Infection Prevention and Control in the Hospital and Home
Upon completing this chapter, you should be able to:
1 List the stages of an infectious process.
2 Identify five ways to decrease the occurrence of health care–associated infections (HAIs).
3 Explain how Transmission-Based Precautions are used with Standard Precautions.
4 Describe how procedures for Airborne Precautions differ from those for Droplet Precautions.
5 Discuss the special requirements for Airborne Precautions when the patient has pulmonary tuberculosis.
6 List techniques for handling of specimens; disposal of dirty linen, trash, and sharps; and the cleaning of equipment in the isolation setting.
7 Compare infection prevention and control procedures appropriate for the hospital with those used in the home.
8 Give three examples of nursing measures used to provide for the psychosocial care of a patient in isolation.
9 State the four rules of surgical asepsis.
1 Use Standard Precautions when caring for patients.
2 Utilize Transmission-Based Precautions when caring for patients.
3 Properly bag and remove soiled linens and trash from an isolation room.
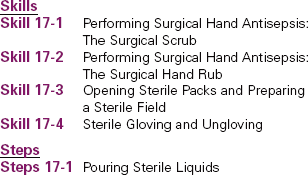
4 Demonstrate performance of a surgical scrub.
5 Teach a patient or family member how to properly dispose of soiled items at home.
Airborne Precautions (p. 237)
Contact Precautions (p. 237)
convalescent (p. 235)
Droplet Precautions (p. 237)
health care–associated infections (HAIs) (p. 235)
human immunodeficiency virus (HIV) ( , p. 236)
, p. 236)
impervious (p. 236)
incubation period ( , p. 234)
, p. 234)
infection prevention and control (p. 235)
isolation ( , p. 235)
, p. 235)
leukocytosis (le , p. 235)
, p. 235)
malaise ( , p. 235)
, p. 235)
prodromal period ( , p. 235)
, p. 235)
Standard Precautions (p. 236)
Transmission-Based Precautions (p. 236)
This chapter will build on concepts learned in Chapter 16, including how microorganisms are spread, the body’s defense mechanisms against infection, and the use of Standard Precautions, including hand hygiene and personal protective equipment (PPE), to protect both patients and health care workers from disease-causing organisms.
INFECTION
Infection occurs when pathogenic microorganisms invade the body and multiply. There are four stages in the infectious process: the incubation period, prodromal period, illness period, and convalescent period. The length of each is influenced by many factors, including the organism itself, the overall health of the host, and the environment in which infection has occurred.
The incubation period begins when the organism firsts enters the body and lasts until the onset of symptoms. During this period the organism multi plies, and the duration of the period varies depending on the type of microorganism. In many viral diseases, the infection can be transmitted during the incubation period.
The prodromal period is the short time from the onset of vague, nonspecific symptoms to the beginning of specific symptoms of infection. The patient may be irritable and experience fatigue, malaise (not feeling “right”), and elevated temperature. This period lasts a few hours to a few days. Microorganisms are most likely to be spread during this highly infectious stage. Typically, precautions against spreading the infection are not taken because people do not realize that they are ill until the more specific symptoms of infection appear.
During the illness period, localized and systemic signs and symptoms appear. The individual may have fever, headache, and malaise. Other specific signs of infection may be detected, such as rash, swollen lymph nodes, leukocytosis (increased white blood cells), purulent wound exudate, diarrhea, and vomiting. The severity of the symptoms and the duration of the illness depend on the virulence of the pathogen and the person’s susceptibility to the causative microorganism. It is in this phase that people perceive they are ill and may seek professional care.
The convalescent (recovery) period begins when the symptoms begin to subside and extends until the patient has returned to a normal state of health. This can take days to weeks, depending on the microorganism and the overall state of health of the affected individual.
HEALTH CARE–ASSOCIATED INFECTIONS (HAIs)
Infections that are transmitted to a person while receiving health care services are called health care–associated infections A health care worker can also contract an HAI (e.g., head cold, flu, staphylococcal skin infection). The Centers for Disease Control and Prevention (CDC) estimate that HAIs just in hospitals cause at least 2 million infections, 90,000 deaths, and $4.5 billion in excess health care costs annually.
Many invasive procedures predispose patients to infection either because the integrity of the skin or mucous membrane is altered, or because an illness reduces the body’s ability to defend itself against invading microorganisms. Patients at greatest risk for HIAs include those with
• Surgical incisions with or without drains
• Artificial airways, including endotracheal tube or tracheostomy
• Intravenous (IV) lines, particularly central venous or arterial lines
• Implanted prosthetic devices (such as heart valves, vascular grafts, or orthopedic joints, rods, and screws)
• Repeated injections or venipunctures for lab specimens
• Immune compromise from such things as chemotherapy, HIV, or long-term steroid use
INFECTION PREVENTION AND CONTROL
Infection prevention and control uses medical and surgical asepsis, Standard Precautions, and Transmission-Based Precautions to prevent or control the spread of microorganisms. The strict use of aseptic technique for all diagnostic and therapeutic procedures involving the use of catheters, IV therapy, endotracheal and tracheostomy tubes, drainage tubes, and wound care reduces the incidence of HAIs. Health Promotion Points 17-1 presents some specific ways to help avoid HAIs in your patients. The current guidelines for infection precautions are delineated in Box 17-1 on p. 237. Isolation is a means of preventing contact between a patient and others to prevent the spread of infection. Emphasis is placed on containing microorganisms and preventing their spread.
Infection prevention and control involves the following:
• Monitoring diagnostic reports related to infection
• Observing patients for signs of infection
• Implementing procedures to contain microorganisms when infection is suspected
• Properly handling, sterilizing, or disposing of contaminated items and equipment
• Utilizing approved sanitation methods
• Recognizing individuals at high risk for infection and implementing appropriate protection
The infection prevention and control practitioner receives a report from the laboratory every time a culture is performed for an infectious organism. A report is also sent from the nursing unit whenever a patient is identified as having an infectious disease or local infection. Appropriate precautions are then initiated for the type of organism present. The practitioner also investigates all HAIs, looking at possible causes, including breaks in the use of approved precautions; and provides ongoing education regarding infection prevention and control for the health care staff.
Infection prevention and control techniques have undergone many changes over the past three decades. In the United States, current precautions are based on guidelines and regulations developed by the CDC and the Occupational Safety and Health Administration (OSHA). Initially, isolation techniques focused on hospitalized patients, but the evolution of human immunodeficiency virus (HIV), hepatitis strains, and a variety of drug-resistant bacteria have caused a broadened focus. Infection prevention and control practices are now focused on protecting patients, health care workers, family members, and social contacts in all settings.
There are two premises underlying the current system of isolation. One is that infection may be present before the diagnosis is made. The second is that the greatest risk of transmitting infection from most organisms comes from direct contact with the organism by the caregiver’s hands or equipment and supplies that have been soiled by blood, body fluids, and other potentially infectious materials. It is known that all body substances may harbor microorganisms and be infectious, and contact with body substances must therefore be avoided.
Current standards consist of two tiers developed by the Hospital Infection Control Practices Advisory Committee (HICPAC) of the CDC. Tier 1 is Standard Precautions, and Tier 2 is Transmission-Based Precautions. Standard Precautions delineate methods for avoiding direct contact with all body secretions except sweat, whether or not visible blood is present. This includes the mucous membranes and all nonintact skin. Standard Precautions were presented in Box 16-3. Transmission-Based Precautions are based on interrupting the mode of transmission by identifying the specific secretions, body fluids, tissues, or excretions that might be infective. Transmission-Based Precautions are used alone or in combination but are always used in addition to Standard Precautions. Box 17-1 lists Transmission-Based Precautions requirements.
CDC and OSHA guidelines have also brought about the development of needleless IV connection systems, and syringes with readily activated protective shields to cover needles immediately following use. These systems decrease opportunities for needle-stick injuries, one of the major factors in health care worker exposure to pathogenic organisms. Use of these devices has significantly reduced the number of needle-stick injuries.
Although Standard Precautions and Transmission-Based Precautions can seem overwhelming at first, the concepts are actually relatively simple. For example, never touch with bare hands anything that contains fluids from a body surface or cavity. Gloves are worn for all contact with body fluids of any sort, including blood, saliva, urine, and feces. The only time gloves are not worn is for contact with intact skin or unsoiled articles. Hand hygiene is performed well and often, paying close attention to areas around and under the fingernails and between the fingers.
Another precaution is the wearing of impermeable gowns when clothing may become soiled with body substances while providing patient care. Masks are worn when contact with respiratory droplet secretions is anticipated, and during suctioning. Protective eyewear is added when there is the possibility of splashing body fluids. All sharps are to be disposed of in puncture-resistant containers located in the patient’s room, with the protective shield activated before disposal. Trash and used linens are placed in impervious, or moisture and particle-proof, plastic bags (Figure 17-1).
APPLICATION of the NURSING PROCESS
At the first encounter with the patient, assess for signs of infection that may require Transmission-Based Precautions. Wounds should be assessed each shift for signs of infection. Monitor the patient’s temperature. Admission lab studies may also give indications of possible infection, such as an increased white blood cell count or a urinalysis that is positive for bacteria. If cultures are ordered, check the reports to see if any microorganism has been identified. Frequent voiding of small amounts, pain on urination, or a decrease in overall output may also indicate infection.
Nursing Diagnosis
The nursing diagnosis would be Infection, risk for, related to surgical wound, open wound, or weakened condition.
Planning
Expected outcomes would include “No health care–associated infection is evident.” When using Transmission-Based Precautions that require putting on personal protective equipment, you must prepare before each entry into the patient’s room. For example, will you need more linen? Are all the dressing supplies in the room? Does the patient need pain medication? Are there routine medications due at this time? Is there ice and drinking water in the room? Speaking to the patient in advance via the intercom can help ensure you will have everything necessary when you don your protective clothing and enter the room.
Implementation
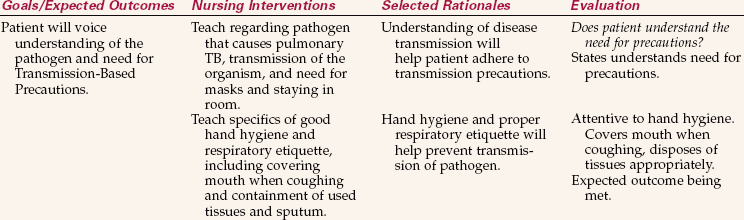
A patient with an infection will need teaching about the disease process, modes of transmission, and precautions necessary to prevent spread of the infection (Nursing Care Plan 17-1). Standard and Transmission-Based Precautions will need to be explained.
Standard Precautions are to be used for each contact with every patient, regardless of whether or not infection is known to be present. Transmission-Based Precautions are implemented based on the individual patient’s infection status.
Hand Hygiene
Hand hygiene is the most important action in preventing the transmission of infection. Guidelinesfor cleaning one’s hands were presented in Chapter 16. Hand hygiene is required before and aftercontact with a patient, wound care, or any invasive procedure.
Frequent hand hygiene is performed when caring for patients susceptible to infection. Patients with decreased immune status are often placed in protective isolation to reduce exposure to infectious organisms. People providing care for these individuals must wear gowns, gloves, and masks, and the patient needs to be in a private room. Specific guidelines vary with the facility and the degree of immune deficiency. Know and follow your agency’s policies and procedures.
Hand hygiene is to be performed before donning gloves and after removing them. Although tasks such as interviewing the patient do not require hand hygiene, if a patient is coughing or sneezing during the interview, hand hygiene should be performed before leaving the room (Safety Alert 17-1).
Personal Protective Equipment
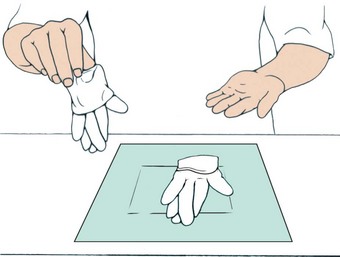
Standard Precautions guidelines state when personal protective equipment (PPE) is to be worn (see Chapter 16). Clean disposable gloves are used for most general care, such as bathing, perineal care, IV site care, and most dressing changes. Masks are worn when working within 3 feet of a patient under Droplet Precautions. (Refer to the companion CD-ROM for Nursing Care Plan 17-2: Care of the Patient Under Droplet Precautions.) The nurse who is coughing should wear a mask when in contact with patients. CDC guidelines state that if full PPE is required, it is donned in the following order: gown, followed by the mask or respirator, then goggles or face shield, and finally gloves. The sequence for removing PPE is gloves, followed by face shield or goggles, then the gown, and finally the mask or respirator. Skill 16-2 shows the correct procedure for putting on a gown and mask. Skill 17-4 on pp. 253–255 shows the correct procedure for putting on and removing sterile gloves. Hand hygiene is always performed after removing gloves or any combination of PPE.
When the patient has known or suspected pulmonary tuberculosis, a special particulate filter mask called an N95 mask must be worn (see Figure 16-5, C). The same type of mask is used when caring for patients with known or suspected rubeola or varicella unless the nurse is immune to these diseases (Figure 17-2).
General Guidelines for Isolation Precautions
Specimen Preparation and Transportation.: Label the specimen container with the patient’s name and medical record number plus the type of specimen before entering the patient’s room. Place the label on the container itself, not the lid, because once the lid is removed in the lab, the specimen is unlabeled. Collect the specimen and carefully place it in the leak-proof container without contaminating the outside of the container. Be sure the lid is fully tightened. Clean or disinfect containers that are visibly contaminated before sending them to the laboratory. Both OSHA and the Clinical Laboratory Improvement Act (CLIA) require that specimens be transported to the laboratory in a plastic bag marked “Biohazard.”
Linens.: Soiled linen is handled as little as possible. Roll it up and place it inside the patient’s linen hamper in the room. When the bag is two-thirds full, tie it closed and send it to the laundry according to agency policy. Double bagging is not necessary.
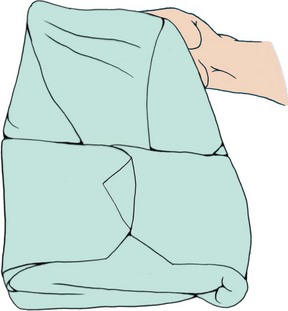
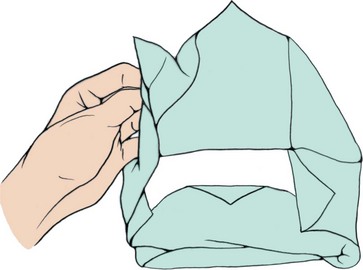
Trash.: Disposable soiled equipment and supplies are placed inside the plastic bag lining the waste receptacle in the patient’s room. Red bags marked with a biohazard symbol are for biohazardous waste only. Ordinary trash is to be placed in standard trash bags and disposed of in the routine manner. Biohazardous waste requires special disposition that is very costly, and non-biohazardous trash should never be mixed in with it. The bag is sealed when it is two-thirds full, removed, and sent to waste collection. The only time double bagging is necessary is if the plastic bag is soiled on the outside. In this instance, another nurse standing just outside the room doorway holds open a second plastic bag, placing her hands under the edge of the bag, which is folded outward to cover the nurse’s gloved hands. This further protects her hands from soiling. The nurse in the patient’s room then places the first bag carefully inside the second one. The nurse outside the room ties the bag closed, being careful not to touch the inner first bag.
Sharps.: Needles are not to be recapped before disposal. All used needles, scalpel blades, IV cannulas, suture needles, and other sharp items are dropped into a puncture-resistant sharps biohazard container. Never put your fingers inside the opening of the sharps container. Shake the container gently to settle the contents and make more room if necessary. Sharps containers should be replaced when they are two-thirds full. The full sharps container is sealed and sent to the biohazard waste storage area for later removal.
Federal policy and The Environment of Care guidelines of the Joint Commission require that sharps containers be secured in patient care areas, and that holding areas for biohazards must be accessible by staff only.
Other Equipment.: Reusable equipment is cleaned if it is visibly soiled and then sent to central supply to be disinfected. A stethoscope and blood pressure cuff are issued to the isolation patient, and only these are used within the isolation room. When the patient is discharged, these items are returned to central supply for disinfection as needed. No special treatment is necessary for dishes. Some agencies use paper dishes and trays for patients under Transmission-Based Precautions but this is not a CDC requirement. Box 17-2 presents other general principles.
Natural Defenses.: You should institute measures to protect and enhance the natural body defenses of the patient. These defenses were discussed in Chapter 16. In particular, you should protect intact skin and mucous membranes, promote a balanced diet and sufficient fluids, provide opportunity for adequate sleep and rest, and decrease stress as much as possible.
Patient Placement.: A patient in need of Transmission-Based Precautions is usually placed in a private room. An exception can be made if another patient has the same type of infection. Then they can be cohorted in the same room. If the patient is under Airborne Precautions, a private room with negative air flow or a portable HEPA (high-efficiency particulate matter) filter machine is essential. The door to the room must remain closed except when someone is entering or leaving. This helps ensure the organism remains contained and does not enter the rest of the unit. Box 17-3 presents recommended isolation precautions for hospitals.
Transporting the Patient.: Transporting the isolation patient is avoided unless absolutely necessary. If transporting is unavoidable, the patient is given a standard mask to wear while out of the room. For a patient under Droplet Precautions, measures are taken to prevent soiling of the environment. The unit or department receiving the patient must be notified ahead of time that a patient under this particular type of Transmission-Based Precautions is coming to the area. Information about any additional precautions required must be shared with those receiving the patient.
Infection Prevention and Control in the Home
The patient at home has less exposure to HAIs, but can still be at risk. The emphasis in the home environment is on containing pathogens and preventing transmission to health care personnel, caregivers, and others in the household. The home health nurse must teach patients and families to dispose of dirty supplies in a safe manner.
When the patient has an infection, care should be taken that his towels, sheets, and clothes are kept away from contact by others until they can be washed. The patient’s clothing and linens can in most cases be laundered with the rest of the household wash. Washing in warm water with standard laundry detergent is usually sufficient. Items should be thoroughly dried prior to use, either in a dryer or outside in the sun.
The patient is taught to perform correct hand hygiene and to dispose of any paper towels or facial tissues in an appropriate container. Other family members must be instructed to perform hand hygiene frequently as well. The bathroom should be cleaned daily with standard household chemicals or a 1:10 solution of chlorine bleach and water. Dishes should be washed on the hot cycle of the dishwasher or soaked in scalding water after washing and allowed to air dry. The patient’s laundry should be washed separately, using hot water and bleach if possible.
Soiled dressings and wound care supplies should be disposed of in plain, unlabeled plastic bags that are tied up securely and stored in an appropriate trash receptacle for pickup with the rest of the household trash. Trash marked with the biohazard symbol cannot be placed in the household trash pickup. Handling or transporting biohazard trash requires special permits.
A heavy plastic jug with a secure top can be used to contain needles and syringes and other sharp objects used in the patient’s care. Placing a 1:10 solution of chlorine bleach and water in the container helps kill microorganisms. Disposal of the jug is subject to local regulations in the city, county, or province where the patient lives.
Clean gloves are used for wound care unless there is an order for sterile dressing changes. Patients and family members should be taught to properly remove and dispose of contaminated gloves. It should be stressed that hands are to be cleansed before putting on gloves, and again after the gloves are discarded. Reinforce that gloves should not be reused.
The patient’s room should be cleaned frequently, with dust kept to a minimum. Fresh air should be allowed to circulate in the room. Sunshine through the windows can elevate the patient’s mood and decrease the presence of some microorganisms. Trash, news-papers, and clutter should be kept to a minimum to discourage transfer of microorganisms. Clean sup-plies should be kept in one area, well away from any contaminated items or trash (Home Care Considerations 17-1).
Protective Isolation
When a patient is immunocompromised, it is very important to protect him from exposure to potential pathogens. The patient is placed in a special isolation room with its own ventilation system. No one with an active infection is allowed in the patient’s room. Until recently, the degree of isolation was as absolute as possible, extending even to sterile dishes and having anyone who entered wear full protective equipment. Recent studies in major medical centers throughout the world are indicating that environments can be less stringent without increasing the rates of HAIs, and that PPE is not required for routine entry into the room. It is important, therefore, to remain aware of your facility’s policies and procedures regarding protective isolation and to follow them at all times (Figure 17-3).
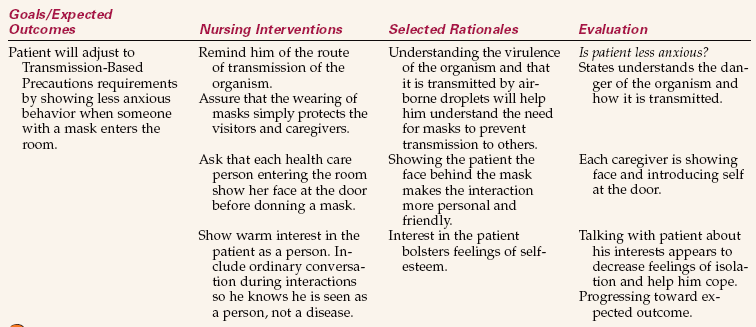
Psychological Aspects of Isolation
The patient in Transmission-Based Isolation precautions is at risk for both decreased self-esteem and sensory deprivation. This is particularly true for young children, who under normal circumstances are rarely alone, and are often used to highly stimulating and entertaining environments. The elderly, too, can find isolation particularly trying, and it may lead to confusion secondary to the lack of normal stimulation and interaction. Assessment for sensory deprivation needs to be ongoing. The signs can include boredom, slowness of thought, disorganized thoughts, excessive sleeping during the day, anxiety, hallucinations, or panic attacks.
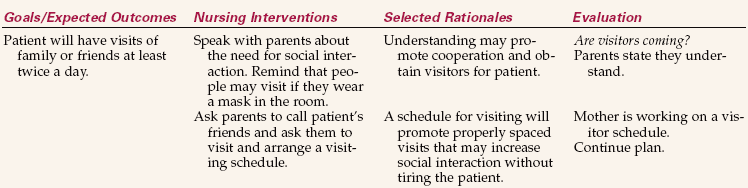
Having visitors at intervals can be very helpful in preventing sensory deprivation. They can talk with the patient about interests they share, and a visitor at mealtime often encourages improved nutritional intake by making mealtime more enjoyable. The nurse should learn about the patient’s interests and provide appropriate activities. These can include games, books, puzzles, phone calls, radio or TV, a video, or a craft project. However, avoid overtiring the patient by also allowing periods of rest between activities.
Sensory deprivation may occur if visitors are intimidated by the isolation precautions. There may be decreased interaction with the health care team because of the need to put on personal protective equipment to enter the room. All of this can lead to a loss of self-esteem because the patient begins to feel that he is somehow unclean or unworthy of attention.
Listen to the patient’s feelings. Make positive comments on efforts at grooming or self-amusement (Cultural Cues 17-1). Try to engage the patient in conversation that is meaningful by asking about particular interests or hobbies. Assisting visitors to feel welcome and to understand that the patient benefits greatly from their presence can also help. Addressing self-esteem needs is very important for complete recovery.
Infection Prevention and Control for the Nurse
OSHA regulations protect health care workers from occupational exposure to blood-borne pathogens in the workplace. In Canada, the Occupational Health and Safety Act addresses worker safety. The three main modes of occupational exposure to blood-borne pathogens are as follows:
• Puncture wounds from contaminated needles or other sharps
• Skin contact, allowing blood, body fluids, and other potentially infectious materials to enter through damaged or broken skin
• Mucous membrane contact, allowing infectious materials to enter through the mucous membranes of the eyes, mouth, and nose
Actions that decrease the nurse’s risk for infection include good hand hygiene and other general medical asepsis techniques, the wearing of personal protective equipment, using needleless IV equipment and needles with guards, and avoiding carelessness in the clinical area.
It is also recommended that health care workers be immunized if they are not shown to have an active immune status to certain diseases. These include hepatitis B, influenza, mumps, measles, rubella, varicella (chickenpox), tetanus, diphtheria, pertussis, and meningococcal disease.
Surgical Asepsis
Surgical asepsis is another method used to prevent infection. Surgical asepsis is practiced in the operating room, obstetric areas, special diagnostic areas, andfor procedures such as administering injections, changing wound dressings, performing urinary catheterization, and administering intravenous therapy. In the operating room, strict surgical asepsis is practiced, and head coverings, sterile gowns, masks, and gloves are worn. To perform a sterile dressing change outside the operating room, sterile gloves, a mask, and a sterile field are used. Talking during the dressing change is discouraged.
The four rules of surgical asepsis are as follows:
The goal in surgical asepsis is to keep an area free of microorganisms. You must constantly be aware of which items and areas are sterile, clean, or contaminated to maintain surgical asepsis. The importance of maintaining sterility must become ingrained, and you must consistently maintain principles of surgical asepsis to protect the safety of patients (Box 17-4). By being constantly sensitive as to what is sterile, what is clean, and what becomes contaminated, breaks in sterile technique are caught and rectified before microorganisms are transferred to the patient.
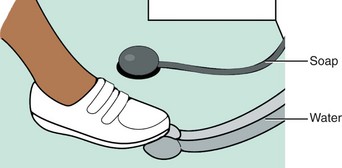
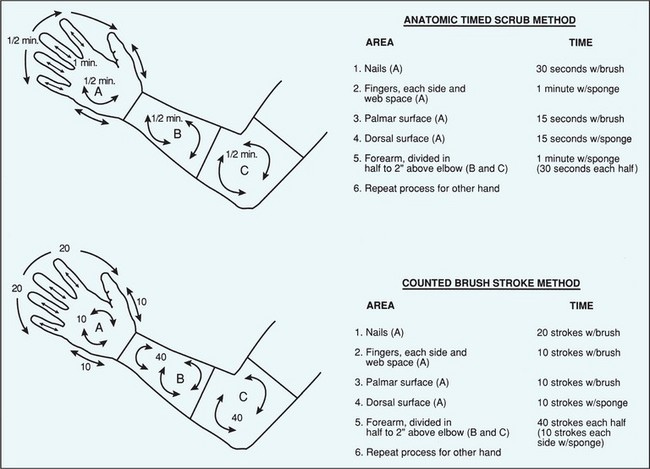
Surgical Scrub.: The surgical scrub is more lengthy and vigorous than normal handwashing. Its purpose is to remove as many microorganisms as possible without damaging the skin of the hands. Skill 17-1 presents the steps for the traditional surgical scrub. Water, a nail stick, an antiseptic agent, a scrub brush or sponge pad, and friction are used to mechanically cleanse the hands and forearms. The scrub begins at the hands and ends 2 inches above the elbows. All rinsing is done under flowing water, not in a container of water (Figure 17-4). The timing for the scrub does not include the rinsing time. Some agencies allow the use of the counted-stroke method of scrubbing rather than by-the-clock timing (Figure 17-5). Current standards regarding the time for the traditional scrub are based on the recommendations of the antiseptic agent manufacturer, and consequently the recommended time varies from one agency to another, depending on the product in use. A 2- to 4-minute scrub is average.
A newer brushless technique, which may be done with or without water, uses an antimicrobial agent that is at least 60% alcohol. This method was shown to be equally effective compared to a standard surgical scrub in a research study (Gruendemann & Bjerke, 2001). For the brushless scrub technique, 2 mL of antimicrobial agent are dispensed into the palm of one hand. With the fingertips of the opposite hand, some of the alcohol-based agent is worked under the nails. The remaining portion of the agent is spread over all surfaces of the hand and arm to just above the elbow. Another 2 mL of the antimicrobial agent is dispensed into the palm of the other hand and the procedure is repeated on the opposite hand and arm. There are variations in technique depending on the product used. Check the manufacturer’s directions for the correct technique. The hands and arms must be allowed to dry before gloving (Skill 17-2).
Opening Sterile Packs and Packages and Setting Up a Sterile Field.: Many sterile supplies are prepared commercially and are disposable or one-time use items. The package, set, or kit provides all the items commonly required in a variety of nursing procedures, such as catheterization, suture removal, dressing change, and irrigation. Individually wrapped items can be obtained to supplement the packs as needed.
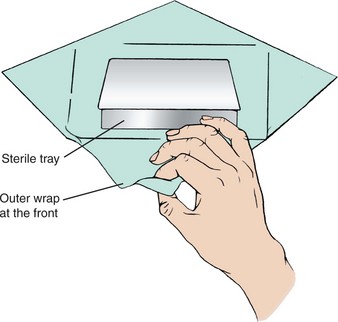
Packs and kits are opened by removing the outer plastic or paper covering, taking out the inner package, and aseptically unfolding the wrapper to form a sterile field (Figure 17-6). The principles of asepsis apply regardless of whether the package is disposable or a wrapped tray is prepared by the central supply department of the hospital. Skill 17-3 shows the steps for opening sterile packs and preparing a sterile field.
The principles to observe when opening sterile packages are as follows:
• Open the sterile package away from the body.
• Touch only the outside of the wrapper.
• Do not reach across a sterile field; go around the sterile field if necessary to reach the other side.
• Always face the sterile field, even when moving to the other side.
• Allow sufficient space (at least 6 inches) between the body and the sterile field.
Most sterile items are available as individually wrapped or separate items, such as sterile packages of cotton-tipped applicators, tongue blades, 4 × 4 gauze dressings, ABD (abdominal) dressings, alcohol swabs, syringes, needles, Foley catheters, sterile gloves, and intravenous catheters. Instructions often appear on the outside of the package directing you where to open it, indicating the direction in which to tear, or showing where to peel at a certain point. Follow these instructions to avoid contaminating the contents.
When sterile supplies have been brought to the patient’s bedside, they should never be returned to the unit stock shelves. The outsides of these items are contaminated, and returning such supplies carries organisms from the patient’s room back to the store of supplies for the unit. Do not stockpile supplies in the patient room to avoid costly waste.
The procedure for pouring sterile liquids is listed in Steps 17-1.
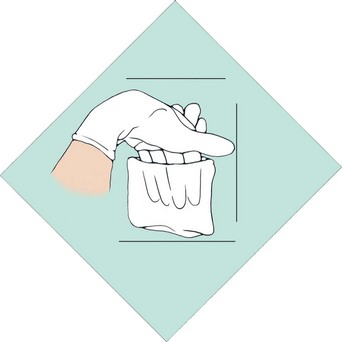
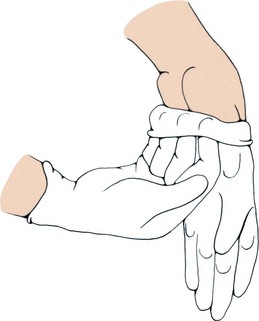
Sterile Gloving.: Sterile gloves must be used for sterile procedures. These gloves are made of various substances, including latex and nitrile, and are less permeable than the disposable plastic gloves. The method of donning and removing sterile gloves is presented in Skill 17-4.
Correcting Breaks in Asepsis.: Whenever it becomes apparent that a break in surgical asepsis has occurred, you must rectify the error. A scrub is begun again if the hands touch the sink, which is always considered contaminated; sterile gloves are discarded and new gloves donned when any part of a glove touches a nonsterile area or item. Sterile supplies are discarded or put aside for re-sterilization if they become contaminated, and new packs or packages are opened aseptically to replace them.
It is up to every nurse to point out breaks insterile technique that occur when others seem unaware that they have contaminated themselves or the sterile field. Surgical asepsis is used in every aspect of nursing.
Evaluation
If the patient is recovering without additional instances of infection from other organisms, or infection of other body areas with a resident organism, goals are being met. Evaluation also includes assessing whether the patient’s infection has been transmitted to any health care worker or any other patient on the unit or in the hospital. The infection prevention and control practitioner monitors for this and, if it occurs, usually works in conjunction with the unit manager to ensure that staff members are correctly implementing infection prevention and control procedures.
Infection prevention and control is the responsibility of each and every nurse. The principles and techniques learned here will protect you and your patients from harmful microorganisms.
NCLEX-PN® EXAMINATION–STYLE REVIEW QUESTIONS
Choose the best answer(s) for each question.
1. The nurse is delivering a meal tray to a patient who is under Droplet Precautions for bacterial pneumonia. Which articles of personal protective equipment (PPE) need to be worn?
2. The nurse is preparing to assist a patient with his bath. He has an infected, draining wound. What PPE would be required for these tasks? (Select all that apply.)
3. Which of the following steps are to be taken when preparing a sputum specimen to go to the laboratory? (Select all that apply.)
2. Collect the specimen and secure the lid.
3. Place the container in a sealed plastic bag marked “Biohazard.”
4. Place the biohazard bag in another plastic bag.
4. A nurse is working in a small hospital with a combined med-surg unit. The only beds available are in two-bed rooms, and each room already has a patient. The recovery room nurse is about to send a 25-year-old female who just had her tonsils removed. Who would be the most appropriate roommate?
1. A 60-year-old woman newly diagnosed with bacterial pneumonia
2. A 23-year-old woman with a draining wound
5. A home care nurse has a patient with a wound infection who is also under Airborne Precautions. The patient’s wife will be doing the dressing change on the days that the nurse does not visit. The wound must be cleansed and then dressed. The nurse must teach the wife to: (Select all that apply.)
1. maintain strict surgical asepsis.
2. cleanse her hands and be careful to touch only the corners of the dressing with her bare hands.
3. contain the used dressings and supplies in a sealed plastic bag before placing them in the trash.
4. wear a mask as well as gloves when changing the dressing.
6. A patient under Contact Precautions wants to know if he may have visitors. The nurse tells him that:
1. visitors may come but they must wear a mask and gown.
2. there are no special requirements for people visiting a patient under Contact Precautions.
3. visitors may come but should wear gloves if they touch the patient.
4. visitors may come but should wash their hands before and after socially touching the patient.
7. When performing a sterile dressing change on a patient, correct technique must be regarded as broken if: (Select all that apply.)
1. supplies are placed touching the edge of the sterile field.
2. a gloved hand touches the dressing table below tabletop surface.
3. a sterile glove touches one of the sterile dressings on the field before the procedure is begun.
4. the nurse reaches over the sterile field when placing a swab used to clean the wound in the discard bag.
8. Standard Precautions are used:
2. for all patients unless they are under Transmission-Based Precautions.
9. The correct actions when donning a pair of sterile gloves include: (Select all that apply.)
1. picking up the first glove by placing the fingers of the opposite hand under the cuff.
2. smoothing the first glove over the hand before putting on the second.
3. picking up the first glove by grasping it on the fold of the cuff.
10. When making up the bed in an isolation room, the nurse: (Select all that apply.)
CRITICAL THINKING ACTIVITIES ? Read each clinical scenario and discuss the questions with your classmates.
Scenario A
You are caring for a 43-year-old man who has an infected leg wound following a hiking accident. He is to keep his leg elevated and is under Contact Precautions. He has recently retired from the military and has just moved to the area. He is bored and restless. How would you help meet his psychosocial needs?
Scenario B
What would you do if you observed the physician’s glove become contaminated during a sterile procedure and the physician appears unaware that this has occurred? Be specific
Scenario C
Your home care patient is an older man with a large abdominal wound that needs daily dressing changes. He lives with his wife, but she has severe arthritis in her hands and is unable to perform the procedure. You are scheduled for three visits per week. How would you solve the problem of getting his daily dressing change done on the days you are not scheduled to visit?