Sexual Growth and Development
Pre-pubertal sexual growth and development
In human embryo sexual growth involves two processes:
Sex determination
Sex determination, also known as genetic differentiation, refers to the genotype of the fetus, whether male or female. The genotype is determined by the presence of sex chromosomes, hence is also known as chromosomal sex differentiation.
Human chromosomes. Each cell (except ovum and sperm) in a normal adult male and female possesses 46 chromosomes (44 autosomes + 2 sex chromosomes) usually arranged in an arbitrary pattern (karyotype).
• Sex chromosomes are called X and Y chromosomes.
• The females possess 44 autosomes plus 2X chromosomes (44 + X).
• The males possess 44 autosomes plus an X chromosome and a Y chromosome (44 + XY).
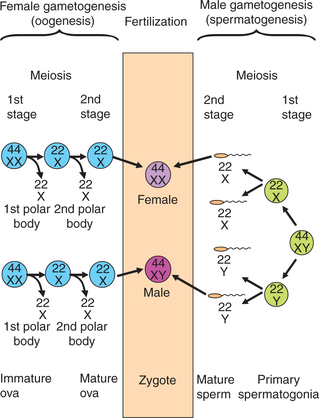
Human gametes. The mature male gametes are called sperms and mature female gametes are called ova. During gametogenesis there occurs meiosis (reduction division); therefore the mature sperm and ovum contain half the number of chromosomes, i.e. 23 (22 autosomes + one sex chromosome). This is called haploid number.
• Since, the primitive female germ cells (oogonia) from which mature ova are formed contain 44 + X chromosomes, so each ovum will contain 22 + X chromosomes (Fig. 9.1-1).
• The primitive male germ cells (spermatogonia) from which mature sperms are formed contain 44 + XY chromosomes, so half of the normal sperms will contain 22 + X and other half will have 22 + Y chromosomes (Fig. 9.1-1).
Genetic sex determination of the embryo occurs during fertilization, i.e. penetration of the ovum by the sperm as:
• When an ovum (22 + X) is fertilized by a sperm containing 22 + X chromosomes, the resultant zygote’s chromosomal pattern will be 44 + X + female genotype).
• When an ovum (22 + X) is fertilized by a sperm containing 22 + Y chromosomes, the resultant zygote’s chromosomal pattern will be 44 + XY (male genotype).
Sex differentiation
After fertilization, the normal sex differentiation in the embryo proceeds sequentially. The stages of sex differentiation are:
Gonadal differentiation
Gonadal differentiation or gonadogenesis refers to the formation of gonads, i.e. testes in males and ovaries in females. Gonadal sex differentiation is dependent on the genotype of the embryo.
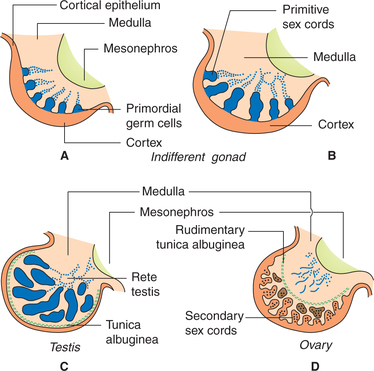
Genital ridge or the urogenital ridge (the condensation of mesenchymal tissue present on each side near the adrenal glands) is the site where gonads develop.
Bipotential gonads. Bipotential gonads are also known as primordial or primitive or indifferent or ambisexual gonads. Up to 6 weeks of gestation the bipotential gonads are identical in both sexes, and have the rudiments of both male and female gonads.
Testicular differentiation
In genetic male (44 + XY) embryo, the bipotential gonads begin to differentiate into testes at approximately sixth week. The Y chromosome plays key role in the process of testicular differentiation.
Role of Y chromosome in testicular differentiation
• Two transcription genes, one for testicular differentiation and another for the formation of Mullerian duct inhibitory substance (MIS), are present on the Y chromosome.
• The gene responsible for testicular differentiation is called SRY gene (SRY=sex-determining region of the Y chromosome).
• The SRY gene encodes the testis-determining factor (TDF), which triggers the testicular differentiation.
• The TDF gene product causes Sertoli cell differentiation, which is critically important for all events in male sexual differentiation.
Ovarian differentiation
• In genetic female (44 + X) embryo, by about 10th week of gestation, ovarian differentiation occurs in the absence of TDF.
• The ovaries develop on each side from the cortical region of the bipotential gonad (Fig. 9.1-2C).
Genital differentiation
Genital sex differentiation, also known as phenotypic sex differentiation, refers to the differentiation of internal and external genitalia.
Differentiation of internal genitalia
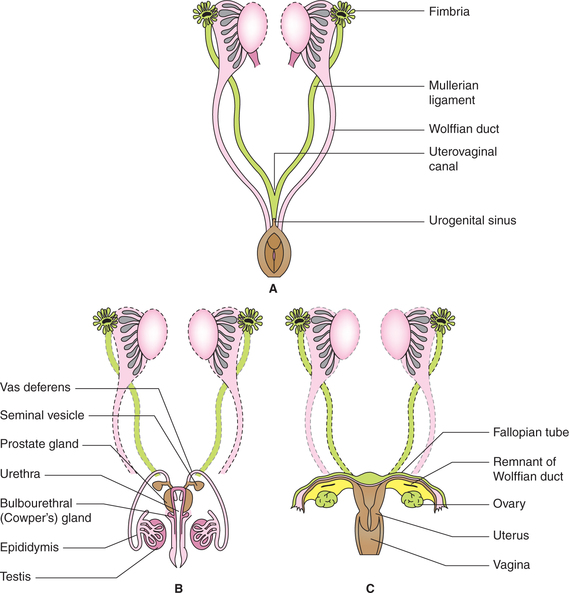
• The internal genitalia differentiate from the neutral sex anlagen, which develops during sixth week of gestation along with the development of bipotential gonad.
• The primordia of internal genitalia are a paired set of Wolffian (male) ducts and a paired set of Mullerian (female) ducts. By seventh week of gestation, the embryo has both male and female primordial ducts (Fig. 9.1-3).
Differentiation of male internal genitalia. In the genetic male fetus (44 + XY) with functioning testes (Fig. 9.1-3B):
• The testosterone secreted by the Leydig cells stimulate the Wolffian ducts to form the epididymis, vas deferens and seminal vesicles.
• The Mullerian inhibiting substance (MIS) causes regression of the Mullerian ducts by apoptosis.
Differentiation of female internal genitalia (Fig. 9.1-3C)
Differentiation of external genitalia
The external genitalia in both sexes develop from common anlagen, which are the urogenital sinus, the genital sinus, the genital tubercle, the genital swelling and the genital (urethral) folds (Fig. 9.1-4).
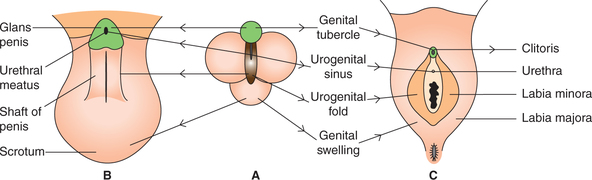
Fig. 9.1-4 Differentiation of external genitalia in male (B) and female (C) from common anlagen (A).
The external genitalia derived from the common anlagen in male and female are shown in Table 9.1-1.
Table 9.1-1
The male and female external genitalia derived from the common anlagen
| Anlagen part | Male derivative | Female derivative |
| Urogenital sinus | Prostate and prostatic urethra | Urethra |
| Urethral fold | Penile urethra and shaft of penis | Labia minora |
| Genital swelling | Scrotum | Labia majora |
| Genital tubercle | Glans penis | Clitoris |
Disorders of sexual development
Abnormalities of sexual development occur due to:
• Defect in sex chromosomes leading to genetic abnormalities.
• Hormonal abnormalities leading to defect in gonadal and genital differentiation.
Chromosomal abnormalities
Chromosomal abnormalities include trisomy and monosomy.
1. Trisomy
Chromosomal abnormalities usually arise during gametogenesis due to non-disjunction of sex chromosomes (Fig. 9.1-5). The presence of extra X or Y chromosome (trisomy) (Fig. 9.1-6) gives rise to many syndromes associated with abnormal development, mental retardation and abnormal growth. Trisomy is presented as follows.
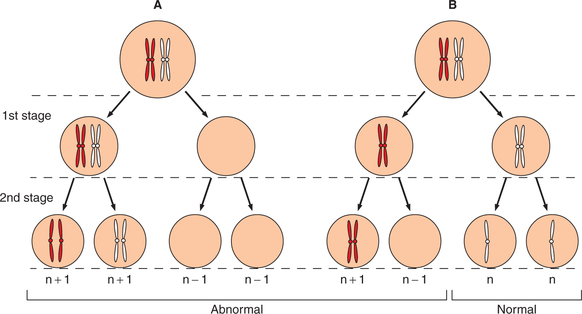
Fig. 9.1-5 Non-disjunction of sex chromosomes during meiotic division; A, in Ist stage and B, in 2nd stage.
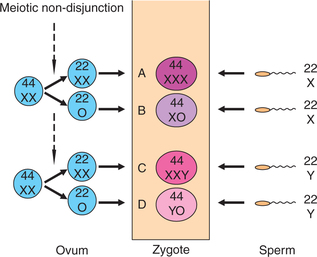
Fig. 9.1-6 Defects due to maternal non-disjunction of sex chromosomes at the time of meiosis: A, superfemale; B, gonadal dysgenesis (Turner’s syndrome); C, seminiferous dysgenesis (Klinefelter’s syndrome) and D, lethal monosomy.
(a) Individual with XXY pattern of chromosomes (Klinefelter’s syndrome) is an abnormal male due to presence of Y chromosome. It is the most common sex chromosome disorder and has an incidence of 1 in 500 males.
Characteristic features in a person with Klinefelter’s syndrome are:
(b) Individual with XXX (genotype) pattern of chromosomes is referred to as ‘superfemale’. However, there is nothing super about them, because there is poor sexual development (infantile), scanty menstruation and mental retardation.
2. Monosomy
As shown in Fig. 9.1-5, when both chromosomes of a pair go to one gamete the other gamete resulting from such a division has only 22 chromosomes; and at fertilization the zygote formed will have only 45 chromosomes. Hence one pair is represented by single chromosome, so it is called monosomy. Depending upon the presence of X or Y chromosome, there will be either female phenotype (44 + XO) or male phenotype (44 + YO). The best known example of monosomy disorder is Turner’s syndrome.
Turner’s syndrome. Characteristic features of Turner’s syndrome are:
Hormonal abnormalities
The most common developmental disorder due to hormonal abnormalities is pseudohermaphroditism.
Pseudohermaphroditism
Pseudohermaphroditism means individual having genotype (gonads) of one sex (either testes or ovaries) and genitalia of other sex. It occurs in two forms:
True hermaphroditism
It is a very rare condition in which gonads of both sexes are present (an ovary on one side and testis on other side), thus resulting in numerous variations in phenotypic (internal and external genitalia) differentiation (Fig. 9.1-7).
Puberty and adolescence
Introduction
Puberty and adolescence are the phases of growth between childhood and adulthood.
• Puberty refers to the stage of gonadal development and maturation to the point where reproduction is possible for the first time.
• Adolescence refers to the period of sudden spurt of physical growth between childhood and adulthood.
Since these two phases (adolescence and puberty) of growth are overlapping, hence the terms are interchangeable. The total period of growth spurt ranges between 3 and 5 years. It starts from the age of 8 years. The average age of onset of puberty is 12 years in girls and 14 years in boys.
Components of puberty
The two principal components of puberty are: sudden spurt of physical growth and appearance of secondary sex characters.
1. Sudden spurt of physical growth
During sudden spurt of physical growth there is increase in height, muscle mass and muscle strength of an individual. The height increases by 7-12 cm in boys and about 6-11 cm in girls.
The muscle mass and muscle strength also increases in both the sexes but the increase is far greater in boys as compared to in girls.
2. Appearance of secondary sex characters
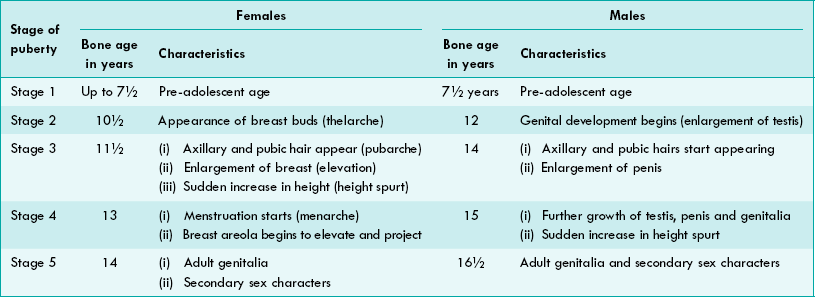
Stages of development of secondary sex characters. The sequence of events of puberty, which occurs in 3-5 years period, have been discussed in five stages (Table 9.1-2).
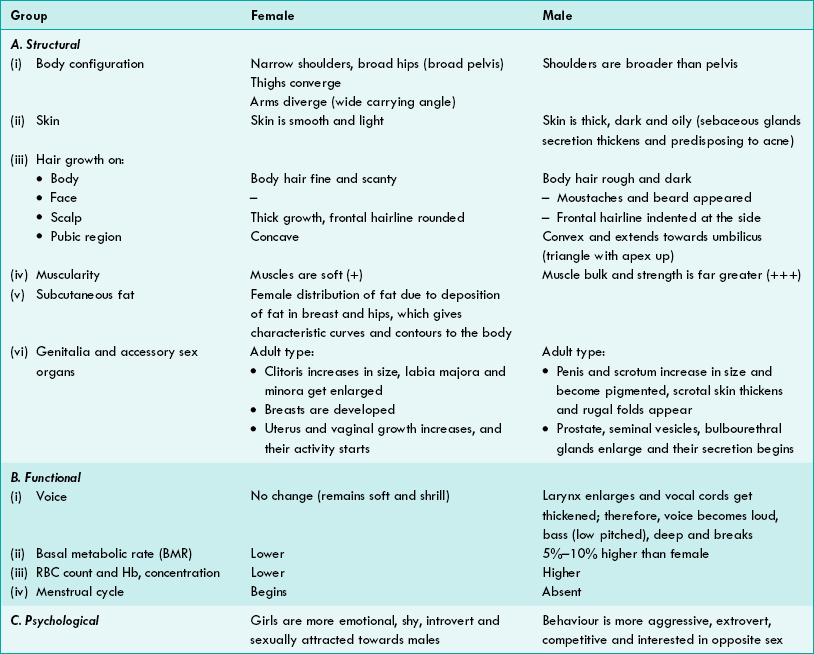
Types of secondary sex characters. The secondary sex characters are almost fully developed by the stage 5 of the puberty both in male and females. These can be grouped as (Table 9.1-3):
Hormonal changes during puberty
Besides ovaries and testes, other endocrinal glands (adrenal, thyroid and anterior pituitary), also grow in size and their activity increases at the onset of puberty. The hormonal changes noticed at the time of puberty are discussed below.
1. Gonadotropins. In both sexes the levels of gonadotropins- follicle stimulating hormone (FSH) and luteinizing hormone (LH)-secreted from the anterior pituitary gland rise slowly from birth of the child up to pre-adolescent age, but at the time of puberty (early teen age) their levels suddenly increase. In pre-pubertal stage the gonadotropin secretion is not under the check of gonadal hormones (oestrogen and testosterone).
2. Adrenal androgens. There is increase in the secretion of adrenal androgens at puberty. The onset of this stage of increase or activation is called adrenarche.
Functions subserved by adrenal androgens at puberty are:
3. Growth hormone. Normally from birth up to pre-pubertal stage, the growth hormone secretion is intermittent (a few peaks every 24 h) but at the time of puberty, though basal level of growth hormone does not rise but there is an increase in the frequency and amplitude of the peaks. It is responsible for generalized growth spurt at adolescence (see page 373).
4. Thyroid gland secretions (thyroxine) also increase during puberty. Thyroxine is necessary for normal growth and development (see page 382).
5. Gonadal hormones (sex hormones). There is slow increase in secretion of sex hormones in children between the age of 7 and 10 years. But, there is a rapid rise in oestrogen secretion (in girls) and testosterone in boys in early teenage.
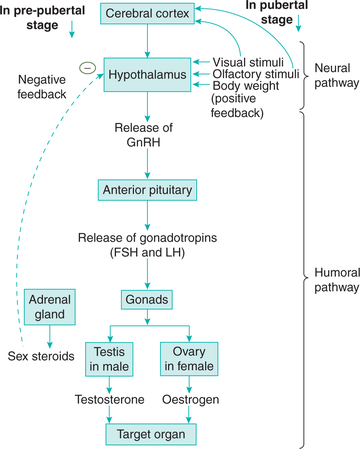
Control of onset of puberty
The exact mechanism of onset of puberty is still not fully understood, but experimental and clinical observations support that the hypothalamus is intimately involved in this process, being a nodal point between nervous and hormonal circuits. The plausible mechanism involved is as follows (Fig. 9.1-8).
• From birth to pre-adolescent age. Gonadotropin-releasing hormone (GnRH) secretion from the hypothalamus is highly sensitive to feedback inhibition by circulating sex hormones (source being adrenal cortex and pre-pubertal testes). Therefore, there is very less or slow release of gonadotropins (FSH and LH) from the anterior pituitary.
• At the time of puberty (12-14 years), hypothalamic cells become more mature and their sensitivity for circulating sex hormones (for negative feedback) decreases.
• As a result, there occurs an increase in secretion of pituitary gonadotropins (FSH and LH). They act on gonads to release gonadal sex hormones.
• Awakening of hypothalamus. Hypothalamus at puberty is also positively stimulated (awakening of hypothalamus) by the critical body mass, visual, external, olfactory and other sensory stimuli.
• Role of leptin. Leptin (a Greek word meaning thin) is a circulating protein formed in the fat cells. It acts on the hypothalamus by feedback control mechanism. Therefore, leptin acts as a link between critical body weight and onset of puberty.
Disorders of puberty
Disorders of puberty are related to the time of its onset, e.g.
1. Precocious puberty
Precocious puberty refers to the onset of puberty in a child before 8 years of age. It is more commonly seen in girls. There is early development of secondary sex characters and gametogenesis also starts earlier (Fig. 9.1-9).
2. Delayed or absent puberty
Puberty is considered to be pathologically delayed in case of female, if menarche does not occur by 17 years of age, or in case of male, testicular development and maturation fails to occur by the age of 20 years.
Delayed puberty is more commonly observed in boys than in the girls. Delayed or absent puberty is a matter of great concern when it occurs in following conditions:
 Sex determination
Sex determination Spurt of physical growth
Spurt of physical growth