Management of Facial Fractures
Trauma to the facial region frequently results in injuries to soft tissue, teeth, and major skeletal components of the face, including the mandible, maxilla, zygoma, nasoorbital-ethmoid (NOE) complex, and supraorbital structures. In addition, these injuries frequently occur in combination with injuries to other areas of the body.1 Participation in the treatment and rehabilitation of the patient with facial trauma involves a thorough understanding of the types of, principles of evaluation for, and surgical treatment of facial injuries. This chapter outlines the fundamental principles for treatment of the patient with facial trauma.
EVALUATION OF PATIENTS WITH FACIAL TRAUMA
Before completing a detailed history and physical evaluation of the facial area, critical injuries that may be life threatening must be addressed. The first step in evaluating a trauma patient is to assess the patient’s cardiopulmonary stability by ensuring that the patient has a patent airway and that the lungs are adequately ventilated. Vital signs, including respiratory and pulse rates and blood pressure, should be taken and recorded. During this initial assessment (i.e., primary survey), other potentially life-threatening problems, such as excessive bleeding, should also be addressed. Immediate measures, such as pressure dressings, packing, and clamping of briskly bleeding vessels, should be accomplished as quickly as possible. An assessment of the patient’s neurologic status and an evaluation of the cervical spine should be completed next. Forces severe enough to cause fractures of the facial skeleton are often transmitted to the cervical spine. The neck should be temporarily immobilized until neck injuries have been ruled out. Careful palpation of the neck to assess possible areas of tenderness and a cervical spine radiographic series should be completed as soon as possible.
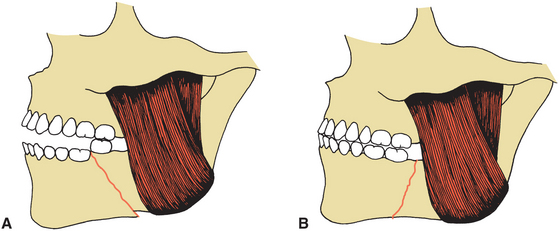
Treatment of head and neck injuries generally should be deferred until a thorough evaluation, assessment, and stabilization of the patient has been accomplished. However, some initial treatment is often necessary to stabilize the patient. Management of the patient’s airway is of vital importance. Frequently, fractures of the facial bones severely compromise the patient’s ability to maintain the airway, particularly when the patient is unconscious or completely supine. Severe mandible fractures, especially bilateral or comminuted fractures, can cause posterior displacement of the mandible and tongue, which results in obstruction of the upper airway (Fig. 24-1).
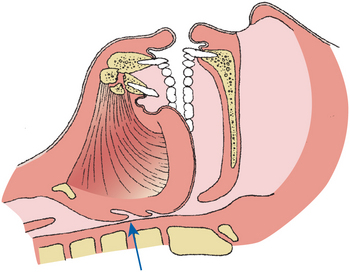
FIGURE 24-1 Posterior displacement of tongue and occlusion of upper airway resulting from bilateral mandibular fractures.
Simply grasping, repositioning, and stabilizing the mandible into a more anterior position may alleviate this obstruction. Placement of a nasopharyngeal or an oropharyngeal airway may also be sufficient to temporarily maintain a patent airway. In some cases, endotracheal intubation may be necessary. Any prosthetic devices, avulsed teeth, pieces of completely avulsed bone, or other debris may also contribute to airway occlusion and must be removed immediately. Any areas of bleeding should be quickly examined and managed with packing, pressure dressings, or clamping. All excess saliva and blood must be suctioned from the pharynx to avoid aspiration and laryngospasm.
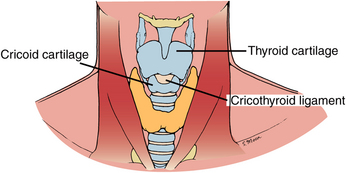
Injuries to the facial region may involve not only bones of the face but also soft tissue, such as the tongue or upper neck areas, or they may be associated with injuries such as a fractured larynx.2 In some cases an emergency tracheostomy may be necessary to provide an adequate airway. In trauma patients who have complete upper airway obstruction, a cricothyrotomy is the most rapid way to access the trachea (Fig. 24-2).
History and Physical Examination
After the patient has been initially stabilized, as complete a history as possible should be obtained. This history should be obtained from the patient; however, because of loss of consciousness or impaired neurologic status, information must often be obtained from witnesses or accompanying family members. Five important questions should be considered: (1) How did the accident occur? (2) When did the accident occur? (3) What are the specifics of the injury, including the type of object contacted, the direction from which contact was made, and similar logistic considerations? (4) Was there a loss of consciousness? (5) What symptoms are now being experienced by the patient, including pain, altered sensation, visual changes, and malocclusion? A complete review of systems, including information about allergies, medications, and previous tetanus immunization, medical conditions, and prior surgeries should be obtained.
Physical evaluation of the facial structures should be completed only after an overall physical assessment that addresses cardiopulmonary and neurologic functions and other areas of potential trauma, including the chest, abdomen, and pelvic areas. Because patients with multiple severe injuries frequently require evaluation and treatment by several specialists, trauma teams have become standard in the emergency departments of major hospitals. These teams usually include general surgeons and specialists in cardiothoracic surgery, vascular surgery, orthopedic surgery, neurosurgery, and anesthesiology; these specialists are on call to provide immediate attention to emergency department patients. Other trauma team specialists include oral and maxillofacial surgeons, ophthalmologists, otolaryngologists, plastic surgeons, and urologists. The combined efforts of these specialists are frequently required to assess and treat the patient’s injuries properly.
Evaluation of the facial area should be performed in an organized and sequential fashion. The face and cranium should be carefully inspected for evidence of trauma, including lacerations, abrasions, contusions, areas of edema or hematoma formation, and possible contour defects. Areas of ecchymosis should be carefully evaluated.
Periorbital ecchymosis, especially with subconjunctival hemorrhage, is often indicative of orbital rim or zygomatic complex fractures (Fig. 24-3). Bruises behind the ear, or Battle’s sign, suggest a basilar skull fracture. Ecchymosis in the floor of the mouth usually indicates an anterior mandibular fracture.
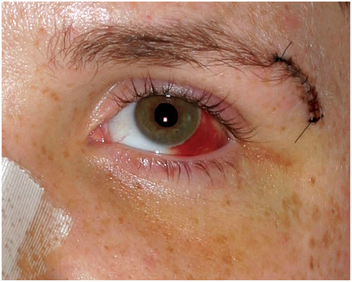
FIGURE 24-3 Periorbital ecchymosis and lateral subconjunctival hemorrhage associated with zygomatic complex fracture.
A neurologic examination of the face should include careful evaluation of all cranial nerves. Vision, extraocular movements, and pupillary reaction to light should be carefully evaluated. Visual acuity or pupillary changes may suggest intracranial (cranial nerve II or III dysfunction) or direct orbital trauma. Uneven pupils (anisocoria) in a lethargic patient suggest an intracranial bleed (subdural or epidural hematoma or intraparenchymal bleed) or injury. An asymmetric or irregular (not round) pupil is most likely caused by a globe (eyeball) perforation. Abnormalities of ocular movements may also indicate central neurologic problems (cranial nerves III, IV, or VI) or mechanical restriction of the movements of the eye muscles resulting from fractures of the orbital complex (Fig. 24-4). Motor function of the facial muscles (cranial nerve VII) and muscles of mastication (cranial nerve V) and sensation over the facial area (cranial nerve V) should be evaluated. Any lacerations should be carefully cleaned and evaluated for possible transection of major nerves or ducts, such as the facial nerve or Stensen’s duct.

FIGURE 24-4 A, 14-year-old patient with a left orbital floor fracture in upward gaze. B, Entrapment of inferior rectus muscle is the result of impingement in area of linear orbital floor fracture. In down gaze, patient is unable to rotate the left eye inferiorly, whereas the right eye is fully rotated inferiorly.
The mandible should be carefully evaluated by extraorally palpating all areas of the inferior and lateral borders and the temporomandibular joint, paying particular attention to areas of point tenderness. The occlusion should be examined, and step deformities along the occlusal plane and lacerations of gingival areas should be assessed (Fig. 24-5). Bimanual palpation of the suspected fracture area should be performed by placing firm pressure over the mandible posterior and anterior to the fracture area in an attempt to manipulate and elicit mobility in this area. The occlusion should be reexamined after this maneuver. Mobility of the teeth in the area of a possible fracture should also be noted.
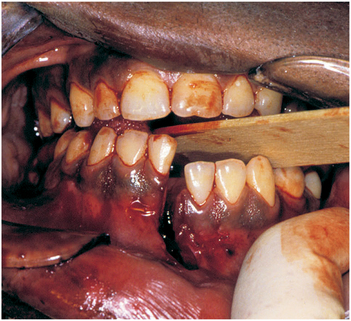
FIGURE 24-5 Irregularity of plane of occlusion and laceration in gingiva and mucosa between the mandibular central incisors, indicating a likelihood of mandibular fracture in this area.
The evaluation of the midface begins with an assessment of the mobility of the maxilla as an isolated structure or in combination with the zygoma or nasal bones. To assess maxillary mobility, the patient’s head should be stabilized by using pressure over the forehead with one hand. With the thumb and forefinger of the other hand, one grasps the maxilla; firm pressure should be used to elicit maxillary mobility (Fig. 24-6).

FIGURE 24-6 Examination of maxilla for mobility. A, Firm pressure on forehead is used to stabilize patient’s head. Pressure is placed on maxilla in attempt to elicit mobility. B, Stabilizing hand can also evaluate mobility in area of nasal bones.
The upper facial and midfacial regions should be palpated for step deformities in the forehead, orbital rim, or nasal or zygoma areas. Firm digital pressure over these areas is used to carefully evaluate the bony contours and may be difficult when these areas are grossly edematous. In checking for a zygomatic complex or arch fracture, an index finger can be inserted in the maxillary vestibule adjacent to the molars while palpating and applying pressure superolaterally. Bony crepitus (the ability to feel the vibration as fractured bone edges are rubbed against one another) or extreme tenderness warrants a further workup. An evaluation of the nose and paranasal structures includes measurement of the intercanthal distance between the innermost portions of the left and right medial canthus. Frequently, nasoorbital ethmoid injuries cause spreading of the nasal bones and displacement of the medial canthal ligaments, resulting in traumatic telecanthus (widening of the medial intercanthal distance; Fig. 24-7). Normally, the medial intercanthal distance should equal the alar base width. The nose should also be evaluated for symmetry. The bony anatomy of the nose should be evaluated by palpation. A nasal speculum is used to visualize internal aspects of the nose to locate excessive bleeding or hematoma formation, particularly in the area of the nasal septum.

FIGURE 24-7 Injury to nasoorbital-ethmoid (NOE) complex, which resulted in the displacement of medial canthal ligaments and a widening of the intercanthal distance (i.e., traumatic telecanthus). A, Diagram of bony fractures and medial canthal ligament displacement. B, Clinical photograph.
Intraoral inspection should include an evaluation of areas of mucosal laceration or ecchymosis in the buccal vestibule or along the palate and an examination of the occlusion and areas of loose or missing teeth. These areas should be assessed before, during, and after manual manipulation of the mandible and midface. Unilateral occlusal prematurities with contralateral open bites are highly suspicious for some type of jaw fracture.
Radiographic Evaluation
After a careful clinical assessment of the facial area, radiographs should be taken to provide additional information about facial injuries.3 In cases of severe facial trauma, cervical spine injuries should be ruled out with a complete cervical spine series (i.e., cross-table, odontoid, and oblique views) before any manipulation of the neck. The facial radiographic examination should depend to some degree on the clinical findings and the suspected injury. Haphazard or excessive radiographic examination is generally not warranted. In the patient with facial trauma, the purpose of radiographs should be to confirm the suspected clinical diagnosis, obtain information that may not be clear from the clinical examination, and more accurately determine the extent of the injury. Radiographic examination should also document fractures from different angles or perspectives.
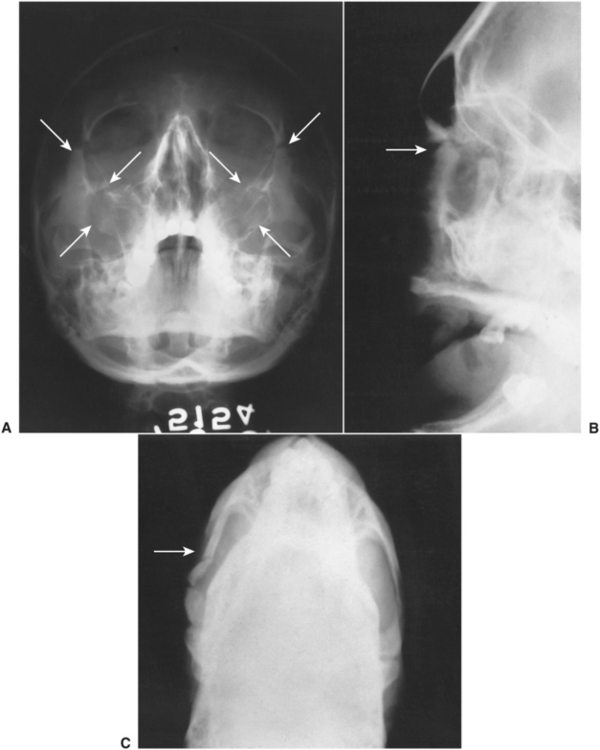
Radiographic evaluation of the mandible generally requires two or more of the following four radiographic views: (1) panoramic view, (2) open-mouth Towne’s view, (3) posteroanterior view, and (4) lateral oblique views (Fig. 24-8). Occasionally, even these radiographs do not provide adequate information; therefore, supplemental radiographs, including occlusal or periapical views, may be helpful.3 Computed tomography (CT) scans, axial views without intravenous contrast medium, may provide information not obtainable from plain radiographs or when cervical spine precautions or other injuries do not permit standard facial films. Because many patients with facial trauma often receive a CT scan to rule out neurologic injury, this scan can also be used to supplement the radiographic evaluation.

FIGURE 24-8 A, Posterior-anterior view demonstrates a fracture in the angle area of the mandible (arrow). B, Lateral oblique view shows a fracture in the angle area (arrow). C, Towne’s view shows a displacement of condylar fracture (arrow). D, Panoramic view shows a displaced fracture of the left mandibular body and right subcondylar fracture (arrows).
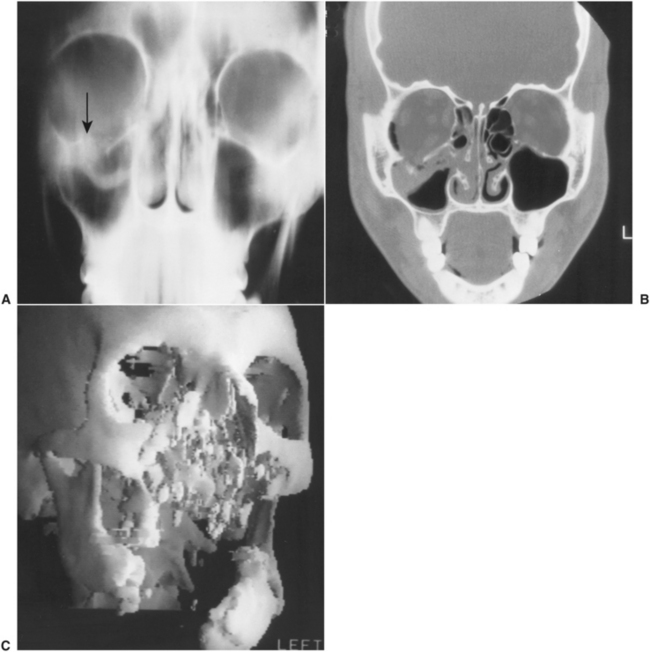
Evaluation of midface fractures was often supplemented with radiographic views, including Waters’ view, lateral skull view, posteroanterior skull view, and submental vertex view (Fig. 24-9). However, because of the difficulty of interpreting plain radiographs of the midface, more sophisticated techniques are generally used. These techniques often include CT scans done in several planes of space (e.g., axial and coronal) or, frequently with three-dimensional reconstruction (Fig. 24-10).4
CAUSE AND CLASSIFICATION OF FACIAL FRACTURES
The major causes of facial fractures include motor vehicle accidents and altercations. Other causes of injuries include falls, sports-related incidents, and work-related accidents.5,6 Facial fractures resulting from motor vehicle accidents are far more frequent in persons who were not wearing restraints at the time of the accident.
Mandibular Fractures
Depending on the type of injury and the direction and force of the trauma, fractures of the mandible commonly occur in several locations. One classification of fractures describes mandibular fractures by anatomic location. Fractures are designated as occurring in the condylar, ramus, angle, body, symphyseal, alveolar, and, rarely, coronoid process areas. Figure 24-11 illustrates the location and frequency of different types of mandibular fractures.7
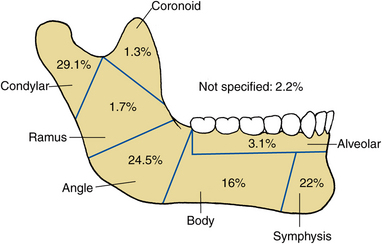
FIGURE 24-11 Anatomic distribution of mandibular fractures. (From Olson RA, Fonseca RJ, Zeitler DL et al: Fractures of the mandible: a review of 580 cases, J Oral Maxillofac Surg 40:23, 1982.)
Another system of classification of mandibular fractures categorizes the type of fracture as greenstick, simple, comminuted, and compound fractures (Fig. 24-12). These categories describe the condition of the bone fragments at the fracture site and possible communication with the external environment. Greenstick fractures are those involving incomplete fractures with flexible bone. Greenstick fractures generally exhibit minimal mobility when palpated and the fracture is incomplete. A simple fracture is a complete transection of the bone with minimal fragmentation at the fracture site. In a comminuted fracture the fractured bone is left in multiple segments. Gunshot wounds, penetrating objects, and other high-impact injuries to the jaws frequently result in comminuted fractures. A compound fracture results in communication of the margin of the fractured bone with the external environment. In maxillofacial fractures, communication with the oral or external environment may result from mucosal tears, perforation through the gingival sulcus and periodontal ligament, communication with sinus linings, and lacerations in the overlying skin. By definition, any jaw fracture within a tooth-bearing segment is an open or compound fracture.
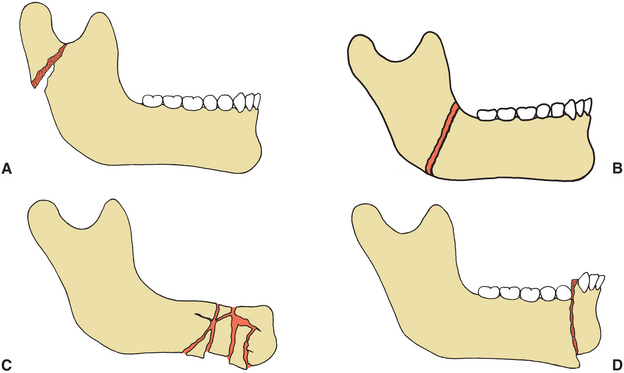
FIGURE 24-12 Types of mandible fractures classified according to extent of injury in area of fracture site. A, Greenstick. B, Simple. C, Comminuted. D, Compound. Bone would be exposed through mucosa near teeth.
Fractures of the mandible are referred to as favorable or unfavorable, depending on the angulation of the fracture and the force of the muscle pull proximal and distal to the fracture. In a favorable fracture, the fracture line and the muscle pull resist displacement of the fracture (Fig. 24-13). In an unfavorable fracture, the muscle pull results in displacement of the fractured segments.
Midface Fractures
Midfacial fractures include fractures affecting the maxilla, the zygoma, and the nasoorbital-ethmoid (NOE) complex. Midfacial fractures can be classified as Le Fort I, II, or III fractures, zygomaticomaxillary complex fractures, zygomatic arch fractures, or NOE fractures. These injuries may be isolated or occur in combination.8
The Le Fort I fracture frequently results from the application of horizontal force to the maxilla, which fractures the maxilla through the maxillary sinus and along the floor of the nose. The fracture separates the maxilla from the pterygoid plates and nasal and zygomatic structures (Fig. 24-14, A). This type of trauma may separate the maxilla in one piece from other structures, split the palate, or fragment the maxilla. Forces that are applied in a more superior direction frequently result in Le Fort II fractures, which is the separation of the maxilla and the attached nasal complex from the orbital and zygomatic structures (Fig. 24-14, B). A Le Fort III fracture results when horizontal forces are applied at a level superior enough to separate the NOE complex, the zygomas, and the maxilla from the cranial base, which results in a so-called craniofacial separation (Fig. 24-14, C). Invariably, midfacial fractures are hybrids or combinations of the previously mentioned injuries.
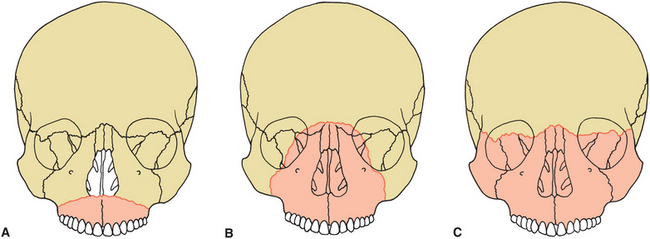
FIGURE 24-14 Le Fort midfacial fractures. A, Le Fort I fracture separating inferior portion of maxilla in horizontal fashion, extending from piriform aperture of nose to pterygoid maxillary suture area. B, Le Fort II fracture involving separation of maxilla and nasal complex from cranial base, zygomatic orbital rim area, and pterygoid maxillary suture area. C, Le Fort III fracture (i.e., craniofacial separation) is complete separation of midface at level of nasoorbital-ethmoid complex and zygomaticofrontal suture area. Fracture also extends through orbits bilaterally.
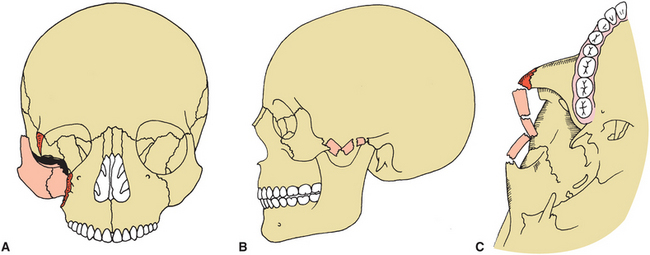
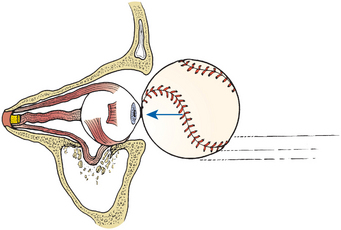
The most common type of midfacial fracture treated in the operating room setting is the zygomatic complex fracture (Fig. 24-15, A). This type of fracture results when an object, such as a fist or a baseball, strikes the lateral aspect of the cheek. Similar trauma can also result in isolated fractures of the nasal bones, the orbital rim, or the orbital floor areas. Blunt trauma to the eye can result in compression of the globe and subsequent blow-out facture of the orbital floor (Fig. 24-16). The zygomatic arch may also be affected, alone or in combination with other injuries (Fig. 24-15, B and C).
TREATMENT OF FACIAL FRACTURES
Whenever facial structures are injured, treatment must be directed toward maximal rehabilitation of the patient. For facial fractures, treatment goals include rapid bone healing; a return of normal ocular, masticatory, and nasal function; restoration of speech; and an acceptable facial and dental esthetic result. During the treatment and healing phases, it is also important to minimize the adverse effect on the patient’s nutritional status and achieve treatment goals with the least amount of discomfort and inconvenience possible.
To achieve these goals, the following basic surgical principles should serve as a guide for treatment of facial fractures: reduction of the fracture (i.e., restoration of the bony segments to their proper anatomic location) and fixation of the bony segments to immobilize segments at the fracture site. In addition, the preoperative occlusion must be restored, and any infection in the area of the fracture must be eradicated or prevented.
The timing of treatment of facial fractures depends on many factors. In general, it is always better to treat an injury as soon as possible. Evidence shows that the longer open or compound wounds are left untreated, the greater is the incidence of infection and malunion. In addition, a delay of several days or weeks makes an ideal anatomic reduction of the fracture difficult if not impossible. Additionally, edema progressively worsens over 2 to 3 days after an injury and frequently makes treatment of a fracture more difficult.
However, treatment of facial fractures is frequently delayed for several reasons. In many cases, patients have other injuries that demand more immediate treatment. An injury such as severe neurologic trauma that precludes presurgical stabilization of the patient and increases anesthetic and surgical risks should obviously be managed before facial fractures. In some cases a delay of 1 or 2 days results in the presence of tissue edema that makes a further wait of 3 to 4 days necessary for elimination of the edema and easier fracture treatment. Although treatments of maxillary and mandibular fractures frequently have many aspects in common, these types of fractures are addressed separately in this chapter. Traditionally, the plan for treatment of most facial fractures was to begin with reduction of mandibular fractures and work superiorly through the midface. The rationale was that the mandible could be most easily stabilized, and the occlusion and remainder of the facial skeleton could be set to the reduced mandible. However, with the advent of and improvement in rigid fixation (plate and screw) techniques, facial fracture treatment may begin in the area where fractures can be most easily stabilized and progress to the most unstable fracture areas.
In approaching facial fractures, the surgeon attempts to rebuild the face based on the concept that certain bony structures within the face provide the primary support in the vertical and anteroposterior directions. Three buttresses exist bilaterally that form the primary vertical supports of the face: (1) the nasomaxillary, (2) the zygomatic, and (3) the pterygomaxillary buttresses (Fig. 24-17).9 The structures that support the facial projection in an anterior-posterior direction include the frontal bar, zygomatic arch and zygoma complex, maxillary alveolus and palate, and the basal segment of the mandible.10 Regardless of the type of facial fracture or the surgical approach used, the initial procedure should be to place the teeth in the proper occlusion and then appropriately reduce the bony fractures. Bony repair should also precede soft tissue repair.
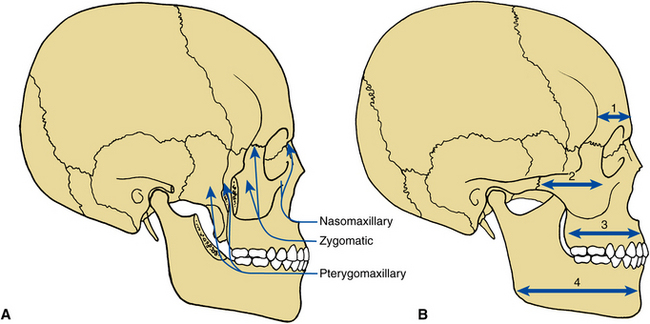
FIGURE 24-17 A, Facial buttresses responsible for vertical support: nasomaxillary, zygomatic, and pterygomaxillary. B, Anteroposterior buttresses: frontal (1), zygomatic (2), maxillary (3), and mandibular (4).
Mandibular Fractures
The first and most important aspect of surgical correction is to reduce the fracture properly or place the individual segments of the fracture into the proper relationship with each other. In the proper reduction of fractures of tooth-bearing bones, it is most important to place the teeth into the preinjury occlusal relationship. Merely aligning and interdigitating the bony fragments at the fracture site without first establishing a proper occlusal relationship rarely results in satisfactory postoperative functional occlusion.
Establishing a proper occlusal relationship by wiring the teeth together is termed maxillomandibular fixation (MMF) or intermaxillary fixation (IMF). Several techniques have been advocated for IMF (Fig. 24-18). The most common technique includes the use of a prefabricated arch bar that is adapted and circumdentally wired to teeth or acid-etch bonded in each arch; the maxillary arch bar is wired to the mandibular arch bar, thereby placing the teeth in their proper relationship. Other wiring techniques, such as Ivy loops or continuous loop wiring, have also been used for the same purpose. When fractures have not been treated for several days or are grossly displaced, it may be difficult to place the fractured segments immediately into their proper position and into adequate IMF. Heavy elastic traction can be used to pull the bony segments into their proper positions gradually over several hours or a few days (Fig. 24-19). Treatment of fractures using only IMF is called closed reduction because it does not involve direct opening, exposure, and manipulation of the fractured area.
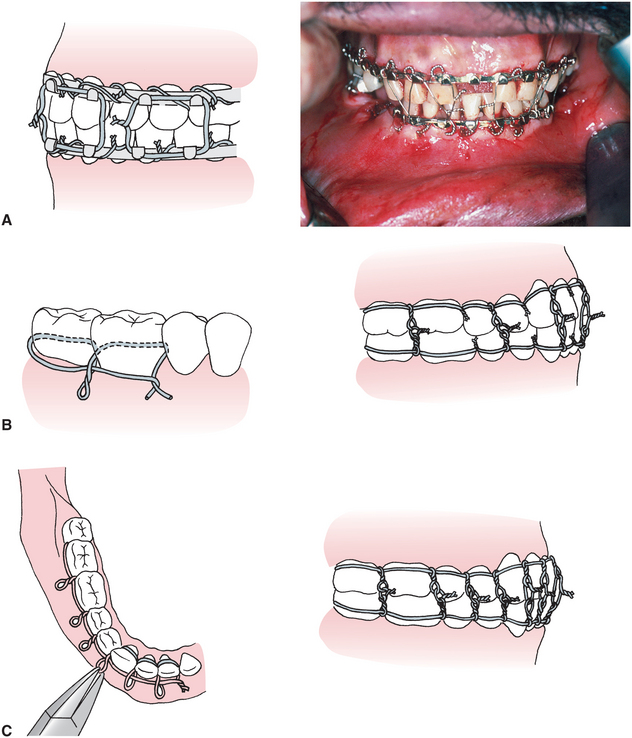
FIGURE 24-18 Intermaxillary fixation wiring techniques. A, Arch bar intermaxillary fixation. B, Ivy loop wiring technique. C, Continuous loop wiring technique. (Modified from Kruger E, Schilli W: Oral and maxillofacial traumatology, vol 1, Chicago, 1982, Quintessence.) Quintessence

FIGURE 24-19 Arch bars used in combination with heavy elastic traction to pull bones gradually into proper alignment and to establish preinjury occlusion. Once the closed reduction had been achieved, maxillomandibular wires replace the elastics and are maintained for 6 weeks.
In the case of a fracture of an edentulous patient, the mandibular dentures can be wired to the mandible with circummandibular wiring, and the maxillary denture can be secured to the maxilla using wiring techniques or bone screws to hold the denture in place. The maxillary and mandibular dentures can then be wired together, which produces a type of IMF. In many instances, the totally edentulous fracture patient undergoes open reduction and internal fixation with anatomic alignment (Fig. 24-20). After an appropriate period of healing (minimum of 4 to 6 weeks), new dentures can be fabricated.
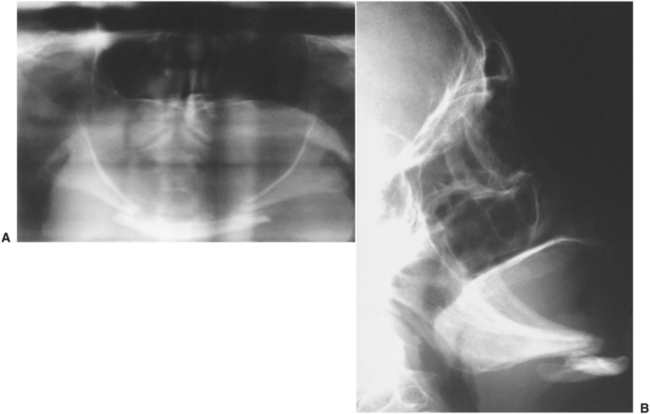
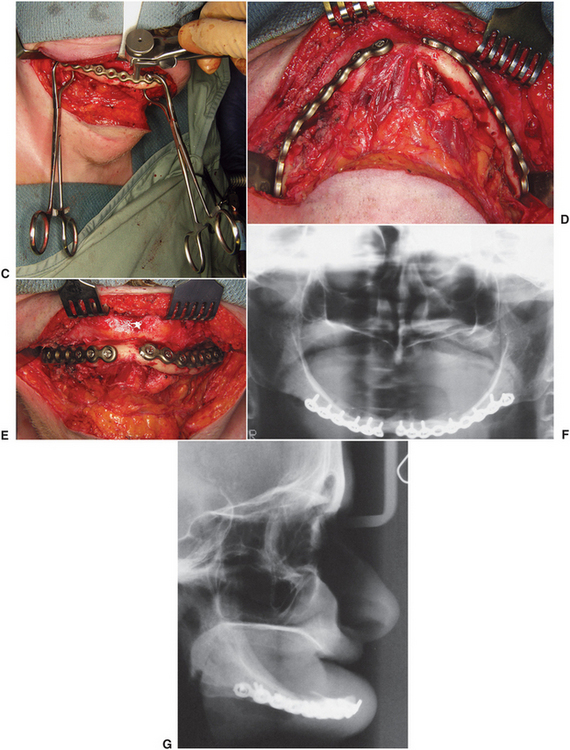
FIGURE 24-20 A, Panoramic radiograph demonstrating bilateral body fractures of an edentulous atrophic mandible. B, Lateral cephalogram showing inferior displacement of the anterior mandibular segment as a result of the suprahyoid muscle pull. C, Intraoperative appearance of the reduced right body fracture approached by a submandibular skin incision. Self-retaining bone clamps are used to hold the rigid fracture plate while a drill guide is used to ensure properly centered drilling within the plate holes. D, Intraoperative submental view of separate rigid plate fixation of the bilateral body fractures. E, Frontal view. F, Postoperative panoramic radiograph and, G, lateral cephalogram with restored anatomic alignment.
A splinting technique that can be used for dentate patients involves the use of a lingual or occlusal splint (Fig. 24-21). This technique is particularly useful in treatment of mandibular fractures in children in whom placement of arch bars and bone plates is difficult because of the configuration of the deciduous teeth, because of developing permanent teeth, and because patient understanding and cooperation is difficult to obtain. After a complete clinical and radiographic examination, all fractures and soft tissue injuries should be identified and categorized. Then, with input from the patient and the patient’s family, a treatment plan should be developed as to method and sequencing of surgery. Discussion regarding closed versus open reduction, any period of IMF, and anticipated morbidity should lead to a decision, and surgical consent should be obtained.
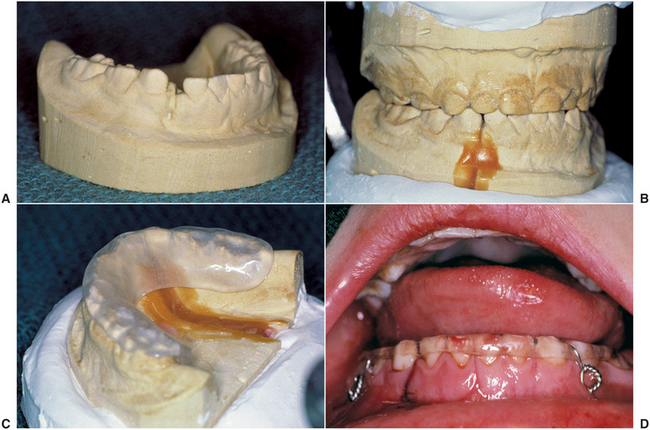
FIGURE 24-21 Five-year-old child with a right symphysis and bilateral intracapsular condyle fractures. A, Mandibular dental cast shows the degree of displacement of the right symphysis fracture. B, The lower cast is cut at the fracture site and reoriented into proper alignment by occluding with the maxillary cast. C, An occlusal/lingual acrylic splint is fabricated on the mandibular cast. D, Occlusal splint wired in place with circummandibular wires reducing and stabilizing the fractured mandible. Intermediate skeletal suspension wires were used to provide closed treatment (2 weeks) of the condylar fractures.
After completing a closed reduction of the mandible and placing the dental component or alveolar process into the proper relationship with the maxilla, the necessity for an open reduction (i.e., direct exposure and reduction of the fracture through a surgical incision) must be determined. If adequate bony reduction has occurred, IMF may provide adequate stabilization during the initial bony healing phase of approximately 6 weeks. Indications for open reduction include continued displacement of the bony segments or an unfavorable fracture, such as in an angle fracture (Fig. 24-13), in which the pull of the masseter and medial pterygoid muscles can cause distraction of the proximal segment of the mandible. With rigid fixation techniques, patients can be allowed to heal without undergoing IMF or at least a decreased time of IMF. This alone may be an important factor in the decision to perform an open reduction. In most instances, patients opt to undergo open reduction and internal fixation, which allows an earlier return to more normal function without IMF.
In some cases it is not be necessary to achieve an ideal anatomic reduction of the fracture area. This is especially true of the condylar fracture. In this fracture, minimal or moderate displacement of the condylar segment generally results in adequate postoperative function and occlusion (but only if a proper occlusal relationship was established during the period of healing of the fracture site). In these cases, IMF is used for a maximum of 2 to 3 weeks in adults and 10 to 14 days in children, after which there is a period of aggressive functional rehabilitation. Longer periods of IMF can lead to bony ankylosis or fibrosis and severe limited mouth opening. When there is significant anatomic displacement of the condylar segment, the outcome of treatment may be improved with open reduction and rigid fixation.11
When open reduction is performed, direct surgical access to the area of the fracture must be obtained. This access can be accomplished through several surgical approaches, depending on the area of the mandible fractured. Intraoral and extraoral approaches are possible. Generally, the symphysis and anterior mandible areas can be easily approached through an intraoral incision (Fig. 24-22), whereas posterior angle or ramus and condylar fractures are more easily visualized and treated through an extraoral approach (Fig. 24-23). In some cases, posterior body and angle fractures can be treated through a combination approach using an intraoral incision combined with insertion of a small trocar and cannula through the skin to facilitate fracture reduction and fixation (Fig. 24-24). In either case a surgical approach should avoid vital structures such as nerves, ducts, and blood vessels and should result in as little scarring as possible.
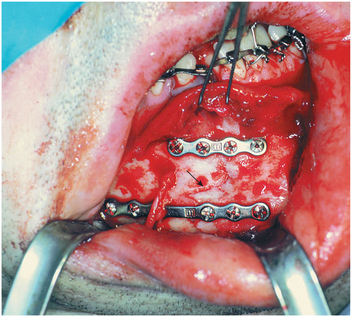
FIGURE 24-22 Intraoral exposure of reduced and fixated fracture in the right anterior body of the mandible (arrow shows fracture line). Preservation of mental nerve is demonstrated.
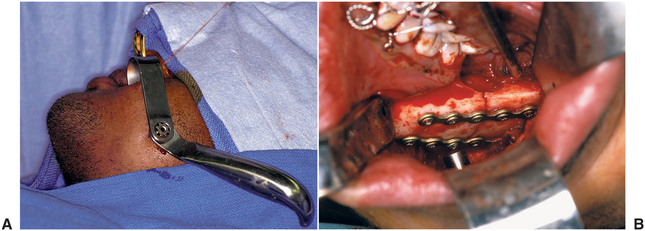
FIGURE 24-24 Use of intraoral incision combined with percutaneous cannula placement for access to mandibular angle region. A, View of left cheek with guarded cannula and handle in place. B, Intraoral view of the left angle fracture plates being percutaneously fixated with screws that are perpendicular to the lateral bone surface. Note that the impacted third molar that was in the line of fracture has been removed.
The traditional and still acceptable method of bone fixation after open reductions has been the placement of direct intraosseous wiring combined with a period of MMF ranging from 3 to 8 weeks. This method of fixation can be accomplished through a variety of wiring techniques (e.g., wire osteosynthesis) and is often sufficient to maintain the bony segments in the proper position during the time of healing (Fig. 24-25). If wire osteosynthesis is used for fixation and stabilization of the fracture site, continued immobilization with IMF (generally 4 to 6 weeks) is required until adequate healing has occurred in the area of the fracture.
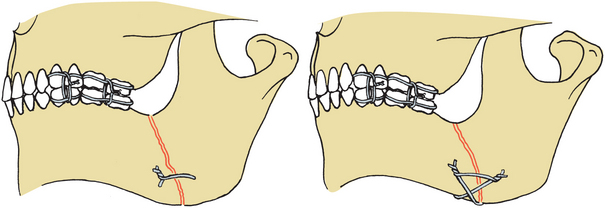
FIGURE 24-25 Surgical wiring of fracture sites for reduction and stabilization of mandible fractures (with wire osteosynthesis of fracture sites, patients must be maintained in intermaxillary fixation during the healing period).
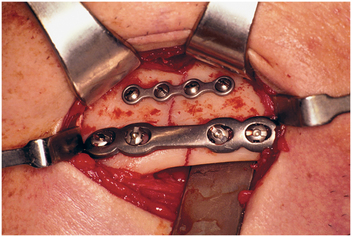
Currently, techniques for rigid internal fixation are widely used for treatment of fractures.12 These methods use bone plates, bone screws, or both to fix the fracture more rigidly and stabilize the bony segments during healing (Figs. 24-26 and 24-27). Even with rigid fixation, a proper occlusal relationship must be established before reduction and fixation of the bony segments. Advantages of rigid fixation techniques for treatment of mandibular fractures include decreased discomfort and inconvenience to the patient because IMF is eliminated or reduced, improved postoperative nutrition, improved postoperative hygiene, greater safety for patients with seizures, and frequently, better postoperative management of patients with multiple injuries.
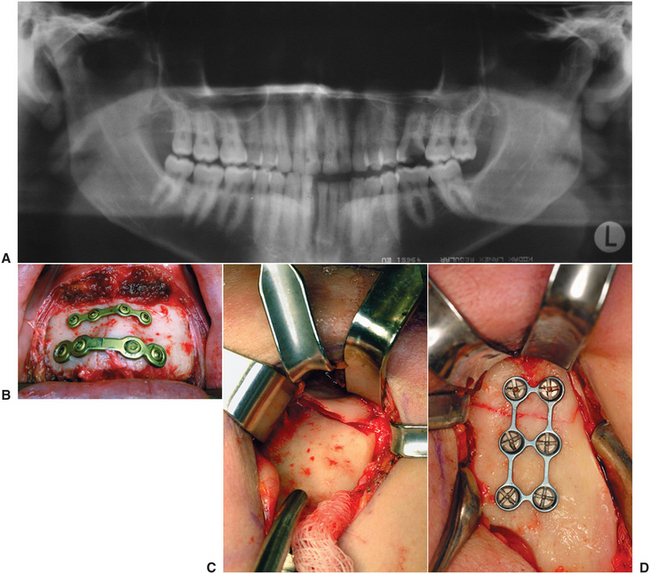
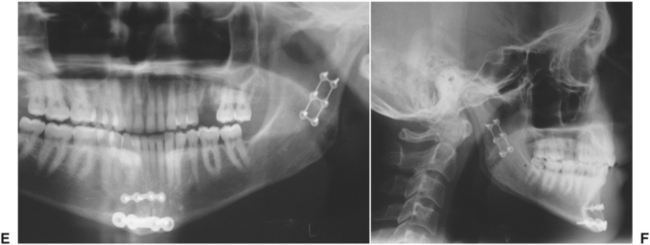
FIGURE 24-26 A, Preoperative panoramic radiograph with vertically displaced right symphysis and displaced and overlapped left condyle fractures. B, Clinical photograph of superior monocortical tension band plate and inferior bicortical plate fixating the right symphysis fracture. C, The left condyle fracture was approached extraorally and the displaced bony segments identified. D, The condylar fracture was reduced and fixated with a monocortical plate. E, Postoperative radiograph shows the fixated fractures and the removal of the nonsalvageable carious left maxillary first molar. F, Postoperative lateral cephalogram shows reestablishment of proper vertical dimensions and occlusion.
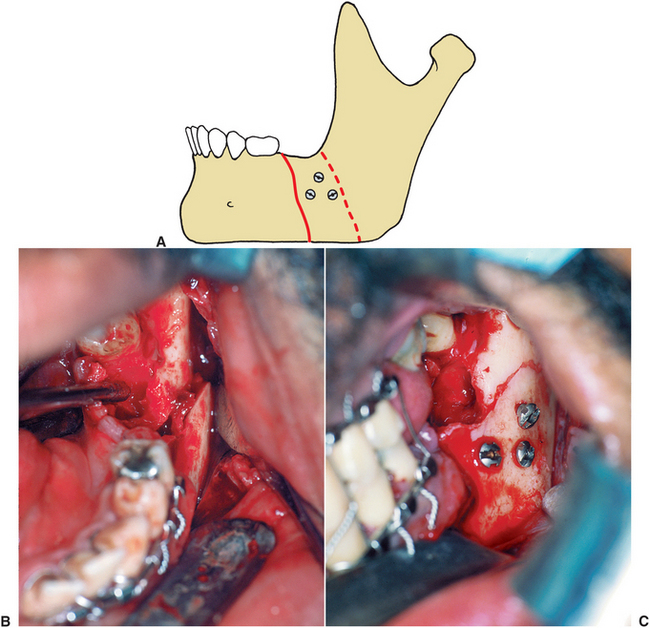
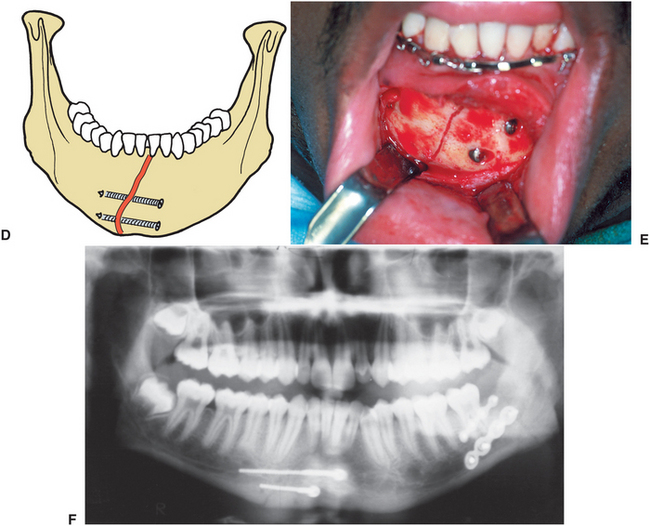
FIGURE 24-27 A, Oblique fracture of mandible stabilized with three lag screws. B, Clinical photograph of oblique fracture. C, Clinical photograph of fixation. D, Two screws placed tangentially across symphysis, stabilizing anterior mandible by engaging facial cortex on both sides of fracture and applying compression across fracture site with lag screws. E, Clinical photograph of screw fixation. F, Radiograph.
Midface Fractures
Treatment of fractures of the midface can be divided into those fractures that affect the occlusal relationship—such as Le Fort I, II, or III fractures—and those fractures that do not necessarily affect the occlusion, such as fractures of an isolated zygoma, zygomatic arch, or nasoorbital-ethmoid (NOE) complex.
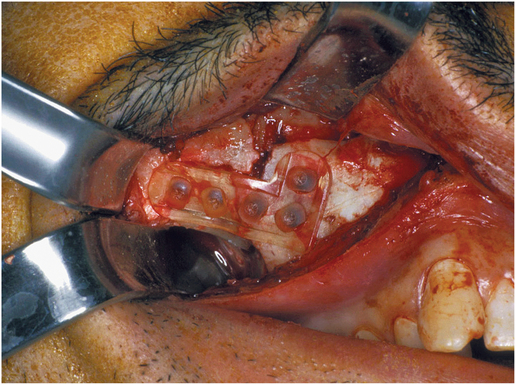
In zygoma fractures, isolated zygomatic arch fractures, and NOE fractures, treatment is primarily aimed at the restoration of normal ocular, nasal, and masticatory function and facial esthetics. In an isolated zygoma fracture (the most common midfacial injury), an open reduction is generally performed through some combination of intraoral, lateral eyebrow or infraorbital approaches. An instrument is used to elevate and place the zygoma into the proper position. If adequate stabilization is not possible by simple manual reduction, bone plating of the zygomaticomaxillary buttress, zygomaticofrontal area, and the inferior orbital rim area may be necessary (Fig. 24-28).
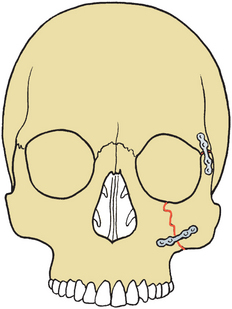
FIGURE 24-28 Plate stabilization of zygomatic complex fracture. Plates stabilize fractures at the zygomatic buttress and zygomaticofrontal suture area.
In a zygomatic arch fracture, an extraoral or an intraoral approach can be used to elevate the zygomatic arch and return it to its proper configuration. In addition to restoring adequate facial contour, this approach eliminates the impingement on the coronoid process of the mandible and the subsequent limitation of mandibular opening. Elevation and reduction of the zygomatic arch should be performed within several days of the injury. Longer delays make maintaining the arch in a stable supported configuration difficult, and it tends to collapse or drift to its injured position.
The goal of treatment for NOE fractures is to reproduce normal nasolacrimal and ocular function while repositioning the nasal bones and medial canthal ligaments into an appropriate position to ensure normal postoperative esthetics. In these situations, open reduction of the NOE area is usually necessary. Wide exposure to the supraorbital rim and nasal, medial canthal, and infraorbital rim areas can be achieved through a variety of surgical approaches. The most popular approach currently in use is the coronal flap, which allows exposure of the entire upper facial and nasoethmoidal complex through a single incision that can be easily hidden in the hairline (Fig. 24-29).13 Small bone plates and direct transnasal wiring appear to be most effective in stabilizing and maintaining bony segments in these types of injuries.
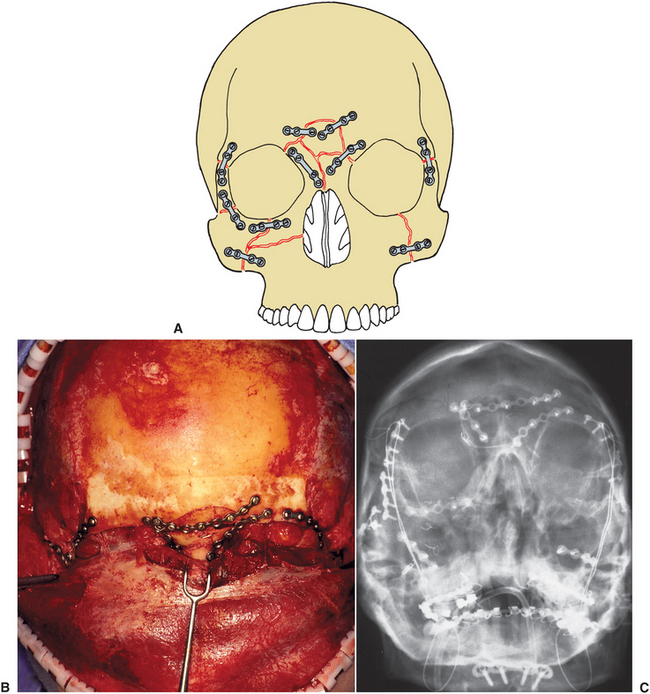
FIGURE 24-29 Plate stabilization of severe midface fracture. A, Diagrammatic representation. B, View of supraorbital area after stabilization of fragments with small bone plates. C, Postoperative Water’s radiograph.
In midfacial fractures involving a component of the occlusion, as in mandibular fractures, it is important to reestablish a proper occlusal relationship by placing the maxilla into the proper occlusion with the mandible. This step is accomplished by methods identical to the various types of IMF for mandibular fractures. However, as with mandibular fractures, reestablishing the occlusal relationship may not provide adequate reduction of the fractures in all areas. In addition to the need for anatomic reduction, additional stabilization of the fracture sites is often required.
When adequate bony reduction occurs after IMF but the fracture remains unstable, direct wiring, suspension wiring techniques, or bone plates may be used to stabilize the fracture. An example of such a case is a Le Fort I, II, or III midfacial fracture with an intact mandible. By placing the patient in IMF, any movement of the mandible tends to dislodge the midfacial bones. Direct wiring techniques (i.e., wire osteosynthesis) or bone plates (i.e., rigid fixation) attempt to fixate the individual fractures directly.
Suspension wiring is sometimes used in addition to direct wiring or bone plating. The purpose of suspension wiring is to provide stabilization of fractured bones by suspending them to a more stable bone superiorly.14 Suspension wiring techniques include those with wires attached to the piriform rim area, infraorbital rims, zygomatic arch, or frontal bone (Fig. 24-30). The suspension wires can be connected directly to the maxillary arch wire, or they can be connected with an intermediate wire to an interocclusal splint or to the mandible. These suspension wires prevent movement of the maxilla caused by the inferior pull of the mandible during attempted opening. The use of direct and suspension wire fixation does have significant limitations in many cases. The limited rigidity of wires may make it difficult to reconstruct and maintain the appropriate anatomic contours, particularly in concave and convex areas, such as orbital rims and the prominence of the zygoma. Wires may not provide adequate resistance to muscular forces during the entire healing period, eventually resulting in some fracture displacement. Rigid fixation using plating systems for the most part has eliminated the need for suspension wires.
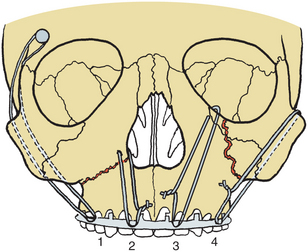
FIGURE 24-30 Suspension wiring techniques: 1, Frontal bone suspension; 2, piriform rim wiring; 3, circumzygomatic suspension; 4, circumzygomatic suspension.
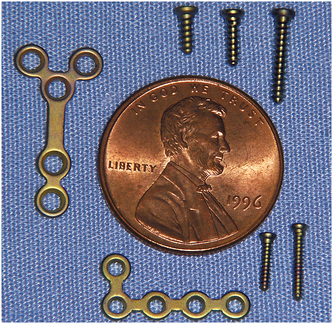
The development and improvement in miniature and micro bone plate systems has greatly enhanced the treatment of midfacial fractures. These titanium alloy plates range in thickness from 0.6 to 1.5 mm and are secured by screws with 0.7- to 2.0-mm external thread diameters (Fig. 24-31). Each of the advantages listed for rigid fixation of mandibular fractures applies to midface fractures. In addition to these advantages, small bone plates have greatly improved the ability to obtain proper bony contours at the time of surgery. When limited to the use of direct-wiring or suspension-wiring techniques, reestablishing curve configurations of bony anatomy is nearly impossible, particularly in the areas of severely comminuted small bone fragments. Severely comminuted unstable midface fractures can now routinely be treated by wide exposure of all fractured segments combined with the use of bone plates to reestablish the facial pillars, develop adequate contours, and stabilize as many facial bone fragments as possible (Fig. 24-32). These titanium bone plates and screws are biocompatible and do not require removal at a second surgery unless they become palpable, infected, or interfere with secondary reconstructive surgery (e.g., bone grafting or implants).
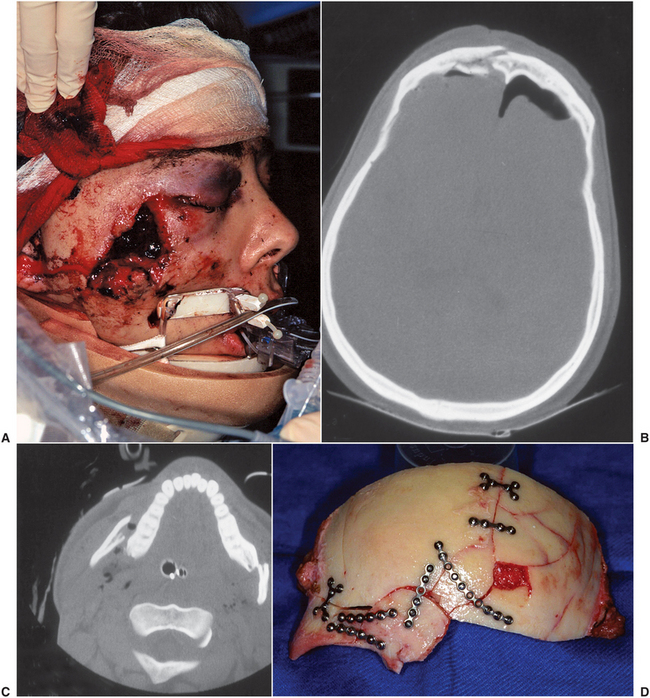
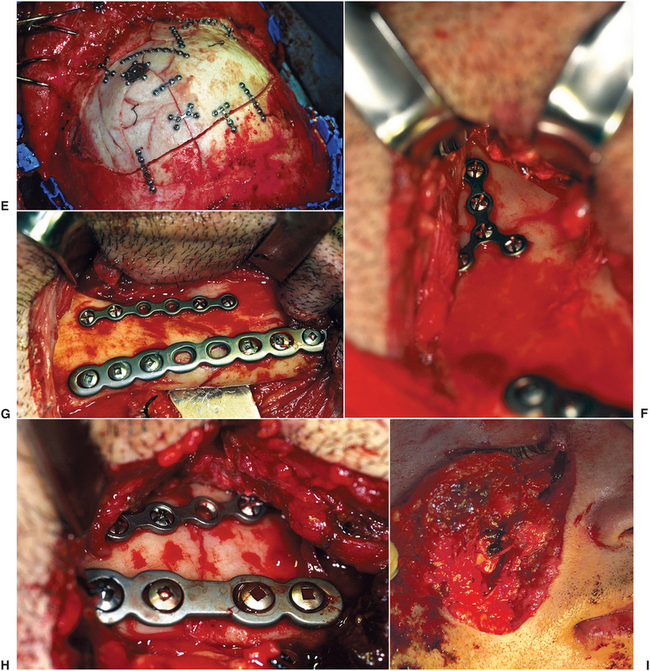
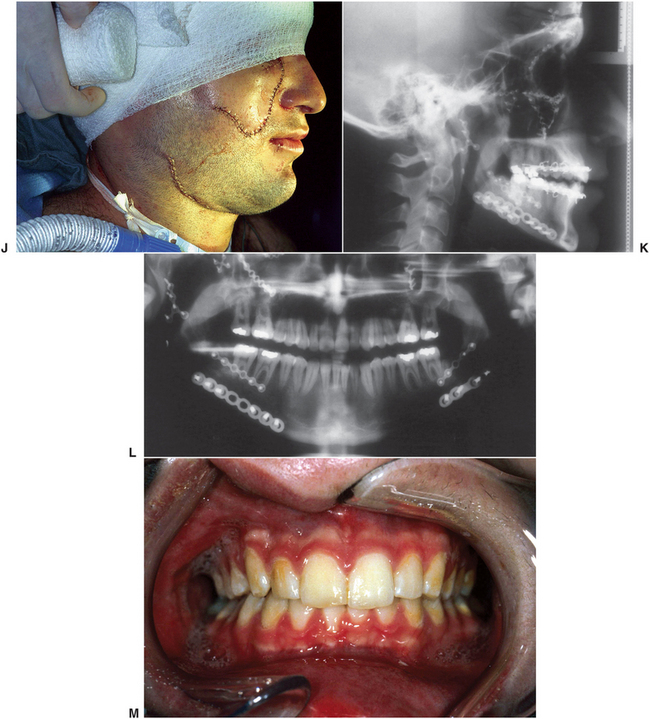
FIGURE 24-32 A, Patient (who sustained severe panfacial trauma from an industrial accident) in the operating department is shown in a cervical spine collar. B, Axial computed tomography scan reveals anterior skull fractures with intracranial air. C, Axial computed tomography scan with bilateral displaced mandible fractures. D, Operative view of skull vault plated while the neurosurgeon was repairing the dural tear. E, Cranial vault plated back in place. F, Right subcondylar fracture. G, Right body fractures plated through a large neck laceration. H, Left angle fracture. I, Revised wound of left cheek through which microplating of midfacial fractures was performed. J, Repaired right cheek and neck lacerations and pressure head dressing being applied. K, Postoperative lateral cephalogram. L, Panoramic radiograph. M, Occlusion 6 weeks after surgery (see Fig. 26-30 for postoperative facial views and scar revision).
Various polymers of polyglycolic acid and polylactic acid have been developed for resorbable plate and screw systems (Fig. 24-33).15,16 Resorbable plating systems may be particularly desirable in pediatric and skull trauma, where growth and CT scan reimaging are considerations. However, because of the current designs, mechanical limitations, need for tapping, and cost, these systems are not routinely used. Use of bone plates and screws has also facilitated the use of immediate bone grafting to replace comminuted or missing bone segments at the time of surgery and to improve stabilization of comminuted segments.
Lacerations
The general guidelines for management of facial lacerations are outlined in Chapter 23. Frequently, fractures of the facial bones are associated with severe facial lacerations. The principles of laceration repair remain the same regardless of how small or large the injury.
Cleansing of the laceration and examination of the area for disruption of any vital structures is important. Possible injuries include lacerations of Stensen’s duct, the facial nerve, or major vessels. In these cases, attempts mus0t be made to reanastomose the duct, identify and perform a primary repair of the severed nerve, or manage all associated bleeding (Fig. 24-34). Examination for these injuries before injection of local anesthesia or induction of general anesthesia is important because structural integrity and function (i.e., facial motion and salivary flow) may not be assessable after anesthesia.

FIGURE 24-34 A, A deep penetrating laceration over the area of the facial nerve and parotid duct. Exploration may be necessary to locate and repair these structures. B, Postoperatively, the patient had breakdown of a wound margin with a persistent salivary fistula due to undetected injury of the parotid duct.
The lacerations should be closed from the inside out, that is, from the oral mucosa to the muscle to the subcutaneous tissue and skin. All closures should be completed in layers to orient tissues properly and to eliminate any dead space within the wound to prevent hematoma formation. Easily identifiable landmarks, such as the vermilion border of the lip, ala of the nose, or areas of the laceration that can be easily identified and properly repositioned, should be sutured first (Fig. 24-35), after which the surgeon should close areas where wound margins are not so clearly reapproximated. All wounds should be cleansed periodically with hydrogen peroxide. Some surgeons advocate including the use of antibiotic ointment in wound care. However, use of dry occlusive dressings, such as Steri-Strip coverings can be equally effective. Sutures from facial wounds are generally removed in 5 to 7 days, depending on the location of the wound and the amount of tension necessary to provide adequate wound closure.
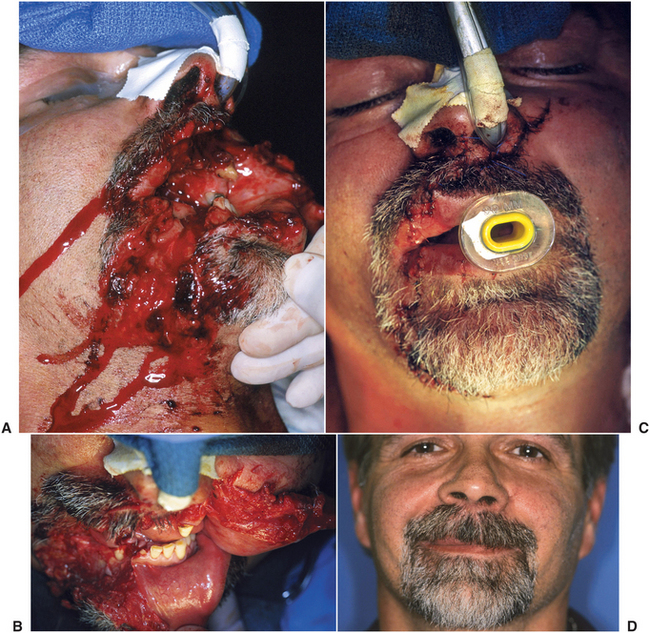
FIGURE 24-35 A, Chainsaw injury to the lips, jaws, and chin, resulting in loss of teeth and bone. B, View from above after hemostasis has been achieved and the wound has been débrided and trimmed. Note the nearly avulsed upper lip pedicled on the left side. C, View of repaired lacerations with patient nasally intubated and an oral airway in place. D, Three-month postoperative facial appearance.
REFERENCES
1. Batters Alvi, A, Doherty, T, Lewen, G. Facial fractures and concomitant injuries in trauma patients. Laryngoscope. 2003;113:102.
2. Verschueren, DS, Bell, RB, Gagheri, SC, et al. Management of laryngo-tracheal injuries associated with craniomaxillofacial trauma. J Oral Maxillofac Surg. 2006;64:203.
3. Gerlock, AJ, Sinn, DP, McBride, KL. Clinical and radiographic interpretation of facial fractures. Boston: Little, Brown, 1981.
4. Saigal, K, Winokur, RS, Finden, S, et al. Use of three-dimensional computerized tomography reconstruction in complex facial trauma. Facial Plast Surg. 2005;21:214.
5. Afzelius, L, Rosen, C. Facial fractures: a review of 368 cases. Int J Oral Surg. 1980;9:25.
6. Ellis, E, El-Attar, A, Moos, K. An analysis of 2067 cases of zygomatical orbital fractures. J Oral Maxillofac Surg. 1985;43:417.
7. Olson, RA, Fonseca, RJ, Zeitler, DL, et al. Fractures of the mandible: a review of 580 cases. J Oral Maxillofac Surg. 1982;40:23.
8. Bagheri, SC, Holmgren, E, Kademani, D, et al. Comparison of the severity of bilateral LeFort injuries in isolated midface trauma. J Oral Maxillofac Surg. 2005;63:1123.
9. Manson, PM, Hoopes, JE, Su, CT. Structural pillars of the facial skeleton: an approach to the management of Le Fort fractures. Plast Reconstr Surg. 1980;60:54.
10. Markowitz, BL, Manson, PM. Panfacial fracture: organization of treatment. Clin Plast Surg. 1989;16:105.
11. Villarreal, PM, Monie, R, Junquera, LM, et al. Mandibular condyle fractures: determinants of treatment and outcome. J Oral Maxillofac Surg. 2004;62:155.
12. Ochs, MW, Tucker, MR. Current concepts in management of facial trauma. J Oral Maxillofac Surg. 1993;51:42.
13. Van Sickels, JE, White, RP, Jr. Rigid fixation for maxillofacial surgery. In: Tucker MR, White RP, Jr., Terry BC, et al, eds. Rigid fixation for maxillofacial surgery. Philadelphia: JB Lippincott, 1991.
14. Bowerman, JE, Fractures of the middle third of the facial skeleton. Rowe, NL, Williams, JI, eds. Maxillofacial injuries, vol 1. New York: Churchill Livingstone, 1984.
15. Eppley, BL, Prevel, CD. Nonmetallic fixation in traumatic midfacial fractures. J Craniofac Surg. 1997;8:103.
16. Bell, RB, Kindsfater, CS. The use of biodegradable plates and screws to stabilize facial fractures. J Oral Maxillofac Surg. 2005;63:1576.