Pelvis
“These, gentlemen, are the tuberosities of the ischia, on which man was designed to sit and survey the works of creation.
OLIVER WENDELL HOLMES (1809-1894),
Life and Letters of Oliver Wendell Holmes, vol. I, Chapter VII
The pelvis provides structural support for the body and encloses the male and female reproductive organs. Because of its role as a support mechanism for the body, the pelvis has a large amount of musculoskeletal anatomy, which, together with the differences in male and female anatomy, makes this area challenging to learn (Figure 8.1). This chapter demonstrates cross-section anatomy of the following structures:
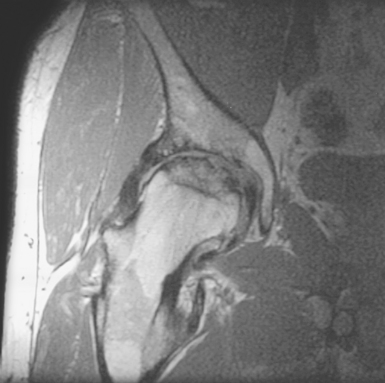
Figure 8.1 Coronal, T1-weighted MR image of right hip demonstrating avascular necrosis involving two thirds of the femoral head.
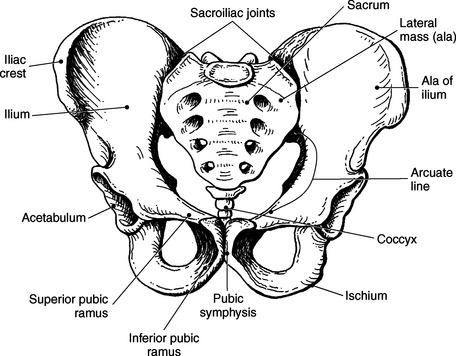
BONY PELVIS
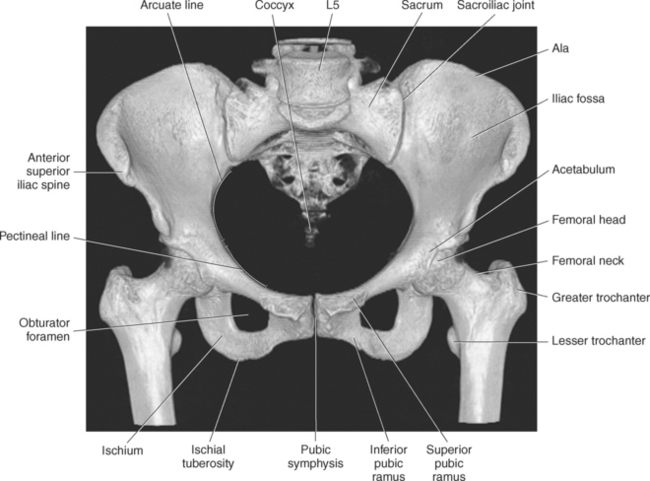
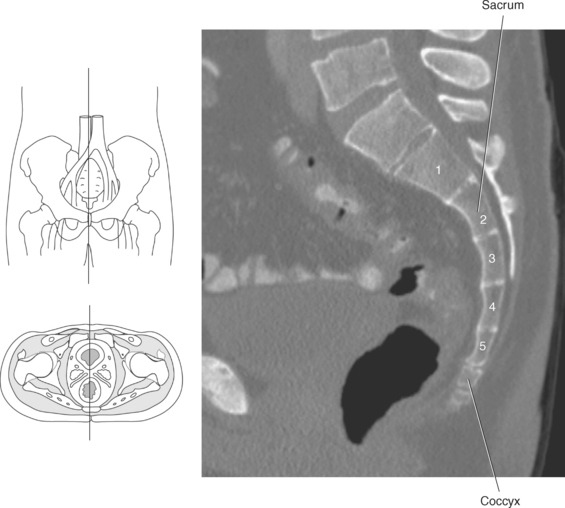
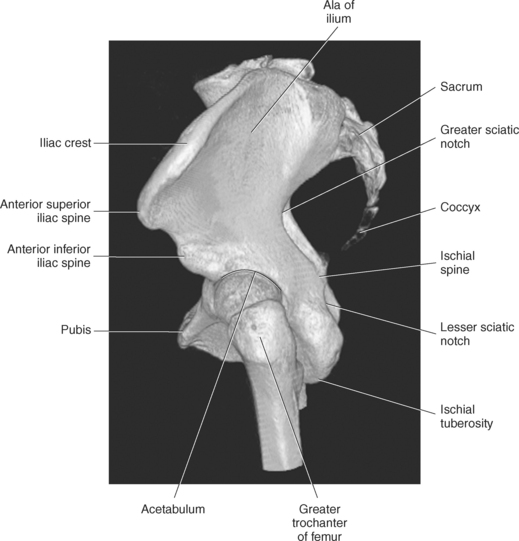
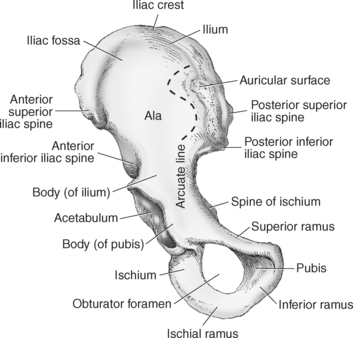
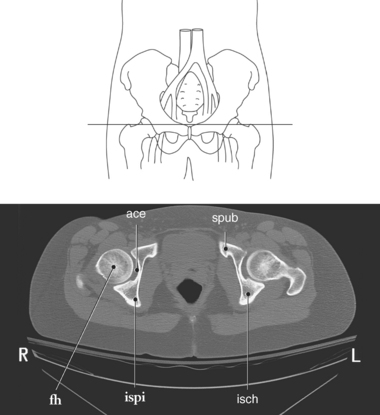
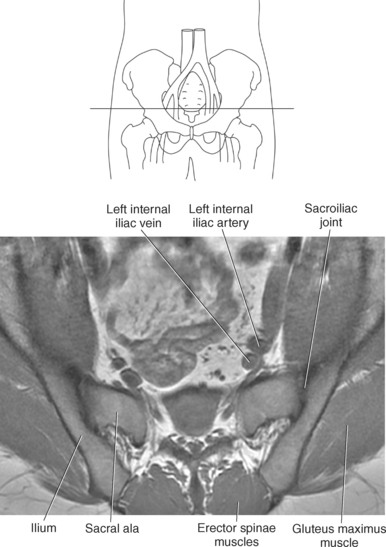
The bony pelvis is formed by the sacrum, coccyx, and two os coxae or innominate bones (Figures 8.2 and 8.3). The sacrum is a triangular-shaped bone formed by the fusion of five vertebral segments. The first sacral segment has a prominent ridge located on the anterior surface of the body termed the sacral promontory, which acts as a bony landmark separating the abdominal cavity from the pelvic cavity. The transverse processes of the five sacral segments combine to form the lateral mass (ala), which articulates with the os coxae at the sacroiliac joints (Figures 8.4 and 8.5). The lateral mass contains sacral foramina that allow for the passage of sacral nerves (Figure 8.6). Articulating with the fifth sacral segment is the coccyx, which consists of three to five small fused bony segments (Figure 8.7).
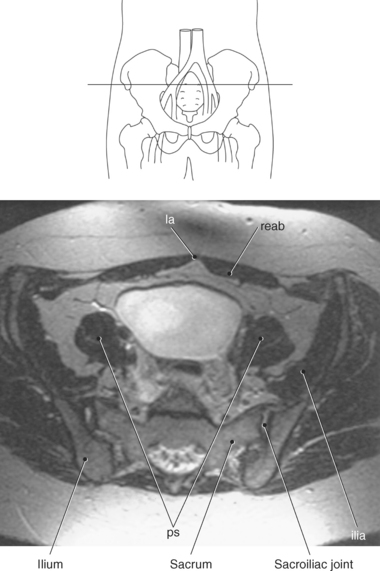
Figure 8.4 Axial, T1-weighted MR scan of ilium and sacroiliac joints.
Key: la, Linea alba; reab, rectus abdominis; ilia, iliacus muscle; ps, psoas muscles.
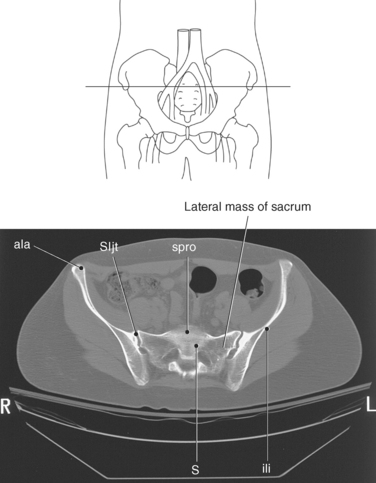
Figure 8.5 Axial CT scan of sacroiliac joints with ala of ilium.
Key: ala, ala of ilium; SIjt, sacroiliac joint; spro, sacral promontory; ili, iliac fossa; S, sacrum.
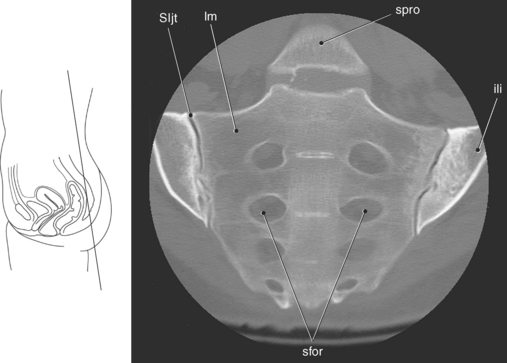
Figure 8.6 Coronal oblique CT scan of sacroiliac joints.
Key: SIjt, sacroiliac joint; lm, lateral mass; spro, sacral promontory; ili, iliac fossa; sfor, sacral foramina.
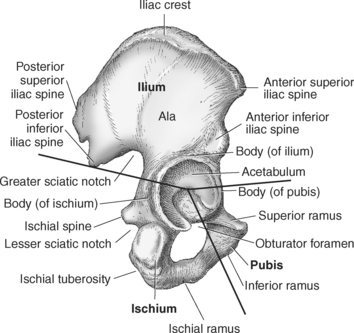
The os coxae are made up of three bones: ilium, pubis, and ischium (Figure 8.8).
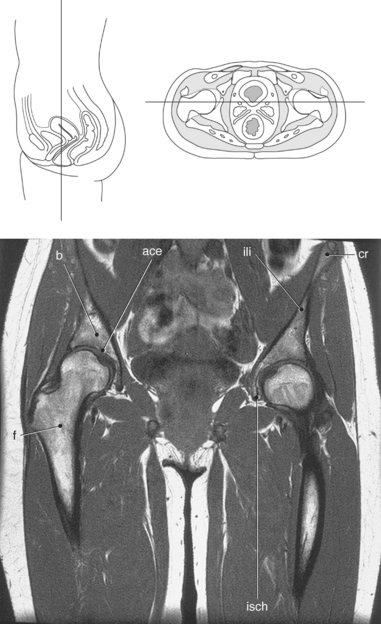
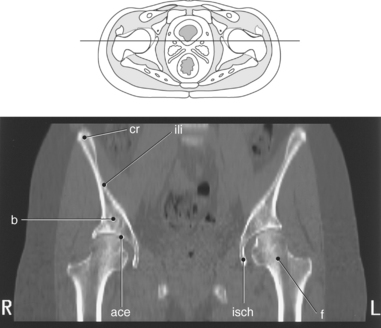
Ilium
The ilium, the largest and most superior portion, consists of a body and a large winglike projection called the ala (Figure 8.9). The concave, anterior surface of the ala is termed the iliac fossa, which is separated from the body by the arcuate line. This arch-shaped line, located on the anterior surface of the ilium, forms part of the pelvic brim (Figures 8.10 and 8.11). The superior ridge of the ala is termed the iliac crest; it slopes down to give rise to the superior and inferior iliac spines on both the anterior and posterior surfaces (Figures 8.9 and 8.10). The body of the ilium creates the upper portion of the acetabulum, which is a deep fossa that articulates with the head of the femur (Figures 8.12 and 8.13).
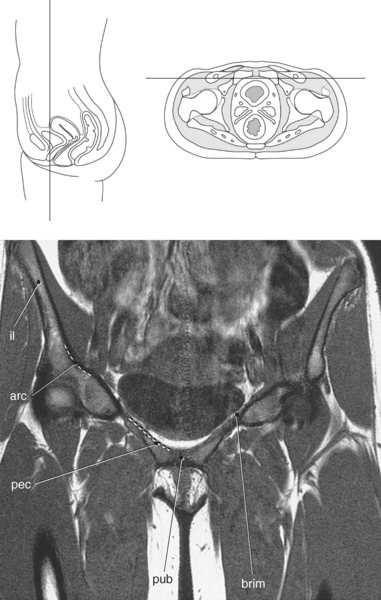
Figure 8.11 Coronal, T1-weighted MR scan of pelvis with pelvic brim.
Key: il, Ilium; arc, arcuate line; pec, pectineal line; pub, pubis symphysis; brim, pelvic brim.
Pubis
The pubis, or pubic bone, forms the lower anterior portion of the acetabulum and consists of a body and a superior and inferior pubic rami (Figure 8.8). The bodies of the two pubic bones meet at the midline to form the pubic symphysis. The superior pubic ramus projects inferiorly and medially from the acetabulum to the midline of the body (Figures 8.14 and 8.15). Located on the upper surface of the superior pubic ramus is a ridge termed the pectineal line, which is continuous with the arcuate line of the ilium, forming the pelvic brim (Figure 8.11). The inferior pubic ramus projects inferiorly and laterally from the body to join the ischium at an indistinct point; as a result, the two together are often referred to as the ischiopubic ramus (Figure 8.16).
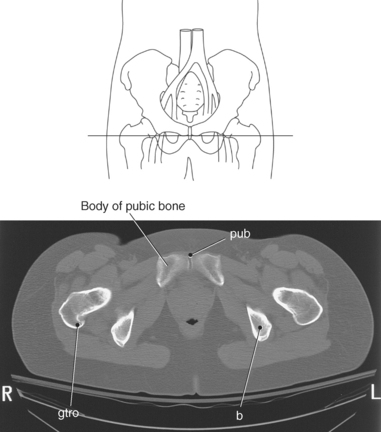
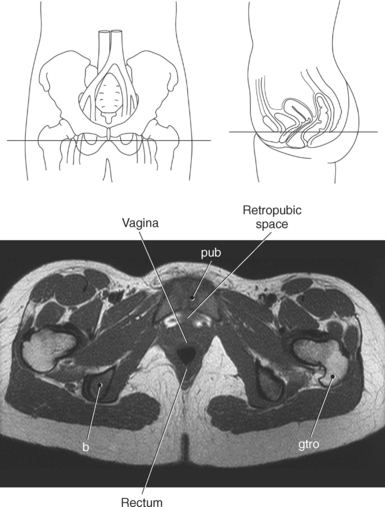
Figure 8.14 Axial CT scan with pubic symphysis and superior pubic ramus.
Key: pub, Pubis symphysis; b, body of ilium; gtro, greater trochanter.
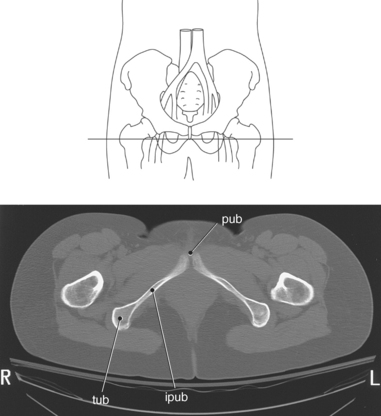
Ischium
The ischium, the inferior portion of the os coxae, like the pubis is composed of a body and two rami. The body of the ischium forms the lower posterior portion of the acetabulum (Figures 8.8, 8.10, and 8.13). The superior ischial ramus extends posteriorly and inferiorly to a roughened, enlarged area termed the ischial tuberosity (Figures 8.9 and 8.16). From the ischial tuberosity, the inferior ischial ramus extends anteriorly and medially to join the inferior pubic ramus. The ischial spine projects from the superior ischial ramus between two prominent notches on the posterior surface of the os coxae (Figures 8.8 through 8.10, and 8.15). The greater sciatic notch extends from the posterior inferior iliac spine to the ischial spine, and the lesser sciatic notch extends from the ischial spine to the ischial tuberosity (Figures 8.8 and 8.9). The two notches are spanned by ligaments that create foramina for the passage of nerves and vessels. The union of the pubic rami and ischium surrounds a large opening termed the obturator foramen, which is enclosed by the obturator muscles (Figures 8.3 and 8.10).
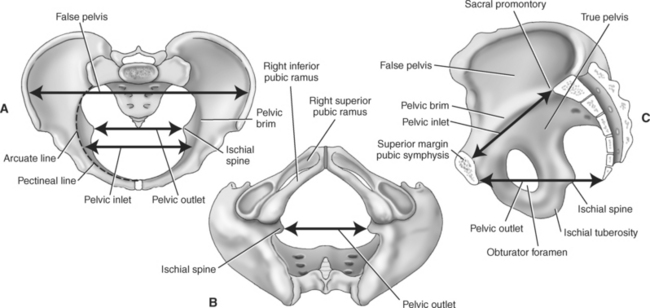
Pelvic Inlet and Outlet
The pelvis is divided into the false or greater pelvis and the true or lesser pelvis by an oblique plane that extends from the upper anterior margin of the sacrum, along the arcuate line, to the upper margin of the pubic symphysis. The boundary line of this plane is called the pelvic brim, which delineates the boundaries of the abdominal and pelvic cavities. The region above the brim is called the false pelvis, and the region below the brim is called the true pelvis, which can be subdivided by the pelvic diaphragm into the main pelvic cavity and the perineum (Figure 8.17, A). The superior aperture or inlet of the true pelvis is measured in the anteroposterior direction from the sacral promontory to the superior margin or crest of the pubic bone (Figure 8.17, B). The pelvic outlet or inferior aperture is an opening bounded by the inferior edges of the pelvis and is measured from the tip of the coccyx to the inferior margin of the pubic symphysis in the anteroposterior direction and between the ischial tuberosities in the horizontal direction (Figure 8.17, C).
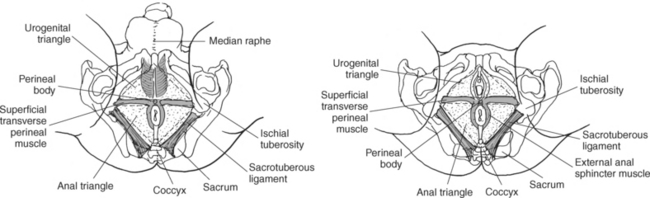
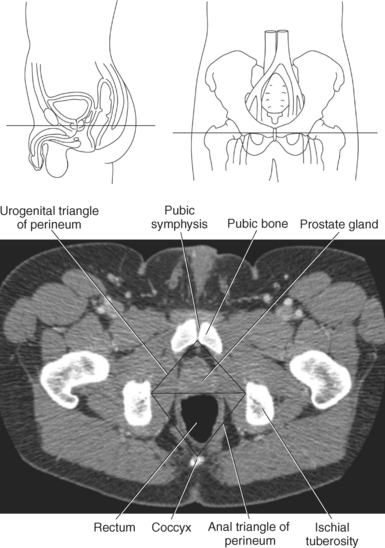
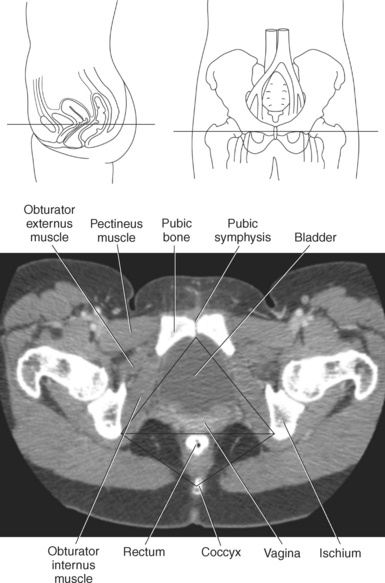
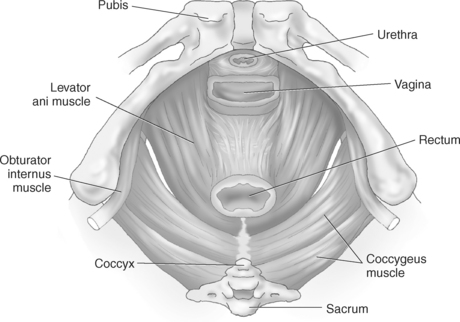
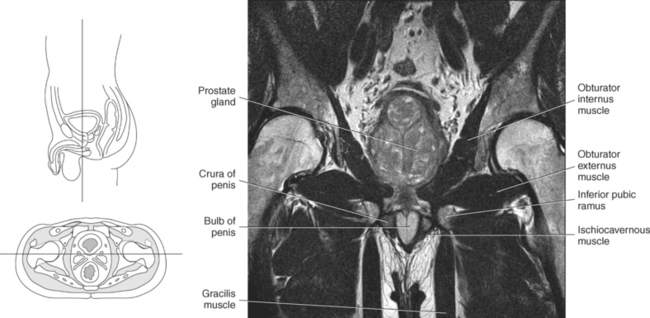
Perineum
The perineum and its contents cover and partially fill the inferior aperture of the bony pelvis. The bony circumferential boundaries of the perineum are the inner edges of the pelvic outlet and consist of the following surface relationships: anteriorly by the pubic symphysis; laterally by the pubic rami, ischial rami, ischial tuberosities, and sacrotuberous ligaments; and posteriorly by the coccyx (Figure 8.18). The region is divided into two triangles, posterior and anterior, by joining the ischial tuberosities by an imaginary line. The posterior triangle is the anal triangle, and the anterior triangle is the urogenital triangle. The anal triangle contains the inferior one third of the anal canal and its sphincter muscles, and ischioanal fossae. The urogenital triangle contains the openings of the urethra and vagina in the female and the urethra and root structures of the penis in the male (Figures 8.18 through 8.20).
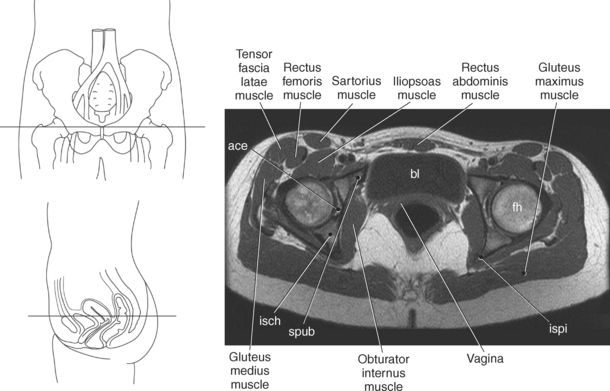
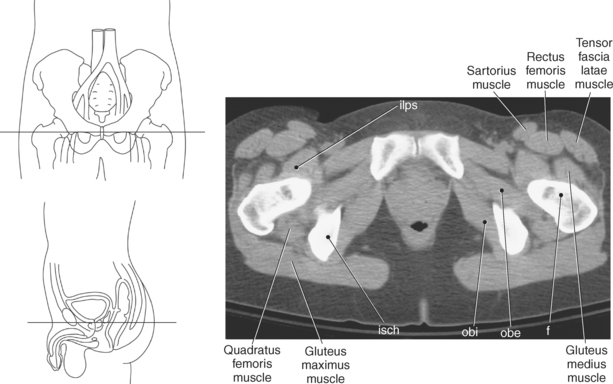
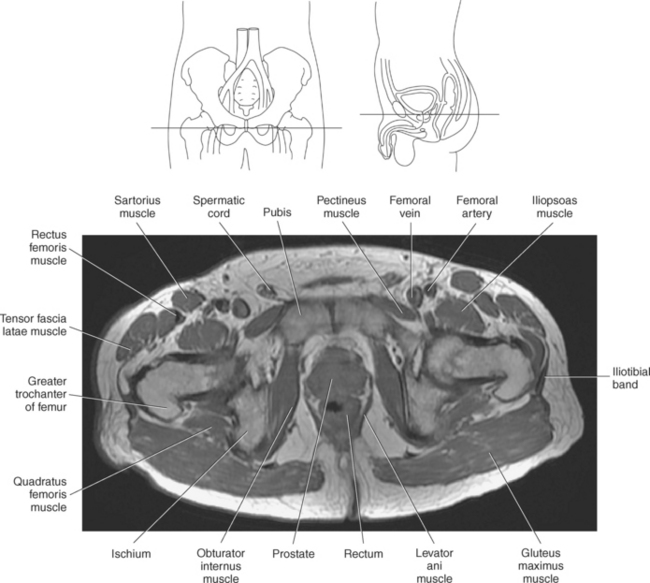
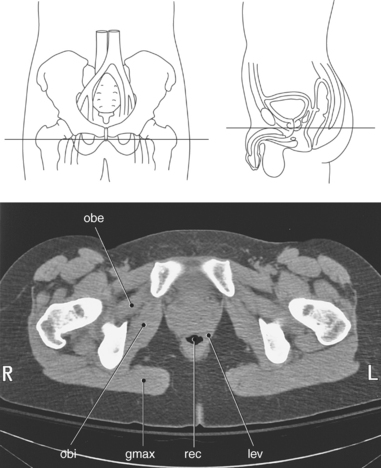
MUSCLES
Multiple muscles are visualized in the pelvis. For ease of description, the major pelvic muscles have been divided into functional groups: extra pelvic, pelvic wall, and pelvic diaphragm.
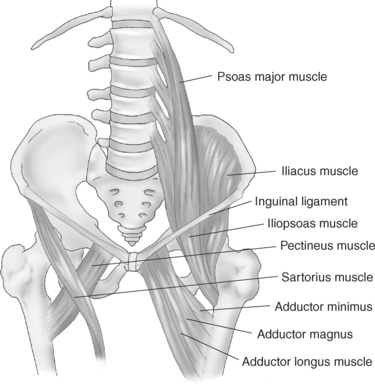
Extrapelvic Muscles
Several of the muscles visualized in the pelvis are actually abdominal muscles such as the rectus abdominis, psoas, and internal and external oblique muscles. The rectus abdominis muscles, visualized on the anterior surface of the abdomen and pelvis, originate from the symphysis pubis and extend to the xiphoid process and the costal cartilage of the fifth, sixth, and seventh ribs. They function to flex the lumbar vertebrae and support the abdomen. The psoas muscles extend along the lateral surfaces of the lumbar vertebrae and act to flex the thigh or trunk. The external and internal oblique muscles are located on the outer lateral portion of the abdomen and span primarily between the cartilages of the lower ribs to the level of the iliac crest. The oblique muscles work together to flex and rotate the vertebral column and compress the abdominal viscera. An inferior band of fibrous connective tissue from the external oblique muscle folds back on itself to form the inguinal ligament, which spans the anterior superior iliac spine and the pubic tubercle (Figures 7.176 through 7.182)
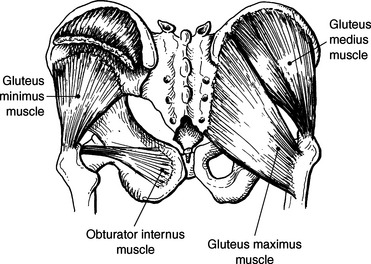
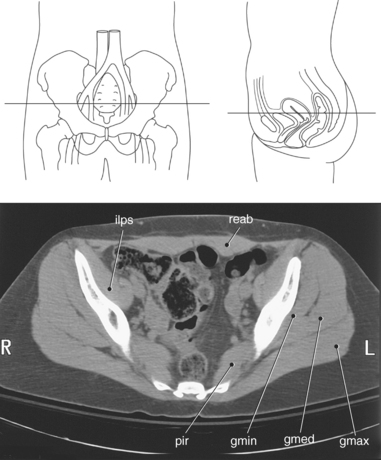
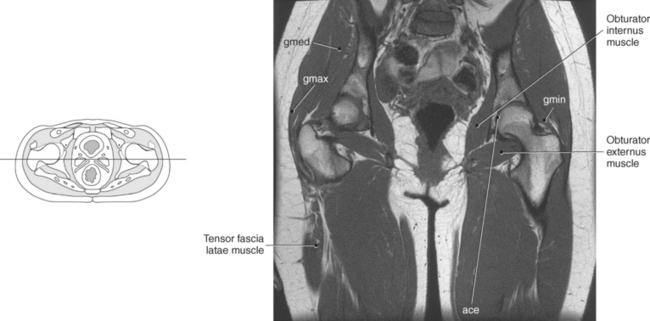
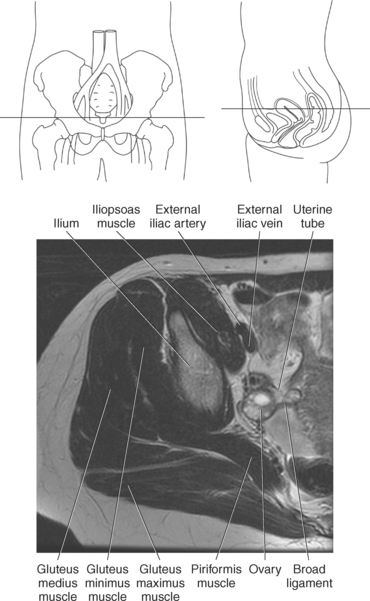
Many of the muscles visualized in the pelvis are considered to be muscles of the hip. The largest of this group are the gluteus muscles (maximus, medius, minimus), which function together to abduct, rotate, and extend the thigh. The largest and most superficial is the gluteus maximus muscle, which makes up the bulk of the buttocks. The gluteus medius and minimus muscles are smaller in size, respectively, and are deep to the gluteus maximus muscle (Figures 8.21 through 8.24; see also Chapter 10).
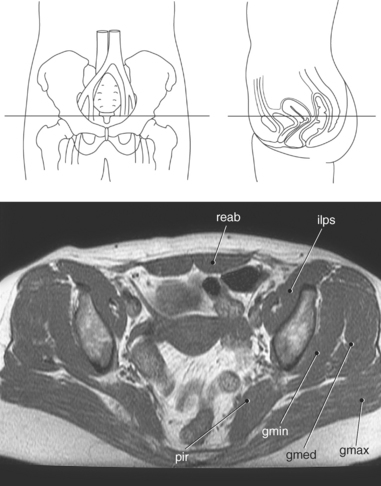
Figure 8.22 Axial, T1-weighted MR scan of pelvis with gluteus muscle group.
Key: reab, Rectus abdominis; ilps, iliopsoas; gmax, gluteus maximus; gmed, gluteus medius; gmin, gluteus minimus; pir, piriformis.
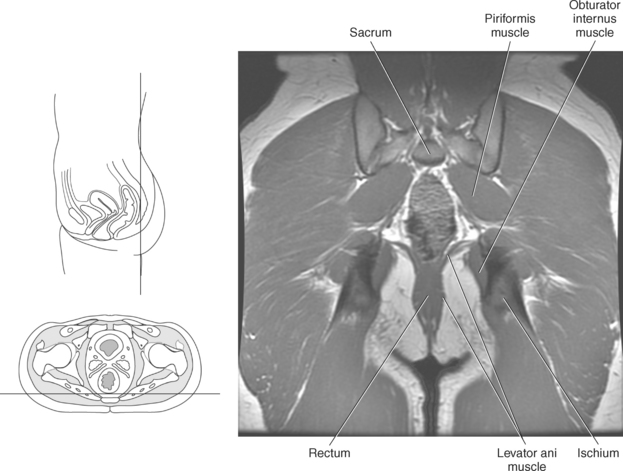
Pelvic Wall Muscles
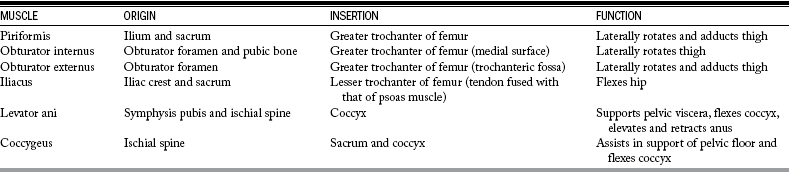
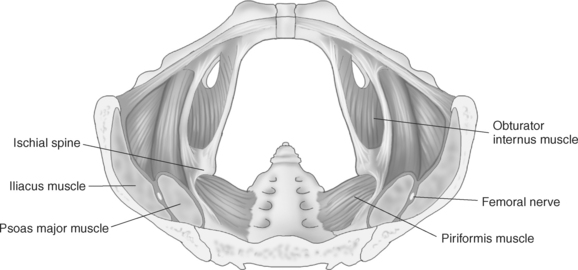
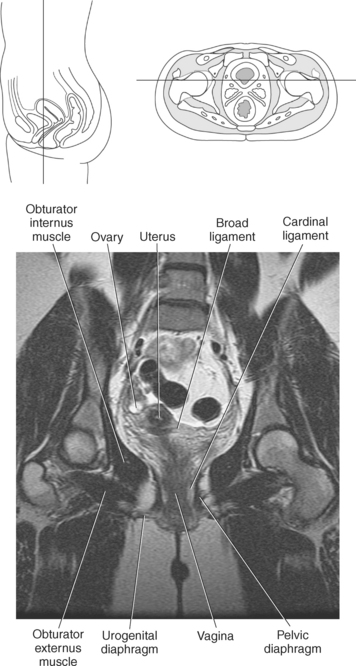
The muscles of the pelvic wall include the piriformis, obturator internus and externus, and iliacus muscles. The piriformis muscle, which acts to rotate the thigh laterally, originates from the ilium and the sacrum and passes through the greater sciatic notch to insert on the greater trochanter of the femur. Also functioning to rotate the thigh laterally is the obturator internus muscle. This fan-shaped muscle extends from the pubic bone and obturator foramen to pass through the lesser sciatic notch and attaches to the greater trochanter of the femur. Inserting on the greater trochanter just below the obturator internus muscle is the obturator externus muscle. This strong muscle originates on the obturator foramen, aiding in adduction and rotation of the thigh. Extending from the iliac crest and sacrum is the triangular-shaped iliacus muscle. As the iliacus muscle spans the iliac fossa it is joined by the psoas muscle to form the iliopsoas muscle, which extends to insert on the lesser trochanter of the femur. The iliopsoas muscle is the most important muscle for flexing the leg, which makes walking possible (Figures 8.25 through 8.30 and Table 8.1; see also Chapter 10).
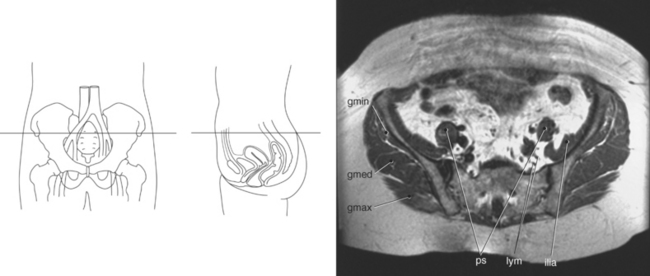
Figure 8.27 Axial, T1-weighted MR scan of pelvis with iliacus muscle.
Key: gmin, Gluteus minimus; gmed, gluteus medius; gmax, gluteus maximus; ps, psoas muscle; lym, lymph nodes; ilia, iliacus.
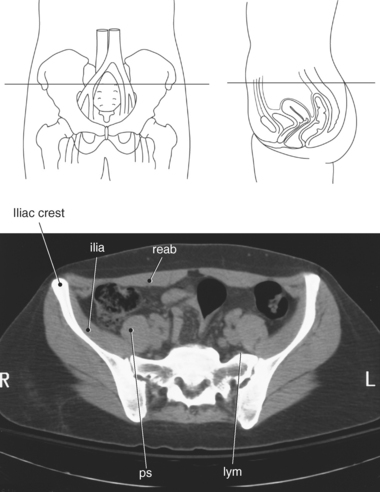
Figure 8.28 Axial CT scan of pelvis with iliacus muscle.
Key: ilia, iliacus; reab, rectus abdominis; ps, psoas muscle; lym, lymph nodes.
Pelvic Diaphragm Muscles
The funnel-shaped pelvic diaphragm is a layer of muscles and fascia that forms the greatest majority of the pelvic floor. The primary muscles of the pelvic diaphragm are the levator ani and coccygeus muscles. The two levator ani muscles are the largest and most important muscles of the pelvic floor, originating from the symphysis pubis and ischial spines to form winglike arches that attach to the coccyx. The levator ani muscle can be subdivided into the pubococcygeus, puborectalis, and iliococ cygeus muscles. The two coccygeus muscles form the posterior portion of the pelvic floor, arising from the ischial spines and fanning out to attach to the lower sacrum and coccyx. Together, the levator ani and coccygeus muscles provide support for the pelvic contents (Figures 8.31 through 8.38 and Table 8.1).
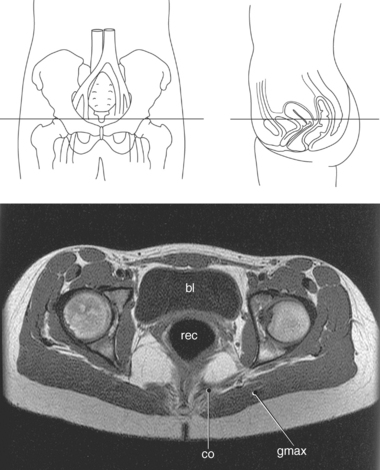
Figure 8.32 Axial, T1-weighted MR scan of pelvis with coccygeus muscles.
Key: bl, Bladder; rec, rectum; co, coccygeus; gmax, gluteus maximus.
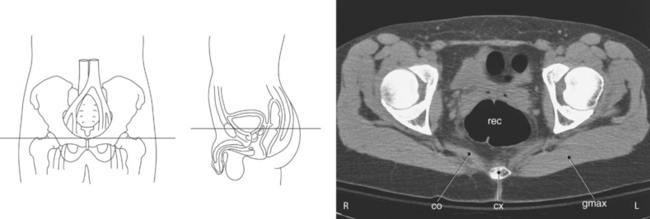
Figure 8.33 Axial CT scan of pelvis with coccygeus muscles.
Key: rec, Rectum; co, coccygeus; cx, coccyx; gmax, gluteus maximus.
VISCERA
The pelvic cavity contains the urinary bladder, rectum, and internal reproductive organs.
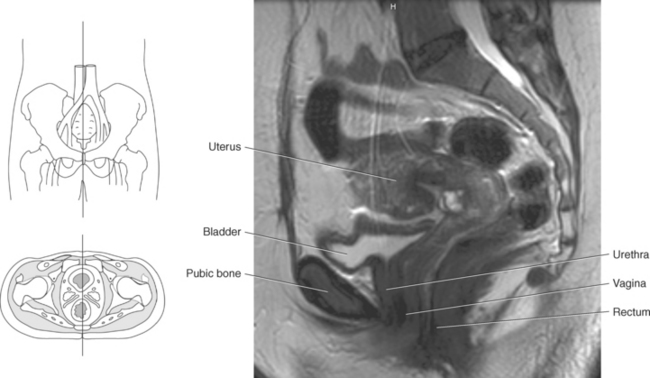
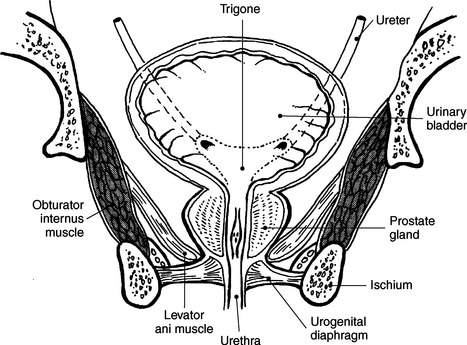
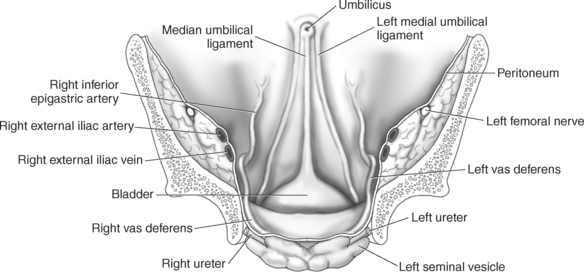
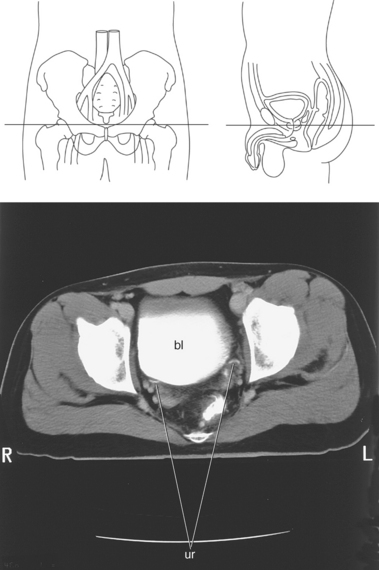
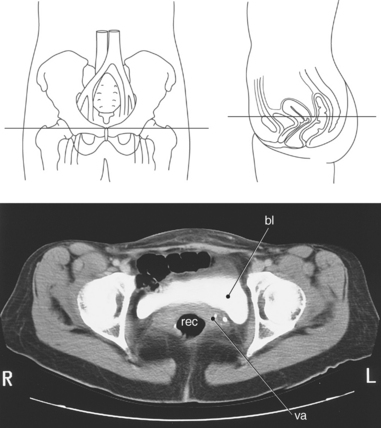
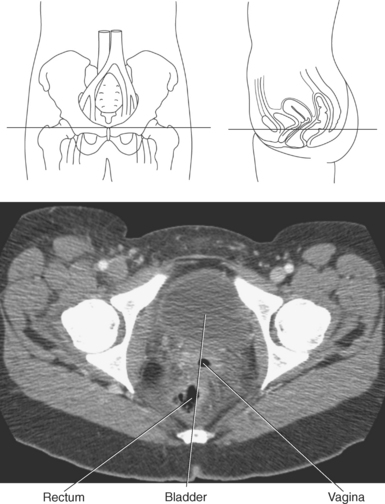
Urinary Bladder
The urinary bladder is a pyramid-shaped muscular organ that rests on the pelvic floor, immediately posterior to the symphysis pubis (Figures 8.39 through 8.44). It functions as a temporary reservoir for the storage of urine. In a normal adult, it takes approximately 250 to 250 mL of urine to accumulate before the urge to urinate is triggered. However, the bladder has the potential storage capacity of approximately 750 mL. When empty, the bladder has four surfaces (superior, posterior, and two inferolateral) and four angles (anterior, inferior, and two posterolateral). The superior surface (body) of the bladder is covered by peritoneum, allowing loops of ileum and sigmoid colon to rest on it. The posterior surface is referred to as the fundus or base of the bladder. This surface is closely related to the anterior wall of the vagina in the female and to the rectum in the male. The two inferolateral surfaces face inferior, lateral, and anterior and are in contact with the fascia covering the levator ani muscles (Figure 8.37). As urine is collected in the bladder, the superior and inferolateral surfaces distend accordingly while the posterior surface remains relatively fixed. The inferior angle is a funnel-shaped narrowing formed by the convergence of the inferolateral and posterior surfaces and is called the neck of the bladder, which is continuous with the urethra (Figure 8.39). The bladder neck contains the muscular internal urethral sphincter, which provides for involuntary control over the release of urine from the bladder. The two posterolateral angles mark the point where the ureters enter the bladder. The anterior angle is formed by the convergence of the superior and inferolateral surfaces and is referred to as the apex of the bladder. The bladder is anchored to the pelvis by peritoneal ligaments. The apex is attached to the anterior abdominal wall by the median umbilical ligament, which is the remains of the fetal urachus (obliterated umbilical artery). Two lateral (medial) umbilical ligaments from the body of the bladder ascend along with the median umbilical ligament to the umbilicus (Figures 8.43 and 8.44). The fibrous cords of these ligaments represent the obliterated remains of the two umbilical arteries that provided blood to the placenta during fetal development. The bladder neck is held in place by the puboprostatic ligament in males and the pubovesical ligament in females. Three openings in the floor of the bladder form a triangular area called the trigone (Figure 8.37). Two of the openings are created by the ureters. The pelvic portions of the ureters run anterior to the internal iliac arteries and enter the posterolateral surface of the bladder at an oblique angle (Figure 8.45). The third opening is located in the apex of the trigone and is formed by the entrance to the urethra (Figures 8.44 and 8.46).
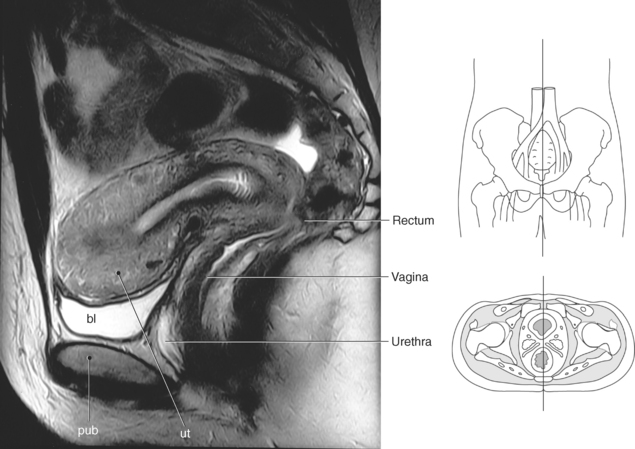
Figure 8.40 Sagittal, T2-weighted MR scan of female pelvis.
Key: bl, Bladder; pub, pubic symphysis; ut, uterus.
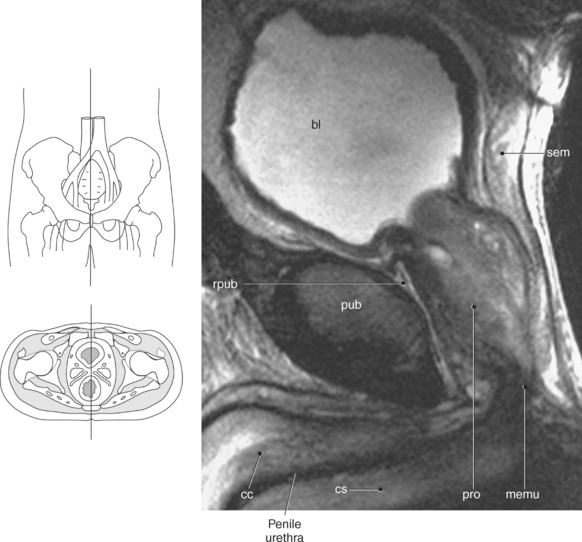
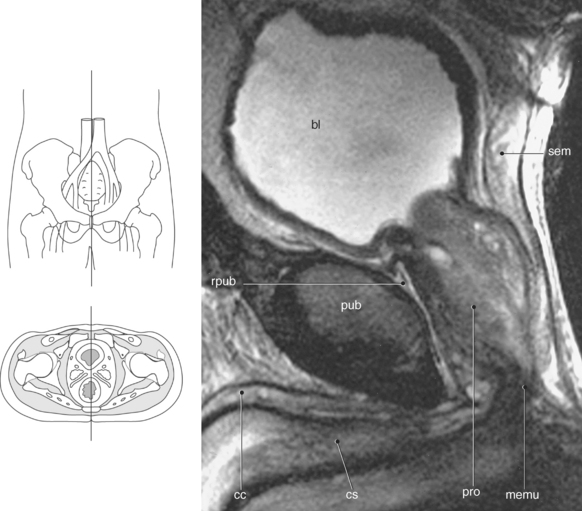
Figure 8.42 Sagittal, T2-weighted MR scan of male pelvis.
Key: bl, Bladder; sem, seminal vesicle; pub, pubic symphysis; rpub, retropubic space; cc, corpora cavernosum; cs, corpus spongiosum; pro, prostate gland; memu, membranous urethra.
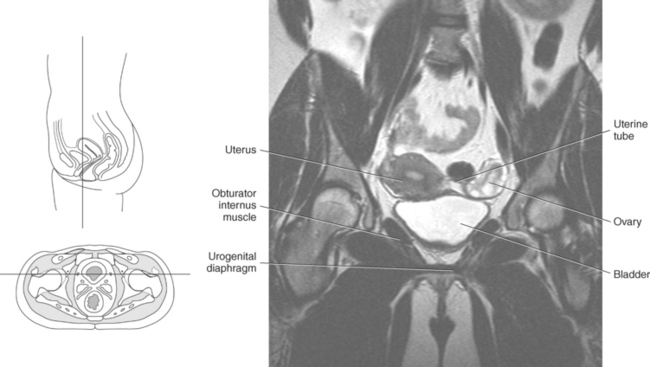
Figure 8.44 Coronal, T2-weighted MR scan of female pelvis with urinary bladder.
Key: bl, Bladder; sem, seminal vesicle; pub, pubic symphysis; rpub, retropubic space; cc, corpora cavernosum; cs, corpus spongiosum; pro, prostate gland; memu, membranous urethra.
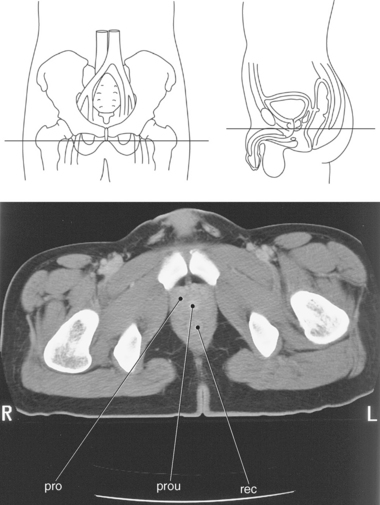
Figure 8.46 Axial CT scan of pelvis with male urethra.
Key: pro, prostate gland; prou, prostatic urethra; rec, rectum.
The urethra in both genders passes through the urogenital diaphragm, which contains the urethral sphincter muscle responsible for the voluntary closure of the bladder.
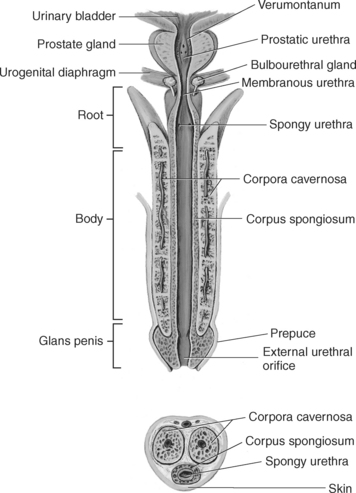
The female urethra is a short (3-4 cm) muscular tube that drains urine from the bladder. It descends inferiorly and anteriorly while embedded in the anterior vaginal wall and terminates at the external urethral opening located between the clitoris and vagina (Figures 8.39 and 8.40). The male urethra is much longer (18-20 cm) and extends from the inferior portion of the bladder to the tip of the penis (Figures 8.41, 8.42, and 8.46). It can be subdivided into three regions: prostatic urethra, membranous urethra, and penile urethra. The prostatic urethra passes through the middle of the prostate gland. The membranous urethra is the shortest and narrowest portion of the urethra and is the portion that penetrates the external urethral sphincter. The penile urethra is the longest portion, extending from the external urethral sphincter to the tip of the penis (Figures 8.41 and 8.42). The male urethra has the dual function to drain urine from the bladder and to receive secretions from the prostatic and ejaculatory ducts and the ducts of the bulbourethral glands.
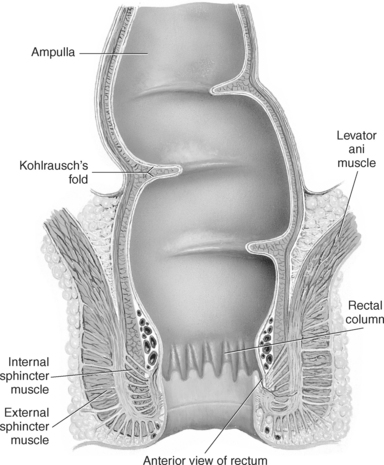
Rectum
The rectum is the terminal part of the large intestine extending from S3 to the tip of the coccyx, approximately 15 cm. It follows the anteroposterior curve of the sacrum and coccyx (sacral flexure) and ends by turning inferiorly and anteriorly (perineal flexure) to become the anal canal, which ends at the anus (Figures 8.39 through 8.42). Between the two flexures is a fold of tissue called the transverse rectal fold (Kohlrausch’s fold) located 5 to 8 cm from the anus (Figure 8.47). It serves as a topographic landmark during a rectal exam marking the posterior side of the prostate in males and the vault of the vagina in females. The upper third of the rectum, the rectal ampulla, has considerable distensibility. As fecal material collects in this area, it triggers the urge to defecate. The anal canal is the distal portion of the rectum and contains small longitudinal folds called rectal or anal columns. The anus marks the exit of the anal canal and is under involuntary control by the internal anal sphincter, a circular muscle layer within the rectal wall. The external anal sphincter consists of a ring of skeletal muscle fibers and is under voluntary control (Figures 8.47 through 8.49).
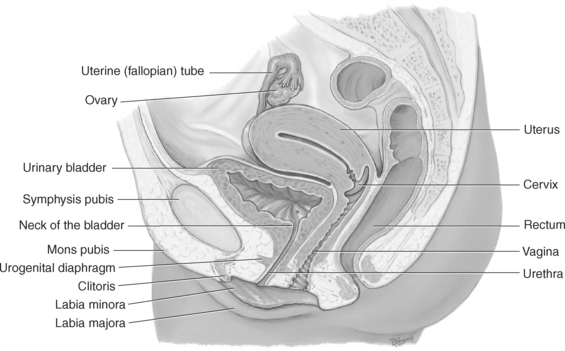
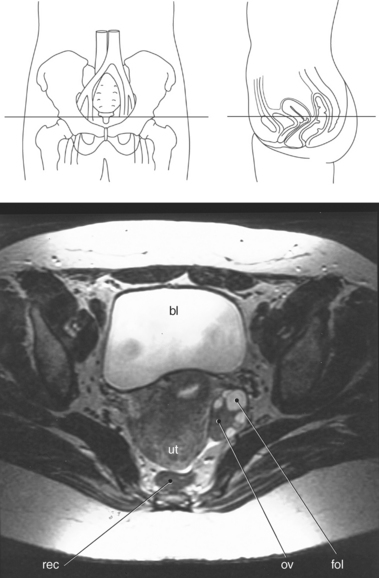
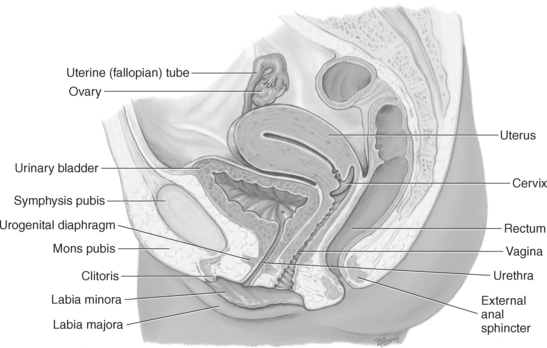
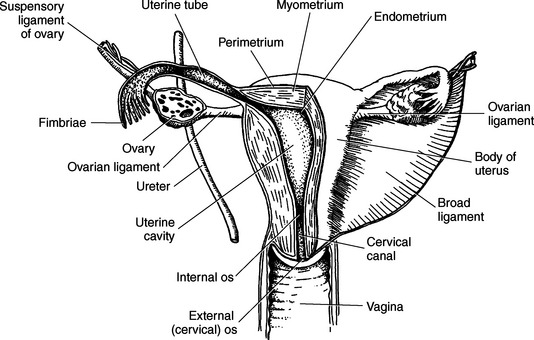
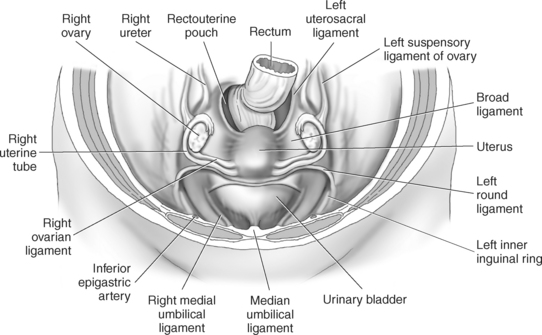
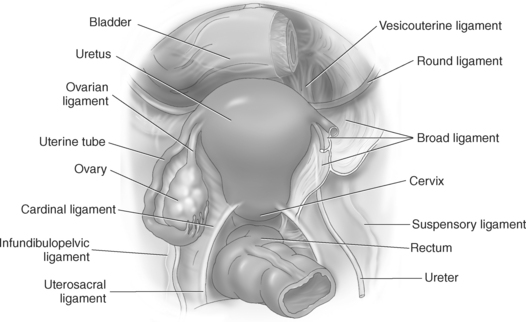
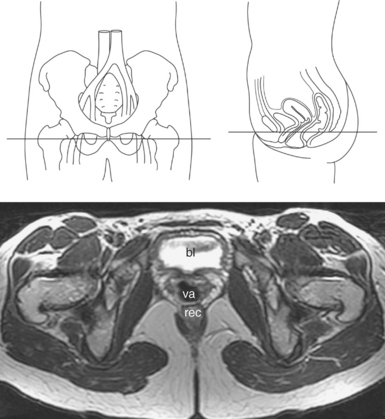
Female Reproductive Organs
The female reproductive system is responsible for producing sex hormones and ova and functions to protect and support a developing embryo. The principal organs of the female reproductive system are located within the pelvic cavity and include the uterus, ovaries, uterine tubes, and vagina (Figures 8.50 and 8.51).
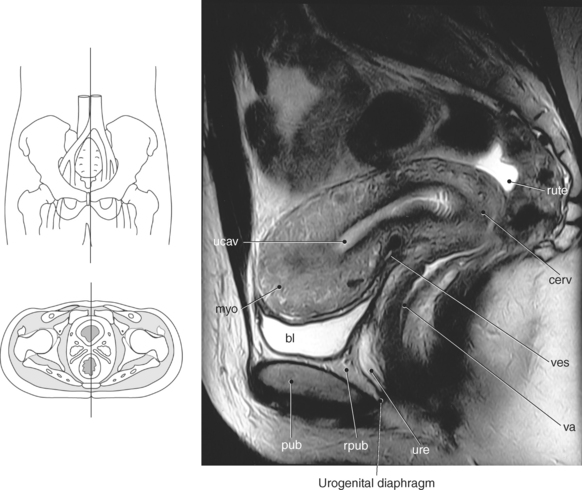
Figure 8.51 Sagittal, T2-weighted MR scan of female reproductive system.
rute, rectouterine pouch; cerv, cervix; ves, vesicouterine pouch; va, vagina; ure, urethra; rpub, retropubic space; pub, pubic symphysis; bl, bladder; myo, myometrium; ucav, uterine cavity.
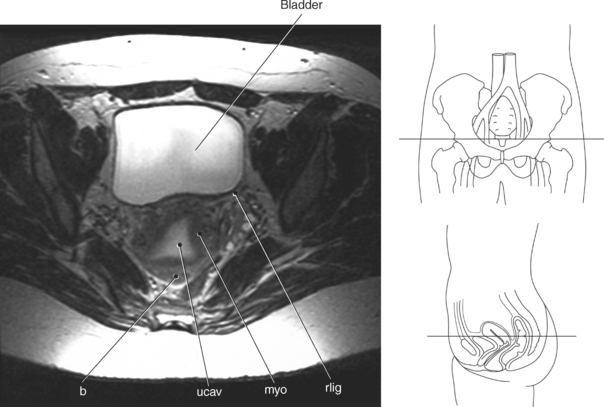
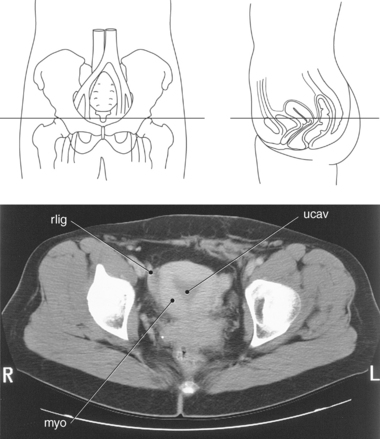
Uterus
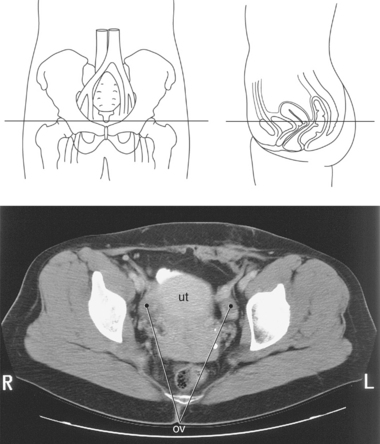
The uterus is a pear-shaped muscular organ located in the anterior portion of the pelvic cavity between the bladder and the rectum (Figures 8.50 and 8.51). The uterus can be subdivided into two anatomic regions: body and cervix. The body is the largest division, comprising the upper two thirds of the uterus. The rounded superior portion of the body is called the fundus, which is located just superior to the region where the uterine tubes enter the uterus. The lateral borders of the fundus contain the cornua, where the uterine tubes attach to the uterus. The narrow inferior third of the uterus is called the cervix, which communicates with the vagina. The narrow lumen within the cervix, called the cervical canal, is a conduit between the uterine cavity superiorly via the internal os and opens inferiorly into the vagina via the external os (Figure 8.52). The most common position of the uterus is with the body projecting superiorly and anteriorly over the bladder, with the fundus adjacent to the anterior abdominal wall and the cervix directed inferior and posteriorly into the vaginal vault. The wall of the uterus is composed of three layers: the endometrium is the inner glandular tissue lining the inner wall; the myometrium is the middle, muscular layer and the thickest component of the uterine wall; and the perimetrium is the outer layer consisting of a serous membrane that covers the fundus and posterior surface of the uterus. The endometrium is lined by a mucous membrane that is continuous with the inner lining of the vagina and uterine tubes. The thick myometrial layer is highly vascular and is responsible for the main contractive force during childbirth. The perimetrium is formed by peritoneum and is firmly attached to the myometrium. The uterus is the reproductive organ responsible for protecting and nourishing the fetus during development (Figures 8.50 through 8.55).
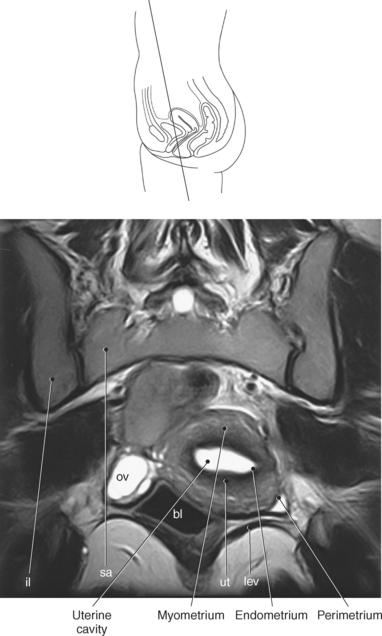
Figure 8.53 Coronal, T2-weighted MR scan of female bladder.
Key: il, ilium; sa, sacrum; ov, Ovaries; bl, bladder; ut, uterus; lev, levator ani.
Suspensory Ligaments of the Uterus
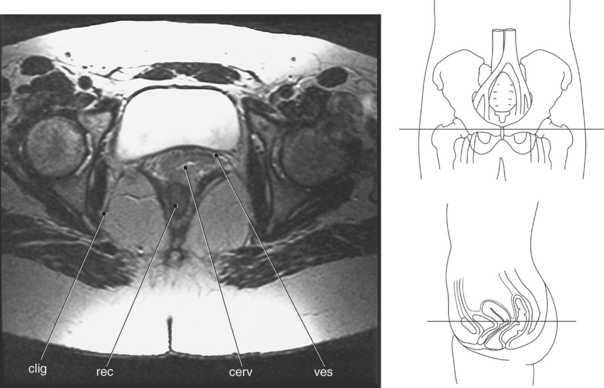
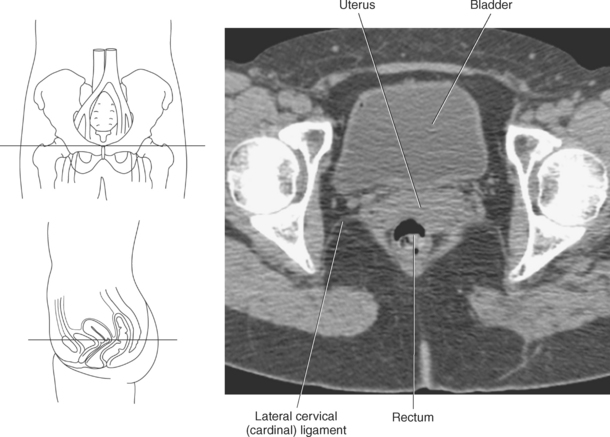
The uterus is stabilized by several pair of suspensory ligaments formed by peritoneum. The round ligaments extend laterally from the uterine cornu to the inner inguinal ring, through the inguinal canal, and anchor to the labia majora (Figures 8.54 and 8.55). They help keep the body flexed anteriorly (anteversion) and help to prevent posterior movement of the uterus (Figures 8.56 and 8.57). The uterosacral ligaments extend from the lateral walls of the cervix to the anterior surface of the sacrum, preventing forward movement of the uterus (Figure 8.58). The lateral cervical (cardinal) ligaments extend like a fan from the lateral walls of the cervix and vagina and anchor into the fascia of the wall of the lesser pelvis. They help suspend the uterus above the bladder and help to prevent downward displacement of the uterus. Additional support is provided by the muscles and fascia of the pelvic floor (Figures 8.59 through 8.61).
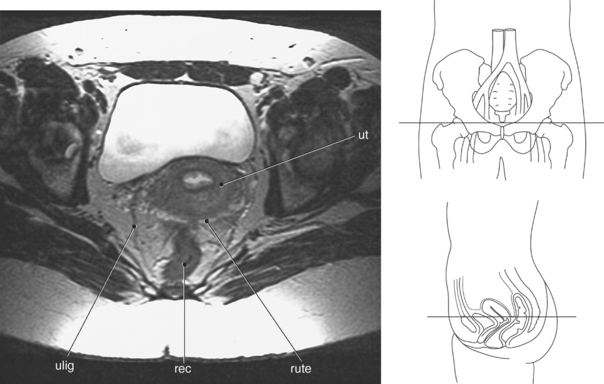
Figure 8.58 Axial, T2-weighted MR scan of pelvis with uterosacral ligaments.
Key: ut, Uterus; rute, rectouterine pouch; rec, rectum; ulig, uterosacral ligament.
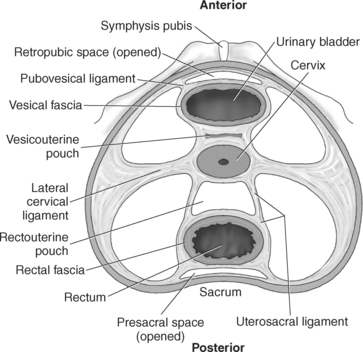
Pelvic Spaces
A peritoneal fold called the broad ligament encloses the ovaries, uterine tubes, and uterus (Figures 8.57 and 8.62). The broad ligament extends from the sides of the uterus to the walls and floor of the pelvis, preventing side- to-side movement of the uterus and dividing the pelvis into anterior and posterior pouches. The anterior vesicouterine pouch is located between the uterus and the posterior wall of the bladder, whereas the posterior rectouterine pouch (pouch of Douglas) lies between the uterus and rectum (Figures 8.58, 8.59, and 8.63). The pelvic spaces are common areas for the accumulation of fluid within the pelvis. Another space in the pelvis is the retropubic space, located between the pubic bones and the bladder and containing extraperitoneal fat and connective tissue for the expansion of the bladder (Figures 8.63 and 8.64).
Ovaries
The paired ovaries are small almond-shaped organs located on either side of the uterus (Figures 8.65 through 8.67). They lie in a depression on the lateral walls of the pelvis and are held in place by the ovarian and suspensory ligaments (Figure 8.57). The cordlike ovarian ligament attaches the inferior aspect of the ovaries to the lateral surface of the uterus and uterine tubes (Figure 8.52). The suspensory ligament attaches the superior aspect of the ovaries to the lateral sides of the pelvic wall and contains the ovarian vessels (Figures 8.56 and 8.57). The ovaries are responsible for the production of ova and the production and secretion of estrogens and progesterone. Estrogens are responsible for the development and maintenance of female characteristics and reproductive organs. Progesterone is responsible for the uterine changes in preparation of pregnancy, such as thickening of the uterine lining and decreasing contractions by uterine muscle.
Uterine Tubes
The uterine (fallopian) tubes are slender, muscular tubes (approximately 8-2 0 cm long) extending laterally from the body of the uterus to the peritoneum near the ovaries (Figure 8.57). They are supported by the broad ligament and at their distal end expand to form a funnel-shaped infundibulum. The infundibulum has numerous 1- to 2-cm fingerlike projections called fimbriae that spread loosely over the surface of the ovaries. During ovulation, the fimbriae trap the ovum and sweep it into the uterine tubes. The proximal portion of the uterine tubes opens into the uterus, and the distal portion opens directly into the peritoneal cavity, immediately superior to the ovaries, thereby providing a direct route for pathogens to enter the pelvic cavity. The uterine tubes provide a method of transport for ova to reach the uterus from the ovaries.
Vagina
The vagina is an 8- to 10-cm muscular tube extending anteroinferiorly from the cervix of the uterus to the external vaginal orifice. The vaginal vault or fornix is the upper vaginal area surrounding the cervical os like a ring and is commonly divided into anterior and posterior fornices. The vagina is located between the bladder and the rectum and functions as a receptacle for sperm and as the lower portion of the birth canal (Figures 8.52 and 8.67 through 8.69).
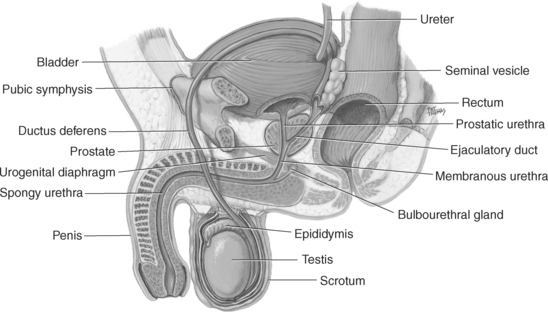
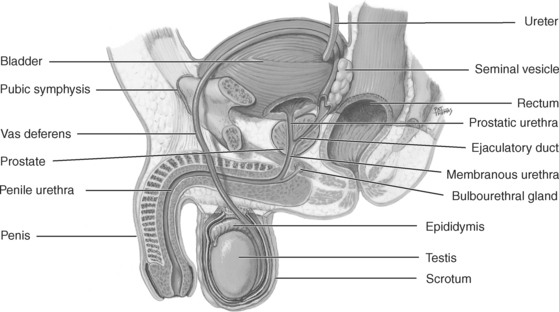
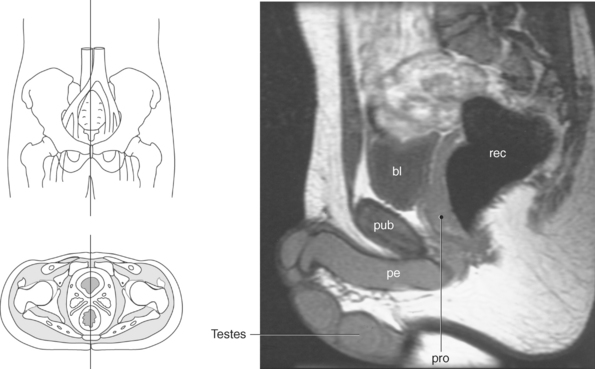
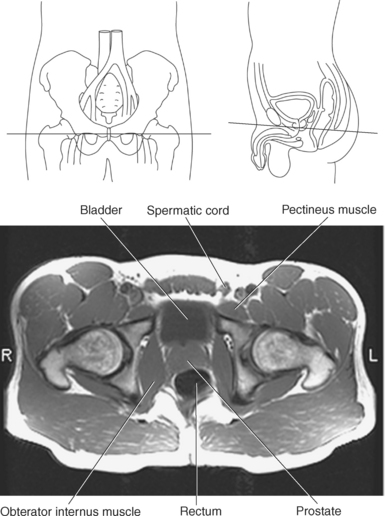
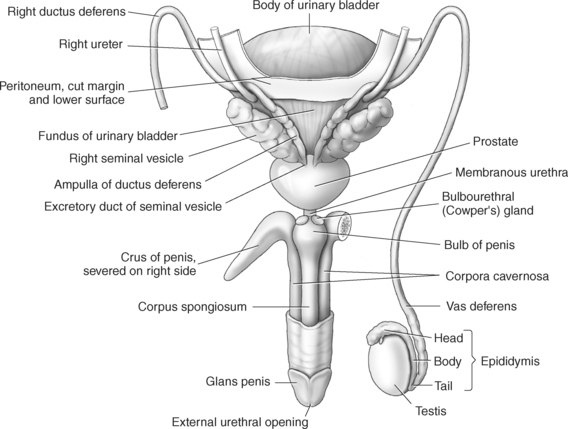
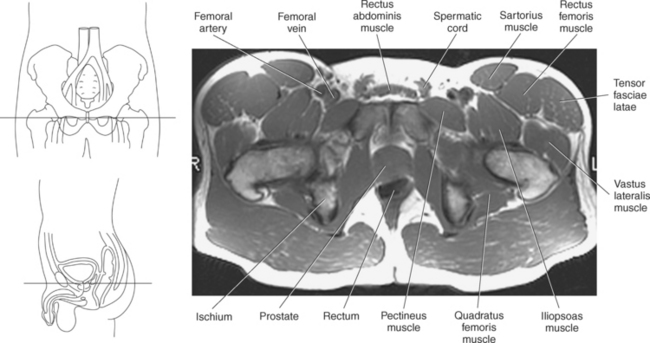
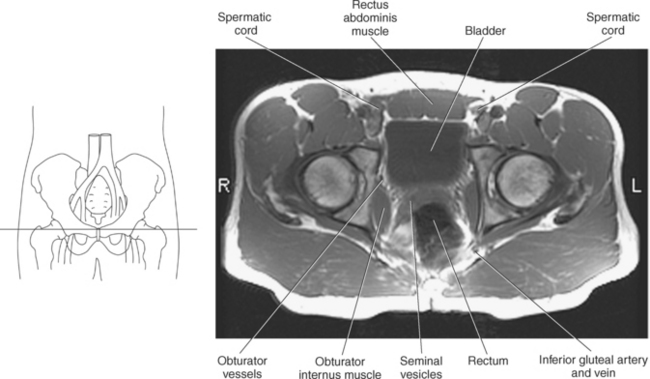
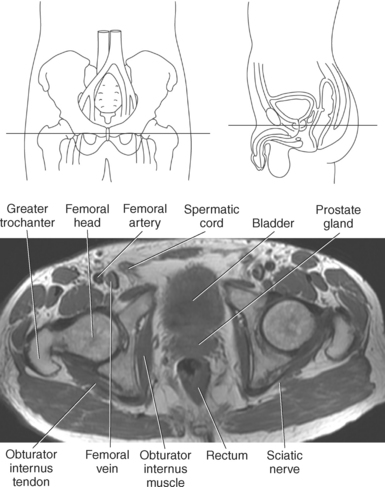
Male Reproductive Organs
The principal structures of the male reproductive system are the testis, epididymis, vas deferens, ejaculatory duct, seminal vesicle, prostate gland, bulbourethral gland, and penis. All these structures, except the testes and penis, are located within the pelvic cavity (Figures 8.70 and 8.71).
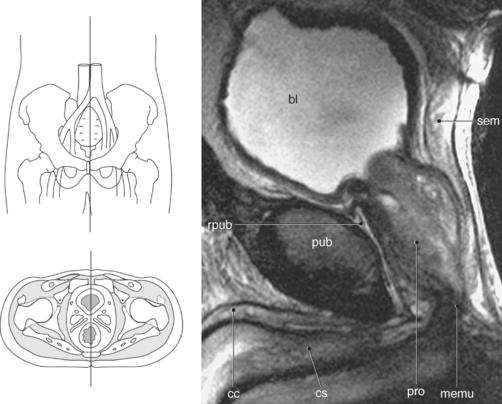
Figure 8.71 Sagittal, T2-weighted MR scan of male pelvis.
Key: bl, Bladder; sem, seminal vesicle; rpub, retropubic space; pub, pubic symphysis; cc, corpora cavernosum; cs, corpus spongiosum; pro, prostate gland; memu, membranous urethra.
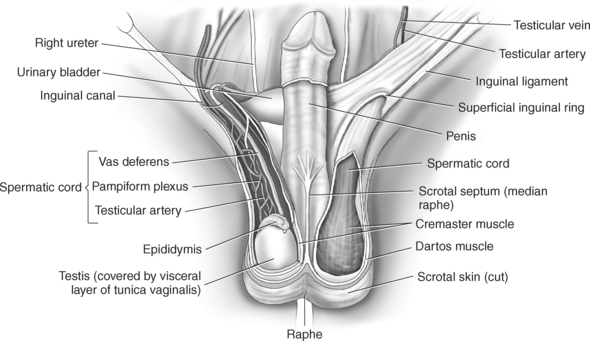
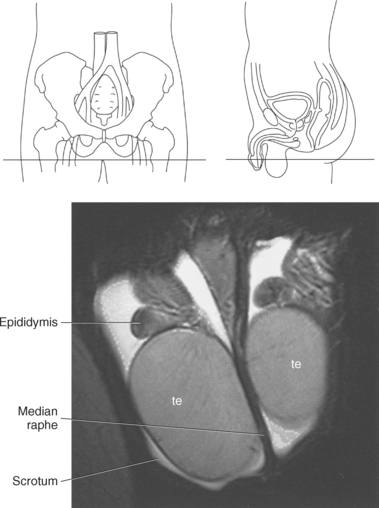
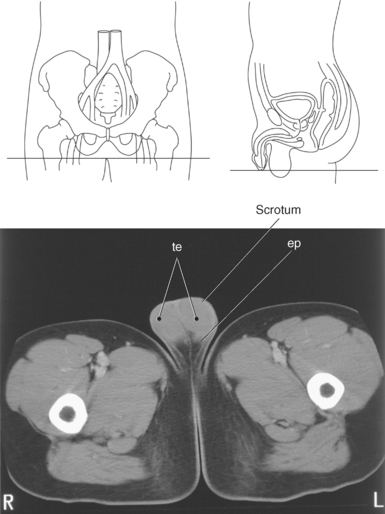
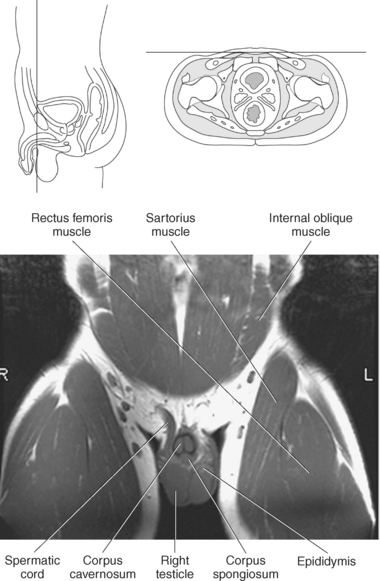
Scrotum
The scrotum is a musculotendinous pouch that encloses the testis, epididymis, and lower portions of the spermatic cord. It is composed of three fascial layers and a connective tissue layer embedded with smooth muscle fibers called the dartos tunica. Internally, the dartos tunic forms a septum that divides the scrotum into right and left compartments (median raphe), each containing a testis (Figures 8.72 and 8.73). The scrotum facilitates sperm formation by distending the testes outside the peritoneum in a cooler environment, in effect regulating the temperature of the testes. In cold temperatures the dartos tunica responds by constricting and pulling the testis closer to the body. This gives the scrotum its wrinkled appearance.
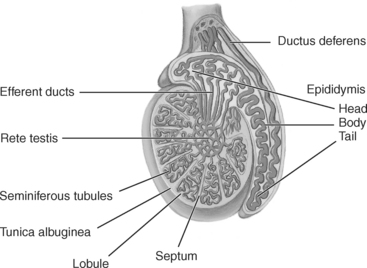
Testes and Epididymis
The paired testes are suspended in the fleshy, pouchlike scrotal sacs. Each testis is an ovoid organ that produces sperm and male sex hormones. The outer fibrous covering of the testes is the tunica albuginea, which also projects into each organ to create wedge-shaped lobules. Each testis is made up of several hundred lobules, with each lobule containing 1 to 4 seminiferous tubules, approximately 800 seminferous tubules in total. The seminiferous tubules leave their respective lobule and converge in an area called the rete testis. From here, about 15 to 20 ductules leave the rete testis to enter the head of the epididymis. The epididymis is a tightly coiled tubular structure located on the superoposterior surface of each testis. The head of the epididymis is located on the upper pole of each testis, whereas the body courses along the posterior surface to the tail, which is located under the lower pole of each testis. Sperm are transmitted from the testis to the epididymis, where they are stored as they undergo the final stages of maturation (Figures 8.70 and 8.75 through 8.78).
Vas Deferens (Ductus) and Ejaculatory Duct
As a continuation from the tail of the epididymis, the vas deferens is a long muscular tube that ascends in the posterior portion of the spermatic cord and traverses the inguinal canal, exiting at the deep inguinal ring. It then leaves the spermatic cord, passing along the lateral pelvic wall over the ureter to the posterior surface of the bladder, where it broadens and becomes the ampulla of the vas deferens. Near its proximal end it joins with the duct of the seminal vesicle to form the ejaculatory duct, which empties into the prostatic urethra. Each vas deferens, along with a testicular artery and vein, is surrounded by the tough connective tissue and muscle of the paired spermatic cords. The spermatic cords begin at the inguinal ring and exit through the inguinal ligament to descend into the scrotum (Figures 8.74 and 8.79 through 8.83).
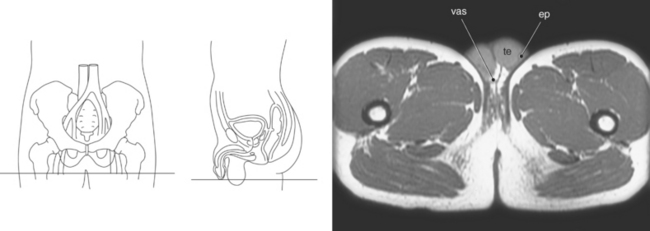
Figure 8.80 Axial, T1-weighted MR scan of pelvis with testes.
Key: vas, Vas deferens; te, testes; ep, epididymis.
Seminal Vesicles
The seminal vesicles are paired accessory glands consisting of coiled tubes that form two pouches, lateral to the vas deferens, on the posterior inferior surface of the bladder. They lie superior to the prostate gland and produce fructose and a coagulating enzyme for the seminal fluid that mixes with sperm before ejaculation (Figures 8.70, 8.79, and 8.84 through 8.88).
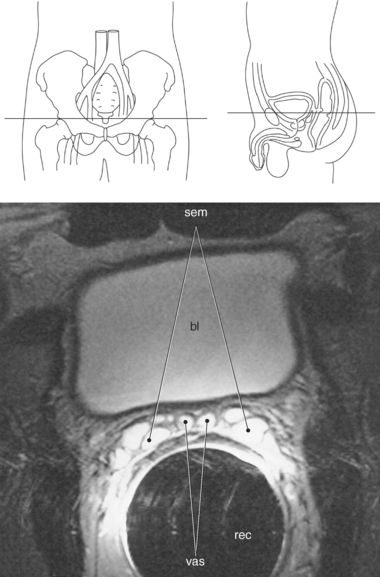
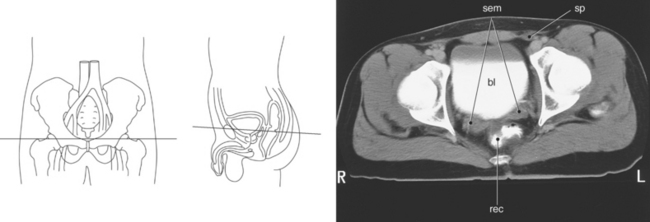
Figure 8.85 Axial, T2-weighted MR scan of male pelvis with bladder.
Key: sem, Seminal vesicle; bl, bladder; vas, vas deferens; rec, rectum.
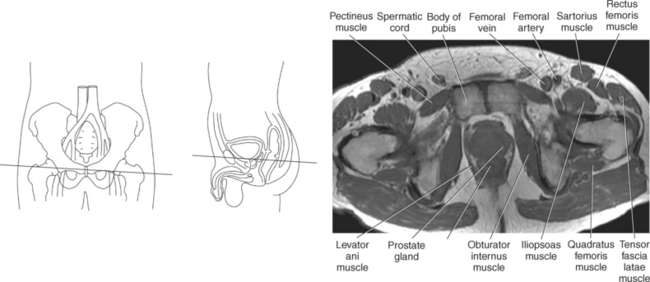
Prostate Gland
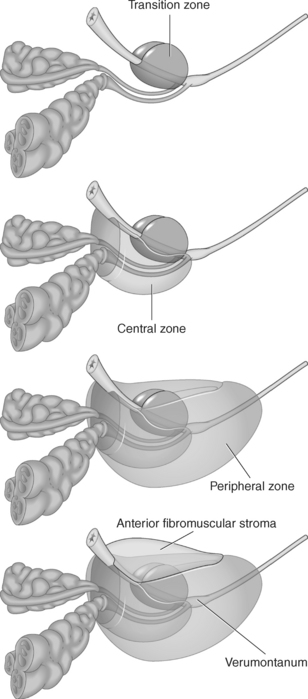
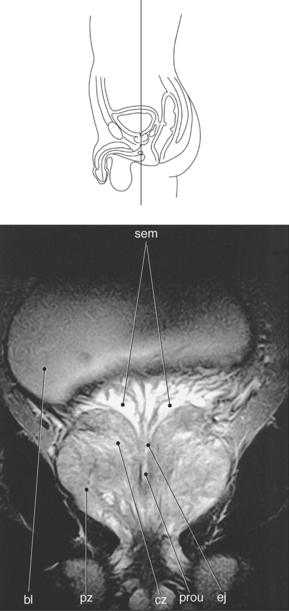
The prostate gland is the largest accessory gland of the male reproductive system. It secretes a thin, slightly alkaline fluid that forms a portion of the seminal fluid. The prostate gland is located inferior to the bladder and surrounds the prosthetic urethra, which courses through the anterior portion of the gland (Figures 8.70, 8.88, and 8.89). The prostate has a base adjacent to the neck of the bladder and an apex that is in contact with the urogenital diaphragm. The prostate gland is composed of glandular and fibromuscular tissue and surrounded by a fibrous capsule. It can be divided into two lateral lobes, a middle lobe, and an anterior fibromuscular portion. The ejaculatory ducts, which are extensions of the seminal vesicles, descend within the central zone of the gland and open into the prostatic urethra at the verumontanum. The verumontanum is a longitudinal mucosal fold that forms an elliptical segment of the prostatic urethra, marking the point where the ejaculatory ducts enter the urethra. The glandular tissue comprises two thirds of the prostate’s parenchymal tissue and in sectional imaging can be divided into zonal anatomy. The four main regions are the central, peripheral, transition, and periurethral zones (Figures 8.90 through 8.92). The central zone is located at the base of the prostate between the peripheral and transition zones and accounts for approximately 25% of the glandular tissue. It surrounds the ejaculatory ducts, then narrows to an apex at the verumontanum. The peripheral zone is the larger of the zones, comprising approximately 70% of the glandular tissue. It extends from the base to the apex along the posterior or rectal surface of the gland and surrounds the distal urethra. The peripheral zone is separated from the central and transition zones by the surgical capsule. The transition zone forms only 5% of the glandular tissue. It consists of two small lobules that are located lateral to the proximal urethra between the verumontanum and the neck of the bladder. This is the portion of the glandular tissue that enlarges due to benign prostatic hypertrophy. The periurethral zone comprises less than 1% of the glandular tissue. It is found embedded along the smooth muscular wall of the urethra. The anterior fibromuscular area is devoid of glandular tissue and is composed of fibrous and muscular elements. As it extends laterally and posteriorly, it thins to form the fibrous capsule that surrounds the prostate gland.
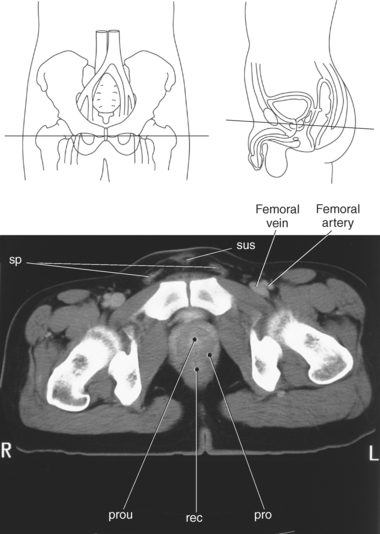
Figure 8.89 Axial CT scan of pelvis with prostate gland.
Key: sp, Spermatic cord; sus, suspensory ligament of penis; prou, prostatic urethra; rec, rectum; pro, prostate gland.
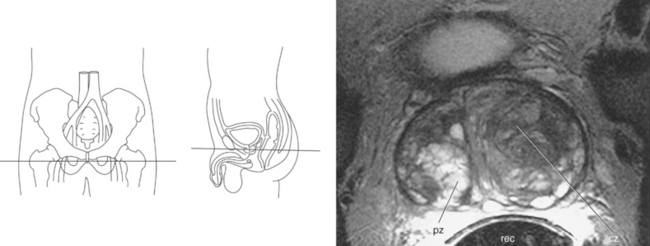
Figure 8.91 Axial, T2-weighted MR scan of pelvis with prostate gland and zones.
Key: pz, Peripheral zone; rec, rectum; cz, central zone.
Bulbourethral Glands
The two small, bulbourethral glands (Cowper’s glands) lie posterolateral to the membranous urethra, embedded in the urogenital diaphragm. These glands secrete an alkaline fluid into the membranous urethra that forms a portion of the seminal fluid (Figure 8.93).
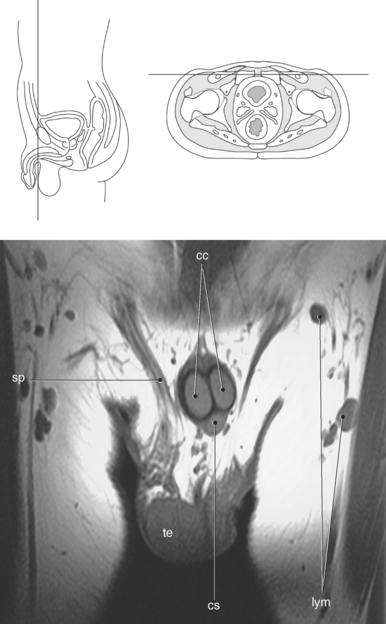
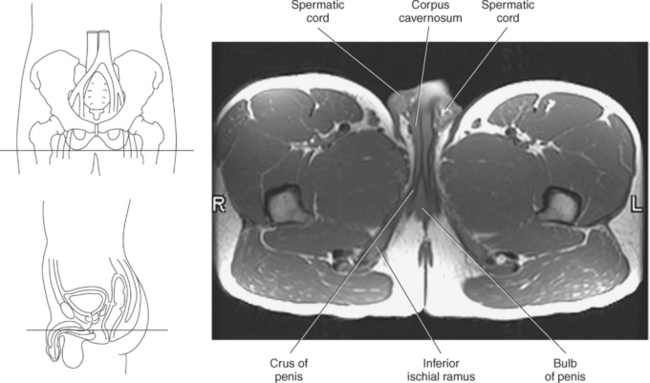
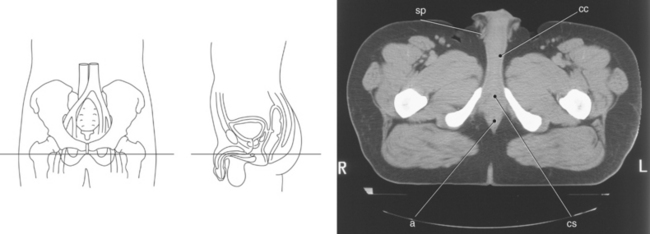
Penis
The penis, the external reproductive organ, is attached to the pubic arch via suspensory ligaments. It has two parts: the root, which is attached to the pubic arch, and the body, which remains free. Three cylindric masses of erectile tissue compose the root of the penis: two corpora cavernosa and the corpus spongiosum. The corpora cavernosa consists of a network of collagen fibers and spaces that become enlarged when filled with blood, contributing to an erection. The corpus spongiosum consists mostly of a dense venous plexus and contributes to an erection. The two corpora cavernosa form the upper surface, whereas the corpus spongiosum forms the undersurface and contains the greater part of the urethra. At the root of the penis the corpora cavernosa forms the crura, which attach along the ischiopubic ramus. The corpus spongiosum forms the bulb of the penis that is located between the two crura and is firmly attached to the inferior aspect of the urogenital diaphragm. The distal end of the cylindric masses forms the glans penis, which surrounds the external urethral meatus (Figures 8.93 through 8.97).
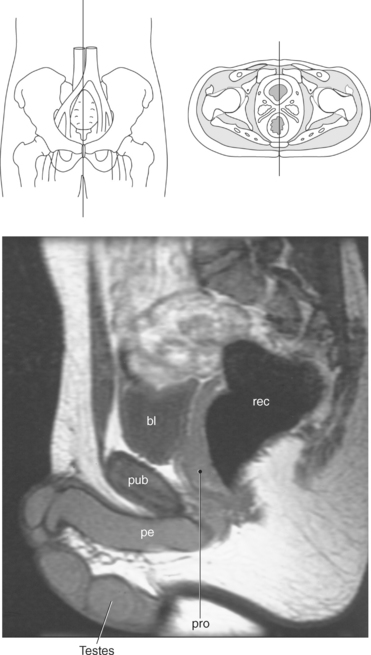
Figure 8.94 Sagittal, T2-weighted MR scan of male pelvis.
Key: bl, Bladder; rec, rectum; pub, pubic symphysis; pe, penis; pro, prostate gland.
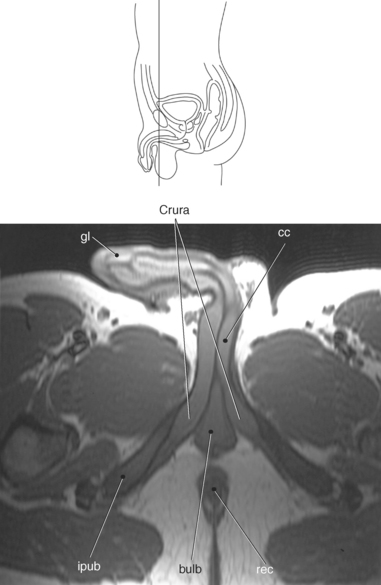
Figure 8.95 Coronal, T1-weighted MR scan of pelvis and penis.
Key: gl, glans of penis; cc, Corpora cavernosum; ipub, inferior pubic ramus; bulb, bulb of penis; rec, rectum.
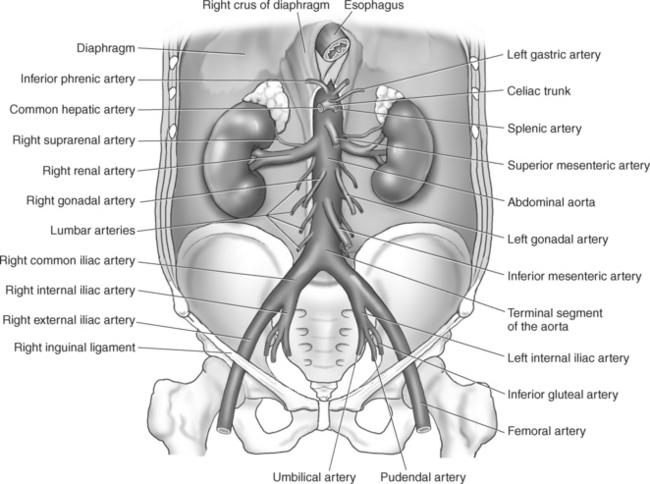
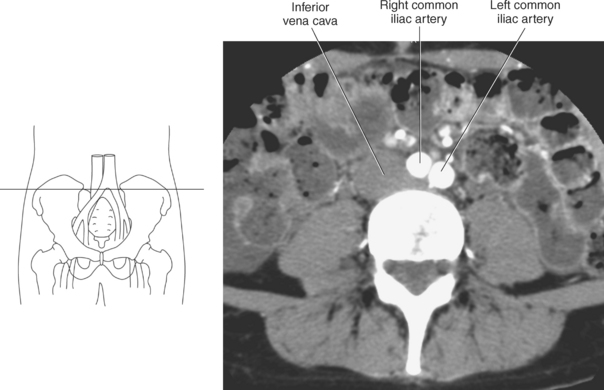
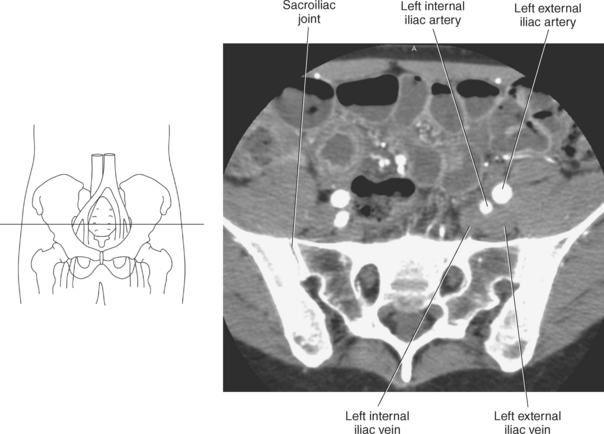
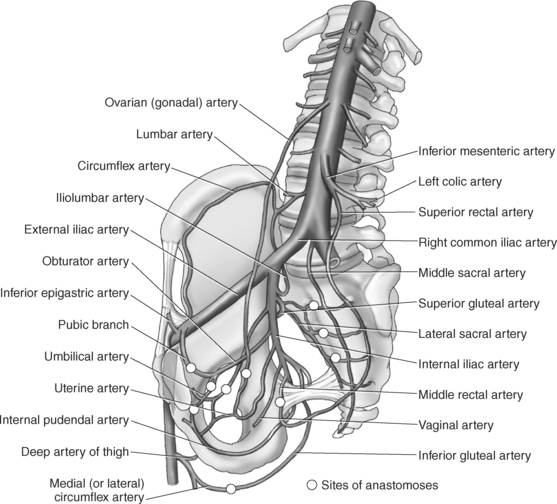
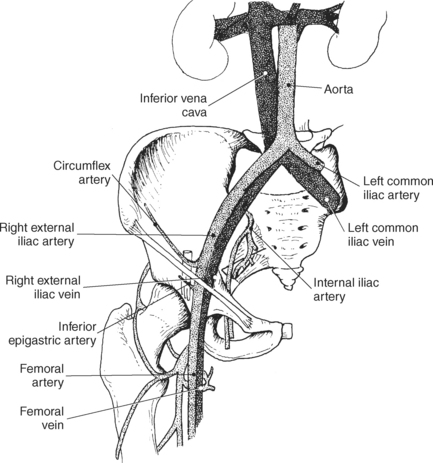
VASCULATURE
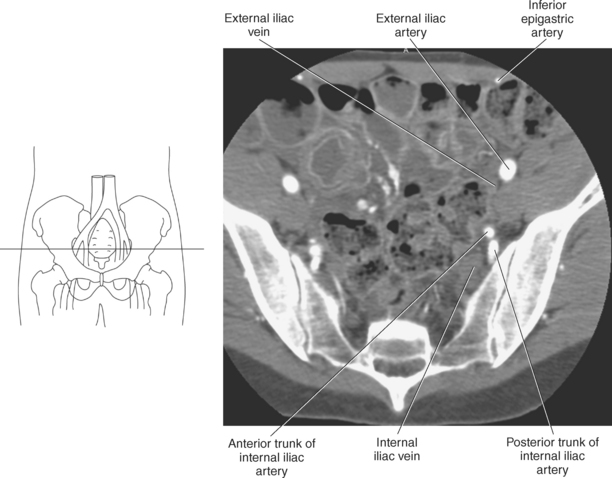
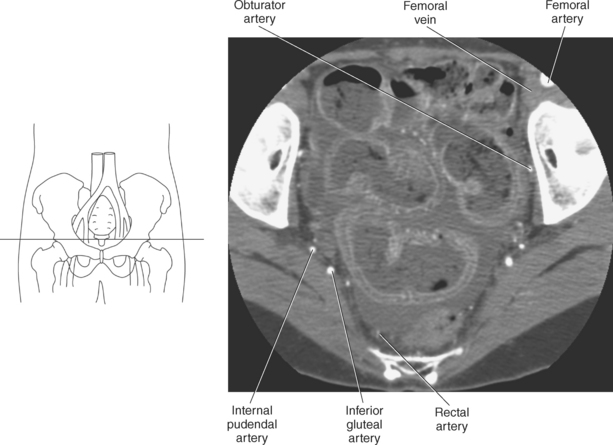
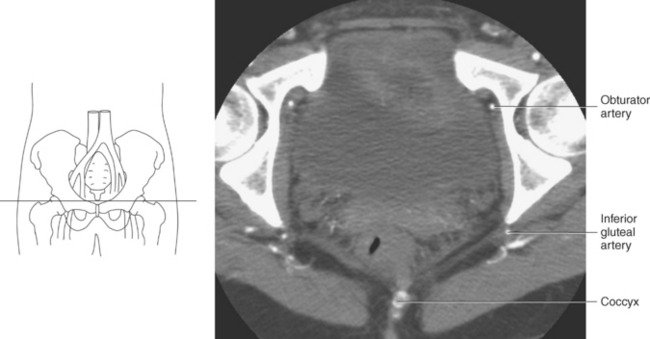
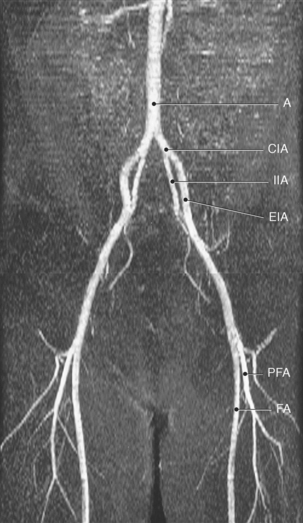
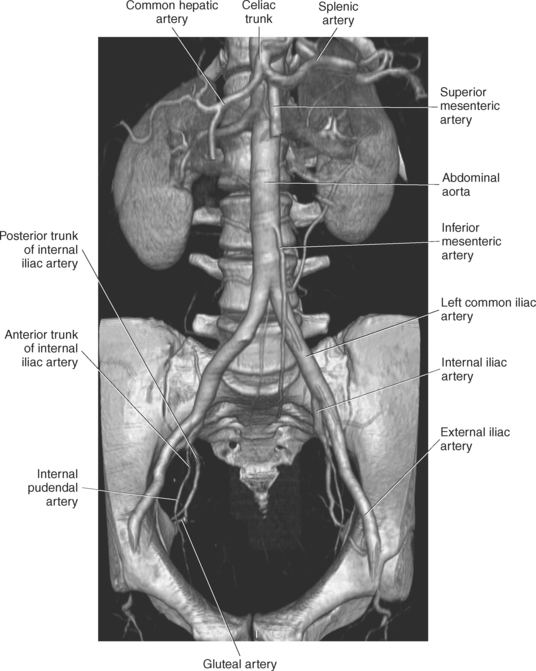
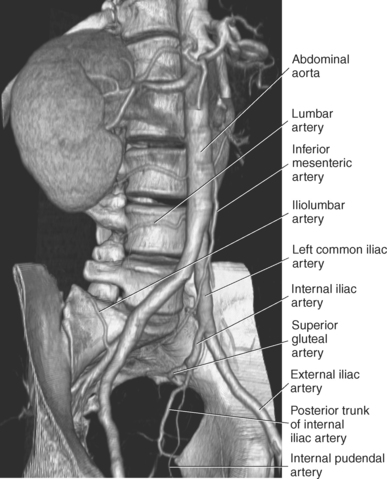
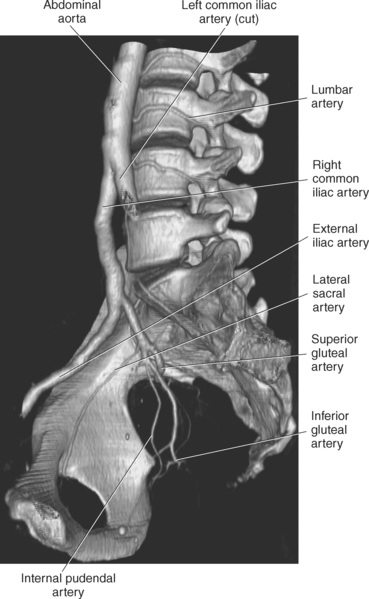
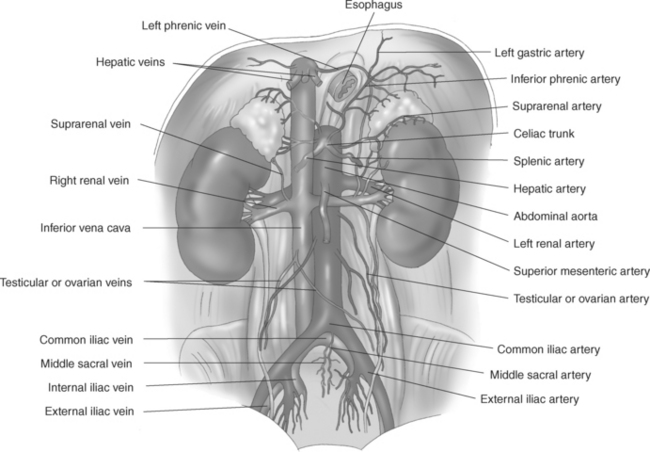
The descending aorta bifurcates at the level of the fourth lumbar vertebra into the right and left common iliac arteries (Figures 8.98 and 8.99). Each common iliac artery bifurcates at the upper margin of the sacroiliac joint into the internal and external iliac arteries (Figure 8.100). The smaller internal iliac artery extends posteromedially into the pelvis just medial to the external iliac vein and branches into an anterior trunk and a posterior trunk. The anterior trunk of the internal iliac artery supplies blood to the perineum, gluteal region, and pelvic viscera. Branches of the anterior trunk of the internal iliac artery include the obturator, umbilical, inferior vesical in males, uterine and vaginal in females, middle rectal, internal pudendal, and inferior gluteal arteries (Figure 8.101). The posterior trunk of the internal iliac artery supplies blood to the posterior and lateral walls of the pelvis, iliac crest, and gluteal region. Branches of the posterior trunk include the iliolumbar, lateral sacral, and superior gluteal arteries. The large external iliac artery does not enter the true pelvis but extends along the pelvic brim to exit the iliac fossa and course under the inguinal ligament to supply the leg. The external iliac artery becomes the femoral artery at approximately the level of the anterior superior iliac spine. Branches of the external iliac artery include the inferior epigastric artery, which supplies blood to the muscles and skin of the anterior abdominal wall, and the deep circumflex iliac artery, which supplies blood to the lateral abdominal muscles (Figures 8.102 through 8.112 and Table 8.2).
TABLE 8-2
Branches of the Internal and External Iliac Arteries
| ARTERIAL BRANCH | STRUCTURES SUPPLIED |
| Anterior Branch of Internal Iliac | |
| Obturator artery | Medial thigh |
| Umbilical artery | Superior bladder, vas deferens |
| Uterine artery | Uterus, cervix, and vagina |
| Vaginal artery | Vagina, posteroinferior bladder, pelvic part of urethra |
| Inferior vesicle artery | Prostate, seminal vesicles, and posteroinferior part of the bladder |
| Middle rectal artery | Distal end of rectum, prostate, and seminal vesicles or vagina. |
| Internal pudendal artery | Anal canal and perineum |
| Inferior gluteal artery | Muscles and skin of the buttock and posterior surface of the thigh |
| Posterior Branch of Internal Iliac | |
| Iliolumbar artery | Psoas, iliacus, quadratus lumborum, and gluteal muscles, cauda equina |
| Lateral sacral artery | Spinal meninges, roots of the sacral nerves, and muscles and skin of dorsal sacrum |
| Superior gluteal artery | Obturator internus, piriformis, and gluteus muscles |
| Branches of External Iliac Artery | |
| Inferior epigastric artery | Ascend abdomen to anastomose with internal thoracic vessels to supply the anterior abdominal wall |
| Deep circumflex iliac artery | Ascend abdomen to anastomose with internal thoracic vessels to supply the lateral aspect of the anterior abdominal wall |
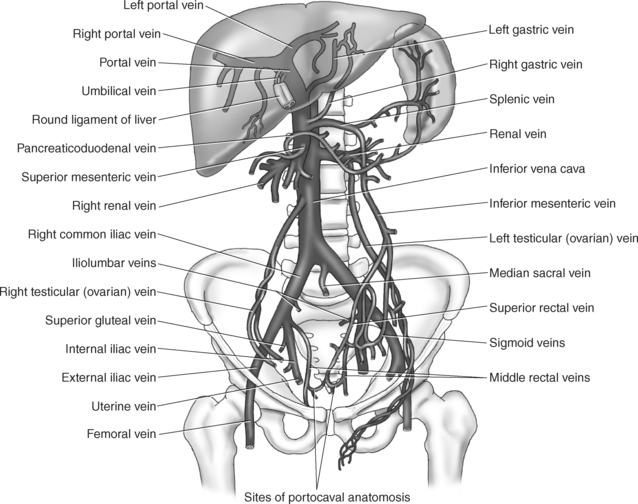
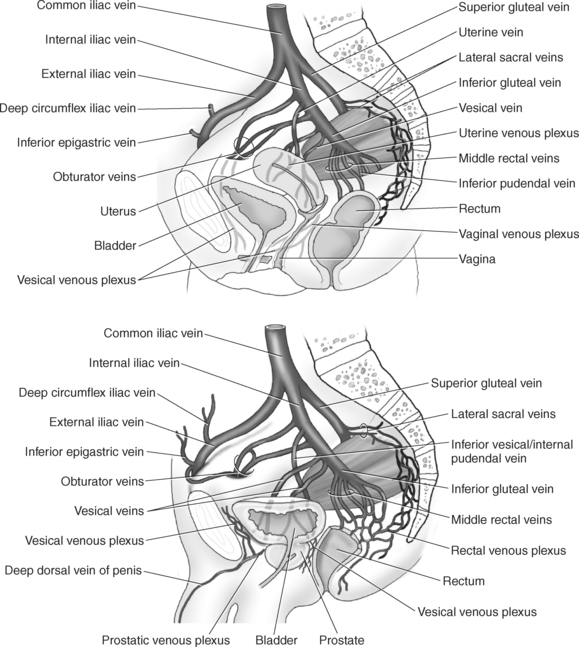
Venous Drainage
Venous drainage of the pelvis follows a pattern similar to that of the arterial supply. Mainly the internal iliac veins and their tributaries drain the pelvis (Figure 8.113). However, there is some drainage through the superior rectal, median sacral, and gonadal veins. The internal iliac vein ascends the pelvis medial to the internal iliac artery as it returns blood from the pelvic viscera. Tributaries of the internal iliac vein are similar to that of the branches of the internal iliac artery with some differences, such as the umbilical vein, which usually obliterates to form the ligamentum teres, and the iliolumbar vein that usually drains into the common iliac vein. In addition, venous plexuses are formed by the veins in the pelvis and unite to drain mainly into the internal iliac vein (Figure 8.114). These plexuses include the uterine, vaginal, prostatic, vesical, and rectal. The external iliac veins, extensions of the femoral veins, return blood from the legs. Typically, both external iliac veins course medial to their respective external iliac artery, then change to a posterior position as they ascend to join the common iliac vein at approximately the level of the sacroiliac joint. The common iliac vein arises posterior to the common iliac artery from the junction of the internal and external iliac veins. The inferior vena cava is formed at the level of L5, just a little to the right of the midline, by the union of the common iliac veins. From this level it continues to ascend the abdomen to the right of the abdominal aorta (Figures 8.99, 8.100, and 8.102 through 8.107).
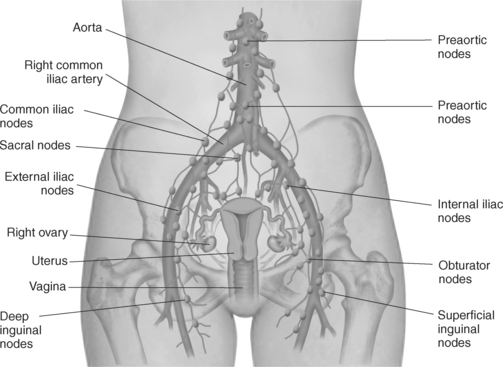
LYMPH NODES
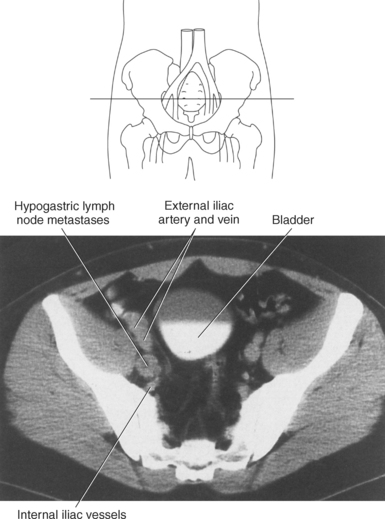
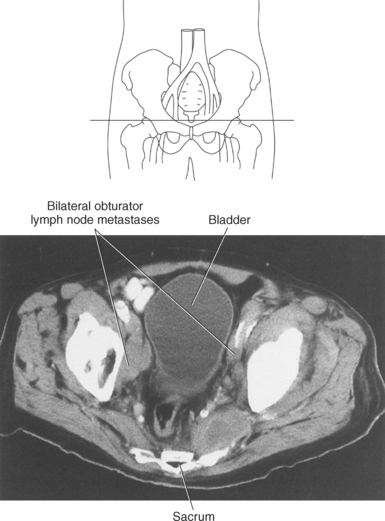
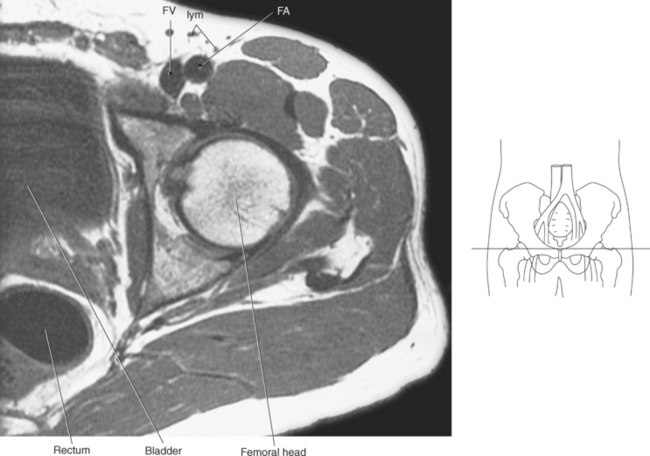
Pelvic lymph nodes include nodal chains or groups that accompany their corresponding vessels and inguinal nodal groups. Those nodal groups that correspond to pelvic vessels include the common iliac, internal iliac, external iliac, and sacral nodal groups (Figure 8.115). The common iliac lymph nodes form two groups along the surface of the common iliac artery: a lateral group and a median group. The lateral common iliac group receives lymph from the lower limb and pelvis via the external and internal iliac lymph nodes. The median common iliac group receives lymph directly from the pelvic viscera and indirectly through the internal iliac and sacral lymph nodes. The obturator nodes that course along the midportion of the obturator internus muscle are included in the medial common iliac group. The external iliac lymph nodes lie on the external iliac vessels and drain lymph from the lower limb, abdominal wall, bladder, and prostate in males or uterus and vagina in females. The internal iliac lymph nodes surround the internal iliac vessels and their branches. They receive lymph from all the pelvic viscera, deep parts of the perineum, and gluteal and thigh regions. Sacral lymph nodes lie along the median and lateral sacral arteries. They receive lymph from the posterior pelvic wall, rectum, neck of the bladder, and prostate or cervix. The inguinal lymph nodes drain lymph from the lower limb, perineum, anterior abdominal wall as far superiorly as the umbilicus, gluteal region, and parts of the anal canal. They can be divided into the superficial inguinal lymph nodes that are situated distal to the inguinal ligament in the subcutaneous tissue anterior and medial to common femoral vessels. The deep inguinal lymph nodes are fewer in number and are situated medial to the femoral vessels at the approximate level of the ischial tuberosity. Pelvic lymph nodes are considered pathologically enlarged when they exceed 10 mm in the short axis (Figures 8.116 through 8.118).