DISPLACEMENT AND VOLVULUS OF THE LARGE (ASCENDING) COLON
Syndromes: nephrosplenic entrapment, renosplenic entrapment, left dorsal displacement of the large colon, right dorsal displacement of the large colon.
ETIOLOGY
• Left dorsal displacement of the large colon (renosplenic or nephrosplenic entrapment and entrapment of the large colon lateral to the spleen)
Etiology Unknown, probably involves disturbance of colonic motility
Epidemiology Volvulus is more common in mares during late gestation or after parturition. Left dorsal displacement (renosplenic entrapment) may be more common in large male horses
Clinical signs Left displacement of the large colon causes signs of mild to moderate colic. Rectal examination reveals large colon in the renosplenic space and ultrasonographic examination confirms the diagnosis. Right dorsal colon displacement causes mild to moderate colic. Rectal examination reveals colon lateral to the base of the cecum. Volvulus of the large colon causes mild to extremely severe abdominal pain, tachycardia, shock and abdominal distension. Rectal examination reveals the distended, displaced colon
Clinical pathology None diagnostic
Diagnostic confirmation Physical examination, laparotomy, necropsy examination
Treatment Volvulus and right dorsal displacement should be treated by surgical correction. Left dorsal displacement can be corrected by rolling the anesthetized horse or jogging the horse after administration of phenylephrine
The etiology of these conditions is unknown but presumably involves some disturbance to normal colonic motility. Other causes of obstruction of the large colon include congenital abnormalities of the right ventral colon,1 cystic duplication of the ascending colon,2 defects in the mesocolon3 and incarceration in epiploic foramen or gastrosplenic ligament.4,5 Intussusception of the large colon causes infarction and severe colic.5
The term volvulus refers to rotation of the segment of bowel about the long axis of its mesentery, while torsion refers to rotation about the long axis of the bowel. Because of the anatomical arrangement of the mesocolon, either term may be correctly used to describe displacements of the large intestine.5
EPIDEMIOLOGY
Left dorsal displacement of the large colon (Fig. 5.1) is the cause of 2–10% of colic cases referred for specialist treatment.6 There is no breed, age or sex predisposition, although some authors suggest that males and large horses are more likely to be affected. The case fatality rate is approximately 5% for horses treated correctly.7-10
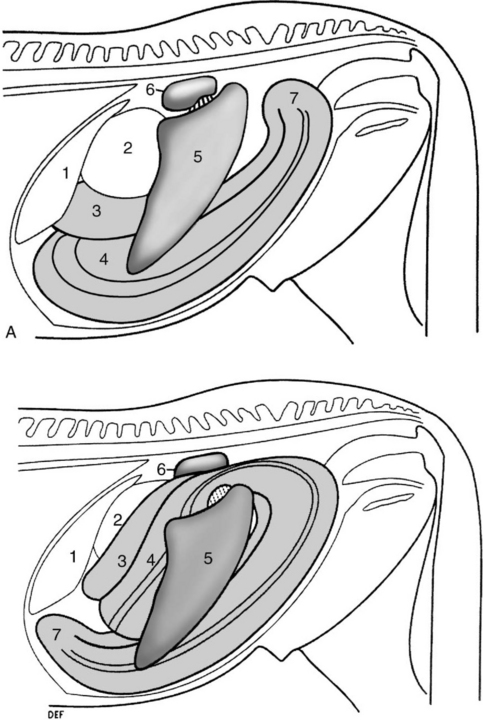
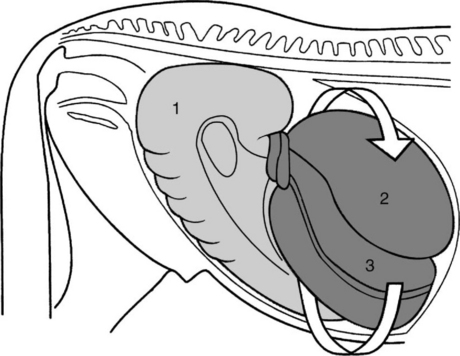
Fig. 5.1 A Left lateral view of abdomen of a normal horse. B Left dorsal displacement of the left colon, left lateral view. The left ventral and dorsal colon is displaced lateral and dorsal to the spleen and occupies the renosplenic space. 1 = liver, 2 = stomach, 3 = left dorsal colon, 4 = left ventral colon, 5 = spleen, 6 = left kidney and renosplenic ligament, 7 = pelvic flexure.
(With permission from Johnston JK, Freeman DE. Vet Clin North Am Equine Pract 1997; 13:317.)
Right dorsal displacement of the large colon (Fig. 5.2) occurs sporadically and without recognized risk factors. The case fatality rate is reported to be as high as 43%.10
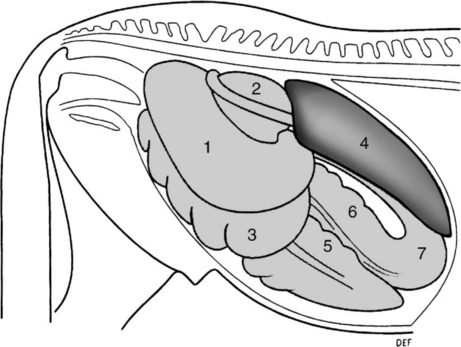
Fig. 5.2 Right dorsal displacement of the colon, right lateral view. The colon has passed lateral to the cecum, the pelvic flexure is displaced cranially and the sternal and diaphragmatic flexures are displaced caudally. 1 = right dorsal colon, 2 = base of cecum, 3 = right ventral colon, 4 = liver, 5 = cecum, 6 = left ventral colon, 7 = pelvic flexure.
(With permission from Johnston JK, Freeman DE. Vet Clin North Am Equine Pract 1997; 13:317.)
Risk factors for noninfarctive displacement of the large colon include cribbing or wind sucking (odds ratio (OR) = 90), number of hours stabled per day (OR for 24 h stabling = 35), lack of regular exercise (OR = 3.3), change in exercise program (OR = 9), lack of anthelmintic administration (OR = 13) and history of transport in the previous 24 hours (OR = 17).11
Volvulus of the large colon is the cause of colic in 11–17% of colic cases in which abdominal surgery is performed.12 The disease occurs commonly in mares, especially those late in gestation or having recently foaled.13,14 The disease has a recurrence rate of up to 15% in brood mares.15 The disease occurs in horses from 2 days of age and there does not appear to be an effect of breed on occurrence of the disease.16 The case fatality rate varies depending on the extent of the volvulus, with lesser degrees of volvulus (< 270°) having a 30% fatality rate and volvulus of 360° or more having a 65% fatality rate.13
Ingestion of large quantities of grain, such as might be fed to horses in heavy work, is associated with changes in plasma electrolyte concentrations, presence of dehydrated, foamy and homogeneous right dorsal colon contents, and fetid, less formed feces.17 These effects of a high-grain diet may be associated with colonic disease in horses.17
PATHOGENESIS
Proximate factors leading to volvulus or displacement are unknown, although risk factors have been identified (see above). A plausible scenario is that altered colonic motility and subsequent distension with gas or ingesta predisposes the colon to displacement, either spontaneously or as a result of the horse rolling or lying down in response to abdominal pain.
Left dorsal and right dorsal displacements of the colon rarely compromise colon blood flow and represent nonstrangulating obstructive lesions. Pathogenesis in equine colic section). The displacement of the large colon (Figs 5.1 & 5.2) impedes aboral movement of ingesta and gas and may result in colonic distension. Should the distension become sufficiently severe, colon blood flow will be impaired and cause ischemia and necrosis of the colon. The obstruction to blood flow is predominantly in venous drainage, resulting in hemorrhagic strangulating obstruction with progressive development of intramural edema, extravasation of red blood cells, microvascular thrombosis, mesothelial cell loss from the serosal surface, and mucosal necrosis with loss of colonic epithelium.18
Volvulus of the large colon of less than 270° does not compromise blood supply but does impede aboral movement of ingesta and gas.13 Volvulus of 360° or more causes ischemia through occlusion of both arterial and venous circulation of the involved large colon with rapid loss of colonic mucosal integrity and colon viability. Irreversible mucosal damage occurs after 3–4 hours of ischemia. Loss of mucosal integrity impairs normal barrier function and permits toxins and substances normally confined to the colonic lumen to enter the systemic circulation. Additionally, loss of barrier function allows leakage of vascular proteins and in severe cases red blood cells into the colonic lumen. Subsequent signs are typical of strangulating obstruction (see Equine colic) with development of toxemia, cardiovascular collapse and death within 12–18 hours.
The most common displacement is medial and dorsal movement of the ventral colon to complete a 360° volvulus of the large intestine (Fig. 5.3).16 Lateral and dorsal displacement of the ventral colon is much less common. The volvulus is usually at the level of the cecocolic fold, although volvulus involving the cecum or at the diaphragmatic and sternal flexures does occur.
CLINICAL FINDINGS
Left dorsal displacement (renosplenic entrapment)
The disease usually has an acute onset and a duration of up to 4 days, although it can be a cause of chronic, recurrent colic.6,9 Abdominal pain in the initial stages is mild to moderate and becomes progressively more severe as distension of the large colon develops. The heart rate is usually between 50 and 70/min, but may be as low as 30/min. Rectal temperature is within normal limits. Mucous membrane color and refill time are usually normal provided that there is no ischemia of the colon. Abdominal distension is appreciable in some affected horses.6 There is more than 2 L of reflux from a nasogastric tube in approximately 28% of cases, although rarely is there profuse reflux.9 Rectal examination reveals the presence of bowel in the renosplenic space in approximately 70% of cases with the typical finding of taenia of the ventral colon being traced into that space. Distension of the large colon may impair detection of bowel in the nephrosplenic space. The spleen is usually displaced caudally, medially and ventrally from its normal position against the left body wall (Fig. 5.1).
Ultrasonographic demonstration of colon in the renosplenic space confirms the diagnosis with an accuracy of 88%.19 Gas in the displaced colon obscures the left kidney and dorsal border of the spleen normally visible on ultrasonographic examination of the left paralumbar region.19
Approximately 8% of horses with nephrosplenic entrapment have an additional lesion.9 Entrapment in which the sternal and diaphragmatic flexures are displaced cranial to the stomach and liver occurs in less than 3% of cases.9
Right dorsal displacement
Severity of colic varies from mild to severe in horses with right dorsal displacement of the colon. Tachycardia (50–80/min) and mild abdominal distension are characteristic provided that the entrapped bowel is not ischemic. There is usually no reflux from a nasogastric tube, although as the disease progresses gastric distension may occur. Rectal examination reveals the presence of large colon lateral to the base of the cecum, although colonic distension may make detection of the displaced bowel difficult. Right dorsal displacement is a not uncommon sequel to impaction of the pelvic flexure.
Volvulus
The onset of pain is abrupt and the duration of the disease ranges from hours, in horses with strangulating lesions, to days in horses with torsion of less than 270°. The pain ranges from mild to severe and intractable, with the horse violently throwing itself to the ground. Pain in horses with volvulus of 360° or greater is often unresponsive to any analgesics. Heart rate is variable and may be less than 40/min in horses with severe disease, although usually it is more than 60/min and increases with severity of the disease. Rectal temperature is within the normal range. The mucous membranes are dark red to blue and capillary refill time is more than 3 seconds in severely affected horses. Abdominal distension is marked, usually severe, and may impair respiration in horses with 360° or greater volvulus. Auscultation of the abdomen reveals a lack of borborygmi and the presence of high-pitched, tympanitic ‘pings’ on simultaneous percussion and auscultation. The pings are due to the presence of gas in tightly distended large colon or cecum. There is usually no reflux through a nasogastric tube. Rectal examination may be limited by the distended, gas-filled colon occupying the caudal abdomen. In untreated cases death occurs within 12–24 hours from cardiovascular collapse. Ultrasonographic examination reveals colon with a mural thickness of 9 mm or greater in horses with colon torsion. The test has a sensitivity of approximately 67% (i.e. correctly predicts presence of colon torsion in two-thirds of horses that have the disease) and specificity of 100% (correctly rules out the diagnosis in 100% of horses that do not have the disease).20
CLINICAL PATHOLOGY
Changes in the hemogram, serum biochemical profile and peritoneal fluid are non-existent to mild in horses with uncomplicated left dorsal displacement, right dorsal displacement and volvulus of less than 270°. Horses with ischemic colon as a result of strangulation usually have a leukopenia with left shift, hemoconcentration and increased anion gap.16
Serum gamma glutamyl transferase (GGT) activity is elevated in approximately 50% of horses with right dorsal displacement of the colon, whereas such elevations are rare in horses with left dorsal displacement.21 The elevated GGT, and less commonly serum bilirubin concentration, in horses with right dorsal displacement is attributable to compression of the common bile duct in the hepatoduodenal ligament by the displaced colon.21
Horses with large-colon volvulus have a high prevalence of abnormalities in hemostatic variables, including thrombin– antithrombin concentration, d-dimer concentration, antithrombin activity, prothrombin time and platelet count. Nonsurviving horses have lower platelet counts, increased prothrombin time and reduced antithrombin activity.22
Peritoneal fluid often has an increased total protein concentration (> 25 g/L, 2.5 g/dL) and white blood cell count (> 8000 cells/μL, 8 × 109 cells/L) in horses with compromised bowel. Examination of peritoneal fluid is often not necessary to achieve a diagnosis in horses with colon torsion, although it does have prognostic value in that horses with blood-tinged peritoneal fluid have a poor prognosis. The risk of inadvertent enterocentesis is increased in horses with severe distension of the colon and abdominocentesis should be attempted with caution in such cases. Use of a bovine teat cannula or similar blunt instrument is preferred to the use of a needle.
NECROPSY FINDINGS
The colon is displaced as described above for each of the diseases. Death usually results from ischemic necrosis of the colon and the associated peritonitis, endotoxemia and shock. Histological lesions in horses dying of colon volvulus are more severe than of those that survive and are characterized by hemorrhage into the lamina propria, edema and loss of the mucosal cells and crypt architecture.13
TREATMENT
Treatment should consist of pain control, correction of fluid, acid–base and electrolyte abnormalities, support of cardiovascular function and correction of the underlying disease (Equine colic). Decompression by trocarization of gas-distended colon or cecum may be beneficial. Correction of colon volvulus or right dorsal displacement of the colon requires surgical exploration of the abdomen and manual correction of the displacement.
Left displacement
Correction of left dorsal displacement can be achieved by either nonsurgical or surgical means. Nonsurgical correction is achieved by rolling the anesthetized horse in a particular sequence that causes the displaced colon to return to its normal position in the abdomen. Nonsurgical correction is successful in approximately 80% of cases,7,27 although complications are reported,28 and is recommended as the initial definitive treatment for horses with uncomplicated left dorsal displacement.27 The sequence of events following diagnosis of the condition is depicted in Figure 5.4.29 Phenylephrine (0.02–0.04 mg/kg, intravenously as a 10 min infusion) causes splenic contraction and is thought to increase the chances of the colon returning to its normal position. The horse is anesthetized within 10 minutes of phenylephrine administration and placed in right lateral recumbency. The horse is then slowly rolled into dorsal recumbency and the abdomen is vigorously massaged in an attempt to cause the colon to move ventrally and medially. If a hoist is available the horse can be lifted into dorsal recumbency. The sequence ends with the horse being rolled into left lateral recumbency and a rectal or ultrasound examination being performed to determine the position of the colon.
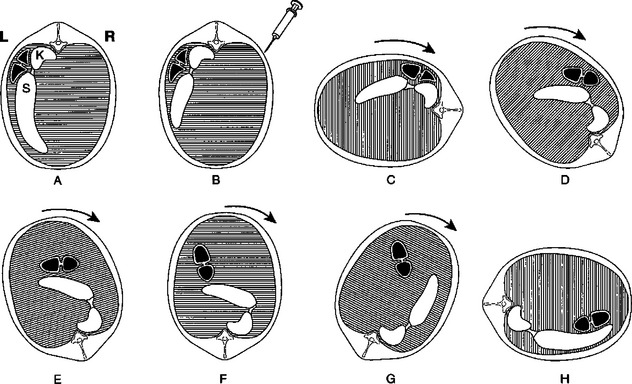
Fig. 5.4 Steps in correction of left dorsal displacement of the colon (renosplenic entrapment). A Caudal view of abdomen of horse with left dorsal displacement of the colon. Entrapped colon is shown in black; K = left kidney, S = spleen. B Injection of phenylephrine and contraction of spleen. C Horse anesthetized and placed in right lateral recumbency. D–H Horse rolled through dorsal recumbency to left lateral recumbency. Entrapped colon moves ventrally and then medially to the contracted spleen.
(Modified with permission from Kalsbeek HC. Equine Vet J 1989; 21:442.)
An alternative means of nonsurgical correction involves administration of phenylephrine (0.01 mg/kg, intravenously, slowly) and then jogging the horse.30,31 This technique was successful in correcting the displacement in 11 of 12 horses.31 It may be advantageous to relieve large-colon distension by percutaneous trocarization before jogging.9
Cases that are refractory to nonsurgical treatment require laparotomy (ventral midline or left flank) and manual correction of the displacement. Recurrence of the displacement occurs in 3–7% of cases.7 Horses with recurrent disease may benefit from surgical ablation of the nephrosplenic space.32
Burba DJ, Moore RM. Renosplenic entrapment: a review of clinical presentation and treatment. Compend Contin Educ Pract Vet. 1997;9:180-184.
Johnston JK, Freeman DE. Diseases and surgery of the large colon. Vet Clin North Am Equine Pract. 1997;13:317-340.
Gibson KT, Steel CM. Strangulating obstructions of the large colon in mature horses. Equine Vet Educ. 1999;11:234-242.
Lopes MA, Pfeiffer CJ. Functional morphology of the Equine pelvic flexure and its role in disease. A review. Histol Histopathol. 2000;15:983-991.
1 Mair TS. Vet Rec. 2002;151:152.
2 Bassage LH, et al. Equine Vet J. 2000;32:565.
3 Latimer FG, et al. Equine Vet Educ. 1999;11:229.
4 Segura D, et al. Equine Vet Educ. 1999;11:227.
5 Gibson KT, Steel CM. Equine Vet Educ. 1999;11:234.
6 Livesey MA, et al. Can Vet J. 1988;29:135.
7 Baird AN, et al. J Am Vet Med Assoc. 1991;198:1423.
8 Knottenbelt DC, Hill FWG. Vet Annu. 1989;29:161.
9 Hardy J, et al. Equine Vet J Suppl. 2000;32:95.
10 Van der Linden MA, et al. J Vet Intern Med. 2003;17:343.
11 Hillyer MH, et al. Equine Vet J. 2002;34:455.
12 Fisher AT, Meagher DM. Compend Contin Educ Pract Vet. 1985;8:S25.
13 Snyder JR, et al. J Am Vet Med Assoc. 1989;195:757.
14 Moore JN, Dreesen DW. Proc Am Assoc Equine Pract. 1993;38:99.
15 Hance SR, Emberstson RM. J Am Vet Med Assoc. 1992;201:782. 87
16 Harrison IW. Vet Surg. 1988;17:77.
17 Lopes MAF, et al. Am J Vet Res. 2004;65:687.
18 Snyder JR, et al. Am J Vet Res. 1988;49:801.
19 Santshi EM, et al. Vet Surg. 1993;22:281.
20 Pease AP, et al. Vet Radiol Ultrasound. 2004;45:220.
21 Gardner RB, et al. J Vet Intern Med. 2005;19:761.
22 Dallap BL, et al. J Vet Emerg Crit Care. 2003;13:215.
23 Steenhaut M, et al. Equine Vet J. 1993;25:550.
24 Dyson S, Orsini JA. J Am Vet Med Assoc. 1983;182:720.
25 Roy MF, et al. Equine Vet J. 2002;34:102.
26 Harvey-Micay J. Can Vet J. 1999;40:729-730.
27 Abutarbush SM, Naylor JM. J Am Vet Med Assoc. 2005;227:603.
28 Markel MD, et al. J Am Vet Med Assoc. 1985;187:1379.
29 Kalsbeek HC. Equine Vet J. 1989;21:442.
30 Johnston JK. Vet Surg. 1996;25:13.