Regional Circulation
Introduction
After discussing the ‘dynamics of circulation’ and ‘cardiovascular regulation mechanisms’, it will be worthwhile to know how these basic principles apply to circulation in various regions of the body. This chapter includes:
Circulation to other regions, such as pulmonary circulation and renal circulation, have been described in the concerned sections.
Coronary circulation
Coronary blood vessels
Coronary arteries
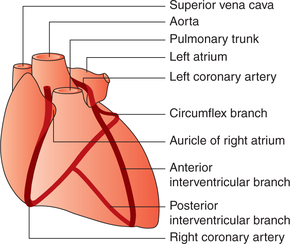
Two coronary arteries (right and left) arise from the root of ascending aorta and supply blood to the myocardium (Fig. 4.6-1).
Right coronary artery supplies blood to the right ventricle, the right atrium, the posterior part of left ventricle, the posterior part of interventricular septum and major portion of the conducting system of heart including SA node.
Left coronary artery supplies blood mainly to the anterior part of left ventricle, left atrium, anterior part of the interventricular septum and a part of the left branch of bundle of His.
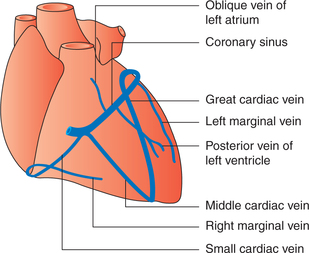
Coronary veins
Coronary sinus is a wide vein about 2-cm long, which drains most of the venous blood from the myocardium (mainly left ventricle) into the right atrium. Its tributaries are the great cardiac vein, the small cardiac vein, the posterior vein of left ventricle and the oblique vein of left ventricle (Fig. 4.6-2).
Anterior cardiac vein draining venous blood mainly from the right ventricle opens directly into the right atrium.
Thebesian veins and coronary luminal vessels (connections between the coronary vessels and the lumen of heart) constitute the deep venous system. These vessels drain only less than 10% of the venous blood from the myocardium directly into the various cardiac chambers, contributing to an anatomic shunt effect. The coronary luminal connections carry a larger proportion of the flow in the right ventricle than in the left ventricle.
Coronary blood flow: characteristic features
Normal coronary blood flow and oxygen demand
A continuous flow of blood to the heart is essential to maintain an adequate supply of O2 and nutrients.
Normal coronary blood flow at rest is about 250 mL (70 mL/100 g tissue/min), i.e. about 5% of the resting cardiac output (5 L). Threefold to sixfold increase in the coronary blood flow may occur during exercise.
Oxygen consumption by the myocardium is very high (8 mL/min/100 g at rest). Because of this, even at rest 70–80% of the oxygen is extracted from each unit of the coronary blood as compared to the whole-body (average of 25%) oxygen extraction at rest. The increased oxygen demand of the myocardium during exercise is met with by almost total (nearly 100%) extraction of oxygen and by manifold increase in the coronary blood flow.
Phasic changes in coronary blood flow
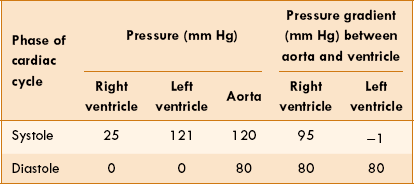
The coronary blood flow shows changes during phases of the cardiac cycle. The blood flow is determined by the balance between pressure head (i.e. aortic pressure) and the resistance (i.e. extravascular pressure exerted by the myocardium on the coronary vessels) offered to the blood flow during various phases of cardiac cycle is shown in Table 4.6-1 and Fig. 4.6-3, and is described here.
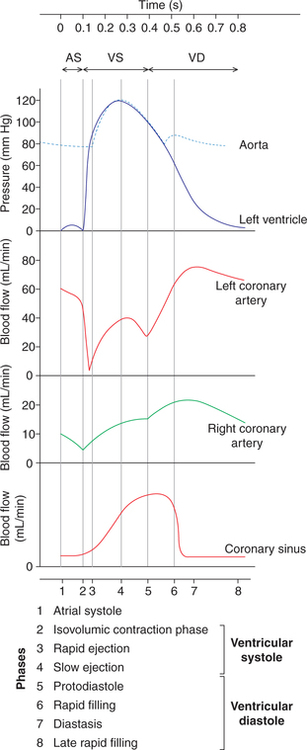
Fig. 4.6-3 Blood flow in right and left coronary arteries and coronary sinus during different phases of cardiac cycle.
During systole the tension developed in the left ventricle is so high that it has throttling effect on the branches of the coronary arteries penetrating through them. As a result, the average blood flow through the capillaries of left ventricles falls to the extent that during isometric contraction phase the blood flow to the left ventricle practically ceases, i.e. becomes zero.
During diastole the cardiac muscles relax and blood flow increases. Thus, most of the coronary blood flow (over 70%) occurs during diastole (Fig. 4.6-3). In severe tachycardia the duration of diastole is drastically reduced. This tends to reduce the coronary blood flow during diastole as well, but due to local metabolic regulation the blood flow to the myocardium is not seriously affected.
Blood flow to right ventricle and atria
Blood passing through coronary capillaries of right ventricle also shows phasic changes similar to the left ventricle. However, the changes in the right ventricular flow are far less because force of contraction of the right ventricle is much less (Table 4.6-1). Thus, the blood flow to the right ventricle and atria occurs both during systole and diastole.
Blood flow through coronary sinus
As shown in Fig. 4.6-3, in the coronary sinus the inflow of blood gradually rises from the isovolumic ventricular contraction phase, reaches its peak during protodiastole phase and then gradually falls.
Regulation of coronary blood flow
I Local control mechanism
1. Autoregulation. Like other vital organs of the body coronary circulation shows well-developed phenomenon of autoregulation, as described in detail on page 167. However, this phenomenon of autoregulation of coronary blood flow fails when blood pressure falls below 70 mm Hg and coronary perfusion is seriously compromised.
2. Role of local metabolites. Metabolic local factors are the most important factors which regulate the coronary blood flow.
• It is important to note that under resting state about 50%–70% of O2 is released to the myocardium from the haemoglobin of arterial blood (in contrast, haemoglobin releases about 25% of its O2 content for the body as a whole). Therefore, not much additional oxygen can be provided to myocardium unless the blood flow increases. The O2 consumption regulates the coronary blood flow probably by the following mechanisms.
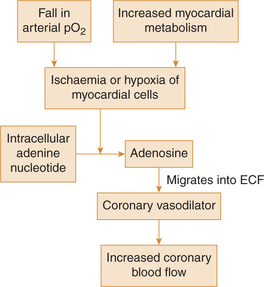
• Role of adenosine (Berne's hypothesis). Adenosine is considered the major factor in production of coronary vasodilation during hypoxic states (Fig. 4.6-4).
• Direct effect of O2 lack. It has been proposed that a decrease in the tissue PO2 could also act directly on the arterioles and cause vasodilation.
• Role of other local metabolites. Hydrogen ions, bradykinin, CO2 and prostaglandins are the other suggested vasodilator substances.
II Nervous control mechanism
Nervous control on coronary circulation is exerted through sympathetic and parasympathetic nerve supply to the coronary vessels.
Sympathetic nerve fibres extensively innervate the coronary vessels. The transmitters released at their nerve endings are epinephrine and norepinephrine. The coronary vessels contain both α- and β-receptors.
Sympathetic stimulation causes increase in the heart rate and increase of force of contraction of the heart. Thus, an increased activity of heart helps conversion of ATP to ADP, which by producing coronary vasodilation increases the coronary blood flow.
Parasympathetic stimulation causes decreased heart rate and decreased force of contraction of heart. Thus, the coronary blood flow is reduced.
Coronary artery disease
Coronary artery disease (CAD) also known as ischaemic heart disease (IHD) results due to the insufficient coronary blood flow.
Since atheromatous coronary artery stenosis is the commonest cause, so it has become synonymous with CAD.
Cerebral circulation
Cerebral blood vessels
Arteries of the brain
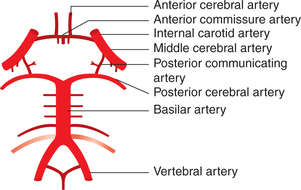
• The arteries which supply blood to the brain are derived from two internal carotid arteries and the basilar artery (formed by union of the right and left vertebral arteries). Branches of the internal carotid arteries and basilar artery anastomose on the inferior surface of the brain to form the circulus arteriosus (circle of Willis).
• The circle of Willis (Fig. 4.6-5) is thus basically a free anastomoses between the two internal carotid arteries and the two vertebral arteries which equalize pressure on the arteries of the two sides. In this way the circulus arteriosus allows blood that enters by either internal carotid or vertebral artery to be distributed to any part of both cerebral hemispheres.
• Six large arteries taking part in the formation of circle of Willis supply by their central and cortical branches to the brain substance.
Venous drainage of the brain
The cerebral hemisphere has two sets of veins: the superficial and deep. The veins draining the brain open into the various dural venous sinuses. Ultimately, the blood from all these sinuses reaches the sigmoid sinuses, which become continuous with the two internal jugular veins. The venous drainage of individual part of the brain is as follows.
Cerebral blood flow: characteristic features
Normal blood flow
• Brain relies on a continuous blood flow for adequate function. It is most susceptible to ischaemia. Interruption of blood flow only for 5–10 s causes a loss of consciousness and circulatory arrest for only 3–4 min results in irreversible brain damage. The vegetative structures in brainstem are more resistant to hypoxia than cerebral cortex.
• Brain has a very rich blood supply. Normal blood flow to brain (which forms less than 2% of the body weight) represents approximately 15% of the resting cardiac output (75 mL/min) or about 50–55 mL blood/100 g tissue/min.
• When cerebral blood flow falls below 18 mL/100 g tissue/ min (critical flow level), there occurs unconsciousness.
Regulation of cerebral blood flow
The cerebral blood flow is regulated by following mechanisms.
1 Metabolic regulation
The important metabolic factors which play important role are given below.
(i) Carbon dioxide. Physiologically, pCO2 is the most potent vasodilator of cerebral blood vessels. A rise in pCO2 is associated with a rise in H+ concentration. Carbon dioxide easily diffuses through the blood–brain barrier and reaches the cerebrospinal fluid (CSF). In the CSF, CO2 combines with water to form carbonic acid, which partially dissociates to form H+ ions. The H+ ions induce cerebral vasodilation in proportion to their concentration.
(ii) pO2. Slight fall in pO2 causes vasodilation and produces increase in cerebral blood flow due to rapid formation of adenosine, which is potent dilator of pial arterioles.
(iii) K+ ions. An increase in K+ concentration in the CSF following hypoxia causes rapid increase in cerebral blood flow.
2 Autoregulation of cerebral blood flow
Like other vital organs of the body cerebral circulation also shows phenomenon of autoregulation. Due to autoregulation cerebral blood flow remains nearly constant between 60 and 140 mm Hg blood pressure; when blood pressure falls below 60 mm Hg, the cerebral blood flow becomes extremely compromised and syncope may result. When blood pressure rises above 140 mm Hg, there may occur disruption of blood–brain barrier due to stretching and cerebral oedema or cerebral haemorrhage may result.
3 Role of intracranial pressure in regulation of cerebral blood flow
The intracranial pressure level regulates cerebral blood flow by the following two mechanisms.
(i) Monro–Kellie doctrine. According to this doctrine the brain, CSF and blood in the cerebral vessels are three elements enclosed in a rigid cranial cavity; and when any of them increases, it is at the expense of other two. This relationship helps to maintain the cerebral blood flow when changes in the arterial blood pressure occur at the level of head.
(ii) Cushing reflex. When intracranial pressure is increased and becomes equal to the arterial pressure, it compresses the arteries in the brain and blood supply to vasomotor area is compromised. The hypoxia and hypercapnia produced locally increases the discharge from vasomotor centre. The resultant rise in a systemic pressure tends to restore the cerebral blood flow (see page 187).
Cutaneous circulation
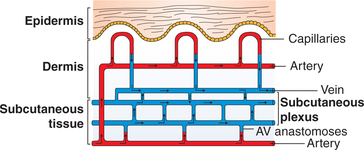
Cutaneous blood vessels (Fig. 4.6-6)
Cutaneous arterioles form a dense network just under the dermis layer of the skin.
• Meta-arterioles which arise from the arterioles are relatively high-resistance conduits present between the arterioles and capillaries.
• Cutaneous capillaries. The meta-arterioles subdivide into capillary loops, which provide a large surface area for heat exchange.
• Venules form an extensive subpapillary venous plexus, which holds large quantity of blood and lie parallel to the surface of skin, and play an important role in maintaining the body temperature.
• Arteriovenous anastomoses are located in the distal parts of the extremities (hands and feet), nose, lips and ear lobules. These vessels serve as shunts and allow blood to bypass the superficial capillary loops and play a major role during control of body temperature.
Cutaneous blood flow: characteristic features
Main function of cutaneous circulation is to aid in the regulation of body temperature.
Resting cutaneous blood flow, i.e. the flow when a person is at thermal equilibrium with the environment (at approximately 27°C atmospheric temperature) is about 10–15 mL/min/ 100 g of skin tissue.
During exposure to cold, when sweating is minimal, the cutaneous blood flow falls to about one-tenth of resting blood flow, i.e. about 1 mL/min/100 g tissue.
During exposure to heat, when sweating is maximum, the cutaneous blood flow may increase 10 times of resting blood flow, i.e. about 150 mL/min/100 g tissue.
Regulation of cutaneous blood flow
The cutaneous blood flow is predominantly regulated by the nervous control instead of metabolic control.
Nerve supply of cutaneous vessels
Sympathetic vasoconstrictor nerves supplying the cutaneous vessels exhibit a sympathetic constrictor discharge under resting condition. The sympathetic tonic discharge is more marked on A–V anastomoses vessels than the other vessels.
Parasympathetic vasodilator nerves do not supply the cutaneous blood vessels. Vasodilation of cutaneous vessels results due to:
Neural control mechanisms
The cutaneous blood flow is regulated by the following neural control mechanisms.
1 Hypothalamic control mechanism
The reflex increase or decrease in the sympathetic discharge to cutaneous vessels during thermoregulation is mediated through the temperature regulation centres of the hypothalamus as:
Under resting conditions, i.e. when the person is at thermal equilibrium with the environment (at about 27°C atmospheric temperature), the sympathetic vasoconstrictor fibres have a mild tonic discharge. The tonic sympathetic discharge normally keeps the A–V anastomoses closed.
During exposure to heat stress, the tonic sympathetic discharge is reflexly abolished by a hypothalamic mechanism. Thus the blood flow to skin is increased by following responses in a chronological sequence:
• First of all, A–V anastomoses of hands, feet and ear lobules dilate due to reduction in the sympathetic tonic discharge.
• Secondly, rest of the cutaneous vessels dilate due to progressive withdrawal of sympathetic vasoconstrictor activity.
• Thirdly, sweat glands get activated due to the cholinergic sympathetic discharge. The bradykinin produced by the secretory activity of the sweat glands acts locally as a powerful vasodilator and increases blood flow to skin.
All the above mechanisms collectively may increase the cutaneous blood flow to as high as 150 mL/min/100 g tissue. The increased blood flow carries heat to the surface of the body, where it is dissipated by radiation, evaporation and conduction to the environment.
During exposure to cold stress, via hypothalamic mechanism, there occurs widespread cutaneous vasoconstriction due to increased sympathetic discharge. Consequently, cutaneous blood flow is markedly decreased to as low as 1 mL/ min/100 g. In this way heat conservation is accomplished by markedly diminishing the rate of blood flow to skin.
2 Baroreceptor-mediated reflex
Cutaneous blood vessels participate in the baroreceptormediated reflexes during conditions of circulatory stress, such as exercise and haemorrhage.
The emotions affect the cutaneous circulation through the corticohypothalamic pathway. The effects of emotions on cutaneous circulation manifest in following forms:
Blanching of skin during situations of fear (pale with fear) occurs due to vasoconstriction mediated through cortical mechanism.
Phenomenon of blushing, i.e. emotional embarrassment occurs due to vasodilation of vessels.
Cutaneous vascular responses
Certain peculiar cutaneous vascular responses are:
White reaction
White reaction refers to an appearance of a pale stroke line when a pointed object is drawn lightly over the skin. This occurs due to the fact that the mechanical stimulus initiates contraction of the precapillary sphincter and blood drains out of the capillaries and small veins. This response appears in about 15 s.
Triple response
Triple response is a three-part response consisting of the red reaction, wheal and flare; when the skin is stroked more firmly with a pointed instrument, instead of white reaction, there occurs triple response.
The red reaction refers to the red line which appears at the site of injury in about 10 s. It occurs due to dilatation of the precapillary sphincters in the injured area. The dilatation of the precapillary sphincters is produced by histamine and/or some polypeptides such as bradykinin released from the damaged skin.
The flare refers to the diffusely spreading and irregularly outlined redness of the skin surrounding the red line.
• It occurs after a few minutes of the appearance of red line.
• It occurs due to the dilatation of the arteriole and precapillary sphincters.
• The dilatation of arteriole is mediated by nerves, since it is abolished by the local anaesthetic agents.
• The flare is mediated by the axon reflex in the cutaneous fibres, which does not involve the central nervous system like a typical reflex.
Wheal refers to the swelling or localized oedema that develops within the area of flare.
• It occurs due to increased capillary permeability with consequent extravasation of fluid.
• The increase in capillary permeability responsible for the wheal formation is produced by histamine or histaminelike substance (released from local mast cells) and by P substance (the transmitter released at the central termination of the sensory fibre neurons).
Reactive hyperaemia
Reactive hyperaemia is a phenomenon by which the vessels control blood flow to the organ after a period of ischaemia following occlusion of the artery to an organ or tissue. This response of the blood vessels occurs in many organs but is visible in the skin as fiery red skin.
Cold vasodilatation
As discussed above, normally during exposure to cold stress, there occurs widespread cutaneous vasoconstriction via hypothalamic mechanism. However, prolonged and severe vasoconstriction may lead to tissue damage known as frostbite. This usually occurs when skin temperature falls below 10°C. The tissue injury so produced is painful and associated with release of histamine and/or some other polypeptide, which excites the sensory terminals and produces vasodilatation due to axon reflex operating particularly on A–V anastomoses. Cold vasodilatation is the cause of ruddy cheeks seen in fair complexioned individuals on a cold day.
Skeletal muscle circulation
Skeletal muscle blood flow: characteristic features
At rest the blood flow to the skeletal muscle is about 2–4 mL/min/100 g of the muscle tissue.
• Since the whole body skeletal muscles weight is approximately 30 kg in adults, so the total blood flow to the body muscle mass is about 750–800 mL/min.
• At rest only 20%–25% of muscle capillaries have flowing blood.
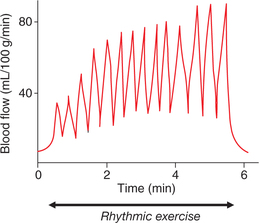
During exercise. During strenuous exercise muscle blood flow can increase up to 20 times, i.e. about 50–80 mL/ min/100 g muscle tissue or over 20 L/min to the whole body skeletal mass. This is called exercise hyperaemia.
• The tremendous increase in the muscle blood flow mainly occurs due to local metabolite-induced vasodilatation.
• During exercise the blood flow to the muscle is intermittent because during each contraction muscle fibres squeeze the blood vessels passing through them and thus the blood flow decreases or even stops (Fig. 4.6-7). During relaxation period, muscle blood flow increases and myoglobin acts as an O2 acceptor and it yields its O2 to the myofibrils during the subsequent muscle contraction.
• Sustained and severe contractions lasting more than 10 s lead to cessation of blood flow, myoglobin supply of O2 is exhausted and anaerobic metabolites accumulate causing fatigue and ischaemic pain.
• Following heavy phasic exercise the blood flow does not subside immediately, but falls exponentially from its high level during the exercise to resting values. This is due to the oxygen debt of exercise.
Regulation of muscle blood flow
The blood flow to the skeletal muscles is regulated by an autoregulation mechanism, metabolic control mechanism and nervous control mechanism.
1 Autoregulation mechanism
Mechanism of autoregulation is well developed in the skeletal muscles like that of kidney, heart and brain.
2 Metabolic control mechanism
Local metabolic control mechanism is chiefly responsible for the tremendous increase in the skeletal muscle blood flow during exercise (exercise hyperaemia). The decreased tissue pO2 leads on to vasodilatation. In addition, the exercising skeletal muscle levels of adenosine, potassium ions, hydrogen ions, lactic acid and carbon dioxide. Further, rise of tissue temperature due to muscular activity may also contribute to the dilatation of arterioles and precapillary sphincter. As a result there is 10–100-fold increase in the number of open capillaries in the skeletal muscles.
3 Nervous control mechanisms
Vessels of the skeletal muscles are supplied by both sympathetic vasoconstrictor and sympathetic vasodilator fibres.
Sympathetic vasoconstrictor control
During circulatory shock and other type of circulatory stress the sympathetic vasoconstrictor mechanism assumes a great physiological importance. Sympathetic vasoconstriction reduces muscle blood flow profoundly. Thus help in diverting substantial amount of blood from the muscles towards the heart and other vital organs.
Sympathetic vasodilator fibres
• Skeletal blood vessels are also supplied by the sympathetic vasodilator fibres which have acetylcholine as neurotransmitter.
• These fibres are activated by corticohypothalamic reticulospinal pathways (see page 181).
• Sympathetic vasodilator fibres play no significant role in increasing the muscle blood flow either during or before exercise.
• These fibres play an important role in preventing the sudden rise in the systemic blood pressure at the beginning of exercise, i.e. these provide a safety valve mechanism as just before the start of exercise there occurs a considerable increase in the sympathetic activity.