Local anaesthetics
Local anaesthetics are drugs that reversibly block the transmission of pain stimuli locally at their site of administration.
Pharmacology
Local anaesthetics produce reversible blockade of nerve conduction and prevent impulse transmission in nerve fibres by inhibiting depolarisation of the cell. At rest, the neuronal cell membrane has only limited permeability to Na+ but about 50–70 times greater permeability to K+ because of the greater number of channels open for passive transport of K+ out of the cell. The maintenance of a negative resting membrane electrical potential is largely determined by the K+ gradient across the cell membrane, with a smaller contribution from the active Na+/K+-ATPase pump, which pumps out three Na+ ions for every two K+ ions it transports in. Conduction of a nerve action potential results from opening of voltage-dependent Na+ channels, and rapid influx of Na+ to depolarise the cell (see Fig. 18.2, below). Na+ channels cycle between three states:
 resting, when the channel is closed but able to open in response to a change in transmembrane potential,
resting, when the channel is closed but able to open in response to a change in transmembrane potential,
 open, when the channel opens in response to an action potential and allows the rapid influx of Na+ ions through to the cytoplasm,
open, when the channel opens in response to an action potential and allows the rapid influx of Na+ ions through to the cytoplasm,
 inactivated due to a very rapid change in conformation at the cytoplasmic end of the channel that occurs very soon after the action potential has passed. During this stage the channel is resistant to depolarising influences, but sensitivity returns when the membrane potential is restored to the resting level.
inactivated due to a very rapid change in conformation at the cytoplasmic end of the channel that occurs very soon after the action potential has passed. During this stage the channel is resistant to depolarising influences, but sensitivity returns when the membrane potential is restored to the resting level.
There is considerable redundancy in the membrane Na+ channels; as a consequence, nerve conduction can continue even when 90% of the channels are blocked.
Local anaesthetics block the voltage-dependent Na+ channels that depolarise the cell. They bind to the Na+ channel at a site on the inner surface of the membrane and hold them in an inactivated state. Local anaesthetics progressively interrupt Na+ channel-mediated depolarisation until conduction fails. The probability that propagation of a nerve impulse will fail at a particular segment of the nerve is related to:
In general, nerve transmission is blocked in smaller-diameter fibres before that in larger fibres (Table 18.1). The myelinated Aδ and small non-myelinated C fibres that transmit pain (nociceptive fibres) are blocked before larger sensory and motor fibres. Therefore, pain pathways are most rapidly and intensely blocked by local anaesthetics (Table 18.1), and also show the longest duration of local anaesthetic effect. In myelinated nerves the drug penetrates at the nodes of Ranvier and must block at least three consecutive nodes to produce conduction block. Unmyelinated nerves must be blocked over a sufficient length and around the full circumference of the nerve.
Table 18.1
Nerve fibres and their responsiveness to local anaesthetics
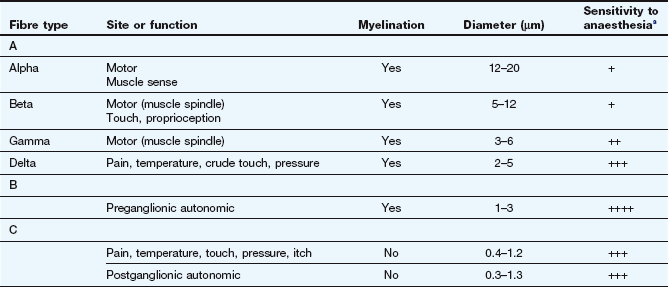
aIncreasing number of + indicates increasing sensitivity to local anaesthesia.
Structural requirements of local anaesthetics
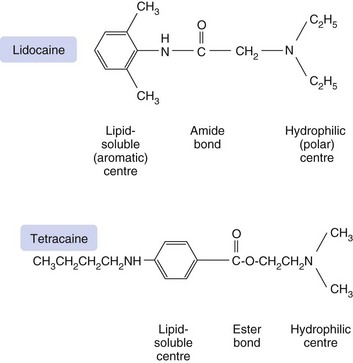
The action of local anaesthetics results mainly from binding of the ionised form of the anaesthetic to a site on the inside (cytoplasmic opening) of the Na+ channel. Membrane penetration, however, is better in the non-ionised (lipid-soluble) form. The structural requirements for local anaesthetic activity appear to involve a minimum of a lipid-soluble hydrophobic aromatic ring structure connected to a hydrophilic amine group by a short ester or amide intermediate linkage (Fig. 18.1). Clinically used potent local anaesthetics are all secondary or tertiary amines with an intermediate amide or ester bond. The length of the intermediate bonding chain is critical to local anaesthetic activity and is optimal between three and seven carbon atoms or equivalent atoms. The lipophilic aromatic group enables the molecule to cross the nerve membrane, and the potency of the drug is directly related to its lipid solubility.
Specific intraneuronal binding
Local anaesthetics bind to a receptor protein within the cytoplasmic opening of the Na+ channel, and compounds with high protein-binding affinity stay at the site of action for longer and have a long duration of action. Thus, procaine, which has a low binding affinity (6% protein bound), has a very short duration of action, whereas bupivacaine has a high binding affinity (95% protein bound) and a long duration of action.
The pKa of the drug determines the extent of ionisation at physiological pH and the speed of onset of the conduction block. All local anaesthetics are weak bases and will be relatively more ionised at a pH below the pKa (which for most local anaesthetics is between 7.7 and 9.1). Because the water solubility of a local anaesthetic is greatest in the ionised form, injectable preparations are formulated as the hydrochloride salts with a pH of 5.0–6.0. However, the base (non-ionised) form is more lipid-soluble and more readily penetrates lipid membranes; therefore, after injection, the drug solution (pH 5.0–6.0) must be buffered in the tissues to physiological pH (7.4) before a significant amount of non-ionised local anaesthetic is available to penetrate the nerve and reach its site of action. A drug with a high pKa will be more ionised at physiological pH, and the speed of onset of anaesthesia will be slower. Alkalinisation of the injected solution by adding bicarbonate will increase the proportion of the drug in its non-ionised lipid-soluble form and therefore increase the rate of absorption of the anaesthetic into the nerve which will accelerate the onset of action.
In contrast, it is the ionised form of the drug that binds to the receptor within the cytoplasmic opening of the Na+ channel. Drugs with a higher pKa will re-ionise to a greater extent within the cell (pH 7.4) and produce more effective blockade. The majority of the local anaesthetic molecules therefore pass across the cell membrane in their non-ionised form and enter the cytosol where they become ionised and available to bind to the protein receptor via the cytoplasm. The binding site is most accessible when the channel is in its open (activated) state (Fig. 18.2). For this reason the effectiveness of most local anaesthetics is dependent on the frequency of firing of the neuron (use-dependency), and a faster onset of local anaesthesia occurs in rapidly firing neurons. Once the local anaesthetic has bound to the channel, the influx of Na+ is blocked and the channel remains in the inactivated state and resistant to further depolarisation. The local anaesthetic does not dissociate from the channel when it is inactivated as it has a high affinity for the channel in this state. The local anaesthetic leaves the binding site when the membrane potential returns to its resting level, and the channel is in the resting state. This is further facilitated when the cytoplasmic concentration of the drug decreases as it diffuses away from the site of administration.
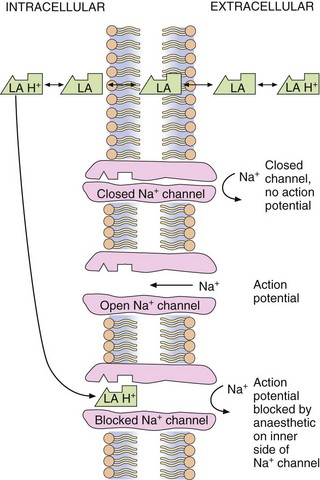
Fig. 18.2 Site and mechanism of action of local anaesthetics.
Local anaesthetics are weak bases and exist in an equilibrium between ionised (LA + H+) and non-ionised (LA) forms. The non-ionised form is lipid-soluble and crosses the axonal membrane, allowing the ionised form to bind to the intracellular end of the receptor. Some non-ionised anaesthetic may reach the ion channel by diffusion within the cell membrane, become ionised within the Na+ channel and then bind to the receptor site.
Local anaesthetics bind to K+ channels, but very weakly compared to Na+ channels. This binding may contribute to toxic effects of local anaesthetics in other organs such as the heart.
Local anaesthetics also bind to other ion channels and cell receptors, including presynaptic Ca2+ channels, tachykinin type 1 receptors, glutamate, bradykinin B2 and acetylcholine receptors. These actions may be involved in reducing nociceptive neurotransmission and in the production of spinal anaesthesia.
Pharmacokinetics
As seen above, the speed of onset of local anaesthetic action is largely determined by the physicochemical properties of the drug molecule. The duration of action of local anaesthetics is dependent on the degree of receptor binding (see above) and on their rate of removal from the site of administration, rather than their systemic elimination by metabolism. Most local anaesthetics cause vasodilation at the site of injection, which will enhance their removal. In contrast, cocaine, which blocks noradrenaline reuptake by noradrenergic neurons (Ch. 4), produces intense vasoconstriction. Because of the risk to local tissue integrity associated with the vasoconstriction, cocaine is never given by injection and its medical use is restricted to topical anaesthesia in otolaryngology. The duration of action of any local anaesthetic can be extended considerably by co-administration with a vasoconstrictor such as an α1-adrenoceptor agonist, for example adrenaline (epinephrine). However, the pH of the solution must be 2.0–3.0 to prevent decomposition of the adrenaline (epinephrine). Local anaesthetic preparations with other vasoconstrictors such as phenylephrine or felypressin are also available.
Once the local anaesthetic has diffused away from the site of administration it enters the general circulation and undergoes elimination from the body. Most local anaesthetics have an intermediate amide bond, and are eliminated at least in part by hepatic hydrolysis of the amide bond. The half-life of amide local anaesthetics within the circulation is generally between 1 and 3 h. In contrast, the plasma half-lives of the ester drugs procaine and tetracaine are 3 min or less, since ester bonds are very rapidly hydrolysed by plasma esterases.
Unwanted effects
These occur at the site of administration and include irritation and inflammation. Local ischaemia can occur if local anaesthetics are co-administered with a vasoconstrictor; therefore this should be avoided in the extremities such as the digits. Tissue damage with necrosis can follow inappropriate administration (e.g. accidental intra-arterial administration or spinal administration of an epidural dose).
Systemic effects
These are related to the anaesthetic action, and usually result from excessive plasma concentrations that affect other excitable membranes such as the heart (see antiarrhythmic action of lidocaine; Ch. 8). After regional anaesthesia, the maximum plasma drug concentration occurs within 30 min, requiring close observation for toxic effects during this period. Toxic plasma concentrations of drug are more likely after accidental intravenous injection, or rapid absorption from highly vascular sites or from inflamed tissues. Intravenous lipid emulsions are a recommended adjunct to resuscitation when treating severe toxicity with circulatory arrest. Lipid emulsion probably works by partitioning the drug away from receptors within tissues.
 Central nervous system (CNS) effects: high concentrations of local anaesthetics can produce light-headedness, paraesthesia, dizziness, nausea and vomiting progressing to sedation and loss of consciousness. Severe reactions can be accompanied by convulsions and respiratory arrest. CNS toxicity tends to occur before cardiovascular toxicity, but this is not invariable.
Central nervous system (CNS) effects: high concentrations of local anaesthetics can produce light-headedness, paraesthesia, dizziness, nausea and vomiting progressing to sedation and loss of consciousness. Severe reactions can be accompanied by convulsions and respiratory arrest. CNS toxicity tends to occur before cardiovascular toxicity, but this is not invariable.
 Cardiovascular effects: high plasma concentrations can cause tachycardia and arrhythmias. Serious arrhythmia is a particular problem with bupivacaine and is caused by its avid tissue binding in the heart. As a result of its high lipid solubility and high protein binding, it has a fast-in, slow-out kinetic pattern at the Na+ channel. Bupivacaine (particularly the R(+)-isomer) blocks the normal cardiac conducting system and predisposes to ventricular re-entrant pathways and intractable ventricular arrhythmias, possibly a consequence of binding to ATP-sensitive K+ channels (see Ch. 8). More profound toxicity can lead to cardiovascular collapse from systemic vasodilation and a negative inotropic effect. Levobupivacaine and ropivacaine have about the same local anaesthetic potency but less potential to produce cardiac effects, having less effect on cardiac Na+ channels.
Cardiovascular effects: high plasma concentrations can cause tachycardia and arrhythmias. Serious arrhythmia is a particular problem with bupivacaine and is caused by its avid tissue binding in the heart. As a result of its high lipid solubility and high protein binding, it has a fast-in, slow-out kinetic pattern at the Na+ channel. Bupivacaine (particularly the R(+)-isomer) blocks the normal cardiac conducting system and predisposes to ventricular re-entrant pathways and intractable ventricular arrhythmias, possibly a consequence of binding to ATP-sensitive K+ channels (see Ch. 8). More profound toxicity can lead to cardiovascular collapse from systemic vasodilation and a negative inotropic effect. Levobupivacaine and ropivacaine have about the same local anaesthetic potency but less potential to produce cardiac effects, having less effect on cardiac Na+ channels.
 Allergy: true allergy is rare, but can occur with ester agents due to their metabolism to p-aminobenzoic acid (PABA). For this reason, amide bond local anaesthetics are more commonly used.
Allergy: true allergy is rare, but can occur with ester agents due to their metabolism to p-aminobenzoic acid (PABA). For this reason, amide bond local anaesthetics are more commonly used.
Techniques of administration
The extent of local anaesthesia depends largely on the technique of administration.
Surface administration
High concentrations (up to 10%) of drug in an oily vehicle can slowly penetrate the skin or mucous membranes to give a small localised area of anaesthesia. Lidocaine can be applied as a cream to an area before a minor skin procedure or venepuncture. Benzocaine is a relatively weak local anaesthetic that is included in some throat pastilles to produce anaesthesia of mucous membranes. Cocaine is restricted to topical use in otolaryngeal procedures, to produce vasoconstriction and reduce mucosal bleeding.
Infiltration anaesthesia
A localised injection of an aqueous solution of local anaesthetic, sometimes with a vasoconstrictor, produces a local field of anaesthesia. The anaesthetic effect produced is more efficient than surface anaesthesia, but requires a relatively large amount of drug. Smaller volumes can be used for field-block anaesthesia, involving subcutaneous injection close to nerves around the area to be anaesthetised. This technique is used extensively in dentistry.
Peripheral nerve block anaesthesia
Injection of an aqueous solution around a nerve trunk produces a field of anaesthesia distal to the site of injection. This can also be used for temporary sympathetic nerve block, such as the stellate ganglion, or for lumbar sympathectomy.
Epidural anaesthesia
Injection or slow infusion via a cannula of an aqueous solution adjacent to the spinal column, but outside the dura mater, produces anaesthesia both above and below the site of injection after 15–30 min. The extent of anaesthesia depends on the volume of drug administered and the rate of delivery. It is unaffected by the position of the person receiving the injection. Epidural anaesthesia is used extensively in childbirth for pain relief (using a local anaesthetic with an opioid) and for surgical anaesthesia, either alone or in combination with a general anaesthetic. The concentration of drug used is the same as that for spinal anaesthesia, but the volume (10–20 mL), and therefore the dose, is greater. For this reason, systemic unwanted effects are more frequent than with spinal anaesthesia. Sympathetic fibres are particularly sensitive to local anaesthetics (Table 18.1); this can result in hypotension that can be particularly exaggerated during pregnancy (probably related to the concurrent effects of high progesterone concentrations). Backache is a frequent postoperative complication with both epidural and spinal anaesthesia.
Spinal anaesthesia
This involves injection of an aqueous solution (1.5–2.5 mL) of local anaesthetic alone (often bupivacaine) or with an opioid into the lumbar subarachnoid space, usually between the third and fourth lumbar vertebrae. The spread of anaesthetic within the subarachnoid space depends on the density of the solution (a solution in 10% glucose is more dense than cerebrospinal fluid) and the posture of the person during the first 10–15 min while the solution flows up or down the subarachnoid space. Anaesthesia is produced after about 5 min and can be used for surgical procedures below the umbilicus lasting for up to 2 h. Spinal and epidural anaesthesia can be used together.
True/false questions
1. The block produced by local anaesthetics is more rapid and complete when the nerve is actively firing.
2. Local anaesthetics have no systemic unwanted effects.
3. Local anaesthetics block smaller myelinated axons more effectively than larger myelinated axons.
4. The α1-adrenoceptor antagonist prazosin is added to local anaesthetics to extend their duration of activity.
5. Local anaesthetics in their non-ionised form penetrate the axon more readily than in their ionised form.
One-best-answer (OBA) question
Which of the following is the most accurate statement about local anaesthetics?
A Raising the pH of a local anaesthetic solution will increase its speed of onset.
B Liver metabolism is the primary mechanism in terminating local anaesthetic action.
C The effectiveness of a local anaesthetic is not altered by local tissue pH.
D Direct effects on blood vessel diameter of most commonly used local anaesthetics prolong their duration of action.
E Adrenaline (epinephrine) is given with a local anaesthetic injection in digits and appendages to increase the duration of anaesthesia.
Extended-matching-item question
Choose the most appropriate drug A–F for each situation 1–4 below.
1. A child needed a minor surgical procedure on her nasopharynx and you chose to use a single agent that could be administered topically to reduce mucous membrane bleeding.
2. An agent that would extend the duration and potency of a local anaesthetic.
3. An agent that could be applied topically to produce anaesthesia of the conjunctiva which would not cause vasoconstriction.
4. An agent that could be administered intravenously in the treatment of ventricular arrhythmias.
1. True. This is because most local anaesthetics gain better access to binding sites in Na+ channels that are in the open state.
2. False. If absorbed, systemic high doses of local anaesthetics can produce cardiovascular collapse and CNS depression.
3. True. For example Aδ axons (2–5 µm diameter) are blocked more readily than motor fibres (12–20 µm diameter).
4. False. Prazosin is a vasodilator and would increase removal of the local anaesthetic from its injection site; a vasoconstrictor like adrenaline (epinephrine) is necessary.
5. True. The non-ionised form is lipophilic and better able to cross the axon membrane.
6. True. Ropivacaine is a long-acting local anaesthetic (2–4 h) similar to bupivacaine but is less arrhythmogenic.
OBA answer
A Most local anaesthetics are weak bases (pKa 7–9). Raising the pH will increase the amount of the non-ionised form and therefore enhance lipid solubility and membrane penetration.
B Local anaesthetic action is terminated mainly by uptake from tissues into the systemic circulation, not by hepatic metabolism.
C Altered local pH could change the ratio of the ionised and non-ionised forms of the local anaesthetic, affecting its potential to penetrate membranes (when non-ionised) and block Na+ channels (as the ionised form).
D With the exception of cocaine, local anaesthetics dilate blood vessels, hastening their removal from the site of injection and shortening their duration of action.
E Adrenaline (epinephrine) should not be given with a local anaesthetic for injection in digits and appendages because of the risk of ischaemic necrosis.
Extended-matching answers
1. Answer A. Cocaine can be administered topically and, unlike other local anaesthetics, inhibits the neuronal uptake of released noradrenaline, resulting in vasoconstriction.
2. Answer B. Adrenaline (epinephrine) causes vasoconstriction and the administered local anaesthetic resides at its site of injection for a longer period.
3. Answer D. Tetracaine is poorly absorbed and is used topically for conjunctival anaesthesia.
4. Answer E. Lidocaine can be given intravenously for the treatment of ventricular arrhythmias (Ch. 8).
Compendium: local anaesthetics
| Drug | Kinetics (half-life) | Comments |
| Articaine | Half-life 1 h when used to produce regional anaesthesia; hydrolysed by plasma esterases | Used in dentistry; concentrations in tooth alveolus are 100 times those in circulation |
| Benzocaine | Minimal oral absorption; hepatic metabolism (<1 min) | Used in throat lozenges |
| Bupivacaine | Hepatic metabolism (2–4 h) | Used for local infiltration anaesthesia, peripheral nerve block, epidural block and sympathetic block; slow onset (1–10 min) and long duration of action (3–9 h); more cardiotoxic than lidocaine |
| Cocaine | Hepatic metabolism (1–2 h) | Very rapid onset of action; used topically on mucosal surfaces (the only legal route!); profound CNS effects limit clinical usefulness |
| Levobupivacaine | Hepatic metabolism (1–3 h) | The S(−)-isomer of bupivacaine; similar to bupivacaine but less cardiotoxic |
| Lidocaine | Hepatic metabolism (1–2 h) | Used for local infiltration anaesthesia, intravenous regional anaesthesia, nerve blocks and dental anaesthesia; also used topically; for use in ventricular dysrhythmia, see Chapter 8 |
| Mepivacaine | Hepatic metabolism (2–3 h) | Used in dentistry |
| Prilocaine | Hepatic metabolism (1–2 h) | Used for local infiltration anaesthesia, intravenous anaesthesia, nerve blocks and dental anaesthesia; may cause methaemoglobinaemia (especially in infants) |
| Procaine | Very rapid ester hydrolysis at site of injection and in plasma (minutes) | Seldom used now; local infiltration anaesthesia |
| Ropivacaine | Hepatic metabolism (2–4 h) | Similar to bupivacaine but less cardiotoxic; used for epidural, major nerve block and field block |
| Tetracaine | Poorly absorbed; rapidly hydrolysed by pseudocholinesterase (3 min) | Mostly used topically |
Heavner, SE. Local anaesthetics. Curr Opin Anaesthesiol. 2007;20:336–342.
Scholz, A. Mechanisms of (local) anaesthetics on voltage-gated sodium and other ion channels. Br J Anaesth. 2002;89:52–61.
Tetzlaff, JE. The pharmacology of local anesthetics. Anesth Clin North Am. 2000;18:217–233.
Veering, BT. Complications and local anaesthetic toxicity in regional anaesthesia. Curr Opin Anaesthesiol. 2003;16:455–459.
Wiklund, RA, Rosenbaum, SH. Anesthesiology. Part II. N Engl J Med. 1997;337:1215–1219.
Yanagidate, F, Strichartz, GR. Local anesthetics. Handb Exp Pharmacol. 2007;177:95–127.