Disorders of the mouth
Disorders of the oral cavity (excluding salivary calculi)
The main oral disorders are dental caries (tooth decay) and its sequelae, inflammations of the gums and supporting bone (periodontal disease), tumours and premalignant conditions of mucosa (leukoplakia and squamous carcinoma) and disorders of the accessory salivary glands such as retention cysts. The main symptoms and signs are summarised in Box 48.1. Salivary gland disorders are covered in Chapter 47.
Dental caries
Pathophysiology and clinical features
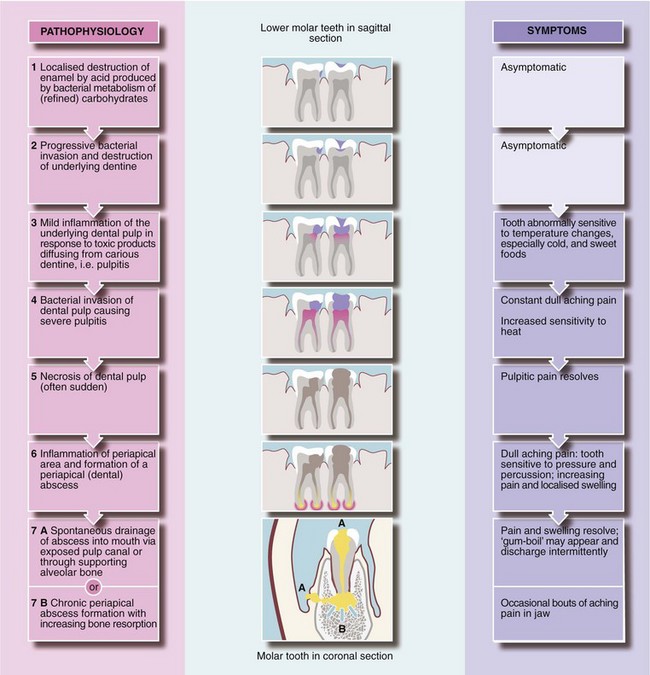
In developed countries, dental caries (dental decay) is a common bacterial disorder. First, the surface enamel of the tooth is breached by the demineralising action of lactic acid generated by commensal oral bacteria as a byproduct of carbohydrate metabolism, particularly of refined sugar. The most vulnerable sites for decay are just below the contact points of adjacent tooth crowns and the pits and fissures on the biting (occlusal) surface of molars and premolars. These sites are inaccessible to natural oral cleansing mechanisms and to tooth brushing.
Once enamel is breached, proteolytic bacteria enter the less calcified dentine beneath and cause progressive destruction. The enamel remains intact until the dentine is undermined and the enamel fractures. Thus, dental caries may be well advanced but invisible, even to a dental mirror and probe, and detectable only on X-ray. The decay process is asymptomatic until close enough to the dental pulp to cause inflammation and pain and, eventually, bacterial invasion and abscess formation. The pathological process and corresponding symptoms are outlined in Figure 48.1.
Once the pulp is exposed, inflammation and bacterial invasion usually destroy it, then spread to the periapical region forming an abscess. This causes painful oral and facial swelling, and if untreated, eventually drains into the mouth or occasionally onto the face. However, the initiating cause, the necrotic pulp, remains, so a chronic abscess flares up intermittently or continues with a persistent discharge.
The pain of dental caries is usually well localised and recognised as a ‘toothache’. Dental pain is sometimes poorly localised and causes non-specific facial pain. In the upper jaw, this may simulate sinusitis. Dental caries should always be considered before rarer diagnoses. Overall, a surprising amount of dental caries, even with periapical infection, is asymptomatic.
Management of dental caries
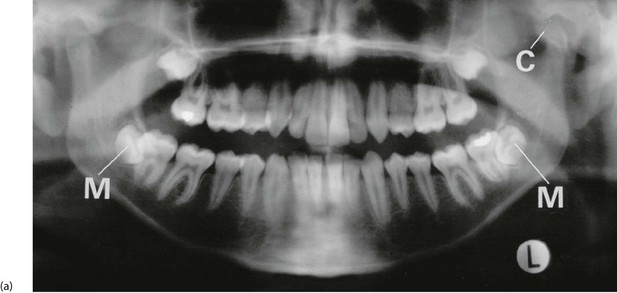
Provided the dental pulp has not been invaded by infection (i.e. become ‘exposed’), a dentist can usually drill out the carious enamel and dentine and restore it (Fig. 48.2) with synthetic resin, silver amalgam or gold, with a sedative insulating lining. Once exposed, the necrotic tissue must be removed by endodontic treatment, and the pulp cavity filled; this is ‘root filling’ (Fig. 48.2). In this way, the tooth can often be preserved.

Fig. 48.2 Dental restorations and root fillings
This oral pantomograph (OPG) film shows silver amalgam restorations for caries in posterior teeth (shown as white radiopacities) and synthetic resin restorations in front teeth (relative radiolucencies in the upper incisors). In addition, the upper left first molar and the lower right first molar (arrowed) have radiopaque root canal fillings, necessitated by dental caries invading the pulp
Management of dental abscesses
A periapical abscess is the most common manifestation of caries seen by general practitioners or casualty officers. Primary treatment, as for other abscesses, is drainage of pus. Extracting the offending tooth is most effective, but better to preserve the tooth by draining the abscess via the root canal then root filling it later. Patients with periapical abscesses should ideally be referred to a dentist.
Large acute abscesses ‘pointing’ within the mouth can be drained by incising at the site of greatest fluctuation. Oral penicillin should be prescribed for spreading infection. Antibiotics have no part in managing toothache unless there is swelling or other signs of an acute abscess. A dental abscess occasionally presents on the face but usually settles with extraction of the offending tooth. Dental abscesses are rarely complicated by osteomyelitis.
Tooth extraction and post-extraction problems
Medical practitioners are rarely required to extract teeth except in isolated places. Caries prevention with fluoride toothpaste and modern restorative and endodontic techniques have made extraction much less common. Patients, however, often attend GPs or accident departments after tooth extraction or surgical tooth removal with bleeding, pain or swelling.
Bleeding tooth socket after extraction
A small amount of blood mixed with saliva may look like severe haemorrhage. The extraction site should be inspected. A normal socket should be filled with firm clot with some ooze from the gingival margin. This is aggravated if the anxious patient disturbs the clot by rinsing or ‘exploring’ the socket with the tongue. Aspirin may also promote bleeding.
Oozing or minor bleeding is easily controlled by the patient biting on a small dry pack such as a folded gauze swab and maintaining pressure for 10–15 minutes. Persistent bleeding can usually be controlled by inserting sutures through the gingival margins across the socket (Fig. 48.3) then biting on a dry gauze pad. Suturing requires local anaesthesia infiltrated into the gingiva on each side of the socket. Absorbable polyglactin sutures are preferred as they do not leave irritating sharp ends and dissolve in 5–10 days. If bleeding continues after these simple measures, the patient should be investigated for a coagulation or platelet abnormality.
Pain after tooth extraction
Forceps extraction or surgical tooth removal may lead to pain soon afterwards. Removal of lower molar teeth may cause trismus (spasm of the muscles of mastication), making jaw movements painful and restricted. If there is no sign of infection, treatment is with analgesia, not antibiotics. Pain appearing several days after extraction is usually due to a superficial osteitis of exposed socket bone caused by failure to fill with organised clot. This condition, known as a dry socket, is intensely painful and requires dental treatment. Antibiotic therapy is not helpful.
Swelling after tooth extraction
Soft tissue swelling is uncommon after extraction, with the exception of surgically removed teeth, especially lower third molars (‘wisdom teeth’). Extraction of these often causes swelling around the angle of the mandible, with trismus and pain. This represents a normal inflammatory response plus interstitial haemorrhage rather than infection. The swelling subsides within a week or so and does not warrant antibiotic therapy.
Inflammation of the periodontal tissues
Teeth are embedded in bony alveolar ridges in both jaws. A thin layer of cementum (a bone-like material) on the root connects to the socket bone by a tough periodontal membrane or ligament. Oral mucosa (gingiva or gums) is bound to the alveolar bone and normally forms a tight cuff around the tooth neck, protecting alveolar bone from bacteria and trauma. The gingival crevice extends down to the cemento-enamel junction where the tough stratified oral epithelium becomes a thin vulnerable layer.
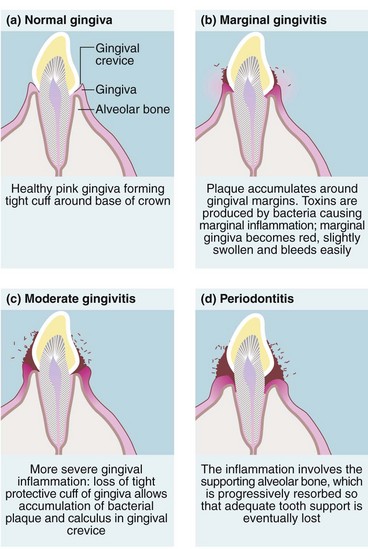
If oral hygiene is inadequate, commensal bacteria colonise the gingival margin and form a white gelatinous plaque (Fig. 48.4). If allowed to persist, plaque becomes adherent to the tooth and becomes mineralised. This is known as calculus, and cannot be removed by tooth brushing. Bacterial toxins then cause gingival inflammation or marginal gingivitis. This appears as swelling and redness of the gums and bleeding during tooth brushing.
Figure 48.5 shows gingivitis causes eversion of the gingival margin. This encourages more plaque and calculus to form and results in greater gum trauma from food, both leading to more inflammation. If untreated, inflammation extends to deeper tissues causing progressive resorption of alveolar bone and destruction of periodontal membrane, known as periodontitis. By this stage, the gingiva is thickened and inflamed with a purulent discharge. This explains the old term ‘pyorrhoea’ or flowing of pus. Despite this, the patient is remarkably pain free, although halitosis is obvious.
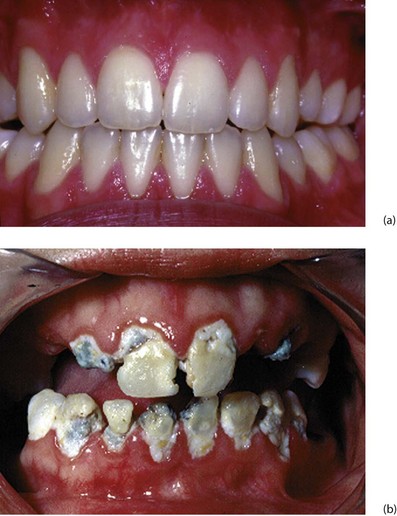
Fig. 48.5 Gingivitis and periodontitis
(a) Normal healthy gingivae. (b) Chronic gingivitis showing accumulated plaque and calculus around the gingival margins. At this stage, no alveolar bone has been destroyed and the inflammatory process is potentially reversible. Many of these teeth had to be extracted, however, because of rampant caries
As periodontal inflammation progresses, more alveolar bone is destroyed and gums recede. The root surface becomes exposed to view, giving rise to the expression ‘long in the tooth’. Teeth gradually become more mobile until they fall out or can be extracted with the fingers! Periodontal disease is an insidious process commencing in early adulthood. It was once thought to be inevitable with advancing age, but is almost entirely preventable. In adults, periodontitis (not dental decay, as is commonly supposed) is responsible for most lost teeth. Inflammatory destruction of alveolar bone makes it difficult to construct satisfactory dentures for many of these patients, due to the lack of a retaining alveolar ridge.
Sometimes an acute periodontal abscess may complicate periodontitis.
Management of gingivitis and periodontitis: Gingivitis and periodontitis is preventable by thorough and regular tooth brushing and use of dental floss, plus periodic dental scaling to remove inaccessible plaque and calculus. Initial scaling and careful oral hygiene instruction and supervision cures gingivitis, which is reversible. During the early stages of improved oral hygiene, bleeding increases through brushing inflamed tissues but soon subsides unless further periodontal treatment is needed.
Once established, periodontitis requires meticulous oral hygiene after thorough cleaning of plaque and calculus. Lost bone is never replaced, and the gingival contour remains abnormal, making effective oral hygiene difficult. Surgical recontouring of the gingiva and underlying bone (gingivoplasty) may be appropriate. Antibiotics play no part in treating chronic gingivitis or periodontitis. Antibiotics are useful for acute gingival conditions such as pericoronitis and Vincent's infection (acute ulcerative gingivitis).
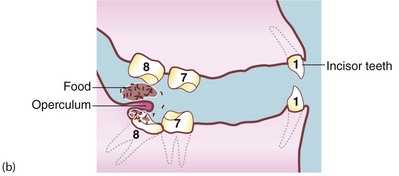
Pericoronitis
This occurs when a lower third molar (wisdom tooth) is impacted against the second molar or the ramus of the mandible so that its eruption is prevented (see Fig. 48.6). If a flap (operculum) of gingiva partly overlies the impacted tooth, this creates a space around the buried tooth crown (Fig. 48.6b). Food and bacterial plaque collect and cause acute infection, which may extend outwards, even into the parapharyngeal area.
The patient complains of severe, poorly localised pain near the mandibular angle. Pain is aggravated by chewing because the opposing tooth bites on the swollen gingival flap. On examination, the pericoronal tissues of the affected tooth are red and swollen with a purulent discharge from beneath the flap. Oral examination may be difficult because of trismus. Externally, the submandibular and upper cervical lymph nodes are enlarged and tender.
Management of pericoronitis: Pericoronitis is cellulitis with incipient abscess formation caused by mixed organisms usually sensitive to penicillin or metronidazole. It is treated by irrigating beneath the flap with hydrogen peroxide and mouth washes several times daily with warm salty water. Rapid relief is obtained by removing the upper wisdom tooth if it impinges on the flap. Oral phenoxymethylpenicillin (penicillin V) and metronidazole are given if the patient is systemically unwell. If attacks are recurrent, the lower wisdom tooth may be removed surgically.
Acute ulcerative gingivitis (vincent's infection)
This is an acute inflammatory condition with necrotising ulceration of the gingival margin. It is caused by a mixture of Gram-negative organisms which are normal oral commensals. The most prominent are Fusobacterium fusiformis, Borrelia vincentii and Bacteroides melaninogenicus. Acute ulcerative gingivitis most commonly occurs in young adults who ‘burn the candle at both ends’ and become run down. Poor oral hygiene, pericoronitis and smoking may contribute. Acute ulcerative gingivitis is now uncommon, but was widespread in the First World War when it gained the name ‘trench mouth’.
There is an abrupt onset of gingival pain and bleeding, accompanied by a foul, often metallic taste and marked halitosis. Cervical nodes are enlarged and tender, and there may be fever, malaise and anorexia. Oral examination reveals characteristic ragged ulceration of the gingiva, especially between the teeth. In severe cases, the pharyngeal mucosa becomes inflamed and ulcerated (Vincent's angina). Acute ulcerative gingivitis is easily distinguished from herpetic gingivo-stomatitis, as the former is confined to the gingival margin, whereas herpetic ulcers are scattered all over the oral mucosa.
Management of acute ulcerative gingivitis: Vincent's infection rapidly responds to metronidazole tablets (200 mg t.d.s.), usually with full recovery of gingival morphology; penicillin is also effective. Tooth brushing is painful during an attack and the mouth should be frequently rinsed with warm water or weak hydrogen peroxide to keep it clean. Afterwards, careful attention to oral hygiene usually prevents recurrence.
Tumours of the oral mucosa
The oral cavity and tongue is invested by stratified squamous epithelium. Oral squamous cell carcinoma (SCC) accounts for about 3% of all malignancies, and is the commonest cancer on the Asian subcontinent. Like their skin counterparts, these usually occur in older people, though this trend is changing as a result of human papillomavirus-induced SCC. Men are affected twice as often as women, but in HPV cancers the ratio is more even.
Tobacco products are the more usual cause, with pipe and cigar smokers and tobacco chewers at greatest risk in the West. The tongue and lower lip are the common sites, each accounting for about 25%. Chronic irritation by ill-fitting dentures, jagged tooth restorations or alcohol abuse may contribute to the aetiology.
In India, Sri Lanka, Papua New Guinea and other countries, the habit of chewing paan, a stimulant package of betel leaf, areka nut, cured tobacco and slaked lime, causes a very high incidence of buccal carcinoma, and submucous fibrosis which results in trismus and is itself pre-malignant.
Leukoplakia is a premalignant dysplasia found in 50% of patients with oral carcinoma.
Clinical features of oral cancer
Oral cancer usually presents as a slowly enlarging chronic indurated ulcer which fails to heal (Fig. 48.7b and c). An early lesion may present as a mucosal swelling. Lesions are usually painless unless secondarily infected, although advanced lesions may cause pain as they invade deeply. Carcinoma of the tongue, for example, may cause pain referred to the ear or pharynx via the lingual nerve or chorda tympani.

Fig. 48.7 Premalignant and malignant conditions of the mouth
(a) Leukoplakia under tongue. (b) Ulcerating squamous cell carcinoma (SCC) of the cheek. (c) Ulcerating SCC of the tongue. (d) Squamous cell carcinoma of the lip. This man of 60 had smoked a pipe most of his life. He tended to keep the pipe constantly in his mouth while he worked. He presented with a non-healing ulcer of the lip, proven to be a well-differentiated SCC on biopsy. A wedge resection of the lip was performed and produced a cure
Oral SCC invades locally and usually metastasises initially to submandibular and upper cervical lymph nodes. Even small tumours can cause metastases. Spreading tumours of the posterior floor of mouth and tongue interfere with speech, mastication and swallowing and are particularly distressing symptoms.
Management of oral cancer
A chronic oral ulcer which fails to heal after removing aggravating factors (such as ill-fitting dentures) should undergo urgent incision biopsy to exclude cancer.
Oral cancers are excised with at least a 1 cm margin of normal tissue. This may not be possible anatomically or cosmetically and often necessitates major reconstructive surgery. Involved lymph nodes are removed by neck dissection, aiming to preserve vital structures such as the accessory nerve and great vessels.
Some cancers, particularly tongue base and oropharynx are best managed with radiotherapy. Induction chemotherapy is often used as a single modality but is never curative. Radiotherapy is usually via external beam, and rarely with radioactive implants. A disadvantage of radiotherapy is that it damages salivary glands, resulting in xerostomia (dry mouth) which can be debilitating. Apart from discomfort, this predisposes to salivary gland infection.
Carcinoma of the lip has the best prognosis. The crude 5-year survival rate of oral cancer is around 50%, with small tumours having the best prognosis. Regional node involvement reduces the chance of cure by half.
Leukoplakia
Leukoplakia means ‘white plaque’, and describes white patches on oral mucosa which cannot readily be scraped off (see Fig. 48.7a). This distinguishes them from candidal infections. White plaques may be caused by friction, oral lichen planus or more rarely lupus erythematosus, but the main importance of leukoplakia is that it may represent epithelial dysplasia or even carcinoma-in-situ.
The cheeks and tongue are most often affected, although dysplastic patches may develop anywhere on oral mucosa. An innocent white line is often seen along the inside of the cheek; this corresponds to the biting surfaces of the teeth and is caused by frictional hyperplasia.
Severe or extensive leukoplakia should be referred for specialist maxillofacial opinion and biopsy. Areas of severe dysplasia require surgical removal, which may necessitate grafting.
Epulis
An epulis is a benign, localised gingival swelling. Two types are recognised: fibrous epulis and giant cell epulis.
A fibrous epulis is simply a benign fibrous tissue tumour arising from periodontal membrane or nearby periosteum. It forms a smooth, firm, slowly growing lump, covered with normal gingiva. A fibrous epulis usually emerges between two teeth, which may be pushed apart by pressure. Treatment is by excision with curettage of the origin to prevent recurrence (Fig. 48.8).
A giant cell epulis arises in a similar location but grows much faster. It forms an irregular red fleshy mass which ulcerates and bleeds. The lesion consists of numerous giant cells in a vascular stroma, which may invade local bone. Treatment involves extracting associated teeth and excising and curetting bone to avoid recurrence (Fig. 48.8).
Pyogenic granulomas may occur on gums or oral mucosa of the lips. They look like pyogenic granulomas of skin and often occur in pregnancy (see Ch. 46, p. 574).
Miscellaneous disorders causing intraoral swelling
Retention cysts of accessory salivary glands
The oral mucosa contains numerous accessory mucous and serous salivary glands. Small retention cysts probably develop as a result of duct trauma. Most retention cysts are smaller than 1 cm in diameter. They commonly occur in the lower lip mucosa where they are irritating and are readily traumatised. Retention cysts are blue-grey and are soft to palpation. They often rupture spontaneously but usually reform. Small retention cysts can usually be enucleated under local anaesthesia; larger ones may need marsupialisation. Swellings in the upper lip are almost always neoplastic and are malignant until proven otherwise.
Tumours of accessory salivary glands
Tumours occasionally arise in accessory salivary glands. These are often malignant adenocystic or muco-epidermoid carcinomas. They present as small, firm lumps in the oral mucosa, upper lip or posterior palate, and are often discovered before invading deeply or metastasising. Treatment is by wide excision but the prognosis is often poor.
Bony exostoses
Local outgrowths of jaw bones are common and produce an intraoral lump which may be suspicious of neoplasia to the uninitiated doctor. The common site is the middle of the hard palate, known as a torus palatinus. A similar exostosis, usually bilateral, occurs on the lingual (tongue) side of the mandible, opposite premolar teeth and is known as torus mandibularis.
These lesions are bony hard and are covered by normal oral mucosa. Excision is rarely needed unless there are problems in wearing a removable denture.
Cysts and tumours of the jaws
Various cystic lesions and tumours arise in the jaws. Many are abnormalities of tooth-forming epithelium, developmental or acquired. Figure 48.9b shows a mandibular dentigerous cyst, a developmental cyst. They are rare and can usually be diagnosed radiologically. The jaws are occasionally the site of benign or malignant bone tumours such as osteosarcoma and osteoclastomas. They can also be affected by metastatic tumours from breast or prostate. Bony growth disorders such as fibrous dysplasia and Paget's disease may also affect the jaw.
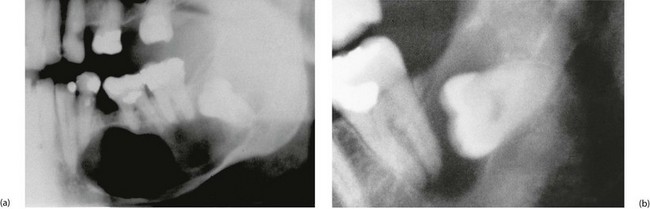
Fig. 48.9 Dental cyst and dentigerous cyst
(a) Large dental cyst in the mandible. This arose from tooth-forming epithelial remnants in the apical area of the lower left second premolar tooth which was extracted several months beforehand due to chronic periapical infection. (b) Dentigerous cyst associated with the crown of an unerupted lower third molar. These cysts originate from epithelial remnants of the tooth bud