Female Reproductive Physiology
An overview of female reproductive system
The female reproductive system comprises internal and external genitalia, which can be organized as (Fig. 9.3-1).
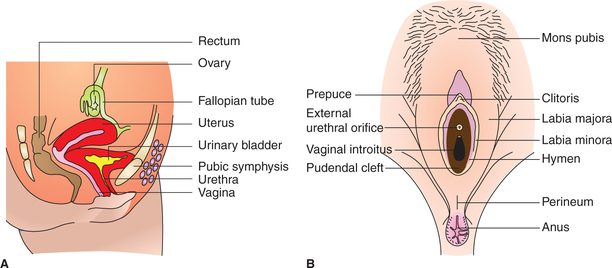
Fig. 9.3-1 Female reproductive organs: A, lateral view showing position of internal reproductive organs in relation to pelvic viscera and B, female external genitalia.
Female internal genitalia
The internal genital organs include uterus, fallopian tubes and vagina.
I Uterus
Uterus is a hollow, thick-walled muscular organ, situated between the urinary bladder and the rectum. It can be divided into two parts (Fig. 9.3-2).
1. Body of the uterus. It forms the upper two-third part of the uterus. Its lower limit is marked by a constriction which corresponds to narrowing of uterine cavity at internal os. Body of the uterus can be divided into two parts:
Fundus is the rounded part of the body that lies superior to the opening of the fallopian tubes.
Isthmus is the relatively constricted region of the body (approximately 1-cm long) just above the cervix.
2. Cervix of the uterus. It is the cylindrical lower part which protrudes into the uppermost part of vagina. It is approximately 2.5-cm long in an adult non-pregnant woman. Its cavity extends from the internal os to external os, which opens into the vagina.
The wall of body of uterus consists of three layers.
1. Perimetrium is the external serosal layer.
2. Myometrium is the middle muscular layer comprising bundles of smooth muscles amongst which there is connective tissue.
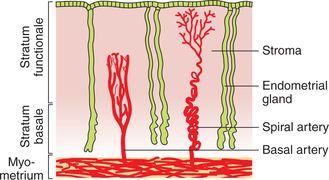
3. Endometrium is inner layer of uterus which consists of epithelial lining and the stroma (Fig. 9.3-3):
• Epithelial lining is made up of columnar cells. Before menarche (i.e. the age-of-onset of menstruation) the cells are ciliated, but thereafter most of the cells may not have cilia.
• Stroma of the endometrium is highly cellular and contains numerous blood vessels and simple tubular uterine glands, which are lined by the columnar epithelium.
Functional divisions of endometrium. Functionally, the endometrium of body of uterus can be divided into two strata.
1. Stratum functionale includes the superficial two-third thickness of endometrium, which undergoes monthly cyclic changes in preparation for the implantation of fertilized ovum and is shed during menstruation. This portion of endometrium is supplied by long and spiral (coiled) arteries.
2. Stratum basale is the deeper one-third layer of endometrium. It does not participate in the cyclic changes but functions as a regenerative layer. This part of endometrium is supplied by short and straight basal arteries.
Structure of cervix of the uterus is somewhat different from that of the body.
1. Perimetrium is the outermost serous layer.
2. Myometrium layer of the cervix is much less muscular as compared to the body of uterus and contains more connective tissue. During child birth, when the myometrium of body of uterus contracts, the myometrium of cervix dilates; consequently, the cervical canal becomes large enough for the fetal head to pass through.
3. Endocervix refers to the innermost mucosal layer of cervix in contrast to the endometrium of the body of uterus. Endocervix is not shed at the time of menstruation.
II Fallopian tubes
Each fallopian tube (also known as uterine tube) is approximately 10 cm in length and 8 mm in diameter. It has a medial or uterine end, which is attached to and opens into the uterus and a lateral end that opens into the peritoneal cavity near the ovary.
Parts. Each fallopian tube can be divided into four parts (Fig. 9.3-2):
1. Uterine or interstitial part is the most medial part which passes through the thick uterine wall.
2. Isthmus is the relatively narrow and thick-walled part, which is just next to the uterine part. It is about 2.5 cm in length.
3. Ampulla is the next thin-walled and dilated part of the uterine tube. It is the largest part (7 cm) of uterine tube.
4. Infundibulum refers to the funnel-shaped lateral end of the tube. It is prolonged into a number of finger-like processes known as fimbria. One fimbria is longer than rest of the fimbriae, and is attached to the outer pole of ovary.
Structure. Fallopian tubes consist of same three coats as of the uterus, viz. endometrium, myometrium and perimetrium.
• The uterine tubes convey ova, shed by the ovaries, to the uterus. Ova enter the tube at its fimbriated end.
• Secretions present in the tubes provide nutrition, oxygen and other requirements for ova and spermatozoa passing through the tube.
• Fertilization takes place in the ampulla, and the fertilized ovum travels towards the uterus through the tube.
III Vagina
• The vagina is a musculomembranous tube (about 8–10-cm long) located anterior to the rectum and posterior to the urethra and urinary bladder.
• Its upper end surrounds the lower part of the cervix and its lower end, i.e. vaginal orifice, opens into the vestibule of vagina (the cleft between the labia minora).
Female external genitalia
The external genital organs include mons pubis, labia majora, labia minora, clitoris, vestibule of vagina, bulbs of vestibule and greater vestibular glands (Fig. 9.3-1B).
The synonymous terms vulva and pudendum include all these parts. The vulva serves:
Ovaries
Functional anatomy
A pair of ovaries are located (one on each side) behind and below the fallopian tubes. The ovaries are ovoid glands with a combined weight of 10–20 gm during reproductive years, which decreases with increasing age. Each ovary is about 3–5 cm in length, and is attached to the uterus by the broad and round ligament of ovary.
Structure
Histologically, each ovary consists of following parts (Fig. 9.3-4).
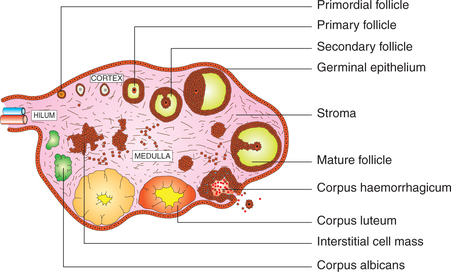
Fig. 9.3-4 Schematic diagram of the histology of ovary depicting various stages of development of follicles and corpus luteum.
1. Germinal epithelium. Germinal epithelium refers to the epithelium lining the outer surface of ovary and consists of a single layer of cuboidal cells. The term germinal epithelium is a misnomer, as it does not produce germ cells.
2. Cortex. The cortex is the outer thick main part of the substance of the ovary. It consists of following tissues:
• Tunica albuginea is the outer condensation of the connective tissue present immediately below the germinal epithelium.
• Stroma of the cortex, present deep to the tunica albuginea.
• Ovarian follicles at various stages of development are scattered in the stroma. Each follicle contains a developing ovum.
3. Medulla. The medulla is the inner small part of the substance of ovary. It consists of connective tissue in which numerous blood vessels (mostly veins), smooth muscles and elastic fibres are present.
4. Hilum. The hilum refers to the area where ovary attaches to mesentery. It is the site for entry of blood vessels and lymphatics.
Functions of ovaries
The two principal functions of ovaries are:
• Gametogenic function, i.e. oogenesis and
• Endocrine function, i.e. secretion of female hormones called ovarian hormones.
Oogenesis
Oogenesis refers to the process of formation of ova from the primitive germ cells.
Primitive germ cells. When the bipotential gonads differentiate into ovaries in genetic female (44 + XX) embryo by 10th week of gestation, the primitive germ cells increase in number by mitosis to form oogonia.
Oogonia are the stem cells from which ova are derived. The oogonia proliferate by mitosis to form primary oocytes.
Primary oocytes, formed from the oogonia, enter a prolonged prophase (diplotene stage) of the first meiotic division and remain in this state until ovulation occurs after puberty.
Primordial follicles. The diploid primary oocytes become enveloped by a single layer of flat granulosa cells and in this form are called primordial follicles.
• After puberty, the oogenesis or formation of ovum occurs in a highly cyclic fashion, once every 28 days till menopause.
• Every month, in each ovary, more than one primordial follicles start undergoing maturation process, but only one reaches maturity and the rest undergo atresia at different stages of development.
• The different stages of maturation of primordial follicle into graafian follicle (folliculogenesis).
Endocrine function of ovaries
The endocrine function of the ovaries is to produce female sex hormones which include:
Oestrogens
Oestrogens are (C-18) steroids. The naturally occurring oestrogens include:
• Oestradiol. It is the principal and physiologically most potent oestrogen. Ovarian oestradiol accounts for more than 90% of the circulating oestrogens.
• Oestrone. It is a weak ovarian oestrogen.
• Oestriol. It is the degradation product of oestradiol and oestrone. It is the weakest of all naturally occurring oestrogens.
Synthesis, plasma levels and transport of oestrogens
In the normal female, oestrogens are mainly secreted by theca interna and granulosa cells of the ovarian follicles. A small quantity is also produced by the adrenal cortex, breast, some areas of brain, placenta (during pregnancy) and by Sertoli cells (in males).
In a normal adult woman, the plasma levels of oestrogen varies in different phases of ovarian cycle (Fig. 9.3-5). As shown in Fig. 9.3-5-D, there are two peaks of oestrogen secretion. The first occurs just before the ovulation (12th–13th day of sexual cycle) and is called oestrogen surge, and the second peak occurs in the mid-luteal phase. The secretion rate of oestrogen in different phases is:
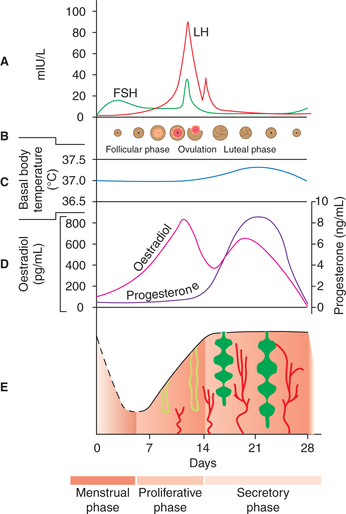
Fig. 9.3-5 Correlation of plasma concentration of gonadotropins (FSH and LH) (A); ovarian cycle changes (B); basal body temperature (C); ovarian hormones (D) and endometrial changes (E) during female sexual cycle.
After menopause, oestrogen level falls to minimum of 50 μg/day.
Metabolism and excretion of oestrogens
The liver is the main site for metabolism of ovarian hormones. The degradation metabolites are excreted by kidney into the urine and a small amount of them is secreted into the bile.
Functions of oestrogens
The functions of oestrogen for descriptive purposes can be grouped as reproductive actions and other actions.
A. At puberty. At puberty, oestradiol is secreted in larger amounts which cause following changes.
1. Growth and development of genital organs
(i) Ovaries increase in size and complete ovarian cycle starts.
(ii) Fallopian tubes become functional.
(iii) Uterus. It enlarges in size, endometrium gets thickened due to increase in stroma and blood flow. The rhythmic cyclic changes (proliferative and secretory) occur with onset of menstrual cycle.
(iv) Cervix also enlarges and with onset of menstrual cycle, endocervix undergoes cyclic changes (see page 448).
(v) Vagina increases in size. Its epithelial lining increases in height (from 2–3 layers cuboidal epithelium to 10–12 layers cornified squamous epithelium).
(vi) External genitalia. The following changes occur in external genitalia:
2. Appearance of secondary sex characters
Oestrogen is responsible for the appearance of secondary sex characters (see page 429).
B. In an adult woman. Oestrogens along with progesterone regulate the ovarian cycle, menstrual cycle and cyclic changes in the cervix, vagina and fallopian tubes (see page 447) in non-pregnant state.
• It plays an important role in the maintenance of pregnancy and then during parturition (see page 455).
The other functions of oestrogens include the effects on following:
(i) Oestradiol accelerates the linear growth of bones at puberty by its osteoblastic activity.
(ii) Oestradiol enlarges the hip and widens the inlet of the pelvic bone to facilitate child birth.
(i) Protein metabolism. Oestrogens cause positive nitrogen balance due to growth-promoting effect.
(ii) Fat metabolism. Oestrogens cause fat deposition in subcutaneous tissues, in the breasts and the thighs.
3. Water and electrolyte balance. Oestrogens like other steroids, in general, cause salt and water retention in the body and produce premenstrual tension in some women.
4. Effects on CNS. Oestrogens are responsible for oestrous behaviour in animals, and also increase the libido in human females.
5. Effects on skin. Oestrogens make the skin soft and more vascular. It makes the sebaceous glands, secretions thin. Therefore, synthetic oestrogens are used as a part of treatment in acne.
Progesterone
Progesterone is C-21 steroid meant for maintenance of pregnancy and is biologically called prostagen or gestagen.
Synthesis, plasma levels and transport of progesterone
In a normal adult non-pregnant woman progesterone is mainly secreted by corpus luteum and during pregnancy by the placenta. A small amount is also secreted by the adrenal cortex and by testes in case of males.
In a normal adult woman, the plasma levels of progesterone varies with different phases of sexual cycle (Fig. 9.3-5D).
In early follicular phase, plasma concentration of progesterone is very low (about 0.9 ng/mL or 9 ng/dL).
In midcycle (late follicular phase) its level starts rising due to secretion from the granulosa cells.
In luteal phase, it reaches to its peak value, i.e. 18 ng/mL.
At the end of cycle, its levels fall to its minimum value.
Note. Throughout the sexual cycle the levels of progesterone are higher than the oestrogens.
During pregnancy, the levels of progesterone further rise (see page 454).
After menopause, progesterone levels fall to its minimum (0.2 ng/mL) or even not detectable.
Metabolism and excretion of progesterone
Functions of progesterone
The physiological actions of progesterone can be grouped as reproductive actions and other actions.
Reproductive actions occur mainly on the reproductive organs primed by oestrogens, and these include the following.
1. Action on uterus. The progesterone is responsible for the secretory phase of the endometrial cycle and prepares the endometrium to receive the zygote. It decreases the uterine motility.
2. Endocervix. The cervical secretions become thick and viscid, and ferning pattern disappears.
3. Vagina. Vaginal epithelium becomes thickened, cornified and infiltrated with leucocytes.
4. Fallopian tubes. Progesterone increases the epithelial-cell secretions rich in nutritive materials to provide nutrition to shed ovum, incoming sperm or zygote, if fertilization occurs.
5. Breast. Progesterone causes lobular and alveolar growth of breast.
6. During pregnancy. The main function of progesterone is to maintain the pregnancy (see page 455).
The other systemic effects of progesterone are:
1. Thermogenic effect. Progesterone is known as a thermogenic steroid, which increases the basal body temperature by 0.5°C in post-ovulatory phase.
2. Effect on CNS. Progesterone alters the secretion and release of various neurotransmitters in the hypothalamus and other areas of the brain, and thereby decreases the appetite and produces somnolence.
3. Effect on respiration. Progesterone increases the sensitivity of the respiratory centre to carbon dioxide stimulation. Due to this fact the pACO2 is slightly less in woman during the luteal phase of sexual cycle.
Other ovarian hormones
Besides female sex steroids (oestrogen and progesterone), ovaries also secrete peptide hormones as follows.
1. Inhibin. Structurally it is polypeptide; it inhibits the FSH release.
2. Activin. Structurally, it is also a polypeptide, its action is to activate FSH secretion from the anterior pituitary.
3. Relaxin is a polypeptide hormone produced by corpus luteum, and other sites include uterus, placenta and mammary glands, and in males from the prostate gland. Its main role is during pregnancy as it relaxes pubic symphysis and pelvic joints, softens and dilates the uterine cervix, and facilitates delivery.
In non-pregnant state, it is released from the corpus luteum and endometrium during secretory phase; its function is not known.
In males, relaxin is present in the semen and helps in sperm motility.
4. Ovarian androgens. A small amount of testosterone is also secreted by the ovaries during biosynthesis of oestrogen and progesterone, but the main source of androgens in female is adrenal cortex.
These androgens are responsible for acne vulgaris, libido and pubic hair.
Female sexual cycle
With the onset of puberty the female sexual cycle starts, which repeats itself every 28 days. The occurrence of first menstrual cycle is called menarche. The permanent stoppage of menstrual cycle is called menopause, which occurs at the age of about 45–50 years. The period between menarche and menopause is called reproductive period. During this period, females have rhythmical sexual cycles.
Components of human female sexual cycle. During each female sexual cycle, rhythmical changes occur in ovaries and accessory sex organs—uterus, cervix and vagina.
Duration of female sexual cycle is usually 28 days. But under physiological conditions it may vary between 20 and 40 days. Traditionally first day of the menstrual bleeding is taken as the first day of female sexual cycle.
Ovarian cycle
Ovarian cycle refers to the rhythmic changes occurring in ovaries. During each cycle, a single mature ovum is released from the ovary. Ovarian changes occurring during the female sexual life completely depend on the gonadotropic hormones (FSH and LH), which are secreted by the anterior pituitary. The ovarian cycle can be divided into three phases:
Pre-Ovulatory phase
Pre-ovulatory or follicular phase of the ovarian cycle extends from the 5th day of the cycle till the time of ovulation (which takes place at about 14th day of the cycle). Thus, this phase generally lasts for 8–9 days (but may vary from 10–25 days).
• Changes in the ovary during this phase are mostly under the influence of FSH from the anterior pituitary. Luteinizing hormone also helps in the maturation of the follicle in the latter part of follicular phase (for details see hormonal control of female sexual cycle; see page 449).
• During this phase of each cycle, some 10–15 primordial follicles start maturing, but only one follicle matures fully and the rest undergo atresia (atrophy) at different stages of development. A fully matured graafian follicle is characterized by (Fig. 9.3-4) following features:
– Size of the follicle increases markedly to about 2–5 mm.
– Antrum becomes larger and distended with fluid. As a result the ovum covered by a layer of cells called corona radiata remains in contact with granulosa cells only at a hill like area called cumulus oophorus.
– Theca interna becomes more prominent.
– Formation of secondary oocyte. Just prior to ovulation, the primary oocyte of the fully matured graafian follicle completes the first meiotic division (which began in fetal life at about 20th, 28th week of gestation, i.e. before birth), and forms the secondary oocyte with a haploid nucleus and the first polar body.
Ovulation
Ovulation refers to the release of secondary oocyte from the ovary (following rupture of graafian follicle) into the peritoneal cavity. It usually occurs 14 days after the onset of menstruation (Fig. 9.3-5B).
Post-Ovulatory phase
Post-ovulatory phase, also called luteal phase of ovarian cycle, is of remarkably constant period of about 14 days. This phase is characterized by following events (Fig. 9.3-4).
Formation of corpus haemorrhagicum. Following ovulation, the outer wall of the graafian follicle collapses and promptly fills with blood forming the so-called corpus haemorrhagicum.
Formation of corpus luteum. Soon, the granulosa cells and theca cells of the follicle lining begin to proliferate, and the clotted blood is rapidly replaced with yellowish lipid-rich luteal cells. This process is called luteinization and the total mass of the cells is now called corpus luteum. LH is responsible for luteinization.
Formation of corpus albicans. If there is no fertilization and pregnancy does not occur, the corpus luteum begins to involute (regress) after 24th day of the sexual cycle, and is eventually replaced by a whitish scar tissue called the corpus albicans. This involution occurs due to falling levels of FSH and LH and also the hormone inhibin secreted by the lutein cells.
Corpus luteum of pregnancy. However, if the ovum released is fertilized and pregnancy occurs, then the corpus luteum formed during post-ovulatory phase persists and serves as the major source of oestrogen and progesterone till the third month of pregnancy when the placenta takes over its endocrine function.
Endometrial cycle
Endometrial cycle refers to the cyclic changes occurring in the endometrium during active reproductive period (menarche to menopause) in females leading to recurrent monthly bleeding per vaginum (menstruation). These cyclic changes in the endometrium are brought about by the cyclic production of oestrogens and progesterone by the ovaries.
Phases of endometrial cycle
The endometrial cycle of 28 days can be divided into three phases (Fig. 9.3-5E):
For the purpose of better understanding, the menstrual phase is described last of all.
Proliferative phase
Extent of proliferative phase of endometrial cycle is from day 6th to 14th day. It follows the phase of menstruation, after which only a thin basal layer of original endometrium is left.
Hormone responsible for the changes in the endometrium during this phase is oestrogen secreted by the developing graafian follicle in the ovary. Thus, proliferative phase of the endometrial cycle coincides with the follicular phase of ovarian cycle.
Changes in endometrium which occur during proliferative phase are:
Secretory phase
Extent of secretory phase (also known as post-ovulatory phase of endometrial cycle) is from day 15th–28th day.
Hormones responsible for changes in the endometrium during this phase are both oestrogen and progesterone secreted by the corpus luteum formed after ovulation. Thus, the secretory phase of endometrial cycle coincides with the luteal phase of ovarian cycle.
Changes in the endometrium which occur during this phase are:
• There is elongation and coiling of the endometrial mucous glands. These glands become secretory and secrete thick viscous fluid containing glycogen.
• Blood supply of endometrium further increases as progesterone promotes spiralling of blood vessels.
• Thickness of endometrium increases to 5–6 mm at the end of secretory phase. Thus the thickened endometrium with large amounts of nutrients is ready to provide appropriate conditions for implantation of ovum during this phase.
• If fertilization does not occur and there is no pregnancy, the corpus luteum in the ovary involutes to form corpus albicans, and on day 26th of the menstrual cycle the levels of oestrogen and progesterone fall suddenly and mark the end of secretory phase of endometrial cycle.
Menstrual phase
The menstrual phase of endometrial cycle is also called bleeding phase. The average duration of this phase is 3–5 days. About 24 h before the end of menstrual cycle, there is sharp decline in the plasma levels of oestrogen and progesterone, which are responsible for menstrual bleeding.
• Endometrial debris contains necrosed, sloughed-tissue, blood, serous fluid and large amounts of prostaglandins and fibrolysins.
• Average amount of blood loss during each menstrual cycle is 30 mL.
• Menstrual blood immediately gets clotted inside the uterine cavity but soon gets liquefied by fibrolysins present in the endometrial debris.
• During menstrual phase, about two-thirds of the superficial endometrium is sloughed off and only a thin basal layer (2 mm thick) is left behind.
Cyclic changes in cervix
The mucosal lining of cervix (endocervix) also shows certain cyclic changes during sexual cycle. These are as follows.
During menstruation phase the mucosa of cervix does not undergo desquamation (shedding off) like that of endometrium.
During proliferative phase (oestrogen phase), the secretions of the mucosal cells of endocervix become thin, watery and alkaline. At the time of ovulation, the cervical mucus is thinnest and its elasticity is maximum. It can be stretched like a long, thin elastic thread up to 8–12 cm (spinnbarkeit effect). The mucus also produces a characteristic fern-like pattern when a drop of mucus is spread on the glass slide and allowed to dry (Fern test).
This characteristic nature of cervical mucus favours the transport of sperms in the female genital tract, and makes the conditions favourable for fertilization.
During secretory phase, under the influence of progesterone, cervical secretions decrease in quantity and become thick, tenacious and cellular, and fern pattern is not seen. These changes make a plug and prevent the entry of sperm through cervical canal.
Cyclic changes in vagina
Vaginal epithelium undergoes following cyclic changes in the endometrial cycle:
In proliferative phase, vaginal epithelium becomes thickened (by adding up more and more layers of epithelium) and cornified.
In secretory phase, under the influence of progesterone, vaginal epithelium proliferates and gets infiltrated with leucocytes, and the vaginal secretions become thick and viscid.
Hormonal control of female sexual cycle
The hypothalamo–hypophyseal–gonadal axis regulates the cyclic changes occurring during the female sexual cycle. The role of each component of the axis is (Fig. 9.3-6).
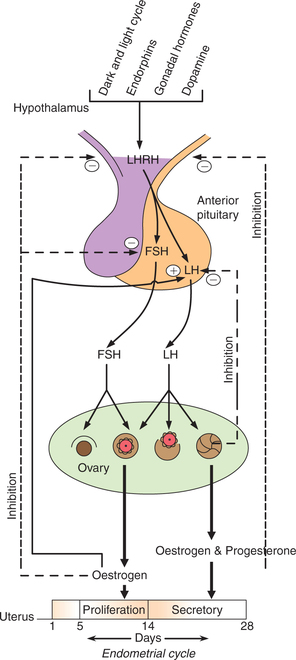
Fig. 9.3-6 Hypothalamo–hypophyseal–ovarian axis regulating the female sexual cycle through positive and negative feedback mechanisms.
Role of hypothalamus
Hypothalamus regulates the secretions of gonadotropins (both FSH and LH) through the gonadotropin-releasing hormone (GnRH). The gonadotropin-releasing hormone (GnRH) is also known as luteinizing hormone-releasing hormone (LHRH). It reaches the anterior pituitary through hypothalamo–hypophyseal portal system, where it is stored as small granules. It stimulates the anterior pituitary cells to release gonadotropins.
Role of anterior pituitary
The anterior pituitary plays its role in the female sexual cycle regulation by releasing gonadotropins (FSH and LH). Gonadotropins in turn regulate the ovarian cycle, i.e. formation of graafian follicles (folliculosis), ovulation and formation of corpus luteum.
Regulation of gonadotropins
The secretion of both FSH and LH is regulated by the following.
1. Gonadal hormones. The gonadal hormones (oestrogen and progesterone) regulate gonadotropin secretion by their feedback effect (Fig. 9.3-6).
• High levels of oestrogen and progesterone in mid-luteal phase inhibit the secretion of FSH and LH (by negative feedback effect).
• Low levels of gonadal hormones (during menstruation phase) increase the secretion of both FSH and LH (by positive feedback effect).
The feedback effect (positive or negative) of ovarian hormones is brought about by its action either directly on anterior pituitary or through the hypothalamus (Fig. 9.3-6).
2. Human chorionic gonadotropin (HCG). It is a glycoprotein secreted by syncytiotrophoblasts during early pregnancy (12–16 weeks of gestation). Like LH, HCG also maintains the functional state of corpus luteum, and thus elevates gonadal hormones resulting in inhibition of gonadotropin release.
3. Prolactin. It is a mammotropic hormone secreted from anterior pituitary during lactation. It inhibits GnRH release and thus lowers the basal secretion of FSH and LH (cause for lactation amenorrhoea).
4. Activin. It is structurally quite similar to inhibin (secreted from ovary). It is synthesized in the cells of the anterior pituitary. It stimulates the synthesis and release of FSH by autocrine and paracrine actions.
Role of ovaries
Ovaries play an important role in the regulation of ovarian cycle and endometrial cycle by secreting gonadal hormones (oestrogen and progesterone).
Oestrogen
In each sexual cycle, the plasma concentration of oestrogen starts rising from first day of the cycle and reaches to its peak just before ovulation (at 12–13th day) called oestrogen surge.
Progesterone
• In the luteal phase of ovarian cycle levels of both oestrogen and progesterone are high, but progesterone rises markedly.
• Progesterone prepares the oestrogen-primed endometrium for implantation. Thus, it is responsible for the secretory phase of endometrial cycle.
If fertilization does not occur the corpus luteum involutes, and levels of oestrogen and progesterone decline.
Withdrawal of hormones support results in menstruation, and at the same time negative feedback effect on anterior pituitary and hypothalamus is also abolished leading to further increase in gonadotropin, and next ovarian and endometrial cycle starts.
If fertilization occurs then HCG level rises, which maintains corpus luteum. Therefore, the levels of oestrogen and progesterone remain high, and by negative feedback effect gonadotropin levels (FSH and LH) remain low.
 Primary sex organs
Primary sex organs Functional anatomy
Functional anatomy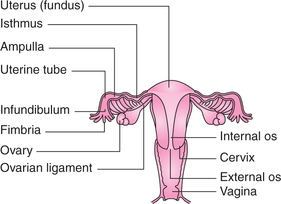
 Important note
Important note