Sagittal discrepancies
Development of a sagittal problem
Diagnosis of sagittal discrepancies
The correction of sagittal discrepancy has been considered a common goal for the patient and the orthodontist. A large proportion of clinical situations is not a single entity and is often associated with significant skeletal and dental imbalances in sagittal plane. Traditionally, orthodontic assessment and diagnosis is mainly based on Angle's sagittal classification of malocclusion.1 Since the dentofacial abnormalities exist in sagittal, transverse and vertical planes, contemporary orthodontic assessment and interpretation must include their understanding in all three dimensions. While studying the various abnormalities in anteroposterior plane, it is also important to identify vertical discrepancies, as their presence impacts the sagittal dimension.
This chapter deals with the systematic approach to the diagnosis and treatment planning of various sagittal discrepancies based on redefined treatment goals, treatment options at various stages of development and their resolution with appropriate treatment mechanics and long-term stability.
The sagittal discrepancies essentially include Class I, Class II and Class III malocclusions; however, defining any one of these malocclusions is difficult because this arbitrary categorization consists of various abnormalities. In their original interpretation and understanding, these abnormalities represent the anteroposterior relationship between the maxillary and the mandibular first permanent molars as described by Edward H. Angle.1 Therefore, this approach does not recognize the dysplastic skeletal sagittal relationship of the maxilla and mandible to each other and to the cranial base. It is critical to identify and assess vertical discrepancies and understand their role in anteroposterior malrelationships. Equally important has been the proper understanding of the functional adaptation to the sagittal and vertical discrepancies. This leads to a posterior and occasionally anterior condylar displacement or autorotation of the mandible due to deficient posterior or excessive anterior facial height.2
The traditional approach to the diagnosis of sagittal discrepancies based on the molar relationship or the habitual occlusion does not reveal the abnormalities in the vertical dimension and in the condylar position in the fossa, dictated by the occlusal guiding forces and the neuromuscular adaptation. Therefore, a contemporary approach should address all these areas in differentially diagnosing variety of sagittal discrepancies. The diagnosis, treatment planning and the orthopaedic and orthodontic management of various Class II and Class III clinical situations and their interaction with the vertical dimension form the basis for this chapter.
Development of a sagittal problem
Various factors play an important role in the development of sagittal discrepancies. Identifying and understanding the involvement of specific causative factors is essential in developing an effective treatment plan. Growth disturbances, tooth size, crowding or spacing of teeth, height of palate and length and width of arch are all influenced by heredity. These, in turn, significantly contribute to the development of Class II and Class III malocclusions. An injury to the maxilla during growth can produce retardation of growth resulting in Class III relationship, while trauma during pregnancy or birth injury damaging the condyle can lead to Class II relationship. Congenital defects like cleidocranial dysostosis, leading to retruded maxilla and prognathic mandible; cerebral palsy resulting in loss of muscular coordination; Down's syndrome (Mongolism); hypothyroidism leading to underdevelopment of mandible and Pierre Robin syndrome resulting in micromandible are all responsible for the development of Class II malocclusion. Class II relationship is also caused by certain local factors like anomalies in number of teeth – missing teeth and supernumerary teeth; anomalies of form and position – large teeth, ectopic positions and transpositions and tootharch disproportion – spacing and crowding. Abnormal pressure habits like thumb sucking and tongue thrusting significantly contribute to the development of sagittal discrepancies. In patients with nasal obstruction, tongue is held in forward position to keep the airway patent leading to short and constricted maxilla and long and expanded mandible. Disturbances in eruption sequence and timing can often result in occlusal interferences leading to a pseudo Class III malocclusion. Certain other factors, like extracted or missing teeth and their nonreplacement, result in drifting of adjacent teeth, thereby developing a dental sagittal discrepancy.
Diagnosis of sagittal discrepancies
Since sagittal discrepancies consist of various components and are often associated with abnormalities in other planes of space, their accurate diagnosis is a key element in the design of any successful treatment plan. It is essential to obtain adequate information about patient's problem through the analysis of high-quality diagnostic records in order to improve diagnostic capabilities. However, increased amount of patient data requires thorough analysis and makes the process of interpretation a complex process. Therefore, a systematic approach to diagnosis is the key to redefining treatment goals and treatment planning of various sagittal discrepancies and their resolution with appropriate treatment mechanics to ensure long-term stability.
Class II malocclusion
‘Class II’ is a broad term designated to a set of various abnormalities that could be either simple or most complex. It is not a single clinical entity, rather it consists of various components of the craniofacial complex having variations in size, shape and position.3 In order to plan an appropriate treatment, the clinician should localize and quantify any skeletal and dental contributions, sagittal and vertical variations and the role of abnormal function and habits to the development of Class II malocclusion. There are many different types of Class II patients with significant variations in skeletal, dental and soft tissue morphology.
Clinical examination and functional assessment
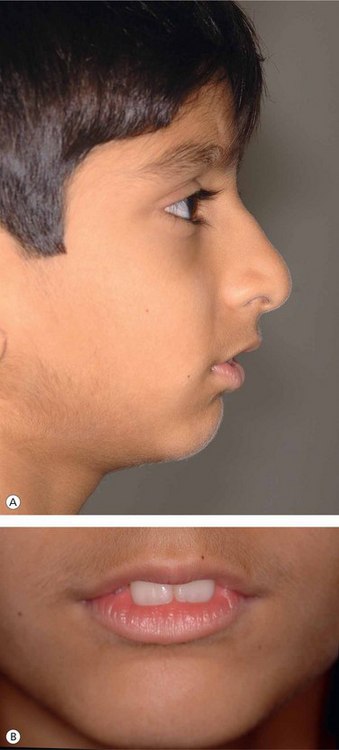
Improvement in facial profile is the most important factor considered by most patients seeking orthodontic treatment. Therefore, the focus of orthodontic treatment should be to achieve pleasing facial profile and soft tissue characteristics rather than just cephalometric norms. In the past few years, the scope of orthodontic assessment and treatment has been expanded, and the ability of the orthodontist to remarkably improve the patient's facial appearance has also been considerably enhanced.4 During the process of clinical examination, while evaluating patient's profile, it is important to study total profile, lip projections and nasolabial angle (Fig 3.1).
Functional assessment
Functional assessment is performed during the clinical examination for planning treatment for Class II malocclusions, especially in growing patients.
• It is important to study the relationship between increased overjet, commonly found in Class II division 1 malocclusion, and lip function (Fig 3.2). If the lower lip is trapped between maxillary and mandibular incisors, its posture and function in the same area along with hyperactive mentalis muscle function leads to progressive deforming activity on dentition.
• To differentiate between functionally true Class II and forced bite Class II malocclusions, it is essential to assess the relationship between rest position and occlusion.
• Tongue posture and function should be carefully assessed to find out its role in the development of malocclusion.
The above-mentioned parameters are of particular interest in establishing soft tissue or facial aesthetic goals, as the face is considered to be the determinant of orthodontic treatment.
Morphologic characteristics
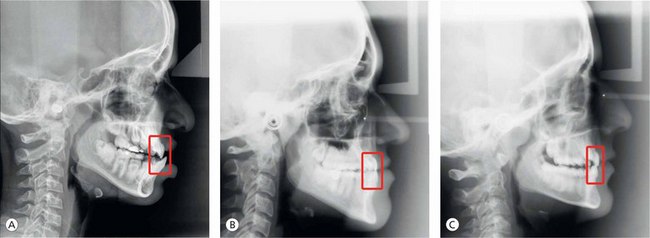
As a clinician, it is critical to identify and locate the structures at fault with the help of cephalometric analysis, which are mainly contributing to the development of Class II malocclusion (Fig 3.3). Their understanding is essential to establish treatment goals and plan a treatment to resolve them. The first simple step is to find out whether it is dental or skeletal Class II malocclusion. Dental Class II malocclusion is caused by tooth migration, which may be confined to the entire arch or a segment of the arch following a missing tooth or abnormally displaced teeth. Skeletal Class II malocclusion could be as a result of prognathic maxilla and normal mandible, retrognathic mandible and normal maxilla or a combination of both – prognathic maxilla and retrognathic mandible. This is just a broad understanding of Class II malocclusion, whether it is dental or skeletal, and identifying the component involved. The Class II patient should be further analyzed cephalometrically to ascertain the involvement of vertical discrepancy or whether it is purely horizontal in nature.
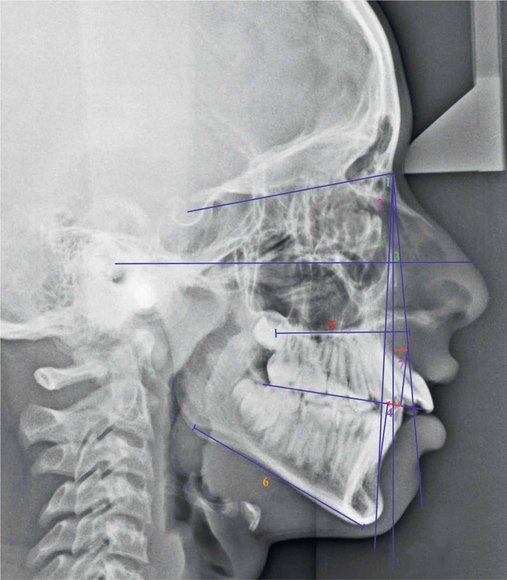
Figure 3.3 Cephalometric assessment (Class II malocclusion). 1, SNA; 2, SNB; 3, ANB; 4, Wits appraisal; 5, Maxillary length; 6, Mandibular length; and 7, Point A – nasion perpendicular. (For a detailed sagittal cephalometric assessment refer to Figures 1.35–1.39 in Chapter 1.)
Björk5 divided Class II malocclusions into forward and backward rotators and suggested that forward rotators are more common and easier to treat than the backward rotators. Classification of Class II malocclusion to group together cases having predominantly similar features is useful for the clinician to design a common treatment. These can be broadly classified as following horizontal types.6
Horizontal types: There are many variations in horizontal types of Class II malocclusions ranging from those having normal skeletal features but Class II dental characteristics to distinctly different skeletal types (Fig 3.4).
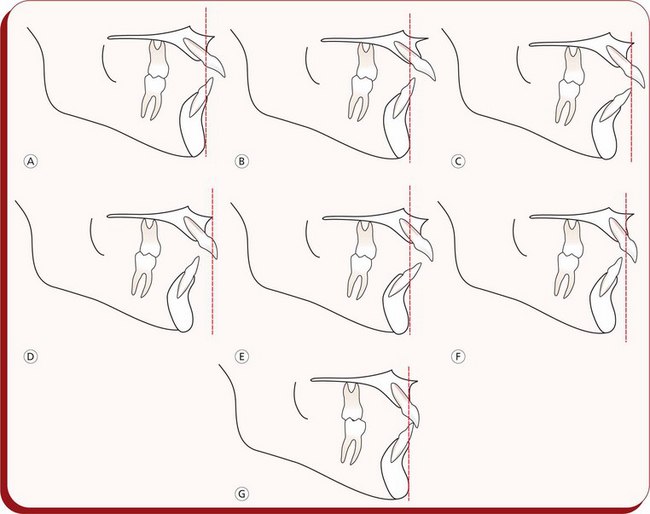
Figure 3.4 Horizontal morphologic characteristics of Class II malocclusion based upon the study by Robert Moyers. (A) Maxillary dental protraction. (B) Midface prognathism. (C) Maxillary retrognathism, dental protraction and mandibular retrognathism, dental protraction. (D) Mandibular retrognathism, maxillary retrognathism and maxillary dental protraction. (E) Maxillary prognathism and dental protraction. (F) Mandibular retrognathism. (G) Normal maxillary and mandibular dental and skeletal relationships.
• Type A: it is characterized by normal sagittal position of the jaws exhibiting normal skeletal profile. The maxillary dentition is protracted with normal mandibular dentition leading to a Class II molar relationship associated with increased overjet and overbite. This type of malocclusion is also called a dental Class II malocclusion.
• Type B: it exhibits a midface prominence with a mandible of normal length. The maxilla is prognathic, while the mandible is in normal anteroposterior relationship.
• Type C: it is characterized by retrognathic maxilla and mandible, the maxillary incisors are either upright or labially tipped and the mandibular incisors are proclined. The patient usually exhibits smaller facial dimensions than other Class II type displaying a Class II profile.
• Type D: it shows a retrognathic skeletal profile with maxillary and mandibular retrognathism. The maxillary incisors are typically proclined, and the mandibular incisors are either upright or lingually inclined.
• Type E: it displays a maxillary prognathism and a normal mandible. The maxillary and mandibular incisors are proclined. Bimaxillary protrusion Class II malocclusions are usually of horizontal type E.
• Type F: it is a large, heterogeneous group with mild skeletal Class II tendencies. Each type F is generally considered to be milder, nonsyndromal forms of types B, C, D or E.
Functional class II with a distally forced bite
This is a functionally created Class II malocclusion, having normal postural rest position but a forced mandibular retrusion in habitual occlusion. The path of closure of the mandible is abnormal or forced; quite often, associated with an infraocclusion of buccal segment teeth leading to an excessive overbite.
In addition to this, it is important for the clinician to predict the Class II malocclusion as forward or backward rotator. Four of the variables – mandibular inclination, shape of the lower border of the mandible, inclination of the symphysis and intermolar angle, when combined, give the best prognostic estimate of mandibular growth rotations.7
Class III malocclusion
Class III malocclusion generally manifests at an early age, and it is one of the difficult clinical situations to treat. The factors responsible for development of Class III malocclusion are different from those in Class II situation. As compared to Class II relationships, most Class III problems have a strong hereditary component.8,9 Environmental influences like habits and mouth breathing also play an important role in the development of Class III malocclusion. A growth stimulus from the constant distraction of the mandibular condyle in patients with abnormal mandibular posture can result in excessive mandibular growth.10 Class III malrelationships are often associated with morphologic and functional consequences. Patients with Class III problems may present with an impairment of dentofacial aesthetics and occasionally with psychological issues. This clinical situation may lead to incorrect loading of the teeth; chewing and speech functions may be altered. The prosthetic rehabilitation of the case may be difficult.
Like Class II malocclusion, Class III malocclusion is not a single clinical entity, rather it consists of various components of dentofacial complex.11 In a broader perspective, it is generally considered to be a manifestation of mandibular prognathism or midface deficiency or a functional forward shift of the mandible on closure to occlusion. Therefore, it could be skeletal Class III, dental Class III or ‘pseudo’ Class III, all resulting from a variety of combinations.
It is critical for the orthodontic professional to localize the disharmonious elements contributing to the Class III malocclusions. Other affected areas in the dentofacial complex of individuals having Class III malocclusions also include larger mandibular plane angles, larger gonial angles, longer mandibles and compensations of the dentition with maxillary dentoalveolar protrusion and mandibular dentoalveolar retrusion.12 While evaluating the Class III relationships, it is important to identify whether the problem is dental, caused by the improper inclination of the maxillary and mandibular incisors; functional, caused by the occlusal interferences; or skeletal, caused by the discrepancies of the maxilla and mandible. Therefore, the evaluation of a patient with Class III morphology should have a prescribed protocol to include (1) assessment of general facial morphology, (2) identification of abnormal components, (3) the vertical position of the mandible in posture and occlusion and (4) the position and angulation of the maxillary and mandibular incisors.
It is important to follow a well-organized and systematic approach to the diagnosis of patients with Class III malocclusion to determine the following variations in the Class III skeletal profile13 (Fig 3.5).
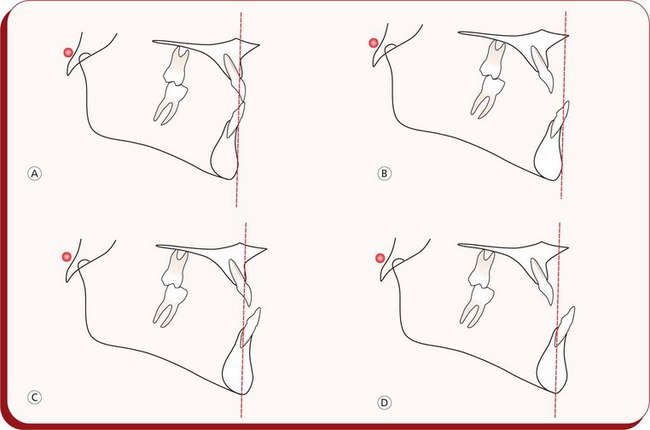
Figure 3.5 Variations in Class III skeletal profile. (A) Normal maxilla and mandible. (B) Maxillary retrusion and normal mandible. (C) Normal maxilla and mandibular prognathism. (D) Maxillary retrusion and mandibular prognathism.
1. Normal maxilla and mandibular prognathism
2. Retruded maxilla and normal mandible
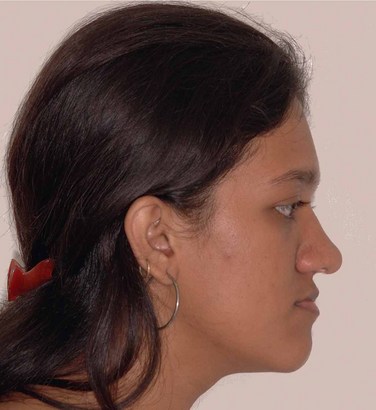
Assessment of facial profile
An evaluation of the facial profile should include an analysis of facial proportions, midface position, chin position and vertical proportions.14 This assessment is done to determine whether the patient's profile is straight, convex or concave (Fig 3.6). Patients with maxillary deficiency usually exhibit a concave profile and flattening of the infraorbital rim and the area adjacent to the nose. It is essential to note that the facial convexity decreases as the patient matures.
Functional assessment
In patients with Class III malocclusion, it is critical to assess the relationship of the mandible to the maxilla to identify whether a centric relation (CR) and centric occlusion (CO) discrepancy exists. This is important because the anterior position of the mandible may be guided by abnormal tooth contacts that shift the mandible forward.
Patients having normal facial profile, Class I skeletal pattern and Class I molar relationship in CR with forward shift of the mandible on closure will exhibit concave profile, Class III skeletal and dental profile in CO. This clinical situation is called pseudo Class III malocclusion. However, patients with no shift of the mandible on closure are most likely to have a true Class III malocclusion. The key diagnostic feature in differentially diagnosing pseudo and skeletal Class III malocclusions is the gonial angle measurement that is usually more obtuse in skeletal Class III.15
Dental assessment
It is essential to assess the position and angulations of maxillary and mandibular incisors and the resultant interincisal relationship. The Class III relationship may be associated with an edge-to-edge relationship, a negative overjet or a positive overjet (Fig 3.7). If it is associated with a negative overjet, the clinician should proceed to functional assessment to differentiate between true and pseudo Class III malocclusion. If the Class III molar relationship is associated with a positive overjet or an edge-to-edge incisal relationship, a compensated Class III malocclusion is suspected. A compensated Class III malocclusion is a clinical situation where maxillary and mandibular incisors compensate for the existing skeletal Class III discrepancy.
Cephalometric assessment
Patients with Class III malocclusion may present with a variety of combinations of skeletal and dentoalveolar components often associated with vertical and transverse discrepancies. Proper understanding of these components is essential to establish appropriate treatment plan so that the underlying cause of the discrepancy can be treated effectively.
Cephalometric analysis is a valuable diagnostic tool that drives the clinician to pinpoint the components responsible for the development of Class III malocclusion. While analyzing the anteroposterior relationship of maxilla and maxillary incisors and mandible and mandibular incisors, it is important to assess the vertical and transverse discrepancies associated with Class III malocclusion. The traditional approach to analyze patients with Class III malocclusion is to use ANB discrepancy. The patients with skeletal Class III malocclusion usually exhibit negative ANB angle with a smaller SNA angle and a larger SNB angle. However, individual variations in cranial base flexure and anteroposterior displacement of nasion often alter the ANB discrepancy.16 Therefore, alternative cephalometric measurements and analysis like Wits appraisal, effective maxillary and mandibular length and nasion perpendicular to ‘A point’ can be used to assess the anteroposterior relationship of the maxilla and mandible (Fig 3.8).
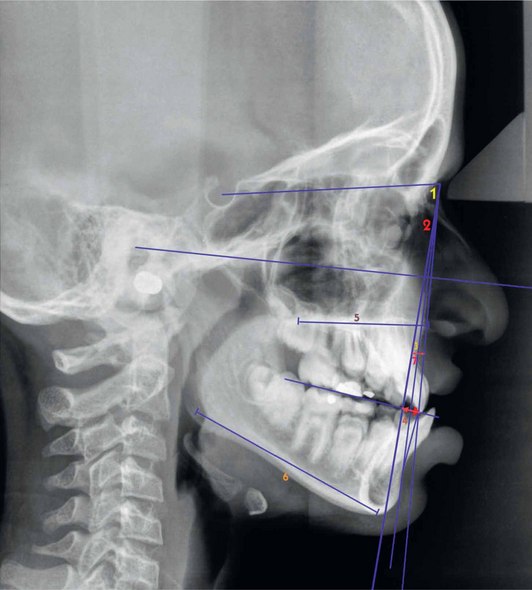
Figure 3.8 Cephalometric assessment (Class III malocclusion). 1, SNA; 2, SNB; 3, ANB; 4, Wits appraisal; 5, Maxillary length; 6, Mandibular length; and 7, Point A – nasion perpendicular. (For a detailed sagittal cephalometric assessment refer to Figures 1.35–1.39 in Chapter 1.)
Treatment planning
Establishing accurate diagnosis is the key element in formulating a successful treatment plan. The practitioner should focus on the development of an individualized treatment plan to improve the treatment results and shorten the treatment duration. The best way to approach treatment planning for a specific malocclusion is to define treatment goals as to what needs to be accomplished by treatment. These include facial, skeletal and dental goals. Making the most of available diagnostic information including the patient's chief complaint forms a basis for establishing treatment goals. This often drives the clinician to an important process of a re-exploration of the diagnostic information and consideration of some important factors.
• Determine whether the malocclusion is skeletal or dentoalveolar.
• Treatment planning for the sagittal discrepancies requires that the clinician should assess the relationship between the postural rest position of the mandible and the habitual occlusion. This will help differentiate between ‘true discrepancy’ with a normal path of closure from postural rest to habitual occlusion and ‘functional discrepancy’ with abnormal path of closure of the mandible.
• While assessing the treatment possibilities for sagittal discrepancies in a growing patient, it is essential to forecast the probable growth direction and magnitude.
• Ascertain the growth potential of the patient based upon the useful diagnostic information. The clinician should assess the growth potential and when a growth spurt can be expected to determine the treatment timing and the method. Growth increments per unit time are a prime consideration.
• Identification of aetiological factors responsible for the development of a sagittal discrepancy, the role of neuromuscular dysfunctions and differentiating hereditary malocclusions are of great value in planning a treatment.
• The dentofacial aesthetics greatly influences the treatment planning process of sagittal discrepancies since it is one of the main reasons why patients seek orthodontic treatment. The clinician must record the expectations of a patient in terms of aesthetics. The aesthetic benefits of orthodontic treatment are universally accepted by both patients and practitioners.17,18 It has been widely recognized that attractive individuals are more likely to be successful in their academic and career accomplishments.19,20 Orthodontic treatment affects aesthetics through three-dimensional alteration of anterior tooth position. Therefore, the impact of proposed orthodontic treatment on dentofacial aesthetics should be analyzed and required alterations, if necessary, be incorporated in the final treatment plan.
• The functional benefits of orthodontic treatment have been universally recognized by practitioners. Achievement of Class I occlusion with proper excursive guidance will lead to maximum intercuspation, optimum aesthetics and long-term stability.21 Patients with anterior open bite or severe overjet may benefit functionally by achieving normal interincisal relationships.22 While planning orthodontic treatment, the clinician should establish functional goals not only related to the occlusal relationships, but they should also be extended to include the relationship of the soft tissues to the teeth. Quite often, patients present with abnormal lip posture due to abnormal jaw and teeth relationships. Therefore, the treatment planning process should include selection of appropriate treatment strategy to achieve adequate lip closure at the conclusion of treatment.23
• One of the most important factors that influence treatment planning is the prediction of long-term stability of tooth positions. Orthodontists should plan tooth movements and determine final jaw and tooth positions that ensure stability. It has been traditionally considered that extractions are required in patients with dental crowding to achieve long-term stability; however, this treatment modality does not necessarily guarantee long-term stability.24,25 Both extraction and nonextraction treatment approaches may result in variable amount of relapse based upon many factors like severity of malocclusion, duration of retention and specific characteristics of individual patients. Therefore, the clinician should identify the areas of potential relapse and take appropriate measures to establish individualized retention protocol for good stability.
Treatment of sagittal discrepancies
There is no universal treatment approach that can address all sagittal discrepancies. As described earlier, Class II and Class III malocclusions are not a single clinical entity, rather they consist of various components. Quite often, they are associated with vertical or transverse discrepancies. Therefore, to design a treatment plan for a particular patient, the clinician should identify and locate the components involved.
There are various treatment methods and numerous appliances available to deal with different types of sagittal discrepancies depending upon the configuration of the malocclusion and the age of the patient. It should be noted that the response of the patient to a prescribed treatment plan is a major factor to be considered in achieving the desired result. Even similar malocclusions respond differently to similar treatment approach, and such differential response should be continually monitored to determine the need for necessary therapeutic alterations.
Treatment of class II malocclusions
There are several treatment strategies available to deal with different types of Class II situations. It is essential for the practitioner to select the appropriate treatment strategy depending upon the recognition of various elements contributing to the existing clinical problems. In other words, the treatment approach should be individualized. There are many Class II cases that require one or a discretionary combination of the various available treatment strategies. These include movement of teeth and alveolar processes, guidance of eruption and alveolar development, differential restraint and control of skeletal growth, differential promotion of skeletal growth, translation of parts during growth, training of muscles and surgical translation of parts.6
For the purpose of discussion, various Class II malocclusions can be grouped into the following categories:
1. Dentoalveolar Class II malocclusions
2. Functional Class II with distally forced bite
3. Skeletal Class II with maxillary prognathism
4. Skeletal Class II with prognathism and anteinclination of maxilla
Treatment of dentoalveolar class II malocclusion
Dentoalveolar Class II malocclusion patients present with normal skeletal jaw relationship and Class II molar position caused by mesial movement of maxillary molars with respect to mandibular molars during developmental stage (Fig 3.9). The unilateral Class II situation may exist due to mesial migration of maxillary permanent first molars following missing or abnormally positioned maxillary second bicuspids or premature loss of deciduous second molar on the affected side (Fig 3.9A and D). Patients with this abnormality are also associated with other parameters like varying degrees of overbite, overjet, crowding, rotations, etc. Not only the severity of Class II molar relationship but parameters like varying degrees of overbite, overjet, crowding, rotations, etc. also determine the complexity of treatment involved. After it has been established that the Class II malocclusion is dental in nature, the clinician should assess the position of all dental units in sagittal, vertical and transverse dimensions to define treatment goals and select appropriate treatment strategy. The contemporary orthodontic treatment illustrates that such patients will have numerous treatment goals and individualized treatment mechanics designed to address those goals. Specific treatment plans for individual patients fall into five major categories: growing patients, nongrowing patients, sagittal discrepancies, vertical discrepancies and transverse discrepancies.
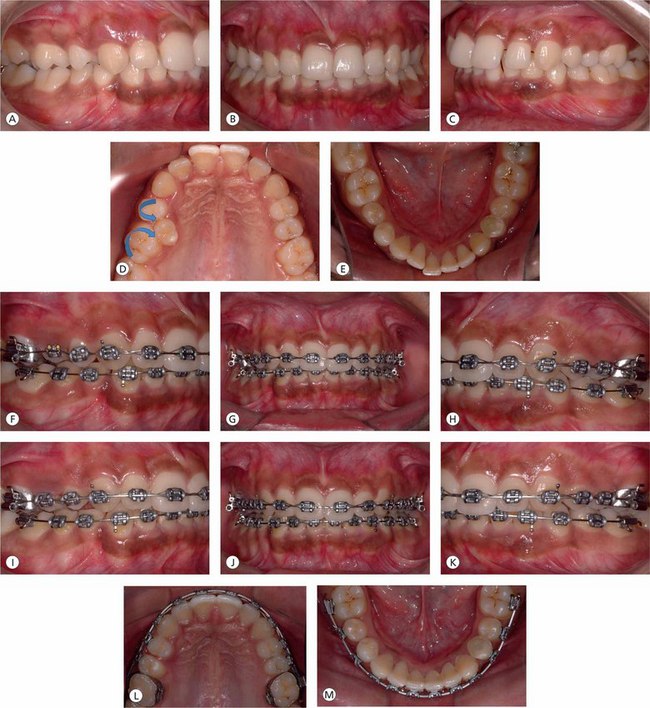
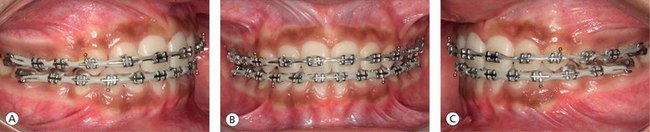
Figure 3.9 (A–E) Pretreatment intraoral photographs showing Class II molar relationship on right side, Class I molars on the left side and deep overbite. The Class II relationship on right side is due to mesiopalatal rotation of the first molar and distopalatal rotation of the first premolar as a result of palatal displacement of the second bicuspid. (F–H) After mesiobuccal rotation and distalization of the first molar to correct molar relationship and gain adequate space for the palatally placed second bicuspid, the second bicuspid is being moved into proper occlusion. (I) Establishing proper torque and fine-tuning the position of the maxillary right second bicuspid with finishing wires. (J–M) Midlines are corrected and proper occlusal relationship and coordinated upper and lower archforms are achieved.
Biologic variables: The basic strategy in the management of dentoalveolar Class II malocclusion is to achieve normal molar and incisal relationships, maintaining the existing normal skeletal relationship and the vertical dimension. Efficient tooth movement is ultimately the result of optimal biologic response to the orthodontic force system. The physiologic activity of alveolar bone resorption and deposition to produce tooth movement is induced by the mechanical stimulus through the delivery of orthodontic force systems. It is important that the force levels produced by orthodontic appliances are optimal, which will promote the most efficient treatment response without any damage to the teeth and the supporting structures (Table 3.1). The clinician should avoid excessive orthodontic force levels to prevent periodontal ligament necrosis and associated pain and bring about efficient tooth movement. It is essential to update on the knowledge of the force levels delivered to teeth through the medium of the appliance to understand optimal forces.26–28 These optimal force values depend on the type of the tooth and the size of the tooth.
Table 3.1
Optimal forces for orthodontic tooth movement
| Type of tooth movement | Force (g) |
| Tipping | 50–75 |
| Bodily movement (translation) | 100–150 |
| Root uprighting | 75–125 |
| Rotation | 50–100 |
| Extrusion | 50–100 |
| Intrusion | 15–25 |
Force values vary according to the size of the tooth; smaller values for incisors and higher values for posterior teeth.
Source: Proffit WR, et al. Contemporary orthodontics. 1993.
Dentoalveolar problems: Early treatment: The sagittal dental discrepancies in the primary dentition, seen in children having sucking habits, are expressed in the form of anterior displacement of upper incisors and posterior displacement of lower incisors. At this stage of development, if the sucking habit stops before the eruption of permanent teeth, it is usually self-correcting and therefore does not require any orthodontic intervention.
The mixed dentition phase is a very critical developmental stage. During this phase, children should be carefully examined and assessed for existing and potential or developing discrepancies. There are many treatment options available, depending upon the severity of the problem. The discrepancies in their severe form are best treated with two phases of treatment: phase 1 in the mixed dentition and phase 2 during the early permanent dentition period. It has been universally recognized that prevention is better than cure. The development of a space discrepancy when primary first or second molars are missing is best prevented by space maintenance protocol. This is indicated when there is adequate available space, and the premolar eruption will take more than 6 months. If the patient presents with bilateral problem, it is better to use lingual arch rather than two isolated appliances in the posterior segments. However, if the available space is not adequate for the permanent tooth or if there is significant amount of space loss due to the drifting of adjacent teeth, the lost space should be regained by repositioning the drifted dental units.
One of the basic tenets of any mixed dentition treatment protocol is to monitor the transition from the mixed to the permanent dentition. The simple procedure of maintaining the available arch length during the mixed dentition period helps to resolve minor to moderate tooth-size and arch-size discrepancies29 along with the other methods of space gaining.
In the mandibular arch, the combined average width of the deciduous cuspid, the first deciduous molar and the second deciduous molar is approximately 1.7 mm greater than the combined width of the canine, the first premolar and the second premolar teeth (Fig 3.10A). In the maxillary arch, this combined width difference is approximately 0.9 mm.30 The practitioner should assess each patient radiographically to determine the size differential between the second deciduous molars and their successors, as the tooth size varies significantly among individuals31 (Fig 3.10B).
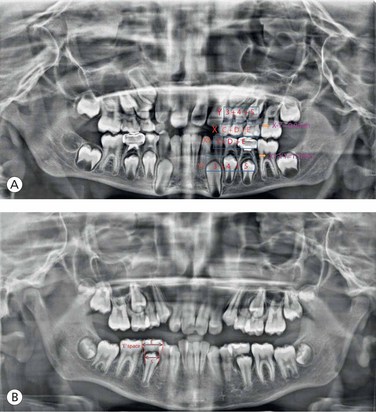
Figure 3.10 (A) Leeway space. On the average, the combined width of the deciduous canine and first and second deciduous molars is 1.7 mm greater than the permanent successors in the mandibular arch and 0.9 mm in the maxillary arch. (B) E-space.
Patients with thumb sucking habit present with flared maxillary incisors and loss of vertical contact with the mandibular incisors and are frequently associated with variable degree of narrowing of the maxillary arch. Prolonged thumb sucking habit increases the severity of symptoms, leading to the development of anterior open bite. In an effort to improve swallowing and speech, the child often positions the tongue anteriorly between the maxillary and mandibular incisors to seal off the anterior open bite with the consequent development of ‘tongue thrust’. In patients with such problems in mixed dentition stage, the treatment goal should be to establish proper lip seal by retraction of maxillary incisors. It is interesting to note that the tongue thrust habit usually disappears following the retraction of maxillary incisors, since it is considered to be due to ‘physiologic adaption’.
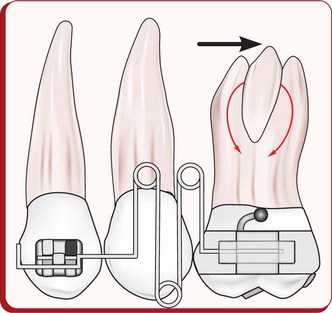
Maxillary molar distalization: Contemporary orthodontic treatment ideologies focus on soft tissue assessment and management. There is a general shift from hard tissue goals, where the face is the determinant of orthodontic treatment. Advances in mechanotherapy and changes in treatment concepts and philosophies now minimize the need for extractions, even in severe discrepancies. One nonextraction treatment approach is the distal movement of maxillary molars to establish Class I molar relationship.
Precise distalization of maxillary molars is of significant value for nonextraction treatment of dentoalveolar Class II malocclusion with a normal mandible. Over the past few years, the focus of the maxillary molar distalization treatment modality has been on the introduction of fixed intra-arch appliances to eliminate the need for patient compliance, following the findings of rapid Class II corrections with nonremovable appliances.32,33
Essentially, this approach is very useful in cases with midline discrepancies, to regain the space lost due to mesial drifting of first molars following premature loss of deciduous teeth, and in cases with Class II molar relationship due to ectopic eruption of first or second bicuspids and impacted or high labially placed cuspids. Based on the author's extensive experience in this field, spanning over last many years, there are basically three elements that determine the efficiency and effectiveness of distal driving of maxillary molars. They are:
1. Three-dimensional control of molars while they are being moved distally
2. Maximum anchorage preservation during the distalization phase
3. Stabilization of molars in their new positions post-distalization during the subsequent phase of space consolidation.
Several appliances have been introduced to accomplish distal molar movement with or without the need for patient cooperation.34–42 Most produce tipping, rotation and extrusion of the molars during distalization therapy; some produce a significant amount of incisor flaring due to anchorage loss, which is seen clinically as increased overjet.39 After distalization of the molars, the distalizing modules and existing palatal anchorage appliances are removed and a Nance palatal button is delivered to maintain the first molars in their new positions.
Case selection criteria The degree of space discrepancy and the facial profile characteristics of the patient are the two main important factors that should be considered in case selection criteria. Patients with mild to moderate space discrepancy are good candidates for maxillary molar distalization therapy. A maximum of 8 mm space has been achieved by certain appliances.43 Even upto 10.5 mm of space gain has been achieved by some clinicians.44
Ideally, the patient should have orthognathic profile; and it is not the modality of choice when there is significant dental protrusion and/or convexity of profile as intraoral distalizing appliances do not cause significant soft tissue changes.45 On the contrary, certain appliances may cause mild increase in profile convexity.46 Therefore, the maxillary molar distalization therapy should be employed when the maxilla and mandible are skeletally normal with mild to moderate maxillary dental proclination or crowding. The patient should exhibit normal lower facial height as most distalizing appliances have an extrusive effect on the molars when they are distalized, leading to an increase in lower facial height.
Also, the patient should not have posterior arch crowding. According to Ricketts,47 the distance between the pterygoid vertical (PTV) plane and the distal aspect of the maxillary first molar should be ‘age + 3 mm’ (Fig 3.11). In normal skeletal and dental relationship, the facial axis passes through the mesiobuccal cusp of the first molar. If the distance M1-PTV is shorter than the normal, the possibility for molar distalization is less and extractions may be required depending upon the growth potential and the presence of third molars.47
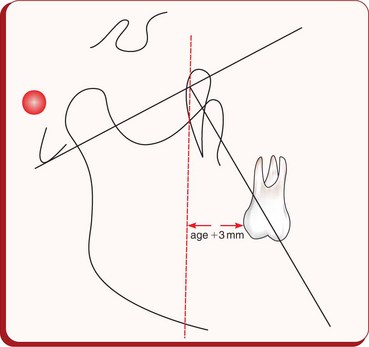
Figure 3.11 The sagittal maxillary first molar relationship is given by its distance to the PTV plane, the norm being ‘age +3 mm’. Under normal circumstances, the facial axis passes through the mesiobuccal cusp of the first molar.
In distalization therapy, the position of the second molar determines the type of the first molar movement.48 If second molar is developing, one should expect more tipping of first molar as compared to fully erupted second molar, as the developing second molar tooth bud acts as a fulcrum for the distal movement of first molar. In the absence of third molars, if second molars are fully erupted, molars will be distalized bodily, requiring greater force levels that result in more anchorage loss.
Appliance selection An ideal distalizing appliance should be rigid and compliance free. It should distalize molars bodily with minimal anchorage loss. Also, it should allow passive free floating of teeth immediately anterior to the distalized teeth. The design of the appliance should be such that it should readily be convertible into a holding appliance after the distalization.
Anchorage The anchorage for intraoral distalizing appliances should ideally be derived from nondental sources like palatal vault and midpalatal screws. However, in most appliances, it is partially obtained from bicuspids. In planning the anchorage system, it is important to consider that rigidity is essential for good anchorage, and the reactive anterior forces generated by the active components are distributed over a large area of the palate. A large acrylic button is made in the region of the vertical portion of the palatal vault.
It extends to approximately 5 mm from the teeth, relieving the incisive papilla anteriorly. The precise fabrication of the palatal button is the key to anchorage preservation, as any space between the palatal tissues and the inner surface of the button would lead to anchorage loss. There is little anchorage value to mobilized teeth. Simultaneous levelling and aligning the rest of the dentition taxes the anchorage, resulting in lesser amount of net distal molar movement. Therefore, it is advisable to distalize maxillary molars without full arch fixed appliance.49
Expansion Some maxillary expansion is often a prerequisite for Class II molar correction. It should either precede or be concomitant with the distalization, which can be made possible by incorporating an expansion device in the distalizing appliance.40
Force levels For efficient and effective distal molar movement, force levels in the range of 100–120 g are considered to be ideal. Continuous forces are preferred than intermittent or interrupted forces. The direction of force should be along the line of arch and should be as close to the centre of resistance of the molar as possible. A good control over the direction and the magnitude of distalizing forces is essential to avoid tipping, rotations and intrusion or extrusion of molars. It is advisable to distal drive maxillary first molars into super Class I relationship to compensate for some anchorage loss during the postdistalization phase of orthodontic treatment.
Stabilization of molars There are various options available to stabilize molars in their new positions, postdistalization. These include utility arch, continuous archwire with molar stops, headgears, Nance holding arch, etc. A secure molar stabilization system should be stable and rigid enough to hold molars and should serve as good anchorage units during the subsequent phase of treatment mechanics.
Postdistalization mechanics Postdistalization stabilization of molars is difficult and highly critical. It should be immediate and as rigid and precise as possible. A lag phase of 3–6 months is desirable before commencing further mechanics to allow passive free floating of bicuspids. It is highly recommended to monitor new molar position and use minimal force levels in postdistalization treatment mechanics.
The Karad's Integrated Distalizing System (KIDS) was developed to address the disadvantages of other distalizing appliances (Figs 3.12–3.16).42 This appliance system is designed on the following principles:
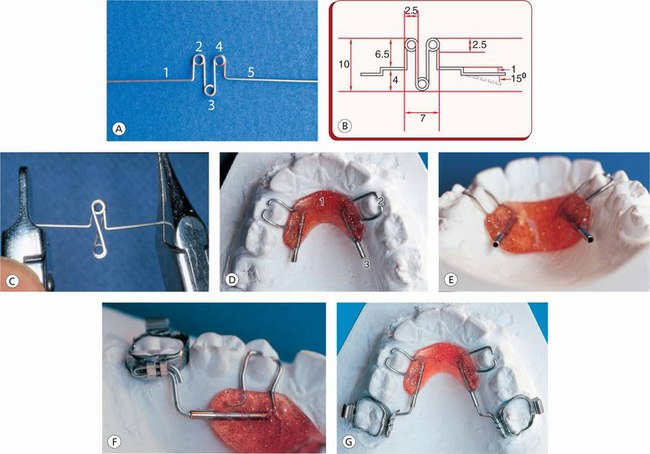
Figure 3.12 (A) Triple helical distalizing spring made from 0.017 × 0.025 TMA wire. 1, Mesial leg; 2, Mesial helical loop; 3, Occlusal helical loop; 4, Distal helical loop; 5, Distal leg. (B) Dimensions of average-sized distalizing spring in mm. (C) Compressed spring when activated. (D) Modified Nance palatal button. 1, Acrylic part; 2, Occlusal rests; and 3, Guiding tubes. (E) Location of the guiding tubes on the lateral curvatures of the palate. (F) Position of sliding tubes into the guiding tubes (palatal button). (G) Components of Karad's Integrated Distalizing System (except for the triple helical distalizing spring). Source: Karad A. World J Orthod 2008; 9:244–254 (Figs 3.12–3.16, Reproduced with permission from Quintessence Publishing Co Inc)a.
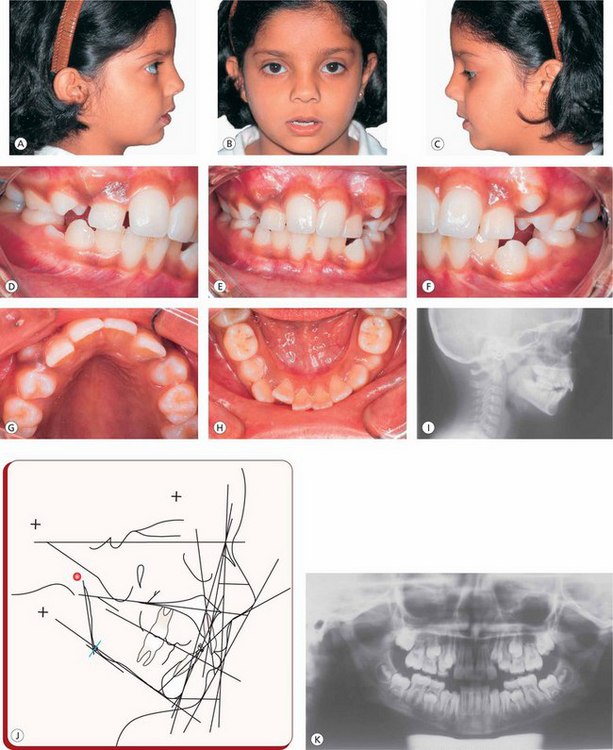
Figure 3.14 (A–H) Pretreatment photographs of a female patient, 11 years of age. (I-K) Pretreatment lateral cephalogram, cephalometric tracing and orthopantomogram.
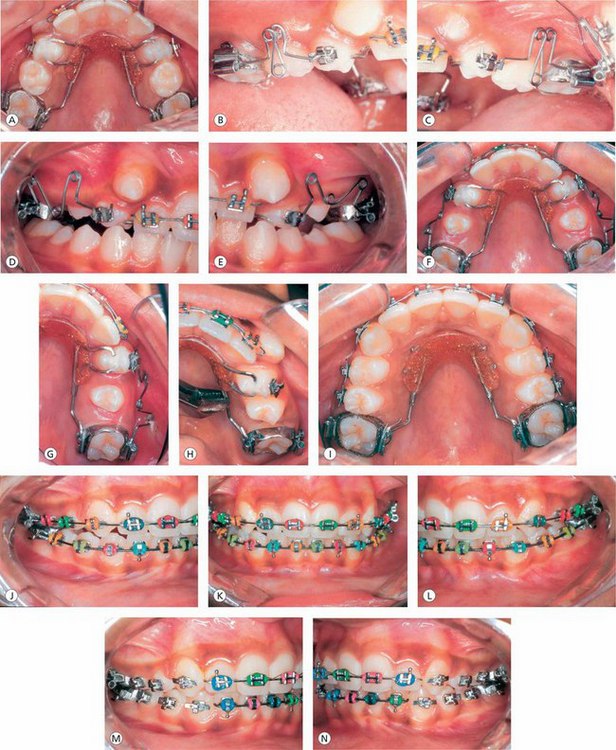
Figure 3.15 (A) Palatal and molar assemblies are bonded and cemented, respectively. (B and C) Initial activation and placement of the distalizing springs. (D–G) Maxillary molars are distalized into super Class I relationship. (H) After the desired amount of distalization, the guiding tubes are crimped with the utility pliers to stabilize the molars in their new positions. (I) Occlusal rests are cut at the palatal button to convert the whole assembly into a holding appliance. (J–N) Finishing and detailing procedures.
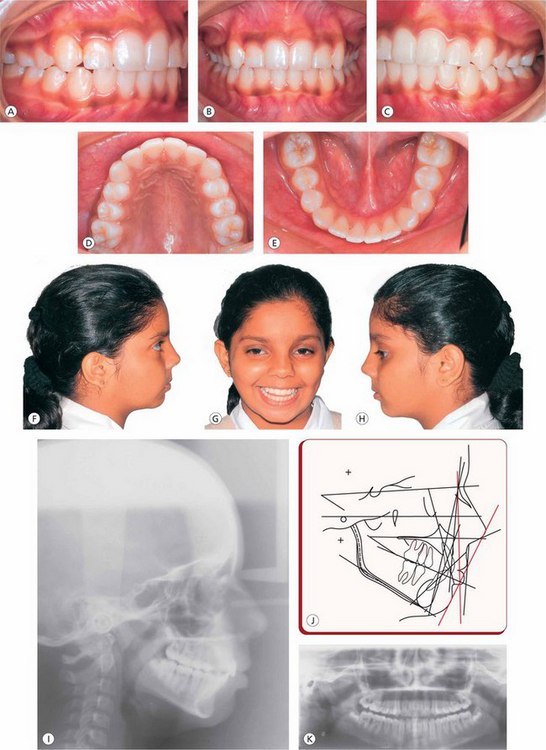
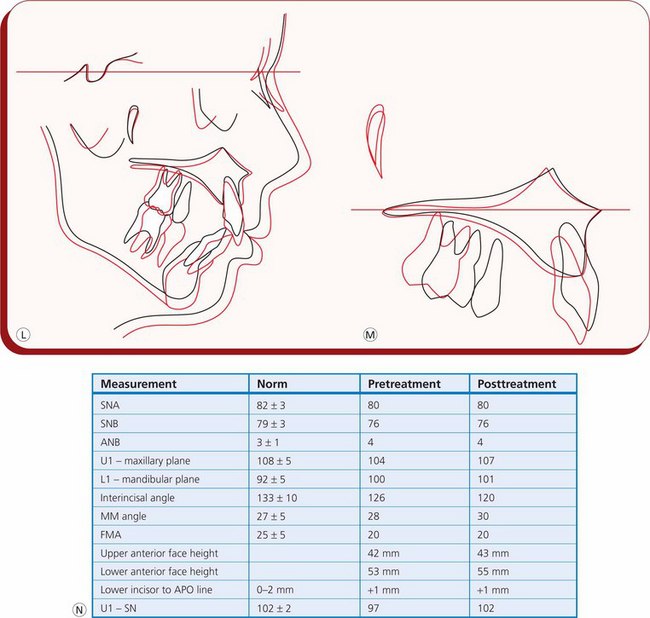
Figure 3.16 (A–H) Posttreatment intraoral and extraoral photographs. (I–K) Posttreatment lateral cephalogram, cephalometric tracing and panoramic radiograph. (L and M) Pretreatment and posttreatment overall and maxillary superimpositions. (N) Table showing pretreatment and posttreatment cephalometric data.
• Light, continuous force system to achieve efficient and predictable molar movement
• Desired moment-to-force ratio for bodily movement of first molars
• Three-dimensional molar control throughout distalization therapy
• Maximum anchorage preservation throughout treatment
• Elimination of need for new Nance palatal button to hold the molars in their new positions after distalization
Nonextraction headgear treatment: The use of headgears in contemporary management of Class II malocclusions is mainly aimed at controlling the anchorage and the cant of the occlusal plane, tooth movement and orthopaedic correction (Figs 3.17–3.22).
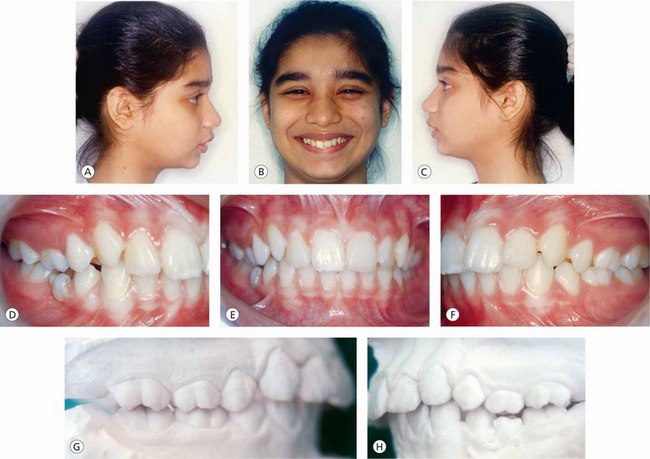
Figure 3.17 (A–C) Pretreatment extraoral photographs of a female patient (age 12 years) showing convex profile, acute nasiolabial angle and incompetent lips. (D–F) Pretreatment intraoral features include proclination of maxillary incisors with crowding. (G–H) Pretreatment models show Class II molar and canine relationship.
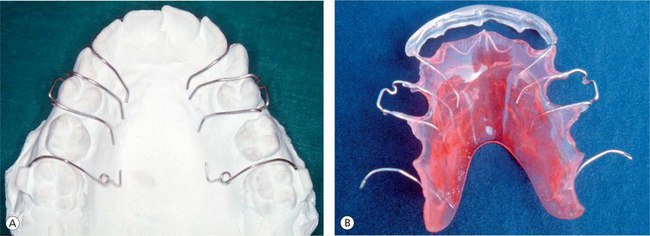
Figure 3.18 Removable appliance component of the combined removable appliance and headgear assembly. (A) Wire components on the model. (B) An appliance with molar distalizing springs, acrylic shield on incisors and Adams clasps on first bicuspids.
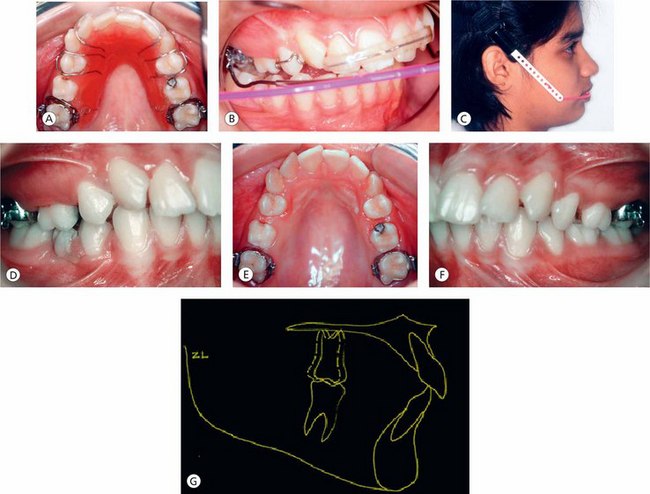
Figure 3.19 (A–C) Combined removable appliance and the molar-inserted combination pull headgear therapy to distalize maxillary first molars. (D–F) The molars are driven distally into Class I relationship. (G) Pretreatment and postdistalization cephalometric superimposition shows bodily movement of maxillary molars.
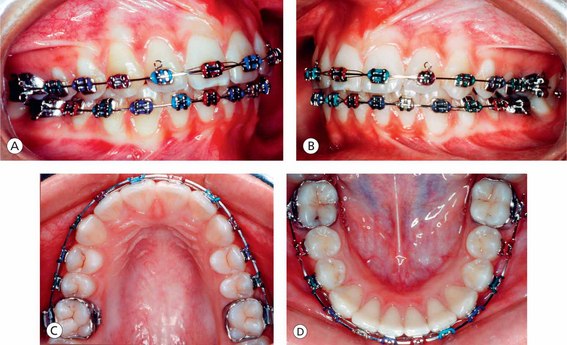
Figure 3.20 (A and B) Postdistalization fixed appliance therapy to resolve anterior discrepancy. (C and D) Coordinated and compatible upper and lower archforms.

Figure 3.21 (A–H) Posttreatment records show good occlusion, archforms, improvement in facial profile, competent lips and pleasing smile.
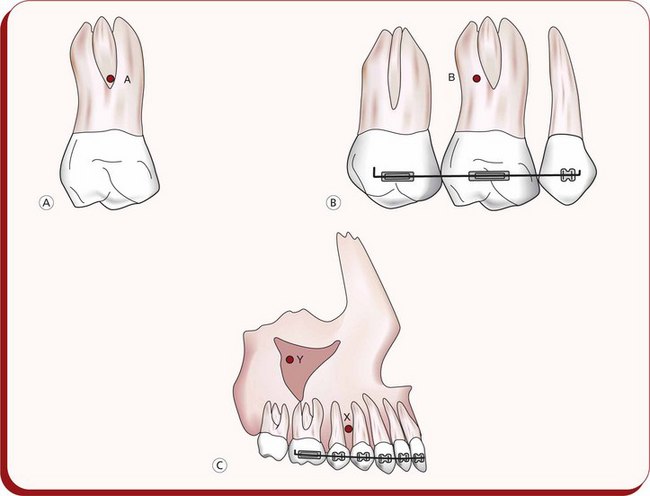
Figure 3.22 Centre of resistance for (A) An individual molar, (B) A segment, (C) the dentition (X) and the maxilla (Y).
With the introduction of fixed intraoral appliances to distalize maxillary molars or other tooth movements in noncompliant patient, the use of headgear has been considerably reduced. However, there are certain clinical situations that require headgear forces to be used in association with contemporary mechanotherapy to prevent adverse effects of intraoral forces from the archwire in order to achieve high quality and stable correction of Class II malocclusions.
For successful use of headgears in clinical Practise, sound knowledge of force systems produced by various designs of headgears is essential. In tipping orthodontic tooth movement, even if the forces are light, the stress levels at the periodontal-tooth and bone interfaces are beyond acceptable physiologic limits.50 Therefore, the practitioner should avoid distal tipping headgear forces to prevent any untoward tissue reactions due to high localized stress levels at the marginal ridge and at the root apices. However, the bodily movement of teeth produced by headgears takes considerable amount of time. In patients with Class II dentoalveolar malocclusion, the use of headgear for 14 h each night, consistently with a force direction passing through the centre of resistance of the maxillary first molar, will move the teeth distally by 2 mm in 2–4 months without tipping.51 In a treatment approach that uses a combination of removable appliance and headgear to gain maxillary arch length, the removable appliance tips the maxillary first molar crown distally and the molar-inserted headgear moves the root distally, resulting in a net bodily distal movement of the tooth.35
The combined removable appliance and headgear essentially consists of three components.
1. Removable appliance consists of molar distalizing springs, modified Adams clasps, acrylic shield on incisors and acrylic plate covering the palate (Fig 3.18).
2. Headgear (Fig 3.19C).
3. Maxillary first molar bands with headgear tubes and lingual sheaths (Fig 3.19B).
The active components of the removable appliance are distalizing springs made from 0.028 inch stainless steel wires, which are activated by 1 mm–1.5 mm exerting a force of approximately 30 g per side. This appliance is worn by the patient for 24 h a day except for meals and hygiene. The headgear, either cervical pull or combination pull, is worn by the patient for 12–14 h per day, exerting a force of approximately 150 g per side. Postdistalization, molars are held in their new positions during the subsequent phase of space consolidation.
For any orthodontic application, the following sequential steps may guide a clinician to design the headgear force system.51,52
1. Select the appropriate size of the inner bow of the facebow. It should be adjusted by placing it against the maxillary plaster model so that it is approximately 3–4 mm away from all teeth except the first molars. At the molar region, it can be adjusted to rest passively in the molar tubes or can be expanded by 1 mm–1.5 mm. The inner bow should rest comfortably between the lips.
2. Determine the centre of resistance of the body to which the headgear force is being applied (tooth or segment or arch or maxilla; Fig 3.22).
3. Mentally, mark the centre of resistance on the patient's cheek.
4. Choose the type of headgear pull – cervical, occipital or combination pull – depending on the vertical relationships observed in the patient.
5. Determine the force system (force and moment at the centre of resistance) through the centre of resistance that will produce the desired changes.
6. Allow the outer bow to rest away from the cheeks and adjust its length and vertical position with respect to the centre of resistance to achieve proper line of force.
7. Choose the headgear force magnitude.
a. In rotating the unit (use a large moment in comparison to the applied force through the centre of resistance), use low-strap forces to avoid high local stress in the periodontal ligament (approximately 150 g per side).
b. If the line of action of the headgear force passes close to or through the unit's centre of resistance, 350–450 g per side can be used.
8. Monitor for changes as treatment proceeds. Adjust the force line of action and force magnitude as necessary.
Extraction treatment approach: Over the last few years, it is certainly true that the advances in orthodontic treatment mechanics, philosophies and material science have curtailed the need for extractions in severe discrepancies. However, on many occasions, it has always been a difficult task for the clinician to make the extraction or nonextraction treatment decision to resolve a specific malocclusion. There are several factors that influence this decision. The severity of malocclusion like the amount of intra-arch crowding requires extraction of some dental units; however, its impact on the soft tissue profile of the face should be considered in the treatment planning process.
Management of extraction space One of the most important factors in extraction treatment approach is effective utilization of extraction space to resolve the existing discrepancy (Fig 3.23). There are several techniques that maybe employed for orthodontic space closure; however, the clinician should select the technique that efficiently brings about the desired tooth movement. Also, the orthodontic space closure planning should be individualized and should address the individual patient problems and the patient's chief complaint. One can use either a two-step space closure mechanics in which individual retraction of cuspids is followed by incisor retraction, or an en masse retraction of all six anterior teeth in a single stage (Fig 3.23E and F). However, it is the author's experience that the two-step space closure method, which is believed to be less detrimental to the anchorage, temporarily impairs the anterior aesthetics due to shifting of the extraction space from the distal of canine to the mesial of canine and prolongs the treatment duration. However, independent cuspid retraction can be the method of choice in certain cases, which requires space for decrowding of anterior teeth.
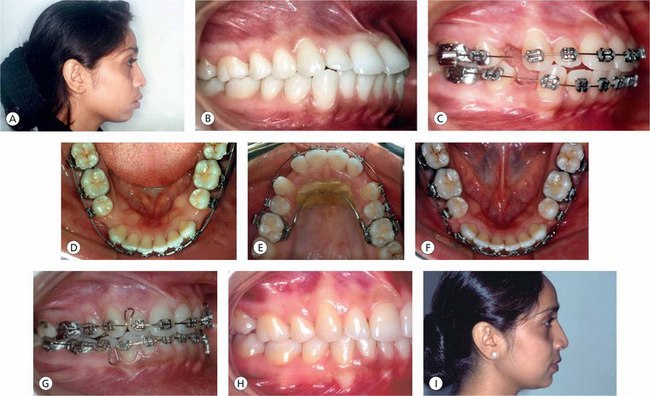
Figure 3.23 Extraction treatment approach. (A) Pretreatment facial profile of an adult female patient exhibiting acute nasolabial angle and protrusive lips. (B) Class I molar relationship and severe maxillary and mandibular incisor proclination. (C) Alignment and levelling of maxillary and mandibular arches before the initiation of retraction mechanics. (D) The management of extraction space is based upon the concept of differential extraction space closure (anterior retraction versus posterior protraction). (E) A two-step space closure mechanics (retraction of cuspids followed by incisor retraction) in the maxillary arch. (F) En masse retraction of six anterior teeth in a single stage in the mandibular arch. (G) Closure of extraction spaces with loop mechanics. (H–I) Posttreatment occlusal relationships and posttreatment balanced facial profile.
The following factors influence extraction space closure.53
1. Severity of discrepancy: the severity of the problems like the degree of proclination, crowding, etc. plays an important role in determining the extent of extraction space required to resolve the discrepancy. The practitioner should plan the mechanism of space closure by determining the amount of extraction space to be utilized by anterior retraction as against the residual space closure by protraction of posterior teeth. This differential space closure mechanics demands a good control over the anterior and posterior dental units.
2. Midline discrepancies: patients with transverse dental problems present with or without asymmetric left- and right-side occlusal relationships. Application of asymmetric forces in an effort to correct midline discrepancies can produce untoward effects like asymmetric anchorage loss, unilateral vertical forces, etc. An efficient and effective approach to the resolution of midline discrepancies is to correct the asymmetries in the early part of treatment followed by symmetric mechanics for the residual discrepancies.
3. Anchorage: control of anchorage units is one of the important elements in space closure mechanics. While planning space closure, the clinician should assess the anchorage units, understand the concept of differential anchorage and determine whether entire extraction space will be closed by retraction or decrowding and alignment of anterior teeth or if some degree of sagittal movement of molars is desired to close the space and then plan the mechanics accordingly. Using the same universal mechanics for different anchorage requirements limits the ability of the practitioner to achieve desired results.
4. Axial inclination of canines and incisors: patients with Class II malocclusions present with variable axial inclinations of cuspids and incisors – mesially inclined, upright or distally inclined. The same degree of force or moment applied to these teeth during the space closure mechanics will result in different types of tooth movements. Therefore, the clinician should assess the axial inclinations of cuspids and incisors and design the force system accordingly to achieve desired tooth movement.
Management of vertical dentoalveolar problems: As mentioned earlier, the sagittal discrepancies are not a single entity and are often associated with vertical problems. Class II malocclusions are also associated with vertical discrepancies like deep overbite or open bite. For the successful and stable correction of Class II malocclusion, the treatment plan must include the identification and the correction of these vertical components. The management of these problems is explained in detail in Chapter 4.
Orthodontic camouflage: A treatment alternative for skeletal discrepancy
Orthodontic camouflage consists of the repositioning of the dentition in order to obtain proper molar and incisor relationships in patients with underlying skeletal discrepancies with a favourable effect on facial aesthetics. For some reason, if the patient does not accept the orthosurgical treatment approach for the correction of a dentofacial deformity, camouflage proves to be quite useful. The goal is to achieve certain degree of dentofacial aesthetics and establish proper occlusion, accepting the limitations in skeletal relationships. The success of camouflage treatment approach depends on the severity of underlying sagittal discrepancy. In mild to moderate skeletal Class II malocclusions, movement of teeth to achieve dentoalveolar changes and aesthetic results is much better than those in severe skeletal Class II problems. In severe Class II patients, the need for greater displacement of teeth relative to their bony bases, either by extraction or by nonextraction approach is possible due to improvements in orthodontic treatment mechanics but only at considerable expense to facial aesthetics. Therefore, the clinician should assess the case carefully for camouflage approach for the underlying skeletal discrepancy to plan treatment mechanics and strike a balance between occlusal and facial aesthetic goals.
Management of functional class II malocclusion
There are many systematic, definitive treatment methods available and possible in typical Class II malocclusions, and there are some cases that require a specific diagnostic protocol to identify the problem and design a treatment plan. One such type of discrepancy is a functional Class II malocclusion (Figs 3.24–3.26).
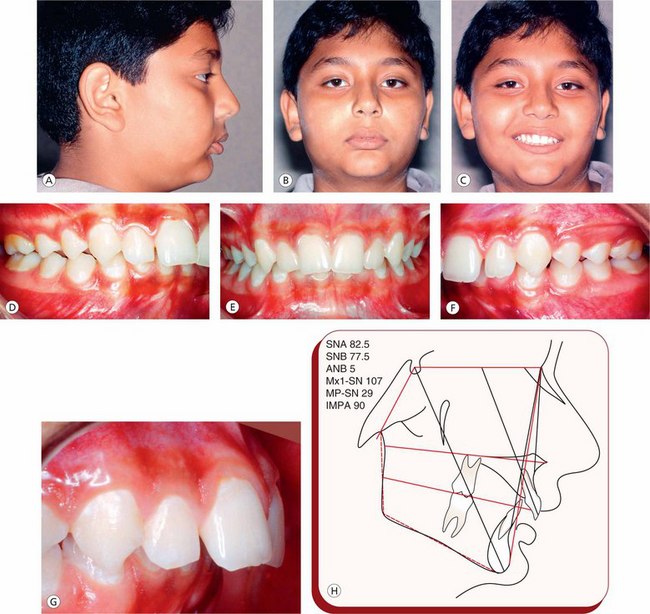
Figure 3.24 Pretreatment records of a growing patient. (A–C) Convex profile and deep mentolabial groove. (D-G) Class II division 1 malocclusion with severe overjet and overbite. The functional examination demonstrated a distally forced bite. (H) Pretreatment lateral cephalometric tracing.
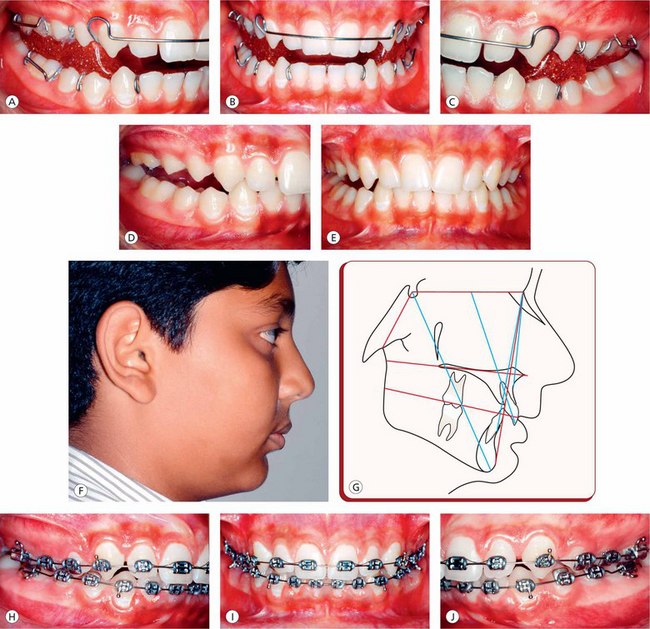
Figure 3.25 The treatment strategy included 8-month use of a twin-block appliance to improve abnormal skeletal relationships, followed by fixed appliance therapy to fine-tune the dentition. (A–C) Use of a twin-block appliance. (D–G) Post twin block therapy occlusion, facial profile and lateral cephalometric tracing. (H–J) Fixed appliance therapy.
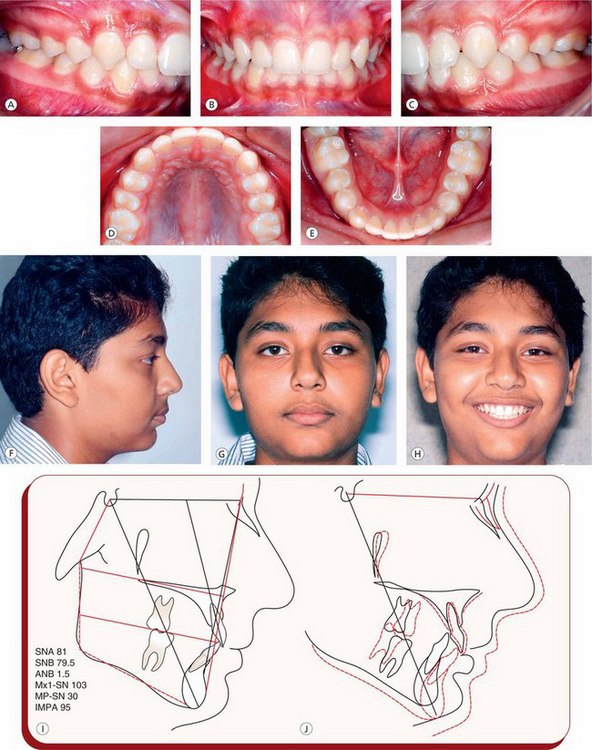
Figure 3.26 Posttreatment records. (A–E) Normal occlusal relationships and archforms. (F–H) Orthognathic profile. (I) Posttreatment lateral cephalometric tracing. (J) Pretreatment and posttreatment lateral cephalometric superimposition.
Functional criteria as the determinant of treatment method: In functional retrusion cases, it is essential to perform a functional analysis as a part of the clinical examination before selecting a specific appliance therapy. The practitioner should determine the path of closure of the mandible and analyze the relationship between the postural rest and habitual occlusal position. The mandible moves upward and backward from rest position into a forced retrusive habitual occlusion. There is a rotary action of the condyle in the glenoid fossa from postural rest to initial contact of teeth. From the initial contact to habitual occlusion, the action of the condyle is rotary and translatory – upward and backward. This is also called a distally forced bite or posterior shift. This type of condylar movement is commonly seen in patients with excessive overbite. The Class II malocclusion with functional disturbances appears more severe than it actually is sagittally.
Usually the base of the mandible is of normal size with no growth deficiency. The SNB angle is smaller in habitual occlusion, but it improves in the postural resting position. The Class II relationship is mainly of dental nature caused by improper intercuspation. The treatment goal is to eliminate the functional disturbance and not to alter the postural resting position of the mandible. The early treatment of such problems involves interceptive functional therapy – screening type of appliances or activators and twin-blocks with or without the occlusal equilibration in the later stages of therapy.
Treatment of skeletal Class II malocclusion
The treatment of skeletal Class II malocclusion is based on careful and accurate diagnosis. In skeletal Class II malocclusions, it is not just that the skeletal bases are at fault; there are many variations involving various skeletal components and dental compensations in anteroposterior plane, often associated with vertical problems. Before planning the treatment, the orthodontist should localize and quantify skeletal contributions and dental displacements associated with the problem. There are numerous variations of skeletal Class II discrepancies, and it is beyond the scope of this chapter to identify each type and discuss its treatment; however, for the purpose of description, the commonly observed skeletal relationships can be grouped as maxillary protrusion with normal mandible, normal maxilla and retrognathic mandible, a combination of maxillary protrusion and mandibular retrusion and a vertical problem. There is no universal treatment approach to deal with skeletal Class II problems; therefore, the treatment should be directed at the individual patient's specific problem area.
Maxillary prognathism: It is characterized by a large maxillary base or a normal maxilla, which is positioned anteriorly with respect to the cranial base associated with a normal mandible (Fig 3.27). In the management of patients with skeletal problems, the growth direction plays an important role in the selection of a treatment strategy. In a Class II relationship, with a fault in the maxilla during mixed dentition, the treatment goal is to inhibit growth in the midface region and allow the normal growth of the mandible. This produces orthopaedic midface changes to alter the maxillary position in relation to the mandible and the anterior cranial base.
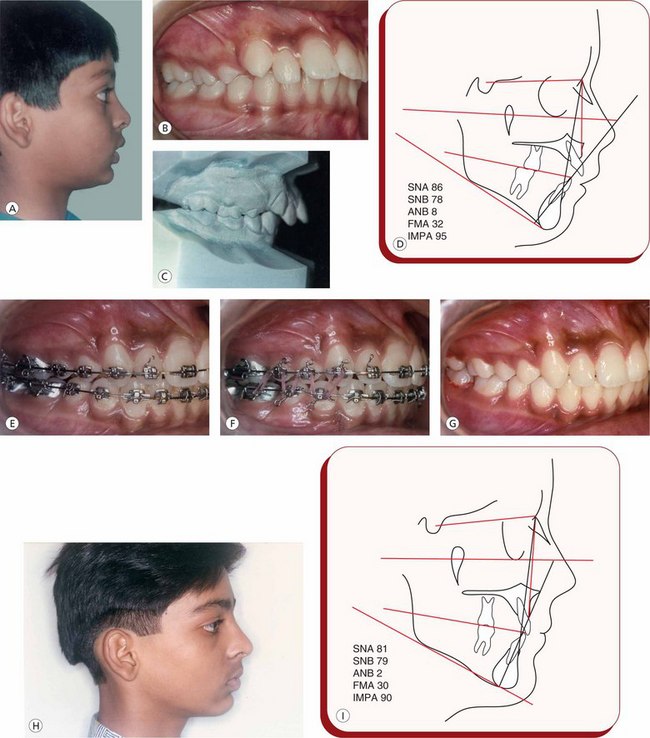
Figure 3.27 Management of maxillary prognathism in a 12-year-old male patient. (A) Pretreatment convex profile, incompetent lips. (B) Intraoral photograph showing late mixed dentition stage and proclination of maxillary incisors and Class II molars. (C) Pretreatment study models in occlusion to demonstrate the magnitude of overjet and overbite. (D) Pretreatment lateral cephalometric tracing showing skeletal Class II relationship due to maxillary prognathism. (E) The treatment approach consisted of the use of molar-inserted combination pull headgear, along with the fixed appliance therapy. Molars are in super Class I relationship with normal overjet and overbite. (F) Settling of posterior teeth with vertical elastics. (G) Posttreatment normal occlusal relationship. (H) Posttreatment orthognathic profile. (I) Posttreatment cephalometric tracing exhibiting normal skeletal and dental relationships.
Extraoral heavy forces, with the help of a headgear assembly, applied to the maxillary first molars are used for growth inhibition in the midface region. This treatment approach used in growing patients produces a desired maxillary skeletal change.54 A headgear used for this purpose should be designed to deliver an optimal extraoral orthopaedic force to compress the maxillary sutures, modifying the pattern of bone apposition at these sites. To be effective for this purpose, the extraoral force should be of much greater magnitude, in the range of 400–600 g per side, worn at least 12–14 h per day to produce a skeletal change and to minimize dental effects.52
Apart from the force magnitude and duration, the direction of the extraoral force should be determined based on the vertical relationships observed in the patient or the growth pattern. The extraoral attachment can be cervical or occipital to establish a low or a high angle of force vector. To achieve the maximum skeletal improvement by affecting the maxillary sutures, a superior and posterior force vector through the centre of resistance of the maxilla appears to be the most appropriate direction. The extraoral force vector also depends on the height and length of outer bow. Raising or shortening the outer bow moves the force vector superiorly, and lowering or lengthening the outer bow moves the force vector inferiorly. Often, the mandibular arch is normal and the occlusal plane is flat; however, if the maxillary incisors are flared and tipped labially, they should be retracted first. If the maxillary arch is constricted, an extraoral traction should be preceded by an initial phase of maxillary expansion.
The goal of orthopaedic treatment with the headgear is to restrict normal downward and forward maxillary growth by compressing the maxillary sutures and altering the growth and apposition of bone at these sutures, while allowing the mandible to grow normally.
Mandibular retrusion: The Class II malocclusion, characterized by mandibular deficiency and orthognathic maxilla, is often associated with some degree of dental compensations. The treatment strategies in such cases are directed to establish orthognathic profile and lip seal and to improve facial muscle function by promoting optimal mandibular growth in the first phase of treatment, followed by detailing of dentition using the contemporary fixed appliances in the second phase (Figs 3.28-3.30). This desired sagittal change can be achieved by posturing the mandible forward using one of the functional jaw orthopaedic appliances.
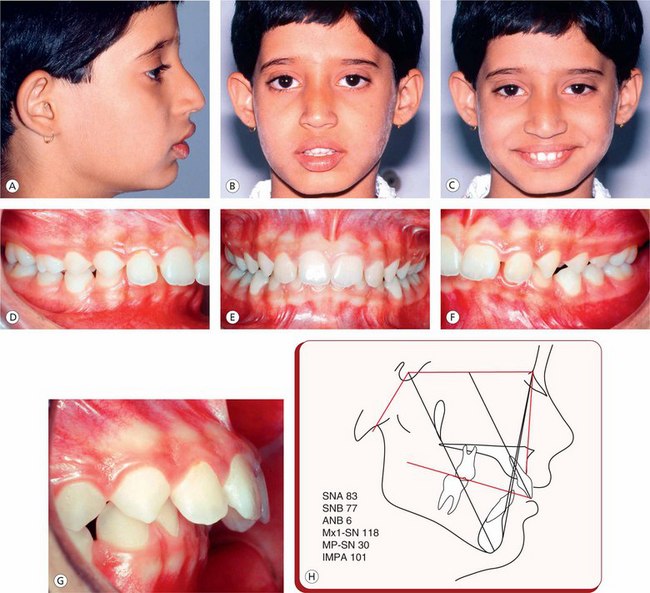
Figure 3.28 Pretreatment records of a female growing patient. (A–C) Convex profile, deep mentolabial groove and incompetent lips. (D–G) Class II division 1 malocclusion with severe overjet and overbite. It is characterized by mandibular skeletal retrusion. (H) Pretreatment lateral cephalometric tracing.
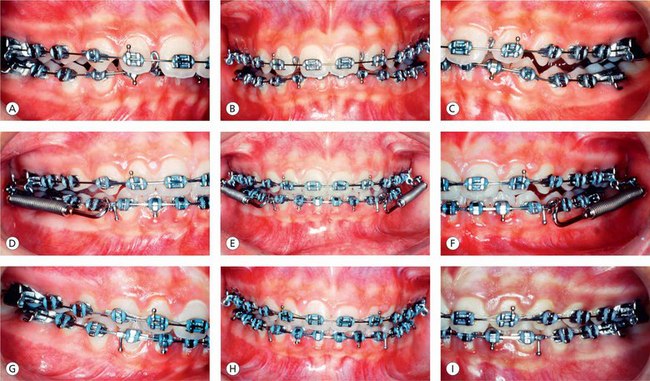
Figure 3.29 Treatment plan included an advancement of retruded mandibular position with a fixed functional appliance. (A–C) Prior to fixed functional appliance mechanotherapy. (D–F) Fixed functional appliance therapy. (G–I) After fixed functional appliance finishing and detailing of dentition.
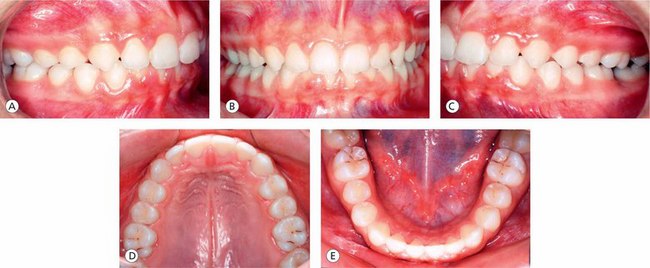
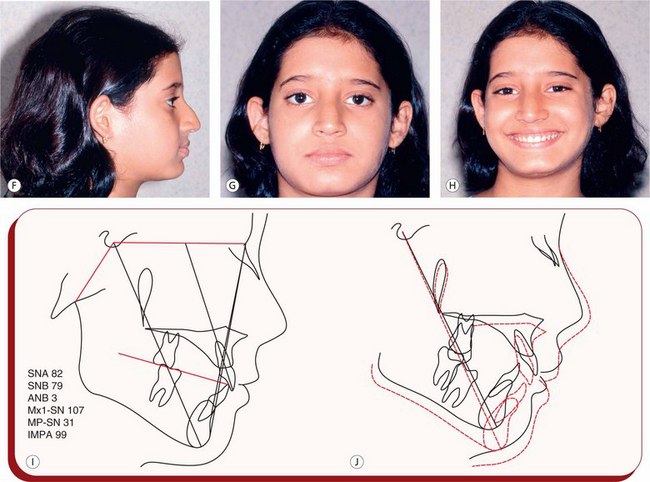
Figure 3.30 Posttreatment records. (A–E) Posttreatment occlusion and archforms. (F–H) Orthognathic profile and normal frontal facial proportions. (I) Posttreatment lateral cephalometric tracing. (J) Pretreatment and posttreatment lateral cephalometric superimposition.
This sagittal change is dependant on growth guidance and adaptive processes for the desired skeletal modification. One of the treatment methods in patients with deficient mandible is to hold the normally positioned maxilla and allow the mandible to express its normal growth. The literature shows that the patients wearing headgear that is attached to the maxilla exhibit more mandibular growth than untreated Class II patients.55 It remains to be seen whether this statistically significant extra mandibular growth is clinically significant. The author's treatment of choice in patients with mandibular deficiency is to enhance the mandibular growth using a variety of functional appliances. It is believed that mere unloading of the condyle by forward mandible posturing contributes to a significant condylar growth.56,57 It should be recognized that it is not only the apparent condylar position in glenoid fossa but the more retruded fossa itself to be used as a criterion in Class II malocclusion.58,59 More condylar growth increments and a change in the direction of growth to a more upward and backward vector are associated with the use of functional appliances.60,61 The research has also shown significant change in the position of the glenoid fossa with respect to the anterior cranial base.62 Unloading of the condyle associated with downward and forward posturing of the mandible also enhances metabolic action in the temporomandibular joint (Fig 3.31).63 It is not just a mere forward posturing of the mandible but an increased anabolic and catabolic exchange that may contribute to enhanced growth of the condyle and posterior wall proliferation.64,65
Treatment of Class III malocclusion
The treatment options for the management of Class III malocclusion are dependant on the age of the patient and the components involved. There are various types of Class III malocclusions; however, for the purpose of discussion these can be categorized into following groups:
2. Functional Class III malocclusion (with pseudo-forced bite or anterior displacement)
3. Class III malocclusion with retruded maxilla
4. Class III malocclusion with mandibular prognathism
5. Class III malocclusion with a combination of maxillary retrognathism and mandibular prognathism
The treatment approach to the correction of Class III malocclusion should be individualized, and it should be designed to address the specific nature of the dental, skeletal or functional imbalances. It has been generally recognized that Class III malocclusions are one of the most difficult problems to treat. It has been observed that before adolescence, some of the features of vertical discrepancy like increased lower anterior face height, steep mandibular plane angle, excessive eruption of posterior teeth, anterior open bite, etc. are located below the palatal plane.66 The goal of early Class III treatment is to create an environment that promotes favourable dentofacial growth.67
Dentoalveolar Class III malocclusion
The dentoalveolar Class III malocclusion is characterized by abnormal sagittal incisor position; the ANB angle within normal limits is suggestive of normal basal relationship. In such cases, the maxillary incisors are tipped lingually and the mandibular incisors are tipped labially. Most Class III malocclusions exhibit these characteristics during the initial stages of development; however, after the eruption of the permanent teeth these problems become more severe. It has been reported that Class III skeletal discrepancies tend to worsen with age.68 If anterior crossbite exists for prolonged duration, it may enhance the mandibular prognathism and retard the maxillary sagittal development. This demands early institution of appropriate treatment, the goal being the establishment of a normal functional engram and stimulus in the developing face. The treatment is aimed at uprighting lingually tipped maxillary incisors and labially tipped lower incisors (Figs 3.32-3.34). Quite often, maxillary arch expansion is required to unravel the transverse component. Several researchers have attempted to predict the growth of Class III malocclusion.69,70 It is infact difficult to predict as to which case will primarily remain as dentoalveolar in nature and which one will become more severe, involving the skeletal components. However, hereditary pattern plays an important role in early prediction.

Figure 3.32 Pretreatment records. (A–C) Facial photographs. (D–F) Dentoalveolar Class III malocclusion. Molars in super Class I relationship and canines in Class III relationship; incisors are in crossbite. (G and H) Square maxillary archform and mild mandibular anterior crowding.
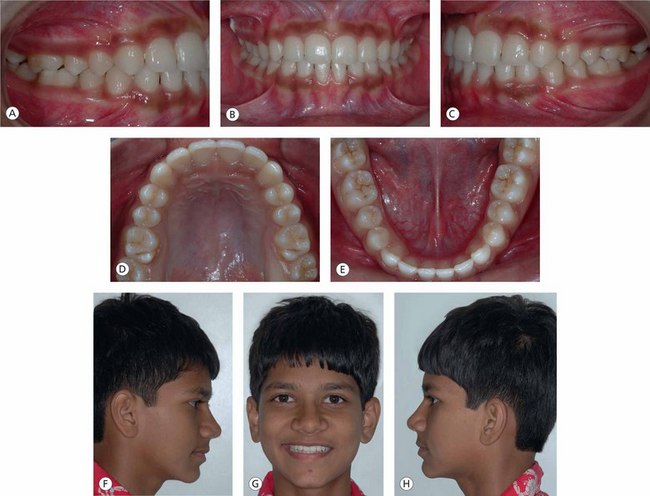
Figure 3.34 Posttreatment records. (A–C) Normal occlusal relationship – Class I molars and canines and normal overjet and overbite. (D and E) Coordinated and compatible archforms. (F–H) Normal facial features.
In some patients, early diagnosis of the problem is sometimes possible with the help of the lateral cephalogram. A long mandibular base with spaces between the developing unerupted teeth may be an indication of future prognathism.
Dentoalveolar movements to camouflage skeletal Class III discrepancy: For patients with Class III malocclusions diagnosed during the permanent dentition period, treatment options are very limited. Such problems that are not resolved during mixed dentition by orthopaedic treatment usually require comprehensive fixed appliance therapy or surgical intervention. For some reasons, if surgical correction is not considered in the final treatment plan to resolve the underlying skeletal discrepancy, camouflage by dentoalveolar movements is the only treatment option (Figs 3.35-3.37). In mild discrepancy cases, camouflage involves the use of mid Class III elastics with or without extraction of teeth to produce acceptance facial profile change.
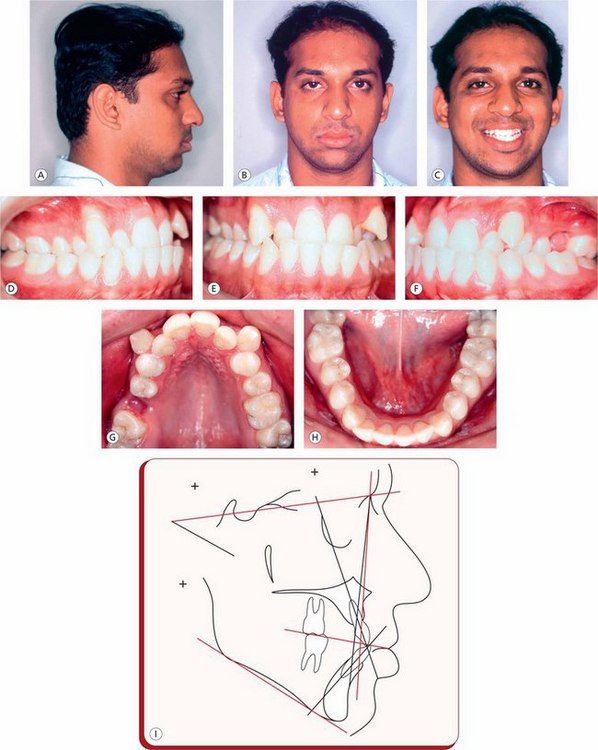
Figure 3.35 Pretreatment records of an adult male patient. (A–C) Extraoral features show obtuse nasolabial angle and prominent lower lip. (D–F) Bilateral posterior crossbite, anterior crossbite and high labially placed maxillary canines. (G) Severe maxillary anterior crowding and contracted arch. (H) Normal mandibular arch. (I) Pretreatment lateral cephalometric tracing.

Figure 3.36 Treatment plan involved dentoalveolar movements to camouflage skeletal Class III discrepancy. (A) Optimal maxillary arch expansion to correct posterior crossbite and gain adequate space for the cuspids. (B–D) Orthodontic treatment mechanics to improve occlusal relationship. (E and F) Normal maxillary and mandibular archforms.

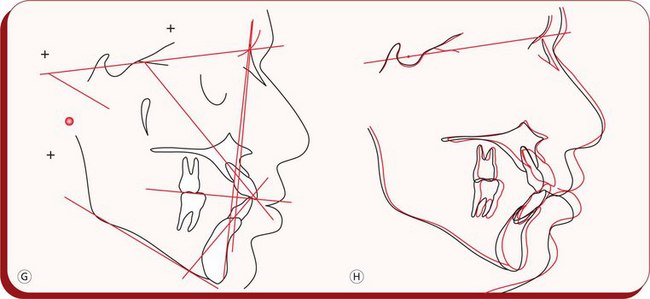
Figure 3.37 (A–F) Posttreatment records demonstrate improved dentition and soft tissue facial features. (G) Posttreatment l ateral cephalometric tracing. (H) Pretreatment and posttreatment lateral cephalometric superimposition.
Though this approach improves interincisal relationship and overall occlusion, retraction of mandibular incisors makes the chin more prominent and often magnifies the facial aesthetic problems. Therefore, camouflage treatment in Class III malocclusions is generally considered less successful than in Class II problems.
Functional Class III malocclusion
Functional Class III malocclusion is characterized by an edge-to-edge incisor relationship or by an anterior cross-bite caused by a premature tooth contact or by an abnormal positioning of the maxillary and mandibular incisors. At an early stage, patients with functional Class III do not show abnormal skeletal relationships. Usually the mandible slides anteriorly due to tooth guidance in the canine region (Fig 3.38). The early correction of this clinical situation involves a careful equilibration of canines to eliminate the prematurity. Some patients having chronic nasorespiratory problems often present with contracted maxillary arch leading to decreased intercanine width with resultant tooth guidance. In such cases, maxillary arch expansion without equilibration of canines is just what is required to eliminate the tooth guidance and settle the occlusion. Such discrepancies should be resolved at an early stage as they are generally considered the beginning signs of true Class III malocclusions.

Figure 3.38 Functional mandibular shift. (A) Pretreatment photograph showing functional shift of the mandible anteriorly and laterally (left side) in a deciduous dentition stage. This has resulted into midline shift and upper and lower arch width discrepancy. (B) Expansion appliance with posterior occlusal coverage. (C) Before the appliance removal, the mandible is in normal position in both sagittal and transverse planes.
In some instances, anterior displacement of the mandible is also associated with skeletal Class III malocclusion. The natural compensation of teeth, expressed as the labial tipping of the maxillary incisors and lingual tipping of the mandibular incisors, makes the patient slide the lingual surfaces of the mandibular incisors against the incisal edges of maxillary incisors after initial contact during closure. This produces anterior displacement of the mandible on the path of closure from postural rest to habitual occlusion. In habitual occlusal position, the mandible appears to be even further anteriorly positioned. This abnormal position of the mandible, coupled with sagittal skeletal discrepancy and unfavourable axial inclinations of maxillary and mandibular incisors makes the orthodontic treatment extremely difficult. The treatment usually consists of surgical orthodontic intervention in adults.
Skeletal Class III malocclusion
The Class III malocclusion with the underlying skeletal discrepancy could be due to maxillary retrusion, mandibular prognathism or due to the combination of maxillary retrusion and mandibular prognathism. The treatment protocol for the resolution of skeletal Class III malocclusion should be individualized based on the location and the specific nature of the affected regions of the craniofacial complex.
Maxillary skeletal retrusion: The skeletal Class III malocclusion due to maxillary skeletal retrusion is characterized by small and retrognathic maxillary base with small SNA and normal SNB angles. Early treatment of such patients involves growth guidance during the eruption of the maxillary incisors.
The orthopaedic facial mask The orthopaedic facial mask is the appliance of choice in the management of patients with mild to moderate Class III malocclusions having a retruded maxilla and a hyperdivergent growth pattern in the early mixed or late deciduous dentition (Figs 3.39–3.41). For patients exhibiting vertical or hyperdivergent growth pattern, the use of bonded acrylic maxillary expansion appliance controls the vertical eruption of molars. The orthopaedic facial mask is a very versatile appliance and produces the most dramatic improvements in the shortest period of time. It affects almost all areas contributing to the development of Class III malocclusion like maxillary basal retrusion, retrusion of maxillary dentoalveolar region, prognathic mandible and decreased lower facial height.
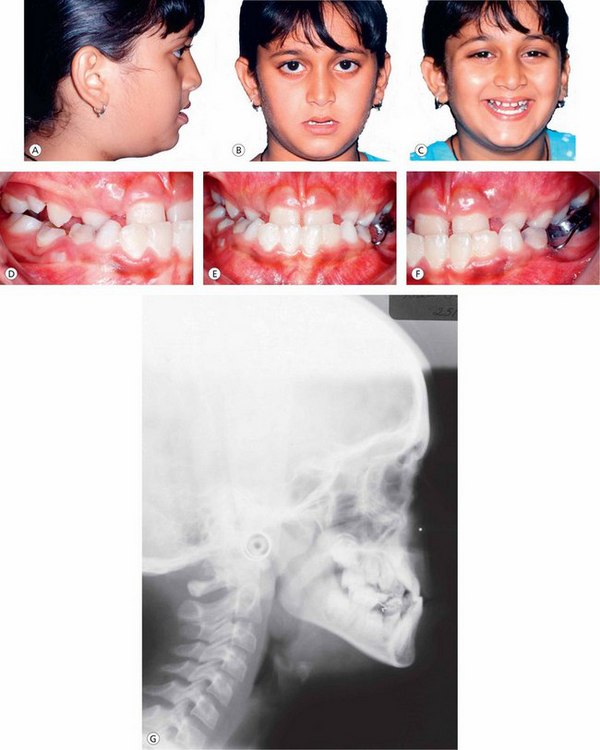
Figure 3.39 Pretreatment records of a female patient in the early mixed dentition stage. (A–C) Extraoral photographs demonstrate premaxillary deficiency. (D–F) Intraoral pictures show anterior and bilateral posterior crossbite. (G) Pretreatment lateral cephalogram.
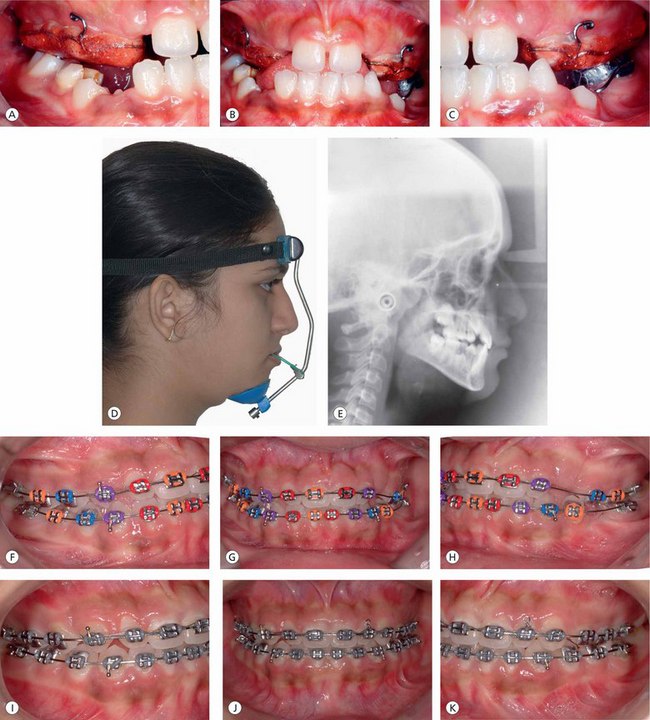

Figure 3.40 Treatment plan consisted of maxillary protraction with reverse pull headgear followed by contemporary fixed appliance therapy for detailing of the dentition. (A–C) Cemented maxillary splint with occlusal coverage and expansion device. (D) Orthopaedic facial mask. (E) Postmaxillary protraction lateral cephalogram. (F–H) Initial alignment and levelling of teeth. (I–K) Finishing and detailing. (L and M) Normal maxillary and mandibular archforms.

Figure 3.41 Posttreatment records. (A–C) Normal occlusal relationships. (D–F) Balanced facial profile. (G) Lateral cephalogram exhibiting normal skeletal, dental and soft tissue relationships.
The orthopaedic facial mask system has various components: an acrylic bonded maxillary splint that provides a rigid maxillary anchorage, the facial mask and elastics (Fig 3.40C and D).
The optimal time to resolve skeletal Class III malocclusion with maxillary basal retrusion and orthopaedic facial mask is at the time of initial eruption of the maxillary central incisors. The primary and early mixed dentition developmental periods are considered to promote better skeletal and dental response.71 However, recent evidence shows that the protraction of maxilla is effective through puberty with less skeletal response as the sutures mature.72,73
To elicit a maximum skeletal change, the patient should wear the appliance for at least 12–14 h a day, with orthopaedic force levels of 300–400 g per side in the primary and mixed dentitions. Most patients with maxillary retrusion are also vertically deficient. Therefore, the elastic pull can be directed little downward to lower the maxilla, which increases the face height and rotates the mandible downward and backward, contributing to the sagittal and vertical skeletal correction. It is the author's experience that, on an average, approximately 6–8 months of prescribed use of orthopaedic facial mask produces desired skeletal changes.
Several circummaxillary sutures – frontomaxillary, nasomaxillary, zygomaticomaxillary, zygomaticotemporal, pterygopalatine, intermaxillary, lacrimomaxillary and ethmomaxillary sutures – contribute to the development of the nasomaxillary complex. To bring about rapid and significant maxillary protraction, it is essential to disarticulate the maxilla and initiate cellular response in the circummaxillary sutures. It has been found that the forward displacement of the maxilla is significantly greater when face mask is used in association with rapid maxillary expansion when compared with the protraction without rapid maxillary expansion.74 The timing of the protraction pull on the retruded maxilla is critical. The protraction of the maxilla appears to be greater when it is carried out during maxillary expansion when compared with protraction after expansion.74
In pseudo-Class III patients, it is common to observe a rapid shift in the occlusal relationship and a correction of a CO-CR discrepancy. Along with skeletal improvements, the face mask produces forward movement of maxillary dentition and lingual tipping of mandibular incisors.
In patients who do not require increase in transverse dimension, it is still advisable to activate the expansion appliance for a week to disrupt the maxillary sutural system to generate more positive reaction to protraction forces.75
The key to prevent posttreatment relapse is to maintain a positive overjet and overbite during the retention period. As some degree of regression of the overjet is expected during the early posttreatment period, it is important to achieve a positive overjet of approximately 4 mm before the facial mask therapy is discontinued.
Mandibular skeletal protrusion: Skeletal Class III malocclusion with a mandibular prognathism and normal maxilla is characterized by larger SNB angle and normal SNA angle, producing a negative ANB difference. The mandible is longer with frequent findings of large gonial angle and small articular angle. Quite often, it is also anteriorly positioned. Patients with this malocclusion exhibit dentoalveolar compensation – maxillary incisors are tipped labially and the mandibular incisors are lingually inclined. A wider part of the mandible occludes with a narrower part of the maxilla, leading to a posterior crossbite. These malocclusions are extremely difficult to correct, and in severe problems, surgery is the only treatment option.
The early treatment of mandibular skeletal protrusion involves the use of functional appliances and orthopaedic chin cups. Functional appliances have very limited role in the management of mandibular prognathism and usually work by rotating the mandible downward and backward, allowing the maxillary posterior teeth to erupt downward and forward while inhibiting the eruption of mandibular teeth and promoting proper occlusal relationships. This treatment approach is indicated in patients with normal or decreased lower anterior facial height and mild mandibular skeletal problem.
Another approach to deal with mandibular prognathism is the use of orthopaedic chin cups of two different types; the occipital-pull chin cup that is indicated in case of mandibular prognathism and vertical-pull chin cup that is advocated in patients with increased lower facial height and steep mandibular plane angle. The treatment with chin cup to influence mandibular skeletal protrusion is effective in patients during the primary or early mixed dentition period76 (Fig 3.42A and B).
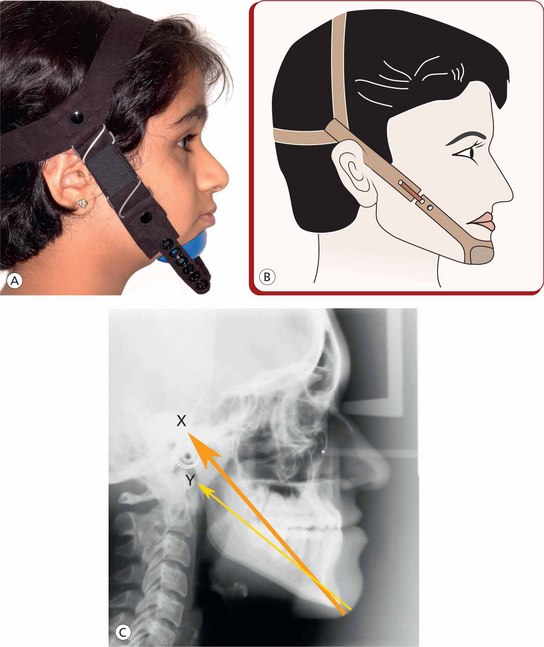
Figure 3.42 (A and B) Chin cup therapy for mandibular prognathism. (C) The direction of the chin cup pull can be applied through the mandibular condyle if the objective is to impede mandibular growth (X), and the line of chin cup force can be below the mandibular condyle to deliberately rotate the chin downward and backward (Y).
There are two ways in which the direction of the chin cup pull is applied. If the orthopaedic force is directed below the condyle, the downward and backward rotation of the mandible is expected. This is helpful in patients with short lower anterior facial height; however, in patients in whom the vertical dimension needs to be maintained, the force should be applied through the condyle to help restrict mandibular growth (Fig 3.42C).
It is recommended that the patient should use the chin cup for 12–14 h per day with orthopaedic force levels of 300–400 g per side. It has been shown that the early correction of an anterior crossbite with a chin cup appliance prevents impaired sagittal growth of the maxilla.76 There has been some concern among clinicians about chin cups creating pressure on the TMJ, since several patients were reported of having temporary soreness of TMJ.77 It is recommended that patients undergoing chin cup therapy should be monitored for TMD signs and if noted, the treatment should be discontinued immediately.
Conclusion
A large portion of sagittal discrepancies are not just a single entity and are often associated with a variety of combinations of significant skeletal, dental and functional imbalances not just in anteroposterior plane but in vertical plane as well. In dealing with these malocclusions, contemporary orthodontic assessment and interpretation must include their proper understanding with respect to the recognition of various components involved and their interaction with the sagittal dimension. However, it should be recognized that the reliable identification of such cases requires the development of extensive diagnostic skills.
In the existing scenario, there appears to be a controversy regarding the facial growth modification, its optimal timing and the efficacy of the various appliances used. The current methods of management of these problems also reveal a great deal of variability in the clinical response of different patients to similar treatment modality. The key to successful resolution of various sagittal discrepancies is that the treatment protocol for each patient be individualized, based on the recognition, location and the specific nature of the affected regions of the craniofacial complex.
A wide spectrum of treatment modalities exist for the sagittal discrepancies at different developmental stages – acceleration or inhibition of the craniofacial growth, and the correction of abnormal dental relationships. This chapter has provided the systematic approach to the diagnosis and treatment planning of various sagittal discrepancies based on refined treatment goals, treatment options for various stages of development and their resolution with appropriate treatment mechanics and long-term stability.
References
1. Angle, E.H. Treatment of malocclusion of the teeth and fractures of the maxillae: angle's systems., 6, Philadelphia: SS White Dental Manufacturing, 1900.
2. Graber, T.M., Rakosi, T., Petrovic, A.G. Treatment of Class II malocclusions. In: In: Dentofacial orthopedics with functional appliances. St Louis, Missouri: The C.V. Mosby company; 1985:346–380.
3. Moyers, R.E., Guire, K.E., Riolo, M. Differential diagnosis of Class II malocclusion. Am J Orthod. 1980;74:477–494.
4. Sarver, D.M. The esthetic impact of orthodontics: planning treatment to meet patient's needs. J Am Dent Assoc. 1993;124:99–102.
5. Björk, A. Prediction of mandibular growth rotation. Am J Orthod. 1969;55:585–599.
6. Moyers, R.E. Analysis of craniofacial skeleton: cephalometrics. In: In: Handbook of orthodontics. Year Book Medical publishers; 1988:270.
7. Skieller, V., Björk, A., Linde-Hansen, T. Prediction of mandibular growth rotation evaluated from a longitudinal implant sample. Am J Orthod. 1984;86:359–370.
8. Litton, S.F., Ackermann, L.V., Isaacson, R.J., et al. A genetic study of Class III malocclusion. Am J Orthod. 1970;58:565–577.
9. Harris, J.E., Kowalski, C.J., Watnick, S.S. Genetic factors in the shape of the craniofacial complex. Angle Orthod. 1973;43:109–111.
10. Rakosi, T., Schilli, W. Class III anomalies: a coordinated approach to skeletal, dental and soft tissue problems. J Oral Surg. 1981;39:860–870.
11. Ellis, E.E., McNamara, J.A., Jr. Components of adult Class III malocclusion. J Oral Maxillofac Surg. 1984;42:295–305.
12. Guyer, E.C., Ellis, E., McNamara, J.A., Jr., Behrents, R.G. Components of Class III malocclusion in juveniles and adolescents. Angle Orthod. 1986;56:7–31.
13. Ngan, P., Hàgg, U., Yiu, C., et al. Soft tissue and dentoskeletal profile changes associated with maxillary expansion and protraction headgear treatment. Am J Orthod Dentofacial Orthop. 1996;109:38–49.
14. Turley, P. Orthopaedic correction of Class III malocclusion with palatal expansion and custom protraction headgear. J Clin Orthod. 1988;22:314–325.
15. Kwong, W.L., Lin, J.J. Comparison between pseudo and true Class III malocclusion by Veterans' General Hospital cephalometric analysis. Clin Dent. 1987;7(2):69–78.
16. Latham, R.A. The sella point and postnatal growth of the human cranial base. Am J Orthod. 1972;61:156–162.
17. Breece, G.L., Nieberg, L.G. Motivations for adult orthodontic treatment. J Clin Orthod. 1986;20:166–171.
18. Shaw, W.C., Rees, G., Dawe, M., Charles, C.R. The influence of dentofacial appearance on the social attractiveness of young adults. Am J Orthod. 1985;87:21–26.
19. Shaw, W.C. The influence of children's dentofacial appearance on their social attractiveness as judged by peers and lay adults. Am J Orthod. 1981;79:399–415.
20. Adams, G.R. Physical attractiveness research: toward a developmental social psychology of beauty. Hum Dev. 1977;20:217–239.
21. Harris, E.F., Behrents, R.G. Intrinsic stability of Class I molar relationship: a longitudinal study of untreated cases. Am J Orthod Dentofacial Orthop. 1988;94:63–67.
22. Laine, T. Malocclusion traits and articulatory components of speech. Eur J Orthod. 1992;14:302–309.
23. Burstone, C.J. Lip posture and its significance in treatment planning. Am J Orthod. 1967;53:262–284.
24. Little, R.M., Wallen, T.R., Riedel, R.A. Stability and relapse of mandibular anterior alignment. First premolar extraction cases treated by traditional edgewise orthodontics. Am J Orthod. 1981;80:349–365.
25. Sadowsky, C., Sakols, E.I. Long-term assessment of orthodontic relapse. Am J Orthod. 1982;82:456–463.
26. Nikolai, R.J. On optimum orthodontic force theory as applied to canine retraction. Am J Orthod. 1975;68:290–302.
27. Tanne, K., Koenig, H.A., Burstone, C.J. Moment to force ratios and the centre of rotation. Am J Orthod. 1988;94:426–431.
28. Hixon, E.H., Aasen, T.O., Arango, J., et al. On force and tooth movement. Am J Orthod. 1970;57:476–488.
29. Gianelly, A.A. Crowding: timing of treatment. Angle Orthod. 1994;64:415–418.
30. Nance, H.N. The limitations of orthodontic treatment Part 1. Am J Orthod. 1947;33:177–223.
31. Leighten, B.C. The early signs of malocclusion. Trans Eur Orthod Soc. 1969;45:353–368.
32. Armstrong, M. Controlling – the magnitude, direction and duration of extraoral force. Am J Orthod. 1971;59:217–243.
33. Pancherz, H. Treatment of Class II malocclusions by jumping the bite with Herbst appliance. A cephalometric investigation. Am J Orthod. 1979;76:423–442.
34. Poulton, D.R. The influence of extraoral traction. Am J Orthod. 1967;53:8–18.
35. Cetlin, N.M., Ten Hoeve, A. Non-extraction treatment. J Clin Orthod. 1983;17:396–413.
36. Gianelly, A.A., Vaitas, A.S., Thomas, W.M. The use of magnets to move molars distally. Am J Orthod. 1989;96:161–167.
37. Locatelli, R., Bednar, J., Dietz, V.S., et al. Molar distalization with super elastic NiTi Wire. J Clin Orthod. 1992;26:277–279.
38. Carano, A., Tests, M. The distal jet for upper molar distalization. J Clin Orthod. 1996;30:374–380.
39. Jones, R.D., White, J.M. Rapid Class II molar correction with an open coil jig. J Clin Orthod. 1992;26:661–664.
40. Hilgers, J.J. The pendulum appliance for Class II non-compliance therapy. J Clin Orthod. 1992;26:706–714.
41. Kalra, V. The K-loop molar distalizing appliance. J Clin Orthod. 1995;29:298–301.
42. Karad, A. KIDS: a new approach to distalize maxillary molars. World J Orthod. 2008;9:244–254.
43. Fortini, A., Lupoli, M., Pari, M. The first class appliance for rapid molar distalization. J Clin Orthod. 1999;33(6):322–328.
44. Pieringer, M., Droschl, H., Permann, R. Distalization with a Nance appliance and coil springs. J Clin Orthod. 1997;31(5):321–326.
45. Polat-Ozsoya, O., Gokcelikb, A., Güngör-Acarc, A., et al. Soft-tissue profile after distal molar movement with a pendulum. K-loop appliance versus cervical headgear. Angle Orthod. 2008;78(2):317–323.
46. Sayinsu, K., Isik, F., Nur Ülgen, A. A comparative study of profile changes with three different distalization mechanics. World J Orthod. 2007;8(1):65–71.
47. Ricketts, R.M., Bench, R.W., Gugino, C.F., et al. Bioprogressive therapy. Denver, CO: Rockey Mountain Orthodontics, 1979.
48. Kinzinger, G.S.M., Fritz, U.B., Sander, F.G., et al. Efficiency of a pendulum appliance for molar distalization related to second and third molar eruption stage. Am J Orthod Dentofacial Orthop. 2004;125(1):8–23.
49. Gutierrez, V.M.E. Treatment effects of the distal jet appliance with and without edgewise therapy. St Louis: Department of Orthodontics, St. Louis University, 2001.
50. Tanne, K., Sakuda, M., Burstone, C.J. Three dimensional finite element analysis for stress in the periodontal tissue by orthodontic forces. Am J Orthod. 1987;92:499–505.
51. Siatkowski, R. The role of headgear in Class II dental and skeletal corrections. In: Nanda R., Kuhlberg A., eds. Biomechanics in clinical orthodontics. Philadelphia: WB Saunders; 1996:109–142.
52. Proffit, W.R., et al, Contemporary orthodontics,. Mosby: St Louis, 1993.
53. Nanda, R., Kuhlberg, A. Biomechanical basis of extraction space closure. In: Nanda R., Kuhlberg A., eds. Biomechanics in clinical orthodontics. Philadelphia: WB Saunders; 1996:156–187.
54. Wieslander, L. The effect of force on craniofacial development. Am J Orthod. 1974;65:531–538.
55. Baumrind, S., Korn, E.L., Molthen, R., et al. Changes in facial dimensions associated with the use of forces to retract the maxilla. Am J Orthod. 1981;80:17–30.
56. Melanson, E., Van Dyken, C. Studies in condylar growth, master's thesis. Ann Arbor: University of Michigan, 1972.
57. Mills, C.M., Mc Culloch, K.J. Treatment effects of the twin block appliance. Am J Orthod Dentofacial Orthop. 1998;114:15–24.
58. Droel, R., Isaacson, R.J. Some relationship between glenoid fossa position and various skeletal discrepancies. Am J Orthod. 1972;61:64–78.
59. Liselot, B., Melsen, B., Terp, S. A laminographic study of the alterations of the temporomandibular joint following activator treatment. Eur J Orthod. 1984;6:157.
60. Woodside, D.G., Metaxas, A., Altuna, G. The influence of functional appliance therapy on glenoid fossa remodeling. Am J Orthod Dentofacial Orthop. 1987;92:181–198.
61. Woodside, D.G. Do functional appliances have an orthopaedic effect? Am J Orthod Dentofacial Orthop. 1998;113:11–14.
62. Buschang, P.H., Santos-Pinto, A. Condylar growth and glenoid fossa displacement during childhood and adolescence. Am J Orthod Dentofacial Orthop. 1998;113:437–442.
63. Ward, D.M., Behrents, R.G., Goldberg, J.S. Temporomandibular joint fluid pressure response to altered mandibular position. Am J Orthod Dentofacial Orthop. 1990;98:22–28.
64. Graber, T.M. The unique nature of temporomandibular joint metabolism: the clinical implications. In: Rabie A.M., Urist M.R.B., eds. Bone formation and repair. Amsterdam: Elsevier; 1997:143–153.
65. Ikai, A., Sugisaki, M., Young-Sung, K., et al. Morphologic study of the mandibular fossa and the eminence of the temporomandibular joint in relation to facial structures. Am J Orthod Dentofacial Orthop. 1997;112:634–638.
66. Fields, H.W., Proffit, W.R., Nixon, W.L., et al. Facial pattern difference in long-faced children and adults. Am J Orthod. 1984;85:217–223.
67. Joondeph, D.R. Early orthodontic treatment. Am J Orthod. 1993;104:199–200.
68. Dietrich, U.C. Morphological variability of skeletal Class III relationships as revealed by cephalometric analysis. Rep Congr Eur Orthod Soc. 1970:131–143.
69. Aki, T., Nanda, R.S., Currier, G.F., et al. Assessment of symphysis morphology as a predictor of the direction of mandibular growth. Am J Orthod Dentofacial Orthop. 1994;106:60–69.
70. Schulof, R.J., Nakamura, S., Williamson, W.V. Prediction of abnormal growth in Class III malocclusions. Am J Orthod. 1977;71:421–430.
71. Baccetti, T., McGill, J.S., Franchi, L., et al. Skeletal effects of early treatment of Class III malocclusion with maxillary expansion and face-mask therapy. Am J Orthod Dentofacial Orthop. 1998;113:333–343.
72. Merwin, D., Ngan, P., Hagg, U., et al. Timing of effective application of anteriorly directed orthopaedic force to the maxilla. Am J Orthod Dentofacial Orthop. 1997;112:292–299.
73. Kapust, A.J., Sinclair, P.M., Turley, P.K. Cephalometric effects of face mask/expansion therapy in Class III children: a comparison of three age groups. Am J Orthod Dentofacial Orthop. 1998;113:204–212.
74. Baik, H.S. Clinical results of the maxillary protraction in Korean children. Am J Orthod Dentofacial Orthop. 1995;108:583–592.
75. Haas, A.J. The treatment of maxillary deficiency by opening the midpalatal suture. Angle Orthod. 1965;35:200–217.
76. Üner, O., Yüksel, S., Üçüncü, N. Long-term evaluation after chin cup treatment. Eur J Orthod. 1995;17:135–141.
77. Deguchi, T., Kitsugi, A. Stability of changes associated with chin cup treatment. Angle Orthod. 1996;66:139–146.