illness (disease of body or mind) to mean, because your perception of these terms influences what you say and do when caring for patients. Because of cultural, educational, and social differences, you and the patient could have totally different ideas about health and illness and what constitutes “good” health and effective health practices. Before working with patients to accomplish health care goals, try to discover their beliefs about health and illness.
TRADITIONAL VIEWS OF HEALTH AND ILLNESS
The traditional view of health in Western culture was influenced by Plato, Aristotle, and other philosophers who were concerned only with biologic well-being . For many years an acceptable definition of health was simply “the absence of disease.”
In 1946 the World Health Organization redefined health as “the state of complete physical, mental, and social well-being and not merely the absence of disease or infirmity.”
In 1974 a change was finally made in the Federal Employees Compensation Act to reimburse federal employees for treatment by psychologists and psychiatrists. Treatment of mental illness became recognized as a legitimate medical cost. Following the lead of the federal government, other third-party payers (such as insurance companies) made similar changes in the 1970s. This willingness to pay for medical care for illnesses other than clearly defined physical diseases reflected a new and expanded understanding of the nature of health.
From birth to death, the health status of an individual can vary from day to day or even hour to hour. People who are partially or completely paralyzed, suffering from a chronic (persisting for a long time) illness, deaf or blind, or living with an anatomic defect may think of themselves as fairly healthy and lead full and productive lives. None of these people can be labeled as “sick,” nor can any one of them be called completely healthy. There are others who have no identifiable organic disease who nevertheless do not feel well and are not able to live their lives to the fullest.
Illness is a pronounced deviation from normal health (sickness). Illness is an unavoidable, common part of life. We all occasionally have a cold or the flu. Illness is a personal thing; it is subjective. Only the person can tell you if she feels ill. Illness may have a detectable basis in disease or trauma or it may not. Disease is a pathologic process with a definite set of signs and symptoms; disease causes illness.
An acute illness is one that develops suddenly and resolves in a short time. Intestinal flu is an example of an acute illness. Chronic illness, such as hypertension, tends to develop slowly over a long period and last throughout life. A terminal illness is one for which there is no cure available; it ends in death. In the terminal phase of illness, death usually occurs within a short period, such as a few months, weeks, or days.
A primary illness is one that develops without being caused by another health problem. A secondary illness results from or is caused by a primary illness. Peripheral vascular disease resulting from diabetes is an example of a secondary illness and occurs because of the effect diabetes has on blood vessels.
Some diseases are inherited (genetic) or congenital (present at birth). Sickle cell anemia is an inherited disease. Fetal alcohol syndrome (FAS) is a congenital disorder caused by the intake of alcohol during pregnancy. An idiopathic illness is one for which there is no known etiology (cause).
STAGES OF ILLNESS
Illness occurs in stages; there is a transition stage (onset), an acceptance stage (sick role), and a convalescence stage (recovery). When experiencing illness, people act in ways called illness behaviors. These behaviors include how people monitor the body, define and interpret symptoms, seek health care, and follow advice and self-care measures to regain wellness (physical and mental well-being). Illness behavior varies according to the stage of illness and the beliefs of the individual.
Transition Stage
The onset of illness may consist of vague, nonspecific symptoms. During this period one may deny feeling ill, but recognize that symptoms of an illness are present. Acknowledgment of a health problem occurs. As symptoms continue or worsen, self-medication may be used or medical assistance may be sought.
Acceptance Stage
Acceptance occurs as denial of illness stops and a “sick role” is assumed. This involves acknowledging illness and engaging in measures to become well. There is withdrawal from usual responsibilities and roles. Remedies from the pharmacy or home medicine cabinet may be used, or the person may go home and go to bed. If symptoms continue to worsen, medical treatment may be sought. Some people will put off going to a physician as long as possible. Fear of what the problem may be and of undergoing examination and diagnostic procedures often causes anxiety.
Convalescence Stage
Convalescence is the process of recovering after the illness and regaining health. If the illness or disease is chronic, a total recovery phase is replaced by adaptation (adjustment in structure or habits) to limitations and positive use of remaining capabilities, or by maladaptation (lack of adjustment).
CURRENT VIEWS OF HEALTH AND ILLNESS
Contemporary definitions of health and illness are more abstract and philosophical, and therefore more vague, than the precise definitions based on measurable criteria. In general, being healthy means being able to function well physically and mentally and to express the full range of one’s potentialities within the environment in which one is living.
This concept takes health beyond the level of meeting basic physiologic needs and recognizes people’s need to accept themselves as worthwhile, to live in harmony with others, and to express their personalities fully, thereby becoming more self-actualized (reaching one’s full potential) and fulfilled. In the words of René Dubos, “Health is primarily a measure of each person’s ability to do (what he wants to do) and become what he wants to become.”
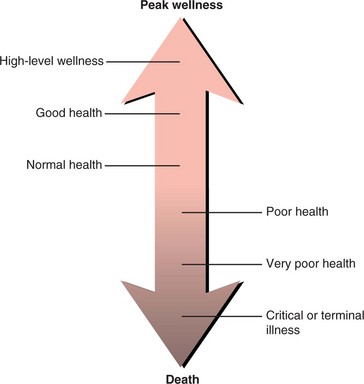
Current views of health and illness are based on the thoughts and ideas of men such as René Dubos and Halbert Dunn, who urged people to look at these concepts in a new and different way. Realizing that people are dynamic beings whose state of health changes daily and even hourly, they suggest that it is better to think of each person as being located somewhere on a graduated scale or continuous spectrum (continuum) ranging from obvious disease through the absence of detectable disease to a state of optimum functioning in every aspect of life. Figure 2-1 shows a model for the current view of health and illness as dynamic states of being. The phrase high-level wellness was first used by Dunn to signify the ideal state of health in every dimension of the human personality. Dunn does not consider high-level wellness to be the same as good health. He thinks of health as being a relatively passive state, one that a person enjoys because of hereditary and environmental factors that are essentially beyond the control of the person. High-level wellness, on the other hand, is described as a dynamic and active movement toward fulfillment of one’s potential.
In Dunn’s view, each person accepts responsibility for and takes an active part in improving and maintaining her own state of wellness. A person with a high level of wellness does so by virtue of her own efforts. A person who works at achieving high-level wellness improves her self-esteem, is able to accept and give love and concern for others, and lives each day of her life to its fullest insofar as possible.
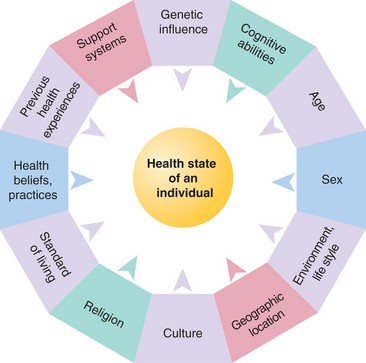
In the contemporary view, health and illness are relative, rather than absolute, terms. This means that each person’s state of health depends on many different things beyond biologic fitness. Figure 2-2 shows the variables that influence health and illness. Among the personal, psychosocial, and spiritual factors that influence a person’s state of health at any given moment are the values and beliefs about what it means to be healthy and what it means to be sick, the image of oneself, and the ability to reach out and relate to others and to search for and find meaning and purpose in life. From this point of view, health is never a static state.
IMPLICATIONS OF CURRENT VIEWS
These views of the nature of health and illness have greatly added to the complexity of health care. They challenge the traditional single-minded goal of curing disease. In the delivery of nursing care, current concepts of health and illness reinforce the value of nursing as primarily a caring profession.
A common theme in all of nursing theory is that nursing is concerned with helping people cope with adverse physiologic, psychosocial, and spiritual responses to illness, rather than with treating the illness itself. Although the nurse is involved in the curing of those who are ill or injured, this goal is primarily under the control of the physician. Nurses have traditionally been concerned with promoting good health habits in their patients and giving them the support they need to cope with illness. Since Florence Nightingale, nurses have encouraged a wholesome environment in the home, hospital or other health care agency, and community.
The nurse knows that it is ultimately the inner resources of the individual that determine whether she will be able to function at an optimum level.
Nurses seek to help patients utilize their coping (adjusting to or accepting challenges) abilities to best advantage and to adapt to conditions that cannot be changed. The patient with a chronic and incurable illness can be helped to minimize its harmful effects and can be encouraged to continue to set and attain goals in other dimensions of life. A patient who is permanently disabled because of traumatic injury is not necessarily limited in every other aspect of life, and it is possible for terminally ill patients to live their final days more fully and perhaps with greater meaning and purpose than during any other stage of life.
THE CONSUMER CONCEPT OF HEALTH AND ILLNESS
Nursing places a high value on working with people to help them become more independent and better able to meet their own health care needs. To achieve the goals of health promotion, disease prevention, and recovery from the effects of illness and injury, people must be both able and willing to accept responsibility for their health-related behavior.
HEALTH AND ILLNESS BEHAVIOR
Health and illness behaviors are based on what a person knows and believes about health and illness and how one’s own health is assessed.
Health behavior can be defined as any action undertaken in order to promote health, prevent disease, or detect disease in an early, asymptomatic (without symptoms) stage. Illness behavior is any activity a person takes in order to determine her actual state of health and to seek a suitable remedy for a health problem.
Some examples of health behavior might include watching dietary intake to avoid becoming overweight, engaging in a regular program of exercise, taking care to obtain available immunizations against communicable diseases, and monthly self-examination of the breasts or testes. These behaviors are encouraged by health care providers because they are perceived by them as valuable. If a patient does not undertake these behaviors when they have been recommended, then the nurse must consider whether there is a conflict in values between health care personnel and the patient. Because of cultural and personal differences, not everyone views certain health practices and behaviors in the same way. What one eats or refuses to eat can be influenced by religious and cultural beliefs. Whether one allows oneself or one’s children to be immunized can be dictated by religious convictions and restrictions. Early detection of disease can depend on a person’s knowledge about normal physiology and psychology, and signs of abnormal conditions of the body and mind.
Illness behavior is equally complex. Because it involves actions undertaken by an ill person, the underlying question to be answered by the person is “What does it mean to be ill?” or “How do I know I am ill?” The nurse must consider what the person knows about health and deviations from health, and what is believed to be an appropriate remedy for the health problems. Examples of illness behavior include consulting a physician or nurse, consulting the pharmacist, visiting a neighborhood health care clinic, and taking prescribed medications.
CULTURAL INFLUENCES ON CONCEPTS OF HEALTH AND ILLNESS
Great cultural diversity in the United States brings many differences between the values and practices of various ethnic and minority groups. Effective nursing care, whatever the setting, is dependent on an appreciation of these differences and adjustments in care to accommodate them.
Some areas in which differences among racial and ethnic groups are most apparent are attitudes and practices related to birth, death, and general health care; susceptibility to specific diseases; responses to pain and suffering; personal hygiene and sense of privacy; and adjustment to life changes. Additionally, the words and concepts used to communicate feelings and behaviors related to health practices and remedies for sickness are quite different in each cultural group (Table 2-1).
Table 2-1
Cross-Cultural Examples of Cultural Phenomena Affecting Nursing Care
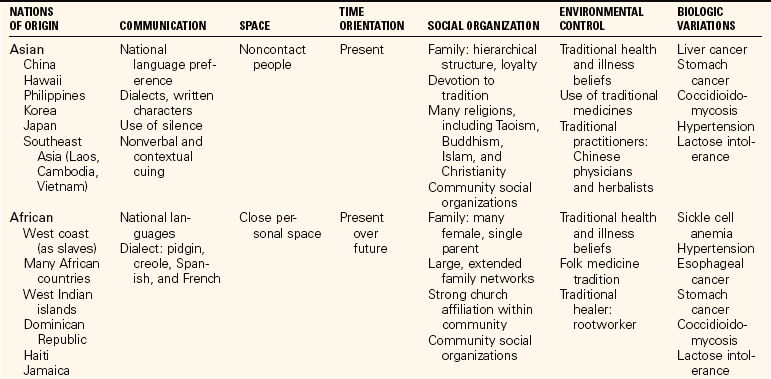
From Potter, P.A., & Perry, A.G. (2005). Fundamentals of Nursing (6th ed.). St. Louis: Elsevier Mosby. Compiled by Rachel Spector, RN, PhD.
The attitudes, beliefs, and practices of a cultural group may or may not conform to the nurse’s idea of what is a productive and beneficial action of health promotion or illness prevention (Cultural Cues 2-1). Typically, health care professionals in the United States and other countries influenced by Western medical science have been taught according to the values and beliefs of a white, middle-class society. At the same time, the cultural groups that they care for may not necessarily share these values and beliefs. Unless this conflict is resolved in some way, there may be a problem in communication and in meeting the goals of health care. The problem for the nurse will occur because of unrealistic expectations of what the patient can be convinced to do or of what can be done for her. The patient may experience problems because the quality and type of care desired may not be delivered.
Many cultural health beliefs are based on folk medicine passed down through the generations within a culture. Many cultures have their own healers’for example, a medicine man, shaman, or curandero. Those within the culture often seek the advice of this person before going to a licensed health professional. Beliefs in the various cures that the cultural healer suggests are very powerful. Respect for the person’s cultural beliefs in all areas is necessary on the part of the nurse in order to gain the trust of the patient and for advice and teaching to be effective.
Assessment must be done without criticism, with an open mind, and with active listening. Judgmental terms such as noncompliant, uncooperative, ignorant, lazy, or unmotivated should not be used to describe another person’s health behavior.
There should be no conditions or strings attached to the unspoken contract between the nurse and the patient. The nurse need not condone what a patient is doing or not doing to maintain or restore health. The nursing point of view may be respectfully conveyed to the patient. Each patient must be dealt with as a unique individual whose concepts of health and illness and health care might be different from one’s own.
THE HOLISTIC APPROACH
Nurses take a holistic approach to caring for the sick and promoting wellness. A holistic approach is one that considers the biologic, psychological, sociologic, and spiritual aspects and needs of the person. The current focus on holism was stimulated by Jan Smuts, a noted South African who formulated a philosophical theory of holism. The value we place on human life, our ability to deal with sickness and death, and our decisions about how to behave toward other people are all profoundly influenced by our basic beliefs about other humans and our relationships with them. Some basic beliefs central to the holistic approach are as follows:
• Each person is a unique integration of body, mind, and spirit, and the unified whole is more than the sum of the body parts. A change in one aspect of a person’s life brings about change in every aspect of her being and alters the quality of the whole.
• Each person has potential for growth in knowledge and skills and in becoming more loving toward herself and others.
• Humans are naturally inclined to be healthy; each of us has responsibility for our own well-being, self-healing, and self-care.
• The “person” of an individual belongs to herself; therefore, decisions about what happens to that person rightfully belong to the owner.
• The focal point of healing efforts is the person, not the disease or injury.
• The relationship between health care professionals and their patients should be one of mutual cooperation. Health care providers intervene on behalf of the adult patient only when their help is sought by the patient or when health needs cannot be met.
In holistic health care, traditional methods of surgical intervention and drug prescription are being combined with or replaced by acupuncture, acupressure, biofeedback, meditation to reduce tension and stress (biologic reactions to an adverse stimulus), and various relaxation techniques for the management of pain, to name but a few of the less traditional approaches. Chiropractic care, once looked upon as questionable, is now covered by many insurance companies. Insurance companies are becoming more inclined to pay for acupressure for treatment of pain.
MASLOW’S THEORY OF BASIC NEEDS
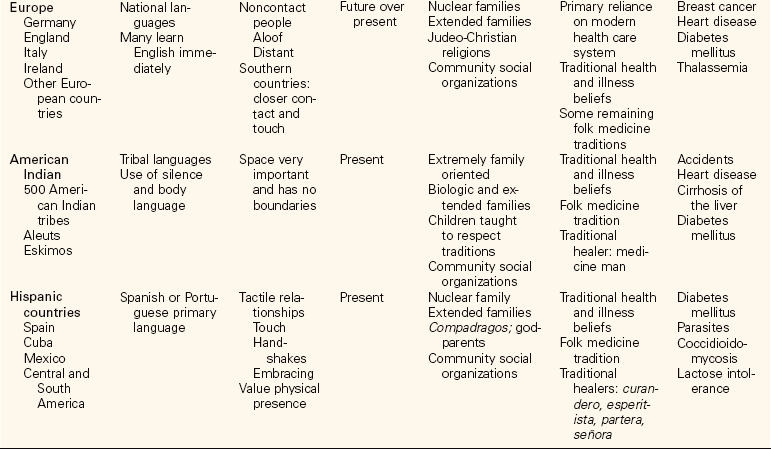
Nurses attempt to assist patients to meet their needs and thereby achieve a higher level of health. People respond to needs as “whole” and integrated beings. Abraham Maslow, a psychologist, identified basic needs necessary for existence and higher level needs for healthy integration of the whole being. He proposed a hierarchy of human needs as an explanation for the forces that motivate human behavior. A hierarchy is defined as the arrangement of objects, elements, or values in order of their importance. Many nursing programs are built on Maslow’s basic needs. Figure 2-3 shows Maslow’s original hierarchy of needs and an adaptation of the hierarchy used to determine priorities of nursing care. Theoretically, the basic physical needs such as food, air, water, and rest must be satisfied before the higher emotional-level needs emerge. This is true in general, but the order in which needs are felt and become important to an individual is different from person to person and from situation to situation.
FIGURE 2-3 A, Maslow’s hierarchy of needs. B, Evolving hierarchy of needs adapted by nursing to help to determine priorities of care.
Once a human need is met, it does not remain satisfied forever. This is obviously true in regard to food, water, air, and other basic first-level physiologic needs. As well as continually needing food, people need continued assurance that they are important, held in es teem, safe, and secure from harm. The patient who is receiving medications and treatments for her illness also needs personal contact with loving and caring people.
Physiologic Needs
Fundamental physical needs are essential to maintaining life. The first physiologic need is for oxygen and is immediately followed by the need for adequate cardiovascular function to supply the tissues with blood. The needs for adequate nutrition and for elimination come next.
Basic safety needs are almost as important as physiologic needs. If the patient cannot be protected from the dangers of a being burned or a severe fall, attending to her physiologic needs is useless. Protection from physical harm, from a nursing standpoint, is often equivalent in importance to physical needs.
The need for rest comes next and includes freedom from pain, which can greatly interfere with rest. Hygiene needs follow the need for rest because good hygiene is a part of providing comfort and adds a measure of safety and protection against the invasion of bacteria.
Musculoskeletal activity is also a basic physiologic need, because without activity of the muscles and joints, atrophy and deformity will occur, preventing normal function of the muscles and joints. Nurses therefore attend to assisting the patient with movement and ambulation or perform passive range-of-motion exercises for immobile patients.
Sexual expression is a physiologic and psychological need. Survival of a group in society clearly depends on sexual intercourse as a means of procreation to extend the existence of the group. Gratification of sexual needs fits best in the areas of self-esteem and love.
Security and Belonging
Once basic physiologic needs are satisfied, the needs for security and belonging demand attention. Security for patients mainly depends on the reassurance that their physiologic and safety needs will be met. Security also includes protection from psychological harm; freedom from anxiety and fear; and the need for structure, order, and a peaceful environment. The hospitalized child and the elderly person are particularly susceptible to stress created by an unfamiliar, disorderly, or hazardous environment. People value order, routine, and rhythm in their daily lives and thrive more readily in an environment in which they believe that these things are present, although it should be remembered that orderliness and routine are much more important to some people than to others.
Adults who suddenly become ill might be anxious about finances, loss of control, change in their body image, continuation of employment, and what will happen to them in the future if they must cope with the effects of a permanently disabling illness or injury. Therefore, emotional support from the nurse is very important. Active listening on the part of the nurse is essential in meeting patients’ security needs because, to feel secure, they must feel that their needs are being accurately perceived.
Each person needs to feel that she belongs or is attached to others. People need to feel cared about, and they function best if they feel a sense of community with others. Some social interaction is essential to a sense of well-being and psychological balance (Figure 2-4).
Communication is the method by which human interaction takes place and is therefore very important. Providing a means of communication, encouraging sharing of thoughts and feelings, and therapeutically interacting with the patient is the core of good nursing practice. One can perhaps meet the basic physiologic needs of a patient without communication, but it is impossible to meet other needs if good communication is not present. Adequate feedback and clarification and validation of communication are essential.
Self-Esteem and Love
Self-esteem and love are interrelated, since it is apparent that one cannot truly love others until one first loves or accepts oneself. Self-esteem develops from feelings of independence, competence, and self-respect and from recognition, appreciation, and respect from others. One’s employment, or work, and various roles (e.g., as husband/wife, father/mother, brother/sister, child, community leader, etc.) all contribute to self-esteem. For many, spiritual belief systems are an integral part of the sense of self and of one’s relationship to the universe. Gratification of sexual needs contributes to the feeling of wholeness of the individual and to one’s identification and behavior as a male or a female.
Freedom from boredom, mental stimulation, motivation to seek knowledge, and learning play a role in self-esteem also. People have a desire and a need to explore the environment and universe around them. Illness often brings about the need for new knowledge in order to provide for adequate self-care. Without this necessary learning, self-esteem will decrease. The nurse must become the teacher, helping the patient to meet these needs.
Balance in a person’s life is brought about by the ability to enjoy leisure activity, to play, and to seek things that bring a measure of happiness.
Illness and adversity, particularly physical adversity, often damage the patient’s self-esteem. Nurses can be instrumental in helping to rebuild feelings of competence, independence, and self-respect.
Love consists of both giving and receiving. Without love and attention, an infant will withdraw and gradually die despite having its physiologic needs met. Extreme, prolonged deprivation of love and esteem can bring about neurotic behavior and organic illness.
Intimacy’the greater degree of connectedness, of feeling that one understands and is understood by another’is one of the fibers of love. The achievement of intimacy is the developmental task of the teenager and young adult. However, illness can greatly interfere with intimacy for all adults. Nurses need to assist patients to find ways for intimacy needs to be fulfilled, especially in patients with long-term or chronic illnesses.
Self-Actualization
Self-actualization (reaching one’s full potential) is an area to which people do not advance until the physiologic, security and belonging, self-esteem, and love needs have been met. Self-actualization occurs when individuals are very comfortable with themselves and are certain of their beliefs and values. These people are self-reliant, flexible, and open to new ideas; have sought knowledge and truth; and function close to their full potential. Creative expression, whether in an area of performance or appreciation, is part of the self-actualization process. Self-actualization is an ongoing process, not something reached at a particular point in time. Nursing actions that facilitate self-actualization are pertinent mainly during rehabilitation periods, when the nurse assists the patient to strive to achieve full potential.
Humans are rational, decision-making beings. A person is believed to want to have control over her life, even when choosing dependence over independence. Although a person is free to choose, there is no guarantee that every choice will be a wise one. Patients can and do decide not to take physician-prescribed medications, to continue drinking to excess, or to ignore advice of any kind offered by health care professionals. Nurses must understand that behavior is based on what a person perceives to be a need and how highly that person values satisfaction of that need.
HOMEOSTASIS
Homeostasis is a term first coined by W.B. Cannon in 1939 to describe a tendency of biologic systems to maintain stability of the internal environment by continually adjusting to changes necessary for survival. The suffix -stasis indicates a static, or balanced state, involving continual adaptation, movement, and change. The term implies a steady state or equilibrium in which there are variations within set limits. These variations take place in a predictable manner’for example, variations in body temperature, changes in the acidity and alkalinity of body fluids, hormonal production and release, and other changes that occur during every 24-hour period. In health, continuous adaptation and change must take place in the internal environment in order to maintain its steady state (equilibrium). Another word for homeostasis is “equilibrium.”
In order to enjoy some degree of health and sense of well-being, one must adapt to factors in the external environment. In other words, one needs to be in harmony with elements outside oneself by interacting with and integrating various elements into one’s life. These elements include the physical, biologic, and psychosocial factors in the world in which one lives and works.
To live in harmony with external environmental factors requires both adaptability and stability.
Wellness is maintained or regained, at least in part, when one is able to keep a sense of balance while adapting to factors that can upset that balance. These factors include such life experiences as socialization, education, mental and physical stress, satisfactions, and rewards. Perhaps one of the most crucial of factors in today’s world is change. When change is required, additional stress is put on a person’s inner resources, and this in turn can increase susceptibility to illness. Health and illness are dynamic states; therefore, adaptability to a changing external environment is essential to stability and health. Adaptation that results in illness is considered maladaptation.
When the equilibrium of the body is disturbed, stress occurs. Stress is the sum of biologic reactions that take place in response to any stressor (adverse stimulus). The stressor may be physical, mental, or emotional and can come from within the body or from the environment. Stress disturbs the homeostasis of the organism and causes the body to attempt to adapt. Physical or psychological illness may result from excessive stress or ineffective coping mechanisms.
ADAPTATION
To adapt is to respond to change. The systems of the body have self-regulatory mechanisms to maintain homeostasis. These mechanisms require pathways of communication between the brain and the various body systems. Coordination of the central nervous system, the autonomic (not subject to voluntary control) nervous system, and the endocrine system is required for the body to adjust, adapt, and maintain equilibrium.
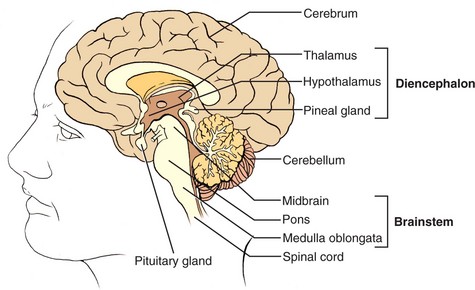
The central nervous system, consisting of the brain and spinal cord, coordinates adaptation within the body. The cortex, the thinking part of the brain, communicates with the midbrain and brainstem, which contain many of the structures involved in adaptation and maintenance of physiologic functions. Along with the action of the endocrine glands, these structures regulate breathing, heart action, blood pressure, body temperature, hunger, and sleepiness (Figure 2-5).
The reticular activating system (RAS), a bundle of nerve fibers in the brainstem, transmits messages to the cortex from the sensory receptors of the body and carries messages back to the hypothalamus in the midbrain to regulate physiologic functions. The hypothalamus helps regulate the autonomic nervous system and the secretion of hormones by the endocrine system.
The autonomic nervous system regulates physiologic functions that are essentially automatic and beyond voluntary control. It is divided into the sympathetic and parasympathetic nervous systems. These two divisions act like the gas and the brake pedals of a car as they increase or decrease physiologic response of the systems and organs of the body. For example, during vigorous exercise, the sympathetic nervous system sends messages to the bronchi of the lungs to dilate so that more oxygen can be delivered. In contrast, when stepping out into bright sunlight, the parasympathetic system relays messages to the muscles controlling the iris of the eye to constrict the pupil so that less light is allowed to hit the retina.
When the brain perceives a situation as threatening, the sympathetic nervous system stimulates the physiologic functions needed for fight or flight. This is the type of reaction that occurs when you are suddenly confronted by a very large, snarling dog on a walking path. The alarmed individual becomes more alert, breathes more deeply, and has muscles poised for fight or flight, and the heart pumps harder. Once the threatening situation is over, the parasympathetic nervous system works to restore equilibrium. In certain situations, the parasympathetic system may be stimulated to slow systems down as a protective measure against a perceived threat.
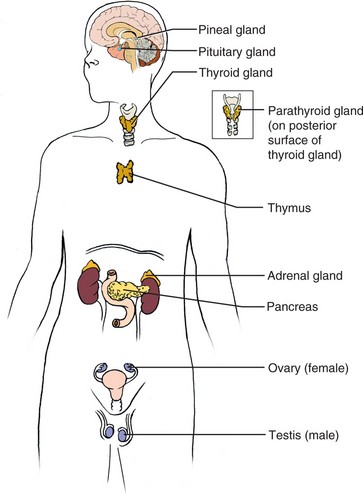
Although the autonomic nervous system reacts immediately to a perceived threat, the endocrine system must become involved to sustain the fight-or-flight state. The glands of the endocrine system produce hormones that act on other organs or systems of the body (Figure 2-6). Initiation of a stimulus for hormone production comes from the cortex of the brain and travels to the hypothalamus. The hypothalamus activates the pituitary gland, which in turn secretes hormones that stimulate the other endocrine glands. As long as the body’s capacity is not overtaxed, the central nervous system, autonomic nervous system, and endocrine system regulate body systems to maintain homeostasis. Table 2-2 presents body responses when a fight-or-flight reaction occurs. Common signs and symptoms of stress are listed in Box 2-1.
Table 2-2
Alarm Reaction: Comparison of Sympathetic and Parasympathetic Actions
| ORGAN | SYMPATHETIC ACTION | PARASYMPATHETIC ACTION |
| Iris of eye | Dilates—pupil becomes larger | Constricts—pupil becomes smaller |
| Bronchial tubes | Dilate—provide greater air flow | Constrict |
| Salivary glands | Stimulate thick secretions—dry mouth | Stimulate profuse, watery secretions |
| Heart | Increases rate and strength of contraction | Decreases rate; no effect on strength of contraction |
| Blood vessels | Generally constrict—increased blood pressure | No effect for many |
| Sweat glands | Stimulate sweat production | No effect |
| Intestines | Inhibit mobility—possible constipation | Stimulate motility and secretion |
| Liver | Stimulates glycogen breakdown for energy | No effect |
| Adrenal medulla | Stimulates secretion of epinephrine and norepinephrine | No effect |
Adapted from Herlihy, B., & Maebius, N.K. (2007). The Human Body in Health and Illness (3rd ed., p. 205). Philadelphia: Elsevier Science.
The General Adaptation Syndrome
In 1950 Hans Selye, a Canadian physician, published his research-based theories on stress. He found that no matter what the nature of the stressor was, the same nonspecific physical response occurred. The body attempted to deal with stressors by secretion of hormones that caused adaptive responses. Selye concluded that stress plays a role in every disease process because of faulty adaptation (maladaptation) by the body. If the body overreacts in defending itself, there is a surplus of hormones that are favorable to the development of inflammation, and problems such as allergy, arthritis, and asthma may develop. When the body underreacts, too many anti-inflammatory hormones are circulating and serious infection or peptic ulcers may result.
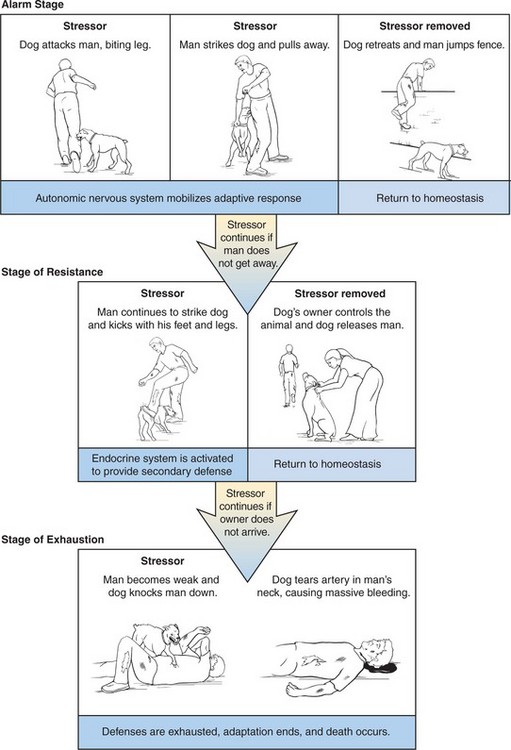
Selye stated that a general adaptation syndrome (GAS) occurs in response to long-term exposure to stress. The stages are the alarm stage, the stage of resistance, and the stage of exhaustion. Brief stress responses result in adjustment by homeostatic mechanisms, and equilibrium is restored. During the alarm stage, hormone release mobilizes the body’s defenses. Nonspecific signs of illness such as a slight rise in temperature, a loss of energy, decreased appetite, and a general feeling of malaise occur. During the second stage, the stage of resistance, the body is battling for equilibrium. If this stage is excessive or prolonged, the response becomes maladaptive and a pathologic condition occurs, which may be in the form of a stress-related disorder. Box 2-2 lists diseases and disorders considered to be stress related.
The stage of exhaustion occurs if the stressor is severe enough or is present over a long enough period of time to deplete the body’s resources for adaptation. Critical illness or death results (Figure 2-7). Examples of stressors that cause the GAS include trauma, burns, infection, severe cold, and emotional upsets.
Selye believed the body adapts to local stressors in similar ways. The local response is called the local adaptation syndrome (LAS). This takes place within a single organ or area of the body, such as when a cut finger becomes inflamed.
THE EFFECTS OF STRESS
We all react or adapt to stress in our own way. What may cause a very mild reaction in one person may cause a much stronger reaction in someone else. A stressor can be helpful or harmful depending on the person’s
• Degree of health and fitness
• Previous life experiences and personality
When there is a total absence of stress, we may become bored and cease to achieve personal growth. Common patient stressors are found in Box 2-3.
Coping with Stress
The body has several types of physiologic defenses. Unbroken skin and an intact immune system that protect us against invasion of viral and bacterial stressors are two examples. Psychological defenses include the personality trait of toughness. Tough people believe that life has meaning and that people can influence the environment, and they see change as a challenge. Hardy people cope well. Coping means adjusting to or solving challenges. Coping mechanisms help us to resist and master stressors. Coping mechanisms are learned and, once used successfully, they become part of our psychological defense armor. There are three types of coping responses:
• Actions or thoughts that change the situation so it is no longer stressful
• Alteration of thoughts to control the meaning of the situation before it triggers a stress response
Ways to achieve these responses are:
• Seeking information (eliminates fear of the unknown)
• Taking direct action (taking yourself away from a dangerous situation)
• Stopping an unhelpful reaction (refraining from shouting or throwing things when angered)
• Discussing the situation with someone from your social support system
• Using defense mechanisms to perceive the situation differently
Defense Mechanisms.: Defense mechanisms are strategies that protect us from increasing anxiety. Defense mechanisms reduce both anxiety and the secretion of stress hormones. Defense mechanisms are used to maintain and improve our self-esteem. Unconsciously using defense mechanisms gives us time to solve the problem and adapt in a positive manner. Using defense mechanisms relieves tension and lessens anxiety. However, they can be overused in a maladaptive way as well. Table 2-3 describes commonly used defense mechanisms and gives examples.
Table 2-3
| DEFENSE MECHANISMS | CHARACTERISTICS | EXAMPLE |
| Repression | Blocking a wish or desire from conscious expression. | You forget the name of someone for whom you have intense negative feelings. |
| Denial | A more serious form of repression. Person lives as though an unwanted piece of information or reality does not exist. There is a persistent refusal to be swayed by evidence. | An alcoholic states, “I do not have a problem with alcohol. I never drink before 5:00 P.M. My stomach problems and liver problems are caused by something else.” |
| Projection | Attributing an unconscious impulse, attitude, or behavior to someone else (blaming or scapegoating). | A man who is attracted to his friend’s wife on an unconscious level accuses his own wife of flirting with his friend. |
| Reaction-formation | An intense feeling regarding an object, person, or feeling is out of awareness and is unknowingly acted out consciously in an opposite manner. | You treat someone whom you unconsciously dislike intensely in an overly friendly manner. |
| Regression | Returning to an earlier level of adaptation when severely threatened. | A child resumes bedwetting, after having long since stopped, when her baby brother is born and fussed over at home. |
| Rationalization | Unconsciously falsifying an experience by giving a contrived, socially acceptable, and logical explanation to justify an unpleasant experience or questionable behavior. | A student who did not study for an examination blames his failure on the teacher’s poor lecture material and the unfairness of the examination. |
| Identification | Modeling behavior after someone else. | A 6-year-old girl dresses up in her mother’s dress and high-heeled shoes. |
| Introjection | A more primitive form of identification. More closely relates to unconscious imitation. | A child who becomes irritable after angry interactions with a parent, taking in (“swallowing whole”) the image of the angry parent, which grows into himself. |
| Displacement | Discharging intense feelings for one person onto another object or person who is less threatening, thereby satisfying an impulse with a substitute object. | A child who has been scolded by her mother hits her doll with a hairbrush. |
| Sublimation | Rechanneling an impulse into a more socially desirable object. You forget the name of someone for whom you have intense negative feelings. | A student satisfies sexual curiosity by conducting sophisticated research into sexual behaviors. |
Adapted from Varcarolis, E.M. (2002). Foundations of Psychiatric Mental Health Nursing (4th ed., p. 26). Philadelphia: Saunders.
Stress Reduction Techniques.: Box 2-4 lists measures that help reduce stress and anxiety in patients. Other measures that help to control the degree of anxiety and reaction to stressors include progressive relaxation, imagery, massage, biofeedback, yoga, and meditation. An additional method of stress reduction is regular physical exercise. Exercise causes endorphin release, which promotes a feeling of well-being and tranquility. More information on these techniques can be found in Chapter 31.
HEALTH PROMOTION AND ILLNESS PREVENTION
A national initiative toward better health was begun in the 1970s. The latest update of direction, goals, and objectives is Healthy People 2010: With Understanding and Improving Health and Objectives for Improving Health (U.S. Department of Health and Human Services, 2000). It is a comprehensive set of objectives for disease prevention and health promotion for the nation and was created by scientists. The overall goals are to (1) increase the quality and years of healthy life, and (2) eliminate health disparities. There are 28 focus areas and more than 400 objectives with a target for improvements to be achieved by the year 2010. Every nurse has a responsibility to patients to promote better health through teaching about illness prevention, periodic diagnostic testing for cancer and diabetes, and safe health practices. Encouraging achievement of appropriate weight, regular exercise, adequate sleep, proper nutrition, quitting use of tobacco products, refraining from recreational drug use, and moderation of alcohol intake should be a standard part of nursing care. Practices to prevent back injury, latex allergy, spread of infectious agents, and needlestick injury help safeguard the health of the nurse.
Illness prevention practices are related to health promotion. They consist of voluntary actions that an individual takes to decrease the potential or actual threat of illness. Such actions are divided into primary, secondary, and tertiary prevention. Primary prevention avoids or delays occurrence of a specific disease or disorder. Secondary prevention consists of following guidelines for screening for diseases that are easily treated if found early or for detecting return of a disease. Tertiary prevention consists of rehabilitation measures after the disease or disorder has stabilized. Health Promotion Points 2-1 lists such behaviors. Following such health practices has been associated with a greater degree of health for persons of any age, sex, or economic status. The United States and Canada have published goals for essential health care services. The priorities in Healthy People 2010 involve teaching for disease and accident prevention, health promotion, and self-care behaviors (see Chapter 9). While caring for patients in different settings, you should always assist patients to mobilize and maintain appropriate coping mechanisms and teach practices that promote good health. Specific Healthy People 2010 objectives are included in the appropriate sections throughout this text.
NCLEX-PN® EXAMINATION–STYLE REVIEW QUESTIONS
Choose the best answer(s) for each question.
1. Which one of the following statements best describes health? Health is:
2. the total state of physical and psychological well-being.
3. the state of functioning well physically, mentally, and socially.
2. Taking on the sick role occurs when a patient:
1. recognizes that vague aches and pains are present.
2. states that she might be getting a cold.
3. refuses to see a physician even though her cough is constant.
3. Current views of health include the concept of:
1. rarely allowing oneself to become ill.
2. allowing others to take responsibility for one’s health.
4. The ability of a person to function at an optimum level is primarily dependent on:
1. inner resources of the person.
2. considerate, expert nursing care.
5. It is important to assess a patient’s actual cultural beliefs because:
1. a patient may not adhere to the usual health beliefs of her culture.
2. cultural beliefs play a major role in how the patient perceives herself.
3. the family’s beliefs are inherent in the patient.
4. cultural diversity is present in all parts of the United States.
6. When nurses set priorities of patient needs according to Maslow’s hierarchy, they should: (Select all that apply.)
1. only consider physiologic needs.
2. consider airway status first.
3. consider safety a high priority.
4. place self-esteem needs before security needs.
5. place activity needs before belonging needs.
6. consider elimination needs before rest and comfort needs.
7. A patient had major surgery and says she’s worried about what is happening at home, is worried about not being there to coach the soccer team tomorrow, is feeling pain, and wants to see her husband. Which one of the following actions would you take first
1. Tell her not to worry about things at home.
2. Allow her to call the children at home.
3. Administer pain medication.
4. Check to see who might be able to coach the soccer team.
5. Put in a call to her husband so she can obtain information and have him arrange for someone to coach the soccer team.
8. Which one of the following is the best description of homeostasis?
1. It is the tendency of the body to constantly adjust to changing conditions.
2. It occurs when the equilibrium of the body is disturbed.
3. It is the biologic reaction that takes place in response to a stressor.
9. The effects of stress on a person partially depend on:
10. Selye’s theory of general adaptation states that homeostasis will be regained: