Diagnostic Imaging of the Temporomandibular Joint
Disorders of the temporomandibular joint are abnormalities that interfere with the normal form or function of the joint. These disorders include dysfunction of the articular disk and associated ligaments and muscles, joint arthritides, inflammatory lesions, neoplasms, and growth or developmental abnormalities.
Clinical Features
Temporomandibular joint (TMJ) dysfunction is the most common jaw disorder, with 28% to 86% of adults and adolescents showing one or more clinical signs or symptoms. A higher incidence of the disorder has been reported in females, although the reason for this preponderance is not clear. Signs and symptoms of dysfunction may include one or more of the following: pain in the TMJ or ear or both, headache, muscle tenderness, joint stiffness, clicking or other joint noises, reduced range of motion, locking, and subluxation. In most cases the clinical signs and symptoms are transitory, and treatment is not indicated. A small group of patients (5%) has severe dysfunction (e.g., severe pain, marked functional impairment, or both), which requires a thorough diagnostic workup, including diagnostic imaging, before treatment is begun.
The clinical signs and symptoms of other disorders of the TMJ may include swelling in and around the joint, an elevated temperature, and redness of the overlying skin.
Application of Diagnostic Imaging
TMJ imaging may be necessary to supplement information obtained from the clinical examination, particularly when an osseous abnormality or infection is suspected, conservative treatment has failed, or symptoms are worsening. Diagnostic imaging also should be considered for patients with a history of trauma, significant dysfunction, alteration in range of motion, sensory or motor abnormalities, or significant changes in occlusion. TMJ imaging is not indicated for joint sounds if other signs or symptoms are absent or for asymptomatic children and adolescents before orthodontic treatment. The purposes of TMJ imaging are to evaluate the integrity and relationships of the hard and soft tissues, confirm the extent or stage of progression of known disease, and evaluate the effects of treatment. The clinician must correlate the radiographic information with the patient’s history and clinical findings to arrive at a final diagnosis and plan the management of the underlying disease process.
Radiographic Anatomy of the Temporomandibular Joint
A thorough understanding of the anatomy and morphology of the TMJ is essential so that a normal variant is not mistaken for an abnormality. The TMJs are unique in that, although they constitute two separate joints anatomically, they function together as a single unit. Each condyle articulates with the mandibular fossa of the temporal bone. A disk composed of fibrocartilage is interposed between the condyle and mandibular fossa. A fibrous capsule lined with synovial membrane surrounds and encloses the joint. Ligaments and muscles restrict or allow movement of the condyle.
CONDYLE
The condyle is a bony ellipsoid structure connected to the mandibular ramus by a narrow neck (Fig. 26-1). The condyle is approximately 20 mm long mediolaterally and 8 to 10 mm thick anteroposteriorly. The shape of the condyle varies considerably; the superior aspect may be flattened, rounded, or markedly convex, whereas the mediolateral contour usually is slightly convex. These variations in shape may cause difficulty with radiographic interpretation; this underlines the importance of understanding the range of normal appearance. The extreme aspects of the condyle are called the medial pole and lateral pole. The long axis of the condyle is slightly rotated on the condylar neck so that the medial pole is angled posteriorly, forming an angle of 15 to 33 degrees with the sagittal plane. The two condylar axes typically intersect near the anterior border of the foramen magnum in the axial or horizontal plane of the skull.

FIG. 26-1 Mandibular Condyle.
The medial pole (arrow) is on the right in each case. A, Anterior aspect. B, Superior aspect.
Most condyles have a pronounced ridge oriented mediolaterally on the anterior surface, marking the anteroinferior limit of the articulating area. This ridge is the upper limit of the pterygoid fovea, a small depression on the anterior surface at the junction of the condyle and neck. It is the attachment site of the superior head of the lateral pterygoid muscle and should not be mistaken for an osteophyte (spur), which indicates degenerative joint disease.
Although the mandibular and temporal components of the TMJ are calcified by 6 months of age, complete calcification of cortical borders may not be completed until 20 years of age. As a result, radiographs of condyles in children may show little or no evidence of a cortical border. In the absence of disease, the cortical borders in adults are visible radiographically. A layer of fibrocartilage covers the condyle but is not visible radiographically.
MANDIBULAR FOSSA
The glenoid (mandibular) fossa, located at the inferior aspect of the squamous part of the temporal bone, is composed of the glenoid fossa and articular eminence of the temporal bone (Fig. 26-2). It is sometimes described as the temporal component of the TMJ. The articular eminence forms the anterior limit of the glenoid fossa and is convex in shape. Its most inferior aspect is called the summit or apex of the eminence. In a normal TMJ, the roof of the fossa, the posterior slope of the articular eminence, and the eminence itself form an S shape when viewed in the sagittal plane. The most lateral aspect of the eminence consists of a protuberance, called the articular tubercle, which is a ligamentous attachment. The squamotympanic fissure and its medial extension, the petrotympanic fissure, form the posterior limit of the fossa. The middle portion of the roof of the fossa forms a small portion of the floor of the middle cranial fossa, and only a thin layer of cortical bone separates the joint cavity from the intracranial subdural space. The spine of the sphenoid forms the medial limit of the fossa. Fossa depth varies, and the development of the articular eminence relies on functional stimulus from the condyle. For example, the mandibular fossa is very flat and underdeveloped in patients with micrognathia or condylar agenesis. The fossa and articular eminence develop during the first 3 years and reach mature shape by the age of 4 years; young infants lack a definite fossa and articular eminence (Fig. 26-3).
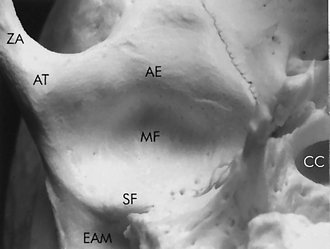
FIG. 26-2 Basal view of the skull showing the mandibular fossa. AE, Articular eminence; AT, articular tubercle; CC, carotid canal; EAM, external auditory meatus; MF, mandibular fossa; SF, squamotympanic fissure; ZA, zygomatic arch.
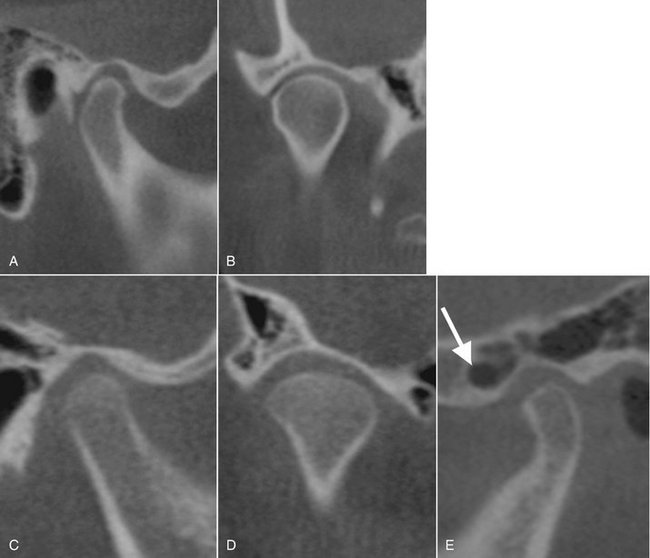
FIG. 26-3 Sagittal reformat (A) and coronal reformat (B) cone-beam computed tomographic images of the right temporomandibular joint (TMJ) in an adult. Note the thick regular cortication of all articulating surfaces and development of the glenoid fossa and articular eminence. Sagittal reformat (C) and coronal reformat (D) cone-beam computed tomographic images of the right TMJ in a 7-year-old child. Note the thin cortication of the articulating surfaces, shallow glenoid fossa, and short articular eminence. E, Sagittal reformat cone-beam computed tomographic image of the left TMJ (adult) showing pneumatization of the temporal component including the articular eminence (arrow) with mastoid air cells.
All aspects of the temporal component may be pneumatized with small air cells derived from the mastoid air cell complex (see Fig. 26-3, E). Pneumatization of the articular eminence is seen radiographically in approximately 2% of patients. Like the condyle, the mandibular fossa is covered with a thin layer of fibrocartilage.
INTERARTICULAR DISK
The interarticular disk (meniscus), composed of fibrous connective tissue, is located between the condylar head and mandibular fossa. The disk divides the joint cavity into two compartments, called the inferior (lower) and superior (upper) joint spaces, which are located below and above the disk, respectively (Fig. 26-4). A normal disk has a biconcave shape with a thick anterior band, thicker posterior band, and a thin middle part. The disk also is thicker medially than laterally. The medial and lateral margins of the disk blend with the capsule. The thin central portion normally serves as an articulating cushion between the condyle and articular eminence. The anterior band is thought to be attached to the superior head of the lateral pterygoid muscle, and the posterior band attaches to the posterior retrodiskal tissues (also called the posterior attachment). The junction between the posterior band and posterior attachment usually lies within 10 degrees of vertical above the condylar head. The disk and posterior attachment are collectively called the soft tissue components of the TMJ.
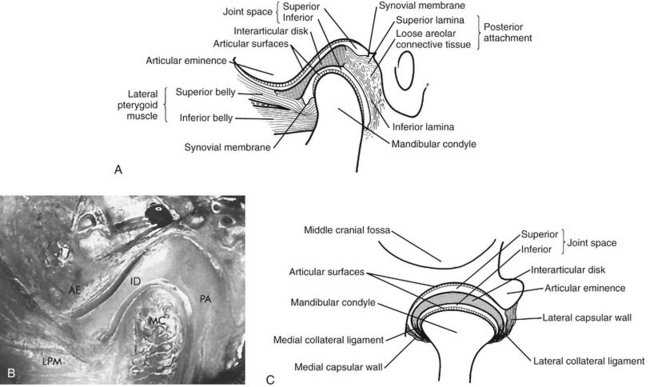
FIG. 26-4 Temporomandibular Joint Anatomy.
A, Lateral view. B, Sectioned cadaver specimen in the same orientation. AE, Articular eminence; ID, interarticular disk; LPM, lateral pterygoid muscle; MC, mandibular condyle; PA, posterior attachment. C, Coronal view. (Courtesy Dr. W.K. Solberg, Los Angeles, Calif.)
During mandibular opening, as the condyle rotates and translates downward and forward, the disk also moves forward and rotates so that its thin central portion remains between the articulating convexities of the condylar head and articular eminence. At maximum opening, the condyle is usually positioned beneath the anterior band of the disk. Laterally and medially the disk attaches to the condylar poles, helping to ensure passive movement of the disk with the condyle so that the condyle and disk translate forward together to the summit of the articular eminence. As the mandible opens, the condyle also rotates against the lower surface of the disk in the inferior joint space. On mandibular closing, this process reverses, with the disk moving back with the condyle into the mandibular fossa.
POSTERIOR ATTACHMENT (RETRODISKAL TISSUES)
The posterior attachment consists of a bilaminar zone of vascularized and innervated loose fibroelastic tissue. The superior lamina, which is rich in elastin, inserts into the posterior wall of the mandibular fossa. The superior lamina stretches and allows the disk to move forward with condylar translation. The inferior lamina attaches to the posterior surface of the condyle. The posterior attachment is covered with a synovial membrane that secretes synovial fluid, which lubricates the joint. As the condyle moves forward, tissues of the posterior attachment expand in volume, primarily as a result of venous distention, and as the disk moves forward, tension is produced in the elastic posterior attachment. This tension is thought to be responsible for the smooth recoil of the disk posteriorly as the mandible closes.
TEMPOROMANDIBULAR JOINT BONY RELATIONSHIPS
Radiographic joint space is a general term used to describe the radiolucent area between the condyle and temporal component (see Fig. 26-4). This general term should not be confused with the terms superior joint space and inferior joint space described earlier, which refer to soft tissue spaces above and below the disk. The radiographic joint space contains the soft tissue components of the joint. The left and right condylar positions within the fossa can be determined and compared by the dimensions of the radiographic joint space viewed on corrected lateral images. A condyle is positioned concentrically when the anterior and posterior aspects of the radiolucent joint space are uniform in width. The condyle is retruded when the posterior joint space width is less than the anterior and protruded when the posterior joint space is wider than the anterior. However, because the radiographic outline of the glenoid fossa and the condyle do not match like a smooth ball-and-socket joint, the joint space often varies from medial to lateral aspects of the joint (Fig. 26-5).
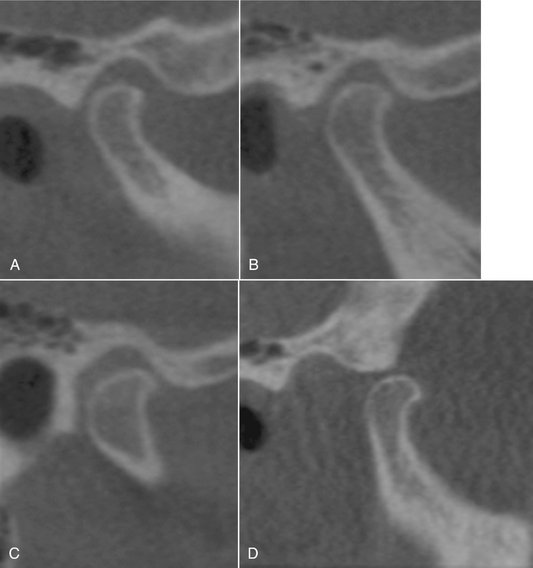
FIG. 26-5 Sagittal Reformat Cone-Beam Computed Tomographic Image.
A to C, Closed position. A, Lateral image slice. B, Central image slice. C, Medial image slice of the same joint. Notice that the condyle appears retruded in the lateral slice, centered in the central slice, and anteriorly positioned in the medial slice. D, Open view showing the degree of condyle translation during mandibular opening.
The diagnostic significance of mild or moderate condylar eccentricity is not clear; condylar eccentricity is seen in one third to one half of asymptomatic individuals and is not a reliable indicator of the soft tissue status of the joint, particularly because the shape of the condylar head is not concentric to the shape of the fossa. Markedly eccentric condylar positioning usually represents an abnormality. For example, inferior condylar positioning (widened joint space) may be seen in cases involving fluid or blood within the joint, and superior condylar positioning (decreased joint space or no joint space, with osseous contact of joint components) may indicate loss, displacement, or perforation of intracapsular soft tissue components. Marked posterior condylar positioning is seen in some cases of disk displacement, and marked anterior condylar positioning may be seen in juvenile rheumatoid arthritis.
CONDYLAR MOVEMENT
The condyle undergoes complex movement during mandibular opening. Downward and forward translation (sliding) of the condyle occurs where the superior surface of the disk slides against the articular eminence; at the same time a hingelike, rotatory movement occurs with the superior surface of the condyle against the inferior surface of the disk. The extent of normal condylar translation varies considerably. In most individuals, at maximal opening the condyle moves down and forward to the summit of the articular eminence or slightly anterior to it (see Fig. 26-5). The condyle typically is found within a range of 2 to 5 mm posterior and 5 to 8 mm anterior to the crest of the eminence. Reduced condylar translation, in which the condyle has little or no downward and forward movement and does not leave the mandibular fossa, is seen in patients who clinically have a reduced degree of mouth opening. Hypermobility of the joint may be suspected if the condyle translates more than 5 mm anterior to the eminence. This may permit anterior locking or dislocation of the condyle if a superior movement also occurs above and anterior to the summit of the articular eminence.
Diagnostic Imaging of the Temporomandibular Joint
The type of imaging technique selected depends on the specific clinical problem, whether imaging of hard or soft tissues is desired, the amount of diagnostic information available from a particular imaging modality, the cost of the examination, and the radiation dose. Both joints should be imaged during the examination, for comparison. When selecting the imaging modality the strengths and weakness of each imaging modality should be considered. The following not only outlines the imaging modalities that can be applied but also the best modalities for displaying osseous or soft tissue structures.
OSSEOUS STRUCTURES
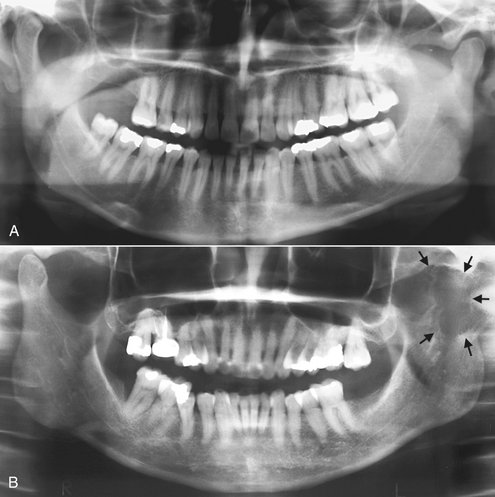
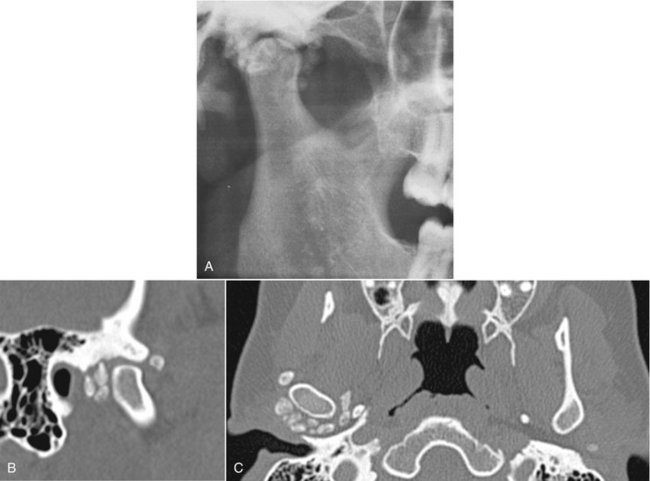
The panoramic projection is often included as part of the examination because it provides an overall view of the teeth and jaws, provides a means of comparing left and right sides of the mandible, and serves as a screening projection to identify odontogenic diseases and other disorders that may be the source of TMJ symptoms. Some panoramic machines have specific TMJ programs, but these are of limited usefulness because of thick image layers and the oblique, distorted view of the joint they provide, which severely limits image quality. Gross osseous changes in the condyles may be identified, such as asymmetries, extensive erosions, large osteophytes, tumors or fractures (Fig. 26-6). However, no information about condylar position or function is provided because the mandible is partly opened and protruded when this radiograph is exposed. Also, mild osseous changes may be obscured, and only marked changes in articular eminence morphology can be seen as a result of superimposition by the skull base and zygomatic arch. For these reasons, the panoramic view should not be used as the sole imaging modality and should be supplemented.
Plain Film Imaging Modalities
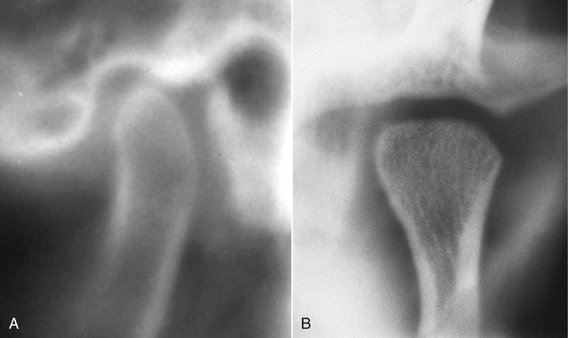
Plain films, usually consisting of a combination of transcranial, transpharyngeal (Parma), transorbital, and submentovertex (basal) projections allow visualization of the TMJs in various planes (Fig. 26-7). Transcranial and transpharyngeal projections provide lateral views. The transcranial view is taken in the closed and open mouth positions and depicts the lateral aspect of the TMJ, whereas the transpharyngeal projection is taken in the mouth open position only and depicts the medial aspect of the condyle. The transorbital projection is taken in the open or protruded position and depicts the entire medial-lateral aspect of the condyle in the frontal plane and is very useful in detecting condylar neck fractures. A submentovertex projection provides a view of the skull base and condyles in the horizontal plane; it is often used to determine the angulation of the long axes of the condylar heads for corrected tomography. These imaging techniques are gradually being replaced with more advanced imaging such as cone-beam computed tomography (CT).
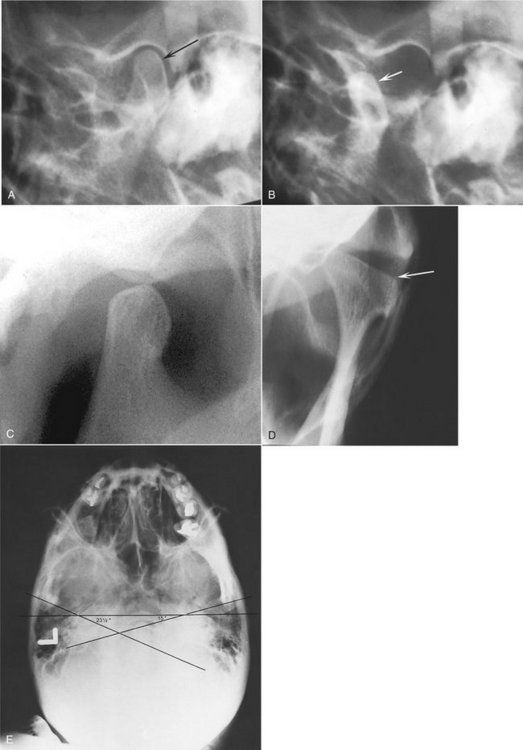
FIG. 26-7 A and B, Transcranial projections providing a profile of the lateral aspect of the condylar head (arrow) in the closed view and the degree of translatory movement (arrow) in the open view. C, An example of a transpharyngeal projection showing a medial profile of the condyle. D, An example of a transorbital projection showing a frontal view of the condyle. The lateral pole is indicated with an arrow. This submentovertex projection (E) shows the measurement of the angle of the long axis of the condylar heads used for tomography.
Conventional Tomography
Tomography is a radiographic technique that produces multiple thin image slices, permitting visualization of the osseous structures essentially free of superimpositions of overlapping structures (see Chapter 14). This technique can provide multiple image slices at right angles through the joint, depicting true condylar position and revealing osseous changes. Conventional tomography is gradually being replaced by cone-beam CT (CBCT) as the imaging technique of choice for assessing the osseous structures of the TMJ. Tomographs typically are exposed in the sagittal (lateral) plane, corrected to the condylar long axis, with several image slices in the closed (maximal intercuspation) position and usually only one image in the maximal open position. It is desirable to supplement the sagittal images with coronal (frontal) tomographs (Fig. 26-8), particularly when morphologic abnormalities or erosive changes of the condylar head are suspected. The entire condylar head is visible in the mediolateral plane.
Computed Tomography
CT provides more information about the three-dimensional shape and internal structure of the osseous components of the joint by providing detailed image slices and three-dimensional images. There are two CT devices available, conventional CT (sometimes referred to as medical CT, see Chapter 14) and CBCT. Both modalities can give excellent images of the osseous structures, but only conventional CT provides images of the surrounding soft tissues; however, this is only required in a minimal number of specific situations. CBCT has the advantage of reduced patient dose compared with medical CT and is likely to replace conventional tomography. In CBCT the patient is usually scanned in the closed position and low-resolution scans can be done in the open or other positions (see Chapter 13). Data from the axial slices can be manipulated to produce (reformat) corrected lateral and frontal images of the TMJs (see Fig. 26-3). Panoramic and three-dimensional reformatted images also can be produced. These are useful for assessing osseous deformities of the jaws or surrounding structures. Conventional and CBCT cannot produce accurate images of the articular disk.
CT is also useful for determining the presence and extent of ankylosis and neoplasms and the degree of bone involvement in some arthritides, for imaging complex fractures, and for evaluating complications from the use of polytetrafluoroethylene or silicon sheet implants, such as erosions into the middle cranial fossa and heterotopic bone growth.
SOFT TISSUE STRUCTURES
Soft tissue imaging is indicated when TMJ pain and dysfunction are present and when the clinical findings suggest disk displacement along with symptoms that are unresponsive to conservative therapy. Imaging should be prescribed only when the anticipated results are expected to influence the treatment plan. Historically, arthrography was the first imaging modality used to image the soft tissues of the joint.
Arthrography is a technique in which an indirect image of the disk is obtained by injecting a radiopaque contrast agent into the joint spaces under fluoroscopic guidance. Magnetic resonance imaging (MRI) has replaced arthrography and is now the imaging technique of choice for the soft tissues of the TMJ. MRI can not only display the articular disk but also the surrounding soft tissue structures and also can reveal the presence of joint effusion. MRI displays the osseous structures of the TMJ but not in the comparable detail seen in CT imaging. The technique is noninvasive and does not use ionizing radiation.
Magnetic Resonance Imaging
MRI uses a magnetic field and radiofrequency pulses rather than ionizing radiation to produce multiple digital image slices (see Chapter 14). Because MRI can provide superb images of soft tissues, this technique can be used for imaging the articular disk. MRI allows construction of images in the sagittal and coronal planes without repositioning the patient (Fig. 26-9). These images usually are acquired in open and closed mandibular positions with use of surface coils to improve image resolution. Sagittal slices should be oriented perpendicular to the condylar long axis. The examinations usually are performed with use of T1-weighted, proton-weighted, or T2-weighted pulse sequences. T1-weighted and proton-weighted images best demonstrate osseous and diskal tissues, whereas T2-weighted images demonstrate inflammation and joint effusion. Motion MRI studies during opening and closing can be obtained by having the patient open in a series of stepped distances and with use of rapid image acquisition (“fast scan”) techniques.
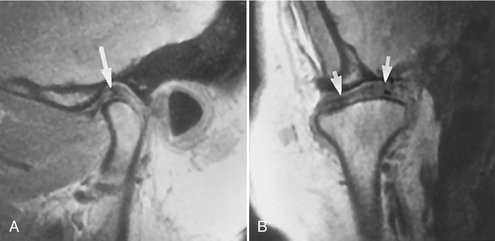
FIG. 26-9 MRI of a Normal Temporomandibular Joint.
A, Closed sagittal view showing the condyle and temporal component. The biconcave disk is located with its posterior band (arrow) over the condyle. B, Closed coronal view showing the osseous components and disk (arrows) superior to the condyle. (Courtesy Dr. Per-Lennart Westesson, Rochester, N.Y.)
MRI is contraindicated in patients who are pregnant or who have pacemakers, intracranial vascular clips, or metal particles in vital structures. Some patients may not be able to tolerate the procedure because of claustrophobia or an inability to remain motionless.
Radiographic Abnormalities of the Temporomandibular Joint
Developmental abnormalities may be broadly categorized as anomalies in the form and size of joint components. The most striking radiographic changes usually are seen in the condyle, although the temporal component also may be deformed, often remodeling to accommodate the abnormal condyle. Condylar articular cartilage is a mandibular growth site, and, as a result, developmental abnormalities at this location may manifest as altered growth on the affected side of the condyle, mandibular ramus, mandibular body, and alveolar process on the affected side(s).
Definition
Condylar hyperplasia is a developmental abnormality that results in enlargement and occasionally deformity of the condylar head; this may have a secondary effect on the mandibular fossa as it remodels to accommodate the abnormal condyle. Some proposed etiologic factors include hormonal influences, trauma, infection, heredity, intrauterine factors, and hypervascularity. The mechanism may be overactive cartilage or persistent cartilaginous rests, which increases the thickness of the entire cartilaginous and precartilaginous layers. This condition usually is unilateral and may be accompanied by varying degrees of hyperplasia of the ipsilateral mandible.
Clinical Features
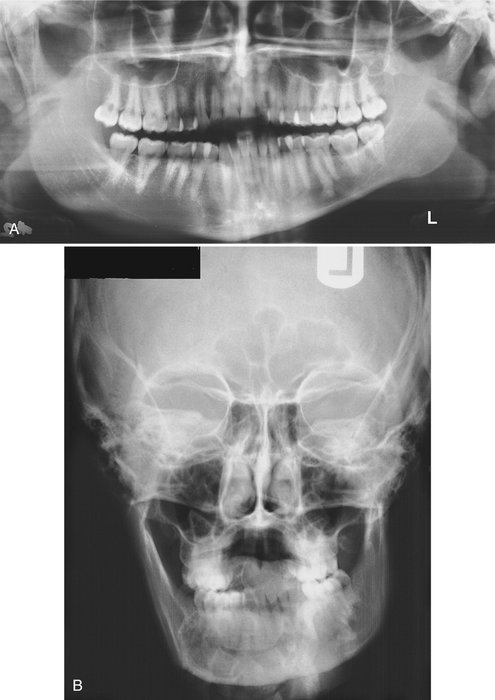
Condylar hyperplasia is more common in males, and it usually is discovered before the age of 20 years. The condition is self-limiting and tends to arrest with termination of skeletal growth, although in a small number of cases continued growth and adult onset have been reported. The condition may progress slowly or rapidly. Patients have a mandibular asymmetry that varies in severity, depending on the degree of condylar enlargement. The chin may be deviated to the unaffected side, or it may remain unchanged but with an increase in the vertical dimension of the ramus, mandibular body, or alveolar process of the affected side. As a result of this growth pattern, patients may have a posterior open bite on the affected side. Patients may also have symptoms related to TMJ dysfunction and may complain of limited or deviated mandibular opening, or both, caused by restricted mobility of the enlarged condyle.
Radiographic Features
The condyle may appear relatively normal but symmetrically enlarged, or it may be altered in shape (e.g., conical, spherical, elongated, lobulated) or irregular in outline. It may be more radiopaque because of the additional bone present. A morphologic variation manifesting as elongation of the condylar head and neck with a compensating forward bend, forming an inverted L, may be seen. Also, the condylar neck may be elongated and thickened and may bend laterally when viewed in the coronal (anteroposterior) plane (Fig. 26-10). The cortical thickness and trabecular pattern of the enlarged condyle usually are normal, which helps to distinguish this condition from a condylar neoplasm. The glenoid fossa may be enlarged, usually at the expense of the posterior slope of the articular eminence. The ramus and mandibular body on the affected side also may be enlarged, resulting in a characteristic depression of the inferior mandibular border at the midline, where the enlarged side joins the contralateral normal mandible. The affected ramus may have increased vertical depth and may be thicker in the anteroposterior dimension.
Differential Diagnosis
A condylar tumor, most notably an osteochondroma, is included in the differential diagnosis. An osteochondroma usually is irregular in shape compared with a hyperplastic condyle. Surface irregularities and continued growth after cessation of skeletal growth should increase suspicion of this tumor. Occasionally a condylar osteoma or large osteophyte that occurs in chronic degenerative joint disease may simulate condylar hyperplasia.
Treatment
Treatment consists of orthodontics combined with orthognathic surgery and it may be initiated before condylar growth is complete to avoid functional problems (mastication and speech) and worsening esthetic disfigurement. If treatment is delayed, severe mandibular deformation and compensatory changes in the maxilla, dentoalveolar structures, and associated soft tissues may result, which may compromise treatment outcome. On the other hand, treatment before condylar growth is completed may result in relapse of occlusal and esthetic problems. Cessation of growth of the condyle may be determined with technetium bone scans.
Definition
Condylar hypoplasia is failure of the condyle to attain normal size because of congenital and developmental abnormalities or acquired diseases that affect condylar growth. The condyle is small, but condylar morphology usually is normal (Fig. 26-11). The condition may be inherited or may appear spontaneously. Some cases have been attributed to early injury or injury to the articular cartilage by birth trauma or intra-articular inflammatory lesions.
Clinical Features
Condylar hypoplasia usually is a component of a mandibular growth deficiency and therefore is often associated with an underdeveloped ramus and (occasionally) mandibular body. Congenital abnormalities may be unilateral or bilateral and usually are a manifestation of a more generalized condition (e.g., micrognathia, Treacher Collins syndrome); they also may be associated with congenital defects of the ear and zygomatic arch. Developmental abnormalities that manifest during growth usually are unilateral. Acquired abnormalities are the result of damage during the growth period from sources, such as therapeutic radiation or infection, that diminish or prevent further condylar growth and development. Patients with condylar hypoplasia have mandibular asymmetry and may have symptoms of TMJ dysfunction. The chin commonly is deviated to the affected side, and the mandible deviates to the affected side during mandibular opening. Degenerative joint disease is a common long-term sequela.
Radiographic Features
The condyle may be normal in shape and structure but is diminished in size, and the mandibular fossa also is proportionally small (Fig. 26-12). The condylar neck and coronoid process usually are very slender and are shortened or elongated in some cases. The posterior border of the ramus and condylar neck may have a dorsal (posterior) inclination. The ramus and mandibular body on the affected side may also be small, resulting in a mandibular asymmetry and occasional dental crowding, depending on the severity of mandibular underdevelopment. The antegonial notch is deepened. The associated mandibular hypoplasia is more pronounced if the effect takes place early in life.
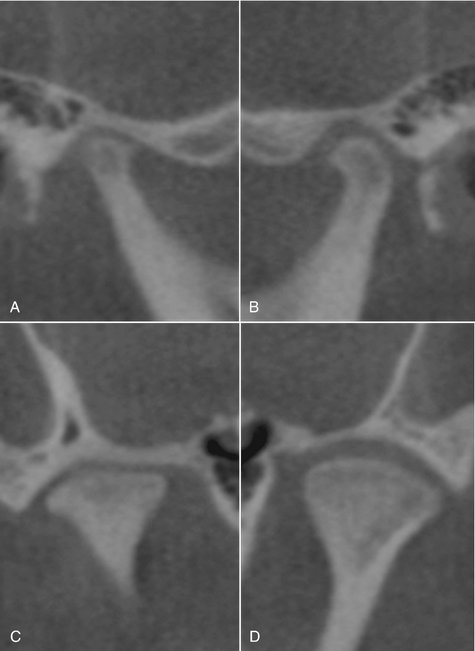
FIG. 26-12 Cone-beam CT of unilateral condylar hypoplasia, sagittal (A and B) and coronal (C and D) reformatted images. A and C, The right condyle is hypoplastic and there is secondary remodeling. The articular surfaces of the condyle and anterior aspect of the glenoid fossa are flattened and the superior joint space is thinner compared with the left. B and D, Left side of same patient showing normal condyle.
Differential Diagnosis
Condylar destruction from juvenile rheumatoid arthritis may appear similar to that of hypoplasia. A survey of other joints or testing for rheumatoid factor may be helpful. Changes in condylar morphology in severe degenerative joint disease or other arthritic conditions may have a similar appearance, although arthritic disease does not cause mandibular hypoplasia of the affected side unless it occurs during growth, and other signs of arthritis are usually visible in the affected joint.
Definition
Juvenile arthrosis, a condylar growth disturbance first described by Boering, manifests as hypoplasia and characteristic morphologic abnormalities. This condition may be a form of condylar hypoplasia but is thought to differ in that the affected condyle at one time was normal, becoming abnormal during growth. Juvenile arthrosis may be unilateral or bilateral, and it predisposes the TMJ to secondary degenerative changes.
Clinical Features
Juvenile arthrosis affects children and adolescents during the period of mandibular growth. It is more common in females. It may be an incidental finding in a panoramic projection, or the patient may have mandibular asymmetry, signs and symptoms of TMJ dysfunction, or both.
Radiographic Features
The condylar head develops a characteristic “toadstool” appearance, with marked flattening and apparent elongation of the articulating condylar surface and dorsal (posterior) inclination of the condyle and neck. The condylar neck is shortened or even absent in some cases, with the condyle resting on the upper margin of the ramus (Fig. 26-13). The articulating surface of the temporal component often is flattened. Progressive shortening of the ramus occurs on the affected side, and the antegonial notch may be deepened, indicating mandibular hypoplasia. In long-standing cases, superimposed degenerative changes may be present.
Differential Diagnosis
The radiographic appearance of juvenile arthrosis may be very similar to, and in some cases is indistinguishable from, developmental hypoplasia of the condyle. Destruction of the anterior aspect of the condylar head from rheumatoid arthritis and severe degenerative joint disease or severe condylar degeneration after orthognathic surgery or joint surgery also may simulate juvenile arthrosis.
Treatment
Orthognathic surgery and orthodontic therapy may be required to correct the mandibular asymmetry. Caution should be exercised in undertaking orthodontic therapy because stress on the joint may result in further degeneration and orthodontic relapse.
Definition
Coronoid process hyperplasia may be acquired or developmental, resulting in elongation of the coronoid process. In the developmental variant, the condition usually is bilateral. Acquired types may be unilateral or bilateral and usually are a response to restricted condylar movement caused by abnormalities such as ankylosis.
Clinical Features
Bilateral developmental coronoid hyperplasia is more common in males, often commencing at the onset of puberty, although the condition was reported in a 3-year-old child. Patients complain of a progressive inability to open the mouth and may have an apparent closed lock. The condition is painless.
Radiographic Features
Coronoid hyperplasia is best seen in panoramic, Waters, and lateral tomographic views and on CT scans. The coronoid processes are elongated, and the tips extend at least 1 cm above the inferior rim of the zygomatic arch (Fig. 26-14). As a result, the coronoid processes may impinge on the medial surface of the zygomatic arch during opening, restricting condylar translation. This can be confirmed by using CT imaging (Fig. 26-15). The coronoid processes may have a large but normal shape or may curve anteriorly and may appear very radiopaque. The posterior surface of the zygomatic process of the maxilla may be remodeled to accommodate the enlarged coronoid process during function. The radiographic appearance of the TMJs usually is normal.
Differential Diagnosis
Unilateral cases should be differentiated from a tumor of the coronoid process such as an osteochondroma or osteoma. Unlike coronoid hyperplasia, tumors usually have an irregular shape. The differential diagnosis also includes any cause of inability to open, such as soft tissue abnormalities and ankylosis, emphasizing the importance of including the coronoid process in images of the TMJs. An axial CT image with the patient in a wide open position is useful in establishing coronoid interference to opening.
Treatment
Treatment consists of surgical removal of the coronoid process and postoperative physiotherapy. Regrowth of the coronoid process after surgery has been reported.
Definition
A bifid condyle has a vertical depression, notch, or deep cleft in the center of the condylar head, seen in the frontal or sagittal plane, or actual duplication of the condyle, resulting in the appearance of a “double” or “bifid” condylar head. This condition is rare and is more often unilateral, although it may be bilateral. It may result from an obstructed blood supply or other embryopathy, although a traumatic cause has been postulated as a result of a longitudinal linear fracture of the condyle.
Clinical Features
Bifid condyle usually is an incidental finding in panoramic views or anteroposterior projections. Some patients have signs and symptoms of temporomandibular dysfunction, including joint noises and pain.
Radiographic Features
A depression or notch is present on the superior condylar surface, giving the anteroposterior silhouette a heart shape; in more severe cases a duplicate condylar head is present in the mediolateral plane (Fig. 26-16). The orientation of the bifid condyle may be anteroposterior or mediolateral. The mandibular fossa may remodel to accommodate the altered condylar morphology.
SOFT TISSUE ABNORMALITIES
Definition
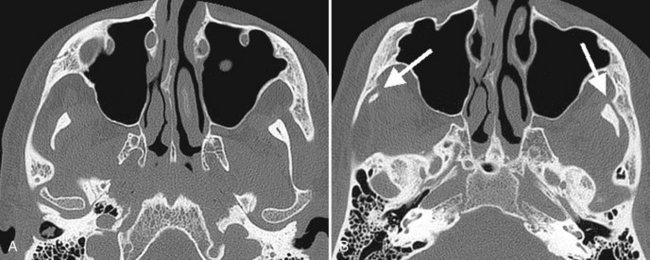
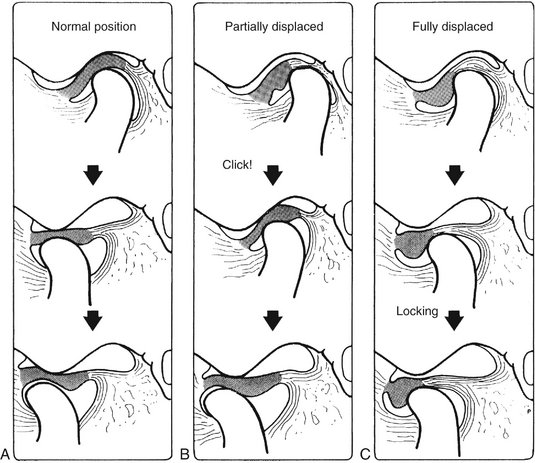
An internal derangement is an abnormality in the position and sometimes the morphology of the articular disk that may interfere with normal function. The disk most often is displaced in an anterior direction, but it may be displaced anteromedially, medially, or anterolaterally. Lateral and posterior displacements are extremely rare. Some hypothesize that disk displacements may be considered a normal variation on the basis of the frequency of this finding in asymptomatic patients. The cause of internal derangements is unknown, although parafunction, jaw injuries (e.g., direct trauma), whiplash injury, and forced opening beyond the normal range have been implicated.
Internal derangements can be diagnosed by MRI. In some instances the disk may resume a normal position with respect to the condyle (called reduction of the disk) during mandibular opening; when the disk remains displaced throughout the entire range of mandibular movement, the term nonreduction is used (Fig. 26-17). A long-standing displaced disk may become deformed, losing its normal biconcave shape, and it may become thickened and fibrotic. Possible complications are degenerative joint disease and perforation through the disk or (more commonly) the posterior attachment.
Clinical Features
Disk displacement has been found both in symptomatic patients and in healthy volunteers, suggesting that it may be a normal variant and not necessarily a predisposing factor in TMJ dysfunction. It is not known why some disks remain displaced or why symptoms of pain and dysfunction are not found in all affected patients. Symptomatic patients may have a decreased range of mandibular motion. Internal derangements can be unilateral or bilateral; unilateral cases may manifest clinically as mandibular deviation to the affected side on opening. Joint noises are common and may manifest as a click as the disk reduces to a normal position during mandibular opening and occasionally as a softer click as the disk becomes displaced again during mandibular closing. Noises may be absent in long-term displaced, nonreducing disks, or crepitus may be heard. Patients may complain of pain in the preauricular region or headaches and may have episodes of closed or open locking of the joint. Patients may have to manipulate the mandible to open it fully past an apparent closed lock by applying medially directed pressure to the affected joint or mandible with the hand.
Radiographic Features
The disk cannot be visualized with conventional radiography or tomography; MRI is the technique of choice. Although a retruded condylar position has been associated with disk displacement, condylar position in maximal intercuspation is not a reliable indicator of disk displacement. Likewise, diminished range of motion at maximal opening is not a reliable indication of a nonreducing disk. In MRI the normal disk has a low signal intensity (is dark between bone and muscle), and the signal intensity of the bilaminar zone is usually higher (i.e., lighter). In the closed-mouth position, the normal disk is positioned with the posterior band directly superior to the condylar head and the thin intermediate part between the anterosuperior surface of the condyle and the posteroinferior surface of the articular eminence (see Fig. 26-9). It is important to note that in all positions of mouth opening the thin intermediate part remains the articulating surface of the disk between condyle and articular eminence.
Disk Displacement
Identifying the disk may be difficult in cases of gross deformation of the disk and other soft tissue components. Anterior displacement is the most common disk displacement. When the mandible is in maximal intercuspation, partial or full anterior disk displacement is indicated by anterior location of the posterior band of the disk from the normal position, which is directly superior to the condylar head. An indication of anterior displacement is positioning of the posterior band forward so that it sits between the anterosuperior surface of the condyle and the eminence (Fig. 26-18). However, correct identification of the posterior band may be impossible if the tissue signal of the bilaminar zone approximates the posterior band, which occurs in chronic disk displacements. Therefore it is also important to evaluate the position of the thin intermediate part of the disk, which should be adjacent to the anterosuperior part of the condyle. Anteromedial displacement is indicated in sagittal image slices when the disk is in a normal position in the medial images of the joint but anteriorly positioned in the lateral images of the same joint. Medial or lateral displacement is indicated in MRI coronal images when the body of the disk is positioned at the medial aspect of the condyle (Fig. 26-18). Posterior disk displacement is rare.
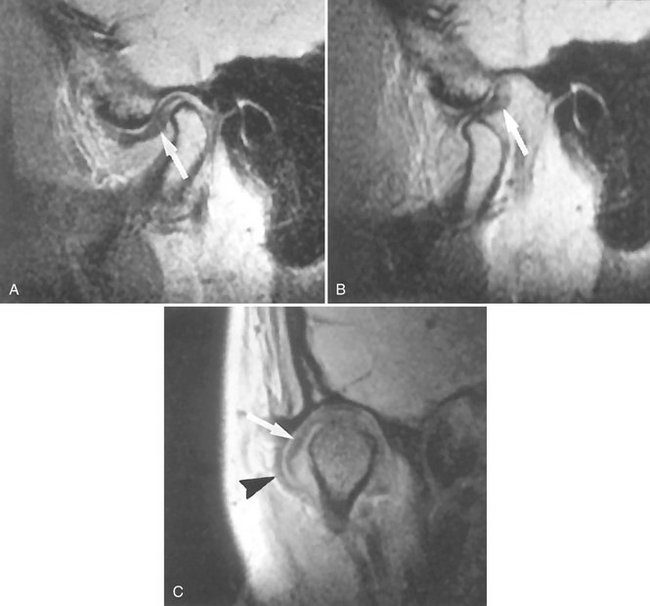
FIG. 26-18 MRI of anterior disk displacement with reduction. A, Closed sagittal view showing the disk with its posterior band (arrow) anterior to the condyle; note the anterior position of the thin intermediate section of the disk. B, Open view showing the normal relationship of the disk and condyle and the posterior band of the disk (arrow). C, Coronal view showing the disk (white arrow) laterally displaced. The joint capsule (black arrowhead) bulges laterally. (B courtesy Dr. Per-Lennart Westesson, Rochester, NY.)
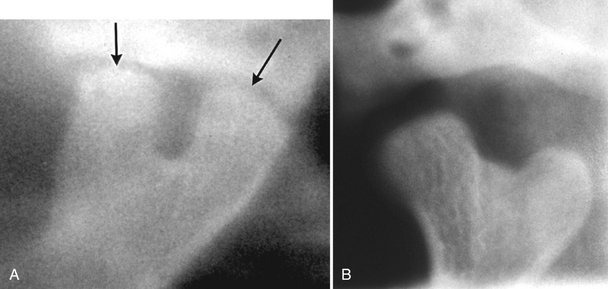
Disk Reduction and Nonreduction
During mouth opening, an anteriorly displaced disk may reduce to a normal relationship with the condylar head during any part of the opening movement. In motion studies, this is usually a rapid posterior movement of the disk and it is often accompanied by an audible click. This is referred to as disk reduction and can be diagnosed if the disk is in a normal position in the open mouth magnetic resonance images (see Fig. 26-18).
If the disk remains anteriorly displaced (nonreduction) on opening, it may bend or deform as the condyle pushes against it (Fig. 26-19). If the disk remains displaced, it will undergo permanent deformation, losing its biconcave shape. The nonreduced disk is readily seen on MRI scans, although fibrotic changes of the bilaminar zone may alter its tissue signal to approximate the signal of the disk and thus make identification of the disk itself difficult. In such cases the disk may be erroneously interpreted as occupying a normal position at maximal opening.
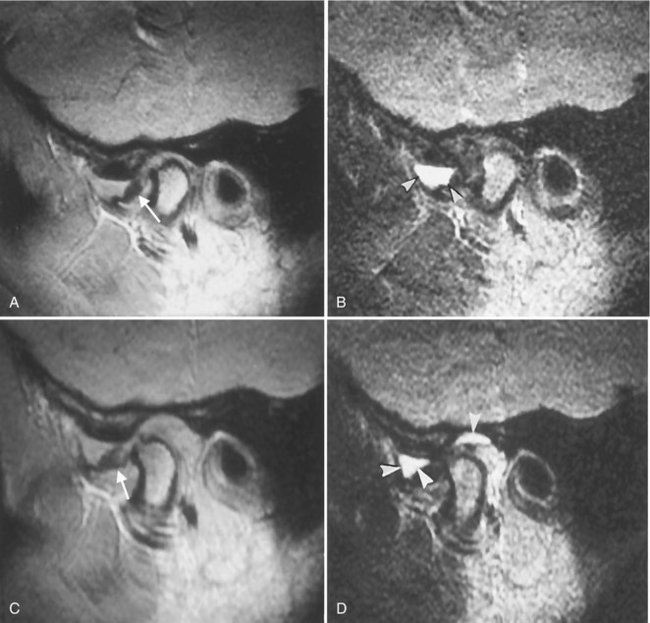
FIG. 26-19 MRI of disk displacement without reduction in the presence of joint effusion. A, The disk (arrow) is anteriorly displaced in this closed T1-weighted image. B, A T2-weighted image of the same section shows the collection of joint effusion (arrowheads) in the anterior recess of the upper joint space. C, Open T1-weighted image showing the disk remains anterior to the condyle. The posterior band of the disk is indicated with an arrow. D, This T2-weighted image is at the same level as C. Note the joint effusion (arrowheads) in the anterior and posterior recesses of the upper joint space. (Courtesy Dr. Per-Lennart Westesson, Rochester, N.Y.)
Perforation and Deformities
Perforations between the superior and inferior joint spaces most commonly occur in the retrodiskal tissue, just behind the posterior band of the disk (Fig. 26-20, C) and can be detected in arthrographic investigations but are not reliably detected with MRI. MRI can indicate alteration in the normal biconcave outline of the disk, which may vary from enlargement of the posterior band to a bilinear or biconvex disk outline. Disk deformities may be accompanied by changes in its signal intensity, sometimes an increase in signal. Changes to the condyle and temporal component of the joint consistent with degenerative joint disease often accompany cases with long-standing displaced disks (Fig. 26-20).
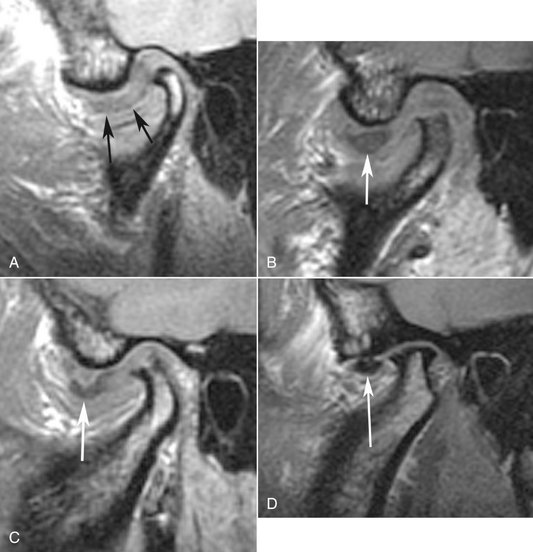
FIG. 26-20 Sagittal MRI of several cases of anteriorly displaced disks (arrows) with various stages of degenerative joint disease. A, An example of severe deformation of the disk and an increase in the tissue signal. B, Severe erosions of the superior aspect of the condyle. C, Erosions involving the condyle and a small osteophyte on the anterior aspect. D, An example of osteophytes forming on both the anterior and posterior surfaces of the condyle.
Fibrous Adhesions and Effusion
Fibrous adhesions are masses of fibrous tissue or scar tissue that form in the joint space, particularly after TMJ surgery. Adhesions are best identified with arthrography by resistance to injection of contrast agent or they may be detected in MRI studies as tissue with low signal intensity. The pressure of injected contrast agent may tear some of these adhesions, resulting in increased joint mobility after the procedure. Joint effusion (fluid in the joint) is considered to be an early change that may precede degenerative joint disease. MRI can detect joint effusion, which presents as an area of high-signal intensity in the joint spaces in T2-weighted images (see Fig. 26-19).
Remodeling and Arthritic Conditions
Definition
Remodeling is an adaptive response of cartilage and osseous tissue to forces applied to the joint that may be excessive, resulting in alteration of the shape of the condyle and articular eminence. This adaptive response may result in flattening of curved joint surfaces, which effectively distributes forces over a greater surface area. The number of trabeculae also increases, increasing the density of subchondral cancellous bone (sclerosis) to better resist applied forces. No destruction or degeneration of articular soft tissues occurs. TMJ remodeling occurs throughout adult life and is considered abnormal only if it is accompanied by clinical signs and symptoms of pain or dysfunction or if the degree of remodeling seen radiographically is judged to be severe. Remodeling may be unilateral and does not invariably serve as a precursor to degenerative joint disease.
Clinical Features
Remodeling may be asymptomatic, or patients may have signs and symptoms of temporomandibular dysfunction that may be related to the soft tissue components, associated muscles, or ligaments. Accompanying internal derangement of the disk may be a factor.
Radiographic Features
Radiographic changes may affect the condyle, temporal component, or both; they first occur on the anterosuperior surface of the condyle and the posterior slope of the articular eminence. The lateral aspect of the joint is affected in early stages, and the central and medial aspects become involved as remodeling progresses. The radiographic appearance may include one or a combination of the following: flattening, cortical thickening of articulating surfaces, and subchondral sclerosis (Fig. 26-21).
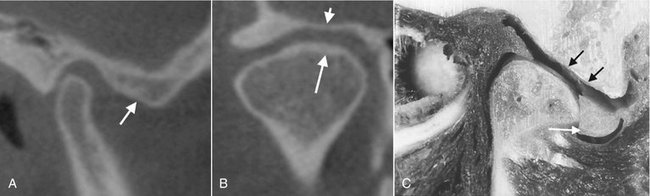
FIG. 26-21 Cone-beam CT, sagittal (A) and coronal (B) reformat images of the right TMJ showing remodeling. A, The right temporal component shows subchondral sclerosis and flattening (arrow). B, The right condyle shows mild flattening of the lateral aspect and subchondral sclerosis of the medial aspect (arrow). The right temporal component is also flattened (arrowhead). C, A cadaver specimen. Note the flattening of the temporal component (black arrows) and large perforation posterior to a residual deformed disk (white arrow).
Differential Diagnosis
Severe joint flattening and subchondral sclerosis may be difficult to differentiate from early degenerative joint disease. It is known that the microscopic changes of degeneration occur before they can be detected radiographically. The radiographic appearance of bone erosions, osteophytes, and loss of joint space are signs signifying degenerative joint disease.
Treatment
When no clinical signs or symptoms are present, treatment is not indicated. Otherwise, treatment directed to relieve stress on the joint, such as splint therapy, may be considered. This should be preceded by an attempt to discover the cause of the joint stress.
Definition
Degenerative joint disease (DJD) is a noninflammatory disorder of joints characterized by joint deterioration and proliferation. Joint deterioration is characterized by loss of articular cartilage and bone erosion. The proliferative component is characterized by new bone formation at the articular surface and in the subchondral region. Usually a variable combination of deterioration and proliferation occurs, but occasionally one aspect predominates; deterioration is more common in acute disease, and proliferation predominates in chronic disease. DJD is thought to occur when the ability of the joint to adapt to excessive forces (remodel) is exceeded. The etiology of DJD is unknown, although a number of factors may be important, including acute trauma, hypermobility, and loading of the joint such as occurs in parafunction. Internal disk derangements may be contributing etiologic factors, but this theory is controversial.
Clinical Features
DJD can occur at any age, although the incidence increases with age. DJD has a female preponderance. The disease may be asymptomatic, or patients may complain of signs and symptoms of TMJ dysfunction, including pain on palpation and movement, joint noises (crepitus), limited range of motion, and muscle spasm. The onset of symptoms may be sudden or gradual, and symptoms may disappear spontaneously, only to return in recurring cycles. Some studies report that the disease eventually “burns out” and symptoms disappear or markedly decrease in severity in long-standing cases.
Radiographic Features
Osseous changes in DJD are more accurately depicted in CT images, but gross osseous changes may be evident in MRI studies, particularly in T1-weighted images. When the patient is in maximal intercuspation, the joint space may be narrow or absent, which often correlates with an internal derangement and frequently with a perforation of the disk or posterior attachment, resulting in bone-to-bone contact of the joint components. Signs of previous remodeling, such as flattening and subchondral sclerosis, may be evident, although degenerative changes may obscure these findings. Loss of cortex or erosions of the articulating surfaces of the condyle or temporal component (or both) are characteristic of this disease (Fig. 26-22). In some cases small, round, radiolucent areas with irregular margins surrounded by a varying area of increased density are visible deep to the articulating surfaces. These lesions are called “Ely” or subchondral bone cysts but are not true cysts; they are areas of degeneration that contain fibrous tissue, granulation tissue, and osteoid (Fig. 26-22).
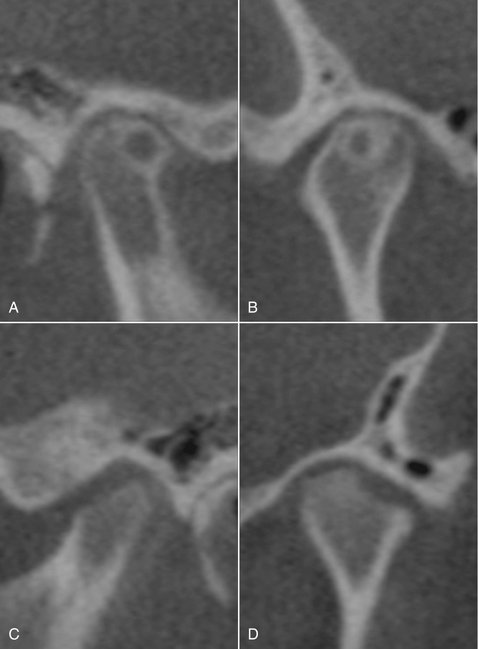
FIG. 26-22 Cone-beam CT, closed position depicting various erosions in degenerative joint disease. A and B, Same patient, right side. Large subchondral cystlike erosion (“Ely cyst”) of the condyle surrounded by a broad zone of sclerosis. Note also the thin joint space. C and D, Same patient, left side. Broad erosion of the anterolateral condylar surface. Note also the lack of cortication of the remaining condylar surface and flattening of the temporal component.
Later in the course of the disease, bony proliferation occurs at the periphery of the articulating surface, increasing the articulating surface area. This new bone is called an osteophyte, which typically appears on the anterosuperior surface of the condyle, the lateral aspect of the temporal component, or both (Fig. 26-23). Osteophytes also may form on the lateral, medial, and posterosuperior aspects of the condyle. In severe cases, osteophyte formation originating in the glenoid fossa extends from the articular eminence to almost encase the condylar head. Osteophytes may break off and lie free within the joint space (these fragments are known as “joint mice”), and these must be differentiated from other conditions that cause joint space radiopacities (Figs. 26-23 and 26-24). It has been reported that joints with long-term nonreducing disk displacement have a higher incidence of progressive radiographic changes of DJD than in joints with no disk displacement or reducing disks.

FIG. 26-23 Sagittal tomogram of the left temporomandibular joint. A large osteophyte emanating from the anterior aspect of the condyle (short arrow) and a “joint mouse” (long arrow) positioned anterior to the condyle in the joint space.
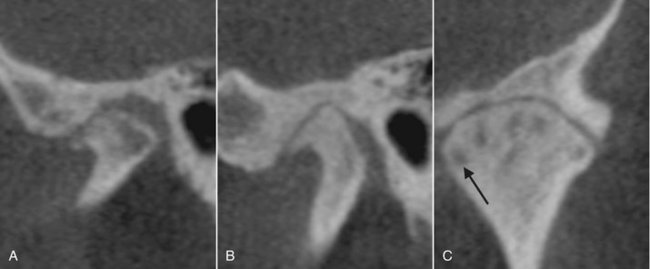
FIG. 26-24 Cone-beam CT, closed position displaying two cases of degenerative joint disease (different patients). A, Sagittal reformat. Surface erosions of the condyle with osteophyte formation at the anterior aspect. Subchondral sclerosis, flattening and erosions of the temporal component. The condyle is also anteriorly positioned in the glenoid fossa. B, Sagittal reformat. Prominent osteophyte formation at the anterior aspect of the condyle, flattening and subchondral sclerosis of all joint components, with decreased width of the joint space. C, Coronal reformat, same patient as B. Multiple subchondral erosions not visible in the sagittal reformat (arrow, one example).
In severe DJD, the glenoid fossa may appear grossly enlarged because of erosion of the posterior slope of the articular eminence, and the condyle may be markedly diminished in size and altered in shape because of destruction and erosion of the condylar head. This in turn may allow the condylar head to move forward and superiorly into an abnormal anterior position that may result in an anterior open bite.
Differential Diagnosis
DJD can have a spectrum of appearances ranging from substantial subchondral sclerosis and osteophyte formation (proliferative component) to extensive erosions (degenerative component). A more erosive appearance may simulate inflammatory arthritides such as rheumatoid arthritis, whereas a more proliferative appearance with extensive osteophyte formation may simulate a benign tumor such as osteoma or osteochondroma.
Treatment
Treatment is directed toward relieving joint stress (e.g., splint therapy), relieving secondary inflammation with anti-inflammatory drugs, and increasing joint mobility and function (e.g., physiotherapy).
Definition
Rheumatoid arthritis (RA) is a heterogeneous group of systemic disorders that manifests mainly as synovial membrane inflammation in several joints. The TMJ becomes involved in approximately half of affected patients. The characteristic radiographic findings are a result of villous synovitis, which leads to formation of synovial granulomatous tissue (pannus) that grows into fibrocartilage and bone, releasing enzymes that destroy articular surfaces and underlying bone.
Clinical Features
RA is more common in females and can occur at any age but increases in incidence with increasing age. A juvenile variant is discussed separately. Usually the small joints of the hands, wrists, knees, and feet are affected in a bilateral, symmetric fashion, whereas TMJ involvement varies. Patients with TMJ involvement complain of swelling, pain, tenderness, stiffness on opening, limited range of motion, and crepitus. The chin appears receded, and an anterior open bite is a common finding because of the bilateral destruction and anterosuperior positioning of the condyles. TMJ involvement usually is bilateral and symmetric.
Radiographic Features
The initial changes may be generalized osteopenia (decreased density) of the condyle and temporal component. The pannus may destroy the disk, resulting in diminished width of the joint space. Bone erosions by the pannus most often involve the articular eminence and the anterior aspect of the condylar head, which permits anterosuperior positioning of the condyle when the teeth are in maximal intercuspation and results in an anterior open bite (Fig. 26-25). Erosion of the anterior and posterior condylar surfaces at the attachment of the synovial lining may result in a “sharpened pencil” appearance of the condyle. Erosive changes may be so severe that the entire condylar head is destroyed, with only the neck remaining as the articulating surface. Similarly, the articular eminence may be destroyed to the extent that a concavity replaces the normally convex eminence. Joint destruction eventually leads to secondary DJD. Subchondral sclerosis and flattening of articulating surfaces may occur, as well as subchondral “cyst” and osteophyte formation. Fibrous ankylosis or, in rare cases, osseous ankylosis, may occur (Fig. 26-26); reduced mobility is related to the duration and severity of the disease.
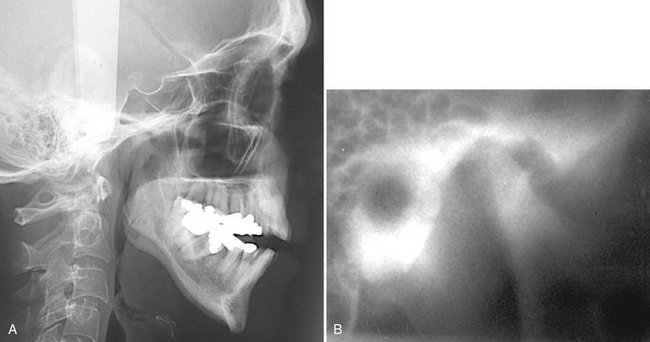
FIG. 26-25 Rheumatoid arthritis. A, Lateral cephalometric view illustrating a steep mandibular plane and anterior open bite. B, Lateral tomogram (closed position) illustrating a large erosion of the anterosuperior condylar head accompanied by severe erosions of the temporal component, including the articular eminence.
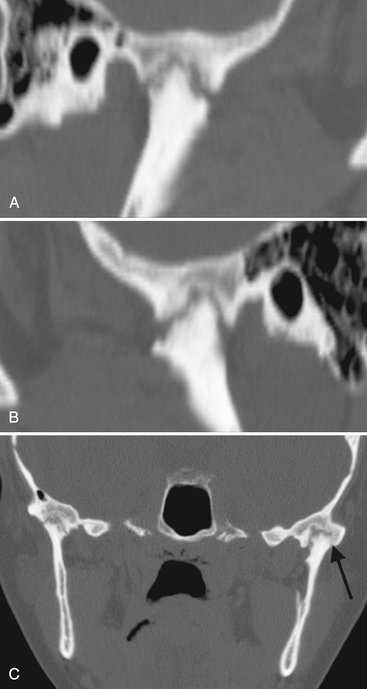
FIG. 26-26 Sagittal reformat (A and B) CT images with bone algorithm of the right and left joints of a case of RA. Note the irregular surface of the condyle and articular eminence and that the shapes are similar to opposing pieces of a puzzle, suggesting the possibility of fibrous ankylosis. Because of erosion of the articular eminentia, the condyles have an abnormal anterior position near the residual articular eminentia. C, A coronal CT image of the same case. Note the osseous ankylosis on the lateral aspect of the left joint (arrow).
Differential Diagnosis
The differential diagnosis includes severe DJD and psoriatic arthritis. Osteopenia and severe erosions, particularly of the articular eminence, are more characteristic of RA. Psoriatic arthritis may be ruled out by the patient’s history.
Treatment
Treatment is directed toward pain relief (analgesics), reduction or suppression of inflammation (nonsteroidal anti-inflammatory drugs, gold salts, corticosteroids), and preservation of muscle and joint function (physiotherapy). Joint replacement surgery may be necessary in patients with severe joint destruction.
Definition
Juvenile arthritis (JA), formerly called juvenile rheumatoid arthritis and juvenile chronic arthritis, is a chronic inflammatory disease that appears before the age of 16 years (the mean age is 5 years). It is characterized by chronic, intermittent synovial inflammation that results in synovial hypertrophy, joint effusion, and swollen, painful joints. As the disease progresses, cartilage and bone are destroyed. Rheumatoid factor may be absent, hence the preferred terminology of JA rather than juvenile rheumatoid arthritis. JA differs from adult RA in that it has an earlier onset, and systemic involvement usually is more severe. TMJ involvement occurs in approximately 40% of patients and may be unilateral or bilateral.
Clinical Features
The patient usually has pain and tenderness in the affected joint or joints, although the disease can be asymptomatic. Unilateral onset is common, but contralateral involvement may occur as the disease progresses. Severe TMJ involvement results in inhibition of mandibular growth. Affected patients may have micrognathia and posteroinferior chin rotation, resulting in a facial appearance known as “bird face,” which may also be accompanied by an anterior open bite. The degree of micrognathia is proportional to the severity of joint involvement and the early onset of disease. Additionally, when only one TMJ is involved or if one side is more severely affected, the patient may have a mandibular asymmetry with the chin deviated to the affected side.
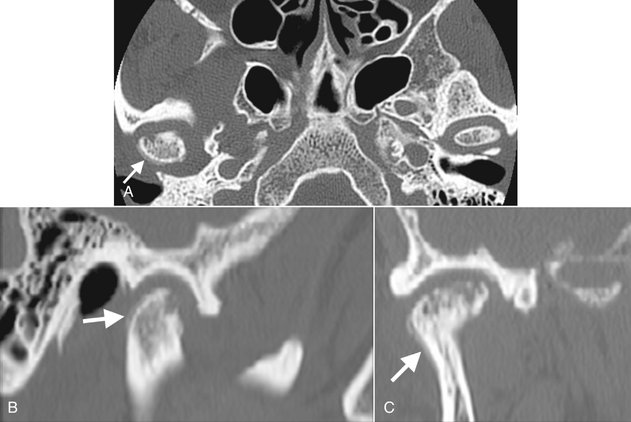
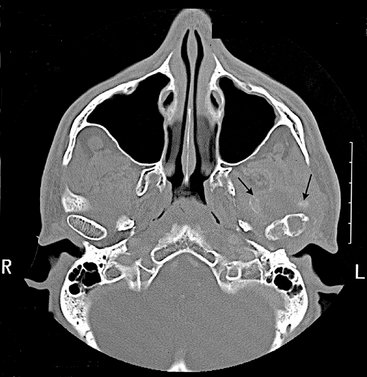
Radiographic Features
Osteopenia (decreased density) of the affected TMJ components may be the only initial radiographic finding. Radiographic findings are similar to those for the adult form except for the addition of impaired mandibular growth. Erosions may extend to the mandibular fossa, and the articular eminence may be destroyed. Similarly, erosion of the anterior or superior aspect of the condyle may occur, and in more severe cases only a pencil-shaped small condyle remains; the condyle may be destroyed. Because the inflammation is intermittent, during quiescent periods the cortex of the joint surfaces may reappear, and the surfaces will appear flattened. As a result of bone destruction, the condylar head typically is positioned anterosuperiorly in the mandibular fossa (Fig. 26-27). Hypomobility at maximal opening is common, and fibrous ankylosis may occur in some cases. Secondary degenerative changes manifesting as sclerosis and osteophyte formation may be superimposed on the rheumatoid changes, and ankylosis may occur. An abnormal disk shape is often observed in patients with long-term TMJ involvement. Manifestations of inhibited mandibular growth, such as deepening of the antegonial notch, diminished height of the ramus, and dorsal bending of the ramus and condylar neck, also may occur unilaterally or bilaterally, resulting in an obtuse angle between the mandibular body and the ascending ramus.
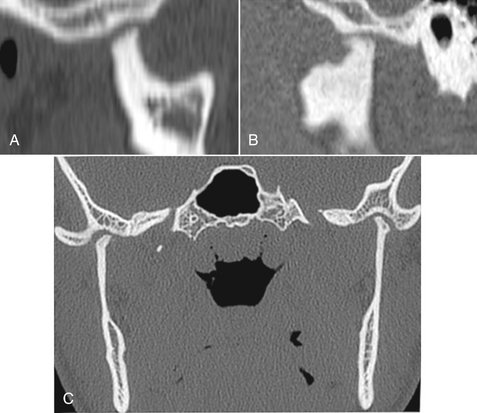
FIG. 26-27 A and B, Sagittal CT reformat images of a case of juvenile arthritis. Note the severe erosion of the articular eminence and the condyles and the abnormal anterior positioning of both condyles. C, This coronal CT image of the same case shows small remnants of the condylar heads after severe erosion.
Psoriatic Arthritis and Ankylosing Spondylitis
Psoriatic arthritis and ankylosing spondylitis are seronegative, systemic arthritides that may affect the TMJs. Psoriatic arthritis occurs in patients with psoriasis of the skin, with inflammatory joint disease occurring in 7% of patients. Ankylosing spondylitis occurs predominantly in males, progressing to spinal fusion. TMJ radiographic changes seen in these disorders may be indistinguishable from those caused by RA, although occasionally a profound sclerotic change is seen in psoriatic arthritis.
Definition
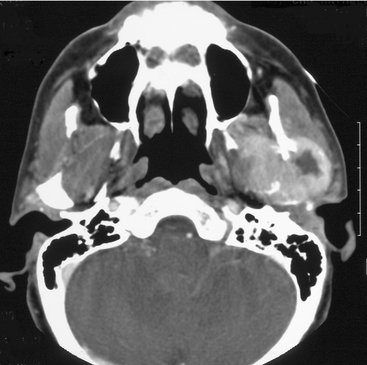
Septic arthritis is infection and inflammation of a joint that can result in joint destruction. It is rare in comparison to the incidence of DJD and RA in the TMJ. Septic arthritis may be caused by direct spread of organisms from an adjacent cellulitis or from parotid, otic, or mastoid infections. It also may occur by direct extension of osteomyelitis of the mandibular body and ramus or spread from a middle ear infection, although hematogenous spread from a distant nidus has also been reported. Other causes include systemic and autoimmune diseases (e.g., RA, diabetes, immunosuppression, hypogammaglobulinemia), prolonged use of systemic steroids, and sexually transmitted diseases. Septic arthritis has also been reported in children after blunt trauma, as a result of hyperemia and increased exposure to microorganisms, damage to local structure allowing bacterial access, or hematoma formation providing a favorable growth medium.
Clinical Features
Individuals can be affected at any age, and the condition shows no sex predilection. It usually occurs unilaterally. The patient may have redness and swelling over the joint; trismus; severe pain on opening; inability to occlude the teeth; large, tender cervical lymph nodes; fever; and malaise. The mandible may be deviated to the unaffected side as a result of joint effusion.
Radiographic Features
No radiographic signs may be present in early stages of the disease, although the space between the condyle and the roof of the mandibular fossa may be widened because of inflammatory exudate in the joint spaces. Osteopenic (radiolucent) changes of the joint components and mandibular ramus may be evident. More obvious bony changes are seen approximately 7 to 10 days after the onset of clinical symptoms. As a result of the osteolytic effects of inflammation, the condylar articular cortex may become slightly radiolucent, erosions of the surface of the condyle and articular eminence may be seen, sequestra may become apparent, and there may be periosteal new bone formation (Fig. 26-28). As the disease progresses, the condyle and articular eminence, including the disk, may be destroyed. Osseous ankylosis may occur after the infection subsides. If the disease occurs during the period of mandibular growth, radiographic manifestations of inhibited mandibular growth may be evident.
Differential Diagnosis
The diagnosis of septic arthritis is ideally made by identification of organisms in joint aspirate, although cultures occasionally remain negative. The radiographic changes caused by septic arthritis may mimic those of severe DJD or RA, although septic arthritis usually occurs unilaterally, and the patient often has clinical signs and symptoms of infection. Inflammatory changes that may accompany septic arthritis may be seen in CT images, such as involvement of mastoid air cells, osteomyelitis of the mandible, and inflammation of surrounding soft tissue. MRI, with T2-weighted images, may show muscle enlargement, joint effusion, or abscess. Scintigraphy by use of a technetium bone scan will show increased bone metabolism within the osseous components, especially the condyle, and gallium confirms the presence of infection.
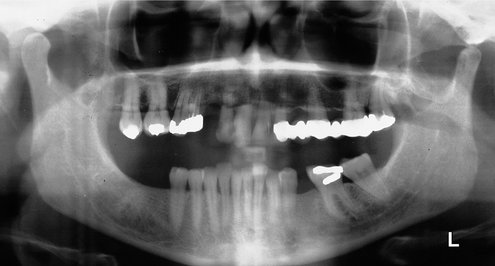
Articular Loose Bodies
Articular loose bodies are radiopacities of varying origin located in the synovium, within the capsule in the joint spaces, or outside the capsule in soft tissue. They appear radiographically as soft tissue calcifications positioned around the condylar head. The loose bodies may represent bone that has separated from joint components, as in DJD (joint mice), hyaline cartilage metaplasia (calcification) that occurs in synovial chondromatosis, crystals deposited in the joint space in crystal-associated arthropathy (pseudogout), or tumoral calcinosis associated with renal disease. In rare cases chondrosarcoma also may mimic the appearance of articular loose bodies.
Definition
Synovial chondromatosis is an uncommon disorder characterized by metaplastic formation of multiple cartilaginous and osteocartilaginous nodules within connective tissue of the synovial membrane of joints. Some of these nodules may detach and form loose bodies in the joint space, where they persist and may increase in size, being nourished by synovial fluid. This condition is more common in the axial skeleton than in the TMJ. When the cartilaginous nodules ossify, the term synovial osteochondromatosis may be used.
Clinical Features
Patients may be asymptomatic or may complain of preauricular swelling, pain, and decreased range of motion. Some patients have crepitus or other joint noises. The condition usually occurs unilaterally.
Radiographic Features
The osseous components may appear normal or may exhibit osseous changes similar to those in DJD. The joint space may be widened, and if ossification of the cartilaginous nodules has occurred, a radiopaque mass or several radiopaque loose bodies may be seen surrounding the condylar head (Fig. 26-29). CT imaging can identify the location of the calcifications. Sclerosis of the glenoid fossa and condyle may be seen, which is considered to be a chronic bone reaction to an active lesion. Occasionally, erosion through the glenoid fossa into the middle cranial fossa may occur, which is best detected with CT. MRI may be useful in defining the tissue planes between the synovial chondromatosis mass and surrounding soft tissue.
Differential Diagnosis
The appearance of synovial osteochondromatosis cannot always be differentiated from chondrocalcinosis; however, often the soft tissue calcifications in osteochondromatosis are larger and may have a peripheral cortex that identifies their bony nature. Conditions that appear similar include DJD with joint mice or chondrosarcoma or osteosarcoma. Either sarcoma may be accompanied by severe bone destruction, which may help in differentiating the condition from synovial chondromatosis.
Treatment
Treatment consists of removal of the loose bodies and resection of abnormal synovial tissue in the joint by arthroscopic or open joint surgery.
Definition
Chondrocalcinosis is characterized by acute or chronic synovitis and precipitation of calcium pyrophosphate dihydrate crystals in the joint space. It differs from gout, in which urate crystals are precipitated, hence the term pseudogout.
Clinical Features
The joints more commonly affected are the knee, wrist, hip, shoulder, and elbow; TMJ involvement is uncommon. The condition occurs unilaterally and is more common in males. Patients may be asymptomatic or may complain of pain and joint swelling.
Radiographic Features
The radiographic appearance of chondrocalcinosis may simulate synovial chondromatosis, described previously. Often the radiopacities within the joint space are finer and have a more even distribution than in osteochondromatosis (Fig. 26-30). Bone erosions and a severe increase in condylar bone density also have been described. Erosions of the glenoid fossa may be present, which require CT for detection. Soft tissue swelling and edema of the surrounding muscles may be seen with MRI.
Trauma
Definition
Effusion is an influx of fluid into the joint, usually as a result of trauma (hemorrhage) or inflammation (exudate). Inflammation may result from an internal derangement, traumatic injuries, arthritis, or rheumatic diseases.
Clinical Features
The patient may have swelling over the affected joint; pain in the TMJ, preauricular region, or ear; and limited range of motion. Patients may also complain of the sensation of fluid in the ear, tinnitus, hearing difficulties, and difficulty occluding the posterior teeth.
Radiographic Features
Joint effusion is more commonly seen in conjunction with internal derangements, although it has been described in normal joints. The joint space is widened, and T2-weighted MRI studies may show a bright signal (white), indicating fluid adjacent to the disk or posterior to the condyle (see Fig. 26-19).
Differential Diagnosis
Effusion must be differentiated from septic arthritis; in the latter case the accompanying signs and symptoms of infection are present.
Treatment
Treatment may include anti-inflammatory drugs, although surgical drainage of the effusion occasionally is necessary.
Definition
Dislocation is abnormal positioning of the condyle out of the mandibular fossa but within the joint capsule. It usually occurs bilaterally and most commonly in an anterior direction. Dislocation may be caused by a failure of muscular coordination, subluxation, or external trauma and may be associated with a condylar fracture. Dislocation may occur into the middle cranial fossa as a result of trauma, but this is rare.
Clinical Features
In anterior dislocation, patients are unable to close the mandible to maximal intercuspation; some patients cannot reduce the dislocation, whereas others may be able to reduce the mandible by manipulation. In the former case associated pain and muscle spasm often are present.
Radiographic Features
In bilateral cases both condyles are located anterior and superior to the summits of the articular eminentia. Clinical information is important because the normal range of motion may extend anterior to the summit of the articular eminence.
Differential Diagnosis
The diagnosis is confirmed by the radiographic findings, although some fracture dislocations may be difficult to visualize, particularly if the dislocation is very slight. For this reason, CT or tomography is essential for diagnosis because routine plain film views may not show the dislocation because of anatomic superimpositions.
Treatment
Treatment consists of manual manipulation of the mandible to reduce the dislocation. Surgery occasionally is necessary to reduce the condyle in the case of a fracture dislocation, although treatment may not be indicated for this type of dislocation if mandibular function is adequate.
Definition
Fractures of the TMJ usually occur at the condylar neck and often are accompanied by dislocation of the condylar head. Fractures may be classified according to the anatomic location of the fracture: condylar head, condylar neck, and subchondral region. Occasionally more than one anatomic location is involved. On rare occasions the fracture may involve the temporal component.
Clinical Features
Unilateral fractures, which are more common than bilateral fractures, may be accompanied by a parasymphyseal or mandibular body fracture on the contralateral side. The patient may have swelling over the TMJ, pain, limited range of motion, and an anterior open bite. Some TMJ fractures are relatively asymptomatic and may not be discovered at the time of trauma; instead, these come to light as incidental findings at a later time when radiographs are taken for other reasons. Condylar fractures should be ruled out if the patient has a history of a blow to the mandible, especially to the anterior aspect.
If a condylar fracture occurs during the period of mandibular growth, growth may be inhibited because of damage to the condylar growth center. The degree of subsequent hypoplasia is related to the stage of mandibular development at the time of injury (younger patients have more profound hypoplasia) and the severity of the injury. Patients younger than 10 years old have a higher remodeling potential and may have less deformity compared with older patients, although injuries in patients younger than 3 years old tend to produce severe asymmetries. Injury to the joint may result in hemorrhage or effusion into the joint spaces that eventually may form bone during the healing process, which in turn may result in severe hypoplasia and limited joint function.
Radiographic Features
In relatively recent condylar neck fractures, a radiolucent line limited to the outline of the neck is visible. This line may vary in width, depending on whether the bone fragments are still aligned (narrow line) or displacement/dislocation has occurred (wider line). If the bone fragments overlap, an area of apparent increase in radiopacity may be seen instead of a radiolucent line (Fig. 26-31). Also, the outer cortical boundary may have an irregular outline or a step defect. Approximately 60% of condylar fractures show evidence of fragment angulation and a variable degree of displacement (dislocation) of the fracture ends. Fractures of the condylar head are less common and may be of the vertical (responsible for the traumatic type of bifid condyle) or compressive type (Fig. 26-32). CT is the preferred imaging modality to evaluate condylar fractures because there is no superimposition of adjacent structures and TMJ reformats provide images in several different planes. Two- and three-dimensional reformatted images are useful to accurately locate a fractured fragment. Alternatively, if CT is not available, multiple right-angle radiographic projections from the lateral, frontal, and basilar aspects may be used to detect a fracture.
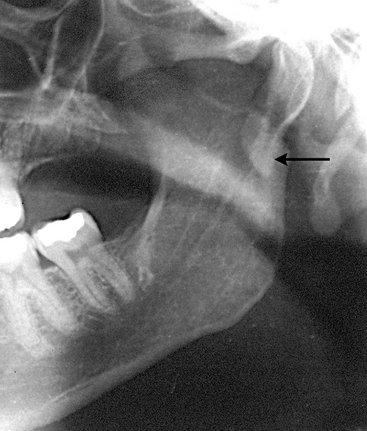
FIG. 26-31 Condylar neck fracture (panoramic image). The arrow points to overlapped fragments, as evidenced by increased radiopacity.
The amount of remodeling seen in the TMJ after a condylar fracture with medial displacement varies considerably. In some cases the condyle remodels to a form that is essentially normal, whereas in other cases the condyle and mandibular fossa become flattened, with loss of vertical height on the affected side. The condyle eventually may show degenerative changes, including flattening, erosion, osteophyte formation, and ankylosis. These changes are more severe if the condyle is displaced. Condylar fractures can also be associated with damage of the intracapsular soft tissues, including the disk, joint capsule and retrodiskal tissues, and with hemarthrosis and joint effusion.
Differential Diagnosis
Occasionally old fractures that have remodeled may be difficult to differentiate from developmental abnormalities of the condyle. The most common difficulty is in determining whether a fracture is indeed present. Panoramic views taken as an initial examination must be supplemented with a Towne’s view, especially if there is suspected medial displacement of the condylar head.
Treatment
Treatment may not be indicated if mandibular mobility is adequate; otherwise, the fracture is reduced surgically.
The use of forceps during delivery of neonates may result in fracture and displacement of the rudimentary condyle, which later manifests as severe mandibular hypoplasia and lack of development of the glenoid fossa and articular eminence. Such cases have a characteristic radiographic appearance in the panoramic image, having the appearance of a partly opened pair of scissors in place of a normal condyle (Fig. 26-33). This presentation results from the overlapping images of the medially displaced carrot-shaped condyle and remnants of the condylar neck.
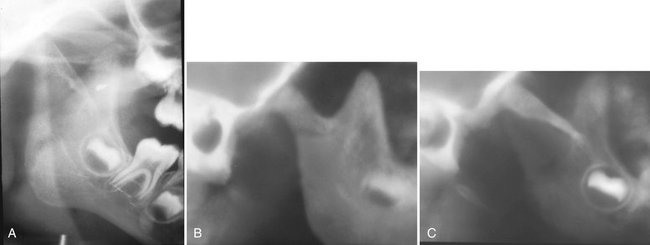
FIG. 26-33 A, A cropped panoramic image of a neonatal fracture of the right condyle. Note the unusual shape of the coronoid notch, similar to a partially opened pair of scissors. B, Tomographic image slice of the lateral aspect of the same joint. Note the normal-appearing coronoid notch but a lack of formation of the glenoid fossa and eminence and the abnormal anterior position of the condyle. C, Medial tomographic slice of the same case disclosing the fractured segment.
Differential Diagnosis
This condition often is not diagnosed until later in life, at which time a diagnosis of fracture may be made without a history that the fracture occurred at the time of birth. The condition must be differentiated from a developmental hypoplasia of the mandible, which is unrelated to birth injury.
Treatment
The fracture usually is not treated, but the mandibular asymmetry may be corrected with a combination of orthodontics and orthognathic surgery.
Definition
Ankylosis is a condition in which condylar movement is limited by a mechanical problem in the joint (“true” ankylosis) or by a mechanical cause not related to joint components (“false” ankylosis). True ankylosis may be bony or fibrous. In bony ankylosis the condyle or ramus is attached to the temporal or zygomatic bone by an osseous bridge. In fibrous ankylosis a soft tissue (fibrous) union of joint components occurs; the bone components appear normal. False ankylosis may result from conditions that inhibit condylar movement, such as muscle spasm, myositis ossificans, or coronoid process hyperplasia.
Clinical Features
Most unilateral cases are caused by mandibular trauma or infection. The most common cause of bilateral TMJ ankylosis is rheumatoid arthritis, although in rare cases bilateral fractures may be the cause. Most if not all cases of TMJ ankylosis in infancy occur as a result of birth injury. Patients have a history of progressively restricted jaw opening, or they may have a long-standing history of limited opening. Some degree of mandibular opening usually is possible through flexing of the mandible, although opening may be restricted to only a few millimeters, particularly in the case of bony ankylosis.
Radiographic Features
In fibrous ankylosis the articulating surfaces are usually irregular because of erosions. The joint space is usually very narrow and the two irregular surfaces may appear to fit one another like a jigsaw puzzle (see Fig. 26-26). Little or no condylar movement is seen. Radiographic signs of remodeling occasionally are visible as the joint components adapt to repeated attempts at mandibular opening. In bony ankylosis the joint space may be partly or completely obliterated by the osseous bridge, which can vary from a slender segment of bone, which may be difficult to locate, to a large bony mass. This extensive new bone may fuse the condyle to the cranial base (Fig. 26-34). Secondary degenerative changes of the joint components are common. Often morphologic changes occur, such as compensatory progressive elongation of the coronoid processes and deepening of the antegonial notch in the mandibular ramus on the affected side as a result of muscle function during attempted mandibular opening. If ankylosis occurs before mandibular growth is complete, growth of the affected side of the mandible is inhibited. Coronal CT images are the best diagnostic imaging method to evaluate ankylosis.

FIG. 26-34 Bony ankylosis (CT, coronal image slice, bone algorithm). The right condyle and ramus are markedly enlarged. The articulating surface is irregular, and the central and lateral aspects are fused to the roof of the glenoid fossa, as evidenced by a lack of joint space. Note that the left condylar articulating surface is eroded, and the joint space is decreased on the medial aspect; these changes are consistent with degenerative joint disease.
Differential Diagnosis
The major differential diagnosis is a condylar tumor. However, a history of trauma, infection, or other joint diseases should help rule out neoplastic disease. Detection of fibrous ankylosis is difficult because fibrous tissue is not visible in the radiographic image and therefore may be difficult to differentiate from false ankylosis.
Tumors
Benign and malignant tumors originating in or involving the TMJ are rare. Tumors may be intrinsic or extrinsic (adjacent) to the TMJ. Intrinsic tumors may develop in the condyle, temporal bone, or coronoid process. Extrinsic tumors may affect the morphology, structure, or function of the joint without invading the joint itself. They may cause indirect effects on growth, such as those seen with vascular lesions or from pressure, or may influence mandibular positioning.
The most common benign intrinsic tumors affecting the TMJ are osteomas, osteochondromas, Langerhans histiocytosis, and osteoblastomas. Chondroblastomas, fibromyxomas, benign giant cell lesions, and aneurysmal bone cysts also occur. Benign tumors and cysts of the mandible (e.g., ameloblastomas, odontogenic keratocysts, simple bone cysts) may involve the entire ramus and in rare cases the condyle. In cases of false ankylosis in which the TMJs appear radiographically normal, hyperplasia or a tumor of the coronoid process must be ruled out.
Clinical Features
Condylar tumors grow slowly and may attain considerable size before becoming clinically noticeable. Patients may complain of TMJ swelling, which may be accompanied by pain and decreased range of motion; the symptoms often mimic TMJ dysfunction. The clinical examination may reveal facial asymmetry, malocclusion, and deviation of the mandible to the unaffected side; these may be accompanied by symptoms of TMJ dysfunction. Tumors of the coronoid process typically are painless, but patients may complain of progressive limitation of motion.
Radiographic Features
Condylar tumors cause condylar enlargement that often is irregular in outline. The trabecular pattern may be altered, resulting in regions of destruction seen as radiolucencies or new abnormal bone formation, which may increase the radiopacity of the condyle with abnormal trabeculae. An osteoma or osteochondroma appears as an abnormal, pedunculated mass attached to the condyle (Fig. 26-35). Osteochondromas often extend from the anterior or superior surface of the condyle. Tumors of the coronoid process may affect TMJ function, which emphasizes the need to image and evaluate the coronoid process when evaluating joint abnormalities. The most common benign tumor is the osteochondroma. This tumor may interfere with joint function and erode adjacent osseous structures.
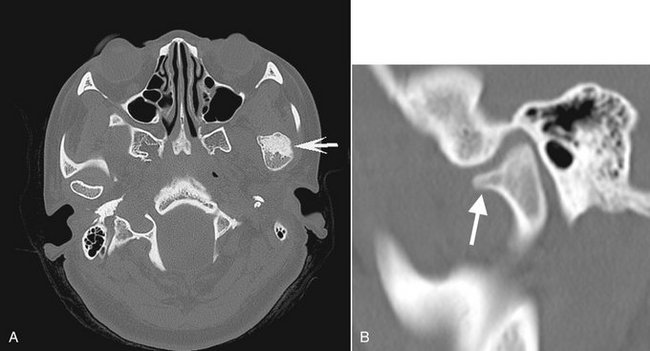
FIG. 26-35 A, Axial bone algorithm CT image of an osteochondroma extending from the anterior surface of the left condylar head (arrow). B, Sagittal reformat CT image of a different case; the internal aspect of the osteochondroma (arrow) is continuous with the cancellous portion of the condylar head.
Differential Diagnosis
Condylar neoplasms may simulate unilateral condylar hyperplasia because of condylar enlargement, although osteomas and osteochondromas give an irregular appearance, such as bulbous or globular expansion of the condyle or, more commonly, a pedunculated growth. Also, the characteristic condylar shape and proportions are better preserved in condylar hyperplasia. Coronoid tumors must be differentiated from coronoid hyperplasia, which differs from a condylar tumor in that the coronoid process remains regular in shape.
Treatment
Treatment consists of surgical excision of the tumor and occasionally excision of the condylar head or coronoid process.
Malignant tumors of the jaws may be primary or, more commonly, metastatic. Primary intrinsic malignant tumors of the condyle are extremely rare and include chondrosarcoma, osteogenic sarcoma, synovial sarcoma, and fibrosarcoma of the joint capsule. Extrinsic malignant tumors may represent direct extension of adjacent parotid salivary gland malignancies, rhabdomyosarcoma (particularly in children), or other regional carcinomas from the skin, ear, and nasopharynx. The most common metastatic lesions include neoplasms originating in the breast, kidney, lung, colon, prostate, and thyroid gland.
Clinical Features
Malignant tumors (primary or metastatic) may be asymptomatic or patients may have symptoms of TMJ dysfunction such as pain, limited mandibular opening, mandibular deviation, and swelling. Unfortunately, a patient occasionally is treated for TMJ dysfunction without recognition that the underlying condition is a malignancy.
Radiographic Features
Malignant primary and metastatic TMJ tumors appear as a variable degree of bone destruction with ill-defined, irregular margins. Most lack tumor bone formation, with the exception of osteogenic sarcoma. Chondrosarcoma may appear as an indistinct, essentially radiolucent destructive lesion of the condyle with surrounding discrete soft tissue calcifications that may simulate the appearance of the articular loose bodies seen in chondrocalcinosis or pseudogout (Fig. 26-36). In the case of metastatic tumors, the radiographic appearance usually is nonspecific condylar destruction (with a few exceptions, such as metastatic prostate carcinoma) and does not indicate the site of origin (Fig. 26-37). CT is the imaging modality of choice to view bone involvement and MRI is useful for displaying the extent of involvement into the surrounding soft tissues.
Differential Diagnosis
Joint destruction caused by a malignant tumor must be differentiated from the osseous destruction seen in severe DJD. Malignant tumors cause profound central bone destruction, whereas DJD causes more peripheral bone destruction. Proliferative changes such as osteophyte formation may be seen in DJD, but unlike with a malignant tumor, no soft tissue mass or swelling is evident. Chondrosarcoma may simulate joint space calcifications (discussed earlier), but in the case of malignancy, severe bone destruction also occurs.
Treatment
In the case of primary malignant tumors, treatment consists of wide surgical removal of the tumor. Tumor extension to vital anatomic structures may compromise survival. Metastatic tumors of the TMJ rarely are treated surgically; treatment mainly is palliative and may include radiotherapy and chemotherapy.
DISORDERS OF THE TEMPOROMANDIBULAR JOINT
Brooks, SL, Brand, JW, Gibbs, SJ, et al. Imaging of the temporomandibular joint, position paper of the American Academy of Oral and Maxillofacial Radiology [review]. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1997;83:609–618.
Helkimo, M. Studies on function and dysfunction of the masticatory system, II: index for anamnestic and clinical dysfunction and occlusal state. Sven Tandlak Tidskr. 1974;67:101–121.
McNeill, C, Mohl, ND, Rugh, JD, et al. Temporomandibular disorders: diagnosis, management, education, and research. J Am Dent Assoc. 1990;120:253. 255, 257
Petrikowski, CG, Grace, MG. Temporomandibular joint radiographic findings in adolescents. Cranio. 1996;14:30–36.
Rugh, JD, Solberg, WK. Oral health status in the United States: temporomandibular disorders. J Dent Educ. 1985;49:398–406.
Wänman, A, Agerberg, G. Mandibular dysfunction in adolescents, I: prevalence of symptoms. Acta Odontol Scand. 1986;44:47–54.
ANATOMY OF THE TEMPOROMANDIBULAR JOINT
Blaschke, DD, Blaschke, TJ. A method for quantitatively determining temporomandibular joint bony relationships. J Dent Res. 1981;60:35–43.
Drace, JE, Enzmann, DR. Defining the normal temporomandibular joint: closed, partially open, and open mouth MR imaging of asymptomatic subjects. Radiology. 1990;177:67–76.
Hansson, LG, Hansson, T, Petersson, A. A comparison between clinical and radiologic findings in 259 temporomandibular joint patients. J Prosthet Dent. 1983;50:89–94.
Ingervall, B, Carlsson, GE, Thilander, B. Postnatal development of the human temporomandibular joint. II. A microradiographic study. Acta Odont Scand. 1976;34:133–139.
Larheim, TA. Radiographic appearance of the normal temporomandibular joint in newborns and small children. Acta Radiol Diagn (Stockh). 1981;22:593–599.
Pullinger, AG, Hollender, L, Solberg, WK, et al. A tomographic study of mandibular condyle position in an asymptomatic population. J Prosthet Dent. 1985;53:706–713.
Taylor, RC, Ware, WH, Fowler, D, et al. A study of temporomandibular joint morphology and its relationship to the dentition. Oral Surg. 1972;33:1002–1013.
Ten Cate, AR. Gross and micro anatomy. In Zarb GA, Carlsson BJ, Mohl ND, eds.: Temporomandibular joint and masticatory muscle disorders, ed 2, Copenhagen: Munksgaard, 1994.
Westesson, P-L, Kurita, K, Eriksson, L, et al. Cryosectional observations of functional anatomy of the temporomandibular joint. Oral Surg Oral Med Oral Pathol. 1989;68:247–251.
Yale, SH, Allison, BD, Hauptfuehrer, JD. An epidemiological assessment of mandibular condyle morphology. Oral Surg. 1966;21:169–177.
DIAGNOSTIC IMAGING OF THE TEMPOROMANDIBULAR JOINT
Brooks, SL, Brand, AW, Gibbs, SJ, et al. Imaging of the temporomandibular joint, position paper of the American Academy of Oral and Maxillofacial Radiology. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1997;83:609–618.
Helms, CA, Kaplan, P. Diagnostic imaging of the temporomandibular joint: recommendations for use of the various techniques. AJR Am J Roentgenol. 1990;154:319–322.
Katzberg, RW. Temporomandibular joint imaging. Radiology. 1989;170:297–307.
Christiansen, EL, Chan, TT, Thompson, JR, et al. Computed tomography of the normal temporomandibular joint. Scand J Dent Res. 1987;95:499–509.
Coin, CG. Tomography of the temporomandibular joint. Med Radiogr Photogr. 1974;50:26–39.
Tsiklakis, K, Syriopoulos, K, Stamatakis, HC. Radiographic examination of the temporomandibular joint using cone beam computed tomography. Dentomaxillofac Radiol. 2004;33:196–201.
Conway, WF, Hayes, CW, Campbell, RL. Dynamic magnetic resonance imaging of the temporomandibular joint using FLASH sequences. J Oral Maxillofac Surg. 1988;46:930–938.
Hansson, LG, Westesson, PL, Eriksson, L. Comparison of tomography and midfield magnetic resonance imaging for osseous changes of the temporomandibular joint. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1996;82:698–703.
Moses, JJ, Salinas, E, Goergen, T, et al. Magnetic resonance imaging or arthrographic diagnosis of internal derangement of the temporomandibular joint. Oral Surg Oral Med Oral Pathol. 1993;75:268–272.
Tomas, X, Pomes, J, Berenquer, J, et al. MR Imaging of temporomandibular joint dysfunction: a pictorial review. Radiographics. 2006;26:765–781.
Gray, RJM, Sloan, P, Quayle, AA, et al. Histopathological and scintigraphic features of condylar hyperplasia. Int J Oral Maxillofac Surg. 1990;19:65–71.
Rubenstein, LK, Campbell, RL. Acquired unilateral condylar hyperplasia and facial asymmetry: report of a case. ASDC J Dent Child. 1985;52:114–120.
Shira, RB. Facial asymmetry and condylar hyperplasia. Oral Surg. 1975;40:567.
Wolford, LM, Mehra, P, Reiche-Fischel, O, et al. Efficacy of high condylectomy for management of condylar hyperplasia. Am J Orthod Dentofacial Orthop. 2002;121:136–151.
Jerell, RG, Fuselier, B, Mahan, P. Acquired condylar hypoplasia: report of a case. ASDC J Dent Child. 1991;58:147–153.
Worth, HM. Radiology of the temporomandibular joint. In: Zarb GA, Carlsson BJ, Mohl ND, eds. Temporomandibular joint function and dysfunction. Copenhagen: Munksgaard, 1979.
Boering, G. Temporomandibular joint arthrosis and facial deformity. Trans Int Conf Oral Surg. 1967:258–260.
Worth, HM. Radiology of the temporomandibular joint. In: Zarb GA, Carlsson BJ, Mohl ND, eds. Temporomandibular joint function and dysfunction. Copenhagen: Munksgaard, 1979.
McLoughlin, PM, Hopper, C, Bowley, NB. Hyperplasia of the mandibular coronoid process: an analysis of 31 cases and a review of the literature. J Oral Maxillofac Surg. 1995;53:250–255.
Satoh, K, Ohno, S, Aizawa, T, et al. Bilateral coronoid hyperplasia in an adolescent: report of a case and review of the literature. J Oral Maxillofac Surg. 2006;64:334–338.
Daniels, JSM, Ali, I. Post-traumatic bifid condyle associated with temporomandibular joint ankylosis: report of a case and review of the literature. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2005;99:682–688.
Loh, FC, Yeo, JF. Bifid mandibular condyle. Oral Surg Oral Med Oral Pathol. 1990;69:24–27.
Dolwick, MF, Sanders, B. TMJ internal derangement and arthrosis. In: Surgical atlas. St. Louis: Mosby; 1985.
Helms, CA, Kaban, LB, McNeill, C, et al. Temporomandibular joint: morphology and signal intensity characteristics of the disk at MR imaging. Radiology. 1989;172:817–820.
Katzberg, RW. Temporomandibular joint imaging. Radiology. 1989;170:297.
Katzberg, RW, Tallents, RH, Hayakawa, K, et al. Internal derangements of the temporomandibular joint: findings in the pediatric age group. Radiology. 1985;154:125–127.
Larheim, TA. Current trends in temporomandibular joint imaging. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1995;80:555–576.
Nuelle, DG, Alpern, MC, Ufema, JW. Arthroscopic surgery of the temporomandibular joint. Angle Orthod. 1986;56:118–142.
Rammelsberg, P, Pospiech, PR, Jäger, L, et al. Variability of disk position in asymptomatic volunteers and patients with internal derangements of the TMJ. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1997;83:393–399.
Sano, T, Westesson, P-L. Magnetic resonance imaging of the temporomandibular joint: increased T2 signal in the retro-diskal tissue of painful joints. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1995;79:511–516.
Wilkes, CH. Internal derangements of the temporomandibular joint: pathological variations. Arch Otolaryngol Head Neck Surg. 1989;115:469–477.
Brooks, SL, Westesson, PL, Eriksson, L, et al. Prevalence of osseous changes in the temporomandibular joint of asymptomatic persons without internal derangement. Oral Surg Oral Med Oral Pathol. 1992;73:118–122.
Moffett, BC, Johnson, LC, McCabe, JB, et al. Articular remodeling in the adult human temporomandibular joint. Am J Anat. 1964;115:119–141.
de Leeuw, R, Boering, G, Stegenga, B, et al. Temporomandibular joint osteoarthrosis: clinical and radiographic characteristics 30 years after nonsurgical treatment—a preliminary report. Cranio. 1993;11:15–24.
Helenius, LMJ, Tervahartiala, P, Helenius, I, et al. Clinical, radiographic and MRI findings of the temporomandibular joint in patients with different rheumatic diseases. Int J Oral Maxillofac Surg. 2006;35:983–989.
Kurita, H, Uehara, S, Yokochi, M, et al. A long-term follow-up study of radiographically evident degenerative changes in the temporomandibular joint with different conditions of disk displacement. Int J Oral Maxillfoacial Surg. 2006;35:49–54.
Mayne, JG, Hatch, GS. Arthritis of the temporomandibular joint. J Am Dent Assoc. 1969;79:125–130.
Radin, EL, Paul, IL, Rose, RM. Role of mechanical factors in pathogenesis of primary osteoarthritis. Lancet. 1972;1:519–522.
Sato, H, Fujii, T, Yamada, N, et al. Temporomandibular joint osteoarthritis: a comparative clinical and tomographic study pre- and post-treatment. J Oral Rehabil. 1994;21:383–395.
Gynther, GW, Tronje, G, Holmlund, AB. Radiographic changes in the temporomandibular joint in patients with generalized osteoarthritis and rheumatoid arthritis. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1996;81:613–618.
Larheim, TA, Smith, HJ, Aspestrand, F. Rheumatic disease of the temporomandibular joint: MR imaging and tomographic manifestations. Radiology. 1990;175:527–531.
Syrjänen, SM. The temporomandibular joint in rheumatoid arthritis. Acta Radiol Diagn (Stockh). 1985;26:235–243.
Ganik, R, Williams, FA. Diagnosis and management of juvenile rheumatoid arthritis with TMJ involvement. Cranio. 1986;4:254–262.
Hu, Y-S, Schneiderman, ED. The temporomandibular joint in juvenile rheumatoid arthritis, I: computed tomographic findings. Pediatr Dent. 1995;17:46–53.
Hu, Y-S, Schneiderman, ED, Harper, RP. The temporomandibular joint in juvenile rheumatoid arthritis, II: relationship between computed tomographic and clinical findings. Pediatr Dent. 1996;18:312–319.
Karhulahti, T, Ylijoki, H, Rönning, O. Mandibular condyle lesions related to age at onset and subtypes of juvenile rheumatoid arthritis in 15-year-old children. Scand J Dent Res. 1993;101:332–338.
Koorbusch, GF, Zeitler, DL, Fotos, PG, et al. Psoriatic arthritis of the temporomandibular joints with ankylosis. Oral Surg Oral Med Oral Pathol. 1991;71:267–274.
Wilson, AW, Brown, JS, Ord, RA. Psoriatic arthropathy of the temporomandibular joint. Oral Surg Oral Med Oral Pathol. 1990;70:555–558.
Locher, MC, Felder, M, Sailer, HF. Involvement of the temporomandibular joints in ankylosing spondylitis (Bechterew’s disease). J Craniomaxillofac Surg. 1996;24:205–213.
Ramos-Remus, C, Major, P, Gomez-Vargas, A, et al. Temporomandibular joint osseous morphology in a consecutive sample of ankylosing spondylitis patients. Ann Rheum Dis. 1997;56:103–107.
Leighty, SM, Spach, DH, Myall, RW, et al. Septic arthritis of the temporomandibular joint: review of the literature and report of two cases in children. Int J Oral Maxillofac Surg. 1993;22:292–297.
Sembronio, S, Albiero, AM, Robiony, M, et al. Septic arthritis of the temporomandibular joint successfully treated with arthroscopic lysis and lavage: case report and review of the literature. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2007;103:e1–6.
Ardekian, L, Faquin, W, Troulis, MJ, et al. Synovial chondromatosis of the temporomandibular joint: report and analysis of eleven cases. J Oral Maxillofac Surg. 2005;63:941–947.
Carls, FR, von Hochstetter, A, Engelke, W, et al. Loose bodies in the temporomandibular joint. J Craniomaxillofac Surg. 1995;23:215–221.
Chuong, R, Piper, MA. Bilateral pseudogout of the temporomandibular joint: report of a case and review of the literature. J Oral Maxillofac Surg. 1995;53:691–694.
Dijkgraaf, LC, Liem, RS, de Bont, LG, et al. Calcium pyrophosphate dihydrate crystal deposition disease: a review of the literature and a light and electron microscopic study of a case of the temporomandibular joint with numerous intracellular crystals in the chondrocytes. Osteoarthritis Cartilage. 1995;3:35–45.
Lustmann, J, Zeltser, R. Synovial chondromatosis of the temporomandibular joint: review of the literature and case report. Int J Oral Maxillofac Surg. 1989;18:90–94.
Orden, A, Laskin, DM, Lew, D. Chronic preauricular swelling. J Oral Maxillofac Surg. 1989;47:390–397.
Pynn, BR, Weinberg, S, Irish, J. Calcium pyrophosphate dihydrate deposition disease of the temporomandibular joint: a case report and review of the literature. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1995;79:278–284.
Yu, Q, Yang, J, Wang, P, et al. CT features of synovial chondromatosis in the temporomandibular joint. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2007;97:524–528.
Emshoff, R, Brandimaier, I, Bertram, S, et al. Magnetic resonance imaging findings of osteoarthrosis and effusion in patients with unilateral temporomandibular joint pain. Int J Oral Maxillofac Surg. 2002;31:598–602.
Schellhas, KP, Wilkes, CH. Temporomandibular joint inflammation: comparison of MR fast scanning with T1- and T2-weighted imaging techniques. AJR Am J Roentgenol. 1989;153:93–98.
Schellhas, KP, Wilkes, CH, Baker, CC. Facial pain, headache, and temporomandibular joint inflammation. Headache. 1989;29:229–232.
Westesson, P-L, Brooks, SL. Temporomandibular joint: relationship between MR evidence of effusion and the presence of pain and disk displacement. AJR Am J Roentgenol. 1992;159:559.
Kai, S, Kai, H, Nakayama, E, et al. Clinical symptoms of open lock position of the condyle: relation to anterior dislocation of the temporomandibular joint. Oral Surg Oral Med Oral Pathol. 1992;74:143–148.
Ohura, N, Ichioka, S, Sudo, T, et al. Dislocation of the bilateral mandibular condyle into the middle cranial fossa: review of the literature and clinical experience. J Oral Maxillofac Surg. 2006;64:1165–1172.
Wijmenga, JP, Boering, G, Blankestijn, J. Protracted dislocation of the temporomandibular joint. Int J Oral Maxillofac Surg. 1986;15:380–388.
Choi, J, Oh, I-K. A follow-up study of condyle fracture in children. Int J Oral Maxillofac Surg. 2005;34:851–858.
Dahlström, L, Kahnberg, KE, Lindahl, L. Fifteen years follow-up on condylar fractures. Int J Oral Maxillofac Surg. 1989;18:18–23.
Gerhard, S, Ennemoser, T, Rudisch, A, et al. Condylar injury: magnetic resonance imaging findings of the temporomandibular joint soft tissue changes. Int J Oral Maxillofac Surg. 2007;36:214–218.
Horowitz, I, Abrahami, E, Mintz, SS. Demonstration of condylar fractures of the mandible by computed tomography. Oral Surg. 1982;54:263–268.
Lindahl, L, Hollender, L. Condylar fractures of the mandible, II: a radiographic study of remodeling processes in the temporomandibular joint. Int J Oral Surg. 1977;6:153–165.
Pharoah, MJ. Radiology of the temporomandibular joint. In Zarb GA, Carlsson BJ, Mohl ND, eds.: Temporomandibular joint and masticatory muscle disorders, ed 2, Copenhagen: Munksgaard, 1994.
Raustia, AM, Pyhtinen, J, Oikarinen, KS, et al. Conventional radiographic and computed tomographic findings in cases of fracture of the mandibular condylar process. J Oral Maxillofac Surg. 1990;48:1258–1264.
Schellhas, KP. Temporomandibular joint injuries. Radiology. 1989;173:211–216.
Pharoah, MJ. Radiology of the temporomandibular joint. In Zarb GA, Carlsson BJ, Mohl ND, eds.: Temporomandibular joint and masticatory muscle disorders, ed 2, Copenhagen: Munksgaard, 1994.
Worth, HM. Radiology of the temporomandibular joint. In: Zarb GA, Carlsson GE, eds. Temporomandibular joint function and dysfunction. Copenhagen: Munksgaard, 1979.
Ferretti, C, Bryant, R, Becker, P, et al. Temporomandibular joint morphology following post-traumatic ankylosis in 26 patients. Int J Oral Maxillofac Surg. 2005;34:376–381.
Rowe, NL. Ankylosis of the temporomandibular joint. J R Coll Surg Edinb. 1982;27:67–79.
Wood, RE, Harris, AM, Nortjé, et al. The radiologic features of true ankylosis of the temporomandibular joint: an analysis of 25 cases. Dentomaxillofac Radiol. 1988;17:121–127.
James, RB, Alexander, RW, Traver, JG, Jr. Osteochondroma of the mandibular coronoid process: report of a case. Oral Surg. 1974;37:189–195.
Nwoku, AL, Koch, H. The temporomandibular joint: a rare localisation for bone tumors. J Maxillofac Surg. 1974;2:113–119.
Pharoah, MJ. Radiology of the temporomandibular joint. In Zarb GA, Carlsson BJ, Mohl ND, eds.: Temporomandibular joint and masticatory muscle disorders, ed 2, Copenhagen: Munksgaard, 1994.
Svensson, B, Isacsson, G. Benign osteoblastoma associated with an aneurysmal bone cyst of the mandibular ramus and condyle. Oral Surg Oral Med Oral Pathol. 1993;76:433–436.
Thoma, KH. Tumors of the mandibular joint. J Oral Surg Anesth Hosp Dent Serv. 1964;22:157–167.
Worth, HM. Radiology of the temporomandibular joint. In: Zarb GA, Carlsson GE, eds. Temporomandibular joint function and dysfunction. Copenhagen: Munksgaard, 1979.
Morris, MR, Clark, SK, Porter, BA, et al. Chondrosarcoma of the temporomandibular joint: case report. Head Neck Surg. 1987;10:113–117.
Rubin, MM, Jui, V, Cozzi, GM. Metastatic carcinoma of the mandibular condyle presenting as temporomandibular joint syndrome. J Oral Maxillofac Surg. 1989;47:507–510.
Takehana dos Santos, D, Cavalcanti, MGP. Osteosarcoma of the temporomandibular joint: report of 2 cases. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2002;94:641–647.