Infection Prevention and Control: Protective Mechanisms and Asepsis
Upon completing this chapter, you should be able to:
1 List the types of microorganisms that can cause infection in humans.
2 Discuss the links in the infection process and give an example of each.
3 Discuss factors that make the elderly more susceptible to infection.
4 Explain how the body’s protective mechanisms work to prevent infection.
5 Explain how the inflammatory and immune responses protect the body.
6 Identify means for removal or destruction of microorganisms on animate and inanimate objects.
7 Compare and contrast medical asepsis and surgical asepsis.
8 Describe accepted methods of disinfection and sterilization.
1 Discuss the surveillance, prevention, and control of infections in hospitalized patients.
2 Demonstrate proper hand hygiene technique.
3 Consistently demonstrate application of Standard and Transmission-Based Precautions while caring for patients.
4 Prepare to teach a home care patient with a wound infection how to prevent the spread of infection to family members.
antibiotic (p. 211)
antimicrobial ( , p. 211)
, p. 211)
antiseptic ( , p. 230)
, p. 230)
asepsis ( , p. 219)
, p. 219)
aseptic ( , p. 214)
, p. 214)
bacteria ( , p. 211)
, p. 211)
contaminated (p. 213)
debris ( , p. 215)
, p. 215)
disinfectants ( , p. 230)
, p. 230)
fungi ( , p. 212)
, p. 212)
helminths ( , p. 212)
, p. 212)
immune response ( , p. 218)
, p. 218)
interferon ( , p. 216)
, p. 216)
medical asepsis (p. 219)
microorganism (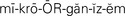 , p. 209)
, p. 209)
pathogens ( , p. 209)
, p. 209)
personal protective equipment (PPE) (p. 220)
prions (p. 211)
protozoa ( , p. 212)
, p. 212)
rickettsia ( , p. 212)
, p. 212)
Standard Precautions (p. 220)
sterile (p. 213)
sterilization ( , p. 213)
, p. 213)
surgical asepsis (p. 219)
viruses (p. 211)
An infection is the entry into the body of an infectious agent, a microorganism (organism only visible with a microscope) that then multiplies and causes tissue damage, and may result in illness and disease. Health care professionals work to eliminate infection from the body and to prevent its spread to others. Careful hand hygiene is essential to prevent cross-contamination. Box 16-1 presents vocabulary related to infection. Microorganisms that are capable of causing disease are called pathogens (Figure 16-1). Nonpathogenic organisms that are prevalent on and in the body are called normal flora (Table 16-1). These normal flora prevent more harmful microorganisms from colonizing and multiplying within the body. They do this by occupying receptor sites on cells, monopolizing the nutrients, and secreting substances that are toxic to other microorganisms. Some pathogenic microorganisms produce harmful toxins and others release endotoxins. Endotoxins are responsible for the symptoms seen in botulism, tetanus, diphtheria, and Escherichia coli infection.
Table 16-1
Normal Flora of the Body*
*The lower respiratory tract, central nervous system, bladder, and upper urinary tract are normally sterile (no microorganisms present).
INFECTIOUS AGENTS
Bacteria
Bacteria are single-cell microorganisms lacking a nucleus that reproduce anywhere from every few minutes up to several weeks. Bacteria are classified according to their need for oxygen, their shape, and their Gram-staining properties. Aerobic bacteria need oxygen to grow and thrive. Anaerobic bacteria can grow only when oxygen is not present. The Gram stain technique helps classify bacteria. For a Gram stain, bacteria placed on a slide are stained and then treated with a contrasting dye; those retaining the stain are gram positive and those losing the stain and taking up the counterstain are gram negative. Many gram-negative bacteria are more dangerous than gram-positive bacteria because they may produce an endotoxin that can cause hemorrhagic shock and severe diarrhea and can alter resistance to other bacterial infection. Classification of bacteria according to their shape, or morphology, is based on whether they belong to one of three main groups. Cocci are round, bacilli are rod-shaped, and spirochetes are spiral or corkscrew-shaped. Some grow in chains (streptococci), some in pairs (diplococci), and some in clusters (staphylococci).
Final identification is by chemical testing of the bacteria grown by culture. To culture the bacteria, the infected body secretion is transferred to a medium in which it can grow. Sensitivity tests are then performed to determine which antibiotic (chemical substance that can kill or alter the growth of microorganisms) is most effective against the bacteria.
When culture results show that a drug-resistant organism is responsible for an infection, extreme care must be taken to prevent the spread of the organism. The four most common multidrug-resistant organisms are (1) methicillin-resistant Staphylococcus aureus (MRSA); (2) vancomycin-resistant Enterococcus (VRE); (3) extended-spectrum beta-lactamase–producing (ESBL) gonorrhea (Neisseria gonorrhoeae); and (4) Clostridium difficile (C. diff). There is a new quick test, the BD GeneOhm StaphSR Assay, that identifies MRSA bacterium in 2 hours. It is performed on a blood sample. Penicillin-resistant Streptococcus pneumoniae causes pneumonia. These organisms, and especially MRSA, are being contracted outside the hospitals now and are an increasing problem (Health Promotion Points 16-1). Patients must be educated about the correct use and possible misuse of antimicrobial (killing or suppressing growth of microorganisms) agents. Encourage each patient to take the entire antibiotic prescription as ordered by the heath care provider for an infection. Taking only part of the prescription prevents the killing of all of the microorganisms responsible for the infection. This gives them a chance to mutate and develop drug resistance. Consistent use of Standard Precautions plus any Transmission-Based Precautions (e.g., Contact or Droplet Precautions) is essential, especially when a drug-resistant organism is present.
Prions
Prions are protein particles that lack nucleic acids and are not inactivated by usual methods for destroying viruses. They do not trigger an immune response, but cause degenerative neurologic disease such as variant Creutzfeldt-Jakob disease (mad cow disease).
Viruses
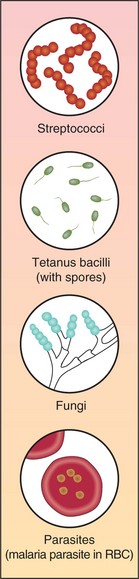
Viruses are extremely small and can be seen only with an electron microscope (Figure 16-2). They are composed of particles of nucleic acids, either DNA or RNA, with a coat of protein, and in some cases a membranous envelope. Viruses can grow and replicate only within a living cell. Once inside cells, viruses can trigger an immune reaction or damage cells in other ways. Their survival and multiplication are dependent upon host tissue. Viruses are identified in the laboratory by fluorescent techniques, electron microscopy, and tissue culture.
Protozoa
Protozoa are one-celled microscopic organisms belonging to the animal kingdom. Protozoa that are pathogenic to humans include the Plasmodium species that causes malaria; Entamoeba histolytica, which causes amebic dysentery; and other strains capable of causing diarrhea.
Rickettsia
Rickettsia are small round or rod-shaped microorganisms that are transmitted by the bites of lice, ticks, fleas, and mites that act as vectors. They multiply only in host cells. Rocky Mountain spotted fever and typhus are caused by rickettsias.
Fungi
Fungi are tiny, primitive organisms of the plant kingdom that contain no chlorophyll. Yeasts and molds are members of this group. Fungi feed on living plants and animals and decaying organic material and thrive in warm, moist environments. Fungi reproduce by means of spores. In humans, fungal infections are called mycoses. When the balance of normal flora is altered by antibiotic therapy, fungal infection may occur. Common fungal infections are vaginal candidiasis and athlete’s foot (tinea pedis).
Helminths
Helminths are parasitic worms or flukes and belong to the animal kingdom. Pinworms, which mostly affect children, are the most common helminths worldwide. Roundworms and tapeworms are other helminths.
Other Infectious Agents
Several types of organisms differ enough in structure to fall outside the above classifications. Mycoplasmas are very small organisms without a cell wall. They cause infections of the respiratory tract or the genital tract. Mycoplasma pneumoniae is an example. Chlamydia, another type of organism, affects the genitourinary and reproductive tract and has become increasingly more common in the last 20 years. In countries where hygiene is poor, Chlamydia trachomatis is responsible for trachoma, an eye disease that can cause blindness. In this country, the same organism causes a significant amount of sexually transmitted infection (Table 16-2).
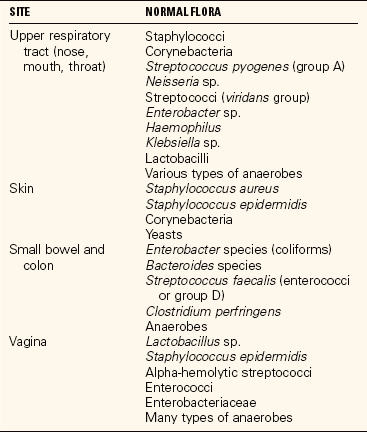
Table 16-2
Disease-Producing Organisms (presented in order of increasing complexity)
*Mastrianni, J.A., & Roos, R.P. (2000). The prion diseases. Seminars in Neurology, 20, 337-352.
†Prusiner, S. (1999). Nobelist believes prions may be at root of Alzheimer’s, Parkinson’s, ALS. Reuter’s Health, October 20. Available at www.reutershealth.com. (Dr. Stanley Prusiner is a 1997 Nobel Prize winner for the discovery of prions.)
From Ignatavicius, D.D., & Workman, M.L. (2006). Medical-Surgical Nursing: Critical Thinking for Collaborative Care (5th ed., p. 508). Philadelphia: Elsevier Saunders.
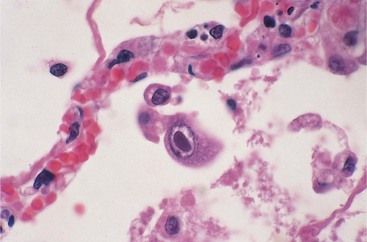
PROCESS OF INFECTION
The process by which an infectious disease is spread from one person to another can be thought of as a continuous chain. Each link must be present in its proper order for the chain to remain intact and for the infection to be passed on to someone else. Figure 16-3 shows how the links of the chain connect and infection occurs.
A causative agent is any microorganism or biologic agent capable of causing disease. These agents include bacteria, viruses, protozoa, rickettsia, fungi, and helminths.
Some microorganisms are more virulent than others. Characteristics that affect virulence are ability to (1) adhere to mucosal surfaces or skin, (2) penetrate mucous membranes, (3) multiply once in the body, (4) secrete harmful enzymes or toxins, and (5) resist phagocytosis (destruction by white blood cells). Microorganisms differ in structure and characteristics (see Figure 16-1).
Pathogenic microorganisms must be destroyed or rendered harmless in order to remove this link from the chain. Disinfection and sterilization (process of destroying all microorganisms and pathogenic products) are methods used to destroy pathogens. Procedures for disinfection should be utilized in all areas in which patients are receiving treatment.
The most effective means for destroying viruses and all other kinds of microorganisms is to expose them to moist heat at a high temperature for 16 to 20 minutes. This is accomplished by using a special machine called an autoclave.
The Centers for Disease Control and Prevention (CDC), a government agency (www.cdc.gov), provides a wealth of information on all aspects of infectious diseases and their prevention and control.
RESERVOIR (LINK TWO)
Reservoirs are places in which microorganisms are found. Reservoirs can be infected wounds, human or animal waste, animals and insects, contaminated (made unclean) food and water, and the person with an infection. Assorted precautions are used to prevent the spread of infection from the reservoir. Good hand hygiene is one of the most effective ways to prevent the spread of microorganisms. Using sterile (without pathologic organisms) technique to insert an indwelling urinary catheter helps prevent the transfer of normal flora from the skin and mucous membranes into the sterile bladder, where it could cause an infection.
PORTAL OF EXIT (LINK THREE)
The portal of exit is the route by which a pathogen leaves the body of its host. An example of a portal of exit is the gastrointestinal tract, through which the feces may transport the typhoid bacillus from an infected person. The respiratory tract can be a portal of exit when microorganisms are released with coughing or sneezing. Measles, mumps, pulmonary tuberculosis, and influenza can be transmitted by exit from the respiratory tract. The skin and mucous membranes can also serve as a portal of exit when an open wound exists.
Portal-of-exit transmission can be interrupted by identifying and treating patients who are infected with pathogens. Isolation techniques and barrier precautions that include the proper handling and disposal of secretions, urine and feces, and exudate can prevent transfer of pathogens. CDC recommendations for Transmission-Based Precautions and isolation techniques are based on scientific evidence that has proven how various pathogens are transmitted. Chapter 17 contains the specific recommendations.
MODE OF TRANSFER (LINK FOUR)
Modes of transfer of pathogens include (1) direct personal contact with body excreta or drainage from an ulcer, infected wound, boil, or chancre; (2) indirect contact with contaminated inanimate objects (called fomites), such as needles, drinking and eating utensils, dressings, and hospital equipment; (3) vectors such as fleas, ticks, mosquitoes, and other insects that harbor infectious agents and transmit infection to humans through bites and stings; (4) droplet infection, or contamination by the aerosol route through sneezing and coughing; and (5) spread of infection from one part of the body to another.
The mode of transmission can be interrupted by effective hand hygiene, proper disinfection and sterilization of medical equipment, use of aseptic (free of microorganisms) technique in performing procedures and diagnostic tests, and use of Standard Precautions to prevent contamination. Teaching patients to cover the mouth when sneezing or coughing, to dispose of soiled tissues correctly, to wash the hands after contact with potentially contaminated items, and to avoid people who have an infection can reduce transmission of pathogens.
Controlling insects with abatement programs, such as for mosquito control, and air filtration in health care facilities are other methods of reducing transmission of pathogens.
PORTAL OF ENTRY (LINK FIVE)
Pathogens can enter the body through the eyes, mouth, nose, trachea, skin, and mucous membranes. Consuming food or water that is contaminated with disease-causing microorganisms is an example of how entrance can occur. Breathing in droplets containing pathogens and contracting a virus through broken skin or abraded mucous membrane are examples for portals of entry. Table 16-3 shows some of the pathogenic organisms that enter through the various body portals.
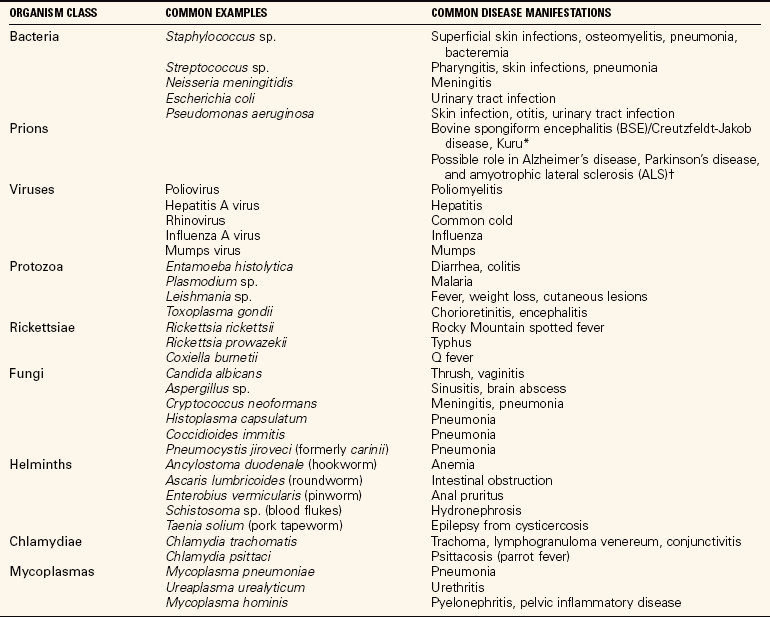
Table 16-3
Portals of Entry of Selected Pathogenic Organisms
From Ignatavicius, D.D., & Workman, M.L. (2006). Medical-Surgical Nursing: Critical Thinking for Collaborative Care (5th ed., p. 509). Philadelphia: Elsevier Saunders.
Using only sterile and clean items when caring for patients reduces the entry of pathogens. Barrier precautions (gloves, masks, condoms), safe handling of food and water, good personal hygiene, avoidance of high-risk behaviors, and protection from insect bites and stings can prevent entry of microorganisms.
SUSCEPTIBLE HOST (LINK SIX)
A human host may be susceptible by virtue of age, state of health, or broken skin. Measures are used to prevent exposure to infectious agents and to improve a person’s state of health by teaching good health and hygiene habits. Immunization to help protect against influenza or pneumococcal pneumonia is another means of decreasing susceptibility.
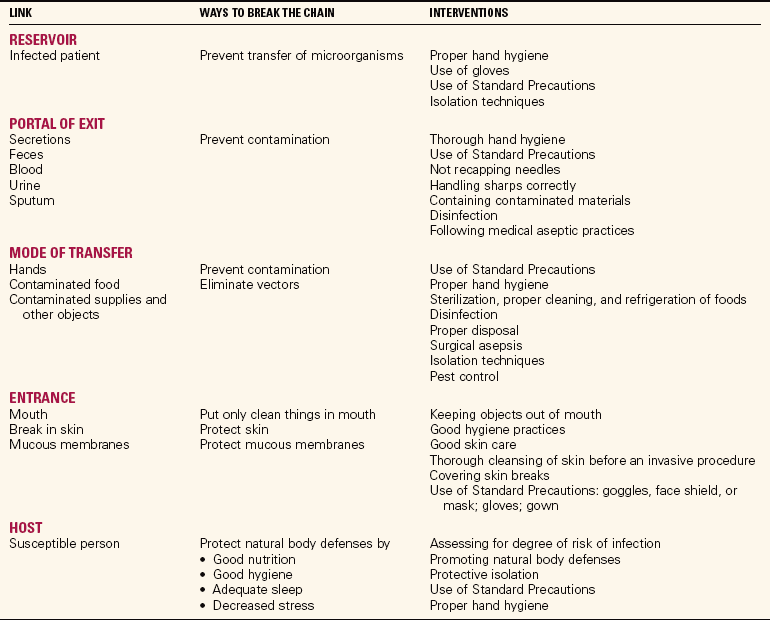
Susceptible hosts can be protected by using aseptic techniques, barrier precautions, and protective isolation (see Chapter 17). Proper nutrition and a healthy lifestyle also increase resistance to infection. Table 16-4 lists factors that increase susceptibility to infectious agents. Table 16-5 shows ways in which the chain of infection can be broken at each link.
Table 16-4
Factors that Increase Susceptibility to Infection
| FACTOR | CONSEQUENCE |
| Age | The elderly and the very young are more susceptible to infection, probably because of declining or immature immune function, respectively. |
| Malnutrition | Poor nutrition interferes with cell growth and replacement, which contributes to decreased immune function. |
| Excessive stress or fatigue | These states seem to interfere with the body’s normal defense mechanisms. |
| Low leukocyte (WBC) count | Fewer white blood cells (WBCs) are available to fight infection. |
| Altered defense mechanisms | Body damage from trauma disrupts the natural defense mechanism of the skin and mucous membranes, allowing entry to microorganisms. |
| Alcoholism | Has an inhibiting effect on the immune system. |
| Chronic illness | Upsets the normal homeostatic balance within the body, impairing the normal defense mechanisms. Serious illness taxes the immune system, causing greater susceptibility to other pathogens. |
| Indwelling tubes or equipment | Fracture pins, catheters, intravenous (IV) cannulas, feeding tubes, heart valves, and hip prostheses all provide either a portal of entry for microorganisms or a place for colonization of microorganisms. |
| Immunosuppressive treatment, chemotherapy, or corticosteroid treatment | Immunosuppressive treatment or chemotherapy depresses the immune system or harms the bone marrow, decreasing the number of leukocytes and macrophages. Corticosteroids depress the inflammatory response, inhibiting one of the body’s defense mechanisms. |
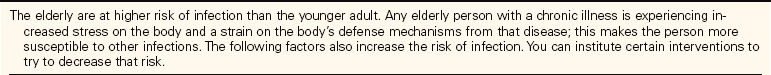
Susceptibility of the Elderly
Many factors can place the elderly person at higher risk of infection. Poor nutrition, poor mobility, poor hygiene, chronic illness, and physiologic changes all contribute to this risk. Table 16-6 presents the physiologic factors involved. Elderly persons are hospitalized more frequently for problems due to a chronic illness or for treatment after a fall than younger people. This places them at higher risk for a health care–associated infection. Health care–associated infections are acquired by patients in health care facilities when microorganisms are transferred to the patient by contaminated objects or infected people.
BODY DEFENSES AGAINST INFECTION
The body has many natural defenses against invasion of pathogens. Intact skin serves as a first line of defense against harmful agents in the environment. It functions as a protective barrier for the underlying tissues. Through excretion of sweat as well as lactic and fatty acids from the sebaceous glands, growth of bacteria is inhibited.
Secretions from the mucous membranes lining the respiratory, gastrointestinal, and reproductive tracts contain an abundance of the enzyme lysozyme, which is bactericidal. This enzyme is also found in tears and saliva. Cilia, which line the respiratory tract, trap microorganisms and debris (dead tissue or foreign matter) and propel them up and out of the body with a wavelike action. The bones protect the more delicate and vital organs from outside trama. The bone marrow produces defensive blood cells.
The Kupffer cells in the liver destroy bacteria that have found their way into the portal liver circulation. Only about 1% of bacteria that enter the portal circulation from the intestines pass through the liver into the general circulation. The intestinal system is a major portal of entry for pathogens, and the liver is an essential part of the body’s defense system. The liver also detoxifies harmful chemicals by isolating various substances and facilitating their breakdown and excretion from the body.
Gastric secretions such as hydrochloric acid easily destroy ingested pathogens. Evacuation of feces flushes bacteria from the intestine, and the formation and elimination of urine flushes the urinary system.
The body’s second line of defense helps destroy pathogens that escape the first line of defense. This includes the mechanisms of fever, leukocytosis, phagocytosis, inflammation, and the action of interferon (biologic response modifier that affects cellular growth).
The body automatically raises its temperature in response to infection. Fever, because of the effect of heat, slows the growth of many pathogens until other body defenses can be mobilized.
Leukocytes, which are white blood cells (WBCs), are released in response to microorganisms, particularly bacteria, entering the body. This increased production or release of leukocytes is termed leukocytosis. They travel through the capillary walls out into the tissues to engulf the invader. The phagocytes, located in the lymphatic tissue, the alveoli of the lungs, the gastrointestinal system, the spleen, and the liver, work to destroy or inactivate them. The macrophages assist in this process by removing cellular debris, engulfing and destroying bacteria and viruses, and removing metabolic waste products. Some phagocytes are called tissue macrophages; others, which are concerned with immunity, are the lymphocytic cells. Phagocytosis is part of the inflammatory response, another defense mechanism of the body. When infection and resultant leukocytosis occur, the WBC count is elevated. If the neutrophil count is decreased on the differential WBC count, while the monocyte count and lymphocyte counts are elevated, the cause of infection is probably viral. Increase in the percentage of basophils may indicate parasitic infection. A large increase in the percentage of monocytes often indicates a bacterial infection.
Interferons are produced in response to viral invasion of the cell. They stimulate antiviral proteins that prevent replication of viruses. Interferons can attack a wide variety of viruses, inhibiting or destroying them. The interferons stimulate the immune system, increase resistance to viral invasion, and interfere with viral replication.
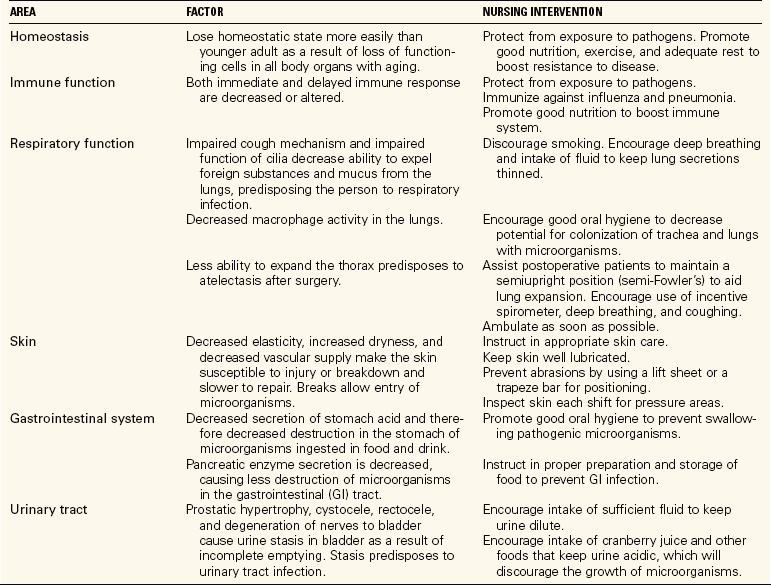
INFLAMMATORY RESPONSE
Inflammation is an immediate response of the body to any kind of injury to its cells and tissues. The inflammatory response can be induced by any mechanical, chemical, or infectious disease–producing factor that injures cells of the body. Inflammation is a localized protective response brought on by injury or destruction of tissues. The blood vessels dilate, bringing more blood to the damaged area, causing redness, warmth, and edema. The basic purposes of the inflammatory response are to (1) neutralize and destroy harmful agents, (2) limit their spread to other tissues in the body, and (3) prepare the damaged tissues for repair. The chemicals histamine and serotonin are released. These chemicals act on the walls of the capillaries, making them more permeable so that water, proteins, and defensive cells can pass out of the blood and into the fluid surrounding the damaged cells. This leakage of fluid is responsible for localized swelling, which in turn causes increased pressure and pain. Fibrinogen promotes clotting, blocking the lymphatic vessels. This results in a walling off of the area that delays spread of bacteria, toxins, and other harmful agents to other parts of the body (Concept Map 16-1). Pus, the debris that sometimes results from the inflammatory process, may accumulate at the site. Phagocytes attracted to the damaged tissue begin their work.
IMMUNE RESPONSE
The immune response is the third line of defense against pathogenic organisms. Microorganisms and other substances that do not belong in the body, such as pollen, are recognized as foreign invaders and trigger an immune response (reaction of the body to substances interpreted as nonself). For example, macrophages in the lungs engulf bacteria, dust particles, and any other foreign material that might threaten to damage the lung tissues. If the foreign particles are not digestible, the leukocytes and later macrophages in the alveoli help wall them off, thereby preventing their spread to other tissues. An example of this process is the localizing of tubercle bacilli that have not been destroyed by the body’s other defenses. Pulmonary tuberculosis bacilli are walled off, preventing their dissemination.
The immune system response is specific to the type of invader. There are unique antigens on the surface of an individual’s cells that aid the immune system in distinguishing self from nonself (invaders) so it can destroy foreign material (antigens). Once exposed to a microorganism, the body will produce antibodies against that invader. In this way, naturally acquired immunity occurs. Every antigen stimulates formation of a specific type of antibody. The next time that same microorganism invades the body, the antibodies respond and attempt to destroy it. Some types of naturally acquired immunity last a lifetime, but others last only a short time.
Passive acquired immunity occurs when a person is given an antitoxin or antiserum that contains antibodies or antitoxins that have been developed in another person. Tetanus antitoxin is an example of a substance that provides passive immunity. It protects a person from the current invasion of microorganisms but does not provide lasting immunity.
Naturally acquired passive immunity occurs when the fetus receives antibodies from the mother through placental blood before birth. This type of immunity is also acquired by the breast-feeding infant. The immunity is temporary and lasts only until the infant’s own immune system matures enough to function properly.
Artificially acquired immunity is achieved through injection of vaccines or immunizing substances that contain dead or inactive microorganisms or their toxins. The vaccine prompts the body to produce antibodies. Vaccinations against polio, measles, hepatitis B, influenza, tetanus, and diphtheria provide this type of immunity.
Artificially acquired passive immunity is provided by injection with antibodies derived from the infected blood of people or animals. Serum immune globulin is often used for this purpose and is given to people who have been exposed to hepatitis A virus or mumps and have not been previously immunized. The injection provides antibodies that will protect the person for a short period of time.
ASEPSIS AND CONTROL OF MICROORGANISMS
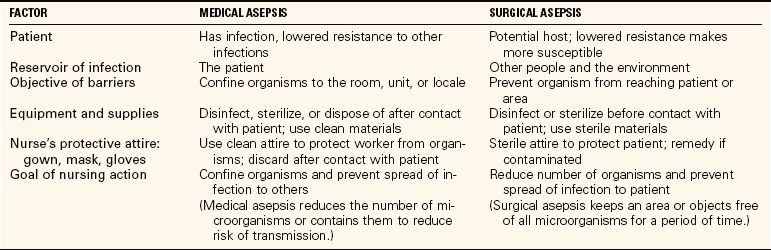
MEDICAL ASEPSIS AND SURGICAL ASEPSIS
Asepsis is the practice of making the environment and objects free of microorganisms. Two types of asepsis are practiced within health care agencies. The first, medical asepsis, is the practice of reducing the number of organisms present or reducing the risk for transmission of organisms. It prevents reinfection of the patient and the spread of infection from person to person. It involves cleanliness and is accomplished by protecting items in the environment from contamination and by disinfecting items that have been contaminated. Medical asepsis is referred to as clean technique because most, but not all, microorganisms are destroyed.
Surgical asepsis is the practice of preparing and handling materials in a way that prevents the patient’s exposure to living microorganisms. Surgical asepsis is referred to as sterile technique. It involves sterilization of all instruments and inanimate equipment, as well as use of sterile supplies and sterile technique for procedures that invade the body and for wound care. Most microorganisms are destroyed. Timed hand scrubs may be used by the personnel working in the operating room to reduce the number of microorganisms on the skin, or a hand rub with an alcohol-based product may be used instead. Barrier garments are used to prevent spread of microorganisms between the health care personnel and the patient. The air in the operating room is filtered and exchanged at least 15 times an hour. The operating room must be thoroughly disinfected after each use. Table 16-7 compares medical and surgical asepsis. Techniques for surgical asepsis are covered in Chapter 37.
HAND HYGIENE
Hand hygiene is one of the most effective ways to reduce the number of microorganisms on the hands, thereby preventing the transfer of microorganisms from one object to another or from person to person by the nurse. Any person may harbor microorganisms that are harmless to that person but may be potentially harmful to another person if they gain a portal of entry.
Gloves should be used to prevent contact with any body fluids. Health care workers must perform hand hygiene before and after giving care to a patient. In 2005, the CDC concluded from research that alcohol hand rubs can be more effective than handwashing in ridding the hands of microorganisms (Centers for Disease Control, 2005). Many hospitals and health care agencies are providing alcohol hand rubs for personnel to use when hands are not visibly contaminated (Figure 16-4). Box 16-2 provides the overview of the new CDC Hand Hygiene Guidelines.
When hands are visibly soiled, the CDC recommends at least a 15-second vigorous washing using soap and friction under running water. The hands should be wet before adding the soap. Drying the hands thoroughly is very important. Skill 16-1 provides the steps for correct hand hygiene. For a surgical scrub, the hands are washed with soap and water first and then scrubbed with an FDA-compliant antimicrobial scrub agent or an FDA-compliant alcohol-based antiseptic hand rub agent. The procedure for surgical hand antisepsis is presented in Chapter 17 (Health Promotion Points 16-2).
You should not wear jewelry when you are providing patient care because microorganisms become lodged in the settings of stones, in the grooves of rings, and on the skin beneath the jewelry. The only exceptions are a plain wedding band and a watch with an expandable band that allows it to be pushed up above the wrist area for hand hygiene. Fingernails should be kept clean and short, both for patient safety and because it is easier to clean fully beneath a short nail. Polish, if used, should not be chipped because it could then harbor bacteria. No artificial nails, nail wraps, or nail jewelry should be worn. Proper hand care includes prevention of hangnails and skin abrasions, which provide a point of entry for bacteria into the body.
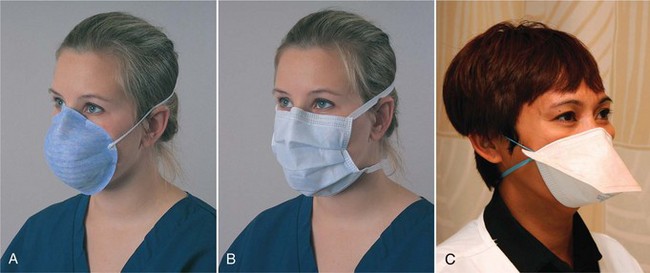
STANDARD PRECAUTIONS
Infectious disease can be controlled by interrupting the chain of infection at any link. This breaks the transmission cycle. Standard Precautions have been developed by the CDC to facilitate breaking the chain of infection. These precautions protect both the nurse and the patient and are to be used for every patient contact; they are listed in Box 16-3 on p. 225 and include the use of hand hygiene and personal protective equipment (PPE). PPE includes gloves, gowns, masks, protective eyewear, shoe covering, and hair covering.
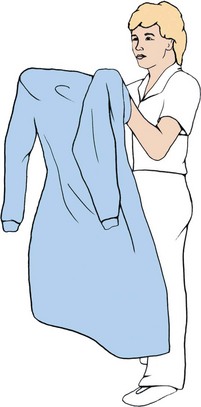
Gown
A clean barrier gown that is impermeable to fluid is worn when there is a chance of being splashed with blood, body fluid, or other potentially infectious materials, or when these fluids may be aerosolized. The gown must be impermeable to water. The gown is removed after use, being careful not to contaminate the skin or clothing. Skill 16-2 on p. 226 explains how to put on and take off a barrier gown.
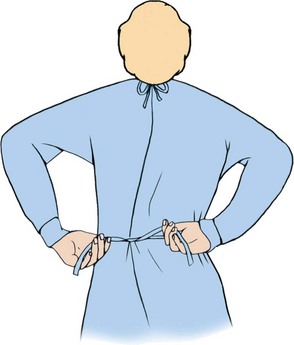
Mask
A mask is applied before entering the room if there is a chance that the nurse will be in contact with an airborne pathogen or splashed body fluids, such as when a patient is coughing or the nurse is performing endotracheal suctioning. The mask is placed over the nose and mouth and is secured in place by an elastic band or ties (Figure 16-5, p. 228). An N95 respirator mask is worn when entering an area where pulmonary tuberculosis or other dangerous airborne microorganisms are known to be present. N95 respirator masks must be approved by the Occupational Safety and Health Administration (OSHA). They prevent passage of 95% of particulate matter. There are several styles of both types of masks. Masks should be removed, handling only the elastic band or ties, and discarded when not in use; they should not be left hanging around the neck. The mask should be changed any time it becomes moist.
Protective Eyewear
Protective eyewear is worn to prevent fluid from entering the eye area and coming in contact with the mucosa or surface of the eye through splattering or aerosolization. Eyewear may be in the form of goggles, a face shield, or glasses with side and top pieces. Protective eyewear may be disposable or durable. If of the durable variety, the eyewear should be disinfected after each use. Eyewear is worn when performing oral, nasotracheal, or endotracheal suctioning (unless a closed system is used); for performing wound irrigations; and whenever performing or assisting with procedures in which blood might splatter. An example of such a procedure is the insertion of a central venous line.
Head Cover
A cap or head cover is placed on the head if there is danger of contamination of the hair or if microorganisms resident in the hair might endanger the patient. The cap is removed by slipping the fingers beneath the elastic and handling only the inner surface of the contaminated head cover to prevent hand contamination.
Shoe Covers
Skin around the ankles should be covered by appropriate protective covers whenever there is a chance of splashing body fluids during a procedure. Shoes are covered so that pathogens are not carried out of the room; the covers are removed when exiting the room in the same manner as the head cover.
Gloves
Disposable gloves are used for Standard Precautions and are worn when there is a chance that there will be contact with blood or body fluids, mucous membranes, nonintact skin, or secretions or excretions. Gloves are also used for handling items contaminated with these substances. They are put on after the other pieces of personal protective equipment have been donned. Gloves reduce the possibility of transmission of microorganisms between the nurse and the patient. Hand hygiene is performed before gloving and immediately after removing the gloves because no glove is 100% protective. Gloves are contaminated once they are used and must be discarded before doing the next task or caring for the next patient. Steps 16-1 show how to properly remove contaminated gloves (Figure 16-6). The gloves are immediately placed in a trash receptacle, and hand hygiene is performed. Gloves are never reused or washed. When a gown is worn, gloves are pulled up over the cuffs of the gown.
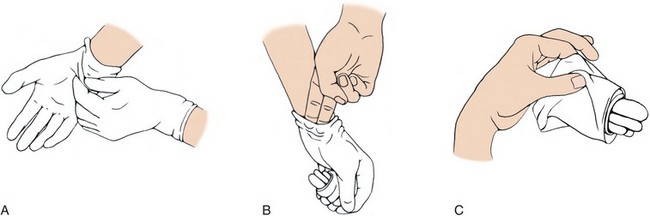
FIGURE 16-6 A, Removal of the right glove. B, Removal of the left glove. C, Method of holding the removed gloves.
Latex Allergy.: Since the adoption of Standard Precautions, the use of latex has dramatically increased in health care. Because of the greater exposure through glove use, more people have developed sensitivity or allergy to latex. Exposure may cause redness, local inflammation and pruritus of the hands, and anaphylaxis. People who have had multiple surgical procedures; who have food allergies to bananas, kiwis, or avocados; or who have had histories of reactions to other latex-containing products are at risk for the development of this allergy. If a health care worker has a latex allergy, by law the employer must supply an alternative type of glove. Measures to help prevent latex sensitivity include using gloves in appropriate situations and not for routine tasks in which a blood, body fluid, or microorganism contact exposure is unlikely. Gloves are removed directly over a trash receptacle without “snapping” them off. Do not use petroleum-based lotions under latex gloves because they attract latex proteins from the gloves, which can increase the risk of developing the allergy.
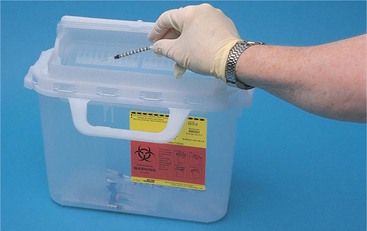
Disposal of Sharps
Disposable sharp instruments, referred to as “sharps,” are placed directly into a special red, puncture-resistant sharps biohazard container immediately after use (Figure 16-7). All needles, intravenous (IV) cannulas, and items that are sharp or might cause a skin break are placed in the sharps container (Safety Alert 16-1). Sharps containers should be replaced when they are three-quarters full.
Contaminated Waste
Items contaminated with infectious material must be disposed of in sealed, impermeable, plastic bags marked “Hazardous Waste” or “Biohazard.” This includes soiled dressings, used sanitary pads, suction drainage containers, and any other item that has been in contact with body fluids. Contaminated linens are handled in a like manner unless all linen in the facility is treated as a contaminated biohazard. Soiled linens should be gathered carefully and bagged at the site of use.
CLEANING AND DISINFECTION
Pathogens can be killed or inactivated by disinfection, sterilization, or the use of sanitizing agents. Eliminating the reservoir is a good way to prevent transmission. Water, sewage treatment, and rodent control eliminate reservoirs for pathogens.
Appropriate cleaning removes and inhibits the growth of microorganisms. Always wear gloves when cleaning visibly soiled objects or whenever performing wound care. Whether in the hospital, a long-term care facility, or a home setting, certain steps should be followed for cleaning objects:
1. Rinse the object with cold water to remove organic material. Hot water coagulates protein contained in organic material, making it adhere to the item.
2. Once all visible organic material has been removed, wash the object in hot, soapy water. Soap’s emulsifying action reduces surface tension and helps remove soil. (How the object is washed and the agent used depends on the object and the manufacturer’s recommendation for cleansing and sanitizing.)
3. Use a stiff-bristled brush or abrasive to clean equipment with grooves and narrow spaces. Friction helps dislodge soil.
4. Rinse the object well with moderately hot water.
5. Dry the object; it is now considered clean, but not sterile.
Always disinfect the cleaning equipment and the sink when you have finished cleaning soiled objects.
Disinfectant agents can be used to eliminate some types of organisms that are left after cleansing. Disinfectants are solutions containing chemical compounds such as phenol, alcohol, or chlorine that kill or inactivate nearly all microorganisms. These chemicals can be caustic to the skin and are used only on inanimate objects. A recommended disinfectant is chlorine bleach and water at a ratio of 1:10. Before disinfection, items must be thoroughly rinsed after cleaning because soap may react with the disinfectant, preventing its killing properties from working. An antiseptic is a chemical compound that is used on skin or tissue to inhibit the growth of or to eliminate microorganisms. Disinfectants and antiseptics have bactericidal or bacteriostatic properties. A bactericidal solution destroys bacteria; a bacteriostatic solution prevents the growth and reproduction of some bacteria. Povidone-iodine is an example of an antiseptic. Items that cannot be sterilized, such as skin, can be disinfected with antiseptic agents.
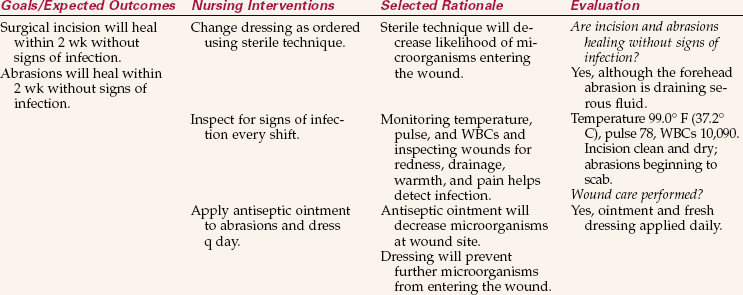
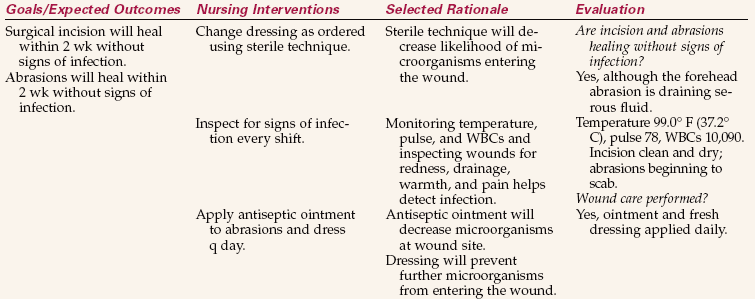
Wounds are cleansed using sterile normal saline or an antiseptic solution. Often a bacteriostatic cream or ointment is applied before the wound is dressed (Nursing Care Plan 16-1). (Also refer to the Companion CD-ROM for Nursing Care Plan 16-2: Care of the Patient with a Foot Wound.)
Sterilization
Sterilization is the best method of eliminating microorganisms from equipment and supplies. There are five methods of sterilization: steam/moist heat, dry heat/hot air, ethylene oxide, low-temperature gas plasma, and radiation.
Moist heat is most often used as steam under pressure in a device called an autoclave. Steam under pressure attains temperatures higher than the boiling point. Under pressure, steam reaches temperatures of 250°to 275°F (121°to 135°C).
Ethylene oxide gas is effective against microorganisms and spores. It is used for heat-sensitive items and where good penetration is essential.
For cleansing items in the home, boiling in water is the easiest method. Items should be boiled for a minimum of 16 minutes. Items that cannot be boiled or disinfected by running them through the dishwasher’s “sanitize” cycle can be exposed to direct sunlight for several hours. The heat and ultraviolet rays will kill exposed microorganisms.
ASEPSIS IN THE HOME ENVIRONMENT
Precautions are not as stringent in the home as in the hospital because the ordinary home does not contain the many pathogens found in a hospital environment. The number and degree of home precautions are based on whether there is an infected person in residence and what microorganism is involved. Contaminated dressings and other disposable supplies are secured in plastic zip-closure bags before disposal. Linens contaminated with blood or body secretions should be placed in a sealed plastic bag until laundered. They should be rinsed in cold water as soon as possible and then washed in hot, soapy water. Hot water causes protein to coagulate, making cleaning more difficult.
A 1:10 solution of chlorine bleach and water can be used to disinfect counters and bathrooms if they become soiled with body secretions. Running the dishwasher on the “sanitize” cycle or scalding eating utensils with boiling water will reduce microorganisms.
Frequent “damp” dusting and vacuuming decreases the number of microorganisms in the environment. Exposing bedding and other items the patient uses that cannot be disinfected to 6 to 8 hours of sunshine may reduce the number of microorganisms on them. Tissues containing expectorated sputum or nasal secretions of an infected patient should be disposed of in a sealable plastic bag.
Forceps, scissors, and other small implements used for dressing changes can be washed with hot water and detergent, and then soaked in a bleach solution. They should be rinsed, drained, allowed to air dry, and then stored in a covered container. Drainage bags can be cleansed, disinfected, dried, and reused.
INFECTION CONTROL SURVEILLANCE
Within each health care agency, there is an infection control practitioner who is responsible for ensuring infection prevention and control measures are followed. When a patient is known to have an infection, the information is typically reported to the infection control professional. This person works with the health care staff to ensure they understand which patient care and environmental cleaning measures are to be used. This professional also assesses for spread of infection. All hospital patients are at risk for health care–associated infection, and each nurse must be vigilant in watching for signs of infection in each patient under his care. Patients at high risk for infection are those who (1) are weakened by injury or severe illness; (2) have another chronic illness; (3) have a central venous catheter, IV cannula, or indwelling drainage tube; (4) are very young or very old; (5) have an open wound; (6) have a surgical incision; or (7) have a compromised immune system from chemotherapy or immunosuppression. Whenever an infection is suspected, additional precautions are taken to prevent the possible spread of microorganisms.
NCLEX-PN® EXAMINATION–STYLE REVIEW OUESTIONS
Choose the best answer(s) for each question.
1. The most common method of microorganism transfer from one person to another in the hospital setting is prevented by:
2. The skin is the first line of defense and protects the body by: (Select all that apply.)
3. The reason for lengthening hand hygiene time when hands are contaminated is to:
1. render the skin totally free of microorganisms.
2. mechanically remove as many microorganisms as possible.
4. Means to decrease susceptibility of individuals to infection include: (Select all that apply.)
1. discouraging visitors who have an infectious illness.
2. using gloves and hand hygiene techniques properly.
3. giving antibiotics prophylactically at the time of surgery.
5. Drug-resistant organisms are a problem within the community as well as within the hospital. Reasons for this include: (Select all that apply.)
1. overprescription of antibiotics by health care providers.
2. lack of proper sanitation within communities.
3. discharging patients with infected wounds before treatment is complete.
4. patients stopping taking antibiotics before all of the prescription is gone.
5. mutation of microorganisms in response to commonly used antibiotics.
6. When applying PPEs before entering a patient’s room, if a gown, gloves, mask, and eyewear are required, indicate the proper sequence for putting them on: _____, _____, _____, and _____ .
7. Malnutrition contributes to the susceptibility to infection because:
1. there is little energy for healing.
2. it decreases immune function.
8. Passive acquired immunity is obtained by:
9. Medical asepsis differs from surgical asepsis in that medical asepsis is aimed at:
CRITICAL THINKING ACTIVITIES ? Read each clinical scenario and discuss the questions with your classmates.
Scenario A
Discuss specific ways in which a person with a cold who goes to the movies can transmit the virus to others.
Scenario B
You are assigned to care for a patient who has viral pneumonia, a disease of the respiratory tract. What precautions would be necessary?